
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Psychiatry , 04 September 2023
Sec. Mood Disorders
Volume 14 - 2023 | https://doi.org/10.3389/fpsyt.2023.1241071
This article is part of the Research Topic Break the Mental Health Stigma: Bipolar Disorder View all 5 articles
 Manuel Gardea-Resendez1,2
Manuel Gardea-Resendez1,2 Javier Ortiz-Orendain2,3
Javier Ortiz-Orendain2,3 Alessandro Miola2,4
Alessandro Miola2,4 Manuel Fuentes Salgado2
Manuel Fuentes Salgado2 Mete Ercis2
Mete Ercis2 Brandon J. Coombes5
Brandon J. Coombes5 Peggy M. Gruhlke2
Peggy M. Gruhlke2 J. Michael Bostwick2
J. Michael Bostwick2 Ian Michel6
Ian Michel6 Jennifer L. Vande Voort2
Jennifer L. Vande Voort2 Aysegul Ozerdem2
Aysegul Ozerdem2 Alastair McKean2
Alastair McKean2 Mark A. Frye2*
Mark A. Frye2* Monica Taylor-Desir2
Monica Taylor-Desir2Background: There is evidence suggesting racial disparities in diagnosis and treatment in bipolar disorder (BD) and schizophrenia (SZ). The purpose of this study is to compare psychiatric diagnoses and psychotropic use preceding a first episode of mania (FEM) or psychosis (FEP) in racially diverse patients.
Methods: Using a comprehensive medical records linkage system (Rochester Epidemiology Project, REP), we retrospectively identified individuals diagnosed with BD or SZ and a documented first episode of mania or psychosis. Illness trajectory before FEP/FEM were characterized as the time from first visit for a mental health complaint to incident case. Pathways to care and clinical events preceding FEP/FEM were compared based on subsequent incident case diagnosis (BD or SZ) and self-reported race (White vs. non-White).
Results: A total of 205 (FEM = 74; FEP = 131) incident cases were identified in the REP. Duration of psychiatric antecedents was significantly shorter in non-White patients, compared to White patients (2.2 ± 4.3 vs. 7.4 ± 6.6 years; p < 0.001) with an older age at time of first visit for a mental health complaint (15.7 ± 6.3 vs. 11.1 ± 6.0 years; p = 0.005). There were no significant differences by race in FEM pathway to care or age of first seeking mental health. Overall non-White patients had lower rates of psychotropic use.
Conclusion: These data are unable to ascertain reasons for shorter duration of psychiatric antecedents and later age of seeking care, and more broadly first age of initial symptom presentation. If symptoms are confirmed to be earlier than first time seeking care in both groups, it would be important to identify barriers that racial minorities face to access timely psychiatric care and optimize early intervention strategies.
Many patients with bipolar disorder (BD) and schizophrenia (SZ) experience a significant diagnostic confirmation delay as early symptoms are often unrecognized and non-specific with a number of different factors that, on balance, delay treatment initiation (1–3). The heterogeneity of the clinical presentations of mood disorders (i.e., BD and major depression) and SZ, with often-overlapping symptomatology including psychotic symptoms in mania and mood symptoms in schizophrenia, challenge the concept of unique prodromes for each mental illness (4, 5). There is a controversy in the ascertainment of BD and SZ prodromes and delineating time-frame and symptom presentation preceding a first episode of mania (FEM) or psychosis (FEP) may help clarify early disease origins and trajectory of illness (6). There is consensus in the utility of prodromes, if reliably defined, for enhancing early signal detection that would facilitate rapid diagnosis or specific early surveillance of symptoms or symptom progression (7–10). In this line, retrospective assessments of pathways to care, such as mental health service utilization before a first episode, patterns of symptom endorsement and psychotropic use preceding a FEM or FEP could further contribute to the ascertainment of prodromal phases (11). However, efforts to define illness trajectories common to all BD and SZ patients, respectively, are further complicated by factors associated with health disparities and barriers to access healthcare, particularly in racially diverse individuals (12–14).
It has long been recognized that race-related factors, including but not limited to barriers to access health care, play a deleterious role in the timely diagnosis at the initial presentation of BD and SZ (13, 14). Furthermore, it has been consistently reported that non-White patients living with a mood disorder have less use of mental health care services, related, in part, to disparities in social determinants of health, discrimination, science and medical mistrust, inadequate health insurance coverage and lack of clinicians’ cultural competency, among others (15–18). However, provider-related factors such as racial biases and lack of cultural sensitivity have a more pervasive effect in symptom underestimation/overestimation and mischaracterization, increasing the risk of a subsequent misdiagnosis (19). The latter accentuates differences in selection of treatment strategies for BD and SZ, with a severe underutilization in racial minorities of psychotropics, many of which are considered first line options, including less overall use of lithium and mood stabilizing anticonvulsants and higher use to atypical and select typical antipsychotics in BD patients of African ancestry (AA), in comparison to European ancestry and a lower likelihood for Hispanic and Black patients with psychosis to receive atypical antipsychotics (16, 20, 21).
Recognizing the known racial disparities in access to care for BD and SZ, in this study we sought to retrospectively review pathways to care and longitudinal patterns of mental healthcare utilization, psychiatric diagnoses and psychotropic treatments in White and non-White individuals from 27 counties in Minnesota who progressed to meet diagnostic criteria for BD or SZ.
Subjects were identified through the Rochester Epidemiology Project (REP) which is an integrated comprehensive medical record utilized thus far for more than 2000 observational studies of acute and chronic disease incidence and outcomes, including bipolar disorder, in a defined population of Olmsted County, Minnesota and 26 additional surrounding counties. Findings from studies using the REP have shown to be extrapolated to other populations in the United States and globally (22). This population-based cohort addresses limitations observed in clinical series, with referral bias, and lack of complete case ascertainment in administrative data bases. Previous studies on schizophrenia and bipolar disorder have been performed using REP, offering long-term perspectives of cohorts with confirmed psychiatric disorders (23–26).
