
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Psychiatry , 05 October 2023
Sec. Psychological Therapy and Psychosomatics
Volume 14 - 2023 | https://doi.org/10.3389/fpsyt.2023.1189970
Introduction: In recent decades, various new psychotherapy approaches have been developed in an effort to overcome issues of non-response, referred to as “third-wave psychotherapies.” How third-wave therapies perform in comparison to each other, to classical CBT, or other common comparators in the treatment of depression has not yet been systematically assessed.
Methods: We firstly determined the scope of the term “third-wave” by conducting a systematic search. The identified approaches were then used as search terms for the systematic review and network meta-analysis (NMA). We searched MEDLINE, CENTRAL, PsychINFO and Web of Science from inception until 31 July 2022. We assessed randomized controlled trials comparing third-wave psychotherapies to each other, CBT, treatment as usual (TAU), medication management, active control conditions, or waitlist (WL) in adult populations with depressive disorders. The treatments included were acceptance and commitment therapy, behavioral activation, cognitive behavioral analysis system of psychotherapy, dialectical behavioral therapy, mindfulness-based cognitive therapy, meta-cognitive therapy, positive psychotherapy and schema therapy. The primary outcome was depression severity (efficacy) at study endpoint, and the secondary outcome was all-cause discontinuation (acceptability). This review was registered in PROSPERO, identifier CRD42020147535.
Results: Of 7,971 search results, 55 trials were included in our NMA (5,827 patients). None of the third-wave therapies were more efficacious than CBT but most were superior to TAU [standardized mean differences (SMD) ranging between 0.42 (95% CI −0.37; 1.19) and 1.25 (0.48; 2.04)]. Meta-cognitive therapy (MCT) was more efficacious than three other third-wave therapy approaches. None of the third-wave treatments were more acceptable than WL or CBT. Twenty-seven percent of the trials were rated as low risk of bias. Confidence in the evidence was largely low according to GRADE. Inconsistency emerged for a small number of comparisons.
Interpretations: Third-wave therapies are largely efficacious and acceptable alternatives to CBT when compared to TAU, with few differences between them. The evidence so far does not point toward superiority or inferiority over CBT. Patient-level research may offer possibilities for tailoring individual psychotherapies to the needs of individual patients and future trials should make this data available. The evidence base needs to be broadened by sufficiently powered trials.
Depressive disorders represent a major challenge in public health, with a 12–month prevalence of 5.37%–6.9% in the European Union and an estimated lifetime prevalence of 6%–25% (1). Depression contributes significantly to the worldwide burden of disease and is globally ranked the 6th most common cause of disability–adjusted life years in the age group of 25–49 years (2).
In the treatment of major depressive disorder (MDD), psychotherapy is recommended as a first–line option by several treatment guidelines (3, 4). Different types of psychotherapy have demonstrated efficacy in the treatment of MDD (5), with response rates of 41% (compared with 17% in usual care) and a number needed to treat of 5.3 (6). In terms of the number of randomized controlled trials (RCT), cognitive–behavioral therapy (CBT) ranks first (7, 8) although other psychotherapy approaches, such as psychodynamic, or interpersonal psychotherapies (IPT), have been shown to be effective in the treatment of MDD (9–11) via several meta-analyses (12–14).
In the past decades, various new psychotherapeutic approaches have been developed, aiming to improve current ones (6, 15). These new approaches were jointly referred to as the “third-wave” of behavioral therapies (16). The first wave of behavioral therapy predominantly drew from the principles of operant classical conditioning; however, the second wave added the “C” to behavioral therapy to reflect the addition of cognitive components such as modifying dysfunctional beliefs, following the “cognitive revolution” of the 1970s. The third–wave of CBT encompasses a range of approaches (17). Hayes and Hoffmann (17) summarized four key features of third-wave CBT psychotherapies: a focus on context and function; being built on other strands of CBT; a focus on broad and flexible repertoires vs. signs and symptoms; and integrating humanistic, existentialist, analytical, or system-oriented approaches. Generally speaking, third-wave psychotherapies focus on patients’ relationships with a certain behavior or thought rather than on their respective content. Conceptually, foci on mindfulness, acceptance, relationships and meta-cognitions are added. Interventions most commonly referred to as third-wave psychotherapies are acceptance and commitment therapy (ACT), mindfulness-based cognitive therapy (MBCT), dialectical behavior therapy (DBT), functional-analytical psychotherapy (FAP), and behavioral activation (BA). Less frequently cited are meta-cognitive therapy (MCT), schema therapy (ST), integrative behavioral couples therapy (IBCT), cognitive behavioral analysis system of psychotherapy (CBASP), positive psychotherapy (PP), and compassion-focused therapy (CFT) (18).
Over the last decade, there has been a growing number of RCTs and meta-analyses investigating the efficacy of third-wave psychotherapies (19–22). Previous reviews and meta-analyses, however, did not focus on clinical depression solely but on a variety of disorders and conditions (16, 18), while others that focused on depression, pooled different third-wave psychotherapies into one category for meta-analytical comparison (23). In this article, we focused on patients with clinical depressive disorders and aimed to synthesize data on the efficacy of individual third-wave psychotherapies in this patient group. We firstly identified the scope of the concept of third-wave psychotherapies for the treatment of clinical depression using a systematic literature review. Secondly, based on the results of our preliminary review, we included in our analysis available efficacy and acceptability data of several third-wave psychotherapy approaches. We performed a network meta-analysis (NMA) to compare individual third-wave psychotherapies (a) to CBT; (b) to other common comparators, such as waitlist (WL), treatment as usual (TAU), medication management (MM), and active controls (ActiveCt; e.g., “sham” psychotherapy); and (c) head-to-head.
We registered the protocol in PROSPERO (CRD42020147535; Supplementary Text S1). We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis in its extended version for NMAs (24).
To firstly define the scope of interventions belonging to the category of third-wave psychotherapies, we combined information from previously published meta-analyses (16, 18) and a systematic database search in MEDLINE and PsycINFO from inception to 31 December 2019. We combined the search terms, “third-wave” and “depression.” The search yielded 137 articles in PsycINFO (books excluded) and 72 in MEDLINE, 24 of which were duplicates.
The literature search identified the following psychotherapies that were mentioned at least once as third-wave psychotherapies: ACT, BA, CBASP, CFT, DBT, emotion-focused therapy (EFT), FAP, IBCT, MCT, MBCT, mindfulness-based stress reduction (MBSR), rumination-focused CBT (RFCBT), PP, ST, and well-being therapy (WBT).
Based on these results of our search, we included all of the mentioned psychotherapies in our main search for the systematic review except for RFCBT because of its strong overlap with CBT and EFT because of its origin in client-centered therapy. We did not include MBSR since it was conceptualized for a broader health-related context, while MBCT is the depression-specific integration of mindfulness practice in a psychotherapy framework (25).
For our NMA, we searched several databases (MEDLINE, Cochrane CENTRAL, Web of Science, PsycINFO) from inception to 31 July 2022. We searched for RCTs using the search terms “depress*” or “depression” and the respective forms of treatment (Supplementary Text S2). We also searched trial registries clinicaltirals.gov and the International Clinical Trials Registry Platform (ICTRP) as well as dissertations (via PsycINFO) for any unpublished data. Studies were searched, screened, selected and data was extracted independently by two authors (CS, CH). Inconsistencies were resolved by discussion between the two authors in consultation with the third and the last author.
