- 1College of Medicine, King Saud bin Abdulaziz University for Health Sciences, Jeddah, Saudi Arabia
- 2King Abdullah International Medical Research Center, Jeddah, Saudi Arabia
- 3College of Medicine, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia
- 4Division of Neurology, King Abdulaziz Medical City, Ministry of the National Guard Health Affairs, Riyadh, Saudi Arabia
- 5Department of Medicine, King Abdulaziz Medical City, Ministry of the National Guard Health Affairs, Jeddah, Saudi Arabia
- 6King Abdullah International Medical Research Center, Riyadh, Saudi Arabia
Background: Multiple sclerosis (MS) is an autoimmune disease characterized by chronic, progressive neurodegeneration of the central nervous system (CNS), and it is the most common inflammatory neurological disease affecting young adults. Given the chronic, progressive nature of the disease, psychiatric disorders are more prevalent among these patients, as reported in the literature; however, data in Saudi Arabia are limited. This study aimed to estimate the prevalence of major depression and generalized anxiety disorder in patients with MS and their association with different patient demographics.
Methods: This was a cross-sectional, multicentered study that included adult patients with MS from 30 June 2021 to 30 June 2022. Participants were interviewed in person and asked to complete a survey that included general demographics, the Patient Health Questionnaire-9 (PHQ-9), and the Generalized Anxiety Disorder-7 (GAD-7) questionnaire. Other variables related to the patients' conditions, such as MS type and Expanded Disability Status Scale (EDSS) score, were collected from the patient's electronic records. Descriptive statistics were performed, and associations were made using the chi-square, Fisher's exact, and analysis of variance tests, as appropriate.
Results: A total of 192 participants were included in this study. Based on a cutoff score of >10 on the GAD-7 and PHQ-9 scales, the prevalence of generalized anxiety disorder was 26.1% (50), with the majority of participants having minimal anxiety (40%); meanwhile, the prevalence of major depression was 42.7% (n = 82), and most of them had mild depression (30%). Female participants scored significantly higher compared to men on the GAD-7 scale (p = 0.0376), but not on the PHQ-9 scale (p = 0.1134). In addition, no statistically significant association was detected between functional disability (EDSS score) and prevalence of anxiety and depression.
Conclusion: This study demonstrated a high prevalence of generalized anxiety disorder and major depression among patients with MS compared with that in the general population, with women being more affected. As these comorbid disorders could negatively affect the disease course, screening is of paramount significance.
1. Introduction
Multiple sclerosis (MS) is a chronic, progressive neurodegenerative autoimmune disease that mainly affects the central nervous system (CNS) (1). The main characteristics of MS are demyelination and inflammation of the myelin sheath, which covers the axons of the CNS cells (1). MS is characterized by multiple different subtypes, with relapsing–remitting multiple sclerosis (RRMS) being the most commonly reported subtype (2). The clinical manifestations of MS vary as the patient's presentation depends mainly on the location of the lesion within the CNS, which can occur in the brain, spinal cord, or optic nerves. However, the most common clinical features reported are impaired vision, weakness, numbness, cognitive and psychiatric symptoms, and bowel or bladder dysfunction (3, 4).
MS is the most common inflammatory neurological disease in young adults, affecting more than 2.3 million people worldwide, and the prevalence of the disease has continued to increase since 1990. In Saudi Arabia, the estimated prevalence of MS was ~40.40 per 100,000 population and 61.95 per 100,000 Saudi nationals in 2018 (3). It is more common among women and usually occurs between the ages of 20 and 40 years (4).
MS is considered one of the leading causes of neurological non-traumatic disability among young people, resulting in a reduction in productivity and quality of life and major psychological and social impairment. As such, the prevalence of psychiatric disorders among these patients is higher. Psychiatric manifestations include, but are not limited to, depression, anxiety, mania, and substance use disorders (5–7). Depression is considered the most commonly reported psychiatric disorder among patients with MS (37–54%). This is followed by anxiety disorders (14–41%) (6, 8). In addition, psychiatric manifestations could be reported as the presenting symptom of MS in some patients; however, they appear later in the course of the disease in the majority of patients with MS. The causes of developing these psychiatric comorbidities may be immunological or biological, or due to poor coping mechanisms (9). More importantly, the effects of the disease itself on the brain, such as neuroinflammation, synapses dysfunction, and other structural changes such as hippocampal shape variation and progressive gray matter loss in limbic basal ganglia, may play a role in the pathogenesis of these disorders (10, 11).
Several studies have evaluated the prevalence of psychiatric disorders in patients with MS. In a study published in 2015 to assess the burden of psychiatric diseases (e.g., depression, anxiety, bipolar disorder, and schizophrenia) among patients with MS in comparison with the general population, the prevalence and incidence of the psychiatric disorders mentioned earlier increased among patients with MS compared with those in the general population (12, 13). In this study, several factors were found to be associated with a higher percentage of depression among patients with MS, including female sex and older age (13). Furthermore, Beiske et al. found that fatigue and being young at the time of diagnosis are linked to the development of depression and anxiety symptoms (14, 15). Locally, a study in Saudi Arabia aimed to assess the prevalence of depression in patients with MS and found that 89.9% of patients had mild to severe symptoms of depression (16). Among the patients with depression, 65.13% were non-smokers, and 37.39% were unemployed (16). An association between educational level and severity of depression was also found (16).
