
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 24 August 2023
Sec. Public Mental Health
Volume 14 - 2023 | https://doi.org/10.3389/fpsyt.2023.1188689
Introduction: Despite the widely known benefits of physical activity (PA), only 25% of people living with HIV (PLHIV) meet the WHO-recommended minimum PA levels. Consequently, it is essential to understand PA barriers and facilitators using objective measures. Although the Exercise Benefits and Barriers Scale (EBBS) is extensively used, its psychometric evidence is fragmented and has not been previously validated in PLHIV. This study aimed to translate and validate the EBBS Shona version in Zimbabwean PLHIV.
Methods: A cross-sectional study was used to recruit 567 PLHIV from four (4/9) randomly selected polyclinics (primary healthcare facilities) in urban Harare, Zimbabwe. We recruited adult patients (aged ≥18 years) with a confirmed diagnosis of HIV. Participants had to be willing to provide informed consent, not acutely unwell, and proficient in the Shona language. We used a forward-backwards translation method to translate the EBBS from English to Shona, a native Zimbabwean language. After cross-cultural adaptation, we pretested the draft version in 10 PLHIV to assess the face validity, understandability and cultural appropriateness using semi-structured interviews. Thereafter, the EBBS was administered to 567 consecutively-selected PLHIV. Factor analyses were performed for construct validity evaluation.
Results: Most participants were female (72.5%) and reached secondary/high school (78.8%), with a mean age of 39.9 (SD 12.1) years. The EBBS-Shona version yielded a four-factor solution consisting of three benefits factors and one barrier factor against the originally postulated six-factor structure. The EBBS-Shona yielded α = 0.85 and intraclass correlation coefficient = 0.86, demonstrating excellent reliability. Increased perception of exercise benefits was positively correlated with increased reports of physical activity, higher health-related quality of life and lower psychiatric morbidity; evidence for construct validity.
Discussion: This study demonstrates the validity and reliability of the EBBS-Shona version in Zimbabwean PLHIV. The EBBS-Shona version can be used for research and clinical purposes to glean data to inform the development, implementation, and evaluation of bespoke PA interventions for PLHIV.
The Sub-Saharan Africa (SSA) region has the world’s highest burden of HIV/AIDS (1). A concurrent high burden of non-communicable diseases (NCDs), including common mental health disorders (CMDs) in people living with HIV/AIDS (PLHIV), is obstructive to efforts to eradicate the HIV/AIDS epidemic (1, 2). For example, depression is thrice as common in PLHIV compared to the general population (3, 4). Poor mental health is regrettably associated with; high morbidity and mortality, high treatment costs, lower economic productivity, increased disability, and lower health-related quality of life (HRQoL) (4–8). Mental healthcare in PLHIV is traditionally mainly offered as pharmacotherapy and psychotherapy, with evolving evidence supporting the effectiveness of complementary interventions, including physical-activity-based regimens (9, 10). However, not all patients managed through pharmacotherapy and psychotherapy get into remission. Also, these core methods neither address the physical problems (e.g., loss in muscle strength, fatigue) associated with CMDs in PLHIV (9, 10). Furthermore, there is a vast mental health treatment gap in low-middle-income countries (LMICs) due to capital and human resource shortages (11, 12). For example, over 75% of PLHIV in LMICs with CMDs do not have equitable access to mental healthcare (11). There is a greater call to consider complementary treatment strategies, such as physical activity (PA), to close the mental health treatment gap in PLHIV (9, 10).
Physical activity is a low-hanging fruit as it is a cost-effective and scalable intervention for managing CMDs in PLHIV (12–14). Despite the demonstrated benefits of physical activity (PA), physical inactivity remains a global epidemic (15, 16). Nearly 30% of the global adult population (≈1.4 billion adults) are physically inactive and at high risk of NCDs (17). The burden of physical inactivity in PLHIV is even more significant, with only 25% of PLHIV meeting the minimum recommended PA levels (10, 18). Further, PLHIV people with CMDs are less likely to engage in PA and exhibit sedentary behaviour, creating a vicious cycle of NCDs risk (18, 19). The high prevalence of bodily pain, depression, HIV-related stigma, lack of social support, and opportunistic infections are salient predictors of physical inactivity in PLHIV (18, 19). Given the high burden of NCDs, the World Health Organization has put forward an ambitious target to decrease physical inactivity by 15% by 2030 as part of a holistic plan to curtail the burden of NCDs (20). The action plan recommends bespoke PA interventions targeting high-risk populations, including PLHIV (17, 20). More so, PA is essential in preventing and treating most NCDs (10, 14). A recent meta-analysis shows the effectiveness of PA in managing depression and anxiety in PLHIV, with large effects [SMD −0.84 (CI: −1.57; −0.011)] (14). Engagement in PA by PLHIV is associated with; increased CD4 count, improved cardiovascular fitness and endurance, lower blood pressure, improved self-esteem and body image, social connectedness, and decreased premature mortality, among many benefits (9, 10, 13, 14, 19). Taken together, PA engagement by PLHIV optimises; immune functioning, mental and physical health, social outcomes, economic productivity, and overall improvement in HRQoL (9, 10, 12–14, 19).
