- Key Laboratory of Human Genetics and Environmental Medicine, School of Public Health, Xuzhou Medical University, Xuzhou, China
Objective: This study aims to establish the precise prevalence of sleep disorders among university students in Jiangsu Province. Utilizing a representative sample of students, we measured their sleep quality based on the Pittsburgh Sleep Quality Index (PSQI). Our objective is to quantitatively assess the magnitude of sleep quality and identify key factors. By detailed analysis of these relationships, our study seeks to provide actionable insights for the development of targeted interventions to enhance sleep quality within this population.
Methods: From October to November 2022, we conducted a cross-sectional web-based survey in Jiangsu Province, China. Using convenient cluster sampling in each college, a total of 8457 participants were selected. The PSQI was applied to assess sleep quality among university students. Data collected included sociodemographic details, scores from the Mobile Phone Dependence Index (MPAI) and psychological resilience measured by the Connor-Davidson Resilience Scale (CD-RISC).
Results: The overall prevalence of poor sleep quality among the participants was 39.30%. Binary logistic regression analysis revealed that higher physical activity (OR = 0.921; 95% CI: 0.779-1.090), earlier roommate bedtimes (OR = 0.799; 95% CI: 0.718-0.888), quieter dormitories (OR = 0.732; 95% CI: 0.647-0.828) and higher psychological resilience (OR = 0.982; 95% CI, 0.979-0.984) were protective factors linked to lower risk of poor sleep quality. Conversely, being a female student (OR = 1.238; 95% CI: 1.109-1.382), being a senior (OR = 1.582; 95% CI: 1.344-1.863), single-child status (OR = 1.195; 95% CI: 1.077-1.326), regular smoking (OR = 1.833; 95% CI: 1.181-2.847), regular alcohol consumption (OR = 1.737; 95% CI: 1.065-2.833), high academic stress (OR = 1.326; 95% CI: 1.012-1.736), high employment stress (OR = 1.352; 95% CI: 1.156-1.582), dissatisfaction with dormitory hygiene (OR = 1.140; 95% CI: 1.028-1.265), poor self-rated physical health (OR = 1.969; 95% CI: 1.533-2.529), poor self-rated mental health (OR = 2.924; 95% CI: 2.309-3.702) and higher mobile phone dependency were risk factors associated with an increased likelihood of poor sleep quality.
Conclusion: The sleep quality among university students should attract immediate attention. The development of public services and mental health education initiatives is crucial in enhancing the sleep health of this population.
1 Introduction
Early studies highlighted the importance of sleep duration for health (1–3), whereas recent research has pivoted attention towards sleep quality. University students normally face poor sleep quality (4) due to social influences, health conditions and academic workload. Sleep deprivation in university students can greatly impinge on students’ cognitive function and scholastic achievements (5, 6), and is also linked to serious health problems like obesity (7) and mental issues including depression, anxiety (8, 9), stress, and burnout (10, 11). Researchers have applied the Pittsburgh Sleep Quality Index across various cultural backdrops to delineate between good and poor sleepers among students (12–14). A spectrum of determinants, from sociodemographic to lifestyle and mental health factors, have been scrutinized for their impact on sleep. Gender appears to play an ambiguous role, with some studies noting that female students tend to have lower quality sleep (15, 16), while others found that there was no significant difference between gender (17, 18). However, influence of Body Mass Index (BMI) were more consistent with higher BMI associated with increased sleep issues (2, 19). Academic advancement has also been identified as a predictor of sleep disturbances, as students in higher grades have lower sleep quality (18, 20). Poor accommodations have also been found to affect sleep comfort and quality (21, 22). A study revealed that family income or wealth can serve as supportive resources for promoting healthy sleep among university students (23), and evidence from cross-sectional studies suggests that students from lower socioeconomic backgrounds are more likely to report sleep disturbances and poor sleep quality (24). Additionally, a study found that poor socioeconomic status increases the risk of developing sleep disorders (25). Risky behaviors such as lack of physical activity (26), smoking (27) and regular alcohol consumption (17) are common among university students and contribute to poor sleep quality in this population. Academic stress has also been identified as a significant factor associated with poor sleep quality among university students. Academic stress exacerbates sleep challenges, often causing students to sleep late (28). Taken together, entering university can be considered a challenging stage in the lives of adolescents, and high levels of perceived stress have been identified as a central predictor of poor sleep quality among university students (29).
Smartphone addiction refers to online behavioral dependence where excessive use of the internet, video games and mobile devices leads to unconscious exposure to the detrimental effects of technology (30). Numerous reports have shown that excessive smartphone use can result in sleep disorders (31, 32). Encouraging physical activity has been suggested as a counteractive measure to this problem (33). Therefore, it is anticipated that the addictive nature of mobile phones may serve as a positive predictor of sleep disorders.
Psychological resilience has emerged as a potential shield against sleep impairment. Studies revealed an inverse relation between resilience levels and the occurrence of sleep disorders (34, 35). Therefore, psychological resilience can serve as a crucial protective factor against sleep disorders.
In summary, lots of studies has been dedicated to explore the factors affecting sleep quality, and many of these studies have approached the issue from a singular perspective or with a narrow focus. Present research has identified various elements, such as sociodemographic, lifestyle, mental health and behavioral patterns, which can influence sleep quality. However, there is a notable gap in a comprehensive approach that integrates these diverse determinants to offer a more holistic understanding of sleep quality among university students. Therefore, a study that amalgamates these factors, specifically tailored to the context of university students in Jiangsu Province, China, is necessary and timely.
2 Data collection procedures
2.1 Study design and period
Between October 27 and November 27, 2022, an online questionnaire was distributed to university students across Jiangsu Province using a convenient cluster sampling method. The survey involved students from 34 higher education institutions, including public and private universities with various sizes and specializations, which can offer a broad perspective of the educational landscape within this economically varied region. A web-based platform aims at protecting participants’ secret, the survey obtained informed consent electronically, students were aware of the study’s objectives, the anonymous nature of their responses and their right. The choice of data collection period during the academic semester was deliberated to optimize student engagement and response rates.
