- 1Sichuan Provincial Center for Mental Health, Sichuan Academy of Medical Sciences & Sichuan Provincial People's Hospital, Chengdu, China
- 2Key Laboratory of Psychosomatic Medicine, Chinese Academy of Medical Sciences, Chengdu, China
Background: Sexual dysfunction is commonly observed in individuals with Major Depressive Disorder (MDD), along with various psychological symptoms such as anxiety, somatic complaints, interpersonal sensitivity, and obsessive-compulsive tendencies. However, there is a research gap in understanding the impact of these psychological symptoms on sexual functioning in MDD. Furthermore, there is limited data on the incidence of sexual dysfunction among drug-naive MDD patients in West China. This study aims to determine the prevalence of sexual dysfunction in this patient population and explore its association with other psychological indicators.
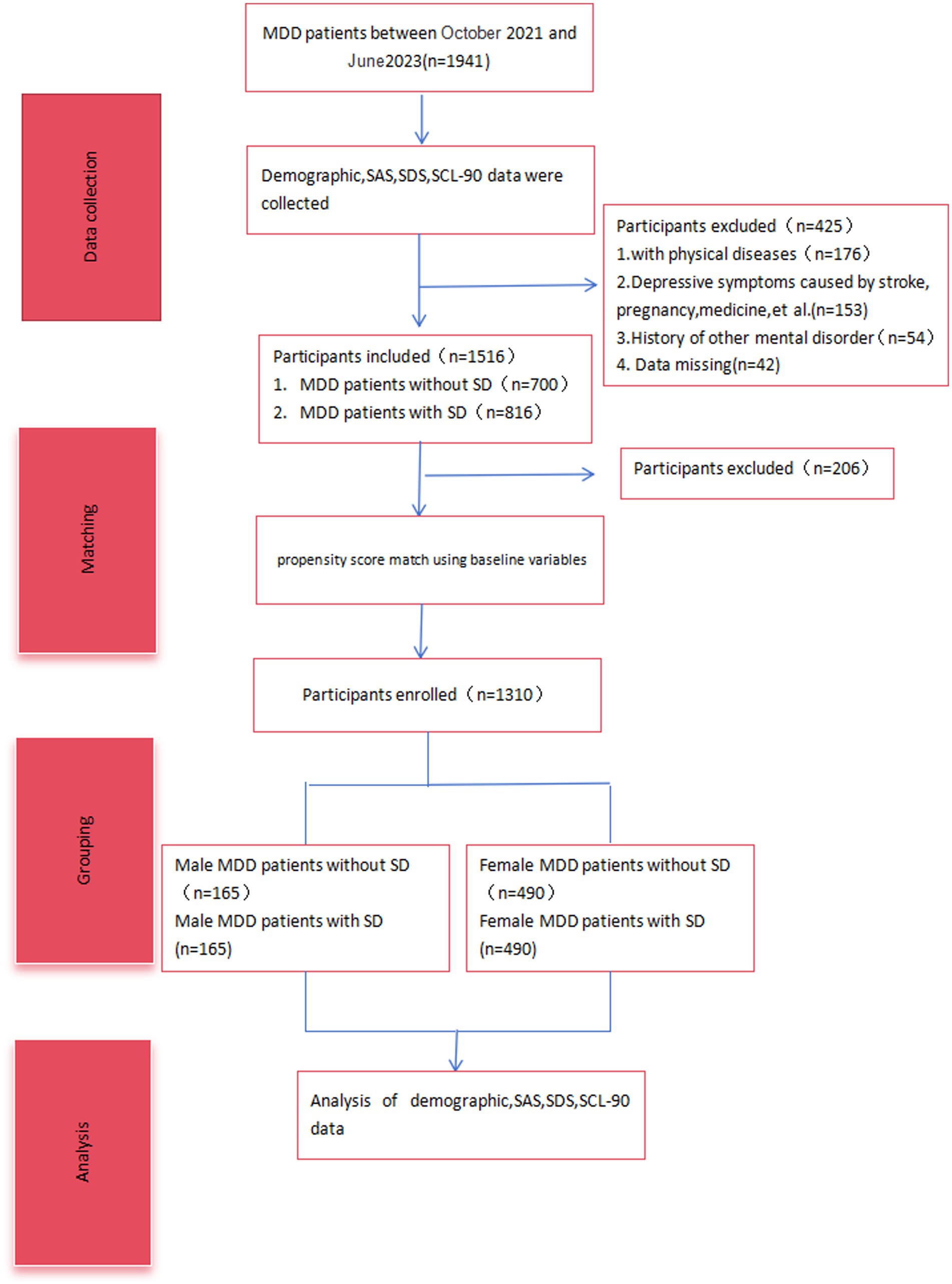
Methods: We conducted a retrospective analysis of patient data from October 2020 to September 2022 using propensity score matching. A focused group of 165 males and 490 females was selected from a total of 1941 MDD patients. This allowed for a comparative analysis of demographic data, as well as scores from the Self-Rating Depression Scale (SDS), Self-Rating Anxiety Scale (SAS), and Symptom Checklist-90 (SCL-90), the Arizona Sexual Experience Scale (ASEX).
Results: Our findings reveal that 46.2% of drug-naive MDD patients experienced sexual dysfunction. Notably, there was a higher prevalence of sexual dysfunction among female patients (50.3%) compared to males (37.5%). MDD patients without sexual dysfunction consistently exhibited higher SDS scores than those with sexual dysfunction (p < 0.01), There were no statistically significant differences between male and female MDD patients with or without concomitant sexual dysfunction in terms of Somatic complaints, Obsessive-compulsive, Interpersonal sensitivity, Anxiety, Phobic anxiety, Paranoid ideation, Psychoticism and Diet/sleep difficulties (p > 0.05). In addition, male MDD patients with sexual dysfunction showed a emerging trend towards elevated Hostility scores on the SCL-90 (p = 0.058), male MDD patients with sexual dysfunction showed an increasing trend in hostility scores on the SCL-90, whereas female MDD patients with sexual dysfunction did not show such a trend.
Conclusion: The study highlights a significant gender difference in the prevalence of sexual dysfunction among MDD patients, with females being more susceptible than males. There is a positive correlation between the severity of depression and sexual dysfunction in both genders. Interestingly, male MDD patients demonstrated a potential protective effect of hostility against sexual dysfunction, which was not observed in female patients.
