
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 04 December 2023
Sec. Schizophrenia
Volume 14 - 2023 | https://doi.org/10.3389/fpsyt.2023.1321233
 Ginevra Lombardozzi1*
Ginevra Lombardozzi1* Giada Trovini1
Giada Trovini1 Emanuela Amici1
Emanuela Amici1 Georgios D. Kotzalidis1,2,3,4*
Georgios D. Kotzalidis1,2,3,4* Filippo Perrini5
Filippo Perrini5 Valeria Giovanetti1
Valeria Giovanetti1 Alessandro Di Giovanni1
Alessandro Di Giovanni1 Sergio De Filippis1
Sergio De Filippis1Background: Partial dopamine D2 receptor agonists are used for psychotic symptoms in adults with schizophrenia spectrum disorders. Recently, interest surged for partial dopamine D2 receptor agonists in substance use disorders (SUDs). Since it is believed that SUDs decrease the efficacy of pharmacotherapy of underlying psychiatric disorders, we tested the efficacy of the partial D2 agonist brexpiprazole in patients with schizophrenia who were either comorbid with a SUD (SUD group) or not comorbid (non-SUD) to assess treatment response and the effect of brexpiprazole on substance craving in SUD.
Methods: We included patients with DSM-5/DSM-5-TR schizophrenia (using SCID-5-CV) aged 18–66 years with either comorbid SUD or non-SUD to treat with brexpiprazole 4 mg/day for 6 months during February–October 2022. Patients were assessed with the Clinical Global Impressions–Severity (CGI-S) scale, the 24-item Brief Psychiatric Rating Scale (BPRS), and the Positive And Negative Syndrome Scale (PANSS) at baseline, weekly for the first 2 months and monthly for the next four. Furthermore, we assessed substance craving in SUD with a visual analog scale for craving (VAScrav) at the same timepoints.
Results: The total sample was 86 (85 analysable) 18- to 64-year-old (mean 39.32 ± 14.09) patients with schizophrenia [51 men (59.3%) and 35 women (40.7%)], of whom 48 SUD (55.8%) (37 men and 11 women) and 38 non-SUD (44.2%) (14 men and 24 women). No serious or persistent adverse events developed over the study period, but one patient dropped out for subjective akathisia. Results indicated the main effects of time with improvements over the course of the study for CGI-S, BPRS, and PANSS in both SUD and non-SUD groups and the entire sample, and for VAScrav in SUD. Brexpiprazole was associated with similar significant improvements in both groups at the 6 month endpoint compared to baseline.
Conclusion: Treatment with brexpiprazole for 6 months improved psychotic symptoms in patients with schizophrenia, independently from whether they belonged to the SUD or the non-SUD group; hence, SUD comorbidity did not confer treatment resistance to brexpiprazole. Furthermore, in the SUD group, we observed reduced substance craving.
Schizophrenia is a severe mental disorder with a pooled annual incidence of 15 per 100,000 people (1). It is a chronic condition that has huge health, social, and economic impacts on patients, their families and caregivers, and on the entire society; it ranked 20th among the leading causes of disability in 2019 (1). Its treatment is still unsatisfactory and is the focus of debate, with newly proposed drugs based on recent developments in the pathophysiology of the disorder (2–4) going beyond the classical dopaminergic hypothesis.
A few months passed since the first report of environmental indifference induced by chlorpromazine (5), which prompted Henri Laborit to advise Delay and Deniker (6) to use the drug in psychiatric patients and to report the efficacy of chlorpromazine in purported schizophrenia cases (7) and in manic agitation (8). From that time until the first rudimentary draft of the dopaminergic theory (9), 11 years elapsed, and a further 3 years were required until its accomplished formulation (10). In the meantime, phenothiazines were considered antihistaminics that failed to induce adequate analgesia, and all antipsychotic drugs produced in these years were variations of methylene blue and chlorpromazine structures. The discovery of the butyrophenone haloperidol also followed a serendipitous path, with the young chemist Bert K. F. Hermans synthesizing the drug on 11 February 1958 at Janssen (11), while Paul A.J. Janssen's group was playing around with the structure of pethidine in an attempt to discover stronger pain killers (12); the discoverers published their results 1 year later (13), but had already passed the molecule to Divry et al. (14, 15) and Paquay et al. (16), who performed the first encouraging clinical trials, something that would not have been feasible in current years for ethical reasons. At these times, the dopamine receptor was unknown to the scientific community, and dopamine was considered to be only a noradrenaline precursor. Carlsson et al. (17, 18) identified dopamine as an independent transmitter in the brain in the late 1950s. Seven more years were still needed to formulate a form of the dopaminergic hypothesis for schizophrenia that posed hyperdopaminergia as the pathological basis of schizophrenia (10). The theory underwent various modifications, with additions, specifications, and enrichment concerning other transmitters and modulators, such as glutamate, γ-aminobutyric acid (GABA), serotonin (5-hydroxytryptamine, 5-HT), acetylcholine, endorphins, other peptides, and adenosine, but the idea that increased mesolimbic dopaminergic activity linked to the development of schizophrenia was never disproved and all adjunctive mechanisms had to fit this idea, as drugs without mesolimbic antidopaminergic (direct or indirect) activity are ineffective. It was hypothesized that abnormally developing dopaminergic projections to the prefrontal cortex affected GABAergic and glutamatergic transmissions in the dorsolateral prefrontal cortex (DLPFC) and its feedback to the mesolimbic dopaminergic system (19). Realizing that dopaminergic activity in the prefrontal cerebral cortex was hypoactive and in the mesolimbic system was hyperactive led to the development of drugs that could slow the activity of dopamine in the mesolimbic system, as all neuroleptics and antipsychotics do, but enhance it in the DLPFC (20), which is the seat of executive functions that help individuals to deal with the tasks of everyday life. These drugs are able, through partial agonist activity on the D2 group of receptors (D2, D3, and D4), to increase dopaminergic activity in the DLPFC and by increasing the dose to block dopaminergic receptors in the mesolimbic system. Simultaneously, they block 5-HT2A (and 5-HT6 and 5-HT7) receptors (21) and partially activate 5-HT1A receptors (22). Hence, the properties of the “atypical” or “second generation” antipsychotics apply to these molecules. This group of drugs comprises aripiprazole, cariprazine, and brexpiprazole, which have shown comparable effectiveness in schizophrenia studies, although each maintains its own unique profile (23). In particular, brexpiprazole is more potent at the 5-HT7 receptors than the other two drugs (Supplementary Table 1). Inhibiting the 5-HT7 receptor has been associated with positive cognitive effects (24, 25), which are essential for recovery from schizophrenia (26).
Currently, there are more than 20 pharmacotherapeutic options to treat schizophrenia symptoms (27, 28) and some focus on non-dopaminergic mechanisms (29), although these mechanisms ultimately affect dopaminergic transmission (30). When choosing a prescription, clinicians should balance efficacy with safety and adverse events. The latter may impair the patient's quality of life (QoL) and lead to treatment discontinuation (31, 32). This, in turn, may be followed by symptom exacerbation, which is the main reason for subsequent hospitalization (33). Hospitalization, besides constituting a traumatic event in a psychiatric patient's life (34), is also related to increasing healthcare costs and social burdens (35).
Schizophrenia treatment is arduous even after treating the acute phase. The main task is to treat the acute phase but also to prevent relapses and lead the patient to recovery, thus ensuring socialization and reintegration into the community. Antipsychotics often need to be taken for very long periods, thus increasing the probability of adverse events, which prompt patients to discontinue medication and decrease adherence (36). A meta-analysis of clinical trials compared 32 commonly prescribed oral antipsychotics and found similar efficacy rates, while the greater differences regarded adverse events (37). This meta-analysis found weak effect sizes for brexpiprazole compared to clozapine but also confirmed a low potential for adverse events. The D2 dopamine receptor partial agonist antipsychotics, due to their potential to increase prefrontal cortical dopamine release, which is related to motivation and cognition (38–40), can decrease the symptoms of mood disorders, such as some core symptoms [but not all (41)] of major depressive disorder (MDD) or bipolar depression. In fact, this group of antipsychotics is used, both in monotherapy and in augmentation, in the treatment of mood (41) and personality disorders (42). While the FDA accepted some antipsychotic drugs as monotherapy in bipolar depression, it does not recommend any antipsychotic alone for unipolar depression.
Brexpiprazole (7-[4-[4-(1-benzothiophen-4-yl)piperazin-1-yl]butoxy]quinolin-2(1H)-one) was first approved in the US by the FDA in 2015 for schizophrenia in adults and pediatric patients older than 13 years, and as an add-on to an antidepressant drug for MDD in adults (43). In 2023, its indication was expanded to the treatment of agitation associated with dementia due to Alzheimer's disease (44). In Europe, it is indicated for schizophrenia in adults (45).
Brexpiprazole was found to be suitable for long-term adult schizophrenia treatment, as it shows a favorable adverse event profile, thus ensuring safety, besides reducing both positive and negative symptoms; this way, it achieves the goals of increasing patient's socialization and reintegration into the community (46).
Brexpiprazole displays a high affinity for serotonin, dopamine, and noradrenaline receptors. It strongly binds (Ki < 1 nM), 5HT1A and 5HT2A serotonin receptors, D2 dopamine receptors, and α1B and α2C adrenoceptors (47, 48). It is a partial agonist at 5HT1A serotonin and D2 dopamine receptors and an antagonist at 5-HT2A serotonin receptors and α1 and α2 adrenoceptors (47, 48). Brexpiprazole shows a fairly high affinity (Ki < 5 nM) for D3 dopamine-, 5HT2B, 5HT7 serotonin-, and α1A and α1D adrenergic receptors, a moderate affinity (Ki = 19 nM) for H1 histamine receptors, and low affinity (Ki > 1,000 nM) for M1 muscarinic cholinergic receptors (47, 48). Compared to aripiprazole and cariprazine, brexpiprazole binds the D2 dopamine and the 5-HT2A serotonin receptors strongly and displays more powerful partial agonist activities on 5-HT1A and 5-HT2C serotonin receptors. Due to its lower intrinsic activity at D2 receptors and higher binding affinities for 5-HT1A/2A receptors than aripiprazole, brexpiprazole would have a favorable antipsychotic potential without D2 receptor agonist- and antagonist-related adverse effects (48). Furthermore, due to its greater 5-HT7-blocking ability compared to other dopamine D2 partial agonists [Supplementary Table 1; (49–51)], brexpiprazole has more robust effects on the cognitive impairment associated with schizophrenia (24, 25, 48).
Brexpiprazole and aripiprazole have low propensities to induce extrapyramidal symptoms (EPS). However, the low EPS risk of brexpiprazole is more likely dependent on its agonist properties on presynaptic 5-HT1A receptors, while that of aripiprazole is less sensitive to 5-HT1A receptor antagonism, as shown in a preclinical study (52).
