
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
COMMUNITY CASE STUDY article
Front. Psychiatry , 16 November 2023
Sec. Public Mental Health
Volume 14 - 2023 | https://doi.org/10.3389/fpsyt.2023.1252037
This article is part of the Research Topic Pediatric Integrated Care: From Vision to Practice View all 8 articles
 Jason Schweitzer1,2*
Jason Schweitzer1,2* Anne Bird1,2
Anne Bird1,2 Hilary Bowers1,2,3
Hilary Bowers1,2,3 Nicole Carr-Lee2
Nicole Carr-Lee2 Josh Gibney1,2
Josh Gibney1,2 Kriston Schellinger2
Kriston Schellinger2 Jasmine R. Holt2†
Jasmine R. Holt2† Devin P. Adams2
Devin P. Adams2 Domonique J. Hensler2
Domonique J. Hensler2 Kathryn Hollenbach2,4†
Kathryn Hollenbach2,4†Introduction: Children and adolescents often do not receive mental healthcare when they need it. By 2021, the complex impact of the COVID-19 pandemic, structural racism, inequality in access to healthcare, and a growing shortage of mental health providers led to a national emergency in child and adolescent mental health in the United States. The need for effective, accessible treatment is more pressing than ever. Interdisciplinary, team-based pediatric integrated mental healthcare has been shown to be efficacious, accessible, and cost-effective.
Methods: In response to the youth mental health crisis, Rady Children’s Hospital-San Diego’s Transforming Mental Health Initiative aimed to increase early identification of mental illness and improve access to effective treatment for children and adolescents. A stakeholder engagement process was established with affiliated pediatric clinics, community mental health organizations, and existing pediatric integrated care programs, leading to the development of the Primary Care Mental Health Integration program and drawing from established models of integrated care: Primary Care Behavioral Health and Collaborative Care.
Results: As of 2023, the Primary Care Mental Health Integration program established integrated care teams in 10 primary care clinics across San Diego and Riverside counties in California. Measurement-based care has been implemented and preliminary results indicate that patient response to therapy has resulted in a 44% reduction in anxiety symptoms and a 62% decrease in depression symptoms. The program works toward fiscal sustainability via fee-for-service reimbursement and more comprehensive payor contracts. The impact on patients, primary care provider satisfaction, measurement-based care, funding strategies, as well as challenges faced and changes made will be discussed using the lens of the Reach, Effectiveness, Adoption, Implementation and Maintenance framework.
Discussion: Preliminary results suggest that the Primary Care Mental Health Integration is a highly collaborative integrated care model that identifies the needs of children and adolescents and delivers brief, evidence informed treatment. The successful integration of this model into 10 primary care clinics over 3 years has laid the groundwork for future program expansion. This model of care can play a role addressing youth mental health and increasing access to care. Challenges, successes, and lessons learned will be reviewed.
The United States (US) faces a youth mental health crisis. Rates of childhood depression and anxiety are increasing. Emergency room visits for mental health crises, suicidal ideation and attempted or completed suicides are also rising (1, 2). Although the COVID-19 pandemic played a role in exacerbating these trends (3), childhood mental health concerns were increasing even prior to 2019.
Between 2007 and 2018, the US saw a 57% increase in suicide completion among people aged 10–24 years (4). Isolation, trauma, bullying, unsafe environments, lack of adequate medical and mental health insurance, as well as relationship issues, have all been associated with adverse mental health symptoms (5, 6). Public attention concerning the negative impact of social media on mental health has been increasing (2). Although the deleterious influence of structural racism is difficult to measure, it is impossible to ignore as rates of suicide from 2003 to 2017 disproportionately increased among African American girls aged 15–17 years (6), and racial minorities continue to face significant barriers to healthcare (7–9).
As rates of mental health symptoms are increasing (10), there is greater awareness of the impact of mental health challenges and of effective interventions. The negative impact of traumatic experiences has been clearly described (11, 12), and psychotherapeutic and psychopharmacologic interventions can decrease trauma related symptoms (13). Interventions to treat anxiety and depressive symptoms are similarly effective (14, 15). Despite this knowledge, inadequate access to care continues to be persistent and widespread (2). Integrated care, or mental healthcare provided or initiated in the primary care setting, can reduce cost and improve mental health outcomes in adults (16), and bridge gaps in mental healthcare for children and adolescents.
In a 2022 American Academy of Child and Adolescent Psychiatry (AACAP) literature review, integrated care for children and adolescents was found to be effective and work best when delivered by a multi-disciplinary team (17). According to the Substance Abuse and Mental Health Services Administration (SAMHSA) the “most collaborative” integrated care model will “function as an integrated team” at “system, team and individual levels,” follows a “shared concept of team care,” and establishes formal meeting processes with “roles and cultures that blur and blend” (SAMHSA/HRSA Center for Integrated Health Solutions, pg. 10, 2020) (18).
Primary Care Behavioral Health (PCBH) (19) and Collaborative Care (CoCM) (20, 21) are well-established integrated care models that employ high levels of collaboration. PCBH is described using the “GATHER” (Generalist, Access, Team-based, High Volume, Education and Routine) acronym (22). In PCBH, licensed mental health clinicians are embedded in the primary care office and work closely with the Primary Care Providers (PCPs). This model has been shown to be effective for children and adolescents, (23) and may reduce costs (24), but more pediatric research is needed. CoCM was initially designed to treat specific mental health conditions, such as depression, in defined patient populations, and differs from the generalist approach in PCBH that readily encourages the mental health provider to treat a range of concerns. In CoCM, a care manager (often called the Depression Care Manager or DCM) provides therapy and helps that patient navigate treatment options. A psychiatrist provides consultation and guidance to PCPs and DCMs. CoCM models often follow algorithmic approaches treatment, such that Measurement Based Care (MBC) scores prompt changes in treatment (e.g., worse scores may trigger a medication change). The Reaching out to Adolescents in Distress (ROAD) intervention (20) is an adolescent CoCM program adapted from the Improving Mood Promoting Access to Collaborative Treatment (IMPACT) model (25), that showed greater reductions in depression symptoms and rates of remission when compared to control youth.
