- 1Department of Psychiatry, Clinical Neurosciences, and Addiction Medicine, All India Institute of Medical Sciences, Guwahati, India
- 2Department of Psychiatry, Devdaha Medical College, Butwal, Nepal
- 3Department of Pediatrics, All India Institute of Medical Sciences, Guwahati, India
- 4Medical Department, Erada Center for Treatment and Rehabilitation in Dubai, Dubai, United Arab Emirates
- 5Psychiatry Unit, Department of Health Sciences, University Magna Graecia of Catanzaro, Catanzaro, Italy
- 6Department of Psychiatry, Faculty of Medicine, Prince of Songkla University, Hat Yai, Thailand
- 7Department of Psychiatry, Imam Hossein Hospital, School of Medicine, Alborz University of Medical Sciences, Karaj, Iran
- 8Mental Health Research Center, Psychosocial Health Research Institute, Department of Psychiatry, School of Medicine, Iran University of Medical Sciences, Tehran, Iran
Introduction
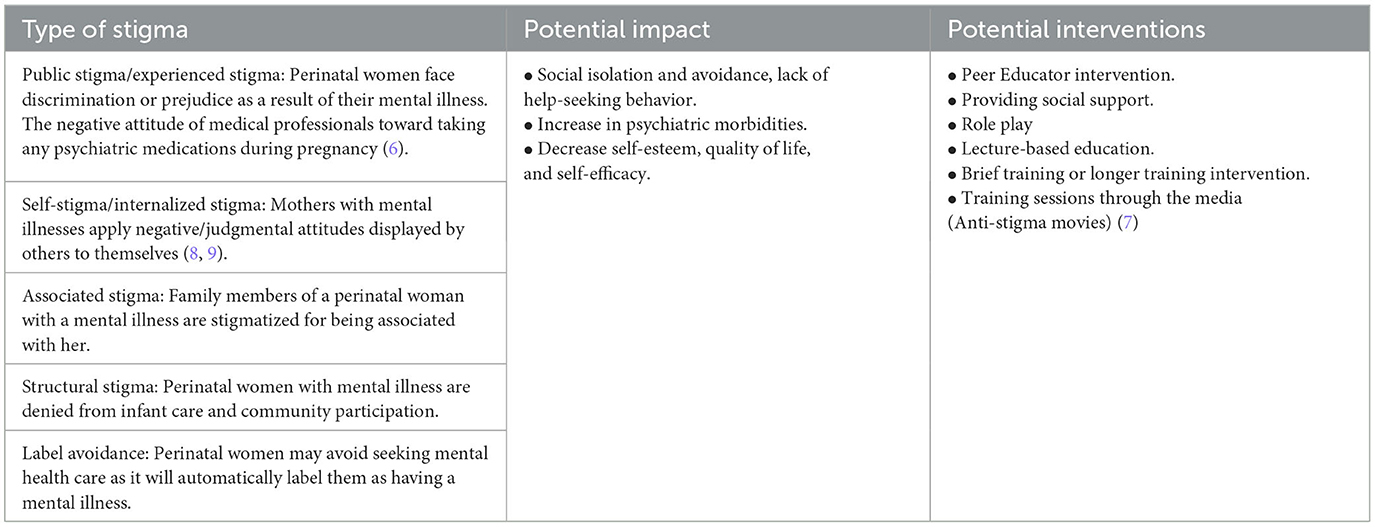
Perinatal mental disorders (PMDs) are prevalent among women in low- and middle-income countries (LMICs), constituting the most frequently encountered complications during the perinatal period, affecting almost 20% of perinatal women (1). The PMDs are associated with adverse obstetrics outcomes (e.g., increased risk of pre-eclampsia, antepartum and postpartum hemorrhage, placental abruption and still-births) and neonatal outcome (e.g., preterm births and fetal growth impairments) (2). PMDs are among the commonest morbidities of pregnancy, associated with high rates of maternal mortality and adverse outcomes, however, these conditions are often remains underdiagnosed and undertreated in LMICs. Lack of access to perinatal mental health services is mainly due to a lack of adequate resources (human, financial), inadequate knowledge among health care workers, stigma, a negative attitude toward mental disorders, a lack of evidence-based integrative or collaborative models of care, and being overlooked by stakeholders (3, 4). Mental illness stigma is also a major barrier to help-seeking, and it contributes to poor quality of life and social withdrawal among person with mental illness. Addressing the stigma associated with perinatal mental disorders has the potential to improve perinatal mental care inclusive of screening, and intervention and thus preventing the complications. However, stigma among perinatal women remains largely unexplored in LMICs (5). In this article, we-a team of early-career psychiatrists (ECPs) attempted to explore stigma toward mental illness among perinatal women residing in LMICs, its impact, and interventions to reduce it using a theoretical model. Table 1 summarizes the stigma associated with perinatal mental illness, its types, possible impact, and interventions. The theme-based approach was used to describe the types of stigma among perinatal women and to propose interventions (8).
