- 1College of Medicine, Hebron University, Hebron, Palestine
- 2Faculty of Medicine and Health Sciences, An-Najah National University, Nablus, Palestine
- 3Department of Family and Community Medicine, Faculty of Medicine and Health Sciences, An-Najah National University, Nablus, Palestine
Background and objectives: Depression and anxiety are common mental health disorders among the elderly worldwide. In this study, we estimated the prevalence of depression and anxiety and related risk factor among elderly attending Primary Health care (PHC) centers in Palestine.
Methods: A cross-sectional study was conducted from February to July 2021 with a sample size of 380 participants aged ≥60 attending PHC centers in West Bank, using an interviewer-administered questionnaire. We used the Geriatric Depression Scale-15 and the Geriatric anxiety Scale to screen for depression and anxiety, respectively. Logistic regression models were used to identify predictors of depression and anxiety.
Results: The prevalence of depression and anxiety was 41.1 and 39.2%, respectively. Elderly people living in rural areas (aOR = 2.63; 95% CI: 1.72–4.20), uneducated (aOR = 2.92; 95% CI: 1.41–6.13), and without monthly income (aOR = 3.42; 95% CI: 1.52–7.61) were more likely to have depression. On the other hand, anxiety was independently associated with living in rural areas (aOR = 1.93, 95% CI: 1.23–3.04) and having non-communicable diseases (aOR = 2.01; 95% CI: 1.13–3.49).
Conclusion: Depression and anxiety are common in Palestine, a developing country with a lack of elderly related services. This should be emphasized at the national and regional levels where geriatric health care services are scarce. Such information is required by policymakers and external funding agencies in order to develop future agendas.
Introduction
Nowadays, the average individual can foresee living well into their sixties and beyond. People over 60 years of age are a growing proportion of the general population. In 2019, the global population of adults aged 60 and over topped one billion. The forecast estimates 1.4 billion people in 2030 and 2.1 billion in 2050 (1). Addressing the specific healthcare needs of the elderly population is essential in health aging (2). While older individuals in the developed world have slightly better health than previous generations, good health later in life is not fairly distributed. About 5% of the population in Palestine consists of individuals aged 60 (3).
Mental health is an important part of living well. Care services are still below optimal in low to middle-income countries. According to World Health Organization 14% of adults 60 and older suffer a mental health condition (4). A recent pooled analysis of depression in a systemic review study on prevalence among the elderly revealed an average predicted prevalence of 31.7% (95% confidence interval (CI): 27.9–35.6). In the subgroup analysis, the pooled prevalence was higher in developing countries, reaching almost 40.8%. The associated risk factors could be being older, female, single or divorced, having a low educational level (low or nonexistent), family history of significant life events (i.e., family death) and having chronic diseases (i.e., diabetes and heart diseases) (5). Along with depression, anxiety is a prevalent mental health condition in the elderly. Community samples revealed up to 15% suffered from anxiety, while clinical settings showed up to 28%. It was significantly higher in terms of anxiety symptoms, ranging between 15 and 52.3% in population samples and 15% to 56% in clinical samples (6).
Healthcare practitioners often underdiagnose mental health conditions, and the stigma associated with these conditions inhibits people from getting help. Few studies evaluated common mental health condition among older people in Arab countries (7). The stigma associated with the significant societal implications of mental health condition might be one barrier to diagnosis and treatment (8).
In Palestine, clinicians do not have screening guidelines and rarely use screening instruments. However, numerous visits to primary health care centers (PHC) with physical symptoms are indicators of mental health conditions that frequently go untreated (9). Furthermore, Palestine faces distinct difficulties with movement restrictions imposed by the Occupation and a dearth of mental health services, making this study crucial. Therefore, our study aim is to determine the prevalence of depression and anxiety among elderly adults presenting to PHC in the Occupied West Bank and factors that influence those mental health diagnoses.
Methods
Design and study population
We conducted a cross-sectional study using an interview-administered questionnaire. Adults aged 60 years and older who attended the three main PHC centers in the West Bank of Palestine were asked to participate between February to July 2021. The sample size was 380, as calculated by Epi Info 6.0, at an 80% power level and a 95% confidence level (10).
Measures
An interviewer-administered questionnaire consisted of 3 sections:
(1) Patient information: a. sociodemographic variables which includes: Gender, age (60–64; 65–70; >70), Marital status (married; single: single or widowed), residency (urban; rural), educational level (uneducated+ primary school; middle + high school; university), living conditions (alone; not alone), professional status (employed; retired; not employed) and source of income (no income/social/saving; from family; retirement salary or private job).
b. Medical history of non-communicable diseases (NCD) such as hypertension, diabetes mellitus, cancer, and ischemic heart disease as reported by the particpants. If a patient presents with one or more NCDs, they are classified as having NCDs.
