
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CLINICAL TRIAL article
Front. Psychiatry, 23 June 2023
Sec. Social Psychiatry and Psychiatric Rehabilitation
Volume 14 - 2023 | https://doi.org/10.3389/fpsyt.2023.1171661
This article is part of the Research TopicSupporting Family Members with Mental Illness: Impact on CaregiversView all 8 articles
Introduction: Schizophrenia is recognized for its severe impact on both patients and caregivers. In a 12-month follow-up randomized clinical trial, we aimed to measure the efficacy of a brief family psychoeducation program in terms of reducing relapse risk and improving medication adherence in patients, as well as reducing caregiver burden, depression and increasing knowledge of the illness.
Methods: A total of 25 days of patients with schizophrenia (DSM-IV-TR) and family primary caregivers were recruited in a single regional psychiatric outpatient facility located in Bordeaux. In the active group, caregivers received a psychoeducational intervention consisting of six sessions spread over 1.5 months, while the control group was placed on a waiting list. Sociodemographic, symptom severity (PANSS) and medication adherence (MARS) from patients were assessed at baseline and relapse rates was recorded during the 12 months follow-up period. Caregivers’ burden (ZBI), depression (CES-D), quality of life (S-CGQoL), knowledge of the disease (KAST) and therapeutic alliance (4PAS-C) were assessed at baseline, three and 6 months.
Results: On the 25 patients included, the mean age was 33.3 years (SD = 9.7) with a mean duration of disease of 7.48 years (SD = 7.1). On the 25 caregivers included, the mean age was 50.6 years (SD = 14.0). Twenty-one were female (84.0%), 12 were married (48.0%) and 11 lived alone (44.0%). For patients, the family psychoeducation intervention significantly reduced the risk of relapse with a significant effect found at 12 months follow-up (p = 0.014). No change was observed on medication adherence. For caregivers, the intervention reduced the burden (p = 0.031), decreased the depression (p = 0.019), and increased the knowledge on schizophrenia (p = 0.024). Analyzes for repeated measures showed a statistically significant difference in therapeutic alliance (p = 0.035).
Conclusion: As confirmed by previous studies, the brief multifamily program (consisting of six sessions over a period of 1.5 months) was found to be effective in improving outcomes for caregivers (e.g., burden, depression, knowledge) and patients (e.g., preventing relapse) in the context of routine care. Given its short duration, this program is expected to be easily implementable within the community.
Clinical trial registration: https://clinicaltrials.gov/, NCT03000985.
Schizophrenia is a chronic and severe mental disorder which has serious consequences for both the patient and caregivers. The burden of schizophrenia on caregivers had been demonstrated (1–4) and justify that family have to be included in the care plan with adequate information and support (5). Therefore, family intervention should be developed to reduce the burden of caregivers and enhance patients’ prognosis. For patients, family psychoeducation has been effective in improving outcomes in schizophrenia with a better level of global functioning, medication adherence, and a reduction in the use of healthcare resources and the frequency of relapse (6–8). A recent systematic review including 11 studies demonstrates consistent improvement in many outcome measures of patients, such as relapse rates and medication adherence, but heterogeneity in symptoms reliefs (9). Its effectiveness has also been demonstrated for individuals at clinical high risk for psychosis although rigorous further studies are required (10). Through psychoeducation, a better understanding of the illness was associated with a better insight and medication adherence (11). For caregivers, increased knowledge of the disease reduces aspects related to stigma, stress and burden which contributes to a supportive social environment to increase the patient’s awareness of the disease and adapted care (12, 13).
It has been demonstrated that family psychoeducation is effective and is considered part of the guideline recommendations in the treatment of schizophrenia (5, 14, 15). A Cochrane review confirmed a 20% reduction in relapse rates compared with usual care (7). Caregivers’ outcomes from family psychoeducation are less commonly studied. The only meta-analysis of family outcomes found considerable positive effects on relatives’ burden and psychological distress, the relationship between relatives and the patient, and family functioning (16). A review of family psychoeducation programs suggested that it was more likely to be effective in families if knowledge of the disease and other outcomes such as burden, family functioning, emotional response etc. were systematically assessed to reflect the specific goals of the intervention (8). Despite recommendations and significant results, family psychoeducation is not a widely accessible option in mental health services, often due to limitations including a lack of interest from families, limited availability of care staff, or a shortage of trained professionals in these programs (5, 17, 18). A review of more than 30 randomized clinical trials (RCTs) pointed out that application of family psychoeducation in routine settings remains limited, reflecting attitudinal, knowledge, practice and systemic barriers to implementation (19).
The objective of this study was to compare the efficacy of a new brief family psychoeducation program (consisting of 6 sessions over 1.5 months) to treatment as usual (TAU) in a single center randomized clinical trial. Our aim was to measure the impact of the intervention on both caregivers and patients over a 12-month follow-up period, in comparison to usual care. We hypothesized that the psychoeducation program would reduce the risk of relapse and improve medication adherence in patients with schizophrenia, while also enhancing the quality of life, reducing caregiver burden, improving the therapeutic alliance, increasing knowledge of the illness, and reducing depression in caregivers.
