- 1Department of Psychiatry, School of Clinical Medicine, LKS Faculty of Medicine, The University of Hong Kong, Pokfulam, Hong Kong SAR, China
- 2Department of Psychiatry, Queen Mary Hospital, Pokfulam, Hong Kong SAR, China
- 3School of Public Health, LKS Faculty of Medicine, The University of Hong Kong, Pokfulam, Hong Kong SAR, China
- 4State Key Laboratory of Brain and Cognitive Sciences, The University of Hong Kong, Pokfulam, Hong Kong SAR, China
Introduction: The extent of cognitive impairment and its association with psychological distress among people with pre-existing mental illness during COVID-19 is understudied. This study aimed to investigate prevalence and correlates of subjective cognitive impairment (SCI) in Chinese psychiatric patients during fifth-wave of COVID-19 in Hong Kong (HK).
Methods: Four-hundred-eight psychiatric outpatients aged 18–64 years were assessed with questionnaires between 28 March and 8 April 2022, encompassing illness profile, psychopathological symptoms, coping-styles, resilience, and COVID-19 related factors. Participants were categorized into moderate-to-severe and intact/mild cognitive impairment (CI+ vs. CI-) groups based on severity of self-reported cognitive complaints. Univariate and multivariate regression analyses were conducted to determine variables associated with CI+ status.
Results: One-hundred-ninety-nine participants (48.8%) experienced CI+. A multivariate model on psychopathological symptoms found that depressive and post-traumatic-stress-disorder (PTSD)-like symptoms were related to CI+, while a multivariate model on coping, resilience and COVID-19 related factors revealed that avoidant coping, low resilience and more stressors were associated with CI+. Final combined model demonstrated the best model performance and showed that more severe depressive and PTSD-like symptoms, and adoption of avoidant coping were significantly associated with CI+.
Conclusion: Almost half of the sample of psychiatric patients reported cognitive complaints during fifth-wave of COVID-19 in HK. Greater depressive and PTSD-like symptom severity, and maladaptive (avoidant) coping were found as correlates of SCI. COVID-19 related factors were not independently associated with SCI in psychiatric patients. Early detection with targeted psychological interventions may therefore reduce psychological distress, and hence self-perceived cognitive difficulties in this vulnerable population.
1. Introduction
Coronavirus disease (COVID-19) is an infectious disease caused by a new strain of severe acute respiratory syndrome coronavirus, SARS-CoV-2 (1). It first emerged in December 2019 in China and was declared as a global pandemic in March 2020 (2). COVID-19 brings about both physical and mental health complications. Adverse mental health outcomes such as increased stress, higher levels of worry and fatigue, pandemic-related fear and anxiety, depressive, anxiety and post-traumatic stress symptoms have been consistently reported in COVID-19 studies on the general population across different countries (3–7). The indirect effects of COVID-19 such as economic ramification (8) and social isolation (9, 10) due to public health policies further compromise individuals’ psychological well-being. In particular, individuals with pre-existing mental illness constitute one of the vulnerable populations in the pandemic. Literature showed that psychiatric patients had higher rates of COVID-19 infection (11, 12) and mortality (13, 14), and experienced greater psychological distress with more severe depressive and anxiety symptoms, and sleep disturbances (15, 16).
Owing to its high contagious nature, many countries have implemented a myriad of preventive measures in containing COVID-19 infection. In Hong Kong (HK), local infections waxed and waned in an early pandemic stage until an emergence of the Omicron variant in the community in late December 2021. Subsequently, a new wave of outbreak began (Supplementary Figure S1) and the 7-day rolling average of COVID-related deaths reached 3.73 per 1000 people at the peak, the highest worldwide, since Omicron variant was detected (17, 18). It was even estimated that approximately half of the HK population (i.e., 3.6 million) have contracted COVID-19 during the fifth wave by mid-March (19). Epidemiological control measures were further tightened, together with the consideration of implementing compulsory mass COVID-19 testing (and the associated lockdown measures) to the entire population by the government (20). Previous studies reported increased prevalence of depression and anxiety in the general population (21–23), and worsening of mood symptoms in psychiatric patients (24) during the early stage of COVID-19 in HK.
Of note, recent data have found that COVID-19 outbreak and its related psychological distress may be associated with poorer cognitive functioning in the general population (25, 26) and psychiatric patients (27). In particular, psychiatric patients may have already experienced certain extent of cognitive deficits due to their pre-existing mental illness, and may be therefore more susceptible to further cognitive deterioration in the midst of pandemic. Despite the significance of cognitive impairment on psychosocial functioning, there is a paucity of research specifically investigating cognitive complaints in psychiatric patients and its relationship with COVID-19 related factors. To this end, the current study aimed to: firstly, examine the prevalence of subjective cognitive impairment (SCI) in a representative cohort of Chinese patients with common and severe mental disorders during the fifth wave of COVID-19 pandemic in HK; and secondly, to identify correlates of SCI among psychiatric patients by comprehensively evaluating a wide array of factors encompassing socio-demographics, psychopathological symptoms, level of resilience, stress coping strategies and COVID-19 related variables.
2. Materials and methods
2.1. Participants and study setting
Participants aged 18–64 years were recruited from adult public psychiatric outpatient clinics between March 28 and April 8, 2022 in Hong Kong West Cluster, a catchment area with a population of approximately 550, 000. Participants who have learning disabilities, head injuries and neurological disease, and who could not understand written Chinese language were excluded. Participants’ principal ICD10 psychiatric diagnosis was ascertained by reviewing electronic medical records of psychiatric services (ICD10 classification is used for psychiatric diagnostic assignment in HK public healthcare system). Participants were further categorized into patients with common mental disorders (CMD, including depression and anxiety disorders) and patients with severe mental disorders (SMD, including schizophrenia-spectrum disorders, bipolar disorder and other non-affective psychoses). The study was approved by the Institutional Review Board of the University of Hong Kong / Hospital Authority Hong Kong West Cluster and all participants provided written informed consent.
