- 1Mood Disorders Center, Department of Psychiatry and Behavioral Sciences, Johns Hopkins School of Medicine, Baltimore, MD, United States
- 2Johns Hopkins Resident Outpatient Continuity Clinic, Department of Psychiatry and Behavioral Sciences, Johns Hopkins School of Medicine, Baltimore, MD, United States
- 3Johns Hopkins Bayview Community Psychiatry Program, Department of Psychiatry and Behavioral Sciences, Johns Hopkins School of Medicine, Baltimore, MD, United States
- 4Department of Psychiatry and Behavioral Sciences, Johns Hopkins Bayview Community Psychiatry Program, Johns Hopkins School of Medicine, Baltimore, MD, United States
Introduction: The objective of this study was to characterize the experiences and overall satisfaction of patients and providers with the March 2020 transition to telehealth in a psychiatric setting (telepsychiatry). The study also investigated how socio-demographic and clinical characteristics impact an individual’s experiences and satisfaction with telepsychiatry.
Methods: Responses were collected from 604 patients and 154 providers engaged in clinical care at one of three participating Johns Hopkins Medicine outpatient psychiatric clinics between January 2020–March 2021. Survey data were collected by self-report via Qualtrics or telephone follow-up.
Results: Respondents were predominately female and White. Over 70% of patients and providers were generally satisfied with telepsychiatry. However, providers were more likely to favor in-person care over telepsychiatry for post-pandemic care 48% to 17% respectively, while 35% rated both modalities equivalently. Patients were more evenly divided with 45% preferring telepsychiatry compared to 42% for in-person care, and only 13% rating them equivalently. Among providers, technical difficulties were significantly associated with both less satisfaction and lower preference for telepsychiatry [odds ratio for satisfaction (ORS) = 0.12; odds ratio for preference (ORP) = 0.13]. For patients, factors significantly associated with both lower satisfaction and lower preference for telepsychiatry included technical difficulties (ORS = 0.20; ORP = 0.41), unstable access to the internet (ORS = 0.46; ORP = 0.50), worsening depression (ORS = 0.38; ORP = 0.36), and worsening anxiety (ORS = 0.41; ORP = 0.40). Factors associated with greater satisfaction and higher preference for telepsychiatry among patients included higher education (ORS = 2.13; ORP = 1.96) and a decrease in technical difficulties over time (ORS = 2.86; ORP = 2.35).
Discussion: Patients and providers were satisfied with telepsychiatry. However, there were greater differences between them in preferences for continuing to use telepsychiatry post-pandemic. These findings highlight factors that influence patient and provider preferences and should be addressed to optimize the use of telepsychiatry in the future.
Introduction
The SARS-CoV-2 (COVID-19) pandemic caused unprecedented changes to healthcare services, including the rapid transition to telemedicine. Telemedicine refers to the provision of healthcare from a distance through information and communications technology (1). Telepsychiatry is the application of telehealth to psychiatric practice, encompassing services such as evaluations, individual or group therapy, psychoeducation, and medication management for behavioral health (2). The use of telepsychiatry and telemedicine in general was limited before the pandemic. For example, a study of over 200,000 privately insured and Medicare Advantage enrollees found that the overall rate of telemedicine encounters was quite low, reaching less than 7 per 1,000 enrollees in 2017 (3). Barriers to employing telepsychiatry prior to the pandemic included concerns about exacerbating challenges in access to care in some populations due to the digital divide, financial constraints, and difficulties faced by providers in understanding and adhering to varying state regulations (4–6).
Despite these concerns, telepsychiatry can have many advantages if implemented in a safe, effective manner that is acceptable to users and adaptable to specific facets of care across different specialties and clinics (2, 4, 7, 8). It is therefore crucial to identify what factors (e.g., dedicated technical support and additional clinical training) are likely to promote a telepsychiatry workflow that is user-friendly while still maintaining care efficacy and safety standards (2, 7, 8). In understanding these factors, both in the literature at large and within a specific clinic, healthcare systems can utilize telepsychiatry in a manner that promotes access to care and increased clinical efficiency in a sustainable and equitable manner (2, 4).
Research prior to the pandemic found that telemedicine consistently demonstrated treatment efficacy and patient acceptability that was comparable to in-person care. For instance, an evaluation of a telemedicine pilot program across five specialties, including psychiatry, found that the majority of patients (63%) and clinicians (59%) did not differentiate between virtual and office visits in terms of the overall quality of the visit (9). Subsequent studies continued to report overall high approval of telemedicine by both patients and providers, with Hubley et al. (10) noting telemedicine’s advantages of convenience and cost while maintaining comparable results to in-person appointments (3, 10–13).
During the pandemic, telepsychiatry utilization dramatically increased, accounting for almost 40% of all mental health and substance use outpatient visits at its peak (14). In contrast to pre-pandemic efforts, pandemic-era telepsychiatry was adopted rapidly and often with minimal planning or training, risking implementation of telepsychiatry in a manner that was neither sustainable nor on par with in-person care (7, 15). However, evaluations of telepsychiatry during this period continued to report high levels of satisfaction among patients and providers (6, 9, 16–21). Both groups identified many benefits, including ease of transportation and scheduling, lowered infection risk, and fewer cancellations (16, 17). Further, some providers noted increased feelings of safety while evaluating patients who may be prone to violence (20). However, ongoing challenges have persisted. For example, while using telehealth, providers must navigate interruptions in clinical care due to technological issues or distractions from the patient’s life (20, 22). Providers also report more challenges in establishing a therapeutic alliance and obtaining a holistic understanding of client health while using telehealth (20). Patient challenges predominantly include limited access to private spaces and technological issues (18). Despite the existing work dedicated to examining factors associated with successful telepsychiatry implementation, data are limited with regard to how patient and provider characteristics and clinical experiences help shape attitudes towards telepsychiatry. A greater understanding of these relationships will be crucial in determining how telepsychiatry has been successfully and equitably implemented during the pandemic, and where additional resources may be needed to help to optimize care.
The goal of the present study was to examine how the rapid transition to telepsychiatry impacted clinical care within a department of psychiatry from the perspective of both the patient and the provider. Specifically, we sought to examine the experiences of patients and providers with telepsychiatry during the COVID-19 pandemic and their preferences for telepsychiatry compared with in-person care for different aspects of treatment. Our work addresses previous limitations by investigating in greater detail patient and provider characteristics that are associated with their experiences and preferences for telepsychiatry. The ultimate goal of this work is to provide insights that can guide the practice of telepsychiatry by clarifying for whom it works well, what challenges persist, and if changes can be made to improve the quality of care delivered through telepsychiatry. These are urgent questions because the use of telepsychiatry has continued to grow beyond the public health crisis spurred by the COVID-19 pandemic.
Methods
Survey population
The survey was reviewed by the Institutional Review Board at the Johns Hopkins University School of Medicine and approved as a Quality Improvement project. Recipients of the survey were identified from two outpatient clinics in the Johns Hopkins Department of Psychiatry & Behavioral Sciences. The first, the Johns Hopkins Bayview Community Psychiatry Program (CPP), is a teaching hospital-based community mental health center of over 25 different ambulatory and school based clinical programs, including large adult and child outpatient programs. The second is the Johns Hopkins Resident Outpatient Continuity Clinic (ROCC), which is composed of psychiatry trainees and their clinical supervisors who provide both psychotherapy and pharmacological management to patients across the range of severe mental illnesses. Like the rest of the hospital system, these clinics made the abrupt transition to telepsychiatry in response to the pandemic between March 9, 2020 and March 16, 2020. Telepsychiatry remained the primary mode of service delivery for the next year including up to the deployment of the survey 1 year later as described below.
The survey
The survey was developed based on a literature review of prior surveys on telemedicine in tandem with feedback from providers across the Johns Hopkins Department of Psychiatry and Behavioral Sciences. Multiple items were adapted for use in this survey from previously validated questionnaires, including the Telemedicine Satisfaction Scale (23); the Telemedicine Usability Questionnaire (24); the System Usability Scale (25); the mHealth App Usability Questionnaire (26); the Consumer Assessment of Healthcare Providers and Systems (CAHPS) Experience of Care and Health Outcomes Survey (ECHO) Version 3.0, including the Managed Behavioral Health Organization and the Managed Care Organization Supplemental Surveys (27, 28); the University of Washington Telemedicine Patient Satisfaction Survey (29); and an adapted CAHPS survey designed by Donelan et al. (9).
The final survey included up to four sections. The first section captured information on participant characteristics, including socio-demographics and other contextual features (i.e., different aspects of either telepsychiatry or in-person encounters, such as internet stability, privacy, or commute times). The second section asked participants about their experiences with telepsychiatry. Responses in this section were collected using a 5-item Likert scale, ranging from not at all to very much. The third section asked participants about their preferences between telepsychiatry and in-person care for specific facets of mental health care. Participants were able to select one of four options: no opinion, no difference, in-person, or telemedicine. The final section asked participants to indicate how the COVID-19 pandemic had affected different aspects of their mental health over the previous 3 months. Participants were asked about changes in different mental health symptoms and substance use during the COVID-19 pandemic and could select one of four response options: never a problem, no change, decreased, or increased.