Promoting and implementing PA interventions is essential, particularly in the SSA region, which faces a dual, high burden of HIV/AIDS and NCDs (10). Unfortunately, physical activity is not integral to most HIV rehabilitation programs in SSA, with dropout rates as high as 30% (10). With the need to promote PA, there is a need to objectively measure PA, including understanding context-specific barriers, facilitators, and general awareness of the importance of PA (10, 12, 21). Perceived benefits and barriers to exercise are salient to PA engagement patterns (22). Importantly, there is a stern need to understand the psychosocial, socioeconomic, ecological and policy-related factors influencing PLHIV engagement in PA using validated, multidimensional outcome measures (10). One commonly used measure is the Exercise Benefits and Barriers Scale (EBBS) (12). Developed in the Unted States, the original EBBS has 43 items; 29 items measure the benefits of exercise, with 14 measuring barriers. The EBBS was initially validated in university students. It yielded a nine-factor solution (five benefits and four barriers factors) that accounted for 67.1% of the variance and yielded a Cronbach’s alpha of 0.74, showing adequate structural validity and reliability, respectively (23). Over decades, the EBBS has been extensively applied globally and has been translated and adapted in Iran (24, 25), Brazil (26), Malaysia (27), Mexico (28), and Turkey (29). However, its transcultural validity and reliability evidence are fragmented. Extensive use does not necessarily equate to psychometric robustness; this may cause inaccurate comparisons and conclusions. More so, follow-up validation studies have yielded differential factorial solutions, with some yielding 10- and 7-factor solutions (22, 30). To improve the EBBS psychometric performance, Koehn and Amiradollahian applied hierarchical confirmatory factor analysis to develop a concise six-factor, 26-item shortened version (22). The shortened version (EBBS-SF) was validated in 565 United Kingdom university students. It yielded excellent psychometric properties and can be of greater utility for routine research and clinical use due to its brevity (22) compared to the original 43-item version (23). However, it is essential to formally adapt and validate the EBBS-SF before use in different contexts. Also, it is paramount to apply robust translation methods to attain semantically and conceptually-equivalent language versions (31). Therefore, this study aimed to translate and validate the EBBS into Shona, a Zimbabwean native language. This study specifically assessed the structural validity, internal consistency, construct validity, known-group validity, and test re-test reliability of the EBBS-Shona version in PLHIV. There is a dearth of data on standardized, validated and culturally sensitive measures of PA in this population.
Participants were recruited from four randomly selected urban polyclinics (4/9) managed by the City of Harare Health Department. Zimbabwean public urban healthcare is structured into a three-tier system. Family healthcare facilities are the basic entry-level, with polyclinics and central hospitals constituting the second-and third-tier levels. HIV services, such as testing and pharmacotherapy, are provided at all primary healthcare facilities. There are dedicated HIV care clinics at all primary care facilities.
This study was done in two phases: the first stage involved the translation and adaptation of the EBBS into Shona. We utilised a forward-backwards translation method (31). First, two translators independently translated the EBBS from English to Shona. The forward translation was reconciled into one consolidated version through a panel discussion between the translators, the research assistant, and the researcher. Emphasis was on the attainment of a colloquial and conceptually-equivalent translation. After that, another set of two independent translators blindly back-translated the Shona version into English. Again, a second panel was convened between the translators and the research team. The emphasis was the attainment of a translation with literal and conceptual meaning. Third, the backward translation was compared against the original version through a panel discussion. We utilised professional and bilingual translators, i.e., they were all proficient in English and Shona. Last, cognitive debriefing interviews were performed by administering the EBBS-Shona version to 10 PLHIV to identify any problematic items and assess the understandability of the translation. Appropriate changes to the Shona version were made according to the feedback received from PLHIV. The EBBS-Shona version was validated using a cross-sectional design in the second phase.
We recruited adult patients (aged ≥18 years) proficient in Shona and with a confirmed diagnosis of HIV, according to doctors/clinician notes. Participants acutely unwell and/or requiring emergency treatment, with cognitive impairments and or in an intoxicated state on the day of data collection were excluded. Trained research assistants (Physiotherapy and Occupational Therapy graduate trainees) subjectively assessed the prospective participants’ mental state as indicated by the coherence in responses. Where appropriate, the Mini-Mental State Examination (cut-off point ≤23) was utilised to quickly assess a participant’s mental status (32).
According to Schmidt et al., the recommended recruitment ratio for confirmatory factory analysis is 5–20 candidates per item (33). Applying a 10:1 participant-to-item ratio, we set to recruit at least 260 participants. We doubled the minimum sample size to ensure two equal datasets for exploratory and confirmatory factor analysis. To evaluate the EBBS-Shona version test–retest reliability, we collected data from 50 randomly selected participants at baseline and after a fortnight per COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) guidelines (34).
Harare polyclinics were first stratified according to the three socioeconomic zones, i.e., low-, medium- and high-density strata. A polyclinic(s) was randomly selected from each of the strata. A priori ratio of 1:1:2 was used to select participants according to socioeconomic status proportionally. The stratification resulted in participants from high-density suburbs being selected more; they were 50% of the study population. Consecutive sampling was used to select cases.
Prospective participants were recruited consecutively as they presented for routine HIV care. On the day, trained research assistants first sensitised patients regarding study procedures and rights. Sensitisation was done as prospective participants waited to receive care in the treatment waiting areas. Participants meeting the inclusion criteria and interested in participating were taken to private spaces reserved for the study to provide written consent. The study questionnaires were interviewer or self-administered depending on the participants’ literacy level or preference for the data collection method. Based on the previous fieldwork, we set the threshold of self-completion to at least secondary education, i.e., 9 years from kindergarten education as a minimum. However, there are instances where participants opted for interviewer-administered mode, for instance, due to impairment, such as bodily pain.