Although several studies have evaluated psychiatric diseases among patients with MS, data in Saudi Arabia are limited, and the other studies were survey-based without direct clinical patients' evaluation. Therefore, the focus of this study was to estimate the prevalence of major depression and generalized anxiety disorder in patients with MS in Saudi Arabia and also to find its association with multiple demographic variables, such as age, sex, marital status, educational level, and monthly income, as well as the effects of duration of the disease on patients' mental health. In addition, we compared MS disease-modifying therapy types and severity of the illness using the clinically confirmed EDSS score of the patient with the development of psychiatric comorbidities.
2. Materials and methods
2.1. Study design and participants
A cross-sectional study with retrospective chart review was conducted at King Abdulaziz Medical City (KAMC) in Jeddah and Riyadh, Saudi Arabia, from 30 June 2021 to 30 June 2022. The inclusion criteria were a confirmed diagnosis of MS based on the McDonald criteria and an age of >18 years. To ensure the quality of the data given, patients were interviewed in person upon attending the neurology clinic and given a survey to fill out. Then, the electronic records of prospective patients were reviewed to complete the data collection process. Informed consent was obtained from each patient to participate in the study.
2.2. Study measures
Participants' demographic data, such as age, sex, marital status, monthly income, employment status, history of psychiatric disorders, or any other comorbidities (e.g., diabetes mellitus, hypertension, and chronic kidney disease), were collected. Data related to the patient's condition, such as MS type, EDSS score, type of MS medications, and any other medications (e.g., antidepressant, anxiolytic, and antiepileptic), were also obtained from the electronic records after being reviewed and confirmed by a neurologist.
Part of the survey was an Arabic-validated version of the Generalized Anxiety Disorder-7 (GAD-7) questionnaire (17). The GAD-7 is a short self-administered scale ranging from 0 to 21, with 0–4 for minimal anxiety, 5–9 for mild anxiety, 10–14 for moderate anxiety, and 15–21 for severe anxiety. We used a cutoff score of 10 for the diagnosis of generalized anxiety disorder (18). The GAD-7 has shown improved internal validity and reliability in studies involving patients with MS (19).
The last part of the survey was an Arabic-validated version of the Patient Health Questionnaire-9 (PHQ-9) (20). The PHQ-9 is a short self-administered scale ranging from 0 to 27, with 0–4 for minimal depression, 5–9 for mild depression, 10–14 for moderate depression, 15–19 for moderately severe depression, and 20–27 for severe depression. With a cutoff score of >9, the scale has good sensitivity and specificity, making it an appropriate tool for depression screening in patients with MS (21).
2.3. Data analysis
Continuous variables were reported as mean and standard deviation. Categorical variables were reported as frequencies and percentages. Data were analyzed using the chi-square, Fisher's exact, and analysis of variance tests, as appropriate. In addition, Spearman's test was used for correlation analysis. Statistical significance was set at p < 0.05. The goodness of fit showed p < 0.001; however, the distribution of the variables displayed on the central limit theorem was just slightly skewed. Therefore, mean and SD were still valid based on the central limit theorem to describe the center and variation of the reported continuous variables. Statistical analyses were performed using JMP statistical software subsidiary, SAS Institute, version 15.2.0.
3. Results
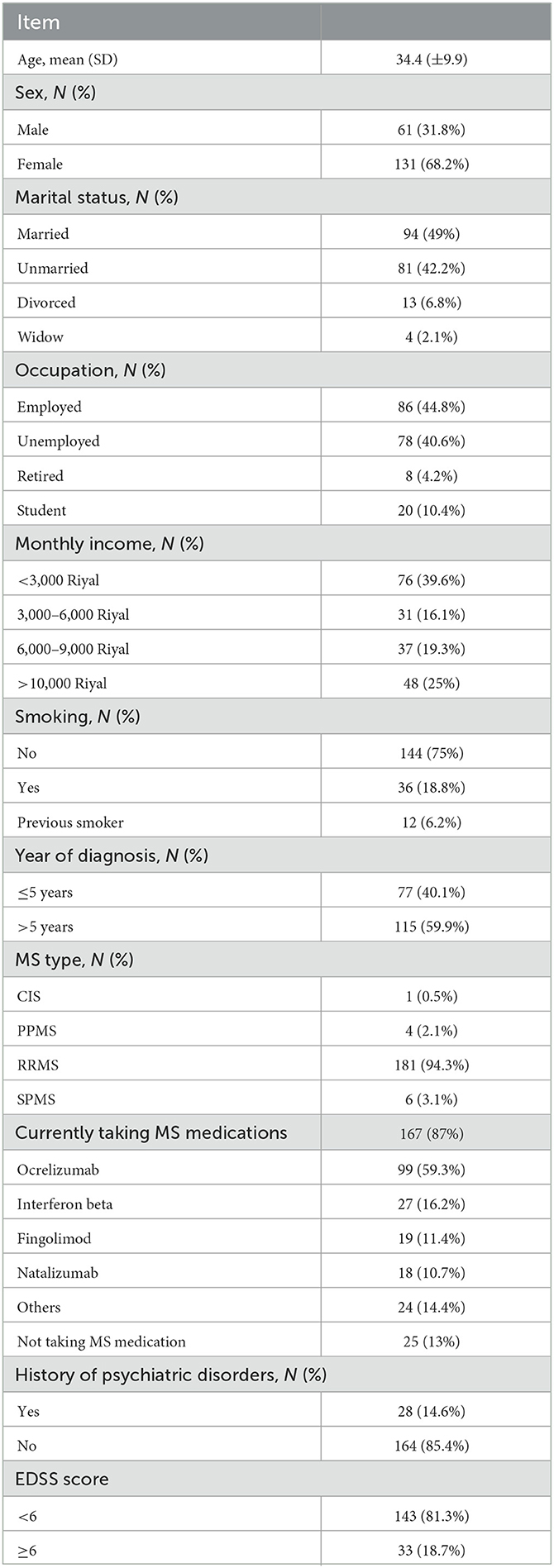
A total of 192 patients were included in this study. The mean age of the participants was 34.4 (±9.9) years. Most of the participants were women (68.2%), whereas 31.8% were men. Nearly half of the patients were married (48.9%), and 44.8% were employed. The majority of participants were non-smokers (75%). More than half of the patients were diagnosed with MS for >5 years (59.9%), with RRMS being the most common type (94.2%). The most frequently reported medications for MS were ocrelizumab (59.3%) and interferon beta (16.2%). Most patients (81.3%) had an EDSS score of < 6. The additional demographic details are presented in Table 1.