2.2 Inclusion and exclusion criteria
During the data collection period, all university students enrolled in Jiangsu Province were included in the study, excluding individuals who were unable to provide accurate data as required by the study, such as those who lacked data records or cooperation.
2.3 Sample size determination
Estimated according to the sample size calculation formula:
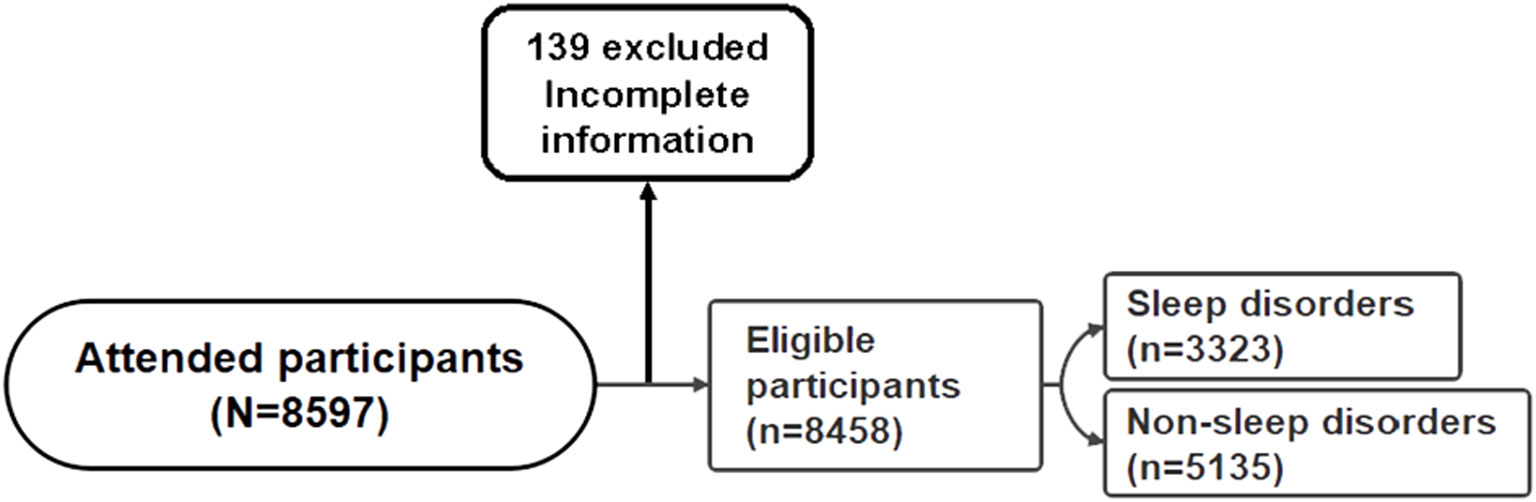
When =0.05, . Let be the expected prevalence rate, and . Based on the preliminary survey results of this study, the estimated detection rate of sleep disorders among college students is . The allowable error is , and the significance level is =0.05. As a result, the estimated sample size for the survey is 2017. Initially, the study included 8597 participants, excluding 139 individuals providing incomplete information (Figure 1). Subsequently, the final analysis included 8458 participants, the validity rate of the questionnaire was 98.4%.
3 Data collection and tools
3.1 Demographic data
This study assessed an array of demographic characteristics: gender (categorized as male or female), grade level (broken down by First-year, Second-year, and Third-year or higher), native place (classified as Rural or Urban), status as an only child (designated as Only child or Not only child), parental education level (divided into High school and Below, Junior university, or Undergraduate and above), family’s economic status (identified as High, Middle, or Low), BMI (segmented into <18.5, 18.5-24, and >24), smoking and drinking habits (Never, Occasional, or Usually), frequency of physical activity (categorized as ≤1 per month, 1-3 times per week, or 4-7 times per week), levels of academic and employment-related pressure (considered Low, Moderate, or High), occurrence of roommates sleeping late (Yes or No), presence of noise in the dormitory (Yes or No), intensity of dormitory lighting at night (Yes or No), acknowledgment of dormitory cleanliness (Yes or No), quality of relationships with classmates (rated as Good, General, or Poor), self-evaluated physical and mental health status (rated as Good, General, or Poor).
3.2 Pittsburgh sleep quality index
The PSQI serves as an tool to evaluate sleep quality (36). This self-administered questionnaire comprises of 18 items, 16 of which are scored individually, omitting data on bedtime and wake-up time - and is engineered to gauge an individual’s subjective assessment of their sleep patterns over one month. Each item score ranges from 0 to 3, and the aggregated total yields the overall sleep quality score, which spans from 0 to 21, wherein higher totals signify diminished sleep quality. A global PSQI score > 5 indicates poor sleep quality (36). The PSQI has been proven to be a reliable and effective tool for assessing the sleep quality of the Chinese population (37). In this study, the Cronbach’s alpha for the PSQI was 0.877 and the Kaiser-Meyer-Olkin value was 0.925.
3.3 Mobile phone addiction index
The mobile phone addiction index (MPAI) revised by Leung (38) is widely recognized for its efficacy in evaluating mobile phone addiction, particularly among university students. The scale comprises 17 items, each scored on a scale of 1 to 5, the higher total score, the greater the indication of addiction to mobile phones. The full scale can be divided into four dimensions: “Inability to control craving,” “Anxiety and Feeling Lost,” “Withdrawal and escape,” and “Productivity loss.” In this study, the Cronbach’s alpha for the MPAI was 0.925 and the Kaiser-Meyer-Olkin value was 0.917.