The primary outcome measure was scores on the EBBS-Shona short version. We also collected secondary data, i.e., HRQOL, anxiety/depression, and physical activity.
• EEBS-SF – the EBBS-SF has 26 items: 19 measure the benefits of exercise, with seven measuring barriers. Perceived benefits of PA are classified into these four domains, i.e., life enhancement (LE), physical performance (PP), psychological outlook (PO), and social interaction (SI). Barriers are classified as facilities access (FA) or time expenditure (TE). The items on the EBBS are measured on a four-point Likert scale ranging from strongly disagree = 1 to strongly agree = 4. The scores range for the benefits and barrier domains are 4–76 and 4–28, respectively (22).
• EQ-5D 5 L – the EQ-5D is a generic, self-report HRQoL outcome measure. Using a five-point scale, respondents rate challenges with; mobility, self-care, usual, pain/discomfort, anxiety, and depression. The Shona version is validated, and normative utility scores are available for the Zimbabwean population (35).
• PHQ-4 – the PHQ-4 is a brief anxiety/depression screener. Respondents rate the frequency of experience of the enlisted anxiety/depressive symptoms in the previous 2 weeks on a four-point Likert scale ranging from “not at all = 0” to “all the time = 3” to give a cumulative score of 0–12. The PHQ-4 has been extensively used for clinical and research purposes and validated in PLHIV in the research setting (36).
• International physical activity questionnaire short form (IPAQ-SF) – the IPAQ-SF is an extensively used and psychometrically-robust seven-item PA measure (37). It assesses PA under the following four levels of intensity: vigorous-intensity activity (e.g., aerobics), moderate-intensity activity (e.g., leisure cycling), walking and sitting (37).
• The sociodemographic questionnaire extracted participants’ demographics, i.e., age, gender, education level, employment status, marital status, and financial status.
Descriptive statistics (e.g., frequencies, means) were used to describe participants’ characteristics and study outcome measures. Data were randomly split into two for exploratory and confirmatory factor analysis to evaluate the EBBS-Shona version’s structural validity – see Supplementary File S1 for the detailed analysis plan. Further, reliability as internal consistency and test–retest reliability were evaluated using Cronbach’s Alpha (criteria: α ≥ 0.7) and the Intraclass Correlation Coefficient (criteria: ICC ≥ 0.4), respectively. The Pearson correlation coefficient was applied to evaluate the construct validity by determining the correlation between EBBS-Shona scores and secondary outcome measures (e.g., depression); criteria, r ≥ 0.4. Known-group validity was assessed using t-tests by assessing differences in EBBS-Shona scores across gender. All analyses were done at α = 0.05 using SPSS (Version 28) and Stata (Version 17).
Ethical approval for the study was granted by the Stellenbosch University Health Research Ethics Committee (Ref: S22/06/111) and the Medical Research Council of Zimbabwe (Ref: MRCZ/B/2397).
Participants interpreted the EBBS-Shona alpha version during the cognitive debriefing stage to assess the understandability and appropriateness of the translation.
Most participants were female (72.5%), reached secondary/high school education (78.8%), married (51.1%), informally employed (33.2%), and reported inadequate finances (72.6%). The participants’ mean age was 39.9 (SD 12.1) years (Table 1).
There were spread responses on the EBBS, with the barriers sub-scale having the lowest means compared to the benefits sub-scale (Supplementary Table S2). Data were factorable given adequate sampling adequacy, i.e., Kaiser–Meyer–Oklin (KMO) =0.918 and 0.806, for benefits and barriers, respectively and statistically significant Bartlett Tests of Sphericity (p < 0.001). Items correlated reasonably with items within the same scale, with few correlations <0.3, and there was no multicollinearity. Except for the psychological outlook scale, the item-total correlation (ITC) range across the factors was reasonable in the range 0.575–0.746; Supplementary Table S3. The Kaiser criterion (Supplementary Table S4) and an inspection of the structure and pattern matrices (Table 2) supported the retention of one and three factors for barriers and benefits, respectively. Multiple cross-loadings were prevalent for factors one and two after Promax (oblique) rotation. The four factors accounted for 71.1% accumulative variance.
Table 3 shows an assessment of the congeneric and combined scale models, including the cross-validation of the EFA solution. Assessment of the congeneric models unequivocally supports a correlated four-factor model for the benefits subscale (Supplementary Table S5). For the barriers subscale, the results were indeterminant; the one-factor and correlated two-factor models are plausible, given the mixed evidence of fit indices. For the combined scale, the correlated six-factor model showed the best fit. However, the likelihood ratio (p < 0.001) and the RMSEA (=0.062) showed misfit, whilst the normed chi-square test displayed slight misfit (X2/df = 2.1). Last, the correlated 4-factor model gleaned from EFA displayed satisfactory model fit; the model parallels the performance of the correlated six-factor model. The 6-factor model demonstrates the greatest parsimony and is illustrated in Figure 1.
