- 1PhD Programme in Mental Health, Department of Psychiatry, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand
- 2King Chulalongkorn Memorial Hospital, The Thai Red Cross Society, Department of Psychiatry, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand
- 3Center of Excellence for Maximizing Children's Developmental Potential, Department of Pediatric, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand
- 4Cognitive Impairment and Dementia Research Unit, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand
- 5IMPACT Strategic Research Center, Barwon Health, Geelong, VIC, Australia
- 6Department of Psychiatry, Medical University of Plovdiv, Plovdiv, Bulgaria
- 7Research Institute, Medical University of Plovdiv, Plovdiv, Bulgaria
- 8Kyung Hee University, Seoul, Republic of Korea
Introduction: Neuroticism, a personality trait, can predict major depressive disorder (MDD). The current study aims to determine whether a) neuroticism is a feature of the acute state of MDD, including suicidal behaviors (SB); and b) adverse childhood experiences (ACEs) are associated with neuroticism in MDD.
Methods: This study included 133 participants, 67 healthy controls and 66 MDD patients, and assessed the Big 5 Inventory (BFI), ACEs using the ACE Questionnaire, and the phenome of depression using the Hamilton Depression Rating Scale (HAM-D), Beck Depression Inventory (BDI), The State-Trait Anxiety Inventory (STAI) and Columbia Suicide Severity Rating Scale (C-SSRS) scores to assess current SB.
Results: Neuroticism was significantly higher in MDD than controls, and it explained 64.9% of the variance in the depression phenome (a latent vector extracted from HAM-D, BDI, STAI, and current SB scores). The other BFI domains had much less (extraversion, agreeableness) or no effect (openness, conscientiousness). One latent vector could be extracted from the phenome, lifetime dysthymia, lifetime anxiety disorders and neuroticism scores. Neglect (physical and emotional) and abuse (physical, neglect and sexual) account for approximately 30% of the variance in this latent vector. Partial Least Squares analysis showed that the effects of neglect on the phenome were partially mediated by neuroticism, whereas the effects of abuse were completely mediated by neuroticism.
Discussion: Neuroticism (trait) and the MDD phenome (state) are both manifestations of the same latent core, with neuroticism being a subclinical manifestation of MDD.
Introduction
Globally, mood disorders, such as major depressive disorder (MDD), are among the leading causes of disability (1). The effects of depressive symptoms, both on individuals and on society, include diminished quality of life, increased health care costs, and increased medical morbidity and mortality (2). Point prevalence and 1-year prevalence estimates for MDD vary among studies. For example, according to the World Health Organization (WHO), 4.4% of the global population suffers from major depressive disorder (MDD), and approximately 4.4% of Thais suffer from depression (Power, 24 July 2013). The point prevalence of depression is approximately 12.9%, with a 1-year prevalence of 7.2% and a lifetime prevalence of 10.8% (3).
Depression can occur at any point in life, but it manifests more notably during adolescence, particularly in females (4). Complex interactions between social, psychological, and biological factors are associated with the onset of depressive episodes (5). Adverse childhood experiences (ACEs) and negative life events are associated with the onset of depressive episodes (5). ACEs, such as emotional neglect and abuse, physical neglect and abuse, and sexual abuse, may also influence the recurrence of illness (ROI) of depressive episodes, lifetime suicidal behaviors including ideation and attempts, and the severity of depression, including neurocognitive deficits and anxiety symptoms (6–11). As a result, ACEs affect the course and progression of disease and the lifetime trajectory of patients with depression (12–14).
Importantly, those who have experienced ACEs also have an increased risk of personality disorders and traits, such as neuroticism (15). For instance, a significant correlation exists between neuroticism and sexual, emotional, and physical abuse, as well as emotional and physical neglect (16). Unlike adverse childhood experiences, negative adult life events have less of an effect on neuroticism (17).
Neuroticism is operationally defined as a personality trait that does not interfere with everyday function but is characterized by a chronic negative emotional state or emotional instability, and increased irritability, anger, sadness, anxiety, worry, self-consciousness, and vulnerability to environmental stressors (18, 19). Moreover, individuals with increased neuroticism experience the environment as unsafe and distressing, and they are frequently self-critical, sensitive to the criticism of others and punishment, they feel personally inadequate, and experience negative affect (20, 21). Neuroticism is associated with mood and anxiety symptoms in clinical (22) and non-clinical (23–25) study groups, as well as in cross-sectional studies (26, 27). Neuroticism can be measured using the Big Five Inventory (BFI), a rating scale that assesses 5 personality traits, including neuroticism, openness to experience, conscientiousness, extraversion, and agreeableness. However, it is unclear how ACEs and the five BFI personality traits interact, as well as if neuroticism plays a role in mediating how ACEs affect the depressed phenome. The latter is defined as the multidimensional set of all traits or phenotypes (a data matrix) of human depression under the impact of environmental factors and adverse outcome pathways, from the genome, proteome to neuronal circuits (28–30). The scientific field that examines the phenome is known as “phenomics.”
Hence, the aims of the present study are to examine whether: (a) ACEs are significantly associated with the 5 BFI personality dimensions in patients with MDD; (b) increased neuroticism or lowered levels of the other personality dimensions are associated with the phenome of MDD including suicidal behaviors; and (c) the effects of ACEs on the phenome of MDD are mediated via increased neuroticism or lowered openness, conscientiousness, extraversion, or agreeableness.
Methods and participants
Participants
In this research, we included 67 healthy controls and 66 depressed patients. We included Thai-speaking participants, ages 18–65 years, both males and females. Patients were recruited as outpatients of the Department of Psychiatry at King Chulalongkorn Memorial Hospital, Bangkok, Thailand. The controls were recruited by word of mouth within the same catchment region, namely Bangkok, from September 2021 to February 2022. The patients were diagnosed as major depressive disorder (MDD) using the DSM-5 criteria (31). The healthy controls were staff, and family or friends of staff, and friends of MDD patients. Exclusion criteria for patients and controls are: (a) psychiatric axis-1 diagnosis including bipolar disorder, schizophrenia, schizo-affective psychosis, and psycho-organic and substance use disorders (SUD) (except tobacco use disorder, TUD); (b) axis-2 diagnosis such as antisocial and borderline personality disorder; (c) neurological disorders such as stroke, epilepsy, brain tumors, and multiple sclerosis, (d) major medical illness including (auto)immune disorders, psoriasis, systemic lupus erythematous, inflammatory bowel disease, and rheumatoid arthritis; (e) pregnant and lactating women; (f) recent surgery; (g) infection 1 month prior to the study; (h) subjects treated with immunomodulatory drugs including glucocorticoids and therapeutically doses of antioxidants and omega-3; and (i) frequent use of pain killers. In addition, controls were excluded when they suffered from MDD (current and lifetime) and DSM-IV anxiety disorders, and showed a positive family history of mood disorders, suicide, and substance use disorders.
All subjects were requested to give voluntary, written informed consent prior to their research participation. The study was conducted in accordance with international and Thai ethical standards and privacy laws. The Institutional Review Board of Chulalongkorn University’s Faculty of Medicine in Bangkok, Thailand (#445/63), authorized the research.
Clinical measurements
Sociodemographic and clinical data were obtained using a semi-structured questionnaire obtained through interviews with patients and controls. The semi-structured interview comprises sex, marital status, employment status, occupational, income, year of education, family history (FHIS) of mood disorders and suicidal behaviors, and FHIS of substance use disorders (SUD), medical history, psychotropic drugs used, and medical history. MDD was diagnosed using DSM-5 criteria and the Mini International Neuropsychiatric Interview (M.I.N.I.) (32). The latter case definition and criteria were also employed to assess lifetime and current diagnoses of dysthymia, generalized anxiety disorder (GAD), panic disorder (PD), agoraphobia, social phobia, obsessive–compulsive disorder (OCD), post-traumatic stress disorder (PTSD), and SUD. We used the DSM-IV concept of anxiety disorders, namely PTSD, GAD, OCD, phobia, agoraphobia, and PD to make the diagnosis of lifetime or current anxiety disorder (14). The severity of depression was measured using the Hamilton Rating Scale for Depression (HAM-D) (33) and the Beck Depression Inventory II (BDI-II) (34). The latter is a 21-item self-report inventory designed to assess the presence and severity of depressive symptoms and was translated into Thai by Mungpanich (35). The severity of anxiety was assessed using the State–Trait Anxiety Inventory (STAI) state version (36) in a validated Thai translation (37). The DSM-5 criteria were used to make the diagnosis of TUD.
The Big Five Inventory (BFI) (38) in a Thai translation (39) was used to assess five major personality dimensions, namely neuroticism, openness to experience, conscientiousness, extraversion, and agreeableness. This scale consists of 44 questions rated on a Likert scale scoring from 1 (lowest) to 5 (highest). In the present study, we used the raw scores of the 5 dimensions as well as factors extracted from a combination of these dimensions. ACEs were assessed using the ACE Questionnaire in a Thai translation (40). This questionnaire consists of 28 items covering the traumatic experiences in childhood in 10 domains, namely: emotional abuse (2 items), physical abuse (2 items), sexual abuse (4 items), emotional neglect (5 items), physical neglect (5 items), domestic violence (4 items), household substance abuse (2 items), mental illness in household (2 items), parental divorce (1 item), and a criminal household member (1 item). The content validity of questionnaire met the standards, with an internal consistency reliability of 0.79 for the abuse domain, 0.82 for the neglect domain and 0.66 for the household dysfunction domain. We used the Columbia Suicide Severity Rating Scale (C-SSRS) (41) to assess the intensity of suicidal ideation and suicidal attempts, either lifetime or current. The C-RRRS measures the severity of suicidal ideation (SI) and attempts (SA), intensity, lethality, and frequency, as well as self-injurious behaviors without suicidal intent.