3.4 Connor-Davidson resilience scale
The Connor-Davidson Resilience Scale (CD-RISC) (39) is a tool to measure the ability to cope with stress and adversity. This study used a revised version (40) translated by Nan Xiao to measure the level of psychological resilience in university students. This scale contains 25 question entries which were divided into three dimensions of “Optimism”, “Self-improvement” and “Tenacity”, using a 5-point Likert scale: not true at all (0) to true almost all the time (4). The total score ranges from 0 to 100, with a higher score indicating more resilience. In this study, the Cronbach’s alpha for the CD-RISC was 0.969 and the Kaiser-Meyer-Olkin value was 0.979.
4 Statistical analysis
Statistical assessment was conducted utilizing SPSS software, version 26.0. Missing data were addressed through methods such as listwise deletion and mean imputation. The threshold for determining statistical significance was established at a P-value less than 0.05. To characterize the study’s sample, descriptive statistics were computed, including means, standard deviations for continuous variables, frequencies and percentages for categorical variables. Differences among categorical demographic variables, mobile phone addiction and sleep quality were examined using chi-square tests. For continuous variables, t-tests were employed to explore the differences. Significant variables from univariate analysis were included in binary logistic regression to model the probability of poor sleep quality. Model construction yielded odds ratios (OR) and corresponding 95% confidence intervals (95%CI) for each predictor.
5 Results
5.1 Comparison of sleep quality at the individual level in subjects with different characteristics
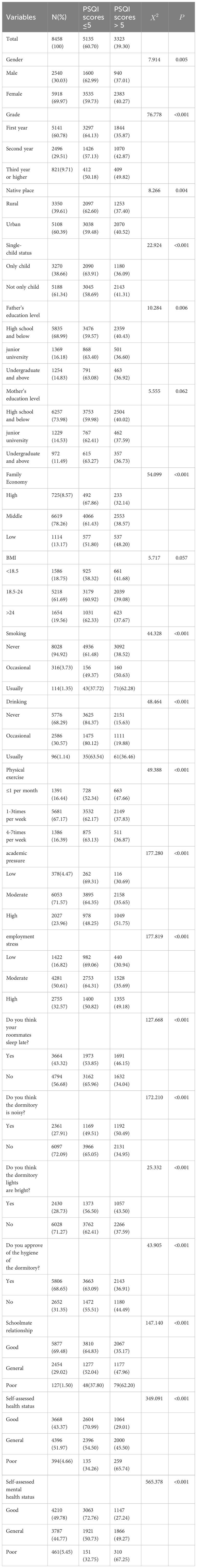
Participants’ Characteristicshowed the demographic information of university students in Jiangsu Province, China (Table 1). The result revealed that the largest proportion of participants consisted of students in their first and second years of study (90.29%). Of these participants, 69.97% were female, 61.34% were not the only child in their family, and the majority hailed from urban and suburban areas (60.39%). When it came to parental education, over half of the participants had either a high school education (68.99% and 73.98%, respectively). Furthermore, majority of the participants belonged to families with a moderate economic status (78.26%). Interestingly, only a small percentage of the participants reported smoking cigarettes (5.08%), and 31.71% of them admitted to consuming alcohol. The majority of university students experienced high levels of academic and employment-related stress (95.53% and 83.18%, respectively). It is worth noting that 56.68% of participants believed their roommates had a habit of staying up late. Additionally, over half of the participants described their physical and mental health as poor (56.63% and 50.22%, respectively). The result further revealed significant correlations between various factors and the sleep quality of university students. Specifically, the participants’ gender, grade level, hometown, father’s education level, family economic status, smoking and drinking habits, physical exercise frequency, academic and employment-related pressures, self-assessment of the dormitory environment, relationships with classmates, as well as their self-assessment of physical and mental health in comparison to others, all demonstrated associations with sleep quality.
5.2 Psychological resilience and mobile phone addiction with sleep quality
The total and domain scores from the MPAI and CD-RISC assessments between individuals with and without sleep disorders were showed in Table 2. The mean total score on the MPAI for individuals with sleep disorders was 47.89 ± 13.87, while the mean score for those without sleep disorders was 42.70 ± 13.24. Similarly, for the CD-RISC total score, individuals with sleep disorders obtained a mean score of 57.07 ± 17.17, whereas those without sleep disorders had a mean score of 63.22 ± 18.53. Across all four domains of the MPAI, patients with sleep disorders exhibited significantly higher scores compared to patients without sleep disorders (P< 0.001). Conversely, patients with sleep disorders demonstrated significantly lower scores across all three domains of the CD-RISC compared to patients without sleep disorders (P< 0.001).
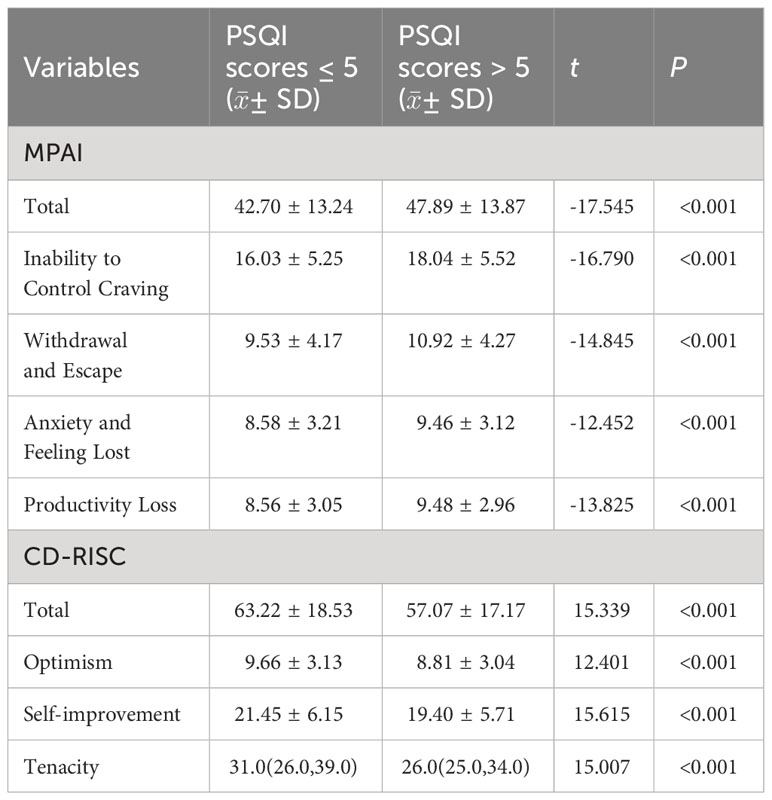
Table 2 Psychological resilience score/Mobile phone addiction score for participants with sleep quality (n=8258).