Both antipsychotics reduce the symptoms of schizophrenia, but brexpiprazole seems to show a peculiar reduction in impulsivity; this latter should lead to better tolerability with a lower incidence of akathisia (53). Brexpiprazole administered to patients with schizophrenia and impulsivity was associated with decreased right ventrolateral prefrontal cortex (VLPFC) activation and decreased stop-signal reaction time (SSRT), supporting a benefit of brexpiprazole on inhibition-related brain activation and behavior (54).
The blockade of mesolimbic receptor D2 results in the inhibition of the reward and reinforcement circuits. While dopamine D2 receptor antagonism reduces positive psychotic symptoms in schizophrenia, it may worsen negative symptoms such as apathy, avolition, reduced motivation, and anhedonia (55). This partly explains an increase in tobacco and substance use in patients treated with classical antipsychotic drugs (56, 57). Substance use disorders (SUDs) are highly comorbid with psychotic disorders (58). Patients with psychosis appear to be particularly vulnerable to the consumption of psychoactive drugs (59). Negative symptoms, either primary or fostered by antipsychotics, may promote the use of psychostimulant drugs, and the latter may be used to treat negative symptoms (60). However, psychostimulant drugs are not easy to manage and cannot be used for long periods of time.
Dose-dependent reductions of cocaine self-administration in rhesus monkeys were obtained when drugs with 5-HT2C receptor agonist and 5-HT1A receptor partial agonist properties were administered (61). 5-HT2A antagonist activity and partial agonist activity on 5-HT1A and 5-HT2C receptors could be active in reducing stimulant drug consumption in patients with SUDs comorbid with psychotic disorders. Thus, in the light of its receptor-binding profile, brexpiprazole appears to be a valid treatment for psychosis and a particularly suitable drug for patients with psychotic symptoms and concomitant SUD.
There are perspectives for the new class of dopamine receptor partial agonists in various psychiatric disorders and neurological diseases, and many molecules are now being tested (62, 63). It appears that those directed to the D1 group of dopamine receptors (D1/D5), such as tavapadon, will not work in schizophrenia, but will be effective in Parkinson's disease (64), while psychotic disorders will respond to the partial agonism of the D2 group of receptors. Recently, there has been a suggestion that by focusing on the partial agonism of this group, especially D3, we could develop drugs that may prove useful in SUDs (65–68). Such drugs can reduce the psychotic symptomatology of schizophrenia in patients with SUD (65). We employed the D2 dopamine receptor partial agonist, brexpiprazole, to assess its efficacy in patients with schizophrenia with or without a comorbid SUD in a study with an open-label design. In this study, we do not report on safety in detail, which was however assessed and will be the object of a future study. Our intent was to assess the efficacy of brexpiprazole in reducing psychotic symptoms in both subpopulations. We also aimed to evaluate if the presence of a comorbid SUD conferred treatment resistance and to assess the effect of brexpiprazole on the craving for the substance used in that specific SUD for 6 months.
We conducted an observational study on inpatients with a diagnosis of schizophrenia hospitalized at the Villa Von Siebenthal neuropsychiatric hospital. Recruitment began on 1st February 2022 and ended on 31st October 2022.
Patients aged from 18 to 66 years were eligible if they had (1) a diagnosis of DSM-5/DSM-5-TR schizophrenia and SUD (cannabis, synthetic cannabinoids, cocaine, amphetamines, opioids, ketamine/phencyclidine or other NMDA receptor inhibitors, khat and other alkaloid cathinones, and alcohol or polysubstance use disorder) or (2) schizophrenia without SUD (69, 70). We admitted SUD patients who were receiving their specific SUD pharmacological treatment, such as methadone, buprenorphine, and naltrexone, or benzodiazepines and gabapentinoids. All patients were initially inpatients, discharged after 1 month and followed-up as outpatients thereafter.
Exclusion criteria were the presence of a comorbid major psychiatric disorder other than schizophrenia; high risk of suicide as assessed with the Columbia-Suicide Severity Risk Scale (C-SSRS) (71); comorbidity with severe organic diseases (autoimmune or systemic connective tissue diseases, treatment-resistant hypertension, type 1 diabetes, metabolic syndrome, severe cardiovascular diseases, and major neurological diseases); history of epilepsy, head injury, electroencephalographic (EEG) abnormalities, and neurodevelopmental disorders; intelligence quotient (IQ) < 75, as assessed with the Wechsler Adult Intelligence Scale (WAIS) (72); unwillingness to participate, and inability to sign the informed consent for oneself or, in case of inability, unwillingness/refusal of the legal guardian to sign.
After meeting the inclusion criteria and not meeting the exclusion criteria, patients were explained study aims and methods and provided free, informed consent. The study received approval from the local ethical committee (CE Lazio 2, Rome, Italy; protocol number 331-306-00387). It was conducted in accordance with the Principles of Human Rights, as adopted by the World Medical Association at the 18th WMA General Assembly, Helsinki, Finland, June 1964, subsequently amended by the 64th WMA General Assembly, held in Fortaleza, Ceará, Brazil, in October 2013.
If the included patients were antipsychotic drug naïve or antipsychotic drug-free for at least 2 weeks, they were immediately treated with brexpiprazole, following the recommended titration from 1 mg once daily to adjustment to 2–4 mg once daily. If they were on other antipsychotic medications, they were prescribed brexpiprazole after a proper wash-out of at least 2 weeks. Once reaching the appropriate dose for each patient (based on clinical course and clinician's decision), usually the target dose of 4 mg/day in monotherapy, the regimen was maintained for 6 months. Patients were not allowed to take other antipsychotic drugs or antidepressants throughout the study period; the only medications allowed were those specifically used for each SUD, i.e., methadone, buprenorphine and naltrexone, and benzodiazepines and gabapentinoids for anxiety and insomnia.
We followed up with our patients for 6 months, evaluating their psychopathology with psychometric scales.
Schizophrenia and SUD (cannabis, synthetic cannabinoids, cocaine, amphetamines, opioids, ketamine/phencyclidine or other inhibitors of NMDA receptors, khat and other cathinone alkaloids, and alcohol and polysubstance use disorder) were diagnosed by professional psychiatrists using SCID-5-CV (73); eligibility was based on schizophrenia diagnosis. Patients were regularly tested for drug use both at intake and during the study.
Patients were assessed at baseline, every week for 2 months, and every month for a further 4 month period (study endpoint at 6 month follow-up) with the following instruments.
To rate psychopathology, we used the Clinical Global Impressions–Severity scale (CGI-S) (74), the 24-item Brief Psychiatric Rating Scale (BPRS) (75), the Italian version (76), and the Positive And Negative Syndrome Scale (PANSS) (77). To evaluate craving in patients with SUD, we used the visual analog scale for craving (VAScrav) (78). The latter rates craving from 0 (no craving) to 10 (the most intense craving according to patient's experience).
The BPRS has been developed from a previous 18-item version (79), which has been factorialised in the following five subscales: anxiety-depression, anergy, thought disorders, activity, and hostility (80). A similar factor structure has also been obtained for the expanded 24-item version (81), so we decided to maintain this five-factor solution as the best fit, although factoralisations of the BPRS have been very inconsistent (82, 83). Our primary goal was to assess the efficacy of brexpiprazole through PANSS, CGI-S, and BPRS scores.
Patients affected by SUD were meant to be compared to those without SUD (non-SUD) to assess if comorbid SUD could hinder brexpiprazole psychosis treatment and if the same treatment is associated with changes in substance craving. Adverse events were recorded as reported.
Frequency distributions and descriptive statistics were performed to analyse the sample. We used Student's t-test for analyzing point differences between the two samples in continuous variables, with all two-tailed analyses, univariate analysis of variance (ANOVA) for analyzing course differences of continuous variables and the chi-squared test (χ2) for nominal variables after ensuring normal distribution with the Shapiro and Wilk test (84) and sphericity with the Mauchly W-test (85). Data were analyzed using the IBM Statistical Package for the Social Sciences (SPSS) Version 23 (IBM, Armonk, New York, 2016). Significance was set at p < 0.05.
Our sample consisted of 86 patients with schizophrenia, with 51 men (59.3%) and 35 women (40.7%). Of these, 48 patients had comorbid SUD (55.8%), 37 men and 11 women, whereas 38 did not have a substance use disorder in comorbidity (non-SUD) (44.2%), 14 men and 24 women. Patients' ages ranged from 18 to 64 years (mean 39.32, standard deviation SD = 14.09). The sociodemographic characteristics of the sample, along with the SUD types, are shown in Table 1. The patients' scores on the clinical scales are shown in Figures 1–4. Of the 86 patients who were included in the sample, 85 were analyzed because one woman of the non-SUD group requested to withdraw after 1 week on 1 mg brexpiprazole due to subjectively perceived akathisia.
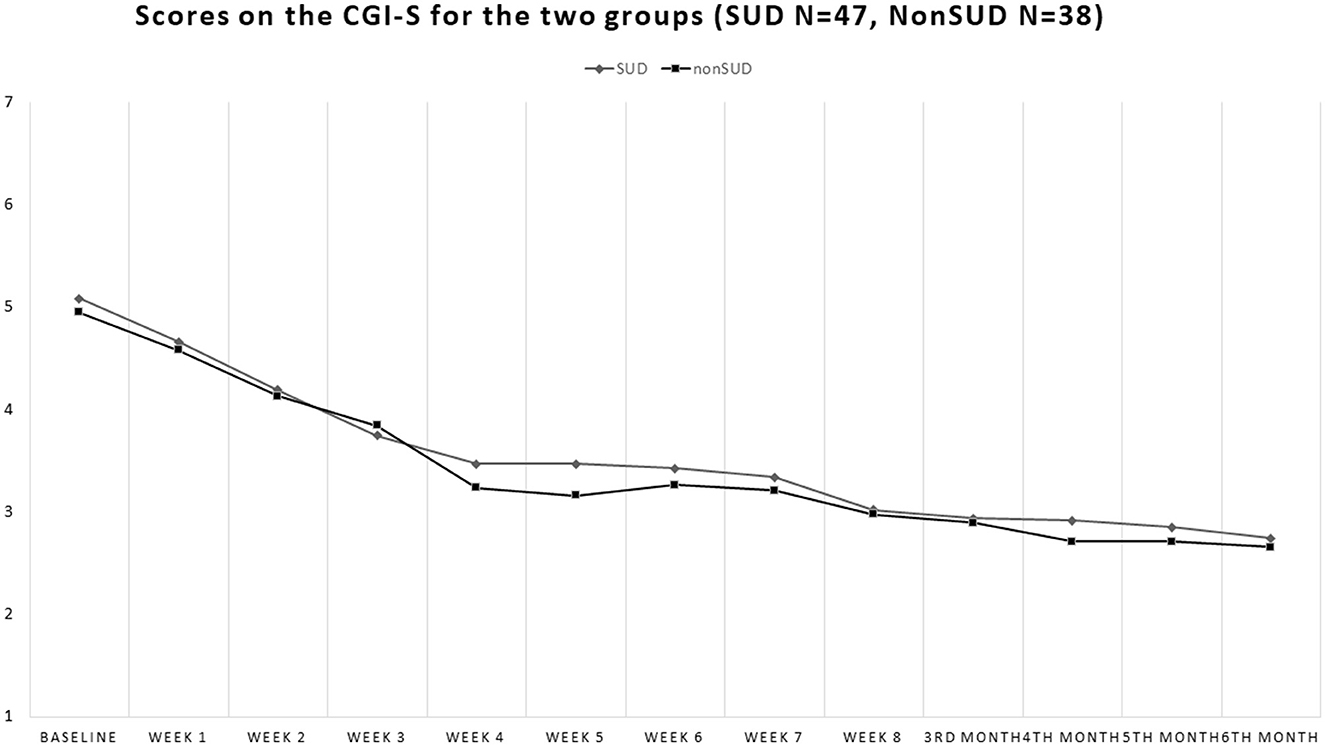
Figure 1. Drop of Clinical Global Impressions (CGI-S) scores during the study in the groups with comorbid substance use disorder (SUD) and the non-comorbid group (non-SUD). The two groups look quite similar in their scores on this scale.
