- 1School of Public Health, Faculty of Health, University of Technology Sydney, Sydney, NSW, Australia
- 2Department of Psychiatry, Faculty of Health Sciences, Madda Walabu University, Shashemene, Ethiopia
- 3School of Public Health and Social Work, Faculty of Health, Queensland University of Technology, Brisbane, QLD, Australia
Background: The use of substances such as alcohol, tobacco, khat, or drugs among young people is becoming a public health concern globally, with particularly high prevalence rates in low and middle-income settings, where socio-cultural and economic factors contribute to distinct challenges in addressing this problem. This review aimed to summarize the current literature on the prevalence of substance use among young people in sub-Saharan Africa (SSA) and identify gaps in the current body of literature.
Methods: Seven databases and Google were searched for studies reporting on substance use prevalence among young people (aged 10-24 years) in SSA, published between January 2010 and May 2024. Observational studies were included, assessed for methodological quality, and checked for the presence of heterogeneity and publication bias using standard methods. A random effect model was used to estimate the pooled proportions for substance use among young people.
Results: The literature search identified 1,889 hits from the databases and Google. Among these 60 eligible studies involving 83,859 respondents were included in the review. The overall lifetime, 12-month, and current prevalence of any substance use among young people in SSA was found to be 21.0% (95% CI= 18.0, 24.0), 18% (95% CI=10,27), and 15% (95% CI=12,18), respectively. Among young people from SSA, alcohol use problem was the most prevalent (40%), followed by khat use (25%), stimulant use (20%), and cigarette smoking (16%). Other substances used by a smaller proportion of young people included cannabis, cocaine, inhalants, sedatives, shisha, hallucinogens, steroids, and mastics. The prevalence of substance use problems was higher among males compared to females, highest in the southern African region followed by Western and Eastern regions, and in community-based studies compared to institutional-based studies.
Conclusions: In SSA, over a fourth of young people use at least one substance in their lifetime, with higher rates among males than females and in community-based compared to institution-based studies. These results emphasize the need for interventions targeting the wider young population and those in specific subgroups identified as being at higher risk of substance use. This approach allows for the provision of tailored support and resources to those who need it most while also promoting positive health outcomes for the entire population of young people in the region.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022366774, identifier CRD42022366774.
Introduction
Young people, defined as individuals aged 10-24 years (1), constitute a significant portion of the global population (24%), estimated at approximately 1.9 billion (2). This demographic is primarily concentrated in low- and middle-income countries (LMICs), where 90% of young people reside (2). Sub-Saharan Africa (SSA) is home to one of the largest and fastest-growing populations of young people, with individuals in this age group making up over 60% of the region’s total population (3). This demographic presents both a potential for economic growth and a challenge in terms of public health and social issues, including substance use (4).
Substance use among young people is a critical public health concern globally, significantly contributing to the burden of disease (5). The Global Burden of Disease (GBD) study identifies substance use disorders (SUDs) as major contributors to morbidity and mortality among young people (6). In SSA, the situation is particularly alarming (7–9). Recent data indicates a rising trend in substance use among adolescents in this region, with substantial implications for their health and well-being (7, 10).
Several risk factors contribute to substance use among young people. These include socio-economic factors such as poverty, unemployment, and lack of education, as well as social and environmental influences like peer pressure, family dynamics, and the availability of substances (11, 12). Additionally, psychological factors such as stress, trauma, and mental health play a significant role (13, 14). Understanding these risk indicators is crucial for developing effective prevention and intervention strategies.
The consequences of substance use among young people are profound and multifaceted. Substance use is associated with a range of risky behaviors, including unprotected sex, violence, and criminal activities (8, 15), directly and indirectly leading to an increase in the likelihood of poor health outcomes, such as sexually transmitted infections (STIs), injuries, and mental health disorders (15–17). Furthermore, substance use can lead to chronic conditions, contributing to long-term morbidity and premature mortality (18, 19). The impact extends beyond individual health, affecting families, communities, and broader societal structures (20).
The present review aimed to address the need for a comprehensive understanding of substance use among young people in SSA. While previous reviews have provided valuable insights in this area, some of them focused on specific countries (12, 21, 22), while others focused on adolescents (10-19 years of age) (10), or on specific substances of use (23, 24). This systematic review and meta-analysis sought to fill the gap by offering a region-wide perspective on the prevalence and risk factors of substance use among young people (covering both adolescents and youth) in SSA. By addressing these gaps, the study will contribute to the understanding of substance use in SSA, informing policy and programmatic responses to mitigate this pressing public health issue among young people.
Materials and methods
Protocol and registration
This review was prepared and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2015 guideline (25). The protocol was registered on the International Prospective Register of Systematic Reviews under CRD42022366774.
Search strategy
Studies published between January 1, 2010, and May 31, 2024, were searched through a comprehensive search in the following databases: African Journals Online (AJOL), PubMed, ProQuest, PsycINFO, Web of Science, Scopus, and African Index Medicus (AIM) library. The chosen databases are widely used for indexing publications in health and substance use, have search functions appropriate for conducting systematic reviews, are generally perceived as trustworthy within academia, and index a large number of journals that include work published in our geographic area of interest (SSA). The body of knowledge in the fields of health and behavioral sciences changes quickly with the acquisition of new knowledge, discoveries, theories, processes, or best practices, and there is a need to share the most recent evidence with practitioners in those fields. Accordingly, our systematic review aimed to provide a synthesis of recent evidence published in the last 14 years in the area of substance use for practitioners, policymakers, clinical practice guideline developers, program designers, and those designing and justifying primary research.
Additional searches were made using the Google search engines, including using the reference lists of identified original research. Comprehensive search terms were designed using Medical Education Subject Heading (MeSH) and keywords, were primarily developed for the PubMed search protocol and applied for other databases as well. Details of the search terms and strategies used are included in the Supplementary Material (Supplementary Material S1).
Inclusion and exclusion criteria
This review considered all observational study designs, including case-control, cohort, and cross-sectional studies, that empirically investigated the prevalence and patterns of substance use among young individuals aged 10-24 years. Young people were defined as those from 10 to 24 years of age, encompassing both adolescents and youths (1, 26). Studies published in English between January 1, 2010, and May 31, 2024, and involving human subjects were eligible for inclusion. The review excluded anonymous reports, letters, editorials, brief communications, comments, and reviews.
Study selection
The articles retrieved were initially loaded into the EndNote program, where authors identified and removed the duplicates. Subsequently, the remaining articles were exported to Covidence for title, abstract, and full-text screening. Each screening stage adhered to the predetermined eligibility criteria. JE conducted the screening, with ongoing discussions among the authors to ensure consistency and consensus at each step. Any minor disagreements that arose in the screening and review process were resolved by discussion.
Data extraction
A standardized data extraction format was adapted from the Joanna Briggs Institute (JBI) data extraction format (27), and implemented in a Microsoft Excel sheet version 365. The data extracted included the following information: author/s, publication year, study location (country), study design, sample size, gender distribution, participant age, types of substances used, prevalence of substance use, tools used to measure substance use, associated factors, and common reasons for use substance (Table 1). JE extracted the required study parameters or information from the included studies, with all authors closely collaborating at each step.
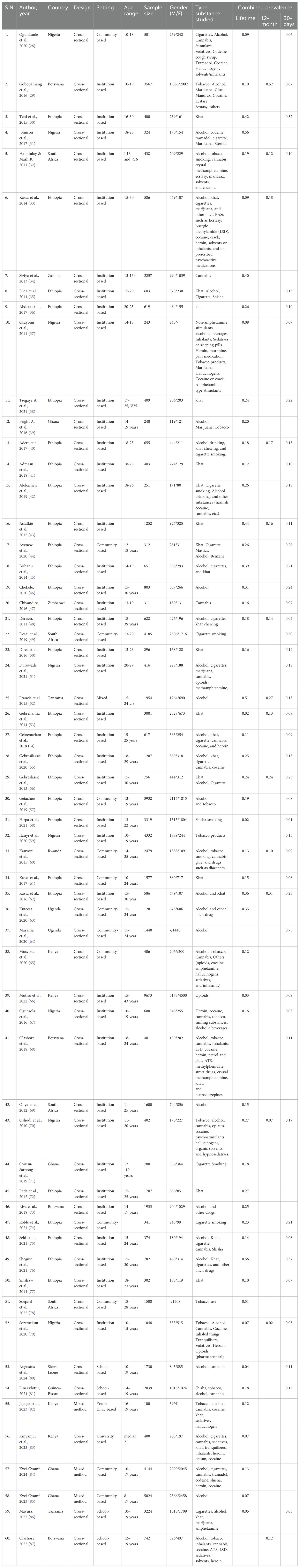
Table 1. Summary characteristics of studies included in the systematic review and meta-analysis of the prevalence of any substance use among young people in sub-Saharan Africa.
Quality appraisal
The quality assessment was primarily done by JE and DD, supplemented via discussions among the authors. The JBI Meta-Analysis of Statistics Assessment and Review Instrument (JBI-MAStARI) quality assessment tool (27) was used to assess quality. JBI-MAStARI tools are among the most commonly used scales for assessing quality, and risk of bias for cross-sectional, cohort, case-control, qualitative, and observational studies (88) (Supplementary Material S2). The appraisal aims to assess the methodological robustness of a study and its effectiveness in addressing the potential bias in the design, conduct, and analysis. All papers chosen for the review were subject to an appraisal based on the scoring guide. Scores were awarded for each criterion as follows: 0 = not fulfilling the criteria; 1 = fulfilling the criteria. The scores of each criterion added up and the result ranged from 0- 9. Those studies with a score above the mean for methodological quality appraisal were included in the review. The scoring relied on JBI guidance notes (88) as well as the judgment and expertise of our review team. Studies with a score below the mean were considered unfit and excluded from the review. Features considered to report as low quality include unmentioned study sample size determination, insufficient sample size, and absence of statistical evaluation on the reliability and validity of relevant assessment tools among others (Supplementary Material S3).
Data analysis and synthesis
The results of this review were organized to include descriptive characteristics of the study, a narrative synthesis of findings organized by subgroups, and a meta-analysis result.
The meta-analysis was conducted using Stata Version 18 statistical software to estimate the effect sizes using a standard error (SE) and 95% confidence interval (CI). To estimate the overall prevalence of substance use, the lifetime, one-year, and current prevalence data from each study were combined, along with their corresponding SE. Lifetime prevalence was defined as the use of a substance at least once in an individual’s lifetime, 12-month prevalence was the use of a substance at any time during the past year, and current prevalence was the use of substances within the past 30 days before data collection. Accounting for the potential overlap between the different substance uses, the combined (overall) prevalence from each study were computed first. Then, the overall prevalence in the three reporting patterns (lifetime, current, and 12 months) was analyzed separately using the combined prevalence and their corresponding SE.
A random effect model, which accounts for potential heterogeneity (89), was used to estimate the pooled effects in the meta-analysis. A forest plot was utilized to illustrate the combined estimate with the 95% CI. Heterogeneity among the studies was assessed through visual inspection of the forest plots and quantified using the I² statistic (90, 91). Heterogeneity levels were classified as low (I² = 25%), moderate (I² = 50%), and high (I² = 75%) based on I² statistics (91). Publication bias was assessed using Egger’s test, with a p-value of less than 0.05 indicating possible publication bias (91).
Furthermore, to minimize random variations between each primary study, sub-group analysis was undertaken by the region and country where a study collected empirical data (east, south, and west Africa); sex of study participants (male, female); year of publication; as well as the study setting type (community-based versus institution-based). These variables were selected due to their inclusion in the majority of reviewed studies.
Results
Search results
The search yielded 1,948 hits from the databases with an additional 166 articles identified through Google searches. After excluding duplicates and studies that did not meet the review inclusion criteria, 79 studies were eligible for review. Out of these, 19 were judged to be of poor methodological quality and excluded. The types of features deemed to present low methodological quality were: no mention of the study sample size determination, insufficient sample size, and a lack of statistical assessment regarding the reliability and validity of relevant measurement tools among others. The remaining 60 were considered for full review (see Figure 1).