5.3 Logistic regression of influential factors contributing to sleep quality
The risk and protective factors that influence the quality of sleep among university students were showed in Table 3. Female students have a higher likelihood of experiencing poor sleep quality compared to male students (OR = 1.238; 95% CI, 1.109-1.382). Seniors are 1.6 times more than juniors to likely to have sleep disorders (OR = 1.582; 95% CI, 1.344-1.863). Non-only children are more susceptible to poor sleep quality (OR = 1.195; 95% CI, 1.077-1.326). Regular smoking increases the risk of sleep disorders (OR = 1.833; 95% CI, 1.181-2.847). Similarly, university students who consume alcohol regularly are 1.74 times more likely to develop sleep disorders than those who abstain from alcohol (OR = 1.737; 95% CI, 1.065-2.833). Higher levels of physical activity are associated with a reduced risk of sleep disorders, as university students who engage in frequent exercise are less likely to experience sleep disturbances compared to those with less physical activity (OR = 0.921; 95% CI, 0.779-1.090). Additionally, university students facing high academic stress are 1.2 times more likely to experience sleep disturbances than those with lower stress levels (OR = 1.326; 95% CI, 1.012-1.736). Similarly, elevated employment stress is associated with a 1.4-fold increase in the likelihood of sleep disturbances (OR = 1.352; 95% CI, 1.156-1.582). Students whose roommates have earlier bedtimes are less likely to experience sleep disturbances (OR = 0.799; 95% CI, 0.718-0.888), and those residing in quieter dormitories have a lower likelihood of acquiring sleep disorders (OR = 0.732; 95% CI, 0.647-0.828). Dissatisfaction with dormitory hygiene increases the likelihood of poor sleep quality by 1.1 times compared to being satisfied with dormitory hygiene (OR = 1.140; 95% CI, 1.028-1.265). Students with poor self-rated physical health face a twofold higher risk of sleep disorders than those with good self-rated physical health (OR = 1.969; 95% CI, 1.533-2.529). Similarly, students with poor self-rated mental health are 2.9 times more likely to have a sleep disorder compared to those with good self-rated mental health (OR = 2.924; 95% CI, 2.309-3.702). A high score on the MPAI (OR = 1.029; 95% CI: 1.026-1.033) was associated with a slightly increased risk of poor sleep quality, suggesting that individuals with higher MPAI values may be more likely to experience sleep disturbances. On the other hand, a higher score on the CD-RISC (OR = 0.982; 95% CI: 0.979-0.984) was linked to a small but statistically significant decrease in the odds of poor sleep quality, indicating that greater resilience, as measured by the CD-RISC, may serve as a protective factor against sleep quality issues.
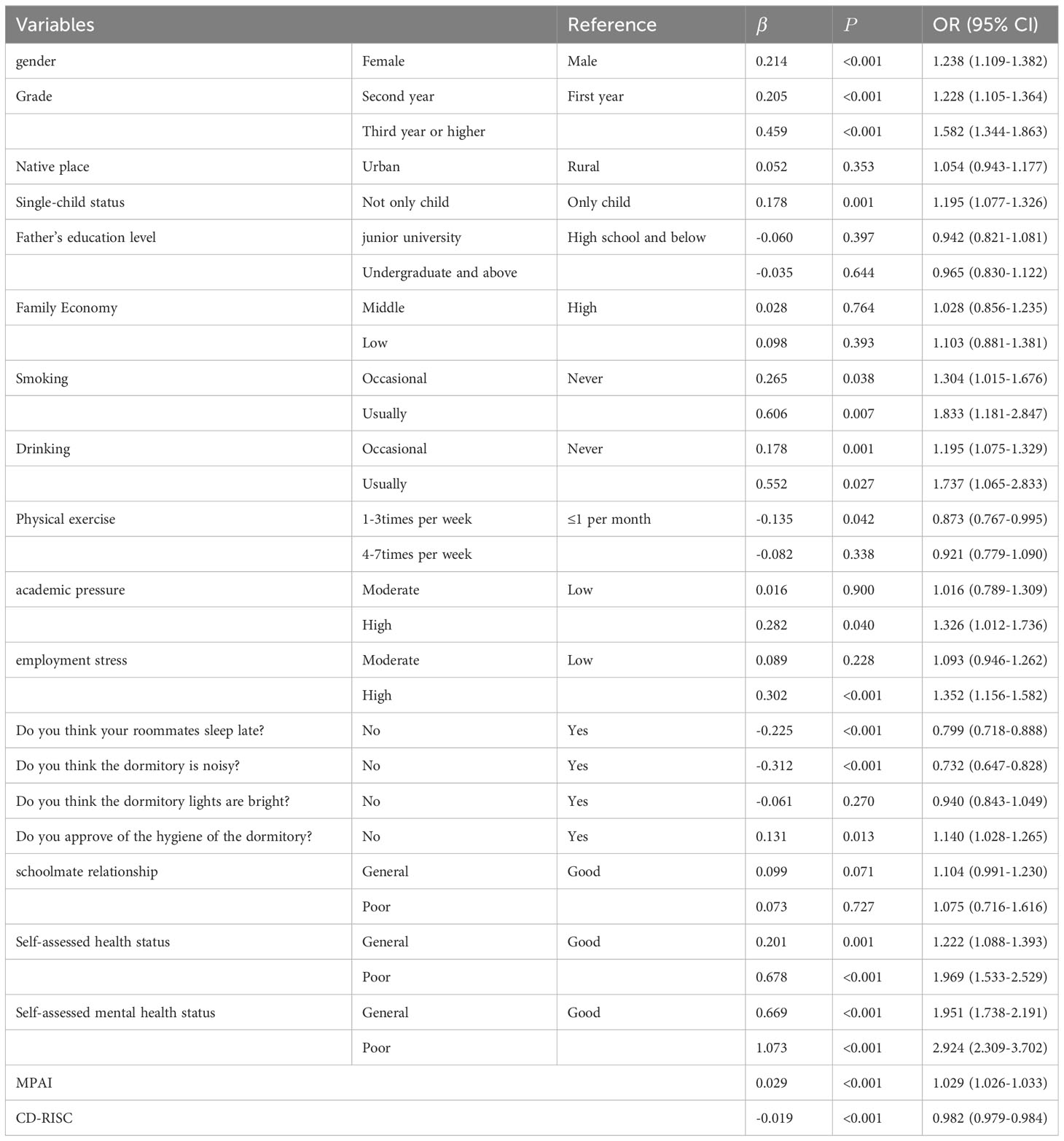
Table 3 Results of logistic regression analysis of sleep quality associated with demographic, psychological and behavioral factors.