The ASSIST (Alcohol, Smoking and Substance Involvement Screening Test) is a tool to evaluate experiences with alcohol consumption, tobacco (TUD), and substance (SUD) abuse (42). This tool focuses on the substance used in the last 3 months. Body mass index (BMI) was calculated as weight (kg) divided by height (m) squared. Metabolic Syndrome (MetS) was defined according to the American Heart Association/National Heart, Lung, and Blood Institute 2009 Joint Scientific Statement (43) as the presence of 3 or more of the following components: (1) waist circumference ≥ 90 cm for men, ≥80 cm for women or BMI ≥ 25 kg/m2; (2) high triglyceride level: ≥150 mg/dL (≥1.69 mmol/l); (3) low HDL cholesterol level: <40 mg/dL (<1.03 mmol/l) for men, <50 mg/dl (<1.29 mmol/l) for women; (4) high blood pressure: ≥130 mm Hg systolic blood pressure, ≥85 mm Hg diastolic blood pressure, or treatment with antihypertensive medication; and (5) high fasting glucose (≥100 mg/dl [≥5.56 mmol/l]) or a diabetes diagnosis.
Statistical analysis
ANOVA was used to compare scale variables among diagnostic groups, while Chi-square or Fisher’s Exact Probability Test was employed to compare nominal variables across categories. Correlations between two sets of scale variables were computed using Pearson’s product moment or Spearman’s rank order coefficients, while associations between scale and binary variables were examined using point-biserial correlation coefficients. Results of multiple comparisons or correlations are p-corrected for false discovery rate (FDR). We performed principal component analysis (PCA) to reduce the number of items (e.g., ACE, BFI domains) into one PC score, which then could be used in other statistical analyses. Factorability was checked using the Kaiser–Meyer–Olkin test for sample adequacy, which is considered satisfactory when >0.5, and the Bartlett’s sphericity test. The first PC is only accepted when the variance explained (VE) is >50% and all loadings on the first PC are >0.65. The effects of explanatory variables (ACEs, Big 5 scores) on dependent variables (such as the phenome score) were examined using multiple regression analysis (manual method). In addition, we used a forward stepwise automatic regression method with p-values of 0.05 to-enter and 0.1 to remove to delineate the best predictors of the model. In addition to F statistics (and p values) and total variance (R2 or partial eta squared as effect size) explained by the model, we calculated the standardized coefficients with t-statistics and exact p-values for each of the explanatory variables in the final regression models. Collinearity and multicollinearity were analyzed utilizing tolerance (cut-off value <0.25), the variance inflation factor (cut-off value >4), the condition index and variance proportions from the collinearity diagnostics table. The White and modified Breusch–Pagan tests were utilized to confirm the existence of heteroskedasticity. All of the aforementioned tests were two-tailed, and an alpha value of 0.05 was considered statistically significant. We employed the IBM, Windows SPSS version 28.
Partial Least Squares path analysis (SmartPLS) was used to determine the causal relationship between the ACEs (input variables) and the phenome of depression (output variable). All variables were entered either as latent vectors (LVs) derived from their manifestations or as single indicators. When the inner and outer models met predefined quality criteria, such as (a) the model fit is <0.08 in terms of standardized root mean squared residual (SRMR), (b) the LVs have a high composite reliability (>0.7), Cronbach’s alpha (>0.7), and rho A (>0.8) values, with an average variance extracted (AVE) > 0.5, and (c) all LV loadings are greater than 0.65 at p < 0.001, a complete PLS analysis was performed using 5,000 bootstrap samples. We also ran a Confirmatory Tetrad Analysis (CTA) to make sure the LVs were not misclassified as reflective models. Using PLS predict and a tenfold cross validation technique, the model’s prediction performance was tested. We computed pathway coefficients (with exact p-values) as well as the total direct and indirect effects and specific indirect effects. An a priori power calculation to estimate the sample size using G*Power 3.1.9.4 showed that to obtain a power of 0.8 in a multiple regression analysis (or PLS analysis) with 5 covariates, the sample size should be at least 70 when using an effect size of 0.2 at p = 005 (two-tailed).
Results
Sociodemographic data of patients and controls
Table 1 shows that there were no significant differences in sex ratio, age, education, BMI, waist circumference, income, TUD, and systolic and diastolic blood pressure between controls and patients. Only the employment rate was significantly different between both groups.
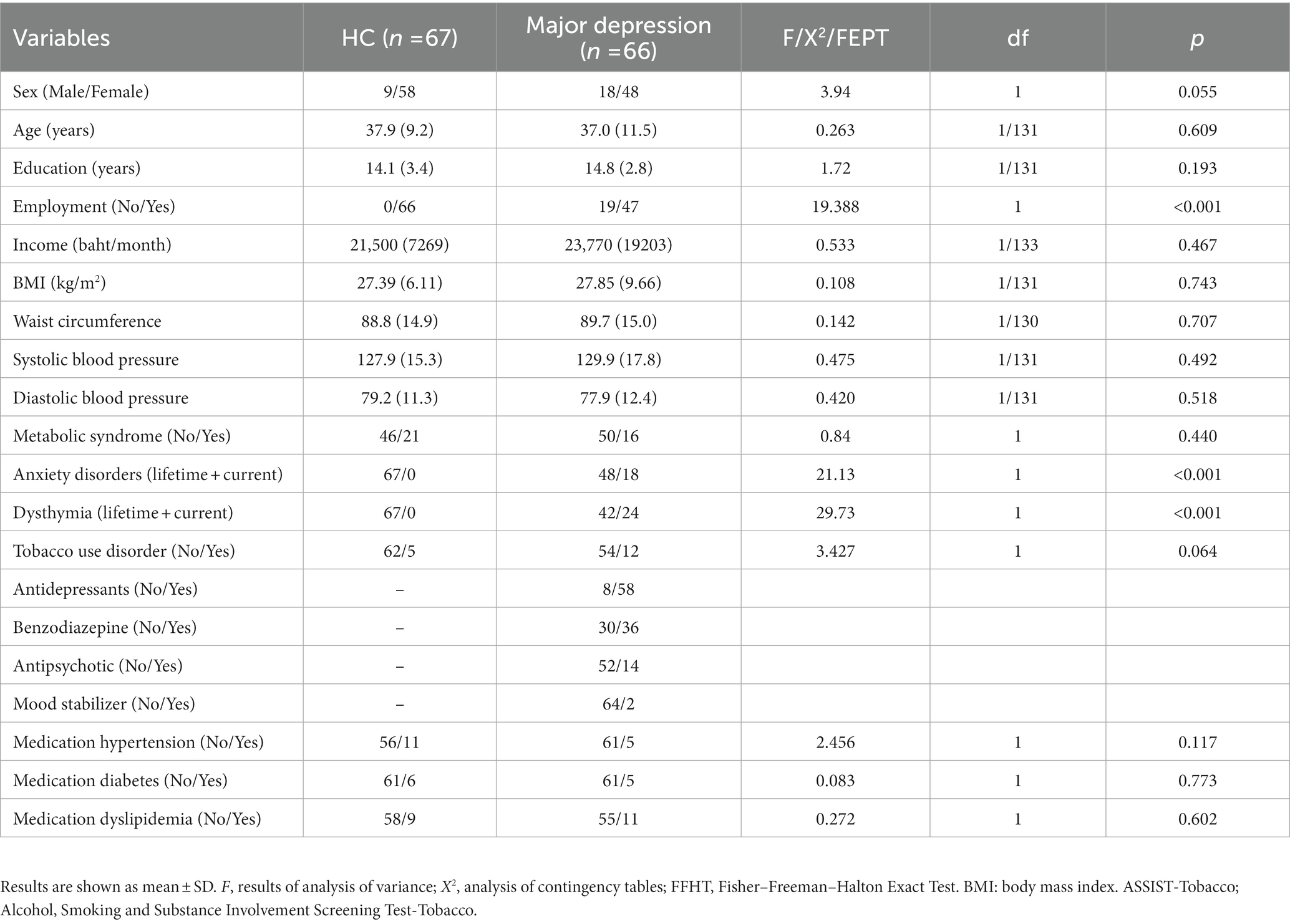
Table 1. Demographic and clinical data of the Major Depression patients and healthy controls (HC) included in the present study.
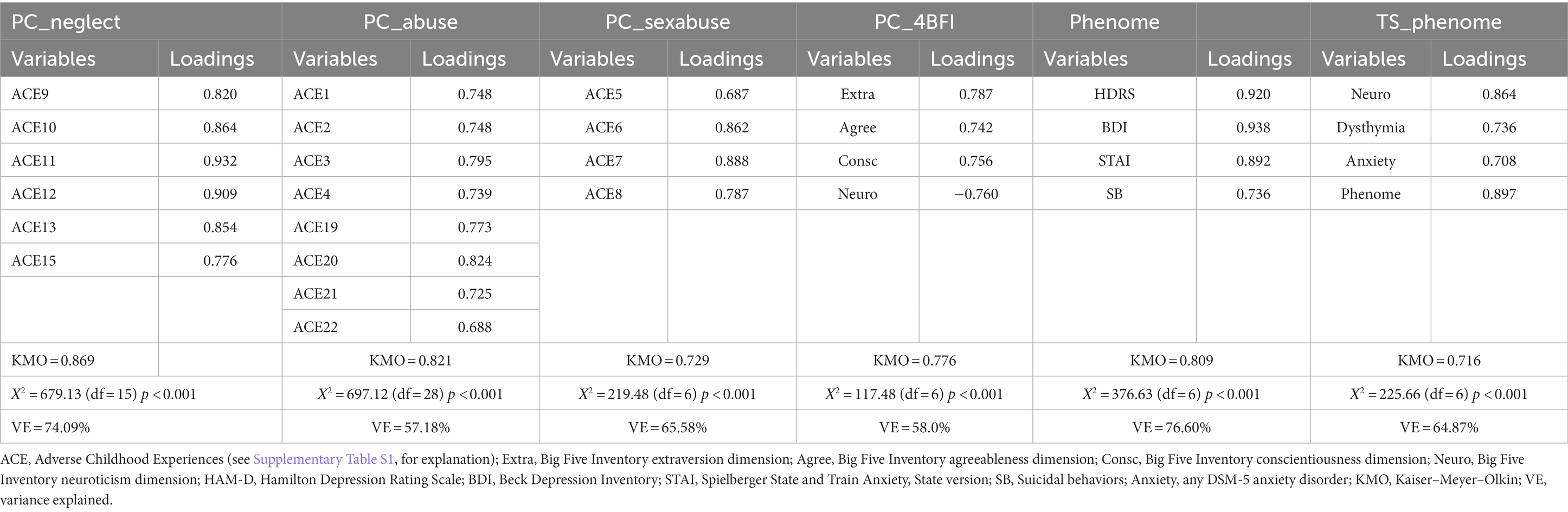
Results of PC analysis
Table 2 shows the results of PC analyses. We were not able to extract one PC from all ACE items; however, three validated PCs could be constructed. First, we were able to extract a PC from ACE9, ACE10, ACE11, ACE12, ACE13, and ACE15 and labeled this “PC_neglect” (see Supplementary Table S1 for explanation of the ACE items). A second validated factor could be extracted from 8 other symptoms, including ACE1, ACE2, ACE3, ACE4, ACE19, ACE20, ACE21, and ACE22, dubbed “PC_abuse.” We were able to extract a third validated PC from ACE5, ACE6, ACE7, and ACE8, and dubbed this “PC_sexabuse.” Other items (including the ACE divorce item) were entered as single indicators in the analysis.