We included trials that compared third-wave psychotherapies:
a. with cognitive therapy (CT)/CBT; or
b. with a control group, such as
WL,
TAU (treatment as usual or care as usual commonly refers to a regimen of varying intensity. TAU does not follow a protocol that is structured within the trial. Most often, it includes antidepressant treatment and follow-up visits to a psychiatrist. Treatments comparing against TAU usually include TAU in the intervention group as well, i.e., they compare intervention + TAU vs. TAU),
MM (antidepressant medication treatment following a structured protocol or algorithm specified within the trial),
ActiveCt conditions (a condition structured within the trial that is roughly equal to treatment intensity in the intervention arm but not applying the active intervention. For example “sham” or “placebo” psychotherapies or psychoeducation only. Comparison against an ActiveCt condition is meant to test whether a treatment’s specific interventions are more efficacious than non-specific factors common to all psychotherapies); or
c. head-to-head.
A main rationale in clustering control conditions was to differentiate structured conditions (MM, ActiveCt) from non-structured ones (WL, TAU). The clustering criteria for nodes are in Supplementary Text S3. Further inclusion criteria were: Adult population, English or German language, a primary diagnosis of major depressive disorder (MDD) or episode, persistent depressive disorder (PDD) according to the DSM-IV or -5 criteria or ICD-10 criteria, depression severity was measured by standard measures of depressive symptoms (Supplementary Text S4; Supplementary Table S5); trials delivered inpatient or outpatient treatments face-to-face, in groups, digitally, or via telephone.
Patient populations with comorbid medical conditions or pregnant women were not excluded.
We defined the differences in depression severity between arms as our continuous primary outcome of efficacy. If data from several outcome measures were reported, we included data according to a prespecified hierarchy, favoring clinician-rated outcomes over self-report (Supplementary Text S4). As a proxy for acceptability, we included all-cause discontinuation as a dichotomous secondary outcome. All-cause discontinuation was defined as the number of patients who withdrew from the study after commencing treatment but before the endpoint. Primary outcome data was obtained at the endpoint of the intervention.
For efficacy, standardized mean differences (SMD) were calculated as Cohen’s d. The superiority of a treatment was expressed by a positive value. For acceptability, summary odds ratios (ORs) were calculated. An OR > 1 indicated a higher probability of discontinuation for the first than for the second treatment.
Effect estimates were synthesized using Bayesian random effects (RE) NMA assuming a common intertrial variance (heterogeneity, tau2). We used the package gemtc (26, 27) in RStudio (R version 4.2.1) (28) applying Monte Carlo Markov Chain sampling as implemented in JAGS, and BUGSnet (29) for network graphs. For continuous outcomes, normal likelihoods were assumed; for dichotomous outcomes, binomial likelihoods were assumed. Results are presented as relative effect sizes and ORs, with 95% credible intervals (CrIs). Vague prior distributions were assumed for the baseline effects, the treatment effects relative to the baseline effect (both normally distributed), and the heterogeneity (uniform distribution) (26). Model specification, parametrization of priors, and assessment of convergence are provided in Supplementary Text S6. Treatment rankings are reported as the surface under the cumulative ranking curve (SUCRA) (30). Inconsistency was assessed locally in node–splitting models as automated in gemtc (31) and globally by comparing the fit (deviance information criterion, DIC) of an inconsistency model (32). Pairwise meta-analyses were calculated in meta (33). Heterogeneity was assessed using the I2 statistic and p-values from Cochran’s Q-test. We tested for small study effects (publication bias) by calculating Egger’s test for pairwise comparisons with k 3 (34).
We assessed sources of heterogeneity in pre-specified meta-regression models: (1) high vs. low risk of bias; (2) manualized vs. non-manualized control conditions; and (3) severity of depression at baseline as a covariate. We performed post-hoc sensitivity analyses by (1) only including trials that focused on PDD and/or treatment-resistant populations, (2) excluding special/comorbid populations, and (3) excluding trials with WL or MM conditions since they might violate the transitivity assumption.
Risk of bias was assessed for the primary outcome using the Cochrane Collaboration’s risk of bias tool 2, which was adapted for psychological interventions given that participants are not blind to the intervention they receive (Supplementary Text S7) (35, 36). Risk of bias ratings were performed by two authors (CS and CH) and all disparities were solved by discussion. Confidence in effect estimates for efficacy outcomes was rated using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) framework, implemented in CINeMA (37).
The database search yielded 7,971 results. A total of 272 full-texts remained after excluding duplicates and screening titles and abstracts, 55 of which were eligible for inclusion in the NMA (Figure 1). No eligible trials were retrieved for WBT, FAP, or IBCT. The final set of 55 studies comprised 72 direct comparisons (Supplementary Table S8). The comparisons included 5,827 patients for efficacy, and 5,757 for acceptability data. A total of 3,009 patients were randomized to third–wave psychotherapies, and 2,818 patients were randomized to control conditions. The mean age of patients was 39.53 (SD 7.98) years (Supplementary Figure S9), the mean percentage of female participants was 65.5% (SD 18.5). Thirty-three studies investigated psychotherapy in a face-to-face format, 18 included group treatments, and four trials included internet- or telephone-delivered formats. The median duration of trials was 12 weeks (inter-quartile range 8–16). Sixteen trials recruited patients from the Americas, thereof 14 from the United States, 24 from Europe, three from Australia and New Zealand, and 12 from Asia, 10 thereof from Iran (Supplementary Table S10). All trials included patients diagnosed with MDD. In 16 trials, persistent and/or treatment-resistant courses were exhibited by at least 30% (mean 87.5%, SD 24.05) of patients. Four trials included special populations or patients with comorbidities: postpartum women, multiple sclerosis, physical disabilities, and chronic pain. Study characteristics are summarized in detail in Supplementary Table S11.
