
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 13 July 2023
Sec. Social Psychiatry and Psychiatric Rehabilitation
Volume 14 - 2023 | https://doi.org/10.3389/fpsyt.2023.1200450
 Matthew E. Sprong1,2*
Matthew E. Sprong1,2* Heaven Hollender3
Heaven Hollender3 Yu-Sheng Lee4
Yu-Sheng Lee4 Lee Ann Rawlins Williams5
Lee Ann Rawlins Williams5 Zach Sneed6
Zach Sneed6 Amir Garakani7,8
Amir Garakani7,8 Frank D. Buono8
Frank D. Buono8Introduction: The purpose of the study was to investigate factors that influence vocational rehabilitation program enrollment and employment at discharge of veterans with psychiatric and co-occurring alcohol and other substance use disorders enrolled at a veteran health administration (VHA) medical center.
Methods: A sample of 2,550 veteran patients referred for VHA vocational rehabilitation between 2016 and 2021 were examined for the current study. The current study was classified as quality improvement/assurance, thus resulting in exempt research by the U.S. Department of Veteran Affairs Institutional Review Board.
Results: Veterans with active alcohol use disorders (AUDs) and co-occurring depression, anxiety, post-traumatic stress disorder, or bipolar disorders were less likely to be enrolled for vocational rehabilitation program services compared to those without these co-occurring diagnoses. Veterans with AUD (active & in-remission status combined into one category) and a diagnosis of anxiety were less likely to be employed at discharge compared to veterans with AUDs and no anxiety diagnosis (anxiety diagnosis – 3.5% vs. no anxiety diagnosis – 5.8%).
Discussion: VHA vocational rehabilitation can be an effective intervention to assist veterans in reintegrating back into the community. Yet, there appears to be some disparities in the program enrollment and employment at discharge, depending on the nature of the psychiatric diagnosis. Investigating the factors contributing (mediating or moderating) to these discrepancies are needed. Although it appears access is not the issue in being referred for vocational rehabilitation services, other factors are likely contributing to program entry.
The trajectory of substance use disorders (SUDs) is expected to rise in the United States (U.S.), and recent research examining 30 geographically-representative VA healthcare systems (6,000 Veteran patients) demonstrated alcohol as the most commonly reported substance (24% use in past 12 months, 11% daily use in past 3 months, with 10% meeting DSM-5 criteria for alcohol use disorder), followed by cannabis (42% lifetime use, 12% use in past 12 months, 5% daily use in past 3 months, 3% met DSM-5 criteria for cannabis use disorder) (1). With significant increases in mortality rates and high prevalence of substance use disorders (SUDs), the administration of President Joseph Biden and Vice-President Kamala Harris have taken action to allocate federal dollars in support of the prevention and reduction of substance abuse disorders (SUDs) (2). Such funding has: (a) allowed for the development of evidence-based interventions; and (b) enhanced service-delivery models by providing funding for additional peer supports and treatment expansion. An estimated 2.3 percent (481,000) of veterans are diagnosed with a mental illness and SUD (3). The literature demonstrates an increased risk of medical hospitalizations when these diagnoses co-occur (4). Evidence has shown that other issues emerging from co-occurring diagnoses, such as homelessness, unemployment, social exclusion, low self-efficacy in community reintegration and military-to-civilian transition, and self-esteem, which all impact quality of life (5).
Members of our armed forces put their lives on hold to protect and serve the U.S. Therefore, it is essential to provide mental health services to reduce the challenges associated with transitioning or return into civilian life. Prevalence rates have shown that 1 in 10 veterans are diagnosed with SUDs (6) and approximately 91% have gone without physical or psychological treatment in 2020 (3). Of the 1.1 million veterans living with a SUD, 25% struggle with illicit drug use and 80% struggle with alcohol use disorders (AUDs) (7). The Substance Abuse Mental Health Services Administration (SAMHSA) has indicated that the most common mental disorders seen in SUD treatment include anxiety and mood disorders, schizophrenia, bipolar disorder, major depressive disorder, conduct disorders, post-traumatic stress disorders, and attention deficit hyperactivity disorders (8). Current estimates show that 1 in 4 adults living with serious mental problems also has an issue with substance use (9). For veterans, mental health (MH) and co-occurring SUD diagnosis rates have been at 5.7% or 1.1 million (10).
Research has shown that in 2020, approximately 5.2 million veterans experienced a behavioral health condition and more than half with a psychiatric disorder did not receive treatment in the prior year (11). As previously mentioned, there are several factors that can impact independent living, quality of life, and having a sense of belonging when veterans have psychiatric diagnoses or SUDs (12, 13). Research has conclusively shown that employment is one factor that is lower for veterans with these diagnoses and combination of diagnoses, with these veterans having lower labor force participation (14–16). Within the Veteran Health Administration (VHA), all medical centers are required to have a vocational rehabilitation (VR) [referred to as Compensated Work Therapy] to improve vocational functioning and employment outcomes of Veterans (17).
VR is a method of assisting veterans to obtain the skills and tools needed to successfully secure and maintain competitive employment. A primary focus is on removing employment-related barriers for veterans that have difficulty obtaining or maintaining employment (18, 19). VHA VR programs are expected to adhere to VHA Policy Directive 1163.02, which was released on August 19, 2019. Prior research has shown that implementation of this policy did not impact program enrollment rates for veterans with SUDs, but veterans with AUDs were less likely to be enrolled prior to the implementation of VHA Policy Directive 1163 (18). This policy explicitly states the following: “no discriminatory practices are acceptable for Veterans with SUD or AUDs “regardless of duration of sobriety, routine vocational testing, or required time in a treatment program or clinical services prior to participation in VHA Vocational Rehabilitation” (p. 43). Additionally, under VHA Policy Directive 1163, all VHA medical facilities must offer two specialty programs within VHA VR including supported employment (SE) and transitional work (TW) (17).
