
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Psychiatry, 29 September 2023
Sec. Autism
Volume 14 - 2023 | https://doi.org/10.3389/fpsyt.2023.1238116
This article is part of the Research TopicWomen in Psychiatry 2023: AutismView all 11 articles
Emotion dysregulation (ED) is a transdiagnostic difficulty prevalent in autism spectrum condition (ASC). Importantly, recent research has suggested that ED is involved in self-harm and suicidality. Pre-existing models on the etiology of ED in ASC focus mainly on biological factors to ASC features, such as sensory sensitivities, poor flexibility, and sensitivity to change. However, although psychosocial factors seem to play a role in the emergence of ED in ASC as well (e.g., childhood maltreatment and camouflaging), there is a lack of a comprehensive model conceptualizing biosocial factors involved in ED in autistic people. Linehan’s biosocial model (1993) is one of the leading etiological models of ED in borderline personality disorder (BPD). It conceptualizes ED as emerging from transactions between a pre-existing emotional vulnerability in the child and an invalidating developmental environment. Beyond its clinical relevance, Linehan’s model has gathered empirical evidence supporting its pertinence in BPD and in other psychiatric disorders. Although ASC and BPD are two distinct diagnoses, because they may share ED, Linehan’s biosocial model might be useful for understanding the development of ED in ASC. Hence, this article aims to provide an application and extension of Linehan’s model to conceptualize ED in ASC. To do so, we conducted a narrative review of the literature on ED and its underlying factors in ASC from a developmental perspective. To investigate the pertinence of the biosocial model applied to ED in autistic people, we were interested on data on (i) ED and its behavioral correlates in ASC, in relation to the biosocial model, (ii) the potential biological and psychosocial correlates of ED in ASC and (iii) the overlapping difficulties in ASC and BPD. Finally, to assess the pertinence of the model, we applied it to the case of an autistic woman presenting with ED and suicidal behaviors. Our review and application to the case of an autistic woman suggest that ED in ASC encompasses factors related to both biological and psychosocial risk factors as conceptualized in the BPD framework, although in both domains ASC-specific factors might be involved.
Emotion dysregulation (ED) refers to emotional experience and/or expression that interferes with appropriate goal-directed behavior (1). ED has been widely studied in borderline personality disorder [BPD; (2, 3)]. Linehan’s biosocial theory (1993), one of the leading etiological models of BPD, places ED at the core of the disorder. Linehan’s theory conceptualizes ED as emerging from transactions between emotional vulnerability and an invalidating developmental environment (4, 5). Emotional vulnerability refers to biological factors with a genetic basis evidenced by disruptions in the emotional system involving different brain areas (e.g., prefrontal regions and amygdala) (6). Linehan’s theory has subsequently added temperamental impulsivity as an additional risk factor for BPD (4). Emotional vulnerability results in dysfunctions in three dimensions: (a) emotional hypersensitivity (i.e., low threshold for emotional reactions), (b) hyperreactivity (i.e., increased change in emotional intensity and extreme reactions), and (c) a slow return to emotional baseline (i.e., long-lasting emotional reactions) (6, 7). Invalidation, on the other hand, refers to the inadequate responses of the environment to the emotional needs of the child (5). It may occur through the neglect, minimization or punishment of the child’s emotional experience, but also through physical and sexual abuse (4, 8). According to Linehan’s theory, in people presenting with emotional vulnerability, early invalidation may result in maladaptive coping (i.e., self-harm with or without suicidal intent) when they are faced with difficult emotions (9, 10). An important corollary of this biosocial perspective is that, during their development, people with BPD did not learn the adaptive skills to regulate their emotions effectively. Hence, they may display rigid and pervasive dysfunctional strategies that were involuntarily targets of operant conditioning (e.g., “mom listens to me and is nice when I cut myself”; “dad says that it is stupid to cry”) or modeling (5). Therefore, as adults, people with BPD lack the skills to regulate their emotions, as they were taught that emotional reactions are not to be trusted (i.e., they self-invalidate) and that emotions are dangerous and should be escaped or avoided (e.g., using crisis behaviors or emotional avoidance) (5). Importantly, Linehan developed dialectical behavior therapy (DBT), the treatment targeting ED with the most empirical support, based on this model (11, 12).
Some empirical studies have tested Linehan’s model in BPD [(e.g., 13, 14)]. Although it is not consensual, the model has amassed considerable evidence in its support. For instance, Reeves et al. (14) found that emotional vulnerability and ED were substantially associated with BPD symptoms, with ED mediating the relationship between emotional vulnerability and BPD symptoms. In addition, Carpenter and Trull (2) gathered findings supporting the role of biological factors such as emotion sensitivity and lability in the emergence of BPD. Interestingly, studies have supported the role of emotional hypersensitivity and slow return to baseline but not hyperreactivity in the emotional vulnerability found in people with BPD (6, 7). Regarding invalidation, Reeves et al. (14) found that parental invalidation in childhood does not predict BPD, while other findings have come to opposite conclusions (15–17), particularly concerning the involvement of maternal invalidation (18). Beyond the association between parental invalidation and BPD, cultural and intra-individual factors seem to be involved in the emergence of BPD. For instance, Keng and Soh (18) found that the association between self-reported maternal invalidation and BPD was moderated by two cultural factors: self-construal (i.e., the extent to which the self is defined independently of others or interdependently with others) and conformity to norms (18). In addition, Keng and Wong (16) showed that low levels of self-compassion were associated with BPD independently of parental invalidation. Finally, regarding the transaction between emotional vulnerability and invalidation, some studies support the transaction (4, 19) while others do not (13).
ED is strongly associated with BPD (3). However, several recent findings suggest that ED is a transdiagnostic mechanism of psychopathology (20–24). Although Linehan’s model has not been directly studied outside BPD, findings support the involvement of biological vulnerability and invalidation in the emergence of ED in various psychiatric disorders (25), including trait impulsivity (26), and childhood maltreatment (linked to invalidation) (27–29).
In autism spectrum condition (ASC),1 there has been a growing interest in overlapping difficulties with BPD, including ED (32, 33). Indeed, there is a considerable overlap in the diagnostic criteria for ASC and BPD (e.g., difficulties in social interactions) (34), which increases the risk of misdiagnosis, especially in women (35, 36). The high prevalence of ED in autistic individuals [e.g., between 50 and 60% in autistic youth; (37–39)] and its association with self-harm and suicidal behaviours (40, 41) may be an additional source of misdiagnosis with BPD (42). Indeed, autistic people presenting with ED and self-harm are reported to be at greater risk of being misdiagnosed with BPD since these difficulties are strongly associated with BPD (36, 42). It should also be noted that ASC and BPD can co-occur (34), with the co-occurrence being linked to higher suicidality than in BPD or ASC alone (43–45).
Few studies have investigated the etiological factors involved in ED in ASC, and most have focused exclusively on the role of ASC-related factors [(e.g., 38, 39, 46)]. Thus, to our knowledge, no studies have attempted to conceptualize ED in ASC in relation to Linehan’s model. This is of special relevance given the emerging interest in DBT to treat ED in ASC (47, 48). Indeed, recently, DBT has been found to be feasible and acceptable in autistic adults without intellectual disability (49, 50). In those with self-harm and suicidal behaviours, initial evidence suggests that DBT is effective in reducing ED (49). Nevertheless, to improve the pertinence of DBT to autistic individuals, it is of the utmost importance to provide treatments that consider the specific features potentially involved in ED in this population (51).
Case formulation is central to effectively implement behavioral treatments (52). Linehan’s biosocial model provides a theoretical framework to inform case formulation when treating clients with BPD. However, it is still unknown whether it might also apply to autistic adults. This is crucial since DBT is in its early stages in ASC and that ED in autistic people is still poorly understood (32).
This article aims to provide an application of Linehan’s model to conceptualize ED in ASC. To do so, we conducted a narrative review of the literature on ED and its underlying factors in ASC across the lifespan. Indeed, narrative reviews are well suited to address research questions with a broad scope to draw conclusions and generate areas for future research questions (53, 54). To investigate the pertinence of the biosocial model applied to the ED found in autistic people, we were interested on data on (i) ED and its behavioral correlates in ASC, in relation to the biosocial model, (ii) the potential biological and psychosocial correlates of ED in ASC and (iii) the overlapping difficulties in ASC and BPD. Finally, to assess the pertinence of the model, we applied it to the case of an autistic woman presenting with ED and suicidal behaviours.
Our review was conducted using PubMed, Medline Ovid SP and PsycINFO search engines. Articles had to meet the following inclusion criteria: (a) articles published after 2000, (b) articles in English, (c) articles published in a peer-reviewed journal (d) articles interested in autistic individuals without intellectual disability and/or individuals with BPD. Given that our approach was developmental, we included articles on ED and its correlates in both youth and adults with these diagnoses. Hence, we specify throughout our review whether the findings relate to youth or adults. Our articles research paired keywords were the following ones: “Emotion dysregulation,” “Emotion regulation,” “Emotion,” “Emotional reactivity,” “Autism,” “Adults,” “Children,” “Youth,” “Adolescents,” “Borderline personality disorder,” “Impulsivity,” “Impulsiveness,” “Self-harm,” “Non-suicidal self-injury,” “Suicidality,” “Suicide,” “Linehan’s biosocial model,”” Linehan theory,” “Emotional vulnerability,” “Invalidation,” “Trauma,” “Adverse events,” “Bullying,” “Autistic camouflaging,” “Emotional scaffolding,” “Predictors,” “Correlates,” “Aetiology,” “Etiology.” To ensure the quality of our narrative review, we referred to the six criteria listed in the Scale for the Assessment of Narrative Review Articles [SANRA; (55)].
For the illustrative case conceptualization, we used the client’s quantitative and qualitative data. The client provided informed consent for the use of her data and participated in building and writing the case conceptualization. The use of personal data was approved by the University of Strasbourg research ethics board (Reference: CE-2022-138).
Recent research suggests that autistic people are more likely to develop ED than the general population (32, 33, 39). In fact, studies have shown fewer emotion regulation abilities and greater maladaptive strategies (e.g., rumination, avoidance) in autistic youth compared to their non-autistic peers (32, 56). Although ED has been mostly studied in autistic youth, it also concerns adults (57). Similar to findings in the general population (58), autistic women appear to present with greater ED than autistic men (59–61).
ED is not a diagnostic criterion for ASC (62), but given its high prevalence in autistic people, some researchers have questioned whether it should be added to ASC core features (39, 40, 63). Indeed, ED has been found to be highly associated with autistic core features (39, 51). Among them, restricted and repetitive behaviours (RRBs) in particular have been found to be the strongest ED predictor in autistic people (39, 64), suggesting that RRBs might contribute to ED, possibly through inhibitory dyscontrol (i.e., executive dysfunction) (39). Indeed, effective emotion regulation relies on inhibitory control and cognitive flexibility, which enables the use of context-dependent strategies (65). This is especially the case for emotion regulation skills that require increased adaptability, such as problem solving and cognitive reappraisal (65). Executive dysfunction might thus interfere with this ability (32, 51, 66), and lead to the increased use of maladaptive emotion regulation strategies (e.g., rumination, avoidance, suppression) but also RRBs (38). However, other findings indicate that RRBs rather stem from ED (39, 64, 67), since one quarter of these behaviours appear in reaction to emotional triggers (67). Irrespective of the direction of the relationship between ED and RRBs, recent data suggest that self-harming behaviours in ASC are similar to those seen in the general population (68). Therefore, contrary to past research suggesting that self-harming behaviours are part of RRBs in autistic people (69, 70), self-harming behaviours might actually be distinct from RRBs. Indeed, recent studies suggest that self-harming behaviours are used by autistic people to regulate painful emotions, particularly low-energy affective states like sadness and high-energy affective states like anger and anxiety (41, 71). By contrast, unlike self-harming behaviours, RRBs may serve the function of sensory stimulation and are primarily characterized by their automatic and stereotyped nature (62).
There is a lack of consensus on whether ED is a core problem in ASC or whether it is stems from co-occurring disorders (38), as co-occurring mental health issues (e.g., anxiety and depression) are prevalent in ASC (72, 73) and that ED is a transdiagnostic difficulty (23). However, a growing number of studies suggest that co-occurring disorders result from preexisting ED in ASC, suggesting that ED predisposes to the emergence of psychiatric disorders especially in adults (40, 57, 74). Given that few studies with a longitudinal design have focused on ED in ASC [(e.g., 64)], the direction of the relationship between ED and psychiatric disorders in ASC has not been yet been fully elucidated.
