
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 25 May 2023
Sec. Neuroimaging
Volume 14 - 2023 | https://doi.org/10.3389/fpsyt.2023.1205126
This article is part of the Research TopicCase Reports in Neuroimaging and StimulationView all 8 articles
Background: Mental health issues, including panic disorder (PD), are prevalent and often co-occur with anxiety and bipolar disorders. While panic disorder is characterized by unexpected panic attacks, and its treatment often involves antidepressants, there is a 20–40% risk of inducing mania (antidepressant-induced mania) during treatment, making it crucial to understand mania risk factors. However, research on clinical and neurological characteristics of patients with anxiety disorders who develop mania is limited.
Methods: In this single case study, we conducted a larger prospective study on panic disorder, comparing baseline data between one patient who developed mania (PD-manic) and others who did not (PD-NM group). We enrolled 27 patients with panic disorder and 30 healthy controls (HCs) and examined alterations in amygdala-based brain connectivity using a seed-based whole-brain approach. We also performed exploratory comparisons with healthy controls using ROI-to-ROI analyses and conducted statistical inferences at a threshold of cluster-level family-wise error-corrected p < 0.05, with the cluster-forming threshold at the voxel level of uncorrected p < 0.001.
Results: The patient with PD-mania showed lower connectivity in brain regions related to the default mode network (left precuneous cortex, maximum z-value within the cluster = −6.99) and frontoparietal network (right middle frontal gyrus, maximum z-value within the cluster = −7.38; two regions in left supramarginal gyrus, maximum z-value within the cluster = −5.02 and −5.86), and higher in brain regions associated with visual processing network (right lingual gyrus, maximum z-value within the cluster = 7.86; right lateral occipital cortex, maximum z-value within the cluster = 8.09; right medial temporal gyrus, maximum z-value within the cluster = 8.16) in the patient with PD-mania compared to the PD-NM group. One significantly identified cluster, the left medial temporal gyrus (maximum z-value within the cluster = 5.82), presented higher resting-state functional connectivity with the right amygdala. Additionally, ROI-to-ROI analysis revealed that significant clusters between PD-manic and PD-NM groups differed from HCs in the PD-manic group but not in the PD-NM group.
Conclusion: Here, we demonstrate altered amygdala-DMN and amygdala-FPN connectivity in the PD-manic patient, as reported in bipolar disorder (hypo) manic episodes. Our study suggests that amygdala-based resting-state functional connectivity could serve as a potential biomarker for antidepressant-induced mania in panic disorder patients. Our findings provide an advance in understanding the neurological basis of antidepressant-induced mania, but further research with larger cohorts and more cases is necessary for a broader perspective on this issue.
Panic disorder (PD) is a common mental disorder often encountered by primary care physicians (1). The hallmark of PD is repeated unexpected panic attacks (2). Its lifetime prevalence in the general population ranges from 3.3 to 7% (3). Among the pharmacological agents, antidepressants, including serotonin-norepinephrine reuptake inhibitors and selective serotonin reuptake inhibitors, are usually considered the first-line treatment for PD (4). However, the use of antidepressants in patients with newly diagnosed PD requires caution, as antidepressants may have a 20–40% risk of inducing mania (5). Antidepressant-induced mania has been proposed as mania or hypomania that develops within 8 week of starting a new conventional antidepressant (6, 7). The unintentional occurrence of mania can have detrimental effects on patients. Therefore, understanding the risk factors for mania in patients with panic attacks is helpful for managing PD.
The comorbidity of anxiety and bipolar disorder (BD) is prevalent (8). In clinical and epidemiological studies on BD, extremely high rates of comorbid anxiety disorders have been reported (9–11). However, there is a lack of knowledge regarding the clinical features and neuroimaging results of mania occurrence in anxiety disorders, including PD (12). According to the Diagnostic and Statistical Manual of mental disorders-5, PD can be diagnosed concurrently with BD (2); however, treatment for panic attacks and related anxiety symptoms differs when there is a comorbid diagnosis of BD (10). Therefore, examining the clinical features and neuroimaging findings before mania in cases where mania develops during treatment for an anxiety disorder without a history of BD is clinically significant.
To our knowledge, research on the clinical and neurological characteristics of patients with anxiety disorders who develop mania after therapy is lacking. Significant advancements in understanding the pathogenesis, making accurate diagnoses, and investigating novel therapeutics for neuropsychiatric disorders can be achieved through the combined efforts of clinical, experimental, and computational medicine (13, 14). There are several findings regarding the clinical characteristics of patients who develop mania during their first depressive episode (15). Some studies have suggested that mania is more likely to occur in depression with prominent anxiety (16). A previous study suggested that comorbid anxiety is a subthreshold bipolarity in depressive episodes (17). However, due to the high comorbidity of depression and anxiety in clinical practice (18) and the limitations of clinical assessment of behavior by interviews (19), there is no consensus on which clinical features suggest subthreshold bipolarity in PD.
Efforts have been made to identify biomarkers for BD prediction using neuroimaging (20). Among the various biomarkers, studies have investigated abnormalities in physiological responses, such as bradycardia, as well as molecular pathways related to mitochondrial function and inflammation (21–24). With advances in techniques, functional magnetic resonance imaging (fMRI), which is the imaging of patterns of brain activity and connections, has been extensively utilized in studies on most psychiatric disorders including BD and PD (25, 26). Resting-state fMRI (rs-fMRI) analyzes variations in blood oxygen level-dependent (BOLD) signals throughout the brain in the absence of emotional or cognitive task involvement (27). rs-fMRI studies have also been conducted extensively in bipolar, bipolar I, and bipolar II disorders and in depressive (hypo) manic, which are acute states of patients with BD (28, 29). Neuroimaging studies have presented several neurobiological hypotheses regarding BD, most of which assume ventral and dorsal brain stream disturbance (20, 28). The ventrolateral prefrontal cortex, dorsal anterior cingulate cortex, dorsolateral prefrontal cortex, and hippocampus comprise the dorsal network, which mediates cognitive processing and executive functions. The ventral neural stream regulates implicit emotions via the amygdala, insula, ventral anterior cingulate cortex, ventral striatum, and ventromedial prefrontal cortex (20, 25, 28).
Alterations in amygdala-based connectivity have been consistently reported in the remission state (euthymic mood) of patients with BD compared with healthy controls (HCs) (30). However, among amygdala-based connectivities, the default mode network (DMN)-related connectivity, depending on mood state, has been reported to decrease in the (hypo) manic episodes (31) and increase in the euthymic or depressive episodes (32). Increased activity in the amygdala-insula, a key region of the DMN, has also been reported to be positively correlated with anxiety (33). Additionally, the medial prefrontal cortex (MPFC), a key component of the DMN, has been demonstrated to be a major contributor to fear inhibition (i.e., fear extinction) in human fear learning models, which are essential in understanding PD (34). Given the risk and impact of mania in treating patients with PD, investigating neuroimaging data before mania onset in patients with PD-mania would be important to determine whether it can be used as a biomarker for prediction of BD. However, to our knowledge, there is insufficient information on this topic.
This report discusses the case of a young man diagnosed with PD with no history of BD who developed mania after treatment with antidepressants. This patient participated in a prospective study related to PD; therefore, we obtained rs-fMRI images before mania onset. In addition, rs-fMRI images of patients with PD who had not developed mania at a follow-up of more than 4 months and of HCs in that study were also acquired. Therefore, this report discusses the differences in the clinical features and amygdala-based resting-state functional connectivity (rsFC) in patients who experience mania during treatment. We believe that this study will support healthcare providers in considering neuroimaging for predicting mania in patients with PD.
The current study is a single case study of antidepressant-induced mania in the longitudinal follow-up of a prospective study aimed to develop a predictive model of treatment response and prognosis in patients with PD using brain images combined with virtual reality-based anxiety behavior evaluation systems (35). In this cross-sectional analysis, baseline data were compared between the single case with mania and other patients without mania.
Patients with PD were recruited through outpatient clinics and public advertisements. A psychiatrist interviewed all patients using the Mini-International Neuropsychiatric Interview to screen for psychiatric illnesses and substance use (36). The eligibility criteria for patients with PD were the same as those used in the feasibility study of the virtual reality-based anxiety behavior evaluation systems (35). The local ethics committee of Korea University Guro Hospital approved the study (2021GR0321). Each participant completed a written informed consent form after being informed of the aims, methodology, and potential risks of the study. The study was conducted in accordance with the Declaration of Helsinki 1964.