SE is a program that serves two groupings of veterans, including: (1) veterans with serious mental illness or medical conditions (e.g., active psychosis, schizoaffective disorder, severe traumatic brain injury, blindness, spinal cord injury); and (2) veterans with significant employment issues as it relates to SUDs (e.g., attendance issues) are eligible for the SE program. Veterans enrolled in TW participate with work restoration services in actual work settings. The goal is to provide vocational supports and resources needed for successful transition to competitive employment. TW is for veterans that do not have a serious mental illness or medical condition as aforementioned but have significant employment related impairments. The Community Based Employment Services (CBES) program is optional for each VHA VR program, and accessible when made readily available. Veterans with mental health conditions or physical disabilities who have a history of sporadic employment, difficulty maintaining a job, or initiating and following through on their job search, or who require a range of supports to obtain or maintain competitive work, are eligible. However, veterans enrolled in these programs do not have the diagnoses as required to be eligible for SE, and have the knowledge, skills, and abilities to engage in competitive employment without the need of work restoration services (TW).
VR is a crucial component of the comprehensive care provided to veterans with and without disabilities, and eligibility for VHA VR includes (a) medically cleared to work and participate in the program, and (b) goal of obtaining competitive employment (17). The efficacy of including VR as a part of treatment has been well-supported in the successful recovery of veterans with SUDs (20–22). Through the provision of employment-related services, such as vocational evaluation, career counseling, and job training, VR helps veterans regain their independence and achieve meaningful employment. Research has shown that VR can significantly improve the employment outcomes of veterans. Bond and colleagues (23) noted veterans who participated in a VR program had a higher likelihood of finding employment and greater job satisfaction than those who did not participate in VR.
In addition to improving employment outcomes, VR can also enhance the mental health and well-being of veterans. By providing a sense of purpose and accomplishment, employment can help veterans to rebuild their self-esteem and self-confidence, and to reduce symptoms of depression and anxiety. Furthermore, vocational rehabilitation can help veterans to develop social connections and establish a sense of belonging within their communities. As reflected upon by the U.S. (17), employment is a critical component of a Veteran’s overall wellness and recovery, and VR plays an important key role in supporting successful reintegration into civilian life. Overall, vocational rehabilitation is a vital component of the care provided to veterans with psychiatric and/or medical disabilities. By improving employment outcomes and enhancing mental health and well-being, VR supports veterans to regain their independence and achieve meaningful lives.
The negative association between employment and psychiatric conditions and SUDs is well-documented, and research has shown that employment participation decreases as the symptoms of the conditions increase as psychiatric and SUD conditions can serve as a significant barrier. For example, after examining nearly 100,000 veterans, Zivin et al. (24) found that veterans with bipolar disorder, depression, post-traumatic stress disorder (PTSD), schizophrenia, or SUDs were more likely to be unemployed, have a disability or be retired than employed. Other studies have shown that veterans with SUD diagnoses or who were homeless at program entry were more likely to be employed at discharge, while receipt of public support income and severe mental illness decreased the inclusion in the competitive labor market (22, 25–28).
National databases connected with VHA VR have been examined to evaluate its efficacy in employment and healthcare outcomes, and research findings have shown improvement in employment obtainment and retention (22) and lower healthcare needs (e.g., fewer visits in VHA vocational rehabilitation, outpatient mental health, homelessness program, and medical hospitalizations) post-discharge (25). However, the co-occurring/co-morbid nature of having both a psychiatric and SUD diagnosis concurrently lowers participation in competitive employment (29). Other non-veteran related research has shown that employment is a strong predictor of SUD treatment compliance and continued abstinence post-discharge (30).
Despite the evidence showing how psychiatric and SUD/AUD diagnoses can impact a veteran’s independent functioning and psychological well-being, the purpose of this study was to focus on the impact of having these diagnoses as they co-occur in terms of how it effects VHA vocational rehabilitation program enrollment and employment at discharge. Studies have shown that employment at discharge decreases when a veteran presents a SUD/AUD diagnosis or a mental health condition (18, 19), but there is limited research examining the impact when both co-occur for veterans enrolled in VR within the VA healthcare system.
The Institutional Review Board (IRB) for the U.S. Department of Veteran Affairs indicated that this was a retrospective and quality assurance study, and therefore no approval (exempt) was needed if no identifying information was released for publication. The co-author’s university granted additional IRB endorsement (approval #13460) as exempt status to verify that institutional support was provided for the current study. The current study included data from a VHA VR program located within VISN-12 and accounted for veterans referred for services between 2016 and 2020. All veteran information was recorded by VR counselors in an access database that was used for programmatic evaluation (e.g., gender, race, homelessness status). It is possible that this data were entered incorrectly (data input errors), and to verify the data’s accuracy, the primary author used the U.S. Department of Veteran Affairs’ Computerized Patient Record System (CPRS) and Joint Legacy Viewer (JLV) – includes data from medical care at other VA medical facilities across the country if applicable, and a search through CPRS progress notes and consults. The database used during the intake interview did not account for the durational period of last SUD/AUD usage (active, early remission, sustained remission) nor psychiatric diagnoses per the DSM 5 TR. Therefore, information was collected from CPRS and JLV to properly code the diagnoses (e.g., early remission from AUD or SUD is 3–12 months post last use). Lab testing was used to verify last usage per the urine drug screening criteria.
The DSM 5-TR classifies SUD into three categories (active usage, early remission, sustained remission) to provide details on the severity of the disorder (31). Researchers examining employment challenges for Veterans have generally combined all drug and alcohol related diagnoses into one category (29, 32), without differentiating whether the diagnoses are in remission or an active problem (18, 19). In the current study, it was intended to (1) evaluate program enrollment rates and employment rates at discharge by only differentiating between SUD or AUD and no SUD or AUD, and (2) separating SUD and AUD into none, active usage, early remission, and sustained remission. Due to low frequencies within early remission and sustained remission, the variable was condensed into no usage, active usage, and inactive usage (sustained and early remission SUD and AUD). Prior literature has shown that veterans with psychiatric disorders experience significant employment-related barriers (22). Therefore, psychiatric disorders was used as the other predictor variable. Additionally, two outcome variables were utilized within the current study, including program enrollment and employment status at discharge. For program enrollment, this variable was dichotomized into enrolled and not enrolled.
