- 1Department of Psychiatry, School of Clinical Medicine, LKS Faculty of Medicine, The University of Hong Kong, Pokfulam, Hong Kong SAR, China
- 2School of Public Health, LKS Faculty of Medicine, The University of Hong Kong, Pokfulam, Hong Kong SAR, China
- 3State Key Laboratory of Brain and Cognitive Sciences, The University of Hong Kong, Pokfulam, Hong Kong SAR, China
Introduction: Literature reveals increased suicidal ideation in the general population during pandemic. However, few COVID-19 studies comprehensively assessed factors associated with suicidal ideation, and mixed findings were observed. We aimed to examine prevalence and correlates of suicidal ideation in general public during the peak of fifth COVID-19 wave in Hong Kong based on a broad array of relevant measures.
Methods: This survey assessed 14,709 community-dwelling adults during March 15–April 3, 2022. Comprehensive assessment was administered including socio-demographics, pre-existing mental/physical morbidity, mental-health symptoms, resilience, loneliness, coping strategies, and pandemic-related factors. Presence of suicidal ideation was evaluated by ratings of item 9 on Patient-Health-Questionnaire-9.
Results: A total of 2,249 (15.3%) participants exhibited suicidal ideation. Multivariable-regression analysis found that being single and unemployed, pre-existing mental disorder, more severe depressive and anxiety symptoms, higher levels of loneliness and engagement in avoidant coping were significantly associated with suicidal ideation. Conversely, attaining tertiary educational level or above, greater resilience and adopting problem-focused coping were associated with lower likelihood of suicidal ideation. Although univariate-analyses revealed that a number of pandemic-related factors were linked to suicidal ideation, none remained significant in the multivariable model.
Conclusion: A significant proportion of people experienced suicidal ideation during the peak of fifth COVID-19 wave. Risk and protective factors identified would facilitate early identification of high-risk individuals and provision of targeted interventions to minimize suicidal ideation and risk of self-harm. Caution should be exercised due to study limitations of a cross-sectional design which precluded establishing causality among variables, and reliance on self-reported data.
Introduction
Coronavirus disease (COVID-19) was declared a global pandemic by the World Health Organization in March 2020 (1), for imposing public health crisis. COVID-19 literature conducted in the community consistently demonstrated its profound impacts on both physical and mental health outcomes, including anxiety, depressive symptoms and psychological distress (2, 3). The effects of the pandemic itself combined with the prolonged implementation of social containment policies led to indirect socioeconomic repercussions, including economic downturn (4), social isolation (5), unemployment (6), and barriers to access mental health services (7) due to public health policies might in turn increase suicidality (8).
An elevated risk of suicide has been consistently linked to pandemic outbreaks across the world (9), with increased completed suicide rate in the United States during the 1918–1919 influenza pandemic (10), and increased rate of suicidal attempts during Ebola outbreak (11). Similarly, increased likelihood of suicide behaviors were observed during the COVID-19 pandemic (12–14). Hong Kong (HK) was the epicentre of the Severe Acute Respiratory Syndrome (SARS) in 2003, which caused 1,755 infections and 300 fatalities (15), and endured months of social unrest in 2019 just before the first local outbreak of COVID-19. Previous studies found an increased suicide rate in the elderlies during SARS epidemic in HK (15, 16). Throughout the whole 2021, there were fewer than 4,000 COVID-19 cases reported in HK (17). HK then experienced the fifth COVID-19 wave after the emergence of the Omicron variant in December 2021, with the 7-day rolling average of COVID-related deaths reaching 3.73 per 1,000 people at the peak, the highest worldwide (18, 19). However, until now, there has been lack of research evaluating suicidal ideations in the general population of HK that had this distinctive pandemic experience.
Suicidal ideation is defined as thinking about, considering or planning suicide (20). It is critical to understand suicidal ideation, which is a strong predictor of subsequent suicide attempts and completed suicides (21). Detecting its prevalence, risk factors and protective factors in the general population is essential for informing effective suicide prevention strategies. Development of suicidal ideation is multifactorial and involves a complex interplay between biological and psychosocial determinants (22). Some sociodemographic characteristics (such as younger age, socioeconomic disadvantage, single marital status and unemployment) and COVID-19 pandemic-related factors (such as contracting COVID-19 and social containment measures) are reported to be associated with suicidal ideations (23–27). Patients with pre-existing mental disorders are more likely than healthy persons to suffer an emotional response to the COVID-19 pandemic, leading to relapse or worsening of symptoms (7). For instance, people with a pre-existing mood or anxiety disorder had considerably higher scores of COVID-19-related traumatic stress symptoms than individuals without a current mental condition (28). Furthermore, while previous studies have consistently reported loneliness as a significant risk factor for suicidal ideation (24, 29–31), there is a gap in the literature simultaneously encompassing other protective psychosocial measures [e.g., different coping styles and resilience that have been linked to improved mental health outcomes in other contexts (32)] in studying suicidal ideations during COVID-19 pandemic. Relatively few studies have been conducted to systematically evaluate a broad range of factors associated with suicidal ideations in the general population during the COVID-19 pandemic.
To this end, the current study aimed to assess the prevalence of suicidal ideation among the general population amidst the peak of the fifth COVID-19 wave in HK (March–April, 2022). Importantly, we examined the correlates of suicidal ideation across a comprehensive array of variables encompassing socio-demographics, pre-existing illness profile, mental health symptoms, psychosocial measures as well as pandemic-related factors.
Materials and methods
Participants and study setting
This cross-sectional survey aimed to recruit community-dwelling adults aged 18 years or above in HK from March 15 to April 3, 2022 (33), during which the city was experiencing the peak of the fifth COVID-19 wave. It was estimated that approximately half of the population (3.6 million) have contracted the infection during the fifth wave by mid-March (34), and public health containment and social-distancing measures were further tightened in response to the surge of COVID cases (17). Details of the study design have been described in our recently published report (33), which examined the association between COVID-19 perseverative cognition and depression, and the moderating effect of potential risk and protective factors on this association in the general public. Briefly, we adopted snowballing sampling technique for data collection, with an online anonymous self-rated questionnaire being administered on a Qualtrics survey platform.1 Virtual snowballing sampling is a commonly-used recruitment strategy during COVID-19 pandemic [(e.g., 35–37)], which enables researchers to obtain a large sample within a short period of time and to minimize the interference of stringent control measures on data collection. The survey was disseminated through social media platforms (e.g., Facebook, Instagram, Twitter, WhatsApp), universities (via emails), and the Hong Kong Public Opinion Research Institute (HKPORI) which sent email invitations with survey link to the members of its probability- and non-probability- based online panels of adult HK residents. HKPORI is a well-established survey agency which has executed numerous independent public surveys for academic institutions and government departments in HK (38). Respondents were encouraged to forward the survey link to their social networks for study participation. Survey participation was on a voluntary basis and online informed consent was obtained before questionnaire assessment. The survey took around 20 min to complete. The study was approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (HKU/HA HKW). The survey received 20,971 responses. Respondents who were not residing in HK during the study period, did not provide consent or failed to complete the questionnaire items on the primary measure of the current study (i.e., the Patient Health Questionnaire [PHQ-9] including the last item which assessed self-reported suicidal ideation) were excluded. A total of 14,709 respondents constituted the final sample for the current analysis.
Assessments
The self-rated study assessment comprised four sections including sociodemographic, illness profile and mental health symptoms, psychosocial measures, and COVID-19-related factors. Sociodemographic characteristics included age, gender, marital status, highest attained educational level, employment status, size of residential housing and monthly household income. Illness profile included pre-existing mental health diagnosis, alcohol/substance use, and chronic physical disease.