Two different versions of the survey were constructed to target patients (Supplementary Table S1) and providers (Supplementary Table S2). The provider survey asked about provider specific experiences and preferences for telepsychiatry, but it did not include the fourth section on changes in mental health during the COVID-19 pandemic. The patient survey asked about patient specific experiences and preferences for telepsychiatry and included all four sections. For patients younger than 18, questions regarding substance use were removed from the fourth section.
Survey dissemination
All patients who had an encounter in one of the two targeted clinics between January 1st, 2020 and February 4th, 2021 (for adult patients 18 years or older) or March 1st, 2021 (for child patients younger than age 18) were eligible to receive the survey. Providers practicing in these two clinics at the time were also eligible. All surveys were built in Qualtrics and disseminated by email. Provider surveys were disseminated on February 2nd, 2021. The patient surveys were disseminated to adult patients on February 16th and 17th, 2021 in the CPP and ROCC clinics, respectively, while they were distributed to child patients on March 4th, 2021 in CPP only. In the instance that the parent of a child received the survey, language was included asking the parent to share the survey with their child. Non-respondents received two follow-up emails per week for 8 weeks. The timing of these reminders fluctuated in an attempt to catch different patterns of availability. On March 31st and April 1st, 2021 300 adult non-responders were randomly selected for a telephone follow-up. Designated patients were called by one of two study team members and were given a reminder to complete the study, either on their own or via phone with the study team member if they preferred. Response collection was closed on May 14th, 2021.
Statistical analysis
Patient and provider characteristics, their experiences with telepsychiatry, and their preferences for telepsychiatry vs. in-person care for different facets of care were reported separately as percentages of total respondents for that specific item. For the presentation of results for experiences with telepsychiatry, Likert responses were grouped into three levels: “not at all or a little”, somewhat, and “moderately or very much”. Separate logistic regression models were then used to examine the relationship between patient and provider characteristics and their experiences with telepsychiatry and their preferences for telepsychiatry vs. in-person care. For the examination of experiences with telepsychiatry, the primary analysis focused on overall satisfaction, while for preferences the primary analysis focused on preference for telepsychiatry vs. in-person care post-pandemic (i.e., “if the pandemic goes away”). In these models, the Likert responses for telepsychiatry experiences were dichotomized across the median response (lower than the median response vs. median or higher response). In instances where the median response was an extreme value (not at all or very much) responses were dichotomized as the median vs. all other values. Similarly, responses for treatment modality preferences (telemedicine, in-person, or no difference) were dichotomized as preference for “telemedicine or no difference” vs. in-person treatment (i.e., standard of care). All logistic regression models except those reported for exploratory analyses were adjusted for age, sex, and race. Results at p ≤ 0.05 were considered statistically significant. We did not correct for multiple testing because the a priori goal was to generate hypotheses about the range of features that might be associated with patient and provider experiences with and preferences for telepsychiatry. R version 4.1.1 was used for all statistical analysis.
Results
Patient characteristics
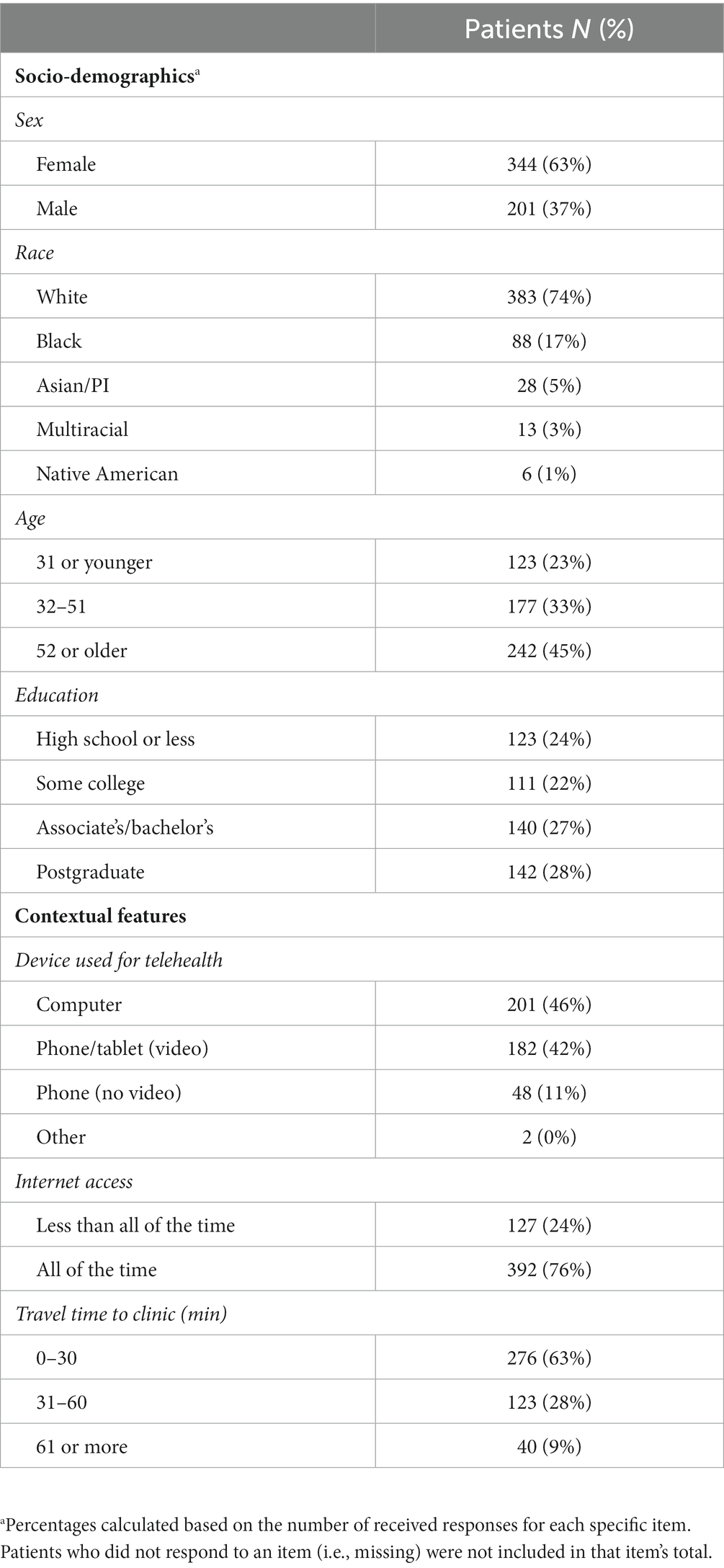
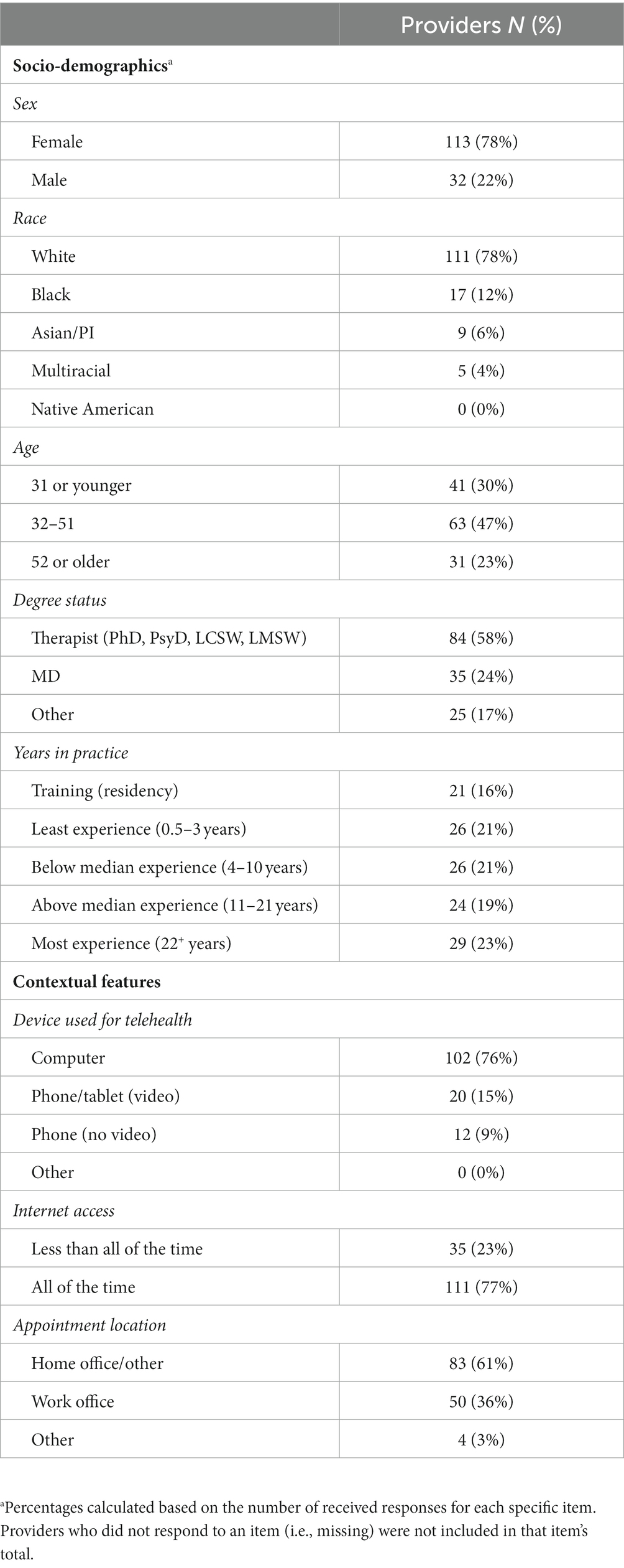
A total of 604 patients out of 3,017 (20%) completed the survey. Patient characteristics are listed in Table 1. The majority of patients were female (63%, n = 344) and White (74%, n = 383). Most patients had some education above the high school level (76%, n = 393). The majority of patients used either their computer (46%, n = 201) or video on their phone/tablet (42%, n = 182) for telepsychiatry visits and had reliable internet all of the time (76%, n = 392). A majority of patients were local, living within 30 min of their respective clinic (63%, n = 276).