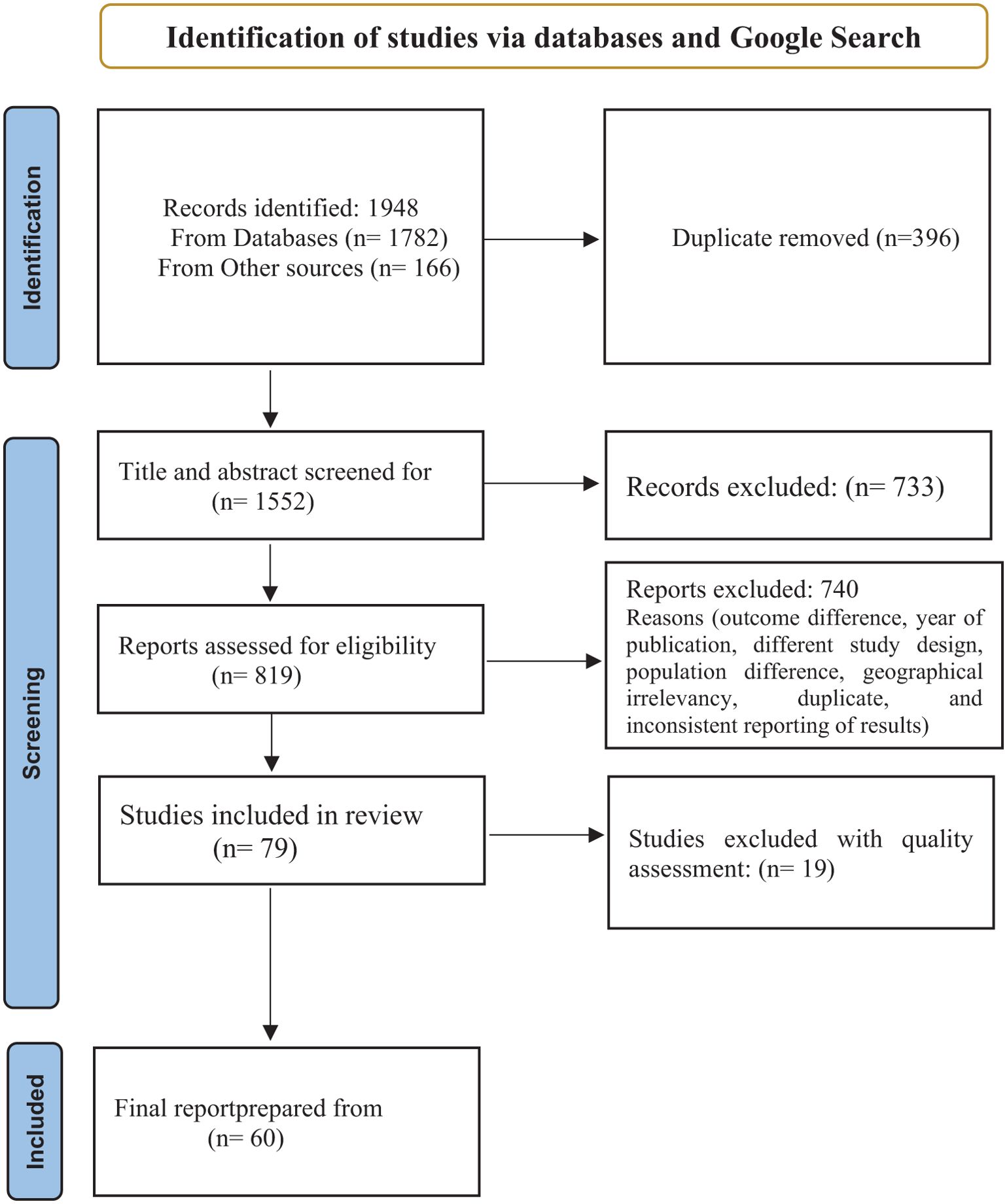
Figure 1. Flow diagram of the studies included in the systematic review and meta-analysis of substance use among young people in Sub-Saharan Africa.
General characteristics of the reviewed studies
The total sample size across the included studies was 83,859 respondents, with 54.0% male, and 46.0% female. Sample sizes in individual studies ranged from 100 (82) to 9,742 (66) participants.
The review considered studies focused on the prevalence of substance use (lifetime, 12-month, and current) among young individuals, with almost all being cross-sectional empirical studies.
Concerning publication trends, Figure 2 shows a relative increase in publication trends on substance use over the last five years in SSA.
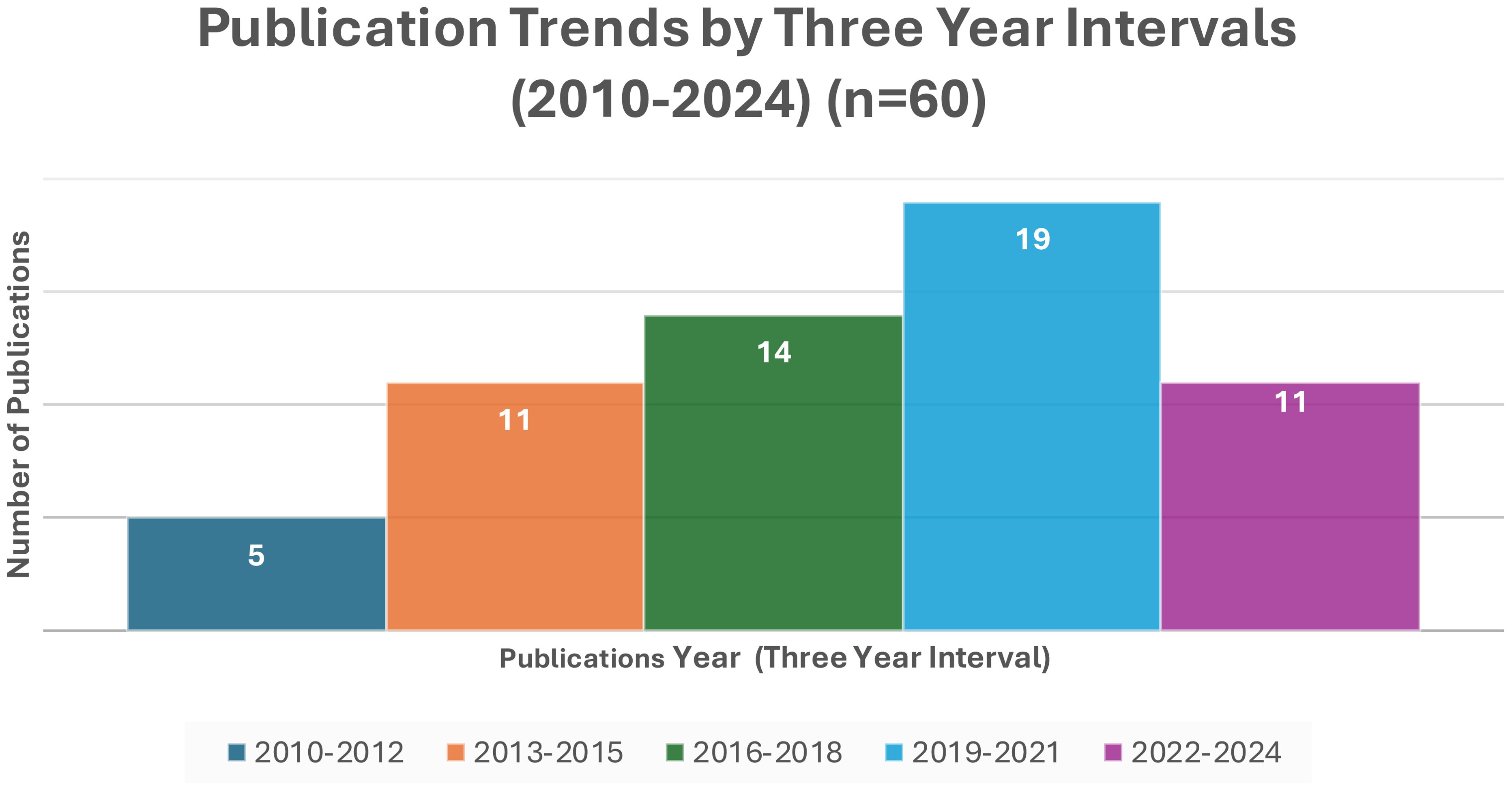
Figure 2. Trends in the publication of substance use studies in three years interval from 2010-2024.
As shown in Table 1, among the reviewed studies, alcohol was the most frequently reported (n=41), followed by cigarette smoking (n=36), khat use (n=28), and cannabis use (n=26), among other substances.
Most studies were conducted in educational institutions, with forty-six studies in schools, universities, and student clinics, and thirteen studies in community settings. Additionally, one study had a mixed population from schools, colleges, local industries, and casual laborers (see Table 1).
To measure substance use, 24 (40.0%) studies employed standardized tools such as the Alcohol, Smoking and Substance Involvement Screening Test (92) (ASSIST), CAGE (93), Alcohol Use Disorders Identification Test (AUDIT) (94), Cannabis Abuse Screening Test (CAST) (95), and the Global Student Drug Use Survey questionnaire (96), while 36 (60.0%) studies used questionnaires adapted from previous literature.
Prevalence of substance use
In general, the prevalence of substance use varied widely among studies, ranging from 2% (95% CI=1.0, 2.0) (58) in a study from Ethiopia to 56.0% (95% CI=51.0, 62.0) (31) in a study from Nigeria.
Lifetime prevalence
The lifetime prevalence of any substance use, pooled from 53 studies, was 21.0% (95% CI= 18.0, 24.0) (Figure 3). Regionally, Southern Africa had the highest lifetime prevalence at 25.0% (95% CI=13.0, 37.0), followed by East Africa at 22.0% (95% CI=18.0, 26.0), and West Africa at 17.0% (95% CI=13.0, 21.0). Country-specific data showed Zambia with the highest lifetime prevalence at 40.0% (95% CI=38.0, 42.0) and Sierra Leone the lowest at 4.0% (95% CI=3.0, 5.0). Analysis by study setting where participants were recruited showed a pooled lifetime prevalence of 20.0% in both community and institutional settings (Figure 4).
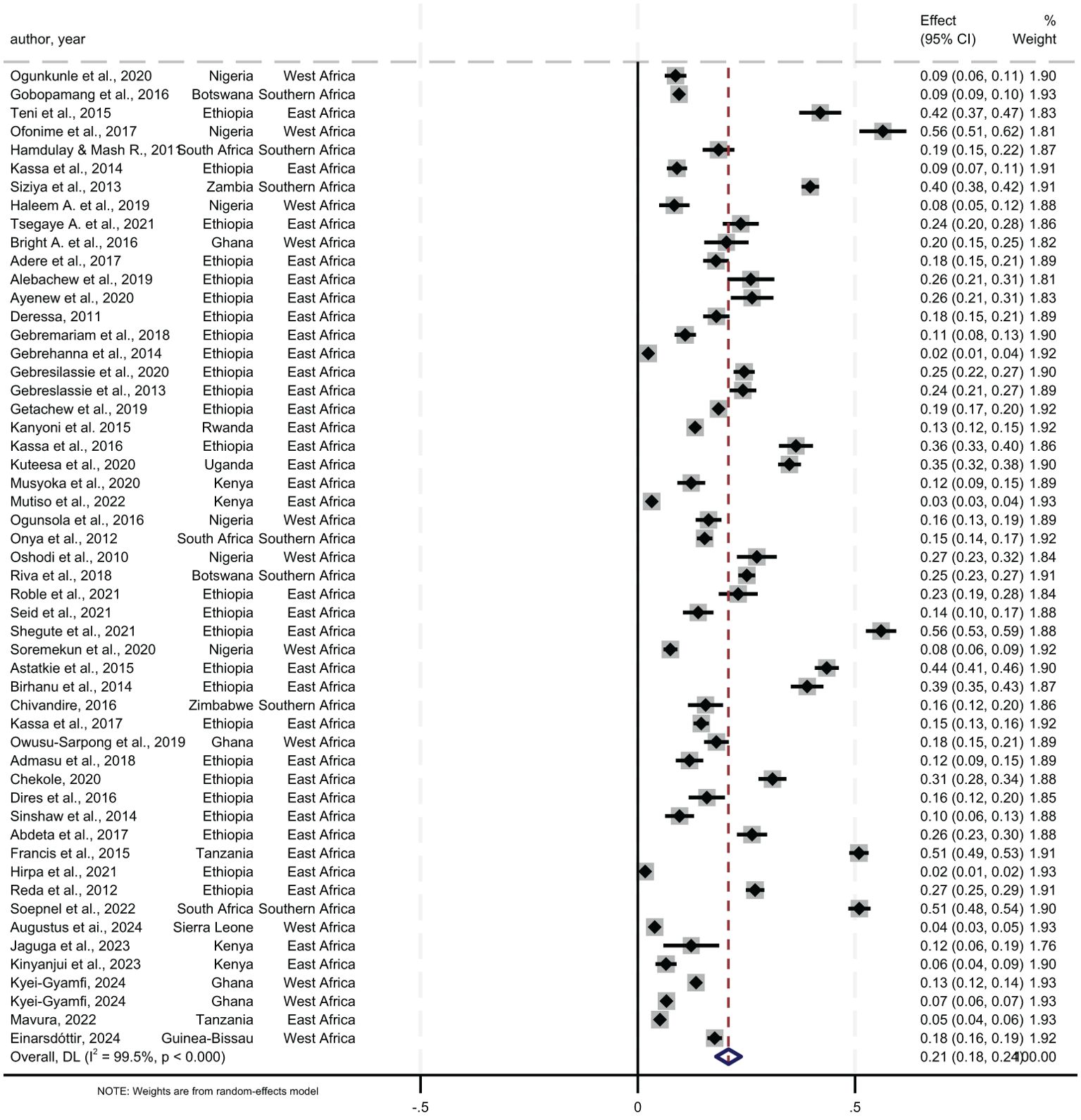
Figure 3. Pooled lifetime prevalence of any substance use among young people in sub-Saharan Africa, 2024.
