- 1Midwifery Department, Reproductive Health Promotion Research Center, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
- 2Midwifery Department, Menopause Andropause Research Center, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
- 3Department of Public Health and Community Medicine, Tufts School of Medicine, Boston, MA, United States
- 4Psychiatry and Behavioral Center, Addiction Institute, Department of Pharmacology, Faculty of Medicine, Mazandaran University of Medical Sciences, Sari, Iran
- 5Psychiatry and Behavioral Sciences Research Center, Addiction Institute, Department of Pharmacology Faculty of Medicine, Mazandaran University of Medical Sciences, Sari, Iran
- 6Biostatistics Department, Public Health School, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
Background: Postpartum depression is a major psychiatric disorder that affects the mother-baby attachment and may impair cognitive development of the child.
Objective: This study aimed to evaluate the effect of curcumax (including ginger, turmeric, and black pepper) on postpartum depression in reproductive-aged women.
Material and methods: This was a randomized controlled trial in which 124 women were recruited and randomly assigned into two groups of curcumax (n=62) and placebo (n=62) who consumed curcumax or placebo for 8 weeks (one capsule each day). Postpartum depression was measured using Edinburgh Depression Scale. Data were analyzed using Chi-square, independent t-test, and GEE.
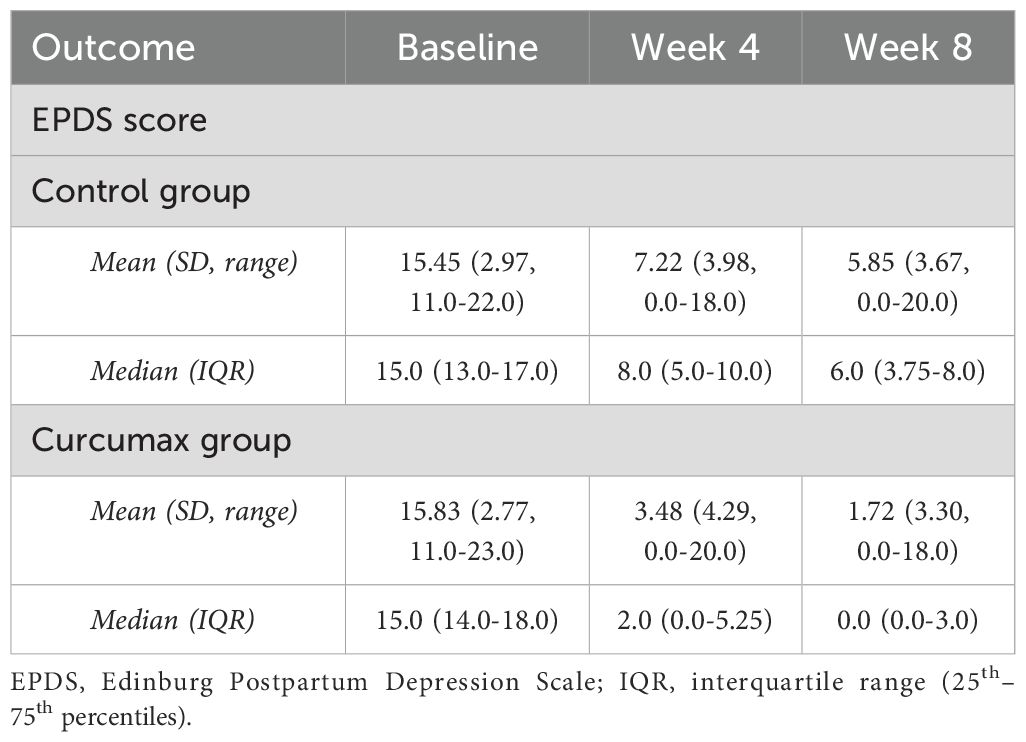
Results: The mean (SD) score of depression score was 15.83 (2.77) and 15.45 (2.97) before intervention, which reduced to 3.48 (4.29) and 7.22 (3.98) in the intervention and control groups, respectively after 4 weeks (p<0.0001). After eight weeks of intervention, these scores reduced to 1.72 (3.30) and 5.85 (3.67) in the intervention and control groups, respectively (p<0.0001).
Conclusion: The results of this study showed that curcumax significantly reduced the mean score of postpartum depression among reproductive-aged women. Because it is the first time this herb was used as an anti-depressant, its effective dose was not available. Therefore, further studies with higher doses of this herb are recommended.
Clinical Trial Registration: https://irct.behdasht.gov.ir/search/result?query=IRCT20210822052254N1, identifier IRCT20210822052254N1.
