- 1Department of Pediatrics, College of Medicine, Yonsei University, Seoul, Republic of Korea
- 2Department of Psychiatry, Institute of Behavioral Sciences in Medicine, College of Medicine, Yonsei University, Seoul, Republic of Korea
- 3Biostatistics Collaboration Unit, College of Medicine, Yonsei University, Seoul, Republic of Korea
Introduction: Suicide is the leading cause of death among Korean adolescents. Suicide has been found to be associated with body mass index (BMI), height, and subjective body image among adults, but investigations of these associations among adolescents are limited. Thus, we aimed to examine to what extent suicide ideation is associated with height, BMI, and subjective body image among Korean adolescents.
Methods: This study examined the data of 6,261 adolescents, selected from a nationally representative survey. The participants were divided into subgroups by sex, suicide ideation, and subjective body image. Logistic regression analyses were performed to examine the association of suicide ideation with height, BMI, and subjective body image.
Results: The proportion of perceived obesity was high in the total sample; the height Z-score was lower for the group with suicide ideation than the group without suicide ideation; the height Z-scores were also lower for female participants with suicide ideation than those female participants without suicide ideation. The proportions of depressed mood, suicide ideation, and suicide attempts were higher among the total sample and female participants with perceived obesity than among those with a normal body image. On logistic regression, perceived obesity was positively associated with suicide ideation even after adjusting for age, height Z-score, weight Z-score, and depressed mood, whereas height Z-score was negatively associated with suicide ideation. These relationships were more prominent among female participants than among male participants.
Conclusion: Low height and perceived obesity, not real obesity, are associated with suicide ideation among Korean adolescents. These findings indicate that the need for an integrated approach to growth, body image, and suicide in adolescents is warranted.
1. Introduction
According to the WHO, suicide is the third leading cause of death among adolescents globally (1). Moreover, the suicide rate in South Korea is the highest among the Organization for Economic Co-operation and Development countries, and suicide is the leading cause of death among Korean adolescents (1–3). In global studies, the prevalence of depression and suicide ideation among adolescents has been reported at 12.0 and 14.0%, respectively (4, 5). Among Korean adolescents, these rates increased to 13.6 and 19.1%, respectively (6, 7). Although it is impossible to prevent all suicides because of the multifactorial complexity, it is important to clarify the modifiable factors of suicide (8).
Short stature, that is, height below the third percentile or more than 2 standard deviations below the corresponding mean height for those of the same sex, age, and race (9), is associated with psychosocial problems and medical conditions, such as poor diet, genetic predisposition, physical activity, and underlying diseases (10, 11). In children and adolescents, regardless of cause, short stature leads to functional impairment in daily life (12). Youths with short stature tend to have behavioral problems as well as negative social experiences, including teasing, lower social acceptance, and lack of friends (13, 14). Although short stature often represents a normal variation in the general population, negative social stereotypes associated with short stature still exist, resulting in poor psychosocial performance in short children who are actually normal (15). A negative association between all-cause mortality and adult height in a cohort study implied that short stature was positively associated with mortality risk owing to genetics, socioeconomic factors, nutritional factors, or a previous infection marker in childhood (10, 11). In a Swedish study, short height was associated with an increased risk of suicide attempts among young men (11). A systematic review reported that depression might be related to relevant neurobiological dysfunctions, in particular, immune-inflammatory abnormalities (16). However, few studies in the literature have examined the exact association between height and suicide among adolescents.
Obesity is a complex disease associated with medical conditions, including chronic diseases as well as psychological distress (17, 18). Bjerkeset et al. (19) reported that body mass index (BMI) was positively associated with the risk of depression among adults (19). Moreover, a population-based study demonstrated that BMI was positively associated with suicide ideation among women (20). Given that the global prevalence of obesity among youth increased from 0.9 to 7.8% in male subjects and from 0.7 to 5.6% in female subjects from 1975 to 2016, the attention paid to the association between obesity and mental health has increased (18). Similar to obese adults, obese adolescents also appear to engage higher in suicide ideation (21). Despite the association between BMI and suicide ideation, it is still unclear if these aspects are directly affected by each other or not.
Obesity usually has a negative influence in the form of psychological distress on weight stigma (22). A meta-analysis reported that negative weight stigma is related to psychological distress, including depression and anxiety (23). Owing to negative attitudes, including prejudice and discrimination, which are widely prevalent in media, healthcare, and educational settings, obese individuals are vulnerable to psychological distress (22): negative attitudes typically stem from the social stereotype that obese people are lazy and unmotivated (24). Although weight stigma can motivate some people to lose weight, it can also worsen obesity by decreasing physical activity and increasing binge eating, owing to social isolation (24). Hunger et al. (25) reported that weight-based discrimination was positively related to suicide ideation among adults. Gavin et al. (26) showed that body image dissatisfaction as well as obesity might be risk factors for depression among women. Body image is strongly related to the self-esteem of young adults, and perceived poor body image is usually prevalent among women. Body image dissatisfaction is known to be associated with being overweight (27), and it can mediate the relationship between obesity and depression (26, 27). Moreover, body image is related to eating disorders. A population-based study reported that disordered eating behaviors are related to body image as well as body weight and BMI among adolescents (28). Calugi et al. (29) reported that the assessment of body image should be considered in the treatment of anorexia nervosa. While obesity, body image, and depression seem to be correlated, studies investigating the association between BMI and subjective body image with suicide ideation among adolescents are limited.
Despite several reviews of the associations among height, body weight, subjective body image, and suicidal ideation, it is still unclear which of these factors could be primary targets of suicide prevention. Therefore, this study aimed to investigate the associations between suicide ideation and BMI, height, and subjective body image among Korean adolescents using data from the Korea National Health and Nutrition Examination Survey (KNHANES). We aimed to test the following: (1) height, BMI, and body image are associated with psychological distress including suicidal ideation among adolescents and (2) negative body image might affect mental health even in adolescents without obesity.
2. Methods
2.1. Study population
We conducted a cross-sectional study of 6,261 adolescents aged 12–18 years included in four phases of the KNHANES: IV (2007–2009), V (2010–2012), VI (2013–2015), and VII (2016–2018). Figure 1 shows a flowchart for the study design and patient inclusion.
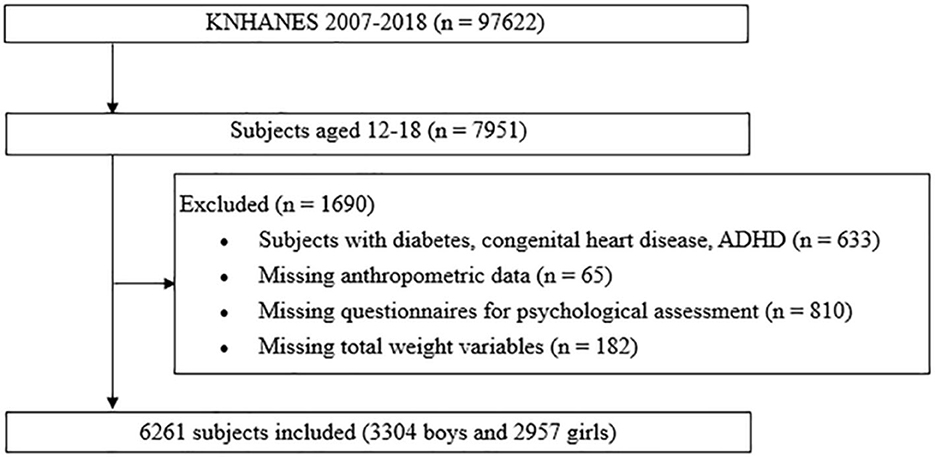
Figure 1. Design and flowchart of the study population. KNHANES, Korea National Health and Nutrition Examination Survey; ADHD, attention deficit hyperactivity syndrome.
