
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 14 September 2023
Sec. Perinatal Psychiatry
Volume 14 - 2023 | https://doi.org/10.3389/fpsyt.2023.1252789
Objective: This study aims to investigate the occurrence of maternal postpartum depression (PPD) during menstruation and analyze the influencing factors and risk prediction modeling of maternal PPD in Chinese puerperal women of sitting the month.
Methods: A total of 286 mothers were selected using convenience sampling, who came for a routine postpartum follow-up visit were surveyed, including face-to-face, telephone, and online. They completed questionnaires including the basic profile questionnaire, Postpartum Partner Support Scale (PPSS), Edinburgh PPD Scale (EPDS), Parenting Self-Efficacy Scale (SICS), and Simple Coping Style Questionnaire (SCSQ), who were advised to complete the survey alone, in private, reducing the impact of husband’s presence on the quality of the questionnaire. Variables showing statistical significance in the one-way analysis were further analyzed using logistic regression analysis. The predictive value of the logistic regression model was analyzed using the Receiver Operating Characteristic Curve (ROC), and the predictive reliability was expressed as the area under the ROC [Area Under the Curve (AUC)].
Results: The total score of PPD was 7.78 ± 4.57, and 22 people (7.69%) experienced depression during the postpartum period. PPD was found to be correlated with postpartum partner support, positive coping, negative coping, and parenting self-efficacy, with correlation coefficient values of −0.63, 0.62, 0.56, and − 0.70, respectively (all p < 0.05). Logistic regression analysis revealed that postpartum partner support and parenting self-efficacy were independent factors influencing PPD, with odds ratios (95% confidence intervals) of 0.76 (0.61 ~ 0.94) and 0.83 (0.75 ~ 0.93), respectively both p < 0.05.The area under the curve, sensitivity, and specificity for postpartum partner support and parenting self-efficacy were 1.00 (95% confidence intervals 0.99 ~ 1.00), 99.24, and 90.91%.
Conclusion: Postpartum partner support and parenting self-efficacy independently predict the occurrence of PPD. Healthcare professionals and maternal families should prioritize timely attention to maternal partner support and parenting issues to reduce the occurrence of PPD.
Postpartum depression (PPD) is a debilitating condition characterized by a spectrum of symptoms, including maternal anxiety, depression, insomnia, irritability, sadness, loneliness, cognitive deficits, diminished self-esteem, inadequate coping skills, loss of interest in activities, sleep disturbances, and even severe cases of suicidal thoughts, impacting mothers (1, 2). The prevalence of PPD varies significantly across countries and regions. This paper presented a systematic review and meta-analysis of 58 studies encompassing 37,294 women, aiming to provide a comprehensive overview of PPD incidence. Findings indicated an overall incidence of 17% (3) among healthy mothers with no history of prior depression. Notably, the Middle East exhibited the highest prevalence (26%), while Europe reported the lowest (8%). Another systematic review and meta-analysis revealed a comparable prevalence of 14% (4). Developing countries displayed a markedly elevated rate of PPD, with China’s prevalence notably exceeding the global average at 21.4%.
Postpartum depression presents a substantial risk to maternal well-being, infant health, and overall family dynamics (5). Despite being a commonly occurring condition, PPD frequently remains undetected and unaddressed (6), resulting in various detrimental consequences. Undiagnosed, untreated or insufficiently treated depression can yield deleterious long-term outcomes. In the case of mothers, PPD is linked to suboptimal physical and psychological well-being, culminating in diminished quality of life and potential psychiatric institutionalization. Moreover, PPD can detrimentally influence a child’s cognitive, social, and socioemotional progress, resulting in reduced intelligence quotient, behavioral challenges, and perturbing family dynamics (7–10).
The etiology of PPD remains elusive, nevertheless, it is risk and mitigation factors encompass psychological, biological, social, and cultural dimensions. A recent systematic review and meta-analysis highlighted a prominent concentration of risk factors within the realm of insufficient social support (11), encompassing spousal, peer, and healthcare professional support. In the realm of Chinese culture, the postpartum phase frequently encompasses a customary practice referred to as “sitting the month,” which prioritizes the provision of exclusive care for newborns and rest for mothers during the initial month following childbirth. This confinement period may limit timely support from relatives and friends, thereby increasing reliance on spousal support. The conducted research has unveiled noteworthy correlations between the presence of strained relationships with spouses or family members and the incidence of PPD among Chinese women (12, 13). Previous research had indicated a substantial inverse association between partner support during this period and PPD (14, 15). In the aftermath of childbirth, women assume the responsibility of infant care, wherein perceived parenting satisfaction and self-efficacy play vital roles. The association between parenting self-efficacy and PPD was supported by a comprehensive meta-analysis of 114 cohort studies. This analysis indicates that the stress resulting from the changing roles and responsibilities of parenthood can be considered a significant risk factor for PPD (16). A longitudinal study conducted over a span of 4 years in the United Kingdom unveiled a noteworthy association between reduced parental self-efficacy and depression within a demanding parenting context (17). Additionally, the categorization of coping styles into positive and negative facets underscores the predictive potential of negative coping strategies for PPD (18).
