- 1Maynooth University, Maynooth, Ireland
- 2Department of Psychology, Sport and Geography, University of Hertfordshire, Hatfield, United Kingdom
Introduction: High levels of depression and low sense of control have been reported during the COVID-19 pandemic. The removal of typical freedoms through public health restrictions may have played an important role. The aim of this review was to examine data collected during the pandemic and (1) estimate the strength of the association between sense of control and depression, (2) examine whether the different types of control measures affected the strength of the association, and (3) whether this changed as a function of pandemic indicators.
Methods: We conducted a systematic review and meta-analysis of studies published in English between December 2019 and November 2022. A total of 993 articles were identified, of which 20 were included in the review and 16 in the meta-analysis after conducting a quality assessment using the standard NIH tool.
Results: The control–depression association gave a bias-independent pooled effect size of r = .41, and grew stronger over the 130 weeks covered by this review but did not change as a function of local COVID incidence rates. Subgroup analyses showed that external and overall control were more strongly related to depression than internal control.
Discussion: These findings emphasize that external factors are important to the sense of control and the importance of preserving the sense of control in situations where the removal of personal freedoms is necessary, such as public health emergencies.
1 Introduction
Sense of control is an important correlate of depression, with a lower sense of control predicting higher levels of depression (1–3). Low-control situations tend to induce cognitive, affective and behavioral changes that can result in depression (4). Given the removal of personal freedom during the COVID-19 pandemic, higher levels of depression are not unexpected (5). Therefore, the key aim of this study was to estimate the size of the association between sense of control and depression using data collected during the pandemic and to determine whether the type of control measured is a factor. A further key prediction tested is whether the strength of the control–depression association would change while the pandemic and as a function of pandemic indicators, such as incidence rates. This is because the sense of control would be predicted to change along with uncontrollable external factors, such as case numbers and changes in the levels of restrictions imposed by authorities. This review examined these questions.
1.1 Background
A large body of work has examined the sense of control and depression in the normal population, e.g (3)., and also in situations that might be considered uncontrollable, such as the case of aging populations (6), people with cancer (7), chronic illness (8), and life changing injuries (9). In all these examples, the relationship between sense of control and depression is evident and significant. People with a low sense of control tend to have higher levels of depression. Moreover, maintaining a sense of control, even if the overall outcome itself is uncontrollable, is key to coping with challenging situation (10).
It is important to note that different aspects of the sense of control have been studied. For example, Lachman and Weaver (3), like others, e.g (11)., distinguished between internally focussed control, sometimes labeled ‘mastery,’ which refers personal effectiveness in getting things done; and externally focussed control, labeled ‘perceived constraints,’ which refers to the external obstacles and factors external to the person which prevent them from reaching their goals. Interestingly, Lachman and Weaver (3) found that the relationship between externally focused control and depression (r range = |.24| to |.48|) was stronger than that between internally focused control and depression (r range = |.19| to |.27|). Similarly, Infurna and Mayer (12) noted that external control was more strongly related to mental health than internal control (13). Given the focus here on restrictions during the pandemic, we would expect that the lack of control with an external focus, such as the perception of large external obstacles blocking goals, would have a stronger predictive value in relation to depression than internal control during this time frame.
Therefore, the question to be answered here is whether the data collected by many researchers on mental health during the pandemic are consistent with this hypothesis. There is evidence of higher levels of depression. For example, a recent meta-analysis reported pre-COVID rates of 8.7% [95% Confidence Limits, CL: 6.2%, 11.5%], which increased to 18.3% during COVID [95% CL 13.5%–24.3%] in data collected up to July 2020 (14). Another meta-analysis (5) showed that depression levels were seven times higher than normal levels. Similarly data from the European COVID Survey, collected in November 2020 and April 2021, showed that the prevalence of ‘probable depression’ was very high at 26% (15). These studies, therefore, demonstrate sharp increases in depression levels during the pandemic, which is consistent with our predictions.
Furthermore, evidence also supports the suggestion that changes in the sense of control as a function of restrictions may have played a role in worsening depression. For example, several studies have shown that sense of control mediated or moderated distress during lockdown (16–18). For example, Gan et al. (18) found that, in China, the two-month impact of province-wide lockdown on psychological distress was moderated by personal control, such that the negative impact was greater in those with lower personal control. Senan et al. (19) found that a greater number of public health restrictions that were perceived as distressful predicted higher depression levels, but this effect was reduced when people had a stronger sense of control. Taken together, these studies provide evidence of a link between people’s subjective experience of the pandemic and their mental health, such that those with a lower sense of control fared worse in terms of higher levels of depression.
Current studies have several limitations in relation to the questions addressed in this study. For example, there is little evidence linking patterns of control and depression to external indicators of pandemic progression and severity, although there is evidence that distress levels change over the over the first few months. Gan et al.’s (18) study compared distress in lockdown and personal quarantine participants in China at two weeks and two months into the pandemic. Fancourt et al. (20) examined depression over the first 20 weeks of the lockdown in the United Kingdom and reported that initial increases in depression were alleviated over that time frame. We have not identified any other studies thus far that link psychological patterns to objective pandemic indicators, or directly examine the nature and changes in the sense of control and depression association. Given the speed at which data on mental health were collected and published during the pandemic, a systematic review is justified. In addition, the availability of open data on pandemic indicators makes it possible to examine mental health data alongside these indicators.
Thus, the aims of this study were to estimate the size of the association between sense of control and depression during the covid pandemic, identify the salient features of the same association, and check whether the effect size for the depression control association changes as a function of pandemic indicators, such as the local incidence rates of covid and the duration of the pandemic. To address these aims, we carried out a systematic review and meta-analysis with all the details described below.
2 Methods
The reporting of this systematic review and meta-analysis was guided by the 2020 PRISMA statement (21).
2.1 Search strategy
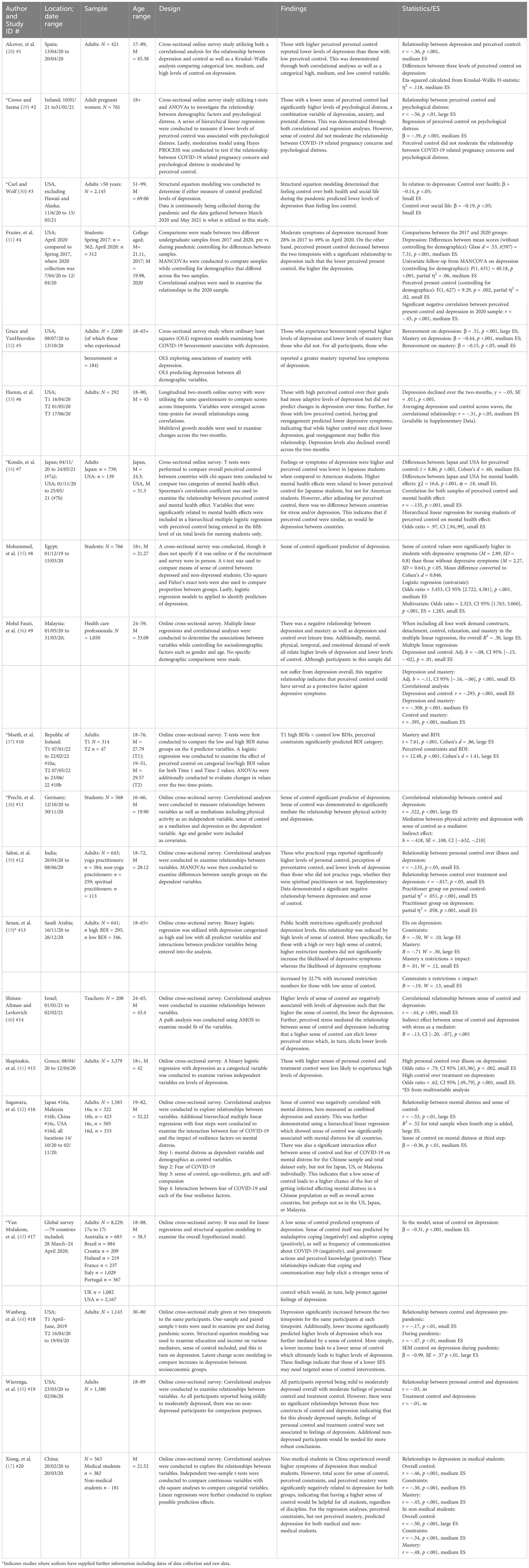
Web of Science, SCOPUS, Embase, PubMed, PsycInfo, CINAHL complete, and EBSCO academic search complete databases were searched using the following keywords: ((covid) OR (covid-19) OR (pandemic) OR (SARS) OR (corona)) AND ((sense of control) OR (perception of control) OR (perceived control)) AND ((depression) OR (depressed) OR (depressive)) in titles, abstracts, and keywords in each database. The authors chose these search terms to address the research questions specified above. Figure 1 shows a flow diagram of the search and selection processes. All papers identified in the searches were imported into Covidence software (23), which automatically removed duplicates. One author (YH) screened the titles and abstracts, while two authors (YH and RM) independently screened the full-text articles. The Covidence platform records agreements, disagreements, and resolutions between the reviewers.
