- 1Department of Physical and Health Education, Graduate School of Education, The University of Tokyo, Tokyo, Japan
- 2Research Fellow of Japan Society for the Promotion of Science, Tokyo, Japan
- 3Institute for Psychopharmacology, Medical Faculty Mannheim, Central Institute of Mental Health, University of Heidelberg, Mannheim, Germany
- 4Department of Genetic Epidemiology in Psychiatry, Medical Faculty Mannheim, Central Institute of Mental Health, University of Heidelberg, Mannheim, Germany
- 5Department of Psychiatry, College of Health Sciences, University of Alberta, Edmonton, AB, Canada
- 6Unit for Mental Health Promotion, Research Center for Social Science & Medicine, Tokyo Metropolitan Institute of Medical Science, Tokyo, Japan
- 7Saitama Prefectural Education Bureau Student Consultation Division, Saitama, Japan
- 8Saitama Prefectural Education Bureau Health and Physical Education Division, Saitama, Japan
Introduction: Parents and guardians (hereafter caregivers) of teenagers need high levels of mental health literacy (MHL) to manage mental health problems arising in teenagers in their care. Previous studies assessing MHL levels in caregivers of teenagers have reported mixed results, making it difficult to clearly estimate caregiver MHL levels. This study aimed to investigate MHL levels in Japanese caregivers of regular teenagers.
Methods: Responses from caregivers (n = 1,397) of students entering junior and senior high schools to a self-administered online questionnaire were analyzed. The questionnaire assessed (a) knowledge about mental health/illnesses and (b) attitudes towards mental health problems in teens in their care (e.g., recognition of depression as a medical illness and intention to engage in helping behaviors).
Results: The average proportion of correct answers to the knowledge questions (n = 7) was 55.4%; about one tenth (9.2%) of caregivers correctly answered only one or none of the questions. Few caregivers correctly answered about the life-time prevalence of any mental illnesses (46.1%) and appropriate sleep duration for teenagers’ health (16.5%). The proportions of caregivers who had the intention to listen to the teen in their care, consult another person, and seek professional medical help if the teen suffered from depression were 99.5%, 91.5% and 72.7%, respectively.
Conclusions: Many teenagers’ caregivers appeared to be willing to help the teens in their care if they were suffering from mental health problems. However, there was much room for improvement in knowledge on mental health/illnesses and intention to seek help from medical professionals. Efforts toward better education should be made.
1 Introduction
The prevalence of mental illnesses sharply increases as children reach their teenage years (1). However, teenagers may have difficulty in recognizing their own mental health (MH) problems (2), and even when they can, they may be reluctant to seek help (3). Therefore, teenagers may need the help of parents or other supportive adults so that they can recognize their own problems and seek appropriate help (2).
Given that parents and/or guardians (hereafter caregivers) are the most familiar adults for most teenagers, caregivers need to be aware of MH problems in the teens in their care and appropriately manage these problems; this requires adequate mental health literacy (MHL). MHL is defined as knowledge and beliefs which aid in the recognition, management or prevention of MH problems (4). More specifically, knowledge about mental health/illnesses, recognition of mental disorders, and attitudes towards appropriate help-seeking are examples of components of MHL (2, 4).
Even caregivers of teens without MH problems need MHL because they need to be able to recognize and manage problems which can occur in future. Levels of MHL in caregivers of regular teens have been studied in a number of previous studies (5–17). The most studied aspect of MHL was knowledge about mental health/illness, with high variation in knowledge levels observed between studies (5, 6, 12, 14, 15). Other components of MHL were also examined including intention to help their teens (10, 11, 13), and belief that a teen with MH problems is weak, not ill (12). In addition, most of the previous studies did not clearly report response rates, leaving room for bias (5–7, 12–17). These mixed results make the estimation of MHL in caregivers of teenagers challenging.
The present school-based study aimed to examine MHL levels in caregivers of regular teenagers. The survey was conducted at school entrance ceremonies, which almost all caregivers, not only those who were interested in MH, attended; this was done to reduce selection bias as much as possible. Analyses were conducted in the whole sample, as well as stratified by age and gender given significant age and gender-related differences in MHL previously observed in the general adult population (18–20).