The KNHANES is a nationally representative cross-sectional survey, with a stratified and multistage sampling design, conducted by the Korea Centers for Disease Control and Prevention, based on the National Health Promotion Act (30). This cross-sectional survey involves a two-step stratified sampling method using sampling units and households as the primary and secondary sampling units, respectively. The sample weights for sample participants are constructed by accounting for the complex survey design, survey non-response, and post-stratification with a multistage and stratified systematic sampling design, considering non-responders to represent the Korean population. The data from health interviews, health examinations, and nutrition surveys provide information about health status and behavior, socioeconomic demographics, and laboratory tests. Trained interviewers and medical technicians conduct interviews using a structured questionnaire.
2.2. Data collection and study variables
Data on demographic, anthropometric, and behavioral characteristics were collected. Height and weight were measured using standard protocols, and BMI was calculated as weight (kg) divided by height squared (m2). Height and BMI were presented as Z-scores based on the 2017 Korean National Growth Charts (31). Short stature was defined as a height Z-score below −2.0.
Depressed mood, suicide ideation, suicide plans, and suicide attempts were assessed via participants' responses to the following questions (possible responses were “yes” and “no”): “During the past year, did you ever face a period of 2 weeks or more when you felt sad, blue, or depressed nearly every day?,” “During the past year, did you think about dying by suicide?,” “During the past year, did you seriously plan a suicide attempt(s)?,” and “Have you attempted suicide during the past year?” These questions are included in the WHO Composite International Diagnostic Interview-Short Form, which has been validated as a cost-effective screening method for public surveys and is a well-documented predictor of suicide attempts that have been previously used in other surveys (32, 33). Subjective body image was assessed by asking, “In your opinion, how do you perceive your body?” The possible responses included “lean,” “normal,” and “obese.”
2.3. Statistical analyses
The sampling weights were considered in all analyses to report representative estimates of the Korean population. The data were analyzed using SAS version 9.4 (SAS Inc., Cary, NC, USA). All continuous variables were expressed as weighted means with standard errors, whereas categorical variables are expressed as weighted percentages with standard errors. We divided the participants into subgroups according to sex, height Z-score, suicide ideation, subjective body image, and KNHANES phase. Independent two-sample t-test and analysis of variance were used to compare the mean values of continuous variables, and the Rao–Scott chi-square test was used to compare the weighted percentages of categorical variables. Logistic regression analyses were performed to explain the relationship between suicide ideation as a dependent variable and various markers. A p-value < 0.05 was considered statistically significant.
3. Results
3.1. Baseline characteristics of the participants according to sex
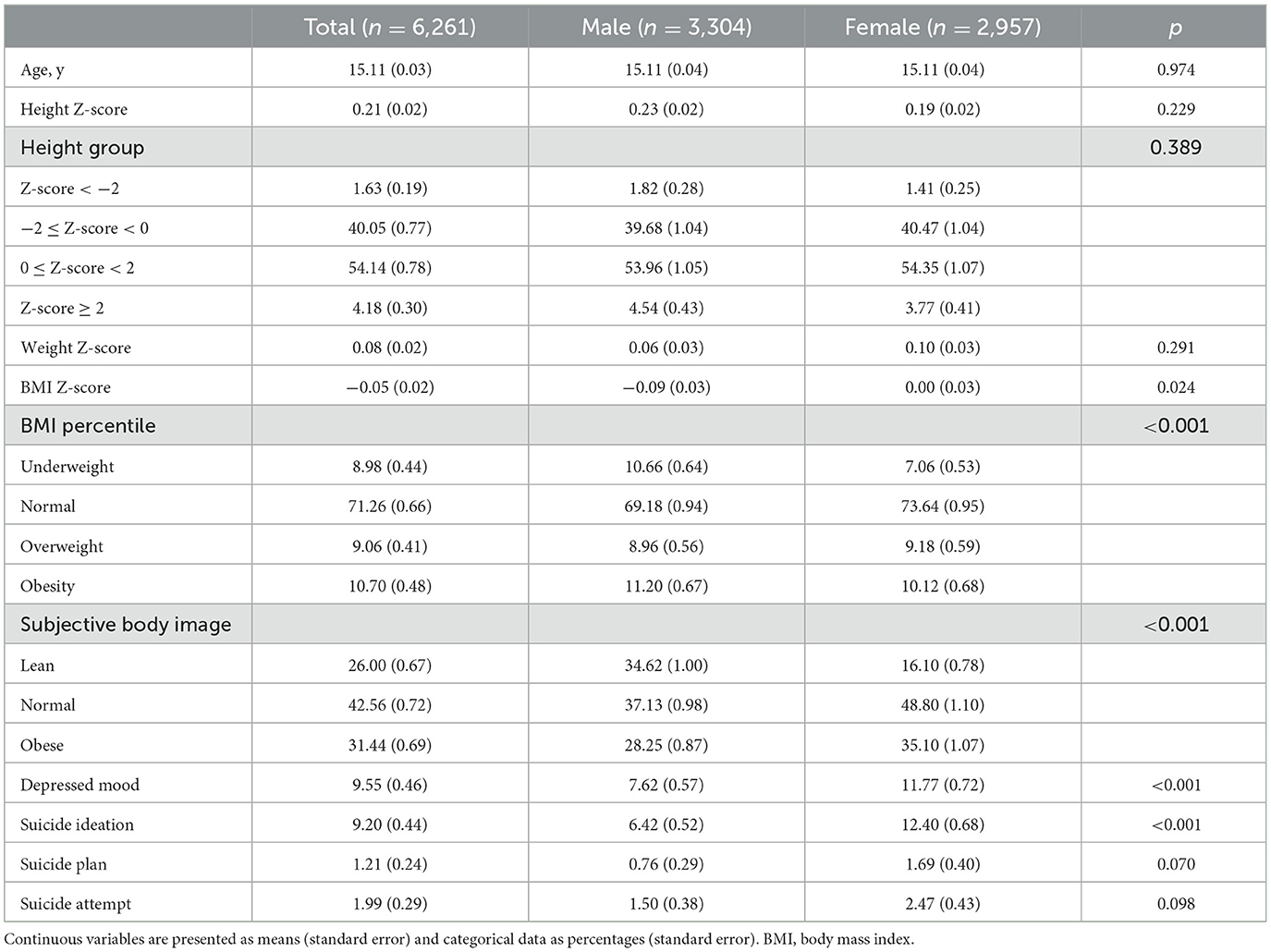
Among the participants, 9.55% reported depressed mood, 9.20% reported suicide ideation, 1.21% had a suicide plan, and 1.99% had attempted suicide (Table 1). Among male participants, 7.62% exhibited depressed mood, 6.42% exhibited suicide ideation, 0.76% had a suicide plan, and 1.50% had attempted suicide. Among female participants, 11.77% reported depressed mood, 12.40% reported suicide ideation, 1.69% had a suicide plan, and 2.47% had attempted suicide. The proportion of participants with obesity was higher among male participants than female participants, whereas the proportion of those with perceived obesity was higher among female participants (all p < 0.001). The proportion of the underweight and those with a lean body image was higher among male participants than in female participants (p < 0.001). In contrast, the proportions of those with depressed mood and suicide ideation were higher among female participants than in male participants (all p < 0.001).
