- 1Department of Psychiatry, Faculty of Medical Sciences, University of Kragujevac, Kragujevac, Serbia
- 2Department of Hygiene and Ecology, Faculty of Medical Sciences, University of Kragujevac, Kragujevac, Serbia
- 3Department of Pharmacy, Faculty of Medical Sciences, University of Kragujevac, Kragujevac, Serbia
- 4Department of Communication Skills, Ethics, and Psychology, Faculty of Medical Sciences, University of Kragujevac, Kragujevac, Serbia
- 5Surgical Oncology Clinic, Institute for Oncology and Radiology of Serbia, Belgrade, Serbia
- 6Department of Gynecology and Obstetrics, Faculty of Medical Sciences, University of Kragujevac, Kragujevac, Serbia
- 7Department of Surgery, Faculty of Medical Sciences, University of Kragujevac, Kragujevac, Serbia
- 8Department of Internal Medicine, Faculty of Medical Sciences, University of Kragujevac, Kragujevac, Serbia
- 9Department of Ophthalmology, Faculty of Medical Sciences, University of Kragujevac, Kragujevac, Serbia
- 10Department of Philology and General Education Subjects, Faculty of Philology and Arts in Kragujevac, University of Kragujevac, Kragujevac, Serbia
- 11Internal Clinic, University Clinical Center Kragujevac, Kragujevac, Serbia
Since the end of 2019, the global spread of COVID-19 has represented a historic event that changed our way of treating patients globally. The use of long-acting injections (LAI) antipsychotics was emphasized. Our goal was to investigate the impact of COVID-19 on the frequency of prescribing LAI and compare it with a period before. All patients (198) who started LAI-risperidone or LAI-paliperidone for the period 2017–2022, in Kragujevac, the city in Central Serbia, were considered. The frequency of prescribing LAI before and during COVID-19 and the total number of prescribed LAI per year were compared. Separately, the frequency of prescribing LAI-R and the frequency of prescribing LAI-P were compared. The significant (p < 0,05) increase in the use of LAI risperidone and paliperidone was in 2020 and 2021 [per year 2017(3), 2018(6), 2019(26), 2020(75), 2021(55), and 2022(33)]. The significant (p < 0,05) increase in monthly and quarterly preparations of LAI paliperidone was in 2020 and 2021 relative to the years before the pandemic. As the pandemic weakened, the inclusion of LAI paliperidone therapy weakened during 2022. A significant increase in usage of LAI risperidone was in 2022, and in 2020 and 2021 was as it was in the period 2017–2019. During COVID-19, especially in years when COVID-19 restriction measures were stricter, there was a significant change in the application method of antipsychotic therapy in favor of LAI. Regardless of the increase in treatment costs, patients’ interests and protection were prioritized in the treatment process.
Introduction
In most countries, the COVID-19 pandemic started suddenly and without warning. The WHO labeled it a pandemic on March 11, 2020, after the first cases were identified in late December 2019 (1). The complexity of health systems worldwide and the challenges of obtaining accurate infection and immunity data contribute to the unexpected nature of COVID-19’s development. Most countries used lockdown as a containment method considering the pandemic’s severity. The pandemic has had far-reaching repercussions on our lives, as well as our jobs. Physical distancing of the general population and isolation of cases was proposed as the most effective measure of disease prevention (2). While the effects of lockdown and isolation have been extensively studied in individuals with mental health problems, the general population, special vulnerable populations, and health care providers, it was less investigated how they impacted treating trends (doses, formulations, regiment).
Disorders from the psychotic spectrum group are mostly chronic diseases that require long-term pharmacotherapy. The advent of antipsychotics in the middle of the 20th century enabled good control of the positive symptoms of schizophrenia, eliminating or reducing them to a tolerable level in as many as 70% of patients. Antipsychotic maintenance therapy is recommended indefinitely, even for those who have achieved remission after a first psychotic episode (3). Compliance with oral maintenance therapy is estimated to be only 40–60% 1 year after symptom reduction of an acute episode of schizophrenia. Inadequate adherence during the maintenance period in patients with psychotic alienation is associated with higher rates of relapses, and frequent hospitalizations, creating potentially enormous costs and burdens for the patient and his family, as well as worse long-term outcomes. The goal of developing long-acting injections antipsychotics was to establish better compliance, a stable drug dose in the blood, and improve the cognitive status and quality of life of these patients (4). The availability of LAI paliperidone and risperidone is quite wide. Namely, in Serbia patients can receive LAI risperidone in a two-week regimen and LAI paliperidone in a monthly and three-month application regimen at the expense of the insurance and without additional payment when it is recommended by specialist of psychiatry.