1 Introduction
Postpartum depression (PPD) is defined as a psychiatric disorder characterized by a drop in mood that can happen four weeks after birth until 30 weeks postpartum (1). Women who suffer from PPD may have symptoms such as depressed mood, irritability, episodes of crying without reason, feeling of tiredness, lack of concentration, and changes in sleep pattern (2). PPD can occur in women with different conditions such as high-risk pregnancy, a history of anxiety and premenstrual syndrome, dissatisfaction with the baby’s gender, and a history of sexual abuse (3). Insufficient social support (emotional and/or financial) may also cause PPD (4).
The prevalence of PPD has been reported differently in different parts of the world. A systematic review including 565 studies in different countries around the world showed that the prevalence of PPD is 17.22% with the highest rate being reported in South Africa (5). Another systematic review showed that the prevalence of PPD in Iran is 25.3%, which is almost doubled among women with a history of depression, illiterate women, and those having an undesired pregnancy (6). During the COVID-19 pandemic, the prevalence of PPD in Iran rose from 24.9% to 68.2% (7).
Untreated and severe PPD may delay the cognitive and language development of children and negatively affect the mother-baby attachment (8). A cohort study showed that women with PPD are more likely to show depression a few years after delivery and obtain low scores of general health in comparison to otherwise healthy women (9).
Diagnosis of PPD can be done using psychometric evaluation tests such as Edinburgh Postnatal Depression Scale (EPDS) (10), Postpartum Depression Screening Scale (PDSS), or Physician’s Health Questionnaire (11).
Treatment of PPD is often based on antidepressant medications such as fluoxetine (12). Other non-pharmacological methods such as cognitive behavioral therapy (13), electroconvulsive therapy (14), and bright light therapy are recommended for treatment of PPD (15).
Complementary and alternative medicine treatments include lavender (16), omega-3 fatty acids, folic acid, St. John’s Wort, exercise, and acupuncture (17). Curcumax is a mixture of three herbs namely turmeric, ginger, and black pepper. The ginger mitigates the pain by inhibiting lipoxygenase and cyclooxygenase and decreasing the secretion of prostaglandin (18). Curcumin derived from rhizome of Curcuma longa has many properties such anti-inflammatory, antioxidant, and anti-depressant effects (19). Black pepper, derived from Piper nigrum L, is a food spice that has been reported to have antidiabetic, hepatoprotective and neuroprotective effects (20). Although there is evidence suggesting the neuroprotective effect of ginger, turmeric and black pepper, there is little, if any, evidence showing the effect of their combination. Therefore, this randomized controlled trial was designed to evaluate the effect of curcumax on postpartum depression of reproductive-aged Iranian women.
2 Methods
This was a randomized controlled trial on 124 women with postpartum depression. The design of the study was approved by the Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (Ref. No: IR.AJUMS.REC.1400.336). The protocol of the study was registered in the Iranian Registry of Randomized Controlled Trials (Code No: IRCT20210822052254N1). All participants provided written informed consent prior to data collection.
2.1 Sample size
The sample size for this study was determined using the below formula based on comparing the means of two independent groups. In a previous study (21), the standard deviation for the EPDS's score (s) at the end of the study was reported as 7.0. The mean difference between the two groups (d) was considered to be 4.0. Using these values, with an alpha level of 0.05, a power of 0.85, and accounting for a 10% attrition rate, the required sample size for each group was calculated to be at least 62 pregnant women.
2.2 Inclusion/exclusion criteria
Women aged 18-35 who obtained scores between 12-23 from Edinburgh Postnatal Depression Scale (EPDS), had basic literacy, had a term and low risk pregnancy with a healthy neonate, and whose childbirth was 6 months prior to data collection were recruited for this study. Women with the following conditions were excluded from the study: allergy to herbal medicine, substance abuse, or severe depression. Women with severe depression and suicidal thoughts were referred to a psychiatrist.
2.3 Randomization and allocation concealment
For randomization, we used permuted block randomization technique with a block size of 6 and an allocation ratio of 1:1. The code dedicated to each group was written on a piece of paper and kept with the ward clerk of health center. Therefore, neither the researcher nor the participants knew about group allocation. Both the researcher who distributed medicines and the participants were blinded.
2.4 Setting
A health clinic (No 3) located in the west bank of Karun River in Ahvaz city was used for data collection. Ahvaz is the capital of Khuzestan province and has a population of 1,136,989 people.
2.5 Instruments
A demographic questionnaire and Edinburgh Postnatal Depression Scale (EPDS) were used to collect the data. The demographic questionnaire included questions about age, education, occupation, economic status, length of marriage, mode of delivery, and husband’s age, education, and occupation. The content validity of the demographic questionnaire was evaluated and confirmed.
EPDS has 10 questions scored based on a four-point scale: from 0: “never” to 3 for “often”. The minimum total score is zero and maximum total score is 30 (22). This scale can be used for the detection of postnatal depression from six weeks after delivery onward. The Persian version of this questionnaire was validated by KaniGolzar et al. in Iran (23).