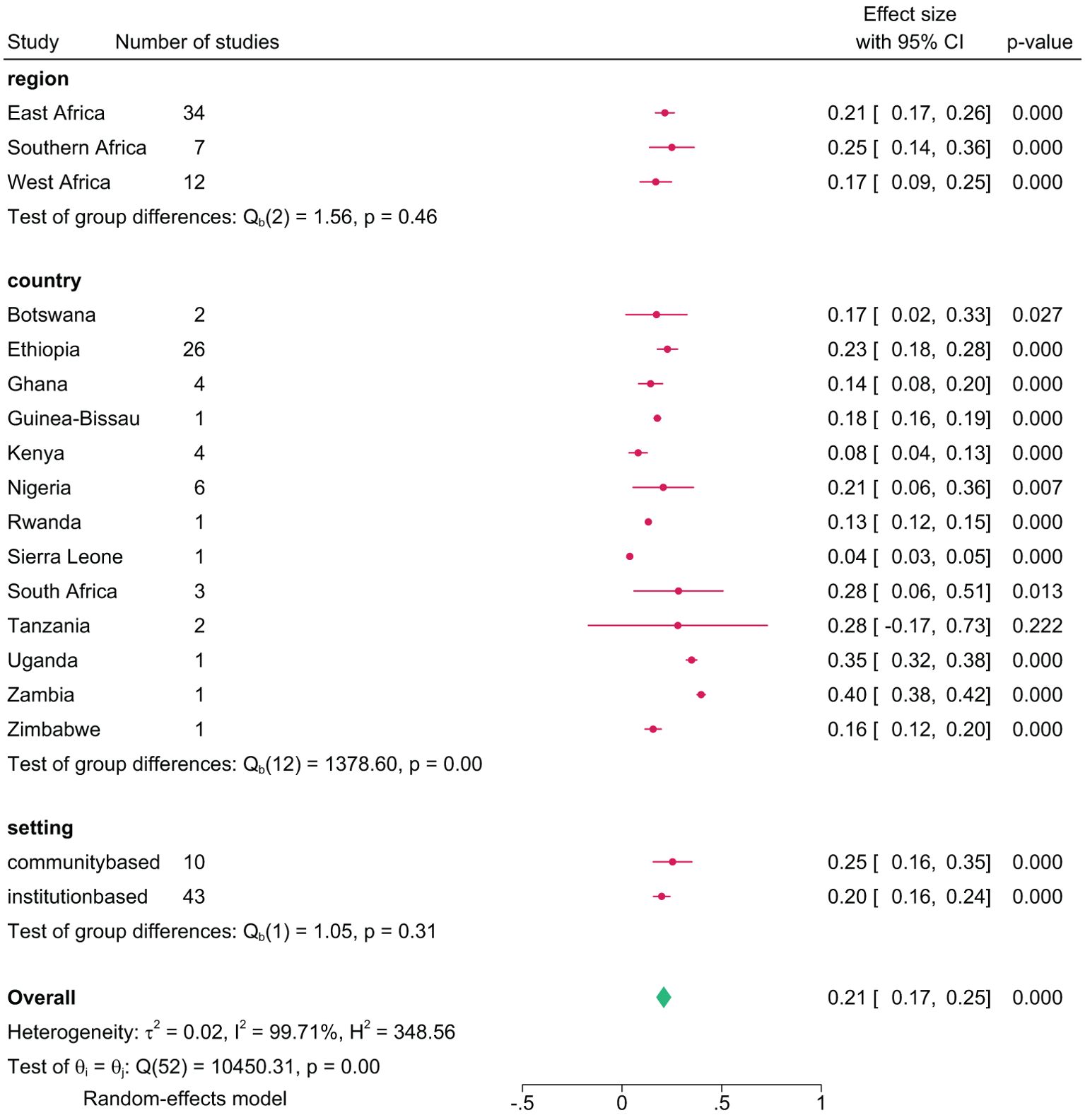
Figure 4. Pooled lifetime prevalence of any substance use among young people in sub-Saharan Africa by subgroup, 2024.
Current prevalence
The pooled current prevalence of any substance use was 15.0% (95% CI=12.0, 18.0), with the lowest at 2.5% (95% CI=1.6, 3.4) (79) and the highest at 75.0% (95% CI=73.0, 78.0) (64) from individual studies (Figure 5). In a further analysis by region, East Africa had the highest current prevalence at 17.4% (95% CI=13.0, 22.0), followed by Southern Africa, 17.1% (95% CI=3.0, 37.0), and West Africa at 10.0% (95% CI=6.0, 14.0). Among countries, the highest current prevalence was recorded in Uganda at 75.0% (95% CI=73.0, 78.0) and the lowest in Zimbabwe at 7.0% (95% CI=5.0, 10.0). Additional analysis by study setting showed a pooled current prevalence of 15.0% (95% CI=11.0, 19.0), with 26% from community-based studies and 13.0% from institution-based studies (Figure 6).
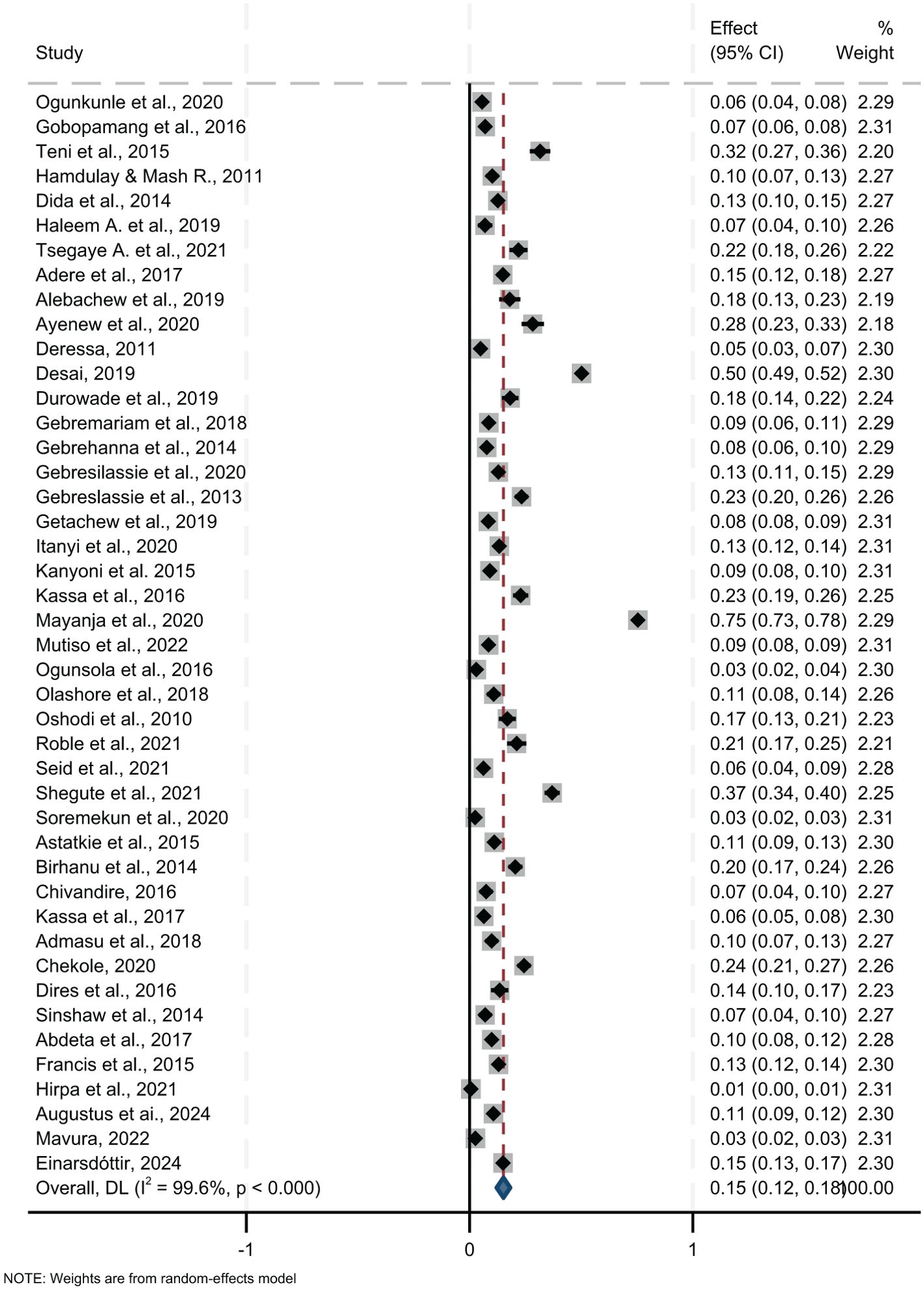
Figure 5. Pooled current prevalence of any substance use among young people in sub-Saharan Africa, 2024.
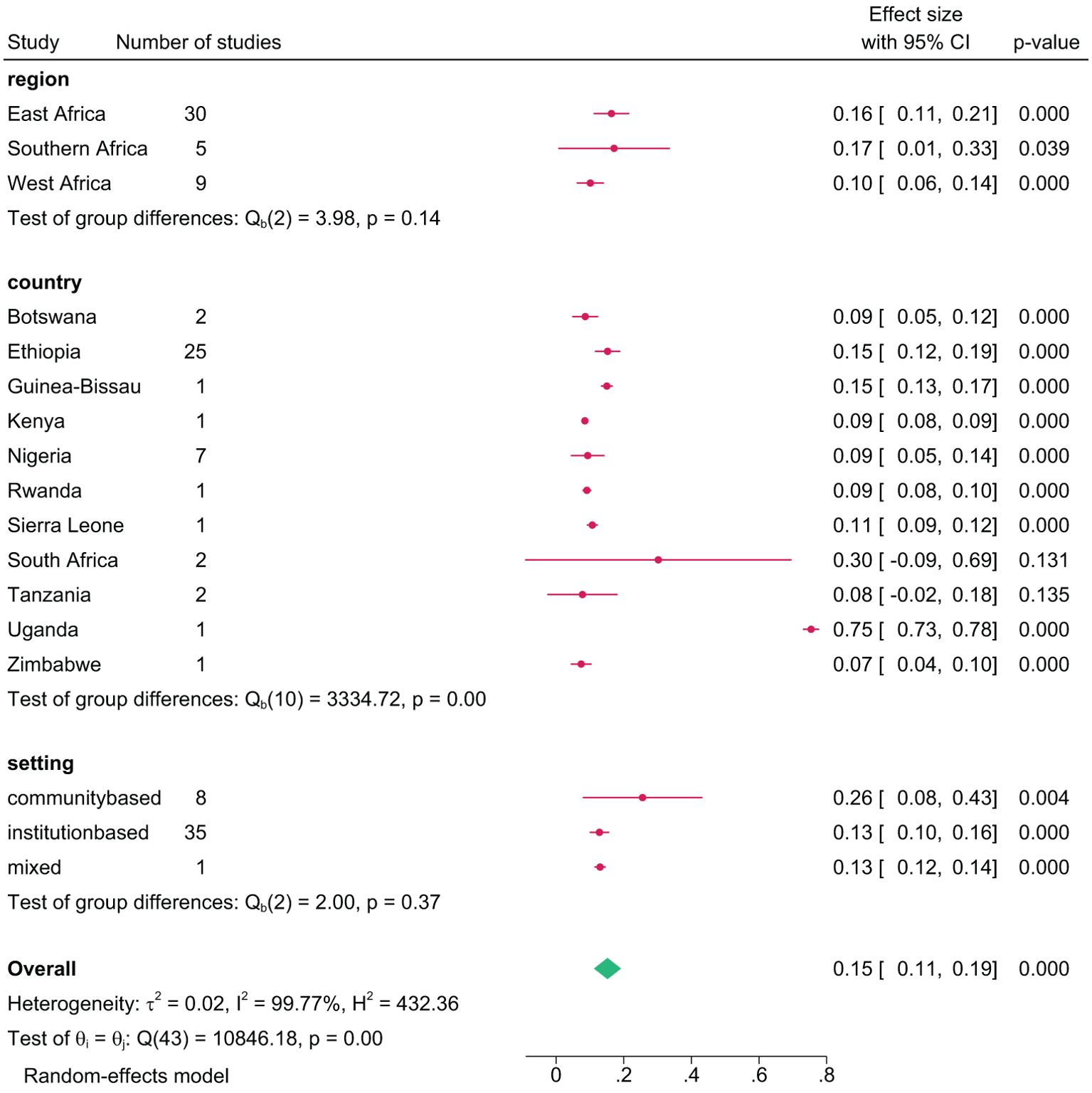
Figure 6. Pooled current prevalence of any substance use among young people in sub-Saharan Africa by subgroup, 2024.
