
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 06 October 2023
Sec. Addictive Disorders
Volume 14 - 2023 | https://doi.org/10.3389/fpsyt.2023.1251032
This article is part of the Research TopicNew Insights on Bringing Social Context Into Addiction NeuroscienceView all 8 articles
Introduction: Elevated levels of behavioral inhibition (BI) may connote risk for both anxiety and substance use disorders. BI has consistently been shown to be associated with increased levels of anxiety, while the association between BI and substance use has been mixed. It is possible that the relationship between BI and substance use varies by individual difference factors. Hispanic/Latinx (H/L) youth in particular may have stronger relationships between BI, anxiety, and substance use.
Methods: The present study therefore evaluated (1) the prospective relationships between BI [assessed via self-reported behavioral inhibition system (BIS) scale scores], anxiety, and substance use in youth (n = 11,876) across baseline, 1-, and 2-year follow-ups of the Adolescent Brain Cognitive Development (ABCD) Study (ages 9–12) and (2) whether these relationships differed by H/L ethnicity while covarying for average behavioral approach system scores, race, sex, age, highest parental income, highest parental education, and past-year substance use (for analyses involving substance use outcomes).
Results: Baseline levels of BIS scores predicted increased anxiety symptoms at both 1- and 2-year follow-ups and did not differ by H/L ethnicity. Baseline levels of BIS scores also prospectively predicted increased likelihood of substance use at 2-year follow-up, but only for H/L youth and not at 1-year follow-up.
Discussion: High scores on the BIS scale contribute risk to anxiety across ethnicities and may uniquely contribute to risk for substance use in H/L youth.
Anxiety disorders and substance use disorders are highly prevalent and frequently co-occur (1–3). Anxiety disorders are associated with significant quality-of-life impairments, carry an economic burden of billions of dollars in the United States, and are one of the top ten leading causes of disability globally (4–7). When anxiety disorders co-occur with substance use disorders, such co-occurrence is associated with markedly worse outcomes such as increased rates of drug-related problems, unemployment, and poorer treatment outcomes (8–11). The onset of both anxiety and substance use disorders often occurs during childhood and adolescence (3) and understanding the potential shared etiological mechanisms underlying both anxiety and substance use disorders may help improve assessment and treatment of these disorders and their co-occurrence.
Gray’s reinforcement sensitivity theory (RST) (12–14) offers explanations of risk for both disorders and possibly also for their co-occurrence. RST describes two major neurophysiological motivational systems that differ in their responsivity to reward and punishment. The behavioral inhibition system (BIS) is activated when punishment or non-reward conflicts with a goal or reward and results in worry, risk assessment, and increased attention to threat. In contrast, the behavioral approach/activation system (BAS) is activated in response to rewarding stimuli and results in impulsivity, goal pursuit, and increased attention to reward. The biologically based temperamental style of BI is similar to the BIS in that it is characterized by anxious, fearful, and vigilant reactions to novel stimuli (15–17). BI is identifiable as early as infancy and has demonstrated trait-like stability (18). Several studies have shown BI (assessed via behavioral observation in infancy or early childhood or maternal ratings across early childhood) to be stable across early and middle childhood and possibly through late adolescence and early adulthood (15, 19–21). However, the stability and predictive validity of BI varies across individuals. For example, BI (assessed via maternal report) is more stable for girls and those who are initially highest in BI as compared to their peers (20). Further, many of the infants and toddlers that are initially high in behaviorally assessed BI no longer display such sensitivity to novel stimuli as they age (15, 22). Degnan et al. (22) showed that only 15% of toddlers displayed initially high levels of BI and continued to display such high levels of BI at age 5. Identification of children with high and stable levels of BI (assessed via behavioral observation and/or maternal report) is particularly important as they are at increased risk for experiencing symptoms of anxiety and the development of anxiety disorders in adolescence (17, 23–28). In fact, nearly half of children high in BI develop social anxiety disorder in adolescence (25). The BIS may be related to and influenced by BI. While the BIS is assessed by self-report and at later stages of childhood through adulthood, as compared to the behavioral assessment of BI, scores on the BIS/BAS scale may yield improved reliability and generalizability in its assessment of BI (29–31).
The relationship between BI and substance use is much more mixed than that of BI and anxiety. BI may be a protective factor against substance use as the conflicting rewarding (e.g., conformity, relief from distress, etc.) and punishing (e.g., negative health consequences, family conflict, etc.) outcomes associated with substance use may activate the BIS and lead to worry and increased attention to the potential negative consequences of use. However, it is also possible that BI may increase the likelihood of substance use through coping motives for use (32). Individuals with alcohol use disorder as well as individuals with co-occurring anxiety and alcohol dependence evidence greater levels of sensitivity to uncertain threat (33–36), a trait associated with, and predicted by, high levels of BI (37). These high levels of sensitivity to uncertain threat in individuals with alcohol use disorder are also positively associated with self-reported coping motives for use.
To further explore BI’s potential risk for, or protection against, substance use, studies have examined BIS and BAS levels on substance use outcomes. These studies have focused on undergraduate populations and yielded mixed results with some studies showing no association between BIS levels and substance use (38, 39), others showing a positive association between BIS levels with substance use problems (40–42), and still others showing a positive association between BIS levels and substance use but only for high BAS levels (41–43). Given these conflicting results, Morris et al. (40) used a cross-sectional design to examine whether BIS and BAS were indirectly associated with alcohol problems through coping and conformity motives among undergraduate students. Results indicated that those high in BIS levels were more likely to experience alcohol problems due to greater coping and conformity motives for use. Importantly this finding was independent of levels of BAS and high BAS levels only further strengthened these relationships. Taken together, these results highlight BI’s nuanced pathways for high or low risk for substance use and demonstrate the need to investigate potential additional factors contributing to the relationships between BI and substance use.