2.6 Intervention
The Curcumax and placebo capsules were made in Pharmacology school of Ahvaz Jundishapur University of Medical Sciences. The curcumax capsules contain turmeric (the dried root powder, 320 mg), ginger (150 mg), and black pepper (4mg). Each placebo capsules (600 mg) contained Avicel (300 mg), Starch (258 mg), Gelatin (39 mg), Magnesium Stearate (3mg).
An equal number of curcumax and placebo capsules to be used for 8 weeks were prepared in separate containers that were identical in terms of shape, color, and size. The containers were coded by a person who was not aware of nature of the study. After randomization, each drug container was given to a participant, and the corresponding code was recorded. Participants were advised to take one curcumax or placebo capsule each day for 8 weeks. In case of they had any question or experienced any the side effect, they could call the researcher.
2.7 Follow-up
Four and eight weeks after initiation of intervention, the EPDS questionnaire was completed by the participants in both groups.
2.8 Statistical analyses
All data were imported into SPSS version 22. Quantitative variables were reported as mean and standard deviation, minimum and maximum. The qualitative variables were reported as numbers and percentages. The normality of quantitative variables was checked using the Shapiro-Wilk test. Chi-square test or Fisher’s exact test was used to examine the relationship between qualitative variables, and the Mann-Whitney test was used to compare quantitative variables between the two independent groups.