2 Methods
2.1 Participants and procedure
A call was put out through the Prefectural board of education in Saitama, Japan, for public junior and senior high schools to participate in various studies on MH education for students and caregivers. The goal was to recruit 8 junior and 8 senior high schools. Twenty-seven junior and 5 senior high schools applied; 8 junior high schools were randomly selected from the 27, and all the 5 senior high schools were included. Of these, 3 junior and 4 senior high schools participated in the MH program involving the present research in 2022. The 7 participating schools are located in suburban metropolitan areas. In Japan, the majority of junior/senior high school students attend public schools. Unlike public junior high schools, public senior high schools have entrance examinations and the achievement levels of the 4 participating high schools on these exams were within ± 1 SD of the national average. The survey was conducted at the school entrance ceremony, which most caregivers of the new students attended. The second half of the ceremony included a MH seminar. Before the MH seminar started, caregivers who attended the ceremony were given a QR code and asked to answer a self-administered online questionnaire about MHL on their own mobile devices. Of 1,741 new students, 1,820 caregivers attended the entrance ceremony (multiple people, e.g. both parents, participated in some families), and of those, 1,655 answered the questionnaire. Of those, 1,562 agreed to have their responses analyzed and participate in this study, completing the online submission of informed consent (response rate = 85.8%). A further n=131 who were found to have submitted their responses after start of the MH seminar were excluded from the analysis. Respondents whose age was under 30 (n = 23) or whose mother tongue was not Japanese (n = 11) were also excluded. In the end, responses from 1,397 caregivers were analyzed. The study was approved by The University of Tokyo Human Research Ethics Committee (#21-348).
2.2 Assessments
2.2.1 Demographic variables
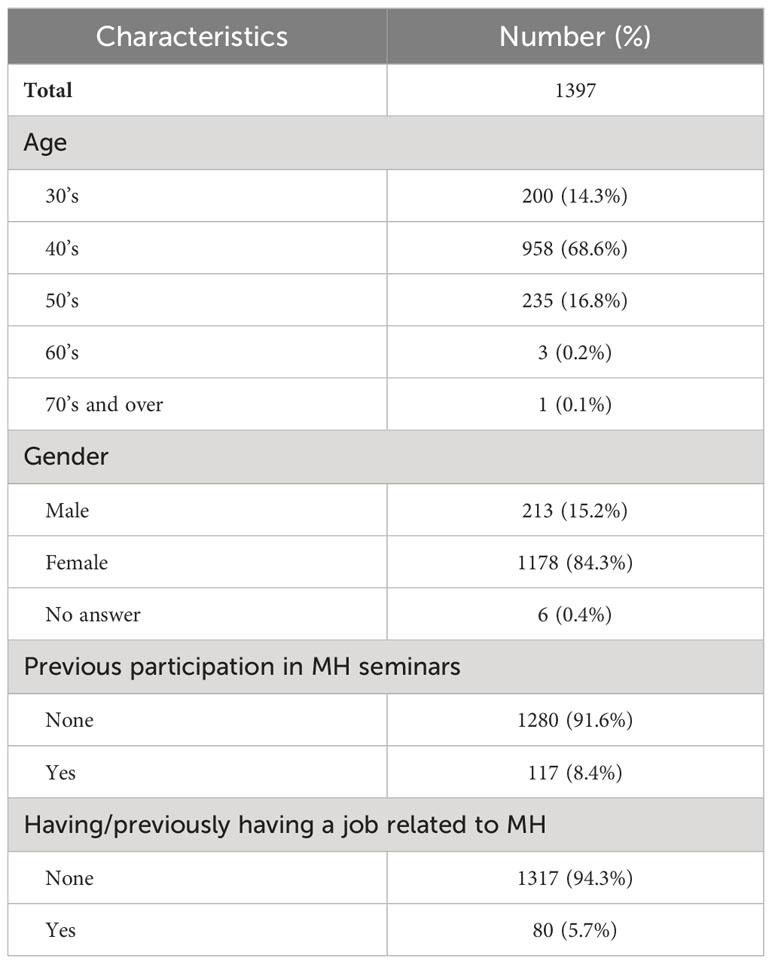
In the first part of the questionnaire, the demographics of caregivers including age, gender, having/previously having a job related to MH, and previous participation in MH seminars were assessed (Table 1).
2.2.2 Knowledge about mental health/illnesses (knowledge)
In the second part, basic knowledge about mental health/illnesses was assessed using seven questions (see Table 2). The questions were developed by the authors (a team including psychiatrists, school teachers, and school nurses). Topics were chosen to determine the extent to which caregivers understood the importance of attention to, care of and prevention of mental illness and suicide risk in teenagers. Questions related to the increase in the prevalence of mental illness (21) and suicide (22) among teenagers (suicide is the leading cause of death among older teens in Japan (23)) and the impact of mental illness on teens’ lives including their academic achievement, were included. Questions about the amount of sleep needed to maintain MH were included, since shorter sleep durations have been associated with increased risk of mental illness and suicidality (24–27), and many teenagers worldwide are found to sleep shorter (28) than the recommended sleep duration for their age (29). Three of the seven questions were modified from items used in a previous study by the authors (30). The questions were to be answered, “True”, “False”, or “I don’t know”. The internal consistency (Cronbach’s alpha) of the 7 questions was 0.56 in the present sample.