6 Discussion
In a cross-sectional survey of 8,458 university students in Jiangsu Province, China, we found that sleep disorders were common among university students. Physical activity and high psychological resilience had a significant positive and protective effect on sleep quality. Higher grades, not being an only child, academic and employment stress, smoking and drinking habits, roommates staying up late, noisy dormitory environment, poor dormitory hygiene, self-rated physical and mental health problems and high MPAI scores had significant negative effects on sleep quality.
This study revealed that 39.30% of the participants experienced poor sleep quality as determined by the PSQI scale with a critical sleep disorders value of 5. This finding notably contrasts with research conducted in other regions of China. For instance, a survey conducted in Shanghai in 2022 during the COVID-19 period reported a prevalence of sleep disorders of 90.2% among dialysis patients (40), and a study conducted in Beijing in 2021 identified a prevalence of 53.2% (41). Meanwhile, a survey conducted in Changsha reported that only 9.8% of university students suffer from sleep disorders (42), suggesting a substantial variation. Furthermore, the prevalence of this health problem is 52.4% in Turkey (43). Such disparate findings could be ascribed to the multitude of factors influencing sleep quality, including but not limited to, the demographic and health status of the surveyed population, the period during which the data was collected, and distinctive regional or cultural influences. Another important consideration is the different psychometric thresholds applied to the PSQI or other sleep assessment tools, as which can influence the classification of sleep quality and the reported prevalence of disorders.
In our study, we identified several demographic variables that were significantly linked to the prevalence of sleep disorders. Specifically, our analysis supports existing literature (44) which is showing that female students are more susceptible to experiencing sleep disturbances, a trend that has been consistently observed across various studies. One study found that the higher prevalence of sleep disorders among female students may be associated with premenstrual syndrome (PMS) (45). It is noteworthy that our sample had an overrepresentation of females, which may skew the results. This overrepresentation could limit the generalizability of our findings to all students. Further research with a more balanced gender sample is necessary. Furthermore, upperclassmen exhibited a significantly higher prevalence of sleep disorders compared to their junior peers. This could be attributed to the escalating pressure associated with graduation, which typically brings about more intense academic workloads and career-related stress. Family structure also appeared to influence sleep quality, as students who were not the only child in their family tended to report more sleep problems. This might be related to the dynamics of parental attention and emotional support, wherein non-only children may receive less focused support, leading to enhanced anxiety which can negatively affect sleep. Lifestyle factors such as smoking and alcohol consumption were found to correlate significantly with poor sleep quality, corresponding to previous research (18). In stark contrast, a beneficial link was noted between physical activity and sleep quality. Regular participation in physical activities was inversely related to poor sleep quality, suggesting that a more active lifestyle could act as a protective factor against sleep disorders, corroborating the findings from other studies (26).
University students facing higher levels of academic and employment stress were more prone to experiencing poor sleep quality. Academic pressures coupled with job-related concerns can lead to heightened worries about the future. Such stress generates considerable psychological strain, which can directly interfere with the ability to obtain restful sleep. The anticipation of future events and obligations often keeps the mind actively engaged at night, preventing the relaxation necessary to initiate sleep.
Environmental elements in a university setting can also be disruptive to sleep. The sleeping habits of roommates, noisy dormitory environments, and poor dormitory hygiene can hinder university students from attaining a conducive sleeping environment, resulting in compromised sleep quality.
Lastly, students who rated their physical and mental health poorly also exhibited noticeable sleep disorder problems. These students may encounter mental health issues such as stress, anxiety, and depression, which can disrupt their ability to fall asleep or maintain good sleep quality. Additionally, physical health problems like chronic pain, digestive issues, and respiratory difficulties can adversely affect sleep patterns.
Furthermore, our study revealed that the level of mobile phone addiction and psychological resilience had significant correlations with sleep quality among university students. Specifically, we observed that university students with higher levels of mobile phone addiction were more prone to experiencing poor sleep quality. Several studies have indicated that the blue light emitted by smartphones is associated with sleep quality (46). When the body is exposed to blue light at night, it disrupts the body’s biological clock. This is because that blue light from smartphones suppresses the brain’s production of melatonin, which in turn affects our ability to fall asleep (47). Conversely, psychological resilience, which serves as a beneficial psychological asset, had a protective influence on sleep quality. University students with higher psychological resilience demonstrated a decreased likelihood of experiencing poor sleep quality. These findings were further supported by a related study (48).