Association between changes in the EPDS's score over time and treatment groups (intervention, placebo) was examined by using generalized estimating equation (GEE) model. The GEE model consists of main effects (for treatment group, time, adjusted variables) and the interaction effect of time and treatment group. Three time points were considered in the analyses as baseline, week 4 and week 8. Pairwise comparisons after Bonferroni correction followed by GEE analysis. All tests were two sided and P-values < 0.05 were considered statistically significant.
3 Results
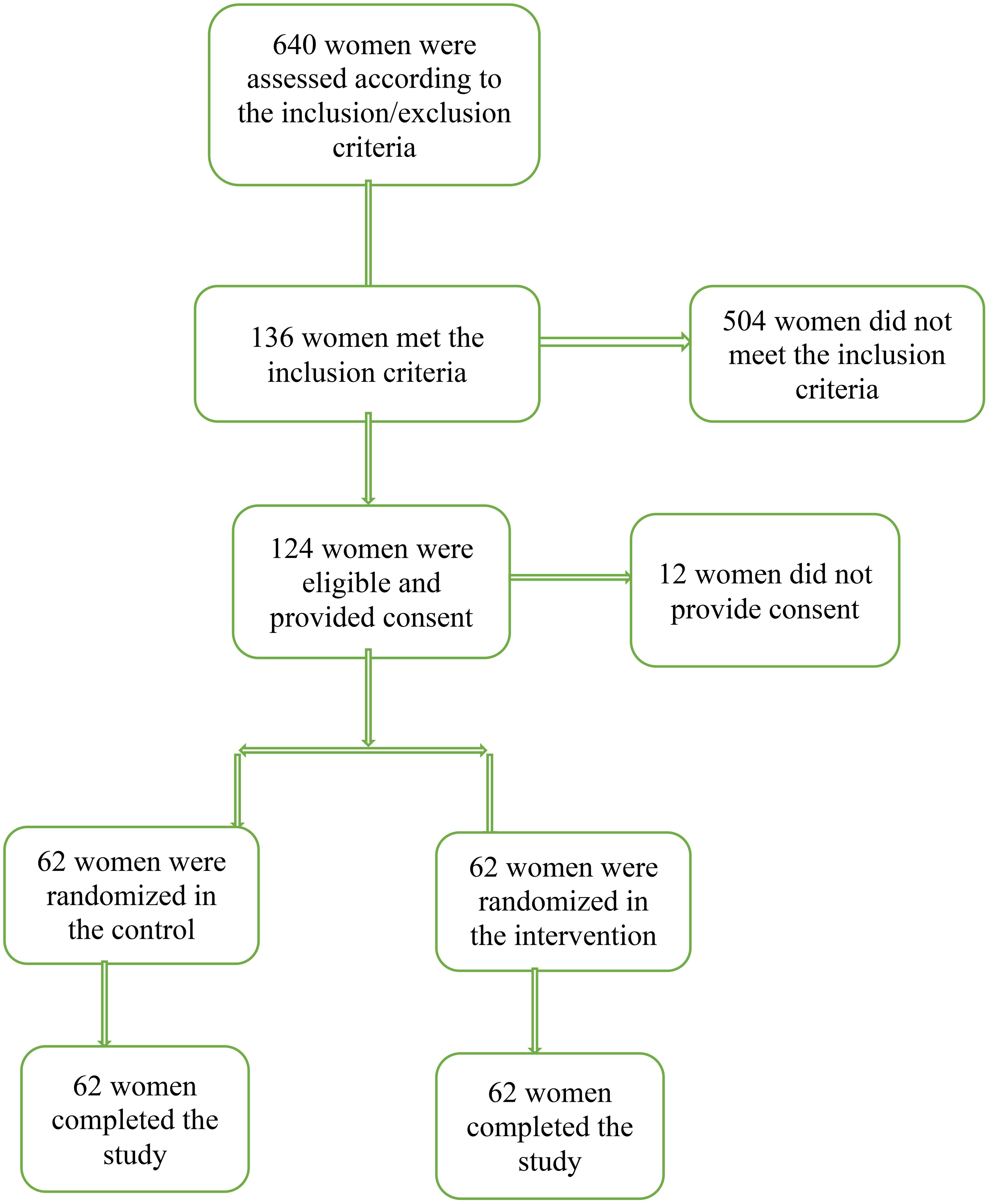
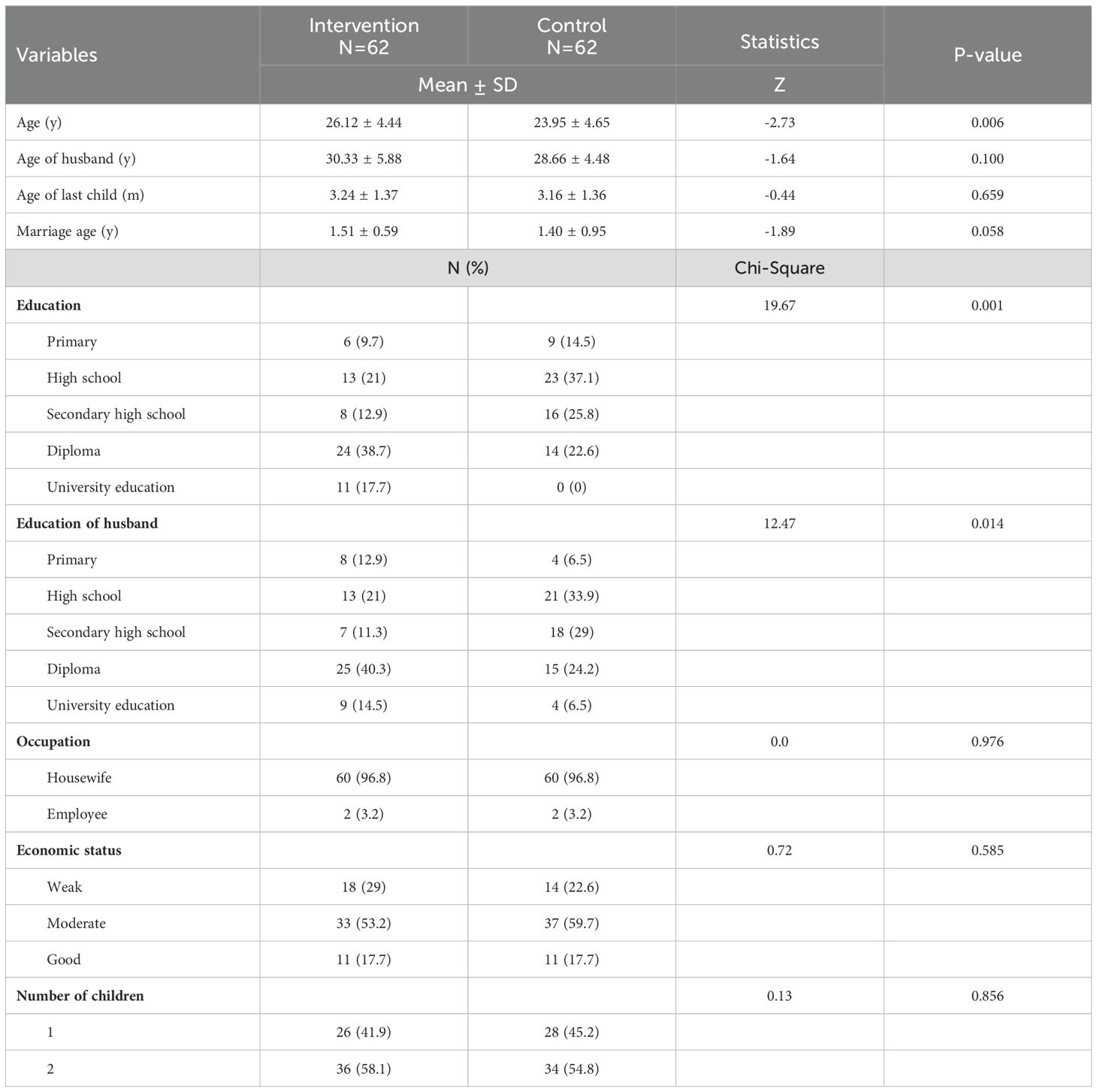
In this study, 124 women were recruited and randomized into two groups of curcumax and control. All women in both groups completed eight weeks of follow-up (Figure 1). The mean age of women in the curcumax and control groups was 26.12 ± 4.44 and 23.95 ± 4.65 years respectively. Most women 24(38.7%) in the intervention group had a diploma, while most women in the control 23(37.1%) group had high school education. Two groups showed a significant difference (p=0.001). The same was true with husbands. That is, 25(40.3%) husbands in the intervention group had a diploma, while most 21(33.9%) husbands in the control group had high school education. Two groups showed a significant difference regarding education of their husbands (p=0.014). Most women in the two groups were house-wives and had a moderate economic status (Table 1).