All veterans that had received a consult for VHA vocational rehabilitation were included in the data analysis. Oftentimes, veterans are not enrolled for services for several reasons such as (1) job obtainment prior to program start, (2) no longer wishing to work competitively, (3) having medical issues arise resulting in a cancellation until medical complications are no longer problematic, or (4) no longer interested in receiving services and seeking competitive employment. All veterans in the database were coded as 0 = not enrolled and 1 = enrolled. For veterans enrolled in the program and discharged, the coding was dichotomized: 0 = discharged without employment, 1 = discharged with employment. The outcome variables of VHA vocational rehabilitation program enrollment and employment at discharge, were evaluated by using a binary logistic regression analysis. In addition, the interaction between SUD and psychiatric disorder was utilized to examine the impact for veterans with both diagnoses on program enrollment and employment at discharge.
The sample consisted of 2,550 veteran patients referred to VHA VR between 2016 and 2021. Of these, the majority of the sample were biologically male (n = 1,740, 87.92%), and had a mean age of 55.24 years (SD 13.16 years). Most of the participants had a high school diploma (n = 2,231, 87.49%), and were Black or African American (n = 1,083, 46.28%), followed by white non-Hispanic (n = 991, 42.35%), Hispanic or Latino (n = 189, 8.08%), and Asian or Other Pacific Islander (n = 25, 1.07%). When considering the presence of clinical diagnosis, Major Depressive Disorder [F33 code, recurrent] (n = 1,019, 40.0%) and PTSD [F43.10] (n = 763, 29.9%) had the highest frequencies, followed by Generalized Anxiety Disorder [F41.1] (n = 391, 15.3%), and adjustment disorder [F43.20] (n = 220, 8.6%). A total of 607 (27.96%) veterans reported that they were on the supplemental nutrition assistance program (SNAP), while 63 veterans (2.54%) were noted as being enrolled in the homeless program and were classified as homeless at program consult. Table 1 provides a breakdown of demographic information. The data are categorized SUD/AUD (none, active, inactive) and representative of psychiatric disorders (i.e., adjustment, anxiety, depression, PTSD) with the highest frequencies.
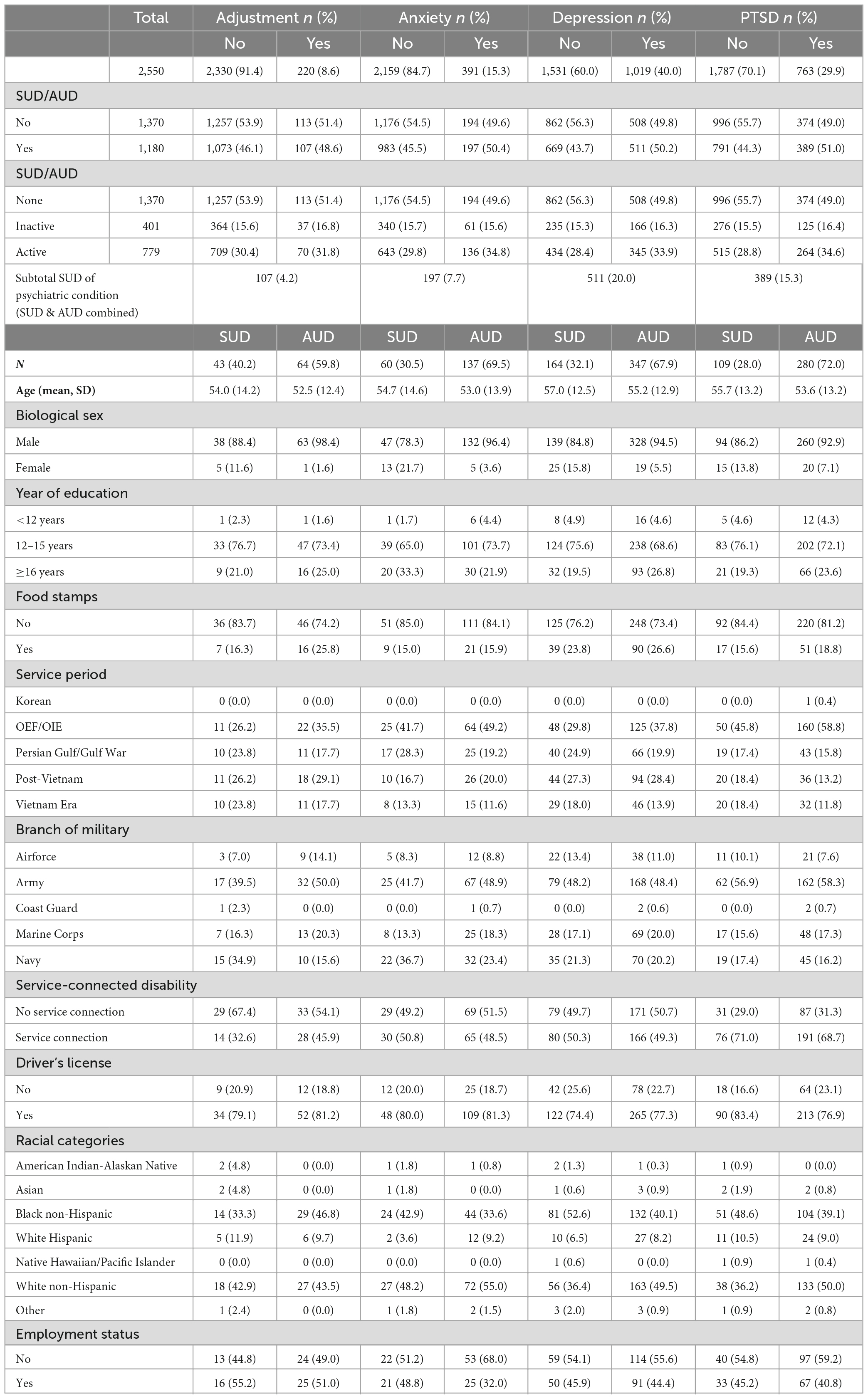
Table 1. Frequency of psychiatric conditions and co-occurring SUD/AUD disorders and other supplemental information.
Program enrollment was analyzed using a chi-square test to compare the impact of SUDs (active, inactive, none), AUDs (active, inactive, none), psychiatric diagnoses (diagnosis, no diagnosis: adjustment, anxiety, depression, PTSD, Bipolar, schizophrenia, schizoaffective), and the co-occurrence of these diagnoses. As shown in Table 2, depression, anxiety, adjustment disorder, and PTSD were significant less likely to enroll in vocational rehabilitation when the veteran also had a SUD diagnosis (note: active, early remission, sustained remission were one category to be consistent with prior research). When splitting SUD and AUD diagnoses into 3 levels (none, active, remission), findings showed that veterans with active AUD combined with a diagnosis of depression or anxiety or adjustment disorder or PTSD or Bipolar disorder were significantly less likely to be employed at discharge. Veterans with an active SUD diagnosis and co-occurring psychiatric diagnosis had similar employment rates at discharge compared to veterans without these diagnoses.
