- 1Connecticut Valley Hospital, Middletown, CT, United States
- 2Department of Psychiatry, University of Connecticut, Farmington, CT, United States
- 3Department of Psychiatry, St. Elizabeth’s Medical Center, Boston University, Boston, MA, United States
- 4Department of Psychiatry, University at Buffalo, Buffalo, NY, United States
- 5Department of Psychiatry, Jawahar Lal Nehru Memorial Hospital, Srinagar, India
- 6Dr. Kiran C. Patel Medical College and Research Institute, Bharuch, India
- 7Department of Medicine, Karachi Medical and Dental College, Karachi, Pakistan
- 8Touro College of Osteopathic Medicine, New York, NY, United States
- 9King Edward Medical University, Lahore, Pakistan
- 10Department of Psychiatry, Cornerstone Family Healthcare, New York, NY, United States
- 11Liaquat College of Medicine and Dentistry, Karachi, Pakistan
- 12Adesh Institute of Medical Sciences and Research, Bathinda, India
- 13Addiction Psychiatry, Rutland Regional Medical Center, Rutland, VT, United States
Background: The socio-cultural response to the Coronavirus Disease 2019 (COVID-19) and the level of adherence to evidence-based guidelines played a crucial role in determining the morbidity and mortality outcomes during the pandemic. This review aims to evaluate the impact of stigma and psycho-socio-cultural challenges on efforts to control the COVID-19 pandemic and to identify ways to mitigate such challenges in future pandemics.
Methods: Using keywords including COVID-19, coronavirus, stigma, psychosocial challenges, and others, the authors searched seven major databases with a time limitation of July 2021, which yielded 2,038 results. Out of these, 15 papers were included in this review.
Results: The findings of the review indicated that several psychosocial, socio-economic, and ethno-cultural factors are linked to the transmission and control of COVID-19. The research revealed that stigma and related psychosocial challenges and others, such as anxiety, fear, and stigma-driven social isolation, have resulted in significant mental health problems.
Discussion: The review underscores the negative impact of stigma on COVID-19 patients, survivors, and the general population. Addressing stigma and psychosocial challenges is crucial to effectively manage the current pandemic and to prevent similar challenges during future public health crises.
1. Introduction
The COVID-19 pandemic has triggered varying responses from cultures and nations across the world. The emergence of the novel SARS-CoV-2 virus led to the dissemination of information through various media channels in an effort to control its spread. However, the promotion of awareness was accompanied by a significant amount of false or misleading information related to COVID-19, which spread rapidly and had a negative impact on our ability to effectively manage the pandemic. This phenomenon, referred to as an “infodemic” (1), contributed to the development of stigma. Stigma, defined as an attribute that links a person to an undesirable stereotype (2), results in social labeling that hinders full acceptance by society and leads to discrimination, elevated individual stress, and healthcare disparities (2). The instinctual fear response to stigma can foster biases and discriminatory behaviors, particularly when coupled with a lack of knowledge. Despite efforts to mitigate its spread, false and unscientific information about COVID-19 and conspiracy theories continue to persist on the internet (2). The COVID-19 pandemic has led to the dissemination of false information and conspiracy theories through various media channels, which has contributed to stigma associated with the disease. The false information and conspiracy theories, such as the belief that 5G technology is responsible for the spread of COVID-19 (3), have spread quickly and led to significant healthcare disparities (4, 5). A survey conducted in 2020 found that 36% of individuals believed that the pandemic was planned when told so as part of the experiment (5). These conspiracy theories not only contribute to the spread of the virus but also cause significant stigma. To flatten the curve of positive cases and deaths from SARS-CoV-2, governments across the world implemented various isolating measures such as stay-at-home orders, social distancing, quarantining potentially infected individuals, face coverings, shutting down non-essential businesses and social ceremonies at varying levels of strictness. However, the strength of a culture’s response to an outbreak and willingness of the people to comply with the public health officials played a significant role in morbidity and mortality outcomes (6). Despite national and global health leaders’ insistence on these isolating measures, psychosocial cultural phenomena—stigma, conspiracy theories, individualism, and political agenda—remained obstacles to the containment of COVID-19. Disregarding the nuances of these obstacles and letting science hold complete sway could alienate the cultures and the people. This may compound barriers to managing the pandemic.
Ultimately, the healthiest horizon for all requires a compromise between the medical and the psychosocial-cultural sectors (7). Insufficient knowledge and awareness about the transmission, treatment, and prevention of SARS-CoV-2 can contribute to increased stigma in communities. To mitigate the impact of stigma, effective strategies can be implemented through social media to reduce fear and provide accurate and timely information about the high-risk groups, preventive measures, and treatment modalities. This scoping review aims to analyze the issues related to stigma and psychosocial challenges that have emerged during the COVID-19 pandemic, and to provide recommendations for authorities and healthcare professionals to address them in preparation for future pandemics.
