
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 15 February 2023
Sec. Public Mental Health
Volume 14 - 2023 | https://doi.org/10.3389/fpsyt.2023.975443
 Yan-Jie Zhao1†
Yan-Jie Zhao1† Cheng Zhang2†
Cheng Zhang2† Tong Guo1†
Tong Guo1† Sha Sha1†
Sha Sha1† Zhaohui Su3
Zhaohui Su3 Teris Cheung4
Teris Cheung4 Todd Jackson5
Todd Jackson5 Feng-Rong An1*
Feng-Rong An1* Yu-Tao Xiang6,7*
Yu-Tao Xiang6,7*Background: Post-traumatic stress symptoms (PTSS) are commonly reported by psychiatric healthcare personnel during the coronavirus disease 2019 (COVID-19) pandemic and negatively affect quality of life (QOL). However, associations between PTSS and QOL at symptom level are not clear. This study examined the network structure of PTSS and its connection with QOL in psychiatric healthcare personnel during the COVID-19 pandemic.
Methods: This cross-sectional study was carried out between March 15 and March 20, 2020 based on convenience sampling. Self-report measures including the 17-item Post-Traumatic Stress Disorder Checklist – Civilian version (PCL-C) and World Health Organization Quality of Life Questionnaire - Brief Version (WHOQOL-BREF) were used to measure PTSS and global QOL, respectively. Network analysis was used to investigate the central symptoms of PTSS and pattern of connections between PTSS and QOL. An undirected network was constructed using an extended Bayesian Information Criterion (EBIC) model, while a directed network was established based on the Triangulated Maximally Filtered Graph (TMFG) method.
Results: Altogether, 10,516 psychiatric healthcare personnel completed the assessment. “Avoidance of thoughts” (PTSS-6), “Avoidance of reminders” (PTSS-7), and “emotionally numb” (PTSS-11) were the most central symptoms in the PTSS community, all of which were in the Avoidance and Numbing domain. Key bridge symptoms connecting PTSS and QOL were “Sleep disturbances” (PTSS-13), “Irritability” (PTSS-14) and “Difficulty concentrating” (PTSS-15), all of which were within the Hyperarousal domain.
Conclusion: In this sample, the most prominent PTSS symptoms reflected avoidance while symptoms of hyper-arousal had the strongest links with QOL. As such, these symptom clusters are potentially useful targets for interventions to improve PTSS and QOL among healthcare personnel at work under pandemic conditions.
Since the coronavirus disease 2019 (COVID-19) was first reported in China at the end of 2019 and a pandemic was declared by the World Health Organization (WHO) in March 2020 (1), more than 200 countries and territories have been affected (2–4). As of December 2022, there have been over 659 million COVID-19 cases globally and over 6.6 million deaths, with the estimated mortality rate of 1.0% (2). In China, more than 400 thousands people had been diagnosed with COVID-19 by December, 2022 (5). The mortality rate caused by COVID-19 in China (1.2%) is similar with the global mortality rate. Due to the fast transmission of the novel virus, a relatively high death rate, the lack of specific medications and strict public health measures (e.g., suspension of public transportation, quarantine, and school closure) during early stages of the pandemic, many sub-populations suffered from mental health problems including depression, anxiety, insomnia, distress, and post-traumatic stress symptoms (PTSS) (6–9).
A previous meta-analysis revealed that 24, 23, 16 and 25% of all sub-populations reported depressive and anxiety symptoms, distress and PTSS, respectively during the COVID-19 pandemic (9). Of the psychological sequelae noted above, the prevalence of PTSS was highest. Healthcare professionals have had a higher prevalence of PTSS than the general population during the COVID-19 pandemic (28% vs. 19%), a difference that underscores how health professionals have been a high-risk population for PTSS during the pandemic (9).
PTSS comprises a host of psychiatric symptoms triggered by a traumatic event such as warfare, traffic collisions or other threats on a person’s life (10–12). PTSS includes disturbing thoughts, feelings, or dreams related to traumatic events, mental or physical distress associated with trauma-related cues, attempts to avoid trauma-related cues, alterations in the way one thinks and feels, and an increase in fight-or-flight responses (10, 13). Negative consequences of PTSS include psychiatric comorbidities, impaired functioning and lowered quality of life (QOL) (14–17).
The epidemiology of PTSS during outbreaks of acute infectious diseases has been examined previously (18–21). For example, one meta-analysis found that 17% of the general population experienced PTSS during the SARS outbreak while the corresponding figure during the COVID-19 pandemic was 25% (9). Recent studies found that up to 70% of healthcare professionals experienced COVID-19-related PTSS, due mainly to heavy clinical workloads and the fear of being infected (22). Apart from frontline health professionals, related populations including medical students who completed internships in hospital wards were also at risk for PTSS during early COVID-19 pandemic stages (23–25).
Similar to health professionals working in intensive care units or emergency departments (18, 19), psychiatric healthcare personnel have been susceptible to experiencing PTSS during the COVID-19 pandemic. In early stages of the pandemic, several nosocomial infections were reported in psychiatric hospitals and over 300 psychiatric inpatients and healthcare personnel were infected with COVID-19 (26, 27) because of significant challenges in patient management and deficient pandemic control measures such as protective equipment shortages, inadequate training in public health emergency responses, and increased vulnerability of psychiatric inpatients to infectious diseases (28). Under such circumstances, psychiatric healthcare personnel often suffered from overwhelming workplace-related stress and were more prone to have COVID-19-related PTSS (28, 29).
A common limitation of studies on PTSS during the COVID-19 pandemic has been an over-reliance upon traditional statistical approaches (e.g., a latent factor approach) based on mean scale scores from measures of PTSS and associated risk factors (30). Key premises underlying latent factor approaches are that all individual symptoms of a disorder are dependent on each other and are typically given equal weights toward calculating total scores; as a result, mutual associations among symptoms cannot be explored or adjusted for (30, 31). However, individual PTSS symptoms such as avoidance, numbing and irritability often exhibit robust associations with each other compared to other PTSS symptoms (32, 33). These data highlight how traditional statistical approaches can fail to capture complexity, nuances or dynamics between individual symptoms (34, 35).
Alternatively, network analysis has emerged as a novel approach to articulating links between psychiatric symptoms (36). Network analysis provides a better understanding of the most prominent symptoms of particular syndromes as well as the nature and strength of interconnections between individual symptoms and associations with other experiences such as QOL (36–39).
To date, two studies have explored the network structure of PTSS in the general population during the COVID-19 pandemic (40, 41); self-destructive/reckless behavior and internal avoidance were key PTSS symptoms. However, the network structure of PTSS and its connections with the widely used health outcome of QOL among psychiatric healthcare personnel remain unknown. Understanding the most prominent PTSS symptoms among frontline healthcare providers dealing with direct effects of the COVID-19 pandemic as well as symptom-level associations between PTSS and QOL is important for adopting effective preventive measures and treatments to reduce negative consequences caused by PTSS in this population. Therefore, this study examined the network structure of PTSS and its connection with QOL among psychiatric healthcare personnel during the COVID-19 pandemic.