At baseline, the non-SUD group scored 4.95 ± 0.61 on the CGI-S, while the SUD group scored 5.06 ± 0.84 [Student's t = 0.71; p = 0.48, not significant (ns)], and at endpoint, they scored 2.66 ± 0.48 and 2.74 ± 0.67, respectively (Student's t = 0.67; p = 0.51, ns). Both groups showed significant decrements from baseline to endpoint Student's t = 18.12; p < 0.00001 for the non-SUD group and Student's t = 15.01; p < 0.00001 for the SUD group (Figure 1).
At baseline, the non-SUD group scored 62.08 ± 13.81 on the BPRS (total score), while the SUD group scored 70.55 ± 19.02 (Student's t = −2.30; p = 0.024, with the latter scoring significantly higher), and at endpoint, they scored 6.82 ± 1.43 and 35.64 ± 12.92, respectively (Student's t = −2.61; p = 0.01, with the SUD group scoring even more significantly higher than the non-SUD). Both groups showed significant decreases from baseline to endpoint Student's t = 13.25; p < 0.00001 for the non-SUD group and Student's t = 10.41; p < 0.00001 for the SUD group (Figure 2).
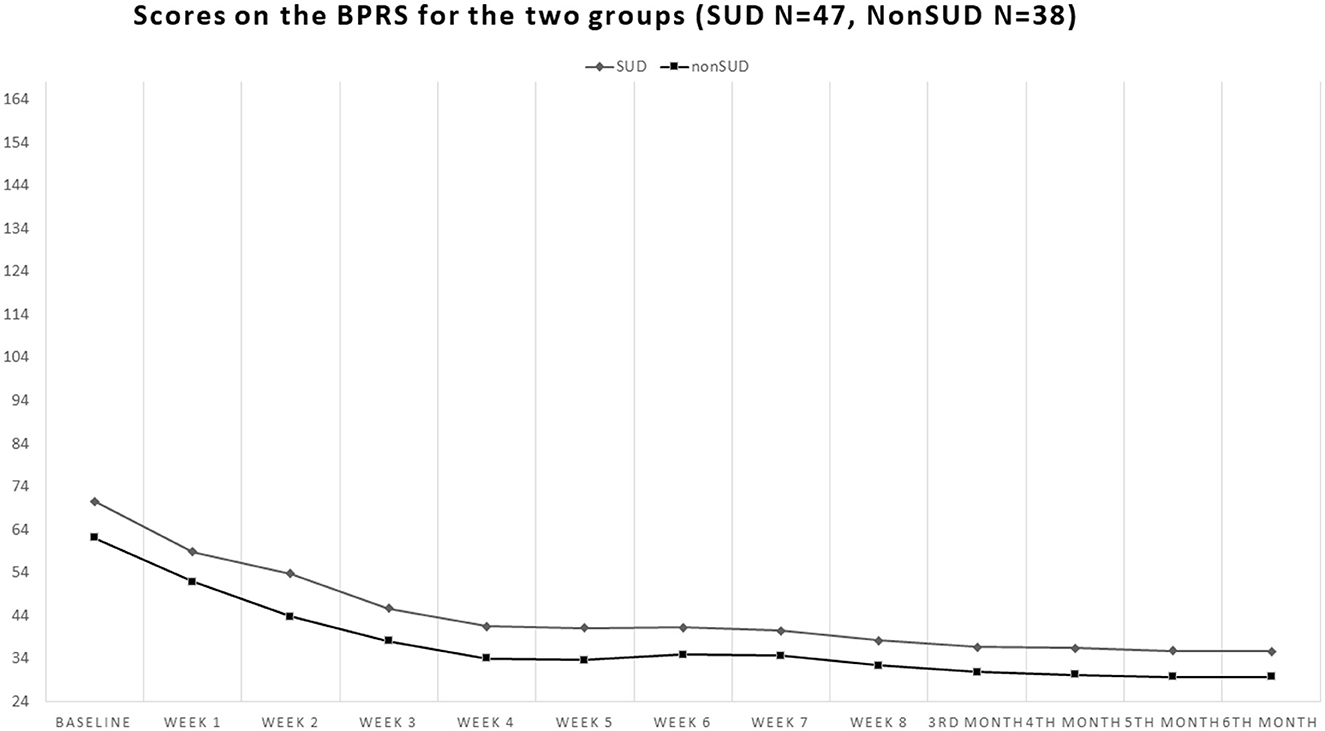
Figure 2. Course of the scores on the 24-item Brief Psychiatric Rating Scale-Expanded version (BPRS-24) in the groups with comorbid substance use disorder (SUD) and in the non-comorbid group (non-SUD). Both groups obtained about a 50% reduction from baseline to endpoint, but the non-SUD group scored constantly lower throughout the study, indicating that its participants fared better than the comorbid SUD group.
Regarding BPRS subscales, the non-SUD group scored 18.76 ± 4.31 at baseline on the BPRS anxiety/depression subscale, while the SUD group scored 16.55 ± 4.15 (Student's t = 2.40; p = 0.019, with the latter scoring significantly lower), and at endpoint, they scored 7.50 ± 2.60 and 7.26 ± 3.04, respectively (Student's t = 0.39; p = 0.69, ns). Both groups showed similar significant decreases from baseline to endpoint Student's t = 13.80; p < 0.00001 for the non-SUD group and Student's t = 12.39; p < 0.00001 for the SUD. On the anergy subscale of the BPRS, the non-SUD group scored 14.92 ± 5.28 at baseline and the SUD group scored 15.00 ± 4.52 (Student's t = −0.07; p = 0.94, ns), while at endpoint, they scored 6.58 ± 2.11 and 7.62 ± 2.91, respectively (Student's t = 1.84; p = 0.07, ns). Both groups showed similar significant decreases from baseline to endpoint (Student's t = 9.04; p < 0.00001 for the non-SUD group and Student's t = 9.42; p < 0.00001 for the SUD). On the thought disorder subscale of the BPRS, the non-SUD group scored 13.29 ± 6.19 at baseline, while the SUD group scored 18.45 ± 8.06 (Student's t = −3.25; p = 0.0017, with the SUD group scoring significantly higher), and at endpoint, they scored 6.58 ± 2.11 and 9.19 ± 4.31, respectively (Student's t = −3.01; p = 0.004, with the SUD group scoring higher and the gap between the two remaining). However, both groups showed similar significant score decreases from baseline to endpoint (Student's t = 6.29; p < 0.00001 for the non-SUD group and Student's t = 6.95; p < 0.00001 for the SUD). On the activity subscale of the BPRS, the non-SUD group scored 10.37 ± 4.00 at baseline and the SUD group 12.72 ± 5.75 (Student's t = −2.14; p = 0.035; the SUD group scored significantly higher), while at endpoint, they scored 5.76 ± 1.17 and 7.02 ± 2.51, respectively (Student's t = −2.85; p = 0.006, with the SUD group scoring higher and the gap between the two remaining and even enlarging). In any case, both groups showed similar significant score decreases from baseline to endpoint (Student's t = 6.81; p < 0.00001 for the non-SUD group and Student's t = 6.23; p < 0.00001 for the SUD). On the hostility/suspiciousness subscale of the BPRS, the non-SUD group scored 4.61 ± 2.63 at baseline and the SUD group scored 7.77 ± 4.26 (Student's t = −4.00; p = 0.0001, with the SUD group scoring significantly higher), while at endpoint they scored 3.11 ± 0.39 and 4.46 ± 2.27, respectively (Student's t = −3.54; p = 0.0007, with the SUD group scoring higher and the gap between the two tending to close but remaining). At any rate, both groups showed similar significant score decreases from baseline to endpoint (Student's t = 3.48; p = 0.0008 for the non-SUD group and Student's t = 4.74; p < 0.00001 for the SUD).
On the PANSS, the non-SUD group obtained a baseline total score of 85.29 ± 14.94 and the SUD 98.40 ± 21.83 (Student's t = −3.15; p = 0.002, with SUD scoring higher). At endpoint, they obtained scores of 41.08 ± 10.03 and 48.17 ± 16.69 (Student's t = −2.30; p = 0.024, with the SUD group still scoring higher, but with the gap tending to close). Both groups showed significant large decreases from baseline to endpoint (Student's t = 15.15; p < 0.00001 for the non-SUD group and Student's t = 12.53; p < 0.00001 for the SUD) (Figure 3).
