- 1Departament de Psicologia Clínica i de la Salut, Universitat Autònoma de Barcelona, Barcelona, Spain
- 2Department of Psychology, University of Illinois at Urbana-Champaign, Champaign, IL, United States
- 3CIBER de Salud Mental, Instituto de Salud Carlos III, Madrid, Spain
Introduction: Childhood adversity is associated with the severity of multiple dimensions of psychosis, but the mechanisms underpinning the close link between the two constructs is unclear. Mentalization may underlie this relationship, as impaired mentalizing is found in various stages of the psychosis continuum. Nonetheless, the differential roles of self- and other-mentalizing in psychosis are not well understood.
Methods: Parallel multiple mediation was conducted for the relationship between a diverse range of childhood adversity types, including intentional and nonintentional harm, and schizotypy (positive, negative, disorganized), psychotic-like experiences (PLE) and paranoia via self-mentalizing (attention to emotions and emotional clarity) and other-mentalizing in n = 1,156 nonclinically ascertained young adults.
Results: Significant parallel multiple mediation models were found for all psychotic outcomes except negative schizotypy. The associations between intentionally harmful childhood adversity and psychotic outcomes were significantly mediated by increased attention to emotions for most models and decreased emotional clarity for some models. No significant mediation was found for parental loss. Paternal abuse was only mediated by attention to emotions whereas the effects of maternal abuse were mediated by attention to emotions and emotional clarity. Other-mentalizing only showed mediating effects on one of thirty models tested.
Conclusion: Results highlight the mediating role of impaired self-mentalizing in the association between childhood adversity and psychosis. This is consistent with disturbances of self-concept and self-boundary characterizing, in particular, the positive dimension of psychosis. Maternal versus paternal figures may contribute differentially to the development of mentalizing. These results could inform future preventative interventions, focusing on the development and maintenance of self-mentalizing.
1 Introduction
Childhood adversity is associated with the severity of multiple domains of psychosis symptoms (1–4) and predicts later transition to psychosis (5). It encompasses a range of experiences including emotional, physical, and sexual abuse, along with emotional and physical neglect, and other ‘nonintentional’ adverse experiences that may occur during childhood such as the loss of a parent. Nonetheless, mechanisms underpinning the close link between the different types of childhood adversity and psychosis remain unclear. One mechanism that may underlie the relationship between childhood adversity and psychosis that is associated with both factors is mentalization, a multidimensional construct that incorporates the ability to notice and understand internal mental states of the self and others (6, 7). The role of mentalization in severe mental health problems such as personality disorders and psychosis has evolved to indicate that it is a transdiagnostic protective factor (8) that can be fostered across the developmental course to improve social, functional, and therapeutic outcomes and wellbeing.
The link between maltreatment and mentalizing is intuitive, as mentalizing is developed through social interaction in which understanding of complex social cues is mirrored from important attachment figures (e.g., parents) back to the child (9). Through identification of children’s mental states, parents help the child to develop understanding of their own mental states (10). In the case of childhood maltreatment, however, attachment relationships are often disrupted, and children may not be given, could dislike, or may even miss learning this crucial developmental skill entirely by avoiding reflection of the caregiver’s mental states (11, 12). Thus, childhood adversity can result in subsequent impairment or delayed development of the ability to mentalize (13–15), as well as discriminate and understand emotions (16–19).
Expanding the knowledge base of mentalization led to rationales for the role of this construct in the psychosis spectrum (20–23) and to proposed (24) and successful mentalization-based interventions for psychosis (25); however, the specific mechanistic relationships between mentalization and psychosis are not well understood (21, 26). Indeed, a novel area of inquiry is understanding the role of mentalization at sub-clinical levels. From a dimensional perspective, schizotypy is conceptualized as a broad phenotype that encompasses personality traits, subclinical expressions like psychotic-like experiences (PLE), and psychotic disorders (e.g., schizophrenia) (27). Consistent with the multidimensionality of psychosis, schizotypy is composed of at least three dimensions, namely, positive, negative and disorganized schizotypy, that have distinct associations with risk factors and associated symptoms similar to psychotic disorders (27–29). Subclinical schizotypy is consistently associated with PLE and psychosis symptoms, and the development of schizophrenia-spectrum disorders (30–32). Studying subclinical manifestations of psychosis helps to avoid the confounding effects associated with clinical status (e.g., symptom severity, medication effects, stigma, comorbidity, etc.), and thus enhances the analysis of etiological factors and mechanisms involved in the developmental course and trajectory of psychosis risk and resilience (33–35).
Research supports poor mentalization, usually operationalized using Theory of Mind tasks to evaluate understanding of others’ mental states, as a risk factor in several stages of the psychosis spectrum. Mentalizing impairments are found in earlier stages of the psychosis spectrum at attenuated levels (36). They are present in help-seeking groups who experience temporary psychotic states (37–41), and in community samples reporting PLE (42, 43). More severe expressions of the psychosis continuum, such as schizoaffective disorder (44) and, in particular, disorganized schizophrenia, are also associated with impaired mentalization (44, 45). Furthermore, mentalization has been shown to mediate the relationship between several risk factors and PLE (46), psychosis symptoms (47, 48), and psychotic disorders (49).
Studies examining the differential relationships of impaired mentalization with psychosis dimensions are scant and clear conclusions cannot be drawn. In clinical psychosis, the negative symptom dimension in general (50) and social dysfunction in particular (51, 52) have been associated with poor mentalization, but hypotheses that mentalization is related to the positive dimension are less often supported by evidence (48, 51). Nonetheless, this could be due to operationalization of mentalization typically focused on understanding others’ mental states, but not understanding of one’s own (i.e., self mentalizing), which may be more closely related to the self-identity and self-boundary disturbances that characterize the positive dimension (53, 54). Although associations between positive symptoms and mentalization have been found between sub-threshold hallucinations/delusions and poor performance on mentalizing tasks (42, 55, 56), contradicting evidence exists (48, 51, 57). Studies examining associations between subclinical disorganized schizotypy and mentalization have been limited and the results are equivocal; to our knowledge, only one study examines this relationship, which found that only social anxiety (negative dimension) and odd speech (disorganized dimension) were associated with impaired mentalization, which mediated the relationship between schizotypy and thought problems, an indicator of disorganized outcomes (58).
Whereas associations between aberrant mentalization and different levels of psychosis expression are established, to date, the great majority of mentalization research has considered the construct as a whole, despite mentalization being understood to operate under four primary dimensions; self-other; automatic-controlled, cognitive-affective, and internal-external (59). Recently, a call for increased focus on the dimensions of mentalizing and their distinct roles and significance in various spectral disorders has been posed (59). Research by our group evaluating self- and other-mentalization as mediators and moderators in mental health symptomatology indicates that self-mentalization is a particularly relevant factor (60–62). Although the role of the self has been a focus of psychosis spectrum research for decades (63–68), a paucity of psychosis research to date has focused on self-mentalization (69).
1.1 The present study
In an aim to integrate both the understudied disorganized schizotypy dimension and the dearth of self-mentalization evidence particularly in subclinical schizotypy, this study will explore the relationship of the self-other polarity of mentalization with the three schizotypy dimensions. First, we aim to explore the associations of self- and other-mentalization with positive, negative, and disorganized schizotypy in a nonclinically ascertained sample. Secondly, we will examine, for the first time, the possible mediating role of self-and other-mentalization in the relationship between a wide range of childhood adversity experiences with schizotypy, PLE, and paranoia. To our knowledge, only one study to date has examined the mediating role of mentalization in the relationship between childhood maltreatment and psychosis, albeit in a clinical sample, which revealed that mentalizing only mediated the relationship between childhood maltreatment and negative symptoms (48). Of note, different forms of intentional (e.g., maltreatment) and nonintentional (e.g., parental loss) adversity experiences, as well as the distinction between paternal versus maternal abuse during childhood, will be examined.
We predicted that positive, negative, and disorganized schizotypy would be associated with impaired self-mentalization. That is, individuals with high schizotypy would notice and understand their own emotions, thoughts, and feelings more poorly. While some evidence suggests that high positive and negative schizotypy dimensions are linked to deficits in emotional awareness and regulation (70), given the lack of clear grounding on the differential contributions of self-mentalizing factors versus other-mentalizing in schizotypy, and that most mentalization research in psychosis has only focused on other-mentalization, the study is exploratory regarding self-mentalization. For other-mentalization, we expected that the associations with schizotypy dimensions in this nonclinical sample would be aligned with previous research (i.e., negatively associated with other-mentalization) (36, 44, 45, 47, 71, 72), albeit at an attenuated level. Next, we expected that self- and other-mentalization would mediate the association between childhood maltreatment and all schizotypy dimensions, PLE and paranoia. Finally, following previous results found in epidemiological studies (73), prospective cohorts (74) and the group’s previous findings using experience sampling methodology (75), we hypothesized that the relationship between childhood adversity and psychotic outcomes via mentalizing would be more pronounced for those types of adversity characterized by an ‘intention to harm’ as compared to accidental adversity such as loss of a parent.
2 Methods
2.1 Participants
Participants were recruited at a university using posters and an email distributed to all students and university staff inviting them to take part in a broader study about environmental sensitivity and mental health (approved by the Ethics Committee of the Universitat Autònoma de Barcelona, ref. 5426). Participants were excluded if they were under 18 years old or had grandparents of non-Spanish origin, an exclusion criterion placed for the context of the broader study for genetic analysis purposes. After removing n = 47 participants of non-Spanish origin, n = 38 participants with careless responses according to the Infrequency Scale (76), and data from n = 7 dropout participants, responses from the original sample of n = 1,246 were reduced to n = 1,156 (Mage = 23.29, SD = 6.49; range 18–62 years; 76.2% female). Of the final samle, n = 545 (47.1%) of participants had previously or were currently undergoing psychological treatment, and n = 204 (17.6%) had previously or were currently undergoing pharmacological treatment related to mental health.
2.2 Procedure
After obtaining informed consent, participants were administered an online questionnaire via Qualtrics survey software that included all materials of the present study. Participants were able to re-enter the questionnaire to complete it in multiple sessions if desired with a maximum allotted time for completion of 3 days.
2.3 Materials
2.3.1 Childhood adversity
The Childhood Trauma Questionnaire-Brief (CTQ-B) (77) is a widely used self-reported measure with 28 items assessing the severity of sexual, physical and emotional abuse and physical and emotional neglect before the age of 18 years old. To reduce factors for childhood adversity, subscale totals for physical abuse, emotional abuse, physical neglect and emotional neglect were reduced to a single component for emotional/physical adversity. A detailed description of this procedure can be referenced in the ‘Data Analysis’ section.
The Childhood Care and Abuse Questionnaire-Brief (CECA.Q) (78–80) assesses aspects of childhood adversity that are not covered in the CTQ-B (e.g., parental loss, role reversal). It includes subscales for maternal antipathy, paternal antipathy, maternal psychological abuse, paternal psychological abuse, parental loss, role reversal and support. All CECA.Q subscales were included in the present study except the support subscale, which does not measure adversity.
2.3.2 Mentalization
The recently developed Mentalization Scale (Ment-S) (81) was administered as it is the only mentalization questionnaire with a distinct factor for other-mentalization. The 10 items of the other-mentalization subscale were assessed and a total sum score was employed for the study. The Trait Meta-Mood Scale-24 (TMMS) (82) was administered to evaluate self-mentalization, as it offers two 8-item factors to further classify emotional self-knowledge: attention to emotions (8 items) and emotional clarity (8 items).
2.3.3 Schizotypy, positive PLE and paranoid traits
The Multidimensional Schizotypy Scale-Brief (MSS-B) (83) is a 38-item self-report measure designed to assess the positive (MSS Positive; 13 items), negative (MSS Negative; 13 items) and disorganized (MSS Disorganized; 12 items) schizotypy dimensions. Evidence shows that this scale overcomes limitations of other schizotypy measures such as an unclear conceptual framework, outdated items, ethnic/sex differences, or exclusion of the disorganized dimension. The scale has good internal reliability and construct validity (28, 83).