Impact of stigma toward perinatal mental illness on mother and baby
Few studies attempted to investigate stigma toward perinatal mental illness in LMICs (9, 10). In our experience, perinatal women with mental illness are frequently stigmatized for seeking treatment, refusing treatment, being on medications, and being associated with a husband or family member (e.g., mother) with a mental illness in LMICs. This frequently results in social withdrawal of perinatal women with mental health conditions, financial burden on the family, and family disruption (e.g., divorce). These negative consequences exacerbate mental health issues and perpetuate the stigmatization cycle. Stigma leads to non-treatment of common perinatal mental disorders. This increases the risk of suicide and substance use among perinatal women and is linked to poor infant outcomes (e.g., preterm delivery, developmental and cognitive delays, and attachment and bonding problems between mother and child) (9, 11, 12) (Table 1). Furthermore, secondary to stigma, it becomes difficult for a mother to understand healthy emotional reactions during the motherhood transition and this can worsen the degree of empathy and the relationship with the child, fueling the vicious circle of postpartum depression (13). Alternatively, many mothers are hesitant to disclose their illness out of fear of losing custody of their child (14). Lastly, cultural factors related to gender preference (e.g., preference for male children) and expectations around social behaviors of mothers often affect treatment-seeking behaviors and worsen stigma toward perinatal mental illness (13, 15).
Interventions to reduce stigma toward perinatal mental illness
Perinatal women with mental illness require supportive care. Despite this, the majority of women are hesitant to discuss their illness with family members and health care workers (HCWs) due to stigma (16). The lack of knowledge about the spectrum of perinatal mental disorders not only increases the stigma associated with the illness, but also limits access to appropriate care for these conditions (6, 16). Although, Electroconvulsive therapy (ECT) is recommended as safe for women with clinical emergencies of perinatal mental disorders (e.g., catatonia, no food or fluid intake, suicide risk) (17). There is a scarcity of data from LMICs on ECT use and its effectiveness for perinatal disorders. ECT is often considered as the least helpful/harmful and inhumane treatment by the general public in LMICs (18). Both ECT and psychotropic medications are stigmatized as primary treatments for psychiatric conditions in pregnant women (6, 19, 20).
An intervention aimed at mitigating the mental illness stigma has been developed and evaluated for its effectiveness in LMICs. These interventions have been shown to be effective in enhancing the knowledge of healthcare professionals (HCWs) and the general community. However, they are minimally effective in improving the attitudinal and behavioral outcomes (21).