The alcohol and other substance use disorders diagnosis was split into active and inactive (in remission) to examine the influence (active, inactive, none) on program enrollment for veterans who additionally have co-occurring psychiatric diagnoses. A chi-square test was performed (see Table 2) and findings revealed that veterans with active AUD combined with depression (7.6 vs. 11.2%, p = 0.0031), anxiety (3.0 vs. 5.1%, p = 0.0081), PTSD (6.3 vs. 9.3%, p = 0.0064), and bipolar disorder (1.4 vs. 2.9%, p = 0.0097) were less likely to be enrolled for program services compared to veterans without these diagnoses. Veterans with adjustment disorder (2.1 vs. 0.8%, p = 0.0122) were more likely to be enrolled for program services.
A logistic regression analysis (see Table 3) comparing the outcome variable of enrollment (i.e., enrolled, not enrolled) indicated veterans with active AUD were less likely (OR = 0.67, 95% CI = [0.52–0.87], p = 0.0021) to be enrolled for program services compared to veterans without AUD. When including the interaction terms in the regression model (see Table 4), it was observed that the program enrollment was different in active AUD veterans with and without depression (p < 0.0001), anxiety (p = 0.0006), PTSD (p = 0.0011), and bipolar disorder (p = 0.0002). Specifically, active AUD veterans with depression (OR = 0.40, 95% CI = [0.26–0.63]), anxiety (OR = 0.53, 95% CI = [0.31–0.88]), PTSD (OR = 0.52, 95% CI = [0.36–0.80]), and bipolar disorder (OR = 0.21, 95% CI = [0.10–0.43]) were less likely to be enrolled for program services than those without these diagnoses.
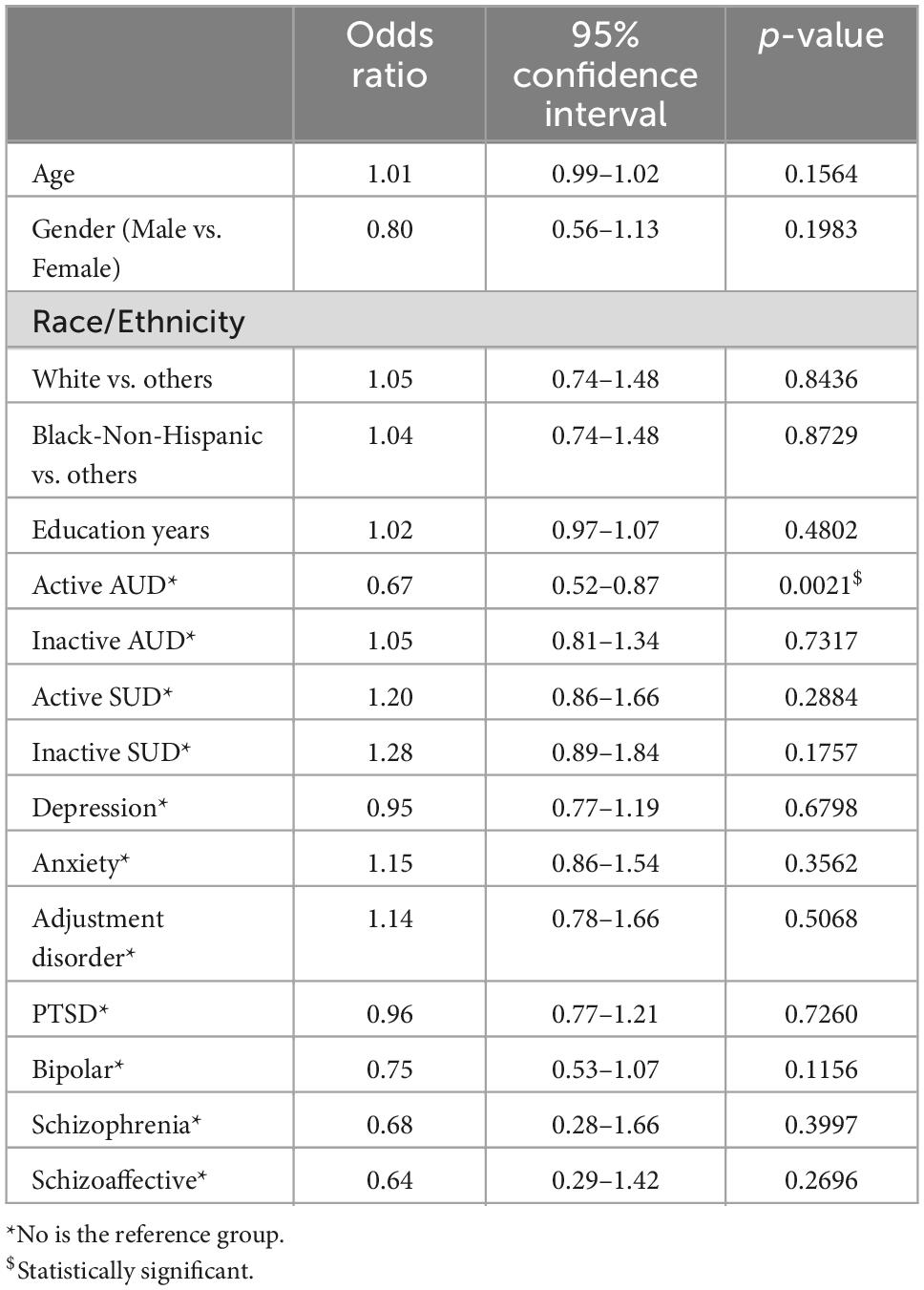
Table 3. Logistic regression of association of program enrollment, active/inactive AUD or SUD, and psychiatric conditions.