This randomized single-blind controlled trial adopted a two arms parallel groups design. The controlled trial was conducted at a single regional psychiatric outpatient facility located in Bordeaux, France, registered in ClinicalTrials.gov (Ref.: NCT03000985). A total of 25 dyads of patients and family primary caregivers were recruited between December 2014 and December 2019. The inclusion criteria for patients were (i) a diagnosis of schizophrenia or schizoaffective disorder according to DSM-IV-TR criteria (20), (ii) age of at least 18 years, and (iii) being in a stable phase and receiving outpatients’ routine care. Exclusion criteria consisted of a history of traumatic head injury, any current or past major medical or neurological illness, and mental retardation. The inclusion criteria for caregivers were males or females aged 18 years or older who were currently caring for a relative diagnosed with schizophrenia or schizoaffective disorder and receiving appropriate outpatient clinical care. Caregivers who had previously received a standardized psychoeducational intervention or had intellectual disability, dementia or any other psychiatric condition were excluded from the study. Participants were assigned to one of the two study groups through a computer-generated random process. On the 25 caregivers 11 were the mother, 7 the father, 2 the sister, 1 the brother, 1 spouse/husband, 1 the aunt and finally 2 were the child of patient. In the active group, caregivers received a psychoeducational intervention consisting of six sessions spread over 1.5 months, while the control group, which received treatment as usual (TAU), was placed on a waiting list without any additional strategies. All participants including patients and caregivers signed an informed consent form prior to randomization and trial inclusion. The study protocol involving human participant was reviewed and approved by the local human subject research ethics committee.
The Schiz’Aides program is a multifamily psychoeducational program, which was built for caregivers of patients with schizophrenia, consisting of six sessions over a 1.5 months period. Each session lasted an average of 1 h and 30 min and was delivered in a group format led by a nurse and a psychologist who were trained to provide psychoeducation. One specific session of the program included the participation of a psychiatrist and a social worker. The program follows international guidelines concerning these interventions (5). The first session focuses on the presentation of each family and the experience of their relative’s illness. It also provides an opportunity to gather families’ expectations and to present the program’s themes. The second session is dedicated in understanding the disease. The objective is to give caregivers the criteria to identify symptoms, as well as etiological factors (multifactorial hypothesis). The third session focuses on drug treatments (role, forms, efficacy, side effects), non-drug treatments (mainly psychotherapies such as cognitive remediation) and finally forms/modes of hospitalization. The fourth session allows the caregiver to better manage their patients’ crisis states. The objective is to identify the warning signs and the adaptive reaction to adopt. The sharing of experiences between the different families is strongly encouraged. The fifth session focuses on the patient’s daily life, i.e., the psychosocial and cognitive consequences, as well as negative symptoms hindering a good rehabilitation. Solutions for care, networks and associations are presented. The sixth session focuses on the caregivers’ experiences: the weight of the disease, verbalization of feelings. Afterward, a review of the program is made and answers to the last questions are given. A booster session is conducted six months after the initial phase. This session allows to improve the program’s efficacy and to monitor the implementation of daily effective strategies. The Schiz’Aides program has a complete manual with a session guide, which can be provided upon request.
Patients were assessed once at inclusion. Sociodemographic information (gender, age, marital status, level of education, living situation) and illness history (duration of illness, lifetime suicide attempt, history of treatments, BMI) were collected. Symptom severity was assessed using the Positive And Negative Syndrome Scale (PANSS) (21) and medication adherence was evaluated with the Medication Adherence Rating Scale (MARS) (Kuder–Richardson-20: 0.60) (22). With the agreement of the authors (23), our team translated the scale into French, then validated it by reverse translation into English with the author. The scale was then used and validated in a large national cohort of 319 patients suffering from schizophrenia (24, 25). Relapses, defined as new psychiatric hospitalization, were recorded by reviewing the computerized medical records at 3, 6, and 12 months from baseline.
Caregivers were assessed at baseline, and at 3 and 6 months after the completion of the psychoeducational program. Self-administered questionnaires were used to assess the different dimensions: the knowledge of the disease using the Knowledge About Schizophrenia Test (KAST). The KAST is an 18-item multiple-choice questionnaire (e.g., “Medicines that are used for hearing voices are called …”; “A person strongly believes that the FBI has put a computer chip in his/her body. This symptom is called a …”) with five response options and the score ranges from 0 to a maximum possible score of 21 (indicating good knowledge) (Kuder–Richardson-20: 0.82) (26); the Quality of Life with Schizophrenia-Caregiver Quality of Life questionnaire (S-CGQoL) contains 25 items scored with a six-point Likert scale and describing seven dimensions, with 100 indicating the best possible level of QoL and 0 the worst (27); the burden of disease was assessed with the Zarit Burden Interview (ZBI). The ZBI includes 22 statements (e.g., “Do you feel that because of the time you spend with your relative that you do not have enough time for yourself?”; “Do you feel your health has suffered because of your involvement with your relative?”) recorded in a 0–4 Likert scale (total score range 0 to 88), that rates the subjective component of burden (Cronbach’s alpha: 0.92) (28); the Center for Epidemiologic Studies – Depression Scale (CES-D) is a 20-item questionnaire that measures depressive symptoms and related behaviors experienced over the past week, with each item rated on a 0–3 Likert scale. Possible scores range from 0 to 60, with higher scores indicating more severe depressive symptoms. A cutoff score of 16 or greater is indicative of individuals at risk for clinical depression (Cronbach’s alpha: 0.90) (29); the 4-Point ordinal Alliance Scale – Caregiver (4PAS-C) is an 11-item questionnaire (e.g., “I believe my doctor is helping us”; “I have a better understanding of the symptoms of my relative’s illness.”) scored using a Likert-type format. Responses range from 1 (“strongly disagree”) to 4 (“strongly agree”) and scores range from 11 to 44, with higher scores indicating of a more positive alliance (Cronbach’s alpha: 0.91). The questionnaire yields two subscores (Empathy and Psychoeducation) and a Visual Analog Scale score (0 to 100) (30); the Compliance Rating Scale (CRS), a seven-point rating scale, score ranging from 1 (complete refusal) to 7 (active participation) (31).