2. Materials and methods
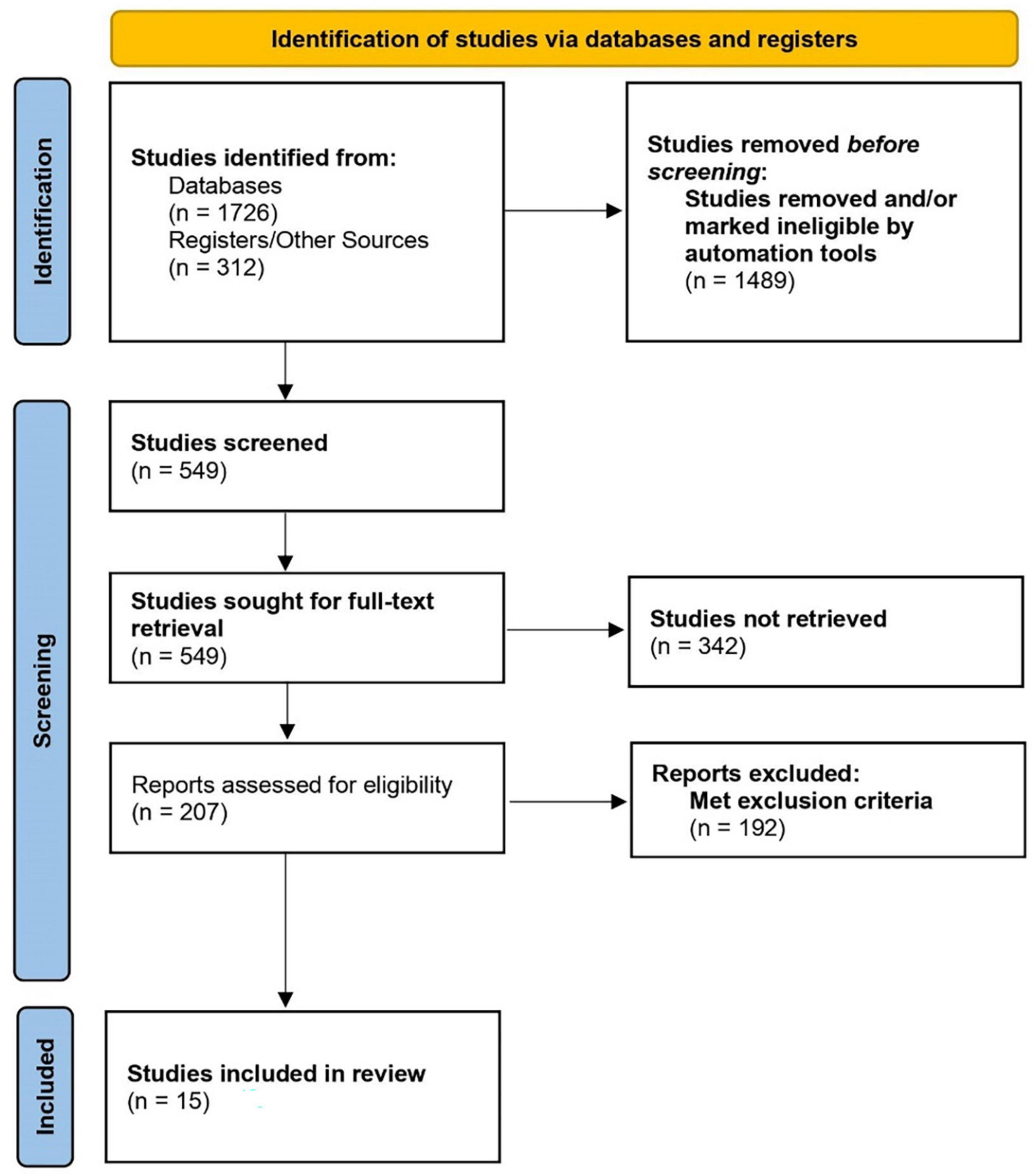
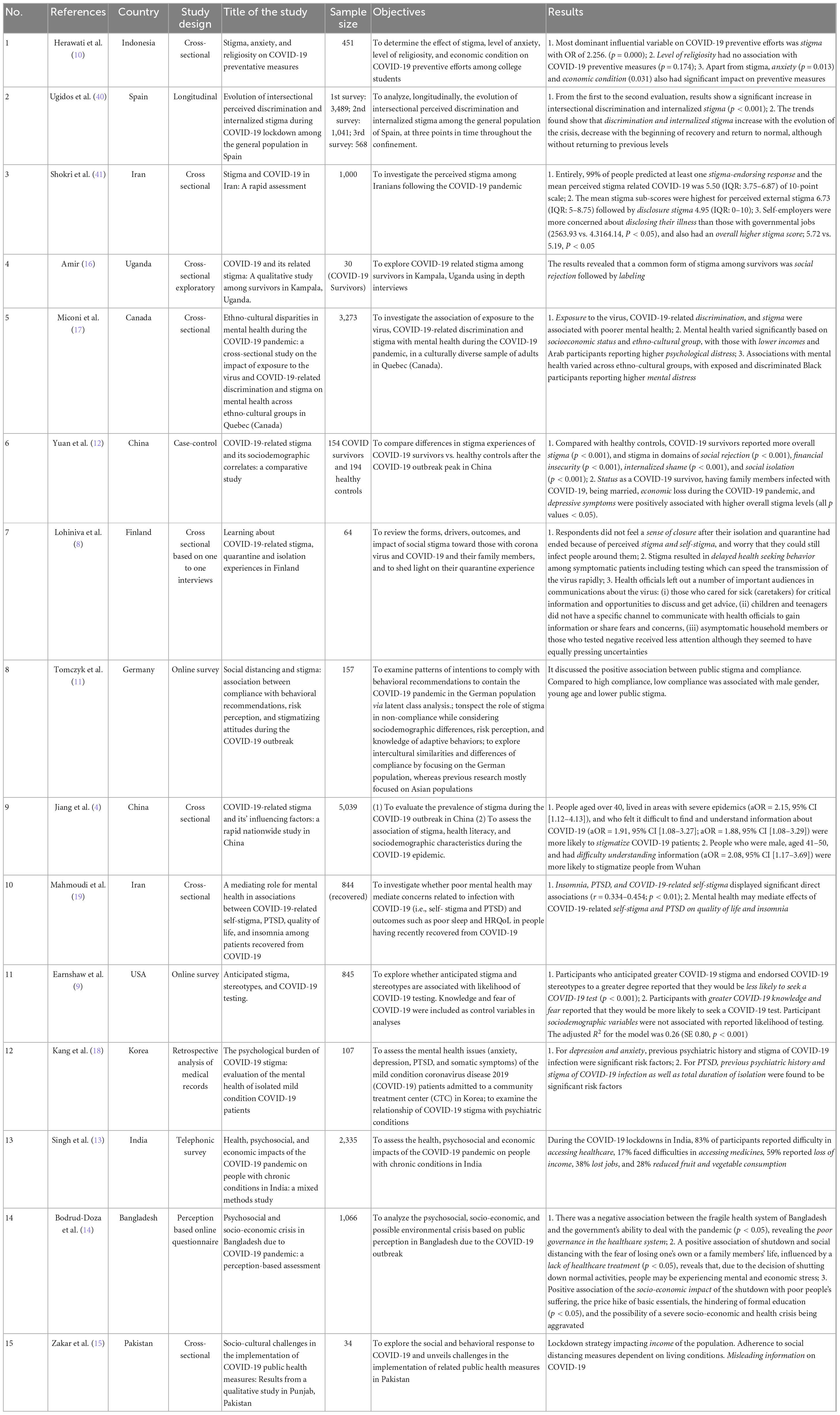
A literature search was performed following PRISMA guidelines using the following databases/registers: PubMed, Embase, Litcovid, bioRxiv, medRxiv, Web of Science, and PsychINFO, from January 2020 to July 2021. Gray literature was searched through a web search and Google Scholar. We used combinations of the following keywords applying BOOLEAN logic (AND/OR): “COVID-19, coronavirus, SARS-CoV-2”, “COVID- 19 pandemic” “Covid” AND “Stigma” OR “psychosocial challenges” OR “mental health” OR “cultural issues” OR “cultural challenges” OR “stigma” OR “mental health access”. The initial search was performed by authors RA and SB through these databases, which generated 2,038 reports. After excluding all duplicates and completely off-topic titles, 549 citations were left. We screened records for inclusion criteria and excluded 342 papers. The remaining 207 publications were manually screened by three authors (SS, HB, VS), any disagreements were mediated by the first author (SA). Studies were removed if they were commentaries, case reports, case series, opinions, workshops, unpublished data, and reviews. A total of 192 papers did not fit the inclusion criteria, resulting in 15 full-text articles that met the inclusion criteria (Figure 1). The included 15 studies are summarized in Table 1.