Twenty-seven PD and 30 HCs met the eligibility criteria and participated in the study. During the study, one patient progressed to a manic episode (PD-manic patient), and the remaining 26 patients with PD did not progress to mania (PD-NM group) after at least 4 months of follow-up. All patients with PD, including PD-manic patient in the study, used serotonin-norepinephrine reuptake and selective serotonin reuptake inhibitors at baseline, according to treatment guidelines.
A 22-year-old man patient visited our psychiatric clinic in April 2022, reporting recurrent panic attacks and anticipatory anxiety since February 2022. The patient, a university student with no psychiatric history, first sought psychiatric care in February 2022 after experiencing a panic attack that manifested as palpitations, shortness of breath, chest pain, dizziness, and a sense of impending doom. He reported impairment in social functioning due to anticipatory anxiety, experienced 1–2 or more panic attacks daily, and feared being alone. After a limited therapeutic response with persistent panic attacks and anxiety for 2 months at the primary clinic, he was referred to our clinic for further evaluation.
The patients did not report any family history of any psychiatric disorder, including PD, mood disorders, or suicide attempts, was not discovered. He denied any history of BD and alcohol or benzodiazepine abuse. Table 1 presents the patient's demographic and psychological characteristics in April 2022. The patient had a Panic Disorder Severity Scale (PDSS) score of 14, indicating moderate to severe social impairment and 2-3 panic attacks per week (37, 38). Other anxiety-related assessments were mostly moderate to severe (LSAS-fear: 44, LSAS-avoidance: 40, GAD: 17, HADS-anxiety: 16). The patient reported a moderate level of depression (HADS-depression: 11) but no neurovegetative symptoms and did not meet the criteria for major depressive disorder (39, 40). Based on his medical history and the Diagnostic and Statistical Manual of mental disorders-5 (2), PD was diagnosed.
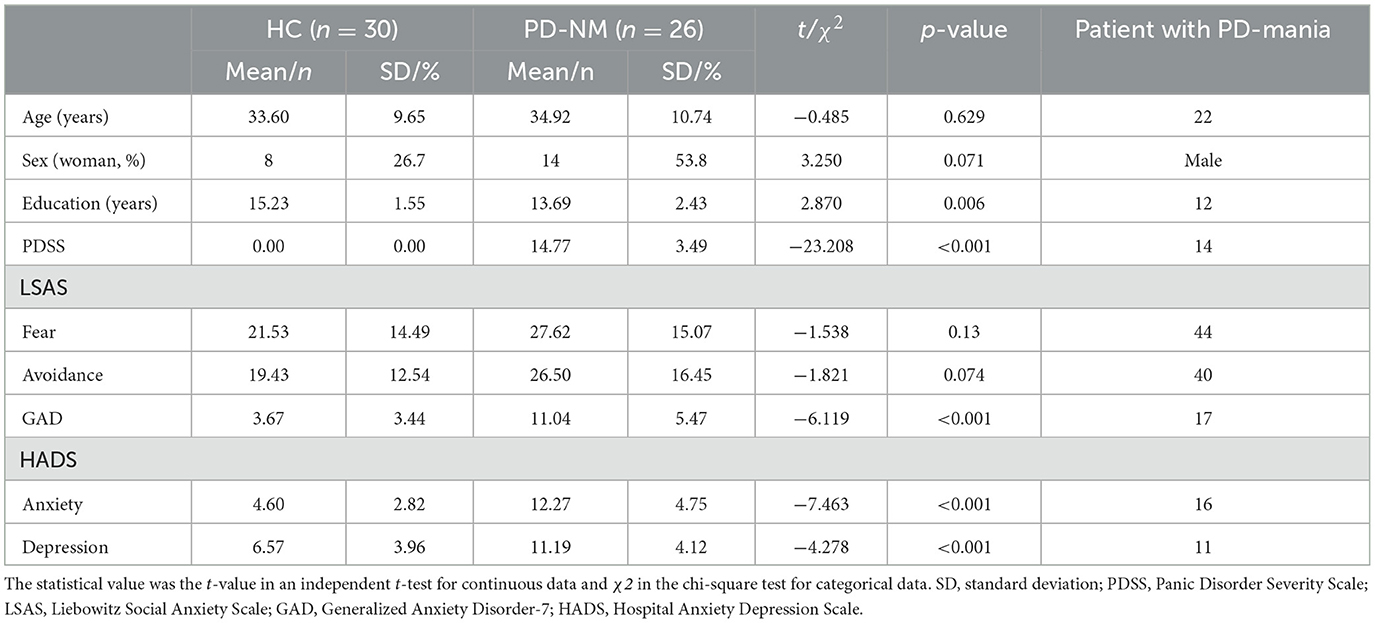
Table 1. Demographic and psychological characteristics of two groups (HC and PD-NM) and the patient with PD-mania.
For the first 2 months, the patient was prescribed medications, including an adequate dose of escitalopram (20 mg/day), desvenlafaxine (100 mg/day), and aripiprazole (5 mg/day), as augmentation treatment. Alprazolam (0.25 mg) and propranolol (10 mg) were prescribed up to three times daily for symptomatic relief of panic attacks and anxiety. After 8 weeks of treatment (June 2022), the patient's frequency of panic attacks decreased to 1–2 times per week, with moderate improvement in the associated anticipatory anxiety, avoidance behaviors, and related social behavior problems. However, he was rated as moderately ill, with a panic disorder severity scale score of 14.
For the patient's symptoms associated with PD, desvenlafaxine was increased from the previous dose to 200 mg/day in June 2022, and aripiprazole was increased to 7 mg/day 4 weeks later. In July 2022, the treatment effect was unsatisfactory, with no further improvement in panic attacks and anxiety (panic disorder severity scale score of 14) and worsening depression with neurovegetative symptoms. In August 2022, increased impulsivity, overspending, and polydipsia were reported, and a manic episode was considered, with a score of 18 on the Young Mania Rating Scale (YMRS). Escitalopram and desvenlafaxine were tapered off and escalated to lithium (900 mg/day) and quetiapine XR (600 mg/day) for 5 weekweeks. The patient returned to a euthymic state with YMRS scores of 12 and 6 in September 2022 and October 2022, respectively. During the 2 months, the patient did not report any panic attacks.
The patient participated in a prospective study conducted in our psychiatric clinic in June 2021; therefore, we obtained fMRI images produced when he was diagnosed with and treated for PD before his manic episode.
The same assessments as those in the VRABES feasibility study were performed at baseline before the fMRI. PDSS was used as an interview measure of PD severity (37), and the Liebowitz Social Anxiety Scale Self-Report Version (LSAS) (41), Generalized Anxiety Disorder Scale (42), and Hospital Anxiety and Depression Scale (HADS) were used to examine anxiety-related traits (43). For patients with mania, YMRS data were collected in an outpatient setting, as clinically indicated (44).
A 3 T Philips Ingenia scanner (Philips Healthcare, Best, Netherlands) was used to collect the images. Coronal anatomical images were acquired using a 3D T1-weighted (T1w) fast gradient echo sequence (repetition time (TR) = 4.6 ms, echo time (TE) = 9.9 ms, 220 slices, slice thickness = 1 mm, and field of view (FOV) = 224 × 224 × 224). For the functional images, a T2*-weighted (BOLD) image was obtained (TR = 2,000 ms, TE = 22 ms, 38 slices, slice thickness = 3 mm, FOV = 210 × 210 × 216, and voxel size = 3 × 3 × 3 mm). Images were acquired in the transverse orientation. The participants were advised to relax, stay awake, keep their eyes open, and focus on the cross symbol displayed on the screen throughout the scanning process.
The results included in this manuscript are from the preprocessing performed using fMRIPrep 21.0.2 (45), which is based on Nipype 1.8.1 (46, 47).