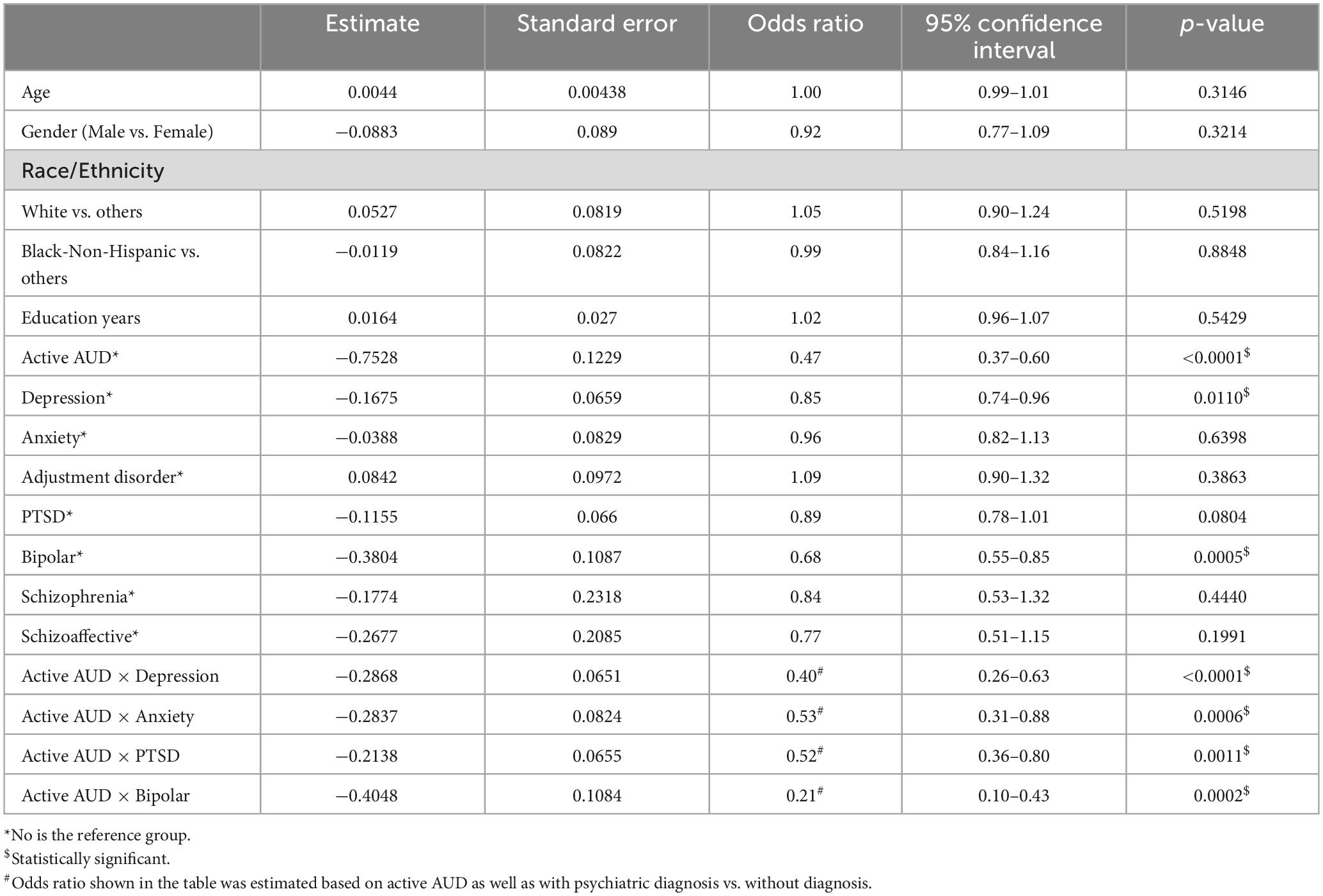
Table 4. Logistic regression of association of program enrollment and active AUD of interaction effect with psychiatric conditions.
A chi-square test of independence showed that veterans with a history of SUDs (see Table 5) had no difference in employment rates at discharge compared to veterans with no SUD diagnosis (30.9% with no SUD diagnosis vs. 29.1% with SUD diagnosis, p = 0.4441). The same findings occurred when comparing veterans with (31.2%) and without (31.9%) an AUD diagnosis and employment rates at discharge. When only examining psychiatric diagnoses, veterans without an adjustment disorder had higher rates of employment at discharge, but no other psychiatric diagnosis comparisons yielded significant differences. The interaction between psychiatric diagnosis and SUD or AUD yielded significant findings for employment rates at discharge for veterans diagnosed with bipolar disorder and SUDs, where the SUD category was categorized into no diagnosis, SUD diagnosis. When examining veterans with and without AUD and psychiatric diagnosis, veterans with anxiety and AUD (no diagnosis, AUD diagnosis) had significant differences. SUD and AUD diagnosis were then split into three levels, including no diagnosis, active diagnosis, and in-remission diagnosis. A logistic regression analysis comparing the outcome variable of employment (i.e., employment at discharge, no employment at discharge) demonstrated veterans with bipolar disorder were more likely (OR = 1.55, 95% CI = [1.01–2.40], p = 0.0492) to be employed at discharge compared to veterans without this disorder (see Table 6).
The benefits of VHA vocational rehabilitation, including the recovery from psychiatric and SUD diagnoses, is well-documented. Additional research reflects improved independent functioning and lowering of the need for medical, psychological, vocational, and homeless program services through the VHA (22, 25, 26, 28). The current study results yielded program enrollment disparities for veterans with a history of AUD diagnoses and a history of depression, adjustment disorder, and PTSD. Although research has shown the effectiveness that VR can have on independent functioning for veterans (20, 22), the intervention cannot be effective for the veterans that are not enrolled, thus indicating a need for research to (a) identify access and treatment enrollment issues, and (b) an intervention to eliminate these identify issues. The co-occurring diagnoses examined in the current study showed that the combination of psychiatric disorders with the presence of a AUD diagnosis resulted in a lower chance of being enrolled for VHA VR (compared to veterans without these diagnoses).
VR is a vital component of the care provided to veterans with or without medical and psychiatric disabilities. By improving employment outcomes and enhancing mental health and well-being, VR supports veterans to regain their independence and achieve meaningful lives. As previously noted, veterans who participated in a VR program had a higher likelihood of finding employment and greater job satisfaction than those who did not participate in VR. In addition to improving employment outcomes, VR can also enhance the mental health and well-being of veterans with a disability by providing a sense of purpose and accomplishment, rebuild their self-esteem and self-confidence, and to reduce symptoms of depression and anxiety.