2.2. Study assessment
The self-rated study assessment comprised four sections including socio-demographics and illness profile, psychopathological symptom severity, coping strategies and resilience, and COVID-19 related factors. It took approximately 15–20 min to complete the questionnaire. Illness profile included psychiatric diagnosis, comorbid substance/alcohol use disorder, history of psychiatric admission and length of receiving psychiatric service. Concerning psychopathological symptoms, depressive and anxiety symptom severity were assessed by Patient Health Questionnaire-9 (PHQ-9) (28, 29) and Generalised Anxiety Disorder-7 scale (GAD-7) (30, 31), respectively, with both scales using a 4-point Likert scale ranging from 0 (never) to 3 (nearly every day). A modified version of Impact of Event Scale–Revised (IES-R) (32, 33) specific to COVID-19 was administered to measure post-traumatic stress disorder (PTSD)-like symptoms in a 5-point Likert scale (0 [never] to 4 [always]). Sleep quality and disturbance was assessed using Insomnia Severity Index (ISI) (34, 35). Positive symptom subdomain items (4 items) of 15-item Community Assessment of Psychic Experiences Scale–Chinese version (CAPE-C15) (36) was employed to assess positive psychotic symptoms. Participants rated their frequency of positive symptoms on a 4-point Likert scale (1 [never] to 4 [nearly always]). We did not apply negative symptom subdomain items of CAPE-C15 to measure negative symptoms as previous studies suggested considerable overlap with depressive symptoms (27, 37). For all of the symptom scales, higher scores indicated greater symptom severity. Self-harm behavior during the fifth wave of COVID-19 was assessed. Subjective cognitive impairment (SCI) of participants was measured by a 5-item self-report questionnaire, adapted from Cognitive Complaints in Bipolar Disorder Rating Assessment (COBRA) (38, 39), which has been applied in a recent study examining SCI in psychiatric patients of CMD and SMD during COVID-19 lockdown (27). The adapted SCI questionnaire comprised 5 items that reflected cognitive complaints manifested in everyday scenario, including cognitive domains of attention, processing speed, memory, learning and executive function. Each item was rated on the frequency of self-reported cognitive complaints on a 4-point Likert scale, ranging from 0 (never) to 3 (nearly every day) (27).
Participants’ coping strategies were assessed by an adapted Coping Orientation to Problems Experienced Inventory–Brief (Brief-COPE) (40, 41), which used a 4-point Likert scale ranging from 0 (never) to 3 (always). The 14 items of the adapted Brief-COPE were grouped into 3 copying styles based on previous factor-analytic study (42), namely avoidant, emotion-focused and problem-focused coping styles for subsequent analysis. A higher item sum score indicated higher level of engagement in that particular coping style. The Brief Resilience Scale (BRS) (43, 44) was used to assess resilience levels on a 5-point Likert scale (1 [strongly disagree] to 5 [strongly agree]), with higher scores indicating greater resilience. Evaluation of COVID-19 related factors comprised items assessing history of contracting COVID-19 infection, receipt of vaccination, fear of contagion, time spent on reading COVID-19 related information, COVID-19 related stressors experienced, specific infection control measures (e.g., under quarantine, mandatory COVID-19 testing) experienced and associated distress. Details of assessment for COVID-19 related factors are summarized in Supplementary Table S1.
2.3. Statistical analysis
The study sample was subdivided into psychiatric patients with moderate-to-severe cognitive impairment (CI+ group) and intact or mild cognitive impairment (CI- group), based on the SCI questionnaire ratings. Following the method of a previous study examining SCI in psychiatric patients during COVID-19 (27), participants attaining a score ≥ 2 in one or more of the 5 items on the adapted SCI questionnaire were categorized as fulfilling CI+ status. A series of univariate binary logistic regression analyses were conducted to examine the association of CI+ status with socio-demographics, illness profile variables, psychopathological symptoms, coping styles, resilience, and COVID-19 related factors. Then, three sets of multivariate binary logistic regression analyses using forward Wald stepwise method were performed. The first multivariate model included psychopathological variables that were significantly related to CI+ status in the preceding univariate analyses to determine which symptom domains were independently associated with CI+ status. The second model included variables of coping style and resilience as well as COVID-19 related factors that were significantly related to CI+ status in prior univariate analyses. The final combined model incorporated variables that were statistically significant in the first and second models, as well as socio-demographic and illness-profile variables that were significantly related to CI+ status in univariate analyses. This final model would determine an array of correlates that were independently associated with CI+ status. Model performance was assessed using receiver-operating characteristic (ROC) curve, area under ROC curve (AUC) and McFadden pseudo-R2. An AUC value of 0.7 to 0.8 is regarded as acceptable, and a value of 0.8 to 0.9 is considered excellent (45). All missing data were imputed for five times using Multiple Imputation by Chained Equations (MICE) (46). All results reported were pooled according to Rubin’s rules (47). All analyses were conducted using R4.2.1, with significance level set as p < 0.05.
3. Results
3.1. Characteristics of the sample
A total of 415 participants were recruited. Seven participants were excluded due to missing data in the SCI questionnaire, resulting in 408 participants as the study sample for analysis. Of the 408 participants, 242 (59.3%) and 166 (40.7%) were CMD and SMD patients, respectively. The median duration of receiving public psychiatric care was 7.4 years. Based on the self-reported SCI assessment, 199 (48.8%) patients were categorized as CI+, while 209 patients (51.2%) were categorized as CI-. Characteristics of CI+ and CI- groups are summarized in Table 1.
