- 1School of Medicine, Institute of Mental Health, University of Nottingham, Nottingham, United Kingdom
- 2Division of Geriatrics and Palliative Medicine, Weill Cornell Medical College, New York City, NY, United States
- 3University of Exeter Medical School, Exeter, United Kingdom
- 4Ecog Pro Ltd, Bristol, United Kingdom
- 5Social, Genetic, and Developmental Psychiatry Centre, King’s College London, London, United Kingdom
Background: The concept of Awareness of Age-Related Changes captures people’s perceptions of the positive (AARC-gains) and negative (AARC-losses) age-related changes they experience in several life domains, including their health. We investigated the cross-sectional associations of number and type of physical and mental health conditions with AARC-gains and AARC-losses.
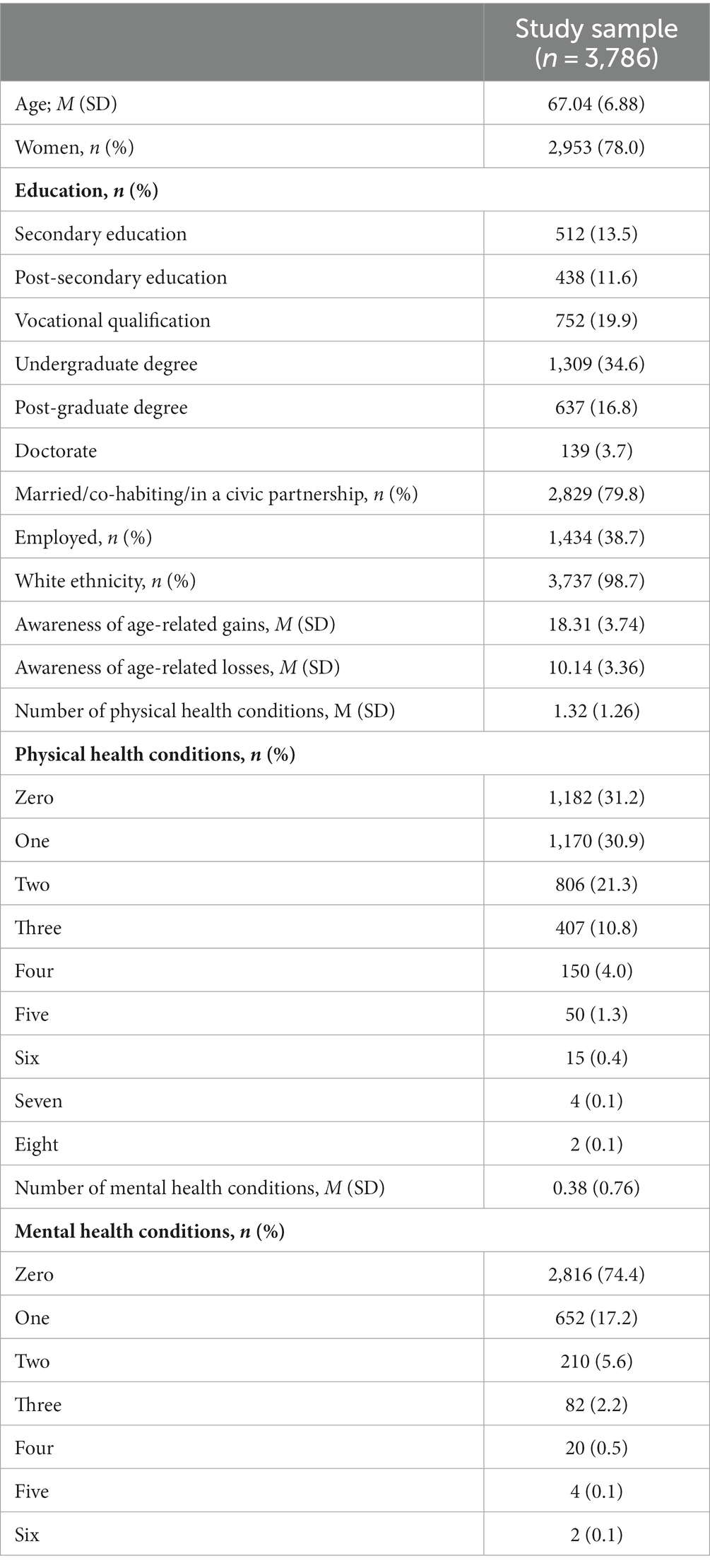
Methods: The sample comprised 3,786 middle-aged and older adults (mean age = 67.04 years; SD = 6.88) participating to the UK PROTECT study. We used hierarchical regression models to analyze whether after having included sociodemographic variables (model 1), number of physical (model 2) and of mental (model 3) health conditions explained a significant additional amount of variance in AARC-gains and AARC-losses, and whether the association between number of conditions and AARC depended on participants’ age. We used multiple regression models to analyze the associations of types of physical and mental health conditions with AARC-gains and AARC-losses.
Results: A higher number of physical health conditions was associated with higher AARC-gains and higher AARC-losses, but the association did not depend on participant age. After controlling for the number of physical health conditions, a higher number of mental health conditions was associated with higher AARC-losses but not with AARC-gains, and the association was stronger among older participants. Small effects were found between greater AARC-gains and current cancer and between greater AARC-losses and diagnoses of mild cognitive impairment, Parkinson’s disease, arthritic condition, cancer in full remission, osteoporosis, depression, anxiety disorders, and personality disorder. The remaining health conditions were either negligibly or non-statistically related to AARC-losses.
Conclusion: Middle-aged and older adults having more physical health conditions and more mental health conditions may be at higher risk of negative views on their own aging. However, specific physical health conditions, such as arthritis, and certain mental health conditions, such as depression, may make adults particularly vulnerable to negative age-related perceptions.
Introduction
Views on aging (VoA) are an important part of developmental regulation and health behavior, especially in midlife and later life. People with more positive VoA are more likely to implement adaptive strategies in the face of age-related challenges (1). These adaptive strategies often include engaging in health-promoting behaviors such as physical activity (2–7). Because of the strong connections between positive VoA and healthy behavioral regulation, more positive VoA are related to better longer-term physical and mental health (8–10). Conversely, people with more negative VoA are less engaged in health-enhancing and adaptive behaviors and are at greater risk of poorer current and future health, including increased risk of mortality (5, 11–14). The promotion of positive VoA, and the decrease of negative VoA, are therefore increasingly recognized as a useful strategy for physical and mental health promotion (15).
Theoretical models of VoA, including the theoretical model of awareness of age-related change (16, 17), posit that although people’s VoA may have an effect on their future physical and mental health, people’s health history and health status can also act as distal antecedents that shape their VoA. People with existing health conditions may have worse VoA; these more negative VoA, in turn, may threaten their positive health behavior regulation. Given the high prevalence of chronic conditions, it is necessary to consider whether people’s VoA are connected to their experiences of specific chronic conditions and multimorbidities. Recent evidence suggests that in England, about 44, 64, and 90% of people aged 40, 60, and 80 years, respectively, have one or more long-term conditions (18, 19).
Views on aging and health conditions
Much of the existing literature focuses on how VoA are associated with health behavior, such as physical activity, and longer-term self-rated health (20). Thus far, explorations of the associations between VoA and objective health markers have been limited to physical health outcomes such as biomarkers for inflammation (21) and mortality (22). This existing literature, taken alongside established theoretical models of VoA (16, 17), would suggest that various existing physical health conditions may be associated with VoA. However, less research focuses on the connections between VoA and specific physical health conditions.
Relatedly, one in four people experiences a mental health problem of some kind each year in England (23) and about 10.7% of the global population has a mental health condition (24). People with a mental health condition may be at a greater risk for experiences that may make them observe for age-related losses (25). Considering depression, for example, 20-year increase in self-reported depression was found related to more negative VoA (20). Further, a recent study compared levels of perceived age-related losses among four groups: (1) people with current and past clinical depression, (2) people with current but not past clinical depression, (3) people with past but not current clinical depression, and (4) people with neither past nor current clinical depression (26). People with both past and current clinical depression reported more negative VoA than the other groups (26).
Unfortunately, the existing scholarship on VoA and mental health conditions is largely limited to depression and anxiety. However, older adults frequently have other mental health conditions. For example, an estimated 11–15% of community-dwelling older adults have a personality disorder (27). Thus, broadening the literature on the connections between VoA and various mental health conditions is urgent.
Only a few studies have simultaneously explored how various physical and mental health conditions were differentially associated with VoA. Schönstein et al. (28) analyzed how physical and mental health conditions at baseline predicted VoA at follow-up (median of 7.7 years) in a sample of 526 German middle-aged and older adults (28). The authors analyzed the VoA constructs of subjective age (how old people feel relative to their chronological age) and attitudes toward own aging (how people self-appraise their aging). They found that, when including a range of both physical and mental health conditions in a single statistical model, back pain, hypertension, depression, anxiety, and rheumatism were most strongly related to more negative attitudes toward own aging, and rheumatism, anxiety, and cancer were most strongly related to participants feeling older than their chronological age. The use of both subjective age and attitudes toward one’s own aging are useful, but additional studies that explore other VoA constructs are necessary. Indeed, the measures used to assess VoA in Schönstein et al.’s study (28) provide a simplified assessment of people’s VoA as they position the individual on a continuum with positive VoA on one hand and negative VoA on the other hand. This is a limitation as people can have co-existing positive and negative VoA. Moreover, as compared to positive VoA, negative VoA are typically more strongly associated with health outcomes (29). Health conditions may also be differentially related to positive and negative VoA. Thus, utilizing a multi-dimensional measure of VoA would be helpful to further understand how various health conditions are associated with VoA.
The value of awareness of age-related gains and losses
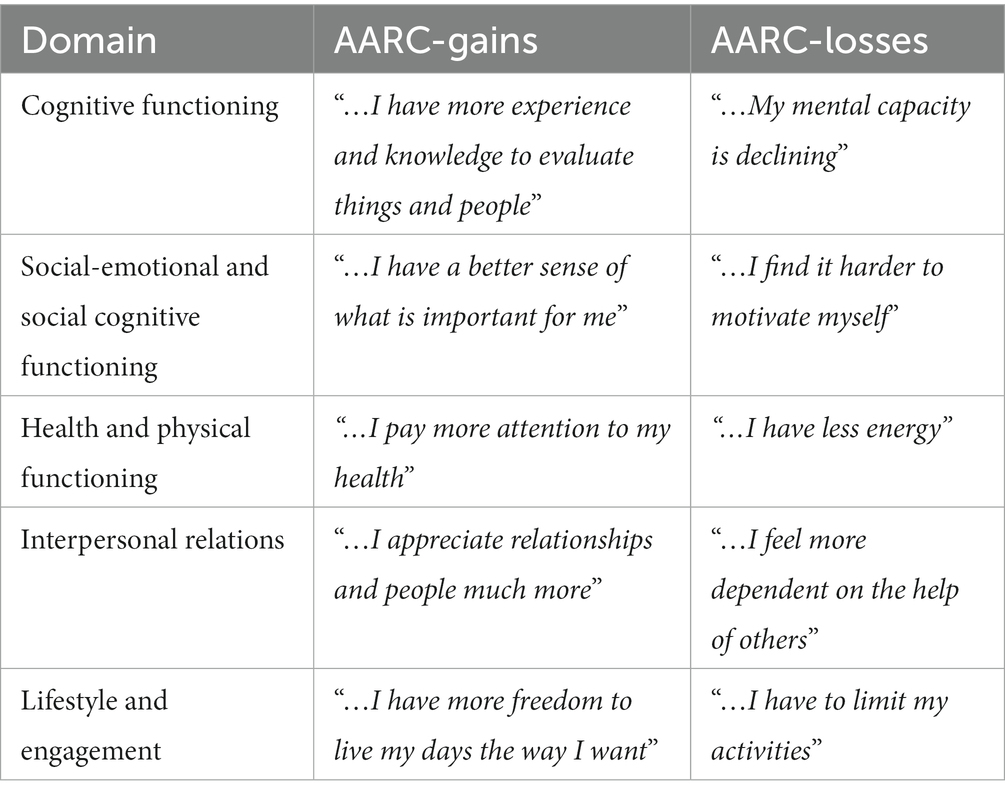
The Awareness of Age-Related Change (AARC) construct captures both the positive (AARC-gains) and negative (AARC-losses) perceptions adults have of the changes they may observe in their daily life and attribute to aging (16, 30). In line with developmental theories and evidence (31, 32), AARC assumes that experiences and perceptions of gains and losses can coexist in five life and behavioral domains: cognitive functioning, social-emotional and social-cognitive functioning, health and physical functioning, interpersonal relations, and lifestyle and engagement. Moreover, the AARC conceptual framework assumes that physical and mental health influence levels of AARC-gains and AARC-losses (16, 30). A qualitative study asked people aged 70–88 years to document on a daily basis whether they have had any positive or negative age-related experience across the AARC life domains (17). This study found that 70% of participants reported age-related experiences in their physical health and, out of these, 82.6% reported negative age-related experiences including the experience of illnesses and health conditions. Such a finding highlights how frequently people recognize age-related changes on a daily basis, and how often these changes are bound to health conditions and are thus attributed as negative.
Quantitative research has thus far mainly focused on the associations of lower AARC-gains and higher AARC-losses with poorer cross-sectional and future scores on subjective indicators of physical health, such as functional status, pain, sleep, and physical symptoms (29, 33–40), and mental health, such as depression (9, 29). Only two studies have investigated more granular associations between various types of both physical and mental health conditions and AARC-gains and AARC-losses. Dunsmore and Neupert’s (41) analysis focused on arthritis, finding that people with arthritis had higher AARC-losses, but not lower AARC-gains, compared to individuals without arthritis. Rupprecht and colleagues (42) analyzed the associations between AARC-gains and AARC-losses and six conditions that were diagnosed in the previous 2 years. However, people who have had a health condition for longer than 2 years may be those who are objectively experiencing, and consequently perceiving, more age-related changes. It is therefore important to complement the analyses conducted by Rupprecht et al. (42) through exploration of associations between health conditions and AARC, regardless of when participants received the diagnosis.
The present study
We investigated, in a large sample of people aged 50+, the cross-sectional associations between 26 types of lifetime physical and mental health conditions with AARC-gains and AARC-losses. First, informed by previous evidence suggesting that health is more closely connected to AARC-losses than AARC-gains (26, 41, 42), we hypothesized that a higher number of physical and mental health conditions would be related to higher AARC-losses but not to AARC-gains. Further, we hypothesized that the interaction between AARC-losses and health conditions would interact with age, with older participants having a stronger association between the number of health conditions and AARC-losses.
Regarding the type of health conditions, we expected stronger associations with AARC-losses for those health conditions that are more typically socially ascribed to old age (e.g., arthritis, osteoporosis, mild cognitive impairment, cardiovascular disease, and Parkinson’s disease) compared to those conditions that are less associated with old age (e.g., asthma and epilepsy). Lastly, due to ruminative thinking, we expect that those with depressive and anxiety symptoms are most likely to pay attention to, and therefore report, age-related losses, compared to people with other mental health conditions (9, 26).
Materials and methods
Study design and protocol
This study uses 2020 secondary data from the UK PROTECT cohort (Platform for Research Online to investigate Genetics and Cognition in Ageing). UK PROTECT inclusion criteria were being a UK resident, English speaker, aged 50+, having access to the internet, and lack of self-reported diagnosis of dementia at baseline (which started in 2015). During recruitment the UK PROTECT study was publicized by national advertisements that directed potential participants to the PROTECT study website where they could enroll to the study. Individuals aged 50+ from existing research cohorts (including Exeter 10,000, Join Dementia Research, and Brains for Dementia Research) were also invited to take part to the study via email. When joining the study participants provided informed consent online. UK PROTECT has ethical approval from the London Bridge NHS Research Ethics Committee and Health Research Authority (Ref: 13/LO/1578). For the scope of this study, in 2020 UK PROTECT participants were optionally invited to complete the AARC questionnaire; 5,353 participants did so. This study comprises those 3,786 participants who, in addition to completing the AARC questionnaire, also self-reported, in 2020, whether they had diagnoses of physical and mental health conditions. Descriptive statistics for those who provided data on AARC and health conditions and those who did not are in Supplementary Table S1.
Measures
Socio-demographics
Sociodemographic variables comprised age, sex, education (secondary education; post-secondary education; vocational qualifications; undergraduate degrees; post-graduate degrees; doctorates), martial status (married/co-habiting/in a civic partnership vs. never married/widowed/divorced), employment status (employed vs. not employed), and ethnicity.
Awareness of age-related change
We measured VoA by capturing participants AARC with a 10-item questionnaire [AARC-10 SF; (43)] comprising five items assessing AARC-gains and five items assessing AARC-losses. An item in each of the AARC-gains and AARC-losses subscales assesses one of the five AARC life and behavioral domains. Questionnaire items are based on the positive and negative age-related changes US and German adults aged 40+ reported noticing in their daily life during focus groups, interviews, and diaries. AARC items capture the changes adults may perceive in their lives, irrespective of whether these match objective changes.
Each item starts with the stem: “With my increasing age, I realize that….” Respondents rate how much items apply to them (1 = not at all; 2 = a little bit; 3 = moderately; 4 = quite a bit; 5 = very much).
Scores can be obtained for the AARC-gains and AARC-losses subscales by summing the five items within the respective subscales. Higher scores indicate higher AARC-gains/losses (range: 5–25). In this sample Cronbach’s alpha for internal consistency for the AARC-gains subscale was 0.74 and for the AARC-losses subscale was 0.81, indicating good scales reliability.
Physical health conditions
Participants indicated whether they received (1 = yes, 0 = no) at any point in their life a diagnosis of each of the 19 examined health conditions (reported in Table 1). Number of physical health conditions was a count of the conditions reported. Although cancer in full remission is not a current physical health condition, we kept it in the count as past history of cancer may influence VoA, our study outcome (44).
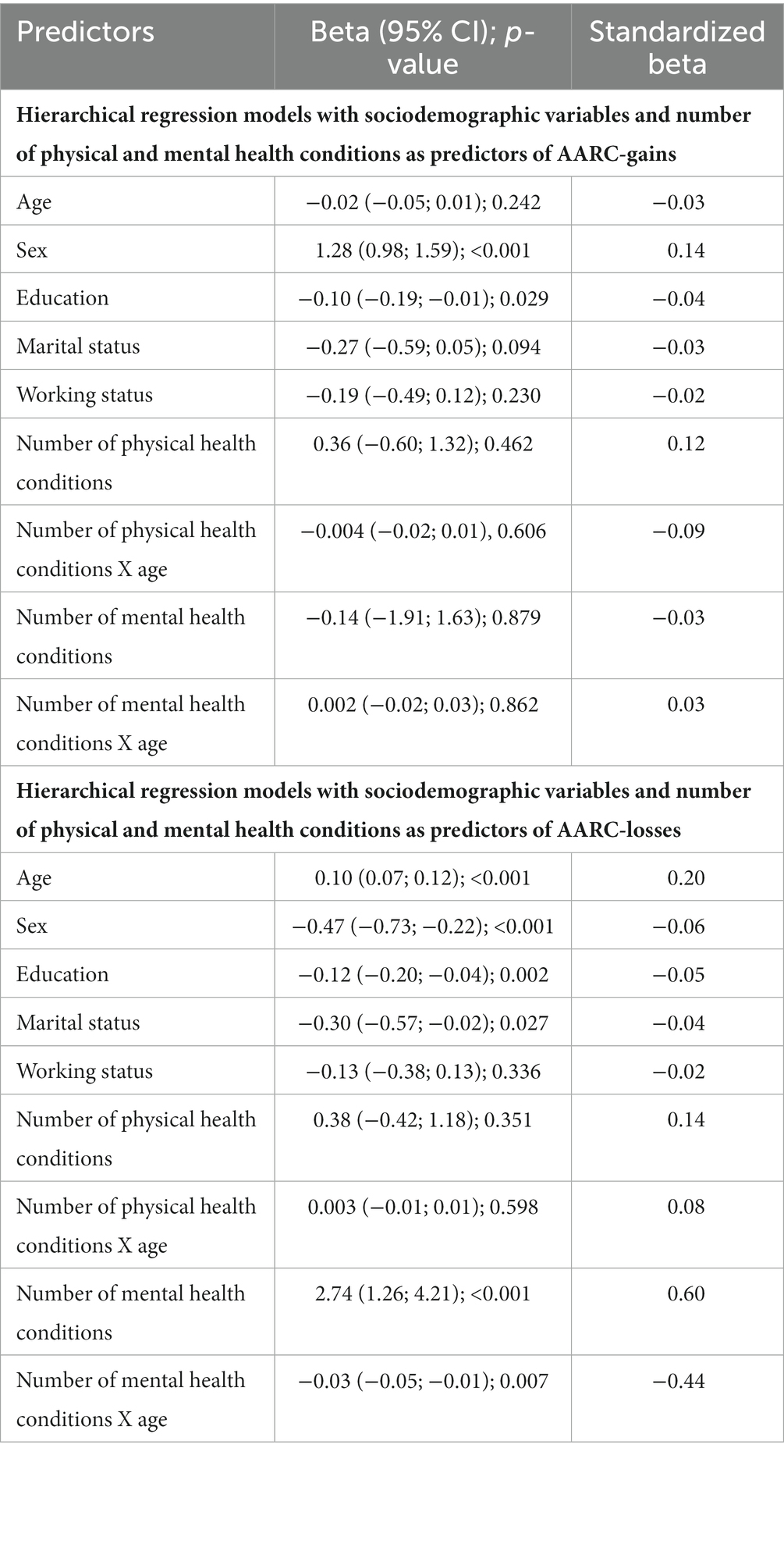
Table 1. Hierarchical regression models with sociodemographic variables, number of physical and mental health conditions, and their interactions with age as predictors of AARC-gains and AARC-losses.
Mental health conditions
Participants indicated whether they received (1 = yes; 0 = no) at any point in their life a diagnosis of each of the 7 examined mental health conditions. Number of mental health conditions was a count of the diagnoses reported.
Study analyses
We used hierarchical linear regression models to explore, at cross-sectional level, the additional explanatory value of number of physical and mental health conditions (predictor), in addition to socio-demographic variables, on AARC-gains and AARC-losses. Model 1 included only socio-demographic variables as predictors. Model 2 added number of physical health conditions as predictor. Model 3 added number of mental health conditions as predictor. We also tested a fourth model adding the interactions of number of physical and mental health conditions with age as additional predictors. We also used linear regression models to explore the cross-sectional associations of presence of each of the examined physical and mental health conditions (predictors) with AARC-gains and AARC-losses. In a further step, we used multiple hierarchical linear regression models to explore the predictive value of each physical and mental health condition on AARC-gains and AARC-losses above and beyond the effect of other conditions. To quantify the associations we reported standardized regression coefficients (β; effects sizes). Values ≤0.09 were considered negligible, 0.10–0.29 small, 0.30–0.49 moderate, and ≥0.50 large (45). We conducted all analyses using STATA version 17 (46).
Results
Descriptive statistics
The sample comprised 3,786 adults between the ages of 52 and 96 (mean age = 67.04 years, SD = 6.88 years; Table 2). The majority of the sample was women (78.0%). Educational achievements varied. The majority were married (79.8%), and the majority were not employed (61.3%). Almost all participants were of White ethnicity (98.7). Participants reported moderate age-related gains (M = 18.31; SD = 3.74) and few age-related losses (M = 10.14; SD = 3.36). 68.8% of the sample had at least one physical health condition, and 25.6% had at least one mental health condition.
Number of physical and mental health conditions
After having included age, sex, education, marital status and employment status as cross-sectional correlates of AARC-gains and AARC-losses (Model 1; Table 3), a higher number of physical health conditions was associated with higher AARC-gains and higher AARC-losses (Model 2). A higher number of mental health conditions was associated with higher AARC-losses, but not to lower AARC-gains (Model 3). After having included in the model the interactions between number of physical and mental health conditions with age, number of physical health conditions and its interaction with age, as well as number of mental health conditions and its interaction with age, were no longer significantly associated with AARC-losses. After having included in the model the interactions between physical and mental health conditions with age, number of physical health conditions and its interaction with age were also not significant predictor of AARC-gains. Higher number of mental health conditions were instead associated with higher AARC-gains, especially among those who were older (Model 4; Table 1). All models explained 3% of the variance in AARC-gains. Models 1, 2, 3, and 4 explained 8, 14, 16, and 16% of the variance in AARC-losses, respectively. The R2 changes from model 1 to model 2 and from model 2 to model 3 were significant.
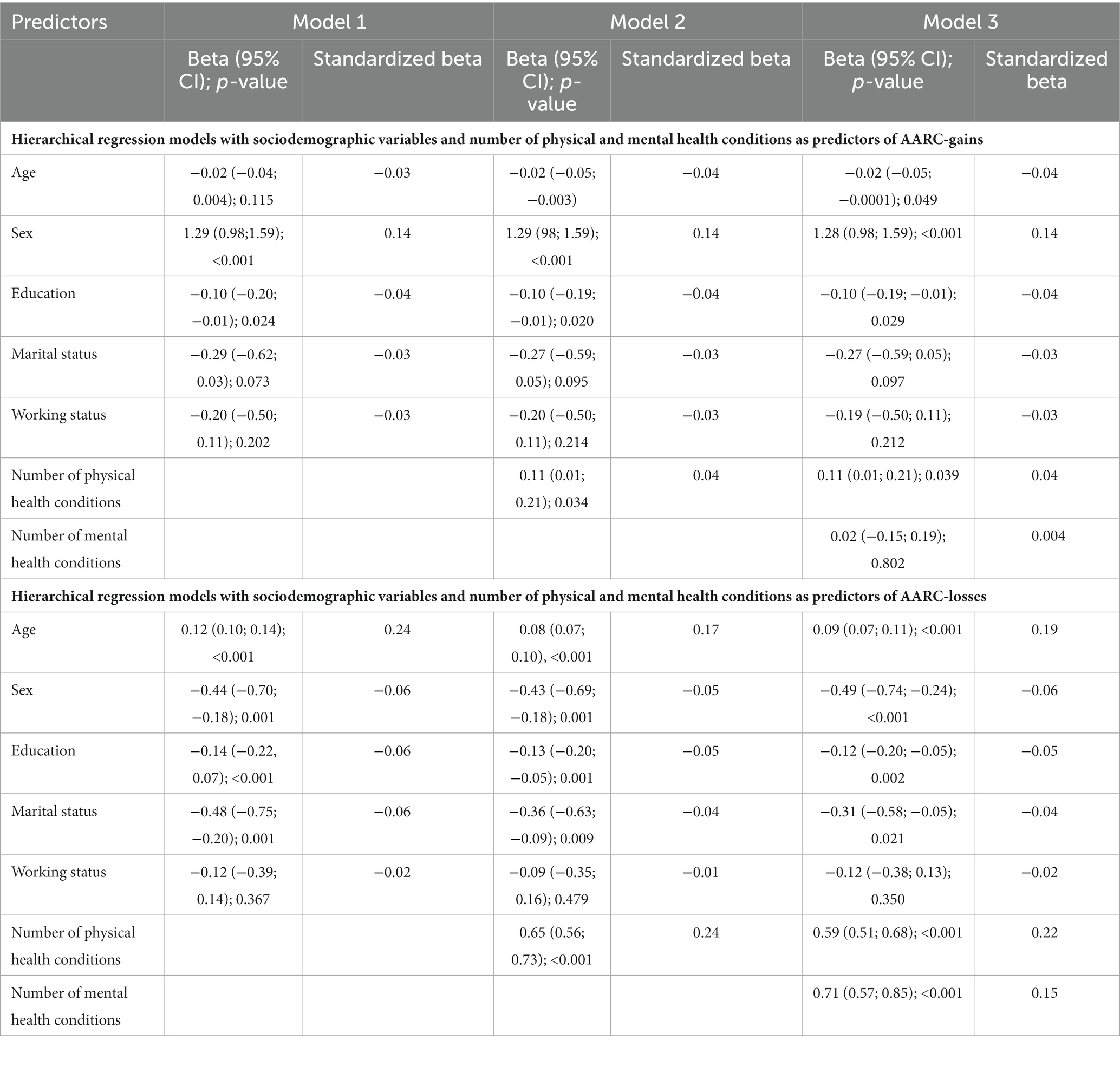
Table 3. Hierarchical regression models with sociodemographic variables and number of physical and mental health conditions as predictors of AARC-gains and AARC-losses.
Type of physical and mental health conditions
Associations for each health condition and AARC-gains and AARC-losses adjusted for sociodemographic variables are in Supplementary Table S2. Table 4 reports results from multiple regressions including all physical and mental health condition as cross-sectional predictors of AARC-gains and AARC-losses. Participants with current cancer reported higher AARC-gains. The remaining physical and mental health conditions were not related to AARC-gains. Diagnoses of mild cognitive impairment, Parkinson’s disease, arthritic condition, cancer in full remission, osteoporosis, depression, anxiety disorders, and personality disorder were associated with higher AARC-losses. Among these conditions, those most strongly related to AARC-losses were depression and arthritic condition.