Analyzes were conducted based on the “intention-to-treat” principle; patients and caregivers were analyzed according to the randomization group they were allocated to and regardless of the intervention they followed. Baseline characteristics of patients and caregivers were compared between intervention and control groups using appropriate tests. They were no dropout at follow-up visits. When normality assumption was not rejected, an independent t-test was used for continuous variables. Otherwise, the Mann–Whitney U test was performed. Categorical data were compared using a chi-squared test or a Fisher’s exact test if necessary. Longitudinal repeated measures (baseline, 3 and 6 months) of caregivers’ scales were analyzed in each randomized group using whether repeated measures ANOVA (for normal distributed data) or Friedman test (for non-normal distributed data), followed by a post-hoc analysis using the Wilcoxon signed-rank test with Benjamini-Hochberg correction.
All p values were two-sided, and the level of statistical significance was set to 5%. Statistical analyzes were performed with IBM SPSS statistics, version 26.0. Complete test statistics are displayed in the respective tables and Supplementary data.
On the 25 patients included, the mean age was 33.3 years (SD = 9.7). They were 6 females (24.0%) with a mean duration of disease of 7.48 years (SD = 7.1). The majority were single (n = 24, 96%), lived alone (n = 15, 60%) and were unemployed (n = 22, 88%). Regarding the clinical variables, patients had a mean duration of illness of 7.5 years (SD = 7.1), a mean number of antipsychotics of 1.20 (SD = 0.5) and a mean antipsychotic dose of 4.55 mg (SD = 4.2) chlorpromazine equivalent. All patients were treated with a second-generation antipsychotic. The mean total PANSS score was 70.76 (SD = 11.8) and the mean score on the MARS scale was 6.52 (SD = 1.9) (moderate compliance). At baseline the two study groups were significant different on PANSS scores, antipsychotic dose, and BMI. The sociodemographic and clinical characteristics of the sample are presented in Table 1.
On the 25 caregivers included, the mean age was 50.6 years (SD = 14.0). Twenty-one were female (84.0%), 12 were married (48.0%) and 11 lived alone (44.0%). Twenty-two had a level of education higher than the high school (88%). The mean quality of life was 70.80 (SD = 16.5). Burden was scored as medium with a mean of 37.75 (SD = 7.9). Knowledge of the disease was rated as “moderate” with a mean score of 13.1 (SD = 2.3) and therapeutic alliance was rated as “good” with a mean sore of 30.94 (SD = 7.4). Depression was rated as “moderate” with a mean score on CES-D of 20.37 (SD = 11.4). No significant difference was found between groups for sociodemographic and psychometrics scores of caregivers at baseline. A positive significant association was found, between the burden (ZBI) and the level of depression (CES-D) [β = 0.78, CI = (0.06, 1.50), p = 0.036].
A lower rate of relapse was observed at 3, 6 and 12 months for patients whose caregivers participated in the intervention group. The difference was significant at 12 months (p = 0.014). Medication adherence assessed by CRS estimated by caregivers was not modified by the intervention (see details in Table 2).
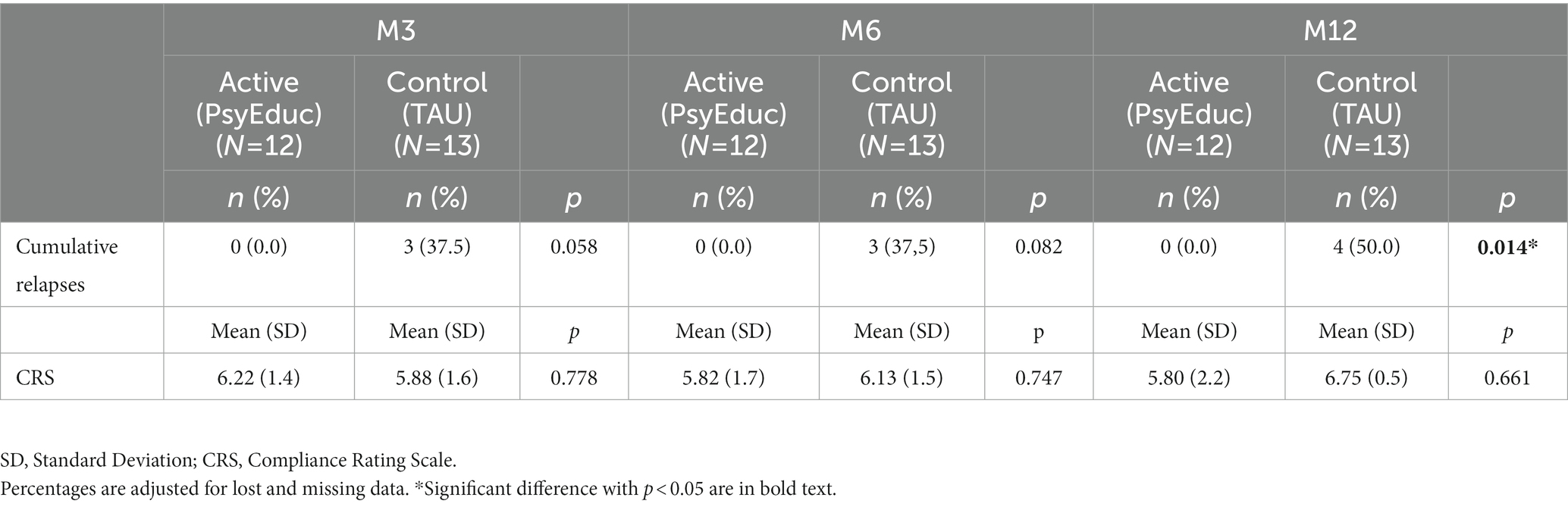
Table 2. Comparison of patients’ outcomes (cumulative relapse (re-hospitalization) rates and perceived medication adherence) following time.
