- 1Xiangya School of Nursing, Central South University, Changsha, China
- 2Clinical Nursing Teaching and Research Section, the Second Xiangya Hospital, Central South University, Changsha, China
- 3Department of Urology, the First Affiliated Hospital of Xinjiang Medical University, Urumqi, China
- 4Centre for Mental Health | Melbourne School of Population and Global Health The University of Melbourne, Melbourne, VIC, Australia
Background: Negative attitudes of nurses toward mental disorders have been reported in various countries. Nurses’ stigmatizing attitudes can harm patients with mental disorders (PWMD), thereby delaying the provision of help to patients and leading to decreased quality of care. In this study, we aimed to assess Chinese nurses’ stigmatizing attitudes toward patients with mental illness and provide a basis for future development and testing of appropriate and culturally adapted interventions to reduce it.
Objective: This study aimed to assess the attitudes of Non-mental Health Nurses (NMHNs) in general hospitals in China toward the stigma of PWMD and determine the factors influencing them.
Methods: A cross-sectional survey of NMHNs in general hospitals were conducted. A self-designed WeChat-based questionnaire was used that included demographic information about the need for training on mental health issues. Participants were provided with a vignette of a depression case with suicidal thoughts. The Depression Stigma Scale (DSS) and Social Distance Scale (SDS) were used to assess attitudes toward mental disorders. Nine questions on the adequacy of knowledge about anxiety and depression and the current status of scale use were used to assess the current status of training needs for mental disorders. Descriptive analysis, chi-square test, and multivariate logistic regression were used for the table.
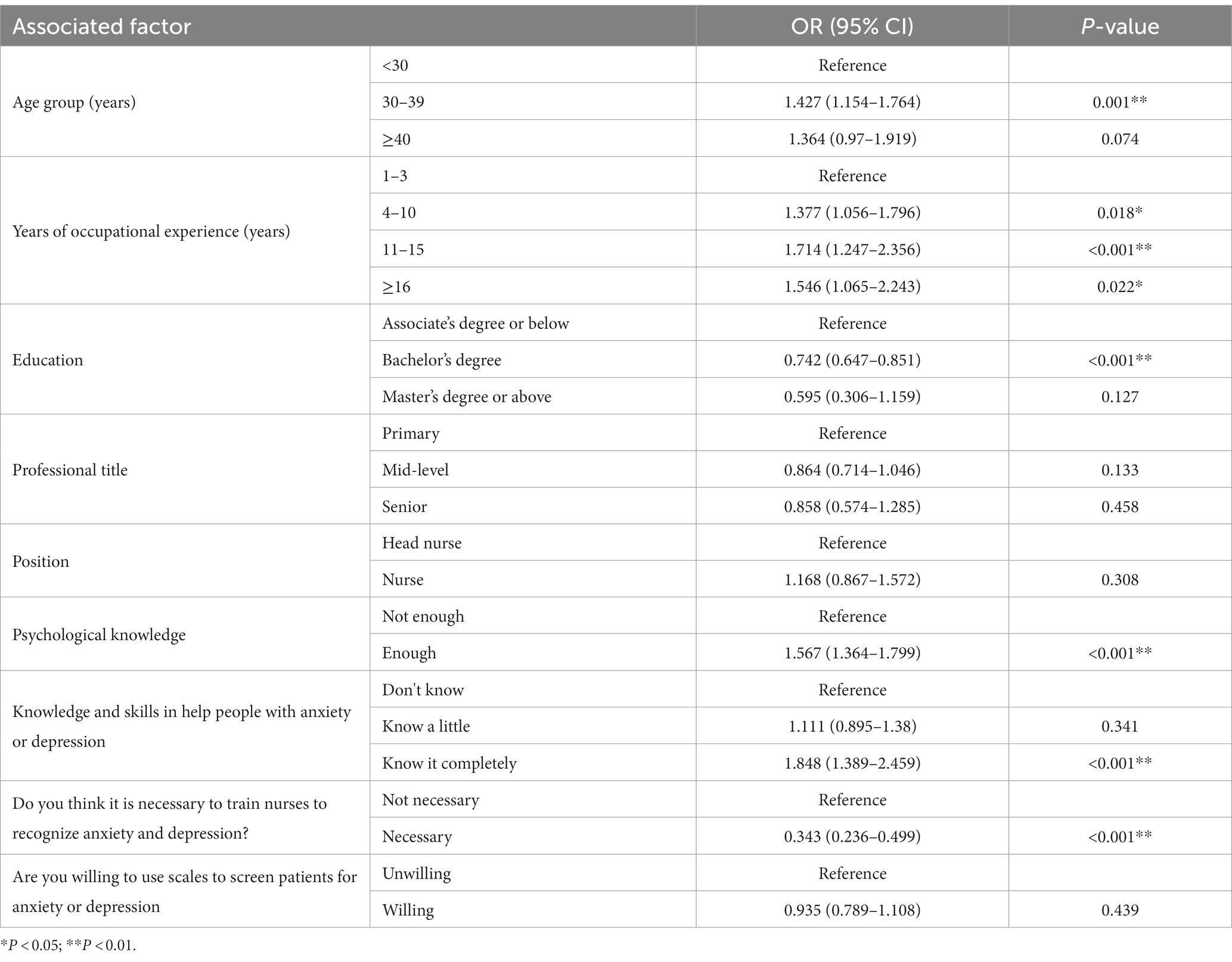
Results: A total of 8,254 nurses in non-mental health professions participated in this study. The mean DSS score of NMHNs was (17.24 ± 6.700), and the SDS score was (10.34 ± 3.154). The total detection rate of stigma among the survey respondents was 13.40% (1,107/8254). Multivariate logistic regression showed that age between 30 and 39 years [p = 0.001, OR = 1.427 (1.154–1.764)], 4 years of work experience and above [p = 0.018, OR = 1.377 (1.056–1.796)], having a bachelor’s degree [p < 0.001, OR = 0.742 (0.647–0.851)], adequate psychological knowledge [p < 0.001, OR = 1.567 (1.364–1.799)], full knowledge of communication with patients with anxiety and depression [p < 0.001, OR = 1.848 (1.389–2.459)], and the need to acquire skills to identify anxiety and depression were the influencing factors associated with stigma [p < 0.001, OR = 0.343 (0.236–0.499)].
Conclusion: Stigmatizing attitudes toward PWMD exist among NMHNs in general hospitals in China. Thus, more mental health education programs for NMHNs are needed. Factors associated with higher morbidity stigma can be used to develop appropriate interventions to improve NMHNs’ stigmatizing attitudes and provide better quality care to PWMD.
Introduction
More than 450 million people suffer from mental disorders worldwide (1, 2), but stigmatizing attitudes toward people with mental disorders (PWMD) are prevalent in the global population (3–6). This is also evident in Chinese culture (7–10). Stigma is “the situation of an individual disqualified from full social acceptance” (11). It reflects an individual’s negative attitude/behavior toward mental disorders (12) and is often divided into personal and perceived stigma. Personal stigma is generally the negative attitudes formed by negative perceptions and emotional experiences of PWMD. Meanwhile, perceived stigma is the derogatory behavior toward and rejection of PWMD by others (13). PWMD can be perceived as dangerous, unpredictable, intellectually disable (3), or personally weak (9, 14–16). Stigmatizing attitudes of PWMD may negatively affect their treatment-seeking behavior, education, social activities, work, and mental health (17). Stigma associated with mental disorders is a significant barrier to accessing mental health services and timely treatment (18–20).
Stigma is common among medical caregivers (19, 21, 22). Such stigmatizing attitudes create severe barriers to good patient-provider communication and quality therapeutic care (19, 23, 24), thereby resulting in delayed help-seeking (24), treatment interruptions, safety concerns (19), and poor prognosis (25, 26). Negative attitudes resulting from caregivers’ lack of experience and knowledge about mental disorders can negatively affect patient interactions and the quality of care (19, 27). Stigma can also negatively affect caregivers’ willingness to seek help or disclose mental health problems (19), and nurses’ stigmatizing attitudes may affect other members of the team and future practitioners (28, 29).
The vital link between stigmatizing attitudes, substance use, and suicidal behavior cannot be ignored, such as cannabis being a relevant risk factor linked to suicidal attempts and behaviors (30).
Medical personnel have the closest contact with patients, and they often encounter patients with mental health problems or psychological crises (31). Fewer than 5% of patients see a psychiatrist first, and more than 70% see a non-mental health professional in general hospitals first (32). Due to these factors, non-mental health nurses in general hospitals are highly likely to come into contact with PWMD and play an essential role in the timely referral of patients to psychiatrists (33). However, nurses cannot better provide appropriate assistance to this population because of their negative attitudes toward mental disorders, lack of identification of PWMD, or lack of skills to assist (34, 35), which further affects the effective treatment, early diagnosis, and effective referral rate of this group of patients, thereby resulting in more extended hospital stays, and patients with mental problems being more prone to doctor-patient disputes (36).
Most published studies have focused on the general public’s attitudes toward mental disorders and people with lived experiences (21). However, there is less research on the extent of stigmatization of people with clinically common anxiety and depression by NMHNs in general hospitals. An Australian study comparing the attitudes of health professionals with those of members of the general community showed that health professionals’ stigmatizing attitudes were comparable to those of members of the general community (37). In addition, a study on the attitudes of Finnish nurses showed positive attitudes (38). A recent study of medical students in 65 countries showed that women and medical and nursing students showed more positive attitudes toward PWMD (22). Meanwhile, a survey of healthcare professionals in Qatar showed that nurses had higher levels of stigma than doctors (25). Moreover, studies in Saudi Arabia and Poland showed that stigmatizing attitudes toward PWMD were common among physicians in tertiary care hospitals (39, 40).