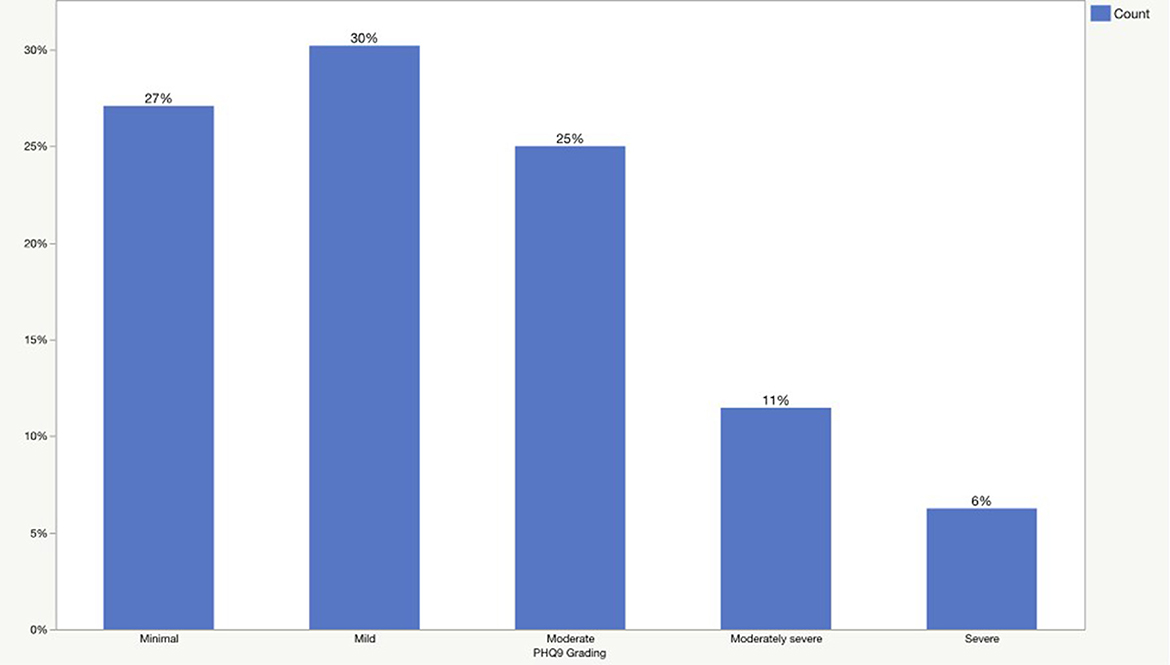
The prevalence of generalized anxiety disorder and major depression is presented in Figures 1, 2. According to the GAD-7 score, 40% of patients had minimal anxiety, followed by mild (34%), moderate (17%), and severe (9%) anxiety. Regarding the PHQ-9 scores, 27% of the patients had a minimal form of depression, followed by mild (30%), moderate (25%), moderately severe (11%), and severe (6%) depression.
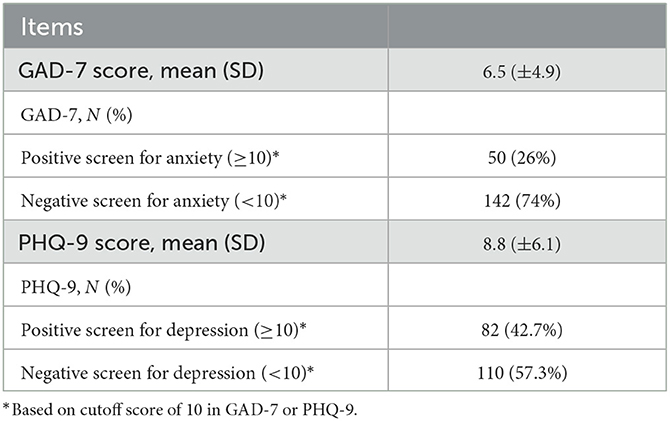
Overall, the mean score of GAD-7 was 6.5 (±4.9), and generalized anxiety disorder was present in 26% (n = 50) of the participants. Meanwhile, the mean score of PHQ-9 was 8.8 (±6.1), and major depression was detected in 42.7% (n = 80) of the participants (Table 2).