1 Introduction
Major Depressive Disorder (MDD) is a widespread mental illness observed worldwide. In the United States, the prevalence of MDD is 10.4% for a duration of 12 months and 20.6% over a lifetime (1). In China, MDD takes precedence as the primary mood disorder, with a lifetime prevalence of 3.4% and a 12-month prevalence of 2.1% (2). The impact of the COVID-19 pandemic has further exacerbated this situation, resulting in a significant increase in depression rates (3, 4). Among mental health conditions, MDD stands out as a key contributor to mortality and disability in the general population. When measured in terms of “years lived with disability,” MDD ranks second as the leading cause of chronic disease burden (5). Moreover, MDD is associated with a higher risk of chronic medical ailments such as diabetes, heart disease, and stroke (6), amplifying its overall impact on disease burden. Tragically, MDD can lead to suicide, with individuals suffering from depression being approximately 20 times more likely to die by suicide compared to the general population (7).
Sexual dysfunction impacts around 43% of females and 31% of males (8) and is a significant comorbidity for depressive symptoms. Its identification as a sign of major depressive disorder (MDD) is apparent in standardized forms for rating depression that include a question evaluating the loss of interest in sexual activities. The connection between sexual dysfunction and depression is cyclical; the former raises the risk for the latter by 2.3 to 3.1-fold (9). 25 to 75% of individuals with depression experience sexual dysfunction, with the intensity of symptoms corresponding to the severity of the depression (10). Treatments for depression, particularly selective serotonin reuptake inhibitors (SSRIs), are linked to a 70% rise in the occurrence of treatment-associated sexual dysfunction (11). Although the usage of antidepressants may influence studies on sexual function (12, 13), many sexual symptoms decrease as mental well-being improves. Various researchers have evaluated the prevalence of sexual dysfunction in patients with MDD (14–16), but there is a scarcity of empirical research, particularly in Western China, on individuals with untreated MDD.
Depression often occurs together with various psychological factors, which can also affect reported sexual problems. These psychological factors include physical symptoms, worry, aggression, and changes in eating or sleeping behaviors, among other things (17–20). While numerous studies have focused on depression, research on depression coexisting with psychological symptoms is still in its early stages. It is crucial to distinguish and explore the various complex psychological aspects that could potentially impact sexual dysfunction. The connection between sexual dysfunction and demographic characteristics, such as age and education (7, 21), further complicates the study of MDD patients with concurrent sexual dysfunction. Given the intricate relationship between sexual dysfunction and MDD in patients. The objective of this study is to determine the prevalence of sexual dysfunction among drug-naive patients with Major Depressive Disorder (MDD) in West China and to explore its association with various psychological symptoms through the use of propensity score matching. These symptoms include, but are not limited to, anxiety, somatic complaints, interpersonal sensitivity, and obsessive-compulsive tendencies. The study aims to fill the research gap in understanding the impact of these psychological factors on sexual functioning in MDD patients and contribute to the limited data on this subject in the context of West China.
2 Methods
2.1 Participants and study design
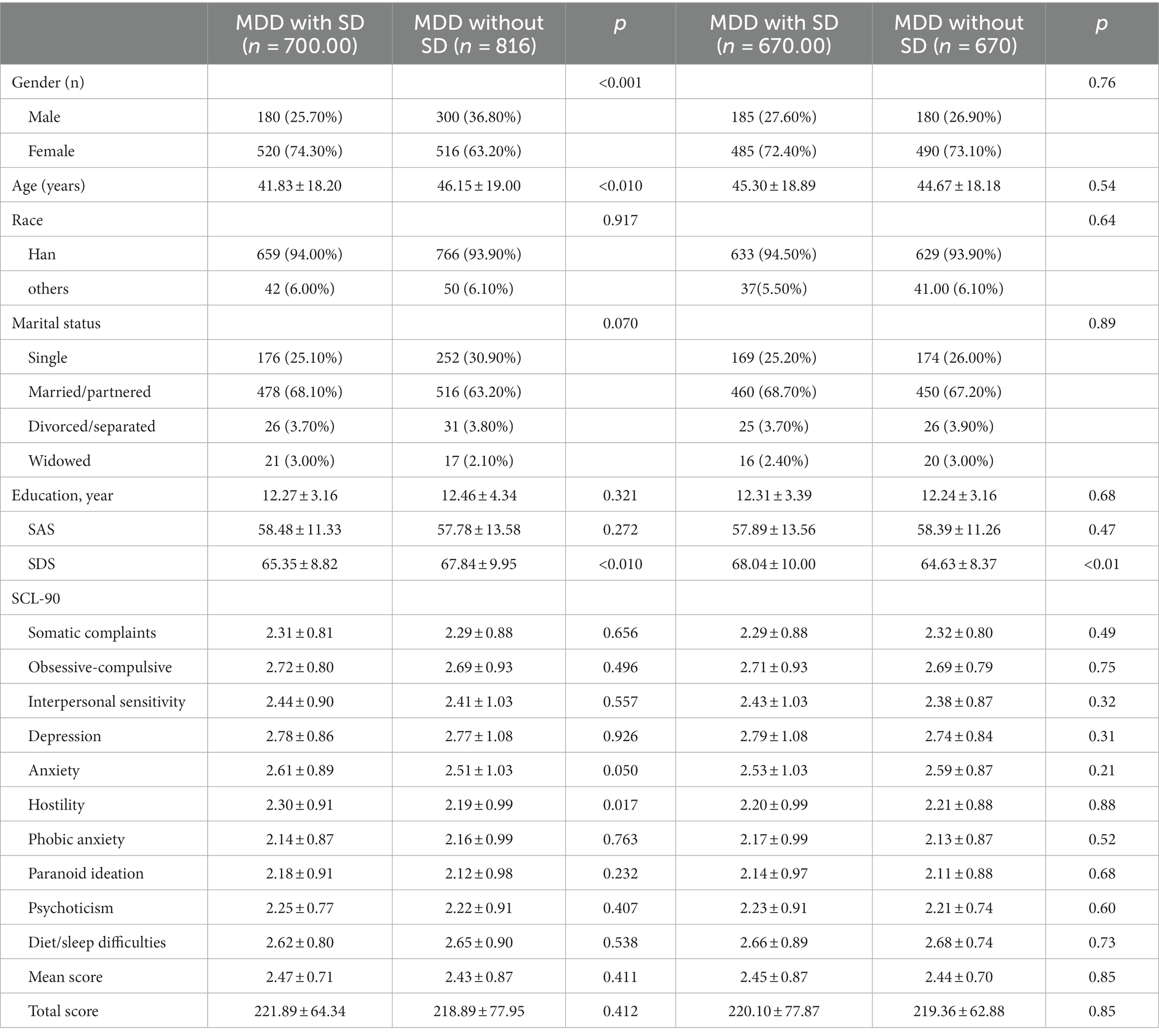
The design of this study is a retrospective cohort conducted at a single center. The Ethics Committee of Sichuan Provincial People’s Hospital approved the study in 2020, and the ethics committees of all participating entities provided further endorsement (approval number: Res-2020-290). To ensure participant confidentiality, all identifying details such as names were anonymized. Table 1 presents the data from October 2020 to September 2022, where the Sichuan Provincial Center for Mental Health attended to a total of 1,941 individuals with Major Depressive Disorder (MDD). Inclusion criteria for this study were as follows: (1) Meeting the diagnostic criteria for MDD outlined in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, and confirmation of diagnosis by two experienced psychiatrists. (2) No presence of significant physical illness, bipolar affective disorder with depressive episodes, other psychiatric disorders, or immune or endocrine system-related diseases. (3) Absence of recent infections or vaccinations. Participants were excluded if they: (1) Demonstrated depressive symptoms associated with physical health issues or other psychiatric disorders. (2) Had severe physical conditions. (3) Had a history of other psychiatric disorders and substance abuse. (4) Were currently taking antidepressant medications or drugs that enhance sexual performance.