Nevertheless, the relationship between maternal PPD and partner support during the traditional practice of “sitting the month” has yet to be determined. The unique cultural context of this period may impact women’s social support systems, with husbands playing a pivotal role. Given the observed negative correlation between partner support and PPD, the lack of a quantitative measurement tool for postnatal partner support in China necessitated the validation of the quantifiable postnatal partner support scale. Most studies (2–4) solely focused on describing the epidemic characteristics, without application of Simple Coping Style Questionnaire or providing prediction model for postpartum partner support and parenting self-efficacy.
In response to this gap in scholarship, we aim to employ this validated scale, along with the Postpartum Partner Support Scale, Self-efficacy in Infant Care Scale, and Simple Coping Style Questionnaire, identify the influencing factors of PPD and establish a targeted early warning model to create effective tools for helping spotting PPD. We also aim to assist healthcare professionals in early identification and targeted prevention of PPD, thus addressing a critical gap in the literature.
In this study, we employ a simple convenience sampling approach to investigate the prevalence of PPD. Utilizing qualitative data, specifically an overall rate estimation, we apply the formula to determine the required sample size (19).
Here, signifies the sample size, denotes the Z-statistic corresponding to a confidence level (at 95% confidence, = 1.96), δ represents the allowable absolute error, typically set at 0.05 for acceptable precision, and p signifies the overall rate. With existing literature reporting a 17% prevalence of PPD via meta-analysis, corroborated by a substantial body of research (3), our study utilizes = 0.17 to calculate a minimum sample size of = 216. To account for potential nonresponse and variations in maternal conditions, a total of 300 questionnaires were distributed in this study, with 286 valid questionnaires returned, yielding an effective rate of 95.33%.
Our study received ethical clearance from the Ethics Committee of Quanzhou Medical College, Quanzhou, Fujian, China (Ethics Code: No. 2021007). The central tenet of voluntary participation was upheld throughout the study. Prior to survey administration, all participants were thoroughly briefed on the study’s objectives, methodologies, potential benefits, and risks. Informed consent was meticulously obtained from every participant, establishing a foundation of trust and transparency.
In accordance with ethical guidelines, a range of strategies were deployed for survey completion. Face-to-face participants were afforded privacy during survey completion, ensuring responses were provided independently and without influence. Similarly, participants completing surveys via telephone or online platforms were instructed to do so in a private setting. The preservation of participant anonymity was ensured through sealed envelopes, preventing any inadvertent bias during data collection. Our rigorous approach aimed to mitigate potential stressors and maintain the integrity of collected data.
A convenience sampling method was employed to select women who had given birth between December 2021 and September 2022 at a hospital of Quanzhou Women and Children’s Hospital in Quanzhou City as the study population. The inclusion criteria were as follows: (1) women in the postpartum period (within 28 days after delivery) and (2) those with clear consciousness and informed consent to participate. Exclusion criteria included: (1) unwillingness or non-cooperation with the survey; (2) visual or hearing impairment that hindered understanding and response to the questionnaire; and (3) those who reported a history of depression or psychiatric disorders before or during pregnancy.
Study participants were recruited at the hospital where they delivered. After delivery, mothers provided their community address, detailed home address, personal phone numbers, and their husband’s contact information to facilitate postpartum health education and follow-up visits.
Medical professionals, including doctors, midwives, nurses, and researchers from the study group, were responsible for recruiting study subjects. Before conducting the survey, the researcher in charge of recruiting subjects received comprehensive training, including an understanding of the questionnaire items and survey guidelines. Precautions, such as maintaining subject confidentiality and ensuring that participants completed the questionnaire independently, were emphasized.
Conducting research during the novel coronavirus pandemic presented challenges in reaching potential participants. Lockdowns, movement restrictions, and concerns about hospital visits impacted the availability of eligible mothers. We coordinated closely with the hospital administration and medical staff to ensure that the recruitment process followed safety protocols. In cases where physical presence was challenging, we incorporated telephonic and online methods for data collection. By providing flexible options, we aimed to accommodate participants’ preferences and alleviate concerns related to the pandemic.
The cultural norm of “sitting the month” during postpartum limited women’s mobility and access to support networks, potentially affecting their willingness to participate in the study. We provided comprehensive explanations to potential participants about the nature of the research, assuring them of confidentiality and the importance of their contribution to maternal health research.
The postpartum period is characterized by significant time demands, making it challenging for new mothers to allocate time for research participation. We designed the survey instruments to be concise and user-friendly, minimizing the time required for completion. Moreover, we offered multiple modes of participation (face-to-face, telephone, and online), allowing participants to choose the most convenient option that aligned with their schedules.
This questionnaire collected maternal and husband’s age, education, gestational age of the newborn at birth, sex of the newborn, type of delivery, the number of pregnancies, the number of deliveries, the gestational weeks, maternal education level, family income, the sex of the babies, feeding method, and mother-in-law/daughter-in-law relationship.