Provider characteristics
A total of 154 providers out of 250 (62%) completed the survey. Provider characteristics are listed in Table 2. The majority of providers were female (78%, n = 113) and White (78%, n = 111). Responding providers included mental health therapists (58%, n = 84), psychiatrists/physicians (24%, n = 35), and second to fourth post-graduate year (PGY-2–PGY-4) psychiatry resident physicians (16%, n = 21). Most providers used computers (76%, n = 102) for their telepsychiatry encounters and had internet access all of the time (77%, n = 111).
Patient experiences with telepsychiatry
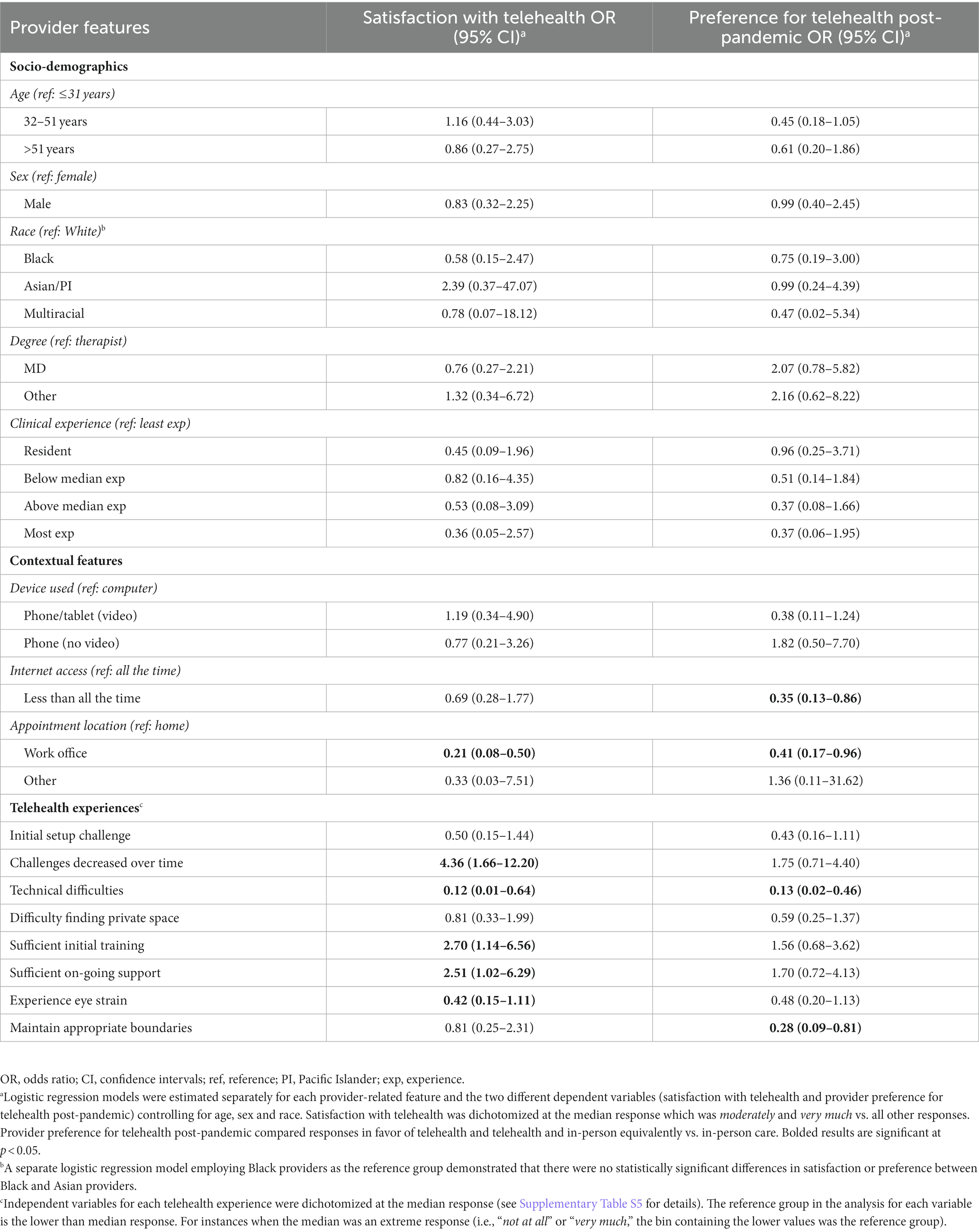
Summary results of patient experiences with telepsychiatry are shown in Figure 1 with more details provided in Supplementary Table S3. Most patients experienced few challenges (i.e., “not at all or a little”) with their initial telepsychiatry encounter (76%, n = 364). Further, most patients felt challenges with telepsychiatry “moderately or very much” decreased over time (61%, n = 147). The majority of patients said that technical difficulties interfered with treatment “not at all or a little” (85%, n = 405). Additionally, most patients responded that it was “not at all or a little” difficult to find private space for an encounter (84%, n = 395). Overall, there was a high level of satisfaction with telepsychiatry. Most patients (74%, n = 354) said they were “moderately or very much” satisfied using telepsychiatry to receive treatment, and most said it was “moderately or very much” helpful for accessing care during the pandemic (78%, n = 393).
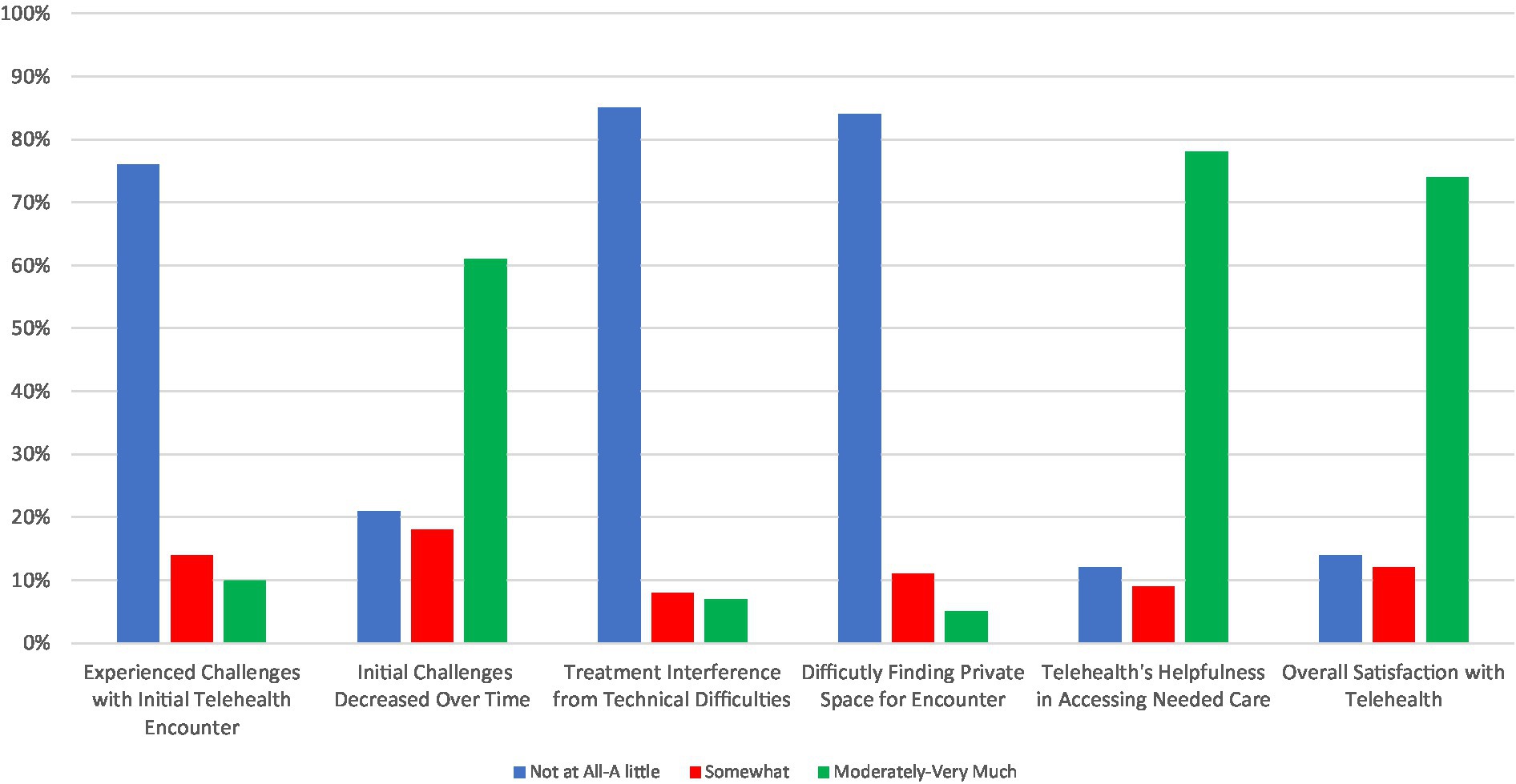
Figure 1. Patient experiences with telehealth rated on a Likert scale with response groups collapsed as “not at all or a little,” “somewhat,” and “moderately or very much.”