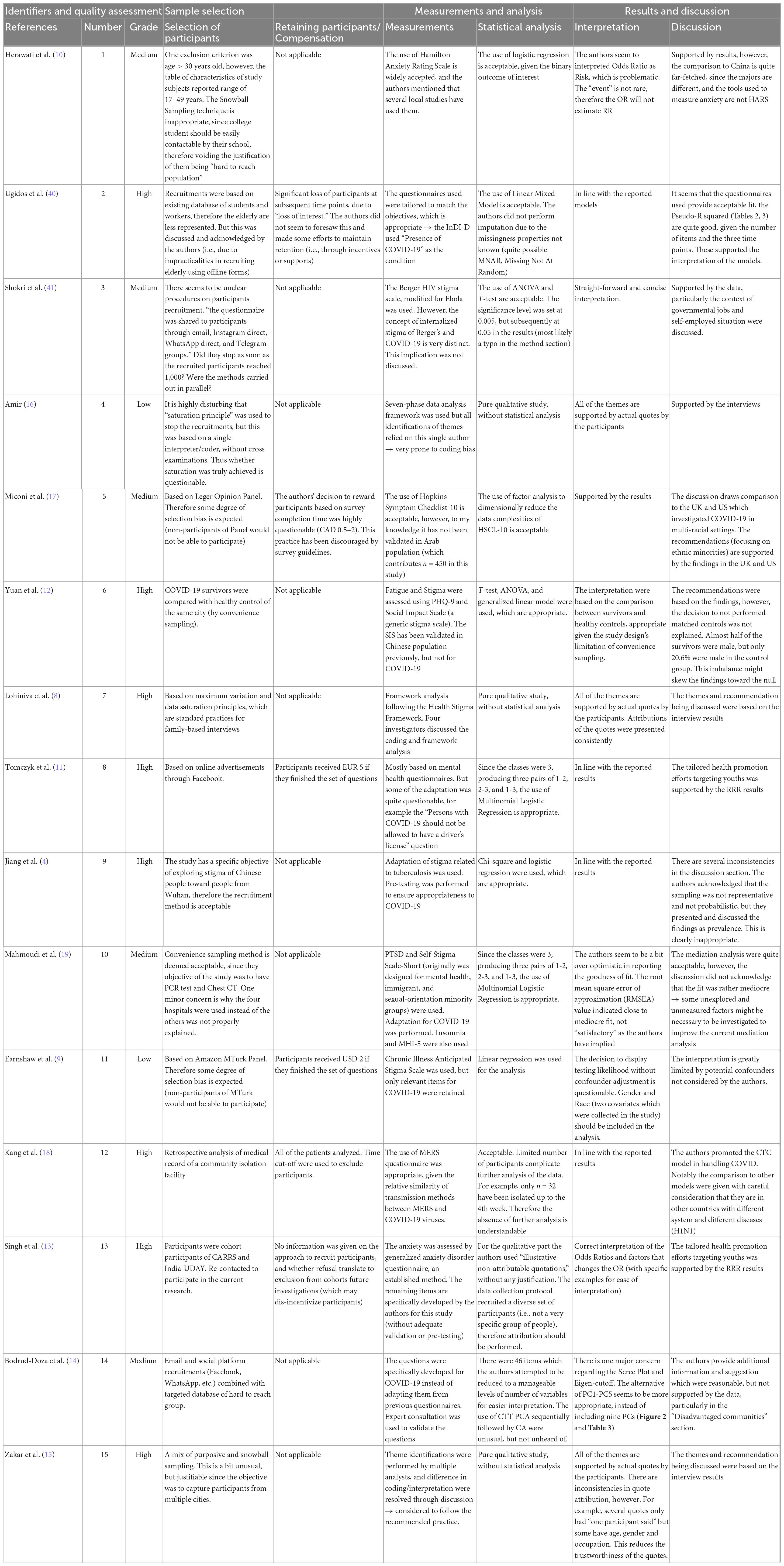
Table 2. Quality assessment, sample selection, measurement scales, analysis, and interpretation of findings.
3. Results
3.1. General population
Studies on stigma and COVID-19 have revealed that it affects not only the COVID-19 patients and survivors, but the general population as well. Stigma resulted in delayed health-seeking behavior and preventive efforts (8), with studies identifying anticipated stigma and stereotypes as barriers to COVID-19 testing (9). Herawati et al. (10) conducted a cross-sectional study with a total sample size of 451 respondents consisting of students in the field of health studies and religious studies in West Java, Indonesia. Data was collected using an online questionnaire, which consisted of variables of anxiety, stigma, economic conditions, religiosity, and prevention of COVID-19. The results showed that the most significant influential variable on COVID-19 preventive efforts was the stigma with an Odds Ratio (OR) of 2.256, that is, individuals who experienced high stigma had twice the risk of making a low preventive effort compared to individuals who experienced a low stigma. This study also observed that due to COVID-19, 62% of respondents reported a decrease in income. However, no relationship was seen between levels of religiosity and COVID-19 preventive efforts (10). Another study surveyed 157 German participants regarding their intention to comply with government issued behavioral recommendations. They found that young males were most likely to display low compliance, stressing the need for selective health promotion efforts. They also observed that public stigma had a positive association with compliance (11).