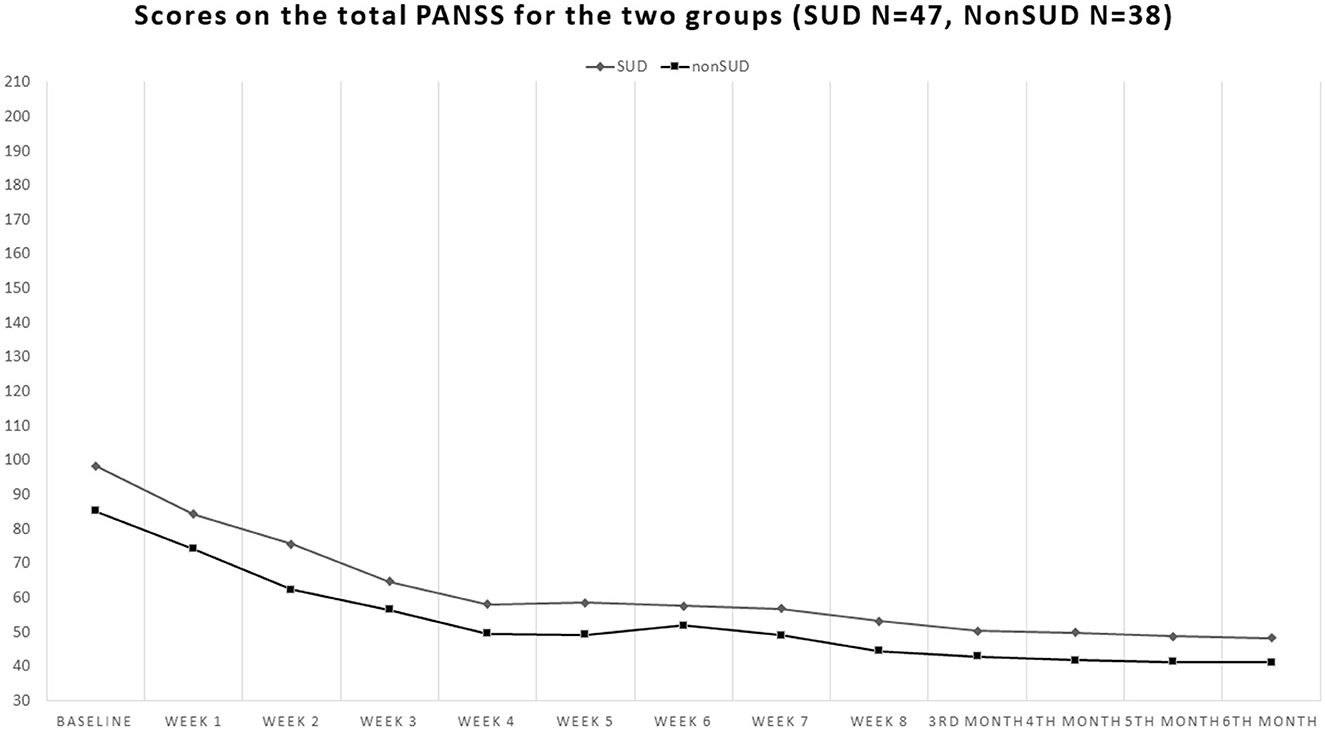
Figure 3. Course of the total scores of the Positive And Negative Syndrome Scale (PANSS) in the groups with comorbid substance use disorder (SUD) and the non-comorbid group (non-SUD). Both groups obtained >50% reduction from baseline to endpoint, compatible with clinical response, but similarly to what occurred with the BPRS-24, the non-SUD group scored constantly lower throughout the study, indicating that the non-comorbid group was clinically better than the comorbid SUD group.
Concerning PANSS subscales, baseline scores on the positive PANSS subscale were 12.95 ± 5.59 for the non-SUD group and 19.62 ± 9.94 for the SUD group (Student's t = −3.69; p = 0.0004, with SUD scoring higher), while at endpoint they were 7.87 ± 1.54 and 9.66 ± 3.81, respectively (Student's t = −2.72; p = 0.008, with SUD continuing to score higher). In both groups, reductions in PANSS positive scores were significant Student's t = 5.39; p < 0.00001 for the non-SUD and Student's t = 6.41; p < 0.00001 for the SUD group. Baseline scores on the negative PANSS subscale were 22.00 ± 6.86 for the non-SUD and 24.26 ± 5.74 for the SUD group (Student's t = −1.65; p = 0.103, ns), while at endpoint, they scored 9.79 ± 3.60 and 11.57 ± 4.48, respectively (Student's t = −1.99; p < 0.05, with the SUD group scoring marginally higher than the non-SUD). Both groups showed significant score decreases from baseline to endpoint (Student's t = 9.72; p < 0.00001 for the non-SUD group and Student's t = 11.95; p < 0.00001 for the SUD). On the general psychopathology PANSS subscale, baseline scores were 50.39 ± 10.68 for the non-SUD and 54.62 ± 11.09 for the SUD group (Student's t = −1.77; p = 0.080, ns), while endpoint scores were 23.42 ± 6.85 and 26.94 ± 10.03, respectively (Student's t = −1.84; p = 0.07, ns), i.e., non-SUD and SUD did not differ on baseline or endpoint scores on the general psychopathology PANSS subscale. However, both groups obtained strong score reductions on this subscale from baseline to endpoint (Student's t = 13.11; p < 0.00001 for the non-SUD group and Student's t = 12.69; p < 0.00001 for the SUD).
In the SUD group, VAS craving scores decreased from 7.47 ± 2.45 at baseline to 1.49 ± 2.06 at endpoint (Student's t = 12.80; p < 0.00001) (Figure 4). The effect size was very large (Cohen's d = 2.67; Glass's delta = 2.49; Hedges' g = 2.67).
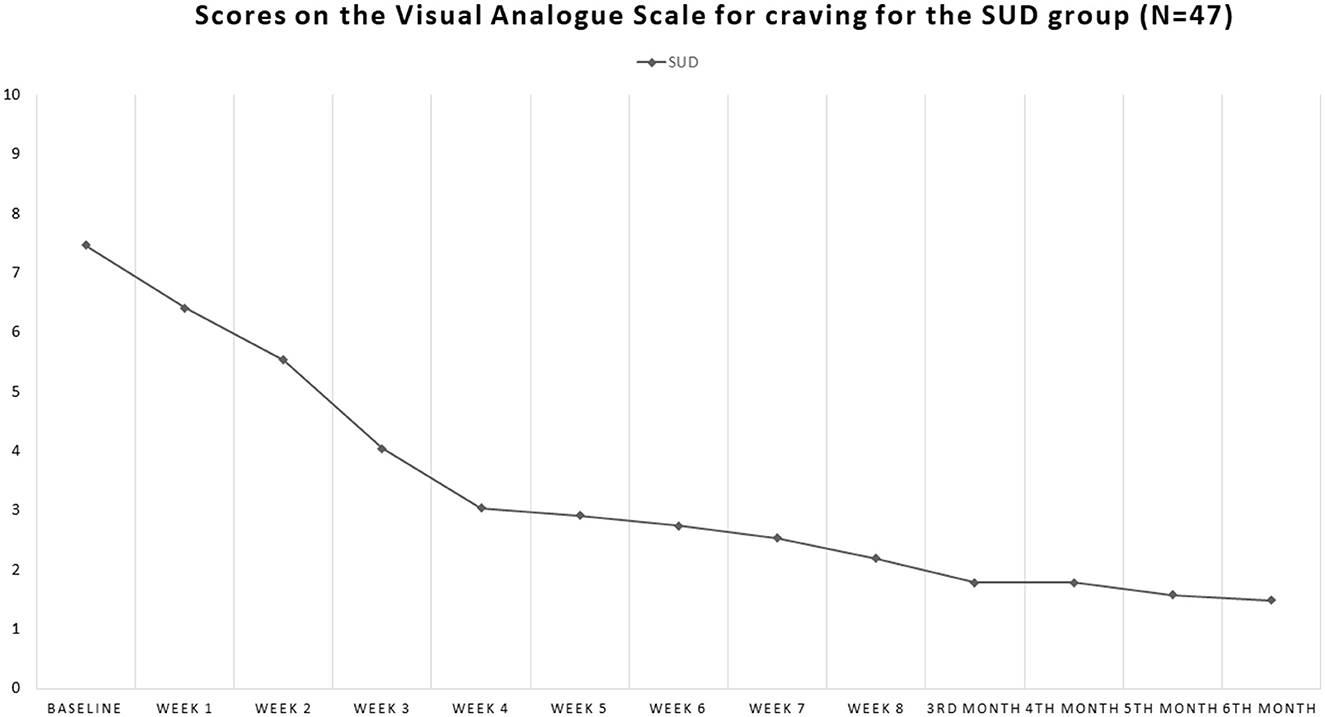
Figure 4. Course of the scores on the Visual Analog Scale for craving (VAScrav) in the SUD comorbid group. This scale is rated by the patient from 0 to 10; at baseline, it was 7.47 and by the 6 month endpoint had dropped to 1.49, i.e., by >80%.
We implemented repeated-measures ANOVA involving the independent variable SUD (presence/absence) as the between-subjects variable, time as the within-subjects variable, and CGI, BPRS, PANSS, and VAScrav scores as dependent variables. In the case of statistical significance, we conducted Tukey's post-hoc test.
Comparing the 12 timepoints, results indicate a main effect of Time [F(1, 913) = 162.798; p < 0.0001], with an improvement of clinical global severity.
Comparing the 12 timepoints for each subscale of the BPRS, a main effect of time was found for anxiety-depression [F(1, 913) = 144.275; p < 0.0001], which highlights an overall improvement of symptomatology over time. Moreover, we found an interaction of Time × SUD (presence/absence) [F(1, 913) = 4.382; p < 0.0001], in which symptoms improve in both conditions over time. For the anergia subscale, there was a main effect of time [F(1, 913) = 94.705; p < 0.0001], with overall improvement over time. A main effect of time [F(1, 913) = 50.333; p < 0.0001] was also found for the thought disorder subscale, with an overall improvement of symptoms. Moreover, there was an interaction effect of time × SUD (presence/absence) [F(1, 913) = 3.415; p < 0.0001], in which symptoms of both conditions improved over time. Main effects of time were also found for the activity [F(1, 913) = 53.494; p < 0.0001] and hostility/suspiciousness [F(1, 913) = 8.443; p < 0.0001] subscales and for the BPRS total score [F(1, 913) = 105.166; p < 0.0001], with overall symptomatologic improvements over time.
Comparing the 12 timepoints for each subscale of the PANSS, we found a main effect of time for the positive symptoms subscale [F(1, 913) = 35.957; p < 0.0001], with an overall improvement in positive symptoms over time. Furthermore, there was an interaction effect of time × SUD (presence/absence) [F(1, 913) = 6.493; p < 0.0001], in which both conditions improved in positive symptoms over time. A main effect of time was also found for the negative symptoms subscale [F(1, 913) = 106.9359; p < 0.0001], for the general psychopathology subscale [F(1, 913) = 132.715; p < 0.0001], and for the PANSS total subscale [F(1, 913) = 135.825; p < 0.0001], with all symptoms decreasing over time.
Comparing the 12 timepoints for the VAScrav questionnaire in SUD outpatients, we found a main effect of time [F(1, 506) = 81.858; p < 0.0001], with an overall amelioration in craving over time.
During the study, no serious adverse event developed, but subjective akathisia in a woman led to her drop-out. All adverse events, i.e., nausea, headache, muscle aches, fatigue, and insomnia, were transient and mild, needing no specific treatment or discontinuation. Detailed safety data will be provided in a future study focusing on safety.
In this study, we evaluated 86 patients with schizophrenia, of whom 48 had a comorbid SUD. These patients were all treated with brexpiprazole at the target dose of 4 mg/day; 79 were already treated with other antipsychotics and underwent an appropriate pharmacological switch, whereas seven were antipsychotic drug naïve. We found no differences between the SUD and non-SUD groups, concerning symptoms assessed with the CGI-S, the PANSS, and the 24-item BPRS. We might conclude from our results that people with schizophrenia who have a comorbid SUD do not respond to brexpiprazole treatment less than non-SUD patients with schizophrenia. Hence, having a SUD in a patient with schizophrenia does not confer resistance to treatment with brexpiprazole. Substance craving for their respective substances, as assessed through the VAScrav, was decreased in SUD-comorbid patients during brexpiprazole treatment.