Concerning mental health symptoms, depressive and anxiety symptom severity were assessed by Patient Health Questionnaire-9 [PHQ-9; (39, 40)] and Generalized Anxiety Disorder-7 scale [GAD-7; (41, 42)], respectively, with both scales using a 4-point Likert scale ranging from 0 (never) to 3 (nearly every day). A validated Chinese version of Obsession with COVID-19 Scale [OCS; (43, 44)] was administered to measure the frequency of persistent and disturbing thinking about COVID-19, within a 2-week timeframe on a 5-point Likert scale ranging from 0 (not at all) to 4 (nearly every day). In the current study, depressive symptom severity was quantified by the sum of the items 1 to 8 on PHQ-9. Sleep quality and disturbance were assessed using Insomnia Severity Index [ISI; (45, 46)]. For all of the symptom scales, higher scores indicated greater symptom severity. Following the method of previous studies examining suicidal ideations in general public during COVID-19 (26, 47), an item 9 on the PHQ-9, namely “During the past 2 weeks, how often have you been troubled by the notion that you would be better off dead or hurting yourself?,” was used to evaluate the presence of suicidal ideation. Specifically, participants who responded to an item 9 as “not at all” (i.e., rating = 0) were considered having no suicidal ideation, whereas those whose rating was 1–3 (i.e., “several days,” “more than half the days,” or “nearly every day”) were categorized as having suicidal ideation.
Regarding psychosocial measures, participants’ coping strategies were assessed by an adapted Coping Orientation to Problems Experienced Inventory–Brief [Brief-COPE; (48, 49)], which used a 4-point Likert scale ranging from 0 (never) to 3 (always). The 14 items of the adapted Brief-COPE were grouped into 3 copying styles based on previous factor-analytic study (50), namely avoidant, emotion-focused and problem-focused coping styles for subsequent analysis. A higher item sum score indicated a higher level of engagement in that particular coping style. The Chinese version of the three-item UCLA Loneliness Scale was applied to measure loneliness on a three-factor structure (51, 52). The Brief Resilience Scale [BRS; (53, 54)] was used to assess resilience levels on a 5-point Likert scale (1 [strongly disagree] to 5 [strongly agree]), with higher scores indicating greater resilience. Evaluation of COVID-19-related factors comprised items assessing history of contracting COVID-19 infection, receipt of vaccination, exposure to COVID-19-related information, COVID-19-related stressors experienced, specific infection control measures (e.g., under quarantine, mandatory COVID-19 testing) experienced and associated distress. Details of assessment of COVID-19 related factors are summarized in Supplementary Table S1.
Statistical analysis
First, a series of univariate binary logistic regression analyses were conducted to examine the association of suicidal ideation status (yes vs. no) with a broad array of variables covering socio-demographics, illness profiles and mental health symptoms, psychosocial measures and COVID-19 related factors. Then, those variables that were found to be statistically significant in the preceding univariate analyses were then included in the multivariable binary logistic regression model, based on backward Wald statistics, to determine factors which were independently associated with suicidal ideation. All analyses were conducted using SPSS 23.0, with significance level set as p < 0.05.
Results
Sample characteristics and prevalence of suicidal ideation
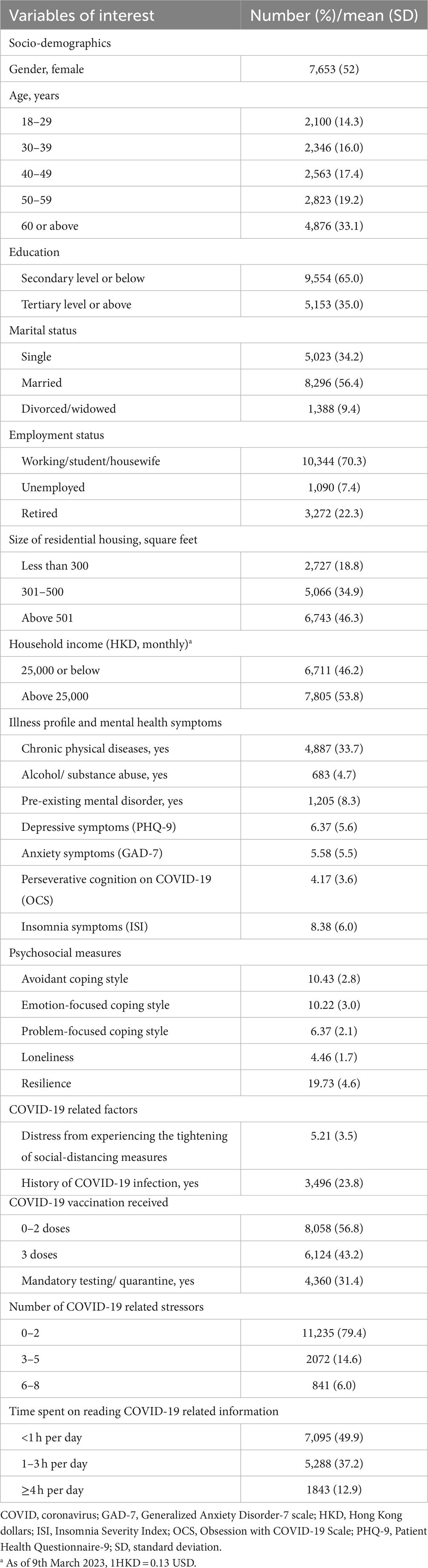
Table 1 summarizes the characteristics of the study sample. A total of 52.9% participants were women, and 14.3, 16.0, 17.4, 19.2 and 33.1% were aged 18–29, 30–39, 40–49, 50–59, and ≥60 years, respectively. Slightly more than half of the sample (56.4%) were married, and 35% attained tertiary educational level. Based on the ratings of item 9 on PHQ-9, 15.3% (n = 2,249) participants were classified as having suicidal ideation, including 10.7% (n = 1,570) seldom reported suicidal ideation, 2.8% (n = 413) often had suicidal ideation and 1.8% (n = 266) always reported suicidal ideation over the past 2 weeks of survey assessment.