2.2 Source of data
We gathered baseline demographic and clinical information. We assessed the severity of depression and anxiety using the Self-Depression Scale (SDS) and the Self-Rating Anxiety Scale (SAS) respectively. Psychological symptoms were evaluated using the Symptom Checklist-90 (SCL-90), and sexual dysfunction (SD) was screened using the Arizona Sexual Experience Scale (ASEX). Self-Rating Anxiety Scale (SAS): The SAS measures levels of anxiety and mood over the previous week with 20 items divided into four categories. An overall score of 20, multiplied by 1.25, reflects the severity of anxiety. This tool has good internal consistency with a Cronbach’s alpha of 0.821 (22). Self-Depression Scale (SDS): We used the SDS to assess the degree of depression in each participant. It consists of 20 items that are rated on a scale from 1 to 4, with higher scores indicating more frequent symptoms. Higher scores suggest more severe depressive symptoms (23). Symptom Checklist-90 (SCL-90): This questionnaire comprises ten factors, with each item graded based on the severity of symptoms. A total score above 160 points or factor scores of ≥2 indicate significant symptoms, with higher scores suggesting severe psychiatric issues (24). Arizona Sexual Experience Scale (ASEX): This scale assesses five domains of sexual function, categorizing SD based on specific criteria. We chose the Chinese ASEX version due to its effectiveness in Chinese individuals with Major Depressive Disorder (MDD), and it has a Cronbach’s alpha of 0.85 (25).Sexual dysfunction is defined as (i) a total ASEX score of 19 or above, (ii) any item with a score of 5 or above, or (iii) any three items with a score of 4 or above. The ASEX is a reliable, valid, and sensitive tool to measure SD in both males and females. All participants received guidance from a psychiatrist before completing the scale.
2.3 Methods for statistical analysis
The statistical analysis of the study results was conducted using SPSS 27.0. All study outcomes were presented using mean ± standard deviations or n (%). In order to accurately compare the different groups (MDD without SD vs. MDD with SD), both qualitative and quantitative variables were analyzed using χ2 or independent sample t-tests, respectively. To minimize any influences from confounding factors and systematic biases, the statistical analyses incorporated Propensity Score Matching (PSM). By utilizing PSM, the baseline characteristics of the MDD groups (with and without SD) were balanced. Binary logistic regression was employed to identify factors contributing to the incidence of MDD with SD. Statistical significance was considered when the p-value was less than 0.05.
3 Results
3.1 Description of overall sample
Out of the initial 1,941 patients that were approached, a total of 1,516 participants were suitable for analysis after excluding 425 patients for various reasons. These reasons included physical illnesses (n = 176), depressive symptoms caused by external factors like stroke, medication, or pregnancy (n = 153), a history of other mental disorders (n = 54), and missing data (n = 42). The final group for this study consisted of 1,036 females and 480 males, with an average age of 43.8 ± 18.7 years (age range from 18 to 88 years). Of these MDD patients, a predominant 93.9% (n = 1,424) were of Han Chinese ethnicity, while the remaining 6.1% (n = 92) belonged to various other ethnic groups. Regarding marital status, the majority of our participants were married, accounting for 65.5% (n = 993), followed by 28.2% (n = 428) who were unmarried, 3.8% (n = 57) divorced, and 2.5% (n = 38) widowed. The average educational attainment among the participants was 12.36 years, with a standard deviation of 3.75 years, indicating a relatively uniform educational background across the study sample. Among the total of 1,516 MDD patients, 46.2% (700 cases) were diagnosed with concurrent sexual dysfunction (SD) (Table 1).
3.2 Sexual dysfunction in males and females with MDD
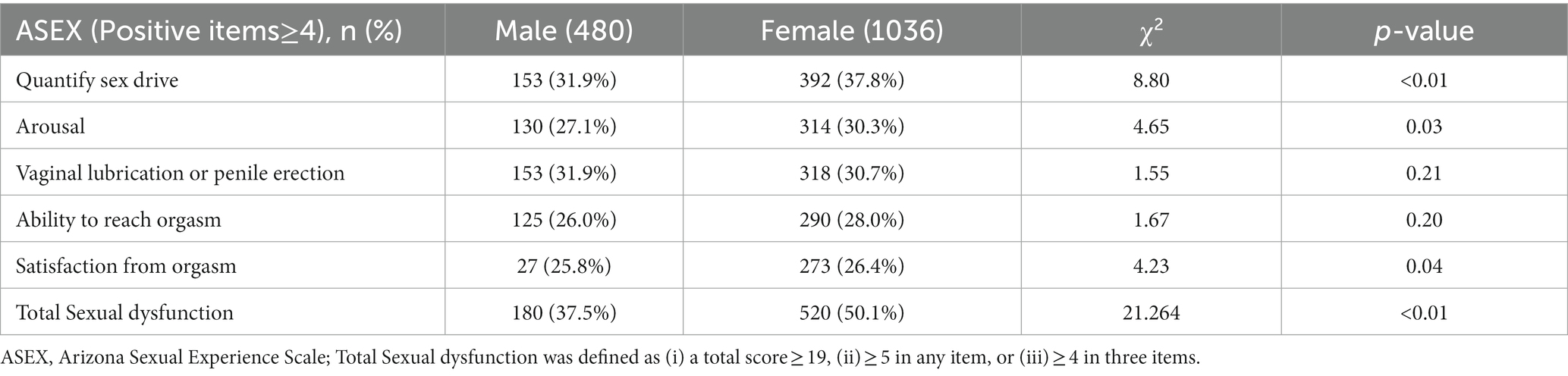
Low sex drive was reported in both males and females, (31.9% vs.37.8%, p < 0.01) and difficulties in sexual arousal (27.1% vs.30.3%, p = 0.03). Within the male MDD patient population, 31.9% experienced issues with penile erection, while 30.7% of female patients faced challenges with vaginal lubrication (p = 0.21). Furthermore, males and females reported difficulties in achieving orgasm (26.0% vs. 28.0%, p = 0.20) and unsatisfying orgasms (25.8%vs.26.4%, p = 0.04). In regards to the occurrence of total sexual dysfunction, it was found that females exhibited a significantly higher frequency compared to males (50.1% vs. 37.5%, p < 0.01). Evaluated with the item scores (Positive items ≥4), Low sex drive and penile erection are the most prevalent sexual dysfunctions among male MDD patients, whereas female MDD patients primarily experience low sex drive as their most common sexual dysfunction (Table 2).