We intended to evaluate the efficacy of treatment with brexpiprazole in psychotic symptom reduction and its ability to improve the global clinical status. Comparing patients with and without comorbid SUD allowed us to evaluate whether brexpiprazole could be a good treatment option in patients with SUD. Comorbid SUD is usually an obstacle to the treatment since it reduces treatment adherence in schizophrenia (86). Furthermore, high-potency dopaminergic blockade in persons with schizophrenia and comorbid SUD may interfere with the reward circuitry (87) and cause dysphoria (88). Lower reward perception may prompt the patient to resume illicit drug use to reinstate their previous state (57, 89). While the activation of D2 receptors in the nucleus accumbens soothes the symptoms of opiate withdrawal in opiate-dependent rats, their blockade elicits somatic symptoms attributable to withdrawal (90). The withdrawal symptom-eliciting and aversive effects of dopamine receptor blockade were related to the blockade of D2 but not D1 dopamine receptors (91). We may presume that by reducing ventral striatal-accumbal dopamine-related reward through D2 receptor inhibition, we may actually worsen addictive behaviors in patients with comorbid schizophrenia and SUD, although differences in baseline reward circuitry function among patients with schizophrenia may play a role (92). We did not observe such worsening or lack of improvement in patients receiving brexpiprazole in our study; we may attribute this effect to the partial agonist effect of brexpiprazole on dopamine D2/D3 receptors in the limbic system (93), mainly to the D2 (94). In this study, we showed a positive effect of brexpiprazole 4 mg/day on craving; currently, there are no studies investigating craving in SUD in patients treated with brexpiprazole. One that investigated it in patients with cocaine use disorder found a medium-to-large effect for olanzapine, with Cohen's d = 0.79 (95), while we found a much larger effect (Cohen's d = 2.67); however, the substance use disorder in their sample differed from ours, as did the craving assessment scale, and sample sizes were different [smaller in Smelson et al. (95)].
We evaluated the psychopathology in our patients using psychometric scales at baseline, i.e., before treatment with brexpiprazole, then every week for 2 months, and then every month until the 6th month of evaluation. We observed the main effects of time for both SUD comorbid and non-comorbid samples for scores on the CGI-S, BPRS-24, and PANSS subscales and total scores. A similar main effect of time with an overall improvement in craving was evident in the SUD-comorbid group. While negative PANSS scores decreased for both SUD and non-SUD groups from baseline to endpoint, and the two groups did not differ for baseline scores on the negative subscale, the final scores of the SUD group were higher than the non-SUD scores, indicating that the latter group's negative symptoms had benefitted from brexpiprazole treatment more than what they did in the SUD group. It should be underlined that the majority of our SUD sample had cannabis use disorder; this subgroup in our study did not show lower negative symptoms compared to the non-SUD sample, in contrast to what has been observed in other studies, where people with cannabis use disorder showed less negative symptoms than individuals without cannabis use disorder (96, 97). There is no sufficient data to speculate as to the neurochemical mechanism underpinning the resistance of negative symptoms to the antipsychotic in SUD patients, but we should recall that most of our sample had cannabis use disorder and that cannabinoid mechanisms may underlie negative symptoms in schizophrenia, although in a most complex way (98).
Regarding differences between SUD and non-SUD groups, the latter had scored higher than the former at baseline on the BPRS Anxiety-Depression subscale. Both populations obtained fair reductions of BPRS scores in this very subscale when treated with brexpiprazole over 6 months. At the study endpoint, the differences in the BPRS Anxiety-Depression subscale disappeared, indicating that depression and anxiety in both SUD comorbid and non-SUD groups with schizophrenia benefitted from drug treatment with brexpiprazole. Decreases in the scores of the BPRS anergy subscale and the negative PANSS dimension were observed with treatment over time.
Patients with comorbid SUD scored higher than their non-comorbid non-SUD counterparts on the BPRS-24 thought disorder subscale at baseline. Both subgroups of patients with schizophrenia improved over time with treatment, with endpoint scores not differing between the two groups. SUD patients scored higher than non-SUD on the PANSS Positive subscale at baseline; both groups responded to drug treatment, with positive symptoms improving over time in both SUD and non-SUD groups.
Patients with comorbid SUD scored higher than non-SUD patients on the BPRS hostility subscale. There is evidence that SUD is related to violent behavior (99); substance use patterns in people with addiction may be related to coping styles associated with aggression and hostility (100). In our study, patients' scores on the hostility subscale of the BRPS decreased over time, independently of whether they had SUD comorbidity or not. The scores on the BPRS activity dimension also decreased over time in both populations.
We have been overcautious in our switch from other antipsychotics to brexpiprazole. Probably, the wash-out we practiced per protocol was not actually needed, as brexpiprazole was well tolerated. In future studies, we are set to switch directly, reducing the dose of the other antipsychotics according to its schedule.
Regarding craving for substances, which we investigated only in the SUD-comorbid population, scores decreased over time, despite the abrupt substance discontinuation and the concomitant use of an antipsychotic such as brexpiprazole. It appears that this antipsychotic has no detrimental effect on the patients' reward system. A recent systematic review focused on the effects of various drugs, including antipsychotics, on cocaine craving (101). This review found no consistent effects of antipsychotics on craving (one study showing positive effects of aripiprazole and two showing results similar to placebo, three studies on risperidone, and one on quetiapine showing no significant results, while among five studies on olanzapine, one showed it to be better than haloperidol, one to be worse than haloperidol, and three showed no significant effects). The results obtained here are legitimate further studies of the effects of antipsychotics on substance craving.
Brexpiprazole was shown to be effective in adult schizophrenia, both in the short- and long-term (102, 103) and as an adjunct, also in major depression (104), even if treatment-resistant (105). There is a current trend to use partial D2/3 agonists in the so-called “dual” disorders, i.e., a major psychiatric disorder comorbid with a SUD (106, 107), and there is a sound rationale to pursue this way (108). For the moment, long-acting injectable antipsychotics were associated with improvement in dual disorders (65), and among them, aripiprazole, a partial D2/3 agonist, holds a preeminent position (109–111). Future studies will establish whether there are differences among the already marketed partial D2/3 agonists aripiprazole, brexpiprazole, and cariprazine in the treatment of comorbid major psychiatric disorders and SUDs (and which SUDs). While evidence for a positive effect of aripiprazole on craving has been obtained in controlled studies (109, 112, 113), data on alcohol use disorder were inconsistent (114, 115). For cariprazine, there are only case reports of efficacy in reducing craving (116, 117), whereas, for brexpiprazole, there are still no reports besides the current study; here, we showed a strong effect of brexpiprazole in reducing craving.
Our study had several limitations. Our sample size was small and needs to increase to enable us to draw valid conclusions. Furthermore, there were no comparison groups, for example, samples with or without SUD treated with other than brexpiprazole antipsychotics or placebo. Open-label studies may affect results and limit generalisability. The fact that our study used a population referring to a single site could have limited the representability of the sample. Moreover, we could not analyse data according to gender or whether they were drug-naïve or switched from another antipsychotic, but there were many more women in the non-SUD group and many more men in the SUD group, and the drug-naïve subsample was very small compared to the sample that switched from another antipsychotic. The substances used in the SUD comorbid group were often multiple, and there were not sufficient subsample sizes to allow us to differentiate the different substances. However, most patients in the comorbid group were using cannabis, although the relative majority were multisubstance users (Table 1).
We found brexpiprazole to be a valid treatment option to treat schizophrenia, with or without substance use disorder. Brexpiprazole proved to be effective on psychotic symptoms, both positive and negative. Comorbid substance use disorder did not confer treatment resistance in this study. Brexpiprazole was found to be suitable to treat patients with comorbid SUD and psychotic disorders since it did not increase craving for illicit substances after their abrupt discontinuation (on the contrary, craving decreased during the study in the SUD group). Furthermore, treatment with brexpiprazole was followed by the leveling of initial differences between SUD and non-SUD patients with schizophrenia on those psychopathological dimensions where the two groups differed at baseline. Further studies with larger samples, randomized control designs, and using healthy controls as comparison groups are needed to confirm these encouraging results. Should our data be confirmed by such studies, new clinical perspectives for the use of brexpiprazole (and partial D2/3 agonists in general) may appear in the therapeutic horizon of schizophrenia, bipolar disorder, and other major psychiatric disorders comorbid with specific substance use disorders.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by CE Lazio 2, Rome, Italy; protocol number 331-306-00387. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
GL: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Supervision, Validation, Writing—original draft, Writing—review & editing. GT: Software, Visualization, Writing—original draft. EA: Data curation, Formal analysis, Methodology, Software, Visualization, Writing—original draft. GK: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Supervision, Validation, Writing—original draft, Writing—review & editing. FP: Data curation, Formal analysis, Investigation, Methodology, Software, Validation, Writing—original draft. VG: Conceptualization, Investigation, Methodology, Validation, Writing—original draft. AD: Conceptualization, Investigation, Methodology, Software, Validation, Writing—original draft. SD: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Validation, Visualization, Writing—original draft.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research has been supported by Otsuka Pharmaceutical Italy and, as its copromotion partner, by Lundbeck Italy. Both Companies were not involved in study conduction, data analyses, and manuscript publication.
We gratefully acknowledge the contribution of the Scientific Administration of the Bibliographic and Bibliometric Support Service, Fondazione Policlinico A. Gemelli IRCCS, in particular, Dr. Maria Pattuglia, as well as Ms. Mimma Ariano, Ms. Ales Casciaro, Ms. Teresa Prioreschi, and Ms. Susanna Rospo, Librarians of the Sant'Andrea Hospital, Faculty of Medicine and Psychology, Sapienza University of Rome, for rendering precious bibliographical material accessible.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1321233/full#supplementary-material
1. GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet Psychiatry. (2022) 9:137–50. doi: 10.1016/S2215-0366(21)00395-3
2. Brannan SK, Sawchak S, Miller AC, Lieberman JA, Paul SM, Breier A. Muscarinic cholinergic receptor agonist and peripheral antagonist for schizophrenia. N Engl J Med. (2021) 384:717–26. doi: 10.1056/NEJMoa2017015
3. Kane JM. A new treatment paradigm: targeting trace amine-associated receptor 1 (TAAR1) in schizophrenia. J Clin Psychopharmacol. (2022) 42:S1–13. doi: 10.1097/JCP.0000000000001596
4. Titulaer J, Radhe O, Danielsson K, Dutheil S, Marcus MM, Jardemark K, et al. Lumateperone-mediated effects on prefrontal glutamatergic receptor-mediated neurotransmission: a dopamine D1 receptor dependent mechanism. Eur Neuropsychopharmacol. (2022) 62:22–35. doi: 10.1016/j.euroneuro.2022.06.009
5. Laborit H, Huguenard P, Alluaume R. Un nouveau stabilisateur végétatif; le 4560 RP [a new vegetative stabilizer; 4560 R.P.]. Presse Méd. (1893). (1952) 60:206–8.
