- 1Department of Psychiatry, College of Medicine and Health Science, University of Gondar, Gondar, Ethiopia
- 2Department of Psychiatry College of Medicine and Health Science, Wollo University, Dessie, Ethiopia
- 3Department of Nursing, College of Medicine and Health Science, Arsi University, Asella, Ethiopia
- 4Department of General Midwifery, College of Medicine and Health Science, University of Gondar, Gondar, Ethiopia
- 5Department of Reproductive Health, Institute of Public Health, College of Medicine and Health Science, University of Gondar, Gondar, Ethiopia
- 6Department of Internal Medicine, University of Gondar College of Medicine and Health Science, Comprehensive Specialized Hospital, Gondar, Ethiopia
Background: The number of people who have been displaced from their homes due to violence, conflict, and natural disasters. The displaced persons are vulnerable to PTSD; however, being women, individuals with lower socio-economic status and intense exposure to physical assault are more vulnerable. The reviews stated that the pooled prevalence of PTSD among refugees in high-income countries was higher than the general population. However, there has been no review done on PTSD among displaced persons in Africa. Therefore, the aim of this review was to summarise the most recent data evidence on the pooled prevalence of posttraumatic stress disorder and the pooled effect of associated factors on adult displaced people in Africa.
Methods: We used an appropriate guideline for systematic reviews and meta-analyses reports, which is the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). This review protocol was registered in PROSPERO (CRD42023411371). The publications were identified from PubMed/Medline, EMBASE, the Cochrane Library, Scopus databases, and other grey searches of Google Scholar and World Health Organisation (WHO) reports. The data was extracted in Microsoft Excel, and then it will be imported into STATA 11.0 for analysis.
Results: We have included 10 studies conducted in African countries with 5287 study participants. In this meta-analysis, the pooled prevalence of PTSD among displaced people in Africa was 55.64 (95% CI: 42.76–68.41%). Further, in subgroup analysis regarding the study participants, the pooled prevalence of PTSD among internally displaced people and refugees was 56.35% and 54.04%, respectively. Among the associated factors, being female, unemployed, and depression were significantly related to PTSD among displaced people.
Conclusions: In this review, the pooled prevalence of PTSD among displaced people in Africa was high. Demographic characteristics (female, single, and unemployed), substance use disorder, and depression were risk factors for PTSD among displaced people. This finding might help the stakeholders (mental health policy makers, administrators, and mental health professionals) to address the prevention, early screening, and management of PTSD among displaced people and to give attention to more vulnerable bodies.
Systematic review registration: PROSPERO, identifier CRD42023411371.
Introduction
The number of people who have been displaced from their homes due to violence, conflict, and natural disasters. In general, displaced people can be classified as migrants, refugees, or asylum seekers, as well as internally displaced persons (IDPs) (1). People who are compelled to leave their native country due to conflict, war, persecution, violations of human rights, and economic and political crises are known as refugees (2–4). Whereas, internally displaced persons (IDPs) are groups of people who have been compelled to leave their homes or residences due to an armed conflict, widespread violence, human rights abuses, or natural or man-made disasters but have stayed within the borders of their own country (5, 6).
The United Nations Human Rights Commission (UNHRC) estimates that almost 80 million people were ejected from their homes forcibly (7). They were divided into three groups: 45.7 million internally displaced people, 29.6 million externally displaced people, and 4.2 million people seeking asylum. The number of people who have been forcibly displaced has increased by 75% globally during the past two decades (8). The number of refugees has significantly increased in recent years (9), with 22.55 million refugees reported worldwide (10). According to GRID, there were around 40 million internally displaced individuals as a result of conflict (11), while additional sources indicated that there were 55 million internally displaced individuals globally, of which more than 87.2% were uprooted due to conflict and violence and 12.8% were uprooted owing to natural catastrophes (12).
The majority of displaced individuals are found in developing nations (13, 14). There are 12.6 million displaced people in Africa as a result of conflict, and sub-Saharan Africa is home to more than 26% of the world’s refugee population (13). 11.8 million people were internally displaced due to conflict and violence in Sub-Saharan Africa, according to the Global Report on Internal Displacement (GRID) (15). Ethiopia had 3.2 million IDPs in 2019, which is the second-highest figure in Africa behind the Democratic Republic of the Congo, which had more than 5 million IDPs in 2019 (16). According to a UNHCR report, 42% of all IDPs worldwide lived in Africa. Nearly 12.6 million individuals were internally displaced in Africa as a result of conflict in 2016 (17).
Displaced persons are more susceptible to traumatic incidents such as physical or sexual assault, torture, threats of death, murder, the death of loved ones, and economic losses (18–21). Generally inadequate recompense for basic human needs and the breakdown of the public order (22) may alter their biopsychosocial domains (23, 24), and they can affect the biopsychosocial domains (23), which can result in post-traumatic stress disorder (25–27).
Post-Traumatic Stress Disorder (PTSD) is holding attention as a mental disorder after observations of battle fatigue, shell shock, and soldiers’ hearts in both World Wars I and II (28). PTSD is marked by increased stress and anxiety following exposure to a traumatic or stressful event, which may be a man-made or natural disaster. Exposure to a traumatic event might mean directly experiencing, witnessing, and learning that the traumatic event(s) occurred to a close family member. As a result, traumatised individuals manifest intrusive distress (memories or dreams) and flashbacks of the traumatic event(s), and then they try to avoid being reminded, persistent avoidance of stimuli, and negative alterations in cognitions and mood associated with the traumatic event(s) (28–34).
As the World Health Organisation’s (WHO) mental health surveys report, the lifetime prevalence of PTSD ranged from 3.9% to 5.6% (35), and in the United States of America (USA), it was 7% to 8% (34). The prevalence of trauma exposure and PTSD in low-income countries was 76% and 11.2%, respectively (36). The displaced persons are vulnerable to PTSD; however, being women, individuals with lower socio-economic status and intense exposure to assault are more vulnerable (28).
The reviews stated that the pooled prevalence of PTSD among refugees in high-income countries or Western countries was higher than the general population (37–39), 29% and 37% for diagnosed and self-reported PTSD, respectively (40), and another review reported that 8% to 37.2% (41). However, there has been no review done on PTSD among displaced persons or separately among refugees and internally displaced persons in Africa. Indeed, the PTSD status of displaced persons has been the topic of a large number of studies, with a large variation in reported prevalence rates from 18.4% (42) to 78% (15).
A systematic review in high-income counties indicates a challenging and persisting disease burden in refugees due to anxiety, mood disorders, and PTSD (40). PTSD in refugees is leading to adverse effects on their children’s mental health due to harsh parenting styles (43). In addition, PTSD, if left untreated, may often complicate other adverse mental health outcomes, presenting as comorbid depression, anxiety, and substance abuse disorders (28, 34, 44). Other reviews revealed that there are limited practices regarding assessment (45) and treating trauma-exposed people (46).
Identifying risk factors and the pooled prevalence of PTSD among displaced persons could help health care professionals and policymakers plan health promotion, prevention, and early intervention programmes (47, 48). However, per our search, there has been no systematic review or meta-analysis of the epidemiology of PTSD among displaced people in Africa. The aim of this systematic review and meta-analysis is to summarise the most recent data on adult displaced persons in Africa from January 2000 to April 2023, covering the first quarter of the twenty-first century, in order to fill up this research vacuum by providing answers to the following questions:
1. What is the pooled prevalence of PTSD among displaced people?
2. What are the factors associated with PTSD among displaced people?
Methods and materials
Design
The publications were searched by PubMed/Medline, EMBASE, Cochrane Library, Scopus, HINARI, PsycINFO, African Journals Online (AJOL), and other grey publications were searched by Google Scholar and World Health Organisation (WHO) reports. The following search items (Mesh) were used (“prevalence” OR “epidemiology” AND “post-traumatic stress disorder” OR “PTSD” AND “associated factors” OR “risk factors” OR “determinants” AND “displaced people” OR “refugees” OR “internal displaced people” AND “Africa”) (Supplementary File 1). The data was extracted from articles. Research reports were included from January 2000 to April 2023, and the studies were evaluated for their eligibility, and then they were included in the meta-analysis using prepared eligibility assessment criteria. We used an appropriate guideline for systematic reviews and meta-analyses reports, which is the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (49) (Supplementary File 2). This review protocol was registered in PROSPERO (CRD42023411371).
Eligibility criteria
The studies meeting the following criteria were part of this systematic review and meta-analysis: the studies conducted in African countries and all relevant observational studies (cross-sectional, cohort, and case-control studies). And also, adults (>=18 years old), published in English or having an English translation, published and unpublished articles were considered. Searching was performed from February 2023 to April 2023, and articles available online from January 2000 to April 2023 were considered. But studies that could not be fully accessed (conference abstracts) after a request was made from their author by email were excluded from the study because we were unable to assess the quality of each article in the absence of full reports.
Based on inclusion criteria, we first screened titles and abstracts of articles retrieved from the initial search, and then, following the selection of pertinent research, the entire text was examined. As seen in Figure 1, we did not include any articles with no interesting variables in our study.