The PPSS comprises 20 items, scored on a scale of 1–4, representing strongly disagree to strongly agree. The total score ranges from 20 to 80, with a higher score indicating a higher level of postpartum partner support. The English version demonstrated a Cronbach’s alpha coefficient of 0.96, a goodness-of-fit index CFI of 0.99, and a root mean square error of approximation SRMR of 0.05, indicating good model fit (14). To ensure the reliability of the scale, a Chinese version was developed and tested by our research group. The Chinese version exhibited a Cronbach’s alpha coefficient of 0.968 and a retest reliability coefficient of 0.905 (p < 0.01). In the validation factor analysis, the χ2/df was 1.476, and the RMSEA was 0.047.
The EPDS consists of 10 items, with each item scored from 0 to 3. The total score ranges from 0 to 30, with higher scores indicating greater severity of maternal depression. A total score of ≥13 is considered indicative of PPD, with a significant increase in specificity of 0.95 (20). EPDS was commonly used to assess the degree of PPD, and many studies reported good validity and reliability of the Edinburgh tool in different contexts, from 0.76 to 0.861 (21, 22), and The Cronbach’s alpha of EPDS in this study was 0.853.
The SICS consists of 44 items, each item indicates one parenting task; the higher the score, the higher the self-efficacy. For instance, women were asked to rate their degree of confidence in performing designated tasks/situations; a score ranging from 0 to 100 was assigned, depending on their confidence response from “not confident at all to do it” to “definitely confident I can do it.” The scale is scored by summing the numerical ratings for each task and dividing the result by the number of tasks. The reported internal consistency was 0.94 for the total scale (23). The Cronbach’s alpha of SICS in this study was 0.950.
The SCSQ was used to measure the coping style of Chinese puerperal mothers,comprised to two dimensions, positive coping and negative coping, with a total of 20 items. Each item is scored from 0 to 3. A high score of the positive coping indicates that the individuals are more inclined to adopt positive coping styles with efforts to solve a stressful situation/problem, and a high score of the negative coping refers that the individuals are more inclined to adopt negative coping styles with distancing or avoiding a stressful situation. The Cronbach’s alpha coefficient of the positive coping and negative coping was 0.863 and 0.741 (24). The Cronbach’s alpha of SCSQ in this study was 0.897 and 0.862.
Medical professionals, including doctors, midwives, nurses, and researchers from the study group, were responsible for recruiting study subjects. Before conducting the survey, the researcher in charge of recruiting subjects received comprehensive training, including an understanding of the questionnaire items and survey guidelines. Precautions, such as maintaining subject confidentiality and ensuring that participants completed the questionnaire independently, were emphasized.
Study participants were recruited at the hospital where they delivered. After delivery, mothers provided their community address, detailed home address, personal phone numbers, and their husband’s contact information to facilitate postpartum health education and follow-up visits. Data collection was carried out through face-to-face interviews (using pen and printed paper questionnaires), telephone interviews, and online questionnaires. In face-to-face interviews, the survey was conducted in a private room with only the mother and newborn present. For telephone or online surveys, mothers were informed that the questionnaire would evaluate their husband’s support and were requested to ensure their husband temporarily left during the survey to allow the wife to complete the questionnaire independently.
Data collected were entered using Epidata 3.0, and descriptive statistical analysis, Pearson’s correlation analysis, and logistic regression analysis were performed using SPSS 22.0. General demographic data were analyzed using percentages and frequencies. Postpartum husband support, parenting self-efficacy, coping style, and PPD were described using mean ± standard deviation and median (interquartile spacing). Pearson’s correlation analysis was employed to examine the correlation between PPD and postpartum husband support, as well as parenting self-efficacy and coping style. We used the Shapiro–Wilk method to group the data (depressed and non-depressed groups) to check if the data conformed to a normal distribution. If the variable was normally distributed, an independent t-test was used to compare PPD according to two groups. If the variable was not normally distributed, the Mann-Whitney U test was used to compare PPD according to two groups. Variables showing statistical significance in the one-way analysis were further analyzed using logistic regression analysis. The predictive value of the logistic regression model was analyzed using the Receiver Operating Characteristic Curve (ROC), and the predictive reliability was expressed as the area under the ROC [Area Under the Curve (AUC)]. Hypothesis testing employed a two-sided test with a significance level of 0.05. A value of p less than 0.05 indicated statistically significant differences.
The mean age of the mothers was 29.83 ± 3.65 years, ranging from 17 to 39 years. The mean age of the husbands was 30.43 ± 3.75 years, ranging from 22 to 42 years. Among the participants, 78 (27.3%) had completed high school or junior college, 112 (39.2%) had a bachelor’s degree or above, and 2 (0.7%) had an elementary school education or below. In terms of maternal personality type, 146 (51.0%) were introverts and 140 (49.0%) were extroverts. The number of pregnancies ranged from 1 to 4, with an average of 2.04 ± 0.82, and the number of deliveries ranged from 0 to 3, with an average of 1.62 ± 0.70. Among the participants, 210 (73.4%) had normal deliveries and 76 (26.6%) had cesarean deliveries. The gestational weeks ranged from 34+5 to 41+0. The sex of the babies was 160 (55.9%) male and 126 (44.1%) female. Regarding feeding method, 120 (42.0%) exclusively breastfed, 52 (18.2%) used formula feeding, and 114 (39.9%) used mixed feeding. Among relationship of mother-in-law/daughter-in-law, 62 (21.7%) think it is not good, 138 (48.3%) think it is general, and 86 (30.1%) think it is good.