Due to the lockdown that we were all in, the treatment of many somatic and psychiatric disorders has changed. The COVID-19 pandemic presented a challenge for all health professionals who provide services to patients with schizophrenia and other psychotic spectrum disorders. To prevent relapses or exacerbation and their consequences, continuity of medical care is crucial for these patients. So, we found ourselves at the point where the need for increased care and restrictions of isolation collided. The LAI antipsychotics were emphasized during the COVID-19 pandemic. LAI ensures treatment continuity for a certain longer period (1 to 3 months without in-person visits). This is advantageous under specific situations which include no access to health care for a certain time such as lockdown in the pandemic. Our goal was to investigate the impact of the COVID-19 pandemic on the frequency of prescribing LAI and compare it with a period before the pandemic.
Methods
Data collection and participants
Our research involved 198 patients who started risperidone or paliperidone LAI in the period 2017–2022, in Kragujevac, city of Central Serbia. The study was conducted at the Clinic for Psychiatry, University Medical Center Kragujevac. The research was approved by the Ethics Committee of the University Clinical Center Kragujevac. Data on patients, medications, and doses were collected from the database located within the Clinic for Psychiatry, the University Clinical Center, and its long-acting injection outpatient clinic.
Inclusion and exclusion criteria
Inclusion criteria for the study were diagnosis from the spectrum of psychotic disorders confirmed by DSM-5 for which the use of LAI Risperidone and Paliperidone is registered, stable status of illness at the time of recruitment, patients treated as outpatients, having stable maintenance doses of their LAIs. Exclusion criteria were unstable (exacerbation) of illness, hospitalized patients, patients with other psychiatric comorbidities, patients with somatic comorbidities, and the use of concomitant therapy that requires frequent visits to a psychiatrist.
Statistical analysis
For the purposes of this study, comorbidities were not considered even though they are common in this population (5). We compared the trend (frequency) of prescribing LAI before and during the COVID-19 pandemic. Separately, the frequency of prescribing LAI of risperidone and the frequency of prescribing LAI paliperidone. Also, the total number of prescribed LAI per year was reached. Chi-Squared test was used to compare using of investigated drugs before and during pandemic. All data were analyzed using IBM SPSS software, version 21. The statistical significance threshold was set at 0.05.
Results
Overall, 198 patients receiving LAI paliperidone and risperidone LAI were identified. According to gender, there were 67 females and 131 males. The largest number of patients were middle-aged, 30–55 years old. In terms of education, 72% had a secondary education, 15% had a university degree, and 3% had no schooling or completed elementary school. The characteristics of the sample are shown in Table 1.
During the COVID-19 pandemic (period 2020–2022), there was a significant change in the application method of antipsychotic therapy in favor of LAI, compared to the period before the pandemic (from 2017 to 2019) (χ2 = 9,111; p = 0,011). The number of every followed dosing form by period of observation is presented in Figure 1A. Compared individually, monthly, and quarterly preparations of LAI paliperidone had a significant increase in usage, compared to LAI risperidone (χ2 = 6,215; p = 0,013). The number of patients that use any followed dosage form by year is presented in Figure 1B.