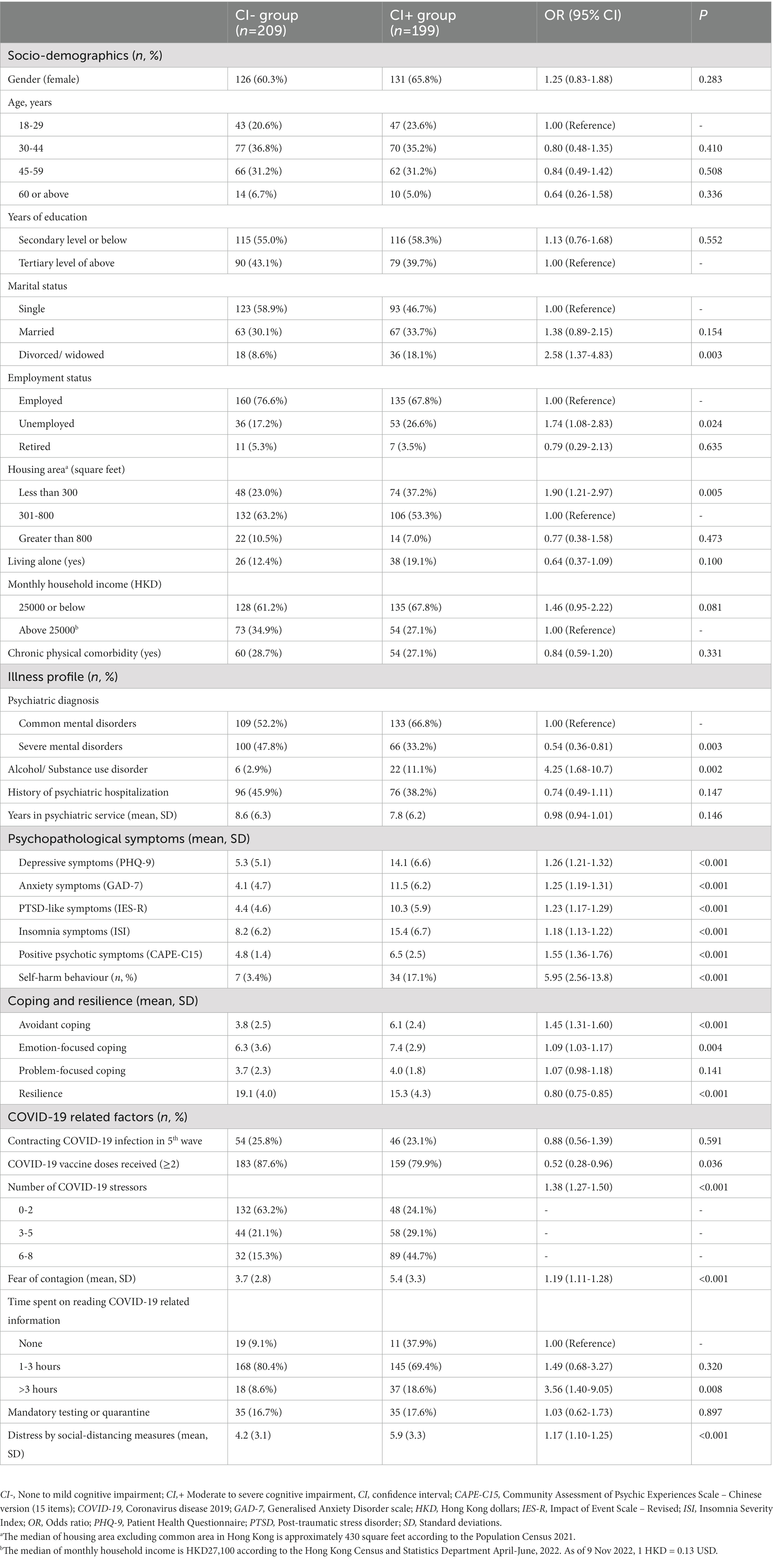
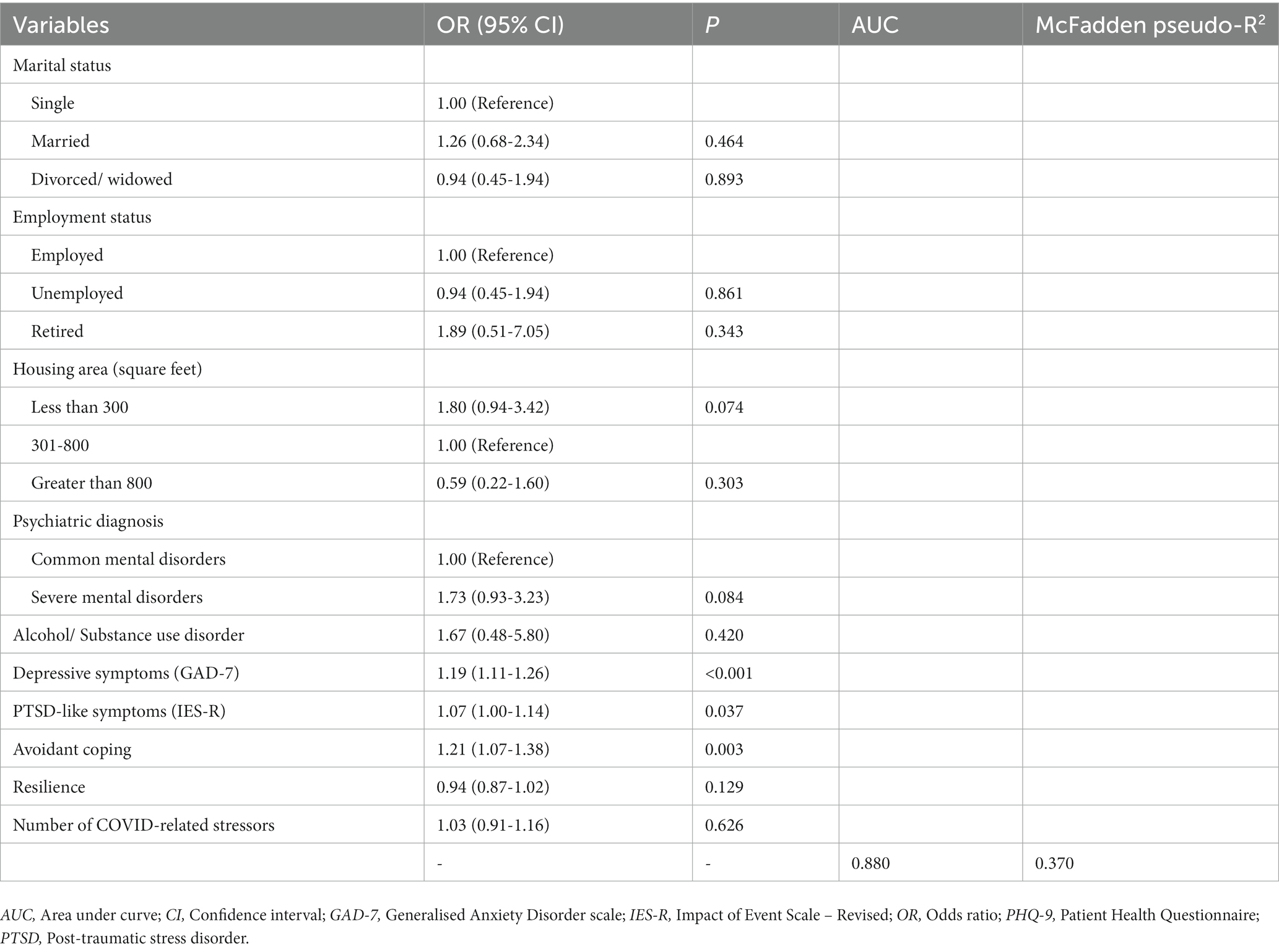
Table 1. Descriptive and univariate logistic regression results of candidate variables for cognitive impairment status.