The US medical system has historically separated mental and physical healthcare (26). This division of care has resulted in mental and physical health developing into separate subsystems, each with their own unique workflow practices, attitudes, expectations and reimbursement mechanisms. Pediatric primary care providers often provide care to 20–30 patients per day, with visit lengths of 15–20 min. PCPs also provide patient advice via telephone or electronic health record (EHR) messaging and complete school, camp, government, and insurance forms. Many pediatricians do not feel they have adequate time or knowledge to treat the mental health concerns of their patients, and, as a result, refer to outside mental health providers, where timely care is often not available. Non-integrated mental health clinics and training programs do not offer learning opportunities to fully prepare for the fast pace of the primary care office. As a result many therapists do not have experience adopting a brief, efficient communication style, which may be necessary to jointly develop treatment plans with PCPs in the primary care setting. The differences between mental and physical healthcare inherent in the US provide important context for understanding the complexities of integrated care.
In response to the youth mental health crisis, Rady Children’s Hospital-San Diego created the Transforming Mental Health Initiative (TMH) to work toward prevention, early identification and treatment of youth mental health concerns through mental health integration, research, education, and advocacy.
In 2019, TMH convened several stakeholder meetings with local leaders and experts in community mental health, pediatrics, and integrated care to help develop plans for a significant mental health intervention. Concurrently, TMH clinical leaders completed site visits with three separate institutions with extensive integrated care experience and evaluated the rates of mental health-related emergency room visits and inpatient stays. Hospital leadership, donor relations teams, and committed donors were also engaged in the review of this information. The result of this stakeholder engagement process led TMH to propose the creation of a new Primary Care Mental Health Integration (PCMHI) program to increase early identification of mental health issues, improve access to care, and prevent the development of severe symptoms that could lead to the utilization of emergency services and significant morbidity and mortality (2).
To create PCMHI, partnerships with existing hospital-affiliated primary care practices in San Diego and Riverside counties were established, including Children’s Primary Care Medical Group (CPCMG), the second largest pediatric primary care medical group in the US. Primary care practices were identified and selected as partners based on electronic health record compatibility, existing mental healthcare infrastructure (e.g., established PHQ-9A screening at well child visits for youth aged 12 years and older), and their shared commitment to providing primary care level mental health interventions (such as PCP medication management for non-comorbid mild symptoms of depression, anxiety, or attention deficit hyperactivity disorder). Administrative leadership from TMH and the affiliated primary care sites agreed to a series of shared objectives, including: (1) increasing access to timely care; (2) using evidence-based approaches; and (3) committing to clear, open communication between PCPs and mental health providers involved in delivering integrated mental healthcare.
Team member roles (Table 1) were developed with input from primary care and mental health disciplines. PCMHI primary care partners committed to participating in ongoing continuing medical education on the management of common mental health conditions in the primary care setting. They also agreed to participate in joint decision making with patients and families on mental health treatment, offer guidance in accessing therapy, and provide psychopharmacology for mild, non-comorbid conditions.
TMH developed a pre- and post-implementation survey to assess PCP’s beliefs and attitudes about mental health integration and the impact of PCMHI on their day-to-day patient care. Surveys were provided online to each PCP before the PCMHI program start date at their clinic. Providers received two follow up surveys at 4 months and 8 months post PCMHI program initiation.
PCMHI is structured to achieve the triple aim of improved health outcomes, reduced healthcare utilization and cost, and improved patient and provider satisfaction. The program embeds therapists in partnering primary care pediatrics practices. PCMHI focuses on early identification of mental health concerns, as well as treatment for those with mild to moderate clinical presentations. It provides short-term, evidence-based treatment, working closely with primary care providers in the medical home. PCMHI also works to promote mental health screening and reduce stigma around talking about mental health in order to identify mental health challenges early, and deliver timely access to treatment to decrease symptoms and prevent clinical worsening and / or mental health crises.
PCMHI provides a continuum of care utilizing a “hub and spoke” model. “Spokes” represent the primary care pediatric sites with embedded therapists, referred to as Integrated Health Therapists (IHTs). “Hubs” represent regional, free standing mental and behavioral health clinics for higher acuity cases that may require longer term therapy or psychiatric support.
PCMHI services begin in the primary care setting where PCPs initiate referrals to the IHT if a patient or family member expresses a mental health need, the PCP is concerned there may be a mental health need contributing to a current visit, or a screening measure identifies a potential mental health concern (e.g., PHQ-9A score of 5 or higher) and the provider deems the referral appropriate. In ideal circumstances, IHTs are introduced to patients via warm handoffs from PCPs. IHTs provide brief, evidence-based therapies delivered over a series of 1–6 sessions (Table 2).
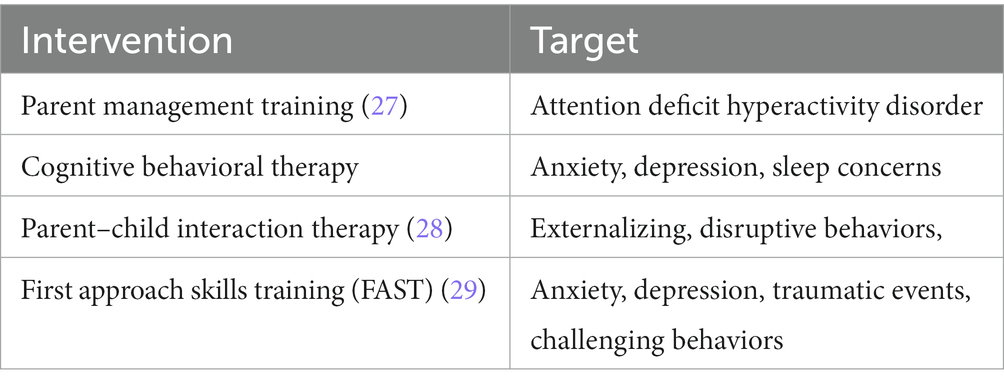
Table 2. Evidence informed interventions employed by integrated health therapists in the primary care mental health integration program.