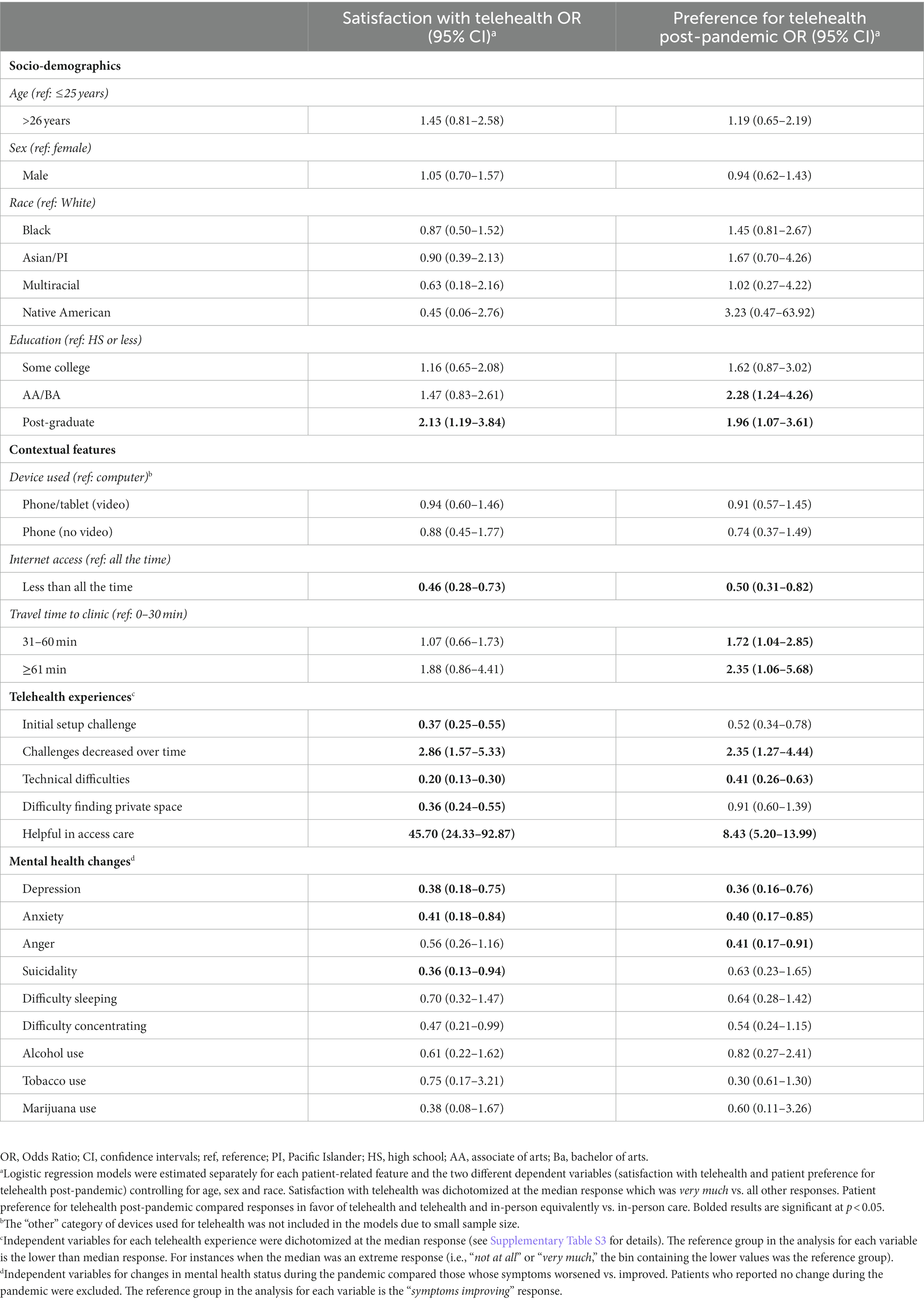
Several features were associated with patient satisfaction in telepsychiatry (Table 3). The only socio-demographic feature was education; patients who had a post-graduate education were the most likely to be satisfied with telepsychiatry (OR = 2.13, 95% CI: 1.19–3.84). Technology and privacy-related features were also associated. Satisfaction was lower among patients who had poorer internet access (OR = 0.46, 95% CI: 0.28–0.73), initial set-up challenges (OR = 0.37, 95% CI: 0.2–0.55), technical difficulties that interrupted treatment (OR = 0.20, 95% CI: 0.13–0.30), or difficulty in finding private space to meet (OR = 0.36, 95% CI: 0.24–0.55). Conversely, patients were more likely to be satisfied with telepsychiatry if their initial set up challenges decreased over time (OR = 2.86, 95% CI: 1.57–5.33). Clinically, patients who experienced worsening mental health symptoms and substance use problems over the course of the pandemic were also less likely to be satisfied with telepsychiatry. This was particularly true for patients who reported worsening depression (OR = 0.38, 95% CI: 0.18–0.75), anxiety (OR = 0.41, 95% CI: 0.18–0.84), and suicidality (OR = 0.36, 95% CI: 0.13–0.94).