The EPDS scores of the 286 women during the menstrual period ranged from 0 to 27, with a mean score of 7.78 ± 4.57. A total score of ≥13 was considered indicative of PPD, with 22 participants meeting this criterion, resulting in a positive rate of 7.69%. The PPSS scores ranged from 20 to 80, with a mean score of 58.20 ± 16.29. The SICS total mean scores ranged from 29.32 to 100, with a mean score of 71.70 ± 14.89. The positive coping scores ranged from 1 to 36, with a mean of 23.25 ± 6.82, and the negative coping scores ranged from 1 to 24, with a mean of 9.75 ± 5.43.
Pearson correlation analysis revealed significant correlations between the total PPD score and the total partner support, positive coping, negative coping, and parenting self-efficacy scores. The correlation coefficient values were − 0.63 (p < 0.001), 0.62 (p < 0.001), 0.56 (p < 0.001), and − 0.70 (p < 0.001), respectively, all of which were statistically significant.
Univariate analysis showed that postpartum partner support, coping style, parenting self-efficacy score, maternal personality type, mode of delivery, and mother-in-law-daughter-in-law relationship significantly influenced PPD (p < 0.05). However, factors such as maternal and husband age and education, number of weeks of pregnancy, infant gender, expected baby’s sex, feeding method, and family economy did not have a significant effect on PPD (p > 0.05). Detailed information can be found in Table 1.
Logistic regression analysis was performed with the occurrence of PPD as the dependent variable and the eight factors that showed significant differences in the univariate analysis (partner support, positive coping, negative coping, parenting self-efficacy score, maternal personality type, mode of delivery, and mother-in-law-daughter-in-law relationship) as independent variables. Logistic regression analysis revealed that postpartum partner support and parenting self-efficacy were independent factors influencing PPD, with odds ratios (95% confidence intervals) of 0.76 (0.61 ~ 0.94) and 0.83 (0.75 ~ 0.93), respectively, both p < 0.05. Further details are provided in Table 2.
The area of the curve for postpartum partner support and parenting self-efficacy analyzed by ROC curve was were 1.00 (95% confidence intervals 0.99–1.00), p < 0.001. The sensitivity and specificity for postpartum partner support and parenting self-efficacy were 99.24 and 90.91%. For details, see Table 3 and Figure 1.
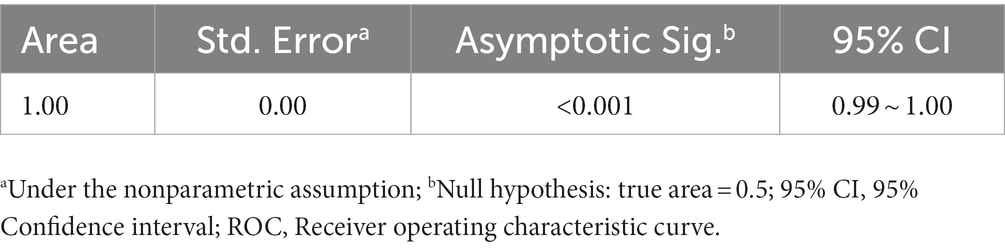
Table 3. ROC curves for postpartum partner support and parenting self-efficacy in assessing the occurrence of PPD.
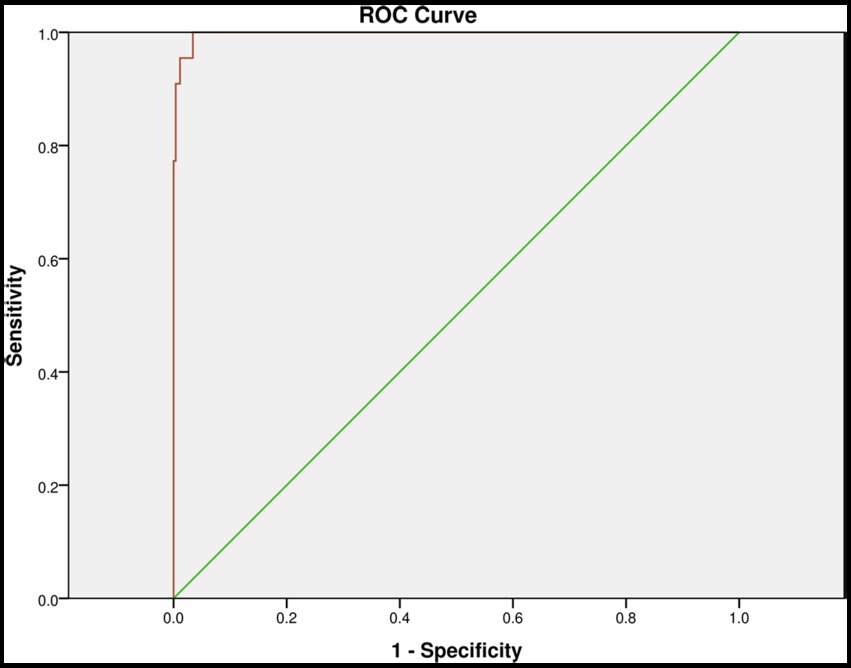
Figure 1. Receiver Operating Characteristic Curve (ROC) curves for postpartum partner support and parenting self-efficacy in assessing the occurrence of PPD.