Correlates of suicidal ideation
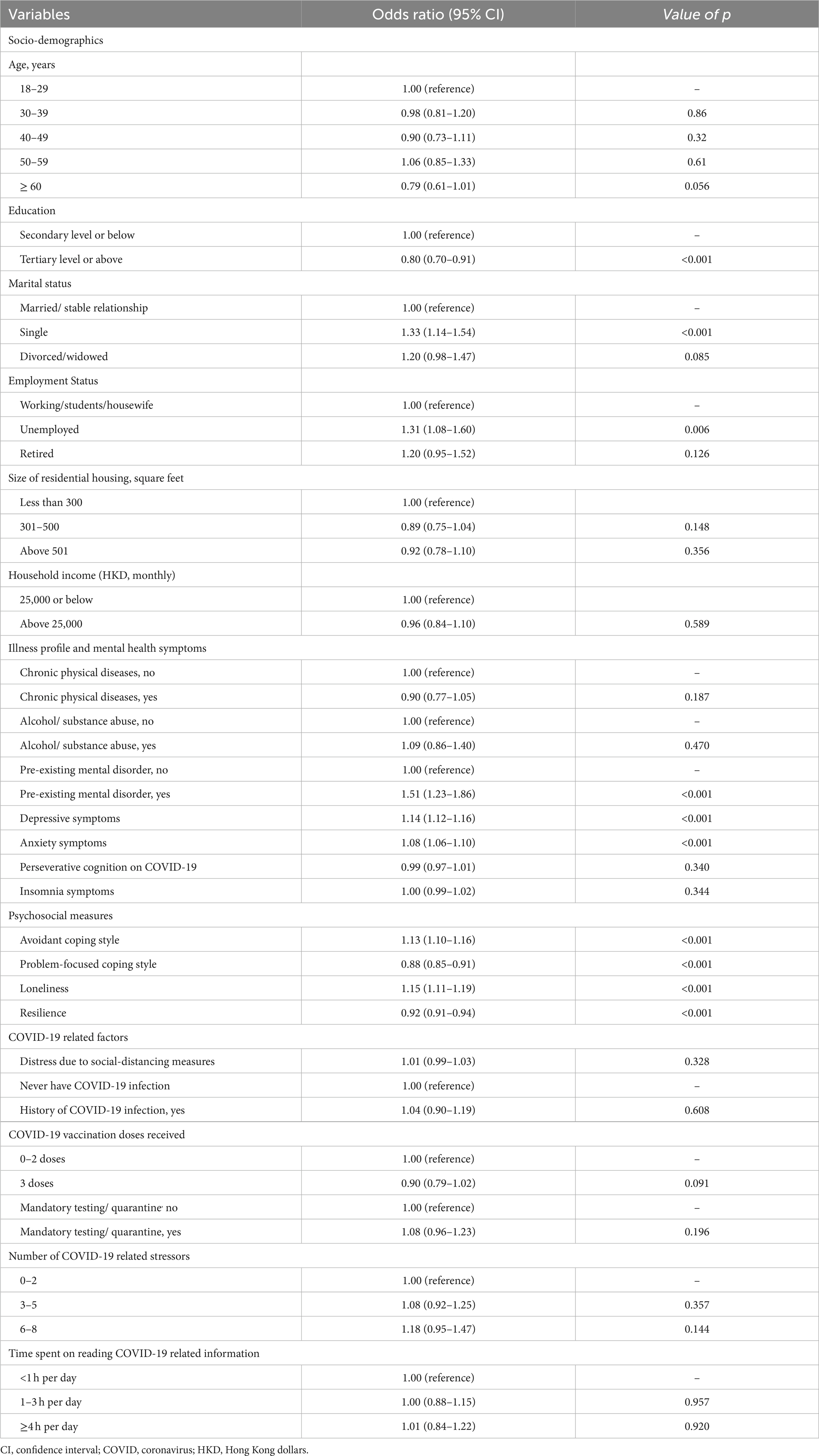
As shown in Table 2, participants’ age, educational level, marital status, employment status, size of residential housing and monthly household income were significantly related to suicidal ideation in univariate regression analyses. Regarding illness profile and mental health symptoms, ratings on PHQ-9, GAD-7, OCS and ISI were associated with suicidal ideation. Table 3 shows that UCLA Loneliness Scale scores, BRS scores, and higher levels of engagement with avoidant and problem-focused coping styles were significantly related to suicidal ideation. For pandemic-related factors, history of COVID-19 infection, vaccination status, history of mandatory testing/quarantine, number of COVID-19 related stressors, exposure on reading pandemic-related information, and level of distress due to social-distancing measures were associated with suicidal ideation in univariate regression analyses.
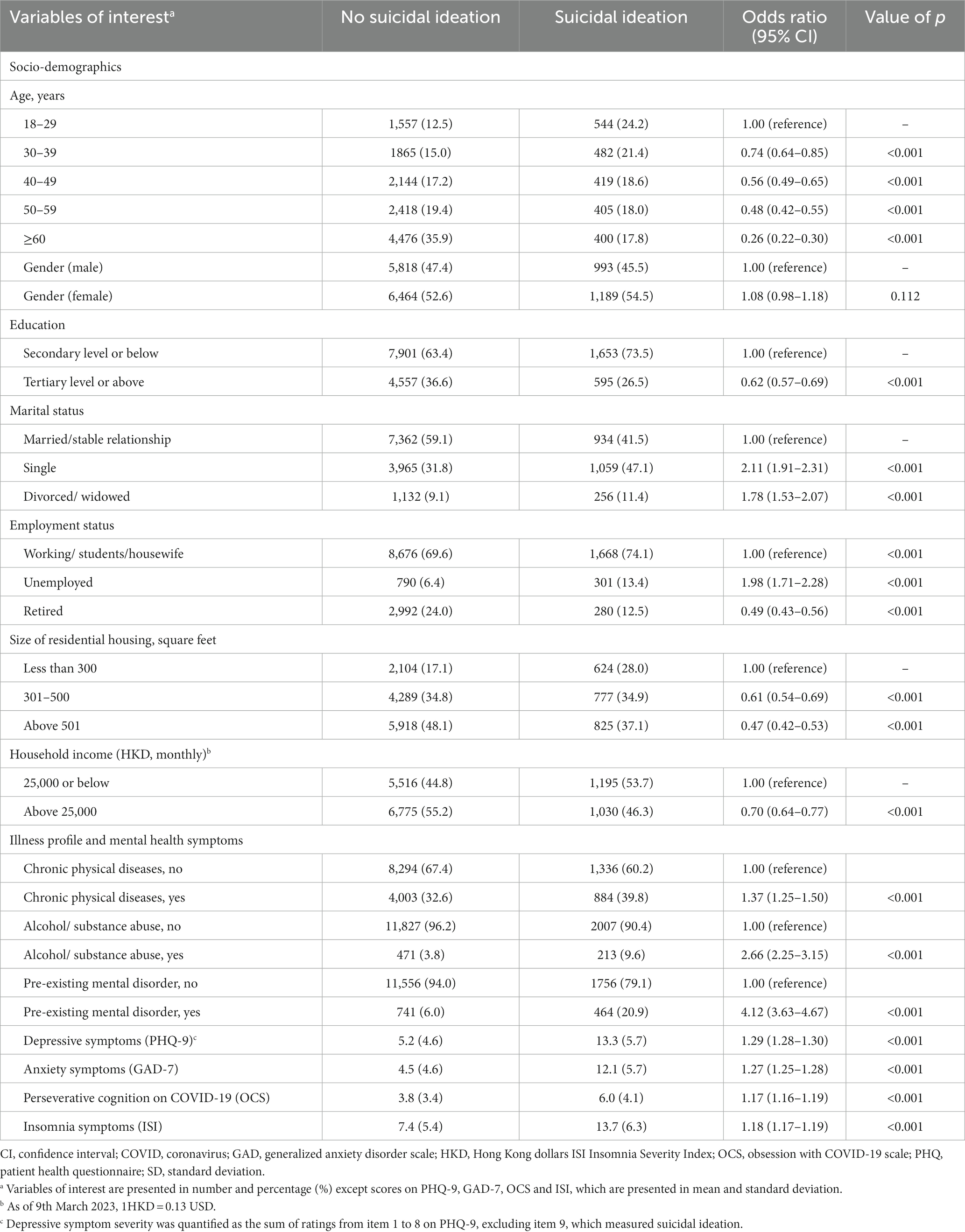
Table 2. Univariate regression analyses on the relationship of suicidal ideation with socio-demographics, illness profile and mental health symptoms.