(2) GDS-15: a short version of the Geriatric Depression Scale that is used for the purpose of assessing depression symptoms in older adults. The Geriatric Depression Scale (GDS) is a measurement tool that assigns scores ranging from 0 to 15. A score of 0 on the GDSsuggets the absence of depressive symptoms, scores between 5 and 8 suggest mild depressive symptoms, scores between 9 and 11 indicate moderate depressive symptoms, and scores between 12 and 15 indicate severe depressive symptoms (11–13). Depressive symptoms was suggested by a cut-off value of six or higher (11, 12).
(3) Geriatric anxiety Scale (GAS): the scoring system used in this study categorizes individuals based on their level of anxiety symptoms. A score ranging from 0 to 11 is indicative of minimum anxiety symptoms, a score between 12 and 21 suggests mild anxiety symptoms, Scores of 22 to 27 suggests moderate anxiety symptoms and scores of 28 and above indicates severe anxiety symptoms (14, 15). To categorize anxiety into two groups, a cut-off score of 16 was chosen based on the literature. Those with a score greater than 16 were have no anxiety, while those with a score less than or equal to 16 were classified as have anxiety (16).
Arabic versions of both the used scales have a high level of reliability (12, 17).
Stastical analysis
The analysis was conducted using IBM SPSS Statistics for Windows, Version 20.0 (IBM Corp., Armonk, NY: IBM Corp). The demographic and clinical features of the subjects were described using descriptive statistics (means, standard deviations for continuous variables, and frequency distributions and proportions for categorical variables). Additionally, “chi-square test” was employed to determine any significant