In ASC, ED has been associated with dysregulated behaviours (e.g., meltdowns, outbursts) (38, 75). Similar to BPD (76), recent studies suggest that ED is involved in self-harm with or without suicidal intent in ASC (40, 41, 71, 77). However, only recently research has started to highlight the high prevalence of self-harm (71, 78, 79) and suicidality in ASC (80, 81). A meta-analysis revealed a prevalence of 42% of self-harm in autistic people, irrespective of age and the presence of intellectual disability (79). Some findings suggest that the characteristics of these behaviours are similar to those found in the general population (68) and might be used by autistic people to regulate painful emotions, particularly low-energy affective states like sadness and high-energy affective states like anger and anxiety (41, 71). Moseley et al. (41) suggest that self-harm in ASC may also have other functions: i.e., self-punishment, deterrence from suicide, sensory stimulation and/or social communication.
Regarding suicidality, reviews have reported prevalence rates in ASC between 10 and 50% (82, 83). High suicidality rates have been reported in both autistic youth (84) and adults (77, 85), with adults without intellectual disability, especially women, being at the highest risk of dying by suicide among the autistic population (85–88). In relation to ED, Conner et al. (40) found that elevated ED was associated with increased suicidal behaviours in autistic youth. Some findings support a strong association between self-harm and suicidality, suggesting that autistic adults may develop capability for suicide through self-harm (78, 89).
Few studies have investigated factors contributing to the heightened rates of ED and suicidality in autistic women relative to autistic men (59, 61). In addition to an increased anxiety (59), recent findings point to an increased use of camouflaging in autistic women contributing to elevated distress and risk of suicidality (90, 91). In addition, autistic women, especially those without intellectual disability, are at higher risk of late diagnosis than men (92), which increases their exposure to invalidation and the pressure of exhibiting socially appropriate behavior (93). Although autistic women might be more likely to mask their social difficulties, these difficulties (e.g., identifying others’ intentions) persist even though they are less visible to others, making them more vulnerable to the societal invalidation toward women, particularly sexual violence (94, 95). These findings suggest the need to pay special attention to mental health in autistic women, especially regarding ED and suicidality.
As in BPD (96), Conner et al. (33) pointed to ED as a risk factor for the use of psychotropic medication, emergency services and psychiatric hospitalizations among autistic people. ED also contributes to impairments in adaptive functioning in ASC in childhood (97, 98) and adulthood (38).
Overall, findings support the implication of both emotional vulnerability and invalidating experiences in the development of ED in ASC [(e.g., 40, 99–101)]. However, to our knowledge, no studies investigated the transactional relationship between the two components in this context.
Numerous studies have linked autistic features, including peculiarities found at the emotional level, to the atypical brain development in ASC (38, 102). Indeed, neuroimaging findings show an atypical neural functioning underlying impaired emotion regulation in ASC (101, 103–105). For instance, in autistic adults without intellectual disability, Richey et al. (101) reported a hyporegulation of key brain regions involved in effortful emotion regulation (i.e., decreased ability to enhance the nucleus accumbens’ activation and to lower the amygdala’s activation) while engaging in cognitive reappraisal compared to non-autistic adults (101). Autistic adults also showed decreased dorsolateral prefrontal cortex activation (dlPFC) during the task, another brain region involved in goal-directed processes (101). By contrast, some previous findings showed a hyperactivation in this region in ASC, suggesting a potential compensatory activation to overcome cortical inefficiency during effortful emotion regulation (106). Moreover, using functional magnetic resonance imaging (fMRI), Mazefsky et al. (103) found a longer lasting brain activity in areas involved in sustained emotional information processing (i.e., insula, pulvinar and dlPFC), akin to rumination, in autistic youth compared to non-autistic peers. These regions have been shown to be involved in ED in conditions other than ASC (107, 108). This suggests an atypical neural activity behind the tendency to ruminate in ASC, which is a maladaptive emotion regulation strategy prevalent in autistic people (103).
Despite the paucity of studies, some findings support the involvement of the three dimensions of emotional vulnerability (i.e., hypersensitivity, hyperreactivity and slow return to emotional baseline) in ASC. For instance, Lassalle et al. (109) found that autistic individuals were hypersensitive to fear stimuli with a significantly higher activation of the amygdala than non-autistic individuals. Sensory hypersensitivities have also been linked to increased psychophysiological arousal and increased anxiety in autistic people (40, 110, 111). Regarding hyperreactivity, the majority of findings have reported an increased physiological response to emotional stimuli in autistic individuals compared to non-autistic individuals [(e.g., 105, 112)]. However, few other studies have rather supported equivalent physiological arousal to emotional triggers between autistic and non-autistic individuals (39, 113). It is noteworthy that discrepant results have also been reported in BPD regarding physiological hyperreactivity (6, 7). Finally, there are findings in support of the long-lasting nature of emotional arousal in autistic children, evidenced by the prolonged duration of cortisol secretion following a stressor compared to non-autistic peers (114).
A growing body of evidence suggests a link between core ASC features and ED, with the higher the autistic traits, the higher the ED (39, 51, 71, 115). Relatedly, Samson et al. (39) found that interventions enhancing emotion regulation skills in autistic children improved not only ED but also difficulties related to ASC features, which indirectly supports the link between ED and autistic traits.
Effortful emotion regulation is a deliberate process of self-regulation (116). Thus, due to the additional daily challenges linked to ASC-related difficulties (e.g., executive dysfunction, social interaction difficulties) and subsequent anxiety and fatigue, it is crucial to acknowledge that emotion regulation may come with increased cost for autistic people (39, 51, 117, 118). Beyond this increased load, ASC-related difficulties might directly interfere with effective emotion regulation (39, 51). Therefore, the “emotional vulnerability” component of the biosocial model that we propose includes the contribution of ASC-features previously acknowledged in Mazefsky and White’s model (2014) and integrates recent findings (Figure 1).
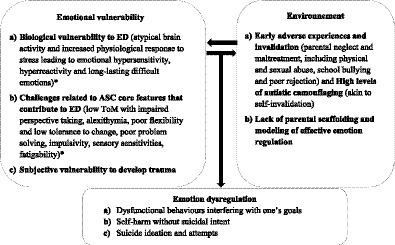
Figure 1. Linehan’s model application to ED in ASC. * Factors included in Mazefsky and White’s model (2014).
Effortful emotion regulation requires accurate identification of key aspects of the situation to use appropriate strategies (65). However, difficulties with social skills in ASC (62), particularly due to theory of mind (ToM) peculiarities, may interfere with effective emotion regulation (51, 119). However, it is important to highlight that the ToM peculiarities are neither specific to nor systematic in ASC (120). Additionally, effortful emotion regulation requires identifying one’s emotional experience to be able to modulate it (121). Yet, alexithymia, which refers to the difficulty in identifying and expressing one’s emotions, is common in ASC (122), limiting insight into one’s own emotions and thus preventing their deliberate modulation (38, 51). In autistic adults, alexithymia has been found to predict self-harm, particularly when experiencing high-energy states (i.e., anger, anxiety) (41). In autistic women in particular, alexithymia has been found to be related to ED, irrespective of BPD traits (123). Together, these difficulties could explain why autistic people may react impulsively to emotional triggers with a lack of goal-directedness (38).
Furthermore, effective emotion regulation relies on cognitive flexibility, which enables the use of context-dependent strategies (65). This is especially the case for skills that require increased adaptability, such as problem solving and cognitive reappraisal (65), and unfamiliar situations that also trigger the change-related anxiety common in ASC (51, 62). Poor cognitive flexibility might thus interfere with this ability in autistic people (32, 51, 66), and lead to the overuse of maladaptive emotion regulation strategies (e.g., rumination) or to the rigid use of adaptive emotion regulation strategies that do not fit the ongoing situation (e.g., distress tolerance skills) (38, 124). Consistent with this view, Aldao and Nolen-Hoeksema (125) suggested that individuals might develop a ‘default’ regulatory approach that interferes with the ability to use new and more adaptive strategies, such as reappraisal. This might be particularly true for autistic people, due to cognitive flexibility difficulties and change-related anxiety. Moreover, RRBs have been found to be the strongest predictor of ED in ASC (39), with one quarter of them appearing in reaction to emotional triggers (67). This points to the difficulty in inhibiting automatic behaviors in ASC, which also interferes with goal-directed behaviors and flexible emotion regulation (38, 39). Interestingly, emotional vulnerability, particularly the increased and sustained physiological activation following emotional triggers, possibly interfere with both cognitive and behavioral control in ASC (126). Thus, increased emotional vulnerability might promote automatic emotional responses in autistic individuals, which interferes with effortful emotion regulation (126). Moreover, it is noteworthy that ADHD, characterized in its hyperactive dimension by impulsivity, frequently co-occurs with ASC, including in adults (e.g., (127) found a prevalence of 33.3%). Therefore, if present, ADHD co-occurring features are likely to contribute to emotional difficulties (128).
Sensory sensitivities, which are common in autistic people (62), have also been reported to be significantly related to ED in ASC (39–41, 51). In a sample of autistic adults without intellectual disability, Moseley et al. (41) found that sensory sensitivities were a strong predictor of self-harming behaviors along with alexithymia, anxiety and depression (41). Importantly, in autistic youth, some studies have suggested that sensory sensitivities were the strongest and single predictor of self-harm (129). This association may be due to the distress reported by autistic people when experiencing intense sensory discomfort (130).
Autistic people are at heightened risk of experiencing adverse childhood events (131–133), particularly autistic girls (134, 135). This increased exposure to adverse experiences can be understood through the double-empathy theory, which highlights difficulties of reciprocity and mutuality between autistic and non-autistic people due to a lack of mutual understanding of each other’s subjective experience (136, 137). Hence, on the one hand, autistic individuals may face challenges in understanding and fitting into a “non-autistic” environment due to their particularities, and, on the other hand, the environment around them may contribute to their exclusion by failing to understand their atypical functioning and needs (138). As a result, from childhood onwards, autistic people are more likely to be rejected and maltreated, both within the family and in the wider community.
Moreover, some studies also highlight an increased vulnerability to be detrimentally affected by adverse events in ASC, with a wider range of events acting as possible catalysts for trauma (e.g., “sensory trauma” and major changes) (139, 140), supporting the hypothesis of a transactional relationship between biological and social factors in the emergence and maintenance of ED in autistic people. Adverse experiences in autistic children are associated with co-occurring disorders and/or the worsening of ASC-related difficulties in childhood (133, 141) and in adulthood (e.g., mood and anxiety disorders, PTSD) (131).
Autistic children may experience different forms of adverse events. First, autistic children, including those without intellectual disability, are at heightened risk of maltreatment, particularly physical neglect, and abuse (99, 100, 135), including sexual abuse (95). In fact, parents of autistic children are more likely to be emotionally and physically punitive at the child’s behavior (e.g., non-responsiveness and rigid adherence to routines) as they may perceive it as oppositional (142). Maltreatment is associated with increased dysregulated behaviors in autistic children (e.g., aggression and self-harm) (100), with those who have been abused being at greater risk of engaging in dysregulated behaviors, including suicide attempts (99). For instance, Taylor and Gotham (133) found that 90% of their sample of autistic children with high mood symptoms had experienced at least one traumatic event. Importantly, heightened exposure to trauma may predispose autistic children to develop a co-occurring BPD given that early traumatic experiences are a key risk factor for the disorder (143).
Additionally, autistic children have a 4-fold increased risk of being bullied at school compared to their non-autistic peers (144, 145) due to the misunderstanding of their atypical functioning and social difficulties (144), with those without intellectual disability being at higher risk (100). Importantly, repeated adverse experiences, including school bullying, have been shown to be associated with higher levels of distress and altered physiological arousal in adulthood (146). Recent findings by Camodeca & Nava (147) add to these results by showing that victimization strongly predicts increased physiological arousal to emotional triggers in non-autistic adults. Interestingly, this association has also been found in the case of exposure to bullying perpetrated to others (i.e., witnessing bullying without intervening) (147).
Furthermore, the heightened exposure of autistic people to adverse experiences persists in adulthood (140, 148). Indeed, autistic adults report more emotional bullying and greater sexual victimization compared to the general population (148, 149), particularly women (94, 95). Additionally, autistic adults, especially those who were diagnosed in adulthood, may suffer from a lack of social support, including from relatives who reject or misunderstand their diagnosis (150–152).
Given that chronic invalidation may be widespread in ASC (i.e., family members, school, society), autistic adults may present with high levels of internalized stigma related to their ASC diagnosis [(e.g., 153, 154)], which may, in turn, contribute to high levels of autistic camouflaging, i.e., efforts of masking and/or compensating for autistic traits to ‘fit in’ in society (155, 156). Recent findings show that autistic camouflaging negatively affects mental health (e.g., depression and anxiety) (91, 93) and is associated with lifetime suicidality in autistic adults without intellectual disability (157, 158), especially autistic women (90, 91). Interestingly, autistic camouflaging is akin to self-invalidation in Linehan’s model in many ways. First, both are the consequence of invalidation in childhood (159). Second, both teach one to mistrust one’s internal states and to rely on the environment for clues on how to respond. Third, the tendency to look for external validation in both cases interferes with developing a sense of self (156). Fourth, both might be of adaptive value to avoid negative reactions such as violence and bullying (155).