PLE were measured using the frequency score of the positive subscale (20 items) of the Community Assessment of Psychic Experiences (CAPE) (84). Paranoia personality traits were assessed with the ideas of reference (9 items) and suspiciousness (8 items) subscales of the Schizotypal Personality Questionnaire (85).
2.4 Data analysis
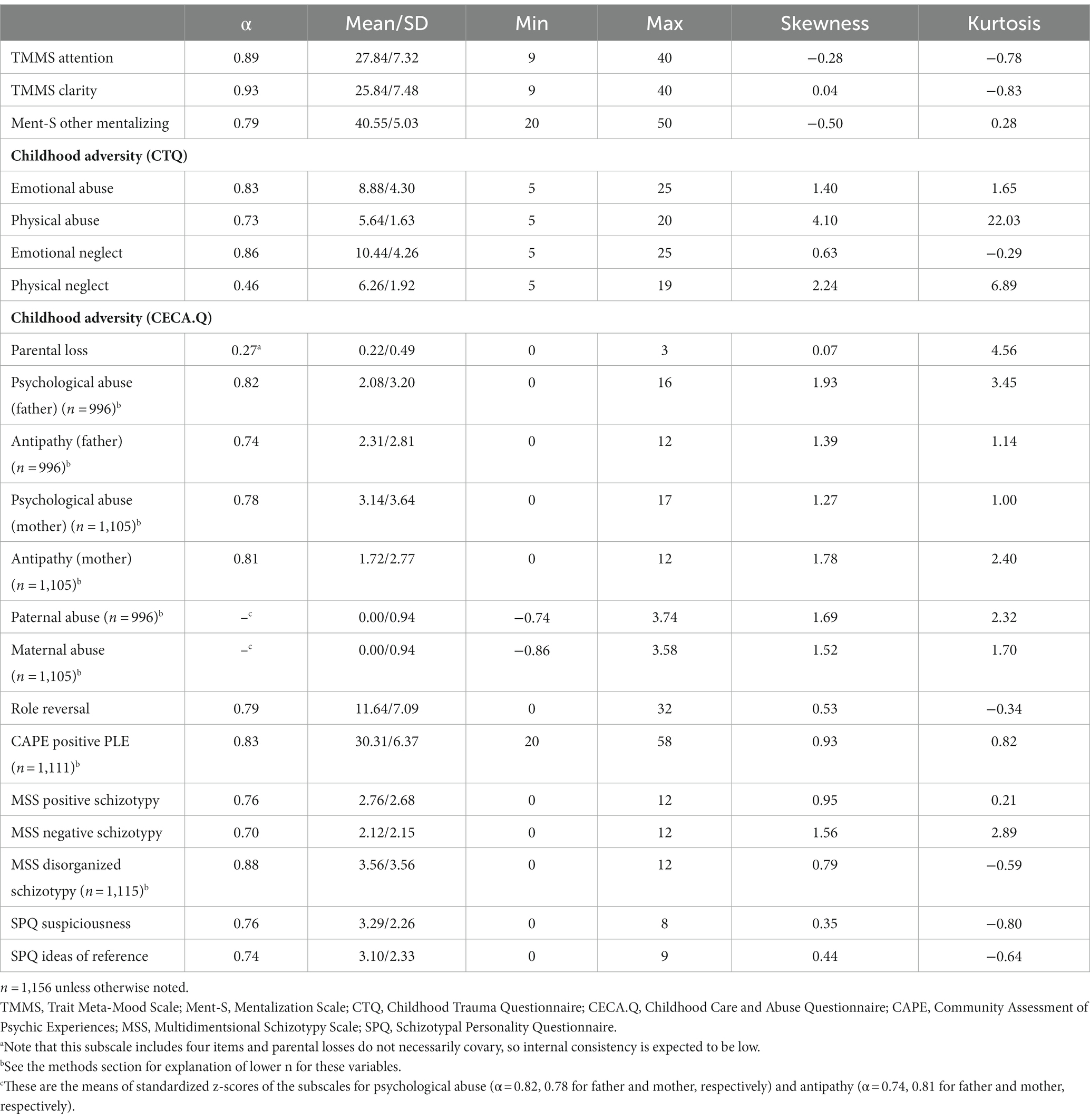
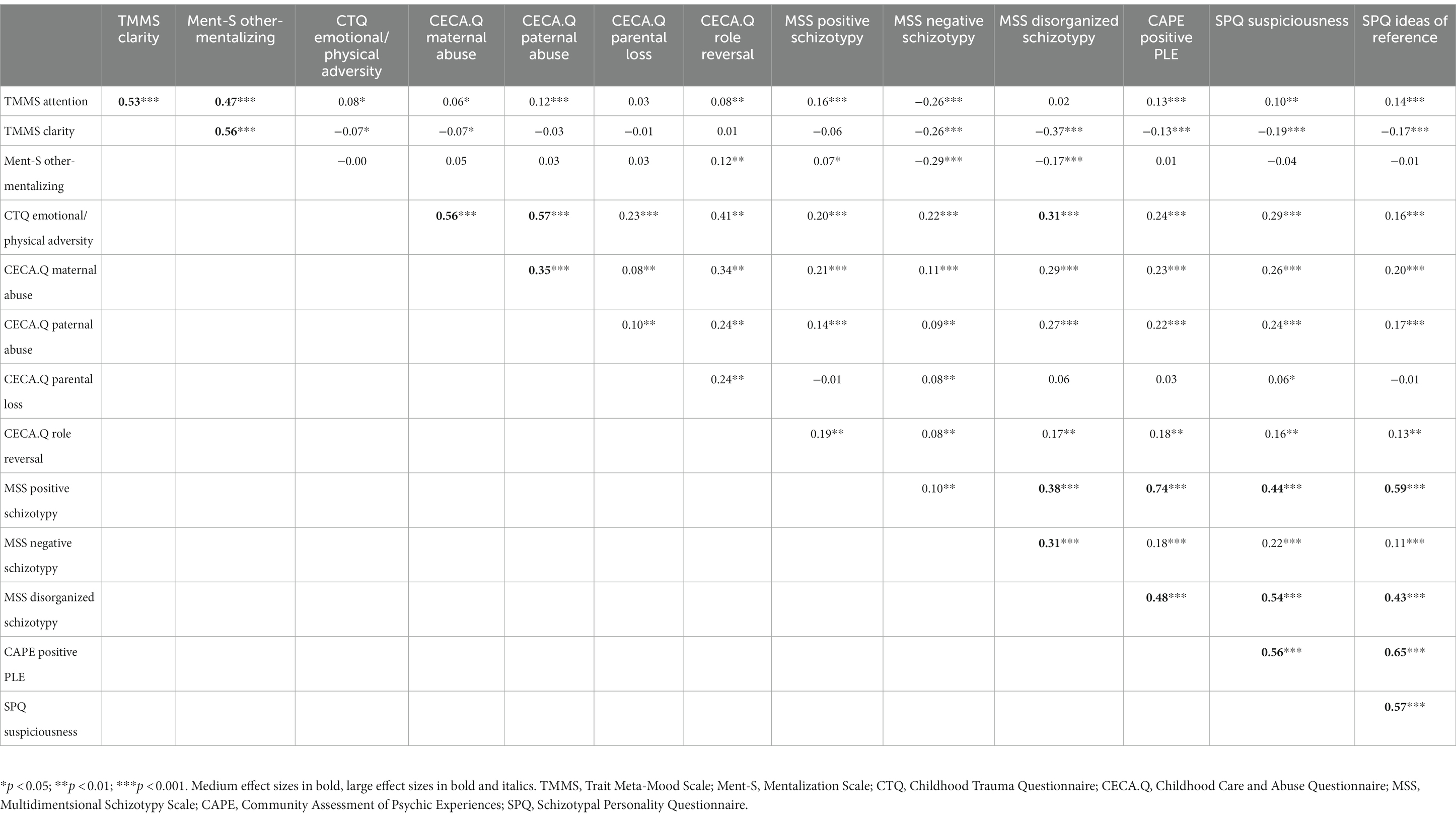
Descriptive statistics, internal consistencies and correlational analysis were conducted for all variables of interest (Table 1). Note that some subscales differ slightly in their number of respondents. For CAPE Positive PLE and MSS Disorganized Schizotypy, missing data is due to a technical error in the data collection software. For CECA.Q psychological abuse and antipathy, reduced responses are reflective of the number of respondents who only had a paternal or a maternal figure, but not both. Sample size for CECA.Q antipathy is in all cases smaller compared to psychological abuse because one item of this subscale was only responded by participants who have siblings.
To reduce factors for childhood trauma (to 5 predictor variables) and the number of mediation models, two a priori analyses were conducted using trauma measures. Given the low-endorsement rates of sexual abuse and that primarily modest-to-high correlations (0.26–0.65) were observed between CTQ non-sexual abuse subscales (emotional abuse, emotional neglect, physical abuse, and physical neglect), and following Sheinbaum et al. (86), principal components analysis (PCA) was conducted to produce a single emotional/physical adversity factor. This PCA yielded one component that explained 59% of the variance. Additionally, due to high correlations (r = 0.75 for father and r = 0.76 for mother, p < 0.001 for both) rather than exploring CECA.Q psychological abuse and CECA.Q antipathy separately for maternal and paternal figures, we elected to combine standardized (z) scores for available data on psychological abuse and antipathy into one measure of adversity for each parent: CECA.Q maternal abuse and CECA.Q paternal abuse.
Moderate-strong correlations (0.47–0.57) were observed between mentalization domains, and thus the three mentalizing factors—attention to emotions, emotional clarity and other-mentalizing—were simultaneously entered into parallel multiple mediation models for all outcome variables. A visual depiction of the a-priori mediation models tested can be seen in Figure 1. Parallel multiple mediation analyses were conducted using Hayes (87) PROCESS Macro Model 4 for assessing indirect pathways. Compared to the use of several single mediation analyses, parallel mediation accounts for the variance of other mediators in the model and is well-suited to inter-correlated mediators, as it offers a more precise estimate of indirect effects. This technique has been repeatedly demonstrated as useful in psychosis research (86, 88, 89).
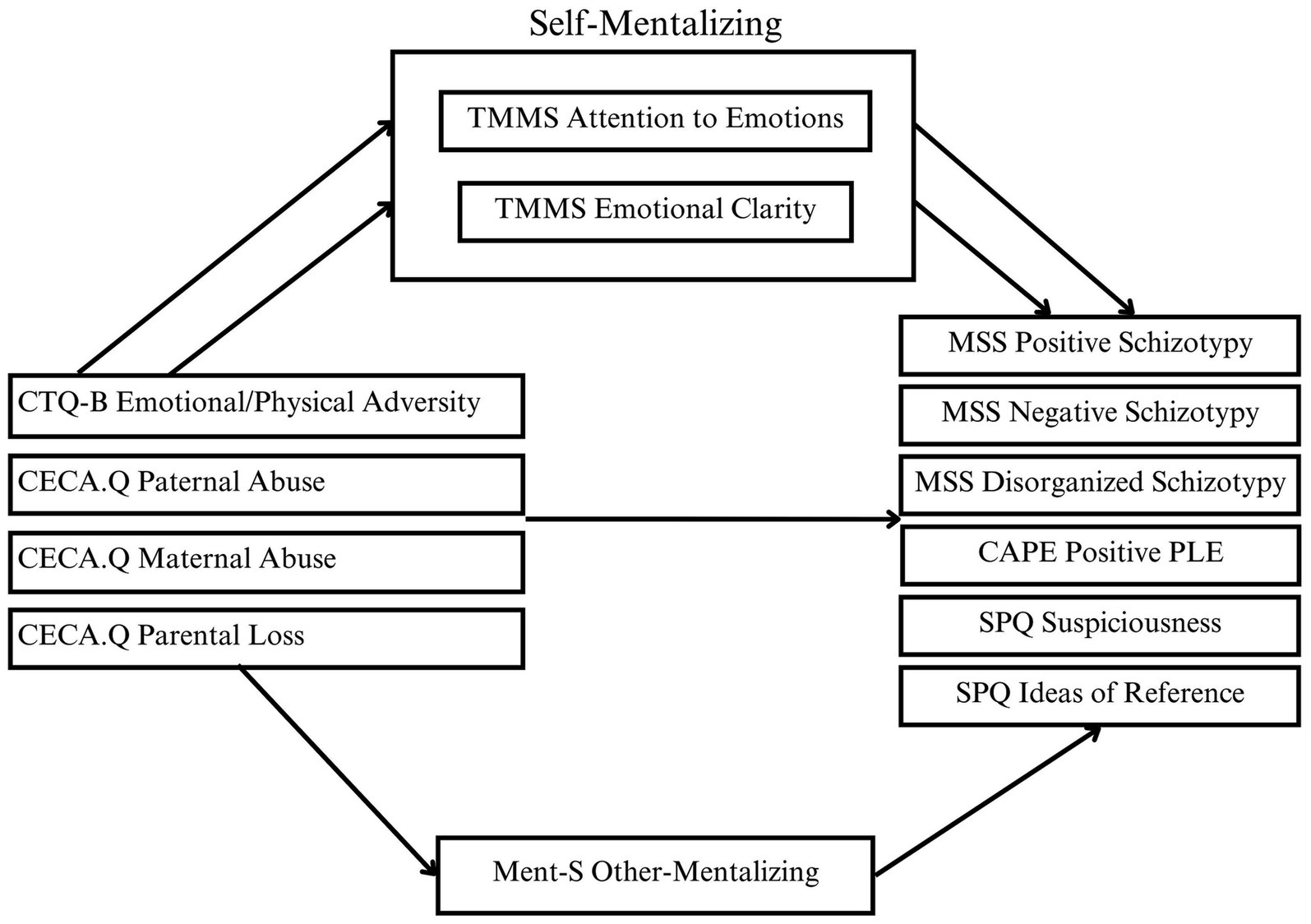
Figure 1. Parallel multiple mediation models evaluating mediation of mentalizing factors in the relationships between childhood adversity and psychotic-like outcomes.
