
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 19 August 2024
Sec. ADHD
Volume 15 - 2024 | https://doi.org/10.3389/fpsyt.2024.1332598
Background: Neurodevelopmental disorders (NDD), psychiatric comorbidity and cognitive deficits are commonly seen in children with obesity; however, little is known about the overlap between these conditions. This study aimed to examine the undiagnosed and diagnosed frequency of NDDs and explore its association with psychiatric conditions and general intellectual ability (IQ) in children presenting for obesity treatment.
Methods: In this observational study at two outpatient obesity clinics during 2018-2019, 80 children (8-17 years) were consecutively recruited, and screened for NDD unless already diagnosed with an NDD. A psychiatric unit evaluated children who screened positive for NDD. Diagnoses and clinical background factors were collected from medical records. IQ was assessed with the Weschler Intelligence Scales and internalizing symptoms were assessed using the Beck Youth Inventories. Associations between background factors, IQ and internalizing symptoms were explored in relation to having an NDD or not.
Results: We found that 47/80 children had at least one NDD. Children with a diagnosed NDD before study start (n = 30) had significantly more comorbidities than children diagnosed after the study screening (n = 17) (P = .01). Greater cognitive impairment was seen in children with NDD compared with children without an NDD (P = .01). Also, 33/73 participants self-reported substantial internalizing symptoms. At follow-up, 21/79 participants, in addition to NDD, had been diagnosed with another psychiatric disorder. Ten of these were children that had been diagnosed with an NDD before study start.
Conclusion: The overlap between NDD, cognitive deficits and psychiatric conditions in children with obesity is an important consideration for clinical practice. Screening for these conditions may be necessary when providing targeted interventions.
Pediatric obesity is a complex multifactorial disease that is considered a global challenge due to its high prevalence and long-term risk of adverse health outcomes. Early identification and multicomponent behavioral interventions are imperative (1, 2), but high attrition (40-80%) is a common problem in obesity treatment (2, 3).
Most multicomponent behavioral interventions require the child and the family to integrate new strategies in everyday life to balance energy intake against energy expenditure. Successful establishment of such strategies may be dependent on the patient’s behavioral and cognitive abilities (1). However, a substantial proportion of children presenting for obesity treatment have recognized or unrecognized neurodevelopmental disorders (NDD) (4, 5), cognitive dysfunction (6), or psychiatric disorders (7). These conditions are suggested to influence obesity management negatively (2, 6). Interestingly, they seem to have a state of vitamin D insufficiency which exhibit in normal conditions neurotrophic and antioxidant effect in the central nervous system (8, 9). So far, most studies have explored NDD, cognitive dysfunction, and other psychiatric disorders separately, and little is known about the co-occurrence of NDD, cognitive dysfunction and psychiatric disorders in children undergoing obesity treatment.
NDD include a group of conditions with early developmental onset (10). The common co-occurrence of NDD, cognitive deficits and psychiatric conditions is presented as ESSENCE (Early Symptomatic Syndromes Eliciting Neurodevelopmental Clinical Examinations) (11). This concept covers conditions with early developmental onset, not only disorders but also difficulties that do not fulfill the criteria for a specific disorder; for instance, borderline intellectual functioning (BIF, i.e., intellectual quotient [IQ] 70–84). Children with BIF are a vulnerable group with an increased risk of psychiatric conditions and negative effects related to educational and behavioral functioning (12). BIF is also common in NDD (11). Among NDD, attention deficit/hyperactivity disorder (ADHD) and autism spectrum disorder (ASD) have repeatedly, but separately, been shown to have high comorbidity with obesity (4, 13, 14). However, there is a lack of studies evaluating a broader range of NDD in relation to obesity.
IQ is a measure of general cognitive functioning and the most robust and reliable measure to predict global functioning and health outcomes (15, 16). Certain studies have indicated lower IQ scores in children with obesity compared with normal weight peers or norm data; however, the results are inconclusive (17–19). The different results between studies may be due to lower IQ scores in some studies being confounded by the generally lower socioeconomic status among children with obesity (17, 20, 21). Contradictory findings may also be related to differences in the assessment of IQ, and abbreviated scales are often used in studies (17). Also, to the best of our knowledge, no study has so far considered NDD when studying IQ in children with obesity, even if cognitive deficits are common in patients with NDD, regardless of their weight status (11).
Furthermore, there is an increased risk of depression or anxiety both in children with obesity (7, 22) and in children with NDD (23, 24), but few studies have investigated such psychiatric conditions in children with both obesity and NDD. However, a Swedish register-based study showed that obesity was associated with an increased risk of depressive and anxiety disorders during childhood (between 6 and 18 years of age). This risk was independent of other risk factors such as NDD, sex and socioeconomic status (22). Nevertheless, register-based research relies on recorded diagnoses, and many mental health disorders may go undetected, thereby accentuating the need for more thorough clinical studies. Early detection may be crucial in preventing the progression of maladaptive development and the risk of subsequent psychiatric disorders (25).
The aim of this study was to explore the co-occurrence of NDD, with focus on ASD, ADHD, specific learning disorders including BIF and motor disorders along with internalizing and externalizing disorders in children presenting for obesity treatment, by 1) determining the frequency of diagnosed NDD (including identified BIF) and diagnosed psychiatric disorders, 2) exploring intellectual abilities and internalizing symptoms in children with and without a diagnosed NDD, and 3) exploring associations between clinical background factors, IQ, and internalizing symptoms.
This observational study consecutively offered participation in the study by the pediatrician during regular medical appointments for children aged 8-17 years undergoing obesity treatment at either of two pediatric outpatient obesity clinics in the Western Region of Sweden (Kungsbacka and Varberg). The period of inclusion was 2018 and 2019. Obesity was defined as a body mass index standard deviation score (BMI SDS) of ≥ 2. Exclusion criteria were, i) conditions or medication that might influence cognitive functioning or weight (insulin treatment for type 1 diabetes mellitus [n=1], verified syndrome with hypothalamic obesity or taking anti-epileptic drugs or oral cortisone), ii) suspected/diagnosed intellectual developmental disorder (n=4), as it may be associated with genetic conditions and implies significantly impaired intellectual and adaptive functioning (10), and iii) families non-fluent in Swedish. In total, 84 children were eligible and the parents of 80 children agreed to study participation. All children with no previously diagnosed NDD underwent a standardized clinical neurodevelopmental evaluation, including an assessment of the child’s intellectual and psychological functioning. Children who screened positive for the NDD were referred to a psychiatric outpatient clinic for further evaluation for diagnosis (26). Figure 1 displays flow chart of the recruitment procedure and time of cognitive and psychological assessment.
