
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 26 October 2023
Sec. Adolescent and Young Adult Psychiatry
Volume 14 - 2023 | https://doi.org/10.3389/fpsyt.2023.1175002
This article is part of the Research Topic Exploration of Major Depressive Disorder among Children and Adolescents: From Pathogenesis to Intervention View all 15 articles
Objective: To date, no national-scale drug usage survey for adolescents with depression has been conducted in China, and the purpose of this study was to examine the national trends in prescriptions in Chinese adolescent depression patients from 2017 to 2021.
Methods: Prescribing data were extracted from the Hospital Prescription Analysis Cooperative Project. The average number of patients per year, the cost of treatment, and the prescription patterns (monotherapy vs. combination therapy) were analyzed, and subgroup analyses were conducted depending on age, sex, and drug class.
Results: The study included 674,099 patients from 136 hospitals located in nine major areas of China. Of all patients, the proportion of adolescents increased from 1.63% in 2017 to 6.75% in 2021. Visits by adolescent depression patients increased from 1,973 in 2017 to 9,751 in 2021, and the corresponding cost increased from 607,598 Chinese Yuan in 2017 to 2,228,884 Chinese Yuan in 2021. The incidence of adolescent depression among female individuals was far beyond that among male individuals. Combination therapy was more frequent than monotherapy, and the most commonly prescribed drugs were antidepressants, antipsychotics, antiepileptics, and antianxietics. Despite the use of sertraline decreasing from 47.90 to 43.39%, it was the most frequently used drug.
Conclusion: In summary, the prescriptions and cost of treatment for adolescent depression patients both increased rapidly. The widespread use of those drugs with weak clinical evidence reflects the current state of China, which should arouse our attention. The study can provide references for clinical treatment decisions and a basis for more efficient allocation of healthcare resources by the government.
Depression is one of the most common mental disorders that seriously affects the patients’ psychosocial functions and quality of life. Adolescence is a key life period characterized by rapid social and emotional development, so it is a vulnerable time for depression (1). Despite all age groups experiencing an increase in depression prevalence, the rate of increase among adolescents was significantly more rapid relative to adults (2). In adolescents aged 13–18 years in the United States, the lifetime and 12-month prevalence of major depressive disorder (MDD) were 11.0 and 7.5%, respectively (3), according to the “China National Mental Health Development Report (2019–2020)” released by the Institute of Psychology of the Chinese Academy of Sciences. Detection rate is the detection rate of depressive symptoms. The survey was conducted using a self-rating scale. According to the score, there is no, mild, or severe depression. The results of the scale can only reflect the severity of depression at a certain time but not a diagnosis. The detection rate of depression among Chinese adolescents was 24.6%, and the rate of MDD was 7.4%. Adolescents with depression have an elevated risk of other psychopathology (4), physical health outcomes (5, 6) and recurrence in later life (7); meanwhile, the increase in suicide attempts, nicotine abuse, alcoholism, and drug abuse have been found to be associated with adolescent depression (8, 9).
Except for psychotherapy, drug therapy is one of the main treatment methods for depression in adolescents, and various factors influence the choice of drug, including the depression type, severity of the symptom, patient age, guidelines, prescribing doctor’s experience, cost, and so on. Therefore, understanding the current situation of adolescent depression drug usage is crucial for improving depression treatment. For now, there is little information available about the use of drugs for adolescent depression in China. Therefore, to assess the time trends and patterns of prescriptions for adolescents with depression, we conducted a cross-sectional study in nine major areas in China from 2017 to 2021.
Ethics approval was obtained from the First Affiliated Hospital of Zhejiang Chinese Medical University for this study. This study was retrospective, so informed consent was not required.
A database from the Hospital Prescription Analysis Cooperative Project was used to extract the data, and this approach has been used widely in Chinese pharmacoepidemiology studies and has been validated (10, 11). Participating hospitals provided prescription information for the database on sampling days. During the year, there were 40 randomized sampling days, not a full year of data; that is, the data were sampled randomly. The prescription data included the code, sex, age of patients, date, location, diagnosis, generic drug name, dose, and cost. This study included outpatient prescriptions meeting the following criteria: (1) prescriptions for patients aged 12–17 years; (2) those for the diagnosis of depression, without restrictions on the diagnostic criteria and severity of disease; (3) those issued from hospitals in Beijing, Shanghai, Guangzhou, Hangzhou, Chengdu, Zhengzhou, Shenyang, Tianjin, and Heilongjiang that participated in the program continuously from 2017 to 2021. Data were obtained from hospitals located in the east, west, south, and north of China, which covered a substantial geographical area and represented the entirety of the country.