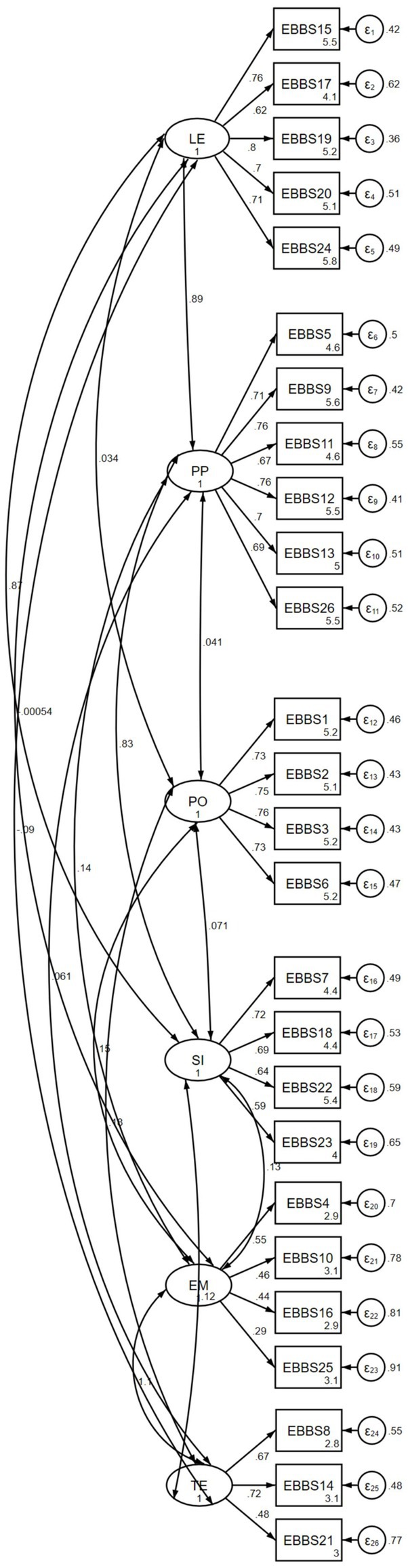
Figure 1. The EBBS six-factor model showing the correlations between the four benefits and two barriers factors.
Except for the barriers factors, the benefits sub-scales (α = 0.77–0.85) and summative EBBS scores (α = 0.85) collectively yielded excellent IC values (Table 4). The scale IC value did not improve by deleting any items (Supplementary Table S6), which is evidence of collective item reliability. The ICC (95% CI) for 52 participants at baseline and after 2 weeks was 0.87 (0.80:0.91); this is evidence of longitudinal stability.
Except for the psychological outlook (PO) domain, scores for all genders were comparable (Supplementary Table S7). Males were more likely to have a higher perception of the psychological benefits of exercise than females, with mean PO scores of 13.8 versus 13.1. the differences were statistically significant; t (df = 565) = 3.59, p < 0.001.
Increased perception of exercise benefits was poorly and positively correlated with increased reports of physical activity (r = 0.099; p = 0.019), higher HRQoL (r = −0.094; p = 0.026) and lower psychiatric morbidity (r = −0.118, p = 0.005). Last, the perceived barriers and benefits subscales were weakly and negatively correlated (r = −0.118; p = 0.005; see Supplementary Table S8).
We set out to translate, adapt, and validate the EBBS-Shona version in Zimbabwean PLHIV. To the best of our knowledge, this is the first study to formally validate the EBBS in PLHIV. Our data provide initial evidence of psychometric robustness regarding structural-, construct- and known-group validity and reliability (internal consistency and test–retest reliability). The EBBS-Shona version yielded a four-factor solution consisting of three benefits factors and one barrier factor against the originally postulated six-factor structure (22). However, our results demonstrate a second-order factor structure with items lumped into benefits and barriers (12, 22, 24). Structural validation results were contradictory; this is not uncommon (38). Exploratory factor analysis (EFA) and confirmatory factor analysis (CFA) supported four- and six factors, respectively. Structural validity is the most essential psychometric; the rest of the psychometric properties depend on the quality thereof (34, 38, 39). Only the physical outlook (PO) factor was replicated for benefits sub-scales in EFA. The homogeneous composition of the items can partially account for the congruency; items in this factor exclusively describe/measure the mental health benefits of physical activity (22, 23). However, the PO factor exhibited the lowest item-subtotal correlations (ITC range: 0.21–0.30) against the ITC range of 0.66–0.77 for the United Kingdom validation study (22). The discrepancies could be accounted for the lack of exact Shona words for “tension,” “stress,” and “mental health”; translation of these items was challenging. The remaining three benefits sub-scales (life enhancement, physical performance, and social interaction) loaded onto two distinct factors with several items cross-loading onto the two factors. The high prevalence of cross-loadings across the two factors could reflect cultural differences and perceptions of items under these factors.
Unlike the postulated two-factor solution, our outcomes support a one-factor solution for perceived barriers. This implies that participants could not differentiate between access-related and time-related barriers to physical activity. The high factor loadings and item-total correlations for the barriers sub-scale further support the one-factor solution. Again, cultural differences and a lack of linguistic diversity in the target language could account for the disparity. The Shona language has a limited vocabulary compared to English (40); this is potentially reflected in the conceptualisation of barrier-related factors as a solitary factor, as some of the words signifying different concepts were used interchangeably.