Table 2 also shows that we were able to extract one PC from 4 BFI dimensions, namely extraversion, agreeableness, consciousness (all positively loaded on the first PC), and neuroticism (negative loaded). Consequently, we used the inverse transformation (to underscore the role of neuroticism) of this PC in the analysis, and we labeled this indicator “PC_4BFI” (which thus reflects the effects of neuroticism and lowered extraversion, agreeableness, and conscientiousness). The fifth BFI dimension (openness to experience) did not load significantly on this first PC (loading of 0.323). Current suicidal ideation (dubbed: SI) was computed as the first PC extracted from 7 C-SSRS items, namely C-SSRS11, C-SSRS12, C-SSRS13, C-SSRS15, C-SSRS16, and C-SSRS17 (14) (KMO = 0.703, Bartlett’s χ2 = 982.510, df = 15, p < 0.001, explained variance = 72.05%, all loadings >0.672). See ESF Table 2 for an explanation of the CSSRS items. The current SA (dubbed SA) score was computed as the first PC extracted from 5 B0C-SSRS items, namely C-SSRS30, C-SSRS31, C-SSRS32, C-SSRS33 and C-SSRS34 (14) (KMO = 0.636, Bartlett’s χ2 = 302.236, df = 3, p < 0.001, explained variance = 81.14%, all loadings >0.807). Current suicidal behaviors (SB) were conceptualized as the first PC extracted from PC_SI and PC_SA.
We were also able to extract one PC from the HAM-D, BDI, STAI, and current SB scores, and labeled this first PC “phenome” (see Table 2). Moreover, as shown in Table 2 we were able to extract one PC from neuroticism, lifetime dysthymia, any lifetime anxiety disorders, and the phenome, and dubbed this PC “trait–state-(TS)-Phenome.”
ACEs and BFI scores in MDD
Table 3 shows that the PC_neglect, PC_abuse, PC_sexabuse, and ACE_divorce scores were significantly higher in MDD than controls. The frequency of FHIS of mood disorders and SBs and FHIS of SUD was significantly higher in patients than in controls. The BFI extraversion and agreeableness scores were significantly lower in MDD than in controls, whereas the BFI neuroticism score was significantly higher in MDD. There were no significant differences in openness and conscientiousness scores between both groups. All clinical scores were significantly higher in patients than in controls.
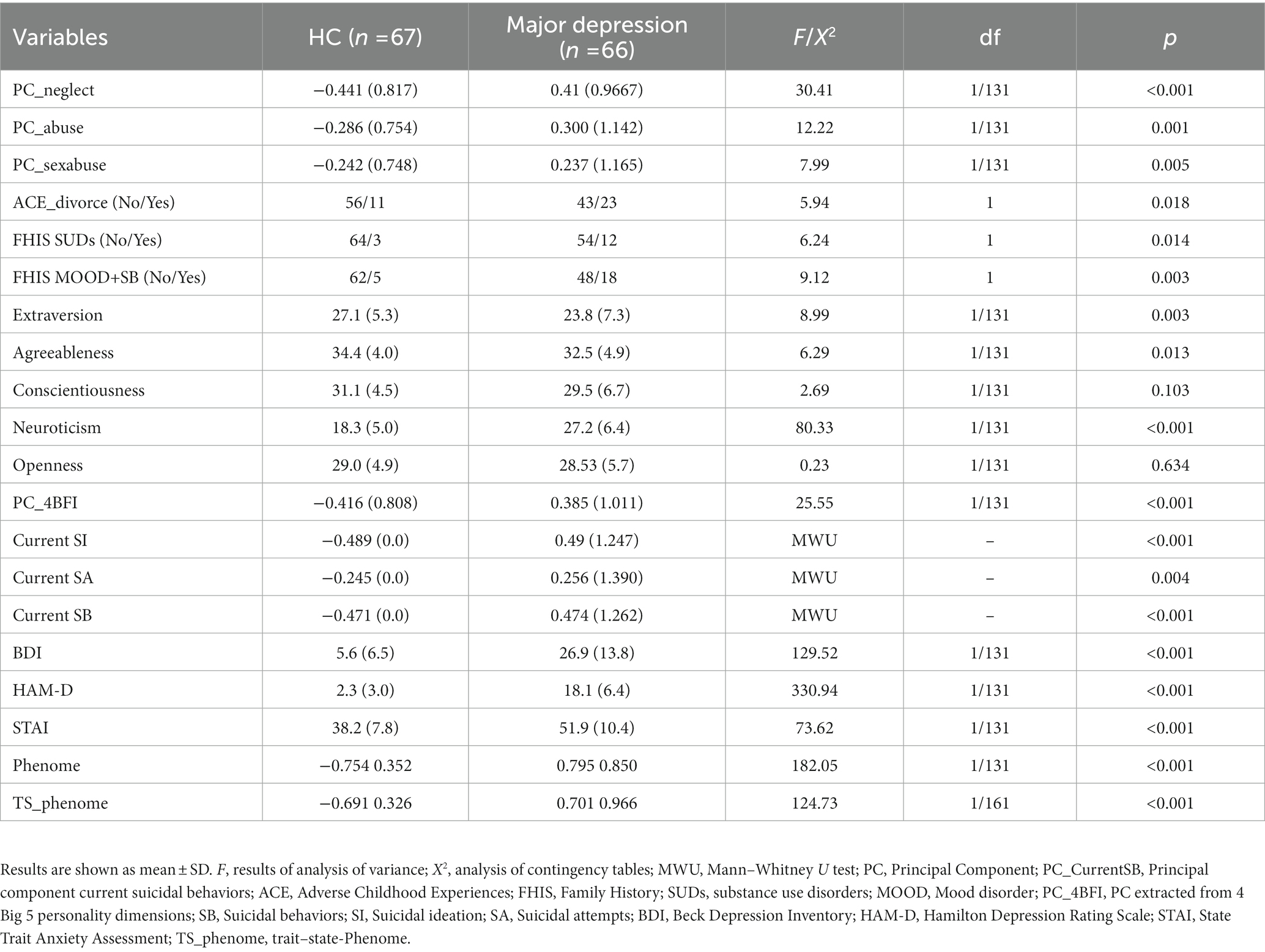
Table 3. Clinical features of major depressive disorder (MDD) and healthy controls (HC), including adverse childhood experiences (ACE), personality dimensions as assessed with the Big Five Inventory (BFI), assessment of depression and anxiety severity, and lifetime and current suicidal behaviors.
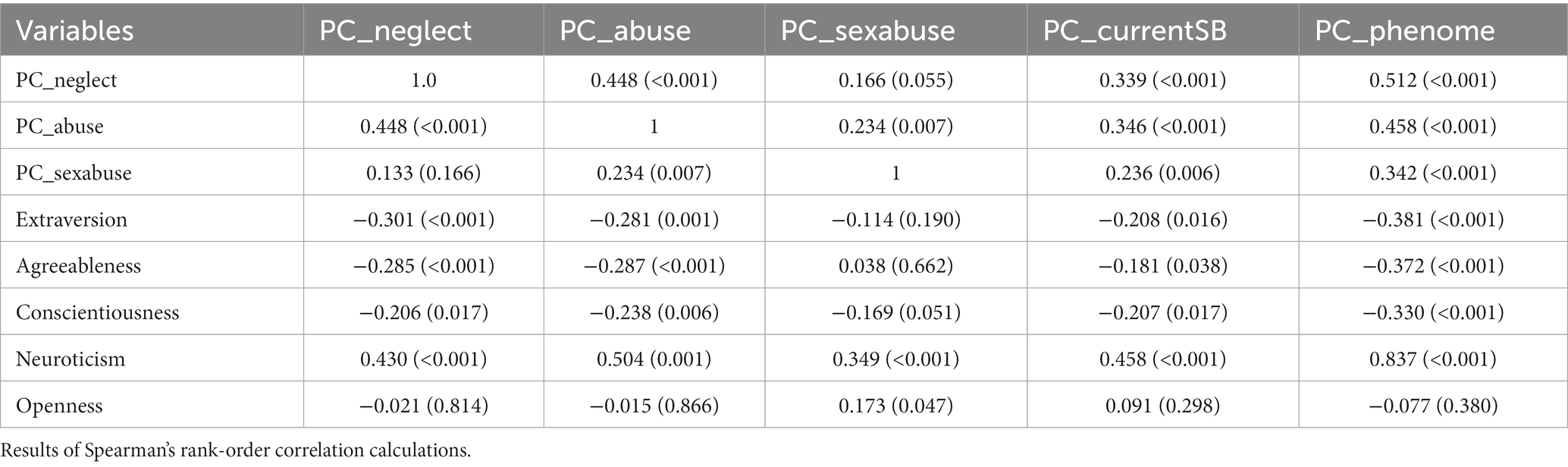
Intercorrelation matrix
Table 4 shows the intercorrelations between the different variables measured in our study. In the total study group, PC_neglect was significantly correlated with extraversion, agreeableness, conscientiousness, and neuroticism. In MDD subjects (n = 66), PC_neglect was significantly associated with extraversion (r = −0.258, p = 0.037). In the total study group, there were significant correlations between PC_abuse and all BFI dimensions, except openness, whereas in MDD patients there were significant associations with agreeableness (r = −0.252, p = 0.041), conscientiousness (r = −0.313, p = 0.010), and neuroticism (r = 0.486, p < 0.001). Table 4 shows that in the total study group, PC_sexabuse was strongly associated with neuroticism but also with openness. In subjects with MDD, there was a strong positive association between ACE_sexabuse and openness (r = 0.339, p = 0.005).