3.2. Characteristics of the participants according to suicide ideation
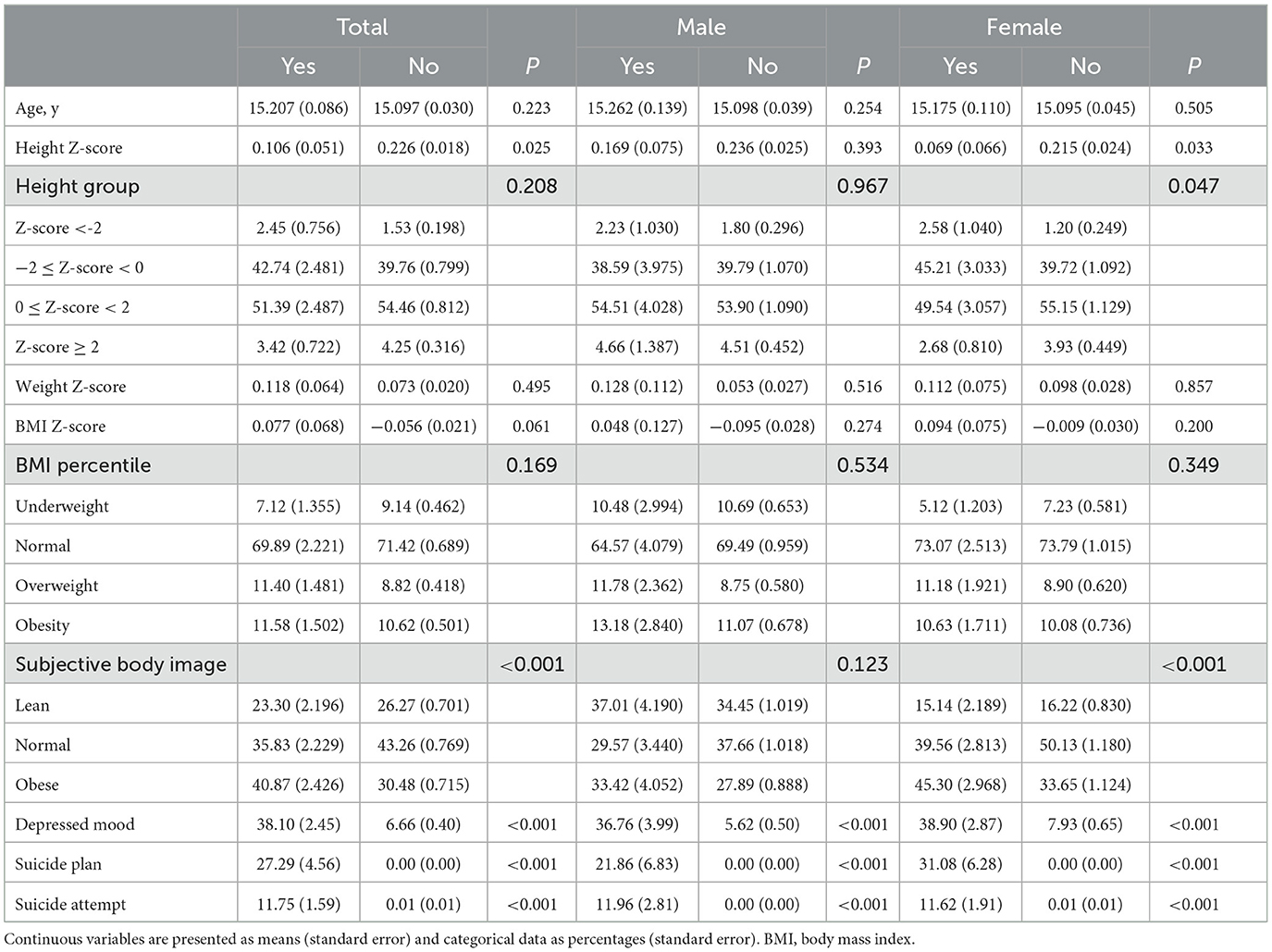
In the subgroup analysis, according to suicide ideation, the height Z-score was lower, and the proportions of individuals with perceived obesity, depressed mood, and a suicide plan and attempt were higher among the participants with suicide ideation than those without suicide ideation (p = 0.025 for height Z-score, all other p < 0.001) (Table 2). Among male participants, the proportions of individuals with depressed mood and a suicide plan and attempt were higher among those with suicide ideation than those without (all p < 0.001). For female participants, the height Z-scores were lower, and the proportions of individuals with short stature, perceived obesity, depressed mood, and suicide plan and attempt were higher in the group with suicide ideation than in the group without (p = 0.033 for height Z-score vs. p = 0.047 for short stature, all other p < 0.001).
3.3. Characteristics of the participants according to subjective body image and height Z-score
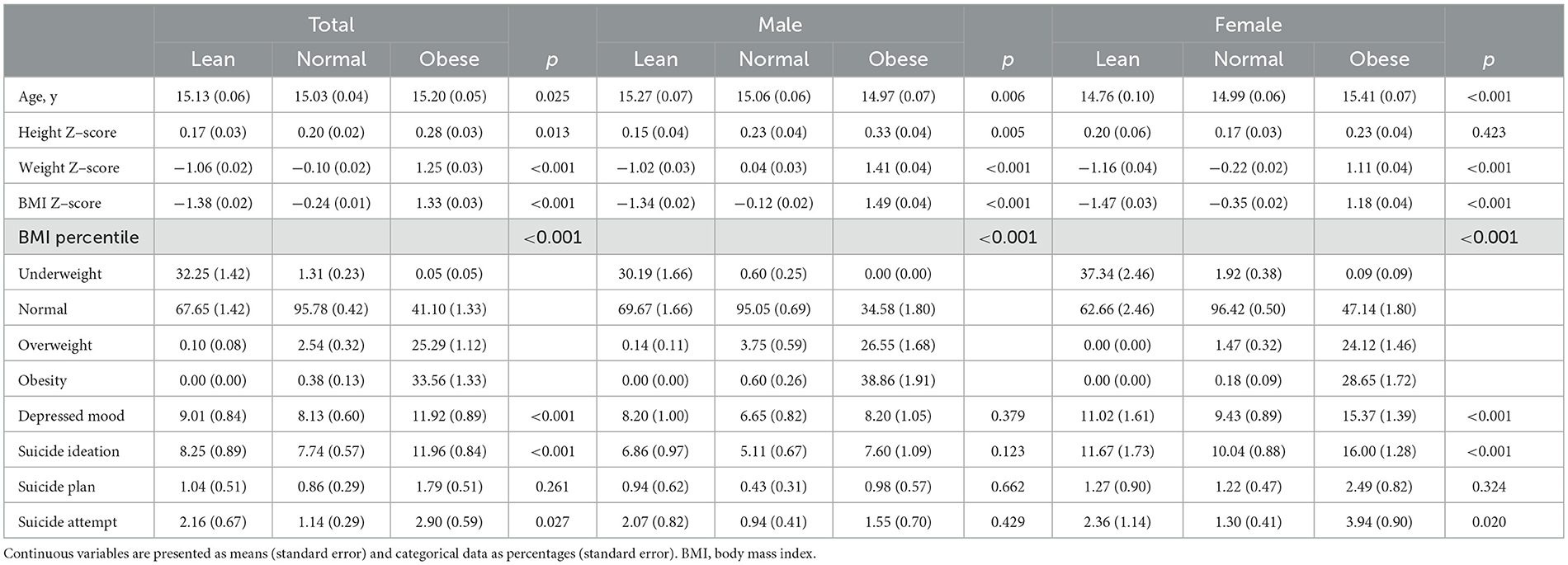
In the subgroup analysis, according to subjective body image, the proportions of depressed mood, suicide ideation, and suicide attempts were higher among all participants with perceived obesity than those with a normal body image (p = 0.027 for suicide attempts, all other p < 0.001) (Table 3). Among all participants with perceived obesity, 41.1% had a normal BMI. Among male participants with perceived obesity, 34.58% had a normal BMI.