Trends in proportions will be tested by the Cochran–Armitage trend test. Other trends will be analyzed by the Mann–Kendall trend test. The statistical analysis was conducted using R Version 4.2.11 software.
A total of 674,099 patients issued from 2017 to 2021 were identified in this study. As Table 1 and Figure 1 indicate, during the study period, there was no significant trend in patients with depression (p = 0.462), while the proportion of adolescents increased from 1.63% in 2017 to 6.75% in 2021 (p < 0.001). The adolescence visits increased from 1,973 in 2017 to 9,751 in 2021 (p = 0.027), and the total expenditure increased dramatically from 607,598 Chinese Yuan (CNY) in 2017 to 2,228,884 CNY in 2021 (p = 0.027).
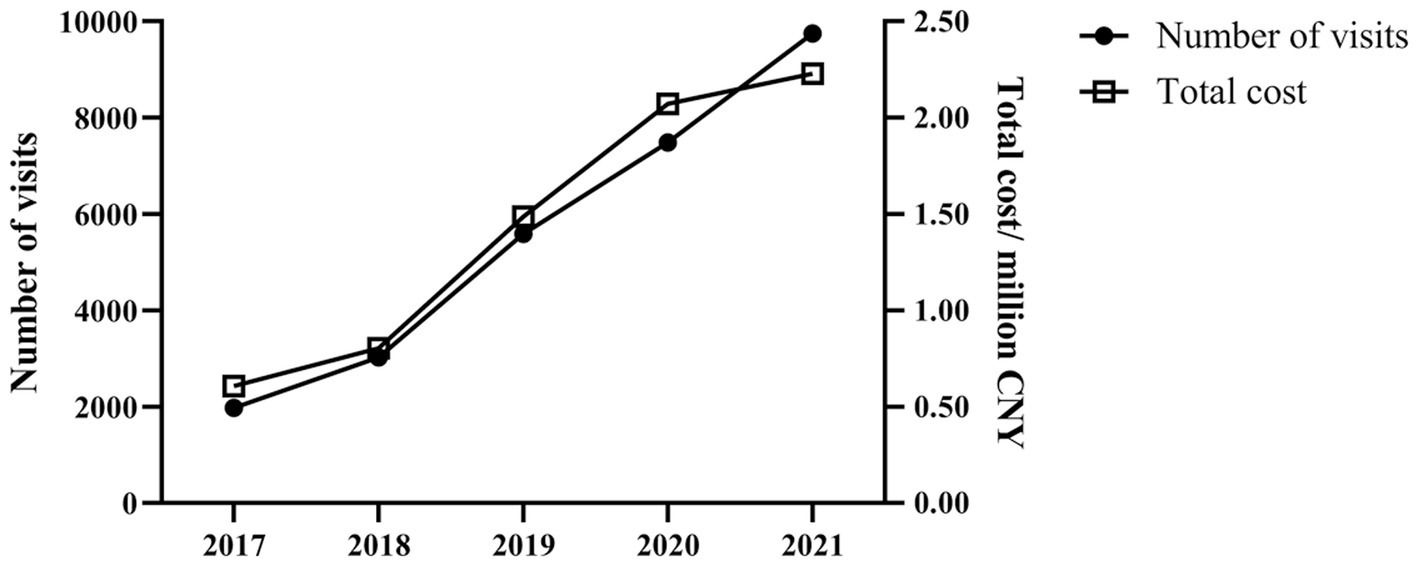
Figure 1. Trends in visits and cost of adolescents with depression in 136 hospitals located in nine major areas of China from 2017 to 2021.
A stratified analysis of the trends in depression among adolescents by sex is shown in Table 2, the proportion of females (67.56–76.68%) was generally higher than male patients (23.32–32.44%), and the proportion of females showed a significant increase trend, while the trend of males decreased obviously (both p < 0.001).
Figure 2 shows the trends in treatment patterns. Combination therapy was the predominant pattern of treatment, monotherapy showed a decreasing trend over time (p < 0.001), while the proportion of dual combination therapy and triple or more combination therapy kept on increasing during the 5-year period (both p < 0.001).