Based on the GAD-7 score, 40 (80%) of those who met the criteria for generalized anxiety disorder were women, whereas only 10 (20%) were men, with a statistically significant difference (p = 0.0376). With respect to other demographic variables, no significant associations were found between those with anxiety and those without. However, patients with anxiety had more previous psychiatric disorders than patients without anxiety (p = 0.0283). More details are shown in Table 3.
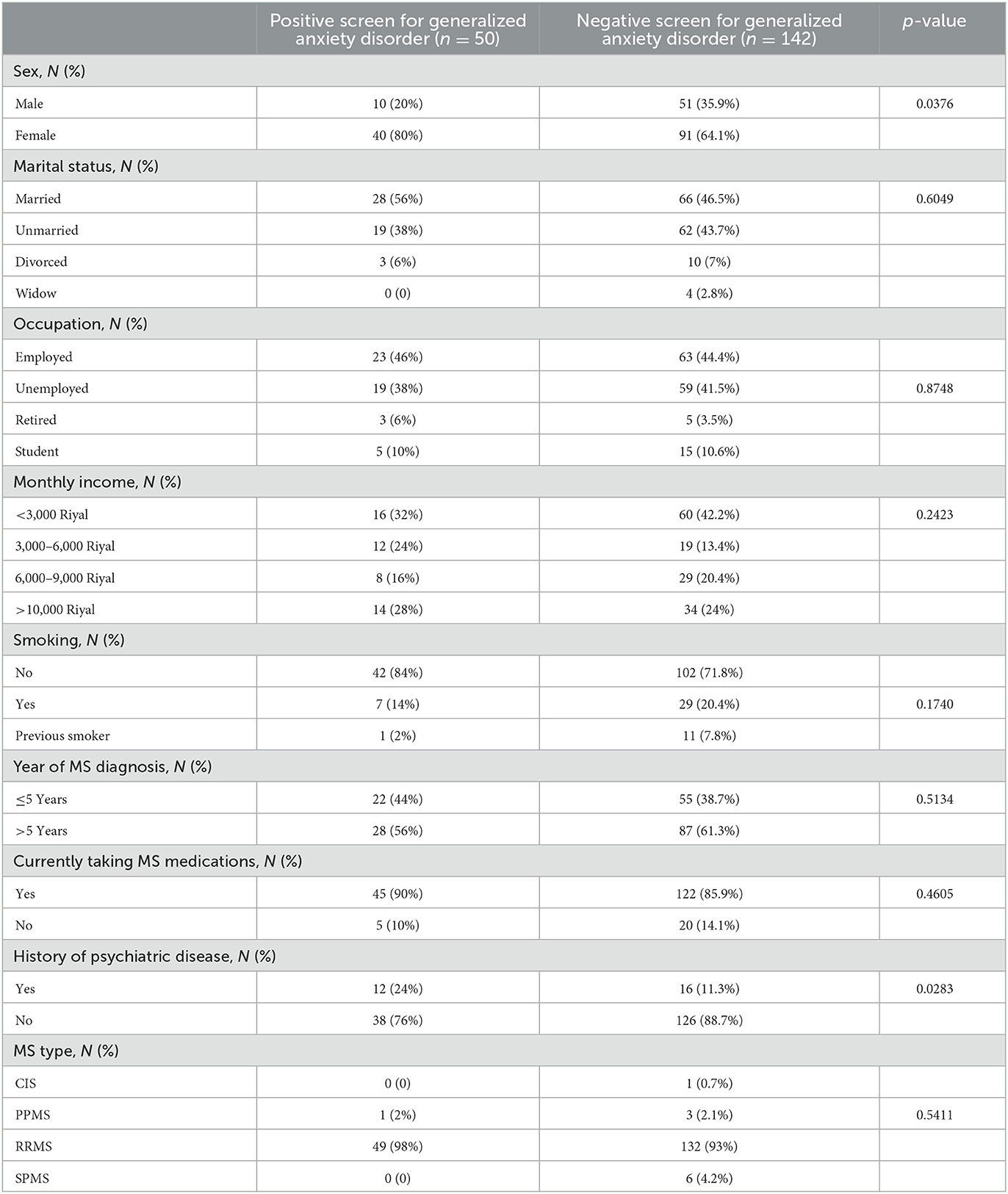
Table 3. The association between the GAD-7 grading and patients' demographics, medical history, and multiple sclerosis-related variables.
Based on the PHQ-9 score, 61 (74.4%) of those who had major depression were women, whereas only 21 (25.6%) were men, with a non-statistically significant difference (p = 0.1134). With respect to other variables, neither demographic nor MS-related variables were found to be significantly associated with depression. The additional details are provided in Table 4.