A total of one T1w images were discovered within the input Brain Imaging Data Structure dataset. All images were corrected for intensity non-uniformity with N4BiasFieldCorrection (48) and distributed with Advanced Normalization Tools (ANTs) 2.3.3 (RRID: SCR_004757) (49). The T1w-reference was then skull-stripped with a Nipype implementation of the antsBrainExtraction.sh workflow (from ANTs), using OASIS30ANTs as the target template. Brain tissue segmentation of the cerebrospinal fluid (CSF), white matter (WM), and gray matter was performed on brain-extracted T1w images using fast (FSL 6.0.5.1:57b01774, RRID: SCR_002823) (50). A T1w-reference map was computed after the registration of two T1w images (after intensity non-uniformity correction) using the mri_robust_template (FreeSurfer 6.0.1) (51). Volume-based spatial normalization to one standard space (MNI152NLin2009cAsym) was performed through non-linear registration with antsRegistration (ANTs 2.3.3) using brain-extracted versions of both the T1w reference and T1w template. The following template was selected for spatial normalization: ICBM 152 Non-linear Asymmetrical template version 2009c (52) (RRID: SCR_008796; TemplateFlow ID: MNI152NLin2009cAsym).
The following preprocessing was performed for each BOLD run obtained per participant (across all tasks and sessions). First, a reference volume and its skull-stripped version were generated using the custom fMRIPrep methodology. Head-motion parameters with respect to the BOLD reference (transformation matrices and six corresponding rotation and translation parameters) were estimated before spatiotemporal filtering using mcflirt (FSL 6.0.5.1:57b01774) (53). The BOLD time series (including slice-timing correction when applied) was resampled onto its original native space by applying transforms to correct for head motion. These resampled BOLD time series are called preprocessed BOLD in original space or just preprocessed BOLD. The BOLD reference was then coregistered with the T1w reference using mri_coreg (FreeSurfer), followed by flirt (FSL 6.0.5.1:57b01774) (54) with the boundary-based registration (55) cost function. Co-registration was configured with six degrees of freedom. Several confounding time series were calculated based on the preprocessed BOLD: framewise displacement (FD), differential variation in signals (DVARS), and three region-wise global signals. The FD was computed using two formulations: power (absolute sum of relative motions) (56) and Jenkinson (relative root-mean-square displacement between affines) (53). The FD and DVARS were calculated for each functional run using their implementations in Nipype (56). Three global signals were extracted from the CSF, WM, and whole-brain masks. In addition, a set of physiological regressors were extracted to allow for component-based noise correction (CompCor) (57). Principal components were estimated after high-pass filtering of the preprocessed BOLD time series (using a discrete cosine filter with a 128 s cut-off) for the two CompCor variants: temporal (tCompCor) and anatomical (aCompCor). The tCompCor components were calculated from the top 2% of the variable voxels within the brain mask. For aCompCor, three probabilistic masks (CSF, WM, and combined CSF+WM) were generated in anatomical space. The implementation differs from that of Behzadi et al.; instead of eroding the masks by two pixels in the BOLD space, the aCompCor masks were subtracted from a mask of pixels that likely contained a volume fraction of the gray matter. This mask was obtained by thresholding the corresponding partial volume map at 0.05, which ensured that the components were not extracted from the voxels containing a minimal fraction of gray matter. Finally, these masks were resampled into the BOLD space and binarized by thresholding at 0.99 (as in the original implementation). The components of the WM and CSF masks were calculated separately. For each CompCor decomposition, the k components with the largest singular values were retained, such that the time series of the retained components was sufficient to explain 50% of the variance across the nuisance mask (CSF, WM, combined, or temporal). The remaining components were excluded from the analysis. The head motion estimates calculated in the correction step were also placed in the corresponding confounding file. The confounded time series derived from the head motion estimates and global signals was expanded by including temporal derivatives and quadratic terms (58). Frames that exceeded a threshold of 0.5 mm FD or 1.5 standardized DVARS were annotated as motion outliers. The BOLD time series was resampled into a standard space, generating a preprocessed BOLD run in MNI152NLin2009cAsym space. A reference volume and its skull-stripped version were generated using the custom methodology of fMRIPrep. All resamplings were performed in a single interpolation step by composing all pertinent transformations (head-motion transform matrices, susceptibility distortion correction when available, and co-registration with anatomical and output spaces). Gridded (volumetric) resampling was performed using antsApplyTransforms (ANTs), configured with Lanczos interpolation to minimize the smoothing effects of other kernels (59). Non-gridded (surface) resampling was performed using mri_vol2surf (FreeSurfer).
In line with our hypothesis that alterations in amygdala-based brain connectivity would appear between the PD-manic patient and PD-NM group prior to a manic episode, we conducted a seed-based, whole-brain analysis using two regions of interest (ROIs): the right and left amygdala. The automated anatomical labeling (AAL2) atlas was employed to define these ROIs (60). Anatomical atlases, such as AAL, have been shown to yield reliable and valid results (61), and recent studies on amygdala-based brain connectivity in panic disorder have also utilized the AAL2 atlas (62, 63). Temporal correlations between the BOLD signals in the left and right amygdala seed regions (AAL41 and AAL42, respectively) were computed using CONN toolbox (64). Pearson's bivariate correlation analysis was performed to calculate the connections between the seeds and other voxels in the whole brain. The resulting values were then converted to z-scores using the Fisher's r-to-z transformation. In the seconds level random effect analysis, a generalized linear model analysis of covariance was conducted to examine between-group (PD-NM group vs. PD-manic patient) differences in FC patterns, controlling for the effects of age, sex, and years of education. Statistical inferences to identify brain regions revealing significant differences were performed at the threshold of cluster-level family-wise error-corrected p (pFWE) < 0.05, with the cluster-forming threshold at the voxel level of uncorrected p < 0.001.
The main hypothesis focuses on differences between the anxiety disorder group, who did not develop mania, and patients who did; however, exploratory comparisons between HCs and the non-manic anxiety group in seed-based functional connectivity were also performed. To evaluate the degree to which observed differences between the PD-NM and PD-manic groups reflect aberrant brain functioning, ROI-to-ROI analyses were performed using both amygdalae (AAL41 & 42) and identified brain regions in the seed-based analysis as seed ROIs. Fisher's z-transformed correlations were calculated to indicate the connectivity strength between each pair of ROIs. Between-group differences (PD-NM vs. HC) were studied using analysis of covariance, controlling for age, sex, and years of education. ROI-to-ROI results were reported as significant if p < 0.05 andROI-level false-discovery rate corrected (pFDR).
Statistical analyses of the demographic and psychological characteristics between the PD-NM and HC groups were conducted using a software package (IBM SPSS Statistics v28.0, IBM Corporation, Armonk, NY, USA). Demographics and psychological evaluations of the PD-NM and HC groups were compared using an independent t-test for continuous data and a chi-square test for categorical data. p < 0.05 was considered statistically significant.
The demographic features and assessment scores of the PD-NM, HC, and PD-manic groups are presented in Table 1. The distributions of age, sex, and marital status between the two groups (PD-NM vs. HC) did not vary significantly. The PD-NM group had more years of education than the HC group. Except for the LSAS-fear and LSAS-avoidance subscale scores, psychological characteristics associated with anxiety differed significantly. The patient in the PD-manic group was relatively younger and had fewer years of education than the recruited patients and HCs. Scores on the LSAS-SR and anxiety subscales of the Generalized Anxiety Disorder Scale and HADS were relatively higher than the mean for the PD-NM group. This was a single case; thus, no statistical analysis could be performed. However, age, years of education, panic disorder severity scale, LSAS, Generalized Anxiety Disorder Scale, and HADS scores were all within two standard deviations of the distribution in the PD-NM group.
After adjusting for the potential effects of age, sex, and years of education, seven clusters with the left amygdala and one with the right amygdala in which the PD-NM group and PD-manic patient differed were identified (Table 2). Compared with the PD-NM group, the PD-manic patient demonstrated lower rsFC between the left amygdala and left precuneus cortex (PrC), right middle frontal gyrus (MFG), and two left supramarginal gyri (SMG), and higher rsFC between the left amygdala and right lateral occipital cortex (LOC), right lingual gyrus (LG), and right middle temporal gyrus (MTG). One identified cluster, the left MTG, presented higher rsFC with the right amygdala (Figure 1).