Certain variables are associated with a greater likelihood of one developing a stigma toward COVID-19, including lack of knowledge about the disease, self-employment, financial constraints, and pre-existing depression (9, 12). A cross-sectional survey by Jiang et al. (4) conducted in 31 provinces in China covering 5,039 respondents identified various factors related to COVID-19 stigma. This study indicated that participants over the age of 40, who were ethnic minorities and who felt it was difficult to find and understand information were more likely to stigmatize COVID-19 patients (4).
Apart from stigma, COVID-19 transmission led to significant economic, political, social, legal, and cultural challenges. Multiple studies have verified that COVID-19-related lockdown strategies have increased unemployment, leading to poverty, hunger, and restricted access to healthcare (13). This widespread economic instability has led to psycho-social and socioeconomic insecurity (14).
Zakar et al. (15) conducted a qualitative study based on 34 telephone or online in-depth interviews with participants from diverse age groups in the Punjab province of Pakistan. A semi-structured interview guide was used for data analysis, which included questions regarding problems the study participants experienced to observe public health measures in their households, in their neighborhoods, and social spaces. Probing questions were added to ask about social and cultural factors and challenges they faced in implementing COVID-19 protective measures. The study showed that apart from people’s poor understanding of the virus and the need for containment measures, false and misleading information about the coronavirus has significant consequences on containing the virus. This study also shed some light on religious practices or beliefs as another obstacle in flattening the COVID-19 curve. This has been observed in developing countries and several African communities (15).
3.2. COVID-19 patients and survivors
There are various types of stigma that COVID-19 patients and survivors have to deal with. Social rejection and labeling were among the most notable domains of stigma experienced by these people (16). Lohiniva et al., indicated that respondents did not feel a sense of closure after their isolation and quarantine had ended because of perceived stigma, self-stigma, and worry that they could still infect people around them (8). In addition to this; perceived external stigma, internalized stigma, disclosure stigma, and financial insecurity were commonly reported by the COVID-19 affected population. Yuan et al., conducted a cross-sectional study comprising 154 COVID-19 survivors and 194 healthy controls. COVID-19-related stigma were measured by the Social Impact Scale (SIS) and stigma differences between the two groups were compared. The study results found that COVID-19 survivors experience significantly more overall stigma and heightened stigma in domains of social rejection, financial insecurity, internalized shame, and social isolation compared with healthy controls. Another interesting finding of the study was that married people reported higher levels of stigma than those who were unmarried, which is consistent with earlier reports (12).
The magnitude of the impact of the pandemic was also influenced by the socio-economic and ethnocultural differences among the population. Miconi et al., performed an online survey to investigate the association of sociocultural characteristics and pandemic-specific risk factors (i.e., exposure to the virus, COVID-19-related discrimination, and stigma) with mental health during the COVID-19 pandemic in a culturally diverse sample of 3,273 adults in Quebec (Canada). The results showed that socioeconomic status (in terms of income and household size) and race/ethnicity were both associated with mental health, beyond the contributions of prior mental health, experiences of discrimination not related to COVID-19, and other sociodemographic variables. In comparison to other sociocultural groups, Black participants reported the worst mental health results when exposed to the virus and/or COVID-19-related discrimination (17).
Fear and stigma that accompany the pandemic have adversely affected the mental health of this subgroup in particular (12, 17). Literature on psychological consequences of stigma on this population reported that higher levels of depression, anxiety, insomnia, and Post Traumatic Stress Disorder (PTSD) were attributed to being the victim of stigma (18). Studies demonstrated that being subjected to stigma also had a detrimental effect on the quality of life of the patients (19).
3.3. Others
There were special subgroups of the population that have been overlooked during the pandemic and need special attention to alleviate their fears and concerns. Firstly, the caretakers who are ill informed and overly burdened required additional guidance and support. Secondly, children and teenagers were easy targets of stigma, as they do not have adequate opportunities to discuss their apprehension and gain correct information. Thirdly, when compared to those who tested positive, asymptomatic family members or those who tested negative received less care, while having equally significant concerns (8).
3.4. Quality appraisal of included studies
Despite the varying objectives and methodologies of the reviewed studies, four aspects merit being discussed to better inform future investigations of stigma and COVID-19. The four aspects were (1) measurement tools, (2) sample selection, (3) use of online platforms, and (4) design of qualitative studies. First, regarding the measurement tools, investigators have used stigma-related questionnaires originally developed for PTSD, AIDS, Ebola, mental health, or general health and Quality-of-Life questionnaires. Although several adaptations and pre-testing have been performed, we should caution that several aspects of the questionnaires might not be appropriate in the context of COVID-19. For example, the behaviors related to the disease transmissions were different for AIDS and COVID-19 (unprotected intercourse vs. not wearing a mask), and the barriers related to their protection efforts are different as well (buying condoms vs. masks). The use of MERS questionnaire by Kang et al. (18) might be more appropriate, given the relative similarity of transmission methods between MERS and SARS-CoV-2 viruses. Ideally, however, we should start developing tools that specifically explore COVID-19-related stigma.
Second, regarding sample selection, in all of the studies reviewed, investigators provided reasonable rationales and criteria for sample selection based on the objectives of the studies. However, we noted one inconsistency in the Herawati et al.’s (10) study, where age above 30 years was an exclusion criterion, but the range of participants was reported as 17–49 years without any explanation (we have sought further clarification from the authors). Despite the small number of participants in the case where consecutive sampling was performed (particularly for qualitative studies), the stopping criteria used were data saturation which we deemed as appropriate considering the objectives.
Third, given the COVID-19 restrictions on face-to-face surveys and interviews, several studies have relied on the use of online survey platforms. However, we found that except for Earnshaw et al. (9) most studies reported insufficient details on the timely completion of the surveys, data quality checks, and duplicate entry prevention measures. These were recommended measures to be taken to minimize bias in online surveys. For example, IP address checks (Internet Protocol address—the label connected to a computer network that uses the Internet) would deter multiple surveys completed by a single person motivated by financial rewards given by the completion of each survey. Similarly, utilizing a platform where durations of surveys were recorded would enable researchers to exclude surveys completed in an unreasonably short time (by automated software’s like Chat GPT or copied and pasted) to weed out bad data submitted.