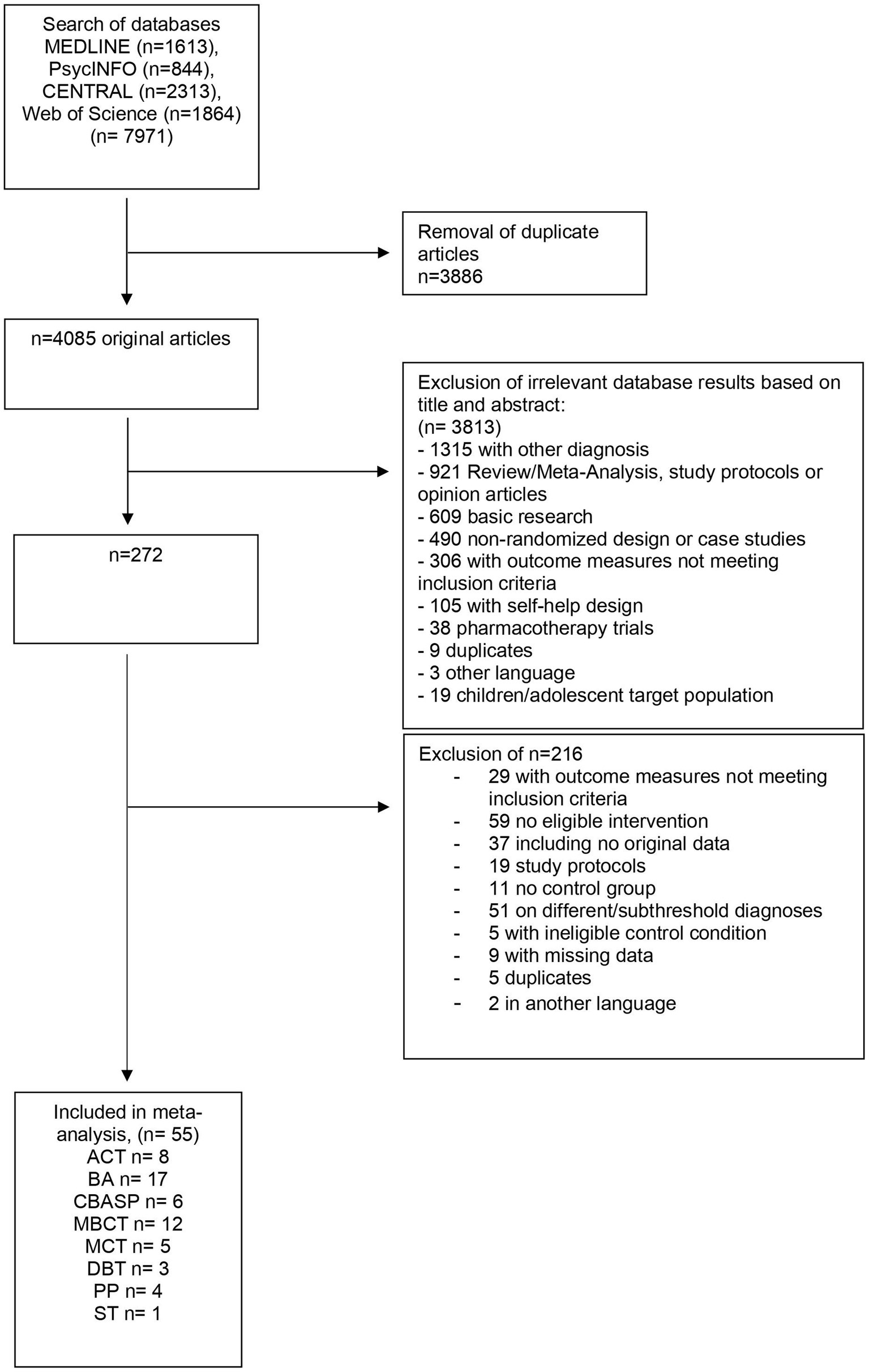
Figure 1. Flow-chart of the study selection process. ACT, acceptance and commitment therapy; BA, behavioral activation therapy; CBASP, cognitive behavioral analysis system of psychotherapy; DBT, dialectical behavioral therapy; MBCT, mindfulness-based cognitive therapy; MCT, meta-cognitive therapy; PP, positive psychotherapy; ST, schema therapy.
The network geometries for both efficacy and acceptability are displayed in Figures 2A,B. The efficacy network included four head-to-head comparisons between third-wave psychotherapies. Seventeen comparisons compared a third-wave psychotherapy with CT/CBT (n = 1,630), 13 with WL (n = 903), 17 with TAU (n = 938), six with MM (n = 1,286), and ten with an ActiveCt (n = 1,427; Supplementary Table S12). All third–wave treatments except DBT were directly compared with CT/CBT.
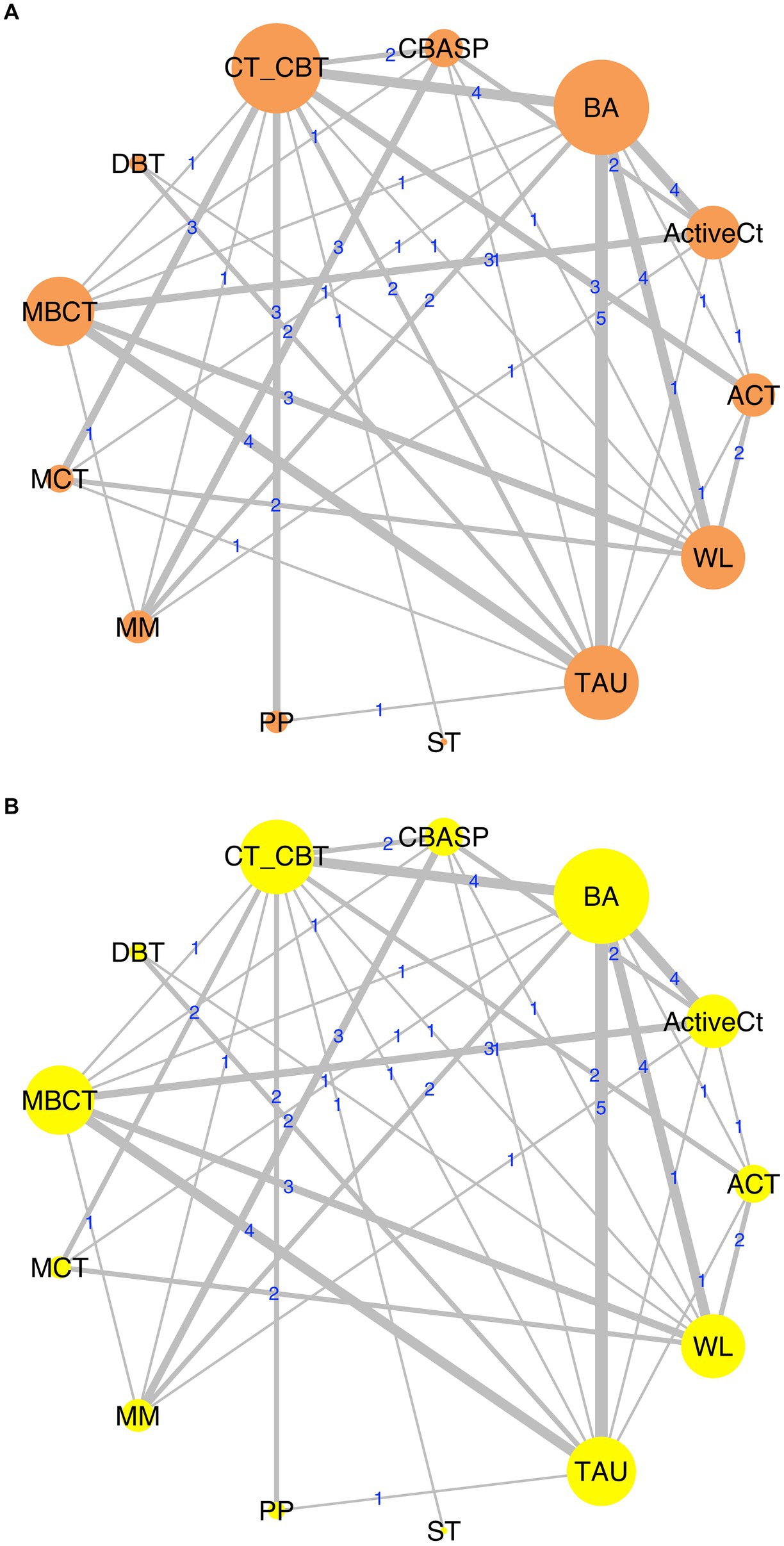
Figure 2. Network graphs of efficacy (A) and acceptability (B) data. ACT, acceptance and commitment therapy; ActiveCt, active control group; BA, behavioral activation therapy; CBASP, cognitive behavioral analysis system of psychotherapy; CT/CBT, cognitive therapy/cognitive-behavioral therapy; DBT, dialectical behavioral therapy; MBCT, mindfulness-based cognitive therapy; MCT, meta-cognitive therapy; MM, medication management; PP, positive psychotherapy; ST, schema therapy; TAU, treatment as usual; WL, waitlist.