Discussion
We found that there is a dearth of research pertaining to the epidemiology, impact, and interventions of mental illness stigma among perinatal women in LMICs. The determinants of mental illness stigma among perinatal women are more likely to differ from other groups of people. This is primarily due to prevailing myths and misinformation regarding the effect of psychotropic medications and ECT on mothers and child across the world including LMICs (6). Moreover, there is a dearth of targeted interventions that specifically address the perinatal mental illness stigma. The collaborative or integrative models [e.g., Brief Psychological intervention during pregnancy BIND-P model (22), Task sharing model (23), Stepped care model (24)] developed in LMICs with the goal of providing screening for common mental disorders (22, 25), and psycho-education have the potential to reduce stigma (inclusive of knowledge, attitude and behavior) and improve access to care for perinatal mental disorders (21). Thus, there is an urgent need to develop HCWs-based psychosocial interventions (including psychoeducation, and training) for stigma reduction (6, 26) (Table 1).
The cultural factors, such as collectivism, Confucianism, face concern and familism, religion, and supernatural beliefs, have a role in shaping stigmatizing behavior and attitudes toward perinatal mental health. Therefore, it is crucial to promote culture-specific mental health services and interventions for reducing stigma, which is a significant barrier to recovery. We used a basic theme-based approach to explore different types of stigma, assess their impact, and offer intervention. The approach has potential to guide for future research and collaboration, as well as the development of targeted theme-based interventions.
The way forward
Due to significant disparities in mental health infrastructure across the world (27), a collaborative framework to address stigma toward perinatal mental illness across countries is required. Such framework should consider cultural, social, and health system-related factors while developing and adopting a psycho-social intervention for stigma toward perinatal mental illness. The existing infrastructure (e.g., community mental health model) of each country should be explored to develop such models of care or interventions. Further, there is an immediate need to undertake cross-country research to explore variations in stigma toward perinatal mental illness and develop tailored interventions to improve access to perinatal mental health services. These efforts have a potential to reduce the burden of perinatal mental health conditions and infant mental disorders across the world. There is a need for ECPs to work together and explore innovative methods to tackle the stigma associated with perinatal mental health in LMICs, such as digital strategies. The digital strategies can expand the reach of or complement the proposed interventions (Table 1). There are, however, several factors that need to be considered when proposing interventions and digital strategies: cultural adaptation to diverse contexts and settings, consideration of reliable measurement of stigma related to mental illness, and the risk that digital media could exacerbate stigma related to mental illness and spread misinformation.
Conclusion
Stigma reduction programs that explicitly address perinatal mental disorders in LMICs are needed.
Effective intervention components, such as educational methods (knowledge, myth-busting), should be incorporated into these programs. Further, there is an urgent need to develop evidence based or culturally adapted interventions to reduce the stigma of perinatal mental disorders in LMICs. The implementation of evidence-based interventions aimed at reducing stigma and discrimination has the potential to improve help-seeking behavior and facilitate access to suitable mental health care in LMICs.
Author contributions