Table 4 shows that SB was significantly correlated with PC_neglect, PC_abuse, PCsexabuse, and all BFI scores (except openness); the strongest correlation was established with neuroticism. In MDD patients, SB was only correlated with neuroticism (r = 0.300, p = 0.014). The same table shows that the severity of the phenome was predicted by all PC_ACE scores, and all BFI scores (except openness). There was a very strong association between phenome and neuroticism with r = 0.837. In the restricted study group of MDD patients, we found strong associations between phenome and PC_neglect (r = 0.319, p = 0.005), PC_abuse (r = 0.345, p = 0.005), extraversion (r = −0.368, p = 0.002), agreeableness (r = −0.264, p = 0.032), conscientiousness (r = −0.358, p = 0.003), and neuroticism (r = 0.643, p < 0.001). In MDD patients, there were significant point-biserial associations between dysthymia and extraversion (r = −0.258, p = 0.037) and neuroticism (r = 0.295, p = 0.016) and significant associations between any anxiety disorder and PC_abuse (r = 0.359, p = 0.003), extraversion (r = −0.263, p = 0.033), neuroticism (r = 0.401, p < 0.001), and openness (r = 0.243, p = 0.049).
Results of multiple regression analysis
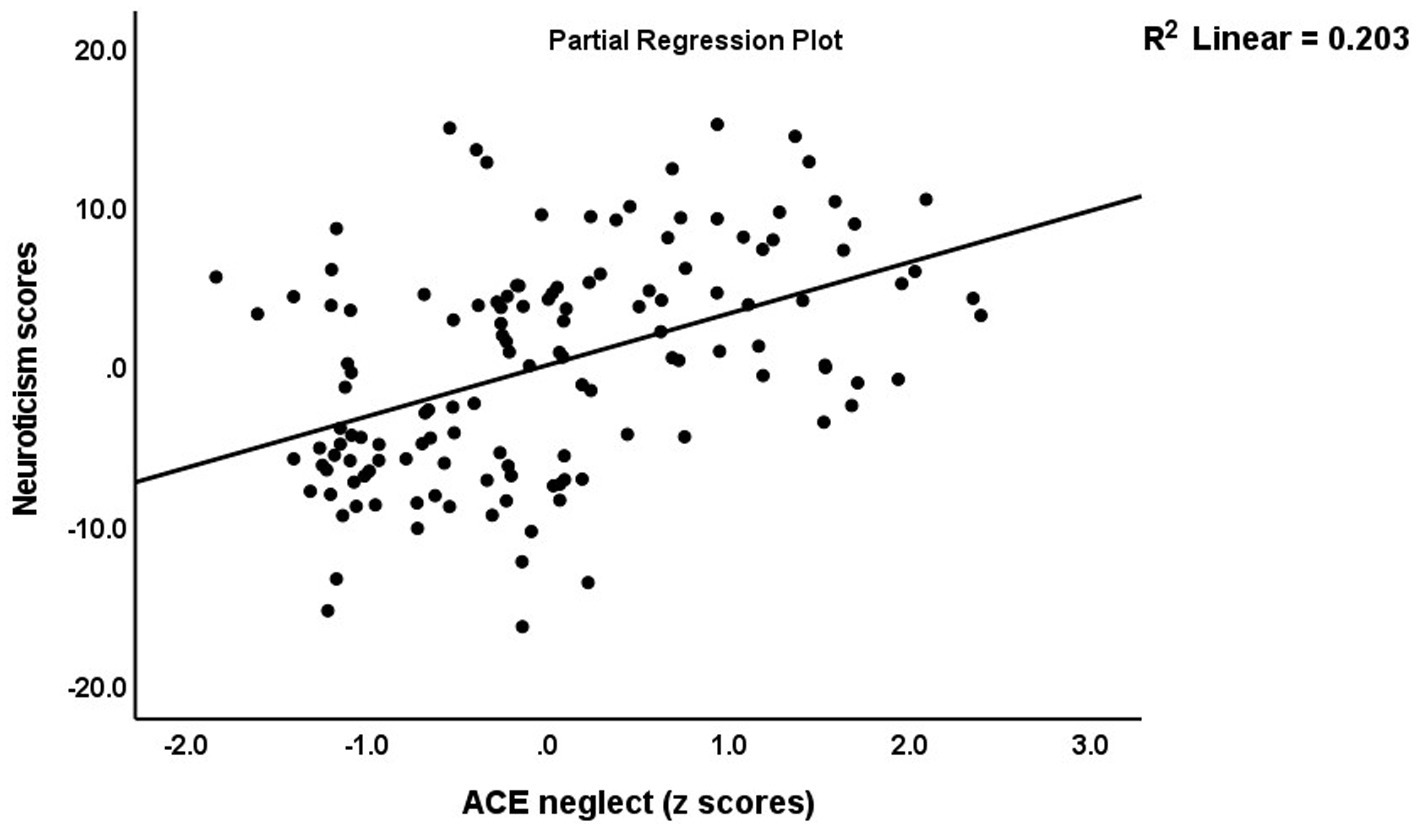
Table 5 (regression #1) shows the results of multiple regression analysis with TS_ phenome, phenome, or SB as dependent variables and the ACEs and BFI subdomain scores as explanatory variables, while allowing for the effects of background variables such as age, sex, education, etc. We found that 30.3% of the TS_phenome was explained by the combined effects of PC_neglect, PC_sexabuse, and PC_abuse (all positively associated) and age (inversely associated). Figure 1 shows the partial regression of TS_phenome on PC_neglect. Regression #2 shows that 70.2% of the variance in the phenome score was explained by the regression on neuroticism and PC_neglect (both positively) and age (inversely associated). Figure 2 shows the partial regression of the phenome score on neuroticism. Introduction of dysthymia (regression #3) improved the prediction by 3.1%. We found that 36.1% in the SB score (regression #4) was explained by PC_4BFI and PC_sexabuse. Regression #5 shows that neuroticism is predicted by the three ACE domains (all positively associated) and age (inversely associated). Figure 3 shows the partial regression of neuroticism on neglect. The 4 other BFI subdomain scores were differently predicted by the three ACE PC scores, with or without age or sex, albeit with a much lower effect size as compared with neuroticism.
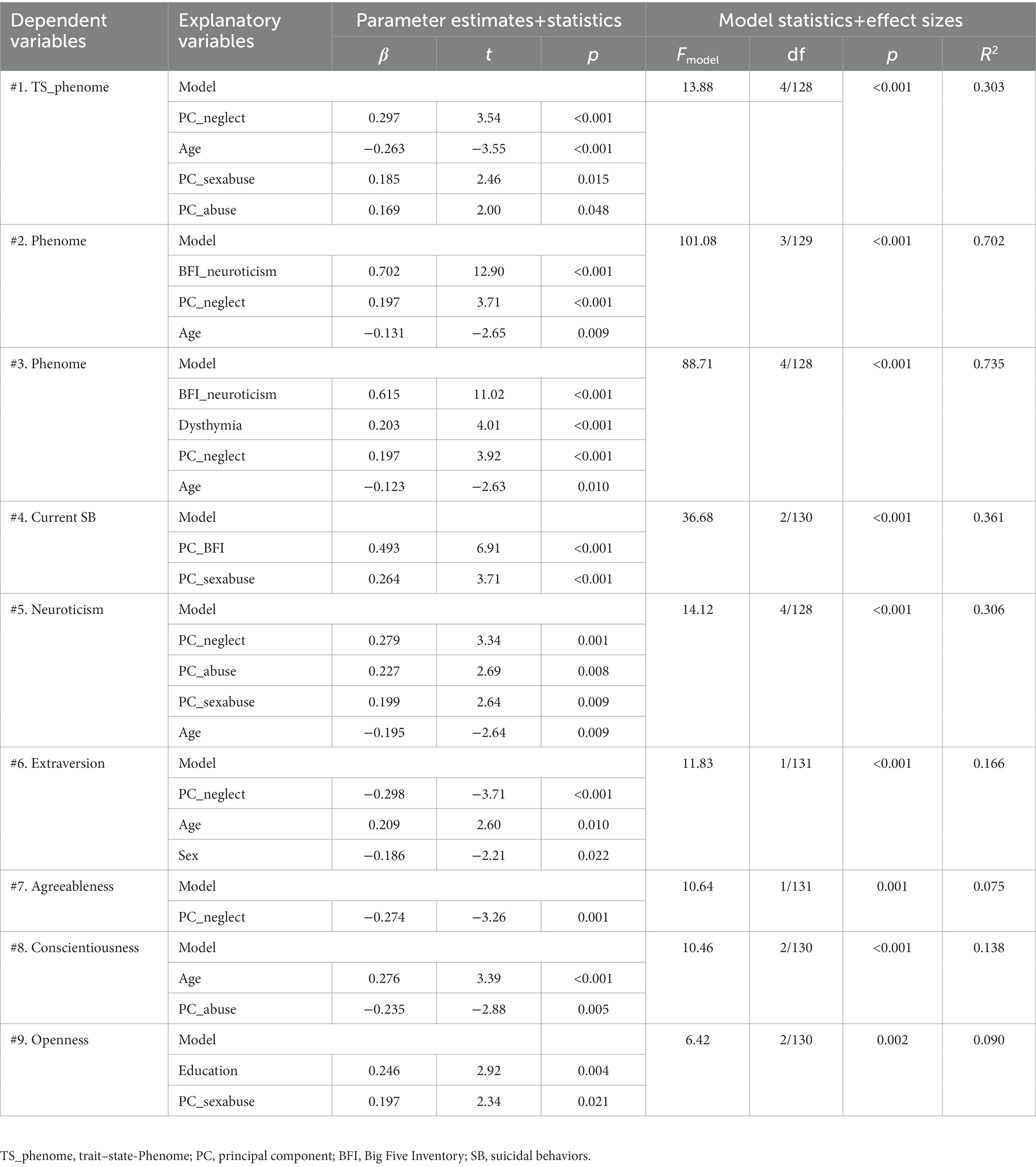
Table 5. Results of multiple regression analyses with phenome data and personality domains as dependent variables and adverse childhood experiences as input variables.