Mediations of the associations of trauma and psychosis outcomes via mentalization are demonstrated by significant indirect coefficients with lower-and upper-bound confidence intervals that do not include zero. Six mediation models were tested for each of the nonclinical psychosis outcomes (positive, negative and disorganized schizotypy, positive PLE, suspiciousness, and ideas of reference) and with each of the five trauma indicators (emotional/physical adversity, maternal abuse, paternal abuse, role reversal, and parental loss) as the independent variable and the three mentalizing domains (attention to emotions, emotional clarity, and other-mentalizing) entered simultaneously as mediators, resulting in a total of 30 mediation models analyzed. Analyses were limited to these a priori hypothesized models. Bootstrapping with 10,000 resamples was conducted to generate bias-corrected confidence intervals.
3 Results
Descriptive statistics for all variables are presented in Table 1 and Pearson correlations are in Table 2. Despite small effect sizes, direction of associations as displayed in Table 2 indicates a pattern of positive associations for attention to emotions with schizotypy, PLE and suspiciousness, but negative associations with emotional clarity. Meanwhile, other-mentalizing was had small to moderate sized associations with negative schizotypy and disorganized schizotypy, but was not associated with positive schizotypy, PLE or paranoia. Moderate or near-moderate associations were observed for negative schizotypy with all mentalization factors and for disorganized schizotypy with emotional clarity.
3.1 Mediation analyses
After entering the three mentalization factors as parallel mediators in the models, increased attention to emotions was a significant partial mediator for most models including intentional forms of adversity (i.e., emotional/physical adversity, maternal and paternal abuse, and role reversal) and decreased emotional clarity for some models. All significant mediations were partial. Note that the general direction of effects for attention to emotions and emotional clarity in the mediation models is consistent with correlational analysis; that is, higher scores for attention to emotions is associated with higher outcomes, while lower clarity is associated with higher outcomes. Other-mentalizing was only a significant mediator in one model that examined the relationship between role reversal and negative schizotypy.
For the model using the combined emotional/physical adversity component, parameter estimates of the direct, total, and indirect effects can be found in Table 3. Indirect effects for increased attention to emotions in this model were significant for positive schizotypy, negative schizotypy, disorganized schizotypy, PLE, suspiciousness and ideas of reference. There was a significant indirect effect for emotional/physical adversity via emotional clarity on positive schizotypy, PLE and suspiciousness. Indirect effects of emotional clarity on positive schizotypy, disorganized schizotypy and positive PLE were such that trauma was associated with lower emotional clarity which is, in turn, associated with higher scores on psychotic outcomes; however, the effect of emotional/physical adversity on suspiciousness via emotional clarity was the opposite, such that lower emotional clarity was related to decreased suspiciousness. Outcomes that were significant for both attention to emotions and emotional clarity in this model reflect relatively equivalent effect sizes for the two specific indirect effects, with the exception of disorganized schizotypy which was driven predominantly by emotional clarity.
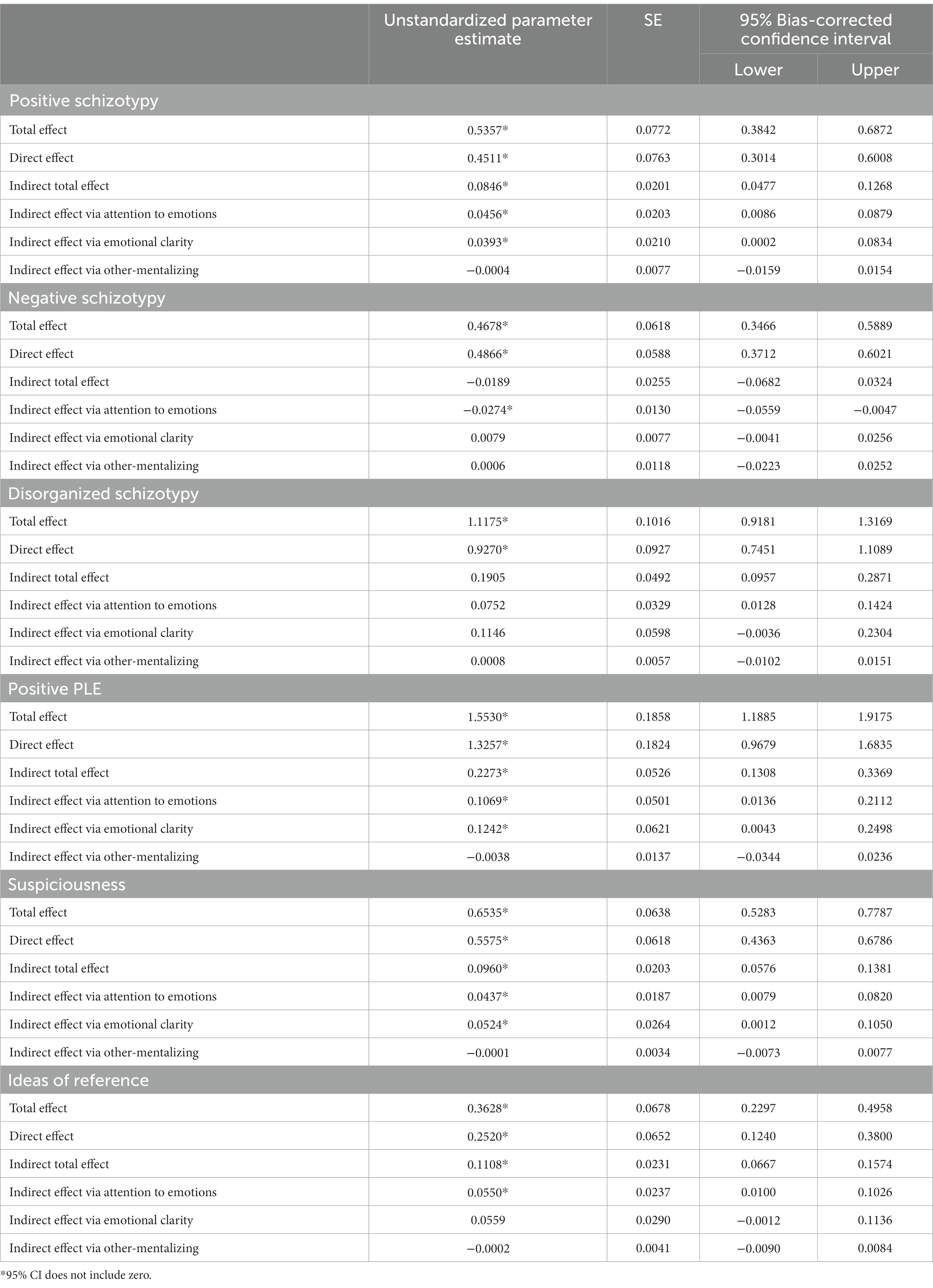
Table 3. Parallel multiple mediation analyses examining indirect effects of CTQ motional/physical adversity on nonclinical psychotic phenomena via self-mentalizing factors (1) attention to emotions and (2) clarity of emotions, and (3) other-mentalizing.
In the model for paternal abuse (Table 4), there was a significant indirect effect of paternal abuse on all outcomes via higher attention to emotions. In the case of negative schizotypy, the indirect total effect of all mediators combined was nonsignificant, indicating that there was no parallel mediation, but that attention to emotions remained a significant mediator of the association between paternal abuse and negative schizotypy after controlling for the other mediators (emotional clarity and other-mentalizing). Unlike other outcomes, the indirect effect of increased attention to emotions for this model was related to lower scores of negative schizotypy. No significant indirect effects were found for emotional clarity or other-mentalizing in the relationships between paternal abuse and psychosis outcomes. Mediating effects of mentalization on all outcomes had relatively small effect sizes but were most pronounced for positive PLE and disorganized schizotypy, which are roughly double those of other outcomes.
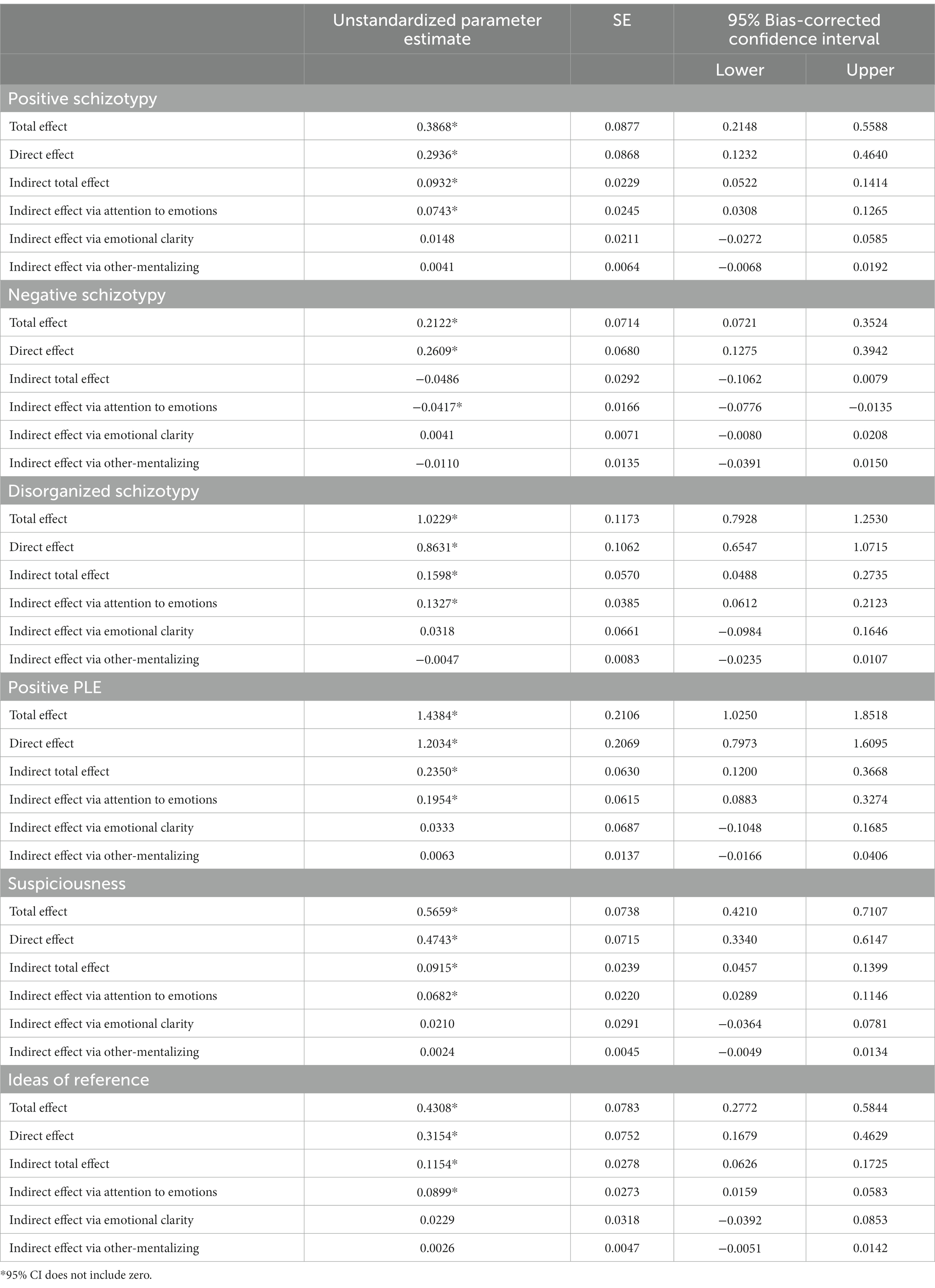
Table 4. Parallel multiple mediation analyses examining indirect effects of CECA.Q paternal abuse on nonclinical psychotic phenomena via self-mentalizing factors (1) attention to emotions and (2) clarity of emotions, and (3) other-mentalizing.