Furthermore, a study in Iran showed that stigmatizing attitudes were higher among internal medicine and cardiology departments than among residents in psychiatry (41). Recently, a Greek study showed that healthcare professionals’ willingness to interact with psychiatric patients is relatively poor, and the prejudice against them is high (42).
In addition, screening for depression in general hospitals can improve the accuracy of detecting depressed patients (43) and the overall treatment of patients (44). Nurses are essential in screening, identification, and referral programs for depression in general hospitals’ physical disease management teams (45, 46). A nurse-based model for early screening of depression in patients with physical illness in general hospitals has been proposed in Korea (46), and there are a few reports on such aspects in China.
Therefore, this study primarily aimed to examine the attitudes and frequency distribution of NMHNs toward PWMD and mental disorders among demographic and occupational characteristics in Chinese general hospitals. Secondly, the study aimed to explore factors associated with morbidity stigma and investigate the current use of depression screening by NMHNs, to provide a basis for further intervention studies.
Methods
Design and setting
This was a descriptive cross-sectional study to explore the attitudes of NMHNs working in Chinese general hospitals toward PWMD. This study aimed to examine factors associated with the detection rate of stigma and understand the current status of knowledge and skills of anxiety and depression and willingness to use screening scales. A convenience sample was used to collect data. This survey was conducted using a self-designed anonymous WeChat-based questionnaire from April 10 to June 1, 2022. The respondents were NMHNs in general hospitals above the second level in China.
Ethical clearance
This study was approved by the Ethics Committee of Xiangya Nursing School of Central South University approved on April 20, 2022 (No. E202255). Informed consent was obtained from all participants. This research received grants from the National Natural Science Foundation of China (No. 81873806) and Major Scientific and Technological Projects in Hunan Province (No. 2020SK2085). Completing the survey questionnaire implied consent to join the study.
Participants’ recruitment and data collection
Firstly, the directors of nursing departments of 14 tertiary-level general hospitals in Xinjiang province were contacted to communicate the considerations related to distributing the questionnaire survey. Then, a link to our questionnaire was sent to the nursing department directors of each hospital via WeChat (social media). Subsequently, the questionnaire link was distributed by the nursing department directors of each hospital to the WeChat groups of the chief nursing officers of each hospital. Afterwards, they separately sent the questionnaire link to the WeChat groups of nurses in their departments. An introduction to the study was displayed on the first page of the questionnaire, and participants selected “agree” to continue the survey or “disagree” to withdraw. Completion of the questionnaire implied consent to join the study. In addition, participants were encouraged to invite colleagues or classmates to participate in the online survey, but no compensation was given. The questionnaire link was distributed among the respondents’ friends and WeChat groups. The sample size was subsequently expanded. Moreover, the study population consisted of front-line nurses working in different departments in Chinese general hospitals above the second level for more than 1 year, excluding nurses specializing in mental health.
The study instruments included the Depression Stigma Scale (DSS) scale, the Social Distance Scale (SDS) scale, and a background questionnaire covering socio-demographic factors, with nine multiple-choice questions on the need for knowledge training and willingness to use the scales for anxiety and depression. Data collection was completed online using WeChat from May 10, 2022, to June 30, 2022. All data were collected anonymously.
Measures
The survey included sociodemographic information such as gender, age, education level, and occupational questions, including hospital care level, work sector, specialty, title, hours worked, and position. Respondents also answered the following nine questions:
1. What are the most common mental disorders you encounter regularly? (Multiple choice).
2. What are your main ways of obtaining knowledge about mental disorders? (Multiple choice).
3. Do you currently have enough psychological knowledge? (Single-choice question).
4. Do you know how to provide help for people with anxiety or depression? (Single-choice question).
5. Do you think it is necessary to train nurses to recognize anxiety and depression? (Multiple choice).
6. Does your department use anxiety or depression scales for patients? (Single-choice question).
7. Are you willing to use scales to screen patients for anxiety or depression? (Single-choice question).
8. If no, what are the reasons? (Multiple choice).
9. If yes, what are the reasons? (Multiple choice).
Personal stigma
The present study used the personal depression stigma subscale of the standardized DSS (47, 48). The DSS-Personal Scale consists of nine items scored on a 5-point Likert scale (0 = strongly disagree, 4 = strongly agree) (47). The total score (range 0–36) is calculated by summing all item scores, with higher total scores indicating higher levels of individual morbidity stigma. The DSS-Personal Scale has been widely used in surveys of different populations (3, 10). Our study used the Chinese scale version, which showed excellent psychometric properties (49, 50). The internal consistency of this sample was 0.824. The study analysis combined the categories of agree and strongly agree for each purpose to indicate that the entry had a personal stigma. If there were ≥ 6 entries with personal stigma, we defined that the survey respondent had a personal stigma against mental disorders.
Social Distance Scale
Willingness to contact the person described in the small case was measured using SDS, a five-item scale developed by Link et al. (51). Each item was rated on a 5-point scale, ranging from absolute willingness (1) to absolute unwillingness (4) (Supplementary material). Our study used the Chinese scale version, which showed good psychometric properties (52). The internal consistency of this sample was 0.886. Lower scores indicate a greater willingness to interact with people with mental illness (for details of the questionnaire in this study, Supplementary material).
Statistical and data analysis
A total of 8,254 valid questionnaires were collected. In this study, descriptive analyses of participants’ demographic characteristics were performed, reporting numerical variables as means and standard deviations (SD), while categorical data were reported as frequencies and percentages. The “agree” and “strongly agree” options of the DSS-Individual Scale were combined, indicating that the entry had a personal stigma. If ≥6 entries had a personal stigma, we defined the survey participant as having a personal stigma of mental disorders or having no stigma. In addition, the mean and SD of the total score of the DSS-Personal Scale were reported for “most commonly encountered mental disorders,” “main way to obtain knowledge about mental disorders.” “Willingness and unwillingness to use the scale to the four questions of most commonly encountered mental disorders,” “main way to obtain knowledge about mental disorders,” and “willingness and unwillingness to use the scale to screen for causes of anxiety or depression” were reported as numbers and percentages and ranked. Factors associated with the detection rate of stigma were included in subsequent multivariate logistic regression analyses at a prespecified p-value of 0.1 to identify significant predictors of the outcome variable having stigma. Associations between the current status of psychological knowledge application and morbidity stigma and social distance were assessed using t-tests, F-tests, and chi-square tests. All analyses were performed using the IBM software SPSS V.28.0 for Windows. In addition, 95% confidence intervals were used, and all comparisons were two-tailed. The threshold of significance was set at p = 0.05.
Results
Background characteristics of participants
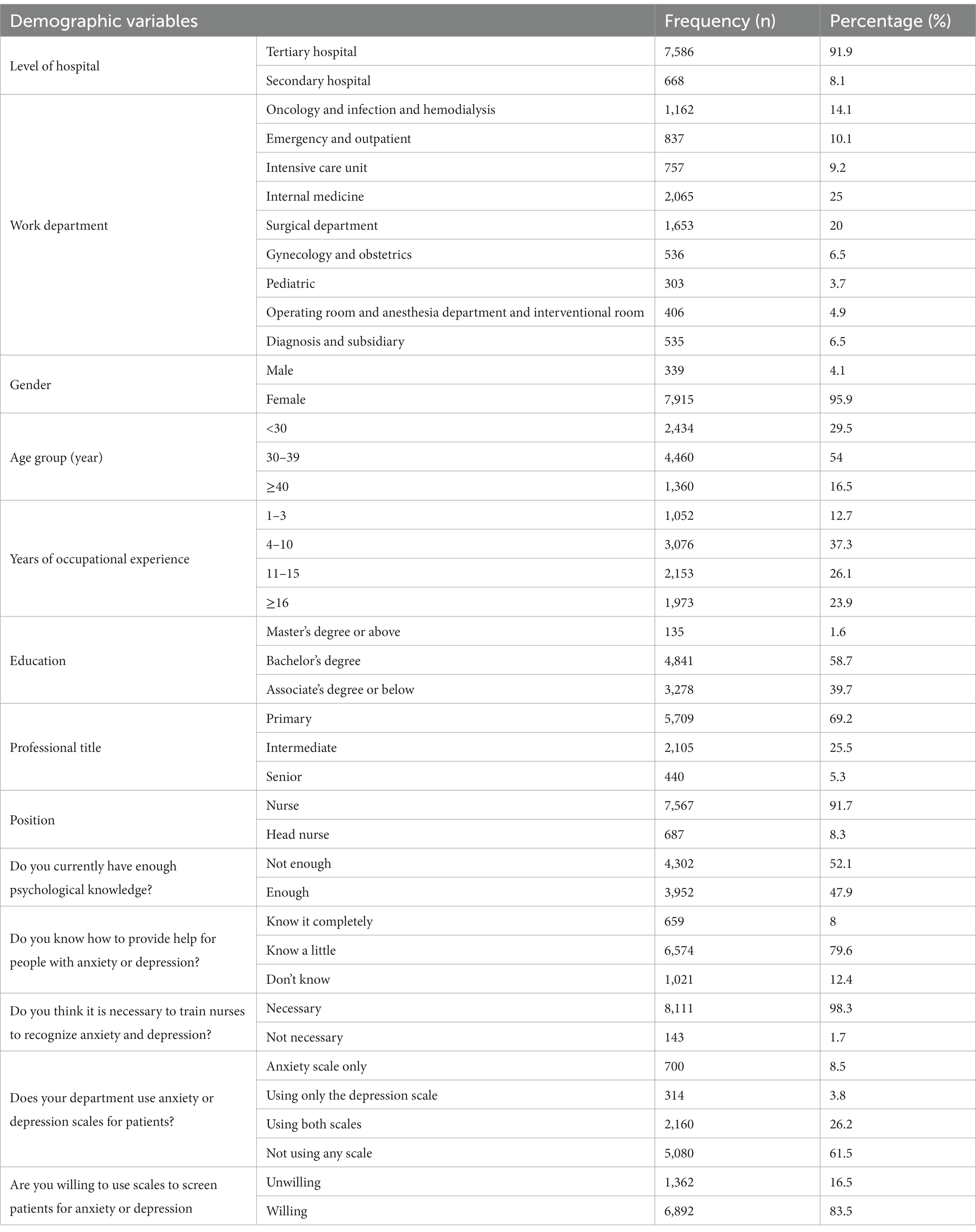
A total of 8,314 nurses from all provinces in mainland China responded to the questionnaire, of which 60 were excluded because of incomplete data. Of the 8,254 respondents, 95.9% were female (n = 7,915), 91.9% worked in a tertiary care hospital (n = 7,586), 69.2% held a junior title (n = 5,709), 58.7% had a bachelor’s degree (n = 4,841), 37.3% had 4–10 years of service (n = 3,076), and 8.3% were head nurses (n = 687). The respondents’ age ranged from 20 to 59 years, of which 54.0% were between 30 and 39 years old (n = 4,469), with a mean age of 33.58 years ±6.823 years. The demographic and training needs of the participants and the distribution of willingness to use the scale are shown in Table 1.