Inclusion criteria for the initial search were (a) patients born after 1985 who (b) diagnosed with bipolar disorder (types I or II) or schizophrenia spectrum disorders, including schizoaffective disorder, (c) between 2000 and 2019 and (d) resided in Olmsted County and surrounding counties on the date of the diagnostic code assignment. The initial search yielded 1,335 subjects who were selected for further manual screening by two psychiatrists (MG and JO-O) for diagnostic confirmation, based on DSM criteria, and for identification of individuals with a recorded first episode of mania or psychosis (FEM or FEP, respectively) in their medical charts. Disagreements in case ascertainment were solved by a panel of three senior psychiatrists (AMc, AO, and MAF). The latter search identified a total of 205 (SZ = 131; BD = 74) with a first episode recorded and were further analyzed for characterization of the illness trajectory and included for this study, while those without a clearly recorded first episode were excluded from the study. Detailed information about the specifics of the search strategy, including specific diagnostic codes used for BD and SZ, coding systems, case ascertainment, extracted data and study population has been previously published (27).
This study received approval from the institutional review boards (IRBs) of Mayo Clinic and Olmsted Medical Center, who provided a Health Insurance Portability and Accountability Act (HIPAA) waiver, in line with state, federal, and international recommendations. Due to the latter, written informed consent was not required for passive medical record review in the REP (28).
Within the REP, race and ethnicity are determined by patient self-report, and listed categories are based on the standardized classification of the National Institutes of Health (NIH) to promote uniformity of data on race and ethnicity, including an additional option for patients who refused to provide these data and one for those who self-identified with another or more than one race (29). Categories for race include American Indian or Alaska Native, Asian or Asian American (including East Asian), Black/African/African American, Native Hawaiian or Other Pacific Islander, White, Other and Unknown (i.e., unavailable data, patient refusal to specify). Categories for ethnicity include Hispanic/Latino, Not Hispanic/Latino and Unknown.
The racial and ethnic composition of the population in the REP is predominantly White but known to be representative of Minnesota and the Upper Midwest and to be similar to the overall composition of the United States’ population (28). Hence, to account for the underrepresentation of some non-White racial and ethnic groups, for this study, participants were further categorized into two broad categories: White (W), for patients of self-reporting as White and not Hispanic/Latino ethnicity, and non-White (nW), which included individuals who self-identified with any race other than White, including those who did not specify their race and/or Hispanic/Latino ethnicity.
We searched the REP and associated medical records to identify distinct types of early life traumatic experiences (e.g., physical or emotional abuse) and diagnostic codes of common child and adolescent psychiatric disorders. Assessment of substance use was defined as the utilization of any licit or illicit substance without necessarily constituting a substance use disorder (i.e., experimental use). Exposure to psychotropic medications prior to an incident case was collected through review of clinical notes and prescription registry in the REP, and medications were classified by psychotropic class (e.g., antipsychotics, antidepressants, etc.) and specific drug name.
The pathway to care start point was defined as the first encounter with a health care provider on which an International Classification of Disease (ICD) code for a psychiatric diagnosis or complaint was added to the patient’s chart, while the first episode, or endpoint, was defined as the clinical encounter in which the patient was first observed to have symptoms of psychosis or mania and received an associated diagnosis, as determined by a clinician’s assessment. The first contact with REP was defined as the first interaction with a health provider in the Olmsted County area (i.e., Mayo Clinic, Olmsted Medical Center) for any health concern.
We first compared sociodemographic and clinical variables, and rates of psychotropic prescriptions between White and non-White individuals with a known diagnosis of BD or SZ using chi-square tests (χ2) for categorical measures and two-sample t-tests for continuous measures, respectively. We then tested for differences in prodrome duration (as defined by age at first visit for a mental health complaint to age at incident), age at first medical visit and first visit for a mental health complaint, and age of first psychiatric hospitalization between the same groups using ANOVA (two-sample t-tests) or Kruskal–Wallis non-parametric ANOVA based on normality assumption. Statistical analyses were performed using Jamovi.1
We identified 205 subjects, 74 with a first episode of mania (FEM) and 131 with a first episode of psychosis (FEP); both samples were comprised mainly of men (FEM = 60.8%; FEP = 80.9%). The self-reported racial composition of the FEM group was 75.7% White, 17.6% African/African American/Black, 1.4% of Asian/Asian American, 3% as Other and 1.4% did not specified their racial background, whereas in the FEP group, 61.1% of the participants self-identified as White, 23.7% were of African/African American/Black, 8.4% as Other race, 2.3% of Asian/Asian American, 0.8% Indigenous American and 3.8% that did not specify their race (Figure 1). Of note, all of the subjects in the “Other” subgroup self-identified as Hispanic/Latino.
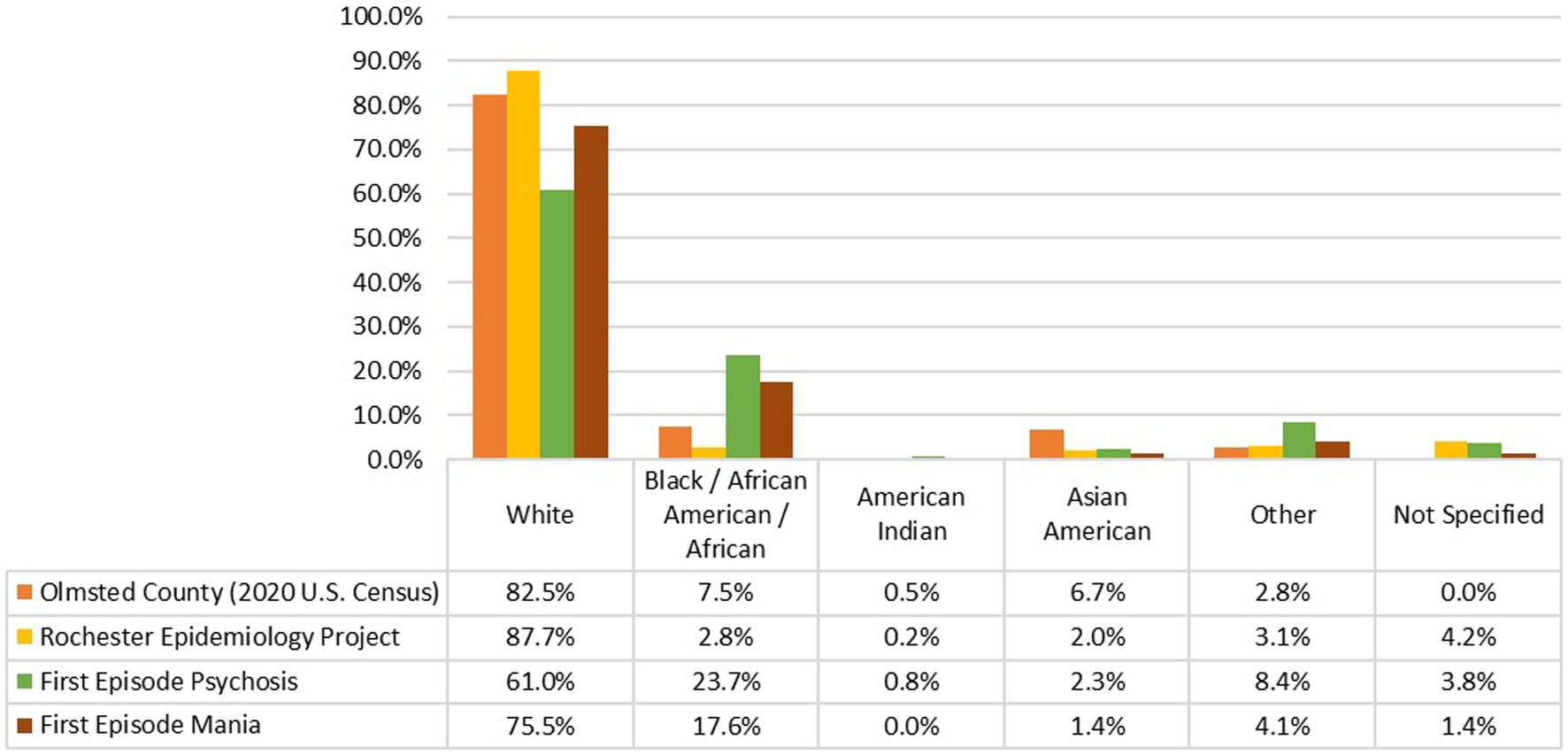
Figure 1. Comparison of the racial composition of population from Olmsted County based on the 2020 U.S. Census (30), population captured in the expanded Rochester Epidemiology Project (E-REP) (28), individuals included in this study and identified in the REP with a first episode of psychosis and, a first episode of mania.