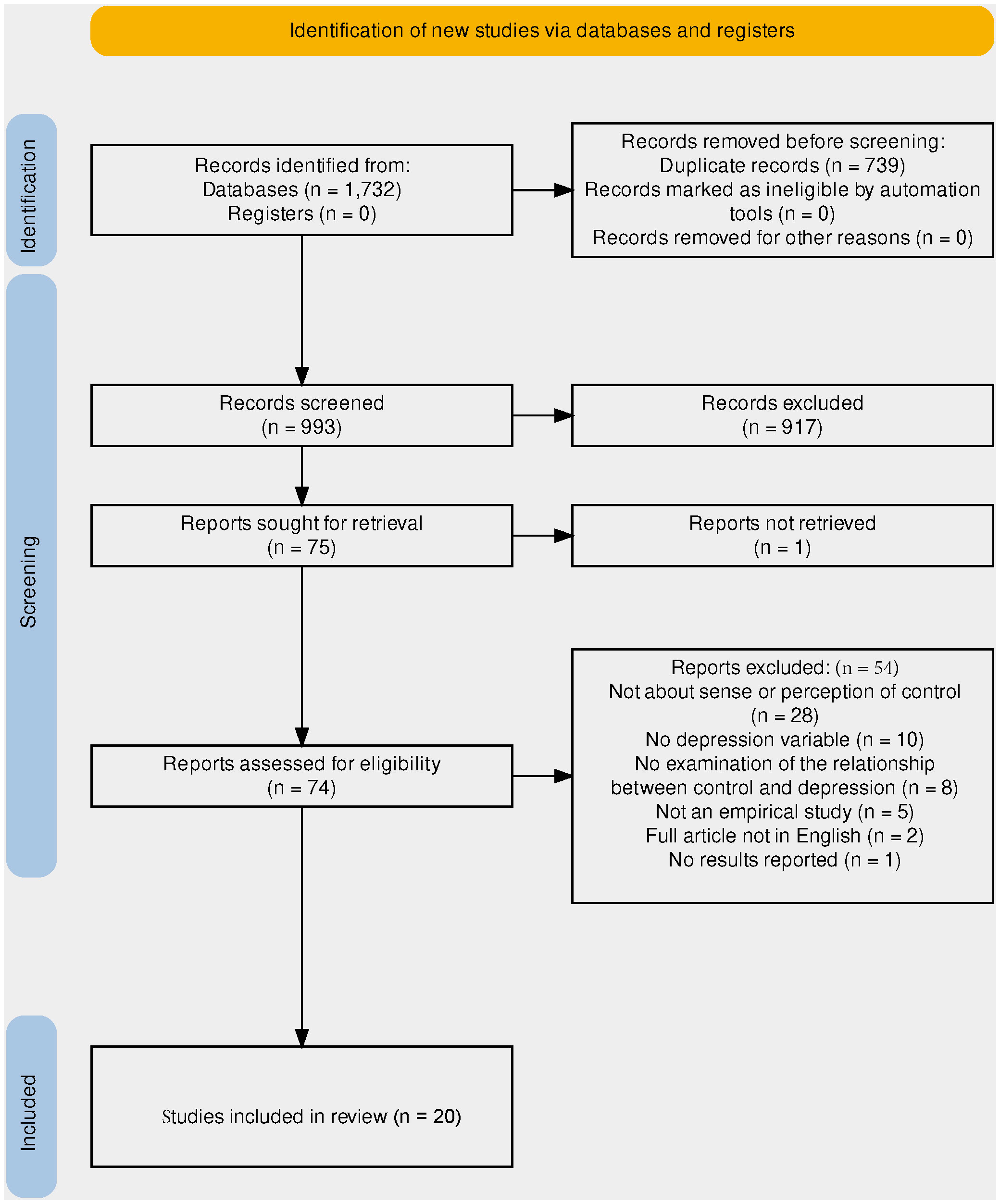
Figure 1 PRISMA flowchart (22) describing the identification and selection of studies for inclusion in the review. *Full article was not available.
2.2 Selection criteria
Studies were eligible for inclusion in this review if they reported the results of empirical investigations using quantitative measures of sense of control and depression, with the relationship between the two variables studied. The inclusion criteria were peer-reviewed journal articles ‘published in English’ after and including December 2019 and up until the final search date of 7 November 2022.
On the other hand, papers were excluded if they did not focus on sense of control, perception of control, or personal control, which are constructs that describe people’s views of themselves in relation to the environment. An example of an exclusion would be a study focusing on locus of control, which is considered to be a general orientation (24) or coping style (25), although it can be malleable to change (26). Studies were also excluded if they did not measure symptoms of depression or examine the relationship between sense of control and depression.