Hub IHTs, psychiatrists, and care coordinators work at regional Hubs. Hub IHTs provide 10–12 therapy sessions and psychiatrists offer assessment and brief treatment over a course of 4–6 sessions. Patients seen at Hub sites may receive therapy, psychiatry, or both services. Care coordinators provide community resources and referrals to PCMHI patients who require ongoing care after completing Hub treatment sessions, or who have more complex disease. Spokes are staffed with approximately one IHT and Hubs with two to four. Telemedicine can be utilized for remote care coordination, therapy and psychiatry when preferred by the patient and clinically appropriate. IHTs in both practice settings work closely with the family to better understand patient needs and to support the family.
PCMHI blends elements of PCBH and CoCM to balance primary care needs (high volumes of patients who need to be seen quickly) and the capacities of mental health providers (who benefit from support by psychiatry to triage patients effectively, while continuing to see high volumes for brief intervention), as well as foster shared decision making for patient care. Similar to PCBH, PCMHI emphasizes a generalist approach (IHTs accept any mental health referral); access to care (IHT schedules are optimized to encourage same day introduction to PCMHI services through warm handoffs); and education (see section 3.6). PCBH elements have been essential in helping IHTs adjust to the fast pace of the primary care office and allowing PCMHI to support all patients and families in the clinic who need mental healthcare, not just specific sub-populations or patients with specific diagnoses (a potential limitation of CoCM).
PCMHI also employs several CoCM components, including routine measurement-based care (see section 3.7), weekly interdisciplinary team meetings (registry conferences) and the presence of a consulting psychiatrist on the team. These components help PCMHI engage in quality improvement through analysis of MBC data (though PCMHI does not use stepped algorithmic care per se), improve teamwork, and blend PCP and mental health cultures through layered communication. Presence of psychiatry also allows PCMHI to support PCPs in their medication management practice through brief psychiatric consultation, teaching or “curbside” feedback in a registry conference.
By blending the PCBH and CoCM models, PCMHI aims to provide highly collaborative, multidisciplinary team-oriented care (SAMHSA/HRSA Center for Integrated Health Solutions, 2020). Without the PCBH generalist approach and emphasis on access, PCMHI would not be able to share care for the wide range of presentations common to primary care. Without the PCBH commitment to education, PCMHI would likely not be able to maintain the workforce. Without CoCM inspired registry conferences, team communication deteriorates. Without psychiatric input and guidance, modeled after CoCM, the team’s capacity to operate at the top of their respective licenses may diminish. These elements allow PCMHI to more effectively help pediatric patients with mild to moderate mental health symptoms maintain their care within their PCP office, while still serving patients experiencing more severe symptoms, either by stabilizing them at the Hub, or bridging their care until they can be connected to higher level, specialty services outside the program. PCMHI does not provide ongoing care for clinical presentations that require specialty mental health (primary psychotic illnesses or bipolar disorder, or cases that require in-home services or partial hospital level of care), but can provide brief interventions and / or advocacy to help connect families with the services they need.
Even with clearly defined team roles, consistent communication between PCPs and mental health providers is essential to ensure patients receive coordinated, high-quality care. Clear communication is especially important with transitions of care or in cases of atypical presentations. PCMHI has developed a range of protocols to strengthen communication.
Team communication begins with the warm handoff. The Agency for Healthcare Research and Quality defines a warm handoff as “a transfer of care between two members of the healthcare team… [that] occurs in front of the patient and family… [allowing] patients and families to hear what is said…giving them the opportunity to clarify or correct information or ask questions about their care.” (30). This interaction is hypothesized to increase engagement in subsequent services (31). Evidence on the impact of warm handoffs for mental healthcare is not entirely clear. One study found warm hand offs to be less effective for adult primary care patients whose primary language was Spanish (32). On the other hand, a systematic review of warm handoffs found increased patient engagement in services (33). The evidence specific to pediatric primary care is narrow, though Peters and colleagues found a correlation between warm handoffs and an increase from 51 to 78% in first appointment show rates (34). Another study on pediatric warm handoffs found an association with improved patient engagement, fewer no-shows and cancelations, shorter time between referral and initial scheduled mental health visit, and more total mental health visits (35).
The warm handoff leverages the PCP’s relationship with the patient and family to address mental health concerns in a trusted and judgement-free environment. PCPs participating in PCMHI are trained to follow the PCMHI-developed CHATS framework [Convene, History, Assessment, Triage, Safety (Figure 1)]. Following CHATS, the PCP, family, and IHT convene together in the PCP exam room to discuss, in a non-judgmental way, relevant background information and history for future PCMHI care. The PCP openly shares their assessment of the patient’s clinical presentation and their belief that PCMHI services may benefit the patient’s care. The PCP may then leave the exam room, allowing the IHT to further assess and triage the presenting concern and discuss treatment options, including the recommended length of care (see section 3.2). The IHT reviews program expectations and agrees upon an initial care plan with the family. The IHT may also perform a safety evaluation, provide supplemental information (e.g., emergency resources), and schedule an intake if indicated. Following the CHATS framework insures information is communicated in a concise, informative, and patient-centered fashion.

Figure 1. ‘CHATS’ mnemonic used to describe and standardize elements of a Warm Handoffs in MHI affiliated pediatrics office.