Caregivers play a key role in helping the child learn effective emotion regulation, particularly through parental scaffolding, defined as a parent’s support of their child’s emotion regulation (115, 160). This is especially the case for autistic children, given their vulnerability to develop ED and the increased influence of parental behavior on their social and emotional development (115, 161). In autistic children, effective parental scaffolding has been associated with enhanced emotion regulation, while low parental scaffolding has been associated with ED (115, 160, 162, 163). In addition, some findings show that parents of autistic children may mainly rely on passive co-regulation strategies while providing emotional scaffolding (i.e., following the child’s lead), instead of active strategies (i.e., prompting/helping, redirection of attention, physical comfort) (162).
Additionally, studies point to parental ED as a potential contributor to ED in autistic youth (57, 97, 162, 164). Indeed, fewer parental externalizing problems (e.g., aggression, hyperactivity) have been linked to adaptive emotion regulation skills in autistic children (162). This may reflect that providing effective parental scaffolding and modeling for emotional regulation requires the parents to be able to use effective emotion regulation strategies to regulation their own emotions (164-166). For this reason, Flujas-Contreras et al. (165) investigated the impact of a clinical intervention aiming at enhancing the parents’ emotion regulation skills (e.g., mindfulness skills, problem solving and strategies for managing their children’s behavior and emotional problems) on their autistic children’s emotion regulation abilities. Unsurprisingly, both the parents’ and the children’s emotion regulation abilities improved significantly following the intervention (165). These results bring additional support to the development of parent-based interventions to enhance ER abilities in autistic children (165, 166). These early interventions may be of preventive value in helping to thwart the development of ED in autistic people since childhood.
Mrs. F. is a 37-year-old woman who has a full-time job and lives with her husband and young child. Mrs. F. was diagnosed with ASC without intellectual disability at the age of 35, in addition to previous diagnoses of postpartum depression and PTSD. She was subsequently diagnosed with ADHD. Mrs. F. has experienced daily suicide ideation since childhood. As a child, she frequently reflected on ways to attempt suicide and tried once to die by stopping to eat. In adulthood, she attempted suicide twice by medication overdose. Both suicide attempts required hospitalizations in an intensive care unit. Mrs. F. does not exhibit self-harm without suicidal intent. She underwent a comprehensive psychiatric evaluation as part of her ASC diagnostic assessment, including the Mini-International Neuropsychiatric Interview (M.I.N.I.; (168, 169), for the French version). No co-occurring BPD was identified. No one else in Mrs. F.’s family is known to have received an ASC diagnosis. Mrs. F’s case formulation using our application of the biosocial model to ASC is in Figure 2 and her scores on self-reported scales measuring dimensions related to the components of the model are shown in Table 1.
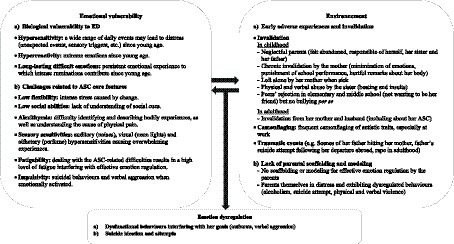
Figure 2. Case conceptualization of Mrs. F. based on our application of Linehan’s model to ED in ASC.
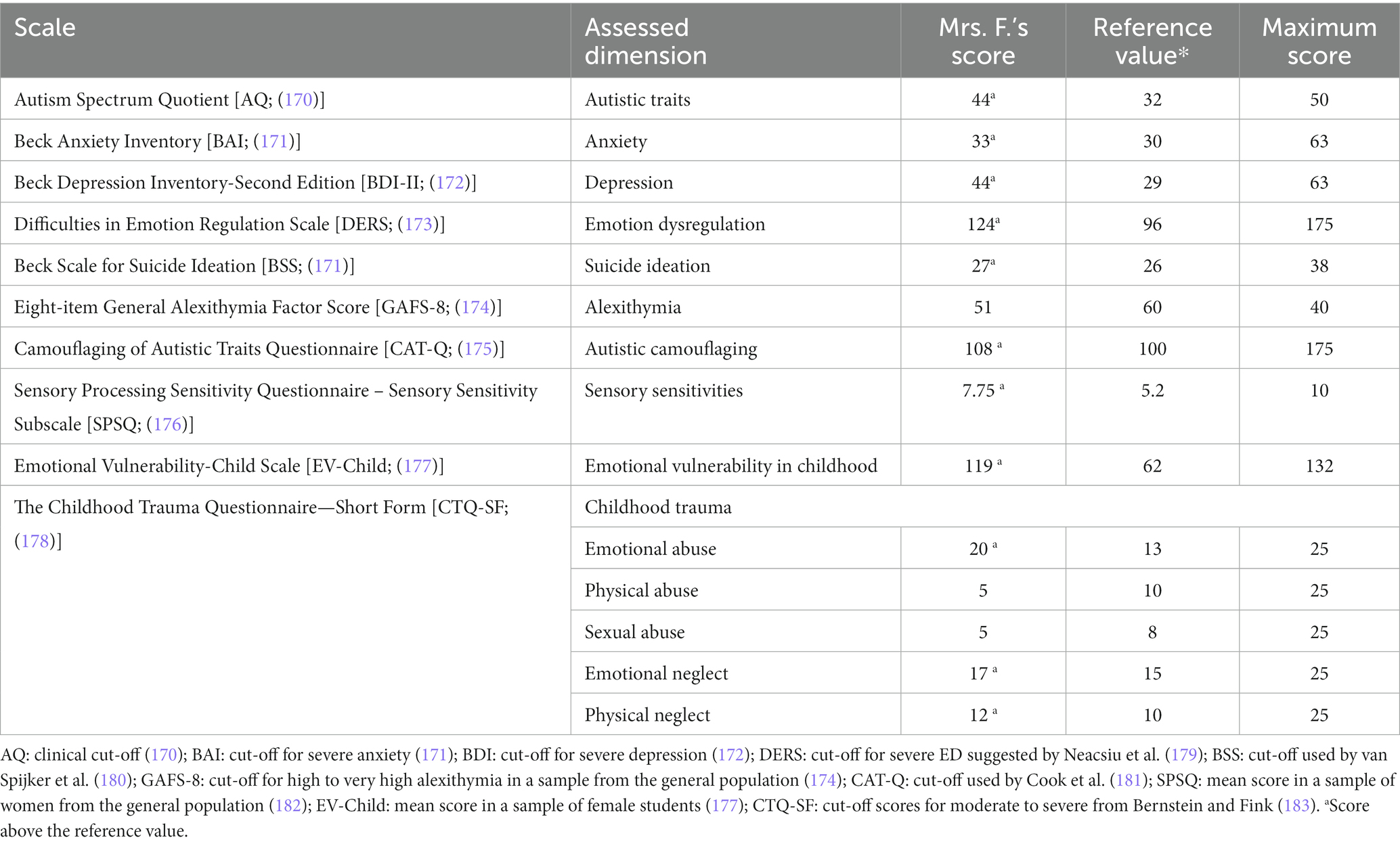
Table 1. Mrs. F.’s scores on a battery of scales measuring the components of Linehan’s model applied to ASC.
Mrs. F. reports that several ordinary events can trigger distress and intense reactions (e.g., bursting into tears), resulting in a wide range of situations as potential crisis triggers (e.g., «I do not understand why I can get so distressed over something that is not really important»). This is akin to hypersensitivity to emotional cues relative to Linehan’s model (1993). She also describes feeling intense and long-lasting emotions fueled by ruminations (e.g., «It [the emotion] feels like a geyser», «It [the emotion] stays there for a long time […] stagnant», «It goes round and round in my head»). This is supportive of the two additional facets relative to emotional vulnerability in Linehan’s model (1993): i.e., emotional hyperreactivity and slow return to baseline when facing difficult emotions. Mrs. F. reports dealing with these emotional difficulties since a very young age. These elements along with Mrs. F.’s self-reported problems in understanding her emotions (i.e., alexithymia) indicated that it was crucial to include these elements into the psychoeducation on the biological vulnerability component of the model. Indeed, these elements, along with the ASC-related difficulties highlighted below, probably contribute to the high level of distress Mrs. F. experiences on a daily basis. This understanding is essential to increase emotional awareness and decrease self-invalidation (e.g., «I do not understand why I can get so distressed over something that is not really important») and shame, which are, respectively, a prerequisite for effective emotion regulation and a motivational factor.
Regarding ASC-related factors associated with ED included in our application of Linehan’s biosocial model to ED in ASC, Mrs. F. reports that, due to her need for sameness, last-minute changes provoke intense anxiety. Becoming a mother at the age of 32 has been a major additional source of stress, as her child’s changing needs and reactions are a source of unrelenting unexpected events and sensory discomfort (e.g., her child’s crying). Difficulties in reading social cues are a major source anxiety, as they are associated with doubts over how to interpret and react to others’ behavior. In addition, Mrs. F. has auditory (noises), visual (neon lights) and olfactory (perfume) hypersensitivities that cause overwhelming sensory experiences (e.g., «It is an invasion [...] it can cause extreme discomfort», «I struggle to put it [the sensory stimulation] aside and be available for the rest of the things»). Mrs. F. also describes having difficulties identifying and describing her bodily experiences, as well as understanding what causes her physical pain. This is especially the case when she is in an emotional crisis (e.g., «When I am overwhelmed, there is no access to anything [in her body and mind], I am just in survival mode»). In extreme cases, Mrs. F.’s impulsivity can lead to verbal aggression or unplanned suicidal behaviors, which was the case in her first suicide attempt. Dealing with the ASC-related difficulties and camouflaging them result in a high level of fatigue. This interferes with her ability to regulate her emotions effectively (e.g., «Compensating for sensory overload, camouflaging, social interactions and, also, managing my emotions… it is exhausting! »). Camouflaging in particular is described as extremely costly and exhausting (e.g., «I do it deliberately to modify my behavior […] it is there all the time and it is exhausting»). Her responsibilities as a mother also add to the daily fatigue, as she needs to attend to the constantly changing needs of her child. Highlighting the ASC-related difficulties and adding them to the biosocial model allowed to specifically target them, especially in individual sessions. Indeed, as highlighted in a first-person account of an autistic person who benefitted from DBT (184), DBT therapists need to consider the specific needs and motivational factors of autistic clients to increase the pertinence of DBT. Here, this means to be aware of ASC-related features that are likely to contribute to ED, integrate them in the biosocial model, as well as in the targets and goals of the therapy. In addition, therapists’ destigmatizing attitudes toward ASC draw upon this conceptualization, as it aids to validate the difficulty to cope with these challenges on a daily basis (e.g., adapt to a non-autistic world), to teach to self-validate instead of self-stigmatize and camouflage, to provide targeted psychoeducation (e.g., on autistic camouflaging and its impact on mental health), to help identify and label emotions, but also problem-solve (e.g., in relation to sensory triggers).
Mrs. F.’s parents had alcohol use disorder. She reports feeling abandoned in her childhood, unable to rely on her parents. During her childhood and adolescence, she witnessed repeated scenes of physical violence perpetrated by her father on her mother, and, at times, by her sister on her mother. Some of these scenes were traumatic. Emotional abuse was frequent, as Mrs. F.’s mother repeatedly told her «no one will love you, you’ll end up alone» or «go look in the mirror how ugly you are» while Mrs. F. was crying. She was an excellent student throughout her school years. In response to her high grades, her mother used to say «you could have done better». Mrs. F. reports that her mother did not care for her even when she was sick, always prioritizing work. Mrs. F. also reports that her sister was physically and verbally violent towards her, hitting and insulting her. Her mother’s invalidation (e.g., punitive and oversimplifying behaviors) continued into adulthood. She explains that her father was the only person she felt understood by. However, her father attempted suicide after she left home to live abroad. Before her departure, he told her that he would attempt suicide if she left. Mrs. F. reports that she still feels guilty over her father’s suicide attempt.
Mrs. F.’s parents exhibited dysregulated behaviors (alcohol use disorder, physical and verbal violence, and suicide attempts) indicative of a great psychological distress and major difficulties to regulate their emotions. Thus, Mrs. F.’s parents were not able to provide her with the necessary emotion regulation scaffolding and modeling. On the contrary, their own difficulties were a source of recurrent invalidation and trauma. In addition to the trauma related to events in her family, Mrs. F. was a victim of rape as a young adult, and subsequently developed a PTSD related to this event.
At school, Mrs. F. reported feeling isolated. Nevertheless, she reported that school was “a safe haven” because it was a structured environment, where she found intellectual fulfillment, and support from the teachers. In middle school, she was the target of bullying from peers. She had difficulty integrating groups of friends (e.g., «I did not have the codes of how things were done») and felt rejected.
In later years, Mrs. F. has experienced high levels of invalidation regarding her ASC diagnosis, both from her family and her husband, e.g., «you are just lazy», leading to increased anger, shame and sadness.