Association of DSS and SDS scores with nurse characteristics
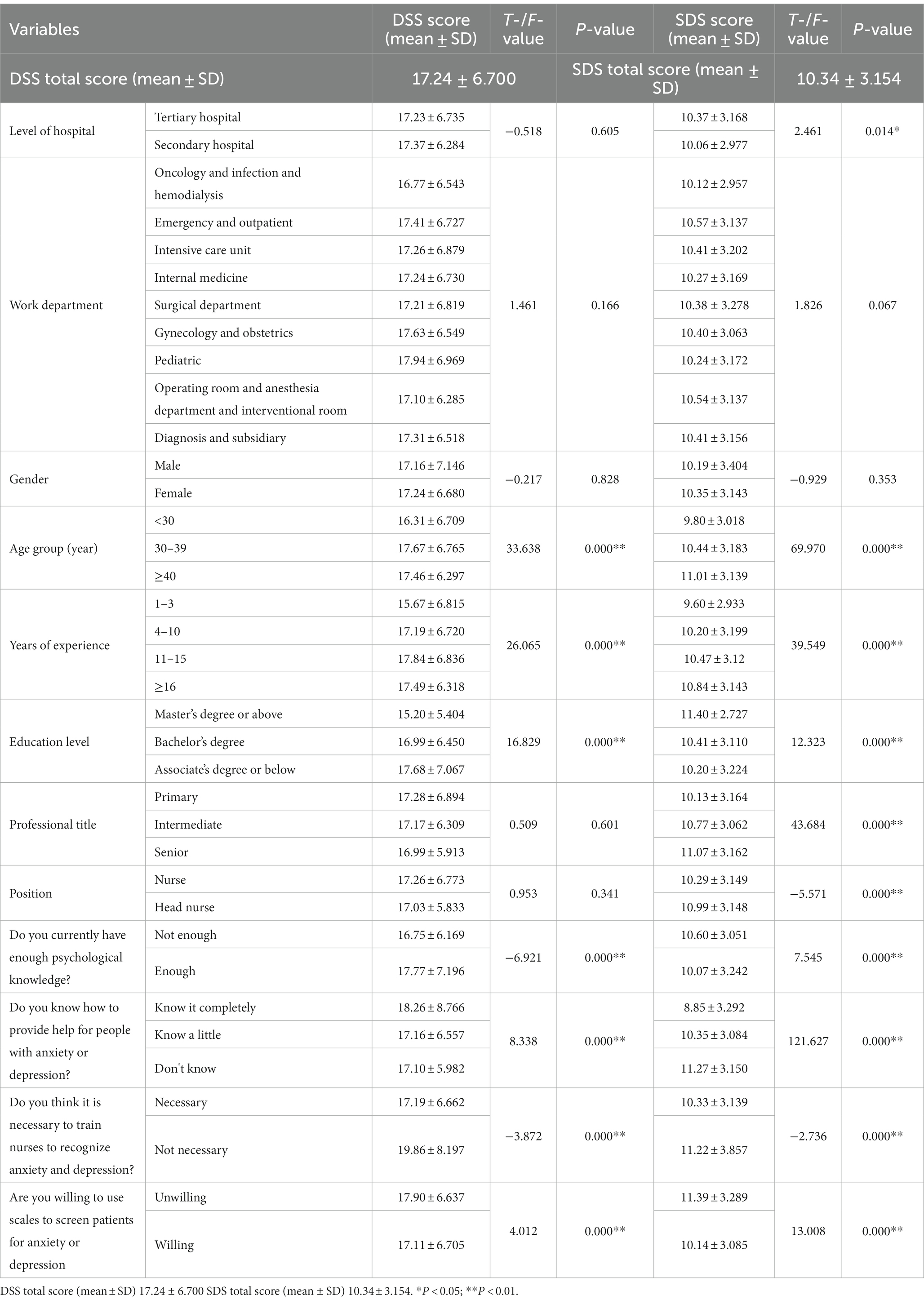
The mean value of the DSS-Personal Scale for NMHNs was (17.24 ± 6.700), and the SDS score was (10.34 ± 3.154).
The internal consistency and reliability of the DSS and SDS scales were good, with Cronbach alpha values of 0.824 and 0.886, respectively.
Table 2 describes the associations between DSS and SDS mean scores and nurse characteristics. At the bivariate level, DSS mean scores were significantly (p < 0.05) related to age, years of experience, level of education, knowledge, knowing ways to communicate with patients with anxiety and depression, having the skills to identify anxiety and depression, and willingness to use scales to screen patients for anxiety and depression. DSS mean scores tend to increase with the increase of age and length of service. Moreover, DSS mean scores tend to decrease with the increase of education levels.
Analysis for mean scores regarding SDS showed that SDS scores were significantly associated with all variables except department and gender (p < 0.05). An increasing trend of SDS scores with age, years of work, education, and title was also found. SDS scores were higher for nurse leaders than for nurses and higher for tertiary hospitals than for secondary hospitals. Not enough psychological knowledge scored higher than enough. Scores ranged from low to high for knowing completely, knowing a little, and not knowing much about providing help to people with anxiety or depression. Those reluctant to train nurses in skills to recognize anxiety and depression scored higher than those willing to train. In terms of using the scale to screen patients for anxiety and depression, those who were reluctant to use it scored higher than those who were willing to use it. Higher scores indicate a greater reluctance to engage and interact with people with mental illness.
Social distance
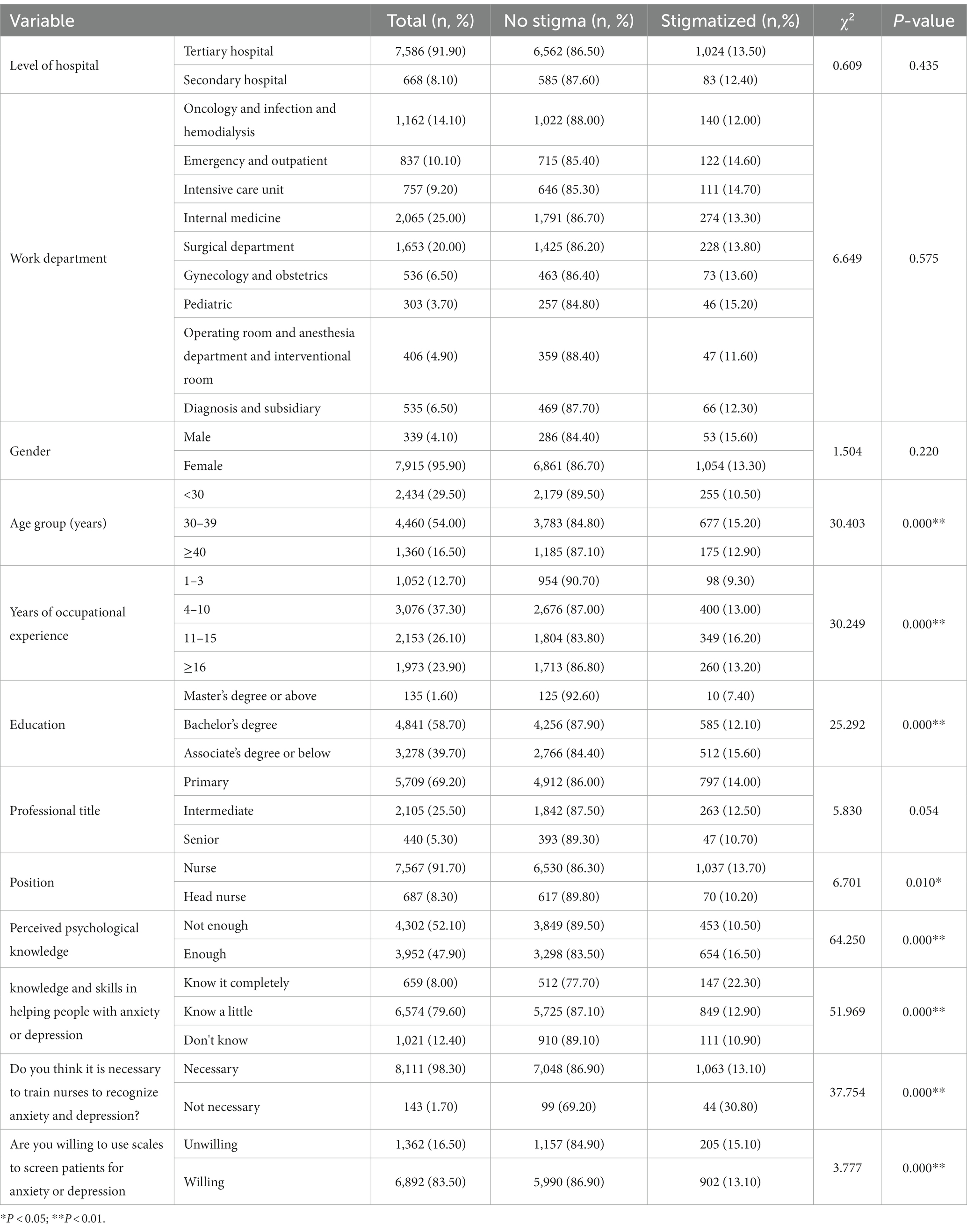
The prevalence rate of stigma
Table 3 shows that the mental disorder stigma prevalence rate was 13.41% (1,107/8,254) among the 8,254 validated respondents. The differences in stigma prevalence rates were statistically significant (p < 0.05) for age, years of work, education level, job title, knowledge adequacy, perception of having skills to identify anxiety and depression, and willingness to use the scale to screen for anxiety and depression. The prevalence rate of stigma was higher among the respondents aged 30–39 than in other age groups, higher in respondents with 11–15 years of work experience than among the other years of service groups, and higher among nurses than among nurse leaders. Interestingly, the prevalence rate of stigma was higher among respondents with sufficient knowledge of psychology than those with insufficient knowledge. In addition, it was higher among those who did not consider it necessary to acquire the skills to identify anxiety and depression than among those who did. Moreover, it was higher among respondents who were not willing to use the scale to screen for anxiety and depression than among the willing group. Furthermore, it was higher in the respondents who fully knew of the need to help people with anxiety and depression than in the other groups.