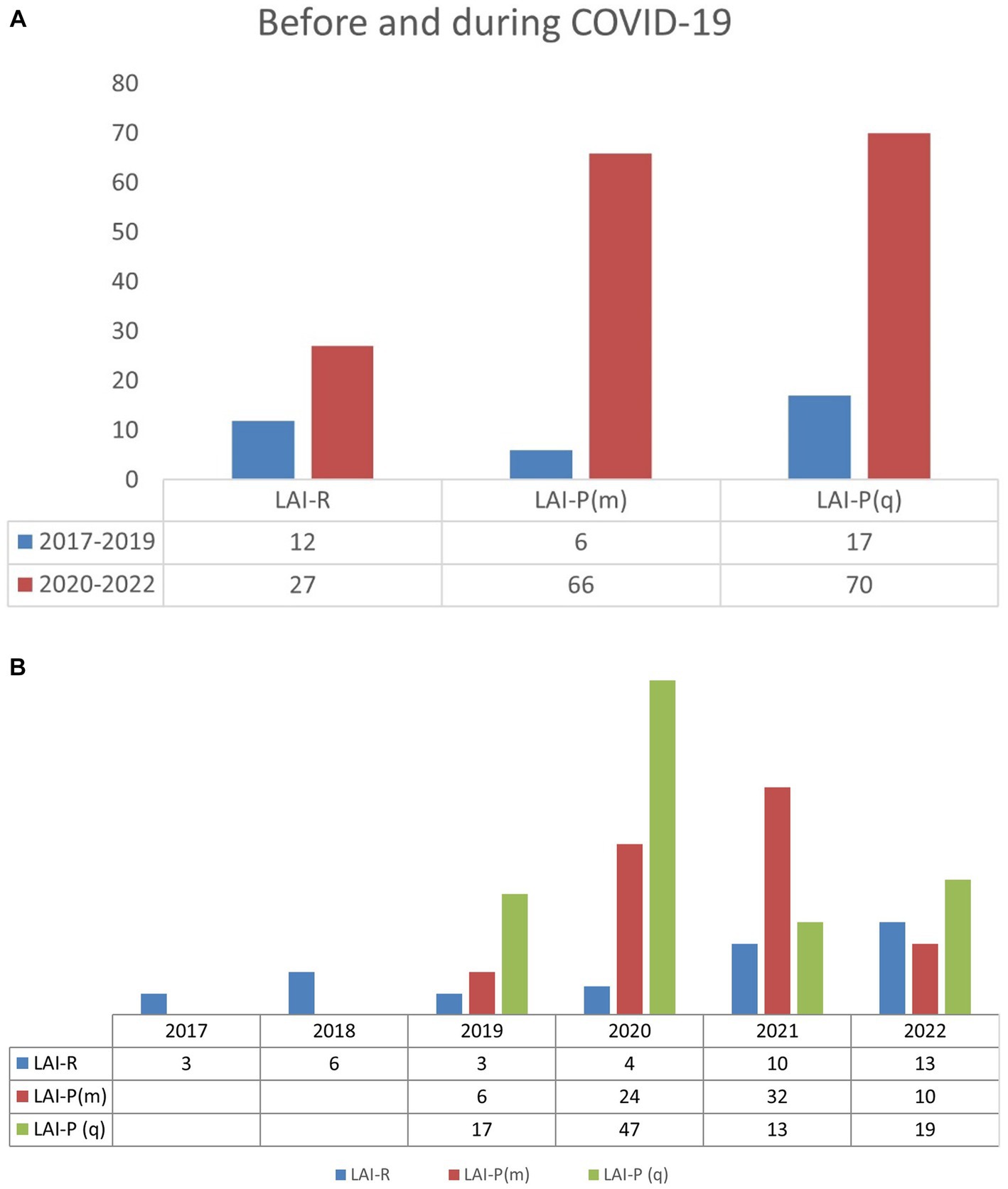
Figure 1. (A) Prescribing of LAI before and during COVID-19. (B) Prescribing of LAI before and during COVID-19. LAI-R, LAI risperidone; LAI-P(m), LAI paliperidone monthly; LAI-P(q), LAI paliperidone quarterly.
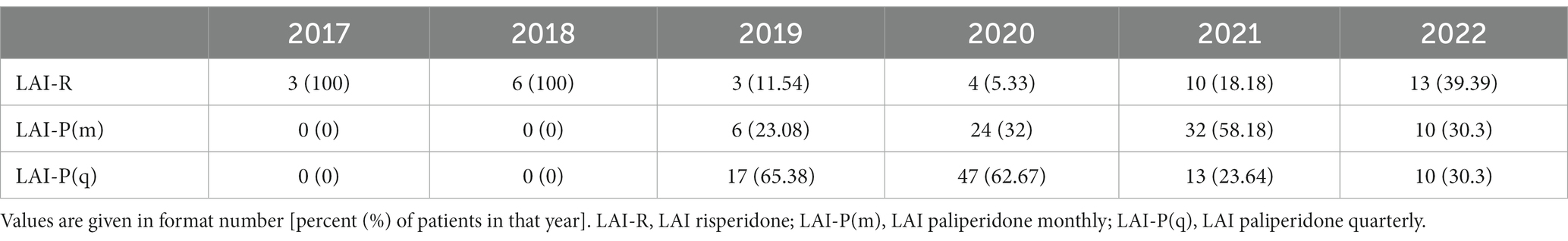
The total number of patients that were introduced to LAI risperidone and paliperidone therapy, according to the year of introduction and according to the long-acting drug that was prescribed is shown in Table 2. From the results, we can observe an increase in the use of LAI risperidone and paliperidone markedly in 2020 and 2021. Per year it was 2017(3), 2018(6), 2019(26), 2020(75), 2021(55), and 2022(33) patients.