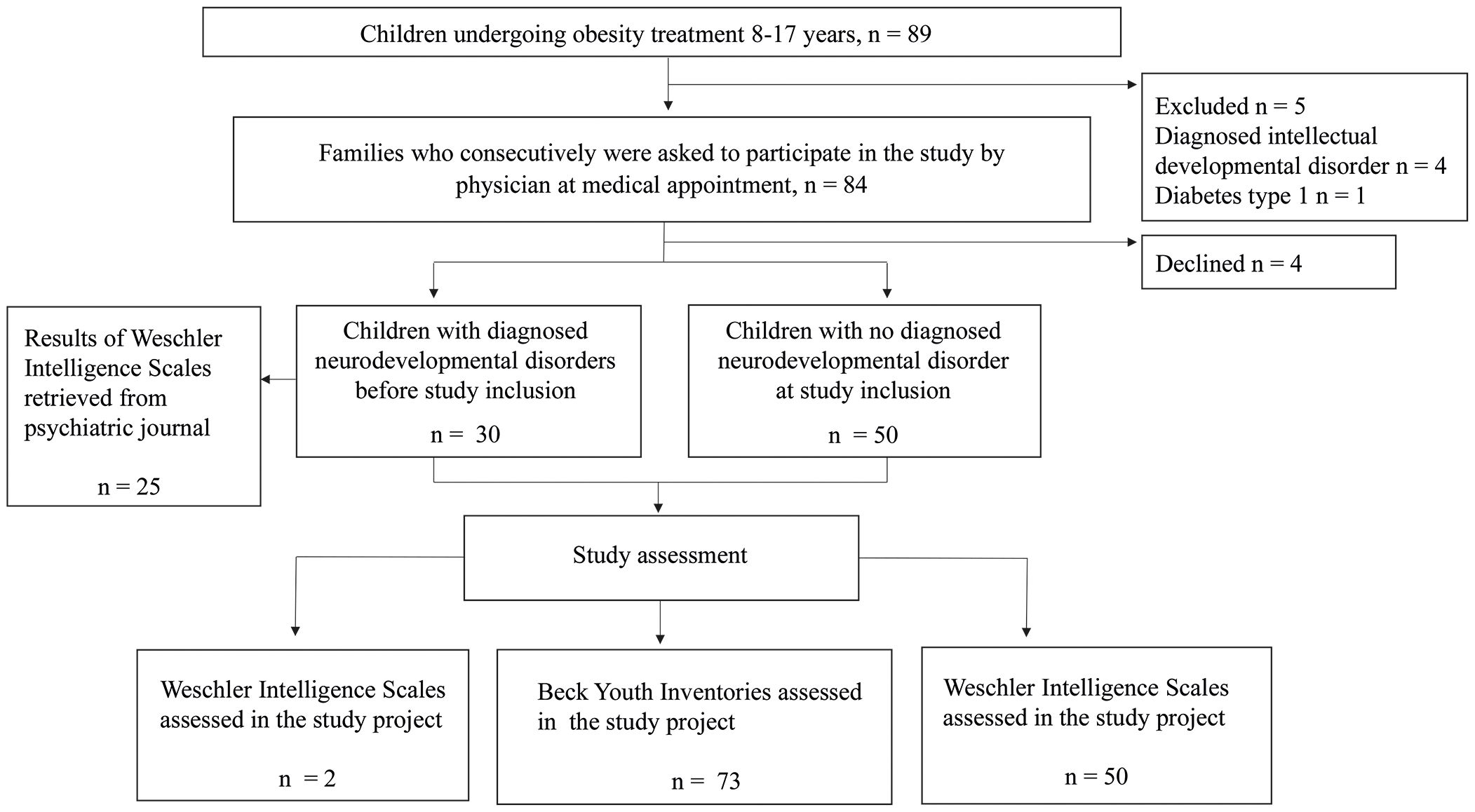
Figure 1. Flow chart of the recruitment procedure and time of cognitive and psychological assessment.
Table 1 provides a detailed description of the assessment battery. General intellectual ability, measured as Full-Scale IQ (FSIQ), was assessed with the Wechsler Intelligence Scales, the golden standard for assessing intellectual ability. Besides FSIQ, the Wechsler Intelligence Scales measure different cognitive domains, defined as indexes (sum of scaled scores). All Wechsler Intelligence Scales used in this study included the following indexes; Verbal Comprehension, Visuo-Spatial/Perceptual Reasoning/Performance, Working Memory and Processing Speed (27).
A clinical psychologist (MDB) assessed all children with no diagnosed NDD at study start; 47 children were assessed with the Wechsler Intelligence Scale for Children-5th Edition (WISC-V) (28) and the remaining three children with Wechsler Adult Intelligence Scale-4th Edition (WAIS-IV) (29). For children previously diagnosed with an NDD, it was assumed that they had already undergone a cognitive assessment as it is a standard part of a neurodevelopmental evaluation. Hence, they were not assessed again, instead we extracted the cognitive results from their psychiatric records. However, at follow-up it was discovered that four children had not undergone a cognitive assessment when diagnosed with an NDD. Two of them underwent assessment with the WISC-V (28) by the psychologist (MDB), whereas two patients (> 18 years at follow-up) were no longer patients at the obesity clinic and were therefore omitted from the cognitive part of the study. Among the other children previously diagnosed with an NDD, the following versions of the Wechsler Intelligence Scales had been used: one child had been assessed with the Wechsler Preschool and Primary Scale of Intelligence-3rd Edition (30), while 20 children had been assessed with the Wechsler Intelligence Scale for Children-4th Edition (WISC-IV) (31) and additional four participants with the WISC-V (28). The WISC-V has been examined in relation to previous editions of the instrument and has shown good correlation (27).
The Wechsler Intelligence Scales assume normal distribution, and raw scores are converted into scaled scores using age-matched norm data. The mean (standard deviation [SD]) of the FSIQ and indexes correspond to 100 (15) and can be qualitatively categorized: extremely low (-69), very low (70-84), low average (85-92), average (93-107), high average (108-115), very high (116-130), and extremely high (131-) (27).
None of the participants were taking psychostimulants at the time of the cognitive assessment. The timepoint of the cognitive assessment (age of the child at cognitive testing) was categorized as the starting point of the diagnostic evaluation process. Per definition this categorization excludes those two previously diagnosed NDD children who were assessed at our study follow-up.
The Beck Youth Inventories (BYI) (age 7-18 years) (32) consist of five reliable (mean Cronbach’s α ≥.89) self-report scales that can be used separately or in combination. The inventories for anxiety and depression (internalizing symptoms) were used in this study. A total raw score is calculated for each scale and translated into percentiles using Swedish gender-specific norms. A higher percentile reflects more symptoms. The 90th percentile corresponds to highly elevated symptoms and can be used as a clinical cut-off. All children filled out BYI during the time of the study project; for children screened in the study at the time of cognitive testing, and for the participants previously diagnosed with an NDD, either at their medical appointment or at home.
In the present study NDD included ASD, ADHD, motor disorders as well as specific learning disorders (e.g., dyslexia, dyscalculia) (10). In this study specific learning disorders were grouped together with, by psychiatric journal, identified BIF and they were categorized as “any learning disabilities”. Further, ADHD was stratified by its different subtypes: predominantly inattentive, predominantly hyperactive/impulsive, and combined. This study also examines the frequency of depressive disorders, anxiety disorders, obsessive-compulsive and related disorders, trauma-compulsive and stressor-related disorders as well as disruptive, impulse-control, and conduct disorders (10). In the current study these disorders are denoted as psychiatric disorders. Psychiatric disorders were categorized as internalizing disorders (the propensity to express distress inwards) or externalizing disorders (the propensity to express distress outwards) (33). The first author (MDB) extracted the diagnoses and identified BIF from psychiatric records two years after the data collection finished in May 2021, to ensure that the psychiatric unit had received sufficient time to assess the children. For children already diagnosed with an NDD, the diagnoses were also confirmed through the records at the time of consent.
Height and weight were measured by a nurse at the clinic with standardized methods and BMI SDS was calculated (34). Sex, age, and BMI SDS were then obtained from medical records from the date the child started the obesity treatment at the clinic, at time of cognitive testing, at inclusion and at follow-up.
The highest educational level of parents in the family was used to defined socioeconomic status. Parental educational level was retrieved from Statistics Sweden corresponding to the year 2018 and is reported in accordance with SUN 2020 (35). In this study, lower educational level involved pre-primary education, primary and lower secondary education less than 9 years and primary and lower secondary education 9 (10) years, whereas advanced educational level was defined as upper secondary education, post-secondary education less than 2 years, post-secondary education 2 years or longer as well as postgraduate education.