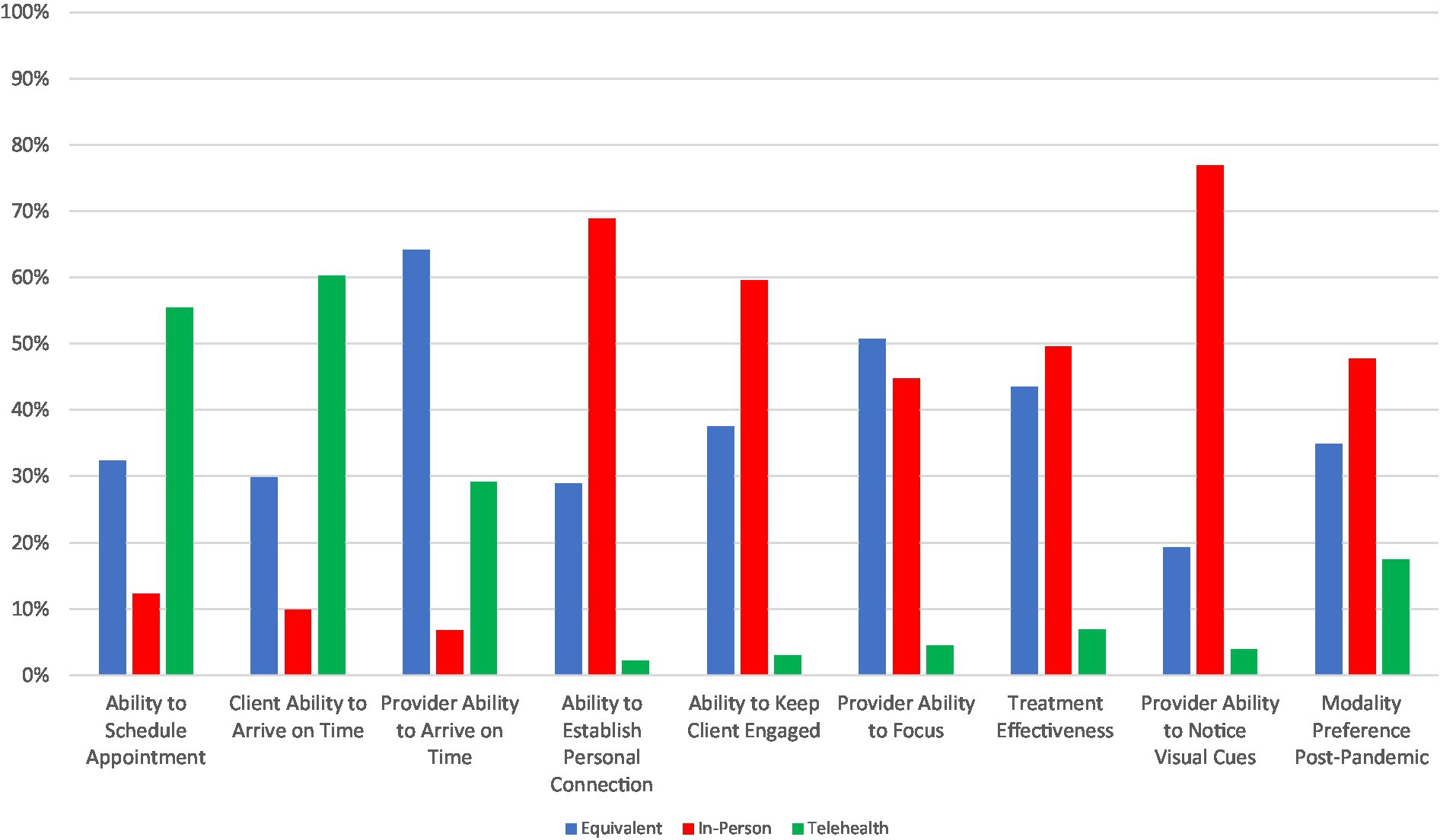
Patient preferences for telepsychiatry
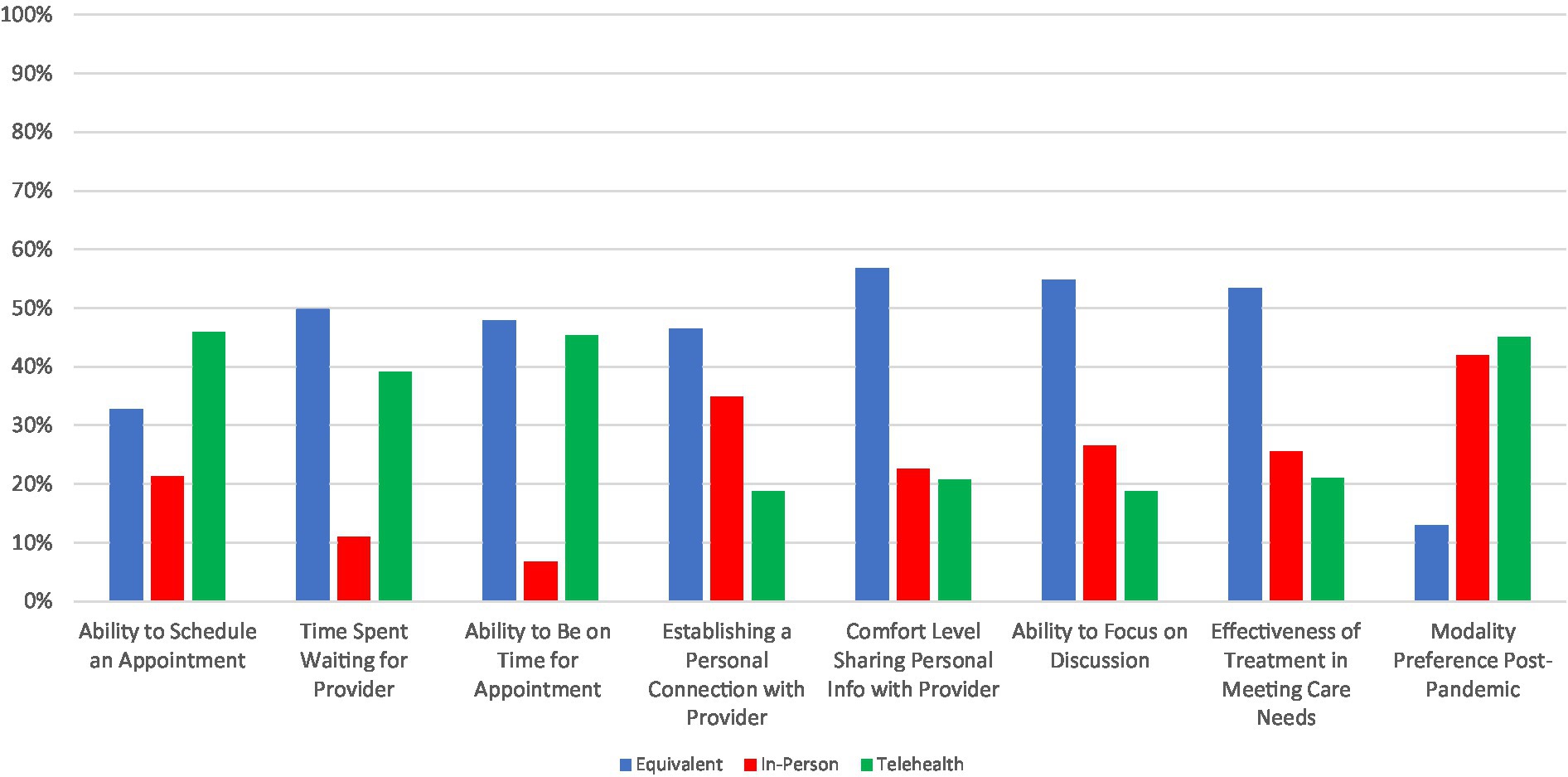
Summary results of patient responses for whether they prefer telepsychiatry, in-person treatment, or view both modalities as equivalent are shown in Figure 2, with more details provided in Supplementary Table S4. Patients more frequently rated telepsychiatry and in-person care as equivalent for many of the facets queried, including amount of time waiting for an appointment to start (50%), ability to be on time for an appointment (48%), establishing a personal connection with the provider (46%), comfort level sharing personal information with the provider (57%), ability to focus on the discussion (55%), and effectiveness of treatment to meet patient needs (53%). Preference for telepsychiatry was endorsed most frequently when considering the ability to schedule a time to meet with a provider (46%), while in-person care was not rated most often for any of the facets probed. There was a relatively even split in preference for telepsychiatry vs. in-person care when anticipating treatment post-pandemic: 45% reported preferring telepsychiatry compared with 42% for in-person care, while only a small minority of 13% rated them equivalently.
Many of the same features that were associated with patients’ overall satisfaction with telepsychiatry were also associated with their preference to continue with it post-pandemic (Table 3). Education was again relevant as patients with an Associates/Bachelor’s degree (OR = 2.28, 95% CI: 1.24–4.26) or post-graduate degree (OR = 1.96, 95% CI: 1.07–3.61) were more likely to prefer telepsychiatry in a post-pandemic setting, compared to those with a high school education or less. Patients with longer travel times to appointments were also more likely to prefer telepsychiatry post-pandemic. Here, there was a clear duration effect: compared to those who travel 0–30 min to the clinic, those who travel 31–60 min were more likely to prefer telepsychiatry (OR = 1.72, 95% CI: 1.04–2.85), and this preference was even stronger for those who travel over an hour (OR = 2.35, 95% CI: 1.06–5.68). Patients with poorer internet access were less likely to prefer telepsychiatry post-pandemic (OR = 0.50, 95% CI: 0.31–0.82). Experiences with telepsychiatry and changes in mental health during the pandemic were again also associated with preferences for seeking care post-pandemic. Patients who experienced technical difficulties with telepsychiatry were less likely to endorse a preference for telepsychiatry (OR = 0.41, 95% CI: 0.26–0.63), while patients who found that the technical challenges decreased over time (OR = 2.35, 95% CI: 1.27–4.44) and telepsychiatry was useful for accessing care (OR = 8.43, 95% CI: 5.20–13.99) were more likely to prefer telepsychiatry for future care. Clinically, patients who experienced worsening symptoms of depression (OR = 0.36, 95% CI: 0.16–0.76), anxiety (OR = 0.40, 95% CI: 0.17–0.85) and anger (OR = 0.41, 95% CI: 0.17–0.91) were less likely to prefer telepsychiatry post-pandemic. Finally, as with overall satisfaction, we again observed that age, sex and race were not associated with patient preferences for telepsychiatry vs. in-person care. However, in an exploratory analysis of patient preferences, we observed that Black patients found it easier to establish a personal connection via telepsychiatry (OR 2.3, 95% CI: 1.23–4.58) and easier to focus on the discussion (OR 2.45, 95% CI: 1.22–5.49) compared to White patients.
Provider experiences with telepsychiatry
Provider experiences with telepsychiatry are shown in Figure 3, with more details provided in Supplementary Table S5. Most said they had few (i.e., “not at all or a little”) challenges (64%, n = 85) with initial encounters and that the challenges decreased “moderately or very much” over time (76%, n = 77). Moreover, most providers reported they had few (i.e., “not at all or a little”) difficulties with finding private space for telepsychiatry encounters (87%, n = 116), experiencing eye strain or headache from increased screen time (63%, n = 82), maintaining appropriate boundaries with patients (59%, n = 77), providing tech support to patients (64%, n = 84), or resolving technical problems that disrupted care (57%, n = 86). A notable minority of providers reported they received insufficient (i.e., “not at all or a little”) training for the initial telepsychiatry encounter (39%, n = 51) and on-going technical support (33%, n = 44). However, overall satisfaction with telepsychiatry was high with 71% (n = 93) of providers reporting they were “moderately or very much” satisfied with telepsychiatry.