The model evaluating the multiple parallel mediation model between maternal abuse and psychosis outcomes with mentalization factors as mediators is presented in Table 5. There was a significant indirect effect of maternal abuse on psychosis outcomes via greater attention to emotions for positive schizotypy, disorganized schizotypy, PLE, suspiciousness and ideas of reference. In the case of negative schizotypy, maternal abuse was associated with higher attention, but decreased negative schizotypy. Contrary to results for paternal abuse, significant indirect effects of decreased emotional clarity were also found for maternal abuse on most outcomes: positive schizotypy, disorganized schizotypy, suspiciousness and ideas of reference. All outcomes had a significant indirect total effect (Table 5) indicating multiple parallel mediation, except for negative schizotypy, which indicates that its only significant mediator, attention to emotions, has an indirect effect on negative schizotypy even after controlling for effects of other mediators. Although emotional clarity did not reach significance as a mediator for paternal abuse, in general, the effect sizes for specific indirect effects of attention to emotions between maternal abuse and outcomes are roughly half of those for paternal abuse.
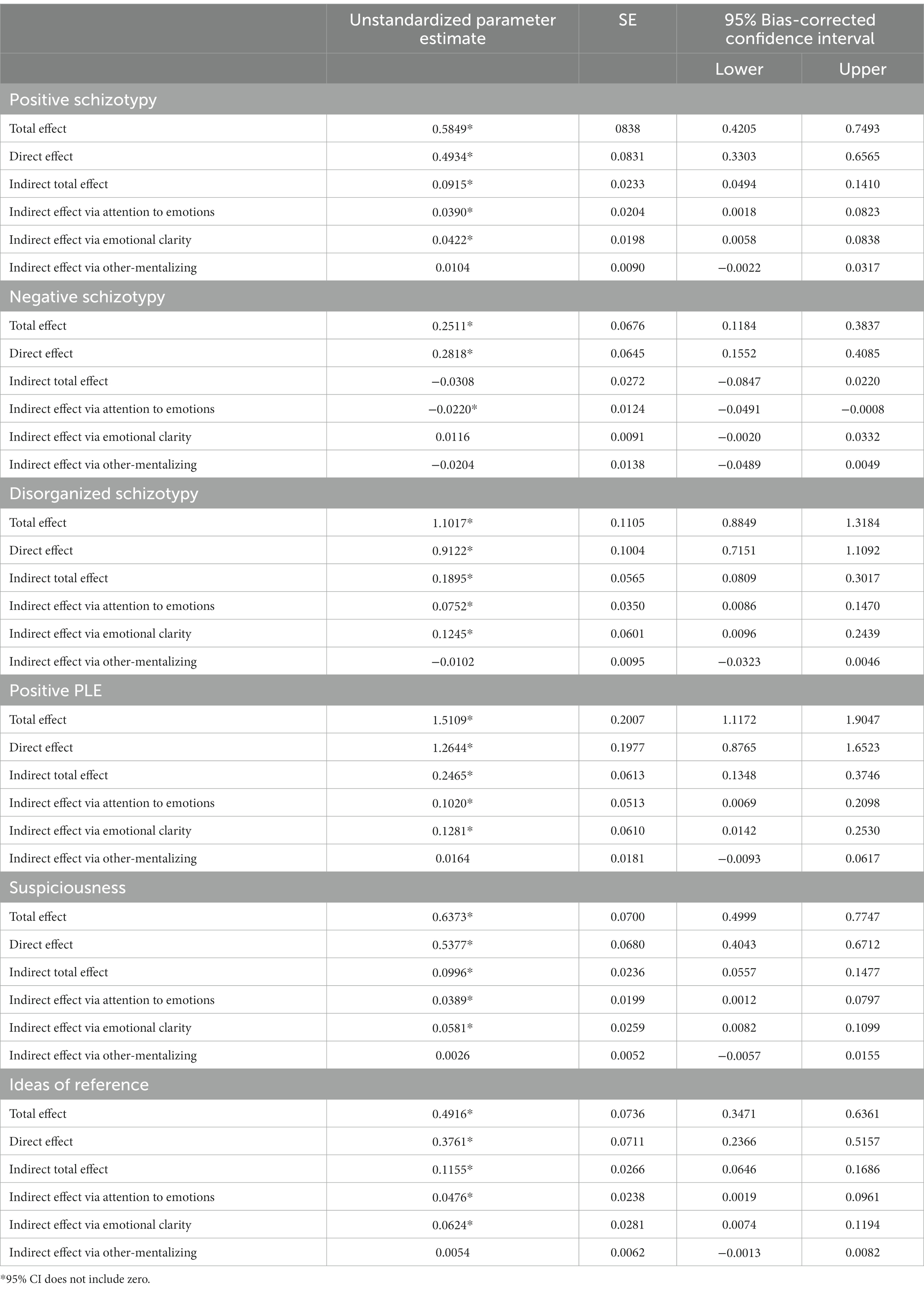
Table 5. Parallel multiple mediation analyses examining indirect effects of standardized scores of CECA.Q maternal abuse on nonclinical psychotic phenomena via self-mentalizing factors (1) attention to emotions and (2) clarity of emotions, and (3) other-mentalizing.
There was a significant indirect effect of role reversal on all indicators of schizotypy, positive PLE and paranoia via attention to emotions, which were most pronounced for the positive dimension (Table 6). Significant indirect effects were found via emotional clarity for suspiciousness, positive schizotypy, and ideas of reference. The only significant indirect effect of other-mentalizing was found in this model for the association between role reversal and negative schizotypy. Effect sizes in this model are attenuated compared to other models.
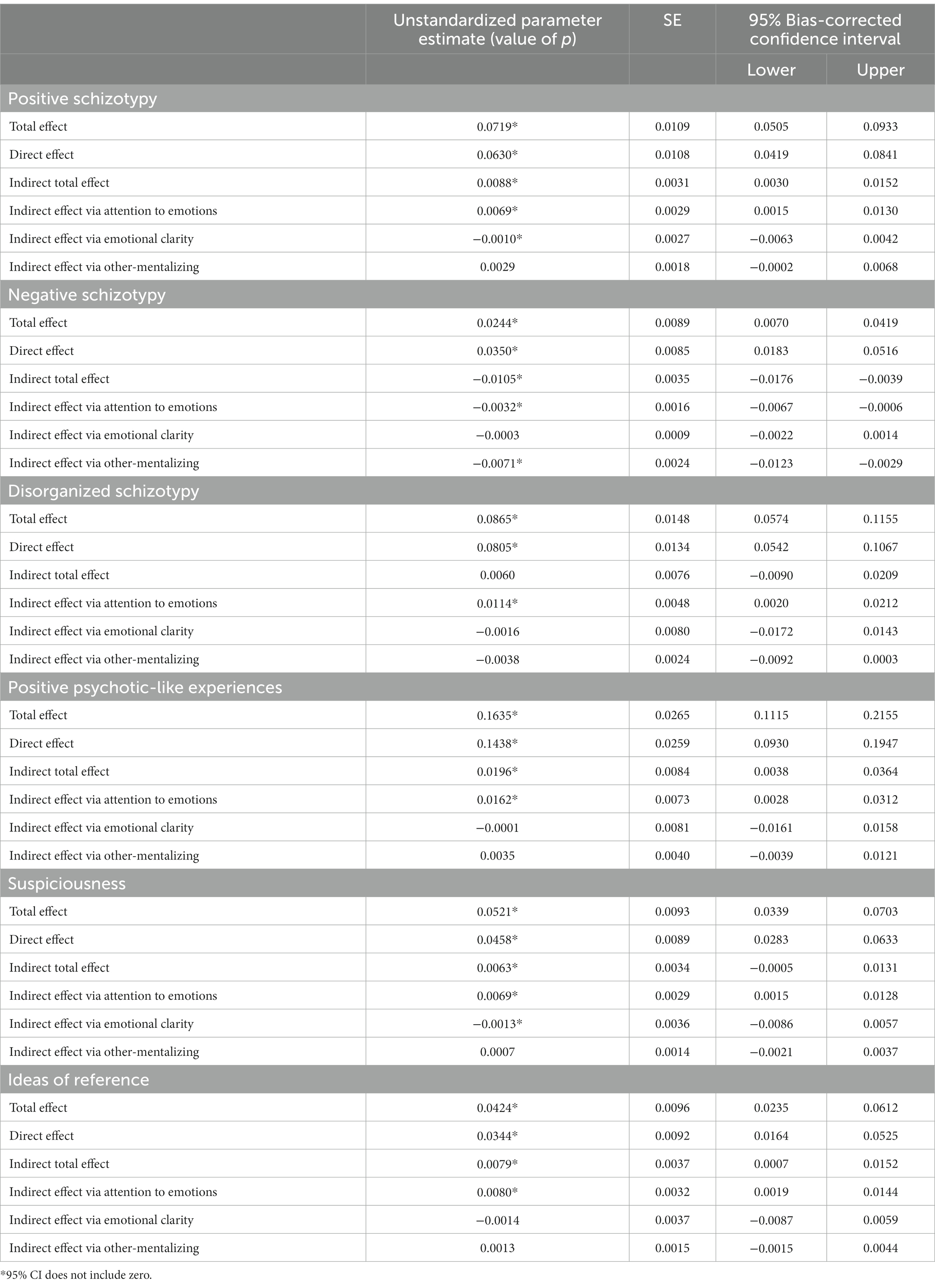
Table 6. Parallel multiple mediation analyses examining indirect effects of CECA.Q Role Reversal on nonclinical psychotic phenomena via self-mentalizing factors (1) attention to emotions and (2) clarity of emotions, and (3) other-mentalizing.
Parental loss was not related to any psychosis outcomes via mentalizing (Table 7). The only significant results were found for negative schizotypy and suspiciousness. There was a significant effect of parental loss on negative schizotypy after controlling for all mediators and a significant total effect of parental loss on negative schizotypy, along with a significant total effect of parental loss on suspiciousness.