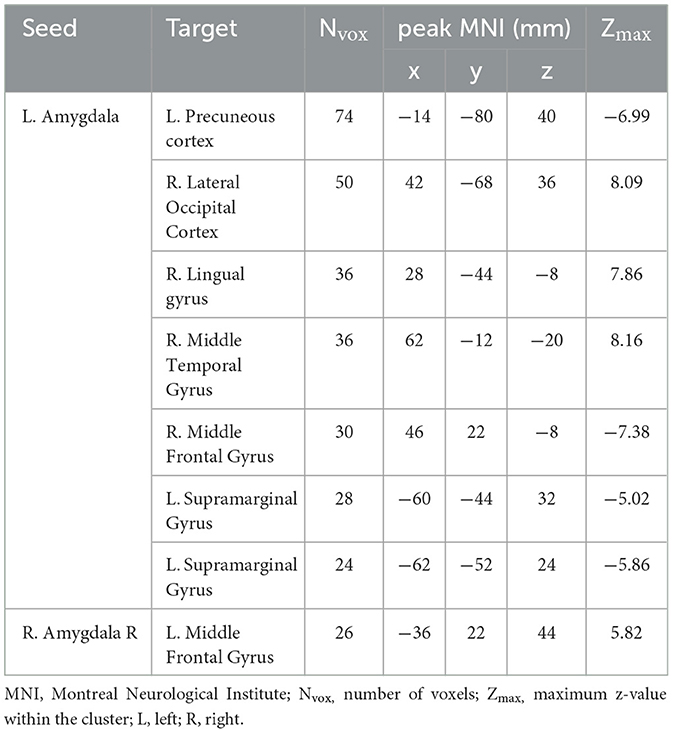
Table 2. Results of the seed-based functional connectivity analysis between the PD-NM group and the patient with PD-mania.
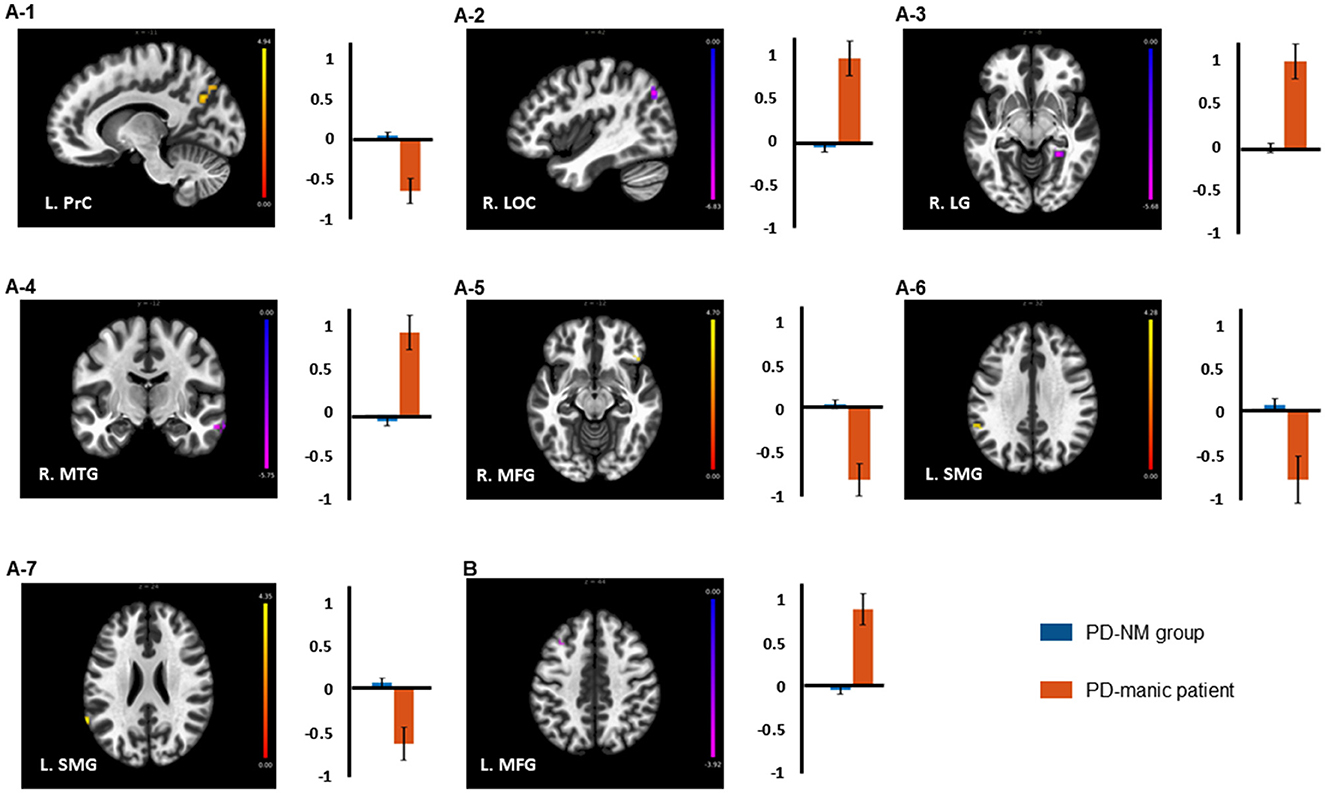
Figure 1. Brain regions revealed a significant difference in resting-state functional connectivity with (A) left and (B) right amygdala seed between the PD-NM and PD-manic groups. Error bars indicate the standard errors of the mean. L, left; R, right; PrC, precuneous cortex; MFG, Middle frontal gyrus; SMG, supramarginal Gyrus; LOC, lateral occipital cortex; LG, right lingual gyrus; MTG, middle temporal gyrus.
The relative HC and PD-NM groups revealed no suprathreshold differences in ROI-to-ROI analysis, considering both the amygdala (AAL41 & 42) and identified brain regions in the seed-based analysis as seed ROIs. However, PD-manic patients revealed lower rsFC from the left amygdala in the ROI of the two ROI in left SMG (t51 = −3.36, pFDR = 0.001; t51 = −3.88, pFDR < 0.001), right FOC (t51 = −6.45, pFDR < 0.001), and left PrC (t51 = −3.74, pFDR = 0.001) and higher rsFC in the right LOC (t51 = 5.95, pFDR < 0.001), right MTG (t51 = 5.37, pFDR < 0.001), right LG (t51 = 6.94, pFDR < 0.001), and left MTG (t51 = 4.73, pFDR 0.001) compared to the HC group.
In summary, the primary differences between the PD-manic patient and the PD-NM group were predominantly observed in the left amygdala-based rsFC. Additionally, an exploratory comparison analysis of the significant clusters revealed that the ROI-to-ROI connectivity between these clusters was significant only when comparing the healthy control (HC) group to the PD-manic patient, and not when comparing the HC group to the PD-NM group.
We investigated the differences in amygdala-based rsFC between the patient with PD who developed mania during treatment and those who did not. Our findings indicate that, in the case of antidepressant-induced mania, left amygdala-based rsFC was lower in the left PrC, right MFG, and left SMG, and higher in the right LOC, right LG, and right MTG when compared to PD patients without mania. Additionally, right amygdala-based rsFC exhibited a stronger association with the left MTG in the PD-manic patient than in the PD-NM group. Furthermore, connectivity associated with significant clusters between the PD-manic patient and PD-NM groups differed from that of the HCs only in the patient with the PD-manic patient and not in the PD-NM group. The implications of these results are discussed below.
We identified reduced L. amygdala–L. PrC connectivity in the PD-manic group compared with the PD-NM group. The PrC is an important region associated with the DMN (65). Changes in functional connectivity between amygdala and DMN have been reported to vary by mood state; decrease in manic or hypomanic mood episodes (31) and increase in depressive episodes (32). The HADS-depression subscale scores of the PD-manic patient and the PD-NM group suggest that both the PD-NM group and the PD-manic patient were experiencing mild depression even though they did not meet the diagnostic criteria for major depressive disorder, which is consistent with findings from general clinical studies (66). Furthermore, although statistical analysis was not possible due to sample size, characteristics related to anxiety and depression in the PD-manic patient were within the 1 SD distribution of the PD-NM group. Consequently, it is notable that the increased rsFC between amygdala-DMN, reported in BD for (hypo)manic mood rather than depression or euthymic mood, was observed in the patient with PD-mania.
In a euthymic state or depressive episode, there is increased functional connectivity between the amygdala and the DMN (28, 32). Additionally, increased rsFC between the amygdala and the DMN has also been reported in patients with PD (53). However, reductions in fractional anisotropy have been observed in several white matter tracts in the bipolar group, including the cingulum bundle connecting the amygdala to the posterior cingulate cortex (PCC), a key region of the DMN (67). Moreover, the previous finding that reduced structural connectivity between the amygdala and DMN was observed in both BD patients and unaffected first-degree relatives suggests that decreased rsFC between the amygdala and DMN could be specific to BD (68). Consequently, the reduced L. amygdala–L. PrC in patients with PD before antidepressant treatment may be a more specific biomarker for the risk of antidepressant-induced mania.