Figure 3 and Table 3 show annual prescriptions of drug classes and specific drugs. The most commonly prescribed drug classes were antidepressants, antipsychotics, antiepileptics, and antianxietics. Antidepressants remained in the leading position of the prescriptions (49.52–55.99%) though the percentage showed a decreasing trend (p < 0.001). The use of antipsychotics (20.55–25.89%), and anxiolytics (9.56–13.86%) increased over the period; however, the percentage of antiepileptics decreased from 10.86% in 2017 to 8.14% in 2021 (all p < 0.001). Nearly half of the patients were prescribed sertraline, the most commonly prescribed drug, but its use rate among visits continued to decrease (p < 0.001). At the end of the study, quetiapine and fluoxetine were the second and third most commonly prescribed drugs, respectively, and both showed an increasing trend (both p < 0.001).
In China, there is limited research being conducted on prescription patterns for adolescents with depression. As far as we know, this study is the most comprehensive evaluation of drug use and trends among this patient group in China because the data were drawn from 136 hospitals located in nine major areas of China, and the results are nationally representative. Adolescents with depression are often accompanied by other complications. There are more than 70 diagnoses including depression in China. The objective of this study was to understand the prescribing patterns of adolescent patients diagnosed with depression in China.
As we know, the prevalence of depression increased significantly in China and around the world (2, 12). However, in this study, over the course of the study period, there were no significant trends among patients with depression. When the data from the last 2 years were excluded, it showed a significant increasing trend. The abnormal fluctuations in 2020 and 2021 may be due to COVID-19, which has spread quickly around the world since December 2019. Many studies have confirmed that outpatient and inpatient volume in healthcare facilities at all levels in China declined significantly during pandemics (13–15). It is important to note that adolescent visits have risen sharply over time, especially in female subjects, and female visits were twice as common as male visits in 2017, while the ratio jumped to 3.1 in 2021, according to several epidemiological studies (16–18), approximately twice as many females suffer from depression as males; however, the factors causing this difference to remain unclear, and biological (19, 20) and social stress (21) mechanisms might account for the gender gap.
Guidelines (22, 23) in many countries suggest a stepwise approach for the treatment of depression in adolescents. For mild depression, the National Institute for Health and Clinical Excellence (NICE) and the American Psychological Association (APA) recommend that psychotherapy and cognitive-behavioral therapy might be sufficient interventions, and antidepressant medication should not be used in the initial stage of treatment. For adolescents with moderate-to-severe depression, NICE recommends combined therapy (fluoxetine and psychological therapy) if adolescents fail to respond to a specific psychological therapy after four to six sessions, and suggests that sertraline or citalopram is the second-line treatment when fluoxetine does not work or is not tolerated due to side effects. Fluoxetine was approved by the US Food and Drug Administration (US FDA) to treat depression in children aged 8 years or older, and escitalopram was approved in adolescents aged 12–17 years. In China, none of the antidepressants was approved for treating depression in adolescents until 31 May 2021; from that day on, fluoxetine was approved by the China Food and Drug Administration (C FDA) for the treatment of moderate-to-severe depression in children aged 8 years or older. In our study, the most commonly prescribed drugs for treating adolescent depression were antidepressants. More than half of the prescriptions and more than 80% of visits used it. Selective serotonin reuptake inhibitors (SSRIs) were the predominant antidepressants in China. Among the antidepressants, sertraline occupies the most prominent position. Although its use rate continued to decrease, those that ranked second to fourth were fluoxetine, fluvoxamine, and escitalopram in 2021, whose proportions were 11.03, 8.89, and 7.47%, respectively. The substantial use of sertraline for adolescents was also reported in other countries (24–27), which may be owing to its effectiveness and well tolerated with mild adverse reactions (28, 29). Fluoxetine was the first drug approved by the US FDA for the treatment of adolescent depression, and according to previous meta-analyses (30, 31), fluoxetine (alone or in combination with cognitive-behavioral therapy) was the most effective treatment for acute moderate-to-severe depressive disorder in adolescents. While only one in ten visits used it in China, the usage of fluoxetine showed a significant increasing trend over the study period, and the latter trend is worth paying attention to. Fluvoxamine was approved for obsessive-compulsive disorder (OCD) and has a good therapeutic effect for depression with psychotic symptoms, anxiety, fear, impulse motion, suicidal behavior, and obsessive thinking. In Japan (27), fluvoxamine was the third-choice agent (selected by 13% of physicians) for adolescents with depression because of the long history of clinical use and safety profile known. Similar results were achieved in our study as the ranked third antidepressant, prescription of fluvoxamine increased progressively and the proportion maintained at approximately 8% for years. Escitalopram, the S-enantiomer of racemic citalopram, was recommended for patients older than 12 years by the US FDA, and a small amount of evidence showed that escitalopram was effective for depression in adolescents (32); however, there was just a small proportion of prescriptions for escitalopram in our study, and the high cost may restrict its use. A significant increase in suicidal behavior was observed in young people taking venlafaxine (31), and NICE guidelines (22) recommend against its usage. A downward trend of venlafaxine has been observed in this study, which is encouraging.