This was a cross-sectional, snowball-sampled study conducted between March 15 and March 20, 2020, shortly after the COVID-19 outbreak first emerged in China (3). Data were collected using the Questionnaire Star program (Changsha Haoxing Information Technology Co., Ltd., Changsha, China). A Quick Response (QR) code linked to the invitation and assessment forms was distributed by panel members of the Chinese Society of Psychiatry, and Chinese Nursing Association Branch of Psychiatry to all public psychiatric hospitals in China with WeChat, a social communication application with around 1.2 billion active monthly users in China (42) that is also used in continuing education projects of public psychiatric hospitals. To be eligible, participants needed to meet the following inclusion criteria: (1) aged 18 years or older; (2) frontline psychiatric healthcare personnel, including psychiatrists, nurses and nursing assistants working in clinical settings during the COVID-19 outbreak; (3) able to read Chinese and understand the purpose and contents of the assessments; (4) provide electronic written informed consent. The study protocol was approved by the Institutional Review Board (IRB) of Beijing Anding Hospital, China.
The presence and severity of COVID-19-related PTSS was assessed by the validated Chinese version of the 17-item Post-Traumatic Stress Disorder Checklist – Civilian version (PCL-C) (43–45). The PCL-C covers three domains: Intrusion (items 1–5), Avoidance and numbing (items 6–12), and Hyperarousal (items 13–17). Each PCL-C item is rated from 1 (not at all) to 5 (extremely), with a higher score indicating more severe PTSS. The PCL-C has been validated with good psychometric properties (45–47).
Global QOL (QOL hereafter) was assessed with the first two items of the World Health Organization Quality of Life Questionnaire - brief version (WHOQOL-BREF). In these two items, participants were asked how they would rate their overall QOL and general health status based on item anchors ranging from 1 to 5; higher scores represented better reported QOL (48, 49). The Chinese version of WHOQOL has been validated in Chinese samples with good psychometric properties (48).
An undirected network model was constructed using the extended Bayesian Information Criterion (EBIC) model graphical least absolute shrinkage and selection operator (gLASSO) with a non-paranormal transformation (50, 51); thicker edges indicated stronger relationships between individual symptoms or nodes. The importance of nodes was evaluated using network centrality indices including strength and bridge strength. Strength is defined as the sum of absolute weights of the edge connecting a certain node to all other nodes (52). Bridge strength is defined as the sum of the absolute value of all edges that exist between node A and all nodes that are not in the same cluster as node A (53).
A directed network model was established based on the Triangulated Maximally Filtered Graph (TMFG) method (54). The TMFG method distinguishes “influencing” and “influenced” nodes based on the concept of node dependence (55). In a directed network figure, arrows indicate the direction of influence. Since the dependency matrix produced by the TMFG method is asymmetric (defining the two-way influences between node i and node j as D(i, j) and D(j, i)), asymmetric relations were calculated by retaining only stronger associations between D(i, j) and D(j, i), as recommended previously (53, 56).
Network stability was assessed using a 1,000-time case-dropping bootstrap method (57–59). In order to examine possible confounding effects of basic demographic factors, undirected networks were re-estimated after controlling for age and sex (34, 60). Visual inspection and Spearman correlation coefficient analyses for network centrality indices were used to evaluate effects of age and sex on the network structure.
All analyses were performed using R, version 4.1.0 (61) with the packages bootnet (59), networktools (62), NetworkToolbox (53), psych (63), mgm (64), and qgraph (65).
Altogether, 10,516 psychiatric healthcare personnel met the study entry criteria and completed the assessment. A majority of the participants was female (84.5%, 8,881/10,516). The sample ranged in age between 18 and 65 years, with an average age of 33.3 ± 8.4 years. The sample mean PCL-C score was 21.4 ± 6.4.
Means, standard deviations (SD), strengths, bridge strengths, predictability, skewness and kurtosis of PTSS symptoms are presented in Table 1. The network structure of PTSS among psychiatric healthcare personnel is displayed in Figure 1. “Avoidance of thoughts” (PTSS-6), “Avoidance of reminders” (PTSS-7), and “Emotionally numb” (PTSS-11) were the three most central nodes in PTSS network, all of which are members of the Avoidance and numbing domain.
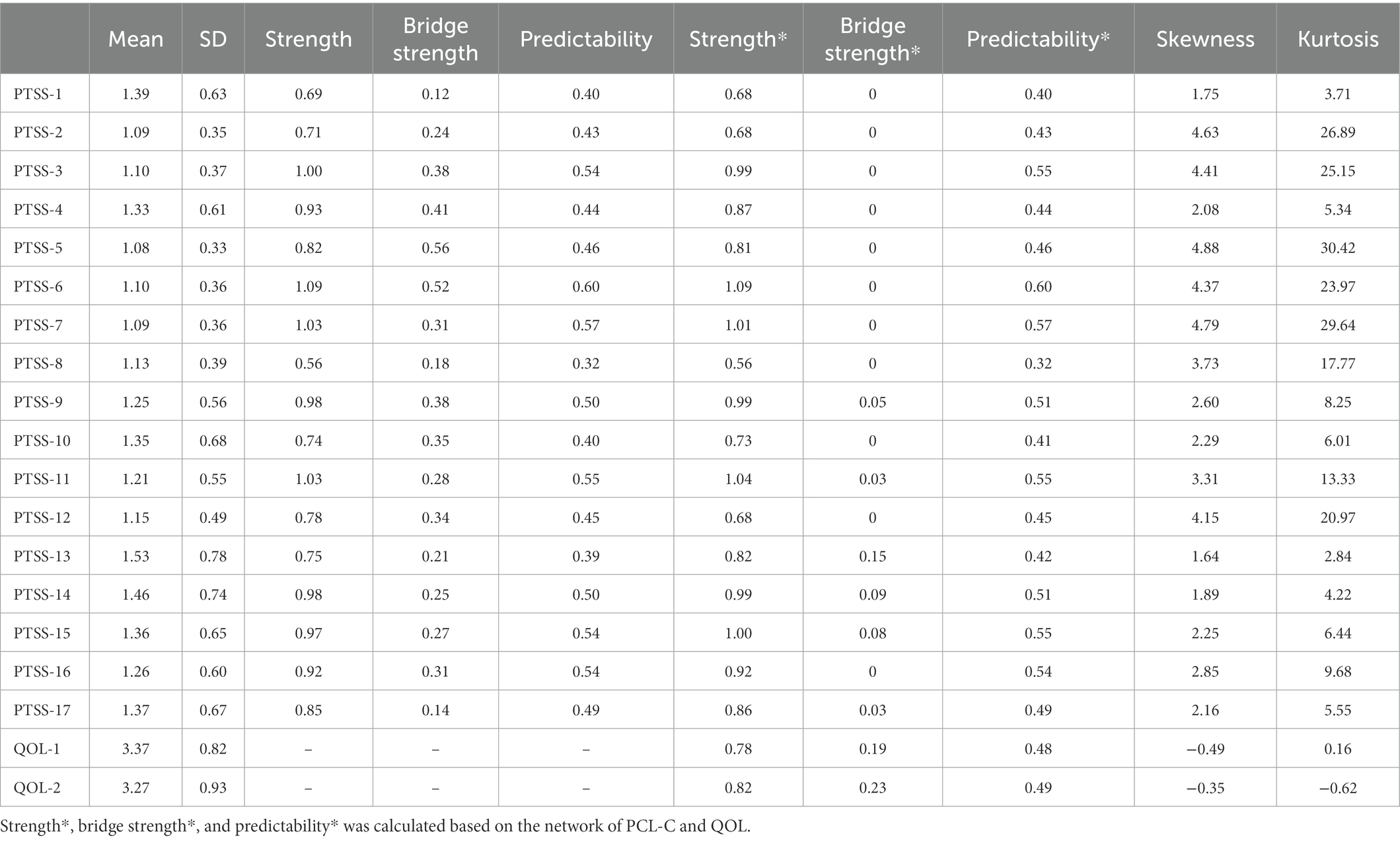
Table 1. Mean, standard deviation, strength, bridge strength, predictability, skewness, and kurtosis of the PCL-C and QOL items (N = 10,516).