Reduced functional connectivity between the L. amygdala, R. MFG, and L. SMG was observed in the PD-manic group compared with the PD-NM group. In contrast, the functional connectivity between the R. amygdala-L. MFG was increased in the PD-manic group compared to the PD-NM group. Additionally, this trend of results was consistent in the exploratory comparison between the HC group and the PD-manic patient, while no significant difference was found between the PD-NM group and the HC group. The SMG and MFG are crucial nodes of the FPN (69). Alterations in rsFC between the amygdala and FPN have been reported in patients with BD (70). These findings were also replicated in a recent study which reported decreased connectivity between the amygdala and inferior frontal regions associated with the FPN in BD with (hypo) mania (28). In patients with PD, the FC between the amygdala and FPN was also decreased when exposed to emotional facial stimuli (71). Moreover, a previous study investigating rsFC following the process of fear extinction, a key component of exposure therapy used to treat panic disorder (72), reported a positive correlation between amygdala-FPN connectivity and the magnitude of fear extinction recall in healthy participants. In contrast, patients with panic disorder exhibited weaker amygdala-FPN connectivity (73). Although the comparison with healthy controls in each disease showed the same direction, to our knowledge, no studies comparing the two disease groups and no studies observing decreased rsFC in patients with PD compared to healthy controls have been identified. Therefore, our finding of decreased connectivity between the L. amygdala and FPN-related clusters in the PD-manic patient compared to the PD-NM group presents a novel result and suggests, for the first time, the possibility that relatively increased amygdala-FPN connectivity in patients with PD may reflect susceptibility to antidepressant-induced mania. Furthermore, our results, which revealed no difference in the exploratory comparison between the PD-NM and HC groups, also support the possibility that these connections could be clinically helpful.
As decreased connectivity between the amygdala and the FPN has been reported in both BD and PD compared to HC, our finding of a significant difference in the PD-manic patient needs to be viewed in the context of clinical presentation. Decreased amygdala-FPN connectivity has been linked to response inhibition (74), which may contribute to disinhibited behavior in patients with BD and their first-degree relatives (75). Moreover, previous studies concerning patients with PD suggested that decreased FC between the amygdala and FPN may play a role in the impaired fear extinction process observed in panic disorder (73). Thus, the lack of significant differences in the PD-NM group from the HC group in our exploratory analysis suggests that the alteration of rsFC between the amygdala and FPN in bipolar may differ from that in PD. It would be clinically valuable if these differences in connectivity could be confirmed by clinically observable differences in behavior, such as abnormalities in response inhibition or fear extinction reported in previous studies. However, larger studies focusing on subregions of the amygdala and FPN and anxiety behaviors are needed to examine these differences directly.
To our knowledge, there have been no reports on the asymmetric nature of the left and right amygdala-based rsFC in patients with BD. A previous study investigating the asymmetry of the left and right amygdala-based rsFC in healthy individuals reported distinct connectivity patterns and a more prominent right amygdala-based rsFC (76). Furthermore, decreases in amygdala-based rsFC in anxiety-related disorders, such as obsessive-compulsive and social anxiety disorders, have been reported only on the left side (77, 78). In task-based fMRI studies, the right amygdala is reportedly more involved in the automatic processing of environmental stimuli, and the left amygdala is more Involved in the continuous assessment of potential threats (79–82). Therefore, the increase in the right amygdala-based rsFC may reflect an increased response to external stimuli rather than anxiety. Increased response to external stimuli is also a repeatedly reported clinical feature in patients with BD (83). Therefore, the increased rsFC between the right amygdala and left MFG in the PD-manic group before a manic episode is an interesting finding that could reflect the clinical features of patients with BD. However, as we identified data from a single case, caution should be exercised when interpreting this previously unidentified finding.
The PD-manic patient revealed stronger rsFC between the L. amygdala–R. LG, R, MTG, R.LOC and R. amygdala–L. MTG than the PD-NM group. The LG, MTG, and LOC are known to be involved in visual processing (84, 85). Previous findings related to the rsFC of these regions have not been investigated in patients with BD or PD. The connectivity of the visual processing network and the amygdala has been investigated in studies utilizing the visual identification of facial expressions in emotional tasks rather than in the resting state (86, 87). These findings may reflect problems with emotional processing (88). Given that problems with emotional processes in patients with BD are also seen in residual symptoms or euthymic states (89, 90)our results may reflect these traits in patients with BD. However, this interpretation should be taken cautiously, as we demonstrated functional connectivity in only one patient. Further studies on amygdala connectivity in the visual processing network are required.
Our study had several limitations that constrain its interpretations. First, this study characterized one unexpected case in a longitudinal study; therefore, the altered amygdala-based functional connectivity discovered in this study cannot be generalized to patients with PD concerning antidepressant induced mania. However, we conducted an exploratory comparison with the HC group to support the specificity of our results and obtained results consistent with our hypotheses. Second, we did not control for the type and dose of medication. As different classes of antidepressants vary in the risk associated with antidepressant induced mania, this may be a confounding factor; thus, our results should be interpreted with caution (91). However, the patients in this study were prescribed either serotonin-norepinephrine reuptake inhibitors or selective serotonin reuptake inhibitors at baseline, which have been reported to have a relatively similar risk of antidepressant-induced mania (91). Third, the study was not designed for antidepressant induced mania; therefore, information such as YMRS scores at baseline was unavailable. The eligibility criteria ensured that participants did not experience mania before participation; however, information on the clinical features associated with mania was limited. Fourth, as this is a single-case study and the analysis was focused on the amygdala to reduce the problem of multiple comparisons, the results are not necessarily informative about overall brain connectivity. To identify biomarkers associated with antidepressant-induced mania, a multicenter cohort study with a large enough number of cases to achieve statistical significance is needed. Given the comorbidity of anxiety and depression, multimodality studies that include comprehensive clinical features and genetic information should be conducted.
According to our findings, altered rsFC between the amygdala-DMN and amygdala-FPN, which has been reported in (hypo)manic episodes of BD, was observed both in patients with PD and HCs without mania. Additionally, differences in rsFC related to the visual processing network were identified, which have not been reported in previous studies. This study provides preliminary evidence and considerations for the future use of amygdala-based rsFC as a biomarker of antidepressant-induced mania in treating patients with PD. Further studies with larger cohorts and different cases are required to verify clinical relevance of our findings. However, given the possible practical benefits of our discovery, we believe that this study will excite both professionals and scholars.
The boilerplate text of “2.5 Preprocessing” was automatically generated by fMRIPrep with the express intention that users should copy and paste this text into their manuscripts unchanged. It was released under the CC0 license.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the local Ethics Committee of Korea University Guro Hospital. The patients/participants provided their written informed consent to participate in this study.
Conceptualization, formal analysis, and writing—original draft preparation: B-HK and JK. Participant evaluation and data acquisition: S-HK, CH, H-GJ, and M-SL. Writing—review and editing and supervision: JK. All authors contributed to the article and approved the submitted manuscript.
This research was supported by the Bio & Medical Technology Development Program of the National Research Foundation (NRF) and funded by the Korean government (MSIT) (NRF-2021R1I1A1A01046025).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
PD, Panic disorder; BD, bipolar disorder; fMRI, functional magnetic resonance imaging; rs-fMRI, resting-state fMRI; BOLD, blood oxygen level-dependent; DMN, default mode network; rsFC, resting-state functional connectivity; YMRS, Young mania rating scale; LSAS, Liebowitz Social Anxiety Scale Self-Report Version; HADS, Hospital Anxiety and Depression Scale; TR, repetition time; TE, echo time; FOV, field of view; T1w, T1-weighted; CSF, cerebrospinal fluid; WM, white-matter; FD, framewise displacement; AAL2, automated anatomical labeling; FWE, family-wise-error-corrected; ROIs, regions of interest; FDR, false-discovery-rate; PrC, precuneous cortex; MFG, Middle Frontal Gyrus; SMG, supramarginal Gyrus; LOC, lateral occipital cortex; LG, right lingual gyrus; MTG, middle temporal gyrus; MNI, Montreal neurological institute; HC, healthy control.
1. Locke Ab, Kirst N, Shultz CG. Diagnosis and management of generalized anxiety disorder and panic disorder in adults. Am Fam Physician. (2015) 91:617–24.