2.2.3 Attitudes towards mental health problems
In the third part, caregivers were asked to read a case vignette describing a teen with symptoms of major depression (see below), and to imagine that the teen in their care is in the same situation as Teen A. The vignette was written by the authors, with reference to the one in Jorm et al. (2007) (10) and the criterion A of DSM-5 criteria of major depressive disorder (31).
Vignette
Teen A has often been late for school over the last 2 weeks. They feel tired and can’t keep their mind on classes. Teen A says that they have trouble sleeping, don’t feel like eating, and don’t have fun watching their favorite TV program. Studying also seems to be difficult for them.
Then, caregivers were asked to choose responses to the following questions which matched their thoughts most closely (2.2.3.1, 2.2.3.2, 2.2.3.3).
2.2.3.1 Recognition of depression as medical illness
Caregivers were asked to what extent they agreed with the following (3 out of the 4) “weak-not-sick” items of the Depression Stigma Scale (32): 1) “The teen could snap out of it if they wanted”; 2) “The teen’s problem is a sign of personal weakness”; 3) “The teen’s problem is not a real medical illness”. The fourth item, “It is best to avoid people with a problem like this child so that you do not develop this problem” was not asked because the item was not relevant to the recognition of depression in teens under the caregivers’ care. Possible responses to each item were as follows: “Agree”, “Somewhat Agree”, “Somewhat Disagree”, or “Disagree”. “Somewhat Disagree” and “Disagree” were considered the desired responses.
2.2.3.2 Intention to engage in helping behaviors if the teen suffers from depression
Caregivers were asked “What would you do in this situation?” to assess the intention to help if the teen in their care were in the same mental state as Teen A. Specifically, they were asked to answer whether they would: 1) listen to what the teen has to say; 2) consult someone about the teen; and 3) seek medical help. Possible responses to each item were “Yes”, “Probably yes”, “Probably no”, or “No”. Caregivers were considered to have the intention to engage in the behavior, when the answer was “Yes” or “Probably yes” (“Yes” and “Probably yes” were considered the desired responses).
2.2.3.3 Acceptance of the teen’s diagnosis
Caregivers were asked “If the teen in your care were diagnosed with a mental illness, how would you feel about the diagnosis?” Possible responses to the question were “I would be able to accept the diagnosis”, “I would probably be able to accept the diagnosis”, “I would probably not be able to accept the diagnosis”, or “I would not be able to accept the diagnosis”. Caregivers were considered to be able to accept the diagnosis, when the response was “I would be able to accept the diagnosis” or “I would probably be able to accept the diagnosis”.
2.3 Statistical analysis
Proportions of correct responses to the knowledge questions and desirable responses to other questions were summarized in all subjects, as well as by age and gender. To examine differences by age/gender, linear or binary logistic regression were performed employing the number of correct responses or whether caregivers had desirable responses as dependent variables, adjusting for experience of having a job related to MH, and previous participation in MH seminar.
3 Results
3.1 Demographic variables
Table 1 shows demographic characteristics of the participants (n = 1,397). Most (84.3%, n = 1,178) of the participants were female, and two-thirds (68.6%, n = 958) were in their 40’s. The proportion of caregivers who had participated in other MH seminars was 8.4% (n =117), and who had had a job related to MH was 5.7% (n = 80).