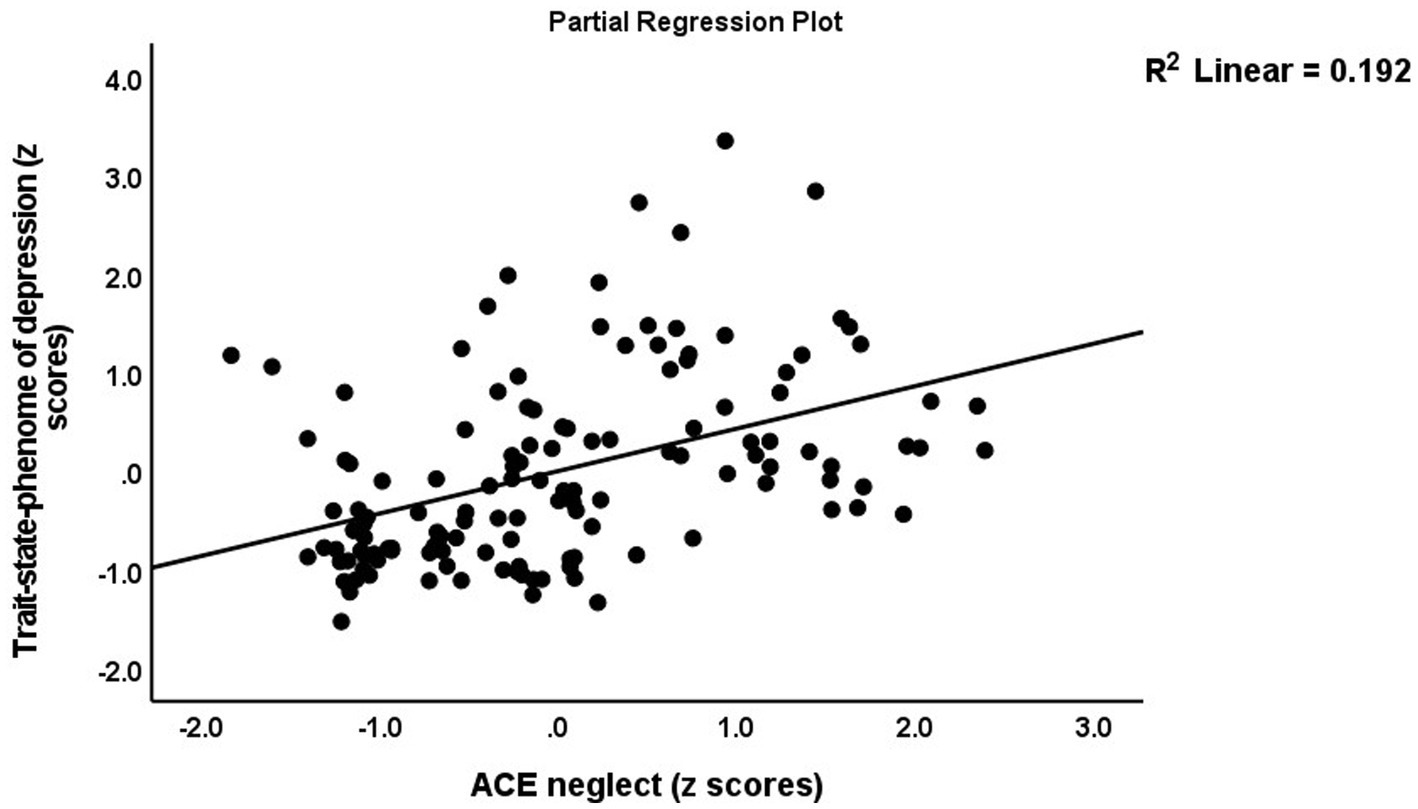
Figure 1. Partial regression of the trait–state phenome on neglect adverse childhood experiences (ACE).
Results of PLS analysis
Figure 4 shows the results of PLS analysis after feature and path selection. The phenome was conceived of as a latent vector derived from HAM-D, BDI, STAI, and SB scores. Predictors were the 5 BFI subdomain scores, the LVs constructed using neglect, abuse and sexabuse ACE scores, age, sex, and a first-degree FHIS of mood disorders + SB and FHIS of SUD. LV_neglect was conceptualized as the first factor extracted from 6 ACE items, and LV_abuse as the first factor extracted from 7 ACE items. We considered that the BFI domains could mediate the effects of ACEs on the phenome. Moreover, we examined moderation models whereby ACE moderate the effects of BFI domains. The three latent vectors constructed here showed adequate construct validity and convergence: (a) all AVEs were >0.50, namely for LV_phenome: 0.898, ACEneglect: 0.739 and ACEabuse: 0.573; (b) the Cronbach’s alpha for the three LV constructs were 0.962, 0.929, and 0.877, respectively; the composite reliabilities 0.972, 0.944, and 0.903, respectively; (c) the SRMR is 0.046; (d) PLSPredict shows that the Q2 predict values are positive (suggesting that the constructed model outperforms the most naïve benchmark); and (e) the Heterotrait-Monotrait ratio showed that discriminatory validity is established. We found that 74.3% of the variance in the phenome score was explained by the regression on LV_neglect, neuroticism (both positively), and age (inversely). Moreover, there was a significant interaction (moderation) between LV_neglect and neuroticism, yielding a positive effect on the phenome. We found that 29.4% of neuroticism was explained by both LV_neglect and LV_abuse. LV_neglect also affected agreeableness and extraversion, whereas LV_abuse also impacted conscientiousness, although only neuroticism yielded a direct effect on the phenome. There were specific indirect effects of LV_abuse (t = 3.79, p < 0.001) and LV_neglect (t = 3.57, p < 0.001) on the phenome which were mediated by neuroticism. There were significant total effects of a family history of mood disorders + SBs (t = 3.09, p = 0.002) on the phenome which were mediated by the paths from LV_neglect and LV_abuse to neuroticism. PLS multigroup analysis and premutation analyses showed that there were no significant differences among men and women and among those with and without metabolic syndrome in any of the model features.
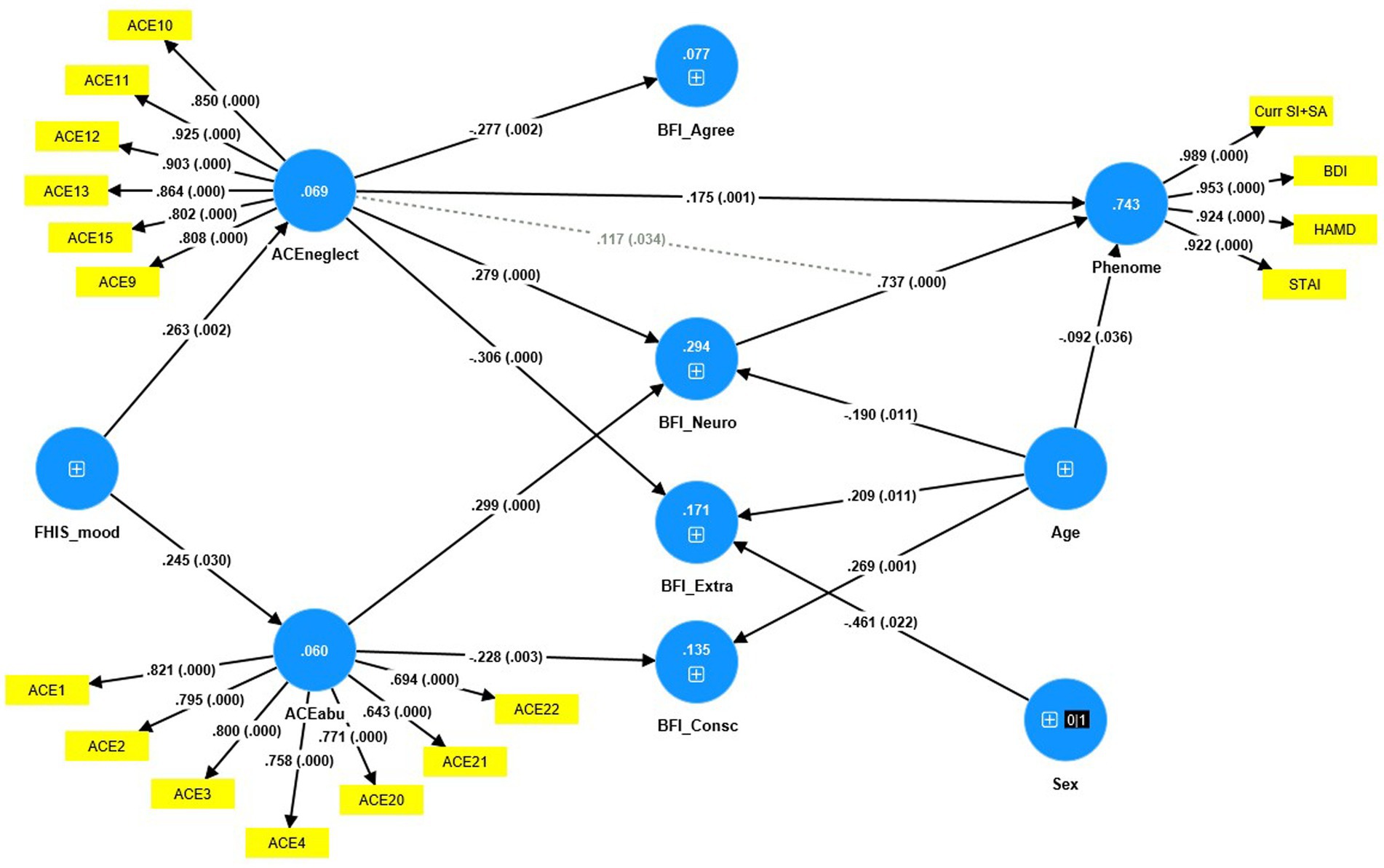
Figure 4. Result of PLS analysis. Shown are the significant paths. The Phenome, neglect adverse childhood experiences (ACEneglect) and ACEabuse were entered as latent vectors extracted from their manifestations. The other variables were entered as single indicators (denoted as +); sex was entered as a binary variable (1 = male, 0 = female). Curr SI + SA: current suicidal ideation + attempts; BDI: Beck Depression Inventory; HAM-D, Hamilton Depression Rating Scale; STAI: State and Trait Anxiety Inventory; ACE items: see Supplementary Table S2 for an explanation; FHISmood: a family history of mood disorders and suicidal attempts. BFI, Big Five Inventory; Agree, agreeableness; Neuro, neuroticism; Extra, extraversion; Consc, conscientiousness. Shown are the path coefficients (with exact p-value) of the inner model, and loadings (with p-values) of the outer model; figures in the blue circles: explained variance.