Descriptive data are presented as means (SD), medians (inter-quartile range [IQR]), or frequencies (N; %). For continuous variables, comparisons between groups were analyzed using the independent sample t-test or ANOVA (if normally distributed), Kruskal-Wallis or Mann-Whitney U (if non-normally distributed), and Fischer’s exact test (low frequencies). Shapiro-Wilks (p ≤ 0.05) and histograms were used to identify non-normal distributions. The Pearson correlation was used for the correlation analysis. The degree of correlation was defined as follows: coefficient value r; small ≤ 0.29; medium 0.3- 0.49; and strong 0.5 – 1. For parametric tests, a p value ≤ 0.05 was considered statistically significant. For non-parametric tests, a p value ≤ 0.10 defined significance due to small sample sizes and great variations within the subgroup BYI scores (36). All statistical analyses were made using IBM SPSS Statistics version 27 (IBM SPSS Statistics, Chicago, IL).
The Regional Ethical Review Board in Gothenburg (reg. no. 409-14) approved the study. Written informed consent was obtained from parents and assent from patients if their age was ≥ 12 years. The study was carried out in line with the Declaration of Helsinki.
Table 2 presents the patient characteristics. One of the screened patients turned out to have a suspected intellectual developmental disorder and was omitted from analysis. We found 30/79 (38%) participants already diagnosed with an NDD when they were included in this study and are henceforth denoted the “pre-diagnosed NDD group”. Additionally, 17/50 (34%) children undergoing screening in this study were subsequently diagnosed with an NDD after referral to the psychiatry unit (26) and are henceforth denoted the “study-diagnosed NDD group”. The remaining 32 participants are denoted the “non-NDD group”. The pre-diagnosed NDD group was significantly older at the time of completing the BYI compared with the study-diagnosed NDD group (P = .02). The delta mean BMI SDS between obesity treatment start and follow-up for the study-diagnosed NDD group was -0.5 SDS. Additionally, a greater number of parents in the non-diagnosed NDD group had advanced educational level compared to pre-diagnosed NDD group (P = .07). The corresponding analysis between non-diagnosed NDD group and study-diagnosed group did not reach a significant level (P = .20).
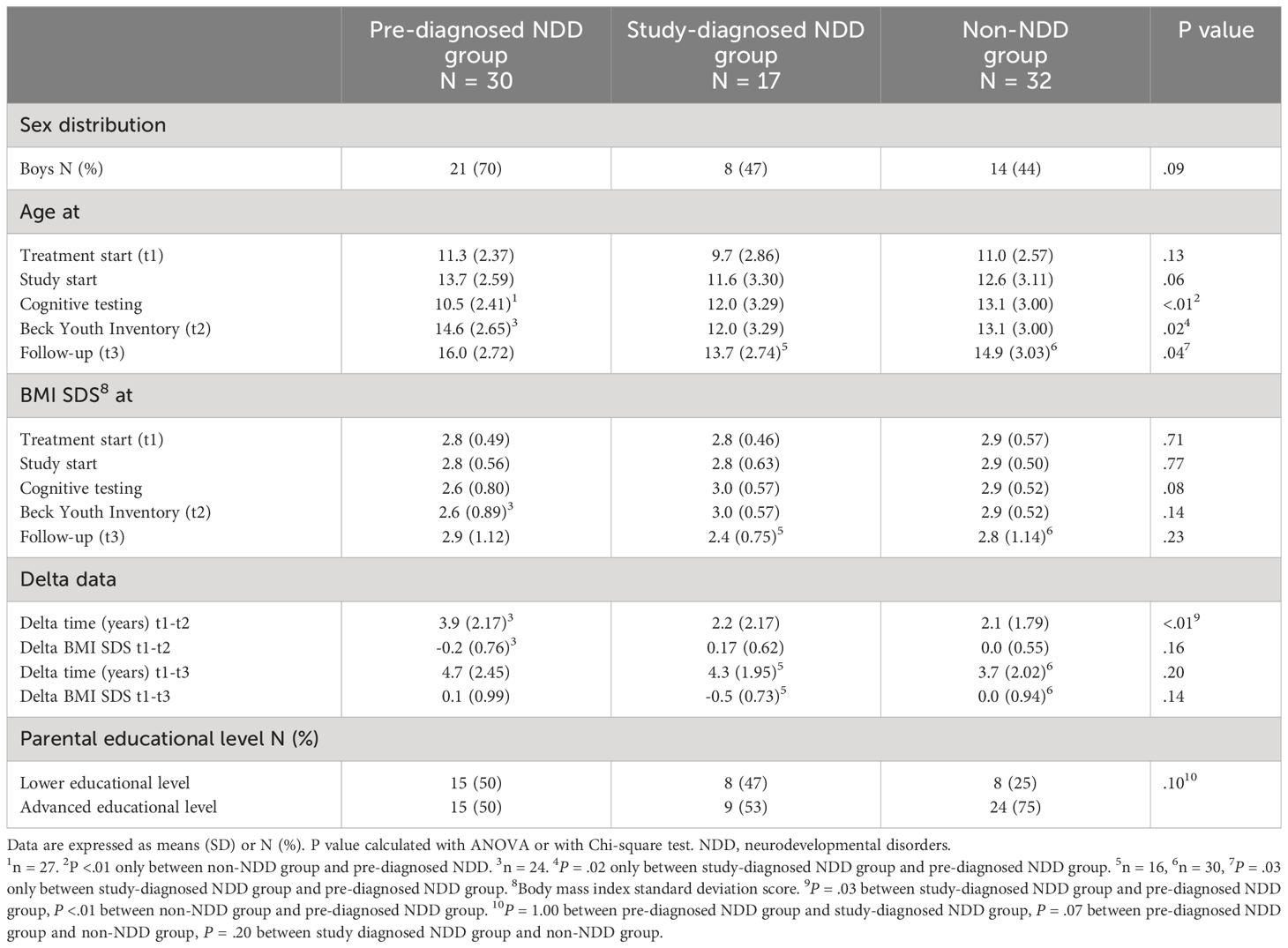
Table 2. Characteristics of children with obesity seeking treatment included in the study, broken down by group.
Table 3 displays the frequency and distribution of the diagnoses in the subgroups, and the merged pre-diagnosed and study-diagnosed NDD groups (denoted “NDD total group”) and the total study sample. At follow-up, a total of 47 patients were diagnosed with an NDD and 45 of these had ADHD (96%). Fourteen participants had ASD (30%) and twelve of them also had ADHD. Eighteen of 47 (38%) patients had more than one identified comorbidity; six children (13%) had ADHD with any learning disability of which one also had with tic disorder, 11 children (23%) had ADHD with ASD including one who had additionally been diagnosed developmental coordination disorder and one child (2%) had ASD and ADHD with any learning disability. In addition to ADHD, internalizing and externalizing disorders were diagnosed in 21 of 79 participants (27%). Depressive disorder was the most common. All but one child in the pre-diagnosed group had been diagnosed with internalizing and/or externalizing disorder before study inclusion, while children in the study- diagnosed NDD group and non-diagnosed NDD group were diagnosed with these psychiatric disorders during study follow-up.