Depressive episodes were not only the core of depressive disorder (unipolar depression) but also the main clinical phase of bipolar disorders (BDs). BDs are psychiatric disorders with both depressive and manic episodes, which include bipolar I disorder and bipolar II disorder (33). By the end of this study, the percentage of patients receiving monotherapy was less than half and showed a significant decreasing trend over time, which suggests that the standard therapeutic approach failed to achieve satisfactory results on a majority of occasions. For adolescents with BD, augmenting the treatment strategy with antipsychotics or mood stabilizers should be considered. Lithium carbonate is classified as an antipsychotic drug in China’s current medical insurance list; therefore, in this study, we analyzed it together with other antipsychotics. Lithium carbonate as the first-generation mood stabilizer was approved by the US FDA for the treatment of manic or mixed episodes in adolescents. Atypical antipsychotics (olanzapine, quetiapine, aripiprazole, and risperidone) as second-generation mood stabilizers were also approved, while valproate (first-generation mood stabilizer) has not been approved up to now. In China, the use of sodium valproate coincides with US-FDA approval which showed a significant downward trend. Unfortunately, due to the fragmented evidence of psychotropic agents in adolescents, there was still no consensus on the efficacy of the drug on BD. For instance, Renk et al. (34) found that atypical antipsychotics were more effective than lithium in the treatment of manic and mixed episodes; however, McIntyre et al. (33) regarded lithium as the gold standard mood stabilizer. When it comes to treating a depressive episode of BD, the US FDA recommends a combination of olanzapine and fluoxetine, while according to experts in China, quetiapine, olanzapine, and a combination of lithium and lamotrigine were recommended as Class A (bipolar I disorder), and quetiapine was recommended as Class A (bipolar II disorder). In our study, quetiapine has replaced olanzapine as the most prescribed antipsychotic since 2018, which was consistent with the Chinese guidelines, and although prescriptions of lithium accounted for a small proportion of visits, its growth rate was the fastest and more than doubled in the 5 years. In addition to the efficacy, the safety of psychotropic agents needs to be considered. A high risk of weight gain was found for olanzapine and quetiapine. Risperidone and olanzapine showed significantly higher prolactin increase (35).
Antianxietic is a type of medication used to relieve anxiety and tension. Throughout the study period, the top four most used antianxietics were alprazolam, lorazepam, oxazepam, and tandospirone; the first three drugs belong to the benzodiazepines (BZDs) and tandospirone is a 5-hydroxytryptamine (5-HT) 1A receptor agonist. For the treatment of anxiety in adolescents, guidelines recommend SSRIs as first-line pharmacotherapy and serotonin-norepinephrine reuptake inhibitors (SNRIs) as the second-line pharmacotherapy (36–38). Studies of BZDs in adolescents with anxiety were limited, and some controlled trials have not shown efficacy. Simeon et al. (39) found that alprazolam and placebo did not differ statistically in terms of clinical global rating. Similarly, in another study of alprazolam (40), there were no significant differences among the alprazolam, imipramine, and placebo groups on change in anxiety scales. In this regard, the rapid rise of BZD prescriptions in China needs attention. Clinicians should use BZDs more cautiously not only because of their low efficiency but also because of the possibility of substance dependence, substance abuse, and side effects (36). Compared with the BZDs, tandospirone has a significantly lower abuse potential (41). In a study of adolescents with anxiety disorder (42), tandospirone has shown safety and efficacy that was not inferior to sertraline; however, larger and longer clinical trials are needed.
This study had some limitations. First, the cohort was not stratified by complication or severity. There are no data on how the prescription pattern differs between patients with depression alone and depressed patients with comorbidities. They require a more detailed investigation. Second, the included hospitals were all located in major cities, which may have caused sampling bias.