Discussion
Neuroticism, depression, and suicidal behaviors
The first major finding of this study is that neuroticism is significantly higher and extraversion and agreeableness are significantly lower in MDD patients compared to controls, whereas there were no significant differences in conscientiousness and openness. Previous research also demonstrated that BFI-measured personality traits are associated with major depression, depressive phenotypes, and depression severity (27, 44–46). For instance, according to Lester (46), the five BFI personality scores were correlated with depression severity scores and accounted for 36% of the variance. Neuroticism, agreeableness, conscientiousness, and extraversion were associated with atypical or melancholic major depression in older adults (45). Jourdy and Petot (47) discovered significant linear associations between quantitative depression severity scores and neuroticism and conscientiousness, but not extraversion, extroversion, or agreeableness. A quantitative review of 175 studies (1980–2007) on the Big Three Inventory and BFI revealed that depressed patients had higher neuroticism and lower conscientiousness scores than controls, while unipolar depression was associated with higher neuroticism and lower extraversion and conscientiousness scores (27). A recent meta-analysis (2022) comprising 243 studies that examined the associations between BFI traits and depression found a positive correlation between depression and neuroticism scores and a significant inverse correlation with conscientiousness, extraversion, and openness (48).
In the stress-diathesis model of depression, neuroticism is considered one of the important diathesis factors that increases the risk of depression and depression severity (48). As a result, it is possible to conclude that elevated neuroticism in conjunction with decreased extraversion and agreeableness (our study) and decreased openness and conscientiousness (see previous studies) increases the risk of depression and suicidal behaviors. However, we discovered that one valid and reliable factor could be extracted from neuroticism (negatively loaded), and extraversion, agreeableness, and conscientiousness (all positively loaded), and that this factor demonstrated adequate convergent and reliability validity. Consequently, these four domains are manifestations of a common core, which can be termed “the NACE dimension” (all first letters of the 4 personality traits). This may appear to contradict the 5-factor structure of the BFI, which was developed using factor analysis (49). These factors were derived from Western study samples, whereas our research involved Thai participants. While population differences may play a role, the most likely explanation for our one-factor model (the NACE dimension) is that the BFI assessment in depression biases trait measurements toward a more depressive phenotype, characterized by changes in motivation, autobiographical memories, attitude, emotion, self-concepts, and social roles, and thus intertwined changes in the 4 NACE domains.
In this regard, Allen et al. (44) proposed that depressive tendencies are determined by the “best two out of three” interaction pattern between a high-risk (withdrawal) and protective (industriousness and enthusiasm) domains. Notwithstanding, our findings indicate that a common trait (NACE-dimension) is associated with the severity of the depressive state and that neuroticism has a greater influence on the phenome of acute depression than PC_NACE. Therefore, neuroticism may be considered the “worst of five traits.” These findings support those of Kotov et al. (27) who concluded that neuroticism is the best predictor of psychopathology.
Another question is whether the depressive state (the phenome of depression) can influence BFI characteristics. In this regard, small effects of depression and anxiety in the acute state on neuroticism were observed (50). The depressive state affected extraversion and conscientiousness, but not agreeableness and openness (50). There is now evidence that personality traits are not fixed, genetically determined traits, but can change over time in response to environmental factors, such as the effects of depression (50–54). Similarly, extraversion may decline during depressive episodes and even increase permanently thereafter (55, 56). During depressive phases, however, agreeableness, conscientiousness, and openness were found to be more stable (22). Lesser known are the effects of anxiety on personality traits (50).
In the present study, however, we discovered that neuroticism accounted for 64.9% of the variance in the severity of depression and that one replicable and validated factor could be extracted from severity of depression, anxiety, suicidal behaviors, and neuroticism. This suggests that neuroticism (assessed as a trait), severity of depression/anxiety (assessed as a state over the last week), and suicidal behaviors (assessed as a state over the last month) are manifestations of a common core that may be termed the “trait–state-(TS) phenome of depression.” In addition, one factor could be extracted from the NACE trait dimension, the depression phenome (a PC extracted from depression, anxiety, and suicidal behaviors), and a positive lifetime history of dysthymia and anxiety disorders. In this respect, dysthymia, GAD, PTSD, panic disorder, agoraphobia, social phobia, and OCD were strongly associated with neuroticism, whereas dysthymia and certain anxiety disorders were also associated with extraversion and conscientiousness (both inversely) (27).
A recent study investigated the common and specific genetic risk factors of a lifetime DSM-IV diagnosis of MDD, neuroticism, present depressive symptoms, and “broadly defined depression,” which is a factor derived from the three aforementioned indicators (57). As in our study, Kendler et al. (2018) demonstrated strong associations between current depression, neuroticism, and lifetime MDD and that common genetic risk factors were associated with “broadly defined depression,” neuroticism, and the lifetime diagnosis. The same authors showed that MDD was also associated with unique risk factors that were not captured by the “broadly defined depression” construct. Nonetheless, the findings of Kendler’s research are very difficult to interpret. First, they diagnosed MDD based on unreliable DSM-IV case criteria (8). In fact, statistical analyses can only be conducted if the output (dependent) variable (thus: the diagnosis) is a correct model (58), which is not the case for the DSM-IV MDD diagnosis (8). Second, research assessing a lifetime diagnosis should not use a binary (one-bit of information) lifetime diagnosis, but rather validated latent variable scores that represent the lifetime trajectory and are built using the relevant lifetime indicators (58). A construct based on diverse assessments, as described in Maes et al. (58), is always more precise than a binary diagnosis. Third, as shown by the present research and Maes et al. (58), the current severity of depression should not be measured by a few self-reported items (which in Kendler’s study were ordinalized and differ between the three research centers), but by a quantitative latent variable score combining depressed, anxious, and other related symptoms as assessed using interviews and self-rating scales. Fourth, it is doubtful whether the broadly defined depression concept as described by Kendler’s can be validated as a reflective latent vector: (a) the loading for lifetime MDD is as low as 0.4, most likely because it is an inaccurate diagnosis and (b) the reliability, convergent validity, and internal consistency reliability of the construct have not been checked.
In the 1970s and 1980s, some scientists conceptualized “neurotic depression” as depression in patients with pre-existing characteristics, such as emotional instability, anxiety, maladaptive coping, internalization, fixation on negative memories, maladaptive processing, low self-esteem, etc. (59–62). Other researchers have hypothesized that emotional dysregulation and maladaptive coping could mediate the relationship between neuroticism and “neurotic depression” (63, 64). As a result, neurotic depression has been proposed as yet another subtype of depression (59), adding to the already unduly long list of depressive subtypes (8, 10). In spite of this, the fact that a single factor can be extracted from personality (a trait), lifetime diagnosis of dysthymia and anxiety disorders (traits), and the acute phenome of depression (state) suggests that these trait and state facets are manifestations of a common core and share a common pathophysiology. Moreover, all components of neuroticism are potential symptoms of depression (is blue, not relaxed, tense, worries, unstable, moody, not calm, nervous). In addition, a portion of the extraversion and agreeableness domain items (which in our study are both decreased in depressed patients) may appear as symptoms of depression, such as less talkative, less energy, less enthusiasm, be quiet, less assertive, inhibited, less sociable (from the extraversion domain), and having quarrels with others, not trusting others, being aloof, and having less cooperation with others (items belonging to the agreeableness trait). Therefore, it is more appropriate to conclude that neuroticism is a “forme fruste” or an intermediate phenotype of major depressive disorder, either as a prodrome (pre-symptoms), subclinical symptoms, or residual symptoms following an acute episode.
ACEs, BFI domains, and the phenome of depression
The second major finding of this study is that a large proportion of the variance in neuroticism (29.4%) is explained by the effects of ACEs, specifically the combined effects of neglect and abuse (both physical and emotional). In addition, higher neglect scores predicted lower agreeableness and extraversion, while abuse predicted lower conscientiousness. Furthermore, neuroticism partially mediated the effects of neglect on the phenome, and there was an additional moderating (or interaction) effect, namely an interaction between neglect and neuroticism. The effects of abuse on the phenome were totally mediated by neuroticism. These findings expand upon those of prior studies indicating that early-life trauma may contribute to neuroticism (62, 65, 66). There is now overwhelming evidence that ACEs are predictors of major depression, depression severity, and suicidal behaviors (9, 10, 12, 13, 58).
Moreover, the common trait–state phenome of depression (thus the first PC extracted from neuroticism and the phenome of depression including suicidal behaviors) is predicted to a significant degree (approximately 30%) by the combined effects of neglect, abuse, and sexual abuse. These results suggest that a common denominator (ACEs) predicts trait (low-grade depression or neuroticism) and state (the acute phenome of depression) phenomena, which are both indicators of the “chronic disorder” major depression. Phrased differently, these findings also indicate that neuroticism is a forme fruste of a major depressive episode.
Explanatory mechanism underpinning the effects of ACEs on depression
Recent research indicates that ACEs may influence the microimmuneoxysome (changes in the microbiome and immune and oxidative pathways), resulting in increased neurotoxicity and, consequently, depressive symptoms (58). First, increased ACEs are associated with a particular compositional gut dysbiosis enterotype, which mediates the effects of ACEs on the severity of the depression phenotype (67). Second, ACEs may lead to decreased antioxidant levels, such as paraoxonase 1 (PON 1) and high-density lipoprotein cholesterol, as well as activated nitro-oxidative stress pathways (10, 12). Thirdly, ACEs induce immune sensitization with increased activation of the cytokine and growth factor networks, which may be re-activated upon stimulation with diverse stressors (10, 68). Consequently, it is tempting to hypothesize that ACE-sensitized microimmuneoxysome pathways result in a low-grade depression trait (neuroticism or prodrome or subclinical symptoms) or major depressive episodes in response to a variety of stressors. Future biomarker research should examine whether neuroticism and major depression share the same biomarkers, and if so, this would further indicate that neuroticism is, indeed, a forme fruste or intermediate phenotype of depression. In this respect, it is important to note that Kendler et al. (57) showed that in three different study samples, genetic risk factors are associated with MDD and neuroticism.