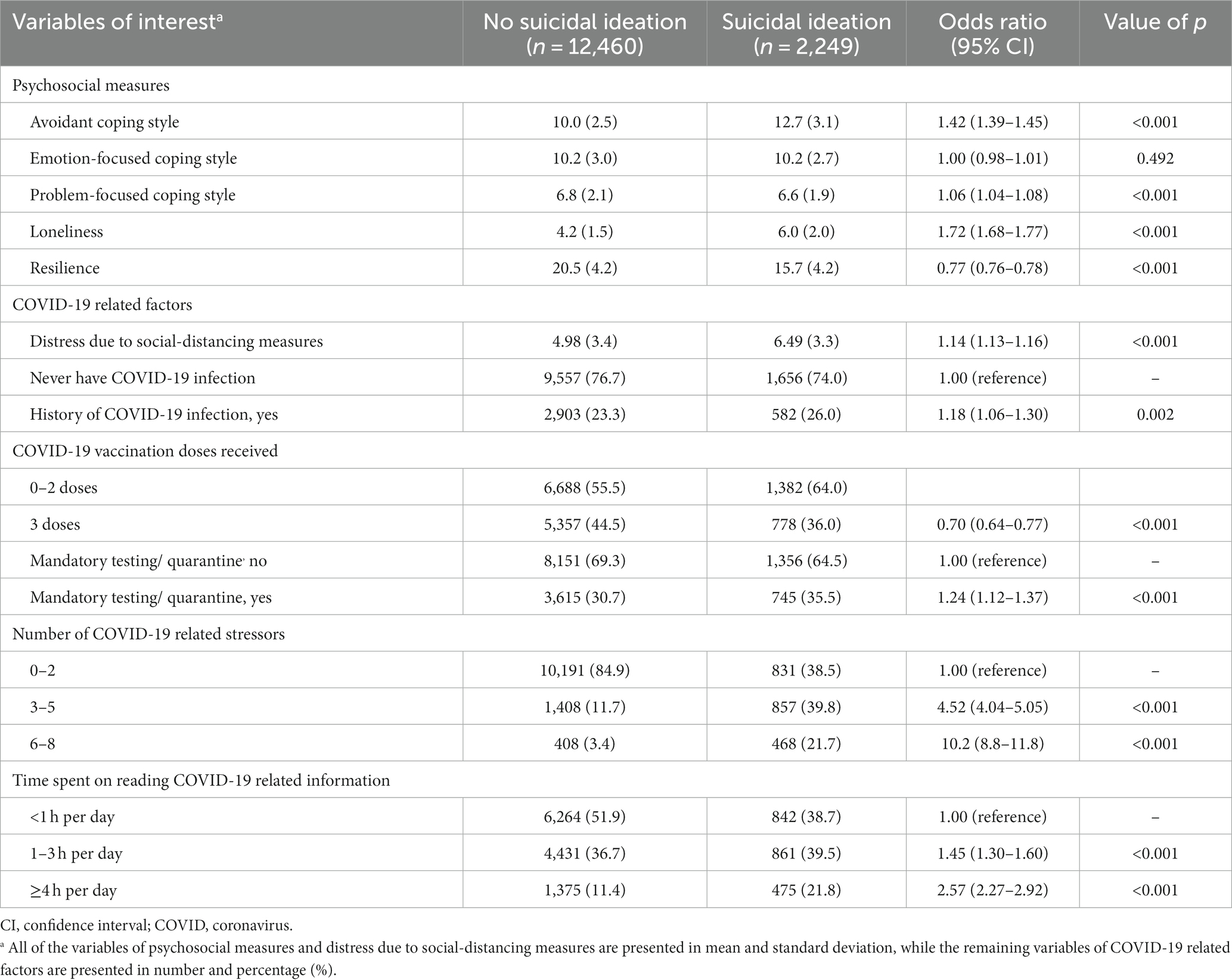
Table 3. Univariate regression analyses on the relationship of suicidal ideation with psychosocial measures and COVID-19 related factors.
A multivariable logistic regression analysis revealed that attainment of tertiary educational level or above, greater resilience, and adoption of problem-focused coping style were independently associated with decreased likelihood of experiencing suicidal ideation (Table 4), while the relationship between older age (≥60 years) and suicidal ideation approached statistical significance (p = 0.056). Conversely, single marital status, being unemployed, pre-existing mental disorder, more severe depressive and anxiety symptoms, higher levels of loneliness, and engagement in avoidant coping style were associated with increased risk of suicidal ideation.
Discussion
The current study aimed to examine the prevalence and correlates of suicidal ideation in the general population (predominantly Chinese) during the peak of the fifth COVID-19 wave in HK. This is among the few studies that comprehensively assessed a wide array of factors associated with suicidal ideation in the general public amidst the pandemic, encompassing socio-demographics, illness profile and mental health symptoms, psychosocial variables of loneliness, resilience and coping strategies, as well as COVID-19 related variables. Our results showed that approximately one-sixths (15.3%) of the study sample experienced suicidal ideation amidst the fifth wave of pandemic. This is slightly higher than the pooled prevalence estimate of suicidal ideation during COVID-19 reported in a recent meta-analysis (26), as well as those observed in the Chinese population from mainland China (13.4%) and Taiwan (10.8%) (26, 54). The distinctive experiences of HK population with unique prior exposure of the SARS epidemic and social unrest just before COVID-19 may have also contributed to the susceptibility to increased suicidal ideation during the fifth wave of pandemic.
Our findings are generally consistent with the notion of the complex interplay among various risk and protective factors for suicidal ideation (22). We affirmed results of previous COVID-19 studies that a number of key socio-demographic characteristics were significantly associated with increased risk of suicidal ideation (6, 23–26). Being single, unemployed and less educated are well-established risk factors for suicidal ideation and behaviors in the literature, irrespective of the pandemic. Alternatively, our observation that aged ≥60 years was related to the lowest likelihood of having suicidal ideation (albeit of trend-wise significance) suggested that people of older age might be relatively susceptible to the development of suicidal ideation during pandemic. This in fact corroborated with some studies examining suicidal ideation during the COVID-19 using online survey design (23, 25, 26). Of note, we are cautious that web-based survey data may potentially bias the results in favor of those more resourceful older-aged participants (among the elderly population) who had access to online platforms and were equipped with the skills to administer the survey questionnaire (55). This is intriguing given the contrary finding that elderly people, but not the younger-age group, had an increased suicide rate during SARS epidemic in HK (15, 16). Alternatively, it is possible that compared to SARS, COVID-19 pandemic is far more long-lasting with more prolonged public health and social-distancing measures for infection control. Yet, older-aged people are in general less likely to be employed or engaged in activities that require frequent face-to-face interactions. Hence, they may be comparatively less affected by the stringent public health polices, with lower degree of persistent exposure to COVID-19 related stressors such as unemployment and financial uncertainty, and the consequent adverse psychological impact including suicidal ideation.