As for CFA, both four- and six-factor solutions are plausible, with the six-factor model being the most robust. However, for both models, the likelihood ratio showed a misfit, the normed chi-square test displayed a slight misfit, and the RMSEA showed evidence of misfit; these results are similar to the Persian and Mexican versions validation studies (24, 28). The likelihood ratio is prone to misfitting in large sample sizes, i.e., samples ≥200 (41); we analysed data for 283 participants. The normed Chi-square is considered a befitting alternative for large samples (38, 41); again, it showed a slight misfit. The RMSEA is a robust absolute fit index for CFA model estimation; it showed a model misfit. Normality violation could have resulted in model misspecification (42). Model misfits are prevalent in CFA due to the stringent assumption that an item must load onto one latent factor (38, 41), which may be impractical when analysing latent constructs such as perceived barriers and benefits. The strict assumption can lead to parameter estimation bias (38, 41). Multiple cross-loadings in benefits items during EFA testify to the potential failings of CFA assumptions (38). Collectively, the misfitting indices may imply a further need for improvements in the EBBS to increase factorial structure robustness. It may also be needful to apply other psychometric evaluation techniques, such as item response theory and exploratory structural equation modelling (ESEM), to overcome CFA limitations. For instance, in ESEM, cross-loadings across factors are permissible; this may yield a more parsimonious solution (38).
If EFA and CFA results are indifferent, CFA outputs usually take precedence (38). Here, mathematically, it was plausible to accept the six-factor model per CFA outputs. However, structural validation is an “art,” and there is a need to consider both the statistical outputs and a qualitative underpinning of the factors, including the understandability and interpretability of the factor solution (38, 41). Given the importance of model parsimony (42), it seems reasonable to adopt the four-factor solution of the EBBS-Shona version. More important, the EFA solution was succinct, accounting for 71.1% of the total variance, demonstrating the adequacy of the solution in measuring benefits and barriers to PA engagement. Also, the fit indices for the four-factor solution were marginally different from the six-factor solution and were within and or above the minimum set criteria (38, 41, 42). Nevertheless, the divergent factor analysis solutions have two-fold implications. First, the perceived barriers and benefits sub-scale should be interpreted separately, as the summative/combined score does not have a mathematically “intuitive” meaning. Second, there is a strong need to expand the content validity of the barriers scale; this may subsequently improve the factorial validity.
The EBBS-Shona is reliable, as evidenced by a high internal consistency at the scale level; this is comparable to previous studies, which also yielded high IC values between 0.67 and 0.83 (22, 25, 30). At the factor level, the two distinct barriers factors had sub-par IC levels. However, the one-factor solution was marginally above the minimum set criteria value (α = 0.72) (42). The lower IC values of the barriers items are unsurprising and comparable to other studies (22, 25). For example, the PO factor yielded α = 0.58 in an Iranian translation and validation study (25). Internal consistency values are a function of item numbers. Generally, the more items a factor consists of, the more it is likely to yield high reliability indices (43). The barriers scales have fewer items than the benefits scale (7 vs. 19), hence the anticipated discrepancies in IC values. There may be a need to increase the number of items to increase the construct and content validity of the barriers factor (22, 30). Still, the high IC values also support the robustness of the one-factor solution for barrier items. Also, similar to other studies (25, 29), our data show the longitudinal stability of the EBBS, as evidenced by high intraclass correlation coefficient values. It is doubtful that participants’ perceptions of the benefits and barriers could have changed drastically within 2 weeks. Collectively, all items on the EBBS-Shona consistently measured the same construct(s) within the 2 weeks.
We also tested the construct validity by assessing the correlations between EBBS scores and secondary outcome measures. Increased perception of exercise benefits was positively correlated with increased reports of physical activity, higher HRQoL, and lower psychiatric morbidity. This is theoretically plausible as previous studies have shown that higher perceived benefits are linked to increased PA engagement per the health beliefs model (10). The increased PA subsequently leads to improved mental health outcomes and HRQoL (10, 22). Conversely, more significant barriers were associated with low PA and a myriad of negative physical and psychosocial indices (9, 22). Also, our results concur with the health beliefs model regarding the negative correlation between perceived barriers and benefits (22, 30). Except for the psychological outlook sub-scale (PO), our findings do not seem to support gender differences in the perception of barriers and benefits; this follows previous studies (22, 30). A previous study postulated that males are likelier to have high perceptions of the recreational and social benefits of exercising than females (30); this may account for the higher PO scores in the current study. However, the low inter-item correlations for the PO sub-scale may have led to a spurious statistical finding; the factor may have unstable performance. Altogether, the EBBS equally performed across the genders, and scores can be used for direct comparison.
Study strengths include applying a robust translation process and using both EFA and CFA to test the EBBS-Shona dimensionality. This study builds upon the methodological limitations of previous studies. First, we used the generalised least squares, common factor analysis method (39). Other studies have incorrectly applied principal component analysis, which is not a true factor analysis method (23, 25, 28). Unlike previous studies that used orthogonal rotation (25, 28, 30), we applied oblique rotation to enhance factors’ interpretability in EFA. Orthogonal rotation must be used in rotating uncorrelated factors, a rare occurrence in behavioural sciences (39). Orthogonal rotation is inappropriate for the EBBS, given the negative correlation between perceived barriers and benefits (22, 30). Third, we used electronic data collection, including implementing mandatory responses and skip logic patterns which negate missing values, an essential methodological consideration for robust factor analysis outputs (43). However, facility-based, cross-sectional studies are prone to non-respondent selection and recall biases. For instance, our sample was gender-biased, with very few men (27.5%); our findings may have limited applicability. Future studies need to optimise the recruitment of men by applying stratified random sampling. The study may not be generalisable to PLHIV living outside Harare. Still, as the capital city, most people migrate to Harare for several reasons, including seeking jobs, so the sample will probably be reasonably representative given the study’s large sample. We recruited participants using consecutive sampling. Ideally, participants should have been recruited using random sampling, a requirement for factor analyses. However, random sampling was not feasible as participants arrived at different intervals, and the reduced patient volumes during the data collection could have prolonged the data collection period beyond the limits of the available study budget.