Fourth, for the studies that have qualitative components in them, we found that the themes or ideas presented by the authors were well-supported by actual quotes from the participants. However, we did not find a study where participants provide corrections on the transcriptions and feedback on the findings. These two important aspects were in line with the consolidated criteria for reporting qualitative studies (COREQ) recommendations by Tong et al. (20), to ensure that the themes reported were in line with what the participants’ thoughts were. We hope that these steps were performed in future investigations.
We also analyzed the studies with some more merits to check the quality. All the included studies have well-defined research questions and objectives. Almost 50% (7) of the included studies have specified and defined the study population. One study (12) reported that the participation rate of eligible participants was at least 50%, others did not report. The studies (8–11, 13, 14) had included the participants from the same population during the defined period with prespecified inclusion and exclusion criteria, uniformly applied to all eligible participants. Only one study (16) reported justification of sample size, power description/variance, and effect estimates.
4. Discussion
This paper aimed to examine the psychosocial and cultural issues associated with the COVID-19 pandemic. We attempted to include as many studies as possible that examined stigma, mental health access, cultural barriers, myths, and misinformation associated with the COVID-19 pandemic. COVID-19 has resulted in a high level of stigma, anxiety, public confusion, and fear in the setting of many unknowns surrounding this virus. Stigma is a key component of inequalities, but it has been largely ignored in the debate over COVID-19’s response. Stopping and controlling pandemics, assisting societies in their recovery from pandemics, and achieving equitable development are all hampered by stigma. For example, African Americans are one of the highest-risk categories when it comes to dying from COVID-19, and yet they may be more resistant to being vaccinated. This mistrust toward people in authority can perhaps be traced back to the dark times of slavery, and has been perpetuated by the violence and apathy, exerted on them ever since. The community remembers, and naturally do not trust any governmental interference in their health, even if it is likely benevolent. The most prominent example of this is the Tuskegee syphilis experiment participants, who were unethically studied in the 1930s through the 1970s by the government in a study on syphilis (21). African American men infected with syphilis were deliberately left untreated to understand what happened to them over time (even when treatment became available and was being prescribed to others). This mistrust also led many African Americans men to fear that racial profiling and police harassment will worsen if they will wear masks (22). Those who choose not to wear a mask in order to not be perceived negatively in the eyes of a racist society can become potential vectors. The failure of the public healthcare system to take these factors into account presents a lose-lose situation.
Common miscomprehensions of what viruses and pandemics are and how they spread lead to resistance in people toward what can help; that being social distancing, temporary but aggressive lockdowns, and the stringent use of face masks. When communities blinded by religion or cultural habits do not look through a scientific lens; they may be more likely to overlook disease symptoms. This was the case in the early days of COVID-19, whose symptoms were deemed akin to those of the common cold or flu (23). An ongoing conflict between culturally appropriate and medically appropriate pandemic practices can cause psycho-cultural trauma. This can hinder the ability of individuals to cope with stressors and can make recovery difficult (24). Collective trauma (trauma that negatively impacts entire societies) leaves even longer-lasting effects with even fewer outlets available to manage despair or allow for cathartic emotional release (i.e., venting). The potential for mass trauma makes it crucial for governmental organizations and public health officials to work together to provide outreach and actively disseminate beneficial coping information.
This “us” vs. “them” dynamic indicates a way in which disease stigma can be viewed as a proxy for other types of fears like xenophobia. The pandemic risk associated with SARS-CoV-2 infection led to the realization of how stigma and discrimination can remain barriers to care for people suspected of being infected; even more if they were frontline healthcare workers or assisting them (2). Recognizing disease stigma; exploring it, and not simply blaming the ignorance of others, can give us insight how these attitudes are formed and how we can disband them. One should keenly reflect on historical evidence to determine what interventions against stigma surrounding infectious diseases has succeeded in the past to determine what may work for COVID-19 pandemic (2).
It is essential to address COVID-19-related stigma to contain the spread of the virus. To overcome this stigma, several agencies, scientific publications, and experts have issued recommendations and taken relevant initiatives. These recommendations have emphasized the usage of inclusive language when talking about the disease, avoiding the spread of misinformation and rumors, being thoughtful and supportive while communicating, and propagating clear, actionable information to support communities affected by this outbreak.
International public health organizations tend to view outbreaks through the lens of epidemiology and hard medical facts. Nevertheless, it could be beneficial to add psycho-cultural nuances to rote medical approaches. For example, during the Ebola crisis, the World Health Organization (WHO) was able to successfully flatten the Ebola transmission rate by melding its treatment strategies with the cultural practices, social norms, and beliefs of affected communities (25). Another example is that Japan’s remarkably lower COVID-19 death rates. This was achieved by telling people to avoid the three “Cs”—closed spaces, crowded places, and close-contact settings, rather than solely instructing them to stay at home (26). Their approach also harnessed a long held cultural belief in several Asian countries that people wear facemasks in public during the influenza season with an expectation that it helps prevent infections (27).
Global health organizations should also study how to mitigate cultural taboos as they apply to COVID-19, even if they may not be up to par with the original standard. For instance, if conditions compliant with hospital protocol were followed, the risk of infectious spread would be lowered, and more people could be permitted to attend gatherings like funerals. To this effect, immediate family members, in full personal protective equipment, could be allowed to visit their passing loved ones, say their goodbyes, and perform their final rites. Such solutions are neither meant to be compromises, nor supposed to be perfect. Rather, they sensitively cater to the needs of different cultures so that individuals can engage in at least some form of their cultural practices or religious rituals while also adhering to health prescriptions for the greater good. Only with innovation, cultural sensitivity, and perseverance can these divides be healed, and the mental trauma induced by COVID-19 be diminished. The current pandemic presents us with an opportunity to introspect, educate ourselves, and understand narratives that have been previously misunderstood or underrepresented.