Multifactorial logistic regression analysis of the prevalence rate of stigma in DSS
Table 4 shows that the presence or absence of stigma was detected as the dependent variable. The variables with p-values greater than 0.2 in Table 3 (nine factors) were included in a multifactorial logistic regression model for analysis, including age, years of experience, education level, professional title, position, adequacy of knowledge, the necessity of skills to identify anxiety and depression, willingness to use the scale to screen for anxiety and depression, and whether or not they were aware of assisting patients with anxiety and depression. Results showed that 30–39 years of age, 4 years or more of work experience, a bachelor’s degree, adequate knowledge, full knowledge of providing help to patients with anxiety and depression, and the need for skills to identify anxiety and depression were the factors influencing the prevalence rate of stigma of the interviewed nurses.
Current status of training needs and willingness to use scale screening for anxiety and depression
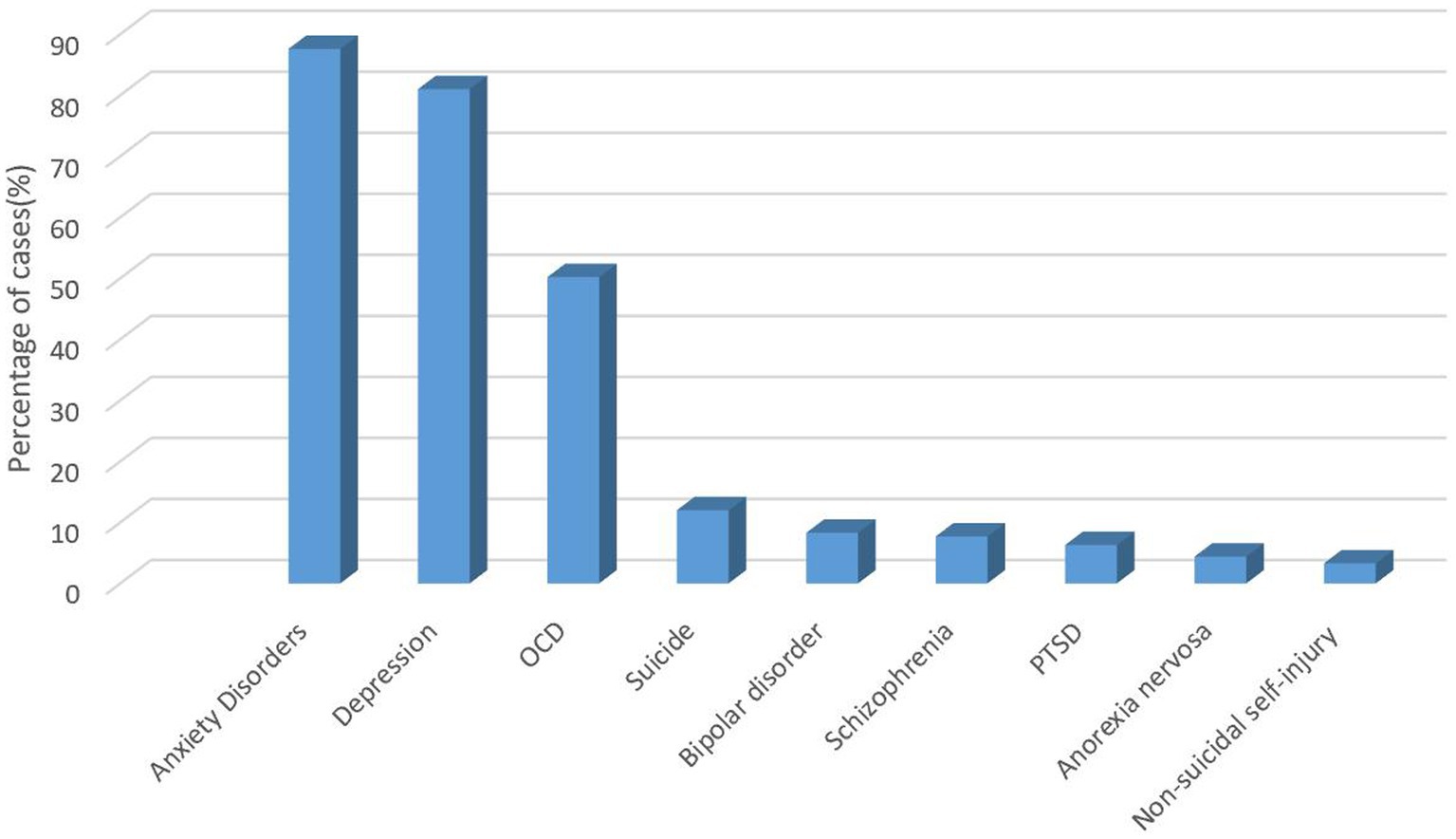
The most common mental disorder encountered by respondents in this survey was anxiety disorder (87.60%), followed by depression (81.00%) and obsessive–compulsive disorder (50.20%) (Figure 1).
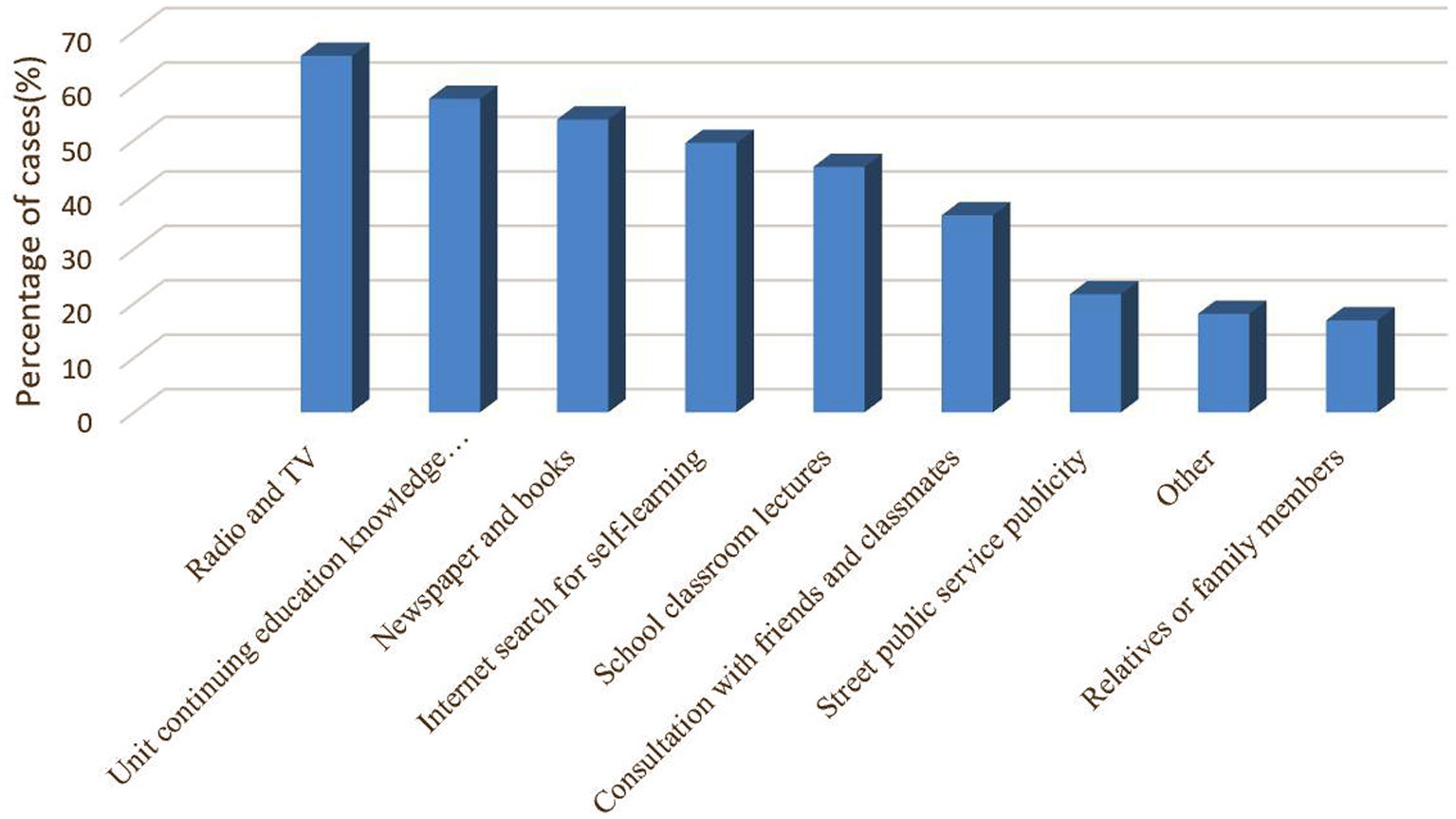
The primary source of knowledge about mental disorders for the respondents in this survey was radio and television (87.60%), followed by unit continuing education knowledge lectures and newspapers and books (Figure 2).