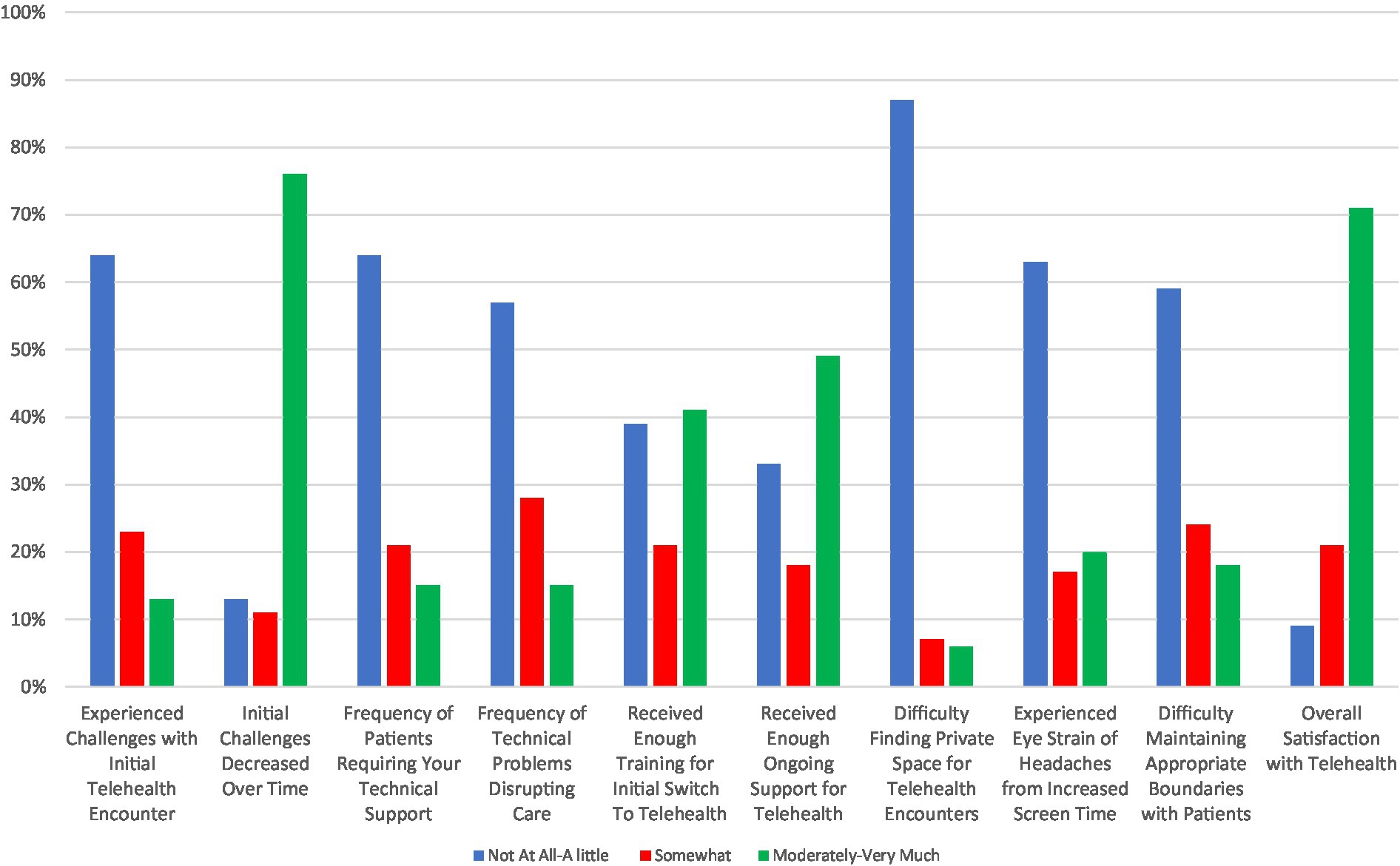
Figure 3. Provider experiences with telehealth rated on a Likert scale with response groups collapsed as “not at all or a little,” “somewhat,” and “moderately or very much.”
Providers were more likely to be satisfied with telepsychiatry if they felt they had received sufficient initial training (OR = 2.70, 95% CI: 1.14–6.56) and on-going support (OR = 2.51, 95% CI: 1.02–6.29) or if the initial challenges with telepsychiatry decreased over time (OR = 4.36, 95% CI: 1.66–12.20) (Table 4). On the other hand, providers who experienced on-going technical challenges with telepsychiatry encounters (OR = 0.12, 95% CI: 0.01–0.64) and who experienced eye strain as a result of these encounters (OR = 0.42, 95% CI: 0.15–1.11) were less likely to be satisfied. In addition, providers who joined appointments from the office instead of home were also less satisfied with telepsychiatry (OR = 0.21, 95% CI: 0.08–0.50). No socio-demographic factors were significantly associated with provider satisfaction with telepsychiatry. There was a trend towards more experienced clinicians being less likely to be satisfied with telepsychiatry, but the differences across provider training levels were not significant.
Provider preferences for telepsychiatry
Summary results of provider preferences for telepsychiatry vs. in-person treatment modalities are shown in Figure 4, with more details provided in Supplementary Table S6. Similar to patients, providers tended to prefer telepsychiatry for administrative-related purposes. A majority of providers preferred telepsychiatry for the ability to schedule appointments (55%) and for facilitating patient punctuality (60%). However, providers rated telepsychiatry and in-person care as equivalent (64%) when considering their own punctuality. By contrast, providers notably preferred in-person care for therapeutic alliance aspects, including the ability to notice visual cues (77%), keep the patient engaged (60%), and establish a personal connection with the patient (69%), as well as for overall treatment effectiveness (50%). Perhaps as a result, and in contrast with patients, a more distinct plurality of providers preferred in-person (48%) vs. telepsychiatry (17%) care post-pandemic, with 35% rating them equivalently.
Providers were less likely to prefer telepsychiatry as a post-pandemic modality if they experienced worse internet access (OR = 0.35, 95% CI: 0.13–0.86), technical difficulties (OR = 0.13, 95% CI: 0.02–0.46), or challenges maintaining appropriate boundaries with clients (OR = 0.28, 95% CI: 0.09–0.81) (Table 4). In addition, providers who did most of their telepsychiatry encounters from their work office also were less likely to prefer telepsychiatry for post-pandemic encounters (OR = 0.41, 95% CI: 0.17–0.96). Similar to what was observed for overall satisfaction, provider socio-demographics and level of training were not associated with their modality preference post-pandemic. However, in exploratory analyses to examine these relationships in more detail, we noted that Black providers were less likely than White providers to feel like they had been provided enough ongoing support with the transition to telepsychiatry (OR 0.27, 95% CI: 0.07–0.97). This did not translate into their being more or less likely to be satisfied with telepsychiatry or prefer it in the future.
Discussion
This paper examined patient and provider experiences and preferences in using telepsychiatry during the COVID-19 pandemic. Overall, patients and providers reported that telepsychiatry was acceptable and worked well, with over 70% of patients and providers reporting they were satisfied with telepsychiatry for delivering mental health care. However, there were greater divergences between patients and providers when asked whether they would prefer telepsychiatry or in-person care after the pandemic. Patients were more evenly divided with 45% preferring telepsychiatry compared to 42% for in-person care, and only 13% rating them equivalently. By contrast, providers were more likely to favor in-person care over telepsychiatry by 48% to 17%, with 35% rating them equivalently.
The high level of overall satisfaction that we observed is consistent with a large body of previous work carried out both before and during the pandemic (3, 9–13, 16, 18–20). For example, both Gentry et al. (6) and Steidtmann et al. (21) recently reported finding high levels of satisfaction with telepsychiatry among providers and clinical staff with patient contact during the pandemic. Both studies also reported high levels of patient satisfaction, which was collected indirectly through provider impression (6, 21).
It is less clear if the observed overall satisfaction with telepsychiatry translates into a preference among patients and providers to continue to use telepsychiatry after the pandemic. In a survey at the University of Michigan Outpatient Psychiatry Clinics, a little over half of the patients (54.1%) responded they would likely continue telepsychiatry even if in-person appointments were resumed (30). This echos our finding that 55% of patients rated telepsychiatry and in-person care equivalently or would prefer telepsychiatry if the pandemic abated. Another survey of clinicians at Mass General Hospital Outpatient Psychiatry Clinics reported a strong preference to continue telepsychiatry after the pandemic, although percentages were not given (20). Similarly, both Gentry et al. (6) and Steidtmann et al. (21) reported a strong preference on the part of the provider to continue telepsychiatry after the pandemic, at least for a significant portion of their caseload (6, 21). By contrast, Hunsinger et al. (31) found that only 17% of providers and 25% of patients preferred telepsychiatry. The lower rates reported by providers in this study were similar to what we observed in our survey.