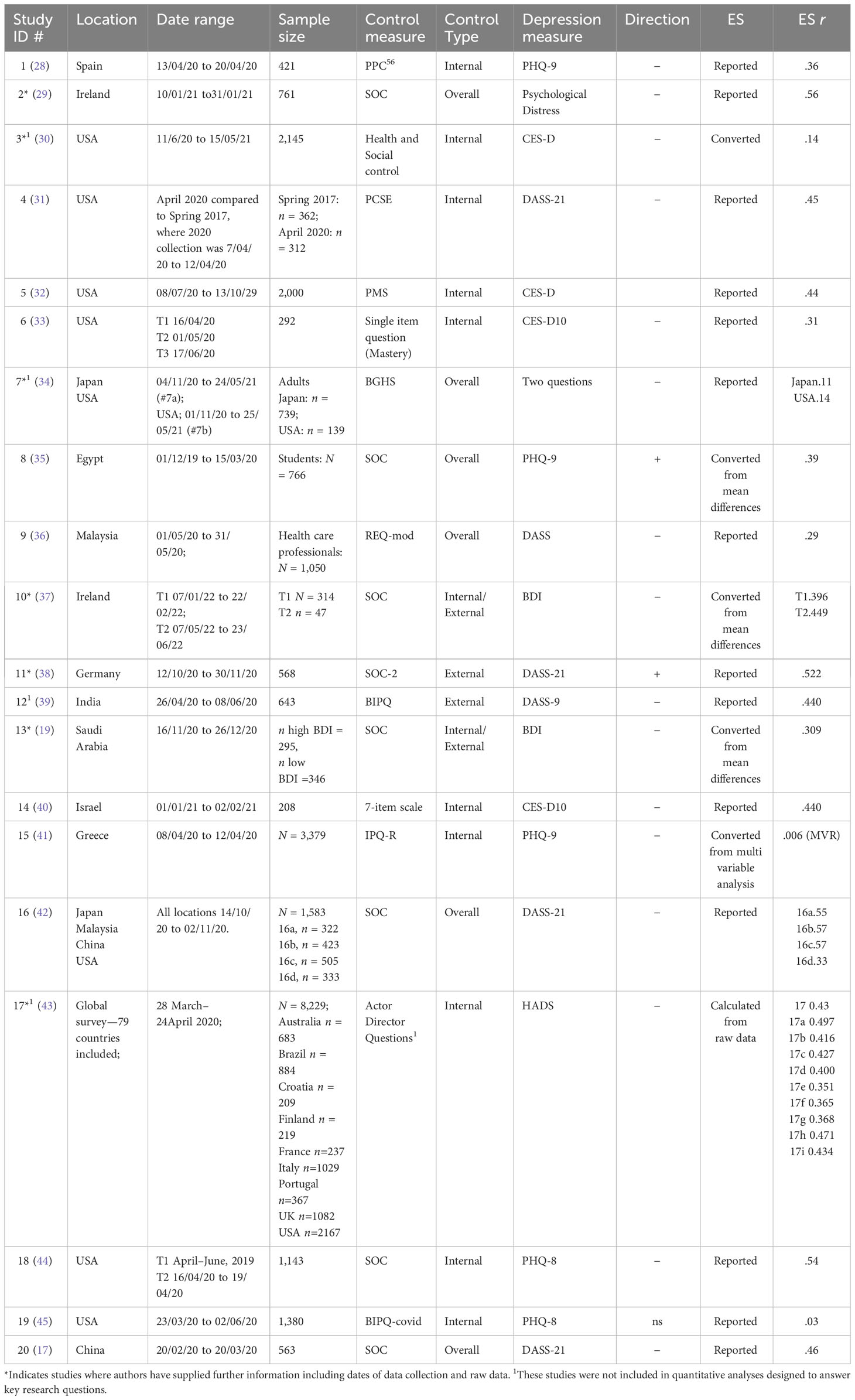
2.3 Quality assessment
The quality of studies was assessed using the National Heart, Lung, and Blood Institute of the National Institutes of Health (NIH) quality assessment tool for observational, cohort, and cross-sectional studies (27). This tool includes 14 criteria or questions that should be addressed; for example, “Was the research question or objective in this paper clearly stated?,” with outcomes being ‘yes,’ ‘no,’ or ‘other’ (including ‘cannot determine,’ ‘not applicable,’ ‘not reported’). In cases where an ‘not applicable’ outcome is not relevant to the quality rating, it does not count negatively to the rating. The evaluation was conducted independently by two of the authors (YH and RM), with any areas of initial disagreement discussed and a consensus reached. Initial inspection of quality evaluations indicated that bias was introduced into most studies due to low participant-to-population ratios (Q3, 19/20 studies) and use of cross-sectional designs (Qs 6, 7, and 10, 16/20 studies). More risky, in relation to the aims of the current review, were quality criteria related to the measurement of the predictor and outcome variables (Q9, sense of control, Q11, depression). Four studies used unusual measures of sense of control and one study used an unusual measure of depression. Other studies have used standard and well validated measurement tools. We weighted the predictor and outcome variable criteria most highly in our evaluation, as assessing the association between them was the key aim of the review, and unusual measurements would be predicted to introduce significant bias. Therefore, a weight of −2 was applied if there was non-compliance with criteria 9 and 11, with weight = −1 given to non-compliance with all other criteria. We then reviewed the overall scores and used them to inform but not to determine our overall evaluation. The classification process concluded with k = 3 studies classified at ‘good,’ k = 13 as ‘fair,’ and k = 4 as ‘poor.’ Note that studies classified as poor were classified as such in relation to the specific questions addressed in this review, which were not necessarily the focus of the original studies. Thus, our quality evaluation should not be interpreted as a general evaluation of the quality of these studies. The results of this quality assessment are presented in Table 1. The implications of the quality evaluation are described in the Results section.
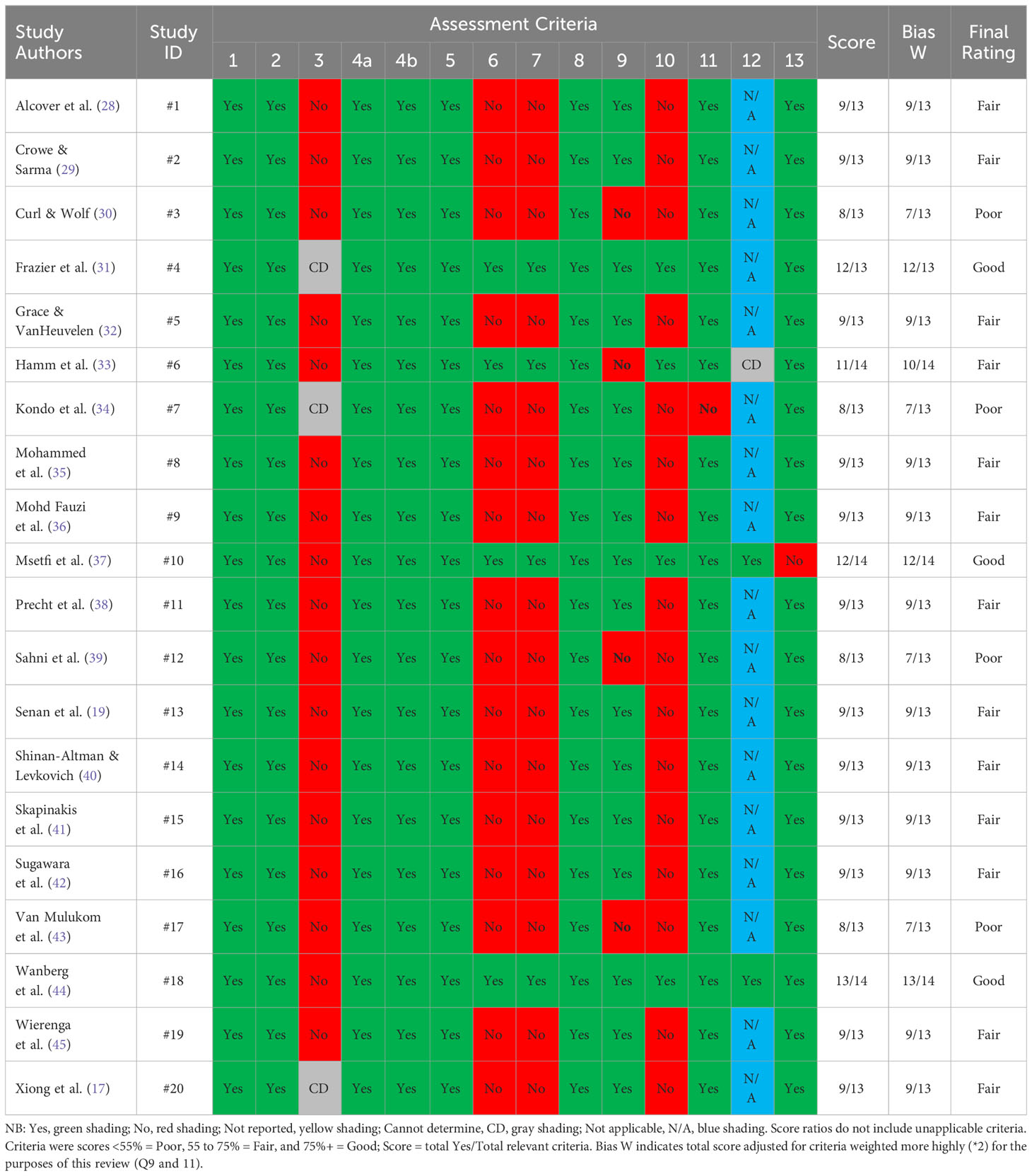
Table 1 Quality assessment of studies included in the review using NIH guidelines for observational cohort and cross-sectional studies.