Enhancing the sleep quality of university students is essential and effective strategies must be deployed. One key initiative is the provision of sleep education (49), which equips students with knowledge regarding the critical role of sleep for both brain function and overall well-being. Practical sleep tips can also be provided to assist students in establishing healthy sleep habits. Additionally, advocating for a harmonious lifestyle that includes routine physical activity and balanced nutrition is instrumental in synchronizing the body’s circadian rhythm, thus facilitating easier transitions into slumber and refining overall sleep quality. The optimization of the sleep environment is eqully critical (50). Schools can create quiet study and living spaces, while employing resources such as blackout curtains, earplugs, and noise machines to foster a tranquil and comfortable sleeping environment. Furthermore, It was found that psychological resilience had a closed association with sleep quality, and enhancing psychological resilience could mitigate the direct and indirect impacts of stressful life events on sleep quality (35). It is vital to provide psychological support and equip students with stress management techniques to mitigate the impact of stress on sleep quality. By offering psychological counseling and support services, schools can aid students in effectively coping with stress and anxiety. To combat the pervasive issue of mobile phone addiction, it is prudent for both educational institutions and households to formulate and enforce sensible mobile phone usage policies. Encouraging students to abstain from mobile phone usage one hour before bedtime and employing mobile phone applications to monitor usage time prove to be beneficial. Presenting an assortment of captivating alternatives such as athletic competitions and social get-togethers serves to shift students’ focus away from their digital screens, thus nurturing healthier lifestyle choices. In parallel, the establishment of set digital downtime encourages students to temporarily detach from their electronic gadgets, granting them the opportunity to relax and enhance their sleep quality.
7 Conclusions
The overall prevalence of poor sleep quality was 39.30%, with a detection rate of 40.27% among female university students and 37.01% among male university students. Binary logistic regression analysis revealed that physical activity and high psychological flexibility significantly improved sleep quality, providing a protective effect. Additionally, higher grade level, not being an only child, academic and employment stress, smoking and drinking habits, roommates staying up late, a noisy dormitory environment, poor dormitory hygiene, self-rated physical and mental health issues, and a high MPAI score were identified as risk factors associated with sleep quality. It is imperative to take actionable measures to improve the sleep quality of university students in Jiangsu Province, China.
7.1 Limitations
Several limitations should be noted in our study. Firstly, the study’s cross-sectional design limits our ability to establish causality. Longitudinal research in the future would be beneficial in determining the predictors of sleep quality rather than merely assessing correlations. Secondly, the reliance on self-reported questionnaires for data collection might have introduced recall bias. Future studies could integrate objective methods such as sleep monitoring devices and activity trackers to obtain more accurate sleep data. Thirdly, we acknowledge that the gender ratio in our study was skewed, with an overrepresentation of female participants. This imbalance could introduce a selection bias affecting the reported prevalences of sleep issues, which may not accurately reflect the broader population. We recommend that subsequent research efforts aim for a balanced gender mix to diminish potential gender-based bias and enhance the representativeness of the findings. Another limitation is that we were unable to track the exact number of students who accessed the survey link in the open-ended online survey, and therefore could not calculate a traditional response rate.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of Xuzhou Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
BH: Conceptualization, Writing – review & editing. QW: Data curation, Investigation, Software, Writing – original draft. WY: Data curation, Writing – review & editing. HZ: Data curation, Writing – review & editing. DY: Conceptualization, Funding acquisition, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the National Natural Science Foundation of China (Grant number 81802101). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Rea EM, DeCarlo Santiago C, Nicholson L, Heard Egbert A, Bohnert AM. Sleep, affect, and emotion reactivity in first-year college students: A daily diary study. Int J Behav Med. (2022) 30:753–68. doi: 10.1007/s12529-022-10127-0.
2. Nicholson LM, Egbert AH, Moreno JP, Bohnert AM. Variability of sleep and relations to body weight among first-year college students. Int J Behav Med. (2021) 28:227–37. doi: 10.1007/s12529-020-09888-3.
3. Han T, Wang W, Kuroda Y, Mizuno M. The relationships of sleep duration and inconsistency with the athletic performance of collegiate soft tennis players. Front Psychol. (2022) 13:791805. doi: 10.3389/fpsyg.2022.791805.
4. Wang T, Yin J, Hu C, Tang W, Che X, Liu Y. Sleep disturbance and medical requests among university and college students in Chongqing, China: A cross-sectional study. Saudi Med J. (2023) 44:1153–9. doi: 10.15537/smj.2023.44.11.20230420.
5. Toscano-Hermoso MD, Arbinaga F, Fernández-Ozcorta EJ, Gómez-Salgado J, Ruiz-Frutos C. Influence of sleeping patterns in health and academic performance among university students. Int J Environ Res Public Health. (2020) 17:2760. doi: 10.3390/ijerph17082760.
6. Musshafen LA, Tyrone RS, Abdelaziz A, Sims-Gomillia CE, Pongetti LS, Teng F, et al. Associations between sleep and academic performance in US adolescents: a systematic review and meta-analysis. Sleep Med. (2021) 83:71–82. doi: 10.1016/j.sleep.2021.04.015.
7. Li DL, Liang G, Yin ZJ, Li YZ, Zheng YJ, Qin Y, et al. Associations between sleep characteristics, chronotype and body mass index among Chinese college freshmen. Chronobiol Int. (2023) 40:803–11. doi: 10.1080/07420528.2023.2210667.
8. Díaz G, Hernández S, Crespo A, Renghea A, Yébenes H, Iglesias-López MT. Macronutrient intake, sleep quality, anxiety, adherence to a mediterranean diet and emotional eating among female health science undergraduate students. Nutrients. (2023) 15:2882. doi: 10.3390/nu15132882.
9. Qu Y, Li T, Xie Y, Tao S, Yang Y, Zou L, et al. Association of chronotype, social jetlag, sleep duration and depressive symptoms in Chinese college students. J Affect Disord. (2023) 320:735–41. doi: 10.1016/j.jad.2022.10.014.
10. Tafoya SA, Aldrete-Cortez V, Tafoya-Ramos F, Fouilloux-Morales C, Díaz-Olavarrieta C. Sleep and perceived stress: an exploratory mediation analysis of the role of self-control and resilience among university students. Int J Environ Res Public Health. (2023) 20:6560. doi: 10.3390/ijerph20166560.