Figure 1. Network model of the PCL-C in the whole sample (N = 10,516) estimated by the Extended Bayesian Information Criterion graphical lasso (EBICglasso) method. The size of each node indicates the relative level of strength. Green edges indicate positive associations; red edges indicate negative associations. The values of strength and bridge strength were transformed into z-scores.
The structure of bridge symptoms linking PTSS and QOL is shown in Figure 2. PTSS was negatively associated with QOL. Apart from the two nodes in the QOL cluster, “Sleep disturbances” (PTSS-13), “Irritability” (PTSS-14) and “Difficulty concentrating” (PTSS-15) were the three strongest bridge symptoms connecting PTSS and QOL. Of all interconnections between PTSS and QOL clusters, the edge between “sleep disturbances” and “general health status (QOL-2) had the strongest connection.
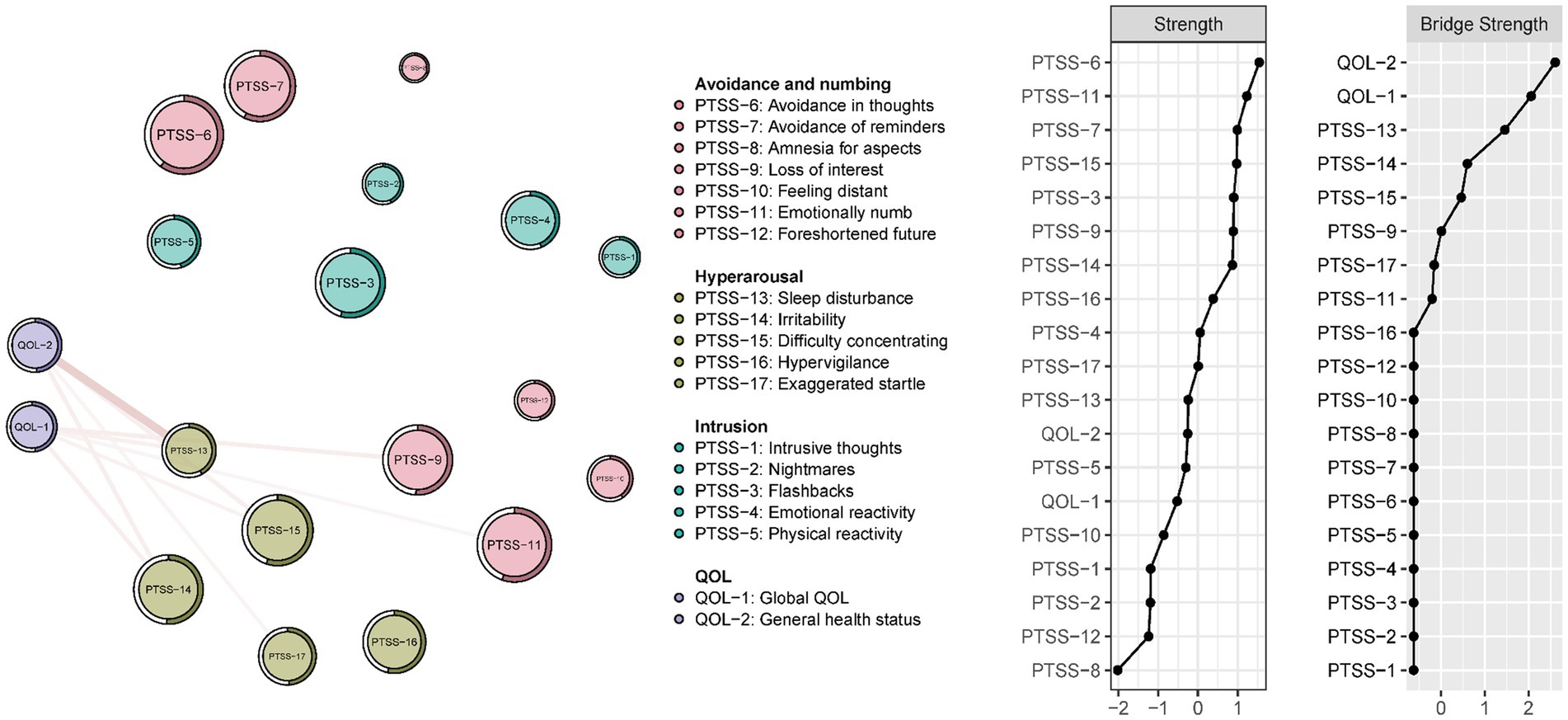
Figure 2. Bridge symptoms between the PCL-C and QOL items in the whole sample (N = 10,516). Green edges indicate positive associations; red edges indicate negative associations. The values of strength and bridge strength were transformed into z-scores.
The directed PTSS-QOL network model is displayed in Figure 3. The most prominent arrows between the two clusters were from PTSS-13, PTSS-14, and PTSS-15 to QOL-1 and QOL-2, paralleling key bridging edges identified in the undirected network. Based on the assumption that PTSS had “influencing” effects on QOL, these results indicated that psychiatric healthcare personnel with severe “Sleep disturbances” (PTSS-13), “Irritability” (PTSS-14) and “Difficulty concentrating” (PTSS-15) had lower QOL compared to healthcare personnel who experienced other PTSS symptoms.
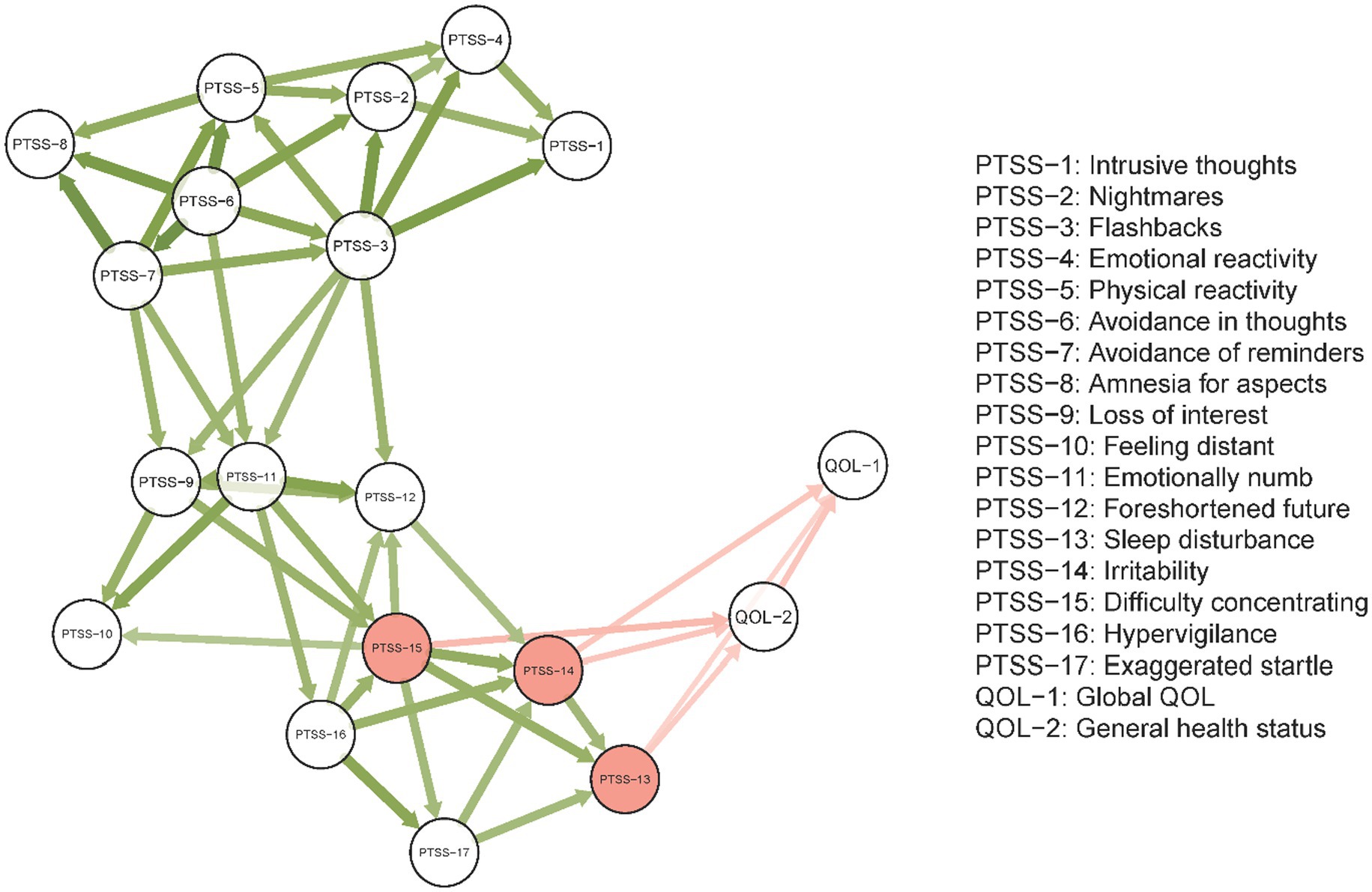
Figure 3. Directed network model of the PCL-C and QOL estimated by the Triangulated Maximally Filtered Graph (TMFG) method. Edge thickness indicates edge weight. Red nodes have the highest bridge strength in the undirected network. Arrows indicate the direction of influence. Defining the two-way influences between node i and node j as D(i, j) and D(j, i), only the greater link between D(i, j) and D(j, i) is retained.