2.4 Data acquisition and coding
Data were extracted from each paper either through Supplementary Information or raw data supplied by the authors. These data included the effect and sample sizes, as well as the start and end dates of data collection. Overall, 38 effect sizes were derived from 20 manuscripts. In addition, data on global 14-day incidence rates per 100,000 COVID-19 cases per country during the pandemic were retrieved from the European Centre for Disease Prevention and Control (46). These data were reported weekly throughout the pandemic, with week 1 representing the first week of January 2020. The dataset ceased to be updated on 1 November 2022.
The ECDC data were matched to the data collection time frame of the retrieved studies per week, from weeks 1 to 128 (where weeks 53 to 104 represent 2021). Where mental health data collection commenced prior to 1 January 2020, or the ECDC reported NA in relation to cases, 0 cases were assumed. Data collection weeks prior to 2020 were given negative values (i.e., −1, −2, etc.) for these analyses.
Given our aim to analyze mental health data alongside COVID data and the time frame of the pandemic for a given location, where data for multiple countries were summarized in the publication, these data are reported here per country, where sample size per country permitted. We also included the continent classification obtained from the ECDC data in the analysis. Where necessary, the corresponding authors were contacted to clarify the data collection time windows and locations, and in some cases, to obtain the raw data so that the relevant values could be recalculated. Values were calculated from the raw data supplied to us, as indicated in the data summary.
2.5 Target variables
The main target variable was the absolute value of the effect size r derived from the simple correlation between sense of control and depression. Where mean differences were available, Cohen’s d was calculated and converted to r. If β values were provided from multiple regression analyses, the simple r value was used if reported, obtained from Supplementary Data, or recalculated from the raw data; otherwise, the β was converted to r. The standard error of r and weight of each case were calculated for each of the 38 effect sizes found in the 20 included articles. The r values were then transformed using Fisher’s r-to-Z transformation, (ESZ). All statistical analyses were performed using ESZ as the target variable.
The key predictor variables in the data set were data collection start week, study duration, COVID incidence rates during start week and end week (indices of pandemic severity), study continent, and type of control (categorized as “internal” referring to mastery or the ‘I’ focussed control, “external” referring to external constraints or external forces which affect the individual’s control, or “overall” control, and a general measure which encompasses both of these factors and other aspects of control.
2.6 Analyses
The meta-analyses were conducted using the RStudio (Version 2022.12.0 + 353). The Metafor package (47) was used to conduct three-level meta-analyses so that multiple effect sizes from each study could be used where available, thus accounting for measure dependence by nesting each measurement within the study. Nested three- and two-level models were examined, with the nested model providing a better fit, AIC and BICNested <AIC and BIC2 level, the likelihood ratio test was significant (χ2 = 32.91, p <.00001). Therefore, nested models were used in this study. Meta-analyses were conducted on Fisher z transformed r-values to avoid bias.
3 Results
3.1 Study characteristics
The search identified 1,732 manuscripts, of which 739 were duplicates. The remaining 993 titles and abstracts were screened using 75 full-text articles that were assessed for eligibility. After applying the exclusion criteria, 20 manuscripts remained with a total of 27,685 participants. The countries covered were Asia (India, China, Korea, Malaysia, Japan), the Middle East (Egypt, Israel, Saudi Arabia), Americas (Brazil, USA, Canada), Europe (Croatia, Finland, France, Greece, Germany, Ireland, Italy, Portugal, Spain, UK), and Australia.
All 20 studies reviewed used a cross-sectional survey design approach. Of these, two were longitudinal variables measured at multiple time points. Two other studies compared data collected prior to the pandemic with data collected to determine if the levels of sense of control and depression changed. The remaining 16 studies examined data collected during a specified timeframe of survey distribution, which varied in duration from one to 49 weeks, with a median data collection time window of 4 weeks (M = 8.38, SE = 1.83). Further information is provided in Table 2, including measures of depression and controls used, the size and nature of samples, the location and timing of the study, and key findings.
All studies, except one (45), reported a significant relationship between sense of control and depression. When comparisons were reported between data collected prior to and during the pandemic, depression levels were higher and sense of control levels were lower in 2017 than in 202 (31), and those studies that compared depression levels at several points during the pandemic reported that levels decreased over time (33, 37).
3.2 Quantitative analyses
A summary of these data is presented in Table 3. The effect sizes varied from r = .006 to.57. Of the 20 studies, 14 studies reported simple correlations, and five reported other effect size values or descriptive statistics, which were converted to r and then Fishers z transformed. The authors of one study provided raw data, and the simple correlation between depression and one of the control items was re-calculated by the current authors. Overall, 38 effect sizes were obtained.
We wanted to check whether studies classified as ‘poor’ should be included in further quantitative analyses. Three-level meta-analysis models were fitted which estimated the overall ESZ across all effect sizes or only across those derived from studies classified as ‘fair’ or ‘good.’ Quality classification was included in each model as a categorical moderator. With all studies included in the model, the effect of quality approached reliability (QM(2) = 5.66, p = .0591). However, with k = 4 ‘poor’ studies removed from the model, quality did not have a reliable effect, QM(1) = 1.16, p = .2823. Therefore, we conducted the remaining analyses with only 16 studies that were categorized as fair or good with 24 nested observations. We were able to use this data to answer the three questions posed below.
Q1. What was the pooled size of the association between sense of control and depression during the covid pandemic?
The overall results are shown as a forest plot in Figure 2. The pooled effect size was significant, ESZ = .44 [95% CL:.36,.52], Z = 10.40, p <.0001, with significant heterogeneity, QE (23) = 798.90, p < .001. This ESZ converts to r = .41, which is a medium to large effect size, using Cohen’s (48) conventions.