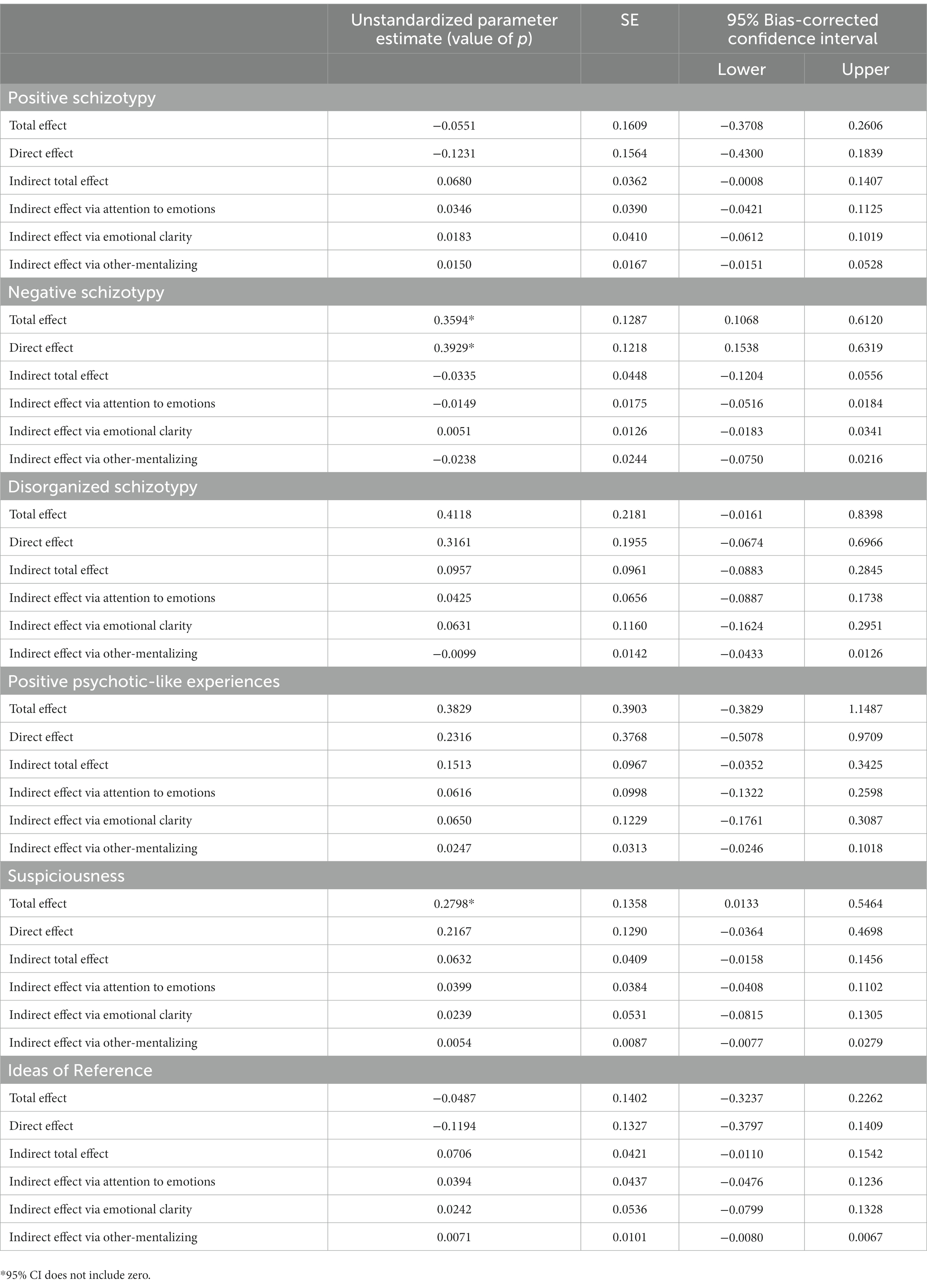
Table 7. Parallel multiple mediation analyses examining indirect effects of CECA.Q parental loss on nonclinical psychotic phenomena via self-mentalizing factors (1) attention to emotions and (2) clarity of emotions, and (3) other-mentalizing.
4 Discussion
The present study explored, for the first time, the relationship between the self and other dimensions of mentalization with schizotypy, and extended these findings by examining the mediating role of self- and other-mentalization in the associations between a wide range of childhood adversities, including intentional (i.e., emotional/physical adversity, maternal and paternal abuse, and role reversal) and nonintentional (i.e., parental loss) harm, and psychotic-like outcomes.
Overall, associations of mentalizing domains with the schizotypy dimensions were consistent with previous research in other mental health phenotypes, such that attention to emotions is positively associated with impairment and increased symptoms, while emotional clarity is consistently supported as a protective factor, or, in other words, one that attenuates impairment (61, 62, 90, 91). The positive schizotypy dimension was directly and more strongly correlated with attention to emotions than with emotional clarity, which is consistent with findings that positive schizotypy is associated with increased attention to emotions in general, lower clarity (90) and lower emotional recognition (92). Interestingly, the disorganized dimension had a nonsignificant correlation with attention to emotions, but a moderate inverse association with emotional clarity, suggesting that independent of how much people with disorganized schizotypy attend to their thoughts, they struggle to understand them and thus, lack clarity. One study found that clarity of self-concept is more transient in clinical psychosis and demonstrated that decreased clarity was associated with both positive and negative psychosis symptoms, however disorganized symptoms were not evaluated (63). Recent studies have suggested that emotional dysregulation is a core component of the disorganized schizotypy dimension (93).
Overall, a pattern of significant parallel multiple mediation was observed for all models including intentional, but not nonintentional, forms of adversity and all psychotic-like traits and experiences except negative schizotypy. Specific indirect effects revealed that childhood adversity is related to increased levels of psychotic-like features through increased attention and secondarily through decreased clarity, but that other-mentalizing is not a relevant factor in these relationships. As the singular exception, the model examining the impact of role reversal showed a significant parallel multiple mediating effect on almost all psychotic-like features, including negative but not disorganized schizotypy, and the association between role reversal and negative schizotypy was significantly mediated by other-mentalizing. Decreased emotional clarity and increased attention to emotions were significant mediators in the associations between maternal abuse and nearly all psychosis spectrum outcomes (except negative schizotypy), whereas for paternal abuse, significant indirect effects were only found for attention to emotions. There was no significant indirect effect of parental loss on psychotic-like features via mentalizing.
Most of the parallel mediation models were not significant for negative schizotypy; however, specific indirect effects suggest that increased attention to emotions was inversely associated with negative schizotypy, consistent with the well-established finding that negative schizotypy is associated with diminished emotional expression and experience (32, 94). This dimension is characterized by alogia, anergia, avolition, anhedonia, flat affect, and a general disinterest in other people and the world as a whole (27). In general, comparisons with antecedent, similar research are difficult to make as only one other study has evaluated such relationships (albeit in a clinical sample) (25), however the models are incomparable as the previous paper followed mediation requirements outlined by Baron & Kenny (95), which supposes that all variables must be associated to conduct mediation and thus indirect effects were only evaluated (and supported) for negative symptoms. Conversely, our study followed the process outlined by Hayes (96), which does not require empirical associations, but instead, theoretical support for proposed indirect associations. Thus, several additional models were conducted that revealed, we believe, thought-provoking results.
4.1 Intentional versus nonintentional childhood adversity
To our knowledge, no previous research has evaluated whether there are differential effects of mentalization on the relationship between intentional versus general, unintentional childhood adversity and psychotic outcomes, and particularly not in a nonclinically ascertained sample. Results revealed that only intentionally harmful childhood adversity (i.e., maltreatment and neglect) impacted mentalization functioning, compared to nonintentional childhood adversity as indexed by parental loss. The measure used for parental loss in this study assesses the loss of one or both parent figures before age 18 due to death, separation, or abandonment. Such losses are certainly impactful to those who suffer them, as they almost inevitably result in a pivotal destabilization of family, extensive emotional consequences, and often essential and monumental family restructuring (97). Despite the repercussions of a central loss such as that of a parent figure, no significant effects were found on psychotic-like features via mentalizing, and parental loss did not affect most outcomes, even after controlling for mentalization levels. This could indicate that mentalization is negatively affected more by central but harmful attachment figures than potential consequences to attachment relationships following parental loss such as (1) a lack of attachment figures, or (2) more ‘distant’ attachment figures, perhaps outside of the family, that develop epistemic trust with a child after they suffer parental loss. Indeed, some literature suggests that adjustment difficulties following bereavement are not consistently related to grieving but are instead accounted for by inadequate care following parental loss (98). Such a finding emphasizes the importance of a parent’s role as a supportive, understanding, and responsible adult figure, rather than a dangerous and untrustworthy one (99).
4.2 Differential effects of maternal and paternal abuse
A non-hypothesized finding that merits further study was the differential effects of maternal versus paternal abuse on self-mentalizing factors. Results suggest that increased attention in the wake of childhood adversity is more impactful in the case of paternal abuse, as coefficients for the mediating role of attention to emotions are roughly double the same coefficients for maternal abuse for all outcomes. Nonetheless, in the case of maternal abuse the additional mediating effect of impaired clarity is present for all outcomes excepting negative schizotypy. Despite gender-role stereotypes whereby maternal figures are responsible for child rearing and paternal figures provide resources for the family outside the home being challenged in recent years, the mean age of our sample suggests that most maternal figures may still be the principal caregiver. Considering that mentalization is usually developed through relationships with said primary caregiver(s) (9), mentalization could be severely impacted if the mother–child relationship is damaged. For example, a ‘good enough mother’ conceptualized by Winnicott (100) and later expanded upon through attachment relationships by Bowlby (101) is suggested to be necessary for adequate child development, particularly of socioemotional abilities such as mentalization. If, for example, the maternal figure is the primary caregiver, but instead of providing security, stability and fostering epistemic trust with the child, fails to play this role and breaks epistemic trust by engaging in abusive or neglectful behavior, the child’s mentalization skills may be more highly impaired than they would in a father-child relationship. This notion is supported in a recent study which demonstrates that maternal psychological states are more impactful on children’s adult clinical psychosis status than paternal psychological states (102). In cases where the father is the primary caregiver, perhaps this dynamic could be expected to be reversed, however, extant literature does not shed light on this question.
4.3 Know thyself: the role of the self
An overwhelming pattern of significant findings for self- but not other-mentalizing was revealed in analyses of this study. Extant literature suggests that adaptive emotional strategies are helpful in preventing psychosis, and that emotional clarity has been shown to be ‘protective’ from the development of other mental health disorders (103). This, combined with evidence of (especially self-) mentalization as a transdiagnostic protective factor (8, 60, 62, 91), suggests that maintaining good self-mentalizing in the wake of adverse events could potentially result in better outcomes. The implication of an impaired understanding of the self in psychosis is well-accepted, with results suggesting that disturbances in understanding and identifying with the self may underpin self-disorders which hyper-aggregate in psychotic spectrum disorders (104, 105). Perhaps the ability to self-mentalize, developed during the formative years, could impede significant impairments in the development of self-identity, protecting from psychotic outcomes. Although the precise role of self-mentalization is not well understood, results that partially support our findings have been found in various stages of the psychosis spectrum; for example in self-concept clarity (63), misattributions of self-referential representations (106, 107), and even after traumatic life events which importantly interact with the self to affect psychosis proneness (108). Evidence supporting good mentalizing as a buffer for the impact of persecutory delusions (positive dimension) on functioning (109) further suggests that mentalizing can be protective, but, when impaired conveys risk.
Until the call for evaluation of distinct mentalization polarities (59), mentalization was evaluated solely as a general construct, without exploring differential contributions of self- vs. other- polarities of mentalization. Nonetheless, positive symptoms are highly implicated in self-identity and self-boundary (53, 54) and thus measures of self-mentalization may more precisely capture characteristics of positive schizotypy than other-mentalization. Indeed, contemporary cognition research suggests that understanding of the ‘self’ forms the stem of understanding the ‘other’ (110). Overall, this evidence combined with the consideration that psychotic symptoms are viewed as a ‘disturbance to the self’, and that self-mentalizing gives rise to self-organization, emotional regulation, and sense of agency, might account for the fact that that psychosis spectrum impairments are substantially associated with self-mentalizing. Of note, self-mentalizing not only impacted positive psychotic-like features, but also the disorganized schizotypy dimension. Potentially, impaired self-mentalizing (i.e., increased attention but decreased clarity, in alignment with our results) after the exposure to childhood adversity negatively impacts the ability to organize and express thoughts and behavior, that is, resulting in a manifestation of disorganized schizotypal features.