The psychosocial factors highlighted here were key to better understand Mrs. F.’s developmental environment, as well as its potential effects on ED and on her overall mental health. Specifically, they helped to identify predisposing factors that seem to have contributed to self-invalidating behaviors [i.e., a secondary target in DBT involved in ED; (5)] and, more broadly, to ED – e.g., repetitive punitive invalidations and lack of scaffolding and modeling of effective emotion regulation from her parents. Given the transaction between the invalidating environment and her emotionally vulnerable temperament, including her ASC-related difficulties, it is understandable that she felt and reacted the way she did. This knowledge, inherent to the dialectical perspective of the biosocial model (5), was crucial for the therapist to validate the client and to teach her to self-validate. In addition, this allowed the therapist to provide psychoeducation on the possible link between adverse events (e.g., parents’ dysregulated behaviors, lack of emotional scaffolding) and current emotional difficulties (in transaction with biological factors), including suicidal behavior. According to the DBT framework and conceptualization (5), Mrs. F. was in stage 1 of DBT, that is, she presented with behavioral dyscontrol (e.g., life-threatening behaviors). It is only in stage 2, once dysregulated behaviors are no longer present, that PTSD and the sequelae of traumatic and invalidating experiences may be directly targeted.
This article aimed at applying and extending Linehan’s biosocial model (5) to ED in autistic people across the lifespan. This is of particular interest as ED is prevalent in this population (57, 185) and seems to be involved in the high rates of self-harm and suicidality (40, 41). Consequently, DBT is an emerging topic in the field of interventions targeting ED in ASC, with promising preliminary results (50, 51). However, no studies so far had focused on the utility of Linehan’s biosocial model, which underlies DBT for BPD, in ASC.
Our review and application to the case of an autistic woman suggest that ED in ASC encompasses factors related to both biological and psychosocial risk factors as conceptualized in the BPD framework, although in both domains ASC-specific factors might be involved. Indeed, in addition to the biological vulnerability similar to BPD (i.e., hypersensitivity, hyperreactivity and slow return to emotional baseline) (105), ToM peculiarities, sensory sensitivities, lack of cognitive flexibility, change-related anxiety and RRBs have been associated with ED in ASC (39, 51). Alexithymia, prevalent in ASC, has also been reported to be linked to ED in autistic adults (41), especially in autistic women (123). It is worth noting that ASC-related difficulties may interfere directly with the ability to self-regulate (32, 39, 51) but also contribute to high levels of anxiety and fatigue making emotion regulation costly for autistic people (39, 51, 117). Such is the case for Mrs. F., whose autistic features (e.g., sensory hypersensitivity, hypervigilance regarding social rules and how to behave in social situations) are both involved in her emotional vulnerability and in the costs of real-life use of adaptive emotion regulation skills. We note, however, that people with BPD might present with autistic-like features, including sensory hypersensitivities (187) and ToM peculiarities (188). Therefore, our findings support the application and extension of Linehan’s model to ASC, but it also highlights under-researched topics in BPD. Indeed, it is likely, for example, that sensory particularities may also play a role in ED in people with BPD, as this has been shown to be the case in the general population (189).
Regarding psychosocial risk factors, our review suggests that, similar to BPD and other psychological conditions (4, 28, 29), invalidating experiences seem to contribute to the emergence of ED also in autistic people. In fact, findings report that autistic children are highly exposed to different early stressful and traumatic experiences (e.g., physical and emotional maltreatment from caregivers and school bullying), especially because of their atypical functioning that cause misunderstanding and rejection from others (131, 132, 139, 187). Autistic girls seem to be particularly vulnerable to experience these adverse events (134, 135). Importantly, adverse experiences have been associated with co-occurring psychopathology and/or the worsening of difficulties related to ASC in childhood (133, 141). As in BPD, these experiences have been associated with self-harming behaviors with or without suicidal intent in autistic children (99, 100), particularly in those who have been sexually abused (99). In adulthood, these experiences have been associated with numerous co-occurring disorders such as mood and anxiety disorders, PTSD (131), and BPD (143, 190).
Beyond the impact of adverse experiences, given the potential transactional link between biological and environmental factors of ED in ASC, it is likely that the specific needs of the autistic child might differ from those of the child at risk to develop BPD. For instance, autistic children might need increased parental scaffolding and modeling to learn effective emotion regulation skills than children who will develop BPD (115, 165). The necessary adjustments of the caregivers (e.g., teachers, parents) can be promoted by an early diagnosis of ASC (191) and enhancing the parents’ emotion regulation skills (165).
In addition, our review and extension of the biosocial model to ASC includes excessive autistic camouflaging as a form of self-invalidation resulting from internalized invalidation from others (192). In addition to being costly, the self-invalidation associated with autistic camouflaging might be detrimental to the development of adaptive emotion regulation skills as well as to the sense of self and self-acceptance in autistic people (156, 193). Importantly, recent studies found a strong negative association between autistic camouflaging and lifetime suicidality in autistic adults, especially autistic women (90, 91, 157). The latter finding can be explained by several factors. Indeed, autistic women, especially those without intellectual disability, are diagnosed later than men (92). Relatedly, greater expectations for adolescent and adult autistic women to engage in adaptive social communication and behavior are more prominent (91). This may, in turn, be involved in the enhanced use of compensatory behavior to mitigate social challenges and mask autistic traits in autistic females, i.e., camouflaging (91, 192). Therefore, if autistic women, especially those who are undiagnosed, are more likely to mask their mindreading and overall social difficulties, this may promote their social inclusion (194). However, they probably lack the social skills that might make them less vulnerable to societal invalidation towards women in general, including sexual violence (94, 95, 195). Mrs. F.’s case illustrates the impact of late diagnosis (at the age of 35) and the resulting autistic camouflaging to “try to fit in” since childhood. We speculate that an early diagnosis could be beneficial in several ways. For example, it could foster the understanding of one’s own functioning, prevent self-invalidation and enhance self-acceptance in autistic people. In autistic women, earlier diagnosis could also be of preventive value in relation to sexual violence, enabling access to targeted sexual education and assertiveness programs (195).
Moreover, regarding the overlap in biosocial correlates of ED between ASC and BPD, it appears crucial to expand our knowledge of ED and its mechanisms in both diagnoses. Thus, we suggest considering the following points of potential differentiation in future studies. First, people with BPD might present with autistic-like features, such as sensory hypersensitivities (187) and ToM peculiarities (188). Thus, comparative studies are needed to investigate the extent to which the ASC-related factors specifically contribute to ED in ASC relative to disorders with ASC-like features such as BPD. We also suggest to further investigate how these factors may interact with each other and contribute to ED. For instance, recent findings suggest an association between high sensory sensitivity (i.e., low sensory threshold and ease of excitation) and alexithymia in non-autistic young adults, with this interaction impacting emotion processing and regulation (196). Second, ED in BPD is significantly involved in interpersonal problems (e.g., conflicts, physical/verbal violence) due to mood swings and chronic fear of abandonment (62, 197). In ASC, relationships are not likely to be affected in the “stormy” way found in BPD, as social difficulties are rather related to poor social abilities that makes it difficult to bond with others (198). It seems therefore relevant to investigate the impact of ED on relationships in both BPD and ASC to potentially highlight distinctions in ED between the two diagnoses. Third, in BPD, ED is strongly linked to affective instability in interpersonal contexts (199). In ASC, by contrast, ED seems to arise from the interaction between ASC traits and contextual factors (e.g., invasive sensory stimuli, changes in the environment/planning) (38, 39). Thus, it seems relevant to further investigate whether and how ED might be more related to widespread context cues in ASC compared to BPD. Fourth, to date, evidence supports the role of emotional vulnerability and invalidation separately in the development of ED in ASC. Thus, the transaction between the two is yet to be empirically tested in ASC. Fifth, previous findings have reported differences in the development of personality styles between ASC and BPD (200). Hence, it seems relevant to explore whether and how the factors inherent to the development of personality in BPD contribute to ED relative to ASC (201).
Finally, we acknowledge that the paucity of data on ED and its mechanisms in ASC might have limited the potential determinants of our application of Linehan’s model. Nevertheless, given the increasing awareness of the impact of ED on autistic individuals’ mental health, our application has the advantage of providing a pragmatic model that can inform the delivery of psychological treatments for this population. Additionally, our application of the model to ASC may foster new and much needed research on the biosocial mechanisms of ED in ASC. For instance, as a growing body of research has shown that autistic women are at greater risk for severe ED (61) and suicidality than men (86). Hence, it seems crucial to consider this discrepancy in future studies by systematically exploring cross-gender (including transgender and gender non-conforming individuals) differences in the implication of the determinants of ED in ASC. Moreover, our application might provide clinicians with a comprehensive framework of ED in ASC, enhancing the systematic assessment of traumatic and invalidating experiences in autistic clients. The latter include different layers of invalidation, which might be related to intersectional factors (e.g., gender) involved in family invalidation, peer invalidation but also societal discrimination leading to self-stigma and self-invalidation (94). Finally, our application of the model may inform psychological treatments targeting ED, especially DBT, the psychotherapy that has amassed the most evidence in the treatment of ED in BPD (5, 12). As DBT was developed based on Linehan’s biosocial theory (5), applying and extending this theory to ED in ASC may foster the adaptation of DBT to treat ED in autistic people, especially since preliminary data on its feasibility and effectiveness in autistic adults are promising (49, 50). This is of particular importance as evidence-based interventions targeting ED in autistic individuals are lacking, especially for adults (202), and that ED might be associated with self-harm and suicidal behaviors in this population (40, 41), especially autistic adults without intellectual disability (86). Furthermore, our application of the Linehan’s biosocial model to ASC might promote specific adaptations to autistic people, increasing the acceptability and efficacy of DBT applied to this population (184). For example, increased scaffolding and modeling from the therapist and the use of a psychoeducational biosocial model that integrates the ASC specificities highlighted here might be particularly valuable to this aim.
DB: conceptualization, methodology, investigation, and writing – original draft. LW: conceptualization, methodology, supervision, and writing – review and editing. All authors contributed to the article and approved the submitted version.
DB’s PhD funding by Fonds de dotation Neuroglia.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. ^Note on terminology:Throughout the manuscript, we use the term “autistic people” (identity-first), rather than “people with autism” or “people with autism spectrum disorder,” as this was the terminology explicitly favoured by the majority of the autistic participants of a large-scale survey (30). We also use “autism spectrum condition” instead of the DSM-5 term of “autism spectrum disorder (ASD)” to be respectful to those on the spectrum who feel that the term “disorder” is stigmatising, whereas the term “condition” acknowledges both the difficulties and the differences and strengths in autistic people (31).
1. Beauchaine, TP. Future directions in emotion dysregulation and youth psychopathology. Journal of clinical child and adolescent psychology: the official journal for the Society of Clinical Child and Adolescent Psychology. Am Psychol Assoc. (2015) 44:875–96. doi: 10.1080/15374416.2015.1038827
2. Carpenter, RW, and Trull, TJ. Components of emotion dysregulation in borderline personality disorder: a review. Curr Psychiatry Rep. (2013) 15:335. doi: 10.1007/s11920-012-0335-2
3. Daros, AR, and Williams, GE. A meta-analysis and systematic review of emotion-regulation strategies in borderline personality disorder. Harv Rev Psychiatry. (2019) 27:217–32. doi: 10.1097/HRP.0000000000000212
4. Crowell, SE, Beauchaine, TP, and Linehan, MM. A biosocial developmental model of borderline personality: elaborating and extending Linehan's theory. Psychol Bull. (2009) 135:495–510. doi: 10.1037/a0015616
5. Linehan, MM. Cognitive-behavioural treatment of borderline personality disorder. New York, NY: Guilford Press (1993).
6. Kuo, JR, and Linehan, MM. Disentangling emotion processes in borderline personality disorder: physiological and self-reported assessment of biological vulnerability, baseline intensity, and reactivity to emotionally evocative stimuli. J Abnorm Psychol. (2009) 118:531–44. doi: 10.1037/a0016392
7. Bortolla, R, Cavicchioli, M, Galli, M, Verschure, PFMJ, and Maffei, C. A comprehensive evaluation of emotional responsiveness in borderline personality disorder: a support for hypersensitivity hypothesis. Borderline Personal Disord Emot Dysregul. (2019) 6:8. doi: 10.1186/s40479-019-0105-4
8. Wagner, AW, and Linehan, MM. Applications of dialectical behaviour therapy to posttraumatic stress disorder and related problems In: VM Follette and JI Ruzek, editors. Cognitive-behavioural therapies for trauma. New York, NY: The Guilford Press (2006).