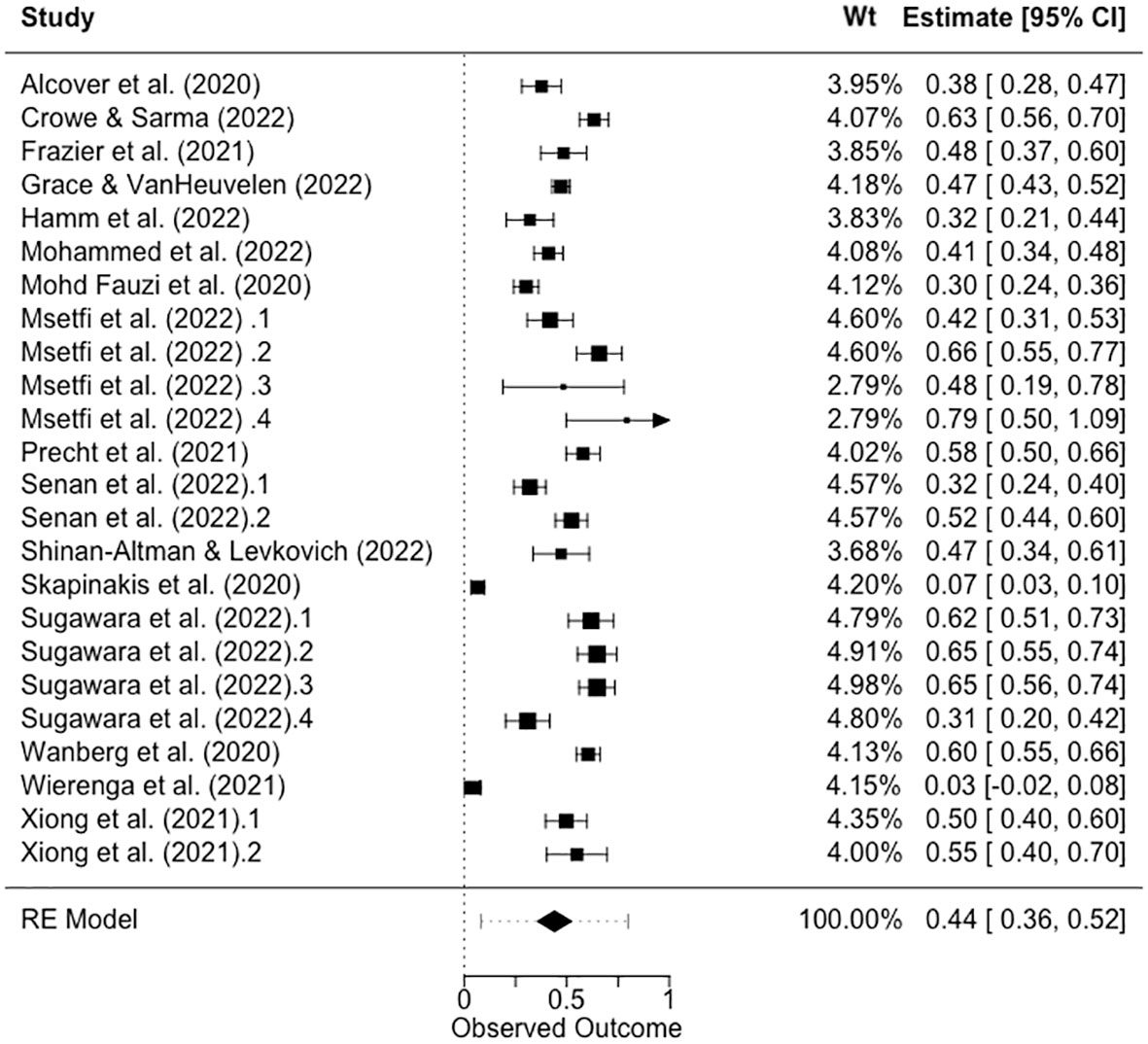
Figure 2 Forest plot showing the ESZ and pooled ESZ for the relationship between sense of control and depression. NB: 95% confidence limits are shown in square brackets.
Q2. What are the salient features of sense of control and depression association during the pandemic?
We fitted a three-level meta-analysis model that included moderator control type (3: internal, overall, and external). The results showed that I2Level 3 = 46.86% of the total variation can be attributed to between-cluster, and I2Level 2 = 47.57% to within-cluster heterogeneity, and that there was significant residual heterogeneity in the model (QE(21) = 569.93, p <.0001). The omnibus test of the control type was significant, F(2, 21) = 4.1465, p = 0.0304. The strongest association between control and depression was based on measuring ‘external’ control, estimate = .60 (se = .0867), t(21) = 6.89, p <.0001, with the association between ‘overall control’ and depression being weaker but not significantly so, estimate = .49 (se = .1103), t(21) = .94, p = .3591, and internal control having the weakest association with depression, estimate = .35 (se = .0905), and this was a significant difference, t(21)=2.68, p = .0141. The forest plot in Figure 3 shows the ESZ ordered per control-type variable.
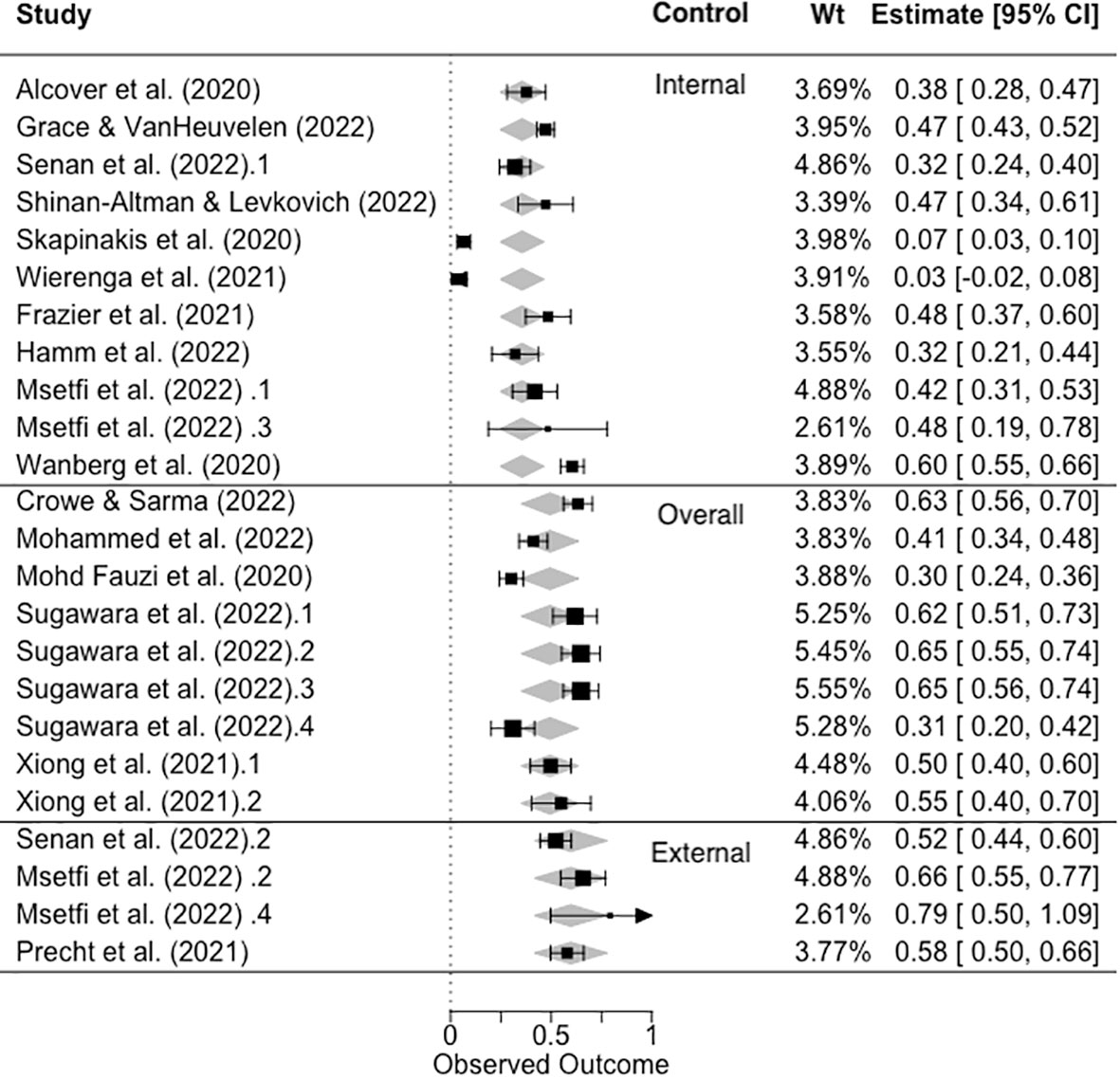
Figure 3 Forest plot showing the observed and fitted values of ESZ as a function of control type (internal, overall, and external). NB. Black symbols = observed values, gray diamonds = fitted values.
Q3. Does the effect size change as a function of pandemic indicators?