3.2. Univariate regression analyses for subjective cognitive impairment
Results of univariate regression analyses examining the associations of CI+ status with variables encompassing socio-demographics, illness profiles, psychopathological symptoms, coping styles and resilience, and COVID-19 related factors are shown in Table 1. Marital status (divorced / widowed), unemployment, median housing area < 300 sq. ft., CMD diagnosis, and substance/alcohol use disorder were associated with increased likelihood of CI+. Patients in CI+ group had higher scores in PHQ-9, GAD-7, IES-R, ISI and CAPE-15C positive symptom subdomain, and were more likely to commit self-harm behavior during the fifth wave of COVID-19 than those in CI- group. Furthermore, CI+ group was more likely to adopt avoidant and emotion-focused coping styles and had lower BRS score relative to CI- group. Regarding COVID-19 related factors, CI+ group experienced greater number of stressors and greater fear of contracting COVID-19, was more likely to have received <2 COVID-19 vaccine doses and spent >3 h reading COVID-19 information, and was more distressed by social-distancing measures than CI- group.
3.3. Multivariate and final combined regression models for subjective cognitive impairment
As shown in Table 2, multivariate regression model 1 on psychopathological symptoms revealed that more severe depressive and PTSD-like symptoms were significantly associated with CI+. Model 2 showed that avoidant coping style, lower resilience and greater number of COVID-19 related stressors were significantly associated with CI+ status (Table 2). Final combined model found that depressive symptoms, PTSD-like symptoms and avoidant coping style were independently associated with CI+ (Table 3). The final model demonstrated superior model performance to models 1 and 2 in determining CI+ status as evidenced by having the highest AUC value and explained variance (Figure 1; Tables 2, 3).
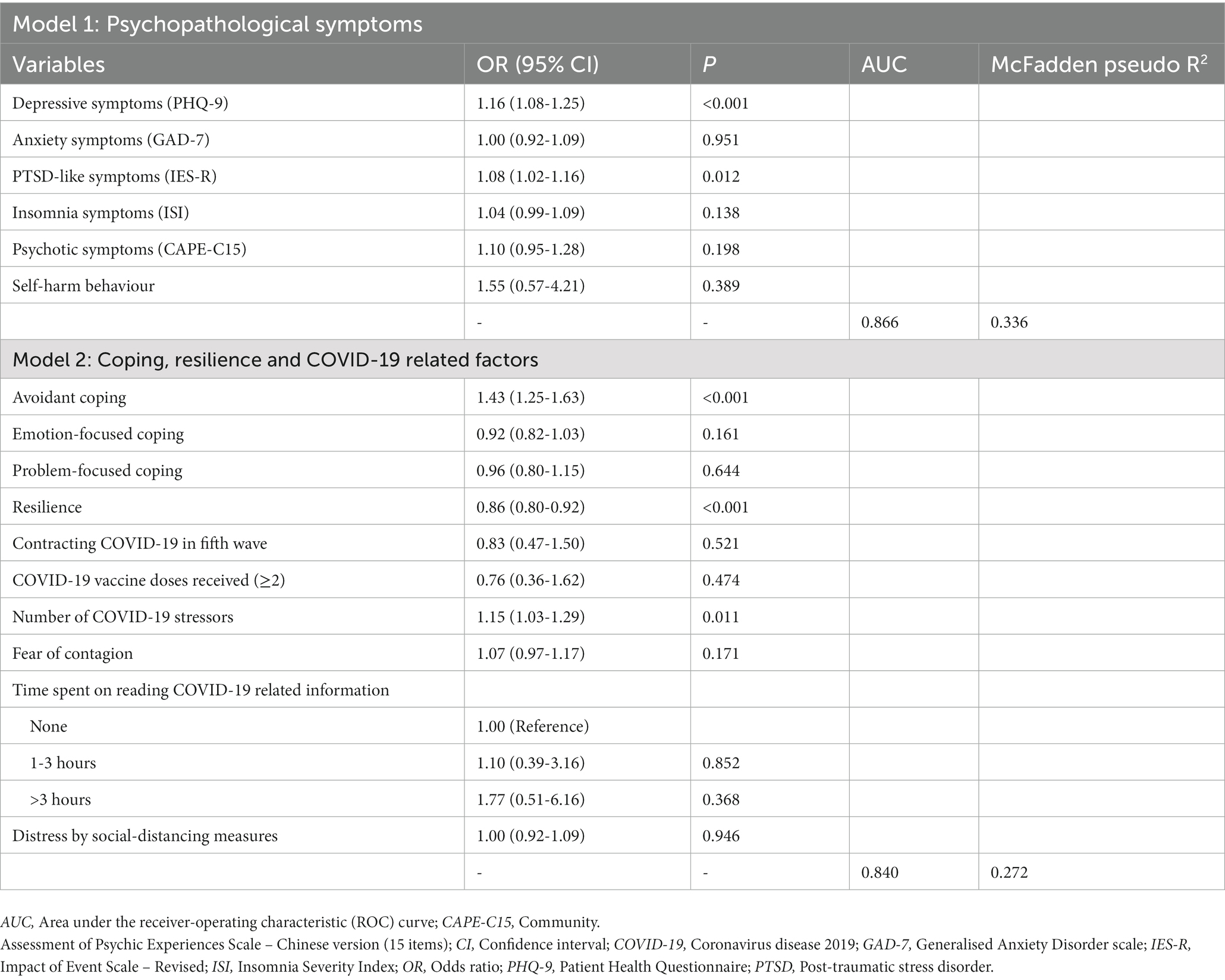
Table 2. Multivariate logistic regression analyses on psychopathological symptoms and coping, resilience & COVID-19 related factors for cognitive impairment status.