relationships between the groups. We employed binary logistic regression in a multivariate analysis to account for potential confounding factors. The models incorporated all variables identified as significant in the univariate analysis, as well as those with a p value below 0.1.
Ethical considerations
All methods involving human participants in this study were conducted per ethical research standards. The study was conducted in conformity with the ethical norms of An-Najah National University (ANNU). The Ministry of Health approved authorization for the study to be conducted in PHC settings, and participants were approached and invited voluntarily to participate. Participants were assured of their confidentiality and anonymity.
Results
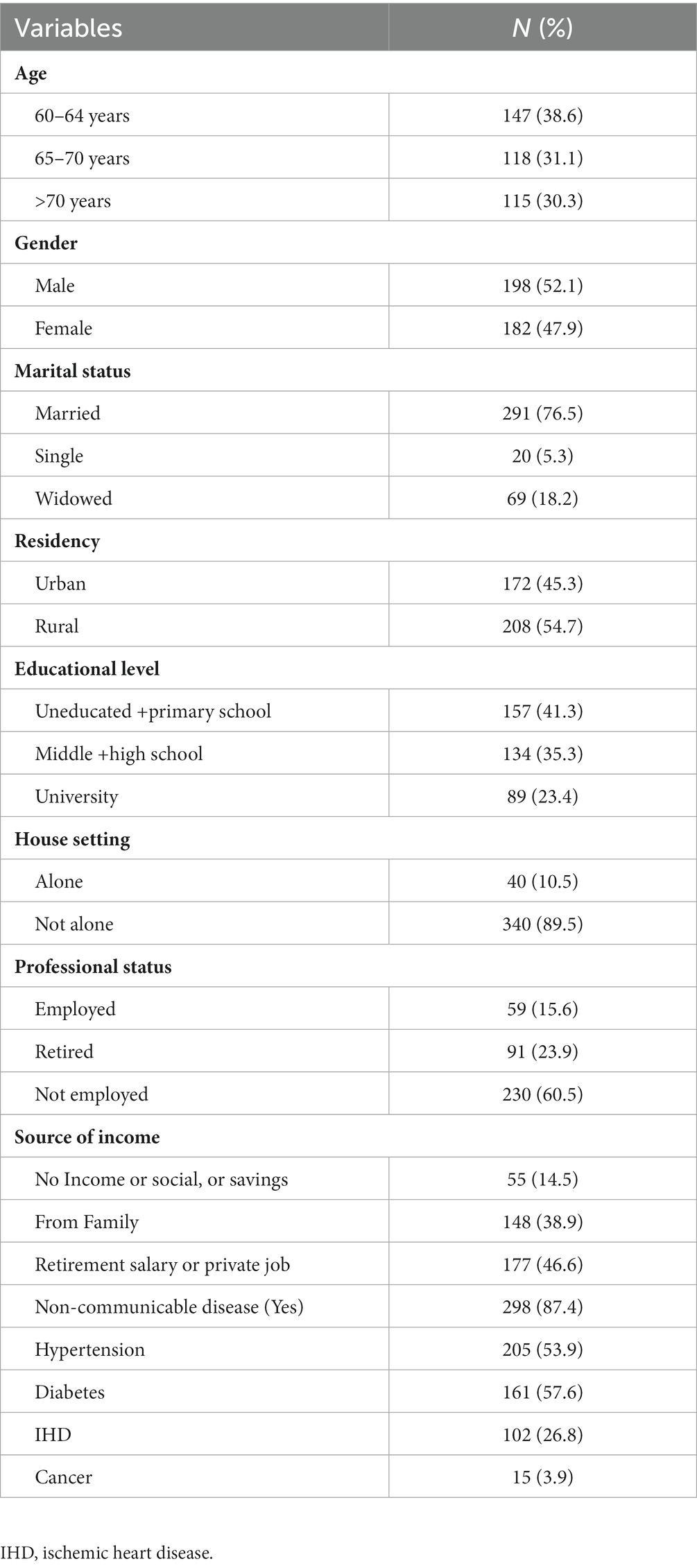
Of the 447 questionnaires distributed, 380 patients agreed to the interview, representing an 85% response rate. Just over half (52.1%) were male, most (76.6%) were married, two thirds (69.9) were between 60 and 70 years of age. Sociodemographics are presented in Table 1.
Prevalence of depressive and anxiety symptoms
Among the participants, 156 [41.1% (95%CI: 36.1–46.2%)] were found to have depressive symptoms, with mild depressive symptoms accounting for 28.4%, moderate depressive symptoms accounting for 13.4%, and severe depressive symptoms accounting for 6.3%. Anxiety symptoms were reported among 149 participants [39.2% (95%CI: 34.3–44.3%)] with mild anxiety symptoms accounting for 30.0%, moderate anxiety symptoms accounting for 8.4%, and severe anxiety symptoms accounting for 18.2% (Figure 1).
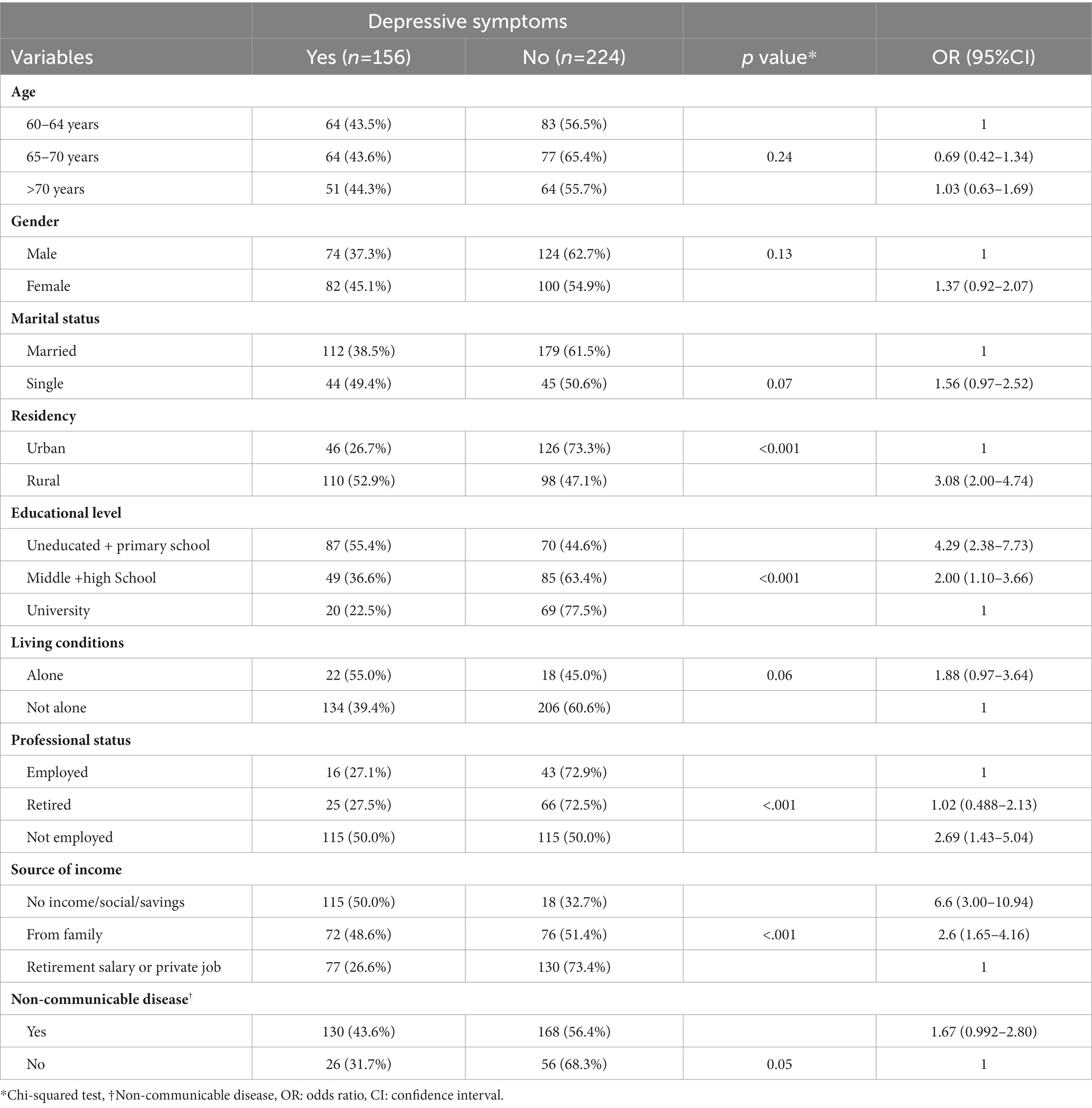
Being older, living in rural areas, lower educational level, unemployed, and no source of income were significantly associated with depressive symptoms (Table 2).