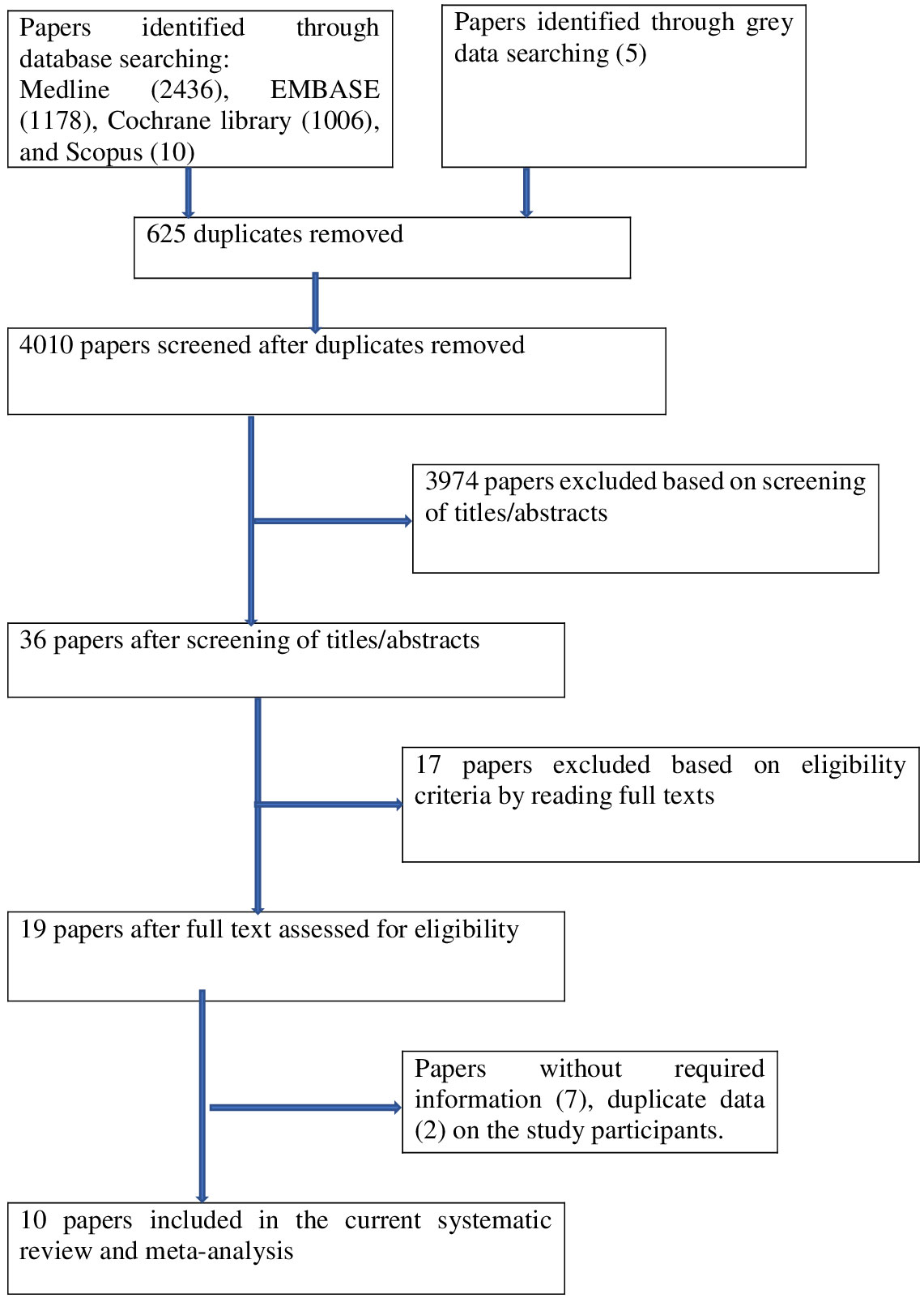
Figure 1 PRISMA flowchart of review search on the prevalence and associated factors of PTSD among displaced people.
Data extraction
MM and GM independently extracted all the necessary data from the articles using a standardised data extraction format. The data extraction format included the following items: the first author’s name, publication year, country where the study was conducted, a screening tool used to examine PTSD, number of participants, prevalence of PTSD, and associated factors with PTSD. The data extraction format was in the form of a two-by-two table. A cross-check was done by MM and GM following searches. If contrasting results occurred between the two authors during data extraction, they were discussing ways to achieve consensus and double extraction with other authors. We have done a sensitivity analysis to assess the robustness of the meta-analytic results.
Tools and validity
Among the ten papers reporting estimates of the prevalence of PTSD were:
1. Three were assessed using the Harvard trauma questionnaire (HTQ) (49) designed by the Harvard Programme in Refugee Trauma at Massachusetts General Hospital for the diagnosis of symptomatic PTSD. The PTSD section consists of 16 questions based on the diagnostic criteria of the Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition (DSM-IV) (50), but all of them were measured at different cut-off points.
2. Two papers were assessed using the Post-Traumatic Stress Disorder Checklist for DSM-5 (PCL-5). The PCL-5 is a standardised instrument and a self-report rating scale for assessing the 20 DSM-5 symptoms of PTSD (51). A total score was computed by adding the 20 items, so that possible scores range from 0 to 80 with a 5-point Likert scale (0–4) with a cut-off point of >=33 (51). The validity and reliability of the PCL-5 have been tested and proven on displaced people and refugees in a number of countries, for example, Iraq (Cronbach’s alpha =0.85) (52) and Zimbabwe (Cronbach’s alpha =0.92) (53).
3. The International Neuropsychiatric Interview 7 (MINI-7). The MINI is a short, structured diagnostic interview compatible with the Diagnostic and Statistical Manual of Mental Disorders 5. It was designed for clinical practice, research in psychiatric primary care settings, and epidemiological surveys (54, 55). The MINI was chosen based on the validity and reliability demonstrated in different populations in Brazil and Japan (56, 57).
4. The Impact of Event Scale-6 (IES-6) measures the level of exposure to traumatic events (58). The questions were measured on a four-point severity scale of 0–4, with a total maximum score of 24. Scores for each respondent were summed up, and individuals with a total score of 10 were considered symptomatic for PTSD.
5. The Impact of Event Scale-Revised (IES-R) (59) is a 22-item self-report measure that assesses subjective distress arising from traumatic events and experiences. The 22 items are rated on a 5-point scale (0 -4). A cut-off score of >=33 was used to identify PTSD (60).
6. The primary care PTSD screen (PC-PTSD) is a four-item screening instrument that was designed for use in primary care and other settings and is currently used to screen for PTSD. It includes an introductory sentence to alert respondents to traumatic events. The results of the PC-PTSD should be considered “positive” if a patient answers “yes” to any three items (61).
7. The National Stressful Events Survey PTSD Short Scale (NSESSS) was used.
Quality appraisal
The quality of the research reports included in this review was assessed using the Joanna Briggs Institute (JBI) for cross-sectional study quality assessment (62). For this quality assessment tool, it included the following components: the methodological quality of the study, comparability of included studies, and quality of original articles with respect to statistical analysis. All authors independently evaluated the quality of the original research using JBI. The tool has a total of 9 scores, and articles with medium and high quality (articles that score 5 and above out of a 9-point scale) were included in this review for analysis. If there were any discrepancies between authors during the quality assessment of the included studies, they were solved by taking the average of each author.
Data processing and analysis
The data was extracted in Microsoft Excel, and then it was imported into STATA 11.0 for analysis. The original studies were shown by using texts, tables, and forest plots. The standard error of prevalence for each primary or original study was analysed using the binomial distribution. The prevalence of the original studies was checked for heterogeneity using a heterogeneity I2 test (63). We used a random-effects meta-analysis model to estimate Der Simonian and Laird’s pooled effect of PTSD. And we made a leave-one-out sensitivity analysis to identify the possible source of heterogeneity in the pooled meta-analysis of the prevalence of PTSD among displaced people in African countries. Publication bias was detected using funnel plot analysis and Egger-weighted regression tests. A p value of less than 5% significance in the Egger test was considered to have statistically significant publication bias (64, 65). Subgroup analyses were carried out to determine if there was any heterogeneity in the results. Predictors of heterogeneity were: study country, year of publication, study participants (whether internal displaced people or refugees), assessment tool of PTSD, type of study design, number of study participants, prevalence of PTSD among participants, females’ prevalence of PTSD among the participants, and methodological quality.
Results
Study identification
There were 4630 publications identified in database searches, and another 5 records were added through grey searches. Among them, 625 papers were removed due to duplicates; 3974 papers were excluded based on screening of titles or abstracts; 17 papers were excluded based on eligibility criteria by reading full texts; and 9 papers were excluded due to (without required information) 7 and duplicate data 2. Finally, a total of 10 studies were involved in this systematic review and meta-analysis (Figure 1).