This study examined the present state of PPD during the traditional Chinese practice of “sitting the month” and analyze the factors that influence maternal PPD in Chinese puerperal women. Our study indicated that a threshold of 10 resulted in sensitivity and specificity values of 0.85 and 0.84, respectively, while a threshold of 13 yielded sensitivity and specificity values of 0.66 and 0.95, respectively (20). Given the evolving landscape of PPD research in China, with recent studies adopting an EPDS threshold of 13 for diagnosis (25–27), our study also employs the EPDS threshold of 13 for diagnosing PPD.
Our results showed that 22 (7.69%) of the women were identified as having PPD. This incidence rate is lower than that reported in previous domestic studies (28, 29). The variation in the incidence of PPD across studies may be attributed to different screening thresholds used in the EPDS scale. Chen and Hu et al. used a threshold of EPDS ≥10 to determine PPD, resulting in a higher incidence rate (28, 29). Additionally, the incidence of PPD can vary among different cities due to variations in maternal lifestyle, work, and economic pressure. Researchers discovered a significant incidence of postpartum depression (19.8–31.0%) within the urban region of Beijing (25), Wuhan (28), and Hangzhou (27), which are categorized as a first-tier city. In the current study, the participants were mothers who gave birth in three hospitals in Quanzhou, a second-tier city, which may explain the slightly lower level of PPD observed (29). However, it is important to note that future research should aim to increase the sample size, expand the scope of the survey, enhance sample representativeness, and incorporate qualitative interviews and objective evaluation methods to conduct more comprehensive and accurate assessments of the current situation of PPD.
In this study, the mean score of postpartum partner support was 58.20 (SD = 16.29), which was slightly lower than the result reported by Eslahi et al. (15) of 64.32 (SD = 10.45). The mean score of the depressed group in this study was 25.73 (SD = 4.81), while the mean score of the non-depressed group was 60.90 (SD = 13.79), which was slightly lower than the result reported by Dennis et al. (14) of 68.09 (SD = 9.52). There was a significant negative correlation between postpartum partner support and PPD (r = −0.626, p < 0.001), which is consistent with the findings of Dennis (r = −0.30, p < 0.01) (14) and Eslahi (r = −0.39, p < 0.001) (15). During the “sitting the month” a traditional Chinese custom where mothers are subjected to various restrictions during the month after delivery, limited socialization and support from family and friends can increase the risk of PPD (30). The spouse is considered the most important source of maternal support during this period. Furthermore, women require support from their partners for infant care, household chores, and emotional well-being (30, 31). Studies had shown that women with poor relationships have at least four times higher incidence of PPD compared to those with good relationships (32).
Therefore, the period of “sitting the month” is a critical time for maternal physical and psychological recovery, and healthcare professionals should acknowledge its importance in postpartum care, especially during the Corona Virus Disease 2019 (COVID-19) pandemic. Maternal partners play a crucial role as a readily accessible source of social support, and postpartum visits should focus on assessing the status of postpartum partner support. Identifying mothers with inadequate postpartum partner support in a timely manner and providing appropriate education and counseling programs for spouses can help reduce the occurrence of PPD and improve the overall well-being of mothers and infants.
Parenting self-efficacy refers to parents’ sense of competence and confidence in their ability to successfully perform various parenting tasks, such as feeding and soothing (33). Our results showed that the total mean score of parenting self-efficacy ranged from 29.32 to 100, with a mean of 71.70 (SD = 14.89). The score of the PPD group of 40.99 (SD = 8.95) was significantly lower than that of the non-depression group of 74.26 (SD = 12.18), and a significant negative correlation (r = −0.698, p < 0.05) was observed between parenting self-efficacy scores and PPD.
Logistic regression analysis also identified parenting self-efficacy as an influential factor for PPD. Hence, it is imperative for healthcare providers to prioritize not only the physical and psychological well-being of mothers during postpartum care and visits, but also to offer a comprehensive range of parenting information and guidance through various online and offline channels. Enhancing mothers’ knowledge of parenting and providing timely feedback on the health status of newborns can improve their sense of parenting competence and confidence, thus reducing the incidence of PPD.