We found that more severe depressive and anxiety symptoms, and the presence of pre-existing mental disorder were independently associated with raised likelihood of developing suicidal ideation. Substantial evidence has noted that individuals with mental disorders are more vulnerable to increased psychological distress than those without mental disorders during the pandemic (7, 28). It is also well-acknowledged that mental disorders represent a key predictor of suicidal ideation and behaviors (56, 57). Consistent with prior research (25), our findings demonstrated that pre-existing mental disorder was the strongest factor associated with suicidal ideation in the general population during the fifth COVID-19 wave. In line with a large body of research (and disregard of the pandemic) (27, 47, 55, 58, 59), we observed that greater depressive and anxiety symptom severity were significantly related to suicidal ideation. Accumulating data have further suggested that these mood symptoms may even persist after the pandemic (60). Overall, our results highlight the significance of early identification of and prompt treatment to depressive and anxiety symptoms, as well as the need to optimize psychiatric treatment for pre-existing mental disorders so as to minimize the risk of suicidal ideation and subsequent self-harm attempts during the pandemic. In this regard, health and welfare polices ensuring adequate access and availability of mental health services and mobilizing community service support would facilitate early detection of high-risk subgroup and timely provision of effective intervention to alleviate mood symptoms and reduce self-harm risk (61). Emerging evidence has also demonstrated the effectiveness of tele-health care including mental health screening, assessment and treatment of depression (62), and indicated this approach as a feasible and reliable alternative of standard healthcare delivery during pandemic (63, 64). Future research should concentrate on evaluating tailor-made mental health interventions to meet the specific need of this high-risk subgroup, who have pre-existing mental disorders and/or persistent mood symptoms, during and after the pandemic (7).
Our results demonstrated that greater resilience and higher level of engagement in problem-focused coping style were significantly associated with lower risk of developing suicidal ideation during the peak of fifth pandemic wave. Alternatively, higher degree of loneliness and adoption of avoidant coping style were linked to suicidal ideation. This generally concurs with the research conducted before COVID-19 showing that avoidant coping strategies are a risk factor for suicidal ideation (65), whereas problem-focused coping can be protective from self-harm (66, 67). Resilience is the capacity and dynamic process of adaptively overcoming stress and adversity while maintaining normal functioning (68). Higher level of resilience has been found to reduce depressive symptoms (69), mitigate the effect of pandemic-related stress on negative mental health outcomes (70), and to be a protective factor against suicide risk (71, 72). Our finding that loneliness was independently associated with suicidal ideation is in line with previous studies, including those conducted during the COVID-19 pandemic, showing that loneliness is a significant predictor of suicidal ideation and behavior (24, 30, 73). It is noteworthy that loneliness and social connection are separate constructs with overlapping features (74). Loneliness, defined as the subjective perception of insufficient social contact, can exacerbate feelings of vulnerability and heighten hypervigilance to social threats, which adversely affect psychosocial functioning and may result in poorer mental health outcomes (75). In this regard, loneliness may be more closely associated with suicidal ideation and behavior than other aspects of social connection, such as social distancing, emotional support and interpersonal conflict (76). An earlier local COVID-19 study also found that subjective feelings of loneliness were associated with increased mental health symptoms among the general public in HK (77). Taken together, these results underscore the importance of promoting resilience (at individual and community levels, for instance via practicing self-care and cultivating community) (72, 78), social support (i.e., reduction of sense of loneliness) and the use of adaptive coping as effective strategies to minimize the adverse impact of pandemic on increased suicidal ideation and self-harm risk (79). On the other hand, although our univariate analyses revealed that a number of COVID-19 related factors, such as number of pandemic-related stressors, distress due to social-distancing measures, history of contracting COVID-19 and vaccination status, are related to suicidal ideation, none of these variables remained significant in the final multivariable model. This is contrary to some past studies which suggested that certain COVID-19 related factors including experience of quarantine and confirmed infection were significantly related to higher odds of suicidal ideation (23, 26, 27). It might be possible that an effect of COVID-19 related factors on suicidal ideation may be fully mediated by other variables included in our final regression model, which incorporated a comprehensive range of candidate factors encompassing illness profile, mental health symptoms and psychosocial measures. Alternatively, it is important to take into consideration the broader context beyond the impact of the fifth pandemic wave. Previous COVID-19 pandemic waves, the accompanying financial/economic crisis (4), and ensuing geopolitical shifts (80) could also pose influences on individuals’ mental wellbeing and suicidality. These broader-contextual factors can compound the stress and isolation imposed by pandemic circumstances, intensifying feelings of loneliness and vulnerability to psychological distress (81). As such, future investigation should clarify the complex interplay between these factors on mental health outcomes.
The study has several limitations. First, the cross-sectional study design precludes establishment of causal relationship. Longitudinal research is warranted to determine the course of suicidal ideations over time and its predictors. Second, although an item 9 on PHQ-9 is a commonly used measure in psychiatric research to determine the presence of suicidal ideation (21, 26, 47, 82), scales that are specifically developed for suicidal ideation/suicide risk assessment would provide a more comprehensive and accurate evaluation (83). Third, the snowballing sampling strategy is non-probabilistic in nature and may compromise the representativeness of the sample and study results. Additionally, the questionnaire was distributed and administered online, people with limited access to smartphone or computers would be excluded from the survey, resulting in some selection bias. Nevertheless, online health survey with virtual snowballing strategy is a widely-used and reliable method to assess psychological distress in the general population amidst the COVID-19 pandemic, particularly in the face of difficulties to access and recruit participants under the circumstances of stringent community containment measures to curb the spread of infection (84). Fourth, psychological symptom assessment was based on participants’ self-reporting (though these scales are well-validated and commonly used in research), which may not well align with the corresponding rating instruments administered by mental health professionals.
Our study showed that around 15% of the general population in HK displayed suicidal ideation during the peak of the fifth wave of the COVID-19 pandemic. People who are single, less educated and unemployed, have pre-existing mental disorder, higher levels of loneliness, depressive and anxiety symptoms, and engagement of avoidant coping style are significantly more likely to experience suicidal ideation. Conversely, greater resilience and the use of problem-focused coping strategies are protective factors for developing suicidal ideation. Prospective follow-up investigation is required to track the trajectories of suicidal ideation and behaviors as well as their predictors in relation to the subsequent course of COVID-19 pandemic and the post-pandemic era.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (HKU/HA HKW). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
WiC and CW designed and conceptualized the study. GW, JL, YS, JC, VF, and RC prepared the questionnaire assessment. HL and JC conducted the statistical analysis. HL wrote the first draft of the manuscript. HL, WiC, and JC interpreted the study data. WiC and HL revised and finalized the manuscript. All authors provided critical feedback to the manuscript and have approved the final manuscript.
Funding
The study was supported by the Hong Kong Research Grants Council (grant number: 10617014). Additional financial support to undertake this research was provided by the State Key Laboratory of Brain & Cognitive Sciences, the University of Hong Kong.
Acknowledgments
We thank the Hong Kong Public Opinion Research Institute to support the study. We are also grateful to the individuals who participated in the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1252600/full#supplementary-material.
Footnotes
References
1. World Health Organisation (WHO). Timeline: WHO’s COVID-19 response. (2020) Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline#! (Accessed December 18, 2022)
2. Blasco-Belled, A, Tejada-Gallardo, C, Fatsini-Prats, M, and Alsinet, C. Mental health among the general population and healthcare workers during the COVID-19 pandemic: a meta-analysis of well-being and psychological distress prevalence. Curr Psychol. (2022):1–12. doi: 10.1007/s12144-022-02913-6 [Epub ahead of print].