None of the third-wave psychotherapies differed from CT/CBT in terms of efficacy. All third–wave psychotherapies except DBT and ST were significantly superior to WL and TAU conditions for lowering depression scores, with effect sizes ranging from 0.78 to 1.99 (Figures 3A,B, TAU in Supplementary Table S13). BA, ACT, PP, and MCT were more efficacious than ActiveCt. Only MCT was more efficacious than MM. In head-to-head comparisons (Table 1), MCT showed superior efficacy to MBCT (SMD 0.92, 95% CrI 0.23–1.65), DBT (SMD 1.27, 95% CrI 0.3–2.33) and CBASP (SMD 0.88, 95% CrI 0.14–1.67). MCT had the highest probability of all treatments to rank first in terms of efficacy, followed by BA. WL ranked last (Figure 4).
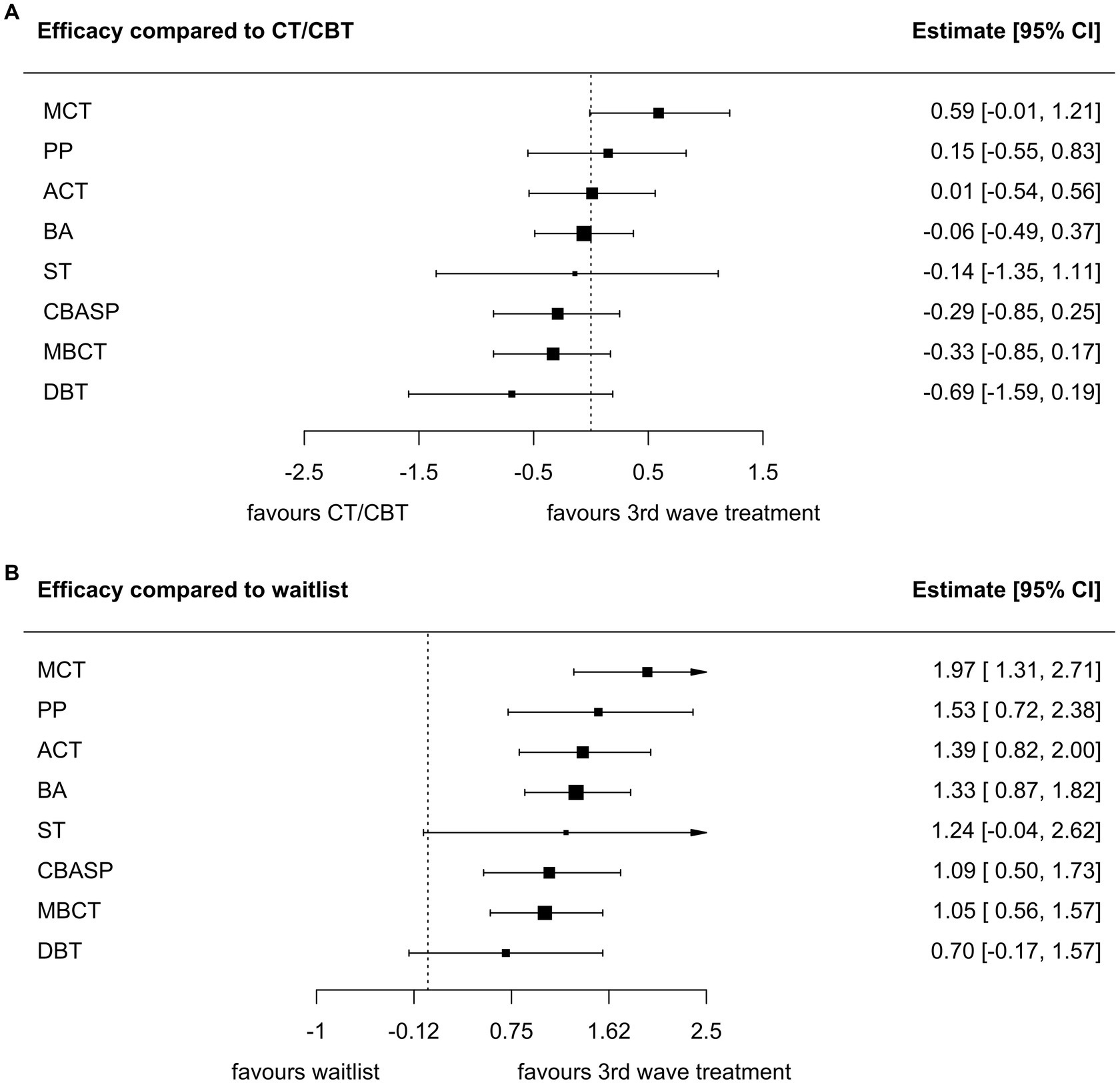
Figure 3. Forest plots of treatment efficacy of third-wave therapies in comparisons with CT/CBT (A) and WL (B) as treatments of reference. ACT, acceptance and commitment therapy; BA, behavioral activation therapy; CBASP, cognitive behavioral analysis system of psychotherapy; DBT, dialectical behavioral therapy; MBCT, mindfulness-based cognitive therapy; MCT, meta-cognitive therapy; PP, positive psychotherapy; ST, schema therapy.
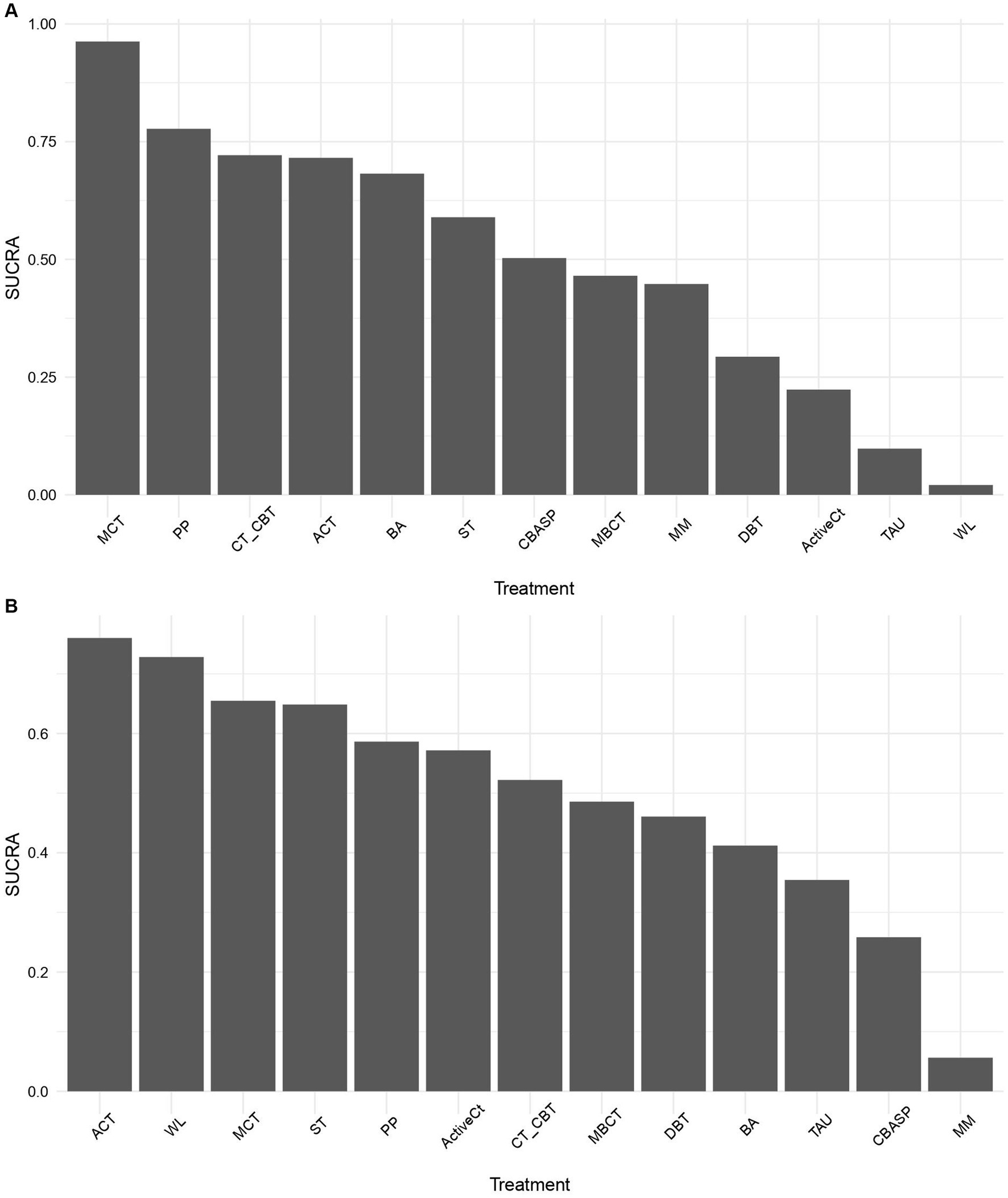
Figure 4. Surface und the cumulative ranking curve (SUCRA) plots of the efficacy (A) and acceptability (B) of third-wave psychotherapies. ACT, acceptance and commitment therapy; ActiveCt, active control group; BA, behavioral activation therapy; CBASP, cognitive behavioral analysis system of psychotherapy; CT/CBT, cognitive therapy/cognitive-behavioral therapy; DBT, dialectical behavioral therapy; MBCT, mindfulness-based cognitive therapy; MCT, meta-cognitive therapy; MM, medication management; PP, positive psychotherapy; ST, schema therapy; TAU, treatment as usual; WL, waitlist.