Overall, our lack of significant findings for other-mentalizing could be due to higher discrimination of the mentalization construct in the current study, whereby self- and other-mentalizing are separated, revealing that self-mentalizing drives associations. In fact, only one model revealed an indirect effect via other-mentalizing, in which childhood experiences of role reversal decreased negative schizotypy through increased other-mentalizing. To date, mentalization has been operationalized primarily using various Theory of Mind tasks, which overall evaluate other-mentalizing. These studies support (other-) mentalizing as a mediator of childhood neglect and psychosis symptoms (47), of trauma/expressed emotion and schizotypal symptoms (72) and have even found that (other-) mentalizing fully mediates the association between social perception difficulties and negative symptoms (71). Although role reversal and its impact on other-mentalizing has not been examined previously, one may speculate that assuming parental responsibilities and providing emotional support to the parent from a young age might subserve the development of an increased capacity to think about and understand other’s emotions and needs (i.e., other-mentalizing) and this, in turn, may increase one’s curiosity and openness to the world (i.e., diminished negative schizotypy).
4.4 Strengths and limitations
This study benefits from (1) its novelty in exploring self- and other-mentalization in a combined study, (2) exploring a wide range of childhood adversity types, including distinctions between intentional and nonintentional harm, (3) a unique examination of the role of maternal versus paternal abuse, and (4) the assessment of psychosis spectrum outcomes in an extensive sample of nonclinical young adults. While assessing impairment at the clinical level is helpful, it may not be early enough to develop interventions and understanding that can ultimately prevent severe functional impairment, particularly in the case of psychosis (110). Schizotypy offers a unifying construct for the psychosis spectrum that provides benefits for understanding the role of mechanisms such as mentalization in the development of disorders (26, 35). More so, acknowledging the multidimensionality of the construct allows to unravel the distinct etiological and developmental pathways that specifically lead to positive, negative or disorganized manifestations (27). Thus, the study of schizotypy features in a nonclinically ascertained sample may, in fact, be a chief strength of the study.
Unfortunately, the cross-sectional nature of our study design does not allow for causal associations to be evaluated, although hypotheses were made based on extant literature and theoretical grounding which guided subsequent analysis; thus, the present findings should be replicated in longitudinal studies. A small amount of missing data due an error in survey administration software resulted in few items being removed from certain measures for some participants. Albeit slight, this limitation should be noted. Small effect sizes are also found throughout the study, which are often frowned upon, however, discovering significant results aligned with theoretical hypotheses in a nonclinical sample suggests that, further along the developmental trajectory for psychotic disorders when differences are more glaring, effect sizes would be more pronounced. Nonetheless, future research could evaluate a similar model in clinical psychosis expressions at a clinical level of psychosis expression.
4.5 Conclusions, implications, and future directions
The present findings assessing self- and other-mentalizing separately but simultaneously offered what could be new understanding of the self-other polarities in the psychosis spectrum: self-mentalizing may be the driver behind evidence of impaired mentalization, particularly in those who have experienced intentionally harmful childhood adversity. Mentalization-based treatment has already shown to be effective in reducing psychosis symptoms (111), but these findings further illuminate awareness of which specific mentalization dimensions should be targeted. Indeed, this offers compelling implications for interventions and psychoeducation across the psychosis spectrum. Psychoeducation and interventions focused on self-mentalization should be prioritized particularly in psychosis’ earliest expressions, that is, schizotypy, as interventions that target mentalization in psychosis suggest that early intervention results in better outcomes (111) and contemporary economics demonstrates that it is more beneficial to invest resources early in development in order to capture the full potential of interventions (112, 113).
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of the Universitat Autònoma de Barcelona (ref. 5426). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JN: Conceptualization, Data curation, Formal analysis, Writing – original draft. PT: Data curation, Formal analysis, Writing – review & editing. TK: Writing – review & editing, Methodology. SB: Writing – review & editing, Conceptualization, Supervision. NB-V: Conceptualization, Supervision, Writing – review & editing, Data curation, Funding acquisition, Project administration, Resources.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Spanish Ministry of Science and Innovation (grant number: PID2020-119211RB-I00) and the Generalitat de Catalunya (Suport als Grups de Recerca: 2021SGR01010) granted to NB-V. NB-V is supported by the ICREA Academia Award, Generalitat de Catalunya. JN is supported by the predoctoral program FI-AGAUR Ajuts de Joan Oró (2023 FI-3 00065) of the Secretary of Universities and Research, Department of Research, Universities of the Generalitat de Catalunya and the European Social Plus Fund.
Acknowledgments
The authors would like to thank Valeria Lavín and Karen Fagián Nuñez for their excellent assistance with data collection. They would also like to thank the enthusiastic participants for their generous contributions to advancing contemporary psychological research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Longden, E, Sampson, M, and Read, J. Childhood adversity and psychosis: generalised or specific effects? Epidemiol Psychiatr Sci. (2016) 25:349–59. doi: 10.1017/S204579601500044X
2. Schenkel, LS, Spaulding, WD, DiLillo, D, and Silverstein, SM. Histories of childhood maltreatment in schizophrenia: relationships with premorbid functioning, symptomatology, and cognitive deficits. Schizophr Res. (2005) 76:273–86. doi: 10.1016/j.schres.2005.03.003
3. Spauwen, J, Krabbendam, L, Lieb, R, Wittchen, H-U, and van Os, J. Impact of psychological trauma on the development of psychotic symptoms: relationship with psychosis proneness. Br J Psychiatry. (2006) 188:527–33. doi: 10.1192/bjp.bp.105.011346
4. Kraan, T, van Dam, DS, Velthorst, E, de Ruigh, EL, Nieman, DH, Durston, S, et al. Childhood trauma and clinical outcome in patients at ultra-high risk of transition to psychosis. Schizophr Res. (2015) 169:193–8. doi: 10.1016/j.schres.2015.10.030
5. Shevlin, M, Dorahy, MJ, and Adamson, G. Trauma and psychosis: an analysis of the National Comorbidity Survey. Am J Psychiatry. (2007) 164:166–9. doi: 10.1176/ajp.2007.164.1.166
6. Bateman, AW, and Fonagy, P. Mentalization-based treatment of BPD. J Personal Disord. (2004) 18:36–51. doi: 10.1521/pedi.18.1.36.32772
7. Fonagy, P. Reflective Self Function in Early Attachment and Borderline States. Washington D.C.: ERIC Clearinghouse (1993).
8. Ballespí, S, Vives, J, Debbané, M, Sharp, C, and Barrantes-Vidal, N. Beyond diagnosis: Mentalization and mental health from a transdiagnostic point of view in adolescents from non-clinical population. Psychiatry Res. (2018) 270:755–63. doi: 10.1016/j.psychres.2018.10.048
9. Fonagy, P, Gergely, G, and Target, M. The parent-infant dyad and the construction of the subjective self. J Child Psychol Psychiatry. (2007) 48:288–328. doi: 10.1111/j.1469-7610.2007.01727.x
10. Kim, S. The mind in the making: developmental and neurobiological origins of mentalizing. Personal Disord. (2015) 6:356–65. doi: 10.1037/per0000102
11. Chiesa, M, and Fonagy, P. Reflective function as a mediator between childhood adversity, personality disorder and symptom distress. Personal Ment Health. (2014) 8:52–66. doi: 10.1002/pmh.1245
12. Korver-Nieberg, N, Fett, A-KJ, Meijer, CJ, Koeter, MWJ, Shergill, SS, de Haan, L, et al. Theory of mind, insecure attachment and paranoia in adolescents with early psychosis and healthy controls. Aust N Z J Psychiatry. (2013) 47:737–45. doi: 10.1177/0004867413484370
13. Cicchetti, D. The impact of social experience on neurobiological systems: illustration from a constructivist view of child maltreatment. Cogn Dev. (2002) 17:1407–28. doi: 10.1016/S0885-2014(02)00121-1
14. Pears, KC, and Fisher, PA. Emotion understanding and theory of mind among maltreated children in foster care: evidence of deficits. Dev Psychopathol. (2005) 17:47–65. doi: 10.1017/s0954579405050030
15. Ensink, K, Normandin, L, Target, M, Fonagy, P, Sabourin, S, and Berthelot, N. Mentalization in children and mothers in the context of trauma: an initial study of the validity of the child reflective functioning scale. Br J Dev Psychol. (2015) 33:203–17. doi: 10.1111/bjdp.12074
16. Camras, LA, Grow, JG, and Ribordy, SC. Recognition of emotional expression by abused children. J Clin Child Adolesc Psychol. (1983) 12:325–8. doi: 10.1207/s15374424jccp1203_16
17. Shipman, KL, and Zeman, J. Emotional understanding: a comparison of physically maltreating and nonmaltreating mother-child dyads. J Clin Child Psychol. (1999) 28:407–17. doi: 10.1207/S15374424jccp280313
18. Pollak, SD, Cicchetti, D, Hornung, K, and Reed, A. Recognizing emotion in faces: developmental effects of child abuse and neglect. Dev Psychol. (2000) 36:679–88. doi: 10.1037/0012-1649.36.5.679
19. Shipman, K, Edwards, A, Brown, A, Swisher, L, and Jennings, E. Managing emotion in a maltreating context: a pilot study examining child neglect. Child Abuse Negl. (2005) 29:1015–29. doi: 10.1016/j.chiabu.2005.01.006
20. Brent, B. Mentalization-based psychodynamic psychotherapy for psychosis. J Clin Psychol. (2009) 65:803–14. doi: 10.1002/jclp.20615
21. Brent, BK, and Fonagy, P. A mentalization-based treatment approach to disturbances of social understanding in schizophrenia In: PH Lysaker, G Dimaggio, and M Brüne, editors. Social Cognition and Metacognition in Schizophrenia: Psychpathology and Treatment Approaches : Elsevier (2014). 245–59.
22. Debbané, M, Salaminios, G, Luyten, P, Badoud, D, Armando, M, Solida Tozzi, A, et al. Attachment, neurobiology, and Mentalizing along the psychosis continuum. Front Hum Neurosci. (2016) 10:406. doi: 10.3389/fnhum.2016.00406
23. Armando, M, Hutsebaut, J, and Debbané, M. A Mentalization-informed staging approach to clinical high risk for psychosis. Front Psych. (2019) 10:385. doi: 10.3389/fpsyt.2019.00385
24. Debbané, M, Benmiloud, J, Salaminios, G, Solida-Tozzi, A, Armando, M, Fonagy, P, et al. Mentalization-based treatment in clinical high-risk for psychosis: a rationale and clinical illustration. J Contemp Psychother. (2016) 46:217–25. doi: 10.1007/s10879-016-9337-4
25. Weijers, J, Ten Kate, C, Viechtbauer, W, Rampaart, LJA, Eurelings, EHM, and Selten, JP. Mentalization-based treatment for psychotic disorder: a rater-blinded, multi-center, randomized controlled trial. Psychol Med. (2021) 51:2846–55. doi: 10.1017/S0033291720001506
26. van Os, J, Kenis, G, and Rutten, BPF. The environment and schizophrenia. Nature. (2010) 468:203–12. doi: 10.1038/nature09563
27. Kwapil, TR, and Barrantes-Vidal, N. Schizotypy: looking back and moving forward. Schizophr Bull. (2015) 41:S366–73. doi: 10.1093/schbul/sbu186
28. Gross, GM, Kwapil, TR, Raulin, ML, Silvia, PJ, and Barrantes-Vidal, N. The multidimensional schizotypy scale-brief: scale development and psychometric properties. Psychiatry Res. (2018) 261:7–13. doi: 10.1016/j.psychres.2017.12.033
29. Kwapil, TR, Kemp, KC, Mielock, A, Sperry, SH, Chun, CA, Gross, GM, et al. Association of multidimensional schizotypy with psychotic-like experiences, affect, and social functioning in daily life: comparable findings across samples and schizotypy measures. J Abnorm Psychol. (2020) 129:492–504. doi: 10.1037/abn0000522
30. Hernández, LM, Kemp, KC, Barrantes-Vidal, N, and Kwapil, TR. Replication of the associations of positive, negative, and disorganized schizotypy with interview-assessed symptoms and impairment: convergence with previous studies. Personal Disord. (2023) 14:527–33. doi: 10.1037/per0000611
31. Kwapil, TR, Gross, GM, Silvia, PJ, and Barrantes-Vidal, N. Prediction of psychopathology and functional impairment by positive and negative schizotypy in the Chapmans’ ten-year longitudinal study. J Abnorm Psychol. (2013) 122:807–15. doi: 10.1037/a0033759
32. Barrantes-Vidal, N, Chun, CA, Myin-Germeys, I, and Kwapil, TR. Psychometric schizotypy predicts psychotic-like, paranoid, and negative symptoms in daily life. J Abnorm Psychol. (2013) 122:1077–87. doi: 10.1037/a0034793
33. Barrantes-Vidal, N, Grant, P, and Kwapil, TR. The role of schizotypy in the study of the etiology of schizophrenia spectrum disorders. Schizophr Bull. (2015) 41:S408–16. doi: 10.1093/schbul/sbu191
34. Debbané, M, and Barrantes-Vidal, N. Schizotypy from a developmental perspective. Schizophr Bull. (2015) 41 Suppl 2:S386–95. doi: 10.1093/schbul/sbu175
35. Grant, P, Green, MJ, and Mason, OJ. Models of schizotypy: the importance of conceptual clarity. Schizophr Bull. (2018) 44:S556–63. doi: 10.1093/schbul/sby012
36. Torok, E, and Keri, S. The relationship between mentalization and the symptoms of subclinical schizophrenia and affective spectrum disorders. PsyArxiv. (2020) 1–15.