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA, US. (2013). doi: 10.1176/appi.books.9780890425596
3. Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, Wittchen HU. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int J Methods Psychiatr Res. (2012) 21:169–84. doi: 10.1002/MPR.1359
4. Bighelli I, Castellazzi M, Cipriani A, Girlanda F, Guaiana G, Koesters M, et al. Antidepressants versus placebo for panic disorder in adults. Cochrane Database of Syst Rev. (2018) 2018:6. doi: 10.1002/14651858.CD010676.PUB2/MEDIA/CDSR/CD010676/IMAGE_N/NCD010676-CMP-006-01.PNG
5. Goldberg JF, Truman CJ. Antidepressant-induced mania: an overview of current controversies. Bipolar Disord. (2003) 5:407–20. doi: 10.1046/J.1399-5618.2003.00067.X
6. Frye MA, McElroy SL, Prieto ML, Harper KL, Walker DL, Kung S, et al. Clinical risk factors and serotonin transporter gene variants associated with antidepressant-induced mania. J Clin Psychiatry. (2015) 76:2941. doi: 10.4088/JCP.14M09127
7. Biernacka JM, McElroy SL, Crow S, Sharp A, Benitez J, Veldic M, et al. Pharmacogenomics of antidepressant induced mania: A review and meta-analysis of the serotonin transporter gene. (5HTTLPR) association. J Affect Disord. (2012) 136:e21–9. doi: 10.1016/J.JAD.2011.05.038
8. Provencher MD, Guimond AJ, Hawke LD. Comorbid anxiety in bipolar spectrum disorders: a neglected research and treatment issue? J Affect Disord. (2012) 137:161–4. doi: 10.1016/J.JAD.2011.12.001
9. Freeman MP, Freeman SA, McElroy SL. The comorbidity of bipolar and anxiety disorders: prevalence, psychobiology, and treatment issues. J Affect Disord. (2002) 68:1–23. doi: 10.1016/S0165-0327(00)00299-8
10. Schaffer A, McIntosh D, Goldstein BI, Rector NA, McIntyre RS, Beaulieu S, et al. The CANMAT task force recommendations for the management of patients with mood disorders and comorbid anxiety disorders. Ann Clin Psychiatry. (2012) 24:6–22.
11. Nabavi B, Mitchell AJ, Nutt D. A lifetime prevalence of comorbidity between bipolar affective disorder and anxiety disorders: a meta-analysis of 52 interview-based studies of psychiatric population. EBioMedicine. (2015) 2:1405–19. doi: 10.1016/J.EBIOM.2015.09.006
12. Spoorthy MS, Chakrabarti S, Grover S. Comorbidity of bipolar and anxiety disorders: An overview of trends in research. World J Psychiatry. (2019) 9:7. doi: 10.5498/WJP.V9.I1.7
13. Tanaka M, Szabó Á, Vécsei L. Integrating armchair, bench, and bedside research for behavioral neurology and neuropsychiatry: editorial. Biomedicines. (2022) 10:2999. doi: 10.3390/BIOMEDICINES10122999
14. Battaglia S, Di Fazio C, Vicario CM, Avenanti A. Neuropharmacological Modulation of N-methyl-D-aspartate, noradrenaline and endocannabinoid receptors in fear extinction learning: synaptic transmission and plasticity. Int J Mol Sci. (2023) 24:5926. doi: 10.3390/IJMS24065926
15. Perlis RH, Brown E, Baker RW, Nierenberg AA. Clinical features of bipolar depression versus major depressive disorder in large multicenter trials. Am J Psychiatry. (2006) 163:225–31. doi: 10.1176/APPI.AJP.163.2.225/ASSET/IMAGES/LARGE/Q113F3.JPEG
16. Ratheesh A, Davey C, Hetrick S, Alvarez-Jimenez M, Voutier C, Bechdolf A, et al. A systematic review and meta-analysis of prospective transition from major depression to bipolar disorder. Acta Psychiatr Scand. (2017) 135:273–284. doi: 10.1111/ACPS.12686
17. Zimmermann P, Brückl T, Nocon A, Pfister H, Lieb R, Wittchen HU, et al. Heterogeneity of DSM-IV major depressive disorder as a consequence of subthreshold bipolarity. Arch Gen Psychiatry. (2009) 66:1341–52. doi: 10.1001/ARCHGENPSYCHIATRY.2009.158
18. Pavlova B, Perlis RH, Alda M, Uher R. Lifetime prevalence of anxiety disorders in people with bipolar disorder: a systematic review and meta-analysis. Lancet Psychiatry. (2015) 2:710–7. doi: 10.1016/S2215-0366(15)00112-1
19. Psychiatry Psychiatry MZ-TCJ of, 2016 undefined. A review of 20 years of research on overdiagnosis and underdiagnosis in the Rhode Island Methods to Improve Diagnostic Assessment and Services (MIDAS). Can J Psychiatry. (2016) 61:71–79. doi: 10.1177/0706743715625935
20. Phillips ML, Swartz HA. A critical appraisal of neuroimaging studies of bipolar disorder: Toward a new conceptualization of underlying neural circuitry and a road map for future research. American Journal of Psychiatry. (2014) 171:829–43. doi: 10.1176/APPI.AJP.2014.13081008/ASSET/IMAGES/LARGE/829F2.JPEG
21. Tanaka M, Szabó Á, Spekker E, Polyák H, Tóth F, Vécsei L. Mitochondrial impairment: a common motif in neuropsychiatric presentation? The link to the tryptophan and kynurenine metabolic system. Cells. (2022) 11:2607. doi: 10.3390/CELLS11162607
22. Battaglia S, Nazzi C, Thayer JF. Fear-induced bradycardia in mental disorders: Foundations, current advances, future perspectives. Neurosci Biobehav Rev. (2023) 149:105163. doi: 10.1016/J.NEUBIOREV.2023.105163
23. Tanaka M, Tóth F, Polyák H, Szabó Á, Mándi Y, Vécsei L, Di Paola R. Immune influencers in action: metabolites and enzymes of the tryptophan-kynurenine metabolic pathway. Biomedicines. (2021) 9:734. doi: 10.3390/BIOMEDICINES9070734
24. Tanaka M, Toldi J, Vécsei L. Exploring the etiological links behind neurodegenerative diseases: inflammatory cytokines and bioactive kynurenines. Int J Mol Sci. (2020) 21:2431. doi: 10.3390/IJMS21072431
25. Waller J, Miao T, Ikedionwu I, Lin KK. Reviewing applications of structural and functional MRI for bipolar disorder. Jpn J Radiol. (2021) 39:414–23. doi: 10.1007/S11604-020-01074-5/TABLES/2
26. Nyatega CO, Qiang L, Adamu MJ, Younis A, Kawuwa HB. Altered dynamic functional connectivity of cuneus in schizophrenia patients: a resting-state fmri study. Applied Sciences. (2021) 11:11392. doi: 10.3390/APP112311392/S1
27. Fox MD, Raichle ME. Spontaneous fluctuations in brain activity observed with functional magnetic resonance imaging. Nat Rev Neurosci. (2007) 8:700–711. doi: 10.1038/nrn2201
28. Claeys EHI, Mantingh T, Morrens M, Yalin N, Stokes PRA. Resting-state fMRI in depressive and. (hypo)manic mood states in bipolar disorders: a systematic review. Prog Neuropsychopharmacol Biol Psychiatry. (2022) 113:110465. doi: 10.1016/J.PNPBP.2021.110465
29. Okanda Nyatega C, Qiang L, Jajere Adamu M, Bello Kawuwa H. Altered striatal functional connectivity and structural dysconnectivity in individuals with bipolar disorder: a resting state magnetic resonance imaging study. Front Psychiatry. (2022) 13:2555. doi: 10.3389/FPSYT.2022.1054380/BIBTEX
30. Syan SK, Smith M, Frey BN, Remtulla R, Kapczinski F, Hall GBC, Minuzzi L. Resting-state functional connectivity in individuals with bipolar disorder during clinical remission: a systematic review. J Psychiatry Neurosci. (2018) 43:298–316. doi: 10.1503/JPN.170175
31. Thomas LA, Brotman MA, Bones BL, Chen G, Rosen BH, Pine DS, Leibenluft E. Neural circuitry of masked emotional face processing in youth with bipolar disorder, severe mood dysregulation, and healthy volunteers. Dev Cogn Neurosci. (2014) 8:110–20. doi: 10.1016/J.DCN.2013.09.007
32. Favre P, Baciu M, Pichat C, Bougerol T, Polosan M. fMRI evidence for abnormal resting-state functional connectivity in euthymic bipolar patients. J Affect Disord. (2014) 165:182–9. doi: 10.1016/J.JAD.2014.04.054
33. Baur V, Hänggi J, Langer N, Jäncke L. Resting-state functional and structural connectivity within an Insula–Amygdala route specifically index state and trait anxiety. Biol Psychiatry. (2013) 73:85–92. doi: 10.1016/J.BIOPSYCH.2012.06.003
34. Battaglia S, Harrison BJ, Fullana MA. Does the human ventromedial prefrontal cortex support fear learning, fear extinction or both? A commentary on subregional contributions. Mol Psychiatry. (2021) 27:784–786. doi: 10.1038/s41380-021-01326-4
35. Kim BH, Kim JJ, Oh J, Kim SH, Han C, Jeong HG, Lee MS, Kim J. Feasibility of the virtual reality-based assessments in patients with panic disorder. Front Psychiatry. (2023) 14:40. doi: 10.3389/FPSYT.2023.1084255/BIBTEX
36. Lecrubier Y, Sheehan DV, Weiller E, Amorim P, Bonora I, Sheehan K, et al. The mini international neuropsychiatric interview. (MINI). A short diagnostic structured interview: reliability and validity according to the CIDI. Eur Psychiatry. (1997) 12:224–231. doi: 10.1016/S0924-9338(97)83296-8
37. Jung-Bum Kim. Development of the Korean version of the panic disorder severity scale. Kor J Psychopathol. (2001) 10:140–51.