The ROC curve is an analytical method represented as a graph, which is employed to assess the performance of binary diagnostic classification methods. It has been widely adopted in the field of medicine to evaluate the efficacy of diagnostic approaches (34–38). The AUC is a frequently used metric for gaging the accuracy of diagnostic tests. An ideal ROC curve has an AUC of 1.0. For a diagnostic technique to hold meaning, the AUC must exceed 0.5, and in general, it should surpass 0.8 to be deemed acceptable. The AUC is often accompanied by a 95% confidence interval (CI) because data collected from samples are not fixed values; they are subject to statistical errors. The 95% CI establishes a range of possible values around the true value. Hence, for any test to carry statistical significance, the lower 95% CI value of the AUC must be greater than 0.5 (39).
In this study, the AUC of the maternal PPD risk model constructed during the “sitting the month” period was1.00, well above the 0.8 threshold for acceptability. The 95% CI was (0.99, 1.00), and p < 0.001. The sensitivity and specificity were 99.24 and 90.91%. These results suggest that postpartum partner support and parenting self-efficacy can serve as valuable indicators for predicting PPD. Healthcare professionals can employ this early warning model to prevent and promptly identify PPD in women during the “sitting the month” period.
Our research employment of convenience sampling introduces potential bias in participant selection. Consequently, our sample may not fully represent the broader population of postpartum mothers experiencing “sitting the month,” may introduce selection bias, challenging the representativeness of our findings. Consequently, the generalizability of our results beyond our specific study population could be restricted.
Recognizing the significance of representative samples, future research endeavors could embrace more rigorous sampling methods, such as random sampling or stratified sampling. By enhancing the representativeness of the sample, the external validity of study results could be bolstered. Additionally, expanding the scope beyond Quanzhou City to include multiple hospitals and diverse regions could provide a more comprehensive insight into the prevalence of postmenstrual depression during “sitting the month.”
In addition to broadening the study’s geographical scope, the temporal span could be extended longitudinally. Beyond the “sitting the month” period and 4 weeks postpartum, future studies could investigate the enduring relationship between maternal depression and partner support. This expanded timeframe would contribute to a more nuanced understanding of the interplay between maternal mental health and partner dynamics.
Future research should aim to expand sample sizes, utilize qualitative interviews, and employ objective evaluation methods to provide a more accurate understanding of the current situation of PPD.
We have successfully identified the significant protective influence of postpartum partner support and parenting self-efficacy, which exhibit a strong predictive capacity for PPD. Our findings highlight the importance of assessing postpartum partner support and providing appropriate support and education programs during the “sitting the month” to mitigate the risk of PPD. Furthermore, the reduction of PPD can be facilitated by augmenting parenting self-efficacy through comprehensive postpartum care and the provision of parenting information.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving humans were approved by the Ethics Committee of Quanzhou Medical College, Quanzhou, Fujian, China (Ethics Code: No. 2021007). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the minor(s)’ legal guardian/next of kin for the publication of any potentially identifiable images or data included in this article.
XS: direct participation, including conceiving and designing the experiment, implementing the study, collecting data, and analyzing and interpreting the data; article writing, including drafting the article and critical review of the intellectual content of the article; and work support, including statistical analysis and obtaining research funding. YZ: direct participation, including conceiving and designing the experiment; article writing, including critical review of the intellectual content of the article; and work support, including mentoring. MC: direct participation, including conceiving and designing the experiment, implementing the study, and collecting data; article writing, including critical review of the intellectual content of the article; and work support, including statistical analysis and mentoring. HW: direct participation, including conceiving and designing the experiment, implementing the study, collecting data, and analyzing and interpreting the data; article writing, including drafting the article; and work support, including statistical analysis. GL: direct participation, including conceiving and designing the experiment, implementing the study, and analyzing and interpreting the data; article writing, including drafting the article and critical review of the intellectual content of the article; and work support, including statistical analysis and mentoring. All authors contributed to the article and approved the submitted version.
This research was supported by the fundamental project Guided Science and Technology Plan Project of Quanzhou City (2021N137S) and School-level project of Quanzhou Medical College (XJS2114B).
The authors would like to acknowledge the staff of the Quanzhou Women and Children’s Hospital, for designing and collecting data, which contributed greatly to the academic community and made this study possible. We thank Dennis for authorizing our study group to use the scale of PPSS.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1252789/full#supplementary-material
1. American Psychiatric Association Postpartum depression: causes, symptoms, risk factors, and treatment options. (2022). Available at: https://www.apa.org/topics/women-girls/postpartum-depression (Accessed November 15, 2022)
2. Zhao, J, Zhou, D, and Yu, G. Research progress on factors influencing postpartum depression. Chin Mater Child Health. (2010) 8:1154–8.