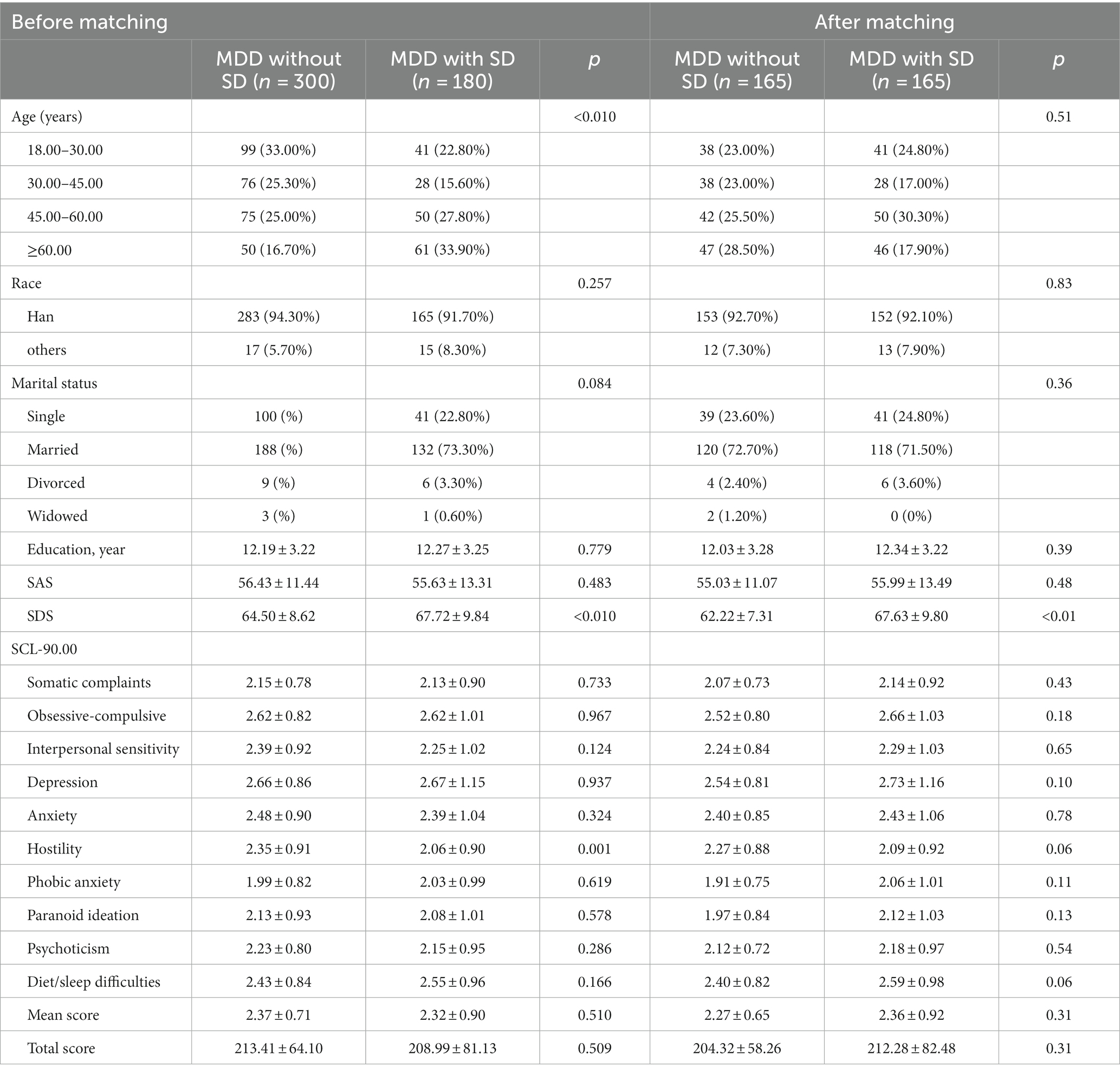
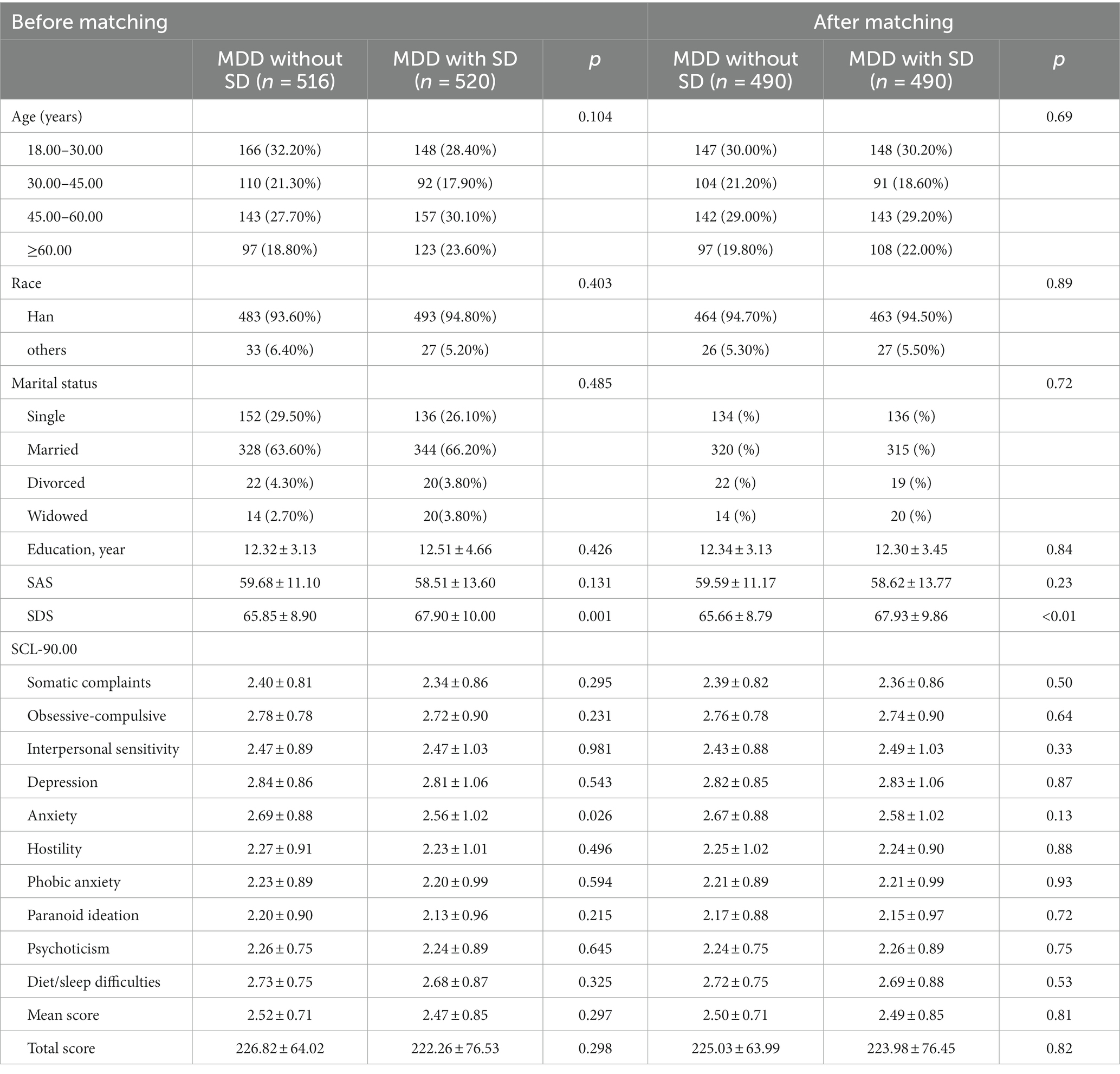
To perform the Propensity Score Matching (PSM) analysis, predictive variables including age, marital status, race, and education were selected. A matching tolerance of 0.1 was established. Tables 23 present the results after PSM. The primary objective of this research was to determine the differences in psychological factors between MDD patients with and without SD. By balancing demographic variables through the PSM procedure, a comparison of the main and secondary results could be made under similar conditions. Out of the 480 male MDD patients, 180 experienced SD, giving them a prevalence rate of 37.5%. Similarly, 520 out of the 1,036 female MDD patients displayed signs of SD, resulting in a detection rate of 50.3%. After PSM, no significant differences were found in terms of age, marital status, race, and education between the groups. Additionally, both male and female MDD patients with SD exhibited significantly higher SDS scores compared to those without SD (p < 0.01). There were no statistically significant differences between male and female MDD patients with or without concomitant sexual dysfunction in terms of Somatic complaints, Obsessive-compulsive, Interpersonal sensitivity, Anxiety, Phobic anxiety, Paranoid ideation, Psychoticism and Diet/sleep difficulties (p > 0.05),Male MDD patients without SD had slightly higher Hostility scores on the SCL-90 (p = 0.058) and a slight decrease in Diet/sleep difficulties scores on the SCL-90 (p = 0.057) compared to those with SD. However, these trends were not observed among female MDD patients (Tables 3 4).