We fitted a three-level meta-analysis model, which included continuous moderators, start week, study duration, start week incidence (end week incidence was not included in the model due to the very high correlation with start week incidence r = .98) and the categorical moderator, continent (of data collection). The results showed that I2Level 3 = 48.63% of the total variation can be attributed to between-cluster heterogeneity, and I2Level 2 = 48.58% to within-cluster heterogeneity. There was significant residual heterogeneity in the model, QE(20) = 607.94, p <.0001 The omnibus test of the moderators was significant, F(4, 20) = 13.93, p <0.0001. Only one pandemic indicator was a significant predictor of effect size; the start week was positively related to effect size, estimate = .006, se = .0017, t (21) = 3.65, p = .0016. Study duration (p = .60), start week incidence (p = .54), and continent, (p = .12), were not predictive of the effect size. This shows that, as the pandemic progressed over the roughly two-year time frame of these data collections, the association between sense of control and depression was stronger (see Figure 4).
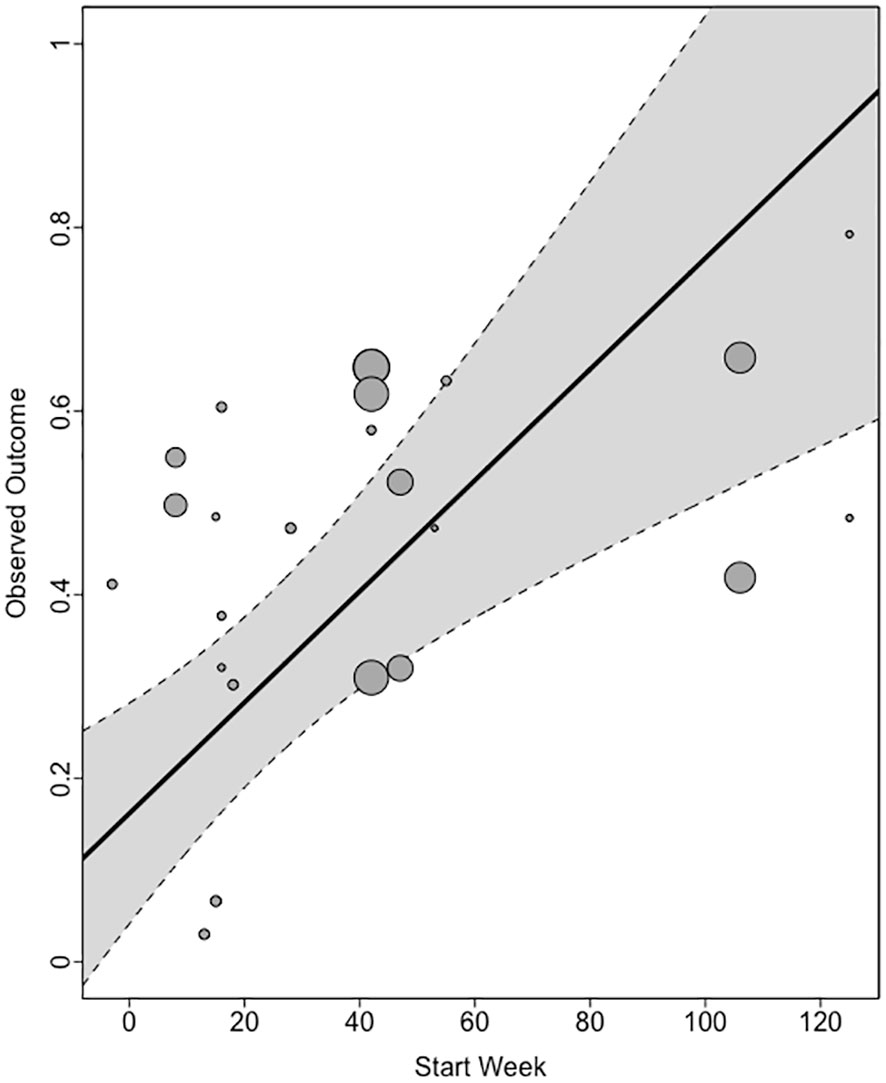
Figure 4 Relationship between start week and ESZ. Gray shading indicates the confidence limits of the model.
4 Discussion
The results of this systematic review and meta-analysis show that most studies (80%) that were conducted very rapidly during the pandemic, measuring sense of control and depression, were of fair or good quality. The key biasing factors identified were primarily related to the aims of this review and the measurement of our variables of interest, as opposed to the aims of the original studies. This review showed that the relationship between sense of control and depression during the pandemic was medium to large. The meta-analysis further indicated that this was strongest for external and overall controls and weakest for internal controls. Finally, the only pandemic indicator that was predictive of the control–depression relationship was the study start week, showing that as the pandemic progressed from 2020 to mid-2022, the relationship between control and depression became stronger. We discuss these findings in relation to the previous evidence and the limitations of this study.
We predicted that the relationship between a sense of control and depression would be strong during the time frame of the pandemic. Consistent with this, the pooled estimate of the correlation was r = .41. We also observed that external control and overall control explained more variance in depression (external control r = .48–.68; overall control r = .29–.57) than internal control (internal control, r = .03–.54). Again, this finding is consistent with our predictions, although it does not tell us whether the observed pattern is significantly different from that of pre-pandemic studies. For example, Lachman and Weaver (3) reported that the results of several large-sample studies showed that the relationship between control and depression varied similarly (r external|constraints = |.24| to |.48|; r internal |mastery = |.19| to |.27|).
On the basis of similar findings, we agree with Infurna and Mayer (12), who argued that internal and external controls, although related, are distinct constructs and should be analyzed separately. This review, and many other examinations of the measurement of the sense of control, emphasize that there is considerable variation in the manner in which this important construct is conceptualized and measured across studies (11), for example (49), and whether control is decomposed into its constituent parts as evidence suggests it should be (12). Consistent with this view, the quality evaluation showed that the measurement of key variables, such as control, introduced significant bias into the review, and we therefore excluded four papers from quantitative analysis for this reason. Moreover, it was not possible to categorize all effect sizes included in the review as reflecting internal or external control measurements, rather some we categorized as ‘overall control.’ In our view, the use of amalgamated overall control measures is limited because it is clear that external control, related to an individual’s perception of the external barriers and restrictions they face, is more strongly related to mental and physical health (3).
A key contribution of the current work is to show, for the first time, that the relationship between control and depression changed over the course of the pandemic from weeks −3 to 130. The relationship grew stronger, indicating that control explained more of the variance in depression over time. Note that this evidence does not speak to absolute levels of depression or control, and how they vary during the pandemic. This is important, as evidence is equivocal on whether increases in depression, observed in the first wave of the pandemic, alleviated (20), continued to accumulate (50), and which groups were most vulnerable (51). Irrespective of this, there are several possible explanations for the growing relationship reported here. First, in the context of high depression levels among those who may not have typically experienced depression symptoms (5), the strength of the sense of control as an explanatory factor grew over the course of the pandemic. This may indicate that the loss of control during the pandemic resulted in this vulnerability. Second, the dynamic nature of the pandemic, involving repeated waves of the virus, lockdowns being imposed, lifted and reimposed, and requirements to be vaccinated, may have cumulatively eroded many people’s sense of control over their lives, particularly in relation to the salience of external obstacles. These findings are consistent with this explanation.