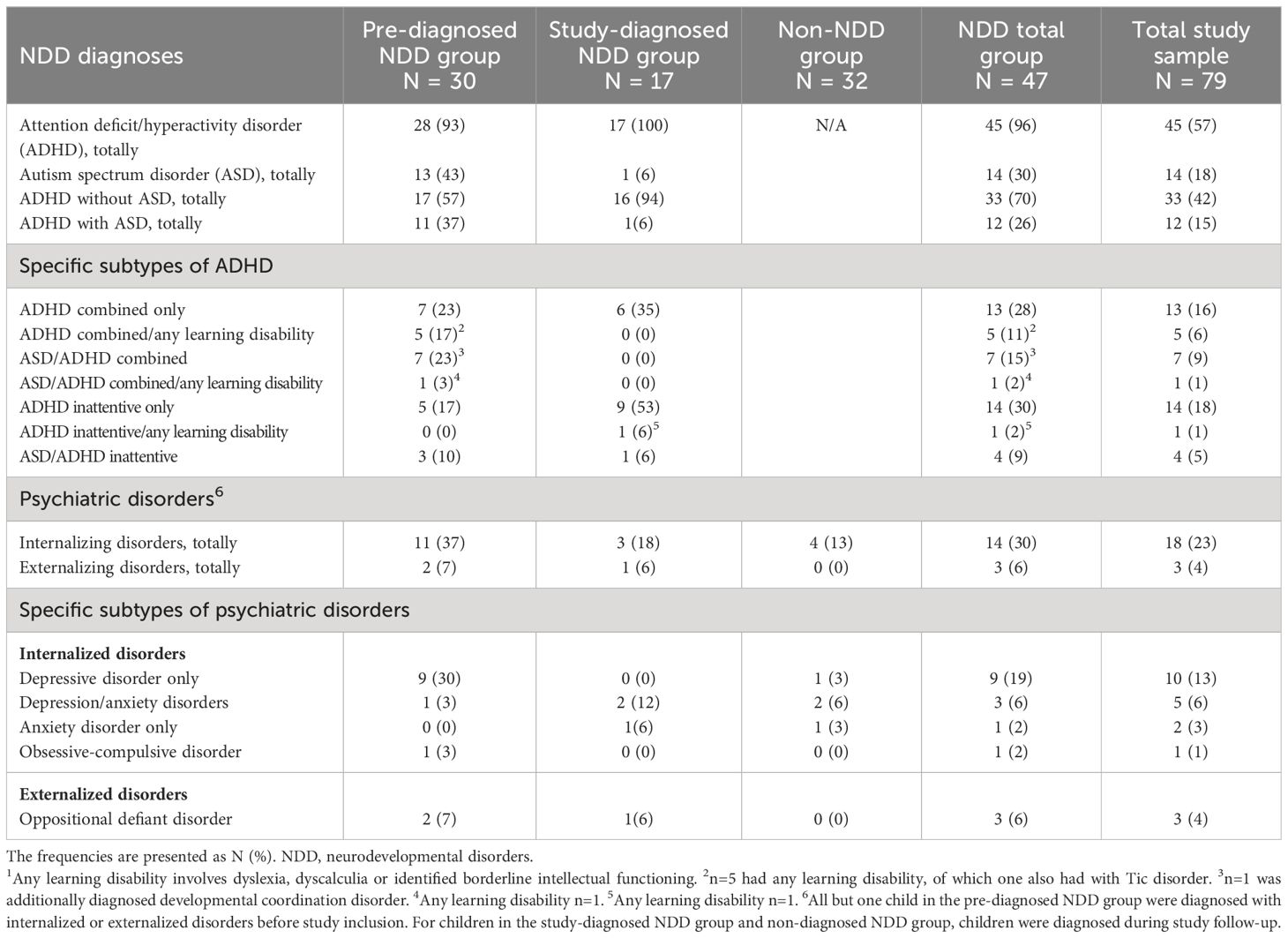
Table 3. Distribution of neurodevelopmental disorders (NDD) including any learning disability 1 and psychiatric disorders in children presenting for obesity treatment, broken down by group.
As expected, pre-diagnosed NDD children were significantly younger, 10.70 (3.10) years, at the time of receiving their first NDD diagnosis, compared with study-diagnosed NDD children, 12.78 [(3.11), P = .03] years. In the pre-diagnosed group, 73% were boys (22/30), compared with 47% (8/17) in the study-diagnosed group. The sex distribution was not significantly different between the groups (P = .12). Table 4 presents number of NDD-related comorbidities in the pre-diagnosed NDD group compared with the study-diagnosed NDD group. Additionally, significantly more pre-diagnosed NDD boys were diagnosed with ASD compared with the study-diagnosed NDD boys (P = .01). A significantly larger number of study-diagnosed NDD girls were diagnosed with ADHD of the inattentive subtype, compared with pre-diagnosed NDD girls (P = .02).
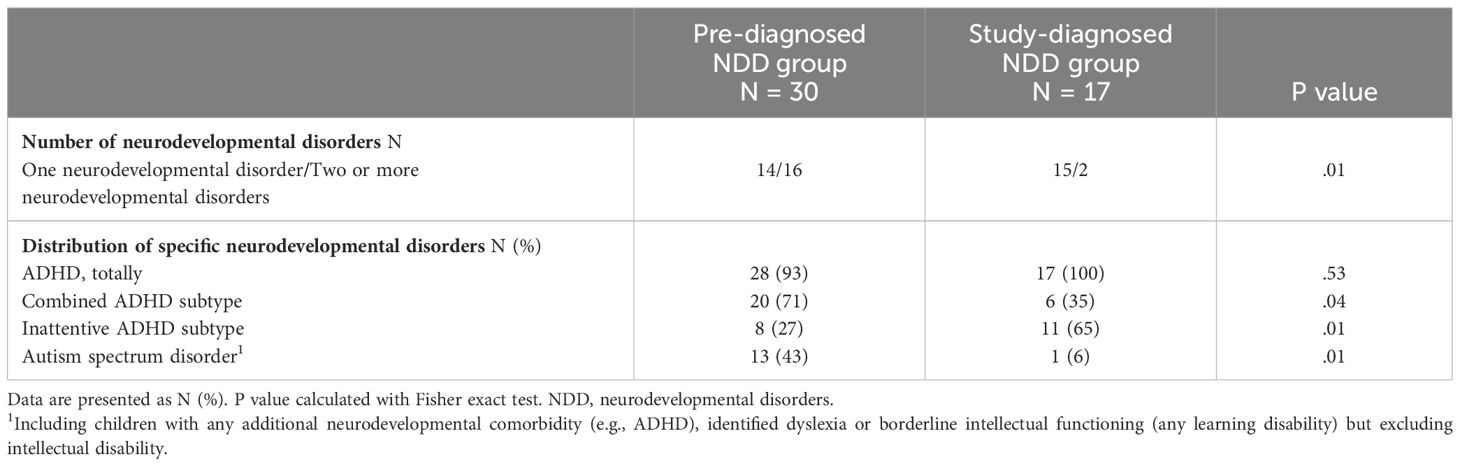
Table 4. Comparison of neurodevelopmental-related comorbidities between children diagnosed with neurodevelopmental disorders before study start (pre-diagnosed NDD group) and children diagnosed with neurodevelopmental disorders by study screening (study-diagnosed NDD group).
The FSIQ results are presented in Table 5 and the additional indexes are shown in Supplementary Table S1. Qualitatively categorized FSIQ was accessible for 76 out of 79 participants, showing that 21 participants (28%) performed within the very low range and one child in the very high. In addition, the NDD total group scored significantly lower on the FSIQ, 89.1 (10.0), compared with the non-NDD group, 95.7 (12.1), (P =.01). The pre-diagnosed NDD group performed worse on the Working Memory index (P = .01) and Processing Speed index (P = .02) relative to the non-NDD group, while the study-diagnosed NDD group achieved lower scores on the Working Memory index compared with the non-NDD group (P = .03). No significant differences were detected between the study-diagnosed and the pre-diagnosed NDD group.
At time of study assessment, 24 of 73 (33%) scored > the 90th percentile on the anxiety inventory on the BYI. The corresponding number for the depression inventory was also 33%. Totally, 33 (45%) of the participants who completed the BYI (n=73) reported at least one of the anxiety or depression inventories > the 90th percentile. Of the 33 participants reporting > the 90th percentile, 15 (45%) reported both highly elevated symptoms of depression and anxiety, while 18 (55%) reported one of the inventories > the 90th percentile (either depression or anxiety). No significant sex differences were found for symptoms of depression (P = .50) or anxiety (P = .31).
Table 6 presents data for internalizing symptoms, compared between subgroups. The pre-diagnosed NDD group scored higher for depressive symptoms than the study-diagnosed NDD group, but it did not reach a statistical significant level. However, ten participants in the pre-diagnosed NDD group were already on treatment for depressive disorder. Three of them did not complete the BYI due to lack of energy related to depression, whereas four of the ten scored < the 90th percentile.