The results indicated a significant difference in the total score of the KAST at 1.5 months (p = 0.024). Caregivers who received psychoeducation had higher scores (mean: 15.45; SD: 1.4) than caregivers in the control group (mean: 12.38; SD: 3.4). This difference was not observed at 6 months (p = 0.098). Two significant results were found at 6 months: first, the ZBI score (burden) (p = 0.031), showed a significant reduction for caregivers in the active group (mean: 20.17; SD: 8.0) compared to the control group (mean: 35.60; SD: 12.1); secondly, the CES-D score (depression) showed a significant reduction (p = 0.019), for caregivers in the active group (mean: 6.20; SD: 4.9) compared to the control group (mean: 14.20; SD: 3.6). No significant differences were found for quality of life and therapeutic alliance, regardless of the visit. Additional details are provided in Table 3.
Analyzes for repeated measures showed a statistically significant difference in therapeutic alliance (4PAS-C total score) (p = 0.035) and two sub-scores: Visual Analogic Scale (p = 0.015), and Psychoeducation (p = 0.036). There was also a significant improvement in the burden, as evaluated by ZBI (p = 0.040; see Table 4 for details). Post hoc analysis did not yield any significant results, despite an overall perceived improvement of therapeutic alliance between caregiver and the healthcare team and a reduction in the burden (Supplementary data).
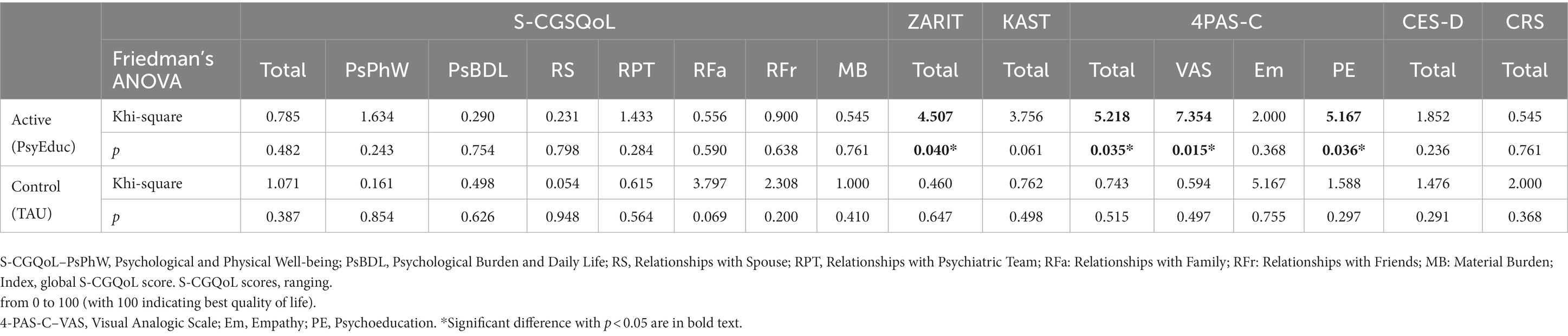
Table 4. Evolutions in psychometric scales’ scores by group: Friedman’s ANOVA for repeated measures.
The efficacy of a family psychoeducational program was assessed through a randomized clinical trial (RCT) on a community dwelling patient with schizophrenia and their caregivers. Principal findings should be summarized as follows: (i) For patients, the family psychoeducation intervention reduced the risk of relapse with a significant effect found at 12 months follow-up. However, no change was observed on medication adherence; (ii) For caregivers, the intervention reduced the burden, decreased the depression, increased the knowledge on schizophrenia, and strengthened the therapeutic alliance.
The efficacy of family psychoeducation in patient with schizophrenia has been well established in previous studies (9, 19). A review of the literature showed that family intervention can improve relapse and hospital admission rates in early psychosis (32). Additionally, studies conducted in chronic schizophrenia found that family psychoeducation can reduce the risk of relapse (25, 26, 33, 34). These interventions have also been shown to be cost saving and are included in international treatment guidelines (14, 15). These findings highlight the importance of incorporating family psychoeducation as a part of the comprehensive treatment plan for patients with schizophrenia.