An alternative explanation for the ‘pandemic effect’ that must be considered is that effect sizes vary over time in a manner unrelated to the pandemic. In other words, it might be a mere coincidence that the time variable (study start week) occurred during the pandemic, and the effect sizes would have changed irrespective of this. Evidence for the alternative explanation is that no other pandemic indicators (covid incidence, continent) tested in this review predicted effect size, and that sense of control changes over time based on mini trends/or changes over the lifespan (6). Another challenge relates to the directionality of the relationship between control and depression. It is unclear from the data reported here whether sense of control is part of the causal pathway to depression or vice versa. Stimpson (52) reported that the relationship between changes in depression and control, from before to and 60-days after a flood disaster, had a reciprocal relationship, such that changes in the sense of control acted like a feedback loop influencing the depression caused by the flood. According to Stimpson, it was the flood experience that caused depression, rather than changes in the sense of control. Irrespective, all this evidence is consistent with the widely held view that the sense of control is important in determining responses to an environment that is constantly changing, whether it is due to floods, a pandemic, or other factors.
Our detailed quality assessment of the studies included in this review emphasized the importance of the measures used in studies as a distinguishing feature between those categorized as poor and fair to good. This meant that four studies and 14 effect sizes were excluded, reducing the noise in the data and reducing the power of our analyses. In addition, many of the effect sizes (11 of 24, 46%) were based on data collected before pandemic week 26 (6 months), so the latter part of the pandemic or after the pandemic is under-researched, and the post-pandemic effects are still unknown. A related point refers to another bias identified in the quality assessment: over-reliance on cross-sectional studies. As Mirowsky (6) described, inferring longitudinal trends from cross-sectional data is fraught with potential misinterpretation. Regarding both points—data mainly derived from early in the pandemic and the reliance on cross-sectional data—long-duration longitudinal studies can reveal distinct and informative trends. For example, one study based in the UK reported that depression decreased from the date of the first lockdown to 20 weeks afterwards (20). Longitudinal data from a nationally representative sample in Denmark showed initial improvements in mental health during the first lockdown; however, mental health deteriorated as the pandemic progressed (50). This contrast demonstrates the need for caution when interpreting time-based trends, as in the current review.
5 Conclusion
The general consensus is that a pandemic has a negative impact on mental health (53, 54). This review confirms that changes in sense of control, particularly the perception of external constraints, played an increasingly large role in depression severity as the pandemic progressed. Future research should measure the components of sense of control to better inform interventions. At the policy level, the clinical implication is that public health restrictions should be designed to provide as much autonomy as possible, preserve people’s feelings of control, and protect their mental health. Good quality longitudinal studies are also important, as the jury is still out regarding the long-term recovery from pandemic-induced mental health deterioration and the long-term effects of the pandemic.
Author contributions
RM: Conceptualization, Data curation, Formal analysis, Methodology, Resources, Supervision, Visualization, Writing – original draft, Writing – review & editing. DK: Formal analysis, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing. YH: Data curation, Formal analysis, Project administration, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1323306/full#supplementary-material
References
1. Mirowsky J, Ross CE. Control or defense? Depression and the sense of control over good and bad outcomes. J Health Soc Behav (1990) 31:71–86. doi: 10.2307/2137046
2. Steptoe A, Tsuda A, Tanaka Y, Wardle J. Depressive symptoms, socio-economic background, sense of control, and cultural factors in university students from 23 countries. Int J Behav Med (2007) 14:97–107. doi: 10.1007/bf03004175
3. Lachman ME, Weaver SL. The sense of control as a moderator of social class differences in health and well-being. JPSP (1998) 74:763. doi: 10.1037/0022-3514.74.3.763
4. Maier SF, Seligman ME. Learned helplessness: Theory and evidence. J Exp Psychology-General (1976) 105:3–46. doi: 10.1037/0096-3445.105.1.3
5. Bueno-Notivol J, Gracia-Garcia P, Olaya B, Lasheras I, Lopez-Anton R, Santabarbara J. Prevalence of depression during the COVID-19 outbreak: A meta-analysis of community-based studies. Int J Clin Health Psychol (2021) 21. doi: 10.1016/j.ijchp.2020.07.007
6. Mirowsky J. Depression and the sense of control: Aging vectors, trajectories, and trends. J Health Soc Behav (2013) 54:407–25. doi: 10.1177/0022146513499022
7. Mystakidou K, Tsilika E, Parpa E, Galanos A. The influence of sense of control and cognitive functioning in older cancer patients’ depression. Psycho-Oncology (2015) 24:311–7. doi: 10.1002/pon.3642
8. Wallhagen MI, Brod M. Perceived control and well-being in Parkinson’s disease. Western J Nurs Res (1997) 19:11–25. doi: 10.1177/019394599701900102
9. Craig A, Hancock K, Chang E, Dickson H. The effectiveness of group psychological intervention in enhancing perceptions of control following spinal cord injury. Aust N Z. J Psychiatry (1998) 32:112–8. doi: 10.1046/j.1440-1614.1998.00376.x
10. Thompson SC, Sobolew-Shubin A, Galbraith ME, Schwankovsky L, Cruzen D. Maintaining perceptions of control: finding perceived control in low-control circumstances. JPSP (1993) 64:293. doi: 10.1037/0022-3514.64.2.293
11. Skinner EA. A guide to constructs of control. JPSP (1996) 71:549–70. doi: 10.1037/0022-3514.71.3.549
12. Infurna FJ, Mayer A. The effects of constraints and mastery on mental and physical health: Conceptual and methodological considerations. Psychol Aging (2015) 30:432. doi: 10.1037/a0039050
13. Infurna FJ, Kappes C, Fraire N. Long-term antecedents of constraints and mastery: Findings from the Health and Retirement Study. Psychol Aging (2018) 33:965–74. doi: 10.1037/pag0000281
14. Schafer KM, Lieberman A, Sever AC, Joiner T. Prevalence rates of anxiety, depressive, and eating pathology symptoms between the pre- and peri-COVID-19 eras: A meta-analysis. J Affect Disord (2022) 298:364–72. doi: 10.1016/j.jad.2021.10.115
15. Hajek A, et al. Prevalence and determinants of probable depression and anxiety during the COVID-19 pandemic in seven countries: Longitudinal evidence from the European COvid Survey (ECOS). J Affect Disord (2022) 299:517–24. doi: 10.1016/j.jad.2021.12.029
16. Brailovskaia J, Margraf J. Predicting adaptive and maladaptive responses to the Coronavirus (COVID-19) outbreak: A prospective longitudinal study. Int J Clin Health Psychol (2020) 20:183–91. doi: 10.1016/j.ijchp.2020.06.002
17. Xiong P, Ming W-k, Zhang C, Bai J, Luo C, Cao W, et al. Factors influencing mental health among Chinese medical and non-medical students in the early stage of the COVID-19 pandemic. Front Public Health (2021) 9:603331. doi: 10.3389/fpubh.2021.603331
18. Gan Y, et al. Immediate and delayed psychological effects of province-wide lockdown and personal quarantine during the COVID-19 outbreak in China. Psychol Med (2022) 52:1321–32. doi: 10.1017/S0033291720003116
19. Senan S, Halbrook Y, Kornbrot DE, Msetfi RM. Depression symptoms and the perception of public health restrictions during the COVID-19 pandemic in Saudi Arabia: The protective effect of sense of control. Prev Med Rep (2022), 101836. doi: 10.1016/j.pmedr.2022.101836
20. Fancourt D, Steptoe A, Bu FF. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiat (2021) 8:141–9. doi: 10.1016/S2215-0366(20)30482-X
21. Page MJ, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev-London (2021) 10. doi: 10.1186/s13643-021-01626-4
22. Haddaway NR, Page MJ, Pritchard CC, McGuinness LA. PRISMA2020: An R package and Shiny app for producing PRISMA 2020-compliant flow diagrams, with interactivity for optimised digital transparency and Open Synthesis. Campbell Syst Rev 18:(2022). doi: 10.1002/cl2.1230
23. Covidence systematic review software. Melbourne, Australia (2022). Available at: www.covidence.org. V. H. I.
24. Rotter JB. Generalized expectancies for internal versus external control of reinforcement. psychol Monographs: Gen Appl (1966) 80:1. doi: 10.1037/h0092976
26. Ryon HS, Gleason ME. The role of locus of control in daily life. Pers Soc Psychol Bull (2014) 40:121–31. doi: 10.1177/0146167213507087
27. NIH National Heart Lung, Blood Institute. NIH quality assessment tool for observational cohort and cross-sectional studies. Study quality assessment tools (2013). Available online at: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed January 2023).