Table 2 shows the mean (SD) of postpartum depression in the intervention and control groups. As evident in this table, the mean score of depression reduced significantly more in the intervention group compared to the control group after 4 weeks (the mean (SD) score of depression was 15.83 (2.77) in the intervention group that reduced to 3.48 (4.29) and 1.72 (3.30) after 4- and 8- weeks intervention respectively. The mean (SD) score of depression was 15.45 (2.97) at baseline in the control group that reduced to 7.22 (3.98) and 5.85 (3.67) after 4- and 8-weeks intervention respectively. These differences were significant in two groups over the time using the generalized estimating equations (GEE) (p<0.0001, Table 3). The Bonferroni-corrected pairwise comparison following generalized estimating equation (GEE) showed that difference between control and curcumax was significant in week 4 (mean=3.97, 95% CI: 2.09, 5.84, p<0.0001) and week 8 (mean=4.35, 95% CI: 2.77, 5.94, P<0.0001) (Table 4). None of the participants experienced any side effects.
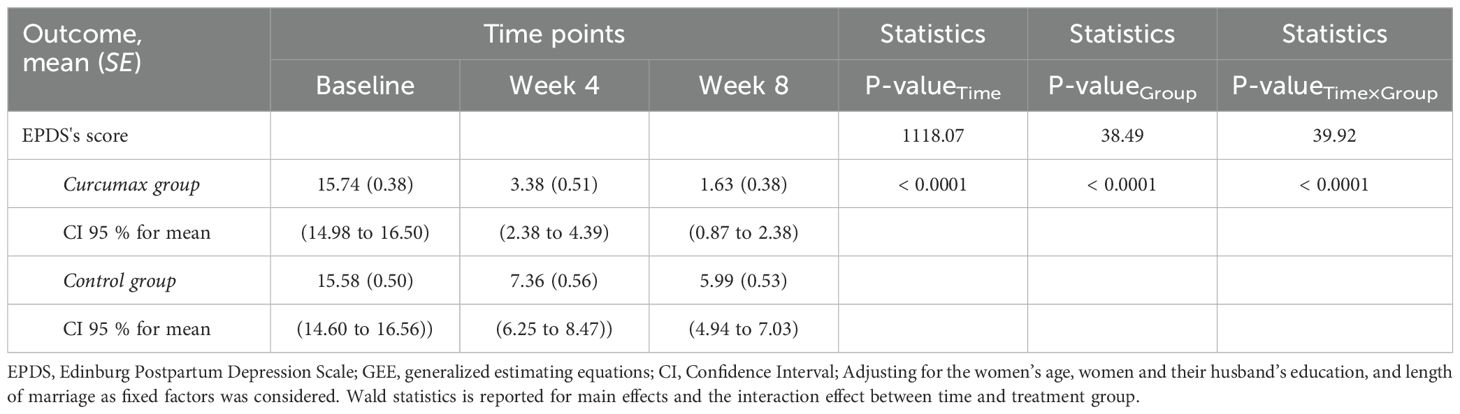
Table 3. Estimated outcomes over time between the two groups according to the generalized estimating equations (GEE) test.