Several factors were associated with overall satisfaction and preference for telepsychiatry among both patients and providers. Technical considerations such as access to stable internet were the most consistently reported factors affecting both satisfaction and future modality preference. Both patients and providers with less than fully stable internet access had more challenging telepsychiatry experiences overall and were significantly less likely to be satisfied with it and to want to continue using it in the future. This makes intuitive sense and is consistent with previous studies. For example, a pre-pandemic cross-sectional study of patients in the Kaiser system in California found a higher likelihood of telemedicine use in neighborhoods with high rates of residential internet access (32). In addition to stable internet access, other technical challenges experienced by patients and providers in using telemedicine had a similarly strong impact on their attitudes towards it. These findings highlight the importance of a robust internet infrastructure to sustain widespread use of telemedicine and technical support to overcome challenges when using audio/video technology.
Education was also strongly associated with overall satisfaction and preference for telepsychiatry among patients. Patients with higher levels of education were more likely to be satisfied with telepsychiatry and prefer using it post-pandemic. One possible explanation is that patients with higher education were also less likely to experience initial technical challenges with telemedicine and more likely to experience a decrease in those challenges over time (data not shown). As noted previously, technical issues significantly impact overall satisfaction and preferences. Education and overall clinical experience were less clearly associated with satisfaction and preferences for telemedicine among providers. There was a trend suggesting that providers with more experience, especially above the median level, were less satisfied with and less likely to prefer telemedicine, but these trends were not significant.
Other sociodemographic factors including age, sex and race were not associated with overall satisfaction or preference for telepsychiatry for both patients and providers. With regard to race, several previous studies have reported greater use and preference for telemedicine among Black patients. For example, a large pre-COVID-19 study from Kaiser on telemedicine use in primary care found that Black patients were significantly more likely than White patients to choose telemedicine over in-person care (32). In addition, the Pew Research Center’s American Trends Panel study found that of all racial/ethnic groups, Black patients were most likely to use telemedicine during the pandemic (33). However, not all studies have found significant associations between race and telemedicine preferences and experiences (30). Although we did not find significant associations either, we did observe several revealing differences in the telepsychiatry experiences of both patients and providers of color that warrant consideration.
We found that Black patients were over two times more likely to find it easier to establish a personal connection and focus on treatment sessions via telepsychiatry compared to White patients. It is unclear from our findings why this is the case, but it merits further investigation to better understand why certain patient populations differ in their experience with telepsychiatry in ways that may affect their care. We also noted that Black providers were less likely than White providers to feel like they had received enough support when switching to telepsychiatry. Although this did not translate into differences in overall satisfaction or preference for telepsychiatry, it demands greater attention in the future. The transition to telepsychiatry was swift with minimal opportunities for formalized training. Such training will likely be important to increase acceptance and satisfaction with telepsychiatry going forward. Previous studies have shown that appropriate training in different areas of telemedicine (such as “digital psychiatry”) strongly influence providers’ perceptions and attitudes regarding the usefulness and effectiveness of remote care (34–36). Indeed, we observed that all providers who felt they received sufficient initial training and on-going support were more than two times as likely to be satisfied with telepsychiatry. The structural factors leading to Black providers feeling less supported at work will need to be addressed to minimize potential disparities in using telepsychiatry.
Finally, we observed that the mental health status of patients strongly influences their attitudes towards telepsychiatry. While there has been some discussion about which mental illnesses are better suited for care via telemedicine, there has been more limited investigation of how the severity or progression of these illnesses is associated with patient attitudes towards telemedicine (37). One small survey from Louisiana State University Health Sciences Center did not find an association between self-report of severity of anxiety/depression symptoms and visit type preference (31). We found that worsening mental health and substance use problems, particularly depression and anxiety, were significantly associated with lower satisfaction and preference for telepsychiatry. Patients with worsening mental health and substance use problems may have been frustrated at the perceived lack of progress in their treatment, and thus less happy with treatment overall. As providers move towards a hybrid model, patients who are not improving may benefit from the option to return to in-person care. Thus, in the future, it may be important for providers to carefully monitor their patient’s clinical status when making decisions about the optimal modality of treatment.
Limitations
Our study had several limitations. The response rates were 20% for patients and 62% for providers, which leaves open the possibility of response bias. However, several steps were taken to minimize this risk. Email reminders to non-responders were distributed twice per week on different days and times, in an attempt to collect responses from patients on different schedules. Furthermore, a telephone follow-up (see Methods) of 300 randomly selected non-responders was employed to minimize bias due to convenience sampling as well as to recruit patients who do not have uniform access to email. However, future work that evaluates the efficacy of telepsychiatry should work to employ a more sustained multi-modal collection effort (e.g., physical mailers and a broader telephone follow-up) to both improve the response rate and to minimize concerns of exacerbating the digital divide (4, 5). In addition, despite having a more diverse sample compared to similar studies, our respondents were still relatively homogeneous with the majority identifying as White and female. Follow-up studies should work to ensure that their samples better reflect the socio-demographic makeup of the participating communities or clinics through more targeted recruitment efforts. Lastly, we did not collect data on the encounter level or at the level of individual patient-provider relationships. As noted by Sabin and Skimming (2) the acceptability of telepsychiatry can change across therapeutic relationships, specific diagnoses (including severity), or even the type of service (e.g., support for caregivers) (2, 5). Further research should seek to investigate how satisfaction with telepsychiatry can change across different patient-provider dyads as well as over time.
Implications and conclusion
Due to the COVID-19 pandemic, mental health clinics were forced to quickly adopt telemedicine to continue delivering care to patients with mental health and substance use problems. The rapid nature of the transition to telepsychiatry necessitates a re-evaluation of how patients and providers perceive utilization of remote care, in order to reveal the benefits and limitations of using telemedicine in psychiatry. Now that the emergency pandemic measures have receded, it is an open question to what extent telepsychiatry will continue to be used to deliver care (15). We found that both patients and providers were generally satisfied with telepsychiatry, especially as a means to continue accessing/providing care during the pandemic when in-person access to care was not feasible. However, there were greater differences in preferences for continuing to use telepsychiatry after the pandemic. The findings reported here can help to inform what may promote positive patient and provider experiences with telepsychiatry, as well as what areas or aspects may require additional resources in order to ensure a more just and equitable practice of telepsychiatry.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
MM, IC, MW, AB, LM, WN, BS, JS, PZ, and AR contributed to the study conception and design and commented on previous versions of the manuscript. MM, IC, AB, JS, PZ, and AR were responsible for data collection and subsequent analysis. The first draft of this manuscript was written by MM, IC, PZ, and AR. All authors contributed to the article and approved the submitted version.
Acknowledgments
The authors would like to thank Dr. Karen Swartz MD and Dr. Fernando Goes, MD, for their contributions to this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1237249/full#supplementary-material
Abbreviations
CPP, Community Psychiatry Program; ROCC, Resident Outpatient Continuity Clinic; CAHPS, Consumer Assessment of Healthcare Providers and Systems; ECHO, Experience of Care and Health Outcomes Survey; PGY, Post-Graduate Year (Residency Status); OR, Odds Ratio; CI, Confidence Interval.
References
1. Bokolo, AJ . Exploring the adoption of telemedicine and virtual software for care of outpatients during and after COVID-19 pandemic. Ir J Med Sci. (2021) 190:1–10. doi: 10.1007/s11845-020-02299-z
2. Sabin, JE , and Skimming, K . A framework of ethics for telepsychiatry practice. Int Rev Psychiatry. (2015) 27:490–5. doi: 10.3109/09540261.2015.1094034
3. Barnett, ML , Ray, KN , Souza, J , and Mehrotra, A . Trends in telemedicine use in a large commercially insured population, 2005–2017. JAMA. (2018) 320:2147. doi: 10.1001/jama.2018.12354
5. Marinelli, S , Basile, G , and Zaami, S . Telemedicine, telepsychiatry and COVID-19 pandemic: future prospects for global health. Healthcare. (2022) 10:2085. doi: 10.3390/healthcare10102085
6. Gentry, MT , Puspitasari, AJ , McKean, AJ , Williams, MD , Breitinger, S , Geske, JR, et al. Clinician satisfaction with rapid adoption and implementation of telehealth services during the COVID-19 pandemic. Telemed J E Health. (2021) 27:1385–92. doi: 10.1089/tmj.2020.0575
7. Ramalho, R , Adiukwu, F , Gashi Bytyçi, D , El Hayek, S , Gonzalez-Diaz, JM , Larnaout, A, et al. Telepsychiatry during the COVID-19 pandemic: development of a protocol for telemental health care. Front Psychiatry. (2020) 11:552450. doi: 10.3389/fpsyt.2020.552450
8. Anthony, B . Implications of telehealth and digital care solutions during COVID-19 pandemic: a qualitative literature review. Inform Health Soc Care. (2021) 46:68–83. doi: 10.1080/17538157.2020.1839467
9. Donelan, K , Barreto, EA , Sossong, S , Michael, C , Estrada, JJ , Cohen, AB, et al. Patient and clinician experiences with telehealth for patient follow-up care. Am J Manag Care. (2019) 25:40–4.