Associations between clinical background factors, FSIQ and internalized symptoms for all subgroups and the total study sample are presented in Table 7. Higher BMI SDS at cognitive testing was significantly associated with lower FSIQ scores among non-NDD children (P = .02). This association was not seen in the other groups. Only in the total sample, children of parents with lower educational level scored significantly poorly on FSIQ compared to children of parents with advanced educational level (P = .04). Also, age at BYI inventory and anxiety symptoms (r = .49, P = .04) and depressive symptoms (r = .78, P <.001) were positively correlated in the study-diagnosed NDD group. For the NDD total group, older age at cognitive testing (starting point of diagnostic evaluation process) was significantly associated with higher FSIQ scores (r = .35, P = .03) and, similarly, a higher FSIQ was significantly associated with anxiety symptoms (r = .40, P = .02). The correlation between older age at the starting point of the diagnostic evaluation process and anxiety symptoms did not reach significance (r = .30, P = .07). The corresponding correlation for depressive symptoms was significant (r = .35, P = .03).
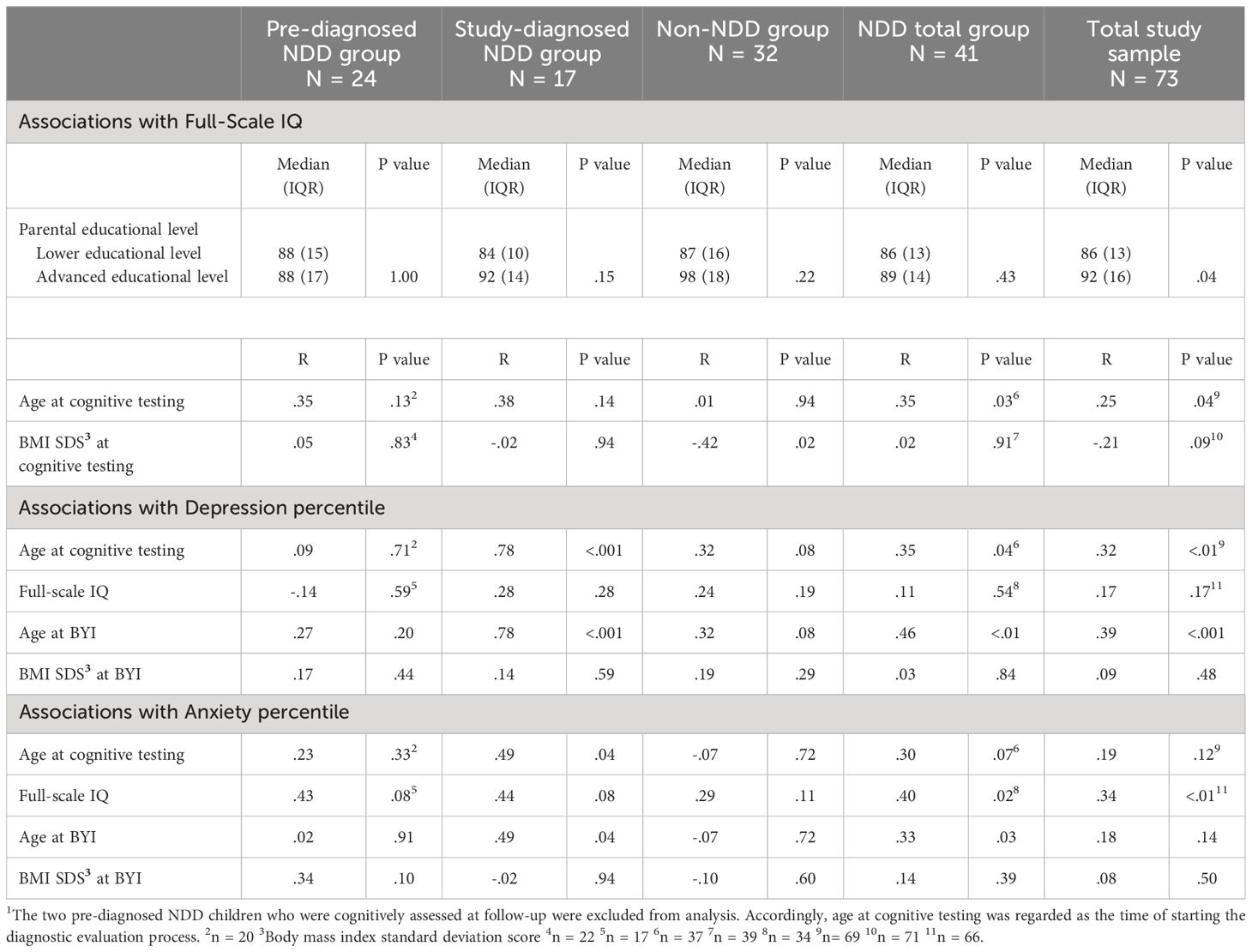
Table 7. Association between clinical background factors, Full-Scale IQ (Weschler Intelligence Scales), depressive percentile and anxiety percentile (Beck Youth Inventory; BYI), broken down by group: children diagnosed with neurodevelopmental disorder before study start (pre-diagnosed NDD group)1, children diagnosed with neurodevelopmental disorder by study screening (study-diagnosed NDD group) and children not diagnosed with any neurodevelopmental disorder (non-diagnosed NDD group), children with diagnosed neurodevelopmental disorder total group (NDD total group)1 as well as total study sample.
This study examined a wide spectrum of neurodevelopmental and psychiatric comorbidities in 80 consecutively recruited children from two pediatric obesity outpatient clinics in Sweden. At least one NDD was found in 59% of the children with obesity, and all but two with NDD had an ADHD diagnosis. Almost 20% of the children with an NDD had ASD. The proportion of children in obesity treatment with ADHD varies between studies, and frequencies between 18% (5) and 58% (37) have been reported. Among previous publications in children with ASD, 17% also had obesity (13).
The clinical presentations in this group of children with obesity fit well into the concept of ESSENCE (11). This is one of the novel findings in the present study. Nearly two fifths (38%) of the children with obesity diagnosed with a NDD had more than one identified NDD defined comorbidity. Another marker of ESSENCE is cognitive impairments and in our study children with NDD showed greater cognitive deviances compared to non-NDD diagnosed children, especially the pre-diagnosed NDD group. Also 33% of the pre-diagnosed children turned out to have depression at follow-up.
Children diagnosed with an NDD before the study were characterized by two or more early-onset developmental problems and disorders such as ASD and/or a combined ADHD subtype. Additionally, ASD was more prevalent in pre-diagnosed boys compared with study-diagnosed NDD boys. Both co-occurring NDDs, which may lead to more severe problems with adaptive functioning (38), and hyperactivity and/or disruptive behavior (23, 24, 39), may enable early detection. A larger proportion of study-diagnosed girls had inattentive ADHD compared with the pre-diagnosed NDD girls. Compared with combined or hyperactive/impulsive ADHD, inattentive ADHD is more common in girls than boys and may be less noticeable to others. This may explain why ADHD in girls is easily overlooked and often identified at an older age (24).
Our study indicates that NDD in children presenting for obesity treatment could be at risk of a delayed NDD diagnosis (40–42) possibly affecting obesity treatment outcome. The participants mean age when receiving the first NDD diagnosis occurred during middle school age, for both the pre-diagnosed and study-diagnosed NDD group (10.7 and 12.8, respectively). The recommended treatment for ADHD is to apply a multimodal approach including medication and psychopedagogical interventions (43, 44). Early detection, prior to starting school, may lead to earlier treatment and better chance of preventing school failure and overweight (17, 24, 45).