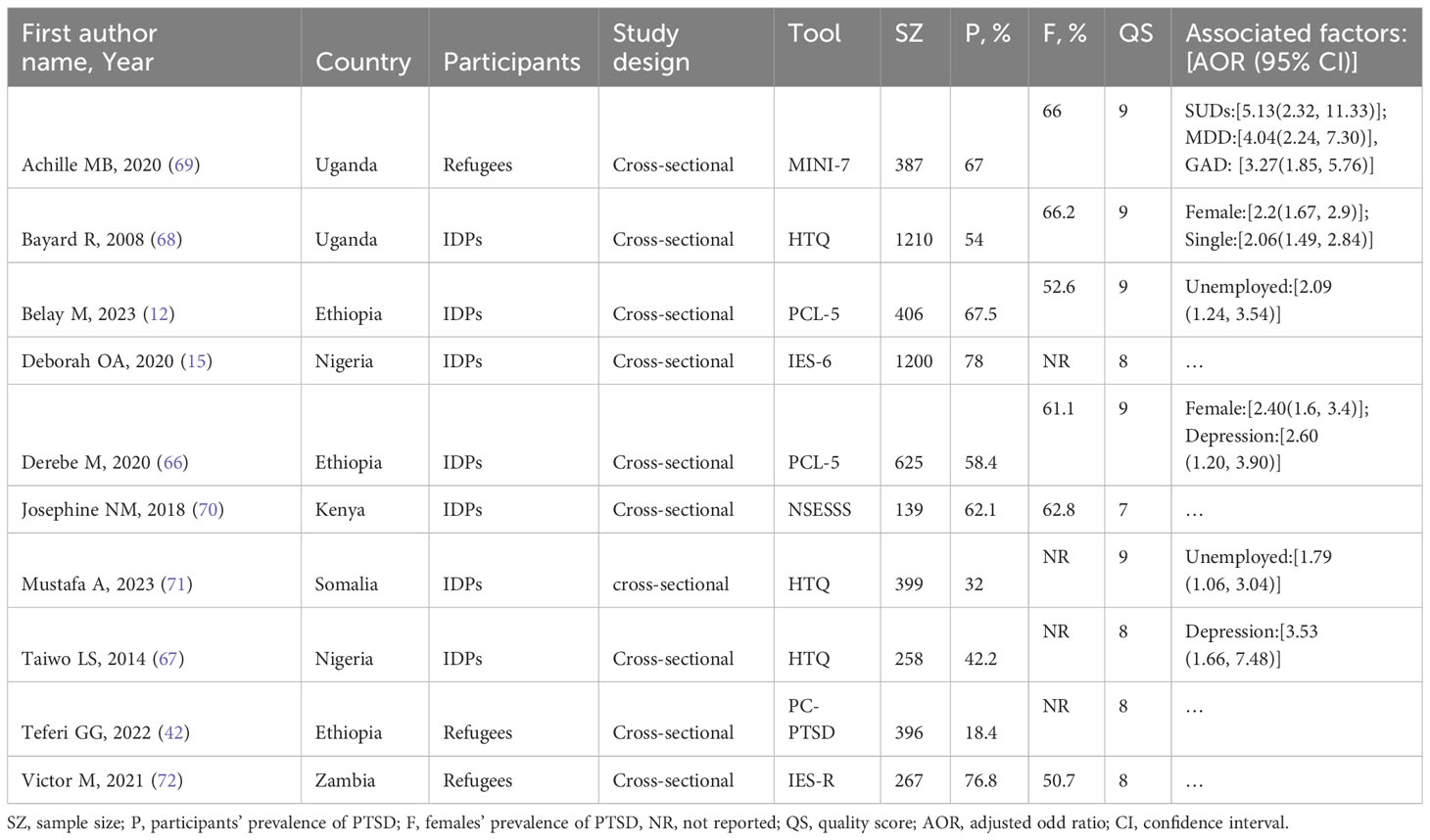
Characteristics of included studies
A total of 10 studies conducted in African countries, including 5287 study participants, were included in the current review. Among the 10 studies included, three were from Ethiopia (12, 42, 66), two from Nigeria (15, 67) and Uganda (68, 69), and one from Kenya (70), Somalia (71), and Zambia (72). Regarding the study design of the included studies, ten of them were cross-sectional study designs. PTSD was assessed by HQT in three studies, PCL-5 in two studies, and each of NSESSS, MINI-7, IES-6, PC-PTSD, and IES-R in one study (Table 1).
Study quality appraisals
The Joanna Briggs Institute (JBI) was used to assess the quality of the studies. All the studies involved in this review have good quality (JBI score >6) (Supplementary File 3).
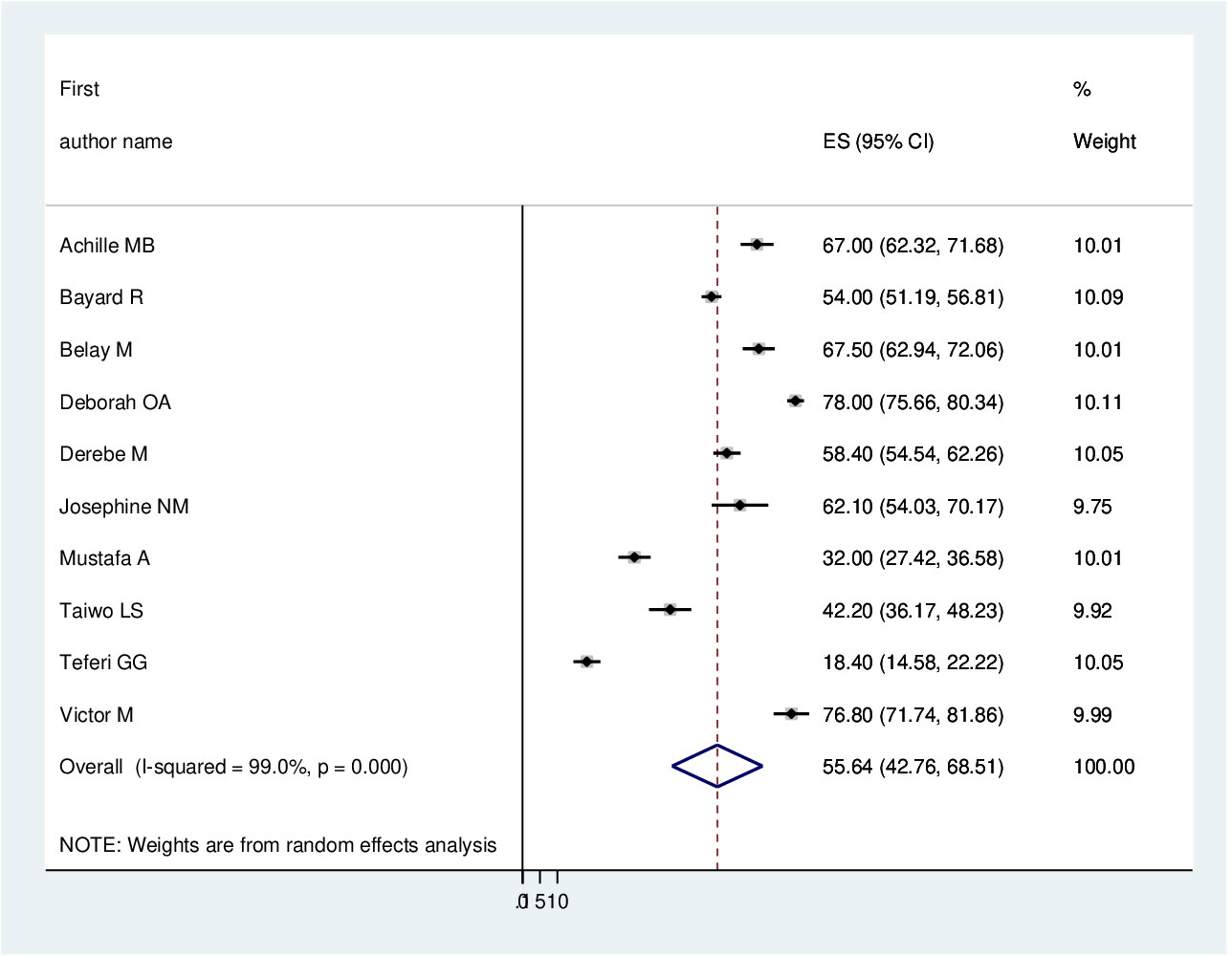
Meta- analysis
The pooled prevalence of PTSD among displaced people in Africa was 55.64 (95% CI: 42.76–68.41%) (Figure 2). Due to apparent heterogeneity across the studies, we have used a random effect model while conducting a meta-analysis (I2 = 99%, p < 0.001).