Within the FEP group, 51% of the non-White participants (n = 26) were born outside of the United States (48% in Somalia, 16% in Sudan, 16% in Mexico, 8% in Ethiopia, 8% in Kenya and 4% in Saudi Arabia). Based on further chart review, within the foreign-born patients, 50% voluntarily immigrated to the U.S. and 26.9% arrived as refugees (forced migration), while no information regarding immigration status was found for the remaining 23.1%. Only four participants with FEM (22.2% of the non-White group) were foreign-born (Somalia), three of which arrived as refugees and one as voluntary immigrant. For both FEP and FEM, mean age (SD) at arrival to the United States of those with available data (n = 28) was 10.3 (6.5) years. In this line, childhood trauma associated with war and terrorism was significantly more common in non-White individuals with a FEP (9.8% vs. 0%; p = 0.004).
Table 1 shows the clinical features preceding a FEM or FEP divided by White and non-White participants. In general, there was increased morbidity of psychiatric diagnoses preceding a first episode of psychosis or mania in White patients. A diagnosis of attention-deficit/hyperactivity disorder in non-White individuals with a FEP was much less common when compared to White individuals (15.7% vs. 52.5%; p < 0.001). This was not observed for FEM. The same trend was observed in autism spectrum disorder before a FEP (0% vs. 8.8%; p = 0.03). No large differences in conduct disorders and oppositional defiant disorder were observed in the two cohorts.
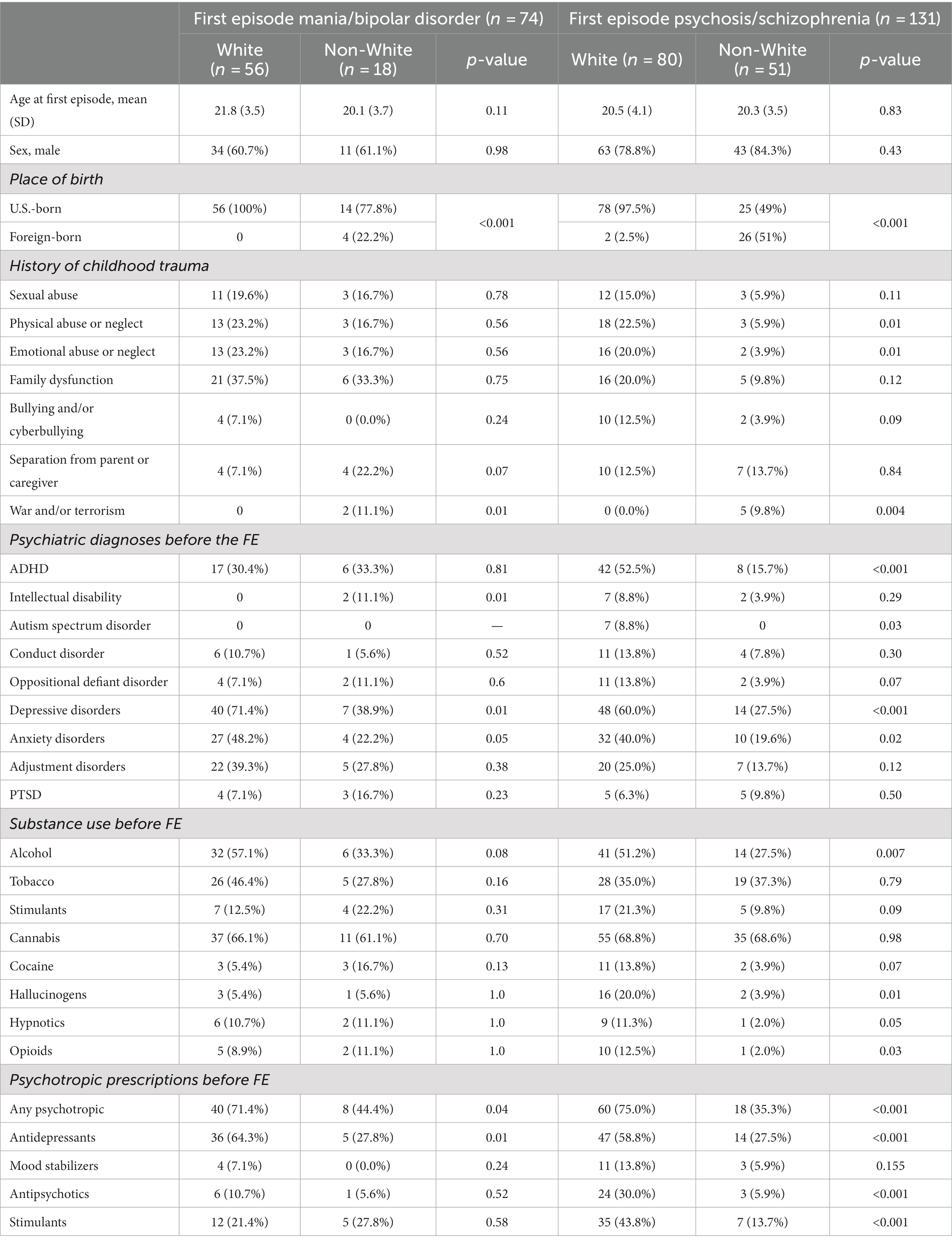
Table 1. Clinical characteristics preceding a first episode mania (FEM) or psychosis (FEP) by racial categories (White vs. non-White patients).