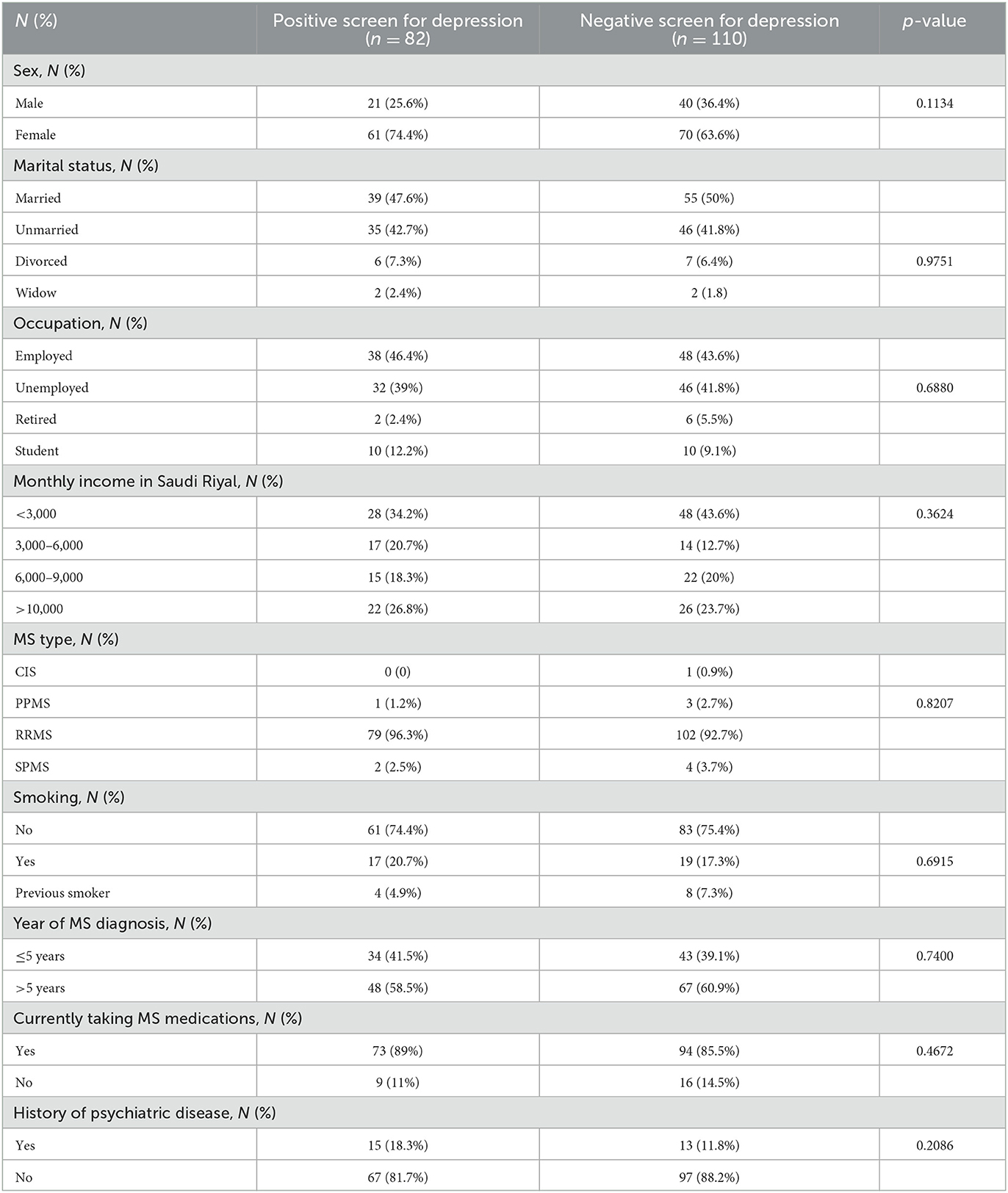
Table 4. The association between the PHQ-9 grading and patients' demographics, medical history, and multiple sclerosis-related variables.
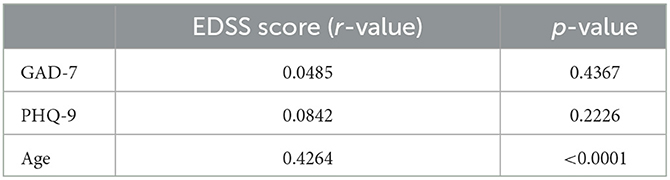
The results showed a positive correlation between the EDSS score and age (r = 0.4264, p < 0.0001). However, no correlation was found between functional disability (EDSS score) and the prevalence of anxiety and depression (Table 5).
4. Discussion
MS is a common neurodegenerative disease that affects the CNS, especially in young adults. A major concern among the population with MS is the high prevalence of psychiatric comorbidities and their association with disease progression. Previous studies have also explained the impact of depression in patients with MS, including no adherence to medications, poor quality of life, deteriorating disability, and impaired cognitive function (22–25). Although the pathogenesis remains unclear, some studies suggest that demyelinating lesions in patients with MS contribute to their emotional disturbances (26, 27). In particular, lesions in the frontal lobe, prefrontal cortex, anterior temporal lobe, and parietal lobe can be associated with an increased incidence of anxiety and depressive disorders (10, 11). Therefore, patients with MS are more susceptible to psychiatric illnesses than the general population (9). This study aimed to determine the prevalence of major depression and generalized anxiety disorder among patients with MS in Saudi Arabia and its association with multiple demographic and MS-related variables.