Despite expectations, we did not show any impact of the family psychoeducation on medication adherence. This result is consistent with a previous study where carers’ knowledge about schizophrenia appeared to be not related to compliance (35). Medication adherence which is recognized as complex and multi-determined phenomenon cannot be resolved by a single, non-specific intervention. Moreover, the caregiver’s judgment of their relative’s medication intake may be influenced by factors such as the amount of time spent together and the patient’s regimen (oral or injectable antipsychotic). This presents a limitation for the interpretation of scores on the CRS and highlights the need for a combination of objective measures (e.g., pill counts, serum levels) and validated self-report scales to accurately assess medication adherence (25, 36). Nevertheless, the level of caregiver burden may also have an impact on medication adherence, as demonstrated by recent studies, which underscore the importance of supportive programs for caregivers (9, 37).
In caregivers we found at baseline a significant association between the level of depression and the burden estimated with the Zarit Burden Interview. This association is confirmed by the study from Mittendorfer-Rutz (4) in a nationwide comparative study of parents of offspring with schizophrenia, rheumatoid arthritis, multiple sclerosis, epilepsy, and healthy controls. The results of this study showed that the parents of a patient with schizophrenia were at a higher risk for burden and had a 2.7 times higher risk of needing specialized psychiatric health care. We found a significant effect in caregiver’s burden at 6 months follow-up, suggesting a temporal learning effect with a gradual reduction in burden over time attributed to the family psychoeducation program. The impact of schizophrenia on caregivers can result in a significant burden including emotional, psychological, physical and financial strain associated with feelings of shame, embarrassment, guilt and blame (16, 37). Reducing caregiver burden is crucial for patient management, and for the caregiver himself, as it can help to reduce depression, burden-related care and associated costs (38).
At baseline, the level of depression is evaluated as “moderate” in both groups, with a score above the threshold fixed at 16 on CES-D scale. Previous studies had shown that caregivers of patients with schizophrenia are at higher risk for developing depression (4, 38). In a large survey, Gupta et al. found a 10% increased of depression in caregivers of patients with schizophrenia compared to non-caregivers and caregivers of adults with other conditions (38). At 6 months, in comparison with TAU, the intervention was found to significantly reduce depression. Depressive symptoms can have a negative impact on family interactions and lead to maladaptive behaviors toward the patient. Our findings is consistent with a previous RCT showed the usefulness of a family intervention in reducing caregiver’s depressive symptoms as measured by the CES-D, and a moderate effect in reducing the subjective burden as assessed by the ZBI over an 8 months follow-up period (2).
The purpose of family psychoeducation is to increase caregiver’s knowledge and understanding of illness and treatment. A significant improvement in the knowledge of the disease (KAST) was found in caregivers in the intervention group. This demonstrates the relevance of the information delivered during psychoeducation and its directly measurable effect (33). However, at 6 months, the difference between the two groups was no longer significant. There was a spontaneous improvement in the score in the control group, which may be related to the caregivers’ self-training by different resources (books, internet, meeting with the treating psychiatrist...). Knowledge of the disease have been found to be associated with a better medication adherence in patients (11). The Cochrane review highlights the benefits of patient psychoeducation in reducing relapse and readmission rates, promoting medication adherence, and shortening hospital stays. These findings suggest that psychoeducation not only has a positive impact on patients, but also on their family caregivers, making it a clinically effective and cost-beneficial intervention (39). The central role of family support in care was recently coroborated in an Italian multicenter study of 136 caregivers, where caregivers’ personal growth was associated with good family functioning and adequate professional support (40). Another study focused on the functioning pointed out that interpersonal relationships and work skills are the impaired functional areas in both patients and caregivers (41).
Therapeutic alliance has been found to be enhanced by the family psychoeducation intervention. To our best knowledge, the therapeutic alliance between caregivers and healthcare staff has never been investigated in cohorts of patients with schizophrenia. Interactions with the health care staff during the family psychoeducation group strengthened the relationship and understanding with the caregiver. This was explored in other pathologies such as cancer (42).
In contrast to the study by Savanaud et al., we did not find any impact of the intervention on quality of life (38, 43). Quality of life may be influenced by the heterogeneous relational degree of the caregiver (parents, partner, child…). Indeed, it has been shown that parents of a patient have a lower quality of life than the patient’s siblings as demonstrated in a recent Croatian study (44). Although 72% of the included caregivers in our sample were the ill loved one, no significant results emerged regarding their quality of life. Most studies with similar design have focused on the patient’s quality of life rather than the caregiver’s (45, 46). We found one recent Indian RCT, that showed a significant improvement in overall quality of life scores in the experimental group caregivers compared to control group at the end of the program, after 6 months (47).
Thus, our study provides evidence of the efficacy of a short multifamily program (six sessions over 1.5 months) for caregivers (depression, knowledge) and patients (preventing relapse) in the context of routine care. This program can be repeated multiple times during the year. Previous RCTs and Evidence-Based Medicine (EBM) have considered the same primary evidence (9); however, the implementation of this evidence in routine care is limited (19). Moreover, To the best of our knowledge, and within the context of French mental health, psychoeducational programs for patients have been more extensively developed than those for caregivers. The brevity of this program should facilitate its implementation in the community.