While depressive disorders were very frequent in both FEP and FEM, non-White patients were less frequently diagnosed with depression (FEP: 27.5% vs. 60%; p < 0.001; FEM: 38.9% vs. 71.4%; p = 0.01). A similar trend was seen in anxiety disorders in both cohorts (FEP: 19.6% vs. 40%; p = 0.02; FEM: 22.2% vs. 48.2%; p = 0.05).
Within the FEP group, physical and emotional abuse were significantly more common in White individuals, while, as mentioned previously, trauma related to war and terrorism was more common in non-White individuals from both cohorts. Nonetheless, rates of PTSD diagnosis did not significantly differ among groups albeit this diagnosis had a low prevalence prior to FEP/FEM.
With regards to substance use before a first episode, White FEP patients had a significantly higher prevalence of alcohol (51.2% vs. 27.5%; p = 0.007), hallucinogens (20% vs. 3.9%; p = 0.01), hypnotics (11.3% vs. 2%; p = 0.05) and opioid use (12% vs. 2%; p = 0.03). While limited by a lower sample size, In FEM, a similar trend was seen for alcohol use, while the opposite was seen for the rest of the assessed substances, where substance use was more common in non-White individuals; these findings, however, were not significant and limited by a lower sample size.
Overall, psychotropic prescriptions before a first episode were significantly more common in White patients who developed a FEM or a FEP than in non-White patients (FEM 71.4% vs. 44.4%, p = 0.04; FEP 75% vs. 35.3%, p < 0.001). After stratifying by psychotropic groups, differences between racial categories were still statistically significant, particularly in FEP. Antidepressant use before a FEM was significantly more common in White patients (64.3% vs. 27.8%, p = 0.01); the same prescription trend was observed in FEP (58.8% vs. 27.5%, p < 0.001). Antipsychotic use before a FEP was also significantly more common in White individuals (30% vs. 5.9%, p < 0.001) and so were stimulant prescriptions (43.8% vs. 13.7%, p < 0.001); no significant differences were observed in antipsychotic and stimulant use before a FEM. Mood stabilizer use before a first episode was uncommon in all groups.
Table 2 shows the illness trajectories preceding a FEM or FEM in White and non-White patients. Non-White patients from both cohorts (FEM and FEP), when compared to White patients, began receiving health care at Olmsted County (as defined by age of first contact with REP) at a significantly older age (BD: 7.4 ± 7.3 vs. 4.5 ± 8.6; p = 0.01; SZ: 11.5 ± 7.4 VS. 3.3 ± 5.9; p < 0.001). Age at the time of a first episode did not vary between groups in both patients with psychosis and with mania and was consistent with the ages of onset reported in the literature (4). However, the overall duration of the prodrome (i.e., time from first visit for a mental health complaint to incident case) was significantly shorter in non-White individuals with a FEP, when compared to White individuals (2.2 ± 4.3 vs. 7.4 ± 6.6 years; p < 0.001); no significant differences were observed in the prodrome duration for bipolar patients. Similarly, non-White patients who further developed a FEP had their first visit for a psychiatric complaint (prodrome onset) at a significantly older age than White patients (15.7 ± 6.3 vs. 11.1 ± 6.0 years; p = 0.005). No significant differences were observed in the age of first psychiatric hospitalization for both cohorts (BD and SZ). However, hospitalization before first episode was uncommon in both cohorts (BD = 17; SZ = 21).
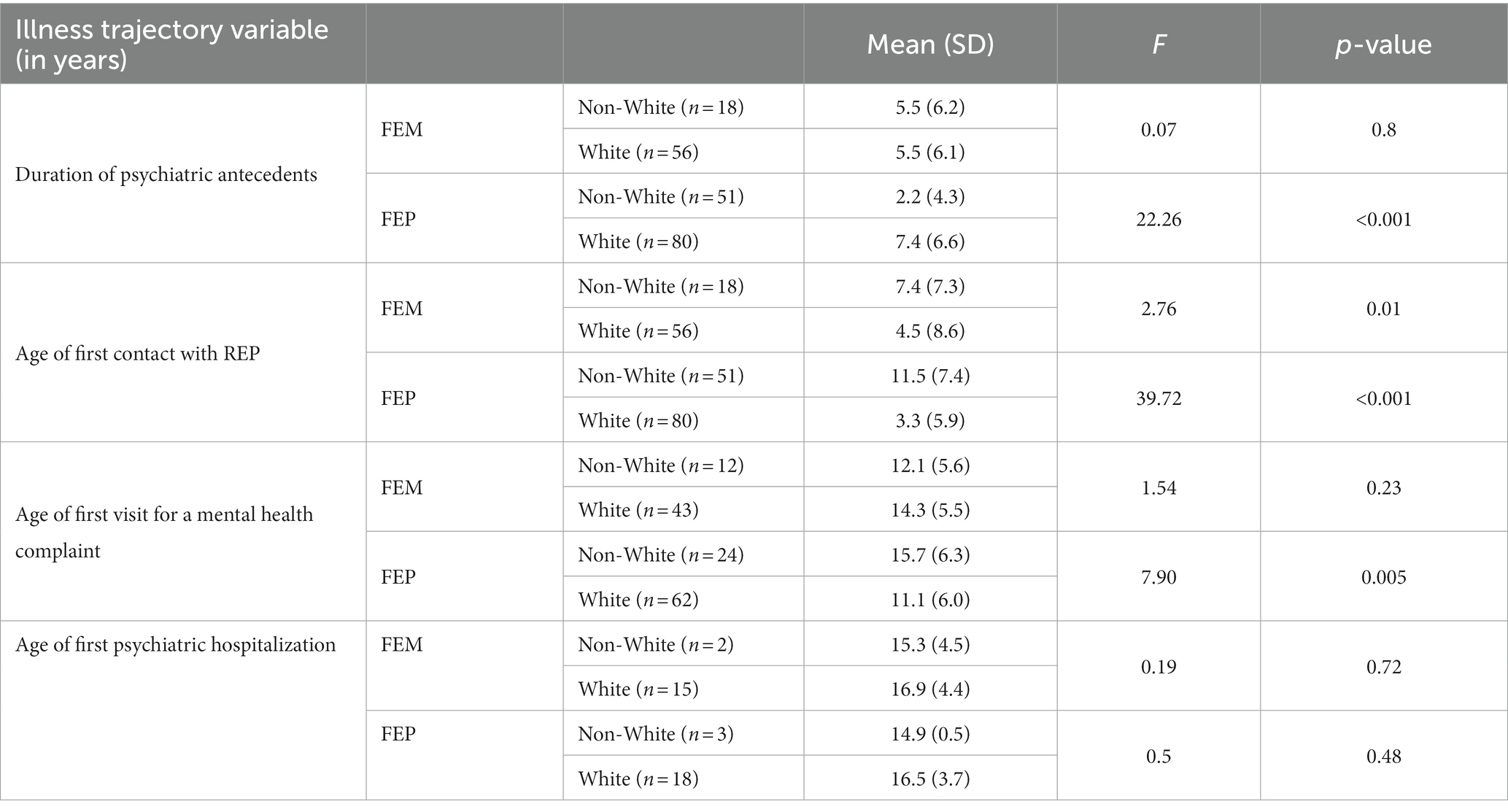
Table 2. Illness trajectory preceding a first episode mania (FEM) or psychosis (FEP) by racial/ethnic categories (White vs. non-White patients).