The proportions of depressed mood, suicide ideation, and suicide attempts were higher among female participants with perceived obesity than those with a normal body image (p = 0.020 for suicide attempts, all other p < 0.001). Among female participants with perceived obesity, 47.17% had a normal BMI. In the subgroup analysis, according to the height Z-score, the proportion of female participants with suicide ideation decreased with an increase in the height Z-score (p = 0.047) (Figure 2).
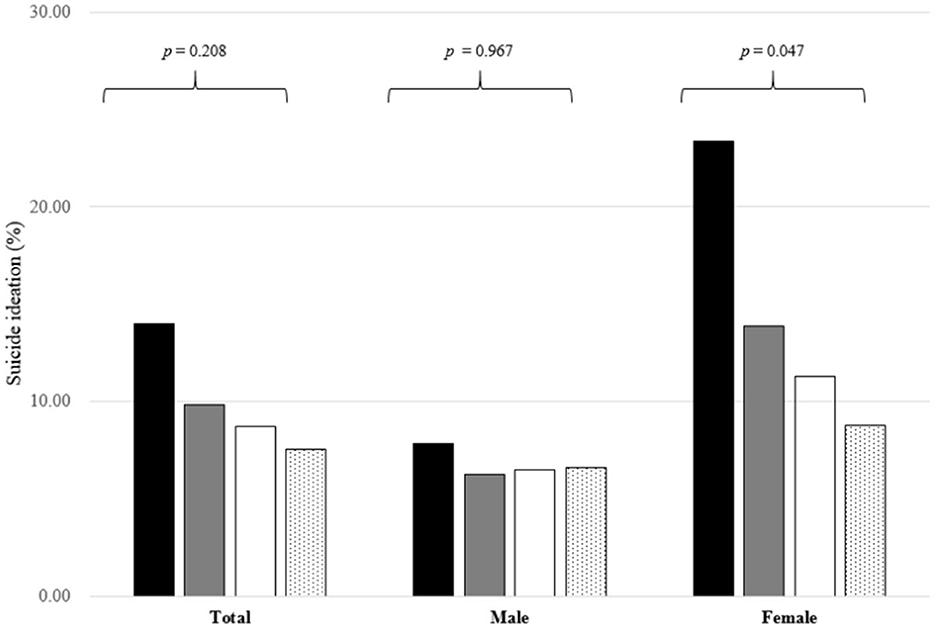
Figure 2. Proportions of individuals with suicide ideation according to height Z-score among the participants. The black bar represents individuals with a height Z-score below −2, the gray bar, with a height Z-score between −2 and 0, the white bar, with a height Z-score between 0 and 2, and the bar with the dotted pattern, with a height Z-score above 2. The number on the bar is the p-value of the analysis of variance.
3.4. Risk factors for suicide ideation in logistic regression analysis
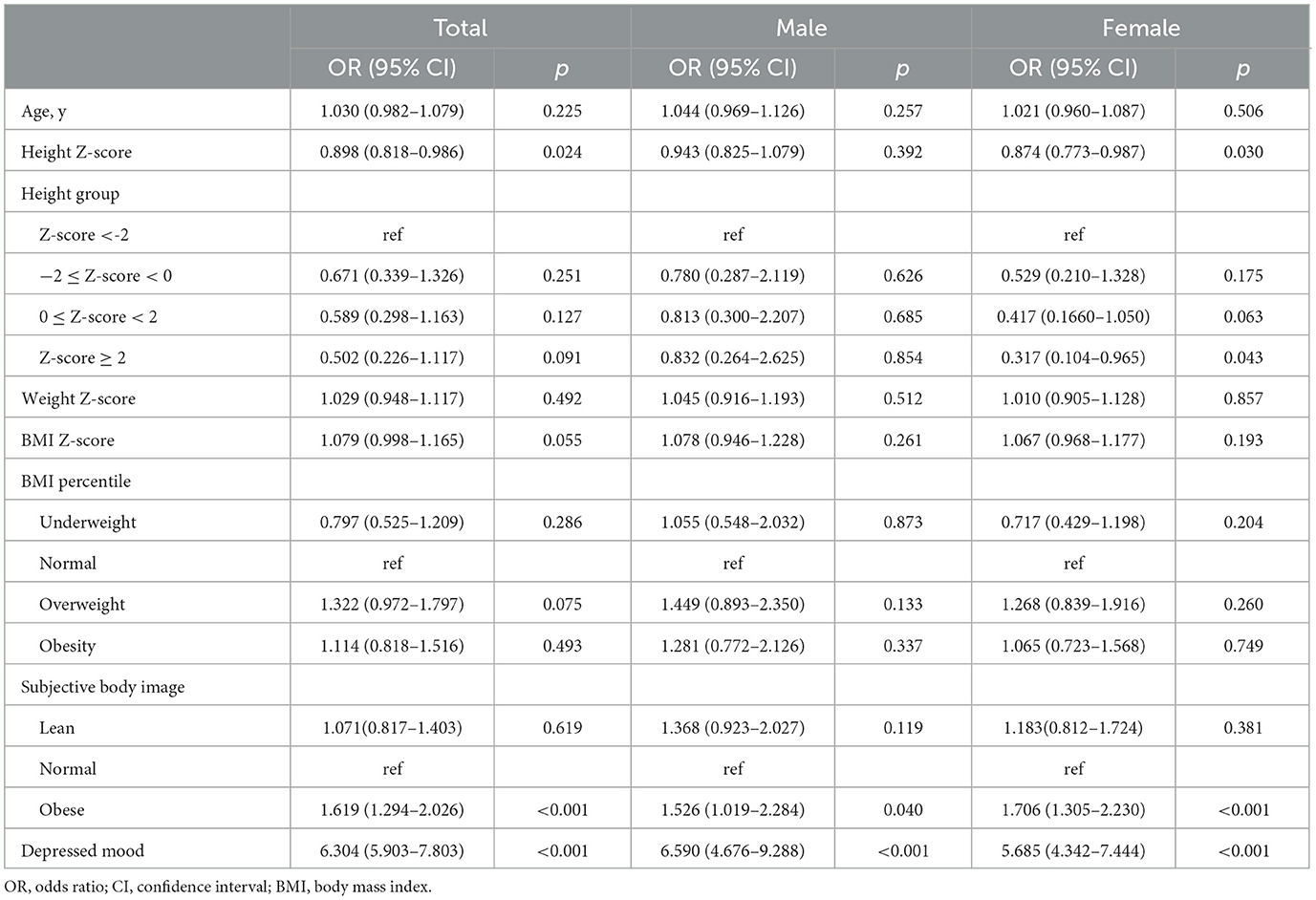
On logistic regression, the odds ratios (ORs) (95% confidence intervals [CIs]) of height Z-score, perceived obesity, and depressed mood in relation to suicide ideation were 0.898 (0.818–0.986), 6.304 (5.903–7.803), and 6.304 (5.903–7.803), respectively, among all participants (Table 4). Among male participants, the ORs (95% CIs) of perceived obesity and depressed mood in relation to suicide ideation were 1.526 (1.019–2.284) and 6.590 (4.676–7.803), respectively. Among female participants, the ORs (95% CIs) of height Z-score, perceived obesity, and depressed mood were 0.874 (0.773–0.987), 5.685 (4.342–7.444), and 5.685 (4.342–7.444), respectively. In addition, female participants with height Z-scores of above 2 were less likely to express suicide ideation than those with height Z-scores below −2 (OR = 0.317, 95% CI = 0.104–0.965).