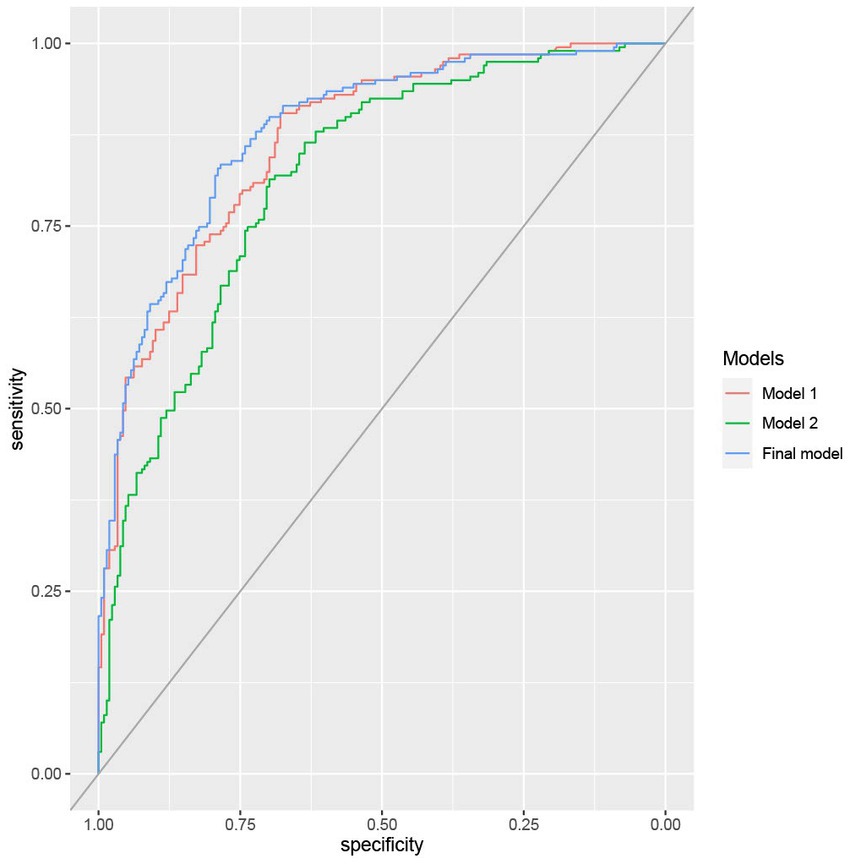
Figure 1. Receiver Operating Characteristic (ROC) curves of the multivariate logistic regression models for prediction of cognitive impairment status. Model 1: Prediction of psychopathological symptoms on cognitive impairment. Model 2: Prediction of resilience, coping and COVID-19 related factors on cognitive impairment. Final model: Combined factors of models 1 and 2 for predicting cognitive impairment.
4. Discussion
The current study aimed to examine the prevalence and correlates of SCI in Chinese psychiatric patients during the fifth wave of COVID-19 in HK. To our knowledge, this is one of the few studies to investigate SCI in psychiatric patients in relation to COVID-19 pandemic, and is the first of its kind in Asia and in Chinese population. Our results showed that almost half of our patient sample reported moderate-to-severe SCI. This is slightly higher than that observed in a recent Spanish study which found that 40.9% of psychiatric patients reported cognitive complaints during COVID-19 lockdown (27).
Our results from a multivariate model 1 on psychopathological symptoms revealed that depressive and PTSD-like symptoms were related to CI+ status. Importantly, these two symptom domains remained significant in the final combined model, indicating that more severe depressive and PTSD-like symptoms were independently associated with moderate-to-severe SCI. In fact, the observed association between depression and CI+ is consistent with a prior Spanish study which demonstrated that psychiatric patients with greater depressive symptom severity were significantly more likely to be categorized in CI+ group (27). It is noteworthy that this Spanish study also found a significant association between CI+ and negative symptoms (as measured by CAPE), which, nonetheless, are greatly overlapped with (and thus likely represent) depressive symptoms (27). There is also ample evidence supporting the link between depression and cognitive impairment. Literature has shown that patients with depression exhibit cognitive dysfunction during an acute phase as well as in remission (48–50). Alternatively, the significant relationship between PTSD-like symptoms and CI+ status corroborates with previous findings suggesting that the pandemic can act as a traumatic stressor, which may compromise individuals’ cognitive functions via the process of maladaptive mind wandering (51). Briefly, maladaptive mind wandering has been put forward as an important pathway mediating the association between PTSD-like symptoms and cognitive impairment by competing for the limited cognitive resources such as working memory capacity (52). In the context of COVID-19, maladaptive mind wandering comprises persistent worries of contagion and other pandemic-related adverse consequences, increased alertness and self-monitoring of physical symptoms, and constant checking of COVID-19 related news, to name a few (51). Taken together, our findings on psychopathological symptoms indicate that early recognition and prompt intervention (e.g., psychological treatments) of depressive and PTSD-like symptoms emerged in the pandemic not only alleviate symptom severity but may also reduce the risk of developing SCI in psychiatric patients.
We have conducted a comprehensive evaluation of coping strategies, resilience and COVID-19 related factors among psychiatric patients. Our multivariate model 2 showed that adoption of avoidant coping style, lower resilience and a greater number of stressors were related to CI+ status. The final model incorporating psychopathological symptoms as well as socio-demographics and illness profiles indicated that avoidant coping style remained significantly associated with CI+. It is acknowledged that avoidant coping is characterized by making cognitive and behavioral efforts in evading traumatic-related stressors (53). An extensive literature has documented the bi-directional association between avoidant coping strategies and various psychopathological symptoms including PTSD symptoms (54, 55), depression and anxiety (56). Recent data have also found that individuals with more frequent use of avoidant coping strategies experienced more depressive and anxiety symptoms during COVID-19 lockdown (57). Given its close relationship with PTSD-like, depressive and anxiety symptoms, avoidant coping style may thus exert an indirect effect on the development of SCI via manifestations of these psychopathological symptoms. Conversely, an earlier Spanish study demonstrated that positive coping strategies including performing physical and relaxing activities, and maintaining a routine during the lockdown were protective factors against cognitive complaints during lockdown, albeit these coping variables became non-significant in their final combined model incorporating psychopathological symptoms (27). Of note, we failed to identify any COVID-19 related factors that were independently associated with CI+. It is possible that the potential effect of COVID-19 related factors on SCI could be fully mediated by psychopathological symptoms and maladaptive coping styles. Owing to the paucity of existing data, further research is required to verify our findings on the relationship between pandemic-related factors and SCI in psychiatric patients.
This study has several methodological limitations. First, although the SCI questionnaire was adapted from COBRA, an established self-report measure of cognitive complaints in psychiatric patients, and has been adopted in a recent study examining SCI in patients with CMD and SMD during pandemic, further research is still needed to verify its psychometric properties. Second, our results were based on patients’ self-perceived cognitive complaints rather than objective cognitive assessment, which was not included in the study. This precludes us from clarifying whether our findings on SCI would be discrepant from data obtained via objective measures. Notably, there is evidence indicating poor concordance between subjective cognitive ratings and objective cognitive performance in healthy participants (58, 59) and psychiatric samples (60, 61). It is postulated that SCI and objectively-measured cognitive functions may represent two relatively distinct, albeit related, constructs. An inherent difference in settings between objective cognitive evaluation using standardized battery conducted in laboratory environment and self-perceived deficits emerged in unstructured real-world situations may also contribute to a lack of concurrence between these two cognitive measures. Third, the cross-sectional study design precludes establishment of causal relationship. Longitudinal research is warranted to determine the course of SCI over time and its predictors. Fourth, we did not collect data regarding the use of pharmacological or psychological treatment, and side-effects of psychotropic medications. Thus, we were not able to assess the potential effect of these treatment modalities on mental health outcomes and cognitive impairment. Lastly, as HK is a highly urbanized city and is categorized by the World Bank as a high-income economy (62), our findings may not be generalizable to mainland China or other Asian regions. Differences in ethno-cultural backgrounds as well as access to and quality of healthcare services across regions may further limit the generalizability of our results to other countries.