3.2 Knowledge about mental health/illnesses
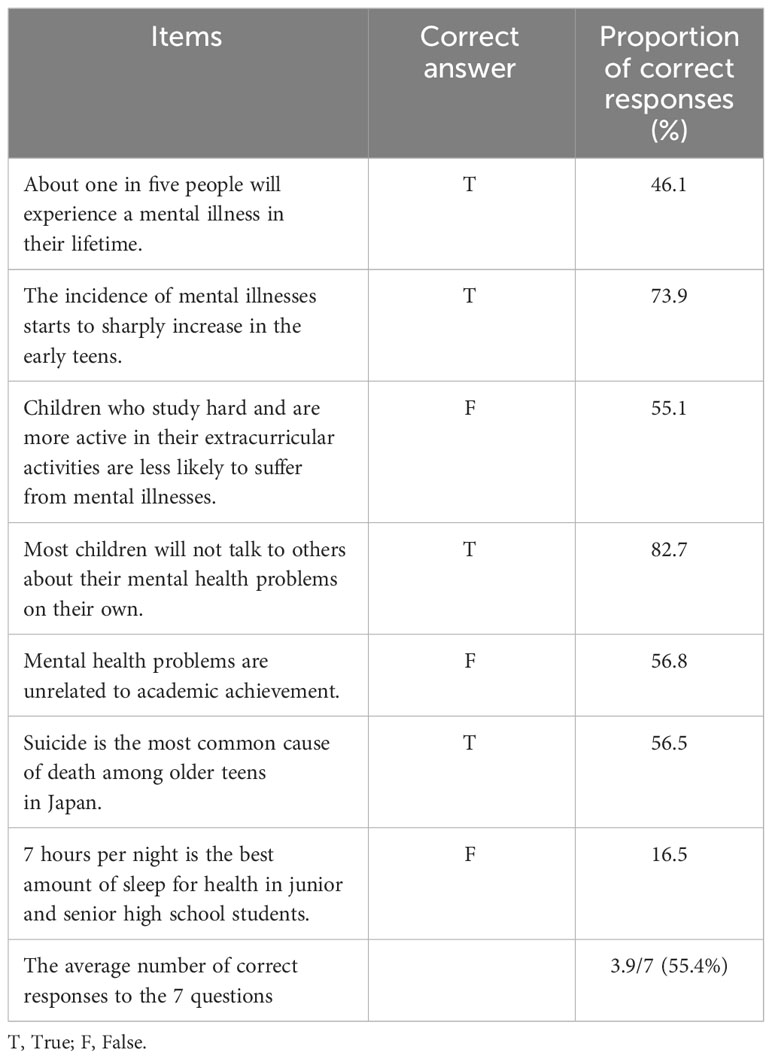
Figure 1 shows the distribution of the number of correct responses to the knowledge questions in the caregivers. The average number of the correct responses was 3.9 (out of 7 questions; standard deviation = 1.7). About one tenth (9.2%) of caregivers correctly answered only one or none of the questions; 38.2% correctly answered to less than half (3 or less) of the questions. Table 2 summarizes the proportion of correct responses to each question. The proportion was low (around or below half) in the following questions: appropriate sleep duration for adolescents at the age of junior and senior high school (16.5%), life-time prevalence of any mental illnesses (46.1%), MH in students who study hard (55.1%), relationship of MH and academic achievement (56.8%), and suicide being the leading cause of death in late teens (56.5%).
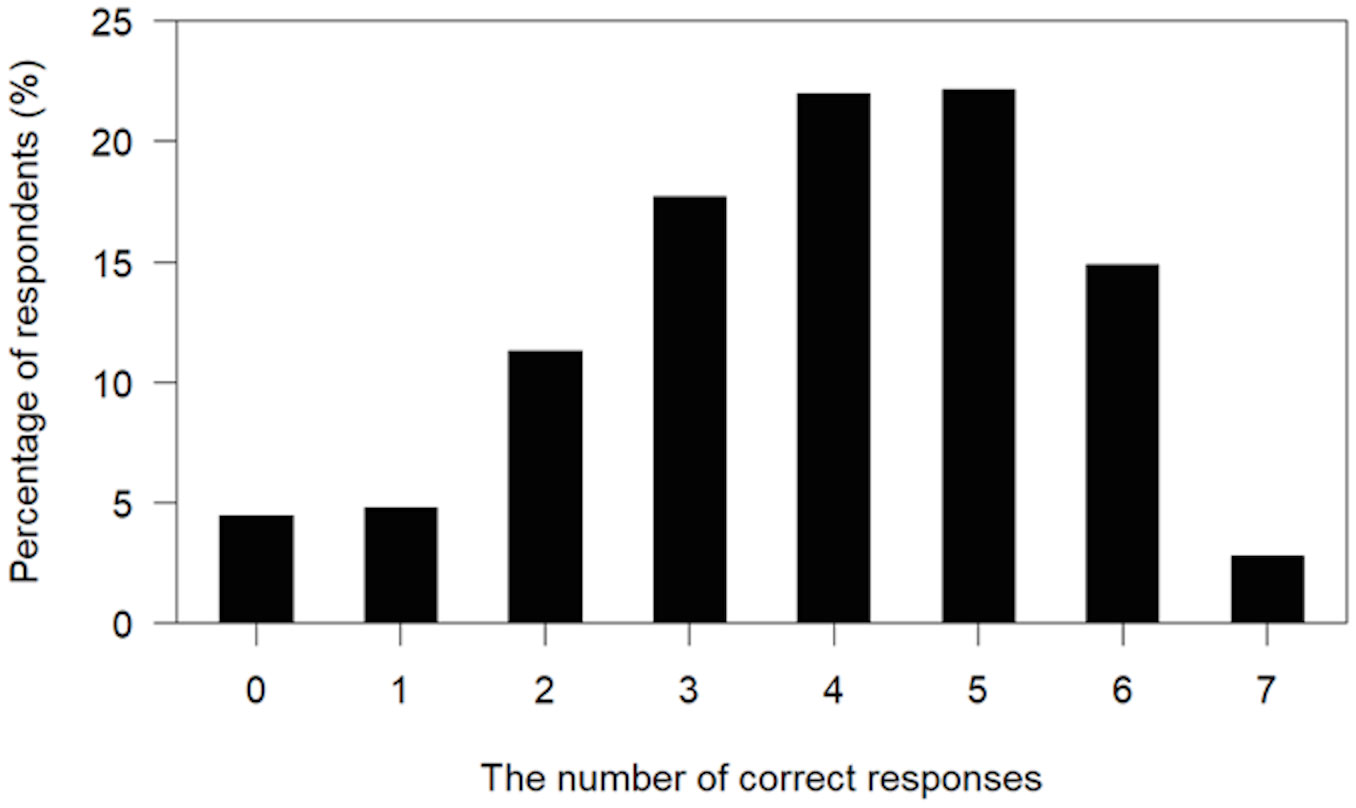
Figure 1 Distribution of the number of correct responses in caregivers to the 7 knowledge questions about mental health/illnesses.