In terms of acceptability, all third-wave psychotherapies were tolerated as well as CT/CBT. Enrollment in a WL condition was not associated with higher dropout rates (Supplementary Table S14). None of the third-wave psychotherapies was more or less acceptable than TAU or ActiveCt. However, ACT had lower discontinuation rates than MM (OR 0.27 95% CrI 0.08, 0.88). ACT and WL had the highest probabilities of ranking first, meaning that discontinuation was least likely in these conditions, and CBASP and MM had the lowest (Figure 4).
Heterogeneity was estimated to be substantial (I2 = 77%) for efficacy measures and low (I2 = 36%) for acceptability measures (38). Egger’s test for small study effects was significant for two comparisons (MBCT vs. TAU and CBASP vs. MM). Summaries of all estimates and pairwise meta–analyses are reported in Supplementary Tables S13–S15 and Supplementary Text S16. The consistency models showed a better trade-off between model fit and complexity than the inconsistency models supporting the assumption of consistency in the networks (Supplementary Table S17).
Three studies contributed disproportionately high to the overall deviance in the efficacy data (Supplementary Figure S18). Patients in the respective control groups of these trials showed no improvement in depression severity over time resulting in large effect sizes. Their exclusion led to a 51% reduction in heterogeneity while the effect estimates of the NMA remained largely the same (Supplementary Table S19).
Locally, three out of 35 (8.5%) efficacy comparisons showed significant inconsistency (ACT vs. ActiveCt, MCT vs. WL, and BA vs. WL; Supplementary Table S21). Herein, for two of the inconsistent comparisons data was derived from the highly deviant trials mentioned above. For acceptability outcomes, five out of 34 comparisons (14.75%) were inconsistent (Supplementary Table S22).
Given the high proportion of studies investigating persistent and/or treatment-resistant depression (TRD; 28.6%), we performed a sensitivity analysis including only the respective subset of trials (16 trials; Supplementary Figure S23). Effect estimates for all treatments in this subnetwork trended toward a higher efficacy of the third-wave treatments (except for ST) compared with CT/CBT; however, all CrIs overlapped with the those of the full network, and included zero. Exclusion of trials with comorbidities reduced heterogeneity by 23%, and excluding trials with WL controls by 28%. Effect estimates did not change significantly. Inclusion of the covariates risk of bias, baseline depression severity (Supplementary Figure S24), and manualization of the control group did not significantly affect any of the estimates. The exclusion of WL controlled trials increased heterogeneity in the acceptability network by 9.55%. The exclusion of MM controlled trials did not alter effect estimates, except for a 17% increase in heterogeneity in the efficacy network. All subgroup and sensitivity analyses are in Supplementary Tables S19, S20.
Twenty-eight of the trials (51%) had adequate sequence generation and allocation concealment, 25 (45%) had low risk of bias due to masked assessments, 26 (47%) trials had low attrition rates or performed adequate intent-to-treat analyses and 20 trials (36%) were of low risk of reporting bias, 8 trials (15%) had retrievable protocols. Overall, 15 trials (27%) were rated as low risk of bias overall. Thirty-one (56%) showed some risk of bias and 9 (16%) trials had high risk ratings (Supplementary Figure S25). Certainty in direct comparisons was predominantly low to moderate according to GRADE criteria; only few direct comparisons were of very low certainty while indirect comparisons were rated mostly low and very low certainty (Supplementary materials S26–S29) (39). The references and raw data of all included trials are in Supplementary Table S30 and Supplementary material S31.
In this systematic review and NMA, we firstly identified the scope of the concept of “third–wave psychotherapies” in a systematic database search; and secondly aggregated 55 studies of the resulting treatments of ACT, BA, CBASP, DBT, MBCT, MCT, PP, and ST in over 5,800 patients treated for MDD and compared these treatments with each other and the most common comparators of CT/CBT (CBT for brevity), WL, MM, TAU, and ActiveCt. This is, to our knowledge, the first network meta-analysis that compared third-wave psychotherapies head-to-head, to CBT and other distinct control conditions for this indication.
All third-wave treatments were more efficacious than WL and TAU, except DBT and ST which did not show significant inferiority or superiority. DBT was conceived and is applied predominantly in the context of borderline personality disorder rather than MDD (40). It addresses other symptoms, which makes the lack of efficacy plausible. For schema therapy, the evidence for efficacy in MDD is still too sparse to draw firm conclusions (41, 42). ACT, BA, MBCT, MCT, and PP were more efficacious than ActiveCt conditions which suggests that specific interventions of the treatments are beneficial beyond non-specific psychotherapy effects. However, none of the third–wave treatments were more efficacious than CBT. In the head-to-head comparisons, only MCT was more efficacious than MBCT, DBT, and CBASP. However, the effect of MCT was partly driven by two trials in which patients in the control conditions did not improve on severity measures over the course of the trials, therefore possibly inflating MCT’s effect. In a more recent high quality trial (43) (n = 155), MCT did not show superiority over CBT in lowering depression scores in the primary outcome. This highlights the need for sufficiently powered trials that overcome the limitations of early small studies reporting large effect sizes (44).
Our results are in line with previous NMAs that compared different sets of psychotherapy approaches (e.g., CBT, interpersonal, psychodynamic, and problem-solving approaches) for unipolar depression which demonstrated that different psychotherapies are efficacious and acceptable, with only little to no significant differences between them (23, 45). However, to our knowledge, this is the first network meta-analysis that differentiates between individual therapies for this indication and thus allows comparison with each other and with established CBT.