9. Brereton, A, and McGlinchey, E. Self-harm, emotion regulation, and experiential avoidance: a systematic review. Archives Suicide Res. (2020) 24:1–24. doi: 10.1080/13811118.2018.1563575
10. Oumaya, M, Friedman, S, Pham, A, Abou Abdallah, T, Guelfi, JD, and Rouillon, F. Personnalité borderline, automutilations et suicide: revue de la littérature [Borderline personality disorder, self-mutilation and suicide: literature review]. L'Encephale. (2008) 34:452–8. doi: 10.1016/j.encep.2007.10.007
11. Linehan, MM, Comtois, KA, Murray, AM, Brown, MZ, Gallop, RJ, Heard, HL, et al. Two-year randomized controlled trial and follow-up of dialectical behaviour therapy vs therapy by experts for suicidal behaviours and borderline personality disorder. Arch Gen Psychiatry. (2006) 63:757–66. doi: 10.1001/archpsyc.63.7.757
12. Panos, PT, Jackson, JW, Hasan, O, and Panos, A. Meta-analysis and systematic review assessing the efficacy of dialectical behaviour therapy (DBT). Res Soc Work Pract. (2014) 24:213–23. doi: 10.1177/1049731513503047
13. Gill, D, and Warburton, W. An investigation of the biosocial model of borderline personality disorder. J Clin Psychol. (2014) 70:866–73. doi: 10.1002/jclp.22074
14. Reeves, M, James, LM, Pizzarello, SM, and Taylor, JE. Support for Linehan's biosocial theory from a nonclinical sample. J Personal Disord. (2010) 24:312–26. doi: 10.1521/pedi.2010.24.3.312
15. Hope, NH, and Chapman, AL. Difficulties regulating emotions mediates the associations of parental psychological control and emotion invalidation with borderline personality features. Personal Disord. (2019) 10:267–74. doi: 10.1037/per0000316
16. Keng, SL, and Wong, YY. Association among self-compassion, childhood invalidation, and borderline personality disorder symptomatology in a Singaporean sample. Borderline Personal Disord Emot Dysregul. (2017) 4:24. doi: 10.1186/s40479-017-0075-3
17. Schaich, A, Assmann, N, Köhne, S, Alvarez-Fischer, D, Borgwardt, S, Schweiger, U, et al. The mediating effect of difficulties in emotion regulation on the association between childhood maltreatment and borderline personality disorder. Eur J Psychotraumatol. (2021) 12:1934300. doi: 10.1080/20008198.2021.1934300
18. Keng, SL, and Soh, CY. Association between childhood invalidation and borderline personality symptoms: self-construal and conformity as moderating factors. Borderline Personal Disord Emot Dysregulation. (2018) 5:19. doi: 10.1186/s40479-018-0096-6
19. Sturrock, B, and Mellor, D. Perceived emotional invalidation and borderline personality disorder features: a test of theory. Personal Ment Health. (2014) 8:128–42. doi: 10.1002/pmh.1249
20. Dvir, Y, Ford, JD, Hill, M, and Frazier, JA. Childhood maltreatment, emotional dysregulation, and psychiatric comorbidities. Harv Rev Psychiatry. (2014) 22:149–61. doi: 10.1097/HRP.0000000000000014
21. McLaughlin, KA, Hatzenbuehler, ML, Mennin, DS, and Nolen-Hoeksema, S. Emotion dysregulation and adolescent psychopathology: a prospective study. Behav Res Ther. (2011) 49:544–54. doi: 10.1016/j.brat.2011.06.003
22. Paulus, FW, Ohmann, S, Möhler, E, Plener, P, and Popow, C. Emotional dysregulation in children and adolescents with psychiatric disorders. A narrative review. Front Psychiatry. (2021) 12:628252. doi: 10.3389/fpsyt.2021.628252
23. Sloan, E, Hall, K, Moulding, R, Bryce, S, Mildred, H, and Staiger, PK. Emotion regulation as a transdiagnostic treatment construct across anxiety, depression, substance, eating and borderline personality disorders: a systematic review. Clin Psychol Rev. (2017) 57:141–63. doi: 10.1016/j.cpr.2017.09.002
24. Weissman, DG, Bitran, D, Miller, AB, Schaefer, JD, Sheridan, MA, and McLaughlin, KA. Difficulties with emotion regulation as a transdiagnostic mechanism linking child maltreatment with the emergence of psychopathology. Dev Psychopathol. (2019) 31:899–915. doi: 10.1017/S0954579419000348
25. Calkins, SD, Dollar, JM, and Wideman, L. Temperamental vulnerability to emotion dysregulation and risk for mental and physical health challenges. Dev Psychopathol. (2019) 31:957–70. doi: 10.1017/S0954579419000415
26. Beauchaine, TP. Physiological markers of emotional and behavioural dysregulation in externalizing psychopathology. Monogr Soc Res Child Dev. (2012) 77:79–86. doi: 10.1111/j.1540-5834.2011.00665.x
27. Gruhn, MA, and Compas, BE. Effects of maltreatment on coping and emotion regulation in childhood and adolescence: a meta-analytic review. Child Abuse Negl. (2020) 103:104446. doi: 10.1016/j.chiabu.2020.104446
28. Guérin-Marion, C, Bureau, JF, Lafontaine, MF, Gaudreau, P, and Martin, J. Profiles of emotion dysregulation among university students who self-injure: associations with parent-child relationships and non-suicidal self-injury characteristics. J Youth Adolesc. (2021) 50:767–87. doi: 10.1007/s10964-020-01378-9
29. Rüfenacht, E, Pham, E, Nicastro, R, Dieben, K, Hasler, R, Weibel, S, et al. Link between history of childhood maltreatment and emotion dysregulation in adults suffering from attention deficit/hyperactivity disorder or borderline personality disorder. Biomedicine. (2021) 9:1469. doi: 10.3390/biomedicines9101469
30. Kenny, L, Hattersley, C, Molins, B, Buckley, C, Povey, C, Pellicano, E, et al. Which terms should be used to describe autism? Perspectives from the UK autism community. Autism. (2016) 20:442–462. doi: 10.1177/1362361315588200
31. Bottema-Beutel, K, Kapp, SK, Lester, JN, Sasson, NJ, and Hand, BN. Avoiding Ableist Language: Suggestions for Autism Researchers. Autism Adulthood. (2021) 3:18–29. doi: 10.1089/aut.2020.0014
32. Cai, RY, Richdale, AL, Uljarević, M, Dissanayake, C, and Samson, AC. Emotion regulation in autism spectrum disorder: where we are and where we need to go. Autism Res. (2018) 11:962–78. doi: 10.1002/aur.1968
33. Conner, CM, Golt, J, Shaffer, R, Righi, G, Siegel, M, and Mazefsky, CA. Emotion dysregulation is substantially elevated in autism compared to the general population: impact on psychiatric services. Autism Res. (2021) 14:169–81. doi: 10.1002/aur.2450
34. May, T, Pilkington, PD, Younan, R, and Williams, K. Overlap of autism spectrum disorder and borderline personality disorder: a systematic review and meta-analysis. Autism Res. (2021) 14:2688–710. doi: 10.1002/aur.2619
35. Dudas, RB, Lovejoy, C, Cassidy, S, Allison, C, Smith, P, and Baron-Cohen, S. The overlap between autistic spectrum conditions and borderline personality disorder. PLoS One. (2017) 12:e0184447. doi: 10.1371/journal.pone.0184447
36. Rinaldi, C, Attanasio, M, Valenti, M, Mazza, M, and Keller, R. Autism spectrum disorder and personality disorders: comorbidity and differential diagnosis. World J Psychiatry. (2021) 11:1366–86. doi: 10.5498/wjp.v11.i12.1366
37. Mayes, SD, Calhoun, SL, Waxmonsky, JG, Kokotovich, C, Baweja, R, Lockridge, R, et al. Demographic differences in disruptive mood dysregulation disorder symptoms in ADHD, autism, and general population samples. J Atten Disord. (2019) 23:849–58. doi: 10.1177/1087054716664409
38. Mazefsky, CA, Herrington, J, Siegel, M, Scarpa, A, Maddox, BB, Scahill, L, et al. The role of emotion regulation in autism spectrum disorder. J Am Acad Child Adolesc Psychiatry. (2013) 52:679–88. doi: 10.1016/j.jaac.2013.05.006
39. Samson, AC, Phillips, JM, Parker, KJ, Shah, S, Gross, JJ, and Hardan, AY. Emotion dysregulation and the core features of autism spectrum disorder. J Autism Dev Disord. (2014) 44:1766–72. doi: 10.1007/s10803-013-2022-5
40. Conner, CM, Golt, J, Righi, G, Shaffer, R, Siegel, M, and Mazefsky, CA. A comparative study of suicidality and its association with emotion regulation impairment in large ASD and US census-matched samples. J Autism Dev Disord. (2020) 50:3545–60. doi: 10.1007/s10803-020-04370-1
41. Moseley, RL, Gregory, NJ, Smith, P, Allison, C, and Baron-Cohen, S. A 'choice', an 'addiction', a way 'out of the lost': exploring self-injury in autistic people without intellectual disability. Mol Autism. (2019) 10:18. doi: 10.1186/s13229-019-0267-3
42. Iversen, S, and Kildahl, AN. Case report: mechanisms in misdiagnosis of autism as borderline personality disorder. Front Psychol. (2022) 13:735205. doi: 10.3389/fpsyg.2022.735205
43. Chabrol, H, and Raynal, P. The co-occurrence of autistic traits and borderline personality disorder traits is associated to increased suicidal ideation in nonclinical young adults. Compr Psychiatry. (2018) 82:141–3. doi: 10.1016/j.comppsych.2018.02.006
44. Dell'Osso, L, Cremone, IM, Amatori, G, Cappelli, A, Cuomo, A, Barlati, S, et al. Investigating the relationship between autistic traits, ruminative thinking, and suicidality in a clinical sample of subjects with bipolar disorder and borderline personality disorder. Brain Sci. (2021) 11:621. doi: 10.3390/brainsci11050621
45. Rydén, G, Rydén, E, and Hetta, J. Borderline personality disorder and autism spectrum disorder in females: a cross-sectional study. Clin Neuropsychiatry. (2008) 5:22–30.
46. Keluskar, J, Reicher, D, Gorecki, A, Mazefsky, C, and Crowell, JA. Understanding, assessing, and intervening with emotion dysregulation in autism spectrum disorder: a developmental perspective. Child Adolesc Psychiatr Clin N Am. (2021) 30:335–48. doi: 10.1016/j.chc.2020.10.013
47. Hartmann, K, Urbano, M, Manser, K, and Okwara, L. Modified dialectical behaviour therapy to improve emotion regulation in autism spectrum disorders In: CE Dans, C Richardson, and RA Wood, editors. Autism spectrum disorders. Hauppauge, NY: Nova Science Publishers (2012)
48. Reyes, NM, Pickard, K, and Reaven, J. Emotion regulation: a treatment target for autism spectrum disorder. Bull Menn Clin. (2019) 83:205–34. doi: 10.1521/bumc.2019.83.3.205
49. Bemmouna, D, Coutelle, R, Weibel, S, and Weiner, L. Feasibility, acceptability and preliminary efficacy of dialectical behaviour therapy for autistic adults without intellectual disability: a mixed methods study. J Autism Dev Disord. (2022) 52:4337–54. doi: 10.1007/s10803-021-05317-w
50. Ritschel, LA, Guy, L, and Maddox, BB. A pilot study of dialectical behaviour therapy skills training for autistic adults. Behav Cogn Psychother. (2022) 50:187–202. doi: 10.1017/S1352465821000370
51. Mazefsky, CA, and White, SW. Emotion regulation: concepts & practice in autism spectrum disorder. Child Adolesc Psychiatr Clin N Am. (2014) 23:15–24. doi: 10.1016/j.chc.2013.07.002
52. Eells, TD. Review of the case formulation approach to cognitive-behaviour therapy. Psychotherapy (Chic). (2009) 46:400–1. doi: 10.1037/a0017014
53. Greenhalgh, T, Thorne, S, and Malterud, K. Time to challenge the spurious hierarchy of systematic over narrative reviews? Eur J Cin Invest. (2018) 48:e12931. doi: 10.1111/eci.12931
54. Rozas, LW, and Klein, WC. The value and purpose of the traditional qualitative literature review. J Evid Based Soc Work. (2010) 7:387–99. doi: 10.1080/15433710903344116
55. Baethge, C, Goldbeck-Wood, S, and Mertens, S. SANRA-a scale for the quality assessment of narrative review articles. Res Integrity Peer Rev. (2019) 4:5. doi: 10.1186/s41073-019-0064-8
56. Khor, AS, Melvin, GA, Reid, SC, and Gray, KM. Coping, daily hassles and behaviour and emotional problems in adolescents with high-functioning autism / Asperger’s disorder. J Autism Dev Disord. (2014) 44:593–608. doi: 10.1007/s10803-013-1912-x
57. Swain, D, Scarpa, A, White, S, and Laugeson, E. Emotion dysregulation and anxiety in adults with ASD: does social motivation play a role? J Autism Dev Disord. (2015) 45:3971–7. doi: 10.1007/s10803-015-2567-6
58. Bender, PK, Reinholdt-Dunne, ML, Esbjørn, BH, and Pons, F. Emotion dysregulation and anxiety in children and adolescents: gender differences. Personal Individ Differ. (2012) 53:284–8. doi: 10.1016/j.paid.2012.03.027
59. Sáez-Suanes, GP, García-Villamisar, D, and Pozo Armentia, AD. Does the gender matter?: anxiety symptoms and emotion dysregulation in adults with autism and intellectual disabilities. Autism Res. (2023) 16:113–21. doi: 10.1002/aur.2839
60. Weiner, L, Perroud, N, and Weibel, S. Attention deficit hyperactivity disorder and borderline personality disorder in adults: a review of their Links and risks. Neuropsychiatr Dis Treat. (2019) 15:3115–29. doi: 10.2147/NDT.S192871
61. Wieckowski, AT, Luallin, S, Pan, Z, Righi, G, Gabriels, RL, and Mazefsky, C. Gender differences in emotion dysregulation in an autism inpatient psychiatric sample. Autism Res. (2020) 13:1343–8. doi: 10.1002/aur.2295
62. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed (2013).