3.3 Attitudes towards mental health problems
Table 3 summarizes responses to questions about recognition of depression as a medical illness and about intention to help teens, when teens in their care were assumed to be in the same situation as Teen A in the vignette. The majority of caregivers disagreed/somewhat disagreed that the problem was not a real medical illness, that the problem was a sign of personal weakness, and that the teen could snap out of it if they wanted. Regarding the intention to help, most caregivers answered that they would/would probably listen to what the teen has to say, consult someone about the teen, and seek medical help. Most caregivers (95.4%) answered that they would/would probably accept having teens in their care diagnosed with a mental illness (not shown in tables).

Table 3 Responses to questions about recognition of depression as a medical illness, intention to help, and acceptance of the teen’s diagnosis.
3.4 MHL in caregivers by gender and age
Proportions of correct/desired responses by gender and age are summarized in Supplementary Table 1. No difference by age was observed in any questions/items. By gender, the proportions appear to be higher in females than males in the items including “The teen’s problem is a sign of personal weakness”, “I will consult someone about the teen”, and “I will seek medical help”; the differences were statistically significant (odds ratio = 2.5, 4.0 and 2.2, respectively, all p < 0.001, reference = males) adjusting for age, current/previous experiences of job related to MH, and previous participation in MH seminar.
4 Discussion
The present study examined the level of MHL among caregivers of regular teenagers. Most caregivers had the desired attitudes towards potential MH problems in teens in their care, except for when it came to seeking professional help. In contrast, knowledge about MH was not sufficient in most caregivers.
Caregivers appear prepared to take basic steps to help if teens in their care have MH problems and the intention to engage in helping behaviors was high; most caregivers answered that they would listen to the teens and try to consult someone about the problems. However, 30% of caregivers did not consider seeking professional help for potential symptoms of depression. This appears in line with previous research, which found that 30% of caregivers would not seek help from doctors (e.g., general practitioners) when teens in their care suffered from depressive symptoms (11). One possible reason contributing to this could be the young people’s unwillingness to visit doctors (11). Based on the present study, emotional unacceptance of the diagnosis may not be a major barrier; most of the present caregivers answered that they could accept having teens in their care diagnosed with a mental illness. It does not appear that not recognizing of depression and its symptoms as a medical illness was a major barrier to seeking treatment; most of the present caregivers recognized the teen in the vignette to be suffering from a medical illness. The reason why caregivers do not seek professional help for the teens in their care needs to be further studied.
Caregivers’ knowledge on mental health/illnesses was insufficient. A substantial portion (10%) of the caregivers correctly answered only one or zero questions; one third correctly answered less than half of the questions. Specifically, half of the caregivers did not know that suicide is the leading cause of death among older Japanese teenagers, that lifetime prevalence of mental illnesses reaches 20% in Japan, and that MH problems are related to academic achievement. Most of the caregivers did not know that the appropriate amount of sleep for teenagers’ health is 8-10 hours (29). In previous studies, while the percentage of correct answers was high (> 75%) in studies asking questions about risk factors, symptoms/influences and treatment of MH problems (6, 15), percentages were lower in a study asking questions such as how to support teenagers with the problems (55%) (12). Another study reported that only half of caregivers knew that medication can be an effective treatment for MH problems and that a full recovery was possible (14). Improving caregivers’ knowledge about appropriate support for teens and lifestyles such as sleep amount is needed. While knowledge can play a role in predicting health behaviors, alone it cannot predict or change behavior; on the other hand it is suggested that beliefs (attitude or intention) related to health may be key predictors (33). For caregivers to take action to encourage a teen to access MH services can involve steps such as recognizing the problem as psychological in nature, considering possible courses of action, and developing the intention to seek out MH services for the teen (34). Knowledge can inform each of these steps, and how it does in real world situations requires further study.