Ethnicity may be one such important moderator of the relationships between BI, anxiety, and substance use. Hispanic/Latinx (H/L) youth have consistently displayed increased rates of anxiety symptoms, anxiety disorders, and initial rates of substance use when compared to their non-H/L peers (44–51). The greater frequency and intensity for which H/L youth experience threats including increased exposure to crime, community violence, chronic stress, and racial discrimination may heighten levels of BI in H/L youth (52–56). In fact, H/L adults have displayed increased attentional biases to threat as compared to non-H/L adults (57). Cultural values may also further impact BI’s association with anxiety in H/L youth. Schneider and Gudiño (58) showed a positive relationship between BI and anxiety symptoms in H/L adolescents and that this relationship was strongest for those H/L adolescents reporting high levels of Latino cultural values. More specifically, H/L youth may also experience increased anxiety due to heightened social stigma of mental illness in the H/L community and factors related to collectivist cultural values, immigration, and acculturation that, especially in combination, put H/L youth at increased risk when compared to other racial/ethnic groups (46, 50, 59). It is possible that the combination of increased exposure to stressors and traumatic experiences as well as the context of heightened social stigma and collectivist cultural values may dissuade H/L youth from utilizing social support as a form of coping with their anxiety. Since high levels of BI may lead to alcohol problems through coping and conformity motives and H/L youth may experience greater exposure to substance use as they have the highest initial rates of substance use, H/L youth high in BI may be uniquely at risk for substance use. Therefore, H/L ethnicity may moderate the relationship between BI and substance use. However, it is presently unclear whether the strengths of the relationships between BI, anxiety, and substance use differ based on H/L ethnicity. Therefore, the present study will prospectively investigate the relationships between BIS scale scores (used as an approximation of BI), anxiety, and substance use and whether H/L ethnicity moderates such relationships in youth (n = 11,876) from the Adolescent Brain Cognitive Development (ABCD) Study at baseline (ages 9–10), 1-year follow-up (ages 10–11), and 2-year follow-up (ages 11–12).
Data for the current study was drawn from baseline (ages 9–10), 1-year follow-up (ages 10–11), and 2-year follow-up (ages 11–12) of the ABCD Data Release 4.0. The ABCD Study is a longitudinal study with 11,876 participants, is funded by the National Institutes of Health, and is a probability sample and not a clinical sample (60, 61). Youth and their parent or guardian completed baseline, 1-year follow-up, and 2-year follow-up study visits separately to maintain confidentiality. These study visits lasted 8 h (or were split into two 4-h visits) and consisted of a battery of assessments including questionnaires on demographics, mental health, and substance use (62, 63). Youth and their parent/guardian were financially compensated for their participation. The University of California, San Diego Institutional Review Board approved all aspects of this study for the ABCD Research Study Consortium. Please see Table 1 for participant demographics and characteristics.
The parent or legal guardian of the participant was asked about the youth participant’s race and ethnicity during the baseline assessment. The parent/legal guardian answered the following two questions derived from the PhenX toolkit (64) to provide information about the youth participant’s race and ethnicity: “Do you consider the child Hispanic/Latino/Latina?” and “What race do you consider the child to be?.”
Youth participants completed a modified version of the BIS/BAS scale (62, 65, 66). The modified version of the BIS/BAS contained 7 items that corresponded to the BIS scale (baseline α = 0.626, 2-year follow-up α = 0.733) and 13 items that corresponded to the BAS scale (baseline α = 0.831, 2-year follow-up α = 0.861). The BAS scale is comprised of three subscales: reward responsiveness, fun seeking, and drive. A mean BAS scale score was created from the average of these 3 BAS subscales.
The DSM-5 anxiety problems subscale T-score from the Child Behavior Checklist (CBCL) (62, 67) was used to capture anxiety symptomatology as an outcome (baseline α = 0.707, 1-year follow-up α = 0.716, 2-year follow-up α = 0.727). The CBCL was completed by parents/guardians who were asked to report on the youth’s behavior. The CBCL DSM-5 anxiety problems subscale assesses symptoms that are consistent with DSM-5 criteria for Generalized Anxiety Disorder, Separation Anxiety Disorder, Social Anxiety Disorder, and Specific Phobia.
Substance use was assessed via the timeline followback interview (TLFB) (63, 68, 69). Youth participants completed the calendar-based and interviewer-administered TLFB which consisted of a retrospective report of substance use days over the past year. Youth reported on the quantity and frequency of which they used any of the following substances: alcohol, cannabis and cannabinoids, nicotine, cocaine or crack cocaine, cathinones, methamphetamine, 3,4-methylenedioxymethamphetamine (“ecstasy, molly or MDMA”), ketamine, gamma hydroxybutyrate, heroin, hallucinogens, inhalants, prescription stimulants, prescription sedative drugs, prescription opioid pain relievers, and cough or cold medicine containing dextromethorphan. The past-year use sum score was created by summing the total number of days in the past year for which the youth endorsed use of any of the above listed substances. These past-year sum scores were then dichotomized into use in the past year vs. no use in the past year.
Logistic regressions were conducted using the “glm()” function in R to evaluate the impact of baseline BIS scores and the interaction between baseline BIS scores and ethnicity (H/L vs. non-H/L) on (1) past-year substance use at 1-year follow-up (use vs. no use) and (2) past-year substance use at 2-year follow-up (use vs. no use). Linear regressions were conducted using the “lm()” function in R to evaluate the impact of baseline BIS scores and the interaction between baseline BIS scores and ethnicity (H/L vs. non-H/L) on (1) 1-year follow-up CBCL DSM-5 anxiety problems T-scores and (2) 2-year follow-up CBCL DSM-5 anxiety problems T-scores. All analyses were conducted in version 4.2.3 of R. While the majority of youth did not report substance use at baseline (99.57%), 0.50% of H/L youth and 0.42% of non-H/L youth did endorse use at baseline. At 1-year follow-up 0.22% of the sample endorsed any substance use and 0.74% endorsed any substance use at 2-year follow-up. Baseline past-year use days was dichotomized into no past-year substance use and past-year substance use (0 and 1, respectively) and included as a covariate. Past-year substance use at baseline was included in both models in which past-year substance use at follow-up was an outcome. Past year substance use at 1-year follow-up was also included as a dichotomous covariate in the model predicting past-year substance use at 2-year follow-up. To control for their effects on anxiety and substance use, all models included the following covariates: mean baseline BAS scores, race, sex, age, highest parental income, and highest parental education.