After adjusting for age, height Z-score, and weight Z-score, the ORs (95% CIs) of perceived obesity for suicide ideation were 1.886 (1.699–2.528) for all participants, 1.277 (0.745–2.189) for male participants, and 2.080 (1.456–2.971) for female participants (p = 0.375 for male participants, all other p < 0.001) (Figure 3A). After adjusting age, height Z-score, weight Z-score, and depressed mood, the ORs (95% CIs) of perceived obesity for suicide ideation were 1.575 (1.175–2.111) for all participants, 1.168 (0.686–1.989) for male participants, and 1.706 (1.192–2.441) for female participants (p = 0.002 for the total number of participants, p = 0.568 for male participants, and p = 0.003 for female participants) (Figure 3B).
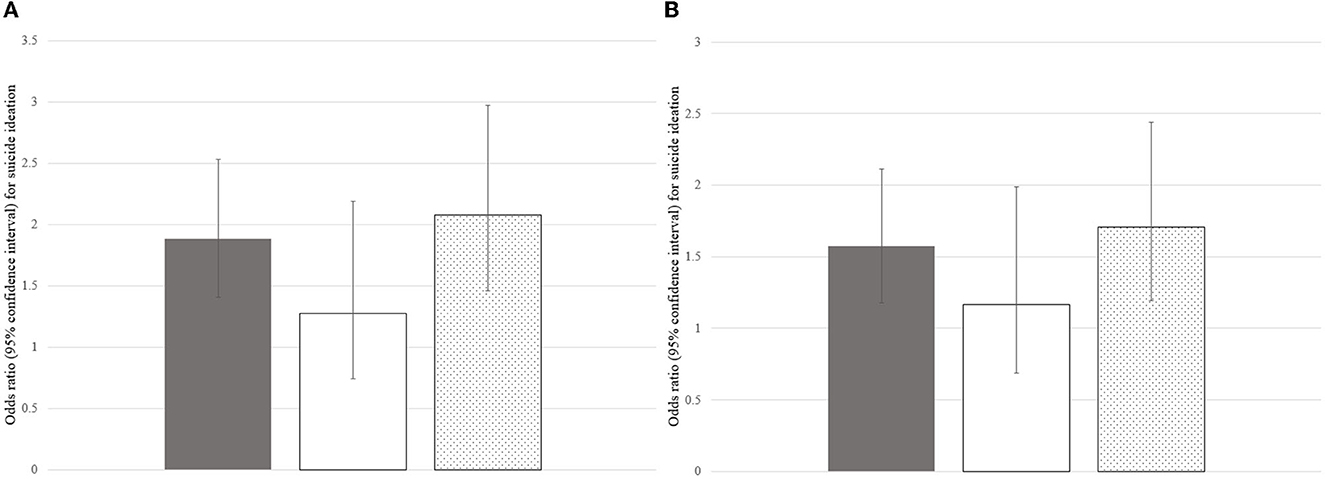
Figure 3. ORs (95% CIs) of perceived obesity for suicide ideation after adjusting for confounding factors. (A) ORs (95% CIs) of perceived obesity for suicide ideation after adjusting for age, height Z-score, and weight Z-score. (B) ORs (95% CIs) of perceived obesity for suicide ideation after adjusting for age, height Z-score, weight Z-score, and depressed mood. The gray, white, and dotted bars represent the ORs (95% CIs) of perceived obesity for suicide ideation among all participants, male participants, and female participants, respectively. OR, odds ratio; CI, confidence interval.
In the subgroup analysis, according to BMI, the ORs (95% CIs) of perceived obesity for suicide ideation were 1.889 (1.426–2.501) for the participants with normal BMI or underweight and 1.202 (0.551–2.622) for the participants who were overweight or obese (Figure 4).
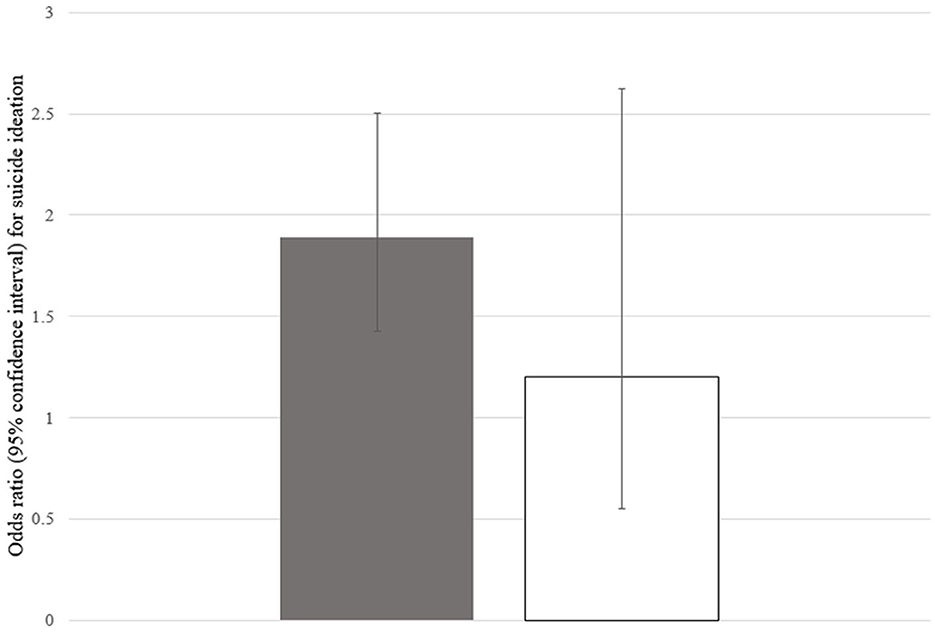
Figure 4. ORs (95% CIs) of perceived obesity for suicide ideation according to BMI. The gray bar represents ORs (95% CIs) of perceived obesity for suicide ideation among the participants with normal BMI or underweight and the white bar among the participants with overweight or obesity. OR, odds ratio; CI, confidence interval; BMI, body mass index.