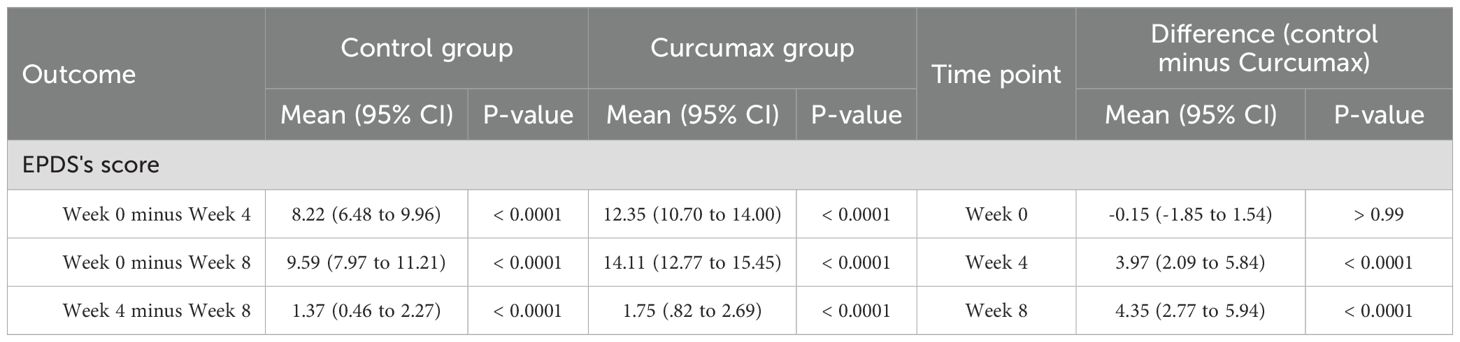
Table 4. Bonferroni-corrected pairwise comparisons following generalized estimating equations (GEE) analysis.
4 Discussion
This study was designed to evaluate the effect of curcumax on postpartum depression in reproductive-aged women. The results showed that the mean score of depression was decreased significantly in the intervention group in comparison to the control group after 4 and 8 weeks follow-up. We could not find any study evaluating the effect of curcumax on postpartum depression. Therefore, we mention studies that evaluated the effect of each ingredient of curcumax. One of the mechanisms of reducing postpartum depression by ginger and turmeric is through their anti-inflammatory effects, and there is some evidence that dietary inflammation index has a relationship with postpartum depression (24).
It is also well documented that ginger could suppress 5-lipooxygenase or prostaglandin, and this suppression can not only inhibit prostaglandin and leukotriene synthesis bur also reduce the level of pro-inflammatory cytokines such as IL-1, TNF-α and IL-8 (25). In a systematic review on 14 studies, Askari et al. found that ginger supplementation could reduce C-Reactive protein, IL-6, and Tumor Necrosis Factor (TNF- α), and increase blood total antioxidant capacity (TAC) significantly (26).
On the other hand, in their systematic review including 10 studies, Matias et al. found that curcumin (component of turmeric) could significantly increase monoamines and brain-derived neurotrophic factor and suppress the production of pro-inflammatory cytokines and neural apoptosis in brain, thus mitigating depression and anxiety (27). In a randomized controlled trial including 65 patients with major depression who were randomized into two groups of curcumin as an adjunctive therapy and placebo, Kanchanatawan et al. found that curcumin could improve the symptoms of major depression in weeks 12 and 16 compared to placebo (28). The anti-inflammatory and anti-arthritic effect of piperine (the active component of black pepper) on rats was evaluated by Bang et al. Their results showed that piperine could suppress the expression of IL6 and matrix metalloproteinase (MMPs), and therefore reduce the synthesis of prostaglandin E2, the symptoms of arthritis, and inflammatory areas in the ankle joint (29). Furthermore, Nagaraju et al. in a study on rats evaluated the anti-inflammatory effect of turmeric, alma (Emblica Officinalis Gaertn), and black pepper (TAB) on sepsis-induced acute lung injury. Their results showed that TAB could significantly decrease the inflammatory cytokines including tissue necrosis factor (TNF) and IL6 in the blood, and improve histopathological changes in the lungs (30). As the curcumin is a component of turmeric which represents about 2-8% of most preparations, the results of Nagaraju et al’s study can support the results of the present study.
A mentioned earlier, we could not find any articles directly dealing with the effect of curcumax on postpartum depression. However, all these mechanisms related to the three ingredients of curcumax capsules show that this substance has anti-inflammatory properties and can change the depression pathways.
4.1 Strengths and limitations of the study
This is the first study to evaluate the combined effect of ginger, turmeric, and black pepper in one capsule on reducing postpartum depression. Despite its merits, this study has some limitations. In this study, we did not measure the blood level of depression markers. Measuring such markers could show a more precise picture of drug effect. We conducted this study at the time of COVID-19 pandemic, which may have increased the level of anxiety, stress, and depression among the studied women. And finally, the curcumax capsules that used in this study contained turmeric (320 mg), ginger (150 mg), and black pepper (4mg), and we followed participants until eight weeks. Further research with different doses of curcumax and longer duration are recommended.