3. Shorey, S, Chee, C, Ng, ED, Chan, YH, Tam, W, and Chong, YS. Prevalence and incidence of postpartum depression among healthy mothers: a systematic review and meta-analysis. J Psychiatr Res. (2018) 104:235–48. doi: 10.1016/j.jpsychires.2018.08.001
4. Liu, X, Wang, S, and Wang, G. Prevalence and risk factors of postpartum depression in women: a systematic review and meta-analysis. J Clin Nurs. (2022) 31:2665–77. doi: 10.1111/jocn.16121
5. Stein, A, Pearson, RM, Goodman, SH, Rapa, E, Rahman, A, McCallum, M, et al. Effects oAf perinatal mental disorders on the fetus and child. Lancet. (2014) 384:1800–19. doi: 10.1016/S0140-6736(14)61277-0
6. Al-Hammadi, FA, Al-Tahri, F, Al-Ali, A, Nair, SC, and Abdulrahman, M. Limited understanding of pap smear testing among women, a barrier to cervical cancer screening in the United Arab Emirates. Asian Pacific J Cancer Prevent. (2017) 18:3379–87. doi: 10.22034/APJCP.2017.18.12.3379
7. Junge, C, Garthus-Niegel, S, Slinning, K, Polte, C, Simonsen, TB, and Eberhard-Gran, M. The impact of perinatal depression on children's social-emotional development: a longitudinal study. Matern Child Health J. (2017) 21:607–15. doi: 10.1007/s10995-016-2146-2
8. Slomian, J, Honvo, G, Emonts, P, Reginster, JY, and Bruyere, O. Consequences of maternal postpartum depression: a systematic review of maternal and infant outcomes. Womens Health. (2019) 15:1745978572. doi: 10.1177/1745506519844044
9. Baird, H, Harris, RA, and Santos, HJ. The effects of maternal perinatal depression on child iq: a systematic review. Matern Child Health J. (2023) 27:1489–502. doi: 10.1007/s10995-023-03715-3
10. Kroska, EB, and Stowe, ZN. Postpartum depression: identification and treatment in the clinic setting. Obstet Gynecol Clin N Am. (2020) 47:409–19. doi: 10.1016/j.ogc.2020.05.001
11. Zhao, XH, and Zhang, ZH. Risk factors for postpartum depression: an evidence-based systematic review of systematic reviews and meta-analyses. Asian J Psychiatr. (2020) 53:102353. doi: 10.1016/j.ajp.2020.102353
12. Chi, X, Zhang, P, Wu, H, and Wang, J. Screening for postpartum depression and associated factors among women in China: a cross-sectional study. Front Psychol. (2016) 7:1668. doi: 10.3389/fpsyg.2016.01668
13. Jones, E, and Coast, E. Social relationships and postpartum depression in south asia: a systematic review. Int J Soc Psychiatry. (2013) 59:690–700. doi: 10.1177/0020764012453675
14. Dennis, CL, Brown, HK, and Brennenstuhl, S. The postpartum partner support scale: development, psychometric assessment, and predictive validity in a Canadian prospective cohort. Midwifery. (2017) 54:18–24. doi: 10.1016/j.midw.2017.07.018
15. Eslahi, Z, Alimoradi, Z, Bahrami, N, Lin, CY, Griffiths, MD, and Pakpour, AH. Psychometric properties of postpartum partner support scale-persian version. Nurs Open. (2021) 8:1688–95. doi: 10.1002/nop2.806
16. Yim, IS, Tanner, SL, Guardino, CM, Hahn-Holbrook, J, and Dunkel, SC. Biological and psychosocial predictors of postpartum depression: systematic review and call for integration. Annu Rev Clin Psychol. (2015) 11:99–137. doi: 10.1146/annurev-clinpsy-101414-020426
17. Anthony, RE, Paine, AL, and Shelton, KH. Depression and anxiety symptoms of british adoptive parents: a prospective four-wave longitudinal study. Int J Environ Res Public Health. (2019) 16:5153. doi: 10.3390/ijerph16245153
18. Zeng, X, Nie, Y, Liu, Y, Xu, B, Ren, L, Huang, N, et al. A study of postpartum depression and coping styles among migrant women in Dongguan. J Guangzhou Med Univ. (2019) 47:107. doi: 10.3969/j.issn.2095-9664.2019.06.28
19. Zheng, W, and He, F. Calculation of sample size for fact-finding missions. Prev Med. (2020) 32:647–8. doi: 10.19485/j.cnki.issn2096-5087.2020.06.028
20. Levis, B, Negeri, Z, Sun, Y, Benedetti, A, and Thombs, BD. Accuracy of the Edinburgh postnatal depression scale (epds) for screening to detect major depression among pregnant and postpartum women: systematic review and meta-analysis of individual participant data. BMJ. (2020) 371:m4022. doi: 10.1136/bmj.m4022
21. Zakeri, MA, Khoram, S, Bazmandegan, G, Ghaedi-Heidari, F, Talebi, B, Ramezani, N, et al. Postpartum depression and its correlates: a cross-sectional study in Southeast Iran. BMC Womens Health. (2022) 22:387. doi: 10.1186/s12905-022-01978-6
22. Hanach, N, Radwan, H, Fakhry, R, Dennis, CL, Issa, WB, Faris, ME, et al. Prevalence and risk factors of postpartum depression among women living in the United Arab Emirates. Soc Psychiatry Psychiatr Epidemiol. (2023) 58:395–407. doi: 10.1007/s00127-022-02372-1