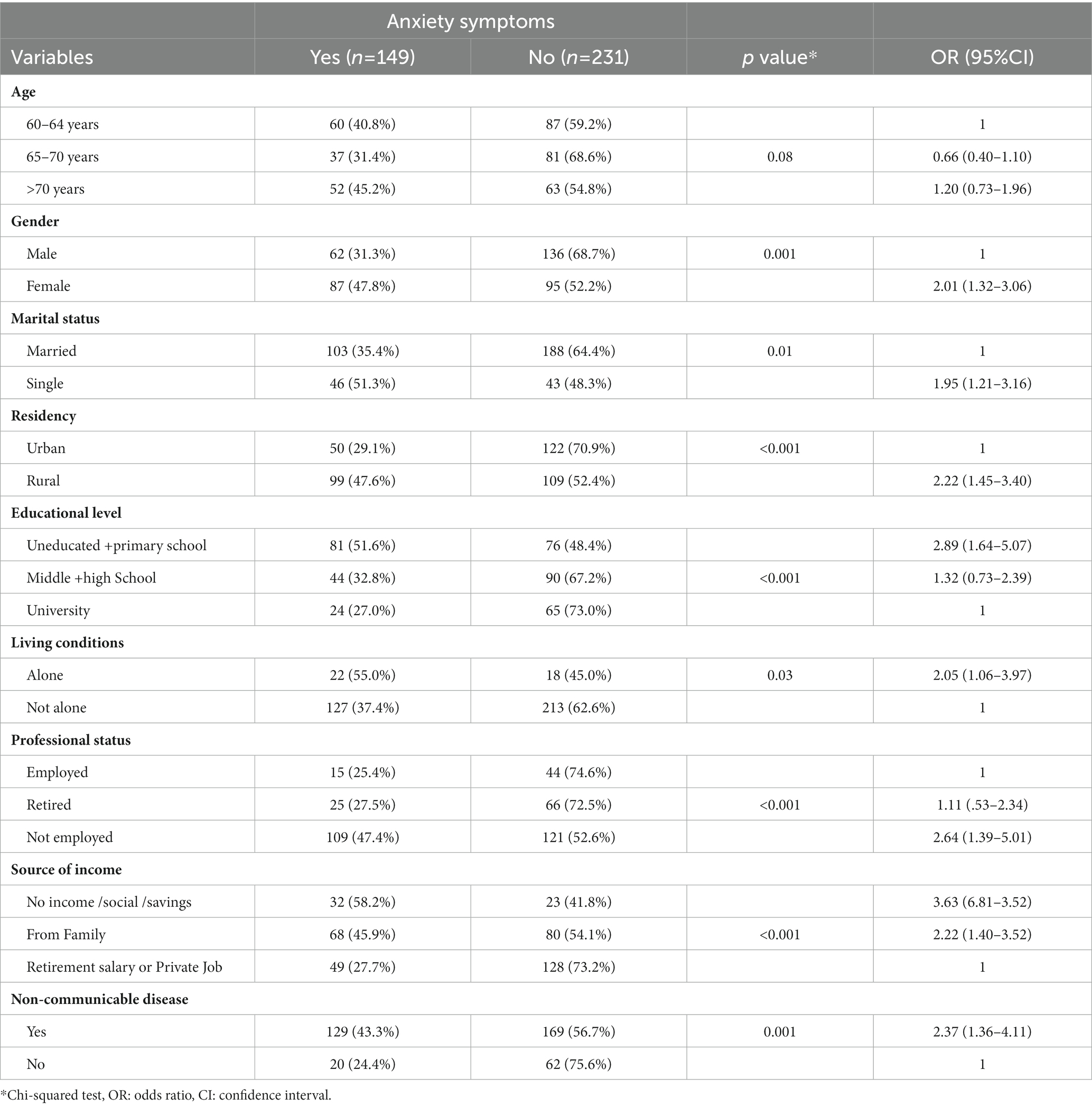
In contrast, being older, female, single, living in rural areas, and having lower educational level were significantly associated with higher level of anxiety symptoms. Furthermore, older people who live alone, are unemployed, have no income, or have a non-communicable disease were found to have significantly more anxiety symptoms (Table 3).
Multivariable analysis showed that being older people, living in rural areas (aOR = 2.63; 95% CI: 1.72–4.20), lower education (aOR = 2.92; 95% CI:1.41–6.13) and no income (aOR = 3.4; 95% CI: 1.52–7.61) were more likely to have depressive symptoms. On the other hand, anxiety symptoms among older people were found to be associated with living in rural areas (aOR = 1.93; 95% CI: 1.23–3.04) and among those with a non-communicable disease (aOR = 2.01; 95% CI: 1.13–3.49) (Table 4).
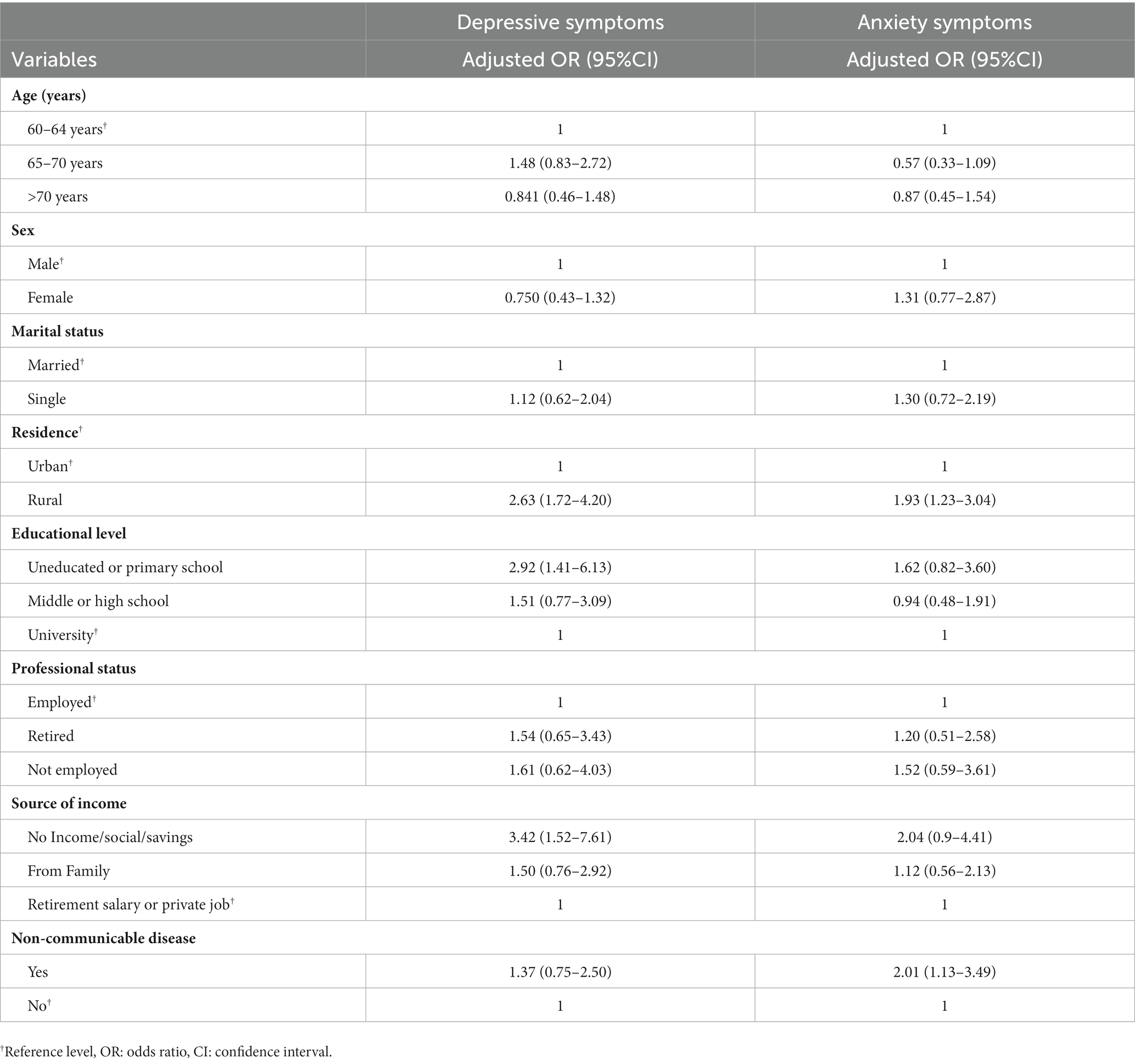
Table 4. Multivariate results of the association between sociodemographic and clinical factors, and depressive and anxiety symptoms.
Discussion
In our study, we found that 41.1% suffer from depressive symptoms, and 39.2% from anxiety symptoms. These findings corroborate a meta-analysis that assessed the global prevalence of depression to be 31.7% and 40.7% in developing countries (5). In this study, Cronbach alpha for depressive symptoms items is 0.83 and anxiety symptoms items is 0.92, which shows excellent reliability. Research conducted in nearby Egypt with similar culture reported a prevalence of depression and anxiety symptoms of 37.5% and 14.2%, respectively (7).