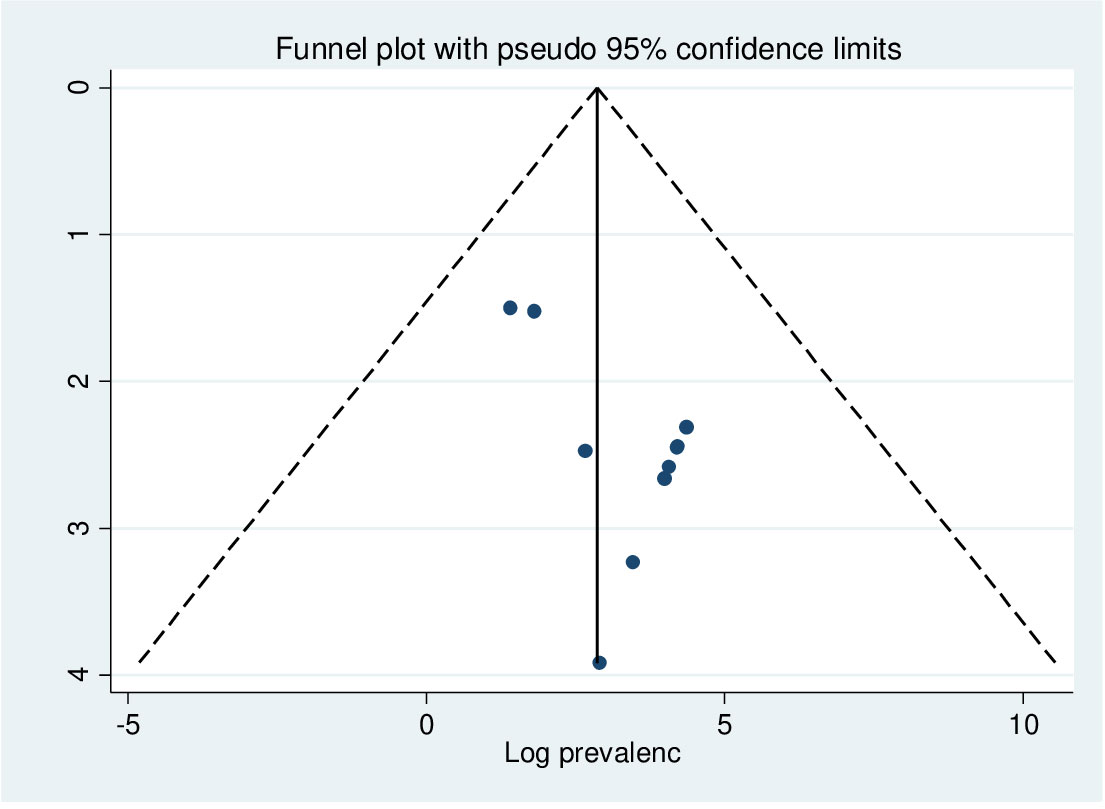
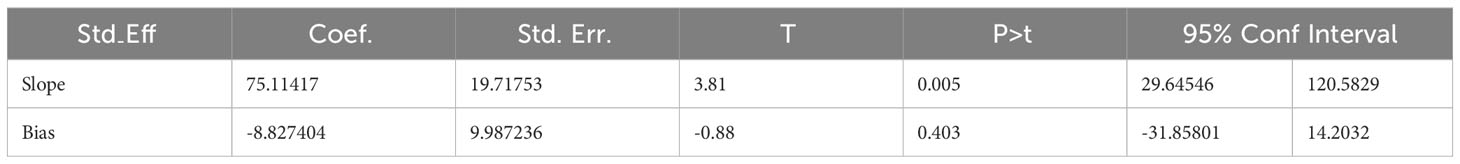
Publication bias
In this study, as shown in Figure 3, a funnel plot was symmetrical, which indicates the absence of publication bias, and Egger’s regression test (P = 0.403) strengthened it (Table 2).
Subgroup analysis
As previously discussed, the presence of heterogeneity was confirmed, and as a result, subgroup analysis was conducted based on the study country, type of participants, and assessment tool. A higher pooled prevalence of PTSD was found among studies conducted in Uganda (60.36%, I2 = 95.4%, p ≤0.001), Nigeria (60.21%, I2 = 99.2%, p ≤0.001), and Ethiopia (48.08%, I2 = 99.4%, p ≤0.001). Regarding the study participants, the pooled prevalence of PTSD among IDPs and refugees was 56.35% (I2 = 98.6%, p ≤0.001) and 54.04% (I2 = 99.5%, p ≤0.001), respectively. In addition, the pooled prevalence of PTSD on the assessment tool was 42.82% (I2 = 97%, p ≤0.001) for HTQ and 62.87% (I2 = 88.87%, p ≤0.001) for PCL-5. Therefore, this result showed there is high heterogeneity among subgroup analyses, as indicated by I2 (88.8 and above), which indicates the need to conduct the sensitivity test (P ≤0.003) (Figures 4–6).
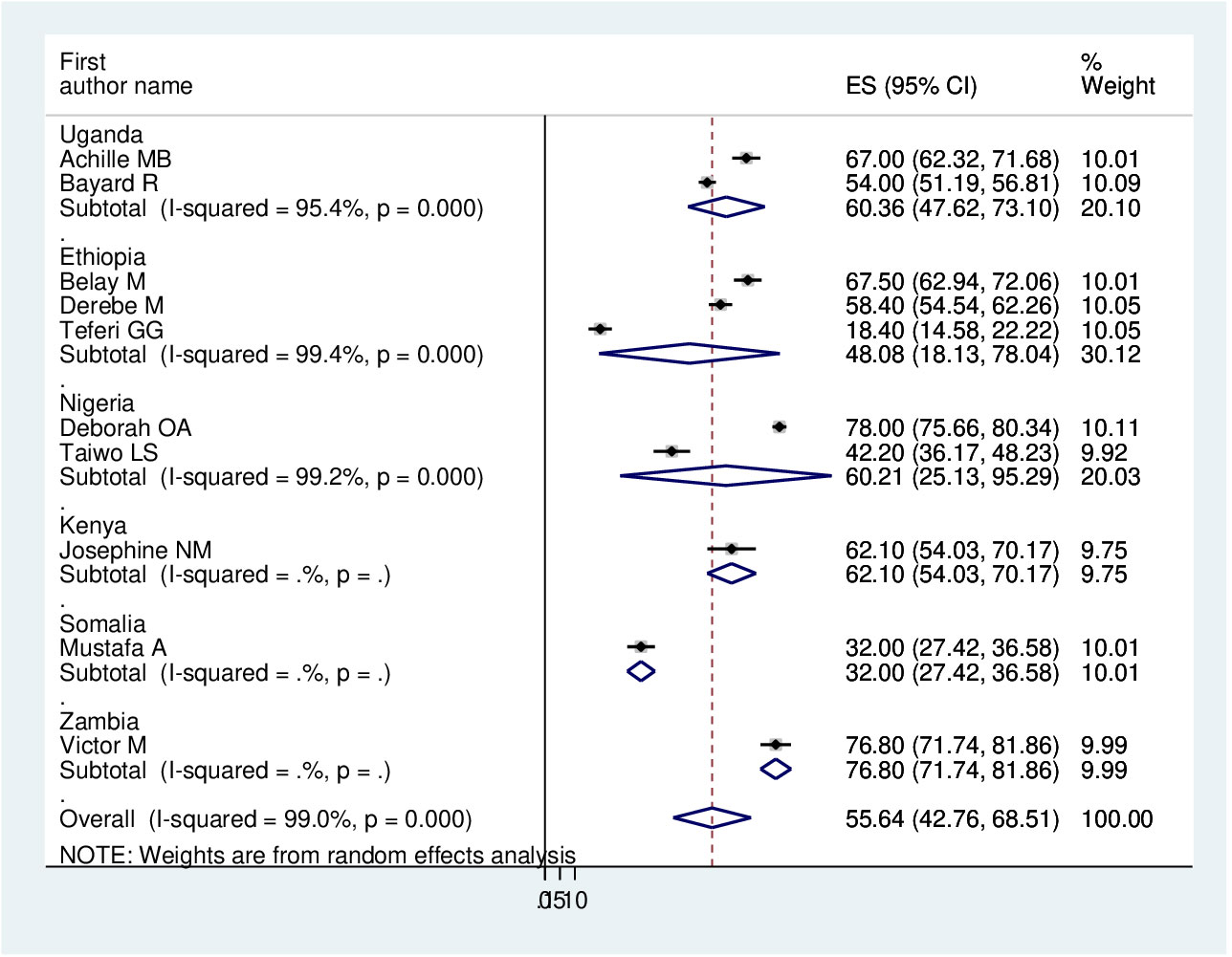
Figure 4 Forest plot on subgroup analysis by study country of the pooled prevalence of PTSD among displaced people in Africa.
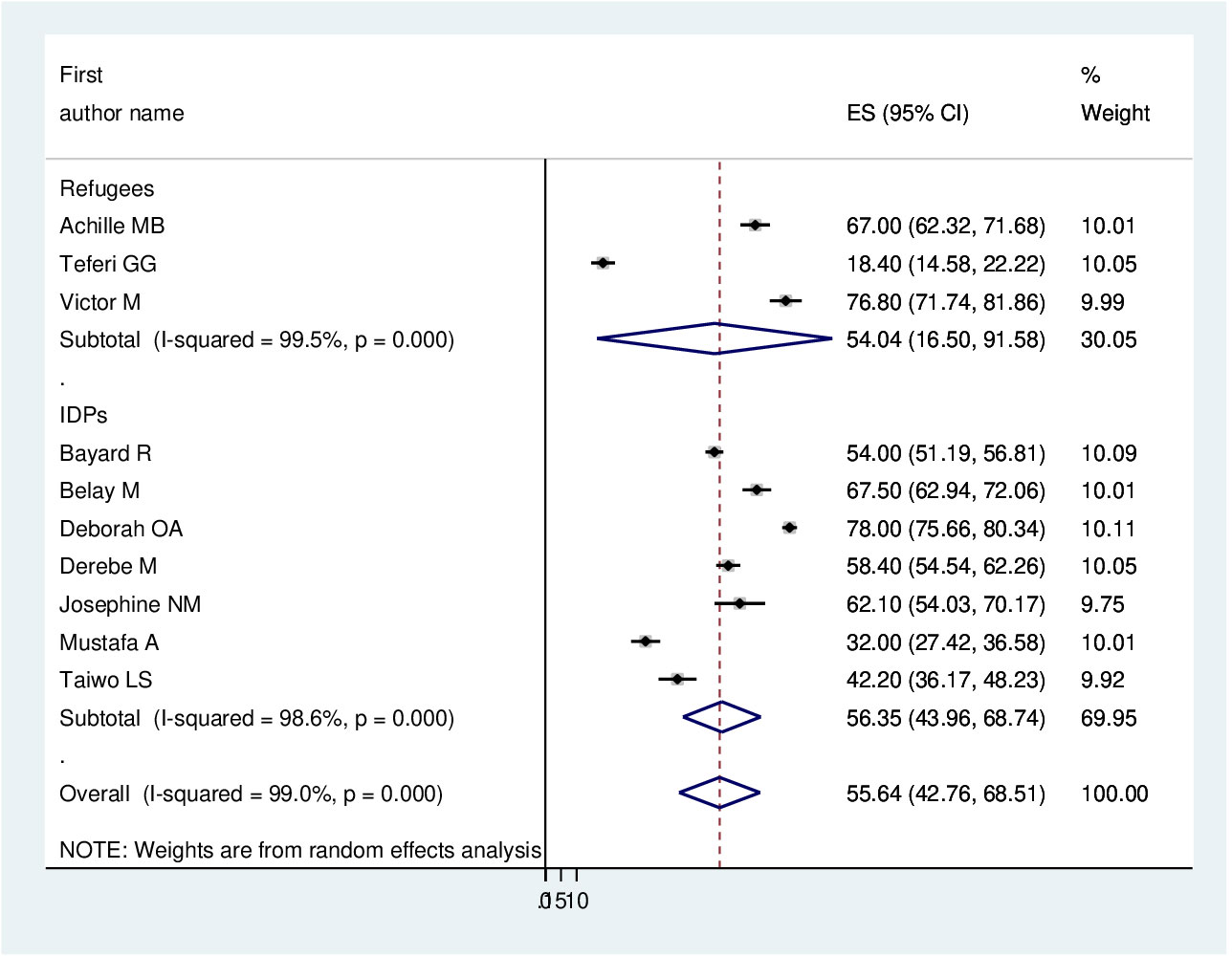
Figure 5 Forest plot on subgroup analysis by type of participants of the pooled prevalence of PTSD among displaced people in Africa.