11. Wang Y, Xiao H, Zhang X, Wang L. The role of active coping in the relationship between learning burnout and sleep quality among college students in China. Front Psychol. (2020) 11:647. doi: 10.3389/fpsyg.2020.00647.
12. Ye J, Jia X, Zhang J, Guo K. Effect of physical exercise on sleep quality of college students: Chain intermediary effect of mindfulness and ruminative thinking. Front Psychol. (2022) 13:987537. doi: 10.3389/fpsyg.2022.987537.
13. García-García J, Mañas A, González-Gross M, Espin A, Ara I, Ruiz JR, et al. Physical activity, sleep, and mental health during the COVID-19 pandemic: A one-year longitudinal study of Spanish university students. Heliyon. (2023) 9:e19338. doi: 10.1016/j.heliyon.2023.e19338.
14. Castelli L, Galasso L, Mulè A, Ciorciari A, Esposito F, Roveda E, et al. Physical activity and morningness: A helpful combination in improving the sleep quality of active Italian university students. Chronobiol Int. (2023) 40:1028–38. doi: 10.1080/07420528.2023.2241906.
15. Zheng W, Chen Q, Yao L, Zhuang J, Huang J, Hu Y, et al. Prediction models for sleep quality among college students during the COVID-19 outbreak: cross-sectional study based on the internet new media. J Med Internet Res. (2023) 25:e45721. doi: 10.2196/45721.
16. Ji W, Shi L, Lin X, Shen Z, Chen Q, Song D, et al. The relationship between sleep quality and daytime dysfunction among college students in China during COVID-19: a cross-sectional study. Front Public Health. (2023) 11:1253834. doi: 10.3389/fpubh.2023.1253834.
17. Li Y, Bai W, Zhu B, Duan R, Yu X, Xu W, et al. Prevalence and correlates of poor sleep quality among college students: a cross-sectional survey. Health Qual Life Outcomes. (2020) 18:210. doi: 10.1186/s12955-020-01465-2.
18. Zhang L, Zheng H, Yi M, Zhang Y, Cai G, Li C, et al. Prediction of sleep quality among university students after analyzing lifestyles, sports habits, and mental health. Front Psychiatry. (2022) 13:927619. doi: 10.3389/fpsyt.2022.927619.
19. Yeboah K, Dodam KK, Agyekum JA, Oblitey JN. Association between poor quality of sleep and metabolic syndrome in Ghanaian university students: A cross-sectional study. Sleep Disord. (2022) 2022:8802757. doi: 10.1155/2022/8802757.
20. Wu Q, Yuan L, Guo XH, Li JA, Yin D. Study on lifestyle habits affecting sleep disorders at the undergraduate education stage in Xuzhou City, China. Front Psychol. (2022) 13:1053798. doi: 10.3389/fpsyg.2022.1053798.
21. Shadzi MR, Salehi A, Vardanjani HM. Problematic internet use, mental health, and sleep quality among medical students: A path-analytic model. Indian J Psychol Med. (2020) 42:128–35. doi: 10.4103/IJPSYM.IJPSYM_238_19.
22. Zhou Y, Bo S, Ruan S, Dai Q, Tian Y, Shi X. Deteriorated sleep quality and influencing factors among undergraduates in northern Guizhou, China. PeerJ. (2022) 10:e13833. doi: 10.7717/peerj.13833.
23. Jones RD, Jackson WB 2nd, Mazzei A, Chang AM, Buxton OM, Jackson CL. Ethnoracial sleep disparities among college students living in dormitories in the United States: a nationally representative study. Sleep Health. (2020) 6:40–7. doi: 10.1016/j.sleh.2019.10.005.
24. Babicki M, Piotrowski P, Mastalerz-Migas A. Insomnia, Daytime Sleepiness, and Quality of Life among 20,139 College Students in 60 Countries around the World-A 2016-2021 Study. J Clin Med. (2023) 12:692. doi: 10.3390/jcm12020692.
25. Maciel FV, Wendt AT, Demenech LM, Dumith SC. Factors associated with sleep quality in university students. Cien Saude Colet. (2023) 28:1187–98. doi: 10.1590/1413-81232023284.14132022.
26. Santos M, Sirtoli R, Rodrigues R, López-Gil JF, Martínez-Vizcaíno V, Guidoni CM, et al. Relationship between free-time physical activity and sleep quality in Brazilian university students. Sci Rep. (2023) 13:6652. doi: 10.1038/s41598-023-33851-3.
27. Bouloukaki I, Tsiligianni I, Stathakis G, Fanaridis M, Koloi A, Bakiri E, et al. Sleep quality and fatigue during exam periods in university students: prevalence and associated factors. Healthcare (Basel). (2023) 11:2389. doi: 10.20944/preprints202306.1542.v1.
28. Zhao C, He J, Xu H, Zhang J, Zhang G, Yu G. Are "night owls" or "morning larks" more likely to delay sleep due to problematic smartphone use? a cross-lagged study among undergraduates. Addict Behav. (2023) 150:107906. doi: 10.1016/j.addbeh.2023.107906
29. Abdulla NK, Obaid RR, Qureshi MN, Asraiti AA, Janahi MA, Abu Qiyas SJ, et al. Relationship between hedonic hunger and subjectively assessed sleep quality and perceived stress among university students: A cross-sectional study. Heliyon. (2023) 9:e14987. doi: 10.1016/j.heliyon.2023.e14987.
30. Sserunkuuma J, Kaggwa MM, Muwanguzi M, Najjuka SM, Murungi N, Kajjimu J, et al. Problematic use of the internet, smartphones, and social media among medical students and relationship with depression: An exploratory study. PloS One. (2023) 18:e0286424. doi: 10.1371/journal.pone.0286424.