In the subgroup analysis, according to the KNHANES phase, the OR (95% CI) of height Z-score for suicide ideation was 0.757 (0.582–0.985) for KNHANES VI (Supplementary Table 1). The ORs (95% CIs) of subjective body image for suicide ideation were significant for KNHANES IV, V, and VI, and the ORs (95% CIs) of depressed mood for suicide ideation were significant for KNHANES IV, V, VI, and VII. Interaction p-values were not significant for variables.
4. Discussion
This study demonstrated the following: (1) perceived obesity was positively associated with the proportion of suicide ideation in adolescents, even among those who fell within the normal BMI range or were underweight; (2) shorter height, even if not of short stature, was associated with suicide ideation in adolescents. These relationships were more prominent among girls than boys. Additionally, a substantial proportion of the participants perceived themselves as being obese even though they were not technically obese or overweight. The proportion of perceived obesity was higher among girls than boys, although the proportion of actual obesity was lower among girls.
In our study, suicide ideation was associated with perceived obesity rather than actual obesity or BMI Z-score, possibly because of weight stigma. Interestingly, research suggests that the perceptions of body weight in adolescents are more important than actual body weight (23, 34). In this study, perceived obesity was positively associated with suicide ideation after adjusting for age, height Z-score, body weight Z-score, and depressed mood. Importantly, weight stigma is not restricted only to obese adolescents. Indeed, Puhl et al. (35) reported that 19% of US adults of normal weight perceived themselves as being overweight. Cruz-Sáez et al. (36) reported that 12.3% of normal-weight women had extreme weight-control behaviors.
We noted that a relatively short height was negatively associated with suicide ideation among adolescents even though they were not particularly short. Considering previous reports suggesting that short stature has no relationship with psychosocial burden (37), we think it would be controversial to insist that short stature induces suicide ideation or vice versa. Nevertheless, short stature in childhood and adolescence can lead to life dissatisfaction and poor subjective health experiences (38). The association between short stature and suicide ideation may be more psychological in nature, such as due to negative self-image, than endocrinological.
As reflected in our results, the association between suicide ideation and perceived obesity or short stature seems to be related to negative body image, although the causality could not be explained. Negative body image should be considered both in psychological and environmental aspects. First, negative body image is related to a distorted perception of body image and is associated with low self-esteem, which can lead adolescents to have a negative self-image (23, 39). A negative self-image can be a predictor of not only psychological problems but also emotional distress (40, 41). Emotional distress is known to be linked to diverse negative cognitive patterns, such as selective processing of depressive information, making dysfunctional attributions, and engaging in negative automatic thinking (42). Moreover, adolescents, especially girls, with major depression tend to have a poorer self-image (43, 44). Considering that body image might be established in early adolescence, careful monitoring of emotional distress in children and adolescents is necessary to prevent negative outcomes as a result of negative body image (45, 46). Second, the influence of media tends to encourage a distorted body image since slim characteristics are often portrayed as being popular and attractive, whereas obese characteristics are depicted as being unpopular and in a negative light (24). In this regard, the association between negative body image and suicide ideation can be explained by the interpersonal theory of suicide, namely, perceived burdensomeness and thwarted belongingness are predictors of the desire to engage in suicide (47). Hunger et al. (25) reported that perceived burdensomeness can mediate weight stigma, and suicide ideation and negative weight stigma could be more powerful risk factors for suicide than BMI itself. Third, especially in adolescence, the association between weight stigma and psychological distress can be stronger, owing to teasing by peers (24, 48). Weight-based teasing is widespread and one of the risk factors for body dissatisfaction (48–50). A population-based study reported that weight-based harassment was associated with low self-esteem, depression, and body dissatisfaction among girls (51). A US study with a nationally representative survey reported that perceived obesity was positively related to suicide ideation, planning, and attempts among adolescents (48).
In our study, the proportion of participants exhibiting suicide ideation and depressed mood was higher among girls than boys; the relationship between perceived obesity and psychological stress was also more prominent among girls than boys. These findings may be attributed to gender differences in emotional expression and the fact that the burden of weight stigma is greater for female participants than for male participants with regard to attractiveness. A KNHANES-based study reported that women with an overweight body image had a higher level of depressive symptoms than those without; this finding was not observed in men (52). Carpenter et al. (20) reported that BMI was negatively related to suicide ideation and attempts in men, whereas it was positively related to both in women. A school based-study reported that obesity was related to psychological distress among girls but not among boys (53).
This study has some limitations. First, this was a cross-sectional study limited to South Korea, which limits the generalizability and causality of our results. In addition, the onset age of suicidal ideation and obesity was not specified in this study. Second, we could not consider confounding factors such as puberty, teasing, and sexual orientation because this information was not provided in the KNHANES. Third, environmental factors including familial factors were not considered in this study. Fourth, it was impossible to conduct structured interviews or use measurement instruments, as this study was based on a large-scale adolescent survey. Self-reported items cannot entirely represent an adolescent's mental health, and our study did not include every psychiatric disorder. To evaluate the effect of psychiatric disorders precisely, structured interviews such as the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders (DSM) should be considered (54). Psychometric instruments such as the Beck depression inventory for depression (55) and the Columbia-suicide severity rating scale for suicidal ideation could be useful for evaluating psychiatric disorders (56). Fifth, we considered only diabetes, congenital heart disease, and attention deficit hyperactivity disorder among chronic diseases associated with psychological distress. Sixth, we could not assess the effect of treatment for depression and suicide ideation because the KNAHNES provides information on medical treatment for psychiatric disease, although pharmacotherapy including antidepressants such as buprenorphine is the recommended treatment strategy for depression (57). However, the study assessed the association of suicide ideation with BMI, height, and subjective body image using nationally representative data from a large number of adolescents.
5. Conclusion
Our study demonstrated that perceived obesity was associated with suicide ideation among adolescents even though they were not really obese. In addition, a relatively short stature was associated with suicide ideation among adolescents even though they were not really short. These associations were more apparent among girls than boys. The findings emphasize a mutual relationship between psychological distress, negative body image, and height and subjective body image in adolescents. In addition, our results emphasize the importance of assessing the risk of suicide ideation in adolescents with perceived obesity and those with relatively short stature. Moreover, adolescents, especially girls, with psychological problems due to body image dissatisfaction, need attentive care from physicians and family members even though they may not be obese. Therefore, it is necessary to determine subjective feelings and psychological distress during the assessment of obesity and growth in adolescents to prevent suicide ideation.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Institutional Review Board of the Yonsei University Gangnam Severance Hospital. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author contributions
KS, JL, SL, and HC: conceptualization. KS, JL, and HC: design, methodology, and conducted the study. KS, JL, SJ, and HL: statistical analysis and interpretation. KS and JL: writing—original draft preparation. HC: writing—reviewing and editing. KS: resources. H-SK: supervision. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1172940/full#supplementary-material
References
1. Park S, Jang H. Correlations between suicide rates and the prevalence of suicide risk factors among Korean adolescents. Psychiatry Res. (2018) 261:143–7. doi: 10.1016/j.psychres.2017.12.055
3. Ministry Ministry of H, Welfare, Korea Foundation for Suicide P. 2022 White Paper on Suicide Prevention. Sejong: Ministry of Health and Welfare (2022).