38. Furukawa TA, Katherine Shear M, Barlow DH, Gorman JM, Woods SW, Money R, Etschel E, Engel RR, Leucht S. Evidence-based guidelines for interpretation of the panic disorder severity scale. Depress Anxiety. (2009) 26:922–9. doi: 10.1002/da.20532
39. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. (1983) 67:361–370.
40. First MB, Williams JBW, Karg RS, Spitzer RL. Structured Clinical Interview for DSM-5 Disorders: SCID-5-CV Clinician Version. Washington, DC: American Psychiatric Association Publishing (2016).
41. Jin Hwa Kang, Jung Ae Lee, Kang Seob Oh, Se Won Lim. Validation and clinical efficacy of the Korean liebowitz social anxiety scale: clinician administered. Kor J Clin Psychol. (2013) 32:291–312.
42. Lee B, Kim YE. The psychometric properties of the generalized anxiety disorder scale. (GAD-7) among Korean university students. Psychiatry Clin Psychopharmacol. (2019) 29:864–71.
43. OH S-M, MIN K-J, PARK D-B. A study on the standardization of the hospital anxiety and depression scale for koreans: a comparison of normal, depressed and anxious groups. J Kor Neuropsychiatric Assoc. (1999) 3:289–96.
44. Jung HY, Cho HS, Joo YH, Shin HK, Yi JS, Hwang S, et al. A validation study of the korean-version of the young mania rating scale. J Kor Neuropsychiatric Assoc. (2003) 3:263–9.
45. Esteban O, Markiewicz CJ, Blair RW, Moodie CA, Isik AI, Erramuzpe A, et al. fMRIPrep: a robust preprocessing pipeline for functional MRI. Nat Methods. (2018) 16:111–116. doi: 10.1038/s41592-018-0235-4
46. Gorgolewski K, Burns CD, Madison C, Clark D, Halchenko YO, Waskom ML, Ghosh SS. Nipype: A flexible, lightweight and extensible neuroimaging data processing framework in Python. Front Neuroinform. (2011) 5:13. doi: 10.3389/FNINF.2011.00013/ABSTRACT
47. Esteban O, Markiewicz CJ, Burns C, Goncalves M, Jarecka D, Ziegler E, et al. nipy/nipype: 1.8.3. (2022) doi: 10.5281/ZENODO.6834519
48. Tustison NJ, Avants BB, Cook PA, Zheng Y, Egan A, Yushkevich PA, Gee JC. N4ITK: Improved N3 bias correction. IEEE Trans Med Imaging. (2010) 29:1310–20. doi: 10.1109/TMI.2010.2046908
49. Avants BB, Epstein CL, Grossman M, Gee JC. Symmetric diffeomorphic image registration with cross-correlation: evaluating automated labeling of elderly and neurodegenerative brain. Med Image Anal. (2008) 12:26–41. doi: 10.1016/J.MEDIA.2007.06.004
50. Zhang Y, Brady M, Smith S. Segmentation of brain MR images through a hidden Markov random field model and the expectation-maximization algorithm. IEEE Trans Med Imaging. (2001) 20:45–57. doi: 10.1109/42.906424
51. Reuter M, Rosas HD, Fischl B. Highly accurate inverse consistent registration: a robust approach. Neuroimage. (2010) 53:1181–1196. doi: 10.1016/J.NEUROIMAGE.2010.07.020
52. Fonov V, Evans A, McKinstry R, Almli C, Collins D. Unbiased nonlinear average age-appropriate brain templates from birth to adulthood. Neuroimage. (2009) 47:S102. doi: 10.1016/S1053-8119(09)70884-5
53. Jenkinson M, Bannister P, Brady M, Smith S. Improved optimization for the robust and accurate linear registration and motion correction of brain images. Neuroimage. (2002) 17:825–41. doi: 10.1006/NIMG.2002.1132
54. Jenkinson M, Smith S. A global optimisation method for robust affine registration of brain images. Med Image Anal. (2001) 5:143–56. doi: 10.1016/S1361-8415(01)00036-6
55. Greve DN, Fischl B. Accurate and robust brain image alignment using boundary-based registration. Neuroimage. (2009) 48:63–72. doi: 10.1016/J.NEUROIMAGE.2009.06.060
56. Power JD, Mitra A, Laumann TO, Snyder AZ, Schlaggar BL, Petersen SE. Methods to detect, characterize, and remove motion artifact in resting state fMRI. Neuroimage. (2014) 84:320–41. doi: 10.1016/J.NEUROIMAGE.2013.08.048
57. Behzadi Y, Restom K, Liau J, Liu TT. A component based noise correction method. (CompCor) for BOLD and perfusion based fMRI. Neuroimage. (2007) 37:90–101. doi: 10.1016/J.NEUROIMAGE.2007.04.042
58. Satterthwaite TD, Elliott MA, Gerraty RT, Ruparel K, Loughead J, Calkins ME, et al. An improved framework for confound regression and filtering for control of motion artifact in the preprocessing of resting-state functional connectivity data. Neuroimage. (2013) 64:240–56. doi: 10.1016/J.NEUROIMAGE.2012.08.052
59. Lanczos C. Evaluation of noisy data. J Soc Indust Appl Math Series B: Num Anal. (2006) 1:76–85. doi: 10.1137/0701007
60. Rolls ET, Joliot M, Tzourio-Mazoyer N. Implementation of a new parcellation of the orbitofrontal cortex in the automated anatomical labeling atlas. Neuroimage. (2015) 122:1–5. doi: 10.1016/J.NEUROIMAGE.2015.07.075
61. Eickhoff SB, Bzdok D, Laird AR, Kurth F, Fox PT. Activation likelihood estimation meta-analysis revisited. Neuroimage. (2012) 59:2349–61. doi: 10.1016/J.NEUROIMAGE.2011.09.017
62. Wu Y, Zhong Y, Zheng G, Liu Y, Pang M, Xu H, et al. Disrupted fronto-temporal function in panic disorder: a resting-state connectome study. Brain Imaging Behav. (2022) 16:888–98. doi: 10.1007/S11682-021-00563-Z/FIGURES/3
63. Ni MF, Zhang BW, Chang Y, Huang XF, Wang XM. Altered resting-state network connectivity in panic disorder: an independent Component analysis. Brain Imaging Behav. (2021) 15:1313–22. doi: 10.1007/S11682-020-00329-Z/FIGURES/3
64. Whitfield-Gabrieli S, Nieto-Castanon A. Conn: a functional connectivity toolbox for correlated and anticorrelated brain networks. Brain Connect. (2012) 2:125–41. doi: 10.1089/BRAIN.2012.0073
65. Buckner RL, Andrews-Hanna JR, Schacter DL. The Brain's Default Network. Ann N Y Acad Sci. (2008) 1124:1–38. doi: 10.1196/ANNALS.1440.011
66. Forstner AJ, Awasthi S, Wolf C, Maron E, Erhardt A, Czamara D, et al. Genome-wide association study of panic disorder reveals genetic overlap with neuroticism and depression. Mol Psychiatry. (2019) 26:4179–90. doi: 10.1038/s41380-019-0590-2
67. Emsell L, Leemans A, Langan C, Van Hecke W, Barker GJ, McCarthy P, et al. Limbic and callosal white matter changes in euthymic bipolar i disorder: an advanced diffusion magnetic resonance imaging tractography study. Biol Psychiatry. (2013) 73:194–201. doi: 10.1016/J.BIOPSYCH.2012.09.023
68. Chaddock C, Barker GJ, Marshall N, Schulze K, Hall MH, Fern A, et al. White matter microstructural impairments and genetic liability to familial bipolar I disorder. Br J Psychiatry. (2009) 194:527534. doi: 10.1192/BJP.BP.107.047498