12-month prevalence
The 12-month prevalence of any substance, pooled from 14 studies, was 18.0% (95% CI=10.0, 27.0) (Figure 7). Botswana had the highest 12-month prevalence at 32.0% (95% CI=7.0, 71.0), and Nigeria lowest at 4.0% (95% CI=1.0, 10.0). Further group analysis by region showed the lowest 12-month prevalence in West Africa at 4.0% (95% CI=1.0, 10.0), and the highest in Southern Africa at 25% (95% CI=4.0, 55.0) (Figure 8). The review showed a pooled 12-month prevalence of 18.0% (95% CI=11.0, 26.0) in institution-based studies and 10.0% (95% CI=9.0, 11.0) in community-based studies (Figure 8).
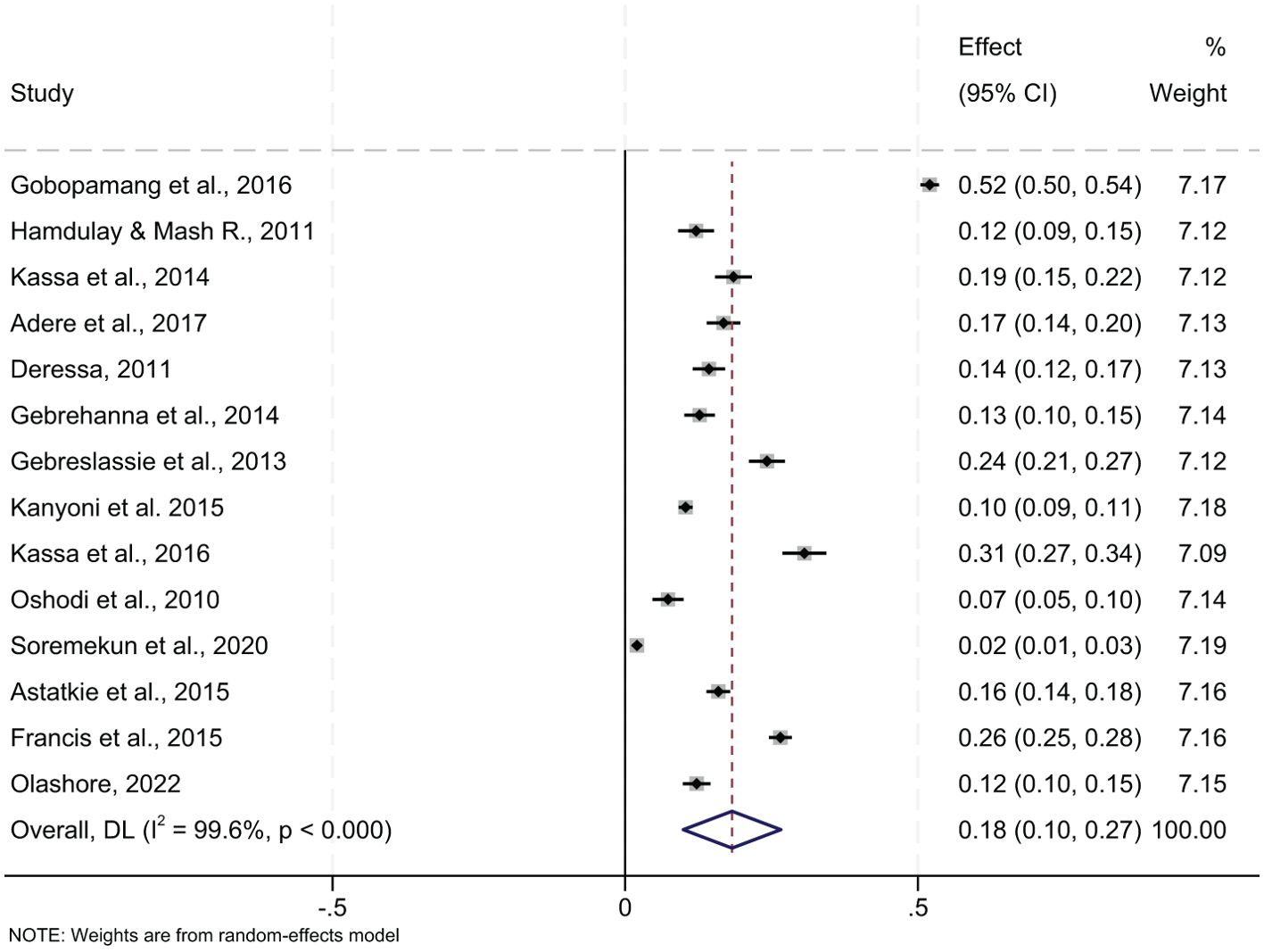
Figure 7. Pooled 12-months prevalence of any substance use among young people in sub-Saharan Africa, 2024.
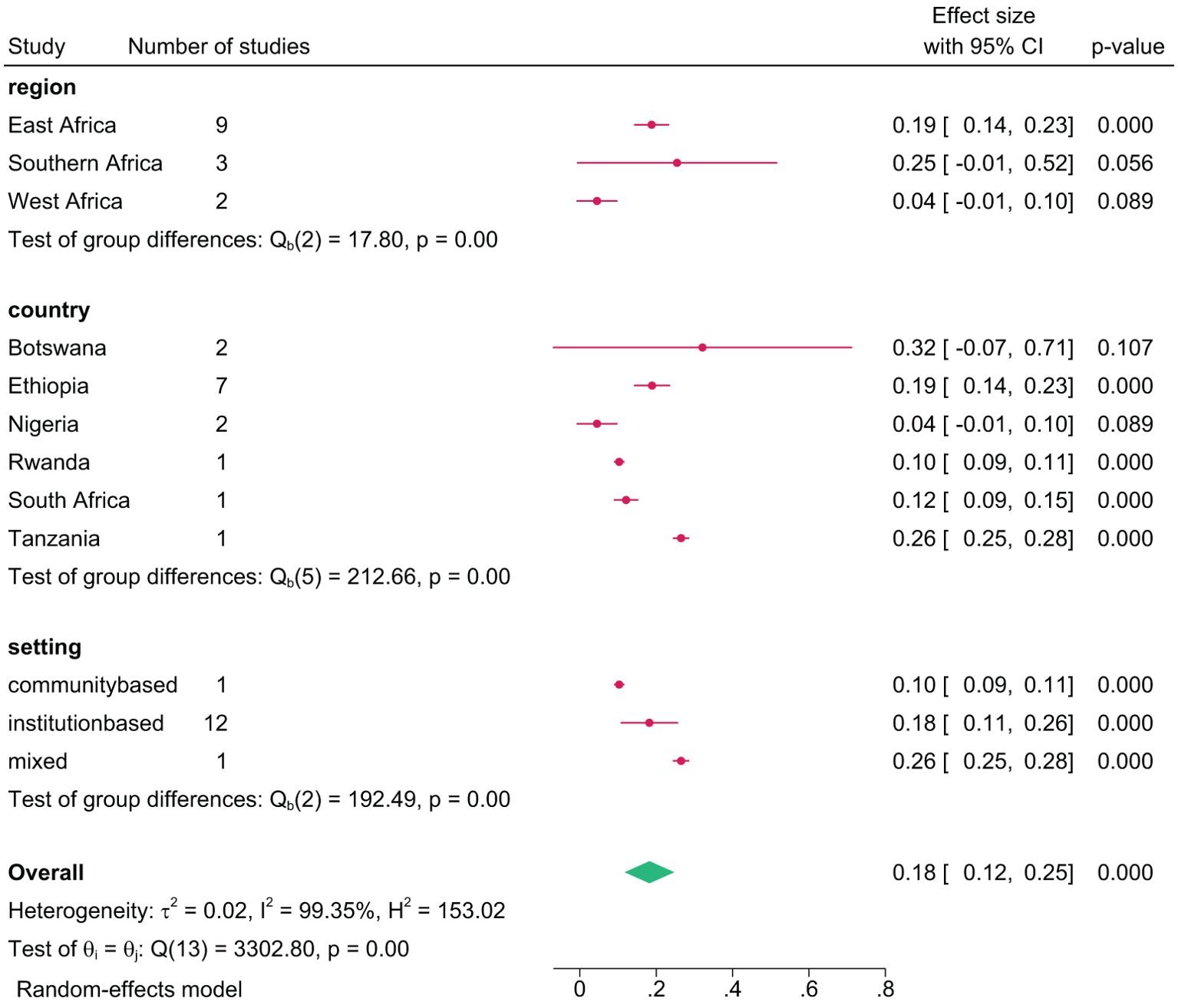
Figure 8. Pooled 12-months prevalence of any substance use among young people in sub-Saharan Africa by subgroup, 2024.
Prevalence of specific substances
Alcohol consumption
The lifetime prevalence of alcohol use, pooled from 39 studies, was 36.2% (95% CI=29.4, 43.0). The prevalence was higher in Uganda at 51.4% (95% CI=48.3, 53.7), followed closely by Rwanda, at 50.6% (95% CI= 49.0, 53.0), while it was comparatively lower in Botswana at 29.0% (95% CI=3.5, 54.5). Alcohol prevalence in individual studies ranged from 2.0% (95% CI=2.0, 2.0) (58) to 69.0% (95% CI=67.0, 71.0) (78). Furthermore, gender-disaggregated data from 19 studies showed a higher lifetime prevalence among males, 45.9% (95% CI=32.5, 59.4) compared to females, 25.6% (95% CI=18.6, 32.7).
The pooled current prevalence of alcohol use, based on 35 studies, was 23.6% (95% CI=19.1, 28.2). Among studies with gender-disaggregated data, 10 reported a prevalence of 48.7% (95% CI=27.8, 32.7) among males and 14.3% (95% CI=9.9, 18.7) among females.
The pooled 12-month prevalence of alcohol use, based on 10 studies, was 30.0% (95% CI=17.0, 44.0). Similarly, pooled data from 10 studies on 12-month prevalence showed 58.9% (95% CI=40.8, 76.9) among males and 25.0% (95% CI=16.4, 33.7) among females. The highest 12-month alcohol use prevalence was recorded in South Africa at 41.0% (95% CI=36.4, 45,6), and the lowest in Nigeria at 3.0% (95% CI=0.3, 0.9).
Cigarette use
The pooled lifetime prevalence of cigarette use, from 36 studies, was 15.2% (95% CI=12.5, 17.9). Country-specific analysis showed highest lifetime cigarette use in South Africa at 30.4% (95% CI=7.6, 53.2) and lowest in Tanzania at 7.6% (95% CI=6.7, 8.5). Prevalence reported by individual studies ranged from 1.0% (95% CI=0.1, 2.0) (41) to 49.7% (95% CI=45.0, 54.4) (78). Gender-disaggregated data from 14 studies showed a higher lifetime prevalence in males at 36.6% (95% CI=15.4, 57.7) compared to females at 10.7% (95% CI=7.2, 14.3).
The pooled current prevalence of cigarette use, based on 31 studies, was 11.8% (95% CI=8.8, 14.8). Among these, 9 studies provided gender-disaggregated data, showing a current prevalence of 27.7% (95% CI=11.1, 44.3) in males and 8.1% (95% CI=3.1, 13.2) in females. By country, South Africa had a higher current prevalence at 42.7% (95% CI=28.0, 57.4), while Tanzania had a lower prevalence at 4.0% (95% CI=3.3, 4.7).
For 12-month prevalence, the pooled estimate from 12 studies was 12.5% (95% CI=7.8, 17.2). Regionally, data from 7 studies showed a higher 12-month prevalence in South Africa at 36% (95% CI=31.0, 41.0) and lower in West Africa at 2.0% (95% CI=0.1, 4.0). Additionally, 3 studies (32, 40, 56) reported 12-month prevalence rates of 50.0% (95% CI=0.1, 100.0) among males and 22.5% (95% CI=2.0, 43.0) among females.
Khat use
The pooled lifetime prevalence of khat use, from 28 studies, was 23.0% (95% CI=16.9, 29.1). Country-specific analysis showed higher lifetime khat consumption in Ethiopia at 25.8% (95% CI=20.3, 31.3) and lower in Tanzania at 2.0% (95% CI=1.2, 2.8). The lifetime prevalence reported by individual studies ranged from 2.0% (95% CI=1.2, 2.8) (86) to 63.0% (95% CI=58.3, 67.7) (44). The current and 12-month prevalence of khat was 17.3% (95% CI=13.4, 21.1) and 16.0% (95% CI:16.0, 21.0), respectively. Generally, the lifetime, 12-month, and current prevalence of khat use were higher among males than females: 51.0% (95% CI: 31.0, 70.0), 48.0% (95% CI: 12.0, 84.0), and 51.0% (95% CI: 31.0, 71.0) for males, compared to 13% (95% CI: 9.0, 17.0), 9% (95% CI: 5.0, 13.0), and 14% (95% CI: 10.0, 18.0) for females, respectively.