In conclusion, our study shows that moderate-to-severe cognitive complaints are prevalent in Chinese psychiatric outpatients during the fifth wave of COVID-19 pandemic. Depressive symptoms, PTSD-like symptoms and avoidant coping style are found to be correlates of CI+ status. Our results have several clinical implications. Although COVID-19 related factors are not independently associated with subjective cognitive impairment, the susceptibility of patients with pre-existing mental illness to COVID-19 related stressors and their ramifications on exacerbation of psychopathological symptoms and the overall psychological wellbeing should not be overlooked. Given the increased vulnerability to exacerbation of pre-existing cognitive dysfunction among psychiatric patients amidst the pandemic (and future public health crisis), early detection and psychosocial interventions of psychopathological symptoms, in particular depressive and PTSD-like symptoms, as well as rectification of maladaptive coping strategies are hence, crucial to minimize negative mental health impact and cognitive impairment. Exploration and development of effective strategies to promote personal resilience and the use of positive coping methods may also enhance protection against elevated risk of cognitive complaints. Prospective follow-up investigation is required to track the longitudinal trajectories of SCI and its predictors in relation to the subsequent course of pandemic and the post-pandemic era as well as the accompanied changes in public health policy measures.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
Wic, EC, and CW designed and conceptualized the study. VF, JaC, JoC, and RC conducted data collection. VF and JaC conducted statistical analysis. VF wrote the first draft of the manuscript. Wic, VF, EC, CW, and CL interpreted the study data. Wic and VF revised and finalized the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The study was supported by the Hong Kong Research Grants Council (grant number: 10617014). The funders had no role in study design, data collection, data analysis, interpretation of the data, manuscript preparation or journal submission.
Acknowledgments
We thank all the coordinating clinicians and staff from the psychiatric outpatient units for their kind assistance. We are also grateful to the individuals who participated in the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1216768/full#supplementary-material
References
1. Wang, C , Horby, PW , Hayden, FG , and Gao, GF . A novel coronavirus outbreak of global health concern. Lancet. (2020) 395:470–3. doi: 10.1016/S0140-6736(20)30185-9
2. World Health Organization (WHO) . Timeline: WHO's COVID-19 response (2020). Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline#! (Accessed December 18, 2022).
3. Blasco-Belled, A , Tejada-Gallardo, C , Fatsini-Prats, M , and Alsinet, C . Mental health among the general population and healthcare workers during the COVID-19 pandemic: a meta-analysis of well-being and psychological distress prevalence. Curr Psychol. (2022):1–12. doi: 10.1007/s12144-022-02913-6
4. Dragioti, E , Li, H , Tsitsas, G , Lee, KH , Choi, J , Kim, J, et al. A large-scale meta-analytic atlas of mental health problems prevalence during the COVID-19 early pandemic. J Med Virol. (2022) 94:1935–49. doi: 10.1002/jmv.27549
5. Brailovskaia, J , Cosci, F , Mansueto, G , and Margraf, J . The relationship between social media use, stress symptoms and burden caused by coronavirus (Covid-19) in Germany and Italy: a cross-sectional and longitudinal investigation. J Affect Disord Rep. (2021) 3:100067. doi: 10.1016/j.jadr.2020.100067
6. Mansueto, G , Lopes, FL , Grassi, L , and Cosci, F . Impact of COVID-19 outbreak on Italian healthcare workers versus general population: results from an online survey. Clin Psychol Psychother. (2021) 28:1334–45. doi: 10.1002/cpp.2644
7. Alhakami, A , Salem, V , Alateeq, D , Nikčević, AV , Marci, T , Palmieri, S, et al. The Arab COVID-19 anxiety syndrome scale (C-19ASS): COVID-19 anxiety syndrome and psychological symptoms in the Saudi Arabian population. Clin Psychol Psychother. (2023). doi: 10.1002/cpp.2860
8. Ueda, M , Stickley, A , Sueki, H , and Matsubayashi, T . Mental health status of the general population in Japan during the COVID-19 pandemic. Psychiatry Clin Neurosci. (2020) 74:505–6. doi: 10.1111/pcn.13105
9. Cavicchioli, M , Ferrucci, R , Guidetti, M , Canevini, MP , Pravettoni, G , and Galli, F . What will be the impact of the Covid-19 quarantine on psychological distress? Considerations based on a systematic review of pandemic outbreaks. Healthcare. (2021) 9:101. doi: 10.3390/healthcare9010101
10. Galea, S , Merchant, RM , Lurie, N , and Galea, S . The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Intern Med. (2020) 180:817–8. doi: 10.1001/jamainternmed.2020.1562
11. Taquet, M , Luciano, S , Geddes, JR , and Harrison, PJ . Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. (2021) 8:130–40. doi: 10.1016/S2215-0366(20)30462-4
12. Wang, Q , Xu, R , and Volkow, ND . Increased risk of COVID-19 infection and mortality in people with mental disorders: analysis from electronic health records in the United States. World Psychiatry. (2021) 20:124–30. doi: 10.1002/wps.20806
13. Fond, G , Nemani, K , Etchecopar-Etchart, D , Loundou, A , Goff, DC , Lee, SW, et al. Association between mental health disorders and mortality among patients with COVID-19 in 7 countries: a systematic review and meta-analysis. JAMA Psychiat. (2021) 78:1208–17. doi: 10.1001/jamapsychiatry.2021.2274
14. Toubasi, AA , AbuAnzeh, RB , Tawileh, HB , Aldebei, RH , and Alryalat, SA . A meta-analysis: the mortality and severity of COVID-19 among patients with mental disorders. Psychiatry Res. (2021) 299:113856. doi: 10.1016/j.psychres.2021.113856
15. Iasevoli, F , Fornaro, M , D'Urso, G , Galletta, D , Casella, C , Paternoster, M, et al. COVID-19 in psychiatry study group. Psychological distress in patients with serious mental illness during the COVID-19 outbreak and one-month mass quarantine in Italy. Psychol Med. (2021) 51:1054–6. doi: 10.1017/S0033291720001841
16. Solé, B , Verdolini, N , Amoretti, S , Montejo, L , Rosa, AR , Hogg, B, et al. Effects of the COVID-19 pandemic and lockdown in Spain: comparison between community controls and patients with a psychiatric disorder. Preliminary results from the BRIS-MHC study. J Affect Disord. (2021) 281:13–23. doi: 10.1016/j.jad.2020.11.099
17. Cheung, PH , Chan, CP , and Jin, DY . Lessons learned from the fifth wave of COVID-19 in Hong Kong in early 2022. Emerg Microbes Infect. (2022) 11:1072–8. doi: 10.1080/22221751.2022.2060137
18. Lee, RS , Hermens, DF , Porter, MA , and Redoblado-Hodge, MA . A meta-analysis of cognitive deficits in first-episode major depressive disorder. J Affect Disord. (2012) 140:113–24. doi: 10.1016/j.jad.2011.10.023
19. Modelling the fifth wave of COVID-19 in Hong Kong (2022). Available at: https://www.med.hku.hk/en/news/press/media/DF5A2F6918764DC4B6517CE7B5F2796B.ashx (Accessed November 24, 2022).