6. Delay J, Deniker P. Neuroleptic effects of chlorpromazine in therapeutics of neuropsychiatry. J Clin Exp Psychopathol. (1955) 16:104–12.
7. Delay J, Deniker P, Harl JM. Utilisation en thérapeutique psychiatrique d'une phénothiazine d'action centrale élective (4560 RP) [therapeutic use in psychiatry of phenothiazine of central elective action (4560 RP)]. Ann Méd Psychol. (1952) 110:112–7.
8. Hamon J, Paraire J, Velluz J. Remarques sur l'action du 4560 R.P. sur l'agitation maniaque [remarks on the action of 4560 R.P. on manic agitation]. Ann Méd-Pychol. (1952) 1:333–5.
9. Carlsson A, Lindqvist M. Effect of chlorpromazine and haloperidol on formation of 3-methoxytyramine and normetanephrine on mouse brain. Acta Pharmacol Toxicol. (1963) 20:140–4. doi: 10.1111/j.1600-0773.1963.tb01730.x
10. van Rossum JM. The significance of dopamine-receptor blockade for the mechanism of action of neuroleptic drugs. Arch Int Pharmacodyn Ther. (1966) 160:492–4.
11. Baumeister AA, Francis JL. Historical development of the dopamine hypothesis of schizophrenia. J Hist Neurosci. (2002) 11:265–77. doi: 10.1076/jhin.11.3.265.10391
12. López-Muñoz F, Alamo C. The consolidation of neuroleptic therapy: janssen, the discovery of haloperidol and its introduction into clinical practice. Brain Res Bull. (2009) 79:130–41. doi: 10.1016/j.brainresbull.2009.01.005
13. Janssen PAJ, van de Westeringh C, Jageneau AHM, Demoen PJA, Hermans BKF, van Daele GHP, et al. Chemistry and pharmacology of CNS depressants related to 4-(4-hydroxy-phenylpiperidino)butyrophenone. I synthesis and screening data in mice. J Med Pharm Chem. (1959) 1:281–97. doi: 10.1021/jm50004a007
14. Divry P, Bobon J, Collard J. Le ≪R 1625≫: nouvelle thérapeutique symptomatique de l'agitation psychomotrice [R-1625: a new drug for the symptomatic treatment of psychomotor excitation]. Acta Neurol Psychiatr Belg. (1958) 58:878–88.
15. Divry P, Bobon J, Collard J, Pinchard A, Nols E. Étude et expérimentation cliniques du ≪R 1625≫ ou halopéridol, nouveau neuroleptique et neurodysleptique [Study and clinical trial of R 1625 or haloperidol, a new neuroleptic and neurodysleptic agent]. Acta Neurol Psychiatr Belg. (1959) 59:337–66.
16. Paquay J, Arnould F, Burton P. Étude clinique de l'action du R 1625 à doses modérées en psychiatrie [clinical study of the action of R 1625 in moderate doses in psychiatry]. Acta Neurol Psychiatr Belg. (1959) 59:882–91.
17. Carlsson A, Lindqvist M, Magnusson T. 3,4-Dihydroxyphenylalanine and 5-hydroxytryptophan as reserpine antagonists. Nature. (1957) 180:1200. doi: 10.1038/1801200a0
18. Carlsson A, Lindqvist M, Magnusson T, Waldeck B. On the presence of 3-hydroxytyramine in brain. Science. (1958) 127:471. doi: 10.1126/science.127.3296.471.a
19. Weinberger DR. Implications of normal brain development for the pathogenesis of schizophrenia. Arch Gen Psychiatry. (1987) 44:660–9. doi: 10.1001/archpsyc.1987.01800190080012
20. Yasuda Y, Kikuchi T, Suzuki S, Tsutsui M, Yamada K, Hiyama T. 7-[3-(4-[2,3-Dimethylphenyl]piperazinyl)propoxy]-2(1H)-quinolinone (OPC-4392), a presynaptic dopamine autoreceptor agonist and postsynaptic D2 receptor antagonist. Life Sci. (1988) 42:1941–54. doi: 10.1016/0024-3205(88)90493-6
21. Lawler CP, Prioleau C, Lewis MM, Mak C, Jiang D, Schetz JA, et al. Interactions of the novel antipsychotic aripiprazole (OPC-14597) with dopamine and serotonin receptor subtypes. Neuropsychopharmacology. (1999) 20:612–27. doi: 10.1016/S0893-133X(98)00099-2
22. Jordan S, Koprivica V, Chen R, Tottori K, Kikuchi T, Altar CA. The antipsychotic aripiprazole is a potent, partial agonist at the human 5-HT1A receptor. Eur J Pharmacol. (2002) 441:137–40. doi: 10.1016/S0014-2999(02)01532-7
23. Mohr P, Masopust J, Kopeček M. Dopamine receptor partial agonists: Do they differ in their clinical efficacy? Front Psychiatry. (2022) 12:781946. doi: 10.3389/fpsyt.2021.781946
24. Waters KA, Stean TO, Hammond B, Virley DJ, Upton N, Kew JN, et al. Effects of the selective 5-HT7 receptor antagonist SB-269970 in animal models of psychosis and cognition. Behav Brain Res. (2012) 228:211–8. doi: 10.1016/j.bbr.2011.12.009
25. Bozkurt NM, Unal G. Vortioxetine improved negative and cognitive symptoms of schizophrenia in subchronic MK-801 model in rats. Behav Brain Res. (2023) 444:114365. doi: 10.1016/j.bbr.2023.114365
26. González-Blanch C, Perez-Iglesias R, Pardo-García G, Rodríguez-Sánchez JM, Martínez-García O, Vázquez-Barquero JL, et al. Prognostic value of cognitive functioning for global functional recovery in first-episode schizophrenia. Psychol Med. (2010) 40:935–44. doi: 10.1017/S0033291709991267
27. Eaves S, Rey JA. Brexpiprazole (rexulti): a new monotherapy for schizophrenia and adjunctive therapy for major depressive disorder. P T. (2016) 41:418–22.
28. Hopkins SC, Lew R, Zeni C, Koblan KS. Challenges in the clinical development of non-D2 compounds for schizophrenia. Curr Med Res Opin. (2023) 39:467–71. doi: 10.1080/03007995.2022.2147342
29. Granger KT, Sand M, Caswell S, Lizarraga-Valderrama LR, Barnett JH, Moran PM, et al. A new era for schizophrenia drug development – lessons for the future. Drug Discov Today. (2023) 28:103603. doi: 10.1016/j.drudis.2023.103603
30. Musselman M, Huynh E, Kelshikar R, Lee E, Malik M, Faden J. Potassium channel modulators and schizophrenia: an overview of investigational drugs. Expert Opin Investig Drugs. (2023) 32:471–7. doi: 10.1080/13543784.2023.2219385
31. Ascher-Svanum H, Nyhuis AW, Stauffer V, Kinon BJ, Faries DE, Phillips GA, et al. Reasons for discontinuation and continuation of antipsychotics in the treatment of schizophrenia from patient and clinician perspectives. Curr Med Res Opin. (2010) 26:2403–10. doi: 10.1185/03007995.2010.515900
32. Stürup AE, Hjorthøj C, Jensen HD, Melau M, Davy JW, Nordentoft M, et al. Self-reported reasons for discontinuation or continuation of antipsychotic medication in individuals with first-episode schizophrenia. Early Interv Psychiatry. (2023) 17:974–83. doi: 10.1111/eip.13389
33. Robinson DG, Schooler NR, Rosenheck RA, Lin H, Sint KJ, Marcy P, et al. Predictors of hospitalization of individuals with first-episode psychosis: data from a 2-year follow-up of the RAISE-ETP. Psychiatr Serv. (2019) 70:569–77. doi: 10.1176/appi.ps.201800511
34. Paksarian D, Mojtabai R, Kotov R, Cullen B, Nugent KL, Bromet EJ. Perceived trauma during hospitalization and treatment participation among individuals with psychotic disorders. Psychiatr Serv. (2014) 65:266–9. doi: 10.1176/appi.ps.201200556
35. Kadakia A, Catillon M, Fan Q, Williams GR, Marden JR, Anderson A, et al. The economic burden of schizophrenia in the United States. J Clin Psychiatry. (2022) 83:22m14458. doi: 10.4088/JCP.22m14458
36. McIntyre RS. Understanding needs, interactions, treatment, and expectations among individuals affected by bipolar disorder or schizophrenia: the UNITE global survey. J Clin Psychiatry. (2009) 70:5–11. doi: 10.4088/JCP.7075su1c.02
37. Huhn M, Nikolakopoulou A, Schneider-Thoma J, Krause M, Samara M, Peter N, et al. Comparative efficacy and tolerability of 32 oral antipsychotics for the acute treatment of adults with multi-episode schizophrenia: a systematic review and network meta-analysis. Lancet. (2019) 394:939–51. doi: 10.1016/S0140-6736(19)31135-3
38. Brenhouse HC, Sonntag KC, Andersen SL. Transient D1 dopamine receptor expression on prefrontal cortex projection neurons: relationship to enhanced motivational salience of drug cues in adolescence. J Neurosci. (2008) 28:2375–82. doi: 10.1523/JNEUROSCI.5064-07.2008
39. Selleck RA, Giacomini J, Buchholtz BD, Lake C, Sadeghian K, Baldo BA. Modulation of appetitive motivation by prefrontal cortical mu-opioid receptors is dependent upon local dopamine D1 receptor signaling. Neuropharmacology. (2018) 140:302–9. doi: 10.1016/j.neuropharm.2018.07.033
40. Vassilev P, Pantoja-Urban AH, Giroux M, Nouel D, Hernandez G, Orsini T, et al. Unique effects of social defeat stress in adolescent male mice on the Netrin-1/DCC pathway, prefrontal cortex dopamine and cognition (Social stress in adolescent vs. adult male mice). eNeuro. (2021) 8:ENEURO.0045-21.2021. doi: 10.1523/ENEURO.0045-21.2021
41. Grinchii D, Dremencov E. Mechanism of action of atypical antipsychotic drugs in mood disorders. Int J Mol Sci. (2020) 21:9532. doi: 10.3390/ijms21249532
42. Orzelska-Górka J, Mikulska J, Wiszniewska A, Biała G. New atypical antipsychotics in the treatment of schizophrenia and depression. Int J Mol Sci. (2022) 23:10624. doi: 10.3390/ijms231810624
43. FDA (US Food and Drug Administration). FDA Approves New Drug to Treat Schizophrenia and as an Add on to an Antidepressant to Treat Major Depressive Disorder. (2015). Available online at: https://www.fda.gov/newsevents/newsroom/pressannouncements/ucm454647.htm (accessed August 4, 2023).