Figures 3, 4 show that the most popular option for respondents in this survey who were willing to use the scale to screen patients with anxiety and depression was that it would help to provide good psychological care to patients, improve treatment compliance, and promote early recovery (21.8%). Secondly, it helps nurses to know which patients have anxiety symptoms or depressive symptoms and focus on them to avoid adverse events (21.1%). Knowing patients’ psychological abnormalities can improve patient satisfaction and avoid some doctor-patient disputes (20.0%). The number one ranked reason for not wanting to use the scale was being too busy to do a screening. The second ranked reason was the scale chosen needs to be short. The third reason was patient refusal (20.1%). However, the number of people who were willing (83.5%) to use the scale to screen for anxiety and depression was much higher than the number of people who were not (16.5%).
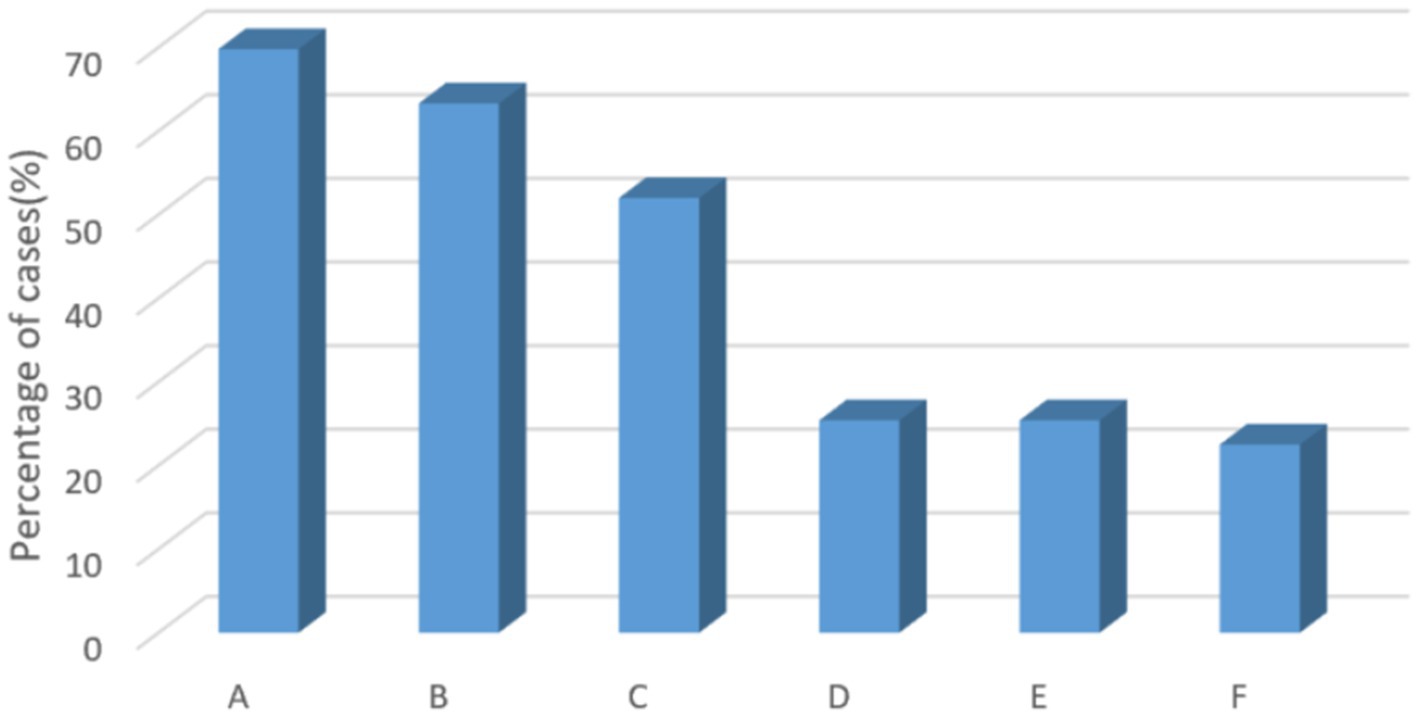
Figure 3. Reasons for reluctance to use scales to screen for anxiety and depression. A, there is no time for screening because of busy work; B, the selected scale takes too long; C, patient refusal; D, this is the doctor’s work area, and the nurse does not need to do this work; E, no need for screening; F, other.
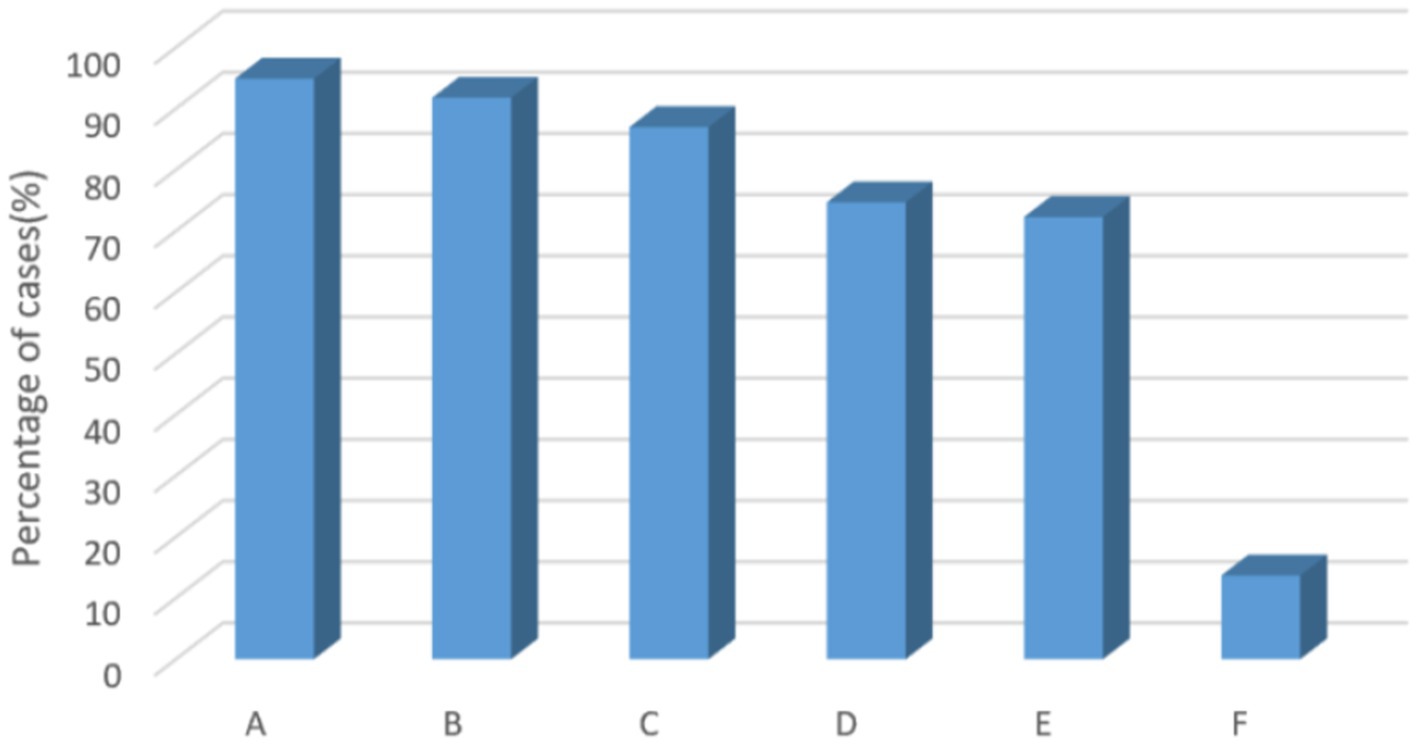
Figure 4. Reasons for willingness to use the scale to screen for anxiety and depression. A, it is conductive to providing better psychosocial care for patients, which can improve treatment compliance and promote early recovery; B, it is beneficial for nurses to find out which patients have anxiety or depression and can focus on them to avoid adverse events; C, knowing more emotional abnormalities of patients, avoiding some doctor-patient disputes, and improving patient satisfaction; D, easy and fast screening using scales; E, it can improve the effective referral rate of patients with psychosomatic abnormalities; F, other.