31. Hamvai C, Kiss H, Vörös H, Fitzpatrick KM, Vargha A, Pikó BF. Association between impulsivity and cognitive capacity decrease is mediated by smartphone addiction, academic procrastination, bedtime procrastination, sleep insufficiency and daytime fatigue among medical students: a path analysis. BMC Med Educ. (2023) 23:537. doi: 10.1186/s12909-023-04522-8.
32. Alahdal WM, Alsaedi AA, Garrni AS, Alharbi FS. The impact of smartphone addiction on sleep quality among high school students in makkah, Saudi Arabia. Cureus. (2023) 15:e40759. doi: 10.7759/cureus.40759.
33. Zhang J, Yuan G, Guo H, Zhang X, Zhang K, Lu X, et al. Longitudinal association between problematic smartphone use and sleep disorder among Chinese college students during the COVID-19 pandemic. Addict Behav. (2023) 144:107715. doi: 10.1016/j.addbeh.2023.107715.
34. Xie G, Wu Q, Guo X, Zhang J, Yin D. Psychological resilience buffers the association between cell phone addiction and sleep quality among college students in Jiangsu Province, China. Front Psychiatry. (2023) 14:1105840. doi: 10.3389/fpsyt.2023.1105840.
35. Li Y, Guo K. Research on the relationship between physical activity, sleep quality, psychological resilience, and social adaptation among Chinese college students: A cross-sectional study. Front Psychol. (2023) 14:1104897. doi: 10.3389/fpsyg.2023.1104897.
36. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4.
37. Du Z, Wang G, Yan D, Yang F, Bing D. Relationships between the Pittsburgh Sleep Quality Index (PSQI) and vertigo outcome. Neurol Res. (2023) 45:291–9. doi: 10.1080/01616412.2022.2132728.
38. Leung L. Linking psychological attributes to addiction and improper use of the mobile phone among adolescents in hong kong. J Children Media. (2008) 2:93–113. doi: 10.1080/17482790802078565.
39. Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety. (2003) 18:76–82. doi: 10.1002/(ISSN)1520-6394.
40. Zhu X, Zheng T, Ding L, Zhang X. Exploring associations between eHealth literacy, cyberchondria, online health information seeking and sleep quality among university students: A cross-section study. Heliyon. (2023) 9:e17521. doi: 10.1016/j.heliyon.2023.e17521.
41. Yan C, Li A, Hao Y, Zhang X, Guo Y, Gu Y, et al. The relationship between circadian typology and dry eye symptoms in chinese college students. Nat Sci Sleep. (2022) 14:1919–25. doi: 10.2147/NSS.S378612.
42. Huang Q, Li Y, Huang S, Qi J, Shao T, Chen X, et al. Smartphone use and sleep quality in chinese college students: A preliminary study. Front Psychiatry. (2020) 11:352. doi: 10.3389/fpsyt.2020.00352.
43. Ozcan B, Acimis NM. Sleep Quality in Pamukkale University Students and its relationship with smartphone addiction. Pak J Med Sci. (2021) 37:206–11. doi: 10.12669/pjms.37.1.3130
44. Schmickler JM, Blaschke S, Robbins R, Mess F. Determinants of sleep quality: A cross-sectional study in university students. Int J Environ Res Public Health. (2023) 20:2019. doi: 10.3390/ijerph20032019.
45. Yi SJ, Kim M, Park I. Investigating influencing factors on premenstrual syndrome (PMS) among female college students. BMC Womens Health. (2023) 23:592. doi: 10.1186/s12905-023-02752-y.
46. Randjelović P, Stojanović N, Ilić I, Vučković D. The effect of reducing blue light from smartphone screen on subjective quality of sleep among students. Chronobiol Int. (2023) 40:335–42. doi: 10.1080/07420528.2023.2173606.
47. Powers P, Gavrilovic M, Santana J, Yi S, Spoor A, Campisi J. A preliminary study on the effect of mobile device backlight spectrum variation on the quality of sleep among undergraduate students. Bios. (2021) 92:86–93. doi: 10.1893/BIOS-D-18-00003.
48. Mohebbian B, Najafi M, Sabahi P. The effect of transcranial direct current stimulation on sleep quality, resilience, and optimism. Curr Psychol. (2023) 42:5785–92. doi: 10.1007/s12144-021-01944-9.
49. D'Orsogna T, Halson SL, Oehmen R. Poor sleep quality during COVID-19 pandemic restrictions associated with reduced psychological wellbeing in healthcare students. Chronobiol Int. (2023) 40:438–49. doi: 10.1080/07420528.2023.2186127.
50. Khazaie H, Behrouz B, Chehri A, Gerber M, Holsboer-Trachsler E, Sadeghi Bahmani D, et al. Among adolescents, addiction susceptibility and sleep-related dysfunction have a common cognitive-emotional base and predict poor sleep quantity. J Subst Use. (2019) 24:426–31. doi: 10.1080/14659891.2019.1588405.
Keywords: university students, sleep quality, psychological resilience, PSQI, MPAI, influencing factors
Citation: Hu B, Wu Q, Wang Y, Zhou H and Yin D (2024) Factors associated with sleep disorders among university students in Jiangsu Province: a cross-sectional study. Front. Psychiatry 15:1288498. doi: 10.3389/fpsyt.2024.1288498
Received: 04 September 2023; Accepted: 09 February 2024;
Published: 23 February 2024.
Edited by:
Lino Nobili, University of Genoa, ItalyReviewed by:
Mubashir Zafar, University of Hail, Saudi ArabiaIzolde Bouloukaki, University of Crete, Greece
Copyright © 2024 Hu, Wu, Wang, Zhou and Yin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bin Hu, eHptY2d3aGJAMTI2LmNvbQ==; Dehui Yin, eWluZGgxNkB4emhtdS5lZHUuY24=
†These authors have contributed equally to this work
 Bin Hu*†
Bin Hu*† Qi Wu
Qi Wu Yue Wang
Yue Wang Dehui Yin
Dehui Yin