Separately, the use of monthly and quarterly preparations of LAI paliperidone was significantly higher in 2020 and 2021 relative to the years before the pandemic (2017–2019). However, as the pandemic weakened, according to our research, the inclusion of LAI paliperidone therapy weakened during 2022. On the other hand, our results showed an increase in usage of LAI risperidone in 2022. There was not a significant difference in 2020 and 2021 compared to the period 2017–2019. The trend lines of usage of every followed dosage form are presented in Figure 2.
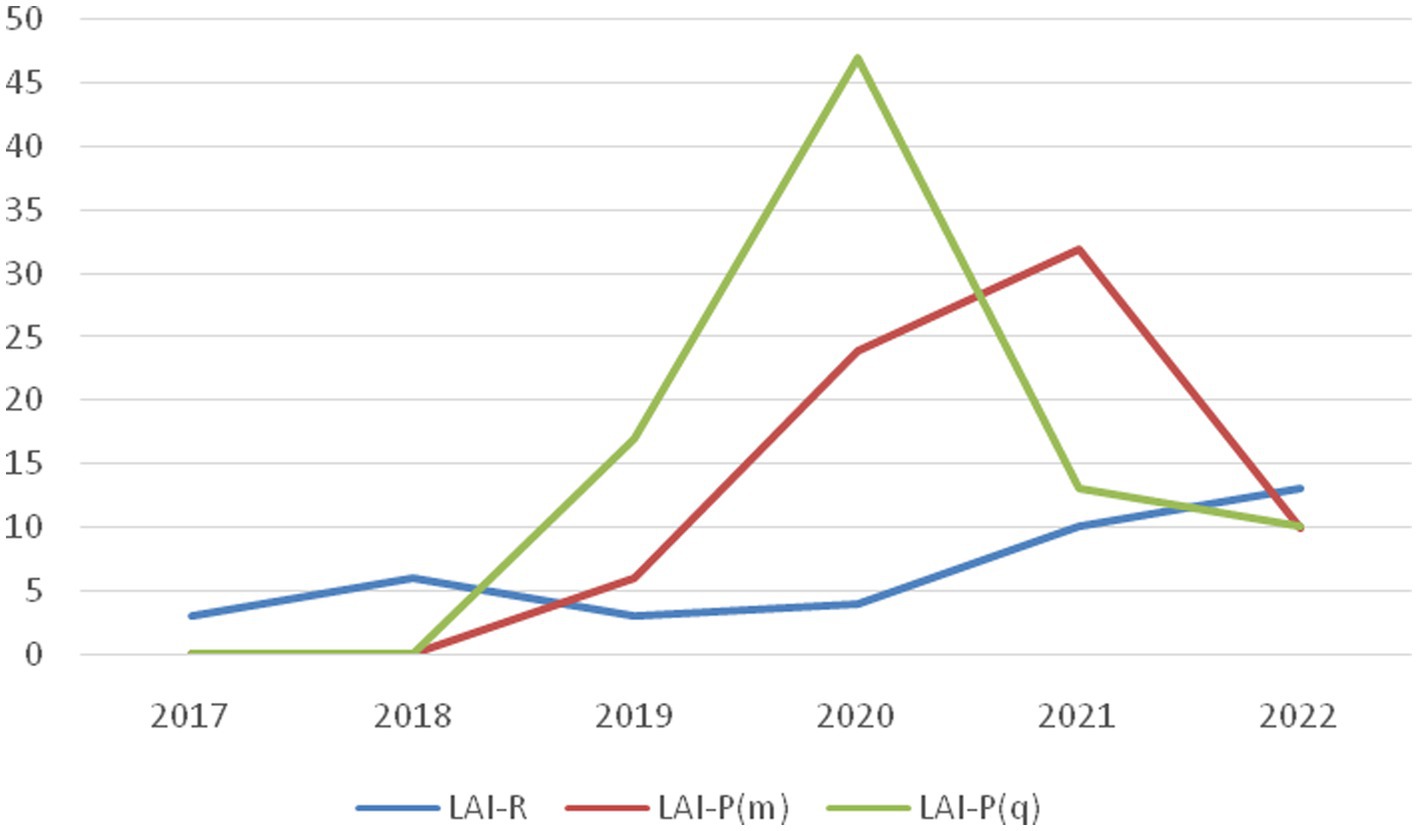
Figure 2. Comparison of drug prescriptions by year. LAI-R, LAI risperidone; LAI-P(m), LAI paliperidone monthly; LAI-P(q), LAI paliperidone quarterly.