To our knowledge, this is the first study using representative data from a community sample to compare racial differences in pathways to care, conceptualized from clinical events and psychiatric care (i.e., diagnoses, psychotropic use, mental health service utilization) preceding a first episode of mania or psychosis. In a U.S. patient database built upon a medical records-linkage system, non-White patients with a known diagnosis of schizophrenia, when compared to White patients, had a significantly shorter duration of the pathways to care, as defined by the time from the first visit for a mental health complaint to the incident case (FEP). This shortened duration appears to be driven, among other factors, by a first mental health-related clinical contact at a significantly older age than White patients. As a potential consequence of this delayed initiation in psychiatric care, particularly in SZ, prodromal phases in non-White patients were characterized by fewer psychiatric diagnoses and lower rates of psychotropic utilization in comparison to White patients. While these some of these differences were not statistically significant in patients with bipolar disorder, the trends were somewhat similar. Furthermore, White patients from both cohorts had their first contact with the health care system in Olmsted County at a significantly earlier age than non-White patients.
The present study has several strengths. First, by focusing on the prodromal phases of bipolar disorder and schizophrenia in racially diverse groups specifically, we addressed an important gap in the literature, offering insights into the pathways to care and clinical experiences that precede an incident case of mania or psychosis in patients of racially diverse backgrounds, enabling a better of understanding of the lived experiences and barriers that minoritized individuals face when seeking mental health care. Second, all cases were individually assessed and had the diagnosis and date of first episode manually confirmed by psychiatrist chart review providing higher diagnostic validity and reliability. In this line, the use of REP resources enabled an extensive follow-up from first contact with the local healthcare providers until incident case of mania or psychosis, allowing for a retrospective assessment of a well-defined population-based cohort while addressing the risk of recall bias (23).
Our finding of a significantly shorter duration of the pathways to care in non-White patients with a FEP, rather than corresponding to a race-specific variation of symptom presentation, may suggest that racially diverse patients experience an aversive pathway to care (i.e., health mistrust, lack of insurance coverage, etc.) that leads to a subsequent delay in the first contact with health services for psychiatric complaints. While, at first sight, the lack of variations at age of first episode in both BD or SZ might suggest that the illness onset was not impacted by the delayed initiation of mental health care, further assessment of the symptom severity of the first episode and the clinical setting (emergency room, outpatient/inpatient clinics, etc.) where it was diagnosed may provide a more comprehensive and accurate assessment of the impact of delayed care. Restricted access to care, which disproportionately impacts racial and ethnic minorities, inevitably prolongs the duration of untreated illness, which has been associated with worse symptomatic and functional outcomes and subsequent illness trajectories of bipolar disorder and schizophrenia (31, 32). Barriers to access timely mental healthcare combined with other racial biases that non-White patients with severe mental illnesses experience can lead to more severe clinical presentations that can further increase the likelihood of an initial misdiagnosis (17). In this line, earlier initiation of psychiatric care and more frequent use of health services may account for the higher prevalence of psychiatric disorders preceding a first episode in White patients seen in our study, whereas the opposite was observed in non-White patients. This hypothesis is further supported by findings from a study conducted using a commercial claims database and focused on health care use before a FEP, which reported lower behavioral health care use rates and outpatient visits in Hispanic and Black patients, when compared to White patients. Similarly, in this study, a lower likelihood of receiving a comorbid psychiatric disorder before a FEP was observed in Black and Hispanic patients (12). Although our study design does not allow the establishment of causality inferences, the coincidence of our findings with the existing body of evidence supports the notion that non-White patients may experience barriers to access timely psychiatric care before an incident case of mania or psychosis resulting in fewer psychiatric diagnoses and lower psychotropic use (11, 17, 33).