The superior efficacy of an active psychological intervention over WL conditions replicates findings of several previous meta-analyses, in which WL conditions were thought to act as a nocebo (46–48). The exclusion of WL conditions as a whole in our sensitivity analyses did not affect effect estimates but reduced overall heterogeneity in the efficacy network.
In regard to acceptability, none of the third–wave treatments showed lower discontinuation rates than that of CBT or WL conditions. Unexpectedly, in absolute terms, WL conditions in our analysis had one of the lowest attrition rates. Previous research on psychotherapy trials has shown that an average of 20% of patients with depression withdraw from participation in psychotherapy trials before the endpoint (49). Moreover, study discontinuation in psychotherapy trials is partly due to the early benefit from treatment (50). If participants who benefit early are excluded from the analysis, the actual effect size may be underestimated and non–acceptability may be overestimated. In contrast, participants randomized to WL conditions may wait until the end of the trial because they continue to require treatment. The opposite effect of lower acceptability, that is, higher attrition, of psychological interventions compared with WL has been shown elsewhere (23).
Notably, all studies were published in the past 20 years, which reflects the dynamic developments in the field of psychotherapy for depression. The developments have been driven and informed by high rates of treatment resistance to well-established psychotherapies, such as CBT and psychodynamic approaches. Our findings do not provide evidence for superiority or inferiority of third–wave approaches over CBT. What might be the reasons for this? Firstly, equal efficacy between treatments does not render them equal or obsolete. Equally effective therapies can and should co-exist since population-level efficacy does not translate into individual response probabilities. As with first-line antidepressant medication, patients need alternatives to choose from. Secondly, global equal efficacy might obscure heterogeneity in the spectrum of depressive disorders which is reflected in treatment resistance. Persistently depressed patients, for example, often present with distinctive complicating features (51, 52). In our sensitivity analysis that included only studies in TRD and PDD populations, third–wave psychotherapies showed a trend toward superiority compared to CBT. Therefore, patient-level variables that mediate differential treatment responses need to be identified, such as experiential avoidance mediating response in studies comparing CBT and ACT (53) or childhood trauma mediating CBASP effects (54). Efforts in this direction are already being taken, by identifying response predictors that can be used by machine learning tools in the development of clinical decision support systems for psychotherapy (55).
In line with the notion of differential benefits between patients, a recent meta–analysis of variance ratios revealed significant heterogeneity in the treatment effects of CBT and third-wave psychotherapies. A finding which helps promote efforts to implement algorithms toward personalized psychotherapy (56) or process–based approaches for CBT (17).
Our study has certain strengths but also several limitations. One of its strengths is the rigorous inclusion criteria (clinical diagnosis of depression) which homogenizes the included samples. However, regarding transitivity of the network, some violations may arguably hold (57). For example, several trials included only patients with a history of PDD or TRD. The included samples consisted of moderately to severely depressed patients and for both conditions antidepressant medication is recommended. Moreover, concomitant treatment has been found to be superior to single treatment (58). It is therefore ecologically valid that most of the included trials intentionally applied or tolerated combined treatments. However, not all of them did and precision of effect sizes might be affected by the heterogeneity of treatment regiments. Possible violations of transitivity may result in statistical inconsistency (59), some of which was observed in our dataset. In our sensitivity analyses we accounted for these possible sources of inconsistency and were able to substantially reduce heterogeneity by removing outliers. Effect sizes were largely robust to our sensitivity analyses. A further limitation lies in the variety of control conditions. Despite their similarities, homonymous control conditions of different trials may offer substantially different treatments, especially if non–manualized, like TAU (60, 61). Lastly, only a 27% fraction of trials had a low risk of bias rating and the certainty in estimates was mostly low. In future studies, focus should preferentially shift toward showing that a “new” therapy is more efficacious, acceptable time or cost efficient than an established one in a patient group or subgroup.
Here we present a first NMA that integrates a systematic definition of the scope of third–wave therapies and the inclusion of data under rigorous criteria. In summary, the majority of third–wave psychotherapies can be regarded as more efficacious than TAU or WL. However, to date, there is no evidence suggesting that they overcome the limitations in efficacy of acceptability of CBT.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
CS and CH had full access to all data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. CS, SK, AG, PS, and E-LB conceived and designed the study. CS, CH, SK, and AG selected the articles and extracted the data. CS and CH analyzed the data. CS, SK, AG, PS, and E-LB interpreted the data. CS and SK prepared the original draft of the manuscript. All authors contributed to the article and approved the submitted version.
This work was supported by the Else Kröner-Fresenius-Stiftung (SK, grant number 2018_A142).
Dr. Guhn, Dr. Brakemeier, Dr. Sterzer, and Dr. Köhler have disclosed their affiliations with the “Deutschsprachige Gesellschaft für CBASP (DsG CBASP).” Moreover, all four authors actively engage in organizing workshops, delivering lectures, and contributing to books, book chapters, and articles related to CBASP. Dr. Brakemeier has also disclosed her membership in the “Deutsche Gesellschaft für Interpersonelle Psychotherapie (DG IPT)” and her involvement in disseminating IPT through training, books, and articles. Furthermore, Dr. Brakemeier has reported receiving grants from the following organizations: BMBF (Federal Ministry of Education and Research), DFG (German Research Foundation), State funds from Mecklenburg-Vorpommern, Bosch Stiftung, and Save the Children. Dr. Köhler has reported receiving grants from DFG and the Else Kröner-Fresenius-Stiftung. Dr Köhler has reported receiving speaker fees from Janssen-Cilag, Otsuka Pharma and Selfapy. Dr. Sterzer has reported receiving grants from BMBF, DFG and Stiftung Charité. Dr. Guhn has reported receiving grants from DFG.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1189970/full#supplementary-material
1. Lim, GY, Tam, WW, Lu, Y, Ho, CS, Zhang, MW, and Ho, RC. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci Rep. (2018) 8:2861. doi: 10.1038/s41598-018-21243-x
2. Vos, T, Lim, SS, Abbafati, C, Abbas, KM, Abbasi, M, Abbasifard, M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the global burden of disease study 2019. Lancet. (2020) 396:1204–22. doi: 10.1016/S0140-6736(20)30925-9
3. DGPPN B, KBV, AWMF für die Leitliniengruppe Unipolare Depression. S3-Leitlinie/Nationale Versorgungsleitlinie Unipolare Depression—Kurzfassung 2. Auflage. Version 1. (2017) Available at: www.depression.versorgungsleitlinien.de (Accessed 16 January 2022).
4. APA. Clinical practice guideline for the treatment of depression across three age cohorts. (2021). Available at: www.apa.org/depression-guideline (Accessed 16 January 2022).