Limitations
This study would have been more interesting if we had also determined the cytokine and growth factor network and oxidative stress pathways. The healthy controls sample was not an unbiased sample as controls were recruited by word of mouth through friends etc. It is also a well control sample as controls were excluded for a family history of suicide, mood disorders, and substance use disorders. It could be argued that the sample size is relatively small. However, an a priori calculation of the sample size showed that a sample size of at least n = 70 is required to achieve a power of 0.80 at p = 0.05 (two-tailed). Moreover, the regressions (including the PLS analysis) of the phenome on the neuroticism and 2 other indicators revealed that, given the study sample of 133 participants (tested at alpha = 0.05 and 3), the actual power was 1.
Conclusion
Neuroticism scores are significantly higher in MDD than in controls and accounted for 64.9% of the variance in the depression phenome. Neuroticism is a much better predictor of the phenome than extraversion and agreeableness, while openness and conscientiousness do not have any significant effect. One latent vector could be extracted from neuroticism, dysthymia, lifetime anxiety disorders (trait features), and the phenome of depression (a state features assessed over the last month or week). Moreover, physical and emotional neglect and physical, emotional, and sexual abuse account for about 30% of the variance in this latent construct. PLS analysis shows that the effects of neglect on the phenome are partially mediated by neuroticism, whereas the effects of abuse were entirely mediated by neuroticism. Neuroticism and major depressive disorder are manifestations of the same latent core, which is in part caused by ACEs. Neuroticism is a less severe manifestation of major depressive disorder and the latter is a magnified manifestation of “neuroticism.” Therefore, the latter should be better described as a forme fruste of major depression, rather than a personality trait. Future research should examine whether the microimmuneoxysome biomarkers of major depression are also biomarkers of neuroticism which would reinforce the idea that neuroticism is a preclinical stage of major depression. Most important is to examine whether neuroticism is associated with the same sensitized cytokine/growth factors networks as MDD and whether reactivation of these pathways through negative life events, infections, or inflammatory stressors is associated with a transitions form neuroticism to a full blown major depressive episode. Both neuroticism and major depression are manifestations of the same latent core, whereby the former is a forme fruste of major depression, and the latter a magnified manifestation. Future biomarker research should evaluate if a general factor (or common psychopathology factor) extracted from quantitative neuroticism and lifetime and current depression and suicide scores (58), is associated with shared genetic variants or microimmuneoxysome biomarkers. If so, this would further demonstrate that neuroticism is an intermediate phenotype of depression.
Data availability statement
The dataset generated during and/or analyzed during the current study will be available from the corresponding author upon reasonable request and once the dataset has been fully exploited by the authors.
Ethics statement
The research project (#445/63) was approved by the Institutional Review Board of the Faculty of Medicine, Chulalongkorn University. All patients and participants provided their written informed consent prior to participation in the study.
Author contributions
MM and KJ: conceptualization and study design. KJ and MM: first draft writing. KJ, AV, CT, and MM: editing. KJ: recruitment of patients. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Ratchadapiseksompotch Fund, Graduate Affairs, Faculty of Medicine, Chulalongkorn University (GA64/21), a grant from the Graduate School and H. M. the King Bhumibhol Adulyadej’s 72nd Birthday Anniversary Scholarship Chulalongkorn University, and the 100th Anniversary Chulalongkorn University Fund for Doctoral Scholarship to KJ and the Sompoch Endowment Fund from the Faculty of Medicine, MDCU (RA66/016) to MM.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1158036/full#supplementary-material
References
1. Walker, ER, Mcgee, RE, and Druss, BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiat. (2015) 72:334–41. doi: 10.1001/jamapsychiatry.2014.2502
2. Katon, WJ, Lin, E, Russo, J, and Unützer, J. Increased medical costs of a population-based sample of depressed elderly patients. Arch Gen Psychiatry. (2003) 60:897–903. doi: 10.1001/archpsyc.60.9.897
3. Lim, GY, Tam, WW, Lu, Y, Ho, CS, Zhang, MW, and Ho, RC. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci Rep. (2018) 8:2861. doi: 10.1038/s41598-018-21243-x
5. Maes, M, and Almulla, AF. Research and diagnostic algorithmic rules (radar) and radar plots for the first episode of major depressive disorder: effects of childhood and recent adverse experiences on suicidal behaviors, Neurocognition and phenome features. Medrxiv. (2022) 2022:18.22283606.
6. Dube, SR, Anda, RF, Felitti, VJ, Chapman, DP, Williamson, DF, and Giles, WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the adverse childhood experiences study. JAMA. (2001) 286:3089–96. doi: 10.1001/jama.286.24.3089
7. Felitti, VJ, Anda, RF, Nordenberg, D, Williamson, DF, Spitz, AM, Edwards, V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The adverse childhood experiences (ACE) study. Am J Prev Med. (1998) 14:245–58. doi: 10.1016/S0749-3797(98)00017-8
8. Maes, MH, and Stoyanov, D. False dogmas in mood disorders research: towards a nomothetic network approach. World J Psychiatr. (2022) 12:651–67. doi: 10.5498/wjp.v12.i5.651
9. Maes, M, Congio, A, Moraes, JB, Bonifacio, KL, Barbosa, DS, Vargas, HO, et al. Early life trauma predicts affective phenomenology and the effects are partly mediated by staging coupled with lowered lipid-associated antioxidant Defences. Biomol Concepts. (2018) 9:115–30. doi: 10.1515/bmc-2018-0010
10. Maes, M, Rachayon, M, Jirakran, K, Sodsai, P, Klinchanhom, S, Debnath, M, et al. Adverse childhood experiences predict the phenome of affective disorders and these effects are mediated by staging, Neuroimmunotoxic and growth factor profiles. Cells. (2022) 11:1564. doi: 10.3390/cells11091564
11. Norman, RE, Byambaa, M, De, R, Butchart, A, Scott, J, and Vos, T. The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis. PLoS Med. (2012) 9:E1001349. doi: 10.1371/journal.pmed.1001349
12. Maes, M, Moraes, JB, Congio, A, Bonifacio, KL, Barbosa, DS, Vargas, HO, et al. Development of a novel staging model for affective disorders using partial least squares bootstrapping: effects of lipid-associated antioxidant defenses and neuro-oxidative stress. Mol Neurobiol. (2019) 56:6626–44. doi: 10.1007/s12035-019-1552-z
13. Maes, M, Moraes, JB, Bonifacio, KL, Barbosa, DS, Vargas, HO, Michelin, AP, et al. Towards a new model and classification of mood disorders based on risk resilience, neuro-affective toxicity, staging, and phenome features using the nomothetic network psychiatry approach. Metab Brain Dis. (2021) 36:509–21. doi: 10.1007/s11011-020-00656-6
14. Maes, M, Moraes, JB, Congio, A, Vargas, H, and Nunes, S. Research and diagnostic algorithmic rules (radar) for mood disorders, recurrence of illness, suicidal Behaviours, and the Patient’s lifetime trajectory. Acta Neuropsychiatrica. (2022) 3:1–15. doi: 10.1017/neu.2022.32
15. Grusnick, JM, Garacci, E, Eiler, C, Williams, JS, and Egede, LE. The association between adverse childhood experiences and personality, emotions and affect: does number and type of experiences matter? J Res Pers. (2020) 85:103908. doi: 10.1016/j.jrp.2019.103908
16. Roy, A. Childhood trauma and neuroticism as an adult: possible implication for the development of the common psychiatric disorders and suicidal behaviour. Psychol Med. (2002) 32:1471–4. doi: 10.1017/S0033291702006566
17. Ogle, CM, Rubin, DC, and Siegler, IC. Changes in neuroticism following trauma exposure. J Pers. (2014) 82:93–102. doi: 10.1111/jopy.12037
18. Costa, PT, and Mccrae, RR. The five-factor model of personality and its relevance to personality disorders. J Personal Disord. (1992) 6:343–59. doi: 10.1521/pedi.1992.6.4.343
19. Goldberg, LR. The structure of phenotypic personality traits. Am Psychol. (1993) 48:26–34. doi: 10.1037/0003-066X.48.1.26
20. Lamb, ME, Chuang, SS, Wessels, H, Broberg, AG, and Hwang, CP. Emergence and Constructvalidation of the big five factors in early childhood: a longitudinal analysis of their ontogeny in Sweden. Child Dev. (2002) 73:1517–24. doi: 10.1111/1467-8624.00487
21. Watson, D, Clark, LA, and Harkness, AR. Structures of personality and their relevance to psychopathology. J Abnorm Psychol. (1994) 103:18–31. doi: 10.1037/0021-843X.103.1.18
22. Malouff, JM, Thorsteinsson, EB, and Schutte, NS. The relationship between the five-factor model of personality and symptoms of clinical disorders: a meta-analysis. J Psychopathol Behav Assess. (2005) 27:101–14. doi: 10.1007/s10862-005-5384-y
23. Jylhä, P, and Isometsä, E. The relationship of neuroticism and extraversion to symptoms of anxiety and depression in the general population. Depress Anxiety. (2006) 23:281–9. doi: 10.1002/da.20167
24. Saklofske, DH, Kelly, IW, and Janzen, BL. Neuroticism, depression, and depression proneness. Personal Individ Differ. (1995) 18:27–31. doi: 10.1016/0191-8869(94)00128-F
25. Uliaszek, AA, Hauner, KK, Zinbarg, RE, Craske, MG, Mineka, S, Griffith, JW, et al. An examination of content overlap and disorder-specific predictions in the associations of neuroticism with anxiety and depression. J Res Pers. (2009) 43:785–94. doi: 10.1016/j.jrp.2009.05.009
26. Griffith, J, Zinbarg, R, Craske, M, Mineka, S, Rose, R, Waters, A, et al. Neuroticism as a common dimension in the internalizing disorders. Psychol Med. (2009) 40:1125–36.
27. Kotov, R, Gamez, W, Schmidt, F, and Watson, D. Linking "big" personality traits to anxiety, depressive, and substance use disorders: a meta-analysis. Psychol Bull. (2010) 136:768–821. doi: 10.1037/a0020327
28. Davis, BD. The isolation of biochemically deficient mutants of bacteria by means of penicillin. Proc Natl Acad Sci U S A. (1949) 35:1–10. doi: 10.1073/pnas.35.1.1
29. Hr, S, Callicott, J, Sommer, T, and Vs, M. From the genome to the phenome and Back: linking genes with human brain function and structure using genetically informed neuroimaging. Neuroscience. (2009) 164:1–6. doi: 10.1016/J.Neuroscience.2009.09.009. Epub 2009 Sep 12.