Discussion
Our results indicated that during the COVID-19 pandemic a significant change in the application method of antipsychotic therapy favoring LAI antipsychotic therapy. LAI paliperidone had a significant increase in usage during the pandemic, while LAI risperidone was prescribed less during the pandemic. The reason for the increase in the use of medication that requires less frequent visits to health facilities should be sought in an attempt to reduce the risk of infection and consequent damage. By using these LAI, the number of patients contacts (GP, psychiatrist, nurses, pharmacist, other patients…) was significantly reduced, practically protecting them. This fact is confirmed by the data that two-week visits were on the decline in favor of monthly and quarterly visits. To our knowledge, this is the only study that compared the prescribing of LAI risperidone and LAI paliperidone before and during the coronavirus pandemic. During the literature search, we found some other studies that compared LAI of other and different antipsychotics.
Comparison with previous studies
There are many changes that the coronavirus pandemic leads to. New techniques and methods were proposed to prevent the spreading of the virus and protect us and patients from the disease. In the literature search, there is one study that shows an increase in the use of LAI antipsychotics, they observed the use of LAI aripiprazole compared to LAI risperidone (6). A statistically significant and consistent increase in weekly aripiprazole depot mentions from March 2020 to September 2020 was observed. Risperidone depot mentions were reduced in March, June, August, and September 2020, which is consistent with our findings.
A previous study on this topic was based on creating programs that provide telehealth services to patients with schizophrenia, improving communication with patients, and promoting telepsychiatry as a new method of care during the pandemic. The onset of the COVID-19 pandemic was associated with a rapid and major shift in the mode of mental healthcare consultations. Early on, in-person visits were switched to remote (online) visits, then afterward switched back to in-person mode. They showed that the incidence of missed appointments decreased as appointments changed from in-person to remote between April and June. Telepsychiatry was suggested as a great option for many mental health problems, but schizophrenia is not one of them due to the lack of insight of these patients about their medical condition (7). During the COVID-19 pandemic, there was flourishing international scientific production, and a large percentage of published articles with data often collected through surveys or telemedicine, which have been adapted due to the impossibility of physical contact during the lockdown period (8).
Clinical implications
LAI antipsychotics were suggested as a mainstay in the treatment of schizophrenia and related psychotic spectrum disorders because of their prolonged effect and consequent prevention of nonadherence that results in relapses and hospitalizations (9). The clinically meaningful superiority of depot medication compared to oral antipsychotics in patients with schizophrenia has been confirmed by the findings that depot formulations significantly reduced relapses from an average of 33.2 to 21.5% (10). Their usage was justified during the pandemic, even if these visits may increase the risk of infection for patients and providers (11). Although schizophrenia is considered a rare disorder, the main problem is its early onset, the chronic nature, and the course of the disease, which presents with exacerbations, frequent progressive worsening, and high comorbidity. Pharmacoeconomically the disease represents a heavy burden on society. In global consumption, direct costs related to treatment represent the lowest proportion. On the other hand, indirect costs, which are an expression of the effects of disorders and effects on care costs, occupy about 60–65% of costs (12). Adequate adherence to a treatment plan is crucial for successful mental healthcare management. For patients diagnosed with schizophrenia and another psychotic spectrum, failure to attend outpatient care following admission increases the risk of relapse and rehospitalization, which relates to larger additional medical costs. The highest costs relate to hospitalization (52.5 – 80.7% of the total costs of care). Adherence is closely related to relapses and hospitalization, as these patients will inevitably relapse at some point after drug discontinuation (13).