After adjusting for baseline BAS scores, race, sex, age, highest parental income, and highest parental education, results indicated a main effect of baseline BIS scores on CBCL DSM-5 anxiety problems scores at the 1-year follow-up (B = 0.191, p < 0.001), as higher scores on the BIS subscale at baseline were related to greater report of anxiety at 1-year follow-up. No main effect of ethnicity or interaction between ethnicity and baseline BIS scores was found (see Table 2).

Table 2. Effects of ethnicity and BIS scores on CBCL DSM-5 anxiety problems scores at year 1 follow-up.
Similarly, after adjusting for the aforementioned covariates, results indicated main effects of baseline BIS scores (B = 0.213, p < 0.001) and baseline BAS scores (B = −0.086, p = 0.005) on CBCL DSM-5 anxiety problems scores at the 2-year follow-up, as higher scores on the BIS subscale and lower scores on the BAS subscale at baseline were related to greater report of anxiety at the 2-year follow-up. No main effect of ethnicity or interaction between ethnicity and baseline BIS scores was found (see Table 3).
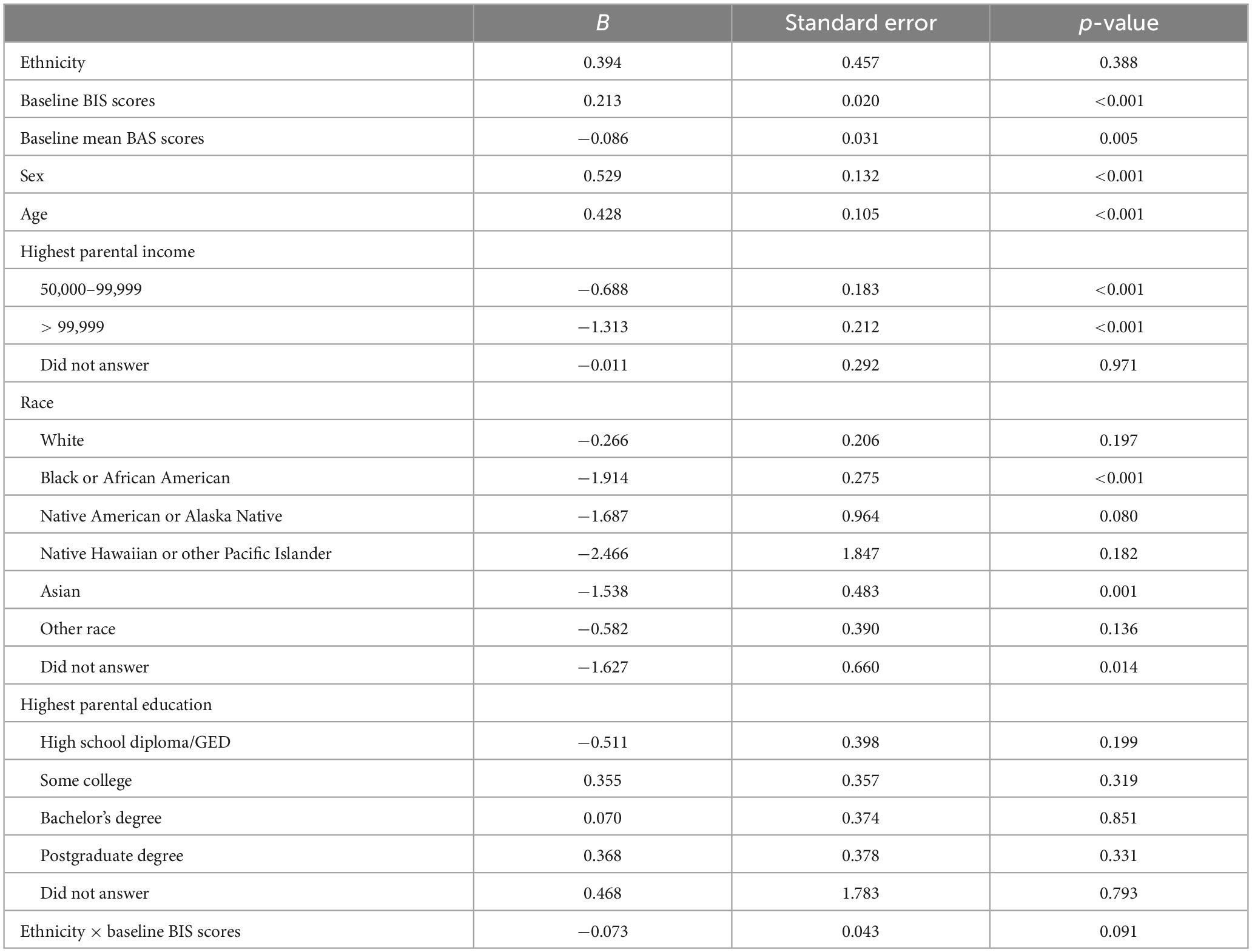
Table 3. Effects of ethnicity and BIS scores on CBCL DSM-5 anxiety problems scores at year 2 follow-up.
After adjusting for baseline BAS scores, race, sex, age, highest parental income, highest parental education, and sum of past-year substance use days at baseline, results indicated that there were no main effects or interactions between ethnicity and baseline BIS scores on past-year substance use at 1-year follow-up (see Table 4).
After adjusting for the aforementioned covariates as well as the sum of past-year substance use days at 1-year follow-up, results revealed a main effect of ethnicity [OR = 0.186, 95% CI (0.032, 0.943), p = 0.042] such that H/L youth were more likely than non-H/L youth to use substances at the 2-year follow-up. Findings also indicated an interaction between ethnicity and baseline BIS scores [OR = 1.195, 95% CI (1.038, 1.378), p = 0.013] on substance use days at year 2 follow-up (see Table 5 and Figure 1). Simple slope analyses were conducted to follow-up the interaction between ethnicity and baseline BIS scores by stratifying by ethnicity. Results showed that BIS scores were associated with increased odds of past-year substance use for H/L youth [p = 0.033, 95% CI (1.012, 1.318), OR = 1.155]. However, baseline BIS scores were not associated with odds of past-year substance use for non-H/L youth [p = 0.257, 95% CI (0.885, 1.033), OR = 0.956].
Elevated levels of BI may contribute risk for both anxiety disorders and substance use disorders. BI has been shown to concurrently and prospectively predict anxiety, while the association between BI and substance use has been mixed. It is possible that the relationship between BI and substance use varies by social and contextual factors. H/L youth in particular may have stronger relationships between BI, anxiety, and substance use. The present study evaluated (1) the prospective relationships between BIS scores, anxiety, and substance use in youth across 1- and 2- year follow-ups of the ABCD study and (2) whether these relationships differed by H/L ethnicity. Results indicated that baseline (ages 9–10) levels of BIS scores prospectively and positively predicted anxiety symptoms at both 1- and 2-year follow-ups (ages 10–12). The relationship between baseline levels of BIS and follow-up levels of anxiety did not differ by ethnicity. Baseline (ages 9–10) levels of BIS also prospectively predicted increased likelihood of substance use at 2-year follow-up (ages 11–12), but only for H/L youth and not for non-H/L youth. No main effects of, or interactions between, ethnicity and BIS scores were found on substance use at the 1-year follow-up.
The results showing that baseline BIS scores prospectively and positively predicted anxiety symptoms across the follow-ups are consistent with prior literature on the relationship between BI and anxiety (17, 23–28). While prior studies have shown that H/L youth report higher levels of anxiety than non-H/L youth (45–51), the present study did not find any ethnic differences in the strength of the relationship between BI and anxiety. It is possible that ethnic differences in anxiety depend on the measure of anxiety (57). H/L are more likely to experience and report physiological symptoms of anxiety (48, 70). The CBCL DSM-5 anxiety problems scales may not best represent H/L youth’s experience of anxiety. Additionally, other risk factors for anxiety may play a more important role in H/L youth’s experience of anxiety and better explain the ethnic differences in anxiety in youth. For example, individual differences in sensitivity to uncertain threat may be a stronger predictor of anxiety, and particularly for H/L (71–74).
Results related to the relationship between BIS scores and substance use varied across the follow-up years. The lack of association between BIS scores and likelihood of substance use at 1-year follow-up may be due to the fact that substance use at 1-year follow-up was infrequent and did not greatly increase from baseline. While overall substance use increased at 2-year follow-up in the sample, BIS scores only predicted increased likelihood of substance us in H/L youth (as compared to non-H/L youth). Similar to the results of Morris et al. (40), these results were independent of levels of BAS scores. This finding is also consistent with results from Chen and Jacobson (44) showing that H/L youth have the highest initial rates of substance use. H/L youth’s increased exposure to crime, community violence, chronic stress, and racial discrimination (52–56) may also increase coping and conformity motives which in turn may increase likelihood of substances use. It is possible that high BI, in addition to, or in conjunction with, additional risk factors such as increased access to substances, reduced parental monitoring, and association with deviant peers (75) may uniquely contribute to risk for early use of substances in H/L. Further research is needed to understand whether and how such risk may change as rates of substance use change across development.
The present study had several limitations and future directions. While the longitudinal nature of the ABCD study allowed for the investigation of prospective and not just concurrent relationships between BIS scores, anxiety, and substance use, it is possible that the age of the sample at baseline and through the follow-ups is still too early to best capture these relationships. As BI is often first assessed in infancy or early childhood (18, 22), the strength of the relationships between BI, substance use, and anxiety may vary across development and the lifespan. Relatedly, assessing BI via behavioral observation in infancy or early childhood may yield different results than the self-reported BIS scale scores utilized in the present investigation. Additionally, as rates of substance use increase across adolescence and early adulthood and use trajectories vary between ethnicities (44), the relationships between BIS scores, ethnicity, and substance use may vary based on the time point in which substance use is measured. These relationships may also vary across H/L youth and could differ based on factors such as time living in the US, social stigma, acculturation, language, nativity, and socioeconomic status (48, 76–83). Lastly, the ABCD study sample is not a clinical or treatment seeking sample and utilizing clinical samples may impact the strength of the relationships explored in the present study. Additional prospective studies are needed to understand how BIS scores and ethnicity relate to substance use as use increases in future follow-up years of the ABCD Study. Additional research is also needed to understand how factors such as trauma exposure, stress, cultural values, discrimination, coping motives, conformity motives, etc. may mediate the relationship between BI and substance use in H/L youth.
In conclusion, high levels of BIS prospectively predict increased rates of anxiety symptoms in both H/L and non-H/L youth. However, BIS scores uniquely predict increased likelihood of substance use for H/L youth. Future studies are needed to further understand the mechanisms ‘underlying the relationship between BI and substance use in H/L youth that will provide a scientific basis to better inform prevention and intervention programs for the H/L community.
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: https://nda.nih.gov/abcd/.
The studies involving humans were approved by the University of California, San Diego Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
ED, AW, and WP substantially contributed to data acquisition, analysis, and interpretation of data, provided critical revisions, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. JJ provided substantial contributions to the conception and design of the work, the acquisition, analysis, interpretation of data for the work, as well as critical revisions for important intellectual content, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors contributed to the article and approved the submitted version.
The ABCD Study was supported by the National Institutes of Health and additional federal partners under award numbers: U01DA041048, U01DA050989, U01DA051016, U01DA041022, U01DA051018, U01DA051037, U01DA050987, U01DA041174, U01DA041106, U01DA041117, U01DA041028, U01DA041134, U01DA050988, U01DA051039, U01DA041156, U01DA041025, U01DA041120, U01DA051038, U01DA041148, U01DA041093, U01DA041089, U24DA041147, and U24DA041123. A full list of supporters is available at https://abcdstudy.org/federal-partners/. Research reported in this publication was also supported by the National Institute of Mental Health (NIMH) T32 MH018399 (KC), the National Institute on Drug Abuse (NIDA) grants U01 DA041089, R21 DA047953, R01 DA054106, R01 DA054980 (JJ), and the National Institute on Alcohol Abuse and Alcoholism (NIAAA) T32 AA013525 (ED).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Conway KP, Compton W, Grant BF. Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: Results from the National Epidemiologic Survey on alcohol and related conditions. J Clin Psychiatry. (2006). 2:247–57. doi: 10.4088/JCP.v67n0211
2. Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. (2005) 62:617. doi: 10.1001/archpsyc.62.6.617
3. Vorspan F, Mehtelli W, Dupuy G, Bloch V, Lépine J-P. Anxiety and substance use disorders: co-occurrence and clinical issues. Curr Psychiatry Rep. (2015) 17:1–7. doi: 10.1007/s11920-014-0544-y
4. Baxter AJ, Vos T, Scott KM, Ferrari AJ, Whiteford HA. The global burden of anxiety disorders in 2010. Psychol Med. (2014) 44:2363–74. doi: 10.1017/S0033291713003243
5. Kessler RC, Aguilar-Gaxiola S, Alonso J, Chatterji S, Lee S, Ormel J, et al. The global burden of mental disorders: an update from the WHO World Mental Health (WMH) surveys. Epidemiol Psichiatria Soc. (2009) 18:23–33.
6. Kroenke K, Spitzer RL, Williams JBW, Monahan PO, Löwe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. (2007) 146:317. doi: 10.7326/0003-4819-146-5-200703060-00004
7. Rapaport MH, Clary C, Fayyad R, Endicott J. Quality-of-life impairment in depressive and anxiety disorders. Am J Psychiatry. (2005) 162:1171–8. doi: 10.1176/appi.ajp.162.6.1171
8. Back SE, Brady KT. Anxiety disorders with comorbid substance use disorders: diagnostic and treatment considerations. Psychiatric Ann. (2008) 38:724–9. doi: 10.3928/00485713-20081101-01
9. Buckner JD, Zvolensky MJ, Schmidt NB. Cannabis-related impairment and social anxiety: the roles of gender and cannabis use motives. Addict Behav. (2012) 37:1294–7. doi: 10.1016/J.ADDBEH.2012.06.013
10. Buckner JD, Carroll KM. Effect of anxiety on treatment presentation and outcome: results from the marijuana treatment project. Psychiatry Res. (2010) 178:493–500. doi: 10.1016/J.PSYCHRES.2009.10.010
11. Ouimette PC, Gima K, Moos RH, Finney JW. A comparative evaluation of substance abuse treatment IV. the effect of comorbid psychiatric diagnoses on amount of treatment, continuing care, and 1-year outcomes. Alcoholism. (1999) 23:552–7. doi: 10.1111/j.1530-0277.1999.tb04152.x
12. Corr PJ. Reinforcement sensitivity theory and personality. Neurosci Biobehav Rev. (2004) 28:317–32. doi: 10.1016/J.NEUBIOREV.2004.01.005
13. Gray JA. Précis of The neuropsychology of anxiety: an enquiry into the functions of the septo-hippocampal system. Behav Brain Sci. (1982) 5:469–84. doi: 10.1017/S0140525X00013066
14. McNaughton N, Corr PJ. The neuropsychology of fear and anxiety: A foundation for Reinforcement Sensitivity Theory. In: Corr PJ editor. The Reinforcement Sensitivity Theory of Personality. Cambridge, MA: Cambridge University Press (2008). doi: 10.1017/CBO9780511819384.003
15. Fox NA, Henderson HA, Rubin KH, Calkins SD, Schmidt LA. Continuity and discontinuity of behavioral inhibition and exuberance: psychophysiological and behavioral influences across the first four years of life. Child Dev. (2001) 72:1–21. doi: 10.1111/1467-8624.00262
16. Kagan J, Reznick JS, Clarke C, Snidman N, Garcia-Coll C. Behavioral inhibition to the unfamiliar. Child Dev. (1984) 55:2212. doi: 10.2307/1129793
17. Rosenbaum JF, Biederman J, Bolduc-Murphy EA, Faraone SV, Chaloff J, Hirshfeld DR, et al. Behavioral inhibition in childhood: a risk factor for anxiety disorders. Harvard Rev Psychiatry. (1993) 1:2–16. doi: 10.3109/10673229309017052
18. Fox NA, Henderson HA, Marshall PJ, Nichols KE, Ghera MM. Behavioral inhibition: linking biology and behavior within a developmental framework. Annu Rev Psychol. (2004) 56:235–62. doi: 10.1146/ANNUREV.PSYCH.55.090902.141532
19. Gest SD. Behavioral inhibition: stability and associations with adaptation from childhood to early adulthood. J Pers Soc Psychol. (1997) 72:467–75. doi: 10.1037/0022-3514.72.2.467
20. Kerr M, Lambert WW, Stattin H, Klackenberg-Larsson I. Stability of inhibition in a swedish longitudinal sample. Child Dev. (1994) 65:138–46. doi: 10.1111/J.1467-8624.1994.TB00740.X
21. Sanson A. Shyness ratings: stability and correlates in early childhood. Int J Behav Dev. (1996) 19:705–24. doi: 10.1080/016502596385532
22. Degnan KA, Almas AN, Henderson HA, Hane AA, Walker OL, Fox NA, et al. Longitudinal trajectories of social reticence with unfamiliar peers across early childhood. Dev Psychol. (2014) 50:2311–23. doi: 10.1037/a0037751
23. Biederman J, Rosenbaum JF, Hirshfeld DR, Faraone SV, Bolduc EA, Gersten M, et al. Psychiatric correlates of behavioral inhibition in young children of parents with and without psychiatric disorders. Arch Gen Psychiatry. (1990) 47:21–6. doi: 10.1001/ARCHPSYC.1990.01810130023004
24. Chronis-Tuscano A, Degnan KA, Pine DS, Perez-Edgar K, Henderson HA, Diaz Y, et al. Stable early maternal report of behavioral inhibition predicts lifetime social anxiety disorder in adolescence. J Am Acad Child Adolescent Psychiatry. (2009) 48:928–35. doi: 10.1097/CHI.0B013E3181AE09DF
25. Clauss JA, Blackford JU. Behavioral inhibition and risk for developing social anxiety disorder: a meta-analytic study. J Am Acad Child Adolescent Psychiatry. (2012) 51:1066.e–75.e. doi: 10.1016/J.JAAC.2012.08.002
26. Hirsfeld DR, Rosenbaum JF, Biederman J, Bolduc EA, Faraone SV, Snidman N, et al. Stable behavioral inhibition and its association with anxiety disorder. J Am Acad Child Adolescent Psychiatry. (1992) 31:103–11. doi: 10.1097/00004583-199201000-00016
27. Hirshfeld-Becker DR, Biederman J, Henin A, Faraone SV, Davis S, Harrington K, et al. Behavioral inhibition in preschool children at risk is a specific predictor of middle childhood social anxiety: a five-year follow-up. J Dev Behav Pediatrics. (2007) 28:225–33. doi: 10.1097/01.DBP.0000268559.34463.D0
28. Van Brakel AML, Muris P, Bögels SM, Thomassen C. A multifactorial model for the etiology of anxiety in non-clinical adolescents: main and interactive effects of behavioral inhibition, attachment and parental rearing. J Child Family Stud. (2006) 15:568–78. doi: 10.1007/S10826-006-9061-X/TABLES/3
29. Eisenberg IW, Bissett PG, Enkavi AZ, Li J, Mackinnon DP, Marsch LA, et al. Uncovering the structure of self-regulation through data-driven ontology discovery. Nat Commun. (2019) 10:2319. doi: 10.1038/s41467-019-10301-1
30. Mazza GL, Smyth HL, Bissett PG, Canning JR, Eisenberg IW, Enkavi AZ, et al. Correlation database of 60 cross-disciplinary surveys and cognitive tasks assessing self-regulation. J Pers Assess. (2021) 103:238–45. doi: 10.1080/00223891.2020.1732994
31. Zeynep Enkavi A, Eisenberg IW, Bissett PG, Mazza GL, MacKinnon DP, Marsch LA, et al. Large-scale analysis of test–retest reliabilities of self-regulation measures. Proc Natl Acad Sci U.S.A. (2019) 116:5472–7. doi: 10.1073/PNAS.1818430116/SUPPL_FILE/PNAS.1818430116.SAPP.PDF
32. Savage JE, Bountress K, Adkins AE, Thomas N, Neale Z, Pedersen K, et al. Internalizing and externalizing subtypes of alcohol misuse and their relation to drinking motives Genotypic data processing and cleaning. Addict Behav. (2022) 136:107461. doi: 10.1016/j.addbeh.2022.107461
33. Gorka SM, Nelson BD, Shankman SA. Startle response to unpredictable threat in comorbid panic disorder and alcohol dependence. Drug Alcohol Depend. (2013) 132:216–22. doi: 10.1016/j.drugalcdep.2013.02.003
34. Gorka SM, Hee D, Lieberman L, Mittal VA, Phan KL, Shankman SA. Reactivity to uncertain threat as a familial vulnerability factor for alcohol use disorder. Psychol Med. (2016) 46:3349–58. doi: 10.1017/S0033291716002415
35. Gorka SM, Kreutzer KA, Petrey KM, Radoman M, Phan KL. Behavioral and neural sensitivity to uncertain threat in individuals with alcohol use disorder: associations with drinking behaviors and motives. Addict Biol. (2020) 25:e12774. doi: 10.1111/ADB.12774
36. Gorka SM, Shankman SA. Preliminary evidence that reactivity to uncertain threat is an endophenotype for alcohol use disorder. Drug Alcohol Depend. (2017) 180:265–71. doi: 10.1016/J.DRUGALCDEP.2017.08.023
37. Mumper EE, Ferry RA, Klein DN, Nelson BD. Effects of early childhood behavioral inhibition and parental anxiety disorder on adolescents’ startle response to predictable and unpredictable threat. Res Child Adolescent Psychopathol. (2022) doi: 10.1007/S10802-022-00942-0/FIGURES/2
38. Hundt NE, Kimbrel NA, Mitchell JT, Nelson-Gray RO. High BAS, but not low BIS, predicts externalizing symptoms in adults. Pers Individ Differ. (2008) 44:565–75. doi: 10.1016/j.paid.2007.09.018
39. O’Connor RM, Colder CR. Predicting alcohol patterns in first-year college students through motivational systems and reasons for drinking. Psychol Addict Behav. (2005) 19:10–20. doi: 10.1037/0893-164X.19.1.10
40. Morris V, Keough MT, Stewart SH, O’Connor RM. Coping and conformity motives mediate the joint effects of the behavioral inhibition and approach systems on alcohol problems in young adults. Substance Use Misuse (2023) 58:2188460. doi: 10.1080/10826084.2023.2188460
41. Wardell JD, O’connor RM, Read JP, Colder CR. Behavioral approach system moderates the prospective association between the behavioral inhibition system and alcohol outcomes in college students. J Stud Alcohol Drugs. (2011) 72: 1028–36.
42. Wardell JD, Read JP, Colder CR. The role of behavioral inhibition and behavioral approach systems in the associations between mood and alcohol consequences in college: A longitudinal multilevel analysis. Addict Behav. (2013) 38:2772–81. doi: 10.1016/j.addbeh.2013.07.012
43. Keough MT, O’Connor RM. Interactive effects of the BIS and the BAS on trajectories of alcohol misuse after university graduation. Substance Abuse (2016) 9:33–40. doi: 10.4137/SART.S31434
44. Chen P, Jacobson KC. Developmental trajectories of substance use from early adolescence to young adulthood: gender and racial/ethnic differences. J Adolescent Health. (2012) 50:154–63. doi: 10.1016/J.JADOHEALTH.2011.05.013
45. Ginsburg GS, Silverman WK. Phobic and anxiety disorders in hispanic and caucasian youth. J Anxiety Disord. (1996) 10:517–28. doi: 10.1016/S0887-6185(96)00027-8
46. McLaughlin KA, Hilt LM, Nolen-Hoeksema S. Racial/ethnic differences in internalizing and externalizing symptoms in adolescents. J Abnormal Child Psychol. (2007) 35:801–16. doi: 10.1007/s10802-007-9128-1
47. Pina AA, Silverman WK. Clinical phenomenology, somatic symptoms, and distress in hispanic/latino and european american youths with anxiety disorders. J Clin Child Adolescent Psychol. (2004) 33:227–36. doi: 10.1207/s15374424jccp3302_3
48. Varela RE, Vernberg EM, Sanchez-Sosa JJ, Riveros A, Mitchell M, Mashunkashey J. Anxiety reporting and culturally associated interpretation biases and cognitive schemas: a comparison of Mexican, Mexican American, and European American Families. J Clin Child Adolescent Psychol. (2004) 33:237–47. doi: 10.1207/s15374424jccp3302_4
49. Varela RE, Sanchez-Sosa JJ, Biggs BK, Luis TM. Parenting strategies and socio-cultural influences in childhood anxiety: Mexican, Latin American descent, and European American families. J Anxiety Disord. (2009) 23:609–16. doi: 10.1016/J.JANXDIS.2009.01.012
50. Varela RE, Hensley-Maloney L. The influence of culture on anxiety in latino youth: a review. Clin Child Family Psychol Rev. (2009) 12:217–33. doi: 10.1007/s10567-009-0044-5
51. Weems CF, Hayward C, Killen J, Taylor CB. A longitudinal investigation of anxiety sensitivity in adolescence. J Abnormal Psychol. (2002) 111:471–7. doi: 10.1037/0021-843X.111.3.471
52. Crouch JL, Hanson RF, Saunders BE, Kilpatrick DG, Resnick HS. Income, race/ethnicity, and exposure to violence in youth: results from the national survey of adolescents. J Commun Psychol. (2000) 28:625–41. doi: 10.1002/1520-6629
53. Hwang WC, Goto S. The impact of perceived racial discrimination on the mental health of Asian American and Latino college students. Cult Divers Ethnic Minority Psychol. (2008) 14:326–35. doi: 10.1037/1099-9809.14.4.326
54. Robinette JW, Charles ST, Almeida DM, Gruenewald TL. Neighborhood features and physiological risk: an examination of allostatic load. Health Place (2016) 41:110–8. doi: 10.1016/j.healthplace.2016.08.003
55. Whitfield GP, Carlson SA, Ussery EN, Watson KB, Brown DR, Berrigan D, et al. Racial and ethnic differences in perceived safety barriers to walking, United States National Health Interview Survey – 2015. Prev Med. (2018) 114:57–63. doi: 10.1016/j.ypmed.2018.06.003
56. Zvolensky MJ, Rogers AH, Bakhshaie J, Viana AG, Walker R, Mayorga NA, et al. Perceived racial discrimination, anxiety sensitivity, and mental health among Latinos in a federally qualified health center. Stigma Health. (2019) 4:473–9. doi: 10.1037/sah0000160
57. Correa KA, Carrillo V, Funkhouser CJ, Shenberger ER, Shankman SA. Ethnic differences in behavioral and physiological indicators of sensitivity to threat. J Anxiety Disord. (2022) 85:102508. doi: 10.1016/J.JANXDIS.2021.102508
58. Schneider A, Gudiño OG. Predicting avoidance symptoms in U.S. Latino youth exposed to community violence: the role of cultural values and behavioral inhibition. J Traumatic Stress. (2018) 31:509–17. doi: 10.1002/JTS.22313
59. Anderson ER, Mayes LC. Race/ethnicity and internalizing disorders in youth: a review. Clin Psychol Rev. (2010) 30:338–48. doi: 10.1016/J.CPR.2009.12.008
60. Garavan H, Bartsch H, Conway K, Decastro A, Goldstein RZ, Heeringa S, et al. Recruiting the ABCD sample: design considerations and procedures. Dev Cogn Neurosci. (2018) 32:16. doi: 10.1016/J.DCN.2018.04.004
61. Volkow ND, Koob GF, Croyle RT, Bianchi DW, Gordon JA, Koroshetz WJ, et al. The conception of the ABCD study: from substance use to a broad NIH collaboration. Dev Cogn Neurosci. (2018) 32:4–7. doi: 10.1016/J.DCN.2017.10.002
62. Barch DM, Albaugh MD, Avenevoli S, Chang L, Clark DB, Glantz MD, et al. Demographic, physical and mental health assessments in the adolescent brain and cognitive development study: Rationale and description. Dev Cogn Neurosci. (2018) 32:55–66. doi: 10.1016/J.DCN.2017.10.010
63. Lisdahl KM, Sher KJ, Conway KP, Gonzalez R, Feldstein Ewing SW, Nixon SJ, et al. Adolescent brain cognitive development (ABCD) study: overview of substance use assessment methods. Dev Cogn Neurosci. (2018) 32:80–96. doi: 10.1016/J.DCN.2018.02.007
64. Stover PJ, Harlan WR, Hammond JA, Hendershot T, Hamilton CM. PhenX: a toolkit for interdisciplinary genetics research. Curr Opin Lipidol. (2010) 21:136. doi: 10.1097/MOL.0B013E3283377395
65. Carver CS, White TL. Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: The BIS/BAS Scales. J Pers Soc Psychol. (1994) 67:319–33. doi: 10.1037/0022-3514.67.2.319
66. Pagliaccio D, Luking KR, Anokhin AP, Gotlib IH, Hayden EP, Olino TM, et al. Revising the BIS/BAS Scale to study development: measurement invariance and normative effects of age and sex from childhood through adulthood. Psychol Assess. (2016) 28:429–42. doi: 10.1037/PAS0000186
67. Achenbach TM. The Achenbach System of Empirically Based Assessment (ASEBA): Development, Findings, Theory and Applications. Burlington, VT: University of Vermont Research Center for Children, Youth, and Families (2009).
68. Robinson SM, Sobell LC, Sobell MB, Leo GI. Reliability of the timeline followback for cocaine, cannabis, and cigarette use. Psychol Addict Behav. (2014) 28:154–62. doi: 10.1037/a0030992
69. Sobell LC, Sobell MB. Timeline Follow-Back. In: Litten RZ, Allen JP editors. Measuring Alcohol Consumption. Totowa, NJ: Humana Press (1992). p. 41–72. doi: 10.1007/978-1-4612-0357-5_3
70. Escovar EL, Craske M, Roy-Byrne P, Stein MB, Sullivan G, Sherbourne CD, et al. Cultural influences on mental health symptoms in a primary care sample of Latinx patients. J Anxiety Disord. (2018) 55:39–47. doi: 10.1016/j.janxdis.2018.03.005
71. Carleton RN. Fear of the unknown: One fear to rule them all? J Anxiety Disord. (2016) 41:5–21. doi: 10.1016/J.JANXDIS.2016.03.011
72. Correa KA, Liu H, Shankman SA. The role of intolerance of uncertainty in current and remitted internalizing and externalizing psychopathology. J Anxiety Disord. (2019) 62:68–76. doi: 10.1016/j.janxdis.2019.01.001
73. Craske MG, Wolitzky-Taylor KB, Mineka S, Zinbarg R, Waters AM, Vrshek-Schallhorn S, et al. Elevated responding to safe conditions as a specific risk factor for anxiety versus depressive disorders: evidence from a longitudinal investigation. J Abnormal Psychol. (2012) 121:315–24. doi: 10.1037/a0025738
74. Oglesby ME, Boffa JW, Short NA, Raines AM, Schmidt NB. Intolerance of uncertainty as a predictor of post-traumatic stress symptoms following a traumatic event. J Anxiety Disord. (2016) 41:82–7. doi: 10.1016/j.janxdis.2016.01.005
75. Atherton OE, Conger RD, Ferrer E, Robins RW. Risk and protective factors for early substance use initiation: a longitudinal study of mexican-origin youth. J Res Adolescence. (2016) 26:864–79. doi: 10.1111/JORA.12235
76. Alegría M, Canino G, Shrout PE, Woo M, Duan N, Vila D, et al. Prevalence of mental illness in immigrant and non-immigrant U.S. Latino groups. Am J Psychiatry. (2008) 165:359–69. doi: 10.1176/appi.ajp.2007.07040704
77. Alegría M, Molina KM, Chen C-N. Neighborhood characteristics and differential risk for depressive and anxiety disorders across racial/ethnic groups in the United States. Depress Anxiety. (2014) 31:27–37. doi: 10.1002/da.22197
78. Alvidrez J, Azocar F. Distressed women’s clinic patients: preferences for mental health treatments and perceived obstacles. Gen Hosp Psychiatry. (1999) 21:340–7. doi: 10.1016/S0163-8343(99)00038-9
79. Arellano-Morales L, Roesch SC, Gallo LC, Emory KT, Molina KM, Gonzalez P, et al. Prevalence and correlates of perceived ethnic discrimination in the hispanic community health study/study of latinos sociocultural ancillary study. J Latina Psychol. (2015) 3:160–76. doi: 10.1037/lat0000040
80. Nadeem E, Lange JM, Edge D, Fongwa M, Belin T, Miranda J. Does stigma keep poor young immigrant and U.S.-born black and Latina women from seeking mental health care? Psychiatric Serv. (2007) 58:1547–54. doi: 10.1176/ps.2007.58.12.1547
81. Ortega AN, Rosenheck R, Alegría M, Desai RA. Acculturation and the lifetime risk of psychiatric and substance use disorders among Hispanics. J Nerv Mental Dis. (2000) 188:728–35. doi: 10.1097/00005053-200011000-00002
82. Potochnick SR, Perreira KM. Depression and anxiety among first-generation immigrant Latino youth: key correlates and implications for future research. J Nervous Mental Dis. (2010) 198:470–7. doi: 10.1097/NMD.0b013e3181e4ce24
Keywords: behavioral inhibition, behavioral activation, anxiety, substance use, Hispanic, Latinx
Citation: Correa KA, Delfel EL, Wallace AL, Pelham WE III and Jacobus J (2023) Hispanic/Latinx ethnic differences in the relationships between behavioral inhibition, anxiety, and substance use in youth from the ABCD cohort. Front. Psychiatry 14:1251032. doi: 10.3389/fpsyt.2023.1251032
Received: 04 July 2023; Accepted: 22 September 2023;
Published: 06 October 2023.
Edited by:
Nicole Schramm-Sapyta, Duke University, United StatesReviewed by:
Casey R. Guillot, University of North Texas, United StatesCopyright © 2023 Correa, Delfel, Wallace, Pelham and Jacobus. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Joanna Jacobus, amphY29idXNAaGVhbHRoLnVjc2QuZWR1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.