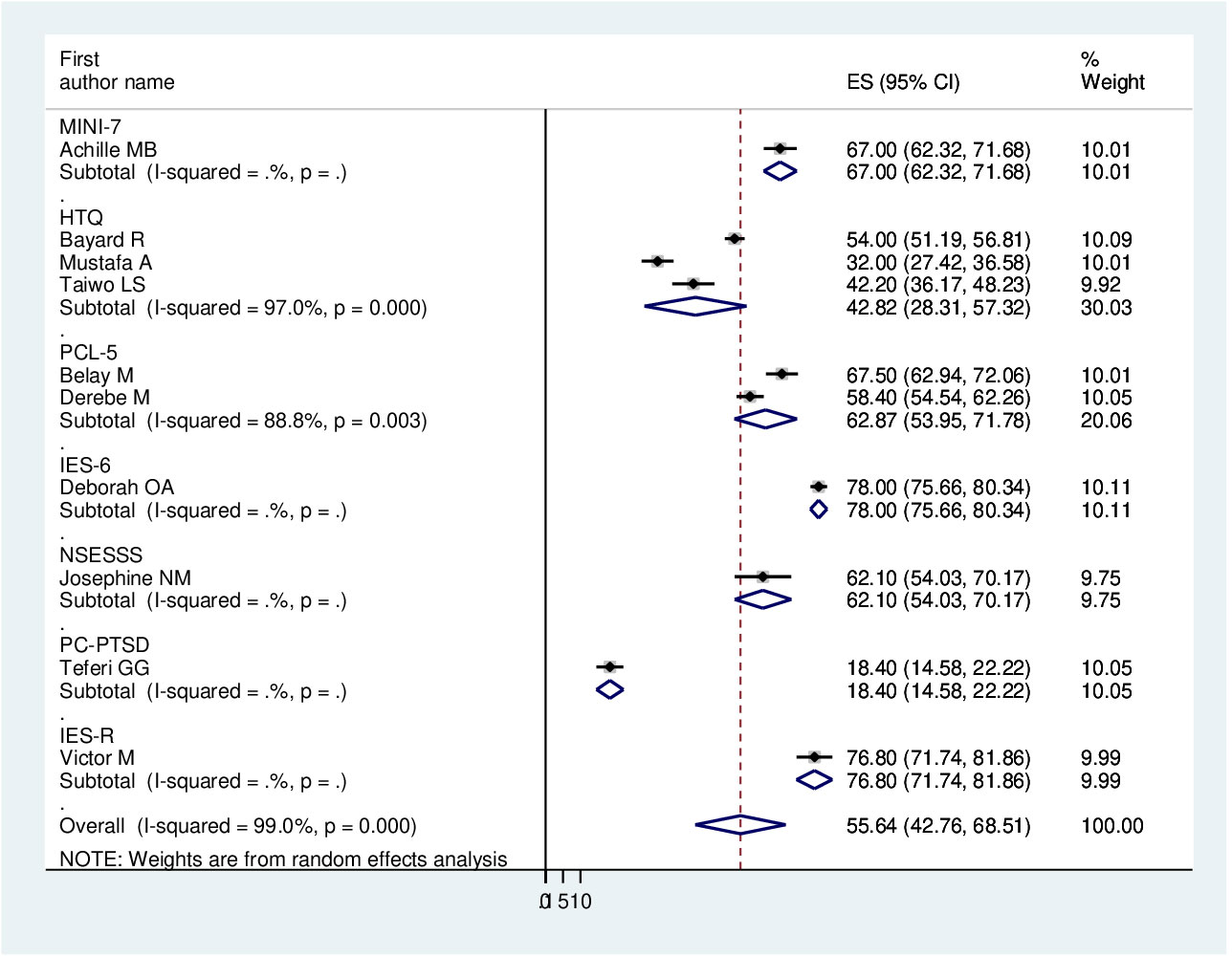
Figure 6 Forest plot on subgroup analysis by assessment tool of the pooled prevalence of PTSD among displaced people in Africa.
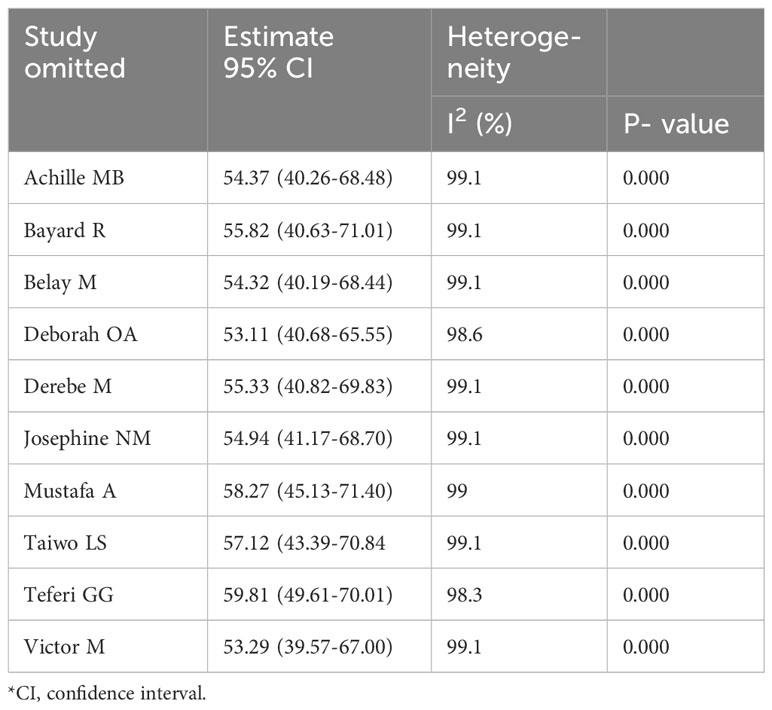
A leave-out-one sensitivity analysis
The sensitivity analysis was done to check the heterogeneity of those studies by omitting one author or one study step by step to check the effect of each study on the overall prevalence of PTSD in this review. As evidenced by the results, all the values are within the estimated 95% CI, which indicates the omission of a single study had no significant difference in the prevalence of this systematic review and meta-analysis (Table 3).