This study demonstrates the validity and reliability of the EBBS-Shona version in Zimbabwean PLHIV. The EBBS-Shona version can be used for research and clinical purposes to glean data to inform the development, implementation, and evaluation of bespoke PA interventions for PLHIV. Also, the EBBS could be applicable to other conditions or general populations in persons living in low-resource settings such as Sub-Saharan Africa, given the potential commonality in the need to increase populations’ physical activity. Also, barriers to PA engagement (e.g., lack of safe environment and equipment) are likely to be universal, hence the potential utility of the EBBS in non-HIV populations. Future studies are needed for continuous psychometric evaluations and gleaning normative data.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethical approval for the study was granted by the Stellenbosch University Health Research Ethics Committee (Ref: S22/06/111) and the Medical Research Council of Zimbabwe (Ref: MRCZ/B/2397). The patients/participants provided their written informed consent to participate in this study.
JD was primarily responsible for study conceptualisation, protocol writing, data collection, data analysis and drafting the first full version of the manuscript. TE was JD’s primary supervisor for the minor dissertation for the MSc Clinical Epidemiology program at Stellenbosch University. BD, MA, DC, and TE conceptualised the study and edited all versions of the manuscript. All authors contributed to the article and approved the submitted version.
We would like to acknowledge the research assistants for data collection efforts. Our sincere gratitude also goes to the participants for participating in this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1188689/full#supplementary-material
AIC, Akaike’s information criterion; BIC, Bayesian information criterion; CFA, confirmatory factor analysis; CFI, comparative fit index; CMDs, common mental health disorders; COSMIN, COnsensus-based Standards for the selection of health Measurement Instruments; EBBS, Exercise Benefits and Barriers Scale; EBBS-SF, Exercise Benefits and Barriers Scale Short Form; EFA, exploratory factor analysis; EQ-5D, EuroQol- 5 Dimension; HRQoL, health-related quality of life; ICC, Intraclass Correlation Coefficient; KMO, Kaiser-Meyer-Oklin; LFI, Tucker-Lewis Index; LMICs, low-middle-income countries; NCDs, non-communicable diseases; PA, physical activity; PHQ-4, Patient Health Questionnaire-4; PLHIV, people living with HIV/AIDS; RMSEA, The Root Mean Square Error of Approximation; SD, standard deviation; SD, the coefficient of determination; SMD, standardized mean difference; SRMR, standardized root mean squared residual; SSA, Sub-Saharan Africa.
1. Ward-peterson, M, Fennie, K, Mauck, D, Shakir, M, Cosner, C, Bhoite, P, et al. Using multilevel models to evaluate the influence of contextual factors on HIV / AIDS, sexually transmitted infections, and risky sexual behavior in sub-Saharan Africa: a systematic review. Ann Epidemiol. (2018) 28:119–34. doi: 10.1016/j.annepidem.2017.11.006
2. Abas, M, Nyamayaro, P, Bere, T, Saruchera, E, Mothobi, N, Simms, V, et al. Feasibility and acceptability of a task-shifted intervention to enhance adherence to HIV medication and improve depression in people living with HIV in Zimbabwe, a low-income country in sub-Saharan Africa. AIDS Behav. (2018) 22:86–101. doi: 10.1007/s10461-016-1659-4
3. Tsai, AC. Reliability and validity of depression assessment among persons with HIV in sub-Saharan Africa: systematic review and meta-analysis. J Acquir Immune Defic Syndr. (2015) 66:503–11. doi: 10.1097/QAI.0000000000000210
4. Wang, T, Fu, H, Kaminga, AC, Li, Z, Guo, G, Chen, L, et al. Prevalence of depression or depressive symptoms among people living with HIV/AIDS in China: a systematic review and meta-analysis. BMC Psychiatry. (2018) 18:1–14. doi: 10.1186/s12888-018-1741-8
5. Sabapathy, K, Hensen, B, Varsaneux, O, Floyd, S, Fidler, S, and Hayes, R. The cascade of care following community- based detection of HIV in sub-Saharan Africa – a systematic review with 90-90-90 targets in sight. PLoS One. (2018) 13:1–23. doi: 10.1371/journal.pone.0200737
6. Weinstein, TL, and Li, X. The relationship between stress and clinical outcomes for persons living with HIV/AIDS: a systematic review of the global literature. AIDS Care. (2016) 28:160–9. doi: 10.1080/09540121.2015.1090532