5. Cuijpers, P, Karyotaki, E, de Wit, L, and Ebert, DD. The effects of fifteen evidence-supported therapies for adult depression: A meta-analytic review. Psychother Res. (2020) 30:279–93. doi: 10.1080/10503307.2019.1649732
6. Cuijpers, P, Karyotaki, E, Ciharova, M, Miguel, C, Noma, H, and Furukawa, TA. The effects of psychotherapies for depression on response, remission, reliable change, and deterioration: A meta-analysis. Acta Psychiatr Scand. (2021) 144:288–99. doi: 10.1111/acps.13335
7. David, D, Cristea, I, and Hofmann, SG. Why cognitive Behavioral therapy is the current Gold standard of psychotherapy. Front Psych. (2018) 9:4. doi: 10.3389/fpsyt.2018.00004
8. Butler, AC, Chapman, JE, Forman, EM, and Beck, AT. The empirical status of cognitive-Behavioral therapy: A review of meta-analyses. Clin Psychol Rev. (2006) 26:17–31. doi: 10.1016/j.cpr.2005.07.003
9. Elliott, K, Barker, KK, and Hunsley, J. Dodo bird verdict in psychotherapy. In: RL Cautin and SO Lilienfeld editors. The encyclopedia of clinical psychology. New Jersey: Wiley Blackwell. (2014). 1–5. doi: 10.1002/9781118625392.wbecp053
10. McAleavey, AA, and Castonguay, LG. The process of change in psychotherapy: common and unique factors. Psychother Res. (2015) 18:293–310. doi: 10.1007/978-3-7091-1382-0_15
11. de Felice, G, Giuliani, A, Halfon, S, Andreassi, S, Paoloni, G, and Orsucci, FF. The misleading dodo bird verdict. How much of the outcome variance is explained by common and specific factors? New Ideas Psychol. (2019) 54:50–5. doi: 10.1016/j.newideapsych.2019.01.006
12. Cuijpers, P, Andersson, G, Donker, T, and van Straten, A. Psychological treatment of depression: results of a series of meta-analyses. Nord J Psychiatry. (2011) 65:354–64. doi: 10.3109/08039488.2011.596570
13. Steinert, C, Munder, T, Rabung, S, Hoyer, J, and Leichsenring, F. Psychodynamic therapy: as efficacious as other empirically supported treatments? A meta-analysis testing equivalence of outcomes. Am J Psychiatry. (2017) 174:943–53. doi: 10.1176/appi.ajp.2017.17010057
14. Cuijpers, P, Berking, M, Andersson, G, Quigley, L, Kleiboer, A, and Dobson, KS. A meta-analysis of cognitive-behavioural therapy for adult depression, alone and in comparison with other treatments. Can J Psychiatr. (2013) 58:376–85. doi: 10.1177/070674371305800702
15. Emmelkamp, PMG. Do we really need a process-based approach to psychotherapy? World Psychiatry. (2021) 20:381–2. doi: 10.1002/wps.20889
16. Öst, LG. Efficacy of the third wave of Behavioral therapies: A systematic review and meta-analysis. Behav Res Ther. (2008) 46:296–321. doi: 10.1016/j.brat.2007.12.005
17. Hayes, SC, and Hofmann, SG. "third-wave" cognitive and Behavioral therapies and the emergence of a process-based approach to intervention in psychiatry. World Psychiatry. (2021) 20:363–75. doi: 10.1002/wps.20884
18. Dimidjian, S, Arch, JJ, Schneider, RL, Desormeau, P, Felder, JN, and Segal, ZV. Considering meta-analysis, meaning, and metaphor: A systematic review and critical examination of "third wave" cognitive and Behavioral therapies. Behav Ther. (2016) 47:886–905. doi: 10.1016/j.beth.2016.07.002
19. A-Tjak, JGL, Davis, ML, Morina, N, Powers, MB, Smits, JAJ, and Emmelkamp, PMG. A meta-analysis of the efficacy of acceptance and commitment therapy for clinically relevant mental and physical health problems. Psychother Psychosom. (2015) 84:30–6. doi: 10.1159/000365764
20. Negt, P, Brakemeier, EL, Michalak, J, Winter, L, Bleich, S, and Kahl, KG. The treatment of chronic depression with cognitive Behavioral analysis system of psychotherapy: A systematic review and meta-analysis of randomized-controlled clinical trials. Brain Behav. (2016) 6:e00486. doi: 10.1002/brb3.486
21. Ekers, D, Webster, L, Van Straten, A, Cuijpers, P, Richards, D, and Gilbody, S. Behavioural activation for depression; an update of meta-analysis of effectiveness and sub group analysis. PLoS One. (2014) 9:e100100. doi: 10.1371/journal.pone.0100100
22. Goldberg, SB, Tucker, RP, Greene, PA, Davidson, RJ, Kearney, DJ, and Simpson, TL. Mindfulness-based cognitive therapy for the treatment of current depressive symptoms: A meta-analysis. Cogn Behav Ther. (2019) 48:445–62. doi: 10.1080/16506073.2018.1556330
23. Cuijpers, P, Quero, S, Noma, H, Ciharova, M, Miguel, C, Karyotaki, E, et al. Psychotherapies for depression: A network meta-analysis covering efficacy, acceptability and long-term outcomes of all Main treatment types. World Psychiatry. (2021) 20:283–93. doi: 10.1002/wps.20860
24. Hutton, B, Salanti, G, Caldwell, DM, Chaimani, A, Schmid, CH, Cameron, C, et al. The Prisma extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. (2015) 162:777–84. doi: 10.7326/M14-2385
25. Crane, RS, Brewer, J, Feldman, C, Kabat-Zinn, J, Santorelli, S, Williams, JM, et al. What defines mindfulness-based programs? The warp and the weft. Psychol Med. (2017) 47:990–9. doi: 10.1017/S0033291716003317
26. van Valkenhoef, G, Lu, G, de Brock, B, Hillege, H, Ades, AE, and Welton, NJ. Automating network meta-analysis. Res Synth Methods. (2012) 3:285–99. doi: 10.1002/jrsm.1054
27. van Valkenhoef, G, Tervonen, T, de Brock, B, and Hillege, H. Algorithmic parameterization of mixed treatment comparisons. Stat Comput. (2012) 22:1099–111. doi: 10.1007/s11222-011-9281-9
28. R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing. Austria: Vienna (2013). Available at: http://www.R-project.org/
29. Beliveau, A, Boyne, DJ, Slater, J, Brenner, D, and Arora, P. Bugsnet: an R package to facilitate the conduct and reporting of Bayesian network meta-analyses. BMC Med Res Methodol. (2019) 19:196. doi: 10.1186/s12874-019-0829-2
30. Salanti, G, Ades, AE, and Ioannidis, JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. (2011) 64:163–71. doi: 10.1016/j.jclinepi.2010.03.016
31. van Valkenhoef, G, Dias, S, Ades, AE, and Welton, NJ. Automated generation of node-splitting models for assessment of inconsistency in network meta-analysis. Res Synth Methods. (2016) 7:80–93. doi: 10.1002/jrsm.1167
32. Dias, S, Welton, NJ, Sutton, AJ, Caldwell, DM, Lu, G, and Ades, AE. Evidence synthesis for decision making 4: inconsistency in networks of evidence based on randomized controlled trials. Med Decis Mak. (2013) 33:641–56. doi: 10.1177/0272989X12455847
33. Schwarzer, G. Meta: an R package for meta-analysis. R News . (2007) 7:40–45. Available at: https://cran.r-project.org/doc/Rnews/Rnews_2007-3.pdf
34. Egger, M, Davey, SG, Schneider, M, and Minder, C. Bias in meta-analysis detected by a simple, Graphical Test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
35. Higgins, JP, Altman, DG, Gotzsche, PC, Juni, P, Moher, D, Oxman, AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928. doi: 10.1136/bmj.d5928