AP: Conceptualization, Investigation, Writing—original draft. SP: Conceptualization, Investigation, Writing—original draft. MK: Conceptualization, Writing—original draft. SE: Writing—review & editing. RF: Writing—review & editing. RR: Conceptualization, Funding acquisition, Supervision, Writing—original draft, Writing—review & editing. MH: Writing—review & editing. MO: Writing—review & editing. MS: Conceptualization, Supervision, Writing—review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was a part of DST-India International research Fellowship program (INSA/DST-ISRF/2023/NEP/1/13) funded by Department of Science and Technology (DST), Government of India.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Doraiswamy S, Jithesh A, Chaabane S, Abraham A, Chaabna K, Cheema S. Perinatal mental illness in the Middle East and North Africa region-a systematic overview. Int J Environ Res Public Health. (2020) 17:5487. doi: 10.3390/ijerph17155487
2. Howard LM, Khalifeh H. Perinatal mental health: a review of progress and challenges. World Psychiatry. (2020) 19:313–27. doi: 10.1002/wps.20769
3. McNab SE, Dryer SL, Fitzgerald L, Gomez P, Bhatti AM, Kenyi E, et al. The silent burden: a landscape analysis of common perinatal mental disorders in low- and middle-income countries. BMC Pregnancy Childbirth. (2022) 22:342. doi: 10.1186/s12884-022-04589-z
4. Webb R, Uddin N, Constantinou G, Ford E, Easter A, Shakespeare J, et al. Meta-review of the barriers and facilitators to women accessing perinatal mental healthcare. BMJ Open. (2023) 13:e066703. doi: 10.1136/bmjopen-2022-066703
5. Shalbafan M, El Hayek S, De Filippis R. Editorial: mental-health-related stigma and discrimination: prevention, role, and management strategies. Front Psychiatry. (2023) 14:1136995. doi: 10.3389/fpsyt.2023.1136995
6. Ransing R, Kukreti P, Deshpande S, Godake S, Neelam N, Raghuveer P, et al. Perinatal depression-knowledge gap among service providers and service utilizers in India. Asian J Psychiatr. (2020) 47:101822. doi: 10.1016/j.ajp.2019.10.002
7. Rezvanifar F, Shariat SV, Shalbafan M, Salehian R, Rasoulian M. Developing an educational package to improve attitude of medical students toward people with mental illness: a Delphi expert panel, based on a scoping review. Front Psychiatry. (2022) 13:860117. doi: 10.3389/fpsyt.2022.860117
8. Subu MA, Wati DF, Netrida N, Priscilla V, Dias JM, Abraham MS, et al. Types of stigma experienced by patients with mental illness and mental health nurses in Indonesia: a qualitative content analysis. Int J Ment Health Syst. (2021) 15:77. doi: 10.1186/s13033-021-00502-x
9. Moore D, Ayers S, Drey N. A thematic analysis of stigma and disclosure for perinatal depression on an online forum. JMIR Ment Health. (2016) 3:e18. doi: 10.2196/mental.5611
10. Monaghan S, Akale MA, Demeke B, Darmstadt GL. Prevalence and stigma of postpartum common mental disorders in the Gurage region of Ethiopia: a mixed-methods observational cohort study. Front Psychol. (2021) 12:626797. doi: 10.3389/fpsyg.2021.626797
11. Chin K, Wendt A, Bennett IM, Bhat A. Suicide and maternal mortality. Curr Psychiatry Rep. (2022) 24:239–75. doi: 10.1007/s11920-022-01334-3
12. Law S, Ormel I, Babinski S, Plett D, Dionne E, Schwartz H, et al. Dread and solace: talking about perinatal mental health. Int J Mental Health Nurs. (2021) 30:1376–85. doi: 10.1111/inm.12884
13. Adlington K, Vasquez C, Pearce E, Wilson CA, Nowland R, Taylor BL, et al. ‘Just snap out of it' – the experience of loneliness in women with perinatal depression: a meta-synthesis of qualitative studies. BMC Psychiatry. (2023) 23:110. doi: 10.1186/s12888-023-04532-2
14. Diaz-Caneja A, Johnson S. The views and experiences of severely mentally ill mothers: a qualitative study. Soc Psychiatry Psychiatr Epidemiol. (2004) 39:472–82. doi: 10.1007/s00127-004-0772-2
15. Insan N, Weke A, Rankin J, Forrest S. Perceptions and attitudes around perinatal mental health in Bangladesh, India and Pakistan: a systematic review of qualitative data. BMC Pregnancy Childbirth. (2022) 22:293. doi: 10.1186/s12884-022-04642-x