Some potential contributions of this study to the field of rehabilitation could include improved understanding of the unique challenges faced by veterans with co-occurring diagnoses when attempting to enroll in vocational rehabilitation programs and obtain employment. By identifying the specific obstacles that these individuals face, researchers and practitioners can develop more targeted interventions and support services to help them succeed. In addition, the study suggests the need for increased awareness for integrated treatment approaches that address both mental health and physical health issues simultaneously. The findings of this study could highlight the importance of providing comprehensive, coordinated care for veterans with complex medical histories. Finally, implications suggest the need for enhanced ability to measure the effectiveness of vocational rehabilitation programs for veterans with co-occurring diagnoses. By examining the impact of these programs on employment outcomes, researchers can determine which interventions are most effective and identify areas where further improvements are needed. Overall, the study has the potential to inform the development of more effective interventions and support services for veterans with co-occurring diagnoses, ultimately improving their employment prospects and quality of life.
As mentioned, previous research necessitates a focus on challenges endured when veterans are referred for vocational services and why program enrollment rates compared to referrals for VHA VR services (e.g., scheduling of intake interview and treatment plan session). Research must (1) identify reasons why Veteran do not enroll in VHA VR after a referral is made, (2) impact of program engagement on VHA VR enrollment, and (3) the efficacy of providing concurrent vocational rehabilitation services while a Veteran is enrolled in mental health and/or substance use counseling services, rather than having a focus placed on vocational needs toward the end of their treatment regimen (note: not all treatment is post-MH and/or SUD counseling services, but further investigation is needed). State-federal (public) VR programs that are designed for civilians have shown higher SUD and or MH treatment compliance when employment is obtained, higher abstinence rates, and more successful vocational outcomes when treatment is concurrent (30, 33). Emphasis should also focus on why veterans are not being enrolled into VHA VR after a referral is made. After this identification is made, evidence-based interventions can be developed to (a) allow for vocational interventions to be implemented in MH or SUD treatment (prior to a referral is made), and (b) creating evidence-based interventions to increase program enrollment so that veterans obtain VR services that may lead to lower healthcare needs (e.g., fewer visits in VHA vocational rehabilitation, outpatient mental health, homelessness program, and medical hospitalizations) post-discharge (22, 25).
As evident by prior research, employment improves self-esteem, recovery, less reliance on medical and psychiatric services, and lesser symptom impact for people with mental illness (22, 25). Likewise, employment is a strong predictor of a higher quality of life, greater self-esteem, fewer psychiatric symptoms, and less absenteeism at work (34). Employment issues for people with medical and psychiatric disabilities/disorders are closely linked with an evolving body of legislation. Over time, laws are updated to keep pace with the changing nature of disability as medicine, science, societal attitudes, and education all advance. Of particular importance are the Rehabilitation Act of 1973, the Americans with Disabilities Act, and amendments for each. The Rehabilitation Act of 1973 is still significant today in that it challenged vocational rehabilitation programs to find new ways to support people with more severe impacts from disabilities to move into the workforce. This law also laid the groundwork for the Americans with Disabilities Act of 1990 (35) and the Americans with Disabilities Amendments Act [ADAAA] (36). The ADAAA affirmed and emphasized the right of workers and job seekers with disabilities to not only participate in the workplace, but also the right to access reasonable accommodations.
Reasonable accommodations are any changes to the workplace, job functions, or to the procedures surrounding the job that make it possible for the person with a disability to perform the essential functions of the job. It is important to note that the accommodation is meant to limit or eliminate the impact of the disability so that workers can perform their jobs. A few examples include changing the location of task-related supplies, modifying a work schedule: acquiring new equipment, or granting access to a private space for breaks. Reasonable accommodations are integral to promote the effectiveness of VR programs and have an impact on independent functioning, job satisfaction and retention, and quality of life indicators (37–39).
The Job Accommodation Network (JAN) provides a public resource for information about accommodations designed to support workers with disabilities and employers. Requests for accommodation ideas for individuals with mental health diagnoses are available. Some of the most common are flexible schedules, if there is required training this training may need to me modified, and a job coach (40). Furthermore, the least commonly requested accommodation type is a physical modification to a workplace for a person who has a mental health diagnosis. Although this is not a direct accommodation, several studies show that having a supervisor who is understanding and supportive lowers the risk factor for absenteeism and longer tenure for workers with mental health diagnosis (41). Potential accommodations for a person living with a mental health diagnosis such as anxiety, PTSD, Bipolar, or depression might include a flexible schedule, modified break schedules, a sound machine or quiet workplace, daily job tasks or itemized task lists, job restructuring, reminders, written instructions, noise canceling headsets, telework, and others as they may relate to supporting that individual.
There is significant psychological stress placed on an individual with severe mental illness and/or SUDs. Literature has found that it is hard for those diagnosed with MH disorders to request support or reasonable accommodations due to fear of retaliation and stigma (42–44). This shows the need for VHA VR services to assist in requesting workplace accommodations and helping the veteran manage work-related stress. The supported employment program within VHA VR uses the evidence-based Individual Placement and Support (IPS) model, which has shown high efficacy in employment outcomes (higher instances of employment and sustainment of employment) for those with serious mental illness due to the supports in requesting workplace accommodations and managing work-related stress (45). Eliminating these types of vocational barriers to employment can be vital is assisting the veteran to obtain and maintain employment despite significant employment related barriers (46).
The current study had initial limitations that were addressed prior to analyzing the data. First, much of the data that were used in the current study was entered by VR counselors during the intake interview with the veteran. It is possible that this data were entered incorrectly into the database by VR counselors, therefore medical records in CPRS and JLV were used by the primary author to confirm that information was inputted correctly (the primary author made corrections if VR counselors inaccurately entered the information into the database – CPRS and JLV were deemed as more accurate than the database). However, it is still possible that data entry errors occurred, as information is manually inputted in CPRS and JLV systems. Another study limitation of the dataset was inaccuracy related to psychiatric diagnosis and past and current alcohol use and other substance use disorder. The database used during the intake interview did not account for the durational period of last SUD/AUD usage (active, early remission, sustained remission) nor psychiatric diagnoses per the DSM 5 TR (F-Code). Therefore, information was collected from CPRS and JLV to properly code the diagnoses (e.g., early remission from AUD or SUD is 3–12 months post last use). To account for stronger representation of access, enrollment, and efficacy of vocational rehabilitation services, a national study should be used to determine if the themes from the current study exist across the U.S.