Undirected network models, adjusted for age and sex (confounds hereinafter), are displayed in Figure 4. Visual inspection of these data indicated the network structures and connection patterns were similar before and after adjusting for sex and age. For PCL-C network models, Spearman correlation coefficients between initial (unadjusted) and subsequent (age- and sex-controlled) models for strength and bridge strength were 0.82 and 0.67, respectively (both p values were < 0.001). For the network model comprising PCL-C and QOL, Spearman correlation coefficients between initial (unadjusted) and subsequent (confound-controlled) models for strength and bridge strength were 0.84 and 0.96, respectively (both p values <0.001). These results indicated that age and sex did not have significant confounding effects on the two primary undirected networks.

Figure 4. Network models in the whole sample (N = 10,516) estimated by the Extended Bayesian Information Criterion (EBIC) method after adjusting for age and sex. Network model of PCL-C after adjusting for covariates (left) and network model of PCL-C and QOL after adjusting for covariates (right). The size of each node indicates the relative level of strength. Green edges indicate positive associations; red edges indicate negative associations. For easy comparison with network graphs without adjusting for covariates, the layouts of panels followed the layouts of the two network graphs without adjusting for covariates (Figure 1 and Supplementary Figure S1).
The case-dropping bootstrap procedure showed that the undirected PCL-C network and undirected PCL-C and QOL network values for strength and bridge strength remained stable after randomly dropping 75% of the sample (Supplementary Figure S2). CS-Coefficients for strength and bridge strength in the two networks were both 0.75, indicating that 75% of the sample could be dropped and network structures would remain stable.
To our knowledge, this is the first study to identify the network structure of PTSS and its connections with QOL among psychiatric practitioners during the COVID-19 pandemic. “Avoidance in thoughts” (PTSS-6), “Avoidance of reminders” (PTSS-7), and “Emotionally numb” (PTSS-11) were the three most influential nodes in the network model, all of which are in the Avoidance and numbing domain of PTSS. This finding contrasts with the network structure of COVID-19-related PTSS found in a study of the general population wherein self-destructive/reckless behavior, emotional reactivity and nightmares were central symptoms (40). Inconsistencies between these models are likely due to different study samples (general population vs. psychiatric healthcare personnel) and possible demands upon psychiatric practitioners to serve others and inhibit from overt personal expressions of distress in their professional roles.
Previous studies have found that, apart from comorbid depression, anxiety and social phobia (32, 66), avoidance coping has strong associations with the development of chronic PTSD (67). In this study “Avoidance of thoughts” (PTSS-6) and “Avoidance of reminders” (PTSS-7) had the highest strengths in the network model of PTSS for psychiatric healthcare personnel. “Avoidance of thoughts” refers to avoiding thinking, talking or having feelings about stressful events (e.g., the COVID-19 pandemic), while “Avoidance of reminders” refers to avoiding activities or situations that would remind an individual of a stressful experience (43). Our findings underscored how many psychiatric healthcare personnel tended to cope during the COVID-19 pandemic by disengaging from relevant thoughts/reminders rather than engaging in them (40). These two items had relatively low mean scores but were the top-ranked centrality indices and support the notion that avoidance symptoms are not openly expressed but represent an important diagnostic indicator of PTSD (32, 68). It should be noted that although avoidant coping could provide short-term psychological protection and reduce distress of those affected by traumatic events (66), chronic avoidance over extended durations is considered to be maladaptive and contributes to sustained stress symptoms and impaired post-traumatic recovery (33, 69).
To highlight the importance of avoidance in PTSD symptom clusters, the Diagnostic and Statistical Manual of Mental Disorders - 5th edition (DSM-V) revised previous PTSD diagnostic criteria by separating the avoidance and numbing cluster into two independent clusters (10, 70). The DSM-V requires both avoidance and numbing symptoms for the diagnosis of PTSD (10), and is consistent with concomitant avoidance and numbing symptoms as the most prominent ones in this study.
As another key central symptom in the current network model, “emotional numbing” refers to having remarkably reduced ability to feel emotions (10), especially positive emotions such as tender, affectionate or loving feelings, accompanied by a lack of care or concern for oneself and others (43, 71). A previous study contended that “emotional numbing” is a unique symptom of PTSD that can be used to differentiate PTSD from major depressive disorder (MDD) despite substantial overlaps in symptomatology and comorbidity between these two disorders (72).
The high centrality of “emotional numbing” in the current PTSS network might be due to several factors. Frontline healthcare professionals are vulnerable to occupational burnout and fatigue due to heavy workloads during the pandemic (73, 74). Due to depleted physiological and psychological reserves in managing chronically heavy clinical workloads and possible personal COVID-19-related hyper-arousal symptoms, emotional resources of frontline psychiatric practitioners may become compromised and contribute to emotional numbing (75, 76). Additionally, emotional numbing can result from avoidance of traumatic triggers rather than exposure to traumatic events per se; avoidance of such triggers might lead, not only to reduced exposure to emotional provoking situations, but also to a “shut down” of affective system (75, 77, 78), per the central role of emotional numbing within the network model from this study. Finally, prospective studies have found that emotional numbing is related to increased future risk for the development of PTSD (33, 67) and depression (72).