63. Mazefsky, CA. Emotion regulation and emotional distress in autism spectrum disorder: foundations and considerations for future research. J Autism Dev Disord. (2015) 45:3405–8. doi: 10.1007/s10803-015-2602-7
64. Greenlee, JL, Stelter, CR, Piro-Gambetti, B, and Hartley, SL. Trajectories of dysregulation in children with autism Spectrum disorder. Journal of clinical child and adolescent psychology: the official journal for the Society of Clinical Child and Adolescent Psychology. Am Psychol Assoc. (2021) 50:858–73. doi: 10.1080/15374416.2021.1907752
65. Kobylińska, D, and Kusev, P. Flexible emotion regulation: how situational demands and individual differences influence the effectiveness of regulatory strategies. Front Psychol. (2019) 10:72. doi: 10.3389/fpsyg.2019.00072
66. Eftekhari, A, Zoellner, LA, and Vigil, SA. Patterns of emotion regulation and psychopathology. Anxiety Stress Coping. (2009) 22:571–86. doi: 10.1080/10615800802179860
67. Militerni, R, Bravaccio, C, Falco, C, Fico, C, and Palermo, MT. Repetitive behaviours in autistic disorder. Eur Child Adolesc Psychiatry. (2002) 11:210–8. doi: 10.1007/s00787-002-0279-x
68. Maddox, BB, Trubanova, A, and White, SW. Untended wounds: non-suicidal self-injury in adults with autism spectrum disorder. Autism. (2017) 21:412–22. doi: 10.1177/1362361316644731
69. Goldfarb, Y, Zafrani, O, Hedley, D, Yaari, M, and Gal, E. Autistic adults' subjective experiences of hoarding and self-injurious behaviors. Autism. (2021) 25:1457–68. doi: 10.1177/1362361321992640
70. Minshawi, NF, Hurwitz, S, Fodstad, JC, Biebl, S, Morriss, DH, and McDougle, CJ. The association between self-injurious behaviors and autism spectrum disorders. Psychol Res Behav Manag. (2014) 7:125–36. doi: 10.2147/PRBM.S44635
71. Licence, L, Oliver, C, Moss, J, and Richards, C. Prevalence and risk-markers of self-harm in autistic children and adults. J Autism Dev Disord. (2020) 50:3561–74. doi: 10.1007/s10803-019-04260-1
72. Hossain, MM, Khan, N, Sultana, A, Ma, P, McKyer, ELJ, Ahmed, HU, et al. Prevalence of comorbid psychiatric disorders among people with autism spectrum disorder: an umbrella review of systematic reviews and meta-analyses. Psychiatry Res. (2020) 287:112922. doi: 10.1016/j.psychres.2020.112922
73. Moseley, DS, Tonge, BJ, Brereton, AV, and Einfeld, SL. Psychiatric comorbidity in adolescents and young adults with autism. J Ment Health Res Intellect Disabil. (2011) 4:229–43. doi: 10.1080/19315864.2011.595535
74. Charlton, AS, Smith, IC, Mazefsky, CA, and White, SW. The role of emotion regulation on co-occurring psychopathology in emerging adults with ASD. J Autism Dev Disord. (2020) 50:2585–92. doi: 10.1007/s10803-019-03983-5
75. Davico, C, Marcotulli, D, Cudia, VF, Arletti, L, Ghiggia, A, Svevi, B, et al. Emotional dysregulation and adaptive functioning in preschoolers with autism spectrum disorder or other neurodevelopmental disorders. Front Psych. (2022) 13:846146. doi: 10.3389/fpsyt.2022.846146
76. Paris, J. Suicidality in borderline personality disorder. Medicina (Kaunas). (2019) 55:223. doi: 10.3390/medicina55060223
77. Jachyra, P, Lai, MC, Zaheer, J, Fernandes, N, Dale, M, Sawyer, A, et al. Suicidal thoughts and behaviours among autistic adults presenting to the psychiatric emergency department: an exploratory chart review. J Autism Dev Disord. (2022) 52:2367–75. doi: 10.1007/s10803-021-05102-9
78. Moseley, RL, Gregory, NJ, Smith, P, Allison, C, and Baron-Cohen, S. Links between self-injury and suicidality in autism. Mol Autism. (2020) 11:14. doi: 10.1186/s13229-020-0319-8
79. Steenfeldt-Kristensen, C, Jones, CA, and Richards, C. The prevalence of self-injurious behaviour in autism: a meta-analytic study. J Autism Dev Disord. (2020) 50:3857–73. doi: 10.1007/s10803-020-04443-1
80. Dell'Osso, L, Carpita, B, Muti, D, Morelli, V, Salarpi, G, Salerni, A, et al. Mood symptoms and suicidality across the autism spectrum. Compr Psychiatry. (2019) 91:34–8. doi: 10.1016/j.comppsych.2019.03.004
81. Hedley, D, and Uljarevic, M. Systematic review of suicide in autism spectrum disorder: current trends and implications. Curr Dev Disord Rep. (2018) 5:65–76. doi: 10.1007/s40474-018-0133-6
82. Richa, S, Fahed, M, Khoury, E, and Mishara, B. Suicide in autism spectrum disorders. Archives Suicide Res. (2014) 18:327–39. doi: 10.1080/13811118.2013.824834
83. Segers, M, and Rawana, J. What do we know about suicidality in autism spectrum disorders? A systematic review. Autism Res. (2014) 7:507–21. doi: 10.1002/aur.1375
84. Mayes, SD, Calhoun, SL, Baweja, R, and Mahr, F. Suicide ideation and attempts in children with psychiatric disorders and typical development. Crisis. (2015) 36:55–60. doi: 10.1027/0227-5910/a000284
85. Cassidy, S, Bradley, P, Robinson, J, Allison, C, McHugh, M, and Baron-Cohen, S. Suicidal ideation and suicide plans or attempts in adults with Asperger's syndrome attending a specialist diagnostic clinic: a clinical cohort study. Lancet Psychiatry. (2014) 1:142–7. doi: 10.1016/S2215-0366(14)70248-2
86. Hirvikoski, T, Mittendorfer-Rutz, E, Boman, M, Larsson, H, Lichtenstein, P, and Bölte, S. Premature mortality in autism spectrum disorder. Br J Psychiatry J Ment Sci. (2016) 208:232–8. doi: 10.1192/bjp.bp.114.160192
87. Kirby, AV, Bakian, AV, Zhang, Y, Bilder, DA, Keeshin, BR, and Coon, H. A 20-year study of suicide death in a statewide autism population. Autism Res. (2019) 12:658–66. doi: 10.1002/aur.2076
88. Kõlves, K, Fitzgerald, C, Nordentoft, M, Wood, SJ, and Erlangsen, A. Assessment of suicidal behaviours among individuals with autism spectrum disorder in Denmark. J Am Med Assoc. (2021) 4:e2033565. doi: 10.1001/jamanetworkopen.2020.33565
89. Moseley, RL, Gregory, NJ, Smith, P, Allison, C, Cassidy, S, and Baron-Cohen, S. Non-suicidal self-injury and its relation to suicide through acquired capability: investigating this causal mechanism in a mainly late-diagnosed autistic sample. Mol Autism. (2022) 13:45. doi: 10.1186/s13229-022-00522-5
90. Beck, JS, Lundwall, RA, Gabrielsen, T, Cox, JC, and South, M. Looking good but feeling bad: "camouflaging" behaviours and mental health in women with autistic traits. Autism. (2020) 24:809–21. doi: 10.1177/1362361320912147
91. Meng-Chuan LaiLombardo, MV, Ruigrok, ANV, Chakrabarti, B, Auyeung, B, Szatmari, P, et al. Quantifying and exploring camouflaging in men and women with autism. Autism. (2017) 21:690–702. doi: 10.1177/1362361316671012
92. Gesi, C, Migliarese, G, Torriero, S, Capellazzi, M, Omboni, AC, Cerveri, G, et al. Gender differences in misdiagnosis and delayed diagnosis among adults with autism spectrum disorder with no language or intellectual disability. Brain Sci. (2021) 11:912. doi: 10.3390/brainsci11070912
93. Hull, L, Levy, L, Lai, MC, Petrides, KV, Baron-Cohen, S, Allison, C, et al. Is social camouflaging associated with anxiety and depression in autistic adults? Mol Autism. (2021) 12:13. doi: 10.1186/s13229-021-00421-1
94. Cazalis, F, Reyes, E, Leduc, S, and Gourion, D. Evidence that nine autistic women out of ten have been victims of sexual violence. Front Behav Neurosci. (2022) 16:852203. doi: 10.3389/fnbeh.2022.852203
95. Ohlsson Gotby, V, Lichtenstein, P, Långström, N, and Pettersson, E. Childhood neurodevelopmental disorders and risk of coercive sexual victimization in childhood and adolescence - a population-based prospective twin study. J Child Psychol Psychiatry. (2018) 59:957–65. doi: 10.1111/jcpp.12884
96. Shaikh, U, Qamar, I, Jafry, F, Hassan, M, Shagufta, S, Odhejo, YI, et al. Patients with borderline personality disorder in emergency departments. Front Psych. (2017) 8:136. doi: 10.3389/fpsyt.2017.00136
97. Berkovits, L, Eisenhower, A, and Blacher, J. Emotion regulation in young children with autism spectrum disorders. J Autism Dev Disord. (2017) 47:68–79. doi: 10.1007/s10803-016-2922-2
98. Joshi, G, Wozniak, J, Fitzgerald, M, Faraone, S, Fried, R, Galdo, M, et al. High risk for severe emotional dysregulation in psychiatrically referred youth with autism spectrum disorder: a controlled study. J Autism Dev Disord. (2018) 48:3101–15. doi: 10.1007/s10803-018-3542-9
99. Mandell, DS, Walrath, CM, Manteuffel, B, Sgro, G, and Pinto-Martin, JA. The prevalence and correlates of abuse among children with autism served in comprehensive community-based mental health settings. Child Abuse Negl. (2005) 29:1359–72. doi: 10.1016/j.chiabu.2005.06.006
100. McDonnell, CG, Boan, AD, Bradley, CC, Seay, KD, Charles, JM, and Carpenter, LA. Child maltreatment in autism spectrum disorder and intellectual disability: results from a population-based sample. J Child Psychol Psychiatry. (2019) 60:576–84. doi: 10.1111/jcpp.12993
101. Richey, JA, Damiano, CR, Sabatino, A, Rittenberg, A, Petty, C, Bizzell, J, et al. Neural mechanisms of emotion regulation in autism spectrum disorder. J Autism Dev Disord. (2015) 45:3409–23. doi: 10.1007/s10803-015-2359-z
102. Andrews, DS, Aksman, L, Kerns, CM, Lee, JK, Winder-Patel, BM, Harvey, DJ, et al. Association of amygdala development with different forms of anxiety in autism spectrum disorder. Biol Psychiatry. (2022) 91:977–87. doi: 10.1016/j.biopsych.2022.01.016
103. Mazefsky, CA, Collier, A, Golt, J, and Siegle, GJ. Neural features of sustained emotional information processing in autism spectrum disorder. Autism. (2020) 24:941–53. doi: 10.1177/1362361320903137