4. Biswas T, Scott JG, Munir K, Renzaho AMN, Rawal LB, Baxter J, et al. Global variation in the prevalence of suicidal ideation, anxiety and their correlates among adolescents: a population based study of 82 countries. EClinicalMedicine. (2020) 24:100395. doi: 10.1016/j.eclinm.2020.100395
5. Shorey S, Ng ED, Wong CHJ. Global prevalence of depression and elevated depressive symptoms among adolescents: a systematic review and meta-analysis. Br J Clin Psychol. (2022) 61:287–305. doi: 10.1111/bjc.12333
6. Yun JY, Chung H, Sim JA, Yun YH. Prevalence and associated factors of depression among Korean adolescents. PLoS ONE. (2019) 14:e0223176. doi: 10.1371/journal.pone.0223176
7. Jeong SC, Kim JY, Choi MH, Lee JS, Lee JH, Kim CW, et al. Identification of influencing factors for suicidal ideation and suicide attempts among adolescents: 11-year national data analysis for 788,411 participants. Psychiatry Res. (2020) 291:113228. doi: 10.1016/j.psychres.2020.113228
8. O'Connor RC, Nock MK. The psychology of suicidal behaviour. Lancet Psychiatry. (2014) 1:73–85. doi: 10.1016/S2215-0366(14)70222-6
9. Song KC, Jin SL, Kwon AR, Chae HW, Ahn JM, Kim DH, et al. Etiologies and characteristics of children with chief complaint of short stature. Ann Pediatr Endocrinol Metab. (2015) 20:34–9. doi: 10.6065/apem.2015.20.1.34
10. Song YM, Smith GD, Sung J. Adult height and cause-specific mortality: a large prospective study of South Korean men. Am J Epidemiol. (2003) 158:479–85. doi: 10.1093/aje/kwg173
11. Jiang GX, Rasmussen F, Wasserman D. Short stature and poor psychological performance: risk factors for attempted suicide among Swedish male conscripts. Acta Psychiatr Scand. (1999) 100:433–40. doi: 10.1111/j.1600-0447.1999.tb10893.x
12. Wheeler PG, Bresnahan K, Shephard BA, Lau J, Balk EM. Short stature and functional impairment: a systematic review. Arch Pediatr Adolesc Med. (2004) 158:236–43. doi: 10.1001/archpedi.158.3.236
13. Sandberg DE, Bukowski WM, Fung CM, Noll RB. Height and social adjustment: are extremes a cause for concern and action? Pediatrics. (2004) 114:744–50. doi: 10.1542/peds.2003-1169-L
14. Lee JM, Appugliese D, Coleman SM, Kaciroti N, Corwyn RF, Bradley RH, et al. Short stature in a population-based cohort: social, emotional, and behavioral functioning. Pediatrics. (2009) 124:903–10. doi: 10.1542/peds.2008-0085
15. Voss LD. Short normal stature and psychosocial disadvantage: a critical review of the evidence. J Pediatr Endocrinol Metab. (2001) 14:701–11. doi: 10.1515/JPEM.2001.14.6.701
16. Serafini G, Parisi VM, Aguglia A, Amerio A, Sampogna G, Fiorillo A, et al. A specific inflammatory profile underlying suicide risk? Systematic review of the main literature findings. Int J Environ Res Public Health. (2020) 17:293. doi: 10.3390/ijerph17072393
17. Quek YH, Tam WWS, Zhang MWB, Ho RCM. Exploring the association between childhood and adolescent obesity and depression: a meta-analysis. Obes Rev. (2017) 18:742–54. doi: 10.1111/obr.12535
18. (NCD-RisC) NRFC. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. (2017) 390:2627–42. doi: 10.1016/S0140-6736(17)32129-3
19. Bjerkeset O, Romundstad P, Evans J, Gunnell D. Association of adult body mass index and height with anxiety, depression, and suicide in the general population: the HUNT study. Am J Epidemiol. (2008) 167:193–202. doi: 10.1093/aje/kwm280
20. Carpenter KM, Hasin DS, Allison DB, Faith MS. Relationships between obesity and DSM-IV major depressive disorder, suicide ideation, and suicide attempts: results from a general population study. Am J Public Health. (2000) 90:251–7. doi: 10.2105/AJPH.90.2.251
21. Zeller MH, Reiter-Purtill J, Jenkins TM, Ratcliff MB. Adolescent suicidal behavior across the excess weight status spectrum. Obesity. (2013) 21:1039–45. doi: 10.1002/oby.20084
22. Tomiyama AJ. Stress and Obesity. Annu Rev Psychol. (2019) 70:703–18. doi: 10.1146/annurev-psych-010418-102936
23. Alimoradi Z, Golboni F, Griffiths MD, Broström A, Lin CY, Pakpour AH. Weight-related stigma and psychological distress: a systematic review and meta-analysis. Clin Nutr. (2020) 39:2001–13. doi: 10.1016/j.clnu.2019.10.016
24. Pont SJ, Puhl R, Cook SR, Slusser W. Stigma experienced by children and adolescents with obesity. Pediatrics. (2017) 140:e20173034. doi: 10.1542/peds.2017-3034
25. Hunger JM, Dodd DR, Smith AR. Weight-based discrimination, interpersonal needs, and suicidal ideation. Stigma Health. (2020) 5:217. doi: 10.1037/sah0000188
26. Gavin AR, Simon GE, Ludman EJ. The association between obesity, depression, and educational attainment in women: the mediating role of body image dissatisfaction. J Psychosom Res. (2010) 69:573–81. doi: 10.1016/j.jpsychores.2010.05.001
27. Forrest KY, Stuhldreher WL. Patterns and correlates of body image dissatisfaction and distortion among college students. Am J Health Studies. (2007) 22:1.