36. Sterne, JAC, Savovic, J, Page, MJ, Elbers, RG, Blencowe, NS, Boutron, I, et al. Rob 2: A revised tool for assessing risk of bias in randomised trials. BMJ. (2019) 366:l4898. doi: 10.1136/bmj.l4898
37. Nikolakopoulou, A, Higgins, JPT, Papakonstantinou, T, Chaimani, A, Del Giovane, C, Egger, M, et al. Cinema: an approach for assessing confidence in the results of a network meta-analysis. PLoS Med. (2020) 17:e1003082. doi: 10.1371/journal.pmed.1003082
38. Turner, RM, Davey, J, Clarke, MJ, Thompson, SG, and Higgins, JP. Predicting the extent of heterogeneity in meta-analysis, using empirical data from the Cochrane database of systematic reviews. Int J Epidemiol. (2012) 41:818–27. doi: 10.1093/ije/dys041
39. Salanti, G, Del Giovane, C, Chaimani, A, Caldwell, DM, and Higgins, JP. Evaluating the quality of evidence from a network meta-analysis. PLoS One. (2014) 9:e99682. doi: 10.1371/journal.pone.0099682
40. Linehan, MM, and Wilks, CR. The course and evolution of dialectical behavior therapy. Am J Psychother. (2015) 69:97–110. doi: 10.1176/appi.psychotherapy.2015.69.2.97
41. Malogiannis, IA, Arntz, A, Spyropoulou, A, Tsartsara, E, Aggeli, A, Karveli, S, et al. Schema therapy for patients with chronic depression: A single case series study. J Behav Ther Exp Psychiatry. (2014) 45:319–29. doi: 10.1016/j.jbtep.2014.02.003
42. Renner, F, Arntz, A, Peeters, F, Lobbestael, J, and Huibers, MJH. Schema therapy for chronic depression: results of a multiple single case series. J Behav Ther Exp Psychiatry. (2016) 51:66–73. doi: 10.1016/j.jbtep.2015.12.001
43. Callesen, P, Reeves, D, Heal, C, and Wells, A. Metacognitive therapy versus cognitive behaviour therapy in adults with major depression: A parallel single-blind randomised trial. Sci Rep. (2020) 10:7878. doi: 10.1038/s41598-020-64577-1
44. Cuijpers, P. Are all psychotherapies equally effective in the treatment of adult depression? The lack of statistical power of comparative outcome studies. Evid Based Ment Health. (2016) 19:39–42. doi: 10.1136/eb-2016-102341
45. Barth, J, Munder, T, Gerger, H, Nuesch, E, Trelle, S, Znoj, H, et al. Comparative efficacy of seven psychotherapeutic interventions for patients with depression: A network meta-analysis. Focus. (2016) 14:229–43. doi: 10.1176/appi.focus.140201
46. Furukawa, TA, Noma, H, Caldwell, DM, Honyashiki, M, Shinohara, K, Imai, H, et al. Waiting list may be a nocebo condition in psychotherapy trials: A contribution from network meta-analysis. Acta Psychiatr Scand. (2014) 130:181–92. doi: 10.1111/acps.12275
47. Mohr, DC, Spring, B, Freedland, KE, Beckner, V, Arean, P, Hollon, SD, et al. The selection and Design of Control Conditions for randomized controlled trials of psychological interventions. Psychother Psychosom. (2009) 78:275–84. doi: 10.1159/000228248
48. Cuijpers, P, van Straten, A, Bohlmeijer, E, Hollon, SD, and Andersson, G. The effects of psychotherapy for adult depression are overestimated: A meta-analysis of study quality and effect size. Psychol Med. (2010) 40:211–23. doi: 10.1017/S0033291709006114
49. Swift, JK, and Greenberg, RP. A treatment by disorder meta-analysis of dropout from psychotherapy. J Psychother Integr. (2014) 24:193–207. doi: 10.1037/a0037512
50. O'Keeffe, S, Martin, P, Goodyer, IM, Wilkinson, P, Consortium, I, and Midgley, N. Predicting dropout in adolescents receiving therapy for depression. Psychother Res. (2018) 28:708–21. doi: 10.1080/10503307.2017.1393576
51. Schramm, E, Klein, DN, Elsaesser, M, Furukawa, TA, and Domschke, K. Review of dysthymia and persistent depressive disorder: history, correlates, and clinical implications. Lancet Psychiatry. (2020) 7:801–12. doi: 10.1016/S2215-0366(20)30099-7
52. Kohler, S, Chrysanthou, S, Guhn, A, and Sterzer, P. Differences between chronic and nonchronic depression: systematic review and implications for treatment. Depress Anxiety. (2019) 36:18–30. doi: 10.1002/da.22835
53. A-Tjak, JGL, Morina, N, Topper, M, and Emmelkamp, PMG. One year follow-up and mediation in cognitive Behavioral therapy and acceptance and commitment therapy for adult depression. BMC Psychiatry. (2021) 21:41. doi: 10.1186/s12888-020-03020-1
54. Nemeroff, CB, Heim, CM, Thase, ME, Klein, DN, Rush, AJ, Schatzberg, AF, et al. Differential responses to psychotherapy versus pharmacotherapy in patients with chronic forms of major depression and childhood trauma. Proc Natl Acad Sci U S A. (2003) 100:14293–6. doi: 10.1073/pnas.2336126100
55. Tanguay-Sela, M, Rollins, C, Perez, T, Qiang, V, Golden, G, Tunteng, JF, et al. A systematic meta-review of patient-level predictors of psychological therapy outcome in major depressive disorder. J Affect Disord. (2022) 317:307–18. doi: 10.1016/j.jad.2022.08.041
56. Kaiser, T., Volkmann, C., Volkmann, A., Karyotaki, E., and Cuijpers, P., Brakemeier E.-L. heterogeneity of treatment effects in trials on psychotherapy of depression. PsyArXiv [Preprint]. (12 March 2020) 2022).
57. Salanti, G. Indirect and mixed-treatment comparison, network, or multiple-treatments meta-analysis: many names, many benefits, many concerns for the next generation evidence synthesis tool. Res Synth Methods. (2012) 3:80–97. doi: 10.1002/jrsm.1037
58. Cuijpers, P, Noma, H, Karyotaki, E, Vinkers, CH, Cipriani, A, and Furukawa, TA. A network meta-analysis of the effects of psychotherapies, pharmacotherapies and their combination in the treatment of adult depression. World Psychiatry. (2020) 19:92–107. doi: 10.1002/wps.20701
59. Efthimiou, O, Debray, TP, van Valkenhoef, G, Trelle, S, Panayidou, K, Moons, KG, et al. Getreal in network meta-analysis: A review of the methodology. Res Synth Methods. (2016) 7:236–63. doi: 10.1002/jrsm.1195
60. Cuijpers, P, Karyotaki, E, Reijnders, M, and Ebert, DD. Was Eysenck right after all? A reassessment of the effects of psychotherapy for adult depression. Epidemiol Psychiatr Sci. (2019) 28:21–30. doi: 10.1017/S2045796018000057
Keywords: third-wave psychotherapies, cognitive-behavioral therapy, depression, major depressive disorder, psychotherapy, network meta–analysis
Citation: Schefft C, Heinitz C, Guhn A, Brakemeier E-L, Sterzer P and Köhler S (2023) Efficacy and acceptability of third-wave psychotherapies in the treatment of depression: a network meta-analysis of controlled trials. Front. Psychiatry. 14:1189970. doi: 10.3389/fpsyt.2023.1189970
Received: 20 March 2023; Accepted: 12 September 2023;
Published: 05 October 2023.
Edited by:
Georgios Paslakis, Ruhr University Bochum, GermanyReviewed by:
Mariusz Stanisław Wiglusz, Medical University of Gdansk, PolandCopyright © 2023 Schefft, Heinitz, Guhn, Brakemeier, Sterzer and Köhler. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cora Schefft, Y29yYS5zY2hlZmZ0QGNoYXJpdGUuZGU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.