104. Pitskel, NB, Bolling, DZ, Kaiser, MD, Pelphrey, KA, and Crowley, MJ. Neural systems for cognitive reappraisal in children and adolescents with autism spectrum disorder. Dev Cogn Neurosci. (2014) 10:117–28. doi: 10.1016/j.dcn.2014.08.007
105. White, SW, Mazefsky, CA, Dichter, GS, Chiu, PH, Richey, JA, and Ollendick, TH. Social-cognitive, physiological, and neural mechanisms underlying emotion regulation impairments: understanding anxiety in autism spectrum disorder. Int J Develop Neurosci. (2014) 39:22–36. doi: 10.1016/j.ijdevneu.2014.05.012
106. Dichter, GS. Functional magnetic resonance imaging of autism spectrum disorders. Dialogues Clin Neurosci. (2012) 14:319–51. doi: 10.31887/DCNS.2012.14.3/gdichter
107. Fresco, DM, Roy, AK, Adelsberg, S, Seeley, S, García-Lesy, E, Liston, C, et al. Distinct functional connectivities predict clinical response with emotion regulation therapy. Front Hum Neurosci. (2017) 11:86. doi: 10.3389/fnhum.2017.00086
108. Goldin, PR, McRae, K, Ramel, W, and Gross, JJ. The neural bases of emotion regulation: reappraisal and suppression of negative emotion. Biol Psychiatry. (2008) 63:577–86. doi: 10.1016/j.biopsych.2007.05.031
109. Lassalle, A, Åsberg Johnels, J, Zürcher, NR, Hippolyte, L, Billstedt, E, Ward, N, et al. Hypersensitivity to low intensity fearful faces in autism when fixation is constrained to the eyes. Hum Brain Mapp. (2017) 38:5943–57. doi: 10.1002/hbm.23800
110. Kuiper, MWM, Verhoeven, EWM, and Geurts, HM. Stop making noise! Auditory sensitivity in adults with an autism spectrum disorder diagnosis: physiological habituation and subjective detection thresholds. J Autism Dev Disord. (2019) 49:2116–28. doi: 10.1007/s10803-019-03890-9
111. Top, DN Jr, Luke, SG, Stephenson, KG, and South, M. Psychophysiological arousal and auditory sensitivity in a cross-clinical sample of autistic and non-autistic anxious adults. Front Psych. (2019) 9:783. doi: 10.3389/fpsyt.2018.00783
112. Lydon, S, Healy, O, Reed, P, Mulhern, T, Hughes, BM, and Goodwin, MS. A systematic review of physiological reactivity to stimuli in autism. Dev Neurorehabil. (2016) 19:335–55. doi: 10.3109/17518423.2014.971975
113. De Groot, K, and Van Strien, JW. Self-report and brain indicators of impaired emotion regulation in the broad autism Spectrum. J Autism Dev Disord. (2017) 47:2138–52. doi: 10.1007/s10803-017-3138-9
114. Spratt, EG, Nicholas, JS, Brady, KT, Carpenter, LA, Hatcher, CR, Meekins, KA, et al. Enhanced cortisol response to stress in children in autism. J Autism Dev Disord. (2012) 42:75–81. doi: 10.1007/s10803-011-1214-0
115. Fenning, RM, Baker, JK, and Moffitt, J. Intrinsic and extrinsic predictors of emotion regulation in children with autism spectrum disorder. J Autism Dev Disord. (2018) 48:3858–70. doi: 10.1007/s10803-018-3647-1
116. Mauss, IB, Evers, C, Wilhelm, FH, and Gross, JJ. How to bite your tongue without blowing your top: implicit evaluation of emotion regulation predicts affective responding to anger provocation. Personal Soc Psychol Bull. (2006) 32:589–602. doi: 10.1177/0146167205283841
117. Normansell-Mossa, KM, Top, DN Jr, Russell, N, Freeston, M, Rodgers, J, and South, M. Sensory sensitivity and intolerance of uncertainty influence anxiety in autistic adults. Front Psychol. (2021) 12:731753. doi: 10.3389/fpsyg.2021.731753
118. Raymaker, DM, Teo, AR, Steckler, NA, Lentz, B, Scharer, M, Delos Santos, A, et al. Having all of your internal resources iexhausted beyond measure and being left with no clean-up cew: defining autistic burnout. Autism Adulthood. (2020) 2:132–43. doi: 10.1089/aut.2019.0079
119. Senju, A. Spontaneous theory of mind and its absence in autism spectrum disorders. Neuroscientist. (2012) 18:108–13. doi: 10.1177/1073858410397208
120. Gernsbacher, MA, and Yergeau, M. Empirical failures of the claim that autistic people lack a theory of mind. Arch Sci Psychol. (2019) 7:102–18. doi: 10.1037/arc0000067
121. Chambers, R, Gullone, E, and Allen, NB. Mindful emotion regulation: an integrative review. Clin Psychol Rev. (2009) 29:560–72. doi: 10.1016/j.cpr.2009.06.005
122. Poquérusse, J, Pastore, L, Dellantonio, S, and Esposito, G. Alexithymia and autism spectrum disorder: a complex relationship. Front Psychol. (2018) 9:1196. doi: 10.3389/fpsyg.2018.01196
123. Weiner, L, Costache, ME, and Bemmouna, D. Emotion dysregulation is heightened in autistic females: A comparison with autistic males and borderline personality disorder. Womens Health (Lond). (2023) 19. doi: 10.1177/17455057231174763
124. Bonanno, GA, and Burton, CL. Regulatory flexibility: an individual differences perspective on coping and emotion regulation. Perspect Psychol Sci. (2013) 8:591–612. doi: 10.1177/1745691613504116
125. Aldao, A, and Nolen-Hoeksema, S. Specificity of cognitive emotion regulation strategies: a transdiagnostic examination. Behav Res Ther. (2010) 48:974–83. doi: 10.1016/j.brat.2010.06.002
126. Mazefsky, CA, Pelphrey, KA, and Dahl, RE. The need for a broader approach to emotion regulation research in autism. Child Dev Perspect. (2012) 6:92–7. doi: 10.1111/j.1750-8606.2011.00229.x
127. Pehlivanidis, A, Papanikolaou, K, Korobili, K, Kalantzi, E, Mantas, V, Pappa, D, et al. Trait-based dimensions discriminating adults with attention deficit hyperactivity disorder (ADHD), autism spectrum disorder (ASD) and, co-occurring ADHD/ASD. Brain Sci. (2020) 11:18. doi: 10.3390/brainsci11010018
128. Soler-Gutiérrez, AM, Pérez-González, JC, and Mayas, J. Evidence of emotion dysregulation as a core symptom of adult ADHD: a systematic review. PLoS One. (2023) 18:e0280131. doi: 10.1371/journal.pone.0280131
129. Duerden, EG, Oatley, HK, Mak-Fan, KM, McGrath, PA, Taylor, MJ, Szatmari, P, et al. Risk factors associated with self-injurious behaviours in children and adolescents with autism spectrum disorders. J Autism Dev Disord. (2012) 42:2460–70. doi: 10.1007/s10803-012-1497-9
130. Robertson, AE, and Simmons, DR. The sensory experiences of adults with autism Spectrum disorder: a qualitative analysis. Perception. (2015) 44:569–86. doi: 10.1068/p7833
131. Fuld, S. Autism Spectrum disorder: the impact of stressful and traumatic life events and implications for clinical practice. Clin Soc Work J. (2018) 46:210–9. doi: 10.1007/s10615-018-0649-6
132. Hellström, L. A systematic review of polyvictimization among children with attention deficit hyperactivity or autism spectrum disorder. Int J Environ Res Public Health. (2019) 16:2280. doi: 10.3390/ijerph16132280
133. Taylor, JL, and Gotham, KO. Cumulative life events, traumatic experiences, and psychiatric symptomatology in transition-aged youth with autism spectrum disorder. J Neurodev Disord. (2016) 8:28. doi: 10.1186/s11689-016-9160-y
134. Bargiela, S, Steward, R, and Mandy, W. The experiences of late-diagnosed women with autism spectrum conditions: an investigation of the female autism phenotype. J Autism Dev Disord. (2016) 46:3281–94. doi: 10.1007/s10803-016-2872-8
135. Fisher, MH, Epstein, RA, Urbano, RC, Vehorn, A, Cull, MJ, and Warren, Z. A population-based examination of maltreatment referrals and substantiation for children with autism spectrum disorder. Autism. (2019) 23:1335–40. doi: 10.1177/1362361318813998
136. Milton, DEM. On the ontological status of autism: the ‘double empathy problem’. Disability Soc. (2012) 27:883–7. doi: 10.1080/09687599.2012.710008
137. Milton, D, Gurbuz, E, and Lopez, B. The 'double empathy problem': ten years on. Autism. (2022) 26:1901–3. doi: 10.1177/13623613221129123
138. Frost, KM, Bailey, KM, and Ingersoll, BR. "I just want them to see me as…me": identity, community, and disclosure practices among college students on the autism Spectrum. Autism Adulthood. (2019) 1:268–75. doi: 10.1089/aut.2018.0057
139. Kerns, CM, Lankenau, S, Shattuck, PT, Robins, DL, Newschaffer, CJ, and Berkowitz, SJ. Exploring potential sources of childhood trauma: a qualitative study with autistic adults and caregivers. Autism. (2022) 26:1987–98. doi: 10.1177/13623613211070637
140. Rumball, F, Happé, F, and Grey, N. Experience of trauma and PTSD symptoms in autistic adults: risk of PTSD development following DSM-5 and non-DSM-5 traumatic life events. Autism Res. (2020) 13:2122–32. doi: 10.1002/aur.2306
141. Mehtar, M, and Mukaddes, NM. Posttraumatic stress disorder in individuals with diagnosis of autistic spectrum disorders. Res Autism Spectr Disord. (2011) 5:539–46. doi: 10.1016/j.rasd.2010.06.020
142. Roberts, AL, Koenen, KC, Lyall, K, Robinson, EB, and Weisskopf, MG. Association of autistic traits in adulthood with childhood abuse, interpersonal victimization, and posttraumatic stress. Child Abuse Negl. (2015) 45:135–42. doi: 10.1016/j.chiabu.2015.04.010
143. Ball, JS, and Links, PS. Borderline personality disorder and childhood trauma: evidence for a causal relationship. Curr Psychiatry Rep. (2009) 11:63–8. doi: 10.1007/s11920-009-0010-4
144. Sterzing, PR, Shattuck, PT, Narendorf, SC, Wagner, M, and Cooper, BP. Bullying involvement and autism spectrum disorders: prevalence and correlates of bullying involvement among adolescents with an autism spectrum disorder. Arch Pediatr Adolesc Med. (2012) 166:1058–64. doi: 10.1001/archpediatrics.2012.790
145. Cappadocia, MC, Weiss, JA, and Pepler, D. Bullying experiences among children and youth with autism spectrum disorders. J Autism Dev Disord. (2012) 42:266–77. doi: 10.1007/s10803-011-1241-x
146. Janson, GR, and Hazler, RJ. Trauma reactions of bystanders and victims to repetitive abuse experiences. Violence Vict. (2004) 19:239–255.