3. Dragioti, E, Li, H, and Tsitsas, G. A large-scale meta-analytic atlas of mental health problems prevalence during the COVID-19 early pandemic. J Med Virol. (2022) 94:1935–49. doi: 10.1002/jmv.27549
4. Ueda, M, Stickley, A, and Sueki, H. Mental health status of the general population in Japan during the COVID-19 pandemic. Psychiatry Clin Neurosci. (2020) 74:505–6. doi: 10.1111/pcn.13105
5. Cavicchioli, M, Ferrucci, R, and Guidetti, M. What will be the impact of the Covid-19 quarantine on psychological distress? Considerations based on a systematic review of pandemic outbreaks. Healthc. (2021) 9:101. doi: 10.3390/healthcare9010101
6. Kawohl, W, and Nordt, C. COVID-19, unemployment, and suicide. Lancet Psychiatry. (2020) 7:389–90. doi: 10.1016/S2215-0366(20)30141-3
7. Yao, H, Chen, J-H, and Xu, Y-F. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry. (2020) 7:e21–1. doi: 10.1016/S2215-0366(20)30090-0
8. Reger, MA, Stanley, IH, and Joiner, TE. Suicide mortality and coronavirus disease 2019—a perfect storm? JAMA Psychiatry. (2020) 77:1093–4. doi: 10.1001/jamapsychiatry.2020.1060
9. Zortea, TC, Brenna, CTA, Joyce, M, McClelland, H, Tippett, M, Tran, MM, et al. The impact of infectious disease-related public health emergencies on suicide, suicidal behavior, and suicidal thoughts: a systematic review. Crisis. (2021) 42:474–87. doi: 10.1027/0227-5910/a000753
10. Gunnell, D, Appleby, L, Arensman, E, Hawton, K, John, A, Kapur, N, et al. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. (2020) 7:468–71. doi: 10.1016/S2215-0366(20)30171-1
11. Secor, A, Macauley, R, Stan, L, Kagone, M, Sidikiba, S, Sow, S, et al. Mental health among Ebola survivors in Liberia, Sierra Leone and Guinea: results from a cross-sectional study. BMJ Open. (2020) 10:e035217. doi: 10.1136/bmjopen-2019-035217
12. Dubé, JP, Smith, MM, Sherry, SB, Hewitt, PL, and Stewart, SH. Suicide behaviors during the COVID-19 pandemic: a meta-analysis of 54 studies. Psychiatry Res. (2021) 301:113998. doi: 10.1016/j.psychres.2021.113998
13. Pathirathna, ML, Nandasena, HMRKG, Atapattu, AMMP, and Weerasekara, I. Impact of the COVID-19 pandemic on suicidal attempts and death rates: a systematic review. BMC Psychiatry. (2022) 22:506. doi: 10.1186/s12888-022-04158-w
14. Pirkis, J, Gunnell, D, Shin, S, Del Pozo-Banos, M, Arya, V, Aguilar, PA, et al. Suicide numbers during the first 9-15 months of the COVID-19 pandemic compared with pre-existing trends: An interrupted time series analysis in 33 countries. EClinicalMedicine. (2022) 51:101573. doi: 10.1016/j.eclinm.2022.101573
15. Chan, SMS, Chiu, FKH, Lam, CWL, Leung, PYV, and Conwell, Y. Elderly suicide and the 2003 SARS epidemic in Hong Kong. Int J Geriatr Psychiatry. (2006) 21:113–8. doi: 10.1002/gps.1432
16. Cheung, YT, Chau, PH, and Yip, PSF. A revisit on older adults suicides and severe acute respiratory syndrome (SARS) epidemic in Hong Kong. Int J Geriatr Psychiatry. (2008) 23:1231–8. doi: 10.1002/gps.2056
17. Burki, T. Hong Kong’s fifth COVID-19 wave—the worst yet. Lancet Infect Dis. (2022) 22:455–6. doi: 10.1016/S1473-3099(22)00167-0
18. Cheung, PHH, Chan, CP, and Jin, DY. Lessons learned from the fifth wave of COVID-19 in Hong Kong in early 2022. Emerg Microbes Infect. (2022) 11:1072–8. doi: 10.1080/22221751.2022.2060137
19. Lee, P. COVID-19 in data: 7 charts showing Hong Kong’s deadly omicron outbreak. Hong Kong Free Press HKFP (2022). Available at: https://hongkongfp.com/2022/03/12/covid-19-in-data-6-charts-showing-hong-kongs-deadly-omicron-outbreak/ (Accessed February 8, 2023)
20. Klonsky, ED, May, AM, and Saffer, BY. Suicide, suicide attempts, and suicidal ideation. Annu Rev Clin Psychol. (2016) 12:307–30. doi: 10.1146/annurev-clinpsy-021815-093204
21. Rossom, RC, Coleman, KJ, Ahmedani, BK, Beck, A, Johnson, E, Oliver, M, et al. Suicidal ideation reported on the PHQ9 and risk of suicidal behavior across age groups. J Affect Disord. (2017) 215:77–84. doi: 10.1016/j.jad.2017.03.037
22. Franklin, JC, Ribeiro, JD, Fox, KR, Bentley, KH, Kleiman, EM, Huang, X, et al. Risk factors for suicidal thoughts and behaviors: a meta-analysis of 50 years of research. Psychol Bull. (2017) 143:187–232. doi: 10.1037/bul0000084
23. Dolsen, EA, Nishimi, K, LeWinn, KZ, Byers, AL, Tripp, P, Woodward, E, et al. Identifying correlates of suicide ideation during the COVID-19 pandemic: a cross-sectional analysis of 148 sociodemographic and pandemic-specific factors. J Psychiatr Res. (2022) 156:186–93. doi: 10.1016/j.jpsychires.2022.10.009
24. Gratz, KL, Tull, MT, Richmond, JR, Edmonds, KA, Scamaldo, KM, and Rose, JP. Thwarted belongingness and perceived burdensomeness explain the associations of COVID-19 social and economic consequences to suicide risk. Suicide Life Threat Behav. (2020) 50:1140–8. doi: 10.1111/sltb.12654
25. McAuliffe, C, Pumarino, J, Thomson, KC, Richardson, C, Slemon, A, Salway, T, et al. Correlates of suicidal ideation related to the COVID-19 pandemic: repeated cross-sectional nationally representative Canadian data. SSM Popul Health. (2021) 16:100988. doi: 10.1016/j.ssmph.2021.100988
26. Shi, L, Que, J-Y, Lu, Z-A, Gong, Y-M, Liu, L, Wang, Y-H, et al. Prevalence and correlates of suicidal ideation among the general population in China during the COVID-19 pandemic. Eur Psychiatry. (2021) 64:e18. doi: 10.1192/j.eurpsy.2021.5
27. Farooq, S, Tunmore, J, Wajid Ali, M, and Ayub, M. Suicide, self-harm and suicidal ideation during COVID-19: a systematic review. Psychiatry Res. (2021) 306:114228. doi: 10.1016/j.psychres.2021.114228
28. Asmundson, GJ, Paluszek, MM, Landry, CA, Rachor, GS, McKay, D, and Taylor, S. Do pre-existing anxiety-related and mood disorders differentially impact COVID-19 stress responses and coping? J Anxiety Disord. (2020) 74:102271–1. doi: 10.1016/j.janxdis.2020.102271
29. Killgore, WD, Cloonan, SA, Taylor, EC, Allbright, MC, and Dailey, NS. Trends in suicidal ideation over the first three months of COVID-19 lockdowns. Psychiatry Res. (2020) 293:113390–11. doi: 10.1016/j.psychres.2020.113390
30. Antonelli-Salgado, T, Monteiro, GMC, Marcon, G, Roza, TH, Zimerman, A, Hoffmann, MS, et al. Loneliness, but not social distancing, is associated with the incidence of suicidal ideation during the COVID-19 outbreak: a longitudinal study. J Affect Disord. (2021) 290:52–60. doi: 10.1016/j.jad.2021.04.044
31. John, A, Lee, SC, Solomon, S, Crepaz-Keay, D, McDaid, S, Morton, A, et al. Loneliness, coping, suicidal thoughts and self-harm during the COVID-19 pandemic: a repeat cross-sectional UK population survey. BMJ Open. (2021) 11:e048123. doi: 10.1136/bmjopen-2020-048123
32. Riepenhausen, A, Veer, IM, Wackerhagen, C, Reppmann, ZC, Köber, G, Ayuso-Mateos, JL, et al. Coping with COVID: risk and resilience factors for mental health in a German representative panel study. Psychol Med. (2022) 53:3897–907. doi: 10.1017/S0033291722000563
33. Lo, HKY, Wong, GHS, Chan, JKN, Wong, CSM, Lei, JHC, So, YK, et al. COVID-19 perseverative cognition and depressive symptoms in Hong Kong: the moderating role of resilience, loneliness and coping strategies. J Affect Disord. (2023) 337:86–93. doi: 10.1016/j.jad.2023.05.058
34. Modelling the fifth wave of COVID-19 in Hong Kong (2022). Available at: https://www.med.hku.hk/en/news/press/media/DF5A2F6918764DC4B6517CE7B5F2796B.ashx (Accessed February 8, 2023).