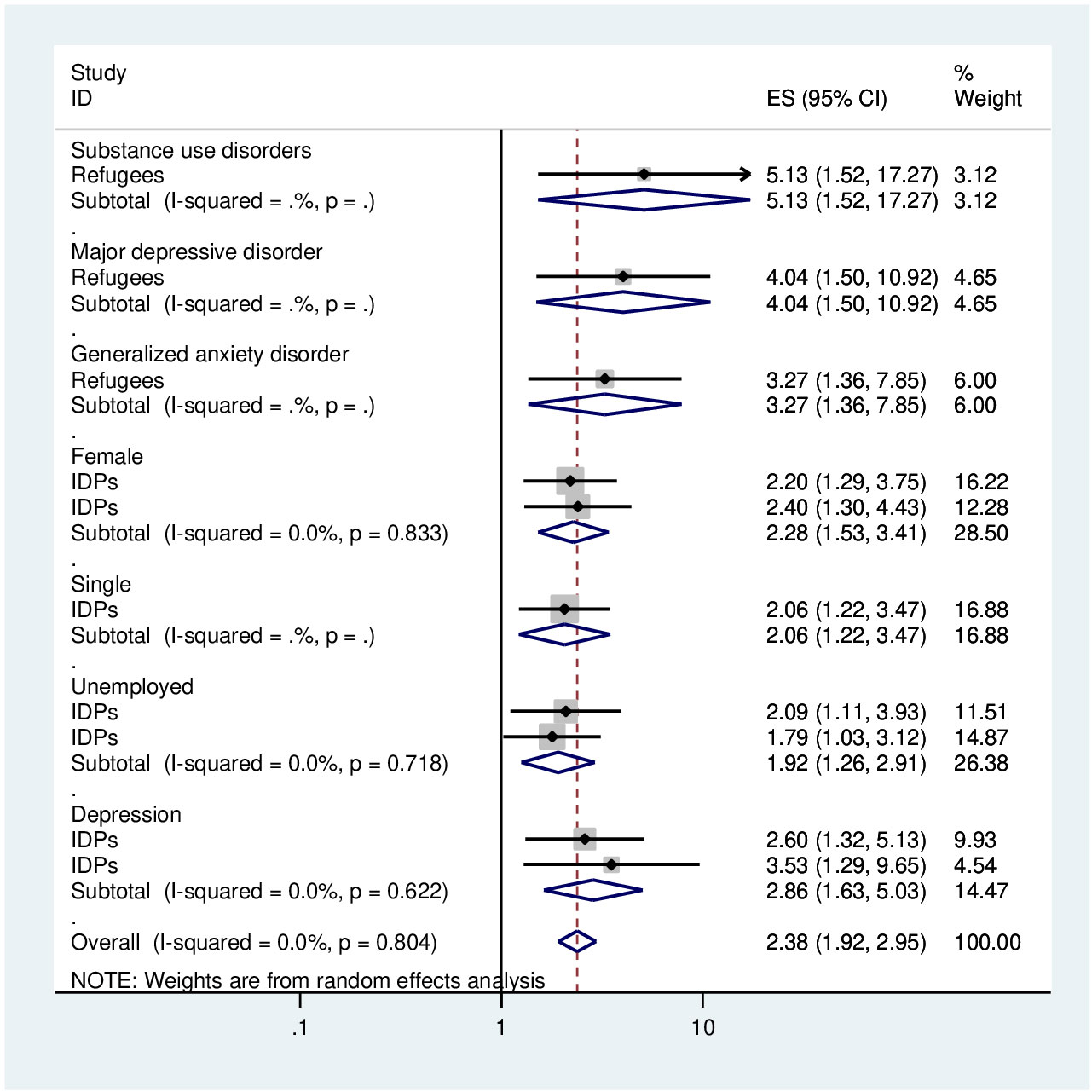
Associated factors analysis
Table 1 presents the significant variables linked to post-traumatic stress disorder (PTSD) in adult African-displaced individuals, based on individual studies assessed using logistic regression and an adjusted odd ratio. Significant variables related to PTSD in Africa have been described in this section. In terms of demographic characteristics, being female (AOR = 2.28, 95% CI: 1.53–3.41) and being unemployed (AOR = 1.92, 95% CI: 1.26-2.91) with two previous studies and within this review were significantly associated with PTSD. Regarding clinical factors, depression (AOR = 3.18, 95% CI: 2.05–4.95) with two previous studies and within the current study was significantly linked with PTSD (Figure 7). These results were obtained from the pooled analysis for these factors and in cases where two or more publications were present.
Discussions
This systematic review and meta-analysis synthesised 10 studies investigating the prevalence and associated factors of PTSD among 5287 displaced people in Africa, of whom 2942 had been screened for PTSD. In this review, the pooled prevalence of PTSD among displaced people in Africa was 55.64 (95% CI: 42.76–68.41%). This result was in line with the study done among refugees in Germany (73) and among resettled Afghan refugees in Australia (47). However, it was higher than the study conducted in Ethiopia (74), in African countries (75), in Western countries (38, 40, 41), in the World Mental Health Survey (76), and in the Global Burden of PTSD (77). This gap might be related to the differences in study participants’ residency, type of participants, sample size, study design, and assessment tool.
This review covered six countries, but 13 studies in Ethiopia (74) with 5874 adult research participants were included. Eleven publications using a sample size of 7078 survivors of traffic accidents were included in a systematic review and meta-analysis conducted in Africa (75). Cross-sectional, longitudinal, and case-control research designs were included. On the other hand, this study used cross-sectional study methods and included studies on refugees and internally displaced people. According to the review, there were 25 surveys conducted with 3936 respondents about refugees and asylum seekers in Germany (38) and 66 publications with 14,882 respondents about refugees in high-income countries (40). However, this review’s participants were IDPs and refugees living in African nations. Another review revealed that six studies with a sample size of 1,912 participants were conducted among Iraqi refugees living in western countries (41). The instruments utilised to assess the participants’ PTSD—PCL-M, PC-PTSD, CAPS, CIDI, HTQ, and DSM-IV—were employed. The World Mental Health Survey indicates that 18 surveys, including 661 respondents, were conducted for disaster-related PTSD. The instruments employed in these surveys were CIDI, DSM-IV, and the Structured Clinical Interview for DSM-IV (SCID) (76). Using the PSS-I, CIDI, MINI, SIQ, and CAPS tools, 22 surveys with 15,420 adult participants in war zones indicated the worldwide burden of PTSD (77). In contrast, the MINI-7, HTQ, PCL-5, IES-6, NSESSS, and PC-PTSD were the instruments utilised in this review. As expressed under the validity of tool assessment, NSESSS has no more explanation about the number of items, cut-off points, or its sensitivity and specificity. So, it could result in differences in screening for PTSD regarding the assessment tool. In other aspects, this result was greater and in line with the findings from Earth Quick Survivors (range: 4.10–67.07%) that were reported (78). The meta-analysis was conducted to determine adult survivors’ PTSD connected to earthquakes. 56,722 people participated in the study, which comprised 37 papers, and different instruments were employed.
In this study, regarding subgroup analysis, the pooled estimate of PTSD among displaced people was higher in Uganda (60.36%, 95% CI: 47.62–73.1%) and Nigeria (60.21%, 95% CI: 25.13–95.29%) compared with Ethiopia (48.08%, 95% CI: 18.13–78.08%). The possible explanation could be the difference between the assessment tool and the sample size. Further, we have used the type of study participants; the pooled prevalence of PTSD among IDPs and refugees was very similar (56.35%, 95% CI: 43.96–68.74%) and (54.04%, 95% CI: 16.5–91.58%), respectively.
Our review identified that being female and unemployed were significantly associated with PTSD among displaced people. Among the psychosocial factors of PTSD are being female and unemployed (28–30). This result was that being female (79, 80)and unemployed (79) were significantly associated with PTSD, as supported by the review studies. In addition to demographic characteristics, depression is a risk factors and/or comorbid with PTSD (28–30). Therefore, our finding confirmed that depression was significantly associated with PTSD among displaced people.
Strengths and limitations
This work could foster new views on how to manage the healthcare system or mitigate the effects of PTSD on quality of life, providing more information about how common PTSD is among those who have been uprooted. Additionally, the evaluation of many moderators was regarded as one of our study’s good points. Whereas, the limitation of this review is that it included only studies published in English that were cross-sectional studies since there were no studies conducted with other study designs and a small number of articles were included. In addition, most studies used very different instruments to screen for PTSD; therefore, it is difficult to compare and summarise the results.
Conclusion
In this review, the pooled prevalence of PTSD among displaced people in Africa was high. Demographic characteristics (female, single, and unemployed), substance use disorder, and depression were risk factors for PTSD among displaced people. This finding might help the stakeholders (mental health policy makers, administrators, and mental health professionals) to address the prevention, early screening, and management of PTSD among displaced people and to give attention to more vulnerable bodies. Future research that focuses on a more accurate diagnosis should include more representative samples, or rather, a cross-sectional study design.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author contributions
FA: Conceptualization, Data curation, Methodology, Software, Writing – original draft, Writing – review & editing. MM: Data curation, Writing – review & editing. GT: Writing – review & editing. GN: Data curation, Writing – review & editing. TT: Writing – review & editing. SF: Writing – review & editing. GR: Writing – review & editing. TD: Writing – review & editing. JS: Writing – review & editing. LF: Writing – review & editing. GM: Writing – review & editing. DA: Writing – review & editing. TG: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to thank the authors of the primary articles.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1336665/full#supplementary-material
Abbreviations
PCL-M, Post-Traumatic Stress Disorder Checklist-Military; CAPS, Clinician-Administered PTSD Scale; CIDI, Composite International Diagnostic Interview; PSS-I, Post-traumatic Symptom Scale Interview; SIQ, Cress Impact Questionnaire.
References
1. Bedaso A, Duko B. Epidemiology of depression among displaced people: a systematic review and meta-analysis. Psychiatry Res. (2022) 311:114493. doi: 10.1016/j.psychres.2022.114493
2. Nicholl C, Thompson A. The psychological treatment of Post Traumatic Stress Disorder (PTSD) in adult refugees: A review of the current state of psychological therapies. J Ment Health. (2004) 13:351–62. doi: 10.1080/09638230410001729807
3. Turrini G, Purgato M, Ballette F, Nosè M, Ostuzzi G, Barbui C. Common mental disorders in asylum seekers and refugees: umbrella review of prevalence and intervention studies. Int J Ment Health Syst. (2017) 11:1–14. doi: 10.1186/s13033-017-0156-0
4. Lafrenière J, Sweetman C, Thylin TJG. Development: Introduction: gender, humanitarian action and crisis response. Gender Dev. (2019) 27:187–201. doi: 10.1080/13552074.2019.1634332
5. Cohen R. The guiding principles on internal displacement: An innovation in international standard setting. Global Governance. (2004) 10:459–80. doi: 10.1163/19426720-01004006
6. Shultz JM, Ceballos ÁMG, Espinel Z, Oliveros SR, Fonseca MF, Florez LJH. Internal displacement in Colombia: fifteen distinguishing features. Disaster Health. (2014) 2:13–24. doi: 10.4161/dish.27885
7. Palattiyil G, Sidhva D, Seraphia Derr A, Macgowan M. Global trends in forced migration: Policy, practice and research imperatives for social work. Int Soc Work. (2022) 65:1111–29. doi: 10.1177/00208728211022791
8. Timm M. The integration of refugees into the German education system: A stance for cultural pluralism and multicultural education. EJournal Educ Policy. (2016).