37. Kim, HS, Shin, NY, Jang, JH, Kim, E, Shim, G, Park, HY, et al. Social cognition and neurocognition as predictors of conversion to psychosis in individuals at ultra-high risk. Schizophr Res. (2011) 130:170–5. doi: 10.1016/j.schres.2011.04.023
38. Boldrini, T, Pontillo, M, Tanzilli, A, Giovanardi, G, Di Cicilia, G, Salcuni, S, et al. An attachment perspective on the risk for psychosis: clinical correlates and the predictive value of attachment patterns and mentalization. Schizophr Res. (2020) 222:209–17. doi: 10.1016/j.schres.2020.05.052
39. Bora, E, and Pantelis, C. Theory of mind impairments in first-episode psychosis, individuals at ultra-high risk for psychosis and in first-degree relatives of schizophrenia: systematic review and meta-analysis. Schizophr Res. (2013) 144:31–6. doi: 10.1016/j.schres.2012.12.013
40. Piskulic, D, Liu, L, Cadenhead, KS, Cannon, TD, Cornblatt, BA, McGlashan, TH, et al. Social cognition over time in individuals at clinical high risk for psychosis: findings from the NAPLS-2 cohort. Schizophr Res. (2016) 171:176–81. doi: 10.1016/j.schres.2016.01.017
41. Thompson, AD, Bartholomeusz, C, and Yung, AR. Social cognition deficits and the ‘ultra high risk’ for psychosis population: a review of literature. Early Interv Psychiatry. (2011) 5:192–202. doi: 10.1111/j.1751-7893.2011.00275.x
42. Langdon, R, and Coltheart, M. Mentalising, schizotypy, and schizophrenia. Cognition. (1999) 71:43–71. doi: 10.1016/S0010-0277(99)00018-9
43. Clemmensen, L, van Os, J, Skovgaard, AM, Væver, M, Blijd-Hoogewys, EMA, Bartels-Velthuis, AA, et al. Hyper-theory-of-mind in children with psychotic experiences. PLoS One. (2014) 9:e113082. doi: 10.1371/journal.pone.0113082
44. Greig, TC, Bryson, GJ, and Bell, MD. Theory of mind performance in schizophrenia: diagnostic, symptom, and neuropsychological correlates. J Nerv Ment Dis. (2004) 192:12–8. doi: 10.1097/01.nmd.0000105995.67947.fc
45. Doody, GA, Götz, M, Johnstone, EC, Frith, CD, and Owens, DG. Theory of mind and psychoses. Psychol Med. (1998) 28:397–405. doi: 10.1017/S003329179700648X
46. Turner, R, Louie, K, Parvez, A, Modaffar, M, Rezaie, R, Greene, T, et al. The effects of developmental trauma on theory of mind and its relationship to psychotic experiences: a behavioural study. Psychiatry Res. (2022) 312:114544. doi: 10.1016/j.psychres.2022.114544
47. Mansueto, G, Schruers, K, Cosci, F, and van Os, J. GROUP investigators. Childhood adversities and psychotic symptoms: the potential mediating or moderating role of neurocognition and social cognition. Schizophr Res. (2019) 206:183–93. doi: 10.1016/j.schres.2018.11.028
48. Weijers, J, Fonagy, P, Eurelings-Bontekoe, E, Termorshuizen, F, Viechtbauer, W, and Selten, JP. Mentalizing impairment as a mediator between reported childhood abuse and outcome in nonaffective psychotic disorder. Psychiatry Res. (2018) 259:463–9. doi: 10.1016/j.psychres.2017.11.010
49. Sprong, M, Schothorst, P, Vos, E, Hox, J, and van Engeland, H. Theory of mind in schizophrenia: meta-analysis. Br J Psychiatry. (2007) 191:5–13. doi: 10.1192/bjp.bp.107.035899
50. Sergi, MJ, Rassovsky, Y, Widmark, C, Reist, C, Erhart, S, Braff, DL, et al. Social cognition in schizophrenia: relationships with neurocognition and negative symptoms. Schizophr Res. (2007) 90:316–24. doi: 10.1016/j.schres.2006.09.028
51. Couture, SM, Penn, DL, and Roberts, DL. The functional significance of social cognition in schizophrenia: a review. Schizophr Bull. (2006) 32 Suppl 1:S44–63. doi: 10.1093/schbul/sbl029
52. Fett, A-KJ, Viechtbauer, W, Dominguez, M-G, Penn, DL, van Os, J, and Krabbendam, L. The relationship between neurocognition and social cognition with functional outcomes in schizophrenia: a meta-analysis. Neurosci Biobehav Rev. (2011) 35:573–88. doi: 10.1016/j.neubiorev.2010.07.001
53. Spark, J, Gawęda, Ł, Allott, K, Hartmann, JA, Jack, BN, Koren, D, et al. Distinguishing schizophrenia spectrum from non-spectrum disorders among young patients with first episode psychosis and at high clinical risk: the role of basic self-disturbance and neurocognition. Schizophr Res. (2021) 228:19–28. doi: 10.1016/j.schres.2020.11.061
54. Benson, TL, and Park, S. Increased plasticity of bodily self-experience in individuals who may carry latent liability for schizophrenia. Schizophr Res. (2019) 207:58–62. doi: 10.1016/j.schres.2018.05.004
55. Kocsis-Bogár, K, Kotulla, S, Maier, S, Voracek, M, and Hennig-Fast, K. Cognitive correlates of different Mentalizing abilities in individuals with high and Low trait Schizotypy: findings from an extreme-group design. Front Psychol. (2017) 8:922. doi: 10.3389/fpsyg.2017.00922
56. Pickup, GJ. Theory of mind and its relation to schizotypy. Cogn Neuropsychiatry. (2006) 11:177–92. doi: 10.1080/13546800444000236
57. Garety, PA, and Freeman, D. Cognitive approaches to delusions: a critical review of theories and evidence. Br J Clin Psychol. (1999) 38:113–54. doi: 10.1348/014466599162700
58. Salaminios, G, Morosan, L, Toffel, E, Tanzer, M, Eliez, S, Badoud, D, et al. Associations between schizotypal personality features, mentalizing difficulties and thought problems in a sample of community adolescents. Early Interv Psychiatry. (2021) 15:705–15. doi: 10.1111/eip.13011
59. Luyten, P, Campbell, C, Allison, E, and Fonagy, P. The mentalizing approach to psychopathology: state of the art and future directions. Annu Rev Clin Psychol. (2020) 16:297–325. doi: 10.1146/annurev-clinpsy-071919-015355
60. Ballespí, S, Vives, J, Nonweiler, J, Perez-Domingo, A, and Barrantes-Vidal, N. Self- but not other-dimensions of Mentalizing moderate the impairment associated with social anxiety in adolescents from the general population. Front Psychol. (2021) 12:721584. doi: 10.3389/fpsyg.2021.721584
61. Ballespí, S, Vives, J, Sharp, C, Chanes, L, and Barrantes-Vidal, N. Self and other Mentalizing polarities and dimensions of mental health: association with types of symptoms, functioning and well-being. Front Psychol. (2021) 12:566254. doi: 10.3389/fpsyg.2021.566254
62. Ballespí, S, Nonweiler, J, Sharp, C, Vives, J, and Barrantes-Vidal, N. Self-but not other-mentalizing moderates the association between BPD symptoms and somatic complaints in community-dwelling adolescents. Psychol Psychother Theory Res Pract. (2022) 95:905–20. doi: 10.1111/papt.12409
63. Cicero, DC, Martin, EA, Becker, TM, and Kerns, JG. Decreased self-concept clarity in people with schizophrenia. J Nerv Ment Dis. (2016) 204:142–7. doi: 10.1097/NMD.0000000000000442
64. Hemsley, DR. The disruption of the ‘sense of self’in schizophrenia: potential links with disturbances of information processing. Br J Med Psychol. (1998) 71:115–24. doi: 10.1111/j.2044-8341.1998.tb01373.x
65. Nelson, B, Sass, LA, and Parnas, J. Basic self disturbance in the schizophrenia spectrum: a review and future directions In: M Kyrios, R Moulding, G Doron, SS Bhar, M Nedeljkovic, and M Mikulincer, editors. The Self in Understanding and Treating Psychological Disorders. Cambridge: Cambridge University Press (2016). 158.
66. Nelson, B, Fornito, A, Harrison, BJ, Yücel, M, Sass, LA, Yung, AR, et al. A disturbed sense of self in the psychosis prodrome: linking phenomenology and neurobiology. Neurosci Biobehav Rev. (2009) 33:807–17. doi: 10.1016/j.neubiorev.2009.01.002
67. Nelson, B, Sass, LA, Thompson, A, Yung, AR, Francey, SM, Amminger, GP, et al. Does disturbance of self underlie social cognition deficits in schizophrenia and other psychotic disorders? Early Interv Psychiatry. (2009) 3:83–93. doi: 10.1111/j.1751-7893.2009.00112.x
68. Nelson, B, and Raballo, A. Basic self-disturbance in the schizophrenia spectrum: taking stock and moving forward. Psychopathology. (2015) 48:301–9. doi: 10.1159/000437211
69. Salaminios, G, and Debbané, M. A mentalization-based treatment framework to support the recovery of the self in emerging psychosis during adolescence In: The Recovery of the Self in Psychosis. Eds. Ilanit, Hasson-Ohayon, and Paul, H. Lysaker. London & New York: Routledge (2021). 12–35.