20. Chau, C. Explainer: how Hong Kong’s Covid policies shifted during the fifth wave crisis (2022). Available at: https://hongkongfp.com/2022/03/20/explainer-how-govt-covid-19-policies-have-shifted-since-the-beginning-of-the-fifth-wave/ (Accessed December 18, 2022).
21. Choi, EP , Hui, BP , and Wan, EY . Depression and anxiety in Hong Kong during COVID-19. Int J Environ Res Public Health. (2020) 17:3740. doi: 10.3390/ijerph17103740
22. Tso, IF , and Park, S . Alarming levels of psychiatric symptoms and the role of loneliness during the COVID-19 epidemic: a case study of Hong Kong. Psychiatry Res. (2020) 293:113423. doi: 10.1016/j.psychres.2020.113423
23. Zhao, SZ , Wong, JY , Luk, TT , Wai, AK , Lam, TH , and Wang, MP . Mental health crisis under COVID-19 pandemic in Hong Kong. China Int J Infect Dis. (2020) 100:431–3. doi: 10.1016/j.ijid.2020.09.030
24. Li, JT , Lee, CP , and Tang, WK . Changes in mental health among psychiatric patients during the COVID-19 pandemic in Hong Kong—a cross-sectional study. Int J Environ Res Public Health. (2022) 19:1181. doi: 10.3390/ijerph19031181
25. Fiorenzato, E , Zabberoni, S , Costa, A , and Cona, G . Cognitive and mental health changes and their vulnerability factors related to COVID-19 lockdown in Italy. PLoS One. (2021) 16:e0246204. doi: 10.1371/journal.pone.0246204
26. Kira, IA , Alpay, EH , Ayna, YE , Shuwiekh, HA , Ashby, JS , and Turkeli, A . The effects of COVID-19 continuous traumatic stressors on mental health and cognitive functioning: a case example from Turkey. Curr Psychol. (2021) 41:7371–82. doi: 10.1007/s12144-021-01743-2
27. Montejo, L , Solé, B , Verdolini, N , Martínez-Arán, A , del Mar, BC , Radua, J, et al. Self-reported neurocognitive symptoms during COVID-19 lockdown and its associated factors in a sample of psychiatric patients. Results from the BRIS-MHC study. Eur Neuropsychopharmacol. (2021) 53:7–18. doi: 10.1016/j.euroneuro.2021.07.006
28. Kroenke, K , Spitzer, RL , and Williams, JB . The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
29. Yu, X , Tam, WW , Wong, PT , Lam, TH , and Stewart, SM . The patient health Questionnaire-9 for measuring depressive symptoms among the general population in Hong Kong. Compr Psychiatry. (2012) 53:95–102. doi: 10.1016/j.comppsych.2010.11.002
30. Spitzer, RL , Kroenke, K , Williams, JB , and Löwe, B . A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
31. Tong, X , An, D , McGonigal, A , Park, SP , and Zhou, D . Validation of the generalized anxiety Disorder-7 (GAD-7) among Chinese people with epilepsy. Epilepsy Res. (2016) 120:31–6. doi: 10.1016/j.eplepsyres.2015.11.019
32. Guo, J , Yang, L , Xu, Y , Zhang, C , Luo, X , Liu, S, et al. Prevalence and risk factors associated with insomnia symptoms among the Chinese general public after the coronavirus disease 2019 epidemic was initially controlled. Nat Sci Sleep. (2021) 13:703–12. doi: 10.2147/NSS.S307996
33. Wu, KK , and Chan, KS . The development of the Chinese version of impact of event scale - revised (CIES-R). Soc Psychiatry Psychiatr Epidemiol. (2003) 38:94–8. doi: 10.1007/s00127-003-0611-x
34. Bastien, CH , Vallières, A , and Morin, CM . Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. (2001) 2:297–307. doi: 10.1016/S1389-9457(00)00065-4
35. Yeung, WF , Chung, KF , Zhang, SP , Yap, TG , and Law, AC . Electroacupuncture for primary insomnia: a randomized controlled trial. Sleep. (2009) 32:1039–47. doi: 10.1093/sleep/32.8.1039
36. Mark, W , and Toulopoulou, T . Validation of the Chinese version of community assessment of psychic experiences (CAPE) in an adolescent general population. Asian J Psychiatry. (2017) 26:58–65. doi: 10.1016/j.ajp.2017.01.012
37. Krynicki, CR , Upthegrove, R , Deakin, JFW , and Barnes, TRE . The relationship between negative symptoms and depression in schizophrenia: a systematic review. Acta Psychiatr Scand. (2018) 137:380–90. doi: 10.1111/acps.12873
38. Rosa, AR , Mercadé, C , Sánchez-Moreno, J , Solé, B , del Mar, BC , Torrent, C, et al. Validity and reliability of a rating scale on subjective cognitive deficits in bipolar disorder (COBRA). J Affect Disord. (2013) 150:29–36. doi: 10.1016/j.jad.2013.02.022
39. Xiao, L , Lin, X , Wang, Q , Lu, D , and Tang, S . Adaptation and validation of the “cognitive complaints in bipolar disorder rating assessment” (COBRA) in Chinese bipolar patients. J Affect Disord. (2015) 173:226–31. doi: 10.1016/j.jad.2014.11.011
40. Carver, CS . You want to measure coping but your protocol is too long: consider the brief cope. Int J Behav Med. (1997) 4:92–100. doi: 10.1207/s15327558ijbm0401_6
41. Ye, S . A longitudinal study of subjective well-being among Chinese university students: The roles of personality, attribution, and coping. [Doctoral Thesis]. Hong Kong: University of Hong Kong (2008).