In the present study, the results of the depressive diagnosis (see Table 3) and the depressive symptoms (see Table 6) are in line with each other. Children diagnosed with an NDD, especially pre-diagnosed NDD children, developed more often depressive symptoms. This trend is probably also driven by age, as the pre-diagnosed NDD children were older compared with the study-diagnosed children. Additionally, only in the NDD group diagnosed in the study, a positive correlation was observed between age at BYI and internalizing symptoms. The influence of age does not seem implausible (46). The prepubertal age has been found to be a special vulnerable period for children with NDD and has been linked to the increase of school and psychosocial demands that comes with an older age (47, 48). Also, for NDD subgroups, a delayed diagnosis may increase the burden of emotional problems due to lack of early adequate support (23, 24, 45). One other explanation might be a surveillance bias, as the pre-diagnosed NDD children were already followed up more closely than the other participants at the psychiatry unit. It is also possible that the higher rate of behavioral comorbidities in addition to obesity, seen in the pre-diagnosed NDD group, could add to the strain of coping with situations in everyday life such as school (38). The severity of the NDD could possibly have a negative effect on emotional development (45, 47) and, thereby, weight management, as these factors are known to have a reciprocal relationship (7). Environmental factors are other examples, such as the steroid hormone vitamin D, which modulates gene regulation decreasing the risk of developing ASD and depression (8, 49, 50). As previously mentioned, NDD as well psychiatric disorders, are found to have vitamin D deficiency (8, 9). This is also true for children with obesity (51), but the pathophysiological mechanisms are not fully understood.
In addition to psychiatric outcomes, we found for the study-diagnosed NDD group the mean delta BMI SDS from obesity treatment start to follow up to be -0.5 SDS, which is considered clinically relevant (52). At follow-up, these children had been diagnosed at the psychiatry unit and support had been initiated. The exact reason for this difference in treatment success is not known, but it could be speculated that an ADHD diagnosis may contribute to tailor the support in obesity treatment, making it more effective (4). Also, psychostimulant treatment for ADHD has been proven to yield significant weight loss (53).
Lower IQ scores in childhood have been suggested to precede the persistence of obesity in adulthood, but this relationship is plausibly mediated by educational progress (17). The mean level FSIQ for all groups fell into the average range. Still, a substantial number of the participants performed worse than expected; 28% of the total sample scored in the BIF range (12). The corresponding expected proportion in a population sample is 6.7% (27). Being identified with BIF is important for the treatment of psychiatric disorders and makes it possible to enhance adapted school situations (54).
We also found the NDD total group to score significantly lower on FSIQ than the non-NDD group. Children with ADHD as a group (regardless of their weight status) has been found to exhibit mild intellectual difficulties compared with healthy controls (55). Interestingly, we did not find any significant relationship between BMI SDS and FSIQ in the NDD groups, but in the non-NDD group, a higher BMI SDS was related to a lower FSIQ score. This finding needs further studies to understand the mechanisms behind. Additionally, children of parents with lower educational level performed more poorly on FSIQ compared to children of parents with advanced educational level. However, this was only significant when not splitting into subgroups. This suggest that it may be an underlying factor in each group but may be biased by the small sample sizes in this study. Studies with larges sample sizes are needed where cognitive function should be investigated from a more multifaceted perspective and thereby evaluating relationships between variables.
Somewhat surprising was that a higher FSIQ score (although mainly within the lower and average range) correlated with anxiety symptoms for the NDD total group. Even though intellectual difficulties have been found to place children at risk of internalizing symptoms (56, 57), a relative higher IQ may partly explain why an NDD more easily remains undetected in some children until school age. It is believed that it could compensate for and/or overshadow (“hide”) other behavioral difficulties and be one of several reasons for delaying the start of the NDD diagnosis procedure (24). A delayed diagnosis is also believed to be one of the reasons why these children develop aggregated stress and emotional problems with increasing age, as the compensatory strategies may put further strain on the child (23, 24, 58). For the NDD total group we observed associations between FSIQ, age at the start of the diagnostic evaluation process and anxiety. This may indicate an indirect effect of age when starting the NDD diagnostic procedure of anxiety symptoms, which is mediated by the FSIQ. This underlying relationship might exist in each of the two NDD subgroups, but due to insufficient sample sizes it may only emerge when the NDD groups are combined. These correlation patterns emerged despite screening one of the groups, and that may have biased the result.
Treatment adherence and school absence are known problems in childhood obesity (3, 59). Successful modification of lifestyle habits and school attendance may be hampered by interactions of emotional, cognitive, and behavioral problems (7, 60). In addition to our results of NDD, we found more than two fifths of the participants (45%) at time of study assessment to self-report anxiety and/or depression above the clinical threshold compared to norms. At follow-up, 22% were diagnosed with depression and/or anxiety disorder/s. It is known that ADHD and a depression symptomatology may overlap (restlessness, irritability, and difficulty concentrating) (61), why our findings suggest that obesity units would benefit from psychiatric competence, allowing for a broad screening of neurodevelopmental and psychiatric conditions to provide adequate support. Early recognition offers the greatest opportunities for adequate adaptations and support in the hope of avoiding worsening of the problems observed (25).
To our knowledge, this is the first study to explore and investigate NDD, psychiatric conditions and cognitive ability in children presenting for obesity treatment. Main strengths include the thorough assessment and the high participation rate (95%). Also, the NDD diagnoses were evaluated at the psychiatry unit that was not involved in this study.
A limitation is the lack of a control group, but the instruments that were used allowed comparisons with normative population data. Another limitation is the exact collection of treatment protocols and data on adherence to these. Also, 80 participants should be regarded as a small sample and the study might have been under-powered to detect important differences between the groups. Cognitive functions and psychiatric conditions were assessed, but we lack information about adaptive functioning. Furthermore, the following should be considered when interpreting the results 1) numerical scores of the Wechsler Intelligence Scales were less accessible for the pre-diagnosed NDD group 2) the study did not include all type of neurodevelopmental disorders such as intellectual developmental disorder, which may affect the results found for cognitive data 3) multiple statistical comparisons were made without correction increasing the risk for false-positive results.
The overlap between NDD, cognitive deficits and psychiatric conditions is an important observation for clinical practice. The present study accentuates regular screening of NDD and psychiatric conditions as an important part of obesity best practice and may benefit the field of personalized childhood obesity treatment.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by The Regional Ethical Review Board in Gothenburg (reg. no. 409-14). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
MD: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Visualization, Writing – original draft, Writing – review & editing. KJ: Conceptualization, Formal analysis, Methodology, Supervision, Validation, Writing – review & editing. LS: Conceptualization, Investigation, Project administration, Supervision, Validation, Writing – review & editing, Data curation. AL: Formal analysis, Methodology, Supervision, Validation, Writing – review & editing. JD: Conceptualization, Funding acquisition, Methodology, Supervision, Validation, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by regional grants from the Swedish Government (ALFGBG 719711 and 965041, VGFOUREG-860301 and 932413 and the Mary von Sydow, Rådman och Fru Ernst Collianders, Herbert and Karin Jacobssons -and Queen Silvia Jubilee Foundations.
The authors are grateful to the families that took part, to the child health care personnel at the obesity units in Kungsbacka/Varberg, especially Karin Sjunnesson, Sofia Gustafsson and Erica Håkansson, to Dr Anna Björk for conducting the start-up of the collection of data and to Associate Professor Eva Tideman, for her support with interpreting the cognitive data.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1332598/full#supplementary-material
NDD, Neurodevelopmental disorders; ESSENCE, Early Symptomatic Syndromes Eliciting Neurodevelopmental Clinical Examinations; SDS, Standard deviation score; FSIQ, Full Scale IQ; BYI, Beck Youth inventories.