Cannabis use
The pooled lifetime prevalence of cannabis use was 11.0% (95% CI=9.0, 13.0), with the highest recorded in Zambia at 37.0% (95% CI=35.0, 39.0) and the lowest in Tanzania at 1.0% (95% CI=0.7, 1.3). The lifetime prevalence reports from individual studies ranged from 0.5% (95% CI=0.1, 2.0) (41) to 61.0% (95% CI=58.0, 64.0) (43). Among nine studies with gender-disaggregated data, the pooled lifetime prevalence of cannabis use was 26.0% (95% CI=3.0, 48.0) among males and 18.0% (95% CI=10.0, 26.0) among females. The current pooled prevalence of cannabis use, based on 17 studies, was found to be 3.7% (95% CI=2.7, 4.7), while the 12-month prevalence, from 5 studies, was 6.0% (95% CI=3.0, 9.0).
Cocaine use
Twelve studies in the review reported a lifetime cocaine use prevalence of 3.0% (95% CI=2.0, 3.0) among young people. The highest prevalence was recorded in Botswana at 6.0% (95% CI=5.3, 6.7) (29), and the lowest was in South Africa at 1.0% (95% CI=0.1, 1.9) (32). The lifetime prevalence of cocaine use reported in individual studies range from 1.0% (95% CI=0.1, 2.0) (32) to 6.0% (95% CI=5.0, 7.0) (29). For the current and 12-month period, the prevalence of cocaine use was 0.8% (95% CI=0.4, 1.1) and 1.3% (95% CI=0.4, 2.3) respectively.
Shisha use
Seven studies (33, 54, 58, 72, 74, 81, 84) reported the lifetime prevalence of shisha use, and four studies (35, 36, 58, 81) reported the current prevalence. The pooled lifetime prevalence was 8.4% (95% CI=5.4, 11.8), and the pooled current prevalence was 6.2% (95% CI:0.3, 12.2).
Hallucinogens
This group includes studies reporting on hallucinogens and LSD (Lysergic Acid Diethylamide). The lifetime prevalence of hallucinogen pooled from 6 studies, was 3.0% (95% CI=1.0, 5.0), ranging from 1.0% in Kenya (82) to 7.0% in Ethiopia (44). Only one study from Ethiopia (44) reported a lifetime prevalence of 0.5% among males and 3.0% among females. The current prevalence of hallucinogens, based on 3 studies (32, 44, 97), was found to be 2.2% (95% CI=0.7, 3.6).
Sedatives
Fifteen studies reported on sedative use prevalence (tranquilizers, sedatives, and Mandrax). The pooled lifetime prevalence of sedative use was 8.9% (95% CI=7.0, 10.8), with individual study reports ranging from 0.1% (95% CI=0.1, 0.2) in Rwanda (60) to 73.8% (95% CI=69.3, 78.3) (97) in Nigeria. Country-specific analysis showed the highest lifetime prevalence in Nigeria at 19.0% (95% CI=9.8, 28.1), and the lowest in Rwanda at 0.1% (95% CI=0.1, 0.2). The current prevalence of sedative use, pooled from 10 studies, was 6.2% (95% CI=4.7, 7.8), while the 12-month prevalence, based on 4 studies, was 6.0% (95% CI=3.0, 10.0).
Opioid group
Of the studies included in the meta-analysis, sixteen reported on an opioid group of drug use among young people. The pooled lifetime prevalence of opioids was 15.9% (95% CI=13.2, 18.5). The current prevalence of opioid use, pooled from 10 studies, was 7.0% (95% CI=5.0, 9.0), while the 12-month prevalence, from 3 studies, was 4.0% (95% CI=1.0, 7.0).
Inhalants group
A total of ten studies reported on inhalant (e.g., benzene, glue, petrol, and solvents) use among young people. The pooled lifetime prevalence of inhalants, from 12 studies, was 6.0% (95% CI=4.0, 8.0). The lowest reported prevalence from an individual study was in Botswana at 0.1% (95% CI=0.01, 0.2) (29), while the highest was 7.40% (95% CI=4.1, 10.7) (97) in Nigeria.
The current prevalence of inhalant use, pooled from 9 studies, was 3.0% (95% CI=2.0, 4.0), while the 12-month prevalence, from 4 studies was 2.0% (95% CI=0.1, 4.0).
Other substances (steroids and mastics)
Two studies reported on this group of substance use, one focusing on mastics in Ethiopia (44) and the other is on steroids in Nigeria (31). The current prevalence of mastics was 42.0% (95% CI=36.5, 47.5), and the lifetime prevalence was 46.0% (95% CI=40.5, 51.5) (44). The lifetime prevalence of steroids was reported at 12.2% (95% CI=7.8, 14.6) (31).
Factors associated with substance use
Out of the 60 studies reviewed, only 48 reported on factors associated with substance use among young people. For simplicity, these factors were grouped into three major categories: individual, family, and community and environmental factors.
Individual factors
Among the studies providing gender distribution data, 18 consistently show a higher prevalence of substance use among male young individuals (29, 30, 33, 35, 36, 38, 40, 42, 48, 50, 53–56, 61, 65, 66, 84). In contrast, while three studies report a higher prevalence of substance use among females (31, 34, 51), two studies indicate lower rates among females (57, 87).
Ten reviewed studies indicate that substance use risk increases with age among young people (31, 44, 50, 55, 57, 63, 66, 72, 84, 85). However, a Zambian study on cannabis use found younger individuals, below 15 years, showing higher rates than older ones (34).
It was indicated in the reviewed studies that the risk of substance use among young people increases with advancing years of study (29, 38, 40, 43, 46, 55, 76, 79). Additionally, factors such as poor academic performance (45), non-attendance of school (44, 71), attending private schools (54, 67), attending rural schools (59), and in-school compared to out-of-school young people (28) are associated with an increased risk of substance use. However, one study presents a different perspective, indicating a lower risk of substance use among high-academic performers (31).
Furthermore, factors such as living alone during school-age (33, 62), living off-campus in rented accommodation (43, 53, 65), low perceived risk of substance use (45), poor social skills (45), engagement in sexual activity (47, 50, 61, 63), being bullied (47, 87), and the perception that substance use improves academic achievement (53) were linked to various forms of substance use among young people.
Additionally, urban residency (55, 76), frequent watching of football games or soccer matches (57), having internet access at home (57), experiencing intimate partner violence (63), involvement in trade and other business activities (71, 84, 85), exposure to substance advertisements (87), and the presence of health conditions such as anxiety symptoms (68, 76), human immunodeficiency virus (63), suicidal ideation (50, 73), and low expectations for the future (73) were also associated with substance use among young people.
Family factors
Peer and family influence significantly impact substance use among young people. As reported by 17 studies in the review, substance use by close friends (31, 33, 35, 38, 41, 43–47, 53, 54, 56, 57, 67, 68, 71) and other family members (21, 31, 33, 36, 43, 47, 54, 56, 68, 71, 75) were associated with substance use among young people.
Young people with negative family dynamics, such as unsatisfactory family relationships (31), parental divorce (39, 76), low family monitoring (73), loss of one or more parents (76), and those who felt poorly understood by their parents (87) had higher odds of substance use. Conversely, a strong parent-child relationship (75), parental disapproval of substance use (67), and close family supervision (34) were associated with a lower tendency to use substances among young people. Additionally, young people whose mothers had secondary or higher education (51, 60, 67), or were civil servants (51) had a higher prevalence of substance use.
Community and environmental factors
Community norms supportive of substance use (75), easy access to substances (75, 79), and lenient school regulations (75, 79) were associated with substance use among young people.
Frequent attendance at religious places (30, 36, 45, 54), regardless of the type of religion, was associated with a lower risk of substance use among young people, while never attending was associated with an increased risk (69).
While two studies indicate low socioeconomic status increases the risk (68, 78), eight other reviewed studies showed higher odds of substance use among individuals from higher socioeconomic and income backgrounds compared to their counterparts (21, 30, 40, 42, 54, 58, 59, 79).
Reasons for substance use among young people
A total of twenty-one studies reported reasons for substance use among young people. Common reasons included alertness (28, 33, 50, 61, 75, 76), boosting confidence (31, 41, 47, 84, 85), exam preparation (28, 36, 38, 41, 43, 50, 70), peer influence (33, 36, 38, 41, 44, 50, 61, 74–76) (51), increasing energy (33, 43), and stress relief (33, 36, 38, 41, 43, 47, 50, 51, 61, 70, 74–76, 84).
Other reported reasons were pleasure/fun (33, 36, 38, 41, 43, 46, 47, 50, 61, 70, 74–76, 84), stomachache relief (33), family influence (33, 36, 76), easy access (36, 38, 44, 75, 76) and socialization (36, 41–44, 46, 50, 76).
Additional reasons included enhanced concentration on religious activities (36, 42, 43, 70), appetite suppression (36, 50), time-killing (41, 43), improving academic performance (41), habit (43, 61), lack of recreational areas (42), affordability (44), curiosity (33, 44, 51, 70, 74) fitting in with friends (47, 76), media influence (51), self-medication (70, 85), having money to buy (75), academic dissatisfaction (76), improving social status (85), and stimulating appetite for meals (85).
Discussion
This review provides a comprehensive overview of substance use prevalence and risk factors among young people in SSA, pooled from 60 different individual studies published between 2010 to 2024. While previous reviews often focused on specific countries (12, 21, 22), adolescents (10-19 years of age) (10), or specific substances (23, 24) have provided valuable insights, this review offers a broader regional perspective on substance use among young people, covering both adolescents and youths, in SSA. This review provides the most recent evidence on the state of substance use among young people in SSA.
The pooled lifetime, 12-month, and current prevalence of any substance use among young people in SSA were 21%, 18%, and 15%, respectively. In general, the pooled prevalence estimated by the current review across different timeframes is lower than the overall prevalence of substance use reported in previous African and non-African studies. For instance, a recent review on substance use among adolescents in SSA reported a lifetime prevalence of 42% (10). Similarly, a review among medical students in India found an overall lifetime prevalence of 40% (98), and a study among young people in Ethiopia reported a 32% lifetime prevalence and a 24% current prevalence (99). Several factors could explain this difference, including the number of studies (60 in our review compared to fewer than 50 in others), the total number of participants (84,434 in our review compared to fewer in others), the characteristics of study participants (such as medical students in India who may use substances to cope with academic stress). Additionally, the scope of substances considered (we included various substances, while some studies focused on fewer substances, like those in Ethiopia focusing only on alcohol, khat, and cigarettes), and the limited geographical focus (Ethiopia and India specifically) contribute to the differences. Other factors, such as study periods, levels of stigma, potential response bias, and other methodological, cultural, and socioeconomic factors, may also justify the observed differences.
In this study, the 12-month and current alcohol prevalence rates, at 30% and 24% respectively, closely align with findings from previous studies. Specifically, our findings are consistent with the 12-month and current alcohol prevalence rates among young people in East Africa (26% and 28%) (100), alcohol prevalence among adolescents in SSA (32%) (10), and current alcohol prevalence among students in Ethiopia (27.6%) (101). Additionally, our results align with the alcohol prevalence among medical students in India (27%) (98), the lifetime (10%) and 12-month (5%) prevalence of cannabis among adolescents in SSA (102), and the current prevalence of khat among young individuals in Ethiopia (17.3%) (103). However, the lifetime prevalence reported in this review (21%) contrasts significantly with findings from other reviews on substance use among young people: Ethiopia (52%) (104), East Africa (52%) (100), students in India (40%) (98), and adolescents in Sub-Saharan Africa (SSA) (42%) (10).
Regionally, the lifetime and 12-month prevalence of any substance use were higher in the southern region, while the current prevalence was higher in the East Africa region. In country-specific analysis, Zambia had the highest lifetime prevalence of any substance use at 40%, Botswana had the highest 12-month prevalence at 32%, and Uganda had the highest current prevalence at 75%. This varying pattern of substance use prevalence among young people across study regions and countries within SSA could be attributed to the availability and variety of substances across regions as well as the number of studies involved from each region. Additionally, the differences could be explained by factors such as production, availability, cost, regulations, social pressure, and urban/rural distinctions (105, 106). Furthermore, distinct patterns of substance use observed between countries, such as the exclusive focus on khat in East Africa, highlight its origin and widespread consumption in countries like Ethiopia, Somalia, and Kenya (106–108). Similarly, the higher prevalence of cannabis reported in South Africa (32), aligns with the existence of indigenous plants of cannabis (known as dagga in Southern Africa) that have been used in traditional cultures for centuries (106). The relatively lower prevalence observed in the Western African region could be explained by the strong regional drug control and prevention policies and regulations (109), upon which Eastern and Southern Africa based their establishment of the Commission for Drug Control (ESACD).