As expected, bridging edges between PTSS and QOL indicated elevations within the PTSS community were associated with lower QOL, consistent with previous findings (79–81). “Sleep disturbances” (PTSS-13), “Irritability” (PTSS-14) and “Difficulty concentrating” (PTSS-15) were the most important bridging symptoms connecting the PTSS community and QOL in this sample. Sleep disturbances contribute to various negative outcomes such as impaired daily functioning (82), lowered career satisfaction (83) and emotional dysregulation (84), all of which could lower QOL (85, 86). “Irritability” refers to being easily provoked, irritated, or having uncontrolled outbursts of anger (87), and is a symptom in the Hyper-arousal domain of PTSS (10). In previous studies, irritability was associated with impaired QOL (88, 89), in line with our findings. One randomized control trial provided evidence that QOL could be improved through the treatment of irritability among autistic children (90), though extensions warrant consideration in psychiatric professionals. “Difficulty concentrating” implies an individual’s cognitive resources are overwhelmed by demands that exceed cognitive resources and is often accompanied by impairments in daily functioning and work performance (91–93) that could contribute to lower QOL (94, 95).
Strengths of this study included its large sample size of an understudied population (i.e., frontline healthcare workers in early stages of a global pandemic) and the use of network analysis to illuminate inter-relationships between particular PTSS symptoms and QOL. Several limitations should also be noted. First, although the TMFG method generated directional arrows between nodes of PTSS and QOL, associated findings must be interpreted in the context of a non-experimental cross-sectional study design. Directions of influence produced by the TMFG method represented more statistically probable “influencing” and “influenced” relationships among symptoms (54, 55) that provide empirically-grounded yet preliminary hypotheses that need to be tested via experimental studies and/or prospective research designs (96). Second, because only psychiatric practitioners were included, findings may not be generalized to related populations such as general health practitioners. Third, for logistical reasons, the mental health status of participants prior to the COVID-19 outbreak was not assessed so the presence and impact of pre-COVID-19 emotional problems on current PTSS and QoL could not be examined. Fourth, due to strictly enforced safety protocols in early stages of COVID-19 pandemic, assessments were limited to validated measures of PTSS and QOL rather in-person examination via structured clinical interviews. Fifth, following other studies conducted during the COVID-19 pandemic (74, 97), for logistical reasons, convenience sampling was used in this study. Hence, selection biases may have affected the data. Furthermore, most of the participants (84.5%) were women. This aligns with the actual gender distribution among healthcare personnel in China. For example, 74.4% of healthcare personnel in China during 2020 were female (98). Nonetheless, the proportion of women in our sample exceeded this national estimate. Finally, because there was no control sample in this study, comparisons of psychiatric healthcare professionals with responses from the general population could not be made.
In conclusion, among psychiatric healthcare professionals working during early stages of the COVID-19 pandemic, central PTSS included “Avoidance of thoughts” “Avoidance of reminders” and “Emotional numbness.” In addition, key bridge symptoms linking PTSS with QOL in this group included hyper-arousal domain facets, “Sleep disturbances,” “Irritability” and “Difficulty concentrating.” Based on these findings, this study suggests that PTSS symptoms of avoidance and hyper-arousal should be monitored among psychiatric healthcare professionals during the pandemic and serve as potentially important targets for prevention and treatment for those with PTSS in these circumstances.
The datasets presented in this article are not readily available because the Institutional Review Board (IRB) of Beijing Anding Hospital that approved the study prohibits the authors from making publicly available the research dataset of clinical studies. Requests to access the datasets should be directed to eHl1dGx5QGdtYWlsLmNvbQ==.
The studies involving human participants were reviewed and approved by the Institutional Review Board (IRB), Beijing Anding Hospital. The patients/participants provided their electronic written informed consent to participate in this study.
F-RA and Y-TX: study design. Y-JZ, CZ, TG, SS, ZS, and F-RA: data collection, analysis, and interpretation. Y-JZ and Y-TX: drafting of the manuscript. TJ: critical revision of the manuscript. All authors: approval of the final version for publication.
This study was supported by the Beijing Anding Hospital, Capital Medical University (No. KY296), Beijing Municipal Science and Technology Commission (Grant No. Z181100001718124), Beijing Talents Foundation (Grant No. 2017000021469G222), University of Macau (No. MYRG2019-00066-FHS), Scientific Research Common Program of Beijing Municipal Commission of Education (No. KM202010025011), and Beijing Municipal Science and Tech Commission (No. Z191100006619061).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.975443/full#supplementary-material
1. World Health Organization. WHO director-general's opening remarks at the media briefing on COVID-19 - 11 march 2020. (2020c) Available at: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.
2. Johns Hopkins University. COVID-19 dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). (2020) Available at: https://coronavirus.jhu.edu/map.html.
3. World Health Organization. COVID-19 - China. (2020a) Available at: https://www.who.int/emergencies/disease-outbreak-news/item/2020-DON233.
4. World Health Organization. Naming the coronavirus disease (COVID-19) and the virus that causes it. (2020b) Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it.
5. Chinese Center for Disease Control and Prevention. The latest situation of the COVID-19 pandemic in China as of 24:00 on December 31, 2022 (in Chinese). (2022) Available at: https://www.chinacdc.cn/jkzt/crb/zl/szkb_11803/jszl_11809/202301/t20230101_263164.html.
6. Gu, Y, Zhu, Y, Xu, F, Xi, J, and Xu, G. Factors associated with mental health outcomes among patients with COVID-19 treated in the Fangcang shelter hospital in China. Asia Pac Psychiatry. (2021) 13:e12443. doi: 10.1111/appy.12443
7. Pan, X, Xiao, Y, Ren, D, Xu, ZM, Zhang, Q, Yang, LY, et al. Prevalence of mental health problems and associated risk factors among military healthcare workers in specialized COVID-19 hospitals in Wuhan, China: a cross-sectional survey. Asia Pac Psychiatry. (2022) 14:e12427. doi: 10.1111/appy.12427
8. Venugopal, VC, Mohan, A, and Chennabasappa, LK. Status of mental health and its associated factors among the general populace of India during COVID-19 pandemic. Asia Pac Psychiatry. (2022) 14:e12412. doi: 10.1111/appy.12412
9. Zhao, YJ, Jin, Y, Rao, WW, Li, W, Zhao, N, Cheung, T, et al. The prevalence of psychiatric comorbidities during the SARS and COVID-19 epidemics: a systematic review and meta-analysis of observational studies. J Affect Disord. (2021) 287:145–57. doi: 10.1016/j.jad.2021.03.016
10. American Psychiatric Association Diagnostic and statistical manual of mental disorders. (2013) 5th ed. Arlington, VA: American Psychiatric Publishing doi: 10.1176/appi.books.9780890425596.