28. Štefanová E, Bakalár P, Baška T. Eating-disordered behavior in adolescents: associations with body image, body composition and physical activity. Int J Environ Res Public Health. (2020) 17:18. doi: 10.3390/ijerph17186665
29. Calugi S, Dalle Grave R. Body image concern and treatment outcomes in adolescents with anorexia nervosa. Int J Eat Disord. (2019) 52:582–5. doi: 10.1002/eat.23031
30. Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, et al. Data resource profile: the korea national health and nutrition examination survey (KNHANES). Int J Epidemiol. (2014) 43:69–77. doi: 10.1093/ije/dyt228
31. Kim JH, Yun S, Hwang SS, Shim JO, Chae HW, Lee YJ, et al. The 2017 Korean national growth charts for children and adolescents: development, improvement, and prospects. Korean J Pediatr. (2018) 61:135–49. doi: 10.3345/kjp.2018.61.5.135
32. Gigantesco A, Morosini P. Development, reliability and factor analysis of a self-administered questionnaire which originates from the World Health Organization's Composite International Diagnostic Interview - Short Form (CIDI-SF) for assessing mental disorders. Clin Pract Epidemiol Ment Health. (2008) 4:8. doi: 10.1186/1745-0179-4-8
33. Gaynes BN, West SL, Ford CA, Frame P, Klein J. Lohr KN. Screening for suicide risk in adults: a summary of the evidence for the US Preventive Services Task Force Ann Intern Med. (2004) 140:822–35. doi: 10.7326/0003-4819-140-10-200405180-00015
34. Eaton DK, Lowry R, Brener ND, Galuska DA, Crosby AE. Associations of body mass index and perceived weight with suicide ideation and suicide attempts among US high school students. Arch Pediatr Adolesc Med. (2005) 159:513–9. doi: 10.1001/archpedi.159.6.513
35. Puhl RM, Himmelstein MS, Quinn DM. Internalizing Weight Stigma: Prevalence and Sociodemographic Considerations in US Adults. Obesity (Silver Spring). (2018) 26:167–75. doi: 10.1002/oby.22029
36. Cruz-Sáez S, Pascual A, Salaberria K, Echeburúa E. Normal-weight and overweight female adolescents with and without extreme weight-control behaviours: emotional distress and body image concerns. J Health Psychol. (2015) 20:730–40. doi: 10.1177/1359105315580214
37. Hwang JW, Seo JY. Parents' perception about child's height and psychopathology in community children with relatively short stature. Ann Pediatr Endocrinol Metab. (2015) 20:79–85. doi: 10.6065/apem.2015.20.2.79
38. Jafari-Adli S, Qorbani M, Heshmat R, Ranjbar SH, Taheri E, Motlagh ME, et al. Association of short stature with life satisfaction and self-rated health in children and adolescents: the CASPIAN-IV study. J Pediatr Endocrinol Metab. (2016) 29:1299–306. doi: 10.1515/jpem-2016-0215
39. KavehFarsani Z, Kelishadi R, Beshlideh K. Study of the effect of family communication and function, and satisfaction with body image, on psychological well-being of obese girls: the mediating role of self-esteem and depression. Child Adolesc Psychiatry Ment Health. (2020) 14:39. doi: 10.1186/s13034-020-00345-3
40. Beck AT. Cognitive models of depression. In:Leahy RL, Dowd ET, , editors. Clinical advances in cognitive psychotherapy: Theory and application. Cham: Springer (2002). p. 29–61.
41. Sperduti M, Martinelli P, Kalenzaga S, Devauchelle AD, Lion S, Malherbe C, et al. Don't be too strict with yourself! rigid negative self-representation in healthy subjects mimics the neurocognitive profile of depression for autobiographical memory. Front Behav Neurosci. (2013) 7:41. doi: 10.3389/fnbeh.2013.00041
42. Ingram RE, Kendall PC, Smith TW, Donnell C, Ronan K. Cognitive specificity in emotional distress. J Pers Soc Psychol. (1987) 53:734–42. doi: 10.1037/0022-3514.53.4.734
43. Chung W-S, Shin K-O, Bae JY. Gender differences in body image misperception according to body mass index, physical activity, and health concern among Korean university students. J Men's Health. (2019) 15:1–9. doi: 10.22374/1875-6859.15.1.1
44. Hards E, Ellis J, Fisk J, Reynolds S. Negative view of the self and symptoms of depression in adolescents. J Affect Disord. (2020) 262:143–8. doi: 10.1016/j.jad.2019.11.012
45. Voelker DK, Reel JJ, Greenleaf C. Weight status and body image perceptions in adolescents: current perspectives. Adolesc Health Med Ther. (2015) 6:149–58. doi: 10.2147/AHMT.S68344
46. Smolak L. Body image in children and adolescents: where do we go from here? Body Image. (2004) 1:15–28. doi: 10.1016/S1740-1445(03)00008-1
47. Brochu PM. Weight stigma as a risk factor for suicidality. Int J Obes. (2020) 44:1979–80. doi: 10.1038/s41366-020-0632-5
48. Daly M, Robinson E, Sutin AR. Perceived overweight and suicidality among US adolescents from 1999 to 2017. Int J Obes. (2020) 44:2075–9. doi: 10.1038/s41366-020-0620-9
49. Gonzaga I, Claumann GS, Scarabelot KS, Silva DAS, Pelegrini A. Body image dissatisfaction in adolescents: Comparison with physical activity, teasing and social support. J Health Psychol. (2021) 26:1651–60. doi: 10.1177/1359105319887796
50. Eisenberg ME, Neumark-Sztainer D, Story M. Associations of weight-based teasing and emotional well-being among adolescents. Arch Pediatr Adolesc Med. (2003) 157:733–8. doi: 10.1001/archpedi.157.8.733
51. Bucchianeri MM, Eisenberg ME, Wall MM, Piran N, Neumark-Sztainer D. Multiple types of harassment: associations with emotional well-being and unhealthy behaviors in adolescents. J Adolesc Health. (2014) 54:724–9. doi: 10.1016/j.jadohealth.2013.10.205
52. Kim Y, Austin SB, Subramanian SV, Kawachi I. Body weight perception, disordered weight control behaviors, and depressive symptoms among korean adults: the korea national health and nutrition examination survey 2014. PLoS One. (2018) 13:e0198841. doi: 10.1371/journal.pone.0198841
53. Gall K, van Zutven K, Lindstrom J, Bentley C, Gratwick-Sarll K, Harrison C, et al. Obesity and emotional well-being in adolescents: Roles of body dissatisfaction, loss of control eating, and self-rated health. Obesity. (2016) 24:837–42. doi: 10.1002/oby.21428
54. First MB. Structured clinical interview for the DSM (SCID). The Encycl Clin Psychol. (2014) 8:1–6. doi: 10.1002/9781118625392.wbecp351
55. Beck AT, Steer RA, Brown GK. Beck Depression Inventory: Harcourt Brace Jovanovich. New York, NY: Elseiver (1987).
56. Posner K, Brent D, Lucas C, Gould M, Stanley B, Brown G, et al. Columbia-Suicide Severity Rating Scale (C-SSRS). New York, NY: Columbia University Medical Center. (2008)
Keywords: height, body image (MeSH), suicide, obesity, adolescent
Citation: Song K, Lee J, Lee S, Jeon S, Lee HS, Kim H-S and Chae HW (2023) Height and subjective body image are associated with suicide ideation among Korean adolescents. Front. Psychiatry 14:1172940. doi: 10.3389/fpsyt.2023.1172940
Received: 24 February 2023; Accepted: 15 May 2023;
Published: 12 June 2023.
Edited by:
David Cohen, Sorbonne Universités, FranceReviewed by:
Paolo Meneguzzo, University of Padua, ItalyCihad Dundar, Ondokuz Mayıs University, Türkiye
Gianluca Serafini, San Martino Hospital (IRCCS), Italy
Copyright © 2023 Song, Lee, Lee, Jeon, Lee, Kim and Chae. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hyun Wook Chae, aG9wZWNoYWVAeXVocy5hYw==
†These authors have contributed equally to this work and share first authorship
 Kyungchul Song
Kyungchul Song Junghan Lee
Junghan Lee San Lee
San Lee Soyoung Jeon
Soyoung Jeon Hye Sun Lee
Hye Sun Lee Ho-Seong Kim
Ho-Seong Kim Hyun Wook Chae
Hyun Wook Chae