Although our study has several strengths, there are some limitations that must be acknowledged. Our limited sample size could limit the reliability of our results. Additionally, the single-center design of our study may introduce a selection bias, which may affect the representativeness of our sample. To fully understand the effects of the intervention and to confirm our encouraging results, a larger, multi-center study should be done. However, in the context of the French mental health psychiatric service, the regional psychiatric outpatient facility should be considering as a good representation of the population of a community dwelling patient suffering of schizophrenia. Although patients were considered to be in a stable phase with only minor modifications to their prescribed medication during follow-up, this issue was not controlled and should be considered as a limitation in assessing the effectiveness of the psychoeducational program in preventing relapse.
In conclusion, as confirmed by previous studies, the brief multifamily program (consisting of six sessions over a period of 1.5 months) was found to be effective in improving outcomes for caregivers (e.g., burden, depression, knowledge) and patients (e.g., preventing relapse) in the context of routine care. Given its short duration, this program is expected to be easily implementable within the community.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Committee for the Protection of Persons–South West and Overseas 3 (CPP-SOOM3) Study folder: 2014/58. Department of Clinical Pharmacology, Bordeaux Hospital, Place Amélie Raba Léon 33076 BORDEAUX Cedex FRANCE Tel: +33 (0)5 57 81 76 07 Email: Y3BwLnNvb20zQHUtYm9yZGVhdXguZnI= Web: http://www.cpp-soom3.u-bordeaux2.fr/. The patients/participants provided their written informed consent to participate in this study.
KR and DM were involved in generating hypotheses, the management of the study and the development of the psychoeducational program. KR, AG, and DM were involved in the conduction of the psychoeducational program (Schiz’Aides). AT and PD conducted statistical analyzes. AT, PD, and DM wrote the first complete manuscript. All authors were involved in the patients’ recruitment, the clinical evaluation, acquisition of the clinical data, modified the manuscript and approved the final version.
This work was supported by a grant from the Nurses and Paramedics Research Hospital Program from the French Ministry of Health (PHRIP “2013–0017–PsyEduc”). The funding source had no role in the conduct or publication of the study.
The authors thank the team of the CMP de Talence (Pôle PGU of the CH Charles Perrens) in the elaboration and the conduction of the program, particularly: the psychiatrist M. Lescarret, J. Libert, and M-C Levassor; the nurses I. Tanguy, M-L Bamas, and F. Campedel; the psychologists A. Rebollo and H. Tastet; the social worker A. Bonnat.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1171661/full#supplementary-material
1. Addington, J, McCleery, A, and Addington, D. Three-year outcome of family work in an early psychosis program. Schizophr Res. (2005) 79:107–16. doi: 10.1016/j.schres.2005.03.019
2. Martín-Carrasco, M, Fernández-Catalina, P, Domínguez-Panchón, AI, Gonçalves-Pereira, M, González-Fraile, E, Muñoz-Hermoso, P, et al. A randomized trial to assess the efficacy of a psychoeducational intervention on caregiver burden in schizophrenia. Eur Psychiatry. (2016) 33:9–17. doi: 10.1016/j.eurpsy.2016.01.003
3. Sari, A, and Duman, ZÇ. Effects of the family support and psychoeducation program based on the Calgary family intervention model on the coping, psychological distress and psychological resilience levels of the family caregivers of chronic psychiatric patients. Arch Psychiatr Nurs. (2022) 41:1–10. doi: 10.1016/j.apnu.2022.07.014
4. Mittendorfer-Rutz, E, Rahman, S, Tanskanen, A, Majak, M, Mehtälä, J, Hoti, F, et al. Burden for parents of patients with schizophrenia-a Nationwide comparative study of parents of offspring with rheumatoid arthritis, multiple sclerosis, epilepsy, and healthy controls. Schizophr Bull. (2019) 45:794–803. doi: 10.1093/schbul/sby130
5. Harvey, C. Family psychoeducation for people living with schizophrenia and their families. BJPsych Advances. (2018) 24:9–19. doi: 10.1192/bja.2017.4
6. Zhang, M, Wang, M, Li, J, and Phillips, MR. Randomised-control trial of family intervention for 78 first-episode male schizophrenic patients. An 18-month study in Suzhou, Jiangsu. Br J Psychiatry Suppl. (1994) 24:96–102.
7. Pharoah, F, Mari, J, Rathbone, J, and Wong, W. Family intervention for schizophrenia. Cochrane Database Syst Rev. (2006) 2006:CD000088. doi: 10.1002/14651858.CD000088.pub2
8. Lobban, F, Postlethwaite, A, Glentworth, D, Pinfold, V, Wainwright, L, Dunn, G, et al. A systematic review of randomised controlled trials of interventions reporting outcomes for relatives of people with psychosis. Clin Psychol Rev. (2013) 33:372–82. doi: 10.1016/j.cpr.2012.12.004
9. Alhadidi, MM, Lim Abdullah, K, Yoong, TL, Al Hadid, L, and Danaee, M. A systematic review of randomized controlled trials of psychoeducation interventions for patients diagnosed with schizophrenia. Int J Soc Psychiatry. (2020) 66:542–52. doi: 10.1177/0020764020919475
10. Herrera, SN, Sarac, C, Phili, A, Gorman, J, Martin, L, Lyallpuri, R, et al. Psychoeducation for individuals at clinical high risk for psychosis: a scoping review. Schizophr Res. (2023) 252:148–58. doi: 10.1016/j.schres.2023.01.008
11. Chan, KWS, Hui, LMC, Wong, HYG, Lee, HME, Chang, WC, and Chen, YHE. Medication adherence, knowledge about psychosis, and insight among patients with a schizophrenia-spectrum disorder. J Nerv Ment Dis. (2014) 202:25–9. doi: 10.1097/NMD.0000000000000068
12. Bilgin, A, and Ozdemir, L. Interventions to improve the preparedness to Care for Family Caregivers of Cancer patients: a systematic review and Meta-analysis. Cancer Nurs. (2022) 45:E689–705. doi: 10.1097/NCC.0000000000001014
13. Brent, BK, Giuliano, AJ, Zimmet, SV, Keshavan, MS, and Seidman, LJ. Insight into illness in patients and caregivers during early psychosis: a pilot study. Schizophr Res. (2011) 127:100–6. doi: 10.1016/j.schres.2010.12.024
14. Canadian Psychiatric Association. Clinical practice guidelines. Treatment of schizophrenia. Can J Psychiatr. (2005) 50:7S–57S.