5 Conclusion
The results of this study showed that curcumax significantly reduced the mean score of postpartum depression among reproductive-aged women. Because it is the first time this herb is used as an anti-depressant, its effective dose was not available. Therefore, further studies with higher doses of this herb are recommended.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ahvaz Jundishapur University of Medical Sciences. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
FN: Data curation, Writing – review & editing, Software, Methodology, Formal analysis, Conceptualization. SA: Supervision, Resources, Project administration, Investigation, Funding acquisition, Writing – review & editing, Software, Methodology, Conceptualization. PA: Writing – original draft, Validation, Formal analysis, Writing – review & editing, Supervision, Software, Methodology, Conceptualization. SJ: Writing – review & editing, Validation, Supervision, Software, Methodology, Formal analysis, Conceptualization. NS: Writing – review & editing, Visualization, Validation, Supervision, Methodology, Conceptualization. GH: Writing – review & editing, Visualization, Validation, Software, Methodology, Conceptualization. EM: Writing – review & editing, Visualization, Validation, Supervision, Software, Methodology, Formal analysis, Conceptualization.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by Ahvaz Jundishapur University of Medical Sciences.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Andrews-Fike C. A review of postpartum depression. Prim Care Companion J Clin Psychiatry. (1999) 1:9–14. doi: 10.4088/pcc.v01n0103
2. Rich M. What is postpartum depression. UNICEF. Available online at: https://www.unicef.org/parenting/mental-health/what-postpartum-depression#postpartum-depression (Accessed 16 September 2023).
3. Mughal S, Azhar Y, Siddiqui W. Postpartum depression. Available online at: https://www.ncbi.nlm.nih.gov/books/NBK519070/ (Accessed 7 October 2022).
4. Escribà-Agüir V, Artazcoz L. Gender differences in postpartum depression: A longitudinal cohort study. J Epidemiol Community Health. (2011) 65:320–6. doi: 10.1136/jech.2008.085894
5. Wang Z, Liu J, Shuai H, Cai Z, Fu X, Liu Y, et al. Mapping global prevalence of depression among postpartum women. Transl Psychiatry. (2021) 11:543. doi: 10.1038/s41398-021-01663-6
6. Veisani Y, Delpisheh A, Sayehmiri K, Rezaeian S. Trends of postpartum depression in Iran: a systematic review and meta-analysis. Depress Res Treat. (2013) 2013:291029. doi: 10.1155/2013/291029
7. Afshari P, Tadayon M, Abedi P, Beheshtinasab M. Comparison of pre-and intra-COVID-19 postpartum depression among reproductive aged women: A comparative cross-sectional study in Ahvaz Iran. Front Psychiatry Sec. Perinatal Psychiatry. (2022) 13:1019432. doi: 10.3389/fpsyt.2022.1019432
8. Netsi E, Pearson RM, Murray L, Cooper P, Craske MG, Stein A. Association of persistent and severe postnatal depression with child outcomes. JAMA Psychiatry. (2018) 75:247–53. doi: 10.1001/jamapsychiatry.2017.4363
9. Abdollahi F, Zarghami M. Effect of postpartum depression on women’s mental and physical health four years after childbirth. EMHJ. (2018) 24:1–13. doi: 10.26719/2018.24.10.1002
10. Cox J, Holden J, Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. (1987) 150:782–6. doi: 10.1192/bjp.150.6.782
11. Hanusa BH, Scholle SH, Haskett RF, Spadaro K, Wisner KL. Screening for depression in the postpartum period: a comparison of three instruments. J Womens Health (Larchmt). (2008) 17:585–96. doi: 10.1089/jwh.2006.0248
12. Appleby L, Warner R, Whitton A, Faragher B. A controlled study of fluoxetine and cognitive-behavioural counseling in the treatment of postnatal depression. BMJ. (1997) 314:932–6. doi: 10.1136/bmj.314.7085.932
13. Cooper PJ, Murray L, Wilson A, Romanuk H. Controlled trial of the short- and long-term effect of psychological treatment of postpartum depression. Br J Psychiatry. (2003) 182:412–9. doi: 10.1192/bjp.182.5.412
14. Forray A, Ostroff RB. The use of electroconvulsive therapy in postpartum affective disorders. J ECT. (2007) 23:188–93. doi: 10.1097/yct.0b013e318074e4b1
15. Epperson CN, Terman M, Terman JS, et al. Randomized clinical trial of bright light therapy for antepartum depression: preliminary findings. J Clin Psychiatry. (2004) 65:3. doi: 10.4088/JCP.v65n0319
16. Babakhanian M, Rashidi Fakari F, Mortezaee M, Bagheri Khaboushan E, Rahimi R, Khalili Z, et al. The effect of herbal medicines on postpartum depression, and maternal-infant attachment in postpartum mother: A systematic review and meta-analysis. Int J Pediatr. (2019) 7:9645–56. doi: 10.22038/ijp.2019.38414.3298
17. Deligiannidis KM, Freeman MP. Complementary and alternative medicine therapies for perinatal depression. Best Pract Res Clin Obstet Gynaecol. (2014) 28:85–95. doi: 10.1016/j.bpobgyn.2013.08.007
18. Pourmaleky S, Najar S, Montazery S, Haghighizadeh MH. Comparison between the effect of zintoma (Ginger) and mefenamic acid on after pain during postpartum in multioarous women. Iran J Obstet Gynecol Infertil. (2013) 16:18–25.