Discussion
This study found that NMHN in Chinese general hospitals have stigmatized attitudes toward patients with mental disorders. Factors associated with stigma and sources of acquiring knowledge about mental disorders inform the next steps in developing interventions to provide a better quality of care for patients.
This study explored the stigmatization of PWMD in Chinese general hospital NMHNs. In this study, the mean DSS-Personal Scale score of Chinese general hospitals NMHNs was (17.24 ± 6.700) (Table 2), which was higher than the scores of Chinese medical students (13.71 ± 5.350) (10) and Portuguese community adults (12.71 ± 5.520) (53). This finding suggests that the stigma of personal mental disorders is higher in Chinese general hospital NMHNs.
In addition, the survey analysis found that the detection rate of stigma for mental disorders among the nurses interviewed was significantly lower than in studies related to the stigma of patients and families attending outpatient clinics in Chinese domestic community hospitals (21.5%) (54). However, Swedish nurses’ attitudes toward PWMD are similar to those of the general public (55). A study by Cattell showed that nurses had higher negative attitudes toward PWMD than physicians (25), which may indicate a global phenomenon. Media portrayals of mental disorders may influence nurses toward seeing patients as potentially dangerous, unpredictable, violent, or weak (56).
The findings showed an effect of stigma of mental disorders among nurses interviewed between ages 30–39 years [OR = 1.427 (1.154–1.764), p = 0.001], which is inconsistent with a study on the stigma of depression in the general population in Canada (57).
In the present study, a bachelor’s degree was also an independent influence on the morbid stigma of mental disorders [OR = 0.742 (0.647–0.851), p < 0.001], which is generally consistent with a Greek study (42). Higher levels of education are associated with less stigmatizing attitudes toward PWMD. However, our study showed that having a master’s degree or higher was not an independent influence on the stigma of mental disorders [OR = 0.595 (0.306–1.159), p = 0.127]. However, univariate analysis showed that the prevalence rate of stigma gradually decreased with the increase of education level (7.40% for master’s degrees and higher, 12.10% for bachelor’s degrees, and 15.60% for college and lower). Those with a master’s degree had the lowest detection rate of stigma.
Years of work experience is another critical variable in our data. The highest OR for stigma was found among the nurses surveyed with 11–15 years of work experience [OR = 1.714 (1.247–2.356), p < 0.001] in a U-shape. Moreover, in the univariate analysis, the stigma prevalence rate was highest among the surveyed nurses with 11–15 years of work experience (16.20%). This may be because most undergraduate medical education programs in China are rarely designed with mental health-related course credit hours (58).
In this study, no independent influences on the stigma of mental disorders were found in the department for NMHNs. However, a study in Qatar showed that stigma was highest among emergency department nurses (25). Individuals requiring acute mental disorder care are initially assessed in the emergency department. Thus, nurses’ attitudes can severely impact the quality of patient care (25). A patient’s physical discomfort may be overlooked and attributed to their mental disorder in the emergency department. This diagnostic masking is a high risk for worsening morbidity and potential mortality. It is a significant barrier to help-seeking behavior and may lead to delays in receiving necessary help (25). A Swedish study showed that staff in inpatient units had more negative attitudes than staff in outpatient departments (21). Greater exposure to mental disorders and higher knowledge of mental disorders predicted lower personal stigma and social distance (59).
This study showed that Chinese NMHNs’ overall mean SDS score was (10.34 ± 3.154). Results also found that the willingness to interact with patients with mental illness was highest among young respondents, those with only a few years of experience, those with low education and title, and who were working in secondary hospitals. Interestingly, we found that the willingness to interact with patients with mental illness was lower for head nurses than for nurses. However, stigma prevalence rates were higher for nurses than for nurse leaders. This finding suggests that a high level of contact with patients with mental illness is not necessarily associated with sufficient willingness to interact with these patients, nor does it decisively reduce existing bias (42, 55).
Therefore, results in Figure 1 indicate that people between the ages of 30–39, with 11–15 years of work experience, with college degrees or less, who believe they have sufficient knowledge and are fully capable of assisting people with anxiety and depression, and who do not believe it is necessary to acquire the skills to identify anxiety and depression, can be the focus of future stigma education and training implementation in the region.
Current status of training needs and willingness to use scales for anxiety and depression
In this study, respondents commonly encountered anxiety disorders (87.60%) and depression (81.00%). This is consistent with a recent epidemiological study in which anxiety disorders were the most common mental disorder (60). However, most people suffering from anxiety or mood disorders do not immediately seek help from a mental health professional but initially seek help at their local general hospital (61). In contrast, NMHNs are the healthcare workers with the most contact with patients in clinical practice. The ability of these NMHNs to identify and refer patients and their attitude toward them is very important, particularly those patients with non-psychotic disorders who do not receive timely referrals or appropriate treatment. Until they can receive timely referrals, the high expenditure on health resources increases the financial burden on patients and takes away from limited healthcare resources. Stigmatizing attitudes toward these patients can further inhibit their treatment-seeking behavior and affect healthcare quality (62). The poor quality of care they receive can further worsen treatment adherence, reduce the stability of mental disorders, shorten their life expectancy, and increase nurse–patient conflict (63).
Interestingly, although the results of this study showed that the number of people willing to use the scale to screen for mental problems was overwhelming (83.5%, Table 1), the rate of stigma detection among those who were unwilling to use the scale (15.1%) was higher than the rate of stigma detection among those who were willing (13.1%, Table 3), that is, stigma among the unwilling was higher than those willing. This also suggests that respondents unwilling to use the scale to screen patients with anxiety and depression are priority targets for intensive stigma education. Early identification of high-risk patients with mental problems facilitates healthcare professionals to provide more accurate treatment services to such patients. The survey results regarding willingness to use the scale may provide meaningful guidance for developing future management strategies for rapidly identifying patients with mental problems.
In this survey, radio and television were the most common sources of mental health knowledge for the nurses interviewed, followed by continuing education knowledge lectures in the unit and then newspapers and books, slightly different from the study by Wu et al. (33). It is suggested that Chinese nurses have inadequate education and training on the most common mental disorders. Mental health resources, particularly human resources, are inadequate worldwide, especially in low- and middle-income countries (64). NMHNs play an essential role in the identification and timely referral of PWMD. The current survey showed that most surveyed nurses (61.5%) had not used screening tools for anxiety and depression. However, most (83.5%) were willing to use screening tools to identify depression in patients with physical illnesses.
Strengths and limitations of the study
This study is the first for NMHNs in China, and results reveal a critical public health issue. Therefore, we innovatively used the stigma detection rate method to explore and analyze the factors that influence the stigma of mental disorders in NMHNs, opening up new research ideas in this field. Second, the sample size of this investigation was relatively large for this type of study. However, this study also has its limitations. First, this study was a national online cross-sectional survey. Although 8,254 nurses from all provinces of mainland China responded, the sample was small and disproportionately distributed compared to the number of nursing staff in China, which may affect the validity and generalizability of our findings. Second, no causal relationship can be inferred from the current study, and future longitudinal studies are needed. Third, in the research analysis, the categories of absolute and possible unwillingness for each item in the SDS scale were not combined; this research will be conducted later. The investigation was conducted during the COVID-19 pandemic. Therefore, we could not assess whether or not personal mental health problems and occupational exhaustion affected participants’ responses. Fourth, the current study analyzed self-reported data from NMHN, which may pose a potential risk to the validity of the measurements. However, based on the critical influencing factors of stigma identified in this research, it may provide meaningful guidance for future efforts to improve intensive education on attitudes toward mental disorders appropriate for NMHNs in Chinese general hospitals.
In clinical practice, biased perceptions may negatively affect how patients with mental illness are treated during hospitalization (42, 65). Nurses are the frontline healthcare workers with the most access to patients; thus, they are the most proportional and widespread force in the healthcare workforce and can play an essential role in anti-stigma efforts (66), more so as healthcare workers. Therefore, appropriate educational programs can improve perceptions of mental illness and of patients (67, 68). Our findings suggest that using stigma detection rate methods can detect people at high risk for stigmatizing attitudes and focus on giving targeted interventions based on this. The construction of the mental health system is a significant public health, livelihood, and social issue related to economic and social development and the physical and mental health of the people in China. The reform of China’s mental health system should not only focus on technology and infrastructure but also on improving the way and attitude of providing services to each patient to meet current mental health service needs.
Conclusion
This study identified a high stigma toward and social distance from mental disorders among NMHNs in Chinese general hospitals and found various associated factors. There were more stigmatizing attitudes among such respondents who were between 30 and 39 years old, had been working for 11–15 years, had a bachelor’s degree, self-identified as having sufficient knowledge of psychology, and thoroughly understood how to communicate with people suffering from anxiety and depression.
The current study also found that anxiety and depression were the most common mental disorders encountered by nurses interviewed, and radio and television were the most common sources of mental health knowledge. The most frequent options for willingness to use the scale to screen for anxiety and depression were facilitating good patient psychological care, improving treatment adherence, and promoting early recovery. In addition, the most frequent reason for being unwilling to use the scale was being too busy at work to do it. The number of people willing to use the scale to screen for anxiety and depression was much higher than those who were not willing to do so. These findings guide the development and implementation of effective interventions for stigma to reduce problems in clinical services in the future.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by The Ethics Committee of Xiangya Nursing School of Central South University approved this study on April 20, 2022 (No. E202255). Informed consent was obtained from all participants. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
LL and YL participated in the conception and design of this study. CX organized the database. LL performed the statistical analysis and wrote the first draft of the manuscript. SL revised the manuscript. YL and SL provided advice on the statistical analysis and interpretation of the results and reviewed the manuscript draft. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the National Natural Science Foundation of China (No. 81873806) and Major Scientific and Technological Projects in Hunan Province (No. 2020SK2085).