In summary, the prescriptions and cost of treatment for adolescent depression patients both increased rapidly. The widespread use of those drugs with weak clinical evidence reflects the current state of China, which should arouse our attention. The study can provide references for clinical treatment decisions and a basis for more efficient allocation of health care resources by the government.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
LW and FW: conceptualization. LZ, YZ, and JY: data curation. LW, LZ, YZ, JY, NB, WF, and FW: formal analysis. FW: funding acquisition and resources. WF and FW: investigation. LZ, YZ, JY, and NB: methodology. WF and FW: validation. All authors contributed to the article and approved the submitted version.
This study was funded by the Health Commission of Zhejiang Province, China (2023RC197).
The authors would like to thank the Hospital Prescription Analysis Corporation Program of China for collecting and providing the data.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Ho, TC. Stress and neurodevelopment in adolescent depression. Biol Psychiatry. (2019) 86:e33–5. doi: 10.1016/j.biopsych.2019.09.012
2. Weinberger, AH, Gbedemah, M, Martinez, AM, Nash, D, Galea, S, and Goodwin, RD. Trends in depression prevalence in the USA from 2005 to 2015: widening disparities in vulnerable groups. Psychol Med. (2018) 48:1308–15. doi: 10.1017/S0033291717002781
3. Avenevoli, S, Swendsen, J, He, JP, Burstein, M, and Merikangas, KR. Major depression in the national comorbidity survey-adolescent supplement: prevalence, correlates, and treatment. J Am Acad Child Adolesc Psychiatry. (2015) 54:37–44.e2. doi: 10.1016/j.jaac.2014.10.010
4. Costello, EJ, and Maughan, B. Annual research review: optimal outcomes of child and adolescent mental illness. J Child Psychol Psychiatry. (2015) 56:324–41. doi: 10.1111/jcpp.12371
5. Goldstein, BI, and Korczak, DJ. Links between child and adolescent psychiatric disorders and cardiovascular risk. Can J Cardiol. (2020) 36:1394–405. doi: 10.1016/j.cjca.2020.06.023
6. Mannan, M, Mamun, A, Doi, S, and Clavarino, A. Prospective associations between depression and obesity for adolescent males and females-a systematic review and Meta-analysis of longitudinal studies. PLoS One. (2016) 11:e0157240. doi: 10.1371/journal.pone.0157240
7. Johnson, D, Dupuis, G, Piche, J, Clayborne, Z, and Colman, I. Adult mental health outcomes of adolescent depression: a systematic review. Depress Anxiety. (2018) 35:700–16. doi: 10.1002/da.22777
8. Groenman, AP, Janssen, TWP, and Oosterlaan, J. Childhood psychiatric disorders as risk factor for subsequent substance abuse: a meta-analysis. J Am Acad Child Adolesc Psychiatry. (2017) 56:556–69. doi: 10.1016/j.jaac.2017.05.004
9. Harrington, R. Depression, suicide and deliberate self-harm in adolescence. Br Med Bull. (2001) 57:47–60. doi: 10.1093/bmb/57.1.47
10. Yu, Z, Zhang, J, Zheng, Y, and Yu, L. Trends in antidepressant use and expenditure in six major cities in China from 2013 to 2018. Front Psych. (2020) 11:551. doi: 10.3389/fpsyt.2020.00551
11. Yu, Z, Wu, X, Zhu, J, Jin, J, Zhao, Y, and Yu, L. Trends in topical Prescriptional therapy for old patients with dry eye disease in six major areas of China: 2013-2019. Front Pharmacol. (2021) 12:690640. doi: 10.3389/fphar.2021.690640
12. Bai, R, Dong, W, Peng, Q, and Bai, Z. Trends in depression incidence in China, 1990-2019. J Affect Disord. (2022) 296:291–7. doi: 10.1016/j.jad.2021.09.084
13. Yang, Z, Wu, M, Lu, J, Li, T, Shen, P, Tang, M, et al. Effect of COVID-19 on hospital visits in Ningbo, China: an interrupted time-series analysis. Int J Qual Health Care. (2021) 33:mzab078. doi: 10.1093/intqhc/mzab078