11. Mayo Clinic. Post-traumatic stress disorder (PTSD) - Symptoms and causes. (2018). Available at: https://www.mayoclinic.org/diseases-conditions/post-traumatic-stress-disorder/symptoms-causes/syc-20355967
12. Toshishige, Y, Kondo, M, and Akechi, T. Interpersonal psychotherapy for complex posttraumatic stress disorder related to childhood physical and emotional abuse with great severity of depression: a case report. Asia Pac Psychiatry. (2022) 14:e12504. doi: 10.1111/appy.12504
13. National Institute of Mental Health. Post-Traumatic Stress Disorder. (2019). Available at: https://www.nimh.nih.gov/health/topics/post-traumatic-stress-disorder-ptsd
14. Johansen, VA, Wahl, AK, Eilertsen, DE, Weisaeth, L, and Hanestad, BR. The predictive value of post-traumatic stress disorder symptoms for quality of life: a longitudinal study of physically injured victims of non-domestic violence. Health Qual Life Outcomes. (2007) 5:26. doi: 10.1186/1477-7525-5-26
15. Johnsen, BH, Eid, J, Laberg, JC, and Thayer, JF. The effect of sensitization and coping style on post-traumatic stress symptoms and quality of life: two longitudinal studies. Scand J Psychol. (2002) 43:181–8. doi: 10.1111/1467-9450.00285
16. O'Donnell, ML, Creamer, M, Bryant, RA, Schnyder, U, and Shalev, A. Posttraumatic disorders following injury: an empirical and methodological review. Clin Psychol Rev. (2003) 23:587–603. doi: 10.1016/S0272-7358(03)00036-9
17. Wang, L, Cao, C, Wang, R, Zhang, J, and Li, Z. The dimensionality of PTSD symptoms and their relationship to health-related quality of life in Chinese earthquake survivors. J Anxiety Disord. (2012a) 26:711–8. doi: 10.1016/j.janxdis.2012.06.005
18. Al Falasi, B, Al Mazrouei, M, Al Ali, M, Al Dhamani, M, Al Ali, A, Al Kindi, M, et al. Prevalence and determinants of immediate and long-term PTSD consequences of coronavirus-related (CoV-1 and CoV-2) pandemics among healthcare professionals: a systematic review and meta-analysis. Int J Environ Res Public Health. (2021) 18:2182. doi: 10.3390/ijerph18042182
19. Ilias, I, Mantziou, V, Vamvakas, E, Kampisiouli, E, Theodorakopoulou, M, Vrettou, C, et al. Post-traumatic stress disorder and burnout in healthcare professionals during the SARS-CoV-2 pandemic: a cross-sectional study. J Crit Care Med. (2021) 7:14–20. doi: 10.2478/jccm-2020-0042
20. Lau, JT, Yang, X, Tsui, HY, Pang, E, and Wing, YK. Positive mental health-related impacts of the SARS epidemic on the general public in Hong Kong and their associations with other negative impacts. J Infect. (2006) 53:114–24. doi: 10.1016/j.jinf.2005.10.019
21. Sim, K, Huak Chan, Y, Chong, PN, Chua, HC, and Wen Soon, S. Psychosocial and coping responses within the community health care setting toward a national outbreak of an infectious disease. J Psychosom Res. (2010) 68:195–202. doi: 10.1016/j.jpsychores.2009.04.004
22. d'Ettorre, G, Ceccarelli, G, Santinelli, L, Vassalini, P, Innocenti, GP, Alessandri, F, et al. Post-traumatic stress symptoms in healthcare workers dealing with the COVID-19 pandemic: a systematic review. Int J Environ Res Public Health. (2021) 18:601. doi: 10.3390/ijerph18020601
23. Dixit, S, Musa, A, Sillva, AB, Reddy, RS, Abohashrh, M, Kakaraparthi, VN, et al. The impact of post-traumatic stress of SARS-CoV-2 affliction on psychological and mental health of student survivors: cross sectional study. Front Public Health. (2022) 10:845741
24. Giusti, L, Salza, A, Mammarella, S, Bianco, D, Ussorio, D, Casacchia, M, et al. #everything will be fine. Duration of home confinement and "all-or-nothing" cognitive thinking style as predictors of traumatic distress in young university students on a digital platform during the COVID-19 Italian lockdown. Front Psych. (2020) 11:574812. doi: 10.3389/fpsyt.2020.574812
25. Nantaayi, B, Ndawula, RK, Musoke, P, Ssewante, N, Nakyagaba, L, Wamala, JN, et al. Psychological distress and access to mental health services among undergraduate students during the COVID-19 lockdown in Uganda. Front Psych. (2022) 13:792217. doi: 10.3389/fpsyt.2022.792217
26. China News Weekly. Hospital-acquired infection in Wuhan mental health center: Around 80 medical staff and patients were diagnosed with (2019)-nCoV pneumonia (in Chinese). (2020) Available at: https://news.sina.com.cn/c/2020-02-08/doc-iimxxste9892538.shtml.
27. National Health Commission of China. 323 patients with severe mental disorders were diagnosed with new coronary pneumonia (in Chinese). (2020). Available at: http://www.bjnews.com.cn/news/2020/02/18/691444.html
28. Xiang, YT, Zhao, YJ, Liu, ZH, Li, XH, Zhao, N, Cheung, T, et al. The COVID-19 outbreak and psychiatric hospitals in China: managing challenges through mental health service reform. Int J Biol Sci. (2020b) 16:1741–4. doi: 10.7150/ijbs.45072
29. Xiang, YT, Zhao, N, Zhao, YJ, Liu, Z, Zhang, Q, Feng, Y, et al. An overview of the expert consensus on the mental health treatment and services for major psychiatric disorders during COVID-19 outbreak: China's experiences. Int J Biol Sci. (2020a) 16:2265–70. doi: 10.7150/ijbs.47419
30. Everett, B. An introduction to latent variable models. (2013) New York, NY: Springer Science & Business Media.
31. Schmittmann, VD, Cramer, AO, Waldorp, LJ, Epskamp, S, Kievit, RA, and Borsboom, D. Deconstructing the construct: a network perspective on psychological phenomena. New Ideas Psychol. (2013) 31:43–53. doi: 10.1016/j.newideapsych.2011.02.007
32. McMillen, JC, North, CS, and Smith, EM. What parts of PTSD are normal: intrusion, avoidance, or arousal? Data from the Northridge, California, earthquake. J Trauma Stress. (2000) 13:57–75. doi: 10.1023/A:1007768830246
33. Tull, MT, and Roemer, L. Alternative explanations of emotional numbing of posttraumatic stress disorder: An examination of hyperarousal and experiential avoidance. J Psychopathol Behav Assess. (2003) 25:147–54. doi: 10.1023/A:1023568822462
35. Mullarkey, MC, Marchetti, I, and Beevers, CG. Using network analysis to identify central symptoms of adolescent depression. J Clin Child Adolesc Psychol. (2019) 48:656–68. doi: 10.1080/15374416.2018.1437735
36. Borsboom, D, and Cramer, AO. Network analysis: an integrative approach to the structure of psychopathology. Annu Rev Clin Psychol. (2013) 9:91–121. doi: 10.1146/annurev-clinpsy-050212-185608
37. Borsboom, D. A network theory of mental disorders. World Psychiatry. (2017) 16:5–13. doi: 10.1002/wps.20375
38. Cramer, AO, van Borkulo, CD, Giltay, EJ, van der Maas, HL, Kendler, KS, Scheffer, M, et al. Major depression as a complex dynamic system. PLoS One. (2016) 11:e0167490. doi: 10.1371/journal.pone.0167490
39. Cramer, AO, Waldorp, LJ, Van Der Maas, HL, and Borsboom, D. Comorbidity: a network perspective. Behav Brain Sci. (2010) 33:137–50. doi: 10.1017/S0140525X09991567
40. Jiang, W, Ren, Z, Yu, L, Tan, Y, and Shi, C. A network analysis of post-traumatic stress disorder symptoms and correlates during the COVID-19 pandemic. Front Psych. (2020) 11:568037. doi: 10.3389/fpsyt.2020.568037
41. Zavlis, O, Butter, S, Bennett, K, Hartman, TK, Hyland, P, Mason, L, et al. How does the COVID-19 pandemic impact on population mental health? A network analysis of COVID influences on depression, anxiety and traumatic stress in the UK population. Psychol Med. (2021) 16:1–9. doi: 10.1017/S0033291721000635
42. China Academy of Information and Communications Technology. WeChat employment impact report 2019–2020 (in Chinese). (2020) Available at: http://www.caict.ac.cn/kxyj/qwfb/ztbg/202005/t20200514_281774.htm.