147. Camodeca, M, and Nava, E. The long-term effects of bullying, victimization, and bystander behaviour on emotion regulation and its physiological correlates. J Interpers Violence. (2022) 37:NP2056–75. doi: 10.1177/0886260520934438
148. Brown-Lavoie, SM, Viecili, MA, and Weiss, JA. Sexual knowledge and victimization in adults with autism spectrum disorders. J Autism Dev Disord. (2014) 44:2185–96. doi: 10.1007/s10803-014-2093-y
149. Weiss, JA, and Fardella, MA. Victimization and perpetration experiences of adults with autism. Front Psych. (2018) 9:203. doi: 10.3389/fpsyt.2018.00203
150. Crane, L, Hearst, C, Ashworth, M, Davies, J, and Hill, EL. Supporting newly identified or diagnosed autistic adults: an initial evaluation of an autistic-led programme. J Autism Dev Disord. (2021) 51:892–905. doi: 10.1007/s10803-020-04486-4
151. Moseley, RL, Turner-Cobb, JM, Spahr, CM, Shields, GS, and Slavich, GM. Lifetime and perceived stress, social support, loneliness, and health in autistic adults. Health Psychol. (2021) 40:556–68. doi: 10.1037/hea0001108
152. Stagg, SD, and Belcher, H. Living with autism without knowing: receiving a diagnosis in later life. Health Psychol Behav Med. (2019) 7:348–61. doi: 10.1080/21642850.2019.1684920
153. Dubreucq, J, Plasse, J, Gabayet, F, Faraldo, M, Blanc, O, Chereau, I, et al. Self-stigma in serious mental illness and autism spectrum disorder: results from the REHABase national psychiatric rehabilitation cohort. Eur Psychiatry. (2020) 63:e13. doi: 10.1192/j.eurpsy.2019.12
154. Turnock, A, Langley, K, and Jones, CRG. Understanding stigma in autism: a narrative review and theoretical model. Autism Adulthood. (2022) 4:76–91. doi: 10.1089/aut.2021.0005
155. Cage, E, and Troxell-Whitman, Z. Understanding the reasons, contexts and costs of camouflaging for autistic adults. J Autism Dev Disord. (2019) 49:1899–911. doi: 10.1007/s10803-018-03878-x
156. Perry, E, Mandy, W, Hull, L, and Cage, E. Understanding camouflaging as a response to autism-related stigma: a social identity theory approach. J Autism Dev Disord. (2022) 52:800–10. doi: 10.1007/s10803-021-04987-w
157. Cassidy, SA, Gould, K, Townsend, E, Pelton, M, Robertson, AE, and Rodgers, J. Is camouflaging autistic traits associated with suicidal thoughts and Behaviours? Expanding the interpersonal psychological theory of suicide in an undergraduate student sample. J Autism Dev Disord. (2020) 50:3638–48. doi: 10.1007/s10803-019-04323-3
158. Moseley, RL, Gregory, NJ, Smith, P, Allison, C, Cassidy, S, and Baron-Cohen, S. The relevance of the interpersonal theory of suicide for predicting past-year and lifetime suicidality in autistic adults. Mol Autism. (2022) 13:14. doi: 10.1186/s13229-022-00495-5
159. Wood-Downie, H, Wong, B, Kovshoff, H, Mandy, W, Hull, L, and Hadwin, JA. Sex/gender differences in camouflaging in children and adolescents with autism. J Autism Dev Disord. (2021) 51:1353–64. doi: 10.1007/s10803-020-04615-z
160. Gulsrud, AC, Jahromi, LB, and Kasari, C. The co-regulation of emotions between mothers and their children with autism. J Autism Dev Disord. (2010) 40:227–37. doi: 10.1007/s10803-009-0861-x
161. Baker, JK, Fenning, RM, Crnic, KA, Baker, BL, and Blacher, J. Prediction of social skills in 6-year-old children with and without developmental delays: contributions of early regulation and maternal scaffolding. Am J Mental Retard. (2007) 112:375–91. doi: 10.1352/0895-8017(2007)112[0375:POSSIY]2.0.CO;2
162. Ting, V, and Weiss, JA. Emotion regulation and parent co-regulation in children with autism spectrum disorder. J Autism Dev Disord. (2017) 47:680–9. doi: 10.1007/s10803-016-3009-9
163. Baker, JK, Fenning, RM, and Moffitt, JA. Cross-Sectional Examination of the Internalization of Emotion Co-regulatory Support in Children with ASD. J Autism Dev Disord. (2019) 49:4332–4338. doi: 10.1007/s10803-019-04091-0
164. Jahromi, LB, Meek, SE, and Ober-Reynolds, S. Emotion regulation in the context of frustration in children with high functioning autism and their typical peers. J Child Psychol Psychiatry. (2012) 53:1250–8. doi: 10.1111/j.1469-7610.2012.02560.x
165. Flujas-Contreras, JM, García-Palacios, A, and Gómez, I. Parenting intervention for psychological flexibility and emotion regulation: clinical protocol and an evidence-based case study. Int J Environ Res Public Health. (2022) 19:5014. doi: 10.3390/ijerph19095014
166. Hendrix, NM, Pickard, KE, Binion, GE, and Kushner, E. A systematic review of emotion regulation in parent-mediated interventions for autism spectrum disorder. Front Psych. (2022) 13:846286. doi: 10.3389/fpsyt.2022.846286
167. DeLucia, EA, McKenna, MP, Andrzejewski, TM, Valentino, K, and McDonnell, CG. A pilot study of self-regulation and behaviour problems in preschoolers with ASD: parent broader autism phenotype traits relate to child emotion regulation and inhibitory control. J Autism Dev Disord. (2022) 52:4397–411. doi: 10.1007/s10803-021-05322-z
168. Hergueta, T, Lecrubier, Y, Sheehan, D, and Weiller, E. Mini international neuropsychiatric interview. French Curr DSM-IV. (2015). doi: 10.13140/RG.2.1.2792.9440
169. Sheehan, DV, Lecrubier, Y, Sheehan, KH, Amorim, P, Janavs, J, Weiller, E, et al. The Mini-international neuropsychiatric interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. (1998) 59:22–57.
170. Baron-Cohen, S, Wheelwright, S, Skinner, R, Martin, J, and Clubley, E. The autism-spectrum quotient (AQ): evidence from Asperger syndrome/high-functioning autism, males and females, scientists and mathematicians. J Autism Dev Disord. (2001) 31:5–17. doi: 10.1023/a:1005653411471
171. Beck, AT, Epstein, N, Brown, G, and Steer, RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. (1988) 56:893–7. doi: 10.1037/0022-006X.56.6.893
172. Beck, AT, Steer, RA, and Brown, GK. Manual for beck depression inventory-II. San Antonio: Psychological Corporation (1996).
173. Gratz, KL, and Roemer, L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess. (2004) 26:41–54. doi: 10.1023/B:JOBA.0000007455.08539.94
174. Williams, ZJ, and Gotham, KO. RETRACTED ARTICLE: improving the measurement of alexithymia in autistic adults: a psychometric investigation and refinement of the twenty-item Toronto alexithymia scale. Mol Autism. (2021) 12:20. doi: 10.1186/s13229-021-00427-9
175. Hull, L, Mandy, W, Lai, M-C, Baron-Cohen, S, Allison, C, Smith, P, et al. Development and validation of the camouflaging autistic traits questionnaire (CAT-Q). J Autism Dev Disord. (2019) 49:819–33. doi: 10.1007/s10803-018-3792-6
176. De Gucht, V, Woestenburg, DHA, and Wilderjans, TF. The different faces of (high) sensitivity, toward a more comprehensive measurement instrument. Development and validation of the sensory processing sensitivity questionnaire (SPSQ). J Pers Assess. (2022) 104:784–99. doi: 10.1080/00223891.2022.2032101
177. Sauer, SE, and Baer, RA. Validation of measures of biosocial precursors to borderline personality disorder: childhood emotional vulnerability and environmental invalidation. Assessment. (2010) 17:454–66. doi: 10.1177/1073191110373226
178. Bernstein, DP, Stein, JA, Newcomb, MD, Walker, E, Pogge, D, Ahluvalia, T, et al. Development and validation of a brief screening version of the childhood trauma questionnaire. Child Abuse Negl. (2003) 27:169–90. doi: 10.1016/S0145-2134(02)00541-0
179. Neacsiu, AD, Eberle, JW, Kramer, R, Wiesmann, T, and Linehan, MM. Dialectical behaviour therapy skills for transdiagnostic emotion dysregulation. A pilot randomized controlled trial. Behav Res Ther. (2014) 59:40–51. doi: 10.1016/j.brat.2014.05.005
180. Van Spijker, BA, Batterham, PJ, Calear, AL, Farrer, L, Christensen, H, Reynolds, J, et al. The suicidal ideation attributes scale (SIDAS): community-based validation study of a new scale for the measurement of suicidal ideation. Suicide Life Threat Behav. (2014) 44:408–19. doi: 10.1111/sltb.12084
181. Cook, J, Crane, L, Bourne, L, Hull, L, and Mandy, W. Camouflaging in an everyday social context: an interpersonal recall study. Autism. (2021) 25:1444–56. doi: 10.1177/1362361321992641
182. Malinakova, K, Novak, L, Trnka, R, and Tavel, P. Sensory processing sensitivity questionnaire: a psychometric evaluation and associations with experiencing the COVID-19 pandemic. Int J Environ Res Public Health. (2021) 18:12962. doi: 10.3390/ijerph182412962
183. Bernstein, DP, and Fink, L. Childhood trauma questionnaire: a retrospective self-report manual San Antonio. TX: The Psychological Corporation (1998).
184. Keenan, EG, Gurba, AN, Mahaffey, B, Kappenberg, CF, and Lerner, MD. Leveling up dialectical behavior therapy for autistic individuals with emotion dysregulation: clinical and personal insights. Autism Adulthood. (2023). doi: 10.1089/aut.2022.0011
185. Morie, KP, Jackson, S, Zhai, ZW, Potenza, MN, and Dritschel, B. Mood disorders in high-functioning autism: the importance of alexithymia and emotional regulation. J Autism Dev Disord. (2019) 49:2935–45. doi: 10.1007/s10803-019-04020-1
186. Warrier, V, and Baron-Cohen, S. Childhood trauma, life-time self-harm, and suicidal behaviour and ideation are associated with polygenic scores for autism. Mol Psychiatry. (2021) 26(5):1670–1684. doi: 10.1038/s41380-019-0550-x
187. Brown, S, Shankar, R, and Smith, K. Borderline personality disorder and sensory processing impairment. Prog Neurol Psychiatry. (2009) 13:10–6. doi: 10.1002/pnp.127
188. Vegni, N, D'Ardia, C, and Torregiani, G. Empathy, mentalization, and theory of mind in borderline personality disorder: possible overlap with autism spectrum disorders. Front Psychol. (2021) 12:626353. doi: 10.3389/fpsyg.2021.626353
189. Brindle, K, Moulding, R, Bakker, K, and Nedeljkovic, M. Is the relationship between sensory‐processing sensitivity and negative affect mediated by emotional regulation? Aust J Psychol. (2015) 67:214–221. doi: 10.1111/ajpy.12084
190. MacIntosh, HB, Godbout, N, and Dubash, N. Borderline personality disorder: Disorder of trauma or personality, a review of the empirical literature. Can Psychol. (2015) 56:227–241. doi: 10.1037/cap0000028
191. Elder, JH, Kreider, CM, Brasher, SN, and Ansell, M. Clinical impact of early diagnosis of autism on the prognosis and parent-child relationships. Psychol Res Behav Manage. (2017) 10:283–92.
192. McQuaid, GA, Lee, NR, and Wallace, GL. Camouflaging in autism spectrum disorder: examining the roles of sex, gender identity, and diagnostic timing. Autism. (2022) 26:552–9. doi: 10.1177/13623613211042131
193. Bernardin, CJ, Lewis, T, Bell, D, and Kanne, S. Associations between social camouflaging and internalizing symptoms in autistic and non-autistic adolescents. Autism. (2021) 25:1580–91. doi: 10.1177/1362361321997284
194. Halsall, J, Clarke, C, and Crane, L. "camouflaging" by adolescent autistic girls who attend both mainstream and specialist resource classes: perspectives of girls, their mothers and their educators. Autism. (2021) 25:2074–86. doi: 10.1177/13623613211012819
195. Pecora, LA, Hancock, GI, Mesibov, GB, and Stokes, MA. Characterising the sexuality and sexual experiences of autistic females. J Autism Dev Disord. (2019) 49:4834–46. doi: 10.1007/s10803-019-04204-9
196. Jakobson, LS, and Rigby, SN. Alexithymia and Sensory Processing Sensitivity: Areas of Overlap and Links to Sensory Processing Styles. Psychol Res Behav Manage. (2017) 10:283–92. doi: 10.2147/PRBM.S117499
197. Biskin, RS. The lifetime course of borderline personality disorder. Front Psychol. (2021) 12:583786. doi: 10.3389/fpsyg.2021.583786
198. Kwan, C, Gitimoghaddam, M, and Collet, JP. Effects of social isolation and loneliness in children with neurodevelopmental disabilities: a scoping review. Brain Sci. (2020) 10:786. doi: 10.3390/brainsci10110786
199. Schmidt, P. Affective instability and emotion dysregulation as a social impairment. Front Psychol. (2022) 13:666016. doi: 10.3389/fpsyg.2022.666016
200. Strunz, S, Westphal, L, Ritter, K, Heuser, I, Dziobek, I, and Roepke, S. Personality pathology of adults with autism spectrum disorder without accompanying intellectual 7impairment in comparison to adults with personality disorders. J Autism Dev Disord. (2015) 45:4026–38. doi: 10.1007/s10803-014-2183-x
201. Van Dijke, A, and Ford, JD. Adult attachment and emotion dysregulation in borderline personality and somatoform disorders. Borderline Personal Disord Emot Dysregul. (2015) 2:6. doi: 10.1186/s40479-015-0026-9
202. Kuroda, M, Kawakubo, Y, Kamio, Y, Yamasue, H, Kono, T, Nonaka, M, et al. Preliminary efficacy of cognitive-behavioral therapy on emotion regulation in adults with autism spectrum disorder: a pilot randomized waitlist-controlled study. PLoS One. (2022) 17:e0277398. doi: 10.1371/journal.pone.0277398
Keywords: autism spectrum condition, emotion dysregulation, self-harm, suicidality, Linehan’s biosocial model, etiology
Citation: Bemmouna D and Weiner L (2023) Linehan’s biosocial model applied to emotion dysregulation in autism: a narrative review of the literature and an illustrative case conceptualization. Front. Psychiatry. 14:1238116. doi: 10.3389/fpsyt.2023.1238116
Received: 13 June 2023; Accepted: 11 September 2023;
Published: 29 September 2023.
Edited by:
Rita Barone, University of Catania, ItalyReviewed by:
Rebecca A. Lundwall, Brigham Young University, United StatesCopyright © 2023 Bemmouna and Weiner. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Doha Bemmouna, ZGJlbW1vdW5hQHVuaXN0cmEuZnI=; Luisa Weiner, d2VpbmVyQHVuaXN0cmEuZnI=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.