15. NICE. Psychosis and schizophrenia in adults: prevention and management guidance. (2014). Available at: https://www.nice.org.uk/guidance/cg178 (Accessed February 9, 2023).
16. Cuijpers, P. The effects of family interventions on relatives’ burden: a meta- analysis. United Kingdom: Centre for Reviews and Dissemination (1999).
17. Harvey, C, and O’Hanlon, B. Family psycho-education for people with schizophrenia and other psychotic disorders and their families. Aust N Z J Psychiatry. (2013) 47:516–20. doi: 10.1177/0004867413476754
18. Casacchia, M, and Roncone, R. Italian families and family interventions. J Nerv Ment Dis. (2014) 202:487–97. doi: 10.1097/NMD.0000000000000149
19. McFarlane, WR, Dixon, L, Lukens, E, and Lucksted, A. Family psychoeducation and schizophrenia: a review of the literature. J Marital Fam Ther. (2003) 29:223–45. doi: 10.1111/j.1752-0606.2003.tb01202.x
20. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. New Delhi: Jaypee Brothers Medical Publishers (2000). 943 p.
21. Kay, SR, Fiszbein, A, and Opler, LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. (1987) 13:261–76. doi: 10.1093/schbul/13.2.261
22. Thompson, K, Kulkarni, J, and Sergejew, AA. Reliability and validity of a new medication adherence rating scale (MARS) for the psychoses k. Schizophr Res. (2000) 42:241–7. doi: 10.1016/S0920-9964(99)00130-9
23. Misdrahi, D, Verdoux, H, Llorca, P-M, and Baylé, F-J. Therapeutic adherence and schizophrenia: the interest of the validation of the French translation of medication adherence rating scale (MARS). Encéphale. (2004) 30:409–10.
24. Fond, G, Boyer, L, Boucekine, M, Aden, LA, Schürhoff, F, Tessier, A, et al. Validation study of the medication adherence rating scale. Results from the FACE-SZ national dataset. Schizophr Res. (2017) 182:84–9. doi: 10.1016/j.schres.2016.10.023
25. Misdrahi, D, Tessier, A, Swendsen, J, Berna, F, Brunel, L, Capdevielle, D, et al. Determination of adherence profiles in schizophrenia using self-reported adherence: results from the FACE-SZ dataset. J Clin Psychiatry. (2016) 77:e1130–6. doi: 10.4088/JCP.15m10115
26. Compton, MT, Quintero, L, and Esterberg, ML. Assessing knowledge of schizophrenia: development and psychometric properties of a brief, multiple-choice knowledge test for use across various samples. Psychiatry Res. (2007) 151:87–95. doi: 10.1016/j.psychres.2006.05.019
27. Richieri, R, Boyer, L, Reine, G, Loundou, A, Auquier, P, Lançon, C, et al. The schizophrenia caregiver quality of life questionnaire (S-CGQoL): development and validation of an instrument to measure quality of life of caregivers of individuals with schizophrenia. Schizophr Res. (2011) 126:192–201. doi: 10.1016/j.schres.2010.08.037
28. Zarit, SH, Todd, PA, and Zarit, JM. Subjective burden of husbands and wives as caregivers: a longitudinal study. Gerontologist. (1986) 26:260–6. doi: 10.1093/geront/26.3.260
29. Morin, AJS, Moullec, G, Maïano, C, Layet, L, Just, J-L, and Ninot, G. Psychometric properties of the Center for Epidemiologic Studies Depression Scale (CES-D) in French clinical and nonclinical adults. Rev Epidemiol Sante Publique. (2011) 59:327–40. doi: 10.1016/j.respe.2011.03.061
30. Misdrahi, D, Verdoux, H, Lançon, C, and Bayle, F. The 4-point ordinal Alliance self-report: a self-report questionnaire for assessing therapeutic relationships in routine mental health. Compr Psychiatry. (2009) 50:181–5. doi: 10.1016/j.comppsych.2008.06.010
31. Kemp, R, Kirov, G, Everitt, B, Hayward, P, and David, A. Randomised controlled trial of compliance therapy. 18-month follow-up. Br J Psychiatry. (1998) 172:413–9. doi: 10.1192/bjp.172.5.413
32. Bird, V, Premkumar, P, Kendall, T, Whittington, C, Mitchell, J, and Kuipers, E. Early intervention services, cognitive-behavioural therapy and family intervention in early psychosis: systematic review. Br J Psychiatry. (2010) 197:350–6. doi: 10.1192/bjp.bp.109.074526
33. Cassidy, E, Hill, S, and O’Callaghan, E. Efficacy of a psychoeducational intervention in improving relatives’ knowledge about schizophrenia and reducing rehospitalisation. Eur Psychiatry. (2001) 16:446–50. doi: 10.1016/s0924-9338(01)00605-8
34. Mayoral, F, Berrozpe, A, de la Higuera, J, Martinez-Jambrina, JJ, de Dios, LJ, and Torres-Gonzalez, F. Efficacy of a family intervention program for prevention of hospitalization in patients with schizophrenia. A naturalistic multicenter controlled and randomized study in Spain. Rev Psiquiatr. Salud Ment. (2015) 8:83–91. doi: 10.1016/j.rpsm.2013.11.001
35. Sellwood, W, Tarrier, N, Quinn, J, and Barrowclough, C. The family and compliance in schizophrenia: the influence of clinical variables, relatives’ knowledge and expressed emotion. Psychol Med. (2003) 33:91–6. doi: 10.1017/s0033291702006888
36. Velligan, DI, Weiden, PJ, Sajatovic, M, Scott, J, Carpenter, D, Ross, R, et al. Expert consensus panel on adherence problems in serious and persistent mental illness. The expert consensus guideline series: adherence problems in patients with serious and persistent mental illness. J Clin Psychiatry. (2009) 70:1–46.