19. Matrisciano F, Epinna G. PPAR and functional foods: rationale for natural neurosteroid-based interventions for postpartum depression. Neurobiol Stress. (2020) 12:100222. doi: 10.1016/j.ynstr.2020.100222
20. Balakrishnan R, Azam S, Kim IS, Choi DK. Neuroprotective effects of black pepper and its bioactive compounds in age-related neurological disorders. Aging Dis. (2023) 14:750–77. doi: 10.14336/AD.2022.1022
21. Mahdizadeh A, Tafazoli M, Mazloum SR, Manteghi A, Asili J, Noras MR. Effect of orange scent on preventing of postpartum depression: A randomized clinical trial. Iran. J Obstet. Gynecol. Infertil. (2018) 21:93–100. doi: 10.22038/ijogi.2018.12139
22. Schaper A, Rooney B, Kay N, Silva P. Use of the Edinburgh Postnatal Depression Scale to identify postpartum depression in a clinical setting. J Reprod Med. (1994) 39:620–4.
23. Ahmadi kani Golzar A, GoliZadeh Z. Validation of Edinburgh Postpartum Depression Scale (EPDS) for screening postpartum depression in Iran. J Nurs Edu. (2015) 3:1–10.
24. Zou H, Sun M, Liu Y, Xi Y, Xiang C, Yong C, et al. Relationship between dietary inflammatory index and postpartum depression in exclusively breastfeeding women. Nutrients. (2022) 14:5006. doi: 10.3390/nu14235006
25. Tjendraputra E, Tran VH, Liu-Brennan D, Roufogalis BD, Duke CC. Effect of ginger constituents and synthetic analogues on cyclooxygenase-2 enzyme in intact cells. Bioorganic Chem. (2001) 29:156–63. doi: 10.1006/bioo.2001.1208
26. Askari G, Aghajani M, Salehi M, Najafgholizadeh A, Keshavarzpour Z, Fadaei A, et al. The effects of ginger supplementation on biomarkers of inflammation and oxidative stress in adults: A systematic review and meta-analysis of randomized controlled trials. J Herb Med. (2020) 22:100364. doi: 10.1016/j.hermed.2020.100364
27. Matias JN, Achete Gm, Campanari GS, dos S, Araujo AC, Buglio DS, et al. A systematic review of the antidepressant effects of curcumin: Beyond monoamines theory. Aust N Z J Psychiatry. (2021) 55:451–62. doi: 10.1177/0004867421998795
28. Kanchanatawan B, Tangwongchai S, Sughondhabhiron A, Suppapitipom S, Hemrunrojn S, Carvalho AF, et al. Add-on treatment with curcumin has antidepressive effects in Thai patients with major depression: results of a randomized double-blind placebo-controlled study. Neurotox Res. (2018) 33:621–33. doi: 10.1007/s12640-017-9860-4
29. Bang JS, Oh DH, Choi HM, Sur BJ, Lim SJ, Kim JY, et al. Anti-inflammatory and antiarthritic effects of piperine in human interleukin 1beta-stimulated fibroblast-like synoviocytes and in rat arthritis models. Arthritis Res Ther. (2009) 11:R49. doi: 10.1186/ar2662
Keywords: curcumax, postpartum depression, Edinburgh scale, reproductive-aged women, ginger, turmeric, black pepper
Citation: Nikpour F, Ansari S, Abedi P, Jahanfar S, Sharifat N, Hooshmand G and Maraghi E (2024) The effect of curcumax on postpartum women’s depression: a randomized controlled trial. Front. Psychiatry 15:1302174. doi: 10.3389/fpsyt.2024.1302174
Received: 26 September 2023; Accepted: 31 July 2024;
Published: 10 September 2024.
Edited by:
Stefania Schiavone, University of Foggia, ItalyReviewed by:
Naseem Akhtar Qureshi, Al-Falah University, IndiaKurt Leroy Hoffman, Autonomous University of Tlaxcala, Mexico
Copyright © 2024 Nikpour, Ansari, Abedi, Jahanfar, Sharifat, Hooshmand and Maraghi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Somayeh Ansari, YW5zYXJpLnNvbWF5ZWg4OEBnbWFpbC5jb20=; Parvin Abedi, cGFydmluYWJlZGlAeW1haWwuY29t
 Fatemeh Nikpour1
Fatemeh Nikpour1 Parvin Abedi
Parvin Abedi Shayesteh Jahanfar
Shayesteh Jahanfar Gholamreza Hooshmand
Gholamreza Hooshmand Elham Maraghi
Elham Maraghi