This systematic review findings align with Social Norms Theory (110), which stipulates that people’s behaviors are influenced by the norms and expectations of their social groups. This theory helps explain why substance use prevalence varies across regions and countries in SSA, where cultural acceptance of substance use may be more pronounced. In environments where substance use is perceived as normative among peers, young individuals may feel pressure to engage in such behaviors to fit in (111).
The review identified that family dynamics, including positive reinforcement or discouragement of substance use, significantly shape young people’s attitudes and behaviors toward substance use. Additionally, family communication, parental monitoring, and parent-child relationships were found to have associations with substance use patterns. Social Learning Theory (Bandura, 1977) also complements these findings by suggesting that individuals, particularly young people, learn behaviors through observation and imitation of influential figures in their lives. Exposure to substance use behaviors among parents or older siblings normalizes these behaviors and increases the likelihood of experimentation and continued use during adolescence and young adulthood. Beyond family influences, it was reported that peer relationships, community norms, and broader societal factors further shape young people’s perceptions and behaviors related to substance use. Gender-disaggregated data of all specific substances from meta-analysis consistently show higher prevalence rates of substance use among males compared to females. For instance, lifetime alcohol use among males was 45.9% compared to 25.6% among females. Studies in Ethiopia and Europe similarly report higher overall substance use prevalence among male adolescents (99, 112, 113). The variations could arise from biological and socio-cultural factors such as childcare responsibilities, addiction stigma, relationship dynamics, peer pressure, group affiliations, and cultural norms (12, 99, 114).
Beyond the context of substance use variation by gender, the theories explain that children may observe their parents or older siblings using substances, which can normalize such behaviors and increase the likelihood of experimentation and continued use in adolescence and young adulthood. This observational learning process is particularly influential during developmental stages when individuals are forming their attitudes and behaviors toward substances (115, 116).
Moreover, family dynamics play a crucial role in shaping attitudes and behaviors related to substance use (117). Positive reinforcement of substance use behaviors within the family, whether overt or subtle, can reinforce these behaviors as acceptable or even desirable. Conversely, negative attitudes or behaviors towards substance use within the family unit can serve as protective factors against substance use initiation or escalation. Family communication patterns, parental monitoring, and the quality of parent-child relationships also were identified as significantly associated with the likelihood of substance use among young people.
In addition to family influences, peer relationships, community norms, and broader societal factors further shape young people’s perceptions and behaviors related to substance use (118).
Another important finding identified by this review is the gap in community-based substance use studies compared to those conducted in institutional settings. Out of the 60 studies reviewed, only about one-quarter involved participants were from the general community, while the rest focused on institutional settings. Community-based studies revealed significantly higher current prevalence rates (26%) than institution-based studies while showing similar lifetime rates. These findings underscore the critical importance of expanding research efforts to include young people from the general community in studies on substance use, to comprehensively understand the prevalence and factors influencing substance use in different contexts, and to develop targeted interventions that address the needs of all young people.
The current review also revealed a relative increase in publication trends on substance use over the last decade with a notable rise in the past five years in SSA. This increase, particularly during the COVID-19 era, might be attributed to an increased focus on research and write-up during the lockdown period. The lockdowns provided researchers with more time to conduct literature reviews, analyze data, and write manuscripts, potentially leading to a significant rise in academic output in this field. The pandemic may also have exacerbated substance use due to heightened stress, anxiety, and disruption of social and economic activities, thereby prompting more research interest in this area. This was supported by studies showing that there was a sharp increase in the publication of articles on different subjects (119, 120).
Strength and limitations
This systematic review synthesized and analyzed a large body of empirical evidence from various studies, providing a comprehensive overview of substance use prevalence and associated factors across the region by using a systematic approach. By including studies covering a wide age range (10-24 years) and various types of substances, the review offers a more thorough understanding of substance use prevalence among young individuals in SSA across different reporting timeframes. It also highlights the differences in substance use prevalence across countries, regions, and genders, emphasizing the need for targeted interventions sensitive to cultural norms and practices.
However, this review has some limitations. Only cross-sectional studies published in peer-reviewed literature were included, missing grey literature such as government reports and unpublished data. This focus on epidemiological studies may have missed valuable insights from other sources. Although we strictly followed PRISMA guidelines, the inclusion of cross-sectional studies could introduce recall bias. Additionally, we observed higher heterogeneity in the review. While the JBI-MAStARI tool is valuable for assessing study quality, we acknowledge that its subjective nature and reliance on evaluator interpretation may introduce bias.
Implications of study findings
The findings of this systematic review and meta-analysis have several important implications. The high prevalence rates of alcohol, cigarette, khat, and cannabis use among young people underscore the need for targeted interventions and policies. Identifying individual, family, and community risk factors provides a comprehensive understanding of the determinants of substance use, which is essential for designing multifaceted prevention strategies. Significant variations in substance use prevalence by gender, region, country, and study setting call for specific prevention and treatment approaches. Early screening and identification of substance use in healthcare and educational settings are crucial for timely intervention.
Conclusions and recommendations
A significant portion of young people in SSA use different substances, at different time points with variations between genders, regions, and countries. Review findings highlight the need for interventions targeting both the broader young population and specific subgroups who may be at higher risk of substance use. Promotive, protective, and curative programs for substance use and substance use disorders in young people at the individual, family, and societal levels can play a key role in achieving sustainable development goals for their health and well-being.
Future longitudinal studies are crucial to understanding the progression of substance use and identifying causal relationships. Exploring regional and cultural differences in substance use patterns and including diverse populations beyond educational institutions, such as those in rural areas and marginalized groups, is also critical. Policy development should focus on targeted prevention programs for high-risk groups, such as males, older adolescents, and those with poor academic performance. Increasing school-based prevention and intervention programs is critical for early detection. Integrating substance use prevention with mental health services and engaging communities in prevention efforts can effectively address local risk factors. Routine screening in healthcare and educational settings, comprehensive substance use education, family engagement, strengthening parent-child relationships, peer support programs, and improved access to youth-friendly and culturally appropriate treatment and counseling services are vital practical measures.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author/s.
Author contributions
JE: Writing – review & editing, Writing – original draft, Visualization, Validation, Software, Project administration, Methodology, Investigation, Formal Analysis, Data curation, Conceptualization. JA: Writing – review & editing, Visualization, Validation, Supervision, Methodology. DD: Writing – review & editing, Visualization, Validation, Supervision, Software, Methodology, Formal Analysis, Conceptualization.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors would like to acknowledge librarians working at the University of Technology Sydney for their technical support during the literature search. We would also acknowledge the authors of the primary studies included in this review for their valuable contributions to the field.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1328318/full#supplementary-material
Abbreviations
AIM, African Index Medicus; AJOL, African Journals Online; DALYs, Disability Adjusted Life Years; GBD, Global Burden of Disease; JBI, Joanna Briggs Institute; LSD, Lysergic Acid Diethylamide; MeSH, Medical Education Subject Heading; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; PRISMA-P, Preferred Reporting Items for Systematic reviews and Meta-Analyses Protocols; PROSPERO, International Prospective Register of Systematic Reviews; SDG, Sustainable Development Goals; SSA, Sub-Saharan Africa; SUD, Substance Use Disorders; WHO, World Health Organization; YLD, Years Lived with Disability.
References
1. United Nations. World Programme of Action for Youth to the Year 2000 and Beyond (1995). Available online at: https://undocs.org/A/RES/50/81. (Accessed October 23, 2023).
2. United Nations Population Fund, U. State of World Population 2023: 8 Billion Lives, Infinite Possibilities - The Case for Rights and Choices. New York: U. N. P. Fund (2023). Available at: https://www.unfpa.org/sites/default/files/swop23/SWOP2023-ENGLISH-230329-web.pdf.
3. United Nations. World Population Prospect. New York: P. D. New York: Department of Economic and Social Affairs (2022). Available at: https://population.un.org/wpp/Download/Standard/Population/.
4. World Health Organization. Global Accelerated Action for the Health of Adolescents (AA-HA)!: Guidance to support country implementation. Geneva, Switzerland: World Health Organization (WHO (2017).
5. Simon KM, Levy SJ, Bukstein OG. Adolescent substance use disorders. NEJM Evid. (2022) 1:EVIDra2200051. doi: 10.1056/EVIDra2200051
6. GBD. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2018) 392:1789–858. doi: 10.1016/s0140-6736(18)32279-7
7. Morojele NK, Ramsoomar L, Dumbili EW, Kapiga S. Adolescent Health Series – Alcohol, tobacco, and other drug use among adolescents in sub-Saharan Africa: A narrative review. Trop Med Int Health. (2021) 26:1528–38. doi: 10.1111/tmi.13687
8. Mutepfa M. Substance Use and Misuse in sub-Saharan Africa Trends, Intervention, and Policy: Trends, Intervention, and Policy. Cham, Switzerland: Springer (2021). doi: 10.1007/978-3-030-85732-5.
9. Kugbey N. Prevalence and correlates of substance use among school-going adolescents (11-18years) in eight Sub-Saharan Africa countries. Subst Abuse Treat Prevent Policy. (2023) 18:44. doi: 10.1186/s13011-023-00542-1
10. Olawole-Isaac A, Ogundupe O, Davies A. Substance use among adolescents in sub-Saharan Africa: a systematic review and meta-analysis. South Afr J Child Health. (2018) 12:79. doi: 10.7196/SAJCH.2018.v12i2b.1524
11. Nawi AM, Ismail R, Ibrahim F, Hassan MR, Manaf MRA, Amit N, et al. Risk and protective factors of drug abuse among adolescents: a systematic review. BMC Public Health. (2021) 21:2088. doi: 10.1186/s12889-021-11906-2
12. Jaguga F, Kiburi SK, Temet E, Barasa J, Karanja S, Kinyua L, et al. A systematic review of substance use and substance use disorder research in Kenya. PloS One. (2022) 17:e0269340. doi: 10.1371/journal.pone.0269340
13. Gopiram P, Kishore MT. Psychosocial attributes of substance abuse among adolescents and young adults: A comparative study of users and non-users. Indian J Psychol Med. (2014) 36:58–61. doi: 10.4103/0253-7176.127252
14. Health, A. I. o., & Welfare. Young people’s use of alcohol, tobacco, e-cigarettes and other drugs (2024). Available online at: https://www.aihw.gov.au/reports/children-youth/young-people-alcohol-smoking-drugs. (Accessed June 07, 2024).
15. Ritchwood TD, Ford H, DeCoster J, Sutton M, Lochman JE. Risky sexual behavior and substance use among adolescents: A meta-analysis. Child Youth Serv Rev. (2015) 52:74–88. doi: 10.1016/j.childyouth.2015.03.005
16. Oppong Asante K, Meyer-Weitz A, Petersen I. Substance use and risky sexual behaviours among street connected children and youth in Accra, Ghana. Subst Abuse Treat Prevent Policy. (2014) 9:45. doi: 10.1186/1747-597X-9-45
17. Jere DL, Norr KF, Bell CC, Corte C, Dancy BL, Kaponda CPN, et al. Substance Use and Risky Sexual Behaviors Among Young Men Working at a Rural Roadside Market in Malawi. J Assoc Nurses AIDS Care. (2017) 28:280–90. https://journals.lww.com/janac/fulltext/2017/03000/substance_use_and_risky_sexual_behaviors_among.7.aspx.
18. McLellan AT. Substance Misuse and Substance use Disorders: Why do they Matter in Healthcare? Trans Am Clin Climatol Assoc. (2017) 128:112–30.
19. Sanchez-Roige S, Kember RL, Agrawal A. Substance use and common contributors to morbidity: A genetics perspective. eBioMedicine. (2022) 83:104212. doi: 10.1016/j.ebiom.2022.104212
20. Daley DC. Family and social aspects of substance use disorders and treatment. J Food Drug Anal. (2013) 21:S73–s76. doi: 10.1016/j.jfda.2013.09.038
21. Abate SM, Chekol YA, Minaye SY. Prevalence and risk factors of psychoactive substance abuse among students in Ethiopia: A systematic review and meta-analysis. Ann Med Surg. (2021) 70:102790. doi: 10.1016/j.amsu.2021.102790
22. Jatau AI, Sha’aban A, Gulma KA, Shitu Z, Khalid GM, Isa A, et al. The burden of drug abuse in Nigeria: A scoping review of epidemiological studies and drug laws. Public Health Rev. (2021) 42:1603960. doi: 10.3389/phrs.2021.1603960
23. Townsend L, Flisher AJ, Gilreath T, King G. A systematic review of tobacco use among sub-Saharan African youth. J Subst Use. (2006) 11:245–69. doi: 10.1080/14659890500420004
24. Belete H, Yimer TM, Dawson D, Espinosa DC, Ambaw F, Connor JP, et al. Alcohol use and alcohol use disorders in sub-Saharan Africa: A systematic review and meta-analysis. Addiction. (2024) 119:561–78. doi: 10.1111/add.16514
25. Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. (2015) 4:1. doi: 10.1186/2046-4053-4-1
26. Sawyer SM, Azzopardi PS, Wickremarathne D, Patton GC. The age of adolescence. Lancet Child Adolesc Health. (2018) 2:223–8. doi: 10.1016/s2352-4642(18)30022-1
27. JBI. Joanna Briggs Institute Reviewers’ Manual: 2014 edition/Supplement. In: Systematic Review; Protocol; Prevalence; Incidence; Survey; Observational; and Methods. Adelaide, South Australia: The University of Adelaide, South Australia 5005: The Joanna Briggs Institute (2014).