Additional interdisciplinary communication is formalized to maintain and encourage collaboration. Each primary care clinic identifies a PCP site lead. Site leads help facilitate communication between the PCPs at the clinic site and PCMHI clinicians. They provide real-time feedback regarding team roles and workflows and encourage their colleagues to refer eligible patients to PCMHI via the CHATS protocol. Monthly PCP site lead meetings with PCMHI leadership also serve as venue for open communication. Each primary care site holds a weekly 30–60 min registry conference, a forum for PCPs, psychiatrists, IHTs and care coordinators to discuss cases and address questions that may require input from each other’s disciplines. While not all PCPs are able to attend on a weekly basis, PCP site leads attend all registry meetings and can address or delegate questions requiring PCP input. Registry conferences also address transitions of care, which may include referrals to community services due to acuity, referrals for short-term psychiatric management, returning psychopharmacologic management to primary care. For lower acuity cases, PCPs can request real-time psychiatric feedback regarding psychopharmacologic care.
The shared EHR is used to enhance communication. IHTs use EHR messaging to provide initial clinical updates to PCPs, and over time, may use messages to coordinate treatment plans or transition care with the PCP or psychiatrist. Psychiatrists use messaging for every visit to ensure the PCP is aware of diagnostic findings or psychopharmacologic course.
Same day access to mental health services is essential to the PCMHI model. When a PCP (through screeners or clinical interaction), patient or a family member identifies a mental health concern, the PCP may initiate a warm handoff. IHT schedule templates are designed to allow for warm handoffs throughout the day to insure same day access to care. Scheduling initial intakes following warm handoff visits is a priority, and the first available appointment generally occurs within 1–2 weeks due to the time needed to obtain insurance authorization.
Integrated care can be unfamiliar to mental health clinicians. Ongoing training and education around integrated care has helped therapist on-board and orient to PCMHI. This is accomplished through bi-weekly, CME-eligible talks on integrated health topics delivered by PCMHI clinicians to their colleagues. IHTs also meet regularly with clinical supervisors to discuss integrated care, logistical challenges, strategies for interdisciplinary communication, and clinical considerations for brief treatment. To support PCPs in their adoption of PCMHI, onboarding procedures to orient new providers to the program model have been developed. PCMHI has also partnered with an outside educational program to provide interested PCPs with a two-day in-depth training on the assessment and treatment of common mental health disorders.
For integrated care models to be sustainable and more widely adopted, PCMHI believes their benefits must be taught to future mental health providers and pediatricians. Every year, PCMHI trains 4–10 pediatric residents via a two-week integrated care elective that includes clinical observation and didactic sessions. The program also trains four child and adolescent psychiatry fellows per academic year through a year-long outpatient rotation, which includes 8 h per week of direct clinical care and 2 hours of didactic training per month. Additionally, the program recently became a training site for two psychology pre-doctoral interns.
Measurement based care is another core component of PCMHI. TMH has been committed to using MBC data from the outset to understand the impact of PCMHI on patients and to guide the future direction of the model’s implementation. IHTs and psychiatrists complete the Clinical Global Impressions (CGI) scale for all mental health visits. Depending on the age of the patient, patient-completed standardized tools are also used, including the Patient Health Questionnaire 9 Adolescent version (PHQ-9A), Generalized Anxiety Disorder-7 (GAD-7) and Patient Symptom Checklist-17 (PSC-17). The results of these scales help guide therapeutic interventions or transitions of care and are discussed during treatment team meetings and registry conferences to support clinical decision making. Table 3. provides an overview of the MBC screening tools used by PCMHI.
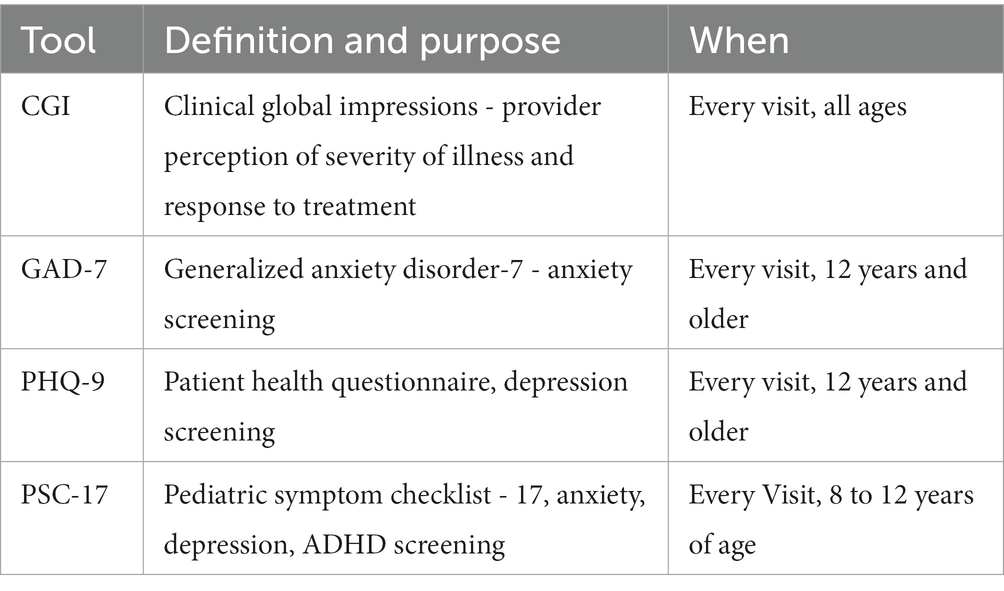
Table 3. Patient scheduled measurement based care screening tools, primary care mental health integration program.
Researchers, clinicians, and grant writers use the Reach, Effectiveness, Adoption, Implementation and Maintenance (RE-AIM) framework to evaluate the impact of behavioral health programs (36, 37). Established in 1999 (38), RE-AIM can be applied to program evaluation, grant writing and quality improvement. In the following section, multiple dimensions of PCMHI will be discussed through the lens of RE-AIM (39).
Since its inception in 2020, PCMHI has expanded from 1 to 10 pediatric primary care clinics and has established four Hub sites across San Diego and Riverside counties. Each clinic has unique demographics, with patient populations ranging from 2,000 to 15,000, and a distinct payor mix that includes both Medicaid (public) and commercial (private) insurances. As of 2023, PCMHI has completed 25,828 patient encounters, including 3,544 warm handoffs, 1,893 virtual triage appointments, 3,980 initial evaluations and 16,404 follow-up visits. Of the above visits, 807 were psychiatry initial evaluations and 3,824 were psychiatry follow-up appointments.