Similar to the current literature, the majority of our study participants were women (68.2%), highlighting the fact that MS is more common in women (1). Based on the current study, the prevalence of generalized anxiety disorder and depression was 26% and 42.7%, respectively. This is consistent with a systematic review that found that anxiety and depression are the most reported psychiatric diseases, affecting more than 20% of patients with MS (28). Similar to our study, another systematic review found the prevalence of depression and anxiety to be 30.5 and 22.1%, respectively (9). However, the prevalence of depression and anxiety in this study is much higher compared to the general population in Saudi Arabia as the Saudi National Mental Health Survey (SNMHS) estimated the prevalence to be 3.8% for depression and 12.3% for anxiety in the general population in Saudi Arabia (29). In addition, a minority of patients (14.5%) reported a positive history of psychiatric disorders, mostly depression and anxiety. This could point out several issues related to this population, including stigma about mental health seeking behavior and beliefs that MS does not have a role in these complaints.
The association between MS and psychiatric disorders is related to several factors, including age, sex, year of diagnosis, EDSS score, and socioeconomic status. In accordance with sex, the majority of patients with depression were women (74.4%, n = 61). These findings are compatible with a recently published local study of 238 patients with MS, which concluded a higher prevalence of depression among women (16). In contrast, some studies have found no sex difference in terms of depression (30–32). In addition, the prevalence of anxiety was high and more pronounced in women in this study, comprising 80% (n = 40) of those with anxiety. Similarly, this was evident in two systematic reviews, associating MS with a higher prevalence of anxiety (28, 33). In this study, we did not find a correlation between disease duration and prevalence of psychiatric disorders. However, other studies suggested that shorter disease duration is a risk factor for anxiety only but not depression (13, 34).
In terms of monthly income, 39.4% (n = 76) of the participants had a low income (< 3,000 riyals). Furthermore, a significant proportion (40.6%, n = 78) of the participants were unemployed. Although unemployment could partially explain low income, it can be an MS sequela. One study found that patients with MS were more likely to be jobless or have changed careers to less skilled jobs as a consequence of their disease (31).
A minority of our sample, 14.6% (n = 28), reported a history of psychiatric disorder, and it was associated with a higher prevalence of anxiety only but not depression. Although both conditions can co-exist and their clinical pictures may overlap, anxiety symptoms are common and occur in 26–63.4% of patients with MS (28). This fact, in addition to the low number of patients with positive psychiatric history in our sample, could explain the association with anxiety and not depression.
Although our data reported a correlation between the EDSS score and age (p < 0.0001), no correlation was found between the EDSS and the GAD-7 or PHQ-9 scales. Similarly, a Norwegian study concluded that the EDSS score was not associated with psychiatric disorders (35). On the other hand, Alsaadi et al. reported a significant association between the EDSS scores and mood disorders (36). One possible explanation for this finding is that the EDSS score focuses mainly on physical disability and motor system dysfunction, rather than on direct relation to mood, cognitive, or psychiatric manifestation (37).
The results of this study must be considered within the context of certain limitations. Owing to the limited number of patients with MS visiting the clinic, the sample size of the study was small. However, this was compensated for by optimizing the quality of the data collected for each patient; therefore, it can be as representative as possible. Subsequent studies should include more participants and a larger sample to assess more demographic as well as MS-related variables, such as different MS phenotypes, which was a limitation in the present study. Moreover, the study relied on PHQ-9 and GAD-7, which are self-administered assessment tools, and the definitive diagnosis can only be made on clinical grounds with a full psychiatric assessment of the patients. Furthermore, a clinical diagnostic interview, such as the MINI International Neuropsychiatric Interview, might be considered in future studies. In addition, patients with MS have a higher chance of experiencing depression and anxiety; therefore, clinicians should routinely screen for these psychiatric disorders.
In conclusion, the current study demonstrated a higher prevalence of major depression and generalized anxiety disorder in patients with MS than in the general population. Female patients generally scored higher on the PHQ-9 and GAD-7 scales than male patients. No correlation was found between the EDSS score and disease duration with regard to the risk of developing depression and anxiety. As depression and anxiety are prevalent comorbidities in patients with MS and could affect the disease course negatively, screening and early intervention are crucial.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Institutional Review Board, King Abdullah International Medical Research Center, Riyadh, Saudi Arabia. The patients/participants provided their written informed consent to participate in this study.
Author contributions
AMA, BA, ARA, and OB were responsible for the design and initial conception of the study. ARA, OB, EA, JA, AAl, and OW participated in data acquisition and assembly. BA and AMA provided statistical expertise and carried out the analysis of the data. AA, YA, AAb, and SM critically revised the manuscript. All authors participated in initial drafting of the manuscript, reviewed, and approved the final draft of the manuscript.
Acknowledgments
The investigators would like to thank the data collectors for their effort in interviewing the participants and gathering the needed data. Also, we would like to acknowledge the great help from the research office at King Abdullah International Medical Research Center, Jeddah, Saudi Arabia, for their guidance throughout this project.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Tafti D, Ehsan M, Xixis KL. Multiple Sclerosis. Treasure Island (FL): StatPearls Publishing. (2022).
2. Ghasemi N, Razavi S, Nikzad E. Multiple sclerosis: pathogenesis, symptoms, diagnoses and cell-based therapy. Cell J. (2017) 19:1–10. doi: 10.22074/cellj.2016.4867
3. AlJumah M, Bunyan R, Al Otaibi, H. Rising prevalence of multiple sclerosis in Saudi Arabia, a descriptive study. BMC Neurol. (2020) 20:49. doi: 10.1186/s12883-020-1629-3
4. Multiple Sclerosis. Amboss. (2020). Available online at: https://www.amboss.com/us/knowledge/Multiple_sclerosis (accessed December 20, 2020).