Conflict of interest
The authors declare that the study was conducted without any commercial or financial relationship, which may be considered a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1180034/full#supplementary-material
Abbreviations
NMHNs, Non-mental health nurses; DSS, Depression Stigma Scale; SDS, Social Distance Scale; OCD, Obsessive–compulsive disorder; PTSD, Post-traumatic stress disorder; PWMD, Patients with mental disorders; GHOC, General hospitals of China.
References
1. Wainberg, ML, Scorza, P, Shultz, JM, Helpman, L, Mootz, JJ, Johnson, KA, et al. Challenges and opportunities in global mental health: a research-to-practice perspective. Curr Psychiatry Rep. (2017) 19:28. doi: 10.1007/s11920-017-0780-z
2. Prasad, R, and Satyanand, SA. Contemporary issues for delivery of mental health services in commonwealth countries. Indian J Psychiatry. (2016) 58:270–4. doi: 10.4103/0019-5545.192012
3. Reavley, NJ, and Jorm, AF. Stigmatizing attitudes towards people with mental disorders: findings from an Australian National Survey of mental health literacy and stigma. Aust N Z J Psychiatry. (2011) 45:1086–93. doi: 10.3109/00048674.2011.621061
4. Mascayano, F, Tapia, T, Schilling, S, Alvarado, R, Tapia, E, Lips, W, et al. Stigma toward mental illness in Latin America and the Caribbean: a systematic review. Braz J Psychiatry. (2016) 38:73–85. doi: 10.1590/1516-4446-2015-1652
5. Parcesepe, AM, and Cabassa, LJ. Public stigma of mental illness in the United States: a systematic literature review. Admin Pol Ment Health. (2013) 40:384–99. doi: 10.1007/s10488-012-0430-z
6. Krajewski, C, Burazeri, G, and Brand, H. Self-stigma, perceived discrimination and empowerment among people with a mental illness in six countries: Pan European stigma study. Psychiatry Res. (2013) 210:1136–46. doi: 10.1016/j.psychres.2013.08.013
7. Yin, H, Wardenaar, KJ, Xu, G, Tian, H, and Schoevers, RA. Mental health stigma and mental health knowledge in Chinese population: a cross-sectional study. BMC Psychiatry. (2020) 20:323. doi: 10.1186/s12888-020-02705-x
8. Liu, J, Yan, F, Ma, X, Guo, HL, Tang, YL, Rakofsky, JJ, et al. Perceptions of public attitudes towards persons with mental illness in Beijing, China: results from a representative survey. Soc Psychiatry Psychiatr Epidemiol. (2016) 51:443–53. doi: 10.1007/s00127-015-1125-z
9. Zhu, Y, Zhang, H, Yang, G, Hu, X, Liu, Z, Guo, N, et al. Attitudes towards mental illness among medical students in China: impact of medical education on stigma. Asia Pac Psychiatry. (2018) 10:e12294. doi: 10.1111/appy.12294
10. Qiu, L, Feng, Y, Luo, J, Zhang, Y, and Yang, Q. Predictors of personal depression stigma in medical students in China: differences in male and female groups. Med Educ Online. (2022) 27:2093427. doi: 10.1080/10872981.2022.2093427
11. Erving, G. Stigma: notes on the management of spoiled identity. Englewood Cliffs, NJ: Prentice Hall (1963).
12. Clement, S, Schauman, O, Graham, T, Maggioni, F, Evans-Lacko, S, Bezborodovs, N, et al. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol Med. (2015) 45:11–27. doi: 10.1017/s0033291714000129
13. Griffiths, KM, Nakane, Y, Christensen, H, Yoshioka, K, Jorm, AF, and Nakane, H. Stigma in response to mental disorders: a comparison of Australia and Japan. BMC Psychiatry. (2006) 6:21. doi: 10.1186/1471-244x-6-21
14. Zhou, C, and Xu, Y. Time to break mental illness-related stigma and discrimination in China. Asian J Psychiatr. (2021) 66:102881. doi: 10.1016/j.ajp.2021.102881
15. Meng, N, Huang, X, Wang, J, Wang, M, and Wang, Y. The factors and outcomes of stigma toward mental disorders among medical and nursing students: a cross-sectional study. BMC Psychiatry. (2022) 22:357. doi: 10.1186/s12888-022-03996-y
16. Jauch, M, Occhipinti, S, and O'Donovan, A. The stigmatization of mental illness by mental health professionals: scoping review and bibliometric analysis. PLoS One. (2023) 18:e0280739. doi: 10.1371/journal.pone.0280739
17. Schnyder, N, Panczak, R, Groth, N, and Schultze-Lutter, F. Association between mental health-related stigma and active help-seeking: systematic review and meta-analysis. Br J Psychiatry. (2017) 210:261–8. doi: 10.1192/bjp.bp.116.189464
18. Royal College of Psychiatrists. Whole-person care: From rhetoric to reality (occasional paper OP88). (2018). Available at: https://www.basw.co.uk/system/files/resources/basw_103627-6_0.pdf (Accessed November 22, 2020).
19. Knaak, S, Mantler, E, and Szeto, A. Mental illness-related stigma in healthcare: barriers to access and care and evidence-based solutions. Healthc Manage Forum. (2017) 30:111–6. doi: 10.1177/0840470416679413
20. Henderson, C, Evans-Lacko, S, and Thornicroft, G. Mental illness stigma, help seeking, and public health programs. Am J Public Health. (2013) 103:777–80. doi: 10.2105/ajph.2012.301056
21. Hansson, L, Jormfeldt, H, Svedberg, P, and Svensson, B. Mental health professionals' attitudes towards people with mental illness: do they differ from attitudes held by people with mental illness? Int J Soc Psychiatry. (2013) 59:48–54. doi: 10.1177/0020764011423176
22. Babicki, M, Małecka, M, Kowalski, K, Bogudzińska, B, and Piotrowski, P. Stigma levels toward psychiatric patients among medical students-a worldwide online survey across 65 countries. Front Psych. (2021) 12:798909. doi: 10.3389/fpsyt.2021.798909
23. de Jacq, K, Norful, AA, and Larson, E. The variability of nursing attitudes toward mental illness: an integrative review. Arch Psychiatr Nurs. (2016) 30:788–96. doi: 10.1016/j.apnu.2016.07.004
24. Lien, YY, Lin, HS, Tsai, CH, Lien, YJ, and Wu, TT. Changes in attitudes toward mental illness in healthcare professionals and students. Int J Environ Res Public Health. (2019) 16:4655. doi: 10.3390/ijerph16234655
25. Ghuloum, S, Mahfoud, ZR, Al-Amin, H, Marji, T, and Kehyayan, V. Healthcare Professionals' attitudes toward patients with mental illness: a cross-sectional study in Qatar. Front Psych. (2022) 13:884947. doi: 10.3389/fpsyt.2022.884947
26. Hamdan-Mansour, AM, and Wardam, LA. Attitudes of Jordanian mental health nurses toward mental illness and patients with mental illness. Issues Ment Health Nurs. (2009) 30:705–11. doi: 10.1080/01612840903131792
27. Ross, CA, and Goldner, EM. Stigma, negative attitudes and discrimination towards mental illness within the nursing profession: a review of the literature. J Psychiatr Ment Health Nurs. (2009) 16:558–67. doi: 10.1111/j.1365-2850.2009.01399.x
28. Smith, JD, Mittal, D, Chekuri, L, Han, X, and Sullivan, G. A comparison of provider attitudes toward serious mental illness across different health care disciplines. Stigma Health. (2017) 2:327–37. doi: 10.1037/sah0000064
29. Glozier, N, Hough, C, Henderson, M, and Holland-Elliott, K. Attitudes of nursing staff towards co-workers returning from psychiatric and physical illnesses. Int J Soc Psychiatry. (2006) 52:525–34. doi: 10.1177/0020764006066843
30. Serafini, G, Pompili, M, Innamorati, M, Rihmer, Z, Sher, L, and Girardi, P. Can cannabis increase the suicide risk in psychosis? A critical review. Curr Pharm Des. (2012) 18:5165–87. doi: 10.2174/138161212802884663
31. Jing, H. Effect of relaxation training on anxiety and depression in parents of children with asthma [Master]. Nanchang University (2021). CNKI. (in Chinese). doi: 10.27232/d.cnki.gnchu.2021.000150
32. Li, X, Zhang, W, Lin, Y, Zhang, X, Qu, Z, Wang, X, et al. Pathways to psychiatric care of patients from rural regions: a general-hospital-based study. Int J Soc Psychiatry. (2014) 60:280–9. doi: 10.1177/0020764013485364
33. Wu, Q, Luo, X, Chen, S, Qi, C, Yang, WFZ, Liao, Y, et al. Stigmatizing attitudes towards mental disorders among non-mental health professionals in six general hospitals in Hunan Province. Front Psych. (2019) 10:946. doi: 10.3389/fpsyt.2019.00946
34. Wu, Q, Luo, X, Chen, S, Qi, C, Long, J, Xiong, Y, et al. Mental health literacy survey of non-mental health professionals in six general hospitals in Hunan Province of China. PLoS One. (2017) 12:e0180327. doi: 10.1371/journal.pone.0180327
35. Lu, S, He, Y, Searle, K, Absetz, P, Oldenburg, B, and Reavley, N. Using stakeholder perceptions to inform future efforts to implement mental health first aid training in China: a qualitative study. Front Psych. (2021) 12:557282–2. English. doi: 10.3389/fpsyt.2021.557282