70. Li, LY, Karcher, NR, Kerns, JG, Fung, CK, and Martin, EA. The subjective-objective deficit paradox in schizotypy extends to emotion regulation and awareness. J Psychiatr Res. (2019) 111:160–8. doi: 10.1016/j.jpsychires.2019.01.026
71. Okruszek, Ł, Chrustowicz, M, Jarkiewicz, M, Krawczyk, M, Manera, V, Piejka, A, et al. Mentalizing abilities mediate the impact of the basic social perception on negative symptoms in patients with schizophrenia. J Psychiatr Res. (2022) 155:85–90. doi: 10.1016/j.jpsychires.2022.07.069
72. Pazar, Ö, Steele, H, and Todman, M. Expressed emotion and reflective functioning across the schizotypy spectrum: developmental experiential factors. Psychoanal Psychol. (2022) 39:266–75. doi: 10.1037/pap0000401
73. van Nierop, M, Lataster, T, Smeets, F, Gunther, N, van Zelst, C, de Graaf, R, et al. Psychopathological mechanisms linking childhood traumatic experiences to risk of psychotic symptoms: analysis of a large, representative population-based sample. Schizophr Bull. (2014) 40:S123–30. doi: 10.1093/schbul/sbt150
74. Arseneault, L, Cannon, M, Fisher, HL, Polanczyk, G, Moffitt, TE, and Caspi, A. Childhood trauma and children’s emerging psychotic symptoms: a genetically sensitive longitudinal cohort study. Am J Psychiatry. (2011) 168:65–72. doi: 10.1176/appi.ajp.2010.10040567
75. Cristóbal-Narváez, P, Sheinbaum, T, Ballespí, S, Mitjavila, M, Myin-Germeys, I, Kwapil, TR, et al. Impact of adverse childhood experiences on psychotic-like symptoms and stress reactivity in daily life in nonclinical young adults. PLoS One. (2016) 11:e0153557. doi: 10.1371/journal.pone.0153557
76. Chapman, JP, Chapman, LJ, and Kwapil, TR. Scales for the measurement of schizotypy In: A Raine, T Lencz, and S Mednick, editors. Schizotypal Personality Disorder. Cambridge: Cambridge University Press (1995). 79–106.
77. Bernstein, DP, Stein, JA, Newcomb, MD, Walker, E, Pogge, D, Ahluvalia, T, et al. Development and validation of a brief screening version of the childhood trauma questionnaire. Child Abuse Negl. (2003) 27:169–90. doi: 10.1016/S0145-2134(02)00541-0
78. Li, M, Cassis, T, D’Arcy, C, Low, N, and Meng, X. Development and validation of a brief form of the childhood adversities questionnaire among a population of mood disorders. J Interpers Violence. (2022) 37:NP2288–312. doi: 10.1177/0886260520933038
79. Bifulco, A, Bernazzani, O, Moran, PM, and Jacobs, C. The childhood experience of care and abuse questionnaire (CECA.Q): validation in a community series. Br J Clin Psychol. (2005) 44:563–81. doi: 10.1348/014466505X35344
80. Smith, N, Lam, D, Bifulco, A, and Checkley, S. Childhood experience of care and abuse questionnaire (CECA.Q). Validation of a screening instrument for childhood adversity in clinical populations. Soc Psychiatry Psychiatr Epidemiol. (2002) 37:572–9. doi: 10.1007/s00127-002-0589-9
81. Dimitrijević, A, Hanak, N, Altaras Dimitrijević, A, and Jolić, MZ. The Mentalization scale (MentS): a self-report measure for the assessment of Mentalizing capacity. J Pers Assess. (2018) 100:268–80. doi: 10.1080/00223891.2017.1310730
82. Salovey, P, Mayer, JD, Goldman, SL, Turvey, C, and Palfai, TP. Emotional attention, clarity, and repair: exploring emotional intelligence using the trait Meta-mood scale In: JW Pennebaker, editor. Emotion, Disclosure, & Health. Washington: American Psychological Association (1995). 125–54.
83. Kemp, KC, Gross, GM, and Kwapil, TR. Psychometric properties of the multidimensional Schizotypy scale and multidimensional Schizotypy scale-brief: item and scale test-retest reliability and concordance of original and brief forms. J Pers Assess. (2020) 102:508–15. doi: 10.1080/00223891.2019.1591425
84. Stefanis, NC, Smyrnis, N, Avramopoulos, D, Evdokimidis, I, Ntzoufras, I, and Stefanis, CN. Factorial composition of self-rated schizotypal traits among young males undergoing military training. Schizophr Bull. (2004) 30:335–50. doi: 10.1093/oxfordjournals.schbul.a007083
85. Raine, A. The SPQ: a scale for the assessment of schizotypal personality based on DSM-III-R criteria. Schizophr Bull. (1991) 17:555–64. doi: 10.1093/schbul/17.4.555
86. Sheinbaum, T, Kwapil, TR, and Barrantes-Vidal, N. Fearful attachment mediates the association of childhood trauma with schizotypy and psychotic-like experiences. Psychiatry Res. (2014) 220:691–3. doi: 10.1016/j.psychres.2014.07.030
87. Hayes, AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach, vol. 1 Guilford Press (2013). 20 p.
88. Mertens, YL, Racioppi, A, Sheinbaum, T, Kwapil, T, and Barrantes-Vidal, N. Dissociation and insecure attachment as mediators of the relation between childhood emotional abuse and nonclinical paranoid traits. Eur J Psychotraumatol. (2021) 12:1888539. doi: 10.1080/20008198.2021.1888539
89. Pearce, J, Simpson, J, Berry, K, Bucci, S, Moskowitz, A, and Varese, F. Attachment and dissociation as mediators of the link between childhood trauma and psychotic experiences. Clin Psychol Psychother. (2017) 24:1304–12. doi: 10.1002/cpp.2100
90. Nonweiler, J, Vives, J, Barrantes-Vidal, N, and Ballespí, S. Value in ‘knowing thyself’: emotional self-knowledge profiles and relationships with mental health indicators. Sci Rep (Under Review).
91. Ballespí, S, Vives, J, Alonso, N, Sharp, C, Ramírez, MS, Fonagy, P, et al. To know or not to know? Mentalization as protection from somatic complaints. PLoS One. (2019) 14:e0215308. doi: 10.1371/journal.pone.0215308
92. Peyroux, E, Prost, Z, Danset-Alexandre, C, Brenugat-Herne, L, Carteau-Martin, I, Gaudelus, B, et al. From “under” to “over” social cognition in schizophrenia: is there distinct profiles of impairments according to negative and positive symptoms? Schizophr Res Cogn. (2019) 15:21–9. doi: 10.1016/j.scog.2018.10.001
93. Kemp, KC, Sperry, SH, Hernández, L, Barrantes-Vidal, N, and Kwapil, TR. Affective dynamics in daily life are differentially expressed in positive, negative, and disorganized schizotypy. J Psychopathol Clin Sci. (2023) 132:110–21. doi: 10.1037/abn0000799
94. Kwapil, TR, Brown, LH, Silvia, PJ, Myin-Germeys, I, and Barrantes-Vidal, N. The expression of positive and negative schizotypy in daily life: an experience sampling study. Psychol Med. (2012) 42:2555–66. doi: 10.1017/S0033291712000827
95. Baron, RM, and Kenny, DA. The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. (1986) 51:1173–82. doi: 10.1037/0022-3514.51.6.1173
96. Hayes, AF. Introduction to Mediation, Moderation, and Conditional Process Analysis, Second Edition: A Regression-Based Approach (Methodology in the Social Sciences). 2nd ed. New York: The Guilford Press (2017).
97. Cerel, J, Fristad, MA, Verducci, J, Weller, RA, and Weller, EB. Childhood bereavement: psychopathology in the 2 years postparental death. J Am Acad Child Adolesc Psychiatry. (2006) 45:681–90. doi: 10.1097/01.chi.0000215327.58799.05
98. Tremblay, GC, and Israel, AC. Children’s adjustment to parental death. Clin Psychol Sci Pract. (1998) 5:424–38. doi: 10.1111/j.1468-2850.1998.tb00165.x
99. Ryan, R, O’Farrelly, C, and Ramchandani, P. Parenting and child mental health. London J Prim Care (Abingdon). (2017) 9:86–94. doi: 10.1080/17571472.2017.1361630
100. Winnicott, DW. Mind and Its Relation to the Psyche-Soma. Through Paediatrics to Psycho-Analysis. Collected Papers: Through Paediatrics to Psychoanalysis; (1949)
101. Bowlby, J. The making and breaking of affectional bonds. II. Some principles of psychotherapy. The fiftieth Maudsley lecture. Br J Psychiatry. (1977) 130:421–31. doi: 10.1192/bjp.130.5.421
102. Ludwig, L, Werner, D, and Lincoln, TM. The relevance of cognitive emotion regulation to psychotic symptoms - a systematic review and meta-analysis. Clin Psychol Rev. (2019) 72:101746. doi: 10.1016/j.cpr.2019.101746
103. Nelson, B, Thompson, A, and Yung, AR. Basic self-disturbance predicts psychosis onset in the ultra high risk for psychosis “prodromal” population. Schizophr Bull. (2012) 38:1277–87. doi: 10.1093/schbul/sbs007
104. Henriksen, MG, Raballo, A, and Nordgaard, J. Self-disorders and psychopathology: a systematic review. Lancet Psychiatry. (2021) 8:1001–12. doi: 10.1016/S2215-0366(21)00097-3
105. Rossi, M, Bruno, G, Chiusalupi, M, and Ciaramella, A. Relationship between pain, somatisation, and emotional awareness in primary school children. Pain Res Treat. (2018) 2018:1–12. doi: 10.1155/2018/4316234
106. Lee, H-S, Hong, S-JJ, Baxter, T, Scott, J, Shenoy, S, Buck, L, et al. Altered peripersonal space and the bodily self in schizophrenia: a virtual reality study. Schizophr Bull. (2021) 47:927–37. doi: 10.1093/schbul/sbab024
107. Gawęda, Ł, Prochwicz, K, Adamczyk, P, Frydecka, D, Misiak, B, Kotowicz, K, et al. The role of self-disturbances and cognitive biases in the relationship between traumatic life events and psychosis proneness in a non-clinical sample. Schizophr Res. (2018) 193:218–24. doi: 10.1016/j.schres.2017.07.023
108. Phalen, PL, Dimaggio, G, Popolo, R, and Lysaker, PH. Aspects of theory of mind that attenuate the relationship between persecutory delusions and social functioning in schizophrenia spectrum disorders. J Behav Ther Exp Psychiatry. (2017) 56:65–70. doi: 10.1016/j.jbtep.2016.07.008
109. Bradford, EEF, Jentzsch, I, and Gomez, J-C. From self to social cognition: theory of mind mechanisms and their relation to executive functioning. Cognition. (2015) 138:21–34. doi: 10.1016/j.cognition.2015.02.001
110. McGorry, PD, Nelson, B, Goldstone, S, and Yung, AR. Clinical staging: a heuristic and practical strategy for new research and better health and social outcomes for psychotic and related mood disorders. Can J Psychiatr. (2010) 55:486–97. doi: 10.1177/070674371005500803
111. Weijers, J, Ten Kate, C, Eurelings-Bontekoe, E, Viechtbauer, W, Rampaart, R, Bateman, A, et al. Mentalization-based treatment for psychotic disorder: protocol of a randomized controlled trial. BMC Psychiatry. (2016) 16:191. doi: 10.1186/s12888-016-0902-x
112. Heckman, JJ. Invest in early childhood development: reduce deficits, strengthen the economy. Heckman Equ. (2012) 7:1–2.
113. Heckman, JJ. The Heckman Equation; (2021). Available at: https://heckmanequation.org/ (Accessed 26 June 26, 2023).
Keywords: mentalization, self-other, schizotypy, parental loss, childhood adversity, paranoia, psychotic-like experiences
Citation: Nonweiler J, Torrecilla P, Kwapil TR, Ballespí S and Barrantes-Vidal N (2023) I don’t understand how I feel: mediating role of impaired self-mentalizing in the relationship between childhood adversity and psychosis spectrum experiences. Front. Psychiatry. 14:1268247. doi: 10.3389/fpsyt.2023.1268247
Edited by:
Javier Ortuño Sierra, University of La Rioja, SpainReviewed by:
Juan Francisco Rodríguez-Testal, Sevilla University, SpainRebeca Aritio, University of La Rioja, Spain
Copyright © 2023 Nonweiler, Torrecilla, Kwapil, Ballespí and Barrantes-Vidal. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Neus Barrantes-Vidal, TmV1cy5CYXJyYW50ZXNAdWFiLmNhdA==
 Jacqueline Nonweiler
Jacqueline Nonweiler Pilar Torrecilla
Pilar Torrecilla Thomas R. Kwapil
Thomas R. Kwapil Sergi Ballespí
Sergi Ballespí Neus Barrantes-Vidal
Neus Barrantes-Vidal