35. García-Fernández, L, Romero-Ferreiro, V, and López-Roldán, PD. Mental health impact of COVID-19 pandemic on Spanish healthcare workers. Psychol Med. (2022) 52:195–7. doi: 10.1017/S0033291720002019
36. Roy, D, Tripathy, S, Kar, SK, Sharma, N, Verma, SK, and Kaushal, V. Study of knowledge, attitude, anxiety and perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J Psychiatry. (2020) 51:102083. doi: 10.1016/j.ajp.2020.102083
37. Wang, S, Zhang, Y, and Ding, W. Psychological distress and sleep problems when people are under interpersonal isolation during an epidemic: a nationwide multicenter cross-sectional study. Eur Psychiatry. (2020) 63:e77. doi: 10.1192/j.eurpsy.2020.78
38. HKPOP Panel - HKPORI. (2020). Available at: https://www.pori.hk/panel.html?lang=en (Accessed February 8, 2023)
39. Kroenke, K, Spitzer, RL, and Williams, JBW. The PHQ-9 validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
40. Yu, X, Tam, WW, Wong, PT, Lam, TH, and Stewart, SM. The patient health Questionnaire-9 for measuring depressive symptoms among the general population in Hong Kong. Compr Psychiatry. (2012) 53:95–102. doi: 10.1016/j.comppsych.2010.11.002
41. Spitzer, RL, Kroenke, K, Williams, JB, and Löwe, B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
42. Tong, X, An, D, McGonigal, A, Park, SP, and Zhou, D. Validation of the generalized anxiety Disorder-7 (GAD-7) among Chinese people with epilepsy. Epilepsy Res. (2016) 120:31–6. doi: 10.1016/j.eplepsyres.2015.11.019
43. Chen, JH, Tong, KK, Su, X, Yu, EW, and AMS, W. Measuring COVID-19 related anxiety and obsession: validation of the coronavirus anxiety scale and the obsession with COVID-19 scale in a probability Chinese sample. J Affect Disord. (2021) 295:1131–7. doi: 10.1016/j.jad.2021.08.104
44. Lee, SA. How much “thinking” about COVID-19 is clinically dysfunctional? Brain Behav Immun. (2020) 87:97–8. doi: 10.1016/j.bbi.2020.04.067
45. Bastien, CH, Vallières, A, and Morin, CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. (2001) 2:297–307. doi: 10.1016/S1389-9457(00)00065-4
46. Yeung, WF, Chung, KF, Zhang, SP, Yap, TG, and Law, AC. Electroacupuncture for primary insomnia: a randomized controlled trial. Sleep. (2009) 32:1039–47. doi: 10.1093/sleep/32.8.1039
47. Papadopoulou, A, Efstathiou, V, Yotsidi, V, Pomini, V, Michopoulos, I, Markopoulou, E, et al. Suicidal ideation during COVID-19 lockdown in Greece: prevalence in the community, risk and protective factors. Psychiatry Res. (2021) 297:113713. doi: 10.1016/j.psychres.2021.113713
48. Carver, CS. You want to measure coping but your protocol’s too long: consider the brief COPE. Int J Behav Med. (1997) 4:92–100. doi: 10.1207/s15327558ijbm0401_6
49. Ye, S. A longitudinal study of subjective well-being among Chinese university students: The roles of personality, attribution, and coping. Doctoral Thesis, Hong Kong: University of Hong Kong (2008).
50. Dias, C, Cruz, JF, and Fonseca, AM. The relationship between multidimensional competitive anxiety, cognitive threat appraisal, and coping strategies: a multi-sport study. Int J Sport Exerc Psychol. (2012) 10:52–65. doi: 10.1080/1612197X.2012.645131
51. Hughes, ME, Waite, LJ, Hawkley, LC, and Cacioppo, JT. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging. (2004) 26:655–72. doi: 10.1177/0164027504268574
52. Liu, T, Lu, S, Leung, DKY, Sze, LCY, Kwok, WW, Tang, JYM, et al. Adapting the UCLA 3-item loneliness scale for community-based depressive symptoms screening interview among older Chinese: a cross-sectional study. BMJ Open. (2020) 10:e041921. doi: 10.1136/bmjopen-2020-041921
53. Hsin, YZ. Reliability and validity of the brief resilience scale. Master thesis, Taiwan: National Pingtung University (2020).
54. Smith, BW, Dalen, J, Wiggins, K, Tooley, E, Christopher, P, and Bernard, J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. (2008) 15:194–200. doi: 10.1080/10705500802222972
55. Podsakoff, PM, Mac Kenzie, SB, Lee, J-Y, and Podsakoff, NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol. (2003) 88:879–903. doi: 10.1037/0021-9010.88.5.879
56. Moitra, M, Santomauro, D, Degenhardt, L, Collins, PY, Whiteford, H, Vos, T, et al. Estimating the risk of suicide associated with mental disorders: a systematic review and meta-regression analysis. J Psychiatr Res. (2021) 137:242–9. doi: 10.1016/j.jpsychires.2021.02.053
57. Xu, YE, Barron, DA, Sudol, K, Zisook, S, and Oquendo, MA. Suicidal behavior across a broad range of psychiatric disorders. Mol Psychiatry. (2023) 28:2764–810. doi: 10.1038/s41380-022-01935-7
58. Oquendo, MA, Galfalvy, H, Russo, S, Ellis, SP, Grunebaum, MF, Burke, A, et al. Prospective study of clinical predictors of suicidal acts after a major depressive episode in patients with major depressive disorder or bipolar disorder. Am J Psychiatry. (2004) 161:1433–41. doi: 10.1176/appi.ajp.161.8.1433
59. Sokero, TP, Melartin, TK, Rytsälä, HJ, Leskelä, US, Lestelä-Mielonen, PS, and Isometsä, ET. Prospective study of risk factors for attempted suicide among patients with DSM–IV major depressive disorder. Br J Psychiatry. (2005) 186:314–8. doi: 10.1192/bjp.186.4.314
60. Ettman, CK, Cohen, GH, Abdalla, SM, Sampson, L, Trinquart, L, Castrucci, BC, et al. Persistent depressive symptoms during COVID-19: a national, population-representative, longitudinal study of U.S. adults. Lancet Reg Health Am. (2022) 5:100091. doi: 10.1016/j.lana.2021.100091
61. Moutier, C. Suicide prevention in the COVID-19 era: transforming threat into opportunity. JAMA Psychiatry. (2021) 78:433–8. doi: 10.1001/jamapsychiatry.2020.3746
62. Snoswell, CL, Chelberg, G, De Guzman, KR, Haydon, HH, Thomas, EE, Caffery, LJ, et al. The clinical effectiveness of telehealth: a systematic review of meta-analyses from 2010 to 2019. J Telemed Telecare. (2023) 29:669–84. doi: 10.1177/1357633X211022907
63. Abraham, A, Jithesh, A, Doraiswamy, S, Al-Khawaga, N, Mamtani, R, and Cheema, S. Telemental health use in the COVID-19 pandemic: a scoping review and evidence gap mapping. Front Psych. (2021) 12:748069. doi: 10.3389/fpsyt.2021.748069
64. Zangani, C, Ostinelli, EG, Smith, KA, Hong, JSW, Macdonald, O, Reen, G, et al. Impact of the COVID-19 pandemic on the global delivery of mental health services and telemental health: systematic review. JMIR Ment Health. (2022) 9:e38600. doi: 10.2196/38600
65. Ong, E, and Thompson, C. The importance of coping and emotion regulation in the occurrence of suicidal behavior. Psychol Rep. (2019) 122:1192–210. doi: 10.1177/0033294118781855
66. Horwitz, AG, Hill, RM, and King, CA. Specific coping behaviors in relation to adolescent depression and suicidal ideation. J Adolesc Lond Engl. (2011) 34:1077–85. doi: 10.1016/j.adolescence.2010.10.004
67. Svensson, T, Inoue, M, Charvat, H, Sawada, N, Iwasaki, M, Sasazuki, S, et al. Coping behaviors and suicide in the middle-aged and older Japanese general population: the Japan public health center-based prospective study. Ann Epidemiol. (2014) 24:199–205. doi: 10.1016/j.annepidem.2013.12.006
68. Luthar, SS. Resilience in development: A synthesis of research across five decades. Developmental psychopathology. Hoboken, NJ, USA: John Wiley & Sons, Inc. (2015).