43. Conybeare, D, Behar, E, Solomon, A, Newman, MG, and Borkovec, TD. The PTSD checklist-civilian version: reliability, validity, and factor structure in a nonclinical sample. J Clin Psychol. (2012) 68:699–713. doi: 10.1002/jclp.21845
44. Weathers, F., Litz, B., and Herman, D. The PTSD checklist: Reliability, validity and diagnostic utility, (1993) Annual meeting of the International Society for Traumatic Stress Studies, San antonio, TX.
45. Yang, X-Y, Yang, H-A, Liu, Q-G, and Yang, L-Z. Reliability, validity and influence factors of PCL-C (in Chinese) In:. Annual conference of Chinese psychological society. (2006) Guangzhou, China. 158.
46. Wang, M-C, Sui, S-G, Li, J-H, and Dai, X-Y. Psychometric properties of the PTSD checklist-civilian version among junior school students from earthquake-hit region (in Chinese). Chin J Behav Med Brain Sci. (2010) 19:566–8.
47. Wang, X-M, Liu, J, Wang, Q, and Yang, Y-P. The revision of PCL-C Chinese version and its preliminary application in cancer inpatient (in Chinese) In:. The third seminar for young and middle-aged mental health scholars of Chinese mental health association. (2012b) Nantong, Jiangsu. 5.
48. Fang, J-Q, Hao, Y-T, and Li, C-X. Reliability and validity for Chinese version of WHO quality of life scale (in Chinese). Chin J Mental Health. (1999) 13:203–5.
49. The WHOQOL GROUP Development of the World Health Organization WHOQOL-BREF quality of life assessment. WHOQOL Group Psychol Med. (1998) 28:551–8. doi: 10.1017/S0033291798006667
50. Epskamp, S, and Fried, EI. A tutorial on regularized partial correlation networks. Psychol Methods. (2018) 23:617–34. doi: 10.1037/met0000167
51. Garabiles, MR, Lao, CK, Xiong, Y, and Hall, BJ. Exploring comorbidity between anxiety and depression among migrant Filipino domestic workers: a network approach. J Affect Disord. (2019) 250:85–93. doi: 10.1016/j.jad.2019.02.062
53. Christensen, AP. NetworkToolbox: methods and measures for brain, cognitive, and psychometric network analysis in R. R J. (2018) 10:422–39.
54. Massara, GP, Di Matteo, T, and Aste, T. Network filtering for big data: triangulated maximally filtered graph. J Comp Netw. (2017) 5:161–78.
55. Jacob, Y., Winetraub, Y., Raz, G., Ben-Simon, E., Okon-Singer, H., Rosenberg-Katz, K., et al. Dependency network analysis (D(EP)NA) reveals context related influence of brain network nodes. (2016) Scientific Reports 6.
56. Kenett, DY, Tumminello, M, Madi, A, Gur-Gershgoren, G, Mantegna, RN, and Ben-Jacob, E. Dominating clasp of the financial sector revealed by partial correlation analysis of the stock market. PLoS One. (2010) 5:e15032. doi: 10.1371/journal.pone.0015032
57. Chernick, MR. Bootstrap methods: A guide for practitioners and researchers. (2011) Hoboken, NJ: John Wiley & Sons.
58. Costenbader, E, and Valente, TW. The stability of centrality measures when networks are sampled. Soc Netw. (2003) 25:283–307. doi: 10.1016/S0378-8733(03)00012-1
59. Epskamp, S, Borsboom, D, and Fried, EI. Estimating psychological networks and their accuracy: a tutorial paper. Behav Res Methods. (2018) 50:195–212. doi: 10.3758/s13428-017-0862-1
60. Dalege, J, Borsboom, D, van Harreveld, F, and van der Maas, HLJ. Network analysis on attitudes: a brief tutorial. Soc Psychol Personal Sci. (2017) 8:528–37. doi: 10.1177/1948550617709827
61. R Core Team. R: A language and environment for statistical computing. (2020). Available at: https://www.R-project.org
62. Jones, P. Network tools: Tools for identifying important nodes in networks, R package version 1.2.3. (2020). Available at: https://CRAN.R-project.org/package=networktools
63. Revelle, W. Psych: Procedures for psychological, psychometric, and personality research. R package version 2.0.9. (2020). Available at: https://CRAN.R-project.org/package=psych
64. Haslbeck, J, and Waldorp, LJ. Mgm: estimating time-varying mixed graphical models in high-dimensional data. J Stat Softw. (2020) 93:1–46. doi: 10.18637/jss.v093.i08
65. Epskamp, S, Cramer, AO, Waldorp, LJ, Schmittmann, VD, and Borsboom, D. Qgraph: network visualizations of relationships in psychometric data. J Stat Softw. (2012) 48:1–18. doi: 10.18637/jss.v048.i04
66. Chawla, N, and Ostafin, B. Experiential avoidance as a functional dimensional approach to psychopathology: an empirical review. J Clin Psychol. (2007) 63:871–90. doi: 10.1002/jclp.20400
67. Feuer, CA, Nishith, P, and Resick, P. Prediction of numbing and effortful avoidance in female rape survivors with chronic PTSD. J Trauma Stress. (2005) 18:165–70. doi: 10.1002/jts.20000
68. Silverman, W.K., and La Greca, A.M. Children experiencing disasters: Definitions, reactions, and predictors of outcomes. (2002).
69. Brooks, M, Graham-Kevan, N, Robinson, S, and Lowe, M. Trauma characteristics and posttraumatic growth: the mediating role of avoidance coping, intrusive thoughts, and social support. Psychol Trauma. (2019) 11:232–8. doi: 10.1037/tra0000372
70. Forbes, D, Fletcher, S, Lockwood, E, O'Donnell, M, Creamer, M, Bryant, RA, et al. Requiring both avoidance and emotional numbing in DSM-V PTSD: will it help? J Affect Disord. (2011) 130:483–6. doi: 10.1016/j.jad.2010.10.032
71. Glover, H. Emotional numbing: a possible endorphin-mediated phenomenon associated with post-traumatic stress disorders and other allied psychopathologic states. J Trauma Stress. (1992) 5:643–75. doi: 10.1002/jts.2490050413
72. Kashdan, TB, Elhai, JD, and Frueh, BC. Anhedonia and emotional numbing in combat veterans with PTSD. Behav Res Ther. (2006) 44:457–67. doi: 10.1016/j.brat.2005.03.001
73. Franza, F, Basta, R, Pellegrino, F, Solomita, B, and Fasano, V. The role of fatigue of compassion, burnout and hopelessness in healthcare: experience in the time of COVID-19 outbreak. Psychiatr Danub. (2020) 32:10–4.