We did not observe effects of age or gender on knowledge. However, there are many other potential confounding factors on the pathway from improved MHL to improved care and outcomes for youth. The diversity of mental health presentations in teenagers, which can make mental illnesses challenging to recognize (30), stigma (including caregiver stigma in accessing MH services), as well as systemic-structural aspects of MH services influencing availability and accessibility (35), can affect access to MH care. Also, given that schools and outpatient settings are the most common locations for youth to receive MH care (36), future research should examine caregivers’ attitudes towards and behaviors of accessing school-based services. Improved in-school access to resources for well-being and welfare may help to intervene before medical services become needed.
Knowledge about mental health/illnesses did not differ by gender in caregivers, but desired attitudes toward MH problems in teens in their care were significantly more frequent in females than males. This appears in line with previous studies in regular adults; females had more desirable attitudes toward MH problems than males (18, 19). Thus far, one previous study had examined caregivers’ MHL by gender, with no significant differences observed (17). A limitation of the present results was that the proportion of males in the participants was low (15.2%), which makes it difficult to draw strong conclusions.
A strength of this study was the high response rate (85.8%). Also, caregivers were asked to answer the questionnaire during the entrance ceremony, which almost all caregivers attended. Thus, the responses are obtained from a sample of caregivers including not only respondents who were interested or knowledgeable about MH, but also those who were not, limiting bias in characteristics of participants. The present study has several limitations. First, participants were caregivers from a single prefecture in Japan. Caution may be needed when generalizing results to other populations. Studies in other regions of Japan (as well as in other countries) will be needed to obtain a more comprehensive picture of caregiver MHL. Second, we did not assess the relationship between the caregivers and teens in their care; while in Japan the majority of caregivers who attend school entrance ceremonies are parents, in future research it would be of interest to study whether MHL differs in parents and other adult caregivers. Third, to fit within time constraints, this study used a single case vignette of a teen with major depression to assess caregivers’ attitude towards mental illnesses in teens in their care. The use of a greater number of scenarios and assessment of attitudes towards other mental illnesses are needed in future studies to give a more comprehensive picture of the situation. Finally, as mentioned above, more desired attitudes toward MH problems in teens were indicated by female than male caregivers, but the proportion of males was relatively small. Future studies with more male respondents will be needed to better understand their attitudes towards mental health.
5 Conclusions
The present study observed that teenagers’ caregivers had good intentions to help the teens in their care if they suffered from MH problems. At the same time, it was found that caregivers have room for improvement in MHL, as they had limited knowledge about mental health/illnesses, and many did not have the intention to seek help from professionals if the teens in their care experienced potential MH symptoms. Educational programs about risk for mental illnesses and their care and prevention are needed to improve caregiver MHL.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by The University of Tokyo Human Research Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin because all participants provided electronic informed consent.
Author contributions
SK: Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Writing – original draft, Writing – review & editing. JF: Writing – review & editing. SY: Methodology, Writing – review & editing. AY: Data curation, Writing – review & editing. TA: Investigation, Writing – review & editing, Methodology. FS: Investigation, Writing – review & editing, Methodology. FT: Supervision, Writing – review & editing. TS: Conceptualization, Funding acquisition, Methodology, Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by grants from the Japan Society for the Promotion of Science (JSPS KAKENHI Grant Numbers 21H00857, JP21J21319, JP22KJ0620).
Acknowledgments
We are grateful to Ms. Kozue Nakagawa and Ms. Michiko Nakahara for their support for collecting data.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1295918/full#supplementary-material
Supplementary Table 1 | Average proportion (%) by gender and age of responses to questions about MH knowledge, attitudes towards MH problems and acceptance of the teen’s diagnosis.