36. Yan, Y. A standardized system of psychological care for inpatients in general hospitals based on a multidisciplinary cooperation model. Chin Nurs Manag. (2019) 19:168–71. (in Chinese) doi: 10.3969/j.issn.1672-1756.2019.z1.066
37. Reavley, NJ, Mackinnon, AJ, Morgan, AJ, and Jorm, AF. Stigmatising attitudes towards people with mental disorders: a comparison of Australian health professionals with the general community. Aust N Z J Psychiatry. (2014) 48:433–41. doi: 10.1177/0004867413500351
38. Ihalainen-Tamlander, N, Vähäniemi, A, Löyttyniemi, E, Suominen, T, and Välimäki, M. Stigmatizing attitudes in nurses towards people with mental illness: a cross-sectional study in primary settings in Finland. J Psychiatr Ment Health Nurs. (2016) 23:427–37. doi: 10.1111/jpm.12319
39. Babicki, M, Kotowicz, K, and Mastalerz-Migas, A. The assessment of attitudes of medical doctors towards psychiatric patients-a cross-sectional online survey in Poland. Int J Environ Res Public Health. (2021) 18:6419. doi: 10.3390/ijerph18126419
40. Saad, SY, Almatrafi, AS, Ali, RK, Mansouri, YM, and Andijani, OM. Stigmatizing attitudes of tertiary hospital physicians towards people with mental disorders in Saudi Arabia. Saudi Med J. (2019) 40:936–42. doi: 10.15537/smj.2019.9.24510
41. Movahedi, S, Shariat, SV, and Shalbafan, M. Attitude of Iranian medical specialty trainees toward providing health care services to patients with mental disorders. Front Psych. (2022) 13:961538. doi: 10.3389/fpsyt.2022.961538
42. Porfyri, GN, Athanasiadou, M, Siokas, V, Giannoglou, S, Skarpari, S, Kikis, M, et al. Mental health-related stigma discrimination and prejudices among Greek healthcare professionals. Front Psych. (2022) 13:1027304. doi: 10.3389/fpsyt.2022.1027304
43. Pignone, MP, Gaynes, BN, Rushton, JL, Burchell, CM, Orleans, CT, Mulrow, CD, et al. Screening for depression in adults: a summary of the evidence for the U.S. preventive services task force. Ann Intern Med. (2002) 136:765–76. doi: 10.7326/0003-4819-136-10-200205210-00013
44. Lopes, AA, Bragg, J, Young, E, Goodkin, D, Mapes, D, Combe, C, et al. Depression as a predictor of mortality and hospitalization among hemodialysis patients in the United States and Europe. Kidney Int. (2002) 62:199–207. doi: 10.1046/j.1523-1755.2002.00411.x
45. Ekers, D, Murphy, R, Archer, J, Ebenezer, C, Kemp, D, and Gilbody, S. Nurse-delivered collaborative care for depression and long-term physical conditions: a systematic review and meta-analysis. J Affect Disord. (2013) 149:14–22. doi: 10.1016/j.jad.2013.02.032
46. Park, SC, Lee, HY, Lee, DW, Hahn, SW, Park, SH, Kim, YJ, et al. Knowledge and attitude of 851 nursing personnel toward depression in general hospitals of Korea. J Korean Med Sci. (2015) 30:953–9. doi: 10.3346/jkms.2015.30.7.953
47. Griffiths, KM, Christensen, H, Jorm, AF, Evans, K, and Groves, C. Effect of web-based depression literacy and cognitive-behavioural therapy interventions on stigmatising attitudes to depression: randomised controlled trial. Br J Psychiatry. (2004) 185:342–9. doi: 10.1192/bjp.185.4.342
48. Griffiths, KM, Christensen, H, and Jorm, AF. Predictors of depression stigma. BMC Psychiatry. (2008) 8:25. doi: 10.1186/1471-244x-8-25
49. Zhu, L, Yao, J, Wu, L, Wang, J, Qiu, M, Zhang, C, et al. Psychometric properties of the depression stigma scale (DSS) in Chinese cancer patients: a cross-sectional study. BMJ Open. (2019) 9:e028429. doi: 10.1136/bmjopen-2018-028429
50. Yang, F, Yang, BX, Stone, TE, Wang, XQ, Zhou, Y, Zhang, J, et al. Stigma towards depression in a community-based sample in China. Compr Psychiatry. (2020) 97:152152. doi: 10.1016/j.comppsych.2019.152152
51. Link, BG, Phelan, JC, Bresnahan, M, Stueve, A, and Pescosolido, BA. Public conceptions of mental illness: labels, causes, dangerousness, and social distance. Am J Public Health. (1999) 89:1328–33. doi: 10.2105/ajph.89.9.1328
52. Haoyu, Y, Yuejiao, S, and Qianjin, T. Reliability and validity of the Chinese version of depression Social Distance Scale. Chin J Clin Psychol. (2020) 28:49–51+81. doi: 10.16128/j.cnki.1005-3611.2020.01.012
53. Lamela, D, Cabral, J, Coelho, S, and Jongenelen, I. Personal stigma, determinants of intention to use technology, and acceptance of internet-based psychological interventions for depression. Int J Med Inform. (2020) 136:104076. doi: 10.1016/j.ijmedinf.2020.104076
54. Siwei, P, Baohua, C, and Wei, W. Stigma against depression among patients and their family members in a clinic of community hospital in Beijing. Chin J Public Health. (2013) 29:1136–9. (in Chinese) doi: 10.11847/zgggws2013-29-08-14
55. Björkman, T, Angelman, T, and Jönsson, M. Attitudes towards people with mental illness: a cross-sectional study among nursing staff in psychiatric and somatic care. Scand J Caring Sci. (2008) 22:170–7. doi: 10.1111/j.1471-6712.2007.00509.x
56. Cremonini, V, Pagnucci, N, Giacometti, F, and Rubbi, I. Health care professionals attitudes towards mental illness: observational study performed at a public health Facility in Northern Italy. Arch Psychiatr Nurs. (2018) 32:24–30. doi: 10.1016/j.apnu.2017.09.007
57. Cook, TM, and Wang, J. Descriptive epidemiology of stigma against depression in a general population sample in Alberta. BMC Psychiatry. (2010) 10:29. doi: 10.1186/1471-244x-10-29
58. Hu, X, Rohrbaugh, R, Deng, Q, He, Q, Munger, KF, and Liu, Z. Expanding the mental health workforce in China: narrowing the mental health service gap. Psychiatr Serv. (2017) 68:987–9. doi: 10.1176/appi.ps.201700002
59. Busby Grant, J, Bruce, CP, and Batterham, PJ. Predictors of personal, perceived and self-stigma towards anxiety and depression. Epidemiol Psychiatr Sci. (2016) 25:247–54. doi: 10.1017/s2045796015000220
60. Huang, Y, Wang, Y, Wang, H, Liu, Z, Yu, X, Yan, J, et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry. (2019) 6:211–24. doi: 10.1016/s2215-0366(18)30511-x
61. Zhang, W, Li, X, Lin, Y, Zhang, X, Qu, Z, Wang, X, et al. Pathways to psychiatric care in urban North China: a general hospital based study. Int J Ment Health Syst. (2013) 7:22. doi: 10.1186/1752-4458-7-22
62. Henderson, C, Noblett, J, Parke, H, Clement, S, Caffrey, A, Gale-Grant, O, et al. Mental health-related stigma in health care and mental health-care settings. Lancet Psychiatry. (2014) 1:467–82. doi: 10.1016/s2215-0366(14)00023-6
63. De Hert, M, Correll, CU, Bobes, J, Cetkovich-Bakmas, M, Cohen, D, Asai, I, et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry. (2011) 10:52–77. doi: 10.1002/j.2051-5545.2011.tb00014.x
64. Kakuma, RD, Minas, HF, van Ginneken, NM, Dal Poz, MRP, Desiraju, KMA, Morris, JEP, et al. Human resources for mental health care: current situation and strategies for action. Lancet. (2011) 378:1654–63. doi: 10.1016/S0140-6736(11)61093-3
65. Corrigan, PW, Mittal, D, Reaves, CM, Haynes, TF, Han, X, Morris, S, et al. Mental health stigma and primary health care decisions. Psychiatry Res. (2014) 218:35–8. doi: 10.1016/j.psychres.2014.04.028
66. Corrigan, PW. Lessons learned from unintended consequences about erasing the stigma of mental illness. World Psychiatry. (2016) 15:67–73. doi: 10.1002/wps.20295
67. Grandón, P, Saldivia, S, Cova, F, Bustos, C, Vaccari, P, Ramírez-Vielma, R, et al. Effectiveness of an intervention to reduce stigma towards people with a severe mental disorder diagnosis in primary health care personnel: programme Igual-Mente. Psychiatry Res. (2021) 305:114259. doi: 10.1016/j.psychres.2021.114259
Keywords: stigma, nurse, mental disorder, survey, China
Citation: Li L, Lu S, Xie C and Li Y (2023) Stigmatizing attitudes toward mental disorders among non-mental health nurses in general hospitals of China: a national survey. Front. Psychiatry. 14:1180034. doi: 10.3389/fpsyt.2023.1180034
Edited by:
Eduardo Fernández-Jiménez, University Hospital La Paz, SpainReviewed by:
Mohammadreza Shalbafan, Iran University of Medical Sciences, IranGianluca Serafini, San Martino Hospital (IRCCS), Italy
Copyright © 2023 Li, Lu, Xie and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yamin Li, YW1pbm55QGNzdS5lZHUuY24=
 Li Li
Li Li Shurong Lu4
Shurong Lu4 Yamin Li
Yamin Li