7. Bernard, C, Dabis, F, and de Rekeneire, N. Prevalence and factors associated with depression in people living with HIV in sub-Saharan Africa: a systematic review and meta-analysis. PLoS One. (2017) 12:1–22. doi: 10.1371/journal.pone.0181960
8. Ayano, G, Solomon, M, and Abraha, M. A systematic review and meta-analysis of epidemiology of depression in people living with HIV in East Africa. BMC Psychiatry. (2018) 18:1–14. doi: 10.1186/s12888-018-1835-3
9. Monteiro, FC, Schuch, FB, Deslandes, AC, Vancampfort, D, Mosqueiro, BP, Messinger, MF, et al. Perceived barriers, benefits and correlates of physical activity in outpatients with major depressive disorder: a study from Brazil. Psychiatry Res. (2020) 284:112751–7. doi: 10.1016/j.psychres.2020.112751
10. Vancampfort, D, Stubbs, B, and Mugisha, J. Physical activity and HIV in sub-saharan Africa: a systematic review of correlates and levels. Afr Health Sci. (2018) 18:394–406. doi: 10.4314/ahs.v18i2.25
11. Kulisewa, K, Stockton, MA, Hosseinipour, MC, Gaynes, BN, Mphonda, S, Udedi, MM, et al. The role of depression screening and treatment in achieving the UNAIDS 90–90–90 goals in sub-Saharan Africa. AIDS Behav. (2019) 23:153–61. doi: 10.1007/s10461-019-02593-7
12. Firth, J, Siddiqi, N, Koyanagi, A, Siskind, D, Rosenbaum, S, Galletly, C, et al. The lancet psychiatry commission: a blueprint for protecting physical health in people with mental illness. Lancet Psychiatry. (2019) 6:675–712. doi: 10.1016/S2215-0366(19)30132-4
13. O'Brien, KK, Tynan, AM, Nixon, SA, and Glazier, RH. Effectiveness of aerobic exercise for adults living with HIV: systematic review and meta-analysis using the Cochrane collaboration protocol. BMC Infect Dis. (2016) 16:1–56. doi: 10.1186/s12879-016-1478-2
14. Heissel, A, Zech, P, Rapp, MA, Schuch, FB, Lawrence, JB, Kangas, M, et al. Effects of exercise on depression and anxiety in persons living with HIV: a meta-analysis. J Psychosom Res. (2019) 126:109823–12. doi: 10.1016/j.jpsychores.2019.109823
15. Ding, D, Kolbe-Alexander, T, Nguyen, B, Katzmarzyk, PT, Pratt, M, and Lawson, KD. The economic burden of physical inactivity: a systematic review and critical appraisal. Br J Sports Med. (2017) 51:1392–409. doi: 10.1136/bjsports-2016-097385
16. Posadzki, P, Pieper, D, Bajpai, R, Makaruk, H, Könsgen, N, Neuhaus, AL, et al. Exercise / physical activity and health outcomes: an overview of Cochrane systematic reviews. BMC Public Health. (2020) 20:1–12. doi: 10.1186/s12889-020-09855-3
17. Guthold, R, Stevens, GA, Riley, LM, and Bull, FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob Health. (2018) 6:e1077–86. doi: 10.1016/S2214-109X(18)30357-7
18. Vancampfort, D, Mugisha, J, De Hert, M, Probst, M, and Stubbs, B. Sedentary behavior in people living with HIV: a systematic review and meta-analysis. J Phys Act Health. (2017) 14:571–7. doi: 10.1123/jpah.2016-0507
19. Vancampfort, D, Mugisha, J, De Hert, M, Probst, M, Firth, J, Gorczynski, P, et al. Global physical activity levels among people living with HIV: a systematic review and meta-analysis. Disabil Rehabil. (2018) 40:388–97. doi: 10.1080/09638288.2016.1260645
20. Hämäläinen, R, Breda, J, da Silva, GF, et al. New global physical activity guidelines for a more active and healthier world: the WHO regional offices perspective. Br J Sports Med. (2020) 54:1449–50. doi: 10.1136/bjsports-2020-103531
21. Garcia, L, Mendonça, G, Benedetti, TRB, Borges, LJ, Streit, IA, Christofoletti, M, et al. Barriers and facilitators of domain-specific physical activity: a systematic review of reviews. BMC Public Health. (2022) 22:1–22. doi: 10.1186/s12889-022-14385-1
22. Koehn, S, and Amirabdollahian, F. Reliability, validity, and gender invariance of the exercise benefits/barriers scale: an emerging evidence for a more concise research tool. Int J Environ Res Public Health. (2021) 18:1–20. doi: 10.3390/ijerph18073516
23. Sechrist, KR, Walker, SN, and Pender, NJ. Development and psychometric evaluation of the exercise benefits/barriers scale. Res Nurs Health. (1987) 10:357–65. doi: 10.1002/nur.4770100603
24. Farahani, LA, Parvizy, B, Mohammadi, E, Asadi-Lari, M, Kazemnejad, A, Hasanpoor-Azgahdy, SB, et al. The psychometric properties of exercise benefits/barriers scale among women. Electron Physician. (2017) 9:4780–5. doi: 10.19082/4780
25. Akbari Kamrani, AA, Zamani Sani, SH, Fathire-Zaie, Z, Bashiri, M, and Ahmadi, E. The psychometric characteristics of the exercise benefits/barriers scale among Iranian elderly. Iran J Public Health. (2014) 43:362–6.