Referrals to PCMHI come directly from PCPs, and there are no fixed exclusion criteria for a referral. Each case is reviewed by a licensed clinician (IHT, clinical supervisor, or psychiatrist) and, if clinical circumstances dictate (e.g., known bipolar disorder, schizophrenia, primary substance abuse disorder), the patient may be referred to community mental health resources for specialty-level care.
PCMHI has relied on patient volume, time to initial appointment, MBC, and provider and patient satisfaction data to measure the effectiveness of the model on access to care and patient outcomes. Clinically, MBC data indicates that patient response to therapy has resulted in a 44% reduction in anxiety symptoms, as measured by the GAD-7, and a 62% decrease in depression symptoms, as assessed by the PHQ-9A. Additional measures, including the CGI Scale for all patients and PSC-17 data for patients less than 12 years of age, have shown preliminary decreases, but the individual domain analyses have not yet been completed.
Results from pre- and post-implementation provider satisfaction surveys, which incorporated feedback from the first five clinic locations to implement PCMHI (a total of 30 PCPs), were encouraging. Prior to participating in PCMHI, many PCPs strongly disagreed that their patients had timely access to behavioral healthcare, but after program implementation, their ratings increased significantly. PCP responses also revealed a strong belief from the start in the potential of mental health integration to ease their workload and increase their capacity to treat their patients more effectively.
Eleven primary care clinics were offered, and initially adopted, every aspect of the PCMHI program. Four hub sites were initiated. Since PCMHI’s start in 2020, one primary care clinic has discontinued its participation in the program (described in section 3.5).
Financing integrated care comes with unique challenges. The separation of medical and mental health reimbursement has resulted in a knowledge gap vis-à-vis mental health services in health system-based and primary care settings. Freeman and colleagues argue that the financial viability of integrated care depends on specific, regional funding environments (40). They recommend several steps toward sustainability, including exploring legal requirements specific to state and clinic type, contacting payors regarding integrated care options, building a workforce with appropriate provider licenses, and establishing a business plan and capacity to audit clinical and fiscal outcomes. These recommendations influenced PCMHI’s fiscal development and have helped lay the groundwork for long-term financial sustainability.
PCMHI was started through a philanthropic donation, and is funded through a combination of philanthropy, net patient revenue and institutional support. PCMHI bills fee-for-service, and continues to seek and create opportunities for additional pay structures, including exploring value-based payments, making more effective use of available billing codes (e.g., codes for interdisciplinary meetings, para-professional services rendered, community health workers/care coordination services), and seeking grant opportunities. CoCM codes have not been used, as the structure of the registry conference has not predictably met core components for billing (41). Table 4. outlines the most billed CPT codes for PCMHI services.
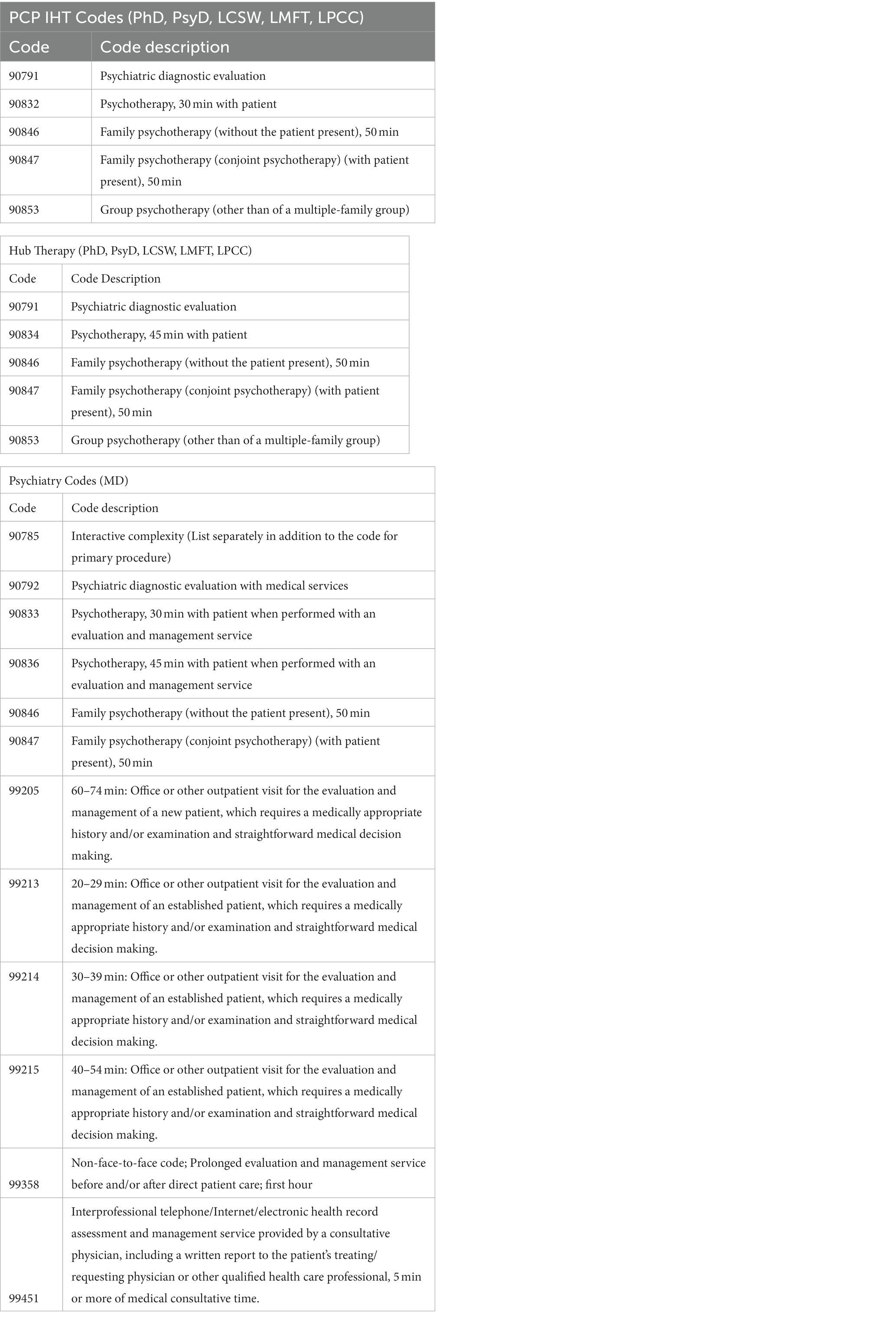
Table 4. Most prevalent CPT codes reported by therapists, primary care mental health integration program.