9. Silove D, Ventevogel P, Rees S. The contemporary refugee crisis: an overview of mental health challenges. World Psychiatry. (2017) 16:130–9. doi: 10.1002/wps.20438
12. Makango B, Alemu ZA, Solomon T, Lemma N, Girma T, Mohammednur T, et al. Prevalence and factors associated with post-traumatic stress disorder among internally displaced people in camps at Debre Berhan, Amhara Region, Ethiopia: a cross-sectional study. BMC Psychiatry. (2023) 23:81. doi: 10.1186/s12888-023-04570-w
13. Csaky A. Global migration trends and Europe. Universitas Budapestiensis “Metropolitan”. (2019) 228.
14. Brundtland GH. Mental health of refugees, internally displaced persons and other populations affected by conflict. Acta Psychiatrica Scand. (2000) 102:159–61. doi: 10.1034/j.1600-0447.2000.102003159.x
15. Aluh DO, Okoro RN, Zimboh A. The prevalence of depression and post-traumatic stress disorder among internally displaced persons in Maiduguri, Nigeria. J Public Ment Health. (2019) 19:159–68. doi: 10.1108/JPMH-07-2019-0071
16. Goodwin-Gill GS, McAdam J. Geneva, Switzerland: UNHCR and climate change, disasters and displacement. Geneva, Switzerland: The United Nations Refugee Agency (UNHCR (2017).
17. Owoaje ET, Uchendu OC, Ajayi TO, Cadmus EO. A review of the health problems of the internally displaced persons in Africa. Nigerian Postgraduate Med J. (2016) 23:161–71. doi: 10.4103/1117-1936
18. Aker T, Ayata B, Ozeren M, Buran B, Bay A. Forced internally displacement: Psychosocial consequences. Anatolian J Psychiatry. (2002) 3:97–103.
19. Kreisberg-Voss D, Kennedy D, Van Arsdale P, Ferguson KJT. Clinical considerations concerning refugees in the Denver region. Torture. (1998) 8:90–7.
20. Petersen HD, Wandall J. Evidence of organized violence among refugees from Indian-held Kashmir. Torture. (1994) 4:90–5.
21. Schick M, Zumwald A, Knöpfli B, Nickerson A, Bryant RA, Schnyder U, et al. Challenging future, challenging past: the relationship of social integration and psychological impairment in traumatized refugees. Eur J Psychotraumatol. (2016) 7:28057. doi: 10.3402/ejpt.v7.28057
22. Hall BJ, Hobfoll SE, Palmieri PA, Canetti-Nisim D, Shapira O, Johnson RJ, et al. The psychological impact of impending forced settler disengagement in Gaza: Trauma and posttraumatic growth. J Traumatic Stress. (2008) 21:22–9. doi: 10.1002/jts.20301
23. Teodorescu DS, Heir T, Hauff E, Wentzel-Larsen T, Lien L. Mental health problems and post-migration stress among multi-traumatized refugees attending outpatient clinics upon resettlement to Norway. Scand J Psychol. (2012) 53:316–32. doi: 10.1111/j.1467-9450.2012.00954.x
24. Porter M, Haslam NJJ. Predisplacement and postdisplacement factors associated with mental health of refugees and internally displaced persons: a meta-analysis. Jama. (2005) 294:602–12. doi: 10.1001/jama.294.5.602
25. Steel Z, Chey T, Silove D, Marnane C, Bryant RA, Van Ommeren M. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: a systematic review and meta-analysis. Jama. (2009) 302:537–49. doi: 10.1001/jama.2009.1132
26. Fontalba-Navas A, Lucas-Borja M, Gil-Aguilar V, Arrebola J, Pena-Andreu J, Perez J. Incidence and risk factors for post-traumatic stress disorder in a population affected by a severe flood. Public Health. (2017) 144:96–102. doi: 10.1016/j.puhe.2016.12.015
27. Shaar KH. Post-traumatic stress disorder in adolescents in Lebanon as wars gained in ferocity: a systematic review. J Public Health Res. (2013) 2:e2017. doi: 10.4081/jphr.2013.e17
28. Sadock BJ. Kaplan & Sadock’s synopsis of psychiatry: behavioral sciences/clinical psychiatry. Wolters Kluwer Philadelphia, PA: Lippincott Williams and Wilkins (2015).
29. Townsend MC. Essentials of psychiatric mental health nursing: Concepts of care in evidence-based practice. Philadelphia, PA: FA Davis (2013).
30. First MB. DSM-5 handbook of differential diagnosis. Washington, DC: American Psychiatric Pub (2013). doi: 10.1176/appi.books.9781585629992
31. Yehuda R, Hoge CW, McFarlane AC, Vermetten E, Lanius RA, Nievergelt CM, et al. Post-traumatic stress disorder. BMJ. (2015) 1:1–22. doi: 10.1136/bmj.h6161
32. Goldmann E, Galea S. Mental health consequences of disasters. Annu Rev Public Health. (2014) 35:169–83. doi: 10.1146/annurev-publhealth-032013-182435
33. Svenaeus F. Diagnosing mental disorders and saving the normal: American Psychiatric Association, 2013. Diagnostic and statistical manual of mental disorders, American Psychiatric Publishing: Washington, DC. 991 pp., ISBN: 978-0890425558. Price: $122.70. Med Health Care Philosophy. (2014) 17:241–4. doi: 10.1007/s11019-013-9529-6
34. Roehr B. American psychiatric association explains DSM-5. Bmj. (2013) 346. doi: 10.1136/bmj.f3591
35. Koenen K, Ratanatharathorn A, Ng L, McLaughlin K, Bromet E, Stein D, et al. Posttraumatic stress disorder in the world mental health surveys. psychol Med. (2017) 47:2260–74. doi: 10.1017/S0033291717000708
36. Norris FH, Murphy AD, Baker CK, Perilla JL, Rodriguez FG, Rodriguez J. Epidemiology of trauma and posttraumatic stress disorder in Mexico. J Abnormal Psychol. (2003) 112:646. doi: 10.1037/0021-843X.112.4.646
37. Fazel M, Wheeler J, Danesh J. Prevalence of serious mental disorder in 7000 refugees resettled in western countries: a systematic review. Lancet. (2005) 365:1309–14. doi: 10.1016/S0140-6736(05)61027-6
38. Hoell A, Kourmpeli E, Salize HJ, Heinz A, Padberg F, Habel U, et al. Prevalence of depressive symptoms and symptoms of post-traumatic stress disorder among newly arrived refugees and asylum seekers in Germany: systematic review and meta-analysis. BJPsych Open. (2021) 7:e93. doi: 10.1192/bjo.2021.54
39. Thompson CT, Vidgen A, Roberts NP. Psychological interventions for post-traumatic stress disorder in refugees and asylum seekers: A systematic review and meta-analysis. Clin Psychol Rev. (2018) 63:66–79. doi: 10.1016/j.cpr.2018.06.006
40. Henkelmann J-R, de Best S, Deckers C, Jensen K, Shahab M, Elzinga B, et al. Anxiety, depression and post-traumatic stress disorder in refugees resettling in high-income countries: systematic review and meta-analysis. BJPsych Open. (2020) 6:e68. doi: 10.1192/bjo.2020.54
41. Slewa-Younan S, Uribe Guajardo MG, Heriseanu A, Hasan T. A systematic review of post-traumatic stress disorder and depression amongst Iraqi refugees located in western countries. J Immigrant Minority Health. (2015) 17:1231–9. doi: 10.1007/s10903-014-0046-3
42. Gebremeskel TG, Berhe M, Tesfa Berhe E. Suicide attempts among adult Eritrean refugees in Tigray, Ethiopia: prevalence and associated factors. Risk Manage Healthc Policy. (2022) 25:133–40. doi: 10.2147/RMHP.S311335
43. Bryant RA, Edwards B, Creamer M, O’Donnell M, Forbes D, Felmingham KL, et al. The effect of post-traumatic stress disorder on refugees’ parenting and their children’s mental health: a cohort study. Lancet Public Health. (2018) 3:e249–58. doi: 10.1016/S2468-2667(18)30051-3
44. McCauley JL, Killeen T, Gros DF, Brady KT, Back SE. Posttraumatic stress disorder and co-occurring substance use disorders: Advances in assessment and treatment. Clin Psychol: Sci Pract. (2012) 19:283. doi: 10.1111/cpsp.12006
45. Gilmoor AR, Adithy A, Regeer B. The cross-cultural validity of post-traumatic stress disorder and post-traumatic stress symptoms in the Indian context: A systematic search and review. Front Psychiatry. (2019) 10:439. doi: 10.3389/fpsyt.2019.00439
46. Forneris CA, Gartlehner G, Brownley KA, Gaynes BN, Sonis J, Coker-Schwimmer E, et al. Interventions to prevent post-traumatic stress disorder: a systematic review. Am J Prev Med. (2013) 44:635–50. doi: 10.1016/j.amepre.2013.02.013
47. Hamrah MS, Hoang H, Mond J, Pahlavanzade B, Charkazi A, Auckland S. The prevalence and correlates of symptoms of post-traumatic stress disorder (PTSD) among resettled Afghan refugees in a regional area of Australia. J Ment Health. (2021) 30:674–80. doi: 10.1080/09638237.2020.1739247
48. Fawa IM, Musa I, Abdullahi A. Assessment of post-traumatic stress disorder among internally displaced persons in Ringim Town, Jigawa State-Nigeria. SLU J Sci Technol. (2021) 2:100–13.