69. Picó-Pérez M, Radua J, Steward T, Menchón JM, Soriano-Mas C. Emotion regulation in mood and anxiety disorders: a meta-analysis of fMRI cognitive reappraisal studies. Prog Neuropsychopharmacol Biol Psychiatry. (2017) 79:96–104. doi: 10.1016/J.PNPBP.2017.06.001
70. Chepenik LG, Raffo M, Hampson M, Lacadie C, Wang F, Jones MM, Pittman B, Skudlarski P, Blumberg HP. Functional connectivity between ventral prefrontal cortex and amygdala at low frequency in the resting state in bipolar disorder. Psychiatry Res Neuroimagg. (2010) 182:207–10. doi: 10.1016/J.PSCYCHRESNS.2010.04.002
71. Bjorkquist OA, Olsen EK, Nelson BD, Herbener ES. Altered amygdala-prefrontal connectivity during emotion perception in schizophrenia. Schizophr Res. (2016) 175:35–41. doi: 10.1016/J.SCHRES.2016.04.003
72. Marin MF, Zsido RG, Song H, Lasko NB, Killgore WDS, Rauch SL, Simon NM, Milad MR. Skin conductance responses and neural activations during fear conditioning and extinction recall across anxiety disorders. JAMA Psychiatry. (2017) 74:622–631. doi: 10.1001/jamapsychiatry.2017.0329
73. Feng P, Zheng Y, Feng T. Resting-state functional connectivity between amygdala and the ventromedial prefrontal cortex following fear reminder predicts fear extinction. Soc Cogn Affect Neurosci. (2016) 11:991–1001. doi: 10.1093/SCAN/NSW031
74. Clauss JA, Avery SN, Blackford JU. The nature of individual differences in inhibited temperament and risk for psychiatric disease: A review and meta-analysis. Prog Neurobiol. (2015) 127–28:23–45. doi: 10.1016/J.PNEUROBIO.2015.03.001
75. Hidiroglu C, Torres IJ, Er A, Işik G, Yalin N, Yatham LN, Ceylan D, Özerdem A. Response inhibition and interference control in patients with bipolar I disorder and first-degree relatives. Bipolar Disord. (2015) 17:781–94. doi: 10.1111/BDI.12335
76. Tetereva AO, Balaev VV. Kartashov SI, Ushakov VL, Ivanitsky AM, Martynova OV. Asymmetry of amygdala resting-state functional connectivity in healthy human brain. Neuroreport. (2020) 31:17–21. doi: 10.1097/WNR.0000000000001353
77. Rus OG, Reess TJ, Wagner G, Zimmer C, Zaudig M, Koch K. Functional and structural connectivity of the amygdala in obsessive-compulsive disorder. Neuroimage Clin. (2017) 13:246–55. doi: 10.1016/J.NICL.2016.12.007
78. Prater KE, Hosanagar A, Klumpp H, Angstadt M, Phan KL. Aberrant amygdala-frontal cortex connectivity during perception of fearful faces and at rest in generalized social anxiety disorder. Depress Anxiety. (2013) 30:234–41. doi: 10.1002/DA.22014
79. Phelps EA. Emotion and cognition: insights from studies of the human amygdala. Annu Rev Psychol. (2005) 57:27–53. doi: 10.1146/ANNUREV.PSYCH.56.091103.070234
80. Baeken C, Marinazzo D, Van Schuerbeek P, Wu GR, De Mey J, Luypaert R, et al. Left and right amygdala - mediofrontal cortical functional connectivity is differentially modulated by harm avoidance. PLoS ONE. (2014) 9:e95740. doi: 10.1371/JOURNAL.PONE.0095740
81. Phan KL, Wager T, Taylor SF, Liberzon I. Functional neuroanatomy of emotion: a meta-analysis of emotion activation studies in PET and fMRI. Neuroimage. (2002) 16:331–48. doi: 10.1006/NIMG.2002.1087
82. Costafreda SG, Brammer MJ, David AS, Fu CHY. Predictors of amygdala activation during the processing of emotional stimuli: a meta-analysis of 385 PET and fMRI studies. Brain Res Rev. (2008) 58:57–70. doi: 10.1016/J.BRAINRESREV.2007.10.012
83. McIntyre RS, Alda M, Baldessarini RJ, Bauer M, Berk M, Correll CU, et al. The clinical characterization of the adult patient with bipolar disorder aimed at personalization of management. World Psychiatry. (2022) 21:364–87. doi: 10.1002/WPS.20997
84. Park HJ, Friston K. Structural and functional brain networks: from connections to cognition. Science. (2013) 342:11. doi: 10.1126/SCIENCE.1238411/ASSET/C8A581FE-33ED-405E-B2C2-AFA912B9F016/ASSETS/GRAPHIC/342_1238411_F4.JPEG
85. Wu Z, Sabel BA. Spacetime in the brain: rapid brain network reorganization in visual processing and recovery. Scient Rep. (2021) 11:1–12. doi: 10.1038/s41598-021-96971-8
86. Sabatinelli D, Fortune EE, Li Q, Siddiqui A, Krafft C, Oliver WT, et al. Emotional perception: Meta-analyses of face and natural scene processing. Neuroimage. (2011) 54:2524–33. doi: 10.1016/J.NEUROIMAGE.2010.10.011
87. Sun S, Yu H, Yu R, Wang S. Functional connectivity between the amygdala and prefrontal cortex underlies processing of emotion ambiguity. bioRxiv. (2023) 3:116. doi: 10.1101/2023.01.24.525116
88. Pessoa L, Adolphs R. Emotion processing and the amygdala: from a “low road” to “many roads” of evaluating biological significance. Nat Rev Neurosci. (2010) 11:773–82. doi: 10.1038/nrn2920
89. Miola A, Cattarinussi G, Antiga G, Caiolo S, Solmi M, Sambataro F. Difficulties in emotion regulation in bipolar disorder: a systematic review and meta-analysis. J Affect Disord. (2022) 302:352–60. doi: 10.1016/J.JAD.2022.01.102
90. Kurtz M, Mohring P, Förster K, Bauer M, Kanske P. Deficits in explicit emotion regulation in bipolar disorder: a systematic review. Int J Bipolar Disord. (2021) 9:1–23. doi: 10.1186/S40345-021-00221-9/TABLES/6
91. Viktorin A, Lichtenstein P, Thase ME, Larsson H, Lundholm C, Magnusson PKE, et al. The risk of switch to mania in patients with bipolar disorder during treatment with an antidepressant alone and in combination with a mood stabilizer. Am J Psychiatry. (2014) 171:1067–1073. doi: 10.1176/APPI.AJP.2014.13111501/ASSET/IMAGES/LARGE/1067F1.JPEG
Keywords: panic disorder, bipolar disorder, resting-state functional connectivity, amygdala, default mode network, frontoparietal network, biomarkers, antidepressant induced mania
Citation: Kim B-H, Kim S-H, Han C, Jeong H-G, Lee M-S and Kim J (2023) Antidepressant-induced mania in panic disorder: a single-case study of clinical and functional connectivity characteristics. Front. Psychiatry 14:1205126. doi: 10.3389/fpsyt.2023.1205126
Received: 13 April 2023; Accepted: 09 May 2023;
Published: 25 May 2023.
Edited by:
Masaru Tanaka, University of Szeged (ELKH-SZTE), HungaryReviewed by:
Simone Battaglia, University of Bologna, ItalyCopyright © 2023 Kim, Kim, Han, Jeong, Lee and Kim. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Junhyung Kim, Y2FiaWxvdmVyQGtvcmVhLmFjLmty
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.