37. Kretchy, IA, Osafo, J, Agyemang, SA, Appiah, B, and Nonvignon, J. Psychological burden and caregiver-reported non-adherence to psychotropic medications among patients with schizophrenia. Psychiatry Res. (2018) 259:289–94. doi: 10.1016/j.psychres.2017.10.034
38. Gupta, S, Isherwood, G, Jones, K, and Van Impe, K. Assessing health status in informal schizophrenia caregivers compared with health status in non-caregivers and caregivers of other conditions. BMC Psychiatry. (2015) 15:162. doi: 10.1186/s12888-015-0547-1
39. Xia, J, Merinder, LB, and Belgamwar, MR. Psychoeducation for schizophrenia. Cochrane Database Syst Rev. (2011) 2011):CD002831. doi: 10.1002/14651858.CD002831.pub2
40. Roncone, R, Giusti, L, Bianchini, V, Casacchia, M, Carpiniello, B, Aguglia, E, et al. Family functioning and personal growth in Italian caregivers living with a family member affected by schizophrenia: results of an add-on study of the Italian network for research on psychoses. Front Psych. (2022) 13:1042657. doi: 10.3389/fpsyt.2022.1042657
41. Galderisi, S, Rossi, A, Rocca, P, Bertolino, A, Mucci, A, Bucci, P, et al. Pathways to functional outcome in subjects with schizophrenia living in the community and their unaffected first-degree relatives. Schizophr Res. (2016) 175:154–60. doi: 10.1016/j.schres.2016.04.043
42. Dionne-Odom, JN, Bakitas, MA, and Ferrell, B. Psychoeducational interventions for cancer family caregivers In:. Cancer caregivers. New York: Oxford University Press (2019). 105–29.
43. Sauvanaud, F, Kebir, O, Vlasie, M, Doste, V, Amado, I, and Krebs, M-O. Therapeutic benefit of a registered psychoeducation program on treatment adherence, objective and subjective quality of life: French pilot study for schizophrenia. Encéphale. (2017) 43:235–40. doi: 10.1016/j.encep.2015.12.028
44. Margetić, M, Jakovljević, J, Furjan, Z, Margetić, B, and Marsanić, V. Quality of life of key caregivers of schizophrenia patients and association with kinship. Cent Eur J Public Health. (2013) 21:220–3. doi: 10.21101/cejph.a3918
45. Greenberg, JS, Knudsen, KJ, and Aschbrenner, KA. Prosocial family processes and the quality of life of persons with schizophrenia. Psychiatr Serv. (2006) 57:1771–7. doi: 10.1176/ps.2006.57.12.1771
46. Khalil, AH, ELNahas, G, Ramy, H, Abdel Aziz, K, Elkholy, H, and El-Ghamry, R. Impact of a culturally adapted behavioural family psychoeducational programme in patients with schizophrenia in Egypt. Int J Psychiatry Clin Pract. (2019) 23:62–71. doi: 10.1080/13651501.2018.1480786
Keywords: psychoeducation, caregivers, schizophrenia, relapse, burden, depression, therapeutic alliance, quality of life
Citation: Tessier A, Roger K, Gregoire A, Desnavailles P and Misdrahi D (2023) Family psychoeducation to improve outcome in caregivers and patients with schizophrenia: a randomized clinical trial. Front. Psychiatry 14:1171661. doi: 10.3389/fpsyt.2023.1171661
Received: 22 February 2023; Accepted: 06 June 2023;
Published: 23 June 2023.
Edited by:
Yann Hode, Association Psychoeducation Profamille, FranceReviewed by:
Mario Luciano, University of Campania Luigi Vanvitelli, ItalyCopyright © 2023 Tessier, Roger, Gregoire, Desnavailles and Misdrahi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Arnaud Tessier, YXRlc3NpZXJAY2gtcGVycmVucy5mcg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.