Social isolation, anxiety, fear of contagion, uncertainty, chronic stress, and financial difficulties may lead to the development or exacerbation of stress-related disorders and suicidality in vulnerable populations including individuals with pre-existing psychiatric disorders, low-resilient persons, individuals who reside in high COVID-19 prevalence areas and people who have a family member or a friend who has died of COVID-19 (28). Social disengagement played an important role in the elevated suicide rate during the 2003 SARS epidemic in Hong Kong (29). It is concerning from the suicide prevention perspective that social isolation is the most crucial public health strategy for the COVID-19 pandemic. COVID-19 survivors, particularly those who experienced severe symptoms are at elevated risk of suicide (30). Stressful events such as learning about the diagnosis of COVID-19, fear of spreading the infection to others, symptoms of the illness, hospitalization, especially admission to an intensive care unit, and loss of income may lead to the emergence of anxiety, depression, and PTSD (30, 31). Suicide prevention in the COVID-19 era is an important and difficult issue and policymakers should create well-defined guidelines to help clinician manage such cases.
During the COVID-19 pandemic, the personal liberties embraced by individuals in the western world made it difficult for public health officials and local and federal governments to contain the spread of this disease (32). United States (U.S.) citizens have defied and protested their state’s stay-at-home orders out of the belief that public health interventions “have gone too far” and violated their rights. This was exacerbated by misinformation disseminated via media (5). For example, some Michigan citizens belonging to working-class population believed that local leaders were “out to get them” by disrupting their local economy, thereby stripping them of their livelihoods and liberty. In April 2020, protesters gathered outside Michigan’s capitol building in Lansing, in large crowds without masks and brandished flags, banners and guns outside and inside the building and at the gates of health facilities (32). They demanded that their politicians repeal the stay-at-home order. Their rally defied social distancing and prevented healthcare workers (some of whom passively counter-protested) from getting to work on time. This situation put the Libertarian protesters, their healthcare worker counter-protesters, their patients, and frontline peers at a greater risk of infection (33). This resistance to quarantine and isolation measures in the U.S. contributed to the ineffective mitigation of the COVID-19 pandemic. Numerous studies pointed to the effectiveness of masks and social distancing, thus identifying a lack of adherence to isolation and masking policies being a major factor in intensifying the spread and impact of COVID-19 (34, 35). People’s intention to comply with recommendations was also found to be an important factor in the successful containment of the COVID-19 pandemic (36).
Some of these same obstacles were seen when the virus broke out in a less liberal society, but not to the same degree (35). In China people have less private control over their lives and the government controls every psycho-cultural echelon of society, including the healthcare system. China saw fewer protests and petitioning as people may have felt that it will be futile, and there were no citizens occupying government buildings or major hospitals. Not surprisingly, when China imposed a lockdown due to COVID-19, the government’s policies were strictly followed. Following the initial outbreak in Wuhan, China implemented “harsh” containment measures, which resulted in a 90 percent reduction in COVID-19 cases in 2 months (37). The doctors who did speak out in the early months of 2020 were summarily suppressed along with their social media accounts, as information spread is tightly regulated (38). Social distancing and the wearing of face masks presented a cultural shock to many communities. Enforcing these guidelines compromised several communal religious events, ceremonies, rituals, and burials. In many communities, people value their rituals and faith as above science and the advice of health experts, and find themselves paralyzed to see their practices being disrupted.
Policymakers and healthcare workers should collaborate in efforts to disseminate factually correct knowledge regarding COVID-19. It is important for governments to consider applying previously established evidence-based stigma reduction strategies to the current pandemic (39), the public should exercise caution in its consumption and response to COVID-19-related media content. This may help minimize the associated anxiety and decrease the likelihood of succumbing to misinformation and conspiracies, hence contributing to improved COVID-19 preventative efforts. It would be beneficial to enable support groups (via the internet if movement restrictions are in place), particularly for COVID-19 affected patients during their confinement and to make mental health services more accessible. All household members of affected patients should receive age appropriate education pertaining to the disease and measures to manage it. Psychological assistance should be specially provided to those traumatized by their experiences, including healthcare workers, caregivers, and victims of COVID-19 hate crimes. Access to healthcare, education, and sustained connectivity to the outside world can help re-establish a sense of “normalcy,” and therefore, be crucial to the success of containment facilities during an outbreak.
We should also acknowledge the role that the COVID-19 pandemic has played in exacerbating preexisting social and ethnic-racial inequalities. Policies should focus on improving social inclusion, reducing the discrimination of minority groups, and ensuring that mental health services are accessible and appropriate to the needs of racial, ethnic, and religious minorities, both during and after the pandemic.
Limitations of our scoping review include the heterogeneity in sample sizes (30–5,039) and the type of study conducted. Another limitation of our scoping review is the rapidly evolving nature of the COVID-19 pandemic, which may lead to outdated information as new research and data become available. Additionally, the review may not cover all relevant aspects of psychosocial and cultural factors due to the vastness of the subject matter and potential language barriers in accessing international sources.
5. Conclusion
The COVID-19 era requires public health officials and government leaders to consider a broad range of cultural and religious involvement when devising a plan to curb the spread of this virulent disease. Aligning healthcare practices with cultural sensitivities is more likely to help control pandemics like COVID-19. Although science-based approaches have been successful in decreasing the spread of COVID-19, the secondary psycho-cultural effects of the virus on minority communities like Asians and Asian Americans (due to the virus’s perceived origins in China) and African American communities (given the racial bias and discrimination prior to the pandemic) remain significant and could persist for years to come. Incorporating more psycho-culturally aware healthcare practices and policies could be advantageous in managing the pandemic and its potentially multilayered aftermath.
Author contributions
SA and SB determined study design, contributed to developing the original protocol, and revised the manuscript. SA contributed to data analysis and interpretation of results. LJ contributed to the original screening of papers, data extraction, writing the first draft of the manuscript, contributed to the introduction, results, discussion section, and references. LJ and SA reviewed the manuscript. SB, LJ, and SA contributed to writing the manuscript, analyzing data, interpreting data, and writing the introduction. HB, SS, and NN contributed to writing the introduction, discussion, and literature search. AM and AZ contributed to analyzing data, interpreting data, and writing the discussion. NM, MJ, and RA contributed to the literature search, writing some sections of manuscript, and making tables. VS contributed to the literature search and writing some sections of manuscript. All authors contributed significantly to the research, have knowledge of the topic, made a substantial contribution to writing, agreed to the final version of the manuscript, and met all ethical requirements.