1. Jebeile H, Kelly AS, O'Malley G, Baur LA. Obesity in children and adolescents: epidemiology, causes, assessment, and management. Lancet Diabetes Endocrinol. (2022) 10:351–65. doi: 10.1016/S2213-8587(22)00047-X
2. Hampl SE, Hassink SG, Skinner AC, Armstrong SC, Barlow SE, Bolling CF, et al. Clinical practice guideline for the evaluation and treatment of children and adolescents with obesity. Pediatrics. (2023) 151:e2022060640. doi: 10.1542/peds.2022-060640
3. Ball GDC, Sebastianski M, Wijesundera J, Keto-Lambert D, Ho J, Zenlea I, et al. Strategies to reduce attrition in managing paediatric obesity: A systematic review. Pediatr Obes. (2021) 16:e12733. doi: 10.1111/ijpo.12733
4. Cortese S, Moreira-Maia CR, St Fleur D, Morcillo-Penalver C, Rohde LA, Faraone SV. Association between ADHD and obesity: A systematic review and meta-analysis. Am J Psychiatry. (2016) 173:34–43. doi: 10.1176/appi.ajp.2015.15020266
5. Wentz E, Bjork A, Dahlgren J. Neurodevelopmental disorders are highly over-represented in children with obesity: A cross-sectional study. Obes (Silver Spring). (2017) 25:178–84. doi: 10.1002/oby.21693
6. Liang J, Matheson BE, Kaye WH, Boutelle KN. Neurocognitive correlates of obesity and obesity-related behaviors in children and adolescents. Int J Obes (Lond). (2014) 38:494–506. doi: 10.1038/ijo.2013.142
7. Rajan TM, Menon V. Psychiatric disorders and obesity: A review of association studies. J Postgrad Med. (2017) 63:182–90. doi: 10.4103/jpgm.JPGM_712_16
8. Muskens J, Klip H, Zinkstok JR, van Dongen Boomsma M, Staal WG. Vitamin D status in children with a psychiatric diagnosis, autism spectrum disorders, or internalizing disorders. Front Psychiatry. (2022) 13:958556. doi: 10.3389/fpsyt.2022.958556
9. Petruzzelli MG, Marzulli L, Margari F, De Giacomi A, Gabellone A, Giannico OV, et al. VitaminD deficiency in autism spectrum disorder: A cross-sectional study. Dis Markers. (2020) 2020:9292560. doi: 10.1155/2020/9292560
10. American Psychiatric Association [APA]. Diagnostic and Statistical Manual of Mental Disorders (DSM-V ed., text rev). (2022). doi: 10.1176/appi.books.9780890425787
11. Gillberg C. The ESSENCE in child psychiatry: Early Symptomatic Syndromes Eliciting Neurodevelopmental Clinical Examinations. Res Dev Disabil. (2010) 31:1543–51. doi: 10.1016/j.ridd.2010.06.002
12. Fernell E, Gillberg C. Chapter 6 - Borderline intellectual functioning. In: Gallagher A, Bulteau C, Cohen D, Michaud LJ, editors. Handbook of Clinical Neurology, vol. 174 . Elsevier (2020). p. 77–81. doi: 10.1016/B978-0-444-64148-9.00006-5
13. Sammels O, Karjalainen L, Dahlgren J, Wentz E. Autism spectrum disorder and obesity in children: A systematic review and meta-analysis. Obes Facts. (2022) 15:305–20. doi: 10.1159/000523943
14. Ahlberg R, Garcia-Argibay M, Hirvikoski T, Boman M, Chen Q, Taylor MJ, et al. Shared familial risk factors between autism spectrum disorder and obesity - a register-based familial coaggregation cohort study. J Child Psychol Psychiatry. (2022) 63:890–9. doi: 10.1111/jcpp.13538
15. Duggan EC, Garcia-Barrera M. Handbook of Intelligence: Evolutionary Theory, Historical Perspective, and Current Concepts. In: Goldenstein DPNJ, editor. Executive Functioning and Intelligence. Springer, New York (2015). p. 435–58.
16. Fergusson DM, Horwood LJ, Ridder EM. Show me the child at seven II: Childhood intelligence and later outcomes in adolescence and young adulthood. J Child Psychol Psychiatry. (2005) 46:850–8. doi: 10.1111/j.1469-7610.2005.01472.x
17. Yu ZB, Han SP, Cao XG, Guo XR. Intelligence in relation to obesity: a systematic review and meta-analysis. Obs Rev. (2010) 11:656–70. doi: 10.1111/j.1467-789X.2009.00656.x
18. Li Y, Dai Q, Jackson JC, Zhang J. Overweight is associated with decreased cognitive functioning among school-age children and adolescents. Obes (Silver Spring). (2008) 16:1809–15. doi: 10.1038/oby.2008.296
19. Xu J, Wang X, Qian C, Han W, Li X, Ding Y. Exploration of the association between obesity and cognitive impairment in chinese children with mild or moderate obstructive sleep apnea hypopnea syndrome. J Pediatr Nurs. (2020) 53:36–40. doi: 10.1016/j.pedn.2020.03.013
20. Olsson GM, Hulting AL. Intellectual profile and level of IQ among a clinical group of obese children and adolescents. Eat Weight Disord. (2010) 15:e68–73. doi: 10.3275/6983
21. Tabriz AA, Sohrabi MR, Parsay S, Abadi A, Kiapour N, Aliyari M, et al. Relation of intelligence quotient and body mass index in preschool children: a community-based cross-sectional study. Nutr Diabetes. (2015) 5:e176. doi: 10.1038/nutd.2015.27
22. Lindberg L, Hagman E, Danielsson P, Marcus C, Persson M. Anxiety and depression in children and adolescents with obesity: a nationwide study in Sweden. BMC Med. (2020) 18:30. doi: 10.1186/s12916-020-1498-z
23. Hus Y, Segal O. Challenges surrounding the diagnosis of autism in children. Neuropsychiatr Dis Treat. (2021) 17:3509–29. doi: 10.2147/NDT.S282569
24. Sonuga-Barke EJS, Becker SP, Bölte S, Castellanos FX, Franke B, Newcorn JH, et al. Annual Research Review: Perspectives on progress in ADHD science - from characterization to cause. J Child Psychol Psychiatry. (2023) 64:506–32. doi: 10.1111/jcpp.13696
25. Weisz JR, Sandler IN, Durlak JA, Anton BS. Promoting and protecting youth mental health through evidence-based prevention and treatment. Am Psychol. (2005) 60:628–48. doi: 10.1037/0003-066X.60.6.628
26. Dellenmark-Blom M, Järvholm K, Sjögren L, Levinsson A, Dahlgren J. Family screening for neurodevelopmental problems and its associations with child cognitive function enable tailored treatment for childhood obesity. Acta Paediatr. (2024). doi: 10.1111/apa.17263
27. Kaufman A, Raiford SE, Coalson D. Intelligent Testing with the WISC-V. 1st ed. Hoboken, NJ: John Wiley (2015).
28. Wechsler D. Wechsler Intelligence Scale 5th ed (WISC-V). San Antonio, TX: Psychological Corporation (2014).
29. Wechsler D. Wechsler Adult Intelligence Scale 4th ed (WAIS-IV). San Antonio, TX: The Psychological Corporation (2008). doi: 10.1037/t15169-000
30. Wechsler D. Wechsler Preschool and Primary Scale of Intelligence 3rd ed (WIPPSI-III). San Antonio, TX: The Psychological Corporation (2002). doi: 10.1037/t15177-000
31. Wechsler D. Wechsler intelligence Scale for Children, 4th ed (WISC-IV). San Antonio, TX: The Psychological Corporation (2003). doi: 10.1037/t15174-000
32. Beck JS, Beck AT, Jolly JB, Tideman E, Näswall K. Beck ungdomsskalor: manual: svensk version: [bedömning av emotionell och social problematik hos barn och ungdomar]. Stockholm: Harcourt Assessment (2007).