28. Alcover CM, et al. Group membership and social and personal identities as psychosocial coping resources to psychological consequences of the COVID-19 confinement. Int J Environ Res Public Health (2020) 17. doi: 10.3390/ijerph17207413
29. Crowe S, Sarma K. Coping with Covid-19: Stress, control and coping among pregnant women in Ireland during the Covid-19 pandemic. BMC Pregnancy Childbirth (2022) 22:1–12. doi: 10.1186/s12884-022-04579-1
30. Curl AL, Wolf KE. The impact of COVID-19 on depressive symptoms and loneliness for middle-aged and older adults. Sustainability (2022) 14:6316. doi: 10.3390/su14106316
31. Frazier P, Liu Y, Asplund A, Meredith L, Nguyen-Feng VN. US college student mental health and COVID-19: Comparing pre-pandemic and pandemic timepoints. J Am Coll Health (2021) 1–11. doi: 10.1080/07448481.2021.1987247
32. Grace MK, VanHeuvelen JS. Psychosocial coping resources and the toll of COVID-19 bereavement. Soc Ment Health (2022) 1–23. doi: 10.1177/21568693221113221
33. Hamm JM, Tan JX, Barlow MA, Delaney RL, Duggan KA. Goal adjustment capacities in uncontrollable life circumstances: Benefits for psychological well-being during COVID-19. Motivation Emotion (2022), 1–17. doi: 10.1007/s11031-022-09941-6
34. Kondo A, Abuliezi R, Niitsu K, Naruse K, Oki T, Ota E, et al. Factors related to mental health effect among nursing students in Japan and the United States during the coronavirus pandemic: A cross-sectional study. Int J Ment Health Nurs (2022). doi: 10.1111/inm.13075
35. Mohammed HM, Soliman SM, Abdelrahman AA, Ibrahim AK. Depressive symptoms and its correlates among medical students in Upper Egypt. Middle East Curr Psychiatry (2022) 29:1–9. doi: 10.1186/s43045-022-00231-y
36. Mohd Fauzi MF, et al. Doctors’ mental health in the midst of COVID-19 pandemic: The roles of work demands and recovery experiences. Int J Environ Res Public Health (2020) 17:7340. doi: 10.3390/ijerph17197340
37. Msetfi R, Kornbrot D, Halbrook YJ, Senan S. Sense of control and depression during public health restrictions and the COVID-19 pandemic. Int J Environ Res Public Health (2022) 19:14429. doi: 10.3390/ijerph192114429
38. Precht L-M, Margraf J, Stirnberg J, Brailovskaia J. It’s all about control: Sense of control mediates the relationship between physical activity and mental health during the COVID-19 pandemic in Germany. Curr Psychol (2021), 1–9. doi: 10.1007/s12144-021-02303-4
39. Sahni PS, Singh K, Sharma N, Garg R. Yoga an effective strategy for self-management of stress-related problems and wellbeing during COVID19 lockdown: A cross-sectional study. PloS One (2021) 16:e0245214. doi: 10.1371/journal.pone.0245214
40. Shinan-Altman S, Levkovich I. Are personal resources and perceived stress associated with psychological outcomes among Israeli teachers during the third COVID-19 lockdown? Int J Environ Res Public Health (2022) 19:5634. doi: 10.3390/ijerph19095634
41. Skapinakis P, et al. Depression and its relationship with coping strategies and illness perceptions during the COVID-19 lockdown in Greece: a cross-sectional survey of the population. Depression Res Treat (2020) 2020. doi: 10.1155/2020/3158954
42. Sugawara D, et al. Mental health and psychological resilience during the COVID-19 pandemic: A cross-cultural comparison of Japan, Malaysia, China, and the US. J Affect Disord (2022) 311:500–7. doi: 10.1016/j.jad.2022.05.032
43. Van Mulukom V, Muzzulini B, Rutjens BT, Van Lissa CJ, Farias M. The psychological impact of threat and lockdowns during the COVID-19 pandemic: Exacerbating factors and mitigating actions. Trans Behav Med (2021) 11:1318–29. doi: 10.1093/tbm/ibab072
44. Wanberg CR, Csillag B, Douglass RP, Zhou L, Pollard MS. Socioeconomic status and well-being during COVID-19: A resource-based examination. J Appl Psychol (2020) 105:1382. doi: 10.1037/apl0000831
45. Wierenga KL, Moore SE, Pressler SJ, Hacker ED, Perkins SM. Associations between COVID-19 perceptions, anxiety, and depressive symptoms among adults living in the United States. Nurs Outlook (2021) 69:755–66. doi: 10.1016/j.outlook.2021.03.020
46. ECDC. European Centre for Disease Prevention and Control. (2005-2022). Available online at: https://www.ecdc.europa.eu/en/publications-data/data-daily-new-cases-covid-19-eueea-country.
47. Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat software (2010) 36:1–48. doi: 10.18637/jss.v036.i03
48. Cohen J. Statistical power analysis for the behavioral sciences. New York: Academic press (2013).
49. Mirowsky J, Ross CE. Eliminating defense and agreement bias from measures of the sense of control: A 2 x 2 index. SPsy (1991), 127–45. doi: 10.2307/2786931
50. Cardona M, Andersen LH, Fallesen P, Bruckner TA. Stress/depression across the COVID-19 pandemic in Denmark. BMC Public Health (2023) 23:169. doi: 10.1186/s12889-023-15129-5
51. Pedersen MT, et al. Time trends in mental health indicators during the initial 16 months of the COVID-19 pandemic in Denmark. BMC Psychiatry (2022) 22:1–13. doi: 10.1186/s12888-021-03655-8
52. Stimpson JP. Prospective evidence for a reciprocal relationship between sense of control and depressive symptoms following a flood. Stress Health: J Int Soc Invest Stress (2006) 22:161–6. doi: 10.1002/smi.1091
53. Leung CMC, Ho MK, Bharwani AA, Cogo-Moreira H, Wang Y, Chow MSC, et al. Mental disorders following COVID-19 and other epidemics: a systematic review and meta-analysis. Trans Psychiatry (2022) 12:205. doi: 10.1038/s41398-022-01946-6
Keywords: public health restrictions, mental health, depression, sense of control, COVID, pandemic (COVID19)
Citation: Msetfi RM, Kornbrot DE and Halbrook YJ (2024) The association between the sense of control and depression during the COVID-19 pandemic: a systematic review and meta-analysis. Front. Psychiatry 15:1323306. doi: 10.3389/fpsyt.2024.1323306
Received: 17 October 2023; Accepted: 09 January 2024;
Published: 13 February 2024.
Edited by:
Renato de Filippis, University Magna Graecia of Catanzaro, ItalyReviewed by:
Tianshu Zhou, City University of Hong Kong, Hong Kong SAR, ChinaSaeid Komasi, Mind GPS Institute, Iran
Copyright © 2024 Msetfi, Kornbrot and Halbrook. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rachel M. Msetfi, cmFjaGVsLm1zZXRmaUBtdS5pZQ==
 Rachel M. Msetfi
Rachel M. Msetfi Diana E. Kornbrot
Diana E. Kornbrot Yemaya J. Halbrook1
Yemaya J. Halbrook1