69. Anyan, F, Worsley, L, and Hjemdal, O. Anxiety symptoms mediate the relationship between exposure to stressful negative life events and depressive symptoms: a conditional process modelling of the protective effects of resilience. Asian J Psychiatry. (2017) 29:41–8. doi: 10.1016/j.ajp.2017.04.019
70. Havnen, A, Anyan, F, Hjemdal, O, Solem, S, Riksfjord, MG, and Hagen, K. Resilience moderates negative outcome from stress during the COVID-19 pandemic: a moderated mediation approach. Int J Environ Res Public Health. (2020) 17:6461. doi: 10.3390/ijerph17186461
71. Johnson, J, Wood, AM, Gooding, P, Taylor, PJ, and Tarrier, N. Resilience to suicidality: the buffering hypothesis. Clin Psychol Rev. (2011) 31:563–91. doi: 10.1016/j.cpr.2010.12.007
72. Sher, L. Resilience as a focus of suicide research and prevention. Acta Psychiatr Scand. (2019) 140:169–80. doi: 10.1111/acps.13059
73. McClelland, H, Evans, JJ, Nowland, R, Ferguson, E, and O’Connor, RC. Loneliness as a predictor of suicidal ideation and behaviour: a systematic review and meta-analysis of prospective studies. J Affect Disord. (2020) 274:880–96. doi: 10.1016/j.jad.2020.05.004
74. Smith, KJ, and Victor, C. Typologies of loneliness, living alone and social isolation, and their associations with physical and mental health. Ageing Soc. (2019) 39:1709–30. doi: 10.1017/S0144686X18000132
75. Hawkley, LC, and Cacioppo, JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med. (2010) 40:218–27. doi: 10.1007/s12160-010-9210-8
76. Shaw, RJ, Cullen, B, Graham, N, Lyall, DM, Mackay, D, Okolie, C, et al. Living alone, loneliness and lack of emotional support as predictors of suicide and self-harm: a nine-year follow up of the UK biobank cohort. J Affect Disord. (2021) 279:316–23. doi: 10.1016/j.jad.2020.10.026
77. Tso, IF, and Park, S. Alarming levels of psychiatric symptoms and the role of loneliness during the COVID-19 epidemic: a case study of Hong Kong. Psychiatry Res. (2020) 293:113423. doi: 10.1016/j.psychres.2020.113423
78. Rosenberg, AR. Cultivating deliberate resilience during the coronavirus disease 2019 pandemic. JAMA Pediatr. (2020) 174:817–8. doi: 10.1001/jamapediatrics.2020.1436
79. Ke, GN, Grajfoner, D, Wong, RMM, Carter, S, Khairudin, R, Lau, WY, et al. Building the positive emotion-resilience-coping efficacy model for COVID-19 pandemic. Front Psychol. (2022) 13:764811. doi: 10.3389/fpsyg.2022.764811
80. Hamrouni, AM, Sharif, RS, Sharif, SI, Hassanein, MM, and Abduelkarem, AR. Impacts of COVID-19 pandemic on geopolitics, health, economics, education and sociocultural events. Risk Manag Healthc Policy. (2022) 15:935–43. doi: 10.2147/RMHP.S362337
81. Jaspal, R, and Breakwell, GM. Socio-economic inequalities in social network, loneliness and mental health during the COVID-19 pandemic. Int J Soc Psychiatry. (2022) 68:155–65. doi: 10.1177/0020764020976694
82. Rotenstein, LS, Ramos, MA, Torre, M, Segal, JB, Peluso, MJ, Guille, C, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA. (2016) 316:2214–36. doi: 10.1001/jama.2016.17324
83. Andreotti, ET, Ipuchima, JR, and Cazella, SC. Instruments to assess suicide risk: a systematic review. Trends Psychiatry Psychother. (2020) 42:276–81. doi: 10.1590/2237-6089-2019-0092
Keywords: suicidal ideation, COVID-19, survey, coping strategies, pre-existing mental disorders, loneliness
Citation: Lo HKY, Chan JKN, Wong CSM, Wong GHS, Lei JHC, So YK, Fung VSC, Chu RST, Ling R, Chung AKK, Lee KCK, Cheng CPW, Chan WC and Chang WC (2024) Prevalence and correlates of suicidal ideation in the general public during the fifth wave of COVID-19 pandemic in Hong Kong. Front. Psychiatry. 14:1252600. doi: 10.3389/fpsyt.2023.1252600
Edited by:
Ondrej Holy, Palacký University Olomouc, CzechiaReviewed by:
Andrea Amerio, University of Genoa, ItalyMarko Ćurković, Sveučilišta u Zagrebu, Croatia
Copyright © 2024 Lo, Chan, Wong, Wong, Lei, So, Fung, Chu, Ling, Chung, Lee, Cheng, Chan and Chang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wing Chung Chang, Y2hhbmd3Y0Boa3UuaGs=
 Heidi Ka Ying Lo
Heidi Ka Ying Lo Joe Kwun Nam Chan
Joe Kwun Nam Chan Corine Sau Man Wong
Corine Sau Man Wong Gabbie Hou Sem Wong
Gabbie Hou Sem Wong Janet Hiu Ching Lei1
Janet Hiu Ching Lei1 Rachel Ling
Rachel Ling Albert Kar Kin Chung
Albert Kar Kin Chung Calvin Pak Wing Cheng
Calvin Pak Wing Cheng Wai Chi Chan
Wai Chi Chan Wing Chung Chang
Wing Chung Chang