Prior research on VHA VR programs have primarily focused on outcomes. Current study findings have showed some disparities in program enrollment and employment at discharge when a veteran has a psychiatric diagnosis. With much focus of the VA related to access and outcomes, there is an apparent need for more research focus on how to increase program enrollment into VHA VR programs (why is the veteran not enrolling in services after referral is made).
The data analyzed in this study is subject to the following licenses/restrictions: The U.S. Department of Veteran Affairs has strict guidelines on the release of Protected Health Information. Due to the policies governing the release or availability of data, we are unable to release the data associated with the current manuscript. Requests to access these datasets should be directed to https://www.research.va.gov/programs/orppe/vacentralirb/default.cfm.
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the participants was not required to participate in this study in accordance with the national legislation and the institutional requirements.
MS, FB, and HH contributed to the conception and design of the study. MS organized the database. MS completed the data analysis with the assistance of Y-SL. MS and Y-SL interpreted all data. HH, LR, FB, ZS, and AG wrote sections of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Hoggatt K, Harris A, Washington D, Williams E. Prevalence of substance use and substance-related disorders among US Veterans Health Administration patients. Drug Alcohol Depend. (2021) 225:108791. doi: 10.1016/j.drugalcdep.2021.108791
2. The White House. Actions taken by the Biden-Harris Administration to address addiction and the overdose epidemic. Washington, DC: The White House (2021).
3. Substance Abuse and Mental Health Services Administration. 2019 National Survey on Drug Use and Health: Veteran Adults. North Bethesda, MD: Substance Abuse and Mental Health Services Administration (2020).
4. Moore D, Rosenheck R. Medical-surgical hospitalization among veterans with psychiatric and substance use disorders. Psychosomatics. (2019) 60:591–8. doi: 10.1016/j.psym.2019.04.005
5. Horan W, Wynn J, Gabrielian S, Glynn S, Hellemann G, Kern R, et al. Motivational and cognitive correlates of community integration in homeless veterans entering a permanent supported housing program. Am J Orthopsychiatry. (2020) 90:181–92. doi: 10.1037/ort0000420
6. Teeters J, Lancaster C, Brown D, Back S. Substance use disorders in military veterans: prevalence and treatment challenges. Subst Abuse Rehabil. (2017) 8:69–77. doi: 10.2147/SAR.S116720
7. Fuehrlein B, Mota N, Arias A, Trevisan L, Kachadourian L, Krystal J, et al. The burden of alcohol use disorders in US military veterans: results from the National Health and Resilience in Veterans Study. Addiction. (2016) 111:1786–94. doi: 10.1111/add.13423
8. Substance Abuse and Mental Health Services Administration. Co-Occurring Disorders and Other Health Conditions. North Bethesda, MD: Substance Abuse and Mental Health Services Administration (2023).
9. Substance Abuse and Mental Health Services Administration. Mental Health and Substance Use Co-Occurring Disorders. North Bethesda, MD: Substance Abuse and Mental Health Services Administration (2023).
10. Substance Abuse and Mental Health Services Administration. 2020 National Survey on Drug Use and Health: Veteran Adults. North Bethesda, MD: Substance Abuse and Mental Health Services Administration (2022).
11. Mobbs M, Bonanno G. Beyond war and PTSD: the crucial role of transition stress in the lives of military veterans. Clin Psychol Rev. (2018) 59:137–44. doi: 10.1016/j.cpr.2017.11.007
12. Chinchilla M, Gabrielian S, Hellemann G, Glasmeier A, Green M. Determinants of community integration among formerly homeless veterans who received supportive housing. Front Psychiatry. (2019) 10:472. doi: 10.3389/fpsyt.2019.00472
13. Inoue C, Shawler E, Jordan C, Jackson C. Veteran and Military Mental Health Issues. Treasure Island, FL: StatPearls Publishing (2023).
14. Greenberg G, Rosenheck R. Compensation of veterans with psychiatric or substance abuse disorders and employment and earnings. Mil Med. (2007) 172:162–8. doi: 10.7205/milmed.172.2.162
15. Merritt V, Jurick S, Crocker L, Keller A, Hoffman S, Jak A. Factors associated with employment and work perception in combat-exposed veterans. Rehabil Psychol. (2020) 65:279–90. doi: 10.1037/rep0000323
16. Van Til L, Fikretoglu D, Pranger T, Patten S, Wang J, Wong M, et al. Work reintegration for veterans with mental disorders: a systematic literature review to inform research. Phys Ther. (2013) 93:1163–74. doi: 10.2522/ptj.20120156
17. US Department of Veterans Affairs. VHA Directive 1163: Psychosocial Rehabilitation and Recovery Services. Washington, DC: US Department of Veterans Affairs (2019).
18. Sprong M, Hollender H, Pechek A, Forziat-Pytel K, Buono F. Effects of VHA Policy Directive 1163 on acceptance and employment rates for veterans with substance use disorders referred to VHA vocational rehabilitation. Subst Abuse. (2022) 16:11782218221132397. doi: 10.1177/11782218221132397
19. Sprong M, Hollender H, Paul E, Gilbert J, Weber K, Garakani A, et al. Impact of substance use disorders on employment for veterans. Psychol Serv. (2022) [Epub ahead of print]. doi: 10.1037/ser0000690
20. Bakken-Gillen S, Berven N, Chan F, Brooks J, Resnick S, Rumrill P, et al. Prediction of employment outcomes among veterans with substance use disorders: a chi-squared interaction detector analysis. J Voc Rehabil. (2015) 43:113–27. doi: 10.1080/09638280500158307
21. LePage J, Lewis A, Crawford A, Washington E, Parish-Johnson J, Cipher D, et al. Vocational rehabilitation for veterans with felony histories and mental illness: 12-month outcomes. Psychol Serv. (2018) 15:56–64. doi: 10.1037/ser0000114
22. Stevenson B, Bakken S, Mueller L, Drebing C. Why open access to vocational services in substance use treatment matters: Commentary on Cosottile and Defulio (2020). Psychol Addict Behav. (2022) 36:117–20.