Factors that Increase the Risk of MDD with SDTo check for plagiarism, a binary logistic regression analysis was conducted where the dependent variable was the presence or absence of SD in individuals with MDD. The variables considered as independent were SAS, SDS, and SCL-90 scores. The analysis demonstrated that the occurrence of SD in both male (OR = 1.084, p < 0.01) and female (OR = 1.026, p < 0.01) MDD patients could be independently predicted by the SDS score, as displayed in Figure 1.
4 Discussion
Our investigation into individuals diagnosed with Major Depressive Disorder (MDD) revealed a notable disparity between genders when it came to sexual dysfunction. Female patients reported a significantly higher prevalence compared to their male counterparts. This observation suggests a connection between the severity of depression and the occurrence of sexual dysfunction across genders. Interestingly, our findings indicate that hostility may act as a protective factor against sexual dysfunction among males with MDD, while this relationship was not observed in females (see Figures 2 3).
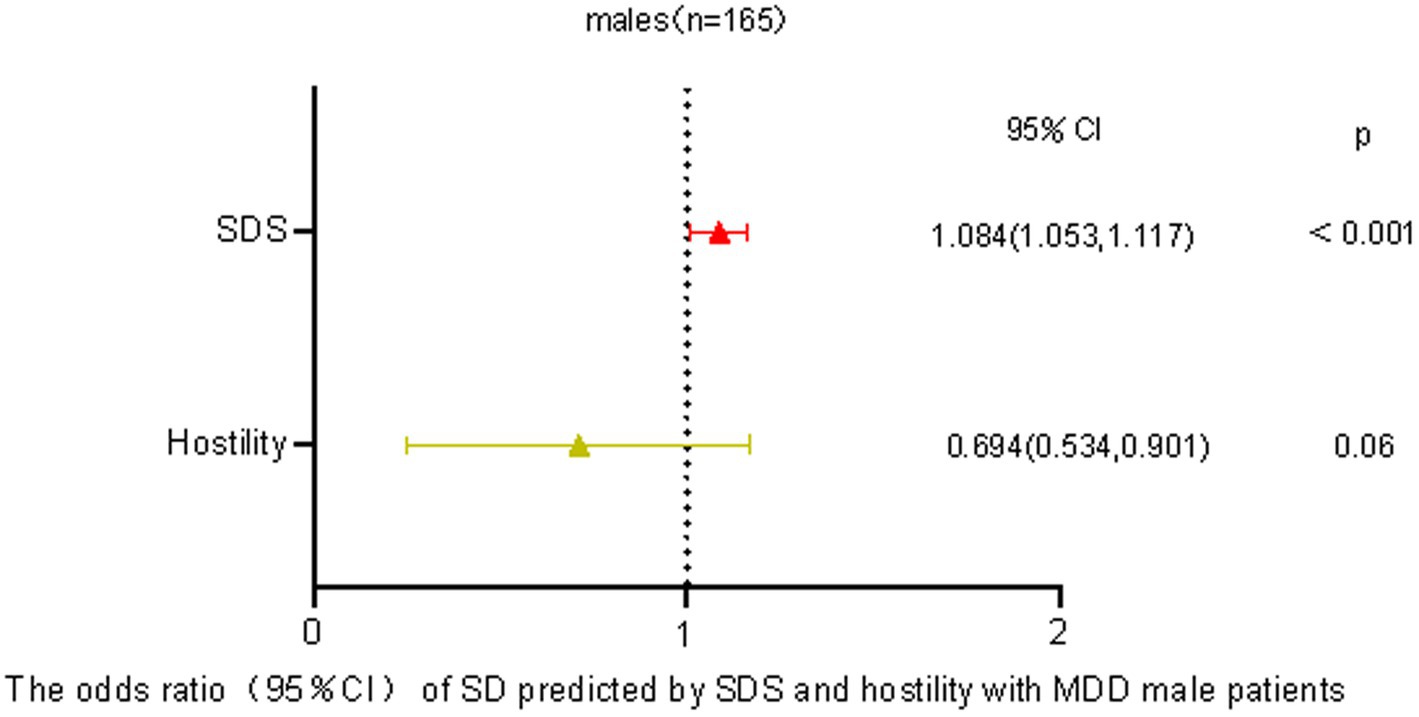
Figure 2. Predicting odds of sexual dysfunction by self-reported depression and hostility in male patients with MDD.