10. Hubley, S , Lynch, SB , Schneck, C , Thomas, M , and Shore, J . Review of key telepsychiatry outcomes. World J Psychiatr. (2016) 6:269. doi: 10.5498/wjp.v6.i2.269
11. Cowan, KE , McKean, AJ , Gentry, MT , and Hilty, DM . Barriers to use of telepsychiatry: clinicians as gatekeepers. Mayo Clin Proc. (2019) 94:2510–23. doi: 10.1016/j.mayocp.2019.04.018
12. Barnett, ML , and Huskamp, HA . Telemedicine for mental health in the United States: making progress, still a long way to go. Psychiatr Serv. (2020) 71:197–8. doi: 10.1176/appi.ps.201900555
13. Kruse, CS , Krowski, N , Rodriguez, B , Tran, L , Vela, J , and Brooks, M . Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. (2017) 7:e016242. doi: 10.1136/bmjopen-2017-016242
14. Lo, J , Rae, M , Amin, K , Cox, C , Panchal, N , and Miller, B . Telehealth has played an outsized role meeting mental health needs during the COVID-19 pandemic. (2022). Available at: https://www.kff.org/coronavirus-covid-19/issue-brief/telehealth-has-played-an-outsized-role-meeting-mental-health-needs-during-the-covid-19-pandemic/. (Accessed January 23, 2023).
15. Ramalho, R , Adiukwu, F , Gashi Bytyçi, D , El Hayek, S , Gonzalez-Diaz, JM , Larnaout, A, et al. Telepsychiatry and healthcare access inequities during the COVID-19 pandemic. Asian J Psychiatr. (2020) 53:102234. doi: 10.1016/j.ajp.2020.102234
16. Guinart, D , Marcy, P , Hauser, M , Dwyer, M , and Kane, JM . Patient attitudes toward Telepsychiatry during the COVID-19 pandemic: a Nationwide, multisite survey. JMIR Ment Health. (2020) 7:e24761. doi: 10.2196/24761
17. Benudis, A , Re’em, Y , Kanellopoulos, D , Moreno, A , and Zonana, J . Patient and provider experiences of telemental health during the COVID-19 pandemic in a New York City academic medical center. Psychiatry Res. (2022) 311:114496. doi: 10.1016/j.psychres.2022.114496
18. Li, H , Glecia, A , Kent-Wilkinson, A , Leidl, D , Kleib, M , and Risling, T . Transition of mental health service delivery to telepsychiatry in response to COVID-19: a literature review. Psychiatry Q. (2022) 93:181–97. doi: 10.1007/s11126-021-09926-7
19. Guinart, D , Marcy, P , Hauser, M , Dwyer, M , and Kane, JM . Mental health care providers’ attitudes toward telepsychiatry: a systemwide, multisite survey during the COVID-19 pandemic. Psychiatr Serv. (2021) 72:704–7. doi: 10.1176/appi.ps.202000441
20. Chen, JA , Chung, WJ , Young, SK , Tuttle, MC , Collins, MB , Darghouth, SL, et al. COVID-19 and telepsychiatry: early outpatient experiences and implications for the future. Gen Hosp Psychiatry. (2020) 66:89–95. doi: 10.1016/j.genhosppsych.2020.07.002
21. Steidtmann, D , McBride, S , and Mishkind, MC . Experiences of mental health clinicians and staff in rapidly converting to full-time telemental health and work from home during the COVID-19 pandemic. Telemed J E Health. (2021) 27:785–91. doi: 10.1089/tmj.2020.0305
22. Nitiema, P . Telehealth before and during the COVID-19 pandemic: analysis of health care workers’ opinions. J Med Internet Res. (2022) 24:e29519. doi: 10.2196/29519
23. Morgan, DG , Kosteniuk, J , Stewart, N , O’Connell, ME , Karunanayake, C , and Beever, R . The telehealth satisfaction scale: reliability, validity, and satisfaction with telehealth in a rural memory clinic population. Telemed J E Health. (2014) 20:997–1003. doi: 10.1089/tmj.2014.0002
24. Parmanto, B , Lewis, AN Jr, Graham, KM , and Bertolet, MH . Development of the telehealth usability questionnaire (TUQ). Int J Telerehabil. (2016) 8:3–10. doi: 10.5195/ijt.2016.6196
25. Brooke, J . Sus: a “quick and dirty’usability. Usability evaluation in industry. (1996) 189, 189–194.
26. Zhou, L , Bao, J , Setiawan, IMA , Saptono, A , and Parmanto, B . The mHealth app usability questionnaire (MAUQ): development and validation study. JMIR Mhealth Uhealth. (2019) 7:e11500. doi: 10.2196/11500
27. Daniels, AS , Shaul, JA , Greenberg, P , and Cleary, PD . “The experience of care and health outcomes survey (ECHO): a consumer survey to collect ratings of behavioral health care treatment, outcomes and plans,” in The Use of Psychological Testing for Treatment Planning and Outcomes Assessment: Instruments for Adults. 3rd ed. Lawrence Erlbaum Associates Publishers (2004) 839–66.
28. Agency for Healthcare Research and Quality . CAHPS mental health care surveys. (2022). Available at: https://www.ahrq.gov/cahps/surveys-guidance/echo/index.html. (Accessed June 3, 2020)
29. Maternal Fetal Medicine . University of Washington telemedicine patient satisfaction survey. University of Washington Medical Center (2014).
30. Severe, J , Tang, R , Horbatch, F , Onishchenko, R , Naini, V , and Blazek, MC . Factors influencing patients’ initial decisions regarding telepsychiatry participation during the COVID-19 pandemic: telephone-based survey. JMIR Form Res. (2020) 4:e25469. doi: 10.2196/25469
31. Hunsinger, N , Hammarlund, R , and Crapanzano, K . Mental health appointments in the era of COVID-19: experiences of patients and providers. Ochsner J. (2021) 21:335–40. doi: 10.31486/toj.21.0039
32. Reed, ME , Huang, J , Graetz, I , Lee, C , Muelly, E , Kennedy, C, et al. Patient characteristics associated with choosing a telemedicine visit vs office visit with the same primary care clinicians. JAMA Netw Open. (2020) 3:e205873. doi: 10.1001/jamanetworkopen.2020.5873
33. Campos-Castillo, C , and Anthony, D . Racial and ethnic differences in self-reported telehealth use during the COVID-19 pandemic: a secondary analysis of a US survey of internet users from late march. J Am Med Inform Assoc. (2021) 28:119–25. doi: 10.1093/jamia/ocaa221
34. Orsolini, L , Pompili, S , Salvi, V , and Volpe, U . A systematic review on TeleMental health in youth mental health: focus on anxiety, depression and obsessive-compulsive disorder. Medicina. (2021) 57:793. doi: 10.3390/medicina57080793
35. Orsolini, L , Appignanesi, C , Pompili, S , and Volpe, U . The role of digital tools in providing youth mental health: results from an international multi-center study. Int Rev Psychiatry. (2022) 34:809–26. doi: 10.1080/09540261.2022.2118521
36. Orsolini, L , Bellagamba, S , Marchetti, V , Menculini, G , Tempia Valenta, S , Salvi, V, et al. A preliminary Italian cross-sectional study on the level of digital psychiatry training, knowledge, beliefs and experiences among medical students, psychiatry trainees and professionals. Healthcare. (2022) 10:390. doi: 10.3390/healthcare10020390
Keywords: telepsychiatry, telemedicine, telehealth, quality improvement, survey
Citation: Morreale M, Cohen I, Van Wert M, Beccera A, Miller L, Narrow W, Schweizer B, Straub J, Zandi P and Ruble A (2023) Determinants of experience & satisfaction in telehealth psychiatry during the COVID-19 pandemic for patients & providers. Front. Psychiatry. 14:1237249. doi: 10.3389/fpsyt.2023.1237249
Edited by:
Gaia Sampogna, University of Campania “L. Vanvitelli”, ItalyReviewed by:
Giulio Longo, Marche Polytechnic University, ItalyBokolo Anthony, Institute for Energy Technology, Norway
Simona Zaami, Sapienza University of Rome, Italy
Copyright © 2023 Morreale, Cohen, Van Wert, Beccera, Miller, Narrow, Schweizer, Straub, Zandi and Ruble. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anne Ruble, YXJ1YmxlQGpobWkuZWR1
†These authors have contributed equally to this work and share first authorship
 Michael Morreale
Michael Morreale Ilana Cohen
Ilana Cohen Michael Van Wert
Michael Van Wert Alexis Beccera
Alexis Beccera Leslie Miller
Leslie Miller William Narrow
William Narrow Barbara Schweizer1
Barbara Schweizer1 Peter Zandi
Peter Zandi