According to previous systematic reviews, the patient’s adherence to LAI paliperidone and LAI risperidone was slightly higher compared to oral antipsychotics, and traditional depots, although they are considerably less expensive than injectable drugs, cost the most overall for patient care due to their lower rates of effectiveness and adherence (14). Moreover, it was shown that LAI paliperidone was associated with a lower risk of healthcare resource utilization compared to oral antipsychotic therapy: in the LAI paliperidone group, the risk of an inpatient hospital admission and mental-health-related utilization was statistically lower (both p < 0.0001), as well as the risk of an emergency department visits (15). These results support the fact that the use of LAI antipsychotics during the COVID-19 pandemic is one of the good measures to prevent relapse. Patients who come in at two-week, monthly, or three-month intervals are at a lower risk of getting an infection, compared to patients who are on oral therapy (16).
Pharmacoeconomic implications
There are many studies concerning the pharmacoeconomic aspects of the use of LAI antipsychotics. Compared to oral medications in a recently diagnosed group, the use of LAI paliperidone is related to higher pharmacy costs (17) Furthermore, it was shown that monthly prescription drug costs for the LAI paliperidone group were higher than the oral antipsychotic therapy group, both for all-cause pharmacy costs (p < 0.0001) and mental-health-related costs (p < 0.0001) (15).
On the other hand, a higher percent (about 55%) of the mental-health-related prescription drug cost associated with LAI paliperidone was offset by lower costs of mental-health-related inpatient and outpatient care and the (p < 0.0001) (15). The economic impact on the budget of prescribing LAI paliperidone appears advantaged compared to the use of oral antipsychotics, also considering second-generation antipsychotics (16). Despite a common active ingredient, treatment with LAI paliperidone represents a cost-effective choice over LAI risperidone. The therapy with LAI paliperidone has shown better treatment patterns, improvements in adherence, lower discontinuation rates, as well as a longer period of days of LAI coverage (18, 19).
Furthermore, many studies conducted across the world confirmed the advantage of LAI paliperidone’s better therapy pattern compared to LAI risperidone for treating patients with schizophrenia because of clinical and economic advantages. The lower overall cost to the healthcare system and greater clinical benefits were confirmed. The higher price of the drug was more than offset by savings accrued from less frequent drug administration and higher adherence rates. Overall, the cost of treatment has shown slightly lower for the healthcare system when PP-LAI was used, despite a higher acquisition cost (10, 20–22).
WHO reported higher health spending in response to the global COVID-19 pandemic. In 2020 reached US$ 9 trillion, or 10.8% of global gross domestic product, and was highly unequal across income groups. Higher health spending was an indicator of the priority given to health, which increased from 2019 to 2020 in all income groups except high-income countries (23).
Limitations
This study was conducted at the University Clinical Center Kragujevac and the Faculty of Medical Sciences, and it is a local investigation. The study is limited to one center and a part of a country in Central Serbia, which may not be representative of broader prescribing patterns. The small sample of included patients, and the little ability to monitor other variables such as drug availability, patient preferences, clinician biases, comorbidities, or previous treatment history.
Future implications
These trends can be significant in the future in the next potentially major crisis. Moreover, we can conduct surveys from the perspective of patients and their satisfaction with these prescribing trends. It is also possible to monitor the quality of life of these patients with such trends. This study can serve as an initial study for a more detailed pharmacoeconomic study and its impact on the improvement of health care.