26. Victor, JF, Ximenes, LB, and De Almeida, PC. Cross-cultural adaptation of the exercise benefits/ barriers scale (EBBS) for application in elderly Brazilians: preliminary version. Cad Saude Publica. (2008) 24:2852–60. doi: 10.1590/S0102-311X2008001200014
27. Kuan, G, Sabo, A, Sawang, S, and Kueh, YC. Factorial validity, measurement and structure invariance of the Malay language decisional balance scale in exercise across gender. PLoS One. (2020) 15:1–14. doi: 10.1371/journal.pone.0230644
28. Enríquez-Reyna, MC, Cruz-Castruita, RM, Ceballos-Gurrola, O, García-Cadena, CH, Hernández-Cortés, PL, and Guevara-Valtier, MC. Psychometric properties of the exercise benefits/barriers scale in Mexican elderly women. Rev Lat Am Enfermagem. (2017) 25:1–8. doi: 10.1590/1518-8345.1566.2902
29. Ortabag, T, Ceylan, S, Akyuz, A, and Bebis, H. The validity and reliability of the exercise benefits/barriers scale for Turkish military nursing students. South African J Res Sport Phys Educ Recreat. (2010) 32:55–70. doi: 10.4314/sajrs.v32i2.59297
30. Brown, SA. Measuring perceived benefits and perceived barriers for physical activity. Am J Health Behav. (2005) 29:107–16. doi: 10.5993/AJHB.29.2.2
31. Wild, D, Grove, A, Martin, M, Eremenco, S, McElroy, S, Verjee-Lorenz, A, et al. Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: report of the ISPOR task force for translation and cultural adaptation. Value Health. (2005) 8:94–104. doi: 10.1111/j.1524-4733.2005.04054.x
32. Schmitt, TA. Current methodological considerations in exploratory and confirmatory factor analysis. J Psychoeduc Assess. (2011) 29:304–21. doi: 10.1177/0734282911406653
33. Prinsen, CAC, Mokkink, LB, Bouter, LM, Alonso, J, Patrick, DL, de Vet, HCW, et al. COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual Life Res. (2018) 27:1147–57. doi: 10.1007/s11136-018-1798-3
34. Jelsma, J, Mhundwa, K, De Weerdt, W, De Cock, P, Chimera, J, and Chivaura, V. The reliability of the Shona version of the EQ-5D. Cent Afr J Med. (2001) 47:8–13. doi: 10.4314/cajm.v47i1.8584
35. Chibanda, D, Verhey, R, Gibson, LJ, Munetsi, E, Machando, D, Rusakaniko, S, et al. Validation of screening tools for depression and anxiety disorders in a primary care population with high HIV prevalence in Zimbabwe. J Affect Disord. (2016) 198:50–5. doi: 10.1016/j.jad.2016.03.006
36. Madhombiro, M, Dube, B, Dube, M, Zunza, M, Chibanda, D, Rusakaniko, S, et al. Intervention for alcohol use disorders at an HIV care clinic in Harare: a pilot and feasibility study. Addict Sci Clin Pract. (2019) 14:1–11. doi: 10.1186/s13722-019-0143-7
37. Marsh, HW, Guo, J, Dicke, T, Parker, PD, and Craven, RG. Confirmatory factor analysis (CFA), exploratory structural equation modeling (ESEM), and set-ESEM: optimal balance between goodness of fit and parsimony. Multivariate Behav Res. (2020) 55:102–19. doi: 10.1080/00273171.2019.1602503
38. Osborne, JW. What is rotating in exploratory factor analysis? Pract Assessment, Res Eval. (2015) 20:1–7.
39. Sylod, C, and Chivhanga, E. The diglossic relationship between Shona and English languages in the teaching and learning situation in Zimbabwe secondary schools. IOSR J Humanit Soc Sci. (2013) 12:43–50. doi: 10.9790/0837-1254350
40. Xia, Y, and Yang, Y. RMSEA, CFI, and TLI in structural equation modeling with ordered categorical data: the story they tell depends on the estimation methods. Behav Res Methods. (2019) 51:409–28. doi: 10.3758/s13428-018-1055-2
41. Hu, LT, and Bentler, PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model. (1999) 6:1–55. doi: 10.1080/10705519909540118
42. Sijtsma, K. On the use, the misuse, and the very limited usefulness of Cronbach’s alpha. Psychometrika. (2009) 74:107–20. doi: 10.1007/s11336-008-9101-0
Keywords: Exercise Benefits and Barriers Scale, translation, validity, reliability, HIV
Citation: Dambi JM, Domingue B, Abas M, Chibanda D and Esterhuizen TM (2023) Reliability and validity of the Shona version of the Exercise Benefits and Barriers Scale in Zimbabwean adult people living with HIV/AIDS. Front. Psychiatry. 14:1188689. doi: 10.3389/fpsyt.2023.1188689
Received: 17 March 2023; Accepted: 31 July 2023;
Published: 24 August 2023.
Edited by:
Wulf Rössler, Charité University Medicine Berlin, GermanyReviewed by:
Zukiswa Zingela, Nelson Mandela University, South AfricaCopyright © 2023 Dambi, Domingue, Abas, Chibanda and Esterhuizen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jermaine M. Dambi, amVybWFpbmVkYW1iaUBnbWFpbC5jb20=
†ORCID: Jermaine M. Dambi orcid.org/0000-0002-2446-7903
Ben Domingue orcid.org/0000-0002-3894-9049
Melanie Abas orcid.org/0000-0003-1716-5584
Dixon Chibanda orcid.org/0000-0003-2505-8607
Tonya M. Esterhuizen orcid.org/0000-0002-8703-1664
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.