Psychotropic medication use before a first episode was significantly lower in racially diverse patients from both of our study groups. This finding was consistent across all psychotropic categories except mood stabilizers. In particular, antidepressant prescriptions were significantly lower in non-White patients which is particularly relevant considering the high rates of depression preceding an index (hypo)manic episode and the frequency of a depressive index episode (over 50% of the cases) (34). However, in our cohort, diagnosis of depressive disorders was significantly more common in White patients from both groups. Considering that the age of FEM did not vary significantly between racial groups despite the differential exposure to antidepressants, there is value in further analyzing if early exposure to antidepressants, or lack thereof, has an impact, either preventive or precipitating, in the onset of a first (hypo)manic episode. A similar assessment focused on the controversy of risk of conversion to psychosis in high-risk subjects exposed to antipsychotics might also provide further data on the disease-modifying effect of neuroleptics (35, 36). Our finding of lower psychotropic use before a first episode aligns with previous studies reporting that among youths with psychiatric complaints, those from racial minority groups, particularly individuals who self-identify as Black, Latino or Asian, are less likely than White individuals to be prescribed psychotropic medications when impaired (37–39). This trend towards lesser prescription of specific psychotropics in non-White adolescents with BD and SZ tends to persist and exacerbate in adulthood, even in well-established illness, were, as previously mentioned, lower rates of lithium and antiepileptic mood stabilizers utilization in African American individuals with BD have been reported, despite lithium being a gold-standard treatment, and persistently higher rates of first-generation antipsychotics in BD and SZ, at the expense of lower atypical antipsychotic use (16, 40, 41). These differences in psychotropic use occur in spite of the increasing evidence supporting their clinical applications and higher tolerability, deviating from psychotropic prescription trends and omitting FDA approvals and clinical guidelines (42). While multifactorial, the origins of these differential prescription patterns have been linked to race-related disparities, including clinicians’ implicit ethnic/racial biases, structural racism, misattribution of sociocultural expressions and behaviors as manifestations of psychopathology arising from the lack of cultural competency, and it’s reasonable to hypothesize that this affects individuals seeking help during prodromal phases of BD and SZ in a similar fashion (11, 43).
While our study offers insights into potential health disparities in non-White patients before a first episode of mania or psychosis, this study has several limitations that need to be considered. In merging individuals of other than White racial backgrounds into one large group (non-White patients) there is a risk of overlooking the unique experiences of each racial group. This decision was made in order to address the relatively small sample size of certain racial groups, a consequence of the racial composition of Olmsted County. Because some patients in the different cohorts were not born in Olmsted County, Minnesota and moved in later, this might have altered the age of first contact with the regional health system. The retrospective design of this study entails several risks of bias including selection bias; however, the REP addresses limitations known to administrative registry-based databases, which are frequently passively fed with diagnoses and procedures, by including longitudinal comprehensive medical information from individual medical records (44). Third, the lack of a standardized definition for prodromes in, both, bipolar disorder and schizophrenia represents a significant challenge for studies assessing clinical events preceding an incident case; we sought to reduce the risk of recall bias by relying on clinical encounters to conceptualize pathways to care, however this approach might omit early mild or subclinical symptoms preceding a first episode. Finally, while 51% of our non-White FEP patients were born outside of the U.S., and recognizing that migration and forced displacement are well-known social risk factors for psychosis and mood disorders and that immigrants and refugees are at higher risk of marginalization and cumulative trauma, among other environmental stressors, we did not conducted a detailed assessment of this cases (i.e., country of birth, age at migration, type of displacement, etc.) that might have helped examine the ways in which risk of severe mental illness intersects with race and migration (45, 46). Our findings suggest race differences in the pathways to care and patterns of psychotropic utilization preceding a first episode of mania or psychosis, specifically an overall lower use of health services and psychotropic medications in non-White patients. While in our study we did not examine the drivers of this delayed treatment initiation in non-White patients, we are aware that, in the U.S., racial minorities with mental health illnesses experience systemic and structural barriers that make timely and affordable access to healthcare and behavioral healthcare difficult, which, in consequence increases the duration of untreated illness and the likelihood of a worse course of illness and adverse outcomes (11, 18). Hence, in the conceptualization of prodromal phases for BD and SZ, it may prove not only advantageous but necessary to integrate racial disparities in healthcare as social risk markers that might exacerbate the diathesis for these disorders and obstruct the identification of at-risk subjects or early-onset disease. Future studies mapping prodromal trajectories of bipolar disorder and schizophrenia must further explore the cause of these racial differences in order to enable the recognition, and subsequent correction, of the adverse lived experiences and health disparities that racial and ethnic minorities face when seeking mental health care.
The data analyzed in this study is subject to the following licenses/restrictions: datasets are not available in order to protect patient confidentiality. Requests to access these datasets should be directed to Z2FyZGVhcmVzZW5kZXoubWFudWVsYW5kcmVzQG1heW8uZWR1.
The studies involving humans were approved by Mayo Clinic Institutional Review Board, Olmstead Medical Center Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
MG-R, AMi, MAF, and JO-O: writing and original draft preparation. MG-R, JO-O, AMi, MFS, ME, BC, PG, MB, IM, JV, AO, AMc, MAF, and MT-D: critical revision of the article contributing with ideas related to their area of expertise. MG-R, JO-O, and PG: data collection. AMi: statistical analysis. MG-R, AMi, BC, JV, JO-O, MAF, MB, MT-D: analysis and interpretation. MG-R, MAF, and BC: contribution to conceptualization. All authors contributed to the article and approved the submitted version.