Conclusion
Our results showed that the use of LAI paliperidone in relation to the use of LAI risperidone increased during the lockdown period of COVID-19. One of the reasons can be that LAI paliperidone requires less frequent visits to the health clinic and therefore the patient’s exposure to risk factors is lower. Regardless of the highest pharmacy costs of LAI antipsychotics compared to oral medications, during the COVID-19 pandemic, we can assume that the safety of the patients was a priority in the treatment process. During the pandemic period, especially in years when COVID-19 restriction measures were stricter usage of therapy that allows the patients to visit the clinic less often was on the rise. In the long term, the lower overall cost to the healthcare system and greater clinical benefits were previously confirmed, and our system was able to provide more care with the same budget.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Ethics Committee of the University Clinical Center Kragujevac. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
MiS: Conceptualization, Data curation, Methodology, Writing – original draft, Writing – review & editing. MaS: Supervision, Writing – review & editing. MJ: Methodology, Writing – review & editing. AK: Methodology, Writing – review & editing. DD: Writing – review & editing. NM: Methodology, Supervision, Writing – original draft, Writing – review & editing. MD: Writing – review & editing. SJ: Writing – review & editing. MSo: Writing – review & editing. BS: Writing – review & editing. SS: Writing – review & editing. AC: Writing – review & editing. TS: Writing – review & editing. OR: Writing – review & editing. BR: Methodology, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
This study was part of a bigger study conducted at the University Clinical Center Kragujevac and the Faculty of Medical Sciences. The authors thank Nikola Subotic MD for his support, helpful suggestions, and language.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1301835/full#supplementary-material
References
1. Cucinotta, D, and Vanelli, M. WHO declares COVID-19 a pandemic. Acta Biomed. (2020) 91:157. doi: 10.23750/abm.v91i1.9397
2. Moreno, C, Wykes, T, Galderisi, S, Nordentoft, M, Crossley, N, Jones, N, et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry. (2020) 7:813–24. doi: 10.1016/S2215-0366(20)30307-2
3. Pietrini, F, D’Anna, G, Tatini, L, Talamba, GA, Andrisano, C, Calderani, E, et al. Changes in attitude towards LAI antipsychotic maintenance treatment: a two-year follow-up study. Eur Psychiatry. (2018) 53:58–65. doi: 10.1016/j.eurpsy.2018.06.002
4. Pietrini, F, Albert, U, Ballerini, A, Calò, P, Maina, G, Pinna, F, et al. The modern perspective for long-acting injectables antipsychotics in the patient-centered care of schizophrenia. Neuropsychiatr Dis Treat. (2019) 15:1045–60. doi: 10.2147/NDT.S199048
5. Nishanth, KN, Chadda, RK, Sood, M, Biswas, A, and Lakshmy, R. Physical comorbidity in schizophrenia & its correlates. Indian J Med Res. (2017) 146:281. doi: 10.4103/ijmr.IJMR_1510_15
6. Patel, R, Irving, J, Brinn, A, Broadbent, M, Shetty, H, Pritchard, M, et al. Impact of the COVID-19 pandemic on remote mental healthcare and prescribing in psychiatry: an electronic health record study. BMJ Open. (2021) 11:e046365. doi: 10.1136/bmjopen-2020-046365
7. Kozloff, N, Mulsant, BH, Stergiopoulos, V, and Voineskos, AN. The COVID-19 global pandemic: implications for people with schizophrenia and related disorders. Schizophr Bull. (2020) 46:752–7. doi: 10.1093/schbul/sbaa051
8. de Filippis, R, El Hayek, S, and Shalbafan, M. Mental illness, culture, and society: dealing with the COVID-19 pandemic. Front Psych. (2022) 13:1073768. doi: 10.3389/fpsyt.2022.1073768
9. Correll, CU, Kim, E, Sliwa, JK, Hamm, W, Gopal, S, Mathews, M, et al. Pharmacokinetic characteristics of long-acting injectable antipsychotics for schizophrenia: an overview. CNS Drugs. (2021) 35:39–59. doi: 10.1007/s40263-020-00779-5
10. Einarson, TR, Geitona, M, Chaidemenos, A, Karpouza, V, Mougiakos, T, Paterakis, P, et al. Pharmacoeconomic analysis of paliperidone palmitate for treating schizophrenia in Greece. Ann General Psychiatry. (2012) 11:18. doi: 10.1186/1744-859X-11-18