References
1. Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry (2005) 62(6):593–602. doi: 10.1001/archpsyc.62.6.593
2. Jorm AF. Mental health literacy: empowering the community to take action for better mental health. Am Psychol (2012) 67(3):231–43. doi: 10.1037/a0025957
3. Rickwood DJ, Deane FP, Wilson CJ. When and how do young people seek professional help for mental health problems? Med J Aust (2007) 187(S7):S35–9. doi: 10.5694/j.1326-5377.2007.tb01334.x
4. Jorm AF, Korten AE, Jacomb PA, Christensen H, Rodgers B, Pollitt P. "Mental health literacy": a survey of the public's ability to recognise mental disorders and their beliefs about the effectiveness of treatment. Med J Aust (1997) 166(4):182–6. doi: 10.5694/j.1326-5377.1997.tb140071.x
5. Choi H, Kim S, Ko H, Kim Y, Park CG. Development and preliminary evaluation of culturally specific web-based intervention for parents of adolescents. J Psychiatr Ment Health Nurs (2016) 23(8):489–501. doi: 10.1111/jpm.12327
6. Chu JTW, Wadham A, Jiang Y, Whittaker R, Stasiak K, Shepherd M, et al. Effect of MyTeen SMS-based mobile intervention for parents of adolescents: a randomized clinical trial. JAMA Netw Open (2019) 2(9):e1911120. doi: 10.1001/jamanetworkopen.2019.11120
7. Gronholm PC, Ford T, Roberts RE, Thornicroft G, Laurens KR, Evans-Lacko S. Mental health service use by young people: the role of caregiver characteristics. PloS One (2015) 10(3):e0120004. doi: 10.1371/journal.pone.0120004
8. Jorm AF, Morgan AJ, Wright A. First aid strategies that are helpful to young people developing a mental disorder: beliefs of health professionals compared to young people and parents. BMC Psychiatry (2008) 8:42. doi: 10.1186/1471-244X-8-42
9. Jorm AF, Wright A. Beliefs of young people and their parents about the effectiveness of interventions for mental disorders. Aust N Z J Psychiatry (2007) 41(8):656–66. doi: 10.1080/00048670701449179
10. Jorm AF, Wright A, Morgan AJ. Beliefs about appropriate first aid for young people with mental disorders: findings from an Australian national survey of youth and parents. Early Interv Psychiatry (2007) 1(1):61–70. doi: 10.1111/j.1751-7893.2007.00012.x
11. Jorm AF, Wright A, Morgan AJ. Where to seek help for a mental disorder? National survey of the beliefs of Australian youth and their parents. Med J Aust (2007) 187(10):556–60. doi: 10.5694/j.1326-5377.2007.tb01415.x
12. Morgan AJ, Fischer JA, Hart LM, Kelly CM, Kitchener BA, Reavley NJ, et al. Does Mental Health First Aid training improve the mental health of aid recipients? The training for parents of teenagers randomised controlled trial. BMC Psychiatry (2019) 19(1):99. doi: 10.1186/s12888-019-2085-8
13. Nakanishi M, Tanaka T, Nishida A, Mandai N, Kitamura N, Yoshii H. An online intervention to promote mental health literacy for psychosis amongst parents of adolescents: A pilot randomized controlled trial. Early Interv Psychiatry (2023) 17(7):737–42. doi: 10.1111/eip.13390
14. Phoa PKA, Ab Razak A, Kuay HS, Ghazali AK, Ab Rahman A, Husain M, et al. Predictors of mental health literacy among parents, guardians, and teachers of adolescents in West Malaysia. Int J Environ Res Public Health (2023) 20(1):825. doi: 10.3390/ijerph20010825
15. Yoshii H, Watanabe Y, Kitamura H, Chen J, Akazawa K. Effect of an education program on improving knowledge of schizophrenia among parents of junior and senior high school students in Japan. BMC Public Health (2011) 11:323. doi: 10.1186/1471-2458-11-323
16. Yoshii H, Watanabe Y, Kitamura H, Nan Z, Akazawa K. Stigma toward schizophrenia among parents of junior and senior high school students in Japan. BMC Res Notes (2011) 4:558. doi: 10.1186/1756-0500-4-558
17. Yoshii H, Watanabe Y, Mazumder AH, Kitamura H, Akazawa K. Stigma toward schizophrenia among parents of high school students. Glob J Health Sci (2013) 5(6):46–53. doi: 10.5539/gjhs.v5n6p46
18. Kaneko Y, Motohashi Y. Male gender and low education with poor mental health literacy: a population-based study. J Epidemiol (2007) 17(4):114–9. doi: 10.2188/jea.17.114
19. Svensson B, Hansson L. How mental health literacy and experience of mental illness relate to stigmatizing attitudes and social distance towards people with depression or psychosis: A cross-sectional study. Nord J Psychiatry (2016) 70(4):309–13. doi: 10.3109/08039488.2015.1109140
20. Wang J, Adair C, Fick G, Lai D, Evans B, Perry BW, et al. Depression literacy in Alberta: findings from a general population sample. Can J Psychiatry (2007) 52(7):442–9. doi: 10.1177/070674370705200706
21. Solmi M, Radua J, Olivola M, Croce E, Soardo L, Salazar de Pablo G, et al. Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Mol Psychiatry (2022) 27(1):281–95. doi: 10.1038/s41380-021-01161-7
22. World Health Organization. Suicide worldwide in 2019: Grobal Health Estimates (2021). Available at: https://www.who.int/publications/i/item/9789240026643 (Accessed December 17, 2023).