There have been several adjustments to the model since inception. To increase the rates of warm handoffs, PCMHI has added PCP on-boarding trainings, increased data sharing about rates of warm handoffs, and offered yearly, site specific re-trainings on warm handoffs. To increase registry attendance, several clinics elected to alter timing or length. Educational sessions have been augmented to include CME to attract more PCPs. The MBC schedule has been altered to simplify collection (previously, MBC was offered at initial, 2 months and completion of services, but this resulted in inconsistent collection) and may continue to be adjusted, if there is evidence that the rate is too high.
As of 2023, 10 out of the 11 primary care sites that initially adopted the PCMHI program continue to offer the program. One site was discontinued as an IHT “spoke” due to a mismatch with primary care expectations around PCMHI limitations on length of care. While it is understandable that PCPs want access to longer term services for their patients, PCMHI remains committed to short-term, evidence-based interventions to increase access to timely, effective care. PCMHI relies on care coordination to connect higher acuity patients to specialty services. This highlights the challenges with maintaining model fidelity and the importance of clear communication around program expectations between PCMHI and PCP site leadership. As a result of this experience, PCMHI developed additional trainings for current and new PCP sites focused on reviewing the program model and updating integrated care teams on any changes to clinical workflows or protocols. All 10 of the current primary care sites and four Hubs remain committed to the program.
In addition to maintaining the ongoing educational efforts referenced in section 2.6, the program plans to extend additional training on First Approach Skills Training (FAST) (Table 1) to its IHTs.
Additional efforts to maintain PCMHI include plans for more extensive analysis of MBC data to include patient level sub-group differences in treatment completion and symptom response and more frequent report outs to clinicians on trends in PHQ-9A, GAD-7, PSC-17 and CGI data. Future areas of investigation include comparing PCMHI to treatment as usual of mental health issues in pediatric primary care, measuring the impact of warm handoffs on no show and cancelation rates, and exploring the impact of training and education on providers and trainees from all disciplines.
PCMHI evolved during a national crisis in child and adolescent mental health. The program was created in response to a need for more accessible and effective youth mental health services. It drew from PCBH and CoCM to balance primary care and mental health provider needs, while simultaneously encouraging shared decision-making in patient care. In the 3 years since its creation, PCMHI has made headway establishing a model that can play a role in addressing youth mental health needs, but the road to change is never easy. Reflecting on the program’s development, implementation, and maintenance through the RE-AIM framework has allowed for a review of the successes and challenges associated with the model’s implementation and an opportunity to share key lessons learned.
Since 2020, PCMHI has completed over 25,000 patient visits across its primary care and Hub sites and has maintained consistent, timely access to care for patients. Preliminary analysis of MBC data shows the model is effective, as patients have reduced anxiety and depression symptoms as measured by changes in GAD-7 and PHQ-9A screenings. Furthermore, PCP attitudes toward PCMHI are positive, as they believe the model increases access to effective mental healthcare for their patients while easing their workload. In addition to the committed and compassionate hard work of all PCPs, mental health providers, and staff involved in PCMHI, the maintenance of clear, ongoing communication across disciplines and focus on continued quality improvement is essential to the success of the program.
As shared in section 3.4, the implementation of integrated care models is fiscally difficult and this proved to be the case for PCMHI. As of 2023, the program relies on fee-for-service reimbursement as well as continued institutional and philanthropic support, while actively working toward long-term fiscal sustainability via additional revenue sources, including more comprehensive payor contracts.
It is PCMHI’s hope that, by sharing this experience, it can help other systems of care realize the potential for positive change through integrated care for children and adolescents. Recognizing that PCMHI is still in its early years and is a work in progress, it will continue to analyze all aspects of the program and adapt as needed.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
JS and KH contributed to the conception and design of the paper. JS wrote the first draft of the manuscript and first draft of revision. KH provided the extensive guidance for the manuscript. JH and NC-L wrote sections of the manuscript and DH, HB, JG, KS, DA, and AB contributed to the sections of the manuscript. JG wrote and designed (Figure 1). DA provided the current patient profile data and data for statistical analysis. KH performed the statistical comparisons for patient screening data. All authors contributed to manuscript revisions and read and approved the submitted version.
The development of the program was funded by the institutional and philanthropic support.
The authors would like the thank the Rady Children’s Hospital-San Diego Transforming Mental Health Initiative, Children’s Primary Care Medical Group, Children’s Physicians Medical Group, Rady Children’s Physician Management Services and the University of California San Diego Department of Psychiatry, Division of Child and Adolescent Psychiatry for their steadfast support of this new program, and their commitment to work collaboratively across institutions. Adam Breslow, Ben Maxwell, Ken Morris and Gina Rosenfeld championed this effort. Thanks to Jennifer Zubyk for her extensive support of the team.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1252037/full#supplementary-material
1. AAP-AACAP-CHA Declaration of a National Emergency in Child and Adolescent Mental Health (2021). Available at: https://www.aap.org/en/advocacy/child-and-adolescent-healthy-mental-development/aap-aacap-cha-declaration-of-a-national-emergency-in-child-and-adolescent-mental-health/.