14. Chen, Y, Cai, M, Li, Z, Lin, X, and Wang, L. Impacts of the COVID-19 pandemic on public hospitals of different levels: six-month evidence from Shanghai. China Risk Manag Healthc Policy. (2021) 14:3635–51. doi: 10.2147/RMHP.S314604
15. Xiao, H, Dai, X, Wagenaar, BH, Liu, F, Augusto, O, Guo, Y, et al. The impact of the COVID-19 pandemic on health services utilization in China: time-series analyses for 2016-2020. Lancet Reg Health West Pac. (2021) 9:100122. doi: 10.1016/j.lanwpc.2021.100122
16. Bromet, E, Andrade, LH, Hwang, I, Sampson, NA, Alonso, J, de Girolamo, G, et al. Cross-national epidemiology of DSM-IV major depressive episode. BMC Med. (2011) 9:90. doi: 10.1186/1741-7015-9-90
17. Platt, JM, Bates, L, Jager, J, McLaughlin, KA, and Keyes, KM. Is the US gender gap in depression changing over time? A meta-regression. Am J Epidemiol. (2021) 190:1190–206. doi: 10.1093/aje/kwab002
18. Salk, RH, Hyde, JS, and Abramson, LY. Gender differences in depression in representative national samples: Meta-analyses of diagnoses and symptoms. Psychol Bull. (2017) 143:783–822. doi: 10.1037/bul0000102
19. Angold, A, and Worthman, CW. Puberty onset of gender differences in rates of depression: a developmental, epidemiologic and neuroendocrine perspective. J Affect Disord. (1993) 29:145–58. doi: 10.1016/0165-0327(93)90029-j
20. Labonté, B, Engmann, O, Purushothaman, I, Menard, C, Wang, J, Tan, C, et al. Sex-specific transcriptional signatures in human depression. Nat Med. (2017) 23:1102–11. doi: 10.1038/nm.4386
21. Horwitz, AV. The sociological study of mental illness: A critique and synthesis of four perspectives. In: CS Aneshensel, JC Phelan, and A Bierman, editors. Handbook of the sociology of mental health. New York, NY: Springer (2013). p. 95–112.
22. National Institute for Health and Care Excellence (NICE). Depression in Children and Young People: Identification and Management. London: National Institute for Health and Care Excellence (NICE) (2019).
23. Guideline Development Panel for the Treatment of Depressive Disorders. Summary of the clinical practice guideline for the treatment of depression across three age cohorts. Am Psychol. (2022) 77:770–80. doi: 10.1037/amp0000904
24. Czaja, AS, and Valuck, R. Off-label antidepressant use in children and adolescents compared with young adults: extent and level of evidence. Pharmacoepidemiol Drug Saf. (2012) 21:997–1004. doi: 10.1002/pds.3312
25. Maršanić, VB, Margetić, BA, and Margetić, B. Outpatient treatment of children and adolescents with antidepressants in Croatia. Int J Psychiatry Clin Pract. (2012) 16:214–22. doi: 10.3109/13651501
26. Braüner, JV, Johansen, LM, Roesbjerg, T, and Pagsberg, AK. Off-label prescription of psychopharmacological drugs in child and adolescent psychiatry. J Clin Psychopharmacol. (2016) 36:500–7. doi: 10.1097/JCP.0000000000000559
27. Saito, T, Reines, EH, Florea, I, and Dalsgaard, MK. Management of Depression in adolescents in Japan. J Child Adolesc Psychopharmacol. (2019) 29:753–63. doi: 10.1089/cap.2019.0023
28. Wagner, KD, Ambrosini, P, Rynn, M, Wohlberg, C, Yang, R, Greenbaum, MS, et al. Sertraline pediatric depression study group. Efficacy of sertraline in the treatment of children and adolescents with major depressive disorder: two randomized controlled trials. JAMA. (2003) 290:1033–41. doi: 10.1001/jama.290.8.1033
29. Ma, D, Zhang, Z, Zhang, X, and Li, L. Comparative efficacy, acceptability, and safety of medicinal, cognitive-behavioral therapy, and placebo treatments for acute major depressive disorder in children and adolescents: a multiple-treatments meta-analysis. Curr Med Res Opin. (2014) 30:971–95. doi: 10.1185/03007995.2013.860020
30. Cipriani, A, Zhou, X, Del Giovane, C, Hetrick, SE, Qin, B, Whittington, C, et al. Comparative efficacy and tolerability of antidepressants for major depressive disorder in children and adolescents: a network meta-analysis. Lancet. (2016) 388:881–90. doi: 10.1016/S0140-6736(16)30385-3