74. Jin, Y, Li, Y, Li, XY, Zhao, YJ, Cheung, T, Ungvari, GS, et al. Prevalence of fatigue and its association with quality of life among frontline clinicians in ophthalmology and otolaryngology departments during the COVID-19 pandemic. Front Psych. (2021) 12:678917. doi: 10.3389/fpsyt.2021.678917
75. Badura, AS. Theoretical and empirical exploration of the similarities between emotional numbing in posttraumatic stress disorder and alexithymia. J Anxiety Disord. (2003) 17:349–60. doi: 10.1016/S0887-6185(02)00201-3
76. Weems, CF, Saltzman, KM, Reiss, AL, and Carrion, VG. A prospective test of the association between hyperarousal and emotional numbing in youth with a history of traumatic stress. J Clin Child Adolesc Psychol. (2003) 32:166–71. doi: 10.1207/S15374424JCCP3201_15
77. Feeny, NC, Zoellner, LA, Fitzgibbons, LA, and Foa, EB. Exploring the roles of emotional numbing, depression, and dissociation in PTSD. J Trauma Stress. (2000) 13:489–98. doi: 10.1023/A:1007789409330
78. Litz, BT, and Gray, MJ. Emotional numbing in posttraumatic stress disorder: current and future research directions. Aust N Z J Psychiatry. (2002) 36:198–204. doi: 10.1046/j.1440-1614.2002.01002.x
79. Bonichini, S, and Tremolada, M. Quality of life and symptoms of PTSD during the COVID-19 lockdown in Italy. Int J Environ Res Public Health. (2021) 18:4385. doi: 10.3390/ijerph18084385
80. Mahmoudi, H, Saffari, M, Movahedi, M, Sanaeinasab, H, Rashidi-Jahan, H, Pourgholami, M, et al. A mediating role for mental health in associations between COVID-19-related self-stigma, PTSD, quality of life, and insomnia among patients recovered from COVID-19. Brain Behav. (2021) 11:e02138. doi: 10.1002/brb3.2138
81. Méndez, R, Balanzá-Martínez, V, Luperdi, SC, Estrada, I, Latorre, A, González-Jiménez, P, et al. Short-term neuropsychiatric outcomes and quality of life in COVID-19 survivors. J Intern Med. (2021) 290:621–31. doi: 10.1111/joim.13262
82. Rahimi, A, Ahmadpanah, M, Shamsaei, F, Cheraghi, F, Sadeghi Bahmani, D, Holsboer-Trachsler, E, et al. Effect of adjuvant sleep hygiene psychoeducation and lorazepam on depression and sleep quality in patients with major depressive disorders: results from a randomized three-arm intervention. Neuropsychiatr Dis Treat. (2016) 12:1507–15. doi: 10.2147/NDT.S110978
83. Karagozoglu, S, and Bingöl, N. Sleep quality and job satisfaction of Turkish nurses. Nurs Outlook. (2008) 56:298–307.e3. doi: 10.1016/j.outlook.2008.03.009
84. Lee, CY, Chen, HC, Meg Tseng, MC, Lee, HC, and Huang, LH. The relationships among sleep quality and Chronotype, emotional disturbance, and insomnia vulnerability in shift nurses. J Nurs Res. (2015) 23:225–35. doi: 10.1097/jnr.0000000000000095
85. Cimete, G, Gencalp, NS, and Keskin, G. Quality of life and job satisfaction of nurses. J Nurs Care Qual. (2003) 18:151–8. doi: 10.1097/00001786-200304000-00009
86. Ibrahim, NK, Alzahrani, NA, Batwie, AA, Abushal, RA, Almogati, GG, Sattam, MA, et al. Quality of life, job satisfaction and their related factors among nurses working in king Abdulaziz university hospital, Jeddah. Saudi Arabia Contemp Nurse. (2016) 52:486–98. doi: 10.1080/10376178.2016.1224123
87. Vidal-Ribas, P, Brotman, MA, Valdivieso, I, Leibenluft, E, and Stringaris, A. The status of irritability in psychiatry: a conceptual and quantitative review. J Am Acad Child Adolesc Psychiatry. (2016) 55:556–70. doi: 10.1016/j.jaac.2016.04.014
88. Jha, MK, Schatzberg, A, Minhajuddin, A, Chin Fatt, C, Mayes, TL, and Trivedi, MH. Cross-sectional associations among symptoms of pain, irritability, and depression and how these symptoms relate to social functioning and quality of life: findings from the EMBARC and STRIDE studies and the VitalSign6 project. J Clin Psychiatry. (2021) 82:3740. doi: 10.4088/JCP.20m13740
89. Perlis, RH, Fava, M, Trivedi, MH, Alpert, J, Luther, JF, Wisniewski, SR, et al. Irritability is associated with anxiety and greater severity, but not bipolar spectrum features, in major depressive disorder. Acta Psychiatr Scand. (2009) 119:282–9. doi: 10.1111/j.1600-0447.2008.01298.x
90. Varni, JW, Handen, BL, Corey-Lisle, PK, Guo, Z, Manos, G, Ammerman, DK, et al. Effect of aripiprazole 2 to 15 mg/d on health-related quality of life in the treatment of irritability associated with autistic disorder in children: a post hoc analysis of two controlled trials. Clin Ther. (2012) 34:980–92. doi: 10.1016/j.clinthera.2012.02.023
91. Buckley, TC, Blanchard, EB, and Hickling, EJ. A confirmatory factor analysis of posttraumatic stress symptoms. Behav Res Ther. (1998) 36:1091–9. doi: 10.1016/S0005-7967(98)00076-X
92. McWilliams, LA, Cox, BJ, and Asmundson, GJ. Symptom structure of posttraumatic stress disorder in a nationally representative sample. J Anxiety Disord. (2005) 19:626–41. doi: 10.1016/j.janxdis.2004.06.003
93. Pietrzak, RH, Tsai, J, Harpaz-Rotem, I, Whealin, JM, and Southwick, SM. Support for a novel five-factor model of posttraumatic stress symptoms in three independent samples of Iraq/Afghanistan veterans: a confirmatory factor analytic study. J Psychiatr Res. (2012) 46:317–22. doi: 10.1016/j.jpsychires.2011.11.013
94. D'Amico, D, Usai, S, Grazzi, L, Rigamonti, A, Solari, A, Leone, M, et al. Quality of life and disability in primary chronic daily headaches. Neurol Sci. (2003) 24:S97–S100. doi: 10.1007/s100720300052
95. Kyle, SD, Espie, CA, and Morgan, K. Not just a minor thing, it is something major, which stops you from functioning daily: quality of life and daytime functioning in insomnia. Behav Sleep Med. (2010) 8:123–40. doi: 10.1080/15402002.2010.487450
96. Jones, PJ, Mair, P, Riemann, BC, Mugno, BL, and McNally, RJ. A network perspective on comorbid depression in adolescents with obsessive-compulsive disorder. J Anxiety Disord. (2018) 53:1–8. doi: 10.1016/j.janxdis.2017.09.008
97. An, Y, Yang, Y, Wang, A, Li, Y, Zhang, Q, Cheung, T, et al. Prevalence of depression and its impact on quality of life among frontline nurses in emergency departments during the COVID-19 outbreak. J Affect Disord. (2020) 276:312–5. doi: 10.1016/j.jad.2020.06.047
Keywords: post-traumatic stress symptoms, quality of life, psychiatric healthcare personnel, COVID-19 pandemic, network
Citation: Zhao Y-J, Zhang C, Guo T, Sha S, Su Z, Cheung T, Jackson T, An F-R and Xiang Y-T (2023) Associations between post-traumatic stress symptoms and quality of life among psychiatric healthcare personnel in China during the COVID-19 pandemic: A network approach. Front. Psychiatry. 14:975443. doi: 10.3389/fpsyt.2023.975443
Received: 22 June 2022; Accepted: 10 January 2023;
Published: 15 February 2023.
Edited by:
Rita Roncone, University of L'Aquila, ItalyReviewed by:
Laura Giusti, University of L'Aquila, ItalyCopyright © 2023 Zhao, Zhang, Guo, Sha, Su, Cheung, Jackson, An and Xiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Feng-Rong An, ✉ YWZyeWxtQHNpbmEuY29t; Yu-Tao Xiang, ✉ eHl1dGx5QGdtYWlsLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.