Funding
This study was funded by departmental resources.
Acknowledgments
We express our gratitude to our co-workers, collaborators, language editors, and librarians for their invaluable support and assistance during the writing of this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Cinelli M, Quattrociocchi W, Galeazzi A, Valensise C, Brugnoli E, Schmidt A, et al. The COVID-19 social media infodemic. Sci Rep. (2020) 10:16598. doi: 10.1038/s41598-020-73510-5
2. Baldassarre A, Giorgi G, Alessio F, Lulli L, Arcangeli G, Mucci N. Stigma and Discrimination (SAD) at the Time of the SARS-CoV-2 Pandemic. Int J Environ Res Public Health. (2020) 17:6341. doi: 10.3390/ijerph17176341
3. Ahmed W, Vidal-Alaball J, Downing J, López Seguí F. COVID-19 and the 5G conspiracy theory: social network analysis of Twitter Data. J Med Internet Res. (2020) 22:e19458. doi: 10.2196/19458
4. Jiang T, Lin L, Zhong Y, Wang X, Zhu H. COVID-19-related stigma and its’ influencing factors: a rapid nationwide study in China. BMJ Open. (2020) 11:e048983. doi: 10.21203/RS.3.RS-66632/V1
5. Jamieson, K, Albarracín D. The relation between media consumption and misinformation at the outset of the SARS-CoV-2 pandemic in the US. Harv Kennedy Sch Misinformation Rev. (2020) 1:1–22. doi: 10.37016/MR-2020-012
6. Victor G, Ahmed S. The importance of culture in managing mental health response to pandemics. In: D Huremović editor. Psychiatry of Pandemics. Cham: Springer International Publishing (2019). p. 55–64. doi: 10.1007/978-3-030-15346-5_5
7. Bruns D, Kraguljac N, Bruns T. COVID-19: facts, cultural considerations, and risk of stigmatization. J Transcult Nurs. (2020) 31:326–32. doi: 10.1177/1043659620917724
8. Lohiniva A, Dub T, Hagberg L, Nohynek H. Learning about COVID-19-related stigma, quarantine and isolation experiences in Finland. PLoS One. (2021) 16:e0247962. doi: 10.1371/journal.pone.0247962
9. Earnshaw V, Brousseau N, Hill E, Kalichman S, Eaton L, Fox A. Anticipated stigma, stereotypes, and COVID-19 testing. Stigma Health. (2020) 5:390–3. doi: 10.1037/sah0000255
10. Herawati C, Dani A, Herlinawati, Bakhri S, Banowati L, Wahyuni N, et al. Stigma, anxiety, religiosity, and economic on Covid-19 preventive efforts. Malays J Public Health Med. (2021) 21:367–73. doi: 10.37268/mjphm/vol.21/no.1/art.846
11. Tomczyk S, Rahn M, Schmidt S. Social distancing and stigma: association between compliance with behavioral recommendations, risk perception, and stigmatizing attitudes during the COVID-19 Outbreak. Front Psychol. (2020) 11:1821. doi: 10.3389/fpsyg.2020.01821
12. Yuan Y, Zhao Y, Zhang Q, Zhang L, Cheung T, Jackson T, et al. COVID-19-related stigma and its sociodemographic correlates: a comparative study. Glob Health. (2021) 17:54. doi: 10.1186/s12992-021-00705-4
13. Singh K, Kondal D, Mohan S, Jaganathan S, Deepa M, Venkateshmurthy N, et al. Health, psychosocial, and economic impacts of the COVID-19 pandemic on people with chronic conditions in India: a mixed methods study. BMC Public Health. (2021) 21:685. doi: 10.1186/s12889-021-10708-w
14. Bodrud-Doza M, Shammi M, Bahlman L, Islam A, Rahman M. Psychosocial and Socio-Economic Crisis in Bangladesh Due to COVID-19 Pandemic: a perception-based assessment. Front Public Health. (2020) 8:341. doi: 10.3389/fpubh.2020.00341
15. Zakar R, Yousaf F, Zakar M, Fischer F. Sociocultural challenges in the implementation of COVID-19 public health measures: results from a qualitative study in Punjab, Pakistan. Front Public Health. (2021) 9:703825. doi: 10.3389/fpubh.2021.703825
16. Amir K. COVID-19 and its related stigma: a qualitative study among survivors in Kampala, Uganda. Stigma Health. (2021) 6:272–6. doi: 10.1037/sah0000325
17. Miconi D, Li Z, Frounfelker R, Santavicca T, Cénat J, Venkatesh V, et al. Ethno-cultural disparities in mental health during the COVID-19 pandemic: a cross-sectional study on the impact of exposure to the virus and COVID-19-related discrimination and stigma on mental health across ethno-cultural groups in Quebec (Canada). BJPsych Open. (2020) 7:e14. doi: 10.1192/bjo.2020.146
18. Kang E, Lee S, Kim M, Jung H, Kim K, Kim K, et al. The Psychological Burden of COVID-19 Stigma: evaluation of the mental health of isolated mild condition COVID-19 patients. J Korean Med Sci. (2021) 36:e33. doi: 10.3346/jkms.2021.36.e33
19. Mahmoudi H, Saffari M, Movahedi M, Sanaeinasab H, Rashidi-Jahan H, Pourgholami M, et al. A mediating role for mental health in associations between COVID-19-related self-stigma, PTSD, quality of life, and insomnia among patients recovered from COVID-19. Brain Behav. (2021) 11:e02138. doi: 10.1002/brb3.2138
20. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int J Qual Health Care. (2007) 19:349–57x. doi: 10.1093/intqhc/mzm042
21. Baker S, Brawley O, Marks L. Effects of untreated syphilis in the negro male, 1932 to 1972: a closure comes to the Tuskegee study, 2004. Urology. (2005) 65:1259–62. doi: 10.1016/j.urology.2004.10.023
22. Bouie J. Opinion | Why Coronavirus Is Killing African-Americans More Than Others - The New York Times. (2020). Available online at: https://www.nytimes.com/2020/04/14/opinion/sunday/coronavirus-racism-african-americans.html (accessed August 5, 2021)
23. Asadi-Aliabadi M, Tehrani-Banihashemi A, Moradi-Lakeh M. Stigma in COVID-19: a barrier to seek medical care and family support. Med J Islam Repub Iran. (2020) 34:98. doi: 10.34171/mjiri.34.98
24. Turmaud D. Trauma of Pandemic Proportions | Psychology Today. (2020). Available online at: https://www.psychologytoday.com/us/blog/lifting-the-veil-trauma/202003/trauma-pandemic-proportions (accessed August 5, 2021).