31. Zhou, X, Teng, T, Zhang, Y, Del Giovane, C, Furukawa, TA, Weisz, JR, et al. Comparative efficacy and acceptability of antidepressants, psychotherapies, and their combination for acute treatment of children and adolescents with depressive disorder: a systematic review and network meta-analysis. Lancet Psychiatry. (2020) 7:581–601. doi: 10.1016/S2215-0366(20)30137-1
32. Hetrick, SE, McKenzie, JE, Bailey, AP, Sharma, V, Moller, CI, Badcock, PB, et al. New generation antidepressants for depression in children and adolescents: a network meta-analysis. Cochrane Database Syst Rev. (2021) 2021:CD013674. doi: 10.1002/14651858.CD013674.pub2
33. McIntyre, RS, Berk, M, Brietzke, E, Goldstein, BI, López-Jaramillo, C, Kessing, LV, et al. Bipolar disorders. Lancet. (2020) 396:1841–56. doi: 10.1016/S0140-6736(20)31544-0
34. Renk, K, White, R, Lauer, BA, McSwiggan, M, Puff, J, and Lowell, A. Bipolar disorder in children. Psychiatry J. (2014) 2014:928685. doi: 10.1155/2014/928685
35. Krause, M, Zhu, Y, Huhn, M, Schneider-Thoma, J, Bighelli, I, Chaimani, A, et al. Efficacy, acceptability, and tolerability of antipsychotics in children and adolescents with schizophrenia: a network meta-analysis. Eur Neuropsychopharmacol. (2018) 28:659–74. doi: 10.1016/j.euroneuro.2018.03.008
36. Connolly, SD, and Bernstein, GA, Work Group on Quality Issues. Practice parameter for the assessment and treatment of children and adolescents with anxiety disorders. J Am Acad Child Adolesc Psychiatry. (2007) 46:267–83. doi: 10.1097/01.chi.0000246070.23695.06
37. Wang, Z, Whiteside, SPH, Sim, L, Farah, W, Morrow, AS, Alsawas, M, et al. Comparative effectiveness and safety of cognitive behavioral therapy and pharmacotherapy for childhood anxiety disorders: a systematic review and Meta-analysis. JAMA Pediatr. (2017) 171:1049–56. doi: 10.1001/jamapediatrics.2017.3036
38. Walter, HJ, Bukstein, OG, Abright, AR, Keable, H, Ramtekkar, U, Ripperger-Suhler, J, et al. Clinical practice guideline for the assessment and treatment of children and adolescents with anxiety disorders. J Am Acad Child Adolesc Psychiatry. (2020) 59:1107–24. doi: 10.1016/j.jaac.2020.05.005
39. Simeon, JG, Ferguson, HB, Knott, V, Roberts, N, Gauthier, B, Dubois, C, et al. Clinical, cognitive, and neurophysiological effects of alprazolam in children and adolescents with overanxious and avoidant disorders. J Am Acad Child Adolesc Psychiatry. (1992) 31:29–33. doi: 10.1097/00004583-199201000-00006
40. Bernstein, GA, Garfinkel, BD, and Borchardt, CM. Comparative studies of pharmacotherapy for school refusal. J Am Acad Child Adolesc Psychiatry. (1990) 29:773–81. doi: 10.1097/00004583-199009000-00016
41. Evans, SM, Troisi, JR 2nd, and Griffiths, RR. Tandospirone and alprazolam: comparison of behavioral effects and abuse liability in humans. J Pharmacol Exp Ther. (1994) 271:683–94.
Keywords: adolescent depression, antidepressant, antipsychotic, sertraline, prescription
Citation: Wang L, Zhou L, Zhu Y, Yan J, Bu N, Fei W and Wu F (2023) Trends in prescription therapy for adolescents with depression in nine major areas of China during 2017–2021. Front. Psychiatry. 14:1175002. doi: 10.3389/fpsyt.2023.1175002
Received: 27 February 2023; Accepted: 06 October 2023;
Published: 26 October 2023.
Edited by:
Kaj Sparle Christensen, Aarhus University, DenmarkReviewed by:
Michihiro Takahashi, Takahashi Psychiatric Clinic, JapanCopyright © 2023 Wang, Zhou, Zhu, Yan, Bu, Fei and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fan Wu, d2Y5MDAyMTJAMTI2LmNvbQ==; Weidong Fei, ZmVpd2VpZG9uZ0B6anUuZWR1LmNu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.