44. FDA (US Food and Drug Administration). FDA Approves First Drug to Treat Agitation Symptoms Associated with Dementia due to Alzheimer's Disease. (2023). Available online at: https://www.fda.gov/news-events/press-announcements/fda-approves-first-drug-treat-agitation-symptoms-associated-dementia-due-alzheimers-disease (accessed August 4, 2023).
45. EMA (European Medicines Agency). Human Medicine European Public Assessment Report (EPAR): Rxulti. Brexpiprazole, Schizophrenia, Adults. (2023). Available online at: https://www.ema.europa.eu/en/medicines/human/EPAR/rxulti (accessed August 4, 2023).
46. Watanabe Y, Yamada S, Otsubo T, Kikuchi T. Brexpiprazole for the treatment of schizophrenia in adults: an overview of its clinical efficacy and safety and a psychiatrist's perspective. Drug Des Devel Ther. (2020) 14:5559–74. doi: 10.2147/DDDT.S240859
47. Maeda K, Sugino H, Akazawa H, Amada N, Shimada J, Futamura T, et al. Brexpiprazole I: in vitro and in vivo characterization of a novel serotonin-dopamine activity modulator. J Pharmacol Exp Ther. (2014) 350:589–604. doi: 10.1124/jpet.114.213793
48. Maeda K, Lerdrup L, Sugino H, Akazawa H, Amada N, McQuade RD, et al. Brexpiprazole II: antipsychotic-like and procognitive effects of a novel serotonin-dopamine activity modulator. J Pharmacol Exp Ther. (2014) 350:605–14. doi: 10.1124/jpet.114.213819
49. Shapiro DA, Renock S, Arrington E, Chiodo LA, Liu LX, Sibley DR, et al. Aripiprazole, a novel atypical antipsychotic drug with a unique and robust pharmacology. Neuropsychopharmacology. (2003) 28:1400–11. doi: 10.1038/sj.npp.1300203
50. Kiss B, Horváth A, Némethy Z, Schmidt E, Laszlovszky I, Bugovics G, et al. Cariprazine (RGH-188), a dopamine D(3) receptor-preferring, D(3)/D(2) dopamine receptor antagonist-partial agonist antipsychotic candidate: in vitro and neurochemical profile. J Pharmacol Exp Ther. (2010) 333:328–40. doi: 10.1124/jpet.109.160432
51. Herman A, El Mansari M, Adham N, Kiss B, Farkas B, Blier P. Involvement of 5-HT1A and 5-HT2A receptors but not α2-adrenoceptors in the acute electrophysiological effects of cariprazine in the rat brain in vivo. Mol Pharmacol. (2018) 94:1363–70. doi: 10.1124/mol.118.113290
52. Mombereau C, Arnt J, Mørk A. Involvement of presynaptic 5-HT1A receptors in the low propensity of brexpiprazole to induce extrapyramidal side effects in rats. Pharmacol Biochem Behav. (2017) 153:141–6. doi: 10.1016/j.pbb.2016.12.015
53. Citrome L, Ota A, Nagamizu K, Perry P, Weiller E, Baker RA. The effect of brexpiprazole (OPC-34712) and aripiprazole in adult patients with acute schizophrenia: results from a randomized, exploratory study. Int Clin Psychopharmacol. (2016) 31:192–201. doi: 10.1097/YIC.0000000000000123
54. van Erp TG, Baker RA, Cox K, Okame T, Kojima Y, Eramo A, et al. Effect of brexpiprazole on control of impulsivity in schizophrenia: a randomized functional magnetic resonance imaging study. Psychiatry Res Neuroimaging. (2020) 301:111085. doi: 10.1016/j.pscychresns.2020.111085
55. Fervaha G, Takeuchi H, Lee J, Foussias G, Fletcher PJ, Agid O, et al. Antipsychotics and amotivation. Neuropsychopharmacology. (2015) 40:1539–48. doi: 10.1038/npp.2015.3
56. Matthews AM, Wilson VB, Mitchell SH. The role of antipsychotics in smoking and smoking cessation. CNS Drugs. (2011) 25:299–315. doi: 10.2165/11588170-000000000-00000
57. Samaha AN. Can antipsychotic treatment contribute to drug addiction in schizophrenia? Prog Neuropsychopharmacol Biol Psychiatry. (2014) 52:9–16. doi: 10.1016/j.pnpbp.2013.06.008
58. Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, et al. Comorbidity of mental disorders with alcohol and other drug abuse. results from the epidemiologic catchment area (ECA) study. JAMA. (1990) 264:2511–8. doi: 10.1001/jama.264.19.2511
59. Khokhar JY, Dwiel LL, Henricks AM, Doucette WT, Green AI. The link between schizophrenia and substance use disorder: a unifying hypothesis. Schizophr Res. (2018) 194:78–85. doi: 10.1016/j.schres.2017.04.016
60. Căpă?înă OO, Miclu?ia IV, Fadgyas-Stănculete M. Current perspectives in treating negative symptoms of schizophrenia: a narrative review (Review). Exp Ther Med. (2021) 21:276. doi: 10.3892/etm.2021.9707
61. Collins GT, France CP. Effects of lorcaserin and buspirone, administered alone and as a mixture, on cocaine self-administration in male and female rhesus monkeys. Exp Clin Psychopharmacol. (2018) 26:488–96. doi: 10.1037/pha0000209
62. Juza R, Musilek K, Mezeiova E, Soukup O, Korabecny J. Recent advances in dopamine D2 receptor ligands in the treatment of neuropsychiatric disorders. Med Res Rev. (2023) 43:55–211. doi: 10.1002/med.21923
63. Liu R, Qi J, Wang H, Fan L, Zhang P, Yu J, et al. Transformation of a dopamine D2 receptor agonist to partial agonists as novel antipsychotic agents. J Med Chem. (2023) 66:6274–87. doi: 10.1021/acs.jmedchem.3c00098
64. Bezard E, Gray D, Kozak R, Leoni M, Combs C, Duvvuri S. Rationale and development of tavapadon, a D1/D5-selective partial dopamine agonist for the treatment of Parkinson's disease. CNS Neurol Disord Drug Targets. (2023). doi: 10.2174/1871527322666230331121028
65. Martinotti G, Chiappini S, Mosca A, Miuli A, Santovito MC, Pettorruso M, et al. Atypical antipsychotic drugs in dual disorders: current evidence for clinical practice. Curr Pharm Des. (2022) 28:2241–59. doi: 10.2174/1381612828666220623092853
66. Galaj E, Bi GH, Klein B, Hempel B, Shaik AB, Gogarnoiu ES, et al. A highly D3R-selective and efficacious partial agonist (S)-ABS01-113 compared to its D3R-selective antagonist enantiomer (R)-ABS01-113 as potential treatments for opioid use disorder. Neuropsychopharmacology. (2022) 47:2309–18. doi: 10.1038/s41386-022-01379-1
67. Gogarnoiu ES, Vogt CD, Sanchez J, Bonifazi A, Saab E, Shaik AB, et al. Dopamine D3/D2 receptor ligands based on cariprazine for the treatment of psychostimulant use disorders that may be dual diagnosed with affective disorders. J Med Chem. (2023) 66:1809–34. doi: 10.1021/acs.jmedchem.2c01624
68. Nickols JER, Dursun SM, Taylor AMW. Preclinical evidence for the use of the atypical antipsychotic, brexpiprazole, for opioid use disorder. Neuropharmacology. (2023) 233:109546. doi: 10.1016/j.neuropharm.2023.109546
69. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th edn (DSM-5). Washington, DC: American Psychiatric Publishing, Inc. (2013). p. 947. doi: 10.1176/appi.books.9780890425596
70. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th edition-Text Revision (DSM-5-TR). Washington, DC: American Psychiatric Publishing, Inc. (2022). p. 1120.
71. Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, et al. The Columbia–suicide severity rating scale: Initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. (2011) 168:1266–77. doi: 10.1176/appi.ajp.2011.10111704
72. Wechsler DA. Wechsler Adult Intelligence Scale, 4th ed. San Antonio, TX: Psychological Corporation (2008). p. 328. doi: 10.1037/t15169-000
73. First MB, Williams JBW, Karg RS, Spitzer RL. Structured Clinical Interview for DSM-5 Disorders-Clinician Version SCID-5-CV. Washington DC: American Psychiatric Association Publishing, Inc. (2016). p. 170.
74. Guy W. Clinical Global Impressions. ECDEU Assessment Manual for Psychopharmacology—Revised. Rockville, MD: U.S. Department of Health, Education, and Welfare; Public Health Service, Alcohol; Drug Abuse, and Mental Health Administration; National Institute of Mental Health; Psychopharmacology Research Branch; Division of Extramural Research Programs (1976). p. 218–22.
75. Ventura J, Lukoff D, Nuechterlein KH, Liberman RP, Green M, Shaner A. Training and quality assurance with the Brief psychiatric rating scale: “the drift busters” appendix 1: Brief Psychiatric Rating Scale (BPRS) expanded version (40) scales, anchor points and administration manual. Int J Methods Psychiatr Res. (1993) 3:221–44.
76. Roncone R, Ventura J, Impallomeni M, Falloon IR, Morosini PL, Chiaravalle E, et al. Reliability of an Italian standardized and expanded Brief Psychiatric Rating Scale (BPRS 40) in raters with high vs low clinical experience. Acta Psychiatr Scand. (1999) 100:229–36. doi: 10.1111/j.1600-0447.1999.tb10850.x
77. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. (1987) 13:261–76. doi: 10.1093/schbul/13.2.261
78. Nicholson AN. Visual analogue scales and drug effects. Br J Clin Pharmacol. (1978) 6:3–4. doi: 10.1111/j.1365-2125.1978.tb01673.x
79. Overall JE. The Brief Psychiatric Rating Scale in psychopharmacology research. In: Pichot P, Oliver-Martin R, editors. Psychological Measurements in Psychopharmacology: Modern Problems in Pharmacopsychiatry 7. Basel: Karger (1974). p. 67–78. doi: 10.1159/000395069
80. Mauri MC, Franco G, Minutillo A, Paletta S, Di Pace C, Reggiori A, et al. The switch from paliperidone long-acting injectable 1- to 3-monthly: clinical pharmacokinetic evaluation in patients with schizophrenia (preliminary data). J Clin Psychopharmacol. (2022) 42:23–30. doi: 10.1097/JCP.0000000000001484
81. Burger GK, Calsyn RJ, Morse GA, Klinkenberg WD, Trusty ML. Factor structure of the expanded Brief Psychiatric Rating Scale. J Clin Psychol. (1997) 53:451–4.