25. World Health Organization [WHO]. The importance of Preparedness - Everywhere. (2015). Available online at: https://www.who.int/news-room/spotlight/one-year-into-the-ebola-epidemic/ebola-response-what-needs-to-happen-in-2015 (accessed August 5, 2021).
26. Wingfield-Hayes R. Coronavirus: Japan’s Mysteriously Low Virus Death Rate - BBC News. (2020). Available online at: https://www.bbc.com/news/world-asia-53188847 (accessed August 5, 2021).
27. Burgess A, Horii M. Risk, ritual and health responsibilisation: Japan’s ‘safety blanket’ of surgical face mask-wearing. Sociol Health Illn. (2012) 34:1184–98. doi: 10.1111/j.1467-9566.2012.01466.x
28. Sher L. The impact of the COVID-19 pandemic on suicide rates. QJM. (2020) 113:707–12. doi: 10.1093/qjmed/hcaa202
29. Yip P, Cheung Y, Chau P, Law Y. The impact of epidemic outbreak: the case of severe acute respiratory syndrome (SARS) and suicide among older adults in Hong Kong. Crisis. (2010) 31:86–92. doi: 10.1027/0227-5910/a000015
30. Sher L. Are COVID-19 survivors at increased risk for suicide? Acta Neuropsychiatr. (2020) 32:270. doi: 10.1017/neu.2020.21
31. McGiffin J, Galatzer-Levy I, Bonanno G. The intensive care unit traumatic? What we know and don’t know about the intensive care unit and posttraumatic stress responses. Rehabil Psychol. (2016) 61:120–31. doi: 10.1037/rep0000073
32. Beckett L. Armed Protesters Demonstrate Against Covid-19 Lockdown at Michigan Capitol. (2020). Available online at: https://www.theguardian.com/us-news/2020/apr/30/michigan-protests-coronavirus-lockdown-armed-capitol (accessed July 1, 2020).
33. Ndegwa S. Religion and Culture Plague Africa’s Fight Against COVID-19 - CGTN. CGTN. (2020). Available online at: https://news.cgtn.com/news/2020-04-26/Religion-and-culture-plague-Africa-s-fight-against-COVID-19-PZNaKEiRFe/index.html (accessed August 5, 2021).
34. Howard J, Huang A, Li Z, Tufekci Z, Zdimal V, von Delft A, et al. An evidence review of face masks against COVID-19. Proc Natl Acad Sci USA. (2021) 118:e2014564118. doi: 10.1073/pnas.2014564118
35. Rader B, White L, Burns M, Chen J, Brilliant J, Cohen J, et al. Mask wearing and control of SARS-CoV-2 transmission in the United States. MedRxiv[Preprint]. (2020): doi: 10.1101/2020.08.23.20078964
36. Röhr S, Müller F, Jung F, Apfelbacher C, Seidler A, Riedel-Heller S. Psychosocial impact of quarantine measures during serious coronavirus outbreaks: a rapid review. Psychiatr Prax. (2020) 47:179–89. doi: 10.1055/a-1159-5562
37. Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet. (2020) 395:1225–8. doi: 10.1016/S0140-6736(20)30627-9
38. Emily Feng A. Critics Say China Has Suppressed And Censored Information In Coronavirus Outbreak : Goats and Soda : NPR. (2020). Available online at: https://www.npr.org/sections/goatsandsoda/2020/02/08/803766743/critics-say-china-has-suppressed-and-censored-information-in-coronavirus-outbrea (accessed August 5, 2021).
39. Cook J, Purdie-Vaughns V, Meyer I, Busch J. Intervening within and across levels: a multilevel approach to stigma and public health. Soc Sci Med. (2014) 103:101–9. doi: 10.1016/j.socscimed.2013.09.023
40. Ugidos C, López-Gómez A, Castellanos MÁ, Saiz J, González-Sanguino C, Ausín B, et al. Evolution of intersectional perceived discrimination and internalized stigma during COVID-19 lockdown among the general population in Spain. Int J Soc Psychiatry. (2022) 68:55–63. doi: 10.1177/0020764020975802
Keywords: COVID-19, pandemic, psychocultural, psychosocial, stigma, mental health, conspiracy, infodemic
Citation: Jain L, Bhivandkar S, Baqir H, Shoib S, Nimavat N, Mohan A, Zubair AS, Jawad MY, Muhammed N, Ahmed R, Sachdeva V and Ahmed S (2023) Beyond physical health: the role of psychosocial challenges and stigma in tackling the COVID-19 pandemic—A scoping review. Front. Psychiatry 14:1180252. doi: 10.3389/fpsyt.2023.1180252
Received: 05 March 2023; Accepted: 30 May 2023;
Published: 11 July 2023.
Edited by:
Samer El Hayek, Erada Center for Treatment and Rehab, United Arab EmiratesReviewed by:
Jasbir Singh, California Northstate University, United StatesTarika Nagi, Columbia University, United States
Avleen Kaur, Maimonides Medical Center, United States
Abdulqadir J. Nashwan, Hamad Medical Corporation, Qatar
Copyright © 2023 Jain, Bhivandkar, Baqir, Shoib, Nimavat, Mohan, Zubair, Jawad, Muhammed, Ahmed, Sachdeva and Ahmed. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lakshit Jain, bGFrc2hpdC5qYWluQGN0Lmdvdg==
 Lakshit Jain
Lakshit Jain Siddhi Bhivandkar
Siddhi Bhivandkar Huma Baqir
Huma Baqir Sheikh Shoib
Sheikh Shoib Nirav Nimavat
Nirav Nimavat Anmol Mohan7
Anmol Mohan7 Aarij Shakil Zubair
Aarij Shakil Zubair Nazar Muhammed
Nazar Muhammed Vishi Sachdeva
Vishi Sachdeva Saeed Ahmed
Saeed Ahmed