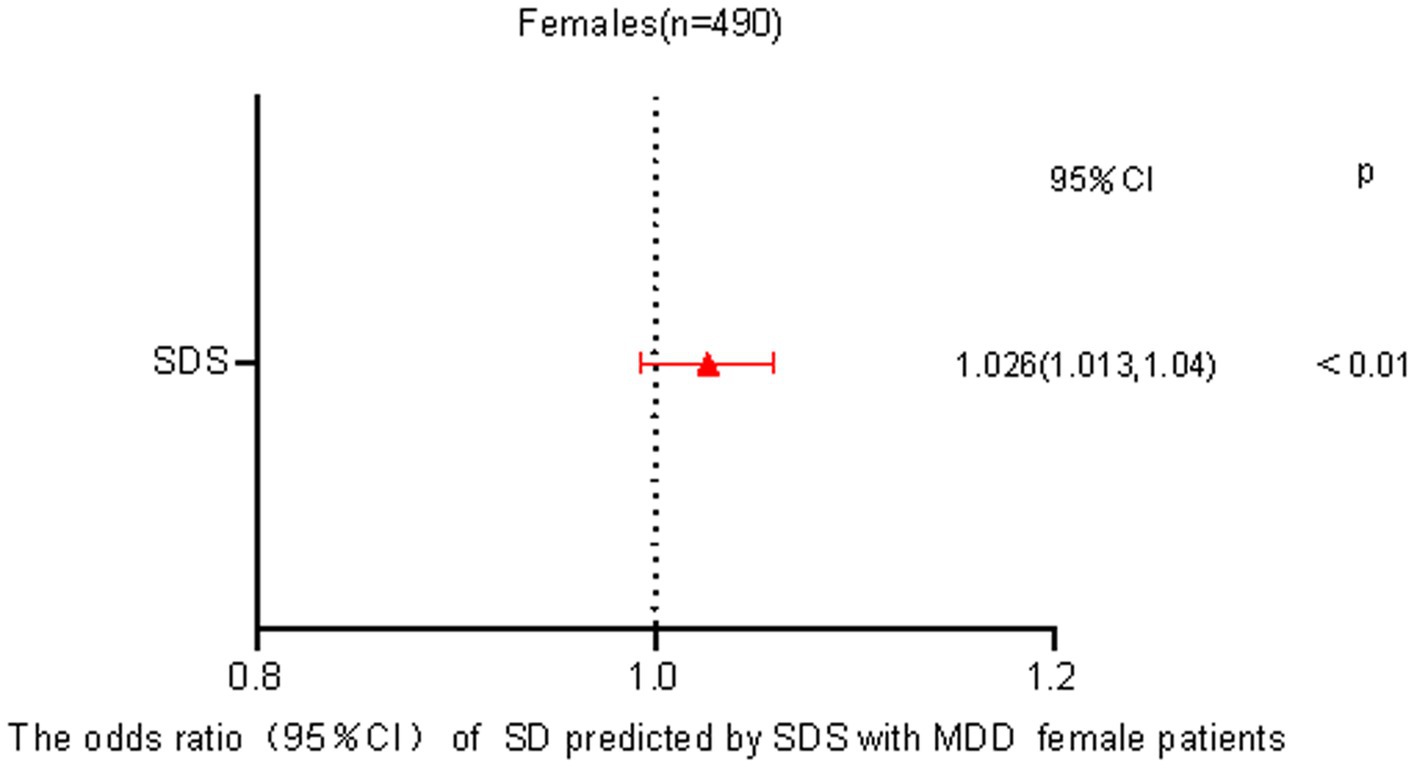
Figure 3. Predicting odds of sexual dysfunction by self-reported depression in female patients with MDD.
A comprehensive analysis comprising 12 studies investigating depressive disorders revealed that 82.75% of females and 63.26% of males encountered sexual problems, excluding those receiving medication (14). Another investigation on sexual issues in Asia disclosed that 37% of males and 45% of females in China undergo at least one form of sexual dysfunction. Generally, within the broader population, females consistently report a higher prevalence of sexual concerns compared to males (26, 27). In our assessment, 46.2% of patients diagnosed with major depressive disorder acknowledged experiencing sexual dysfunction, with a significantly higher occurrence in females (50.3%) as compared to males (37.5%). This finding is consistent with previous studies, which have indicated a more pronounced sexual dysfunction in females with MDD (28). One suggested explanation for this gender discrepancy centers around variations in the neurobiological aspect. Depressed females, in contrast to their mentally healthy counterparts, display reduced activity in specific regions of the brain, including the hypothalamus, septal region, anterior cingulate gyrus, and parahippocampal gyrus (29). However, recent years have observed an increased focus on men’s sexual health, although discussions relating to sexuality are still regarded as somewhat taboo in many Asian cultures (30). A prevalent lack of sexual knowledge often leads to dysfunction, particularly among women (31).
Our research supports the claim that the severity of depression in MDD patients is connected to the prevalence of sexual dysfunction, aligning with previous studies (10). Sexual dysfunction tends to worsen with increasing severity of depression (32). The association between sexual dysfunction prevalence and depression severity in MDD patients was not found with the SCL-90 metrics, possibly because the SCL-90 focuses mainly on depression and does not cover the entire range of clinical symptoms. It is important to note that various factors, such as gender differences, testosterone levels, brain structure, medication effects, and coexisting conditions like alcohol dependence, can influence the relationship between sexual dysfunction prevalence and depression severity in MDD patients (33–36). Another significant finding in our study relates to the potential protective effect of higher hostility levels (measured by the SCL-90) against sexual dysfunction (37, 38). Patients with pronounced hostility levels appeared to be less susceptible to sexual dysfunction, which differs from previous research. One possible explanation is that heightened hostility may be a result of factors like increased testosterone levels, which could enhance sexual function while also increasing feelings of hostility (34). Additionally, meta-analyses have emphasized the impact of different personality traits on various aspects of human sexuality (39–41). It should be noted that our study primarily focused on patients at high risk of suicide or aggression. Such individuals, characterized by heightened hostility and aggression, may inherently exhibit increased sexual behaviors (42).
Yet, there are constraints to our study. It was a clinical study conducted retrospectively in a single-center and small number of men, neglecting the consideration of potential economic factors’ impact on sexual dysfunction, which could potentially introduce confounding variables. To obtain a more exhaustive analysis and enhance the generalizability of our findings, a more comprehensive evaluation of clinical particulars would have been beneficial. Lastly, our research did not incorporate a sample size customized to its specific objectives.