28. Ogunkunle T, Gobir A, Makanjuola A, Ojuawo A. Educational status and other socio-demographic correlates of current use of psychoactive substances among Nigerian adolescents. Nigerian J Paedia. (2020) 47:23–9. doi: 10.4314/njp.v47i1.5
29. Letamo G, Bowelo M, Majelantle RG. Prevalence of substance use and correlates of multiple substance use among school-going adolescents in Botswana. Afr J Drug Alcohol Stud. (2016) 15:75–89.
30. Teni FS, Surur AS, Hailemariam A, Aye A, Mitiku G, Gurmu AE, et al. Prevalence, reasons, and perceived effects of khat chewing among students of a college in Gondar town, Northwestern Ethiopia: A cross-sectional study. Ann Med Health Sci Res. (2015) 5:454–60. doi: 10.4103/2141-9248.177992
31. Johnson O, Akpanekpo E, Okonna. E, Adeboye. S, Udoh. A. The Prevalence and Factors affecting Psychoactive Substance Use among Undergraduate Students in University of Uyo, Nigeria. J Community Med Prim Health Care. (2017) 29:11–22.
32. Hamdulay A, Mash RJ. The prevalence of substance use and its associations amongst students attending high school in Mitchells Plain, Cape Town. South Afr Family Pract. (2011) 53:83–90. doi: 10.1080/20786204.2011.10874065
33. Kassa A, Taddesse F, Yilma A. Prevalence and factors determining psychoactive substance (PAS) use among Hawassa University (HU) undergraduate students, Hawassa Ethiopia. BMC Public Health. (2014) 14:1044. doi: 10.1186/1471-2458-14-1044
34. Siziya S, Muula AS, Besa C, Babaniyi O, Songolo P, Kankiza N, et al. Cannabis use and its socio-demographic correlates among in-school adolescents in Zambia. Ital J Pediatr. (2013) 39:13. doi: 10.1186/1824-7288-39-13
35. Dida N, Kassa Y, Sirak T, Zerga E, Dessalegn T. Substance use and associated factors among preparatory school students in Bale Zone, Oromia Regional State, Southeast Ethiopia. Harm Reduct J. (2014) 11:21. doi: 10.1186/1477-7517-11-21
36. Abdeta T, Tolessa D, Adorjan K, Abera M. Prevalence, withdrawal symptoms and associated factors of khat chewing among students at Jimma University in Ethiopia. BMC Psychiatry. (2017) 17:142. doi: 10.1186/s12888-017-1284-4
37. Osayomi T, Iyanda AE, Adeleke R, Osadolor OJ. Geographical analysis of illicit drug use in Nigeria: evidence from the first national drug use survey, 2018. Professional Geograph. (2021) 73(3):377–91. doi: 10.1080/00330124.2021.1883445
38. Adane T, Worku W, Azanaw J, Yohannes L. Khat chewing practice and associated factors among medical students in Gondar town, Ethiopi. Subst Abuse. (2021) 15:1178221821999079. doi: 10.1177/1178221821999079
39. Addo B, Mainoo GO, Dapaah JM, Babayara MNK. Prevalence of substance use in a sample of Ghanaian adolescents experiencing parental divorce. J Child Adolesc Subst Abuse. (2016) 25:428–37. doi: 10.1080/1067828X.2015.1056867
40. Adere A, Yimer NB, Kumsa H, Liben ML. Determinants of psychoactive substances use among Woldia University students in Northeastern Ethiopia. BMC Res Notes. (2017) 10:441. doi: 10.1186/s13104-017-2763-x
41. Admasu E, Tariku B, Andargie G, Hibdye G, Asegidew W. Prevalence, pattern and associated factors of khat chewing among debre Berhan university students, Ethiopi. Biol Med. (2018) 10:1–8. doi: 10.4172/0974-8369
42. Alebachew W, Semahegn A, Ali T, Mekonnen H. Prevalence, associated factors and consequences of substance use among health and medical science students of Haramaya University, eastern Ethiopia 2018: a cross-sectional study. BMC Psychiatry. (2019) 19:343. doi: 10.1186/s12888-019-2340-z
43. Astatkie A, Demissie M, Berhane Y, Worku A. Prevalence of and factors associated with regular khat chewing among university students in Ethiopia. Subst Abuse Rehabil. (2015) 6:41–50. doi: 10.2147/sar.S78773
44. Ayenew M, Kabeta T, Woldemichael K. Prevalence and factors associated with substance use among street children in Jimma town, Oromiya national regional state, Ethiopia: a community based cross-sectional study. Subst Abuse Treat Prevent Policy. (2020) 15:61. doi: 10.1186/s13011-020-00304-3
45. Birhanu AM, Bisetegn TA, Woldeyohannes SM. High prevalence of substance use and associated factors among high school adolescents in Woreta Town, Northwest Ethiopia: multi-domain factor analysis. BMC Public Health. (2014) 14:1186. doi: 10.1186/1471-2458-14-1186
46. Chekole YA. Prevalence of alcohol use and associated factors among dilla university students, dilla town, southern Ethiopia: A cross-sectional study. J Addict. (2020) 2020:3971090. doi: 10.1155/2020/3971090
47. Chivandire CT, January J. Correlates of cannabis use among high school students in Shamva District, Zimbabwe: A descriptive cross-sectional study. Malawi Med J. (2016) 28:53–6. doi: 10.4314/mmj.v28i2.5
48. Deressa W, Azazh A. Substance use and its predictors among undergraduate medical students of Addis Ababa University in Ethiopia. BMC Public Health. (2011) 11:660. doi: 10.1186/1471-2458-11-660
49. Desai R, Mercken LAG, Ruiter RAC, Schepers J, Reddy PS. Cigarette smoking and reasons for leaving school among school dropouts in South Africa. BMC Public Health. (2019) 19:130. doi: 10.1186/s12889-019-6454-5
50. Dires E, Soboka M, Kerebih H, Feyissa G. Factors associated with khat chewing among high school students in jimma town southwest Ethiopia. J Psychiatry Omics. (2016) 19:4–372. doi: 10.4172/2378-5756.1000372
51. Durowade KA, Elegbede OE, Pius-Imue GB, Omeiza A, Bello M, Mark-Uchendu C, et al. Substance use: prevalence, pattern and risk factors among undergraduate students in a tertiary institution in southwest Nigeria. J Community Med Prim Health Care. (2021) 33:83–99. doi: 10.4314/jcmphc.v33i2.6
52. Francis JM, Weiss HA, Mshana G, Baisley K, Grosskurth H, Kapiga SH. The epidemiology of alcohol use and alcohol use disorders among young people in Northern Tanzania. PLoS ONE. (2015) 10(10):e0140041. doi: 10.1371/journal.pone.0140041
53. Gebrehanna E, Berhane Y, Worku A. Khat chewing among Ethiopian University Students- a growing concern. BMC Public Health. (2014) 14:1198. doi: 10.1186/1471-2458-14-1198
54. Gebremariam T, Mruts K, Neway T. Substance use and associated factors among Debre Berhan University students, Central Ethiopia. Subst Abuse Treat Prevent Policy. (2018) 13:13. doi: 10.1186/s13011-018-0150-9
55. Gebresilassie A, Hadush Z, Gidey G, Hagos W, Mussie M, Gebregiorgis G, et al. Prevalence of, Factors Associated with and Level of Dependence of Psychoactive Substance Use among Mekelle University Students, Ethiopia. Int J Environ Res Public Health. (2020) 17. doi: 10.3390/ijerph17030847
56. Gebreslassie M, Feleke A, Melese T. Psychoactive substances use and associated factors among Axum University students, Axum Town, North Ethiopia. BMC Public Health. (2013) 13:693. doi: 10.1186/1471-2458-13-693
57. Getachew S, Lewis S, Britton J, Deressa W, Fogarty AW. Prevalence and risk factors for initiating tobacco and alcohol consumption in adolescents living in urban and rural Ethiopia. Public Health. (2019) 174:118–26. doi: 10.1016/j.puhe.2019.05.029
58. Hirpa S, Fogarty A, Addissie A, Bauld L, Frese T, Unverzagt S, et al. An emerging problem of shisha smoking among high school students in Ethiopia. J Environ Res Public Health. (2021) 18. doi: 10.3390/ijerph18137023
59. Itanyi IU, Onwasigwe CN, Ossip D, Uzochukwu BSC, McIntosh S, Aguwa EN, et al. Predictors of current tobacco smoking by adolescents in Nigeria: Interaction between school location and socioeconomic status. Tob Induc Dis. (2020) 18:13. doi: 10.18332/tid/117959
60. Kanyoni M, Gishoma D, Ndahindwa V. Prevalence of psychoactive substance use among youth in Rwanda. BMC Res Notes. (2015) 8:190. doi: 10.1186/s13104-015-1148-2
61. Kassa A, Loha E, Esaiyas A. Prevalence of khat chewing and its effect on academic performance in Sidama zone, Southern Ethiopia. Afr Health Sci. (2017) 17:175–85. doi: 10.4314/ahs.v17i1.22
62. Kassa A, Wakgari N, Taddesse F. Determinants of alcohol use and khat chewing among Hawassa University students, Ethiopia: a cross sectional study. Afr Health Sci. (2016) 16:822–30. doi: 10.4314/ahs.v16i3.24
63. Kuteesa MO, Weiss HA, Cook S, Seeley J, Ssentongo JN, Kizindo R, et al. Epidemiology of alcohol misuse and illicit drug use among young people aged 15-24 years in fishing communities in Uganda. Int J Environ Res Public Health. (2020) 17. doi: 10.3390/ijerph17072401
64. Mayanja Y, Kamacooko O, Bagiire D, Namale G, Seeley J. Epidemiological findings of alcohol misuse and dependence symptoms among adolescent girls and young women involved in high-risk sexual behavior in Kampala, Uganda. Int J Environ Res Public Health. (2020) 17. doi: 10.3390/ijerph17176129
65. Musyoka CM, Mbwayo A, Donovan D, Mathai M. Alcohol and substance use among first-year students at the University of Nairobi, Kenya: Prevalence and patterns. PloS One. (2020) 15:e0238170. doi: 10.1371/journal.pone.0238170
66. Mutiso VN, Ndetei DM, Muia EN, Musyimi C, Osborn TL, Kasike R, et al. Prevalence and perception of substance abuse and associated economic indicators and mental health disorders in a large cohort of Kenyan students: towards integrated public health approach and clinical management. BMC Psychiatry. (2022) 22:191. doi: 10.1186/s12888-022-03817-2
67. Ogunsola OO, Fatusi AO. Risk and protective factors for adolescent substance use: a comparative study of secondary school students in rural and urban areas of Osun State, Nigeria. Int J Adolesc Med Health. (2016) 29. doi: 10.1515/ijamh-2015-0096
68. Olashore AA, Ogunwobi O, Totego E, Opondo PR. Psychoactive substance use among first-year students in a Botswana University: pattern and demographic correlates. BMC Psychiatry. (2018) 18:270. doi: 10.1186/s12888-018-1844-2
69. Onya H, Tessera A, Myers B, Flisher A. Adolescent alcohol use in rural South African high schools. Afr J Psychiatry (Johannesbg). (2012) 15:352–7. doi: 10.4314/ajpsy.v15i5.44
70. Oshodi OY, Aina OF, Onajole AT. Substance use among secondary school students in an urban setting in Nigeria: prevalence and associated factors. Afr J Psychiatry (Johannesbg). (2010) 13:52–7. doi: 10.4314/ajpsy.v13i1.53430
71. Owusu-Sarpong AA, Agbeshie K. Cigarette smoking among in-school adolescents in Yilo Krobo municipality in the Eastern Region of Ghana. Ghana Med J. (2019) 53:273–8. doi: 10.4314/gmj.v53i4.4
72. Reda AA, Moges A, Biadgilign S, Wondmagegn BY. Prevalence and determinants of khat (Catha edulis) chewing among high school students in eastern Ethiopia: a cross-sectional study. PloS One. (2012) 7:e33946. doi: 10.1371/journal.pone.0033946
73. Riva K, Allen-Taylor L, Schupmann WD, Mphele S, Moshashane N, Lowenthal ED. Prevalence and predictors of alcohol and drug use among secondary school students in Botswana: a cross-sectional study. BMC Public Health. (2018) 18:1396. doi: 10.1186/s12889-018-6263-2
74. Roble AK, Osman MO, Lathwal OP, Aden AA. Prevalence of cigarette smoking and associated factors among adolescents in eastern Ethiopi. Subst Abuse Rehabil. (2021) 12:73–80. doi: 10.2147/SAR.S331349
75. Seid L, Gintamo B, Mekuria ZN, Hassen HS, Gizaw Z. Substance use and associated factors among preparatory school students in Kolfe-Keranyo sub-city of Addis Ababa, Ethiopia. Environ Health Prev Med. (2021) 26:110. doi: 10.1186/s12199-021-01032-1
76. Shegute T, Wasihun Y. Prevalence of substance use in university students, Ethiopia. Subst Abuse. (2021) 15:11782218211003558. doi: 10.1177/11782218211003558
77. Sinshaw A, Kassa H, Messele A. Prevalence and associated factors of khat chewing among atse fasil campus students, university of Gondar, Northwest Ethiopia June 2013. J Psychol Clin Psychiatry. (2014) 1(6):00040. doi: 10.15406/jpcpy.2014.01.00040
78. Soepnel LM, Kolkenbeck-Ruh A, Crouch SH, Draper CE, Ware LJ, Lye SJ, et al. Prevalence and socio-structural determinants of tobacco exposure in young women: Data from the Healthy Trajectories Initiative (HeLTI) study in urban Soweto, South Africa. Drug Alcohol Depend. (2022) 232:109300. doi: 10.1016/j.drugalcdep.2022.109300
79. Soremekun RO, Folorunso BO, Adeyemi OC. Prevalence and perception of drug use amongst secondary school students in two local government areas of Lagos State, Nigeria. S Afr J Psychiatr. (2020) 26:1428. doi: 10.4102/sajpsychiatry.v26i0.1428
80. Osborne A, Aboagye RG, Olorunsaiye CZ, James PB, Bangura C, Seidu A-A, et al. Alcohol use among in-school adolescents in Sierra Leone. BMJ Open. (2024) 14:e080222. doi: 10.1136/bmjopen-2023-080222
81. Einarsdóttir J, Baldé A, Jandi Z, Boiro H, Gunnlaugsson G. Prevalence of and Influential Factors for Waterpipe Smoking among School-Attending Adolescents in Bissau, Guinea-Bissau. Adolescents. (2024) 4:138–57. https://www.mdpi.com/2673-7051/4/1/10.