11. Correll, CU, Citrome, L, Haddad, PM, Lauriello, J, Olfson, M, Calloway, SM, et al. The use of long-acting injectable antipsychotics in schizophrenia: evaluating the evidence. J Clin Psychiatry. (2016) 77:1–24. doi: 10.4088/JCP.15032su1
12. Tajima-Pozo, K, de Castro Oller, MJ, Lewczuk, A, and Montañes-Rada, F. Understanding the direct and indirect costs of patients with schizophrenia. F1000Res. (2015) 4:182. doi: 10.12688/f1000research.6699.1
13. Ascher-Svanum, H, Zhu, B, Faries, DE, Salkever, D, Slade, EP, Peng, X, et al. The cost of relapse and the predictors of relapse in the treatment of schizophrenia. BMC Psychiatry. (2010) 10:1–7. doi: 10.1186/1471-244X-10-2
14. Einarson, TR, Vicente, C, Zilbershtein, R, Piwko, C, Bø, CN, Pudas, H, et al. Pharmacoeconomics of depot antipsychotics for treating chronic schizophrenia in Sweden. Nord J Psychiatry. (2014) 68:416–27. doi: 10.3109/08039488.2013.852243
15. Pesa, JA, Muser, E, Montejano, LB, Smith, DM, and Meyers, OI. Costs and resource utilization among Medicaid patients with schizophrenia treated with paliperidone palmitate or oral atypical antipsychotics. Drugs Real World Outcomes. (2015) 2:377–85. doi: 10.1007/s40801-015-0043-4
16. Valsecchi, P, Barlati, S, Garozzo, A, Deste, G, Nibbio, G, Turrina, C, et al. Paliperidone palmitate in short-and long-term treatment of schizophrenia. Riv Psichiatr. (2019) 54:235–48. doi: 10.1708/3281.32542
17. Pilon, D, Muser, E, Lefebvre, P, Kamstra, R, Emond, B, and Joshi, K. Adherence, healthcare resource utilization and Medicaid spending associated with once-monthly paliperidone palmitate versus oral atypical antipsychotic treatment among adults recently diagnosed with schizophrenia. BMC Psychiatry. (2017) 17:1–8. doi: 10.1186/s12888-017-1358-3
18. Joshi, K, Pan, X, Wang, R, Yang, E, and Benson, C. Healthcare resource utilization of second-generation long-acting injectable antipsychotics in schizophrenia: risperidone versus paliperidone palmitate. Curr Med Res Opin. (2016) 32:1873–81. doi: 10.1080/03007995.2016.1219706
19. Luther, K, Fung, GM, and Khorassani, F. Cost comparison of atypical antipsychotics: paliperidone ER and risperidone. Hosp Pharm. (2019) 54:389–92. doi: 10.1177/0018578718809269
20. Zeidler, J, Mahlich, J, Greiner, W, and Heres, S. Cost effectiveness of paliperidone palmitate for the treatment of schizophrenia in Germany. Appl Health Econ Health Policy. (2013) 11:509–21. doi: 10.1007/s40258-013-0050-0
21. Einarson, TR, Pudas, H, Goswami, P, van Impe, K, and Bereza, BG. Pharmacoeconomics of long-acting atypical antipsychotics for acutely relapsed chronic schizophrenia in Finland. J Med Econ. (2016) 19:121–30. doi: 10.3111/13696998.2015.1100115
22. Druais, S, Doutriaux, A, Cognet, M, Godet, A, Lançon, C, Levy, P, et al. Cost effectiveness of paliperidone long-acting injectable versus other antipsychotics for the maintenance treatment of schizophrenia in France. PharmacoEconomics. (2016) 34:363–91. doi: 10.1007/s40273-015-0348-x
23. World Health Organization. Global spending on health: rising to the pandemic’s challenges World Health Organization (2022) Available at: https://www.who.int/publications/i/item/9789240064911.
Keywords: COVID-19 pandemic, LAI risperidone, LAI paliperidone, mental health, psychotic disorders
Citation: Stojkovic M, Sekulic M, Jovanovic M, Kocovic A, Djokovic D, Minic N, Djordjic M, Joksimovic S, Sorak M, Stojanovic B, Sretenovic S, Cvetkovic A, Stojanovic T, Radmanovic O and Radmanovic B (2023) The impact of the COVID-19 pandemic on the trend of prescribing long-acting injections of paliperidone and risperidone in Central Serbia. Front. Psychiatry. 14:1301835. doi: 10.3389/fpsyt.2023.1301835
Edited by:
Mohammadreza Shalbafan, Iran University of Medical Sciences, IranCopyright © 2023 Stojkovic, Sekulic, Jovanovic, Kocovic, Djokovic, Minic, Djordjic, Joksimovic, Sorak, Stojanovic, Sretenovic, Cvetkovic, Stojanovic, Radmanovic and Radmanovic. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marija Sekulic, bXNla3VsaWM4MkBnbWFpbC5jb20=
 Milena Stojkovic
Milena Stojkovic Marija Sekulic
Marija Sekulic Mirjana Jovanovic
Mirjana Jovanovic Aleksandar Kocovic
Aleksandar Kocovic Danijela Djokovic1
Danijela Djokovic1 Milan Djordjic
Milan Djordjic Bojan Stojanovic
Bojan Stojanovic Branimir Radmanovic
Branimir Radmanovic