49. Mollica RF, Caspi-Yavin Y, Bollini P, Truong T, Tor S, Lavelle J. The Harvard Trauma Questionnaire: Validating a cross-cultural instrument for measuring torture, trauma, and posttraumatic stress disorder in Indochinese refugees. J Nervous Ment Dis. (1992) 180:111–6. doi: 10.1097/00005053-199202000-00008
51. Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The ptsd checklist for dsm-5 (pcl-5). J Traumatic Stress. (2013).
52. Ibrahim H, Ertl V, Catani C, Ismail AA, Neuner F. The validity of Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5) as screening instrument with Kurdish and Arab displaced populations living in the Kurdistan region of Iraq. BMC Psychiatry. (2018) 18:1–8. doi: 10.1186/s12888-018-1839-z
53. Verhey R, Chibanda D, Gibson L, Brakarsh J, Seedat S. Validation of the posttraumatic stress disorder checklist–5 (PCL-5) in a primary care population with high HIV prevalence in Zimbabwe. BMC Psychiatry. (2018) 18:1–8. doi: 10.1186/s12888-018-1688-9
54. Van Vliet I, De Beurs E. The MINI-International Neuropsychiatric Interview. A brief structured diagnostic psychiatric interview for DSM-IV en ICD-10 psychiatric disorders. Tijdschrift voor Psychiatrie. (2007) 49:393–7.
55. Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. (1998) 59:22–33.
56. de Azevedo Marques JM, Zuardi AW. Validity and applicability of the Mini International Neuropsychiatric Interview administered by family medicine residents in primary health care in Brazil. Gen Hosp Psychiatry. (2008) 30:303–10. doi: 10.1016/j.genhosppsych.2008.02.001
57. Otsubo T, Tanaka K, Koda R, Shinoda J, Sano N, Tanaka S, et al. Reliability and validity of Japanese version of the Mini-International Neuropsychiatric Interview. Psychiatry Clin neurosci. (2005) 59:517–26. doi: 10.1111/j.1440-1819.2005.01408.x
58. Thoresen S, Tambs K, Hussain A, Heir T, Johansen VA, Bisson JI. Brief measure of posttraumatic stress reactions: Impact of Event Scale-6. Soc Psychiatry Psychiatr Epidemiol. (2010) 45:405–12. doi: 10.1007/s00127-009-0073-x
59. Weiss DS. The impact of event scale: revised. Cross-cultural Assess psychol Trauma PTSD. (2007), 219–38.
60. Hussain A, Weisæth L, Heir T. Posttraumatic stress and symptom improvement in Norwegian tourists exposed to the 2004 tsunami–a longitudinal study. BMC Psychiatry. (2013) 13:1–11. doi: 10.1186/1471-244X-13-232
61. Cameron RP, Gusman D. The primary care PTSD screen (PC-PTSD): development and operating characteristics. Primary Care Psychiatry. (2003) 9:9–14.
62. Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. JBI Evid Implement. (2015) 13:147–53. doi: 10.1097/XEB.0000000000000054
63. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.1186
64. Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. bmj. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
65. Sterne JA, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol. (2001) 54:1046–55. doi: 10.1016/S0895-4356(01)00377-8
66. Madoro D, Kerebih H, Habtamu Y, G/tsadik M, Mokona H, Molla A, et al. Post-traumatic stress disorder and associated factors among internally displaced people in South Ethiopia: a cross-sectional study. Neuropsychiatr Dis Treat. (2020) 16:2317–26. doi: 10.2147/NDT.S267307
67. Sheikh TL, Mohammed A, Agunbiade S, Ike J, Ebiti WN, Adekeye O. Psycho-trauma, psychosocial adjustment, and symptomatic post-traumatic stress disorder among internally displaced persons in Kaduna, Northwestern Nigeria. Front Psychiatry. (2014) 5:127. doi: 10.3389/fpsyt.2014.00127
68. Roberts B, Ocaka KF, Browne J, Oyok T, Sondorp E. Factors associated with post-traumatic stress disorder and depression amongst internally displaced persons in northern Uganda. BMC Psychiatry. (2008) 8:1–9. doi: 10.1186/1471-244X-8-38
69. Bapolisi AM, Song SJ, Kesande C, Rukundo GZ, Ashaba S. Post-traumatic stress disorder, psychiatric comorbidities and associated factors among refugees in Nakivale camp in southwestern Uganda. BMC Psychiatry. (2020) 20:1–10. doi: 10.1186/s12888-020-2480-1
70. Musau JN, Omondi M, Khasakhala L. The prevalence of post-traumatic stress disorder (PTSD) among internally displaced persons (IDPs) in Maai Mahiu Camp in Nakuru County, Kenya. J Internal Displacement. (2018) 8:20–33.
71. Ali M, Mutavi T, Mathai M, Mburu J. Prevalence of posttraumatic stress disorder and depression among internally displaced persons in Mogadishu. (2022), 1–16. doi: 10.21203/rs.3.rs-1257017/v1
72. Mwanamwambwa V, Pillay BJ. Posttraumatic stress disorder and psychological distress in Rwandan refugees living in Zambia. South Afr J Psychol. (2022) 52:175–88. doi: 10.1177/00812463211031812
73. Nesterko Y, Jäckle D, Friedrich M, Holzapfel L, Glaesmer H. Prevalence of post-traumatic stress disorder, depression and somatisation in recently arrived refugees in Germany: an epidemiological study. Epidemiol Psychiatr Sci. (2020) 29:e40. doi: 10.1017/S2045796019000325
74. Melkam M, Tinsae T, Andualem F, Nakie G. Post-traumatic stress disorder and associated factors among adults exposed to stress in Ethiopia: A meta-analysis and systematic review. SAGE Open Med. (2023) 11:20503121231160884. doi: 10.1177/20503121231160884
75. Mekonnen N, Duko B, Kercho MW, Bedaso A. PTSD among road traffic accident survivors in africa: A systematic review and meta-analysis. Heliyon. (2022) 8:e11539. doi: 10.1016/j.heliyon.2022.e11539
76. Bromet EJ, Atwoli L, Kawakami N, Navarro-Mateu F, Piotrowski P, King A, et al. Post-traumatic stress disorder associated with natural and human-made disasters in the World Mental Health Surveys. psychol Med. (2017) 47:227–41. doi: 10.1017/S0033291716002026
77. Hoppen TH, Priebe S, Vetter I, Morina N. Global burden of post-traumatic stress disorder and major depression in countries affected by war between 1989 and 2019: a systematic review and meta-analysis. BMJ Global Health. (2021) 6:e006303. doi: 10.1136/bmjgh-2021-006303
78. Tang B, Deng Q, Glik D, Dong J, Zhang L. A meta-analysis of risk factors for post-traumatic stress disorder (PTSD) in adults and children after earthquakes. Int J Environ Res Public Health. (2017) 14:1537. doi: 10.3390/ijerph14121537
79. El Hajj M. Prevalence and associated factors of post-traumatic stress disorder in Lebanon: A literature review. Asian J Psychiatry. (2021) 63:102800. doi: 10.1016/j.ajp.2021.102800
Keywords: epidemiology, prevalence, posttraumatic stress disorder, PTSD, displaced people, refugees, internal displaced people, Africa
Citation: Andualem F, Melkam M, Takelle GM, Nakie G, Tinsae T, Fentahun S, Rtbey G, Begashaw TD, Seid J, Tegegn LF, Gedef GM, Bitew DA and Godana TN (2024) Prevalence of posttraumatic stress disorder and associated factors among displaced people in Africa: a systematic review and meta-analysis. Front. Psychiatry 15:1336665. doi: 10.3389/fpsyt.2024.1336665
Received: 11 November 2023; Accepted: 19 February 2024;
Published: 05 March 2024.
Edited by:
S. M. Yasir Arafat, Biomedical Research Foundation, BangladeshReviewed by:
Sarya Swed, University of Aleppo, SyriaMohammadreza Shalbafan, Iran University of Medical Sciences, Iran
Valentina Cesari, Medical and Molecular Pathology and Critical Care Medicine, Italy
Copyright © 2024 Andualem, Melkam, Takelle, Nakie, Tinsae, Fentahun, Rtbey, Begashaw, Seid, Tegegn, Gedef, Bitew and Godana. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fantahun Andualem, ZmFudGFhbmR1MjdAZ21haWwuY29t
 Fantahun Andualem
Fantahun Andualem Mamaru Melkam1
Mamaru Melkam1 Girmaw Medfu Takelle
Girmaw Medfu Takelle Girum Nakie
Girum Nakie Techilo Tinsae
Techilo Tinsae Setegn Fentahun
Setegn Fentahun Gidey Rtbey
Gidey Rtbey Tesfaye Derbie Begashaw
Tesfaye Derbie Begashaw Jemal Seid
Jemal Seid Getachew Muluye Gedef
Getachew Muluye Gedef Tilahun Nega Godana
Tilahun Nega Godana