42. Dias, C , Cruz, JF , and Fonseca, AM . The relationship between multidimensional competitive anxiety, cognitive threat appraisal, and coping strategies: a multi-sport study. Int J Sport Exerc Psychol. (2012) 10:52–65. doi: 10.1080/1612197X.2012.645131
43. Hsin, YZ . Reliability and validity of the brief resilience scale. [Master thesis]. Taiwan: National Pingtung University (2020).
44. Smith, BW , Dalen, J , Wiggins, K , Tooley, E , Christopher, P , and Bernard, J . The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. (2008) 15:194–200. doi: 10.1080/10705500802222972
45. Hosmer, DW Jr, Lemeshow, S , and Sturdivant, RX . Applied logistic regression. Hoboken, New Jersey: John Wiley & Sons (2013).
46. van Buuren, S , and Groothuis-Oudshoorn, K . Mice: multivariate imputation by chained equations in R. J Stat Softw. (2011) 45:1–67. doi: 10.18637/jss.v045.i03
48. Conradi, HJ , Ormel, J , and de Jonge, P . Presence of individual (residual) symptoms during depressive episodes and periods of remission: a 3-year prospective study. Psychol Med. (2010) 41:1165–74. doi: 10.1017/S0033291710001911
49. Lee, P. Covid-19 in data: 7 charts showing Hong Kong’s deadly omicron outbreak (2022). Available at: https://hongkongfp.com/2022/03/12/covid-19-in-data-6-charts-showing-hong-kongs-deadly-omicron-outbreak/ (Accessed December 18, 2022).
50. Semkovska, M , Quinlivan, L , O'Grady, T , Johnson, R , Collins, A , O'Connor, J, et al. Cognitive function following a major depressive episode: a systematic review and meta-analysis. Lancet Psychiatry. (2019) 6:851–61. doi: 10.1016/S2215-0366(19)30291-3
51. Boals, A , and Banks, JB . Stress and cognitive functioning during a pandemic: thoughts from stress researchers. Psychol Trauma. (2020) 12:S255–7. doi: 10.1037/tra0000716
52. Banks, JB , and Boals, A . Understanding the role of mind wandering in stress-related working memory impairments. Cogn Emot. (2017) 31:1023–30. doi: 10.1080/02699931.2016.1179174
53. Penley, JA , Tomaka, J , and Wiebe, JS . The association of coping to physical and psychological health outcomes: a meta-analytic review. J Behav Med. (2002) 25:551–603. doi: 10.1023/A:1020641400589
54. Thompson, NJ , Fiorillo, D , Rothbaum, BO , Ressler, KJ , and Michopoulos, V . Coping strategies as mediators in relation to resilience and posttraumatic stress disorder. J Affect Disord. (2018) 225:153–9. doi: 10.1016/j.jad.2017.08.049
55. Tiet, QQ , Rosen, C , Cavella, S , Moos, RH , Finney, JW , and Yesavage, J . Coping, symptoms, and functioning outcomes of patients with posttraumatic stress disorder. J Trauma Stress. (2006) 19:799–811. doi: 10.1002/jts.20185
56. Grant, DM , Wingate, LR , Rasmussen, KA , Davidson, CL , Slish, ML , Rhoades-Kerswill, S, et al. An examination of the reciprocal relationship between avoidance coping and symptoms of anxiety and depression. J Soc Clin Psychol. (2013) 32:878–96. doi: 10.1521/jscp.2013.32.8.878
57. Fluharty, M , Bu, F , Steptoe, A , and Fancourt, D . Coping strategies and mental health trajectories during the first 21 weeks of COVID-19 lockdown in the United Kingdom. Soc Sci Med. (2021) 279:113958. doi: 10.1016/j.socscimed.2021.113958
58. Chaytor, N , and Schmitter-Edgecombe, M . The ecological validity of neuropsychological tests: a review of the literature on everyday cognitive skills. Neuropsychol Rev. (2003) 13:181–97. doi: 10.1023/B:NERV.0000009483.91468.fb
59. van der Elst, W , van Boxtel, MP , van Breukelen, GJ , and Jolles, J . A large-scale cross-sectional and longitudinal study into the ecological validity of neuropsychological test measures in neurologically intact people. Arch Clin Neuropsychol. (2008) 23:787–800. doi: 10.1016/j.acn.2008.09.002
60. Chang, WC , Chan, TC , Chiu, SS , Hui, CL , Chan, SK , Lee, EH, et al. Self-perceived cognitive functioning and its relationship with objective performance in first-episode schizophrenia: the subjective cognitive impairment scale. Compr Psychiatry. (2015) 56:42–50. doi: 10.1016/j.comppsych.2014.10.004
61. Serra-Blasco, M , Torres, IJ , Vicent-Gil, M , Goldberg, X , Navarra-Ventura, G , Aguilar, E, et al. Discrepancy between objective and subjective cognition in major depressive disorder. Eur Neuropsychopharmacol. (2019) 29:46–56. doi: 10.1016/j.euroneuro.2018.11.1104
62. World Bank . World Bank Country and Lending Groups. (n.d.)Available at: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (Accessed 25 July 2023).
Keywords: self-reported cognitive complaints, mental disorders, COVID-19, depression, traumatic stress symptoms, coping styles
Citation: Fung VSC, Chan JMT, Chui EMC, Wong CSM, Chan JKN, Chu RST, So YK, Chung AKK, Lee KCK, Cheng CPW, Law CW, Chan WC and Chang WC (2023) Prevalence and correlates of subjective cognitive impairment in Chinese psychiatric patients during the fifth wave of COVID-19 in Hong Kong. Front. Psychiatry. 14:1216768. doi: 10.3389/fpsyt.2023.1216768
Edited by:
Raúl Durón-Figueroa, National Autonomous University of Mexico, MexicoReviewed by:
Camilla Gesi, ASST Fatebenefratelli Sacco, ItalyGiovanni Mansueto, University of Florence, Italy
Copyright © 2023 Fung, Chan, Chui, Wong, Chan, Chu, So, Chung, Lee, Cheng, Law, Chan and Chang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wing Chung Chang, Y2hhbmd3Y0Boa3UuaGs=
 Vivian Shi Cheng Fung1
Vivian Shi Cheng Fung1 Corine Sau Man Wong
Corine Sau Man Wong Joe Kwun Nam Chan
Joe Kwun Nam Chan Albert Kar Kin Chung
Albert Kar Kin Chung Calvin Pak Wing Cheng
Calvin Pak Wing Cheng Chi Wing Law
Chi Wing Law Wai Chi Chan
Wai Chi Chan Wing Chung Chang
Wing Chung Chang