33. Cosgrove VE, Rhee SH, Gelhorn HL, Boeldt D, Corley RC, Ehringer MA, et al. Structure and etiology of co-occurring internalizing and externalizing disorders in adolescents. J Abnorm Child Psychol. (2011) 39:109–23. doi: 10.1007/s10802-010-9444-8
34. Karlberg J, Luo ZC, Albertsson-Wikland K. Body mass index reference values (mean and SD) for Swedish children. Acta Paediatr. (2001) 90:1427–34. doi: 10.1080/08035250152708851
36. Webbsite Andrews University, Hall S. Applied Statistics-Lesson 11: Power and Sample Size (2005). Available online at: http://www.andrews.edu/~calkins/math/edrm611/edrm11.htm (Accessed June 15, 2023).
37. Agranat-Meged AN, Deitcher C, Goldzweig G, Leibenson L, Stein M, Galili-Weisstub E. Childhood obesity and attention deficit/hyperactivity disorder: a newly described comorbidity in obese hospitalized children. Int J Eat Disord. (2005) 37:357–9. doi: 10.1002/(ISSN)1098-108X
38. Scandurra V, Emberti Gialloreti L, Barbanera F, Scordo MR, Pierini A, Canitano R. Neurodevelopmental disorders and adaptive functions: A study of children with autism spectrum disorders (ASD) and/or attention deficit and hyperactivity disorder (ADHD). Front Psychiatry. (2019) 10:673. doi: 10.3389/fpsyt.2019.00673
39. Sciutto MJ, Nolfi CJ, Bluhm C. Effects of child gender and symptom type on referrals for ADHD by elementary school teachers. J Emot Behav Disord. (2004) 12:247–53. doi: 10.1177/10634266040120040501
40. Visser SN, Danielson ML, Bitsko RH, Holbrook JR, Kogan MD, Ghandour RM, et al. Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003-2011. J Am Acad Child Adolesc Psychiatry. (2014) 53:34–46.e2. doi: 10.1016/j.jaac.2013.09.001
41. Brett D, Warnell F, McConachie H, Parr JR. Factors Affecting Age at ASD Diagnosis in UK: No Evidence that Diagnosis Age has Decreased Between 2004 and 2014. J Autism Dev Disord. (2016) 46:1974–84. doi: 10.1007/s10803-016-2716-6
42. Mandell DS, Novak MM, Zubritsky CD. Factors associated with age of diagnosis among children with autism spectrum disorders. Pediatrics. (2005) 116:1480–6. doi: 10.1542/peds.2005-0185
43. Barkley RA. Attention-deficit hyperactivity disorder: A handbook for diagnosis and treatment. 4th ed. New York: The Guilford Press (2015).
44. Felt BT, Biermann B, Christner JG, Kochhar P, Harrison RV. Diagnosis and management of ADHD in children. Am Fam Physician. (2014) 90:456–64.
45. Arnett AB, Macdonald B, Pennington BF. Cognitive and behavioral indicators of ADHD symptoms prior to school age. J Child Psychol Psychiatry. (2013) 54:1284–94. doi: 10.1111/jcpp.12104
46. Thapar A, Collishaw S, Pine DS, Thapar AK. Depression in adolescence. Lancet. (2012) 379:1056–67. doi: 10.1016/S0140-6736(11)60871-4
47. Doering S, Halldner L, Larsson H, Gillberg C, Kuja-Halkola R, Lichtenstein P, et al. Childhood onset versus adolescent-onset anxiety and depression: Epidemiological and neurodevelopmental aspects. Psychiatry Res. (2022) 312:114556. doi: 10.1016/j.psychres.2022.114556
48. Stern A, Agnew-Blais JC, Danese A, Fisher HL, Matthews T, Polanczyk GV, et al. Associations 530 between ADHD and emotional problems from childhood to young adulthood: a longitudinal 531 genetically sensitive study. J Child Psychol Psychiatry. (2020) 61(11):1234–42. doi: 10.1111/jcpp.13217
49. Petruzzelli MG, Marzulli L, Giannico OV, Furente F, Margari M, Matera E, et al. Glucose metabolism, thyroid function, and prolactin level in adolescent patients with first episode of schizophrenia and affective disorders. Front Psychiatry. (2020) 11:775. doi: 10.3389/fpsyt.2020.00775
50. Yasumitsu-Lovell K, Thompson L, Fernell E, Eitoku M, Suganuma N, Gillberg C, et al. Vitamin D deficiency associated with neurodevelopmental problems in 2-year-old Japanese boys. Acta Paediatr. (2024) 113:119–26. doi: 10.1111/apa.16998
51. Zakharova I, Klimov L, Kuryaninova V, Nikitina I, Malyavskaya S, Dolbnya S, et al. Insufficiency in overweight and obese children and adolescents. Front Endocrinol (Lausanne). (2019) 10:103. doi: 10.3389/fendo.2019.00103
52. Reinehr T, Lass N, Toschke C, Rothermel J, Lanzinger S, Holl RW. Which amount of BMI-SDS reduction is necessary to improve cardiovascular risk factors in overweight children? J Clin Endocrinol Metab. (2016) 101:3171–9. doi: 10.1210/jc.2016-1885
53. Fast K, Björk A, Strandberg M, Johannesson E, Wentz E, Dahlgren J. Half of the children with overweight or obesity and attention-deficit/hyperactivity disorder reach normal weight with stimulants. Acta Paediatr. (2021) 110:2825–32. doi: 10.1111/apa.15881
54. Fernell E, Ek U. Borderline intellectual functioning in children and adolescents - insufficiently recognized difficulties. Acta Paediatr. (2010) 99:748–53. doi: 10.1111/j.1651-2227.2010.01707.x
55. Frazier TW, Demaree HA, Youngstrom EA. Meta-analysis of intellectual and neuropsychological test performance in attention-deficit/hyperactivity disorder. Neuropsychology. (2004) 18:543–55. doi: 10.1037/0894-4105.18.3.543
56. Weeks M, Wild TC, Ploubidis GB, Naicker K, Cairney J, North CR, et al. Childhood cognitive ability and its relationship with anxiety and depression in adolescence. J Affect Disord. (2014) 152-154:139–45. doi: 10.1016/j.jad.2013.08.019
57. Emerson E, Hatton C. The mental health of children and adolescents with learning disabilities in britain. Adv Ment Health Learn Disabil. (2007) 1:62–3. doi: 10.1192/bjp.bp.107.038729
58. Arnett AB, Pennington BF, Willcutt EG, DeFries JC, OlsoN RK. Sex differences in ADHD symptom severity. J Child Psychol Psychiatry. (2015) 56:632–9. doi: 10.1111/jcpp.12337
59. An R, Yan H, Shi X, Yang Y. Childhood obesity and school absenteeism: a systematic review and meta-analysis. Obes Rev. (2017) 18:1412–24. doi: 10.1111/obr.12599
60. Gren Landell M. School attendence problems: A research update and where to go. Stockholm: Jerringfonden (2021).
Keywords: obesity, neurodevelopmental disorders, intellectual ability, cognition, depression, anxiety, psychiatric disorders
Citation: Dellenmark-Blom M, Järvholm K, Sjögren L, Levinsson A and Dahlgren J (2024) Neurodevelopmental disorders in children seeking obesity treatment- associations with intellectual ability and psychiatric conditions. Front. Psychiatry 15:1332598. doi: 10.3389/fpsyt.2024.1332598
Received: 03 November 2023; Accepted: 08 July 2024;
Published: 19 August 2024.
Edited by:
Li Yang, Peking University Sixth Hospital, ChinaReviewed by:
Maria Giuseppina Petruzzelli, University of Bari Aldo Moro, ItalyCopyright © 2024 Dellenmark-Blom, Järvholm, Sjögren, Levinsson and Dahlgren. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maria Dellenmark-Blom, bWFyaWEuZGVsbGVubWFyay5ibG9tQGd1LnNl
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.