2. Office of the Surgeon General (OSG). Protecting youth mental health: the U.S. Surgeon General’s advisory. Washington, DC: US Department of Health and Human Services (2021).
3. Meherali, S, Punjani, N, Louie-Poon, S, Abdul Rahim, K, Das, JK, Salam, RA, et al. Mental health of children and adolescents amidst COVID-19 and past pandemics: a rapid systematic review. Int J Environ Res Public Health. (2021) 18:3432. doi: 10.3390/ijerph18073432
4. Curtin, SC. State suicide rates among adolescents and young adults aged 10–24: United States, 2000–2018 In:. National Vital Statistics Reports, vol. 69. Hyattsville, MD: National Center for Health Statistics (2020)
5. Ong, MS, Lakoma, M, Gees Bhosrekar, S, Hickok, J, McLean, L, Murphy, M, et al. Risk factors for suicide attempt in children, adolescents, and young adults hospitalized for mental health disorders. Child Adolesc Ment Health. (2021) 26:134–42. doi: 10.1111/camh.12400
6. Sheftall, AH, Vakil, F, Ruch, DA, Boyd, RC, Lindsey, MA, and Bridge, JA. Black youth suicide: investigation of current trends and precipitating circumstances. J Am Acad Child Adolesc Psychiatry. (2022) 61:662–75. doi: 10.1016/j.jaac.2021.08.021
7. Lu, W. Adolescent depression: National Trends, risk factors, and healthcare disparities. Am J Health Behav. (2019) 43:181–94. doi: 10.5993/AJHB.43.1.15
8. Douglas, CM, Richardson, L, and Evans, YN. Utilization of mental health services among black adolescents during the COVID-19 pandemic: a narrative review of the literature. Curr Pediatr Rep. (2023) 11:7–12. doi: 10.1007/s40124-023-00282-7
9. Lu, W, Todhunter-Reid, A, Mitsdarffer, ML, Muñoz-Laboy, M, Yoon, AS, and Xu, L. Barriers and facilitators for mental health service use among racial/ethnic minority adolescents: a systematic review of literature. Front Public Health. (2021) 9:641605. doi: 10.3389/fpubh.2021.641605
10. Ghandour, RM, Sherman, LJ, Vladutiu, CJ, Ali, MM, Lynch, SE, Bitsko, RH, et al. Prevalence and treatment of depression, anxiety, and conduct problems in US children. J Pediatr. (2019) 206:256–267.e3. doi: 10.1016/j.jpeds.2018.09.021
11. Felitti, VJ, Anda, RF, Nordenberg, D, Williamson, DF MS, PhD, Spitz, AM MS, MPH, Edwards, V BA, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. Am J Prev Med. (1998) 14:245–58. doi: 10.1016/S0749-3797(98)00017-8
12. Shonkoff, JP, Garner, AS, The Committee on Psychosocial Aspects of Child and Family Health, Committee on Early Childhood, Adoption, and Dependent Care, and Section on Developmental and Behavioral Pediatrics, Siegel, BS, Dobbins, MI, Earls, MF, et al. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. (2012) 129:e232–46. doi: 10.1542/peds.2011-2663
13. Substance Abuse and Mental Health Services Administration. SAMHSA’s Concept of Trauma and Guidance for a Trauma-Informed Approach. HHS Publication No. (SMA) 14-4884. Rockville, MD: Substance Abuse and Mental Health Services Administration (2014). Available at: https://store.samhsa.gov/sites/default/files/d7/priv/sma14-4884.pdf.
14. Compton, SN, Walkup, JT, Albano, AM, Piacentini, JC, Birmaher, B, Sherrill, JT, et al. Child/adolescent anxiety multimodal study (CAMS): rationale, design, and methods. Child Adolesc Psychiatry Ment Health. (2010) 4:1. doi: 10.1186/1753-2000-4-1
15. March, JS, Silva, S, Petrycki, S, Curry, J, Wells, K, Fairbank, J, et al. The treatment for adolescents with depression study (TADS): long-term effectiveness and safety outcomes. Arch Gen Psychiatry. (2007) 64:1132–43. doi: 10.1001/archpsyc.64.10.1132
16. Rocks, S, Berntson, D, Gil-Salmerón, A, Kadu, M, Ehrenberg, N, Stein, V, et al. Cost and effects of integrated care: a systematic literature review and meta-analysis. Eur J Health Econ. (2020) 21:1211–21. doi: 10.1007/s10198-020-01217-5
17. Schlesinger, A, Sengupta, S, Marx, L, Hilt, R, Martini, DR, DeMaso, DR, et al. Clinical update: collaborative mental health Care for Children and Adolescents in pediatric primary care. J Am Acad Child Adolesc Psychiatry. (2023) 62:91–119. doi: 10.1016/j.jaac.2022.06.007
18. SAMHSA/HRSA Center for Integrated Health Solutions: six levels of collaboration/integration (core descriptions). Available at: https://www.thenationalcouncil.org/wp-content/uploads/2020/01/CIHS_Framework_Final_charts.pdf?daf=375ateTbd56.