5 Conclusion
Our study confirms a significant gender disparity in sexual dysfunction among individuals diagnosed with Major Depressive Disorder (MDD), with females reporting a higher prevalence than males. These findings align with previous research highlighting the consistent reporting of heightened sexual concerns among females. Our research also underscores the potential link between depression severity in MDD patients and the prevalence of sexual dysfunction. A remarkable observation from our study is the potential protective role of hostility against sexual dysfunction in male MDD patients.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Sichuan Provincial People's Hospital, Sichuan Academy of Medical Sciences & Sichuan Provincial People's Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants' legal guardians/next of kin because the study was conducted in accordance with the principles of the Declaration of Helsinki. Because of the retrospective nature of the study, patient consent for inclusion was waived.
Author contributions
FJ: Conceptualization, Methodology, Resources, Writing – original draft, Writing – review & editing. ZL: Data curation, Formal analysis, Writing – review & editing. XW: Data curation, Project administration, Software, Writing – review & editing. AT: Formal analysis, Investigation, Writing – review & editing. XQ: Investigation, Supervision, Validation, Visualization, Writing – original draft. RS: Methodology, Writing – review & editing. HL: Funding acquisition, Project administration, Resources, Writing – review & editing. HW: Resources, Software, Writing – original draft. JX: Resources, Funding acquisition, Project administration, Supervision, Validation, Visualization, Writing – review & editing. BZ: Funding acquisition, Project administration, Resources, Writing – review & editing, Supervision, Validation, Visualization.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by Epidemiological Survey on Mental Health in Sichuan Province (Grant numbers:(2019-YF09-00099-SN).
Acknowledgments
We would like to express our gratitude to all participants who have taken part in the assessments and interviews carried out during the course of our research. Additionally, we extend our thanks to the investigators who have provided valuable assistance to our study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hasin, D, Sarvet, AL, Meyers, JL, Saha, TD, Ruan, WJ, Stohl, M, et al. Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatry. (2018) 75:336–46. doi: 10.1001/jamapsychiatry.2017.4602
2. Huang, Y, Wang, Y, Wang, H, Liu, Z, Yu, X, Yan, J, et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry. (2019) 6:211–24. doi: 10.1016/S2215-0366(18)30511-X
3. Klaser, K., Thompson, E.J., Nguyen, L.H., Sudre, C.H., Antonelli, M., Murray, B., et al., Anxiety and depression symptoms after COVID-19 infection: results from the COVID symptom study app. medRxiv, [Epub ahead of preprint] (2021). doi: 10.1101/2021.07.07.21260137
4. Oh, DJ, Yang, HW, Suh, SW, Byun, S, Kim, TH, Kwak, KP, et al. The impact of the COVID-19 pandemic on depression in community-dwelling older adults: a prospective cohort study. Psychol Med. (2023) 53:2992–9. doi: 10.1017/S0033291721005018
5. Vos, T, Barber, RM, Bell, B, Bertozzi Villa, A, Biryukov, S, Bolliger, I, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the global burden of disease study 2013. Lancet. (2015) 386:743–800. doi: 10.1016/S0140-6736(15)60692-4
6. Elderon, L, and Whooley, MA. Depression and cardiovascular disease. Prog Cardiovasc Dis. (2013) 55:511–23. doi: 10.1016/j.pcad.2013.03.010
7. Chesney, E, Goodwin, GM, and Fazel, S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry. (2014) 13:153–60. doi: 10.1002/wps.20128
8. Laumann, EO, Paik, A, and Rosen, RC. Sexual dysfunction in the United States: prevalence and predictors. JAMA. (1999) 281:537–44. doi: 10.1001/jama.281.6.537
9. Drozdowicz, L, Gordon, E, Shapiro, D, Jacobson, S, Zalpuri, I, Stewart, C, et al. Sexual health in child and adolescent psychiatry: multi-site implementation through synchronized videoconferencing of an educational resource using standardized patients. Front Psych. (2020) 11:593101. doi: 10.3389/fpsyt.2020.593101
10. Williams, K, and Reynolds Margaret, JC. Spectrums, sexual dysfunction in major depression. CNS spectrums. (2006) 11:19–23. doi: 10.1017/S1092852900026729
11. Winter, J, Curtis, K, Hu, B, and Clayton, AH. Sexual dysfunction with major depressive disorder and antidepressant treatments: impact, assessment, and management. Expert Opin Drug Saf. (2022) 21:913–30. doi: 10.1080/14740338.2022.2049753
12. Kennedy, S, Dickens, SE, Eisfeld, BS, and Bagby, RM. Sexual dysfunction before antidepressant therapy in major depression. J Affect Disord. (1999) 56:201–8. doi: 10.1016/S0165-0327(99)00050-6
13. Liu, X, Feng, Z, Galling, B, Qi, N, Zhu, XQ, Xiao, L, et al. Gender specific sexual dysfunction in patients with depression. Front Psych. (2023) 14:1194228. doi: 10.3389/fpsyt.2023.1194228
14. Gonçalves, WS, Gherman, BR, Abdo, CHN, Coutinho, ESF, Nardi, AE, and Appolinario, JC. Prevalence of sexual dysfunction in depressive and persistent depressive disorders: a systematic review and meta-analysis. Int J Impot Res. (2023) 35:340–9. doi: 10.1038/s41443-022-00539-7
15. Masiran, R, Sidi, H, Mohamed, Z, Mohd Nazree, NE, Nik Jaafar, NR, Midin, M, et al. Female sexual dysfunction in patients with major depressive disorder (MDD) treated with selective serotonin reuptake inhibitor (SSRI) and its association with serotonin 2A-1438 G/a single nucleotide polymorphisms. J Sex Med. (2014) 11:1047–55. doi: 10.1111/jsm.12452
16. Nazree, NE, Mohamed, Z, Reynolds, GP, Mohd Zain, S, Masiran, R, Sidi, H, et al. Association of brain-derived neurotrophic factor valine to methionine polymorphism with sexual dysfunction following selective serotonin reuptake inhibitor treatment in female patients with major depressive disorder. Asia Pac Psychiatry. (2016) 8:260–8. doi: 10.1111/appy.12210