23. Wang, Q, Zhang, Y, Li, X, Ye, Z, Huang, L, Zhang, Y, et al. Exploring maternal self-efficacy of first-time mothers among rural-to-urban floating women: a quantitative longitudinal study in China. Int J Environ Res Public Health. (2021) 18:18. doi: 10.3390/ijerph18062793
24. Jing, X, Meng, H, Li, Y, Lu, L, and Yao, Y. Associations of psychological capital, coping style and emotional intelligence with self-rated health status of college students in China during covid-19 pandemic. Psychol Res Behav Manag. (2022) 15:2587–97. doi: 10.2147/PRBM.S383743
25. Zhao, J, and Jin, L. Analysis of the depression status of postpartum women in Beijing and its influencing factors. Chin Matern Child Health Res. (2022) 33:83–8. doi: 10.3969/j.issn.1673-5293.2022.11.014
26. Chu, Y, Li, Y, Chen, X, and Yu, F. Analysis of the correlation between maternal and infant health literacy and other psychosocial factors and postpartum depression. Prac Prevent Med. (2022) 29:995–7. doi: 10.3969/j.issn.1006-3110.2022.08.025
27. He, X, Sun, J, and Gao, M. Survey on the current situation of postpartum depression among primiparous women and analysis of its influencing factors. Chin J Fam Plan. (2022) 30:2683–7. doi: 10.3969/j.issn.1004-8189.2022.12.004
28. Hu, J, Wang, Y, and Liu, Y. A study on the correlation between maternal sitting behavior and postpartum depression. J Nurs. (2017) 32:30–2. doi: 10.3870/j.issn.1001-4152.2017.24.030
29. Chen, X, Qian, F, Luo, T, Wu, F, Zhou, Y, and Su, Y. Screening for depressed mood at 6 weeks postpartum and analysis of factors influencing it. Chin Matern Child Health Res. (2022) 33:70–5. doi: 10.3969/j.issn.1673-5293.2022.11.012
30. Almutairi, AF, Salam, M, Alanazi, S, Alweldawi, M, Alsomali, N, and Alotaibi, N. Impact of help-seeking behavior and partner support on postpartum depression among saudi women. Neuropsychiatr Dis Treat. (2017) 13:1929–36. doi: 10.2147/NDT.S135680
31. Rowe, HJ, and Fisher, JR. Development of a universal psycho-educational intervention to prevent common postpartum mental disorders in primiparous women: a multiple method approach. BMC Public Health. (2010) 10:1–15. doi: 10.1186/1471-2458-10-499
32. Qiu, Z, Wang, J, and Lv, C. Investigation on emotion assessment of pregnant women and prevention of postpartum depression. China maternal and child. Health. (2010) 25:2710–2.
33. Prasopkittikun, T, Tilokskulchai, F, Sinsuksai, N, and Sitthimongkol, Y. Self-efficacy in infant care scale: development and psychometric testing. Nurs Health Sci. (2006) 8:44–50. doi: 10.1111/j.1442-2018.2004.00266.x
34. Guo, L, Ding, Y, Zhang, Z, Gao, H, and Fang, L. Establishment of predictive model of midwives' decision on episiotomy during childbirth. Chin J Nurs. (2019) 54:1469–74. doi: 10.3761/j.issn.0254-1769.2019.10.005
35. Li, J, Luo, J, Liu, G, and Yan, S. Influencing factors and risk prediction model for cervical cancer recurrence. Zhong Nan Da Xue Xue Bao Yi Xue Ban. (2022) 47:1711–20. doi: 10.11817/j.issn.1672-7347.2022.210722
36. Xie, T, Xin, Q, Cao, X, Chen, R, Ren, H, Liu, C, et al. Clinical characteristics and construction of a predictive model for patients with sepsis related liver injury. Clin Chim Acta. (2022) 537:80–6. doi: 10.1016/j.cca.2022.10.004
37. Liu, X, Liu, L, Jiang, H, Zhao, C, and He, H. Establishment of a nomogram model for predicting necrotizing enterocolitis in very preterm infants. Chin J Contemp Pediatr. (2022) 24:778–85. doi: 10.7499/j.issn.1008-8830.2202093
38. Yong, SX, Qiao, C, Gang, LT, Yuan, SY, Jian, SY, and Juan, C. Analysis of factors influencing insomnia and construction of a prediction model: a cross-sectional survey on rescuers. Biomed Environ Sci. (2020) 33:502–9. doi: 10.3967/bes2020.067
Keywords: sitting the month, postpartum depression, partner support, prediction modeling, puerperal women
Citation: Su X, Zhang Y, Chen M, Wang H and Liu G (2023) Influencing factors and risk prediction modeling of maternal postpartum depression: a cross-sectional study in Chinese puerperal women of sitting the month. Front. Psychiatry. 14:1252789. doi: 10.3389/fpsyt.2023.1252789
Received: 06 July 2023; Accepted: 29 August 2023;
Published: 14 September 2023.
Edited by:
David Ramiro-Cortijo, Autonomous University of Madrid, SpainReviewed by:
Sophida Phuthong, Khon Kaen University, ThailandCopyright © 2023 Su, Zhang, Chen, Wang and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuezhen Zhang, NDk5MzY4MzAwQHFxLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.