To our knowledge, this is the first study examining the prevalence of depression and anxiety in adults over 60 years seeking care in primary care centers in Palestine. Consistent with other studies, physical illness is a common risk factor for mental illness, particularly in the elderly (18).
Our results for both anxiety and depressive symptoms were surprising because the female gender and single status, which are considered risk factors (19), are not significant in our sample. In contrast to the findings of an Indian study that demonstrated a positive correlation between aging and the prevalence of depression and anxiety, our analysis did not reveal any significant associations between age and either anxiety or depressive symptoms (20). This is likely due to local culture and traditions that value the elderly and encourage people, particularly women and unmarried women, to assist them financially and socially.
In the relationship between depressive symptoms and education, low education was significantly associated with depressive symptoms in developing and developed countries. In contrast, income was not strongly related to depressive symptoms in low- to middle-income countries, contradicting our findings (21). This could indicate that educated individuals better understand the issue and are more likely to seek medical treatment early. In terms of income, as previously stated, a significant proportion of Palestinian families frequently rely on retired older people financially, increasing pressure and the possibility of economic violence; of course, this association warrants further examination to ascertain the patterns implicit in these complex relationships.
The findings of our investigation indicate a correlation between symptoms of anxiety and the process of aging. This conclusion exhibits a correlation with a prior study that was undertaken in Egypt and China (22, 23). Furthermore, a noteworthy correlation was identified between anxiety symptoms and factors like place of residence, source of income, and educational attainment, which aligns with findings from a previous investigation.
Although there is no substantial association between urban and non-urban residency and symptoms of depression and anxiety,rural–urban differences in mental disorders have piqued the interest of researchers and policymakers involved in mental health care. Due to community ties and social isolation, city inhabitants may be more prone to depressive symptoms than rural residents (24).
Our study limitations include beginning with the global pandemic of COVID-19, which prevented the researchers and patients from accessing the primary healthcare centers. The social desirability bias could be expected in an interview-based questionnaire about sensitive objects because patients tend to answer positively to the questions, but we hypothesize that this may be minimal in our study because elderly people are fully aware of the consequences of their contribution, which may reflect in their quality of care. Furthermore, the tools employed serve the purpose of screening, while additional diagnostic measures should be employed to accurately diagnose depression and anxiety. Nonetheless, this study provides an in-depth assessment of the prevalence of depression and anxiety symptoms among older individuals. Any individuals who screened positive were subsequently referred for further investigation. Finally, this is a cross-sectional study that measures the prevalence in a snapshot of time, and the prevalence may change over time.