82. Jaguga F, Kwobah EK, Giusto A, Apondi E, Barasa J, Korir M, et al. Feasibility and acceptability of a peer provider delivered substance use screening and brief intervention program for youth in Kenya. BMC Public Health. (2023) 23:2254. doi: 10.1186/s12889-023-17146-w
83. Kinyanjui DW, Sum AM. Personality traits and substance use among college students in Eldoret, Kenya. PLOS ONE. (2023) 18(5):e0286160. doi: 10.1371/journal.pone.0286160
84. Kyei-Gyamfi S, Kyei-Arthur F, Alhassan N, Agyekum MW, Abrah PB, Kugbey N. Prevalence, correlates, and reasons for substance use among adolescents aged 10-17 in Ghana: a cross-sectional convergent parallel mixed-method study. Subst Abuse Treat Prev Policy. (2024) 19:17. doi: 10.1186/s13011-024-00600-2
85. Kyei-Gyamfi S, Wellington N, Kyei-Arthur F. Prevalence, reasons, predictors, perceived effects, and regulation of alcohol use among children in Ghana. J Addict. (2023) 2023:9032348. doi: 10.1155/2023/9032348
86. Mavura RA, Nyaki AY, Leyaro BJ, Mamseri R, George J, Ngocho JS, et al. Prevalence of substance use and associated factors among secondary school adolescents in Kilimanjaro region, northern Tanzania. PloS One. (2022) 17:e0274102. doi: 10.1371/journal.pone.0274102
87. Olashore AA, Paruk S, Maphorisa T, Mosupiemang B. Pattern of substance use and substance use disorder in adolescent learners at public secondary schools in Gaborone, Botswana. PloS One. (2022) 17:e0268961. doi: 10.1371/journal.pone.0268961
88. Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, Tungpunkom P. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Healthc. (2015) 13:132–40. doi: 10.1097/XEB.0000000000000055
89. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. (1986) 7:177–88. doi: 10.1016/0197-2456(86)90046-2
90. Ioannidis JP. Interpretation of tests of heterogeneity and bias in meta-analysis. J Eval Clin Pract. (2008) 14:951–7. doi: 10.1111/j.1365-2753.2008.00986.x
91. Lin L, Chu H. Quantifying publication bias in meta-analysis. Biometrics. (2018) 74:785–94. doi: 10.1111/biom.12817
92. The WHO ASSIST Working Group. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): development, reliability and feasibility. Addiction. (2002) 97:1183–94. doi: 10.1046/j.1360-0443.2002.00185.x
93. Bush B, Shaw S, Cleary P, Delbanco TL, Aronson MD. Screening for alcohol abuse using the CAGE questionnaire. Am J Med. (1987) 82:231–5. doi: 10.1016/0002-9343(87)90061-1
94. De Meneses-Gaya C, Zuardi AW, Loureiro SR, Crippa JAS. Alcohol Use Disorders Identification Test (AUDIT): An updated systematic review of psychometric properties. Psychol Neurosci. (2009) 2:83–97. doi: 10.3922/j.psns.2009.1.12
95. Bastiani L, Potente R, Scalese M, Siciliano V, Fortunato L, Molinaro S. The Cannabis Abuse Screening Test (CAST) and its applications. In: Handbook of cannabis and related pathologies: Biology, pharmacology, diagnosis, and treatment. San Diego, CA (California): Elsevier Academic Press (2017). p. 971–80. doi: 10.1016/B978-0-12-800756-3.00117-4
96. Adelekan ML, Odejide OA. The reliability and validity of the WHO student drug-use questionnaire among Nigerian students. Drug Alcohol Depend. (1989) 24:245–9. doi: 10.1016/0376-8716(89)90062-8
97. Abdurahman H, Adejumo O, Abdulmalik J. Prevalence of psychoactive substance use among male adolescents in Southwest Nigeria. J Subst Use. (2019) 24:475–80. doi: 10.1080/14659891.2019.1604840
98. Sahu A, Bhati N, Sarkar S. A systematic review and meta-analysis of substance use among medical students in India. Indian J Psychiatry. (2022) 64:225–39. doi: 10.4103/Indianjpsychiatry.Indianjpsychiatry_672_21
99. Amanuel A, Kassa GM. Magnitude of substance use among young people in Ethiopia: a meta-analytic review. Ethiopian Med J. (2019) 57:295–307.
100. Francis JM, Grosskurth H, Changalucha J, Kapiga SH, Weiss HA. Systematic review and meta-analysis: prevalence of alcohol use among young people in eastern Africa. Trop Med Int health: TM IH. (2014) 19:476–88. doi: 10.1111/tmi.12267
101. Roba HS, Gebremichael B, Adem HA, Beyene AS. Current substances use among students in Ethiopia: A systematic review and meta-analysis of 20-years evidence. Subst Abuse. (2021) 15:11782218211050352. doi: 10.1177/11782218211050352
102. Belete H, Mekonen T, Espinosa DC, Ambaw F, Connor J, Chan G, et al. Cannabis use in sub-Saharan Africa: A systematic review and meta-analysis. Addiction. (2023) 118:1201–15. doi: 10.1111/add.16170
103. Alemu WG, Zeleke TA, Takele WW, Mekonnen SS. Prevalence and risk factors for khat use among youth students in Ethiopia: systematic review and meta-analysi. Ann Gen Psychiatry. (2020) 19:16. doi: 10.1186/s12991-020-00265-8
104. Roba HS, Beyene AS, Irenso AA, Gebremichael B. Prevalence of lifetime substances use among students in Ethiopia: a systematic review and meta-analysis. System Rev. (2019) 8:326. doi: 10.1186/s13643-019-1217-z
105. Mupara LM, Tapera R, Selemogwe-Matsetse M, Kehumile JT, Gaogane L, Tsholofelo E, et al. Alcohol and substance use prevention in Africa: systematic scoping review. J Subst Use. (2022) 27:335–51. doi: 10.1080/14659891.2021.1941356
106. Onaolapo OJ, Olofinnade AT, Ojo FO, Adeleye O, Falade J, Onaolapo AY. Substance use and substance use disorders in Africa: An epidemiological approach to the review of existing literature. World J Psychiatry. (2022) 12:1268–86. doi: 10.5498/wjp.v12.i10.1268
107. Gebrie A, Alebel A, Zegeye A, Tesfaye B. Prevalence and predictors of khat chewing among Ethiopian university students: A systematic review and meta-analysis. PloS One. (2018) 13:e0195718. doi: 10.1371/journal.pone.0195718
108. Ahmed A, Ruiz MJ, Cohen Kadosh K, Patton R, Resurreccion DM. Khat and neurobehavioral functions: A systematic review. PloS One. (2021) 16:e0252900. doi: 10.1371/journal.pone.0252900
109. Model drug law for West Africa: A tool for policymakers. (2018). Available online at: https://www.globalcommissionondrugs.org/wp-content/uploads/2018/08/WADC-MDL-EN-WEB.pdf. (Accessed July 03, 2024).
110. Berkowitz AD. Applications of social norms theory to other health and social justice issues. In: The social norms approach to preventing school and college age substance abuse: A handbook for educators, counselors, and clinicians. San Francisco, CA: Jossey-Bass/Wiley (2003). p. 259–79.
111. Agisilaou VH. Children, youth, and development. In: The Routledge Handbook of Global Development. England, London: Routledge. (2022). p. 566–75. doi: 10.4324/9781003017653-53
112. Amendola S. Burden of mental health and substance use disorders among Italian young people aged 10-24 years: results from the Global Burden of Disease 2019 Study. Soc Psychiatry Psychiatr Epidemiol. (2022) 57:683–94. doi: 10.1007/s00127-022-02222-0
113. Castelpietra G, Knudsen AKS, Agardh EE, Armocida B, Beghi M, Iburg KM, et al. The burden of mental disorders, substance use disorders and self-harm among young people in Europe 1990-2019: Findings from the Global Burden of Disease Study 2019. Lancet Reg Health Eur. (2022) 16:100341. doi: 10.1016/j.lanepe.2022.100341
114. Bago BJ. Prevalence of cigarette smoking and its associated risk factors among students of Hawassa University, College of Medicine and Health Science. J Addict Res Ther. (2017) 8:2. doi: 10.4172/2155-6105
115. Trucco EM. A review of psychosocial factors linked to adolescent substance use. Pharmacol Biochem Behav. (2020) 196:172969. doi: 10.1016/j.pbb.2020.172969
116. Yates JR. Chapter 10 - Social and sociocultural factors associated with addiction. In: Yates JR, editor. Determinants of Addiction. Cambridge, MA: Academic Press (2023). p. 393–435. doi: 10.1016/B978-0-323-90578-7.00012-8
117. Boyer C, Oudekerk P, Reilly K, Abraham S. Family dynamics in patients diagnosed with substance use. Substance use and misuse (2020) 15:6–15. doi: 10.1080/10826084.2020.1728684
118. Loke AY, Mak YW. Family process and peer influences on substance use by adolescents. Int J Environ Res Public Health. (2013) 10:3868–85. doi: 10.3390/ijerph10093868
119. Else H. How a torrent of COVID science changed research publishing – in seven charts. Nature. (2020) 588:553. https://link.gale.com/apps/doc/A649636898/AONE?u=anon~97cc65a&sid=googleScholar&xid=b75b71cd.
Keywords: substance use, substance use problems, substance use disorders, alcohol use, drug use, khat use, sub-Saharan Africa, young people
Citation: Ebrahim J, Adams J and Demant D (2024) Substance use among young people in sub-Saharan Africa: a systematic review and meta-analysis. Front. Psychiatry 15:1328318. doi: 10.3389/fpsyt.2024.1328318
Received: 26 October 2023; Accepted: 05 August 2024;
Published: 11 September 2024.
Edited by:
John Martin Corkery, University of Hertfordshire, United KingdomReviewed by:
André Luiz Monezi Andrade, Pontifical Catholic University of Campinas, BrazilMoses Kachama Nyongesa, Aga Khan University (Kenya), Kenya
Copyright © 2024 Ebrahim, Adams and Demant. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jemal Ebrahim, amVtYWxlYnJhaGltLnNoaWZhQHN0dWRlbnQudXRzLmVkdS5hdQ==
 Jemal Ebrahim
Jemal Ebrahim Jon Adams
Jon Adams Daniel Demant
Daniel Demant