5. de Cerqueira AC, de Andrade PS, Barreiros JM, Teixeira AL, Nardi AE. Psychiatric disorders in patients with multiple sclerosis. Compr Psychiatry. (2015) 63:10–4. doi: 10.1016/j.comppsych.2015.08.001
6. Beier M, D'Orio V, Spat J, Shuman M, Foley FW. Alcohol and substance use in multiple sclerosis. J Neurol Sci. (2014) 338:122–7. doi: 10.1016/j.jns.2013.12.029
7. Diaz-Olavarrieta C, Cummings JL, Velazquez J, Garcia de la Cadena C. Neuropsychiatric manifestations of multiple sclerosis. J Neuropsychiatry Clin Neurosci. (1999) 11:51–7. doi: 10.1176/jnp.11.1.51
8. Chalah MA, Ayache SS. Psychiatric event in multiple sclerosis: could it be the tip of the iceberg? Braz J Psychiatry. (2017) 39:365–8. doi: 10.1590/1516-4446-2016-2105
9. Boeschoten RE, Braamse AMJ, Beekman ATF, Cuijpers P, van Oppen P, Dekker J, et al. Prevalence of depression and anxiety in multiple sclerosis: a systematic review and meta-analysis. J Neurol Sci. (2017) 372:331–41. doi: 10.1016/j.jns.2016.11.067
10. Pujol J, Bello J, Deus J, Martí-Vilalta JL, Capdevila A. Lesions in the left arcuate fasciculus region and depressive symptoms in multiple sclerosis. Neurology. (1997) 49:1105–10. doi: 10.1212/WNL.49.4.1105
11. Bakshi R, Czarnecki D, Shaikh ZA, Priore RL, Janardhan V, Kaliszky Z, et al. Brain MRI lesions and atrophy are related to depression in multiple sclerosis. Neuroreport. (2000) 11:1153–8. doi: 10.1097/00001756-200004270-00003
12. Marrie RA, Fisk JD, Tremlett H, Wolfson C, Warren S, Tennakoon A, et al. CIHR Team in the Epidemiology and Impact of Comorbidity on Multiple Sclerosis. Differences in the burden of psychiatric comorbidity in MS vs the general population. Neurology. (2015) 85:1972–9. doi: 10.1212/WNL.0000000000002174
13. Marrie RA, Walld R, Bolton JM, Sareen J, Walker JR, Patten SB, et al. Estimating annual prevalence of depression and anxiety disorder in multiple sclerosis using administrative data. BMC Res Notes. (2017) 10:619. doi: 10.1186/s13104-017-2958-1
14. Beiske AG, Svensson E, Sandanger I, Czujko B, Pedersen ED, Aarseth JH, et al. Depression and anxiety amongst multiple sclerosis patients. Eur J Neurol. (2008) 15:239–45. doi: 10.1111/j.1468-1331.2007.02041.x
15. Marrie RA, Horwitz R, Cutter G, Tyry T, Campagnolo D, Vollmer T. The burden of mental comorbidity in multiple sclerosis: frequent, underdiagnosed, and undertreated. Mult Scler. (2009) 15:385–92. doi: 10.1177/1352458508099477
16. Alhussain H, Aldayel AA, Alenazi A, Alowain F. Multiple sclerosis patients in saudi arabia: prevalence of depression and its extent of severity. Cureus. (2020) 12:e7005. doi: 10.7759/cureus.7005
17. AlHadi AN, AlAteeq DA, Al-Sharif E, Bawazeer HM, Alanazi H, AlShomrani AT, et al. An arabic translation, reliability, and validation of Patient Health Questionnaire in a Saudi sample. Ann Gen Psychiatry. (2017) 16:32. doi: 10.1186/s12991-017-0155-1
18. Spitzer RL, Kroenke K, Williams JB, Löwe B, A. brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
19. Löwe B, Decker O, Müller S, Brähler E, Schellberg D, Herzog W, et al. Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Med Care. (2008) 46:266–74. doi: 10.1097/MLR.0b013e318160d093
20. Summaka M, Zein H, Abbas LA, Elias C, Elias E, Fares Y, et al. Validity and reliability of the arabic patient health questionnaire-9 in patients with spinal cord injury in Lebanon. World Neurosurg. (2019) 125:e1016–22. doi: 10.1016/j.wneu.2019.01.234
21. Patrick S, Connick P. Psychometric properties of the PHQ-9 depression scale in people with multiple sclerosis: a systematic review. PLoS ONE. (2019) 14:e0197943. doi: 10.1371/journal.pone.0197943
22. Mohr DC, Goodkin DE, Likosky W, Gatto N, Baumann KA, Rudick RA. Treatment of depression improves adherence to interferon beta-1b therapy for multiple sclerosis. Arch Neurol. (1997) 54:531–3. doi: 10.1001/archneur.1997.00550170015009
23. Samartzis L, Gavala E, Zoukos Y, Aspiotis A, Thomaides T. Perceived cognitive decline in multiple sclerosis impacts quality of life independently of depression. Rehabil Res Pract. (2014) 2014:128751. doi: 10.1155/2014/128751
24. Silveira C, Guedes R, Maia D, Curral R, Coelho R. Neuropsychiatric symptoms of multiple sclerosis: state of the art. Psychiatry Investig. (2019) 16:877–88. doi: 10.30773/pi.2019.0106
25. Arnett PA. Longitudinal consistency of the relationship between depression symptoms and cognitive functioning in multiple sclerosis. CNS Spectr. (2005) 10:372–82. doi: 10.1017/S1092852900022744
26. Berg D, Supprian T, Thomae J, Warmuth-Metz M, Horowski A, Zeiler B, et al. Lesion pattern in patients with multiple sclerosis and depression. Mult Scler. (2000) 6:156–62. doi: 10.1177/135245850000600304