Conclusion
Palestine is classified as a developing nation that faces challenges in providing comprehensive aging-related care, particularly in the area of screening for common ailments prevalent among the senior population, among economically disadvantaged nations like Palestine, the presence of these mental disorders can place a substantial financial and institutional burden on primary healthcare establishments. Depression and anxiety are prevalent conditions that warrant regular screening of elderly individuals in primary healthcare (PHC) institutions. It is recommended that guidelines for screening be implemented and that doctors receive appropriate training to adhere to these guidelines. Also, there is a need to create interventions aimed at the prevention and management of depression. There is a need to establish campaigns aimed at educating the general population about depression. Policymakers and external funding bodies necessitate such information for the purpose of formulating future agendas. It is imperative to prioritize the implementation of referral mechanisms for individuals exhibiting symptoms of moderate to severe depression and anxiety.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
All methods involving human participants in this study were conducted per ethical research standards. The study was conducted in conformity with the ethical norms of An-Najah National University (ANNU). The Ministry of Health approved authorization for the study to be conducted in PHC settings, and participants were approached and invited voluntarily to participate. Participants were assured of their confidentiality and anonymity. This study was performed in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. It was approved by the Institutional Review Board (IRB) of An-Najah National University.
Author contributions
BM: Methodology, Software, Writing – original draft, Writing – review & editing. ZN: Conceptualization, Investigation, Methodology, Software, Supervision, Writing – original draft, Writing – review & editing. SH: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Supervision, Validation, Writing – original draft, Writing – review & editing. BA: Writing – original draft, Writing – review & editing. ER: Writing – original draft, Writing – review & editing. AQ: Supervision, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We are grateful to the Palestinian Ministry of Health for assisting us in distributing and collecting questionnaires, and we are grateful to the Palestinian women who attend primary health care centers for responding to our questions.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization. Ageing [Internet] (2022). Available at: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health
2. World Health Organization. Decade of healthy ageing [internet]. World Health Organization. (2020). Available at: https://www.who.int/initiatives/decade-of-healthy-ageing#:~:text=The United Nations Decade of,communities in which they live.
3. Tina, I. Violence Against the Elderly: Palestine (2019);1–60. Available at: https://palestine.unfpa.org/sites/default/files/pub-pdf/violence_against_the_elderly_palestine.pdf
4. World Health Organization. Mental health of older adults. (2023). Available at: https://www.who.int/news-room/fact-sheets/detail/mental-health-of-older-adults
5. Zenebe, Y, Akele, B, Selassie, M, and Necho, M. Prevalence and determinants of depression among old age: a systematic review and meta-analysis. Ann General Psychiatry. (2021) 20:55. doi: 10.1186/s12991-021-00375-x
6. Andreescu, C, and Lee, S. Anxiety disorders in the elderly. Adv Exp Med Biol. (2020). 1191:561–576, doi: 10.1007/978-981-32-9705-0_28
7. Ahmed, D, El Shair, IH, Taher, E, and Zyada, F. Prevalence and predictors of depression and anxiety among the elderly population living in geriatric homes in Cairo. Egypt J Egypt Public Health Assoc. (2014) 89:127–35. doi: 10.1097/01.EPX.0000455729.66131.49
8. Ciftci, A, Jones, N, and Corrigan, PW. Mental health stigma in the Muslim community. J Muslim Ment Health. (2012) 7:17–32. doi: 10.3998/jmmh.10381607.0007.102
9. Nazzal, Z, Maraqa, B, Abu Zant, M, Qaddoumi, L, and Abdallah, R. Somatic symptom disorders and utilization of health services among Palestinian primary health care attendees: a cross-sectional study. BMC Health Serv Res. (2021) 21:1–9. doi: 10.1186/s12913-021-06671-2
10. Dean, AG, Dean, JA, Burton, AH, Dicker, RC, Coulombier, D, Brendel, KA, et al. Epi info: a word-processing, database, and statistics program for public health on IBM-compatible microcomputers. Version 6. Atlanta, Georgia: Centers for Disease Control and Prevention (1995) Produced by the Division of Surveillance and Epide.