23. Ministry of Health Labour and Welfare. Vital Statistics / Vital statistics of Japan Final data General mortality (2022). Available at: https://www.e-stat.go.jp/en/stat-search/files?stat_infid=000032235948 (Accessed December 21, 2023).
24. Ojio Y, Nishida A, Shimodera S, Togo F, Sasaki T. Sleep duration associated with the lowest risk of depression/anxiety in adolescents. Sleep (2016) 39(8):1555–62. doi: 10.5665/.6020
25. Morishima R, Yamasaki S, Ando S, Shimodera S, Ojio Y, Okazaki Y, et al. Long and short sleep duration and psychotic symptoms in adolescents: Findings from a cross-sectional survey of 15 786 Japanese students. Psychiatry Res (2020) 293:113440. doi: 10.1016/j.psychres.2020.113440
26. Sarchiapone M, Mandelli L, Carli V, Iosue M, Wasserman C, Hadlaczky G, et al. Hours of sleep in adolescents and its association with anxiety, emotional concerns, and suicidal ideation. Sleep Med (2014) 15(2):248–54. doi: 10.1016/j.sleep.2013.11.780
27. Zhang J, Paksarian D, Lamers F, Hickie IB, He J, Merikangas KR. Sleep patterns and mental health correlates in US adolescents. J Pediatr (2017) 182:137–43. doi: 10.1016/j.jpeds.2016.11.007
28. Matricciani L, Blunden S, Rigney G, Williams MT, Olds TS. Children's sleep needs: is there sufficient evidence to recommend optimal sleep for children? Sleep (2013) 36(4):527–34. doi: 10.5665/sleep.2538
29. Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, et al. National Sleep Foundation's sleep time duration recommendations: methodology and results summary. Sleep Health (2015) 1(1):40–3. doi: 10.1016/j.sleh.2014.12.010
30. Yamaguchi S, Foo JC, Kitagawa Y, Togo F, Sasaki T. A survey of mental health literacy in Japanese high school teachers. BMC Psychiatry (2021) 21(1):478. doi: 10.1186/s12888-021-03481-y
31. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Fifth Edition. Arlington, VA: American Psychiatric Association (2013).
32. Yap MB, Mackinnon A, Reavley N, Jorm AF. The measurement properties of stigmatizing attitudes towards mental disorders: results from two community surveys. Int J Methods Psychiatr Res (2014) 23(1):49–61. doi: 10.1002/mpr.1433
33. Ogden J. 3. Health beliefs. In: Health psychology: a textbook, 5th ed. Berkshire: Open University Press (2012). p. 37–64.
34. Logan DE, King CA. Parental facilitation of adolescent mental health service utilization: A conceptual and empirical review. Clin Psychol Sci Pract (2001) 8(3):319–33. doi: 10.1093/clipsy.8.3.319
35. Reardon T, Harvey K, Baranowska M, O'Brien D, Smith L, Creswell C. What do parents perceive are the barriers and facilitators to accessing psychological treatment for mental health problems in children and adolescents? A systematic review of qualitative and quantitative studies. Eur Child Adolesc Psychiatry (2017) 26(6):623–47. doi: 10.1007/s00787-016-0930-6
Keywords: mental health literacy, parents, caregivers, teenagers, health education
Citation: Kusaka S, Foo JC, Yamaguchi S, Yukawa A, Arai T, Sawamura F, Togo F and Sasaki T (2024) A survey of mental health literacy in parents and guardians of teenagers. Front. Psychiatry 15:1295918. doi: 10.3389/fpsyt.2024.1295918
Received: 17 September 2023; Accepted: 25 January 2024;
Published: 09 February 2024.
Edited by:
Lawrence T. Lam, Macau University of Science and Technology, Macao SAR, ChinaReviewed by:
Liza Hopkins, The Alfred Hospital, AustraliaIvan Gualco, Independent researcher, Genoa, Italy
David C. N. Wong, University Grants Committee Secretariat, Hong Kong SAR, China
Copyright © 2024 Kusaka, Foo, Yamaguchi, Yukawa, Arai, Sawamura, Togo and Sasaki. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tsukasa Sasaki, cHN5dG9reW9AeWFob28uY28uanA=
 Sakurako Kusaka
Sakurako Kusaka Jerome Clifford Foo
Jerome Clifford Foo Satoshi Yamaguchi
Satoshi Yamaguchi Ayuko Yukawa
Ayuko Yukawa Takuya Arai7
Takuya Arai7 Fumiharu Togo
Fumiharu Togo