16. Legere LE, Wallace K, Bowen A, McQueen K, Montgomery P, Evans M. Approaches to health-care provider education and professional development in perinatal depression: a systematic review. BMC Pregnancy Childbirth. (2017) 17:239. doi: 10.1186/s12884-017-1431-4
17. Stein A, Pearson RM, Goodman SH, Rapa E, Rahman A, McCallum M, et al. Effects of perinatal mental disorders on the fetus and child. Lancet. (2014) 384:1800–19. doi: 10.1016/S0140-6736(14)61277-0
18. Maughan D, Molodynski A. An international perspective on the acceptability and sustainability of electroconvulsive therapy. BJPsych Int. (2016) 13:10–2. doi: 10.1192/S2056474000000891
19. Pompili M, Dominici G, Giordano G, Longo L, Serafini G, Lester D, et al. Electroconvulsive treatment during pregnancy: a systematic review. Expert Rev Neurother. (2014) 14:1377–90. doi: 10.1586/14737175.2014.972373
20. Frayne J, Ellies R, Nguyen T. Experiences of decision making about psychotropic medication during pregnancy and breastfeeding in women living with severe mental illness: a qualitative study. Arch Womens Ment Health. (2023) 26:379–87. doi: 10.1007/s00737-023-01325-0
21. Heim E, Kohrt BA, Koschorke M, Milenova M, Thornicroft G. Reducing mental health-related stigma in primary health care settings in low- and middle-income countries: a systematic review. Epidemiol Psychiatr Sci. (2018) 29:e3. doi: 10.1017/S2045796018000458
22. Ransing R, Kukreti P, Raghuveer P, Mahadevaiah M, Puri M, Pemde H, et al. Development of a brief psychological intervention for perinatal depression (BIND-P). Asia Pac Psychiatry. (2021) 13:e12436. doi: 10.1111/appy.12436
23. Badiya PK, Siddabattuni S, Dey D, Hiremath AC, Nalam RL, Srinivasan V, et al. Task-sharing to screen perinatal depression in resource limited setting in India: comparison of outcomes based on screening by non-expert and expert rater. Asian J Psychiatr. (2021) 62:102738. doi: 10.1016/j.ajp.2021.102738
24. Honikman S, Van Heyningen T, Field S, Baron E, Tomlinson M. Stepped care for maternal mental health: a case study of the perinatal mental health project in South Africa. PLoS Med. (2012) 9:e1001222. doi: 10.1371/journal.pmed.1001222
25. Ransing R, Deshpande SN, Shete SR, Patil I, Kukreti P, Raghuveer P, et al. Assessing antenatal depression in primary care with the PHQ-2 and PHQ-9: can it be carried out by auxiliary nurse midwife (ANM)? Asian J Psychiatr. (2020) 53:102109. doi: 10.1016/j.ajp.2020.102109
26. Rahman A, Fisher J, Bower P, Luchters S, Tran T, Yasamy MT, et al. Interventions for common perinatal mental disorders in women in low- and middle-income countries: a systematic review and meta-analysis. Bull World Health Organ. (2013) 91:593–601I. doi: 10.2471/BLT.12.109819
Keywords: mental health, mental disorders, psychiatry, perinatal care, social stigma
Citation: Pokharel A, Philip S, Khound M, El Hayek S, de Filippis R, Ransing R, Heidari Mokarar M, Orooji M and Shalbafan M (2023) Mental illness stigma among perinatal women in low- and middle-income countries: early career psychiatrists' perspective. Front. Psychiatry 14:1283715. doi: 10.3389/fpsyt.2023.1283715
Received: 26 August 2023; Accepted: 10 November 2023;
Published: 05 December 2023.
Edited by:
Yuka Kotozaki, Iwate Medical University, JapanReviewed by:
Mahsa Nahidi, Mashhad University of Medical Sciences, IranTheddeus Iheanacho, Yale University, United States
Copyright © 2023 Pokharel, Philip, Khound, El Hayek, de Filippis, Ransing, Heidari Mokarar, Orooji and Shalbafan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mohammadreza Shalbafan, c2hhbGJhZmFuLm1yQGl1bXMuYWMuaXI=
†ORCID: Renato de Filippis orcid.org/0000-0001-6928-1224
Mohammadreza Shalbafan orcid.org/0000-0002-4536-3441
 Arpana Pokharel
Arpana Pokharel Sharad Philip1
Sharad Philip1 Samer El Hayek
Samer El Hayek Renato de Filippis
Renato de Filippis Ramdas Ransing
Ramdas Ransing Mohammadreza Shalbafan
Mohammadreza Shalbafan