17. Laurent, SM, and Simons, AD. Sexual dysfunction in depression and anxiety: conceptualizing sexual dysfunction as part of an internalizing dimension. Clin Psychol Rev. (2009) 29:573–85. doi: 10.1016/j.cpr.2009.06.007
18. Lin, CF, Juang, YY, Wen, JK, Liu, CY, and Hung, CI. Correlations between sexual dysfunction, depression, anxiety, and somatic symptoms among patients with major depressive disorder. Chang Gung Med J. (2012) 35:323–31. doi: 10.4103/2319-4170.106138
19. Elgellaie, A, Thomas, SJ, Kaelle, J, Bartschi, J, and Larkin, T. Pro-inflammatory cytokines IL-1α, IL-6 and TNF-α in major depressive disorder: sex-specific associations with psychological symptoms. Eur J Neurosci. (2023) 57:1913–28. doi: 10.1111/ejn.15992
20. Cho, JW, and Duffy, JF. Health, sleep, sleep disorders, and sexual dysfunction (2019) 37:261–75. doi: 10.5534/wjmh.180045,
21. Alidost, F, Pakzad, R, Dolatian, M, and Abdi, F. Sexual dysfunction among women of reproductive age: a systematic review and meta-analysis. Int J Reprod Biomed. (2021) 19:421–32. doi: 10.18502/ijrm.v19i5.9251
22. Olatunji, BO, Deacon, BJ, Abramowitz, JS, and Tolin, DF. Dimensionality of somatic complaints: factor structure and psychometric properties of the self-rating anxiety scale. J Anxiety Disord. (2006) 20:543–61. doi: 10.1016/j.janxdis.2005.08.002
23. Zung, WW, Richards, CB, and Short, MJ. Self-rating depression scale in an outpatient clinic. Further validation of the SDS. Arch Gen Psychiatry. (1965) 13:508–15. doi: 10.1001/archpsyc.1965.01730060026004
24. Derogatis, LR, Rickels, K, and Rock, AF. The SCL-90 and the MMPI: a step in the validation of a new self-report scale. Br J Psychiatry. (1976) 128:280–9. doi: 10.1192/bjp.128.3.280
25. McGahuey, CA, Gelenberg, AJ, Laukes, CA, Moreno, FA, Delgado, PL, McKnight, K, et al. The Arizona sexual experience scale (ASEX): reliability and validity. J Sex Marital Ther. (2000) 26:25–40. doi: 10.1080/009262300278623
26. Mercer, CH, Fenton, KA, Johnson, AM, Copas, AJ, Macdowall, W, Erens, B, et al. Who reports sexual function problems? Empirical evidence from Britain's 2000 National Survey of sexual attitudes and lifestyles. Sex Transm Infect. (2005) 81:394–9. doi: 10.1136/sti.2005.015149
27. Lewis, RW. Epidemiology of sexual dysfunction in Asia compared to the rest of the world. Asian J Androl. (2011) 13:152–8. doi: 10.1038/aja.2010.108
28. Yang, JC. Functional neuroanatomy in depressed patients with sexual dysfunction: blood oxygenation level dependent functional MR imaging. Korean J Radiol. (2004) 5:87–95. doi: 10.3348/kjr.2004.5.2.87
29. Yang, JC, Park, K, Eun, SJ, Lee, MS, Yoon, JS, Shin, IS, et al. Assessment of cerebrocortical areas associated with sexual arousal in depressive women using functional MR imaging. J Sex Med. (2008) 5:602–9. doi: 10.1111/j.1743-6109.2007.00737.x
30. Ho, CCK, Singam, P, Hong, GE, and Zainuddin, ZM. Male sexual dysfunction in Asia. Asian J Androl. (2011) 13:537–42. doi: 10.1038/aja.2010.135
32. Sreelakshmy, K, Velayudhan, R, Kuriakose, D, and Nair, R. Sexual dysfunction in females with depression: a cross-sectional study. Trends Psychiatry Psychother. (2017) 39:106–9. doi: 10.1590/2237-6089-2016-0072
33. Rizvi, SJ, Kennedy, SH, Ravindran, LN, Giacobbe, P, Eisfeld, BS, Mancini, D, et al. The relationship between testosterone and sexual function in depressed and healthy men. J Sex Med. (2010) 7:816–25. doi: 10.1111/j.1743-6109.2009.01504.x
34. Thase, ME, Danchenko, N, Brignone, M, Florea, I, Diamand, F, Jacobsen, PL, et al. Comparative evaluation of vortioxetine as a switch therapy in patients with major depressive disorder. Eur Neuropsychopharmacol. (2017) 27:773–81. doi: 10.1016/j.euroneuro.2017.05.009
35. Piani, MC, Maggioni, E, Delvecchio, G, Ferro, A, Gritti, D, Pozzoli, SM, et al. Sexual dimorphism in the brain correlates of adult-onset depression: a pilot structural and functional 3T MRI study. Front Psych. (2021) 12:683912. doi: 10.3389/fpsyt.2021.683912
36. Acharya, RK, Panigrahi, S, Samani, MJ, and Choudhary, AK. Prevalence and pattern of sexual dysfunction in male patients with alcohol dependence. Addict Health. (2022) 14:192–7. doi: 10.34172/ahj.2022.1335
37. Kotler, M, Cohen, H, Aizenberg, D, Matar, M, Loewenthal, U, Kaplan, Z, et al. Sexual dysfunction in male posttraumatic stress disorder patients. Psychother Psychosom. (2000) 69:309–15. doi: 10.1159/000012413
38. O’Connor, DB, Archer, J, and Wu, FCW. Effects of testosterone on mood, aggression, and sexual behavior in young men: a double-blind, placebo-controlled, cross-over study. J Clin Endocrinol Metabol. (2004) 89:2837–45. doi: 10.1210/jc.2003-031354
39. van Amsterdam, J, Opperhuizen, A, and Hartgens, F. Adverse health effects of anabolic–androgenic steroids. Regul Toxicol Pharmacol. (2010) 57:117–23. doi: 10.1016/j.yrtph.2010.02.001
40. Allen, MS, and Walter, EE. Linking big five personality traits to sexuality and sexual health: a meta-analytic review. Psychol Bull. (2018) 144:1081–110. doi: 10.1037/bul0000157
41. Carvalho, J, and Nobre, PJ. Five-factor model of personality and sexual aggression. Int J Offender Ther Comp Criminol. (2019) 63:797–814. doi: 10.1177/0306624X13481941
Keywords: major depressive disorder, sexual dysfunction, ASEX, prevalence, psychological symptom
Citation: Jiang F, Liu Z, Wu X, Tan A, Qin X, Su RC, Li H, Wang H, Xiao J and Zhou B (2023) Prevalence of sexual dysfunction and its association with psychological symptoms in drug-naive major depressive disorder patients in West China. Front. Psychiatry. 14:1291988. doi: 10.3389/fpsyt.2023.1291988
Edited by:
Roberto Esposito, ASUR Marche, ItalyReviewed by:
Sharmilla Kanagasundram, University of Malaya, MalaysiaReza Hekmat, Mashhad University of Medical Sciences, Iran
Copyright © 2023 Jiang, Liu, Wu, Tan, Qin, Su, Li, Wang, Xiao and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jun Xiao, MTQ1ODkzNTgwM0BxcS5jb20=; Bo Zhou, dG9ueWFjNzcyMUAxNjMuY29t
 Fugui Jiang
Fugui Jiang Zenghui Liu1,2
Zenghui Liu1,2 Bo Zhou
Bo Zhou