30. Rt, F, and Tester, M. Phenomics--technologies to relieve the phenotyping bottleneck. Trends Plant Sci. (2011) 16:635–44.
31. American Psychiatric Association, D.-T. F. Diagnostic and statistical manual of mental disorders: Dsm-5™. 5th ed. Arlington, VA: American Psychiatric Publishing, Inc (2013).
32. Kittirattanapaiboon, P, and Khamwongpin, M. The validity of the mini international neuropsychiatric interview (M.I.N.I.)-Thai version. J Mental Health Thailand. (2005) 13:126–36.
33. Hamilton, M. A rating scale for depression. J Neurol Neurosurg Psychiatry. (1960) 23:56–62. doi: 10.1136/jnnp.23.1.56
34. Beck, AT, Steer, RA, and Brown, GK. Bdi-ii, Beck depression inventory: manual. San Antonio, TX, USA: Psychological Corporation (1996).
35. Mungpanich, A. (2008). The development of the Beck depressive inventory-II (BDI-II), Thai Version. Khonkaen, Thailand.
36. Spielberger, C, Gorsuch, R, Lushene, R, Vagg, P, and Jacobs, G In:, et al.Et Al., editor. Manual for the state-trait anxiety inventory, vol. 1983. Palo Alto, CA: Consulting Psychologists Press (1983).
37. Iamsupasit, S., and Phumivuthisarn, P. (2005). A study of cognitive factors related to anxiety sensitivity. In Proceedings of the East-West Psychology Science Research Center, Bangkok, Thailand.
38. John, OP, and Srivastava, S. The big five trait taxonomy: history, measurement, and theoretical perspectives. In: Pervin LA, John OP, editors. Handbook of Personality: Theory and Research. New York, NY: Guilford Press (1999). p. 102–38.
39. Luangsurong, N. Relationship between big 5 personality traits and climate friendly product purchase intention. Bangkok, Thailand: Thammasat University (2016).
40. Rungmueanporn, L, Buathong, N, Chandarasiri, P, and Wittayasai, W. Development of the adverse childhood experiences (ace) questionnaire Thai version. Chulalongkorn Med Bull. (2019) 1:251–60.
41. Posner, K, Brown, GK, Stanley, B, Brent, DA, Yershova, KV, Oquendo, MA, et al. The Columbia–suicide severity rating scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatr. (2011) 168:1266–77. doi: 10.1176/appi.ajp.2011.10111704
42. Assanangkornchai, S, Balthip, Q, and Edwards, JG. Implementing the alcohol, smoking, substance involvement screening test and linked brief intervention service in primary care in Thailand. J Public Health (Oxf). (2014) 36:443–9. doi: 10.1093/pubmed/fdu011
43. Alberti, KG, Eckel, RH, Grundy, SM, Zimmet, PZ, Cleeman, JI, Donato, KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the international diabetes federation task force on epidemiology and prevention; National Heart, lung, and blood institute; American Heart Association; world heart federation; international atherosclerosis society; and international association for the study of obesity. Circulation. (2009) 120:1640–5. doi: 10.1161/CIRCULATIONAHA.109.192644
44. Allen, TA, Rueter, AR, Abram, SV, Brown, JS, and Deyoung, CG. Personality and neural correlates of Mentalizing ability. Eur J Personal. (2017) 31:599–613. doi: 10.1002/per.2133
45. Koorevaar, A, Hegeman, J, Lamers, F, Dhondt, A, Van Der Mast, R, Stek, M, et al. Big five personality characteristics are associated with depression subtypes and symptom dimensions of depression in older adults. Int J Geriatr Psychiatry. (2017) 32:E132–40. doi: 10.1002/gps.4670
46. Lester, D. Depression, suicidal ideation and the big five personality traits, vol. 7 (2021). #1077 p.
47. Jourdy, R, and Petot, J-M. Relationships between personality traits and depression in the light of the “big five” and their different facets. Evol Psychiatr. (2017) 82:E27–37. doi: 10.1016/j.evopsy.2017.08.002
48. Chavoshi, P. (2022). The relationship between the big-five personality traits and depressive symptoms: A meta-analysis.
49. Srivastava, S. (2016). Measuring the big five personality factors. Available at: Http://Psdlab.Uoregon.Edu/Bigfive.Html
50. Karsten, J, Penninx, BWJH, Riese, H, Ormel, J, Nolen, WA, and Hartman, CA. The state effect of depressive and anxiety disorders on big five personality traits. J Psychiatr Res. (2012) 46:644–50. doi: 10.1016/j.jpsychires.2012.01.024
51. Costa, PT, Bagby, RM, Herbst, JH, and Mccrae, RR. Personality self-reports are concurrently reliable and valid during acute depressive episodes. J Affect Disord. (2005) 89:45–55. doi: 10.1016/j.jad.2005.06.010
52. Mccrae, RR, and Costa, PT Jr. A five-factor theory of personality. Handbook of personality: Theory and research. 2nd ed. New York, NY: Guilford Press (1999).
53. Roberts, BW, Walton, KE, and Viechtbauer, W. Patterns of mean-level change in personality traits across the life course: a meta-analysis of longitudinal studies. Psychol Bull. (2006) 132:1–25. doi: 10.1037/0033-2909.132.1.1
54. Srivastava, S, John, OP, Gosling, SD, and Potter, J. Development of personality in early and middle adulthood: set like plaster or persistent change? J Pers Soc Psychol. (2003) 84:1041–53. doi: 10.1037/0022-3514.84.5.1041
55. Griens, AMGF, Jonker, K, Spinhoven, P, and Blom, MBJ. The influence of depressive state features on trait measurement. J Affect Disord. (2002) 70:95–9. doi: 10.1016/S0165-0327(00)00371-2
56. Kendler, KS, Neale, MC, Kessler, RC, Heath, AC, and Eaves, LJ. A longitudinal twin study of personality and major depression in women. Arch Gen Psychiatry. (1993) 50:853–62. doi: 10.1001/archpsyc.1993.01820230023002
57. Ks, K, Co, G, Mc, N, Aggen, S, Heath, A, Colodro-Conde, L, et al. Shared and specific genetic risk factors for lifetime major depression, depressive symptoms and neuroticism in three population-based twin samples. Psychol Med. (2019) 49:2745–53. doi: 10.1017/S003329171800377x
58. Maes, M, Jirakran, K, Vasupanrajit, A, Boonchaya-Anant, P, and Tunvirachaisakul, C. Towards a major methodological shift in depression research by assessing continuous scores of recurrence of illness, lifetime and current suicidal behaviors and phenome features: focus on Atherogenicity and adverse childhood experiences. Medrxiv. (2023):23286462. doi: 10.1101/2023.02.26.23286462
59. Chamberlain, J. M. (2023). Neurotic depression: signs, symptoms, and treatments. Available at: https://www.choosingtherapy.com/neurotic-depression/ (Accessed April 4, 2023).
60. Klerman, GL, Endicott, J, Spitzer, R, and Hirschfeld, RM. Neurotic depressions: a systematic analysis of multiple criteria and meanings. Am J Psychiatry. (1979) 136:57–61.
61. Nierenberg, AA, and Ellard, KK. Neurotic depression as the missing link: old wine with a new twist on anxiety and major depressive disorder. Epidemiol Psychiatr Sci. (2015) 24:230–2. doi: 10.1017/S2045796015000323
62. Winokur, G, Black, DW, and Nasrallah, A. Neurotic depression: a diagnosis based on preexisting characteristics. Eur Arch Psychiatry Neurol Sci. (1987) 236:343–8. doi: 10.1007/BF00377423
63. Guo, W, Yao, S, Lu, Y, Zhu, X, and Wu, D. Study on life events and social support characteristics of patients with depression. Chin J Men Health. (2003) 17:693–5.
64. Yoon, KL, Maltby, J, and Joormann, J. A pathway from neuroticism to depression: examining the role of emotion regulation. Anxiety Stress Coping. (2013) 26:558–72. doi: 10.1080/10615806.2012.734810
65. Barlow, DH, Ellard, KK, Sauer-Zavala, S, Bullis, JR, and Carl, JR. The origins of neuroticism. Perspect Psychol Sci. (2014) 9:481–96. doi: 10.1177/1745691614544528
66. Lahey, BB. Public health significance of neuroticism. Am Psychol. (2009) 64:241–56. doi: 10.1037/a0015309
67. Maes, M, Lin, A-H, Delmeire, L, Van Gastel, A, Kenis, G, De Jongh, R, et al. Elevated serum Interleukin-6 (Il-6) and Il-6 receptor concentrations in posttraumatic stress disorder following accidental man-made traumatic events. Biol Psychiatry. (1999) 45:833–9. doi: 10.1016/S0006-3223(98)00131-0
68. Maes, M, Vasupanrajit, A, Jirakran, K, Klomkliew, P, Chanchaem, P, Tunvirachaisakul, C, et al. Adverse childhood trauma and reoccurrence of illness impact the gut microbiome, which affects suicidal behaviors and the phenome of major depression: towards Enterotypic-phenotypes. Medrxiv. (2023) 2023:14.23284564
Keywords: major depression, personality, adverse childhood, biomarkers, mood disorders, neuro-immune
Citation: Jirakran K, Vasupanrajit A, Tunvirachaisakul C and Maes M (2023) The effects of adverse childhood experiences on depression and suicidal behaviors are partially mediated by neuroticism: A subclinical manifestation of major depression. Front. Psychiatry. 14:1158036. doi: 10.3389/fpsyt.2023.1158036
Edited by:
Fushun Wang, Nanjing University of Chinese Medicine, ChinaReviewed by:
Antonia New, Icahn School of Medicine at Mount Sinai, United StatesMarta Kubera, Institute of Pharmacology, Polish Academy of Sciences, Poland
Copyright © 2023 Jirakran, Vasupanrajit, Tunvirachaisakul and Maes. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chavit Tunvirachaisakul, Y2hhdml0LnRAY2h1bGEuYWMudGg=
 Ketsupar Jirakran
Ketsupar Jirakran Asara Vasupanrajit1,2
Asara Vasupanrajit1,2 Chavit Tunvirachaisakul
Chavit Tunvirachaisakul Michael Maes
Michael Maes