11. Shin, C, Park, MH, Lee, S-H, Ko, Y-H, Kim, Y-K, Han, K-M, et al. Usefulness of the 15-item geriatric depression scale (GDS-15) for classifying minor and major depressive disorders among community-dwelling elders. J Affect Disord. (2019) 259:370–5. doi: 10.1016/j.jad.2019.08.053
12. Chaaya, M, Sibai, A-M, El, RZ, Chemaitelly, H, Chahine, LM, Al-Amin, H, et al. Validation of the Arabic version of the short geriatric depression scale (GDS-15). Int Psychogeriatr. (2008) 20:571–81. doi: 10.1017/S1041610208006741
13. Greenberg, SA. The geriatric depression scale: short form. Am J Nurs. (2007) 107:60–9. doi: 10.1097/01.NAJ.0000292204.52313.f3
14. Segal, DL, June, A, Payne, M, Coolidge, FL, and Yochim, B. Development and initial validation of a self-report assessment tool for anxiety among older adults: the geriatric anxiety scale. J Anxiety Disord. (2010) 24:709–14. doi: 10.1016/j.janxdis.2010.05.002
15. Callow, DD, Arnold-Nedimala, NA, Jordan, LS, Pena, GS, Won, J, Woodard, JL, et al. The mental health benefits of physical activity in older adults survive the COVID-19 pandemic. Am J Geriatr psychiatry. (2020) 28:1046–57. doi: 10.1016/j.jagp.2020.06.024
16. Gottschling, J, Segal, DL, Häusele, C, Spinath, FM, and Stoll, G. Assessment of anxiety in older adults: translation and psychometric evaluation of the German version of the geriatric anxiety scale (GAS). J Psychopathol Behav Assess. (2015) 38:136–48. doi: 10.1007/s10862-015-9504-z
17. Hallit, S, Hallit, R, Hachem, D, Daher Nasra, MC, Kheir, N, and Salameh, P. Validation of the Arabic version of the geriatric anxiety scale among Lebanese population of older adults. J Psychopathol. (2017) 23:26–34.
18. Menta, C, Bisol, LW, Nogueira, EL, Engroff, P, and Neto, AC. Prevalence and correlates of generalized anxiety disorder among elderly people in primary health care. J Bras Psiquiatr. (2020) 69:126–30. doi: 10.1590/0047-2085000000267
19. Girgus, JS, Yang, K, and Ferri, CV. The gender difference in depression: are elderly women at greater risk for depression than elderly men? Geriatr (Basel, Switzerland). (2017) 2:35. doi: 10.3390/geriatrics2040035
20. Behera, P, Sharan, P, Mishra, AK, Nongkynrih, B, Kant, S, and Gupta, SK. Prevalence and determinants of depression among elderly persons in a rural community from northern India. Natl Med J India. (2016) 29:129–35.
21. Bromet, E, Andrade, LH, Hwang, I, Sampson, NA, Alonso, J, de Girolamo, G, et al. Cross-national epidemiology of DSM-IV major depressive episode. BMC Med. (2011) 9:90. doi: 10.1186/1741-7015-9-90
22. Hamed, A, Yousf, F, and Hussein, MM. Prevalence of nocturnal enuresis and related risk factors in school-age children in Egypt: an epidemiological study. World J Urol. (2016) 35:459–65. doi: 10.1007/s00345-016-1879-2
23. Lu, L, Shen, H, Tan, L, Huang, Q, Chen, Q, Liang, M, et al. Prevalence and factors associated with anxiety and depression among community-dwelling older adults in Hunan, China: a cross-sectional study. BMC Psychiatry. (2023) 23:1–15. doi: 10.1186/s12888-023-04583-5
Keywords: depression, anxiety, elderly, primary health, mental health
Citation: Maraqa BN, Nazzal Z, Hamshari S, Alutt B, Rishmawi E and Qawasmeh A (2024) Prevalence of depression and anxiety among elderly primary care patients in Palestine. Front. Psychiatry. 14:1291829. doi: 10.3389/fpsyt.2023.1291829
Edited by:
Mustafa M. Husain, University of Texas Southwestern Medical Center, United StatesReviewed by:
Nadine Hamieh, UMR1295 Centre d'Epidémiologie et de Recherche en santé des Populations (CERPOP), FranceHassan Kanani, United States Department of Veterans Affairs, United States
Copyright © 2024 Maraqa, Nazzal, Hamshari, Alutt, Rishmawi and Qawasmeh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Suha Hamshari, cy5oYW1zaGFyaUBuYWphaC5lZHU=
 Beesan Nader Maraqa
Beesan Nader Maraqa Zaher Nazzal
Zaher Nazzal Suha Hamshari
Suha Hamshari Barlant Alutt2
Barlant Alutt2