82. Picardi A, Viroli C, Tarsitani L, Miglio R, de Girolamo G, Dell'Acqua G, et al. Heterogeneity and symptom structure of schizophrenia. Psychiatry Res. (2012) 198:386–94. doi: 10.1016/j.psychres.2011.12.051
83. Shafer A, Dazzi F. Meta-analytic exploration of the joint factors of the Brief Psychiatric Rating Scale - Expanded (BPRS-E) and the positive and negative symptoms scales (PANSS). J Psychiatr Res. (2021) 138:519–27. doi: 10.1016/j.jpsychires.2021.04.016
84. Shapiro SS, Wilk MB. An analysis of variance test for normality (complete samples). Biometrika. (1965) 52:591–611. doi: 10.1093/biomet/52.3-4.591
85. Mauchly JW. Significance test for sphericity of a normal n-variate distribution. Ann Math Stat. (1940) 11:204–9. doi: 10.1214/aoms/1177731915
86. Werner FM, Covenas R. Long-term administration of antipsychotic drugs in schizophrenia and influence of substance and drug abuse on the disease outcome. Curr Drug Abuse Rev. (2017) 10:19–24. doi: 10.2174/1874473710666171020104524
87. Juckel G. Inhibition of the reward system by antipsychotic treatment. Dialogues Clin Neurosci. (2016) 18:109–14. doi: 10.31887/DCNS.2016.18.1/gjuckel
88. Kirsch P, Ronshausen S, Mier D, Gallhofer B. The influence of antipsychotic treatment on brain reward system reactivity in schizophrenia patients. Pharmacopsychiatry. (2007) 40:196–8. doi: 10.1055/s-2007-984463
89. Chambers RA, Krystal JH, Self DW. A neurobiological basis for substance abuse comorbidity in schizophrenia. Biol Psychiatry. (2001) 50:71–83. doi: 10.1016/S0006-3223(01)01134-9
90. Harris GC, Aston-Jones G. Involvement of D2 dopamine receptors in the nucleus accumbens in the opiate withdrawal syndrome. Nature. (1994) 371:155–7. doi: 10.1038/371155a0
91. Funada M, Shippenberg TS. Differential involvement of D1 and D2 dopamine receptors in the expression of morphine withdrawal signs in rats. Behav Pharmacol. (1996) 7:448–53.
92. Nielsen MØ, Rostrup E, Broberg BV, Wulff S, Glenthøj B. Negative symptoms and reward disturbances in schizophrenia before and after antipsychotic monotherapy. Clin EEG Neurosci. (2018) 49:36–45. doi: 10.1177/1550059417744120
93. Wong DF, Raoufinia A, Bricmont P, Brašić JR, McQuade RD, Forbes RA, et al. An open-label, positron emission tomography study of the striatal D2/D3 receptor occupancy and pharmacokinetics of single-dose oral brexpiprazole in healthy participants. Eur J Clin Pharmacol. (2021) 77:717–25. doi: 10.1007/s00228-020-03021-9
94. Girgis RR, Forbes A, Abi-Dargham A, Slifstein M, A. positron emission tomography occupancy study of brexpiprazole at dopamine D2 and D3 and serotonin 5-HT1A and 5-HT2A receptors, and serotonin reuptake transporters in subjects with schizophrenia. Neuropsychopharmacology. (2020) 45:786–92. doi: 10.1038/s41386-019-0590-6
95. Smelson DA, Ziedonis D, Williams J, Losonczy MF, Williams J, Steinberg ML, et al. The efficacy of olanzapine for decreasing cue-elicited craving in individuals with schizophrenia and cocaine dependence: a preliminary report. J Clin Psychopharmacol. (2006) 26:9–12. doi: 10.1097/01.jcp.0000194624.07611.5e
96. Compton MT, Furman AC, Kaslow NJ. Lower negative symptom scores among cannabis-dependent patients with schizophrenia-spectrum disorders: preliminary evidence from an African American first-episode sample. Schizophr Res. (2004) 71:61–4. doi: 10.1016/j.schres.2004.01.005
97. Carrà G, Johnson S, Crocamo C, Angermeyer MC, Brugha T, Azorin JM, et al. Psychosocial functioning, quality of life and clinical correlates of comorbid alcohol and drug dependence syndromes in people with schizophrenia across Europe. Psychiatry Res. (2016) 239:301–7. doi: 10.1016/j.psychres.2016.03.038
98. Bloch Priel S, Yitzhaky A, Gurwitz D, Hertzberg L. Cannabinoid receptor gene CNR1 is downregulated in subcortical brain samples and upregulated in blood samples of individuals with schizophrenia: a participant data systematic meta-analysis. Eur J Neurosci. (2023) 58:3540–54. doi: 10.1111/ejn.16122
99. Cavalera C, Ferrari C, Bianconi G, Bulgari V, Candini V, Carrà G, et al. Substance use disorders and violent behaviour in patients with severe mental disorders: a prospective, multicentre study. Aust N Z J Psychiatry. (2020) 54:1212–23. doi: 10.1177/0004867420963732
100. McCormick RA, Smith M. Aggression and hostility in substance abusers: the relationship to abuse patterns, coping style, and relapse triggers. Addict Behav. (1995) 20:555–62. doi: 10.1016/0306-4603(95)00015-5
101. Lassi DLS, Malbergier A, Negrão AB, Florio L, De Aquino JP, Castaldelli-Maia JM. Pharmacological treatments for cocaine craving: what is the way forward? a systematic review. Brain Sci. (2022) 12:1546. doi: 10.3390/brainsci12111546
102. Siwek M, Wojtasik-Bakalarz K, Krupa AJ, Chrobak AA. Brexpiprazole-pharmacologic properties and use in schizophrenia and mood disorders. Brain Sci. (2023) 13:397. doi: 10.3390/brainsci13030397
103. Kishi T, Ikuta T, Matsuda Y, Sakuma K, Iwata N. Aripiprazole vs. brexpiprazole for acute schizophrenia: a systematic review and network meta-analysis. Psychopharmacology. (2020) 237:1459–70. doi: 10.1007/s00213-020-05472-5
104. Yoon S, Jeon SW, Ko YH, Patkar AA, Masand PS, Pae CU, et al. Adjunctive brexpiprazole as a novel effective strategy for treating major depressive disorder: a systematic review and meta-analysis. J Clin Psychopharmacol. (2017) 37:46–53. doi: 10.1097/JCP.0000000000000622
105. Kishi T, Sakuma K, Nomura I, Matsuda Y, Mishima K, Iwata N. Brexpiprazole as adjunctive treatment for major depressive disorder following treatment failure with at least one antidepressant in the current episode: a systematic review and meta-analysis. Int J Neuropsychopharmacol. (2019) 22:698–709. doi: 10.1093/ijnp/pyz040
106. Grunze H, Csehi R, Born C, Barabássy Á. Reducing addiction in bipolar disorder via hacking the dopaminergic system. Front Psychiatry. (2021) 12:803208. doi: 10.3389/fpsyt.2021.803208
107. Peris L, Szerman N. Partial agonists and dual disorders: focus on dual schizophrenia. Front Psychiatry. (2021) 12:769623. doi: 10.3389/fpsyt.2021.769623
108. Grunze H. The role of the D3 dopamine receptor and its partial agonist cariprazine in patients with schizophrenia and substance use disorder. Expert Opin Pharmacother. (2023) 1–8. doi: 10.1080/14656566.2023.2266359
109. Cuomo I, Kotzalidis GD, de Persis S, Piacentino D, Perrini F, Amici E, et al. Head-to-head comparison of 1-year aripiprazole long-acting injectable (LAI) versus paliperidone LAI in comorbid psychosis and substance use disorder: impact on clinical status, substance craving, and quality of life. Neuropsychiatr Dis Treat. (2018) 14:1645–56. doi: 10.2147/NDT.S171002
110. Szerman N, Basurte-Villamor I, Vega P, Martinez-Raga J, Parro-Torres C, Cambra Almerge J, et al. Once-monthly long-acting injectable aripiprazole for the treatment of patients with schizophrenia and co-occurring substance use disorders: a multicentre, observational study. Drugs Real World Outcomes. (2020) 7:75–83. doi: 10.1007/s40801-020-00178-8
111. Margolese HC, Boucher M, Therrien F, Clerzius G. Treatment with aripiprazole once-monthly injectable formulation is effective in improving symptoms and global functioning in schizophrenia with and without comorbid substance use – a post hoc analysis of the ReLiAM study. BMC Psychiatry. (2022) 22:773. doi: 10.1186/s12888-022-04397-x
112. Moran LM, Phillips KA, Kowalczyk WJ, Ghitza UE, Agage DA, Epstein DH, et al. Aripiprazole for cocaine abstinence: a randomized-controlled trial with ecological momentary assessment. Behav Pharmacol. (2017) 28:63–73. doi: 10.1097/FBP.0000000000000268
113. Beresford T, Buchanan J, Thumm EB, Emrick C, Weitzenkamp D, Ronan PJ. Late reduction of cocaine cravings in a randomized, double-blind trial of aripiprazole vs perphenazine in schizophrenia and comorbid cocaine dependence. J Clin Psychopharmacol. (2017) 37:657–63. doi: 10.1097/JCP.0000000000000789
114. Vergne DE, Anton RF. Aripiprazole: a drug with a novel mechanism of action and possible efficacy for alcohol dependence. CNS Neurol Disord Drug Targets. (2010) 9:50–4. doi: 10.2174/187152710790966731
115. Schacht JP, Voronin KE, Randall PK, Anton RF. Dopaminergic genetic variation influences aripiprazole effects on alcohol self-administration and the neural response to alcohol cues in a randomized trial. Neuropsychopharmacology. (2018) 43:1247–56. doi: 10.1038/npp.2017.298
116. Ricci V, Di Salvo G, Maina G. Remission of persistent methamphetamine-induced psychosis after cariprazine therapy: presentation of a case report. J Addict Dis. (2022) 40:145–8. doi: 10.1080/10550887.2021.1945398
Keywords: antipsychotic medications, brexpiprazole, partial dopamine D2 receptor agonists, schizophrenia, substance use disorder
Citation: Lombardozzi G, Trovini G, Amici E, Kotzalidis GD, Perrini F, Giovanetti V, Di Giovanni A and De Filippis S (2023) Brexpiprazole in patients with schizophrenia with or without substance use disorder: an observational study. Front. Psychiatry 14:1321233. doi: 10.3389/fpsyt.2023.1321233
Received: 13 October 2023; Accepted: 13 November 2023;
Published: 04 December 2023.
Edited by:
Octavian Vasiliu, Dr. Carol Davila University Emergency Military Central Hospital, RomaniaReviewed by:
Vassilis Martiadis, Asl Napoli 1 Centro, ItalyCopyright © 2023 Lombardozzi, Trovini, Amici, Kotzalidis, Perrini, Giovanetti, Di Giovanni and De Filippis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ginevra Lombardozzi, Z2luZXZyYWxvbWJhcmRvenppQGdtYWlsLmNvbQ==; Georgios D. Kotzalidis, Z2lvcmdpby5rb3R6YWxpZGlzQGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.