This study was supported, in part, by the Luther Automotive Foundation and Mayo Foundation; neither had a role in the design, conduct, analysis, or submission of the study. This study was also made possible using the resources of the Rochester Epidemiology Project, which is supported by the National Institute on Aging of the National Institutes of Health under Award Number R01AG034676. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Lublóy, Á, Keresztúri, JL, Németh, A, and Mihalicza, P. Exploring factors of diagnostic delay for patients with bipolar disorder: a population-based cohort study. BMC Psychiatry. (2020) 20:75. doi: 10.1186/s12888-020-2483-y
2. Hirschfeld, RMA, Lewis, L, and Vornik, LA. Perceptions and impact of bipolar disorder: how far have we really come? Results of the National Depressive and Manic-Depressive Association 2000 survey of individuals with bipolar disorder. J Clin Psychiatry. (2003) 64:161–74. doi: 10.4088/JCP.v64n0209
3. Vanasse, A, Courteau, J, Courteau, M, Roy, MA, Stip, E, Fleury, MJ, et al. Multidimensional analysis of adult patients’ care trajectories before a first diagnosis of schizophrenia. Schizophrenia. (2022) 8:52. doi: 10.1038/s41537-022-00256-6
4. Carvalho, AF, Firth, J, and Vieta, E. Bipolar disorder. N Engl J Med. (2020) 383:58–66. doi: 10.1056/NEJMra1906193
5. Vieta, E, Berk, M, Schulze, TG, Carvalho, AF, Suppes, T, Calabrese, JR, et al. Bipolar disorders. Nature. (2018) 4:18008. doi: 10.1038/nrdp.2018.8
6. Geoffroy, PA, and Scott, J. Prodrome or risk syndrome: what’s in a name? Int J Bipolar Disord. (2017) 5:7. doi: 10.1186/s40345-017-0077-5
7. Correll, CU, Hauser, M, Penzner, JB, Auther, AM, Kafantaris, V, Saito, E, et al. Type and duration of sybsyndromal symptoms in youth with bipolar I disorder prior to their first manic episode. Bipolar Disord. (2014) 16:478–92. doi: 10.1111/bdi.12194
8. Faedda, GL, Baldessarini, RJ, Marangoni, C, Bechdolf, A, Berk, M, Birmaher, B, et al. An International Society of Bipolar Disorders task force report: precursors and prodromes of bipolar disorder. Bipolar Disord. (2019) 21:720–40. doi: 10.1111/bdi.12831
9. Fusar-Poli, P, Sullivan, SA, Shah, JL, and Uhlhaas, PJ. Improving the detection of individuals at clinical risk for psychosis in the community, primary and secondary care: an integrated evidence-based approach. Front Psychiatry. (2019) 10:1–16. doi: 10.3389/fpsyt.2019.00774
10. Hafeman, DM, Merranko, J, Axelson, D, Goldstein, BI, Goldstein, T, Monk, K, et al. Toward the definition of a bipolar prodrome: dimensional predictors of bipolar spectrum disorders in at-risk youths. Am J Psychiatry. (2016) 173:695–704. doi: 10.1176/appi.ajp.2015.15040414
11. Oluwoye, O, Davis, B, Kuhney, FS, and Anglin, DM. Systematic review of pathways to care in the U.S. for Black individuals with early psychosis. NPJ Schizophr. (2021) 7:58. doi: 10.1038/s41537-021-00185-w
12. Heun-Johnson, H, Menchine, M, Axeen, S, Lung, K, Claudius, I, Wright, T, et al. Association between race/ethnicity and disparities in health care use before first-episode psychosis among privately insured young patients. JAMA Psychiatry. (2021) 78:311–9. doi: 10.1001/jamapsychiatry.2020.3995
13. Strakowski, SM, McElroy, SL, Keck, PE, and West, SA. Racial influence on diagnosis in psychotic mania. J Affect Disord. (1996) 39:157–62. doi: 10.1016/0165-0327(96)00028-6
14. Mukherjee, S, Shukla, S, Woodle, J, Rosen, AM, and Olarte, S. Misdiagnosis of schizophrenia in bipolar patients: a multiethnic comparison. Am J Psychiatry. (1983) 140:1571–4. doi: 10.1176/ajp.140.12.1571
15. Gardea-Resendez, M, Taylor-Desir, MJ, Romo-Nava, F, Bond, D, Vallender, EJ, Cuellar-Barboza, AB, et al. Clinical phenotype of tardive dyskinesia in bipolar disorder. J Ciln Psychopharmacol. (2022) 42:159–62. doi: 10.1097/JCP.0000000000001532
16. Akinhanmi, M, El-Amin, S, Balls-Berry, JE, Vallender, EJ, Ladner, M, Geske, J, et al. Decreased core symptoms of mania and utilization of lithium/mood stabilizing anticonvulsants in U.S. bipolar I patients of African vs European ancestry. J Affect Disord. (2020) 260:361–5. doi: 10.1016/j.jad.2019.09.022
17. Akinhanmi, MO, Biernacka, JM, Strakowski, SM, McElroy, SL, Balls Berry, JE, Merikangas, KR, et al. Racial disparities in bipolar disorder treatment and research: a call to action. Bipolar Disord. (2018) 20:506–14. doi: 10.1111/bdi.12638
18. Faber, SC, Khanna Roy, A, Michaels, TI, and Williams, MT. The weaponization of medicine: early psychosis in the Black community and the need for racially informed mental healthcare. Front Psychiatry. (2023) 14:1098292. doi: 10.3389/fpsyt.2023.1098292
19. Strakowski, SM, Keck, PE, Arnold, LM, Collins, J, Wilson, RM, Fleck, DE, et al. Ethnicity and diagnosis in patients with affective disorders. J Clin Psychiatry. (2003) 64:747–54. doi: 10.4088/JCP.v64n0702
20. Salcedo, S, McMaster, KJ, and Johnson, SL. Disparities in treatment and service utilization among Hispanics and non-Hispanic Whites with bipolar disorder. J Racial Ethn Health Disparities. (2017) 4:354–63. doi: 10.1007/s40615-016-0236-x
21. Herbeck, DM, West, JC, Ruditis, I, Duffy, FF, Fitek, DJ, Bell, CC, et al. Variations in use of second-generation antipsychotic medication by race among adult psychiatric patients. Psychiatr Serv. (2004) 55:677–84. doi: 10.1176/appi.ps.55.6.677
22. St Sauver, JL, Grossardt, BR, Leibson, CL, Yawn, BP, Melton, LJ, and Rocca, WA. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc. (2012) 87:151–60. doi: 10.1016/j.mayocp.2011.11.009
23. Capasso, RM, Lineberry, TW, Bostwick, JM, Decker, PA, and St Sauver, JL. Mortality in schizophrenia and schizoaffective disorder: an Olmsted County, Minnesota cohort: 1950–2005. Schizophr Res. (2008) 98:287–94. doi: 10.1016/j.schres.2007.10.005
24. Foroughi, M, Medina Inojosa, JR, Lopez-Jimenez, F, Saeidifard, F, Suarez, L, Stokin, GB, et al. Association of bipolar disorder with major adverse cardiovascular events: a population-based historical cohort study. Psychosom Med. (2021) 84:97–103. doi: 10.1097/PSY.0000000000001017
25. Palmer, BA, Pankratz, VS, and Bostwick, JM. The lifetime risk of suicide in schizophrenia: a reexamination. Arch Gen Psychiatry. (2005) 62:247–53. doi: 10.1001/archpsyc.62.3.247
26. Prieto, ML, Schenck, LA, Kruse, JL, Klaas, JP, Chamberlain, AM, Bobo, WV, et al. Long-term risk of myocardial infarction and stroke in bipolar I disorder: a population-based cohort study. J Affect Disord. (2016) 194:120–7. doi: 10.1016/j.jad.2016.01.015
27. Ortiz-Orendain, J, Gardea-Resendez, M, Castiello-de Obeso, S, Golebiowski, R, Coombes, BJ, Gruhlke, PM, et al. Antecedents to first episode psychosis and mania: comparing the prodromes of schizophrenia and bipolar disorder in a retrospective population cohort: antecedents of schizophrenia and bipolar disorder. J Affect Disord. (2023) 340:25–32. doi: 10.1016/j.jad.2023.07.106
28. Rocca, WA, Grossardt, BR, Brue, SM, Bock-Goodner, CM, Chamberlain, AM, Wilson, PM, et al. Data resource profile: expansion of the Rochester Epidemiology Project medical records-linkage system (E-REP). Int J Epidemiol. (2018) 47:368–368J. doi: 10.1093/ije/dyx268
29. National Institutes of Health. (2001). NIH policy on reporting race and ethnicity data: subjects in clinical research (NOT-OD-01-053).