23. Bond G, Al-Abdulmunem M, Ressler D, Drake R, Davis L, Meyer T, et al. Evaluation of an employment intervention for veterans transitioning from the military: a randomized controlled trial. J Nerv Ment Dis. (2022) 210:321–9. doi: 10.1097/NMD.0000000000001472
24. Zivin K, Bohnert A, Mezuk B, Ilgen M, Welsh D, Ratliff S, et al. Employment status of patients in the VA health system: implications for mental health services. Psychiatr Serv. (2011) 62:35–8. doi: 10.1176/ps.62.1.pss6201_0035
25. Abraham K, Chang M, Van T, Resnick S, Zivin K. Employment after vocational rehabilitation predicts decreased health care utilization in veterans with mental health diagnoses. Mil Med. (2021) 186:850–7. doi: 10.1093/milmed/usab113
26. Davis L, Resnick S, Maieritsch K, Weber K, Erbes C, Strom T, et al. Employment outcomes from VA vocational services involving transitional work for veterans with a diagnosis of posttraumatic stress disorder. Psychiatr Rehabil J. (2019) 42:257–67. doi: 10.1037/prj0000357
27. Kerrigan A, Kaough J, Wilson B, Wilson J, Bostick R. Vocational rehabilitation of participants with severe substance use disorders in a VA veterans industries program. Subst Use Misuse. (2004) 39:2513–23. doi: 10.1081/ja-200034695
28. Resnick S, Rosenheck R. Posttraumatic stress disorder and employment in veterans participating in Veterans Health Administration Compensated Work Therapy. J Rehabil Res Dev. (2008) 45:427–35. doi: 10.1682/jrrd.2007.06.0093
29. Humensky J, Jordan N, Stroupe K, Hynes D. Employment status of veterans receiving substance abuse treatment from the U.S. Department of Veterans Affairs. Psychiatr Serv. (2013) 64:177–80. doi: 10.1176/appi.ps.201200024
30. Melvin A, Davis S, Koch D. Employment as a predictor of substance abuse treatment completion. J Rehabil. (2012) 78:31–7.
31. American Psychiatric Association Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association (2022). doi: 10.1176/appi.books.9780890425787
32. Meshberg-Cohen S, Reid-Quiñones K, Black AC, Rosen MI. Veterans’ attitudes toward work and disability compensation: associations with substance abuse. Addict Behav. (2014) 39:445–8. doi: 10.1016/j.addbeh.2013.09.005
33. Sprong M, Dallas B, Melvin A, Koch D. Substance abuse and vocational rehabilitation: a survey of policies & procedures. J Rehabil. (2014) 80:4–9.
34. Luciano A, Bond G, Drake R. Does employment alter the course and outcome of schizophrenia and other severe mental illnesses? A systematic review of longitudinal research. Schizophr Res. (2014) 159:312–21. doi: 10.1016/j.schres.2014.09.010
35. US Department of Labor. Americans with Disabilities Act. Washington, DC: US Department of Labor (2020).
36. Equal Employment Opportunity Commission. ADA AMENDMENTS ACT OF 2008. Washington, DC: Equal Employment Opportunity Commission (2008).
37. Lindsay S, Cagliostro E, Leck J, Shen W, Stinson J. Disability disclosure and workplace accommodations among youth with disabilities. Disabil Rehabil. (2019) 41:1914–24.
38. Rangarajan S, Muliyala K, Jadhav P, Philip S, Angothu H, Thirthalli J. Reasonable accommodation at the workplace for professionals with severe mental illness: a qualitative study of needs. Indian J Psychol Med. (2020) 42:445–50.
39. Su H, Wong J, Kudla A, Park M, Trierweiler R, Capraro P, et al. Disability phenotypes and job accommodations utilization among people with physical disability. J Occup Rehabil. (2022) 33:352–61.
40. McDowell C, Fossey E. Workplace accommodations for people with mental illness: a scoping review. J Occup Rehabil. (2015) 25:197–206.
41. de Vries G, Koeter M, Nieuwenhuijsen K, Hees H, Schene A. Predictors of impaired work functioning in employees with major depression in remission. J Affect Disord. (2015) 185:180–7.
42. Appelbaum P. Workplace Discrimination Against People With Mental Disorders and the ADA. Psychiatr Serv. (2022) 73:1193–5.
43. Dong S, Hoeflich C, Sirota P. An examination of the psychosocial factors impacting workplace accommodation requests in individuals with mental disabilities. Work. (2022) 72:865–74.
44. King A, Fortune T, Byrne L, Brophy L. Supporting the Sharing of Mental Health Challenges in the Workplace: Findings from Comparative Case Study Research at Two Mental Health Services. Int J Environ Res Public Health. (2021) 18: 12831.
45. Wallstroem I, Pedersen P, Christensen T, Hellstrom L, Bojesen A, Stenager E, et al. A systematic review of individual placement and support. employment, and personal and clinical recovery. Psychiatr Serv. (2021) 72:1040–7.
Keywords: employment, substance use disorders, veterans, vocational rehabilitation, mental health, co-occurring disorders, psychiatric disorders, Department of Veteran Affairs
Citation: Sprong ME, Hollender H, Lee Y-S, Rawlins Williams LA, Sneed Z, Garakani A and Buono FD (2023) Disparities in program enrollment and employment outcomes for veterans with psychiatric and co-occurring substance use disorders referred or enrolled for VHA vocational rehabilitation. Front. Psychiatry 14:1200450. doi: 10.3389/fpsyt.2023.1200450
Received: 18 April 2023; Accepted: 26 June 2023;
Published: 13 July 2023.
Edited by:
Hector Wing Hong Tsang, Hong Kong Polytechnic University, Hong Kong SAR ChinaReviewed by:
Jane Burke-Miller, University of Illinois Chicago, United StatesCopyright © 2023 Sprong, Hollender, Lee, Rawlins Williams, Sneed, Garakani and Buono. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Matthew E. Sprong, bXNwcm8yQHVpcy5lZHU=, bWF0dGhldy5zcHJvbmdAdmEuZ292
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.