19. Hunter, CL, Funderburk, JS, Polaha, J, Bauman, D, Goodie, JL, and Hunter, CM. Primary care behavioral health (PCBH) model research: current state of the science and a call to action. J Clin Psychol Med Settings. (2018) 25:127–56. doi: 10.1007/s10880-017-9512-0
20. Richardson, LP, Lukman, E, McCauley, E, Lindenbaum, J, Larison, C, Zhou, C, et al. Collaborative care for adolescents with depression in primary care: a randomized clinical trial. JAMA. (2014) 312:809–16. doi: 10.1001/jama.2014.9259
21. Wright, DR, Haaland, WL, Ludman, E, McCauley, E, Lindenbaum, J, and Richardson, LP. The costs and cost-effectiveness of collaborative care for adolescents with depression in primary care settings: a randomized clinical trial. JAMA Pediatr. (2016) 170:1048–54. doi: 10.1001/jamapediatrics.2016.1721
22. Reiter, JT, Dobmeyer, AC, and Hunter, CL. The primary care behavioral health (PCBH) model: an overview and operational definition. J Clin Psychol Med Settings. (2018) 25:109–26. doi: 10.1007/s10880-017-9531-x
23. Remoue Gonzales, S, and Higgs, J. Perspectives on integrated behavioral health in pediatric care with immigrant children and adolescents in a federally qualified health Center in Texas. Clin Child Psychol Psychiatry. (2020) 25:625–35. doi: 10.1177/1359104520914724
24. Dopp, AR, Smith, AB, Dueweke, AR, and Bridges, AJ. Cost-savings analysis of primary care behavioral health in a pediatric setting: implications for provider agencies and training programs. Clin Pract Pediatr Psychol. (2018) 6:129–39. doi: 10.1037/cpp0000231
25. Unützer, J, Katon, W, Callahan, CM, Williams, Jr, JW, Hunkeler, E, Harpole, L, et al. Collaborative care management of late-life depression in the primary care setting. JAMA. (2002) 288:2836–45. doi: 10.1001/jama.288.22.2836
26. Sowers, WE, McQuistion, HL, Ranz, JM, Maus Feldman, J, and Runnels, PS. Textbook of community psychiatry: American association for community psychiatry. 2nd ed Springer Nature Switzerland AG: Springer International Publishing (2022).
27. Wolraich, ML, Hagan, JF Jr, Allan, C, Chan, E, Davison, D, Earls, M, et al. Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. (2019) 144:e20192528. doi: 10.1542/peds.2019-2528
28. Valero-Aguayo, L, Rodríguez-Bocanegra, M, Ferro-García, R, and Ascanio-Velasco, L. Meta-analysis of the efficacy and effectiveness of parent child interaction therapy (PCIT) for child behaviour problems. Psicothema. (2021) 33:544–55. doi: 10.7334/psicothema2021.70
29. Schoenfelder Gonzalez, E, Jungbluth, N, McCarty, CA, and Hilt, R. Barriers to increasing access to brief pediatric mental health treatment from primary care. Psychiatr Serv. (2022) 73:235–8. doi: 10.1176/appi.ps.202000457
31. Sanderson, D, Braganza, S, Philips, K, Chodon, T, Whiskey, R, Bernard, P, et al. Increasing warm handoffs: optimizing community based referrals in primary care using QI methodology. J Prim Care Community Health. (2021) 12:21501327211023883. doi: 10.1177/21501327211023883
32. Horevitz, E, Organista, KC, and Arean, PA. Depression treatment uptake in integrated primary care: how a "warm handoff" and other factors affect decision making by Latinos. Psychiatr Serv. (2015) 66:824–30. doi: 10.1176/appi.ps.201400085
33. Taylor, RM, and Minkovitz, CS. Warm handoffs for improving client receipt of services: a systematic review. Matern Child Health J. (2021) 25:528–41. doi: 10.1007/s10995-020-03057-4
34. Peters, KM, Sadler, G, Miller, E, and Radovic, A. An electronic referral and social work protocol to improve access to mental health services. Pediatrics. (2018) 142:e20172417. doi: 10.1542/peds.2017-2417
35. Young, ND, Mathews, BL, Pan, AY, Herndon, JL, Bleck, AA, and Takala, CR. Warm handoff, or cold shoulder? An analysis of handoffs for primary care behavioral health consultation on patient engagement and systems utilization. Clin Pract Pediatr Psychol. (2020) 8:241–6. doi: 10.1037/cpp0000360
36. Harden, SM, Gaglio, B, Shoup, JA, Kinney, KA, Johnson, SB, Brito, F, et al. Fidelity to and comparative results across behavioral interventions evaluated through the RE-AIM framework: a systematic review. Syst Rev. (2015) 4:155. doi: 10.1186/s13643-015-0141-0
37. Holtrop, JS, Estabrooks, PA, Gaglio, B, Harden, SM, Kessler, RS, King, DK, et al. Understanding and applying the RE-AIM framework: clarifications and resources. J Clin Transl Sci. (2021) 5:e126. doi: 10.1017/cts.2021.789
38. Glasgow, RE, Vogt, TM, and Boles, SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. (1999) 89:1322–7. doi: 10.2105/ajph.89.9.1322
39. Measuring the Use of the RE-AIM Model Dimensions Items Checklist (2012). RE-AIM and PRISM: Implementation in context. Available at: https://re-aim.org/wp-content/uploads/2016/09/checklistdimensions.pdf.
40. Freeman, DS, Manson, L, Howard, J, and Hornberger, J. Financing the primary care behavioral health model. J Clin Psychol Med Settings. (2018) 25:197–209. doi: 10.1007/s10880-017-9529-4
Keywords: primary care, pediatrics, primary care behavioral health, integration, mental health, collaborative care, adolescents, children
Citation: Schweitzer J, Bird A, Bowers H, Carr-Lee N, Gibney J, Schellinger K, Holt JR, Adams DP, Hensler DJ and Hollenbach K (2023) Developing an innovative pediatric integrated mental health care program: interdisciplinary team successes and challenges. Front. Psychiatry. 14:1252037. doi: 10.3389/fpsyt.2023.1252037
Received: 03 July 2023; Accepted: 24 October 2023;
Published: 16 November 2023.
Edited by:
Kathryn L. Lovero, Columbia University, United StatesReviewed by:
Courtney Wolk, University of Pennsylvania, United StatesCopyright © 2023 Schweitzer, Bird, Bowers, Carr-Lee, Gibney, Schellinger, Holt, Adams, Hensler and Hollenbach. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jason Schweitzer, amFzY2h3ZWl0emVyQGhlYWx0aC51Y3NkLmVkdQ==
†ORCID: Jasmine R. Holt https://orcid.org/0000-0003-4539-3920
Kathryn Hollenbach https://orcid.org/0000-0001-9719-0397
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.