30. United States Census: Olmsted County, Minnesota (2020). Available at: https://www.census.gov/quickfacts/fact/table/olmstedcountyminnesota/BZA110220
31. Baeza, I, de la Serna, E, Mezquida, G, Cuesta, MJ, Vieta, E, Amoretti, S, et al. Prodromal symptoms and the duration of untreated psychosis in first episode of psychosis patients: what differences are there between early vs. adult onset and between schizophrenia vs. bipolar disorder? Eur Child Adolesc Psychiatry. (2023). doi: 10.1007/s00787-023-02196-7
32. Clarke, M, Whitty, P, Browne, S, McTigue, O, Kamali, M, Gervin, M, et al. Untreated illness and outcome of psychosis. Br J Psychiatry. (2006) 189:235–40. doi: 10.1192/bjp.bp.105.014068
33. Shim, RS. Dismantling structural racism in psychiatry: a path to mental health equity. Am J Psychiatry. (2021) 178:592–8. doi: 10.1176/appi.ajp.2021.21060558
34. O’Donovan, C, and Alda, M. Depression preceding diagnosis of bipolar disorder. Front Psychiatry. (2020) 11:1–9. doi: 10.3389/fpsyt.2020.00500
35. Preti, A, Raballo, A, Meneghelli, A, Cocchi, A, Meliante, M, Barbera, S, et al. Antipsychotics are related to psychometric conversion to psychosis in ultra-high-risk youth. Early Interv Psychiatry. (2022) 16:342–51. doi: 10.1111/eip.13158
36. Zeng, J, Raballo, A, Gan, R, Wu, G, Wei, Y, Xu, L, et al. Antipsychotic exposure in clinical high risk of psychosis: empirical insights from a large cohort study. J Clin Psychiatry. (2022) 83:21m14092. doi: 10.4088/JCP.21m14092
37. Cook, BL, Carson, NJ, Kafali, EN, Valentine, A, Rueda, JD, Coe-Odess, S, et al. Examining psychotropic medication use among youth in the U.S. by race/ethnicity and psychological impairment. Gen Hosp Psychiatry. (2017) 45:32–9. doi: 10.1016/j.genhosppsych.2016.12.004
38. Cummings, JR, and Druss, BG. Racial/ethnic differences in mental health service use among adolescents with major depression. J Am Acad Child Adolesc Psychiatry. (2011) 50:160–70. doi: 10.1016/j.jaac.2010.11.004
39. Kirby, JB, Hudson, J, and Miller, GE. Explaining racial and ethnic differences in antidepressant use among adolescents. Med Care Res Rev. (2010) 67:342–63. doi: 10.1177/1077558709350884
40. Cook, TB, Reeves, GM, Teufel, J, and Postolache, TT. Persistence of racial disparities in prescription of first-generation antipsychotics in the USA: racial disparities in prescription of antipsychotics. Pharmacoepidemiol Drug Saf. (2015) 24:1197–206. doi: 10.1002/pds.3819
41. Taylor-Desir, MJ, Balls-Berry, JE, McElroy, SL, Bond, DJ, Vallender, EJ, Ladner, M, et al. Comparison of demographic and clinical features of bipolar disorder in persons of African and European ancestry. J Racial Ethn Health Disparities. (2022) 10:367–72. doi: 10.1007/s40615-022-01228-3
42. Tchikrizov, V, Ladner, ME, Caples, FV, Morris, M, Spillers, H, Jordan, CD, et al. Health disparities in the treatment of bipolar disorder. Pers Med Psychiatry. (2023) 37-38:100101. doi: 10.1016/j.pmip.2023.100101
43. Jegarl, AM, Jegede, O, Isom, J, Ciarleglio, N, and Black, C. Psychotic misdiagnosis of racially minoritized patients: a case-based ethics, equity, and educational exploration. Harv Rev Psychiatry. (2023) 31:28–36. doi: 10.1097/HRP.0000000000000353
44. Kremers, HM, Myasoedova, E, Crowson, CS, Savova, G, Gabriel, SE, and Matteson, EL. The Rochester epidemiology project: exploiting the capabilities for population-based research in rheumatic diseases. Rheumatology. (2011) 50:6–15. doi: 10.1093/rheumatology/keq199
45. Anglin, DM, Ereshefsky, S, Klaunig, MJ, Bridgwater, MA, Niendam, TA, Ellman, LM, et al. From womb to neighborhood: a racial analysis of social determinants of psychosis in the United States. Am J Psychiatry. (2021) 178:599–610. doi: 10.1176/appi.ajp.2020.20071091
Keywords: first episode mania, first episode psychosis, prodrome, bipolar disorder, schizophrenia
Citation: Gardea-Resendez M, Ortiz-Orendain J, Miola A, Fuentes Salgado M, Ercis M, Coombes BJ, Gruhlke PM, Bostwick M, Michel I, Vande Voort JL, Ozerdem A, McKean A, Frye MA and Taylor-Desir M (2023) Racial differences in pathways to care preceding first episode mania or psychosis: a historical cohort prodromal study. Front. Psychiatry. 14:1241071. doi: 10.3389/fpsyt.2023.1241071
Received: 16 June 2023; Accepted: 16 August 2023;
Published: 04 September 2023.
Edited by:
Arghya Pal, AII India Institute of Medical Sciences, Raebareli, IndiaReviewed by:
Rakesh Karmacharya, Harvard University, United StatesCopyright © 2023 Gardea-Resendez, Ortiz-Orendain, Miola, Fuentes Salgado, Ercis, Coombes, Gruhlke, Bostwick, Michel, Vande Voort, Ozerdem, McKean, Frye and Taylor-Desir. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mark A. Frye, bWZyeWVAbWF5by5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.