27. Minden SL. Mood disorders in multiple sclerosis: diagnosis and treatment. J Neurovirol. (2000) 6:S160–7.
28. Marrie RA, Reingold S, Cohen J, Stuve O, Trojano M, Sorensen PS, et al. The incidence and prevalence of psychiatric disorders in multiple sclerosis: a systematic review. Mult Scler. (2015) 21:305–17. doi: 10.1177/1352458514564487
29. Altwaijri YA, Al-Habeeb A, Al-Subaie AS, Bilal L, Al-Desouki M, Shahab MK, et al. Twelve-month prevalence and severity of mental disorders in the Saudi national mental health survey. Int J Methods Psychiatr Res. (2020) 29:e1831. doi: 10.1002/mpr.1831
30. Sparaco M, Lavorgna L, Bonavita S. Psychiatric disorders in multiple sclerosis. J Neurol. (2021) 268:45–60. doi: 10.1007/s00415-019-09426-6
31. Ron MA, Logsdail SJ. Psychiatric morbidity in multiple sclerosis: a clinical and MRI study. Psychol Med. (1989) 19:887–95. doi: 10.1017/S0033291700005602
32. Pinkston JB, Alekseeva N. Neuropsychiatric manifestations of multiple sclerosis. Neurol Res. (2006) 28:284–90. doi: 10.1179/016164106X98170
33. Peres DS, Rodrigues P, Viero FT, Frare JM, Kudsi SQ, Meira GM, et al. Prevalence of depression and anxiety in the different clinical forms of multiple sclerosis and associations with disability: a systematic review and meta-analysis. Brain Behav Immun Health. (2022) 24:100484. doi: 10.1016/j.bbih.2022.100484
34. Hanna M, Strober LB. Anxiety and depression in Multiple Sclerosis (MS): Antecedents, consequences, and differential impact on well-being and quality of life. Mult Scler Relat Disord. (2020) 44:102261. doi: 10.1016/j.msard.2020.102261
35. Dahl OP, Stordal E, Lydersen S, Midgard R. Anxiety and depression in multiple sclerosis. A comparative population-based study in Nord-Trøndelag County, Norway. Mult Scler. (2009) 15:1495–501. doi: 10.1177/1352458509351542
36. Alsaadi T, El Hammasi K, Shahrour TM, Shakra M, Turkawi L, Mudhafar A, et al. Prevalence of depression and anxiety among patients with multiple sclerosis attending the MS Clinic at Sheikh Khalifa Medical City, UAE: cross-sectional study. Mult Scler Int. (2015) 2015:487159. doi: 10.1155/2015/487159
37. Meyer-Moock S, Feng YS, Maeurer M, Dippel FW, Kohlmann T. Systematic literature review and validity evaluation of the expanded disability status scale (EDSS) and the multiple sclerosis functional composite (MSFC) in patients with multiple sclerosis. BMC Neurol. (2014) 14:58. doi: 10.1186/1471-2377-14-58
Keywords: multiple sclerosis, autoimmune disease, central nervous system, psychiatric disorder, generalized anxiety disorder, major depression
Citation: Alswat AM, Altirkistani BA, Alserihi AR, Baeshen OK, Alrushid ES, Alkhudair J, Aldbas AA, Wadaan OM, Alsaleh A, Al Malik YM, Abulaban AA and Makkawi S (2023) The prevalence of major depression and generalized anxiety disorder in patients with multiple sclerosis in Saudi Arabia: a cross-sectional multicentered study. Front. Psychiatry 14:1195101. doi: 10.3389/fpsyt.2023.1195101
Received: 28 March 2023; Accepted: 04 August 2023;
Published: 29 August 2023.
Edited by:
Emanuele D'Amico, University of Foggia, ItalyReviewed by:
Mario Stampanoni Bassi, Mediterranean Neurological Institute Neuromed (IRCCS), ItalyVictor Rivera, Baylor College of Medicine, United States
Copyright © 2023 Alswat, Altirkistani, Alserihi, Baeshen, Alrushid, Alkhudair, Aldbas, Wadaan, Alsaleh, Al Malik, Abulaban and Makkawi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Seraj Makkawi, U2VyYWptYWtrYXdpQGdtYWlsLmNvbQ==
 Anas M. Alswat
Anas M. Alswat Bsaim A. Altirkistani
Bsaim A. Altirkistani Anas R. Alserihi
Anas R. Alserihi Osama K. Baeshen
Osama K. Baeshen Eythar S. Alrushid
Eythar S. Alrushid Joud Alkhudair
Joud Alkhudair Abdulaziz A. Aldbas
Abdulaziz A. Aldbas Osama M. Wadaan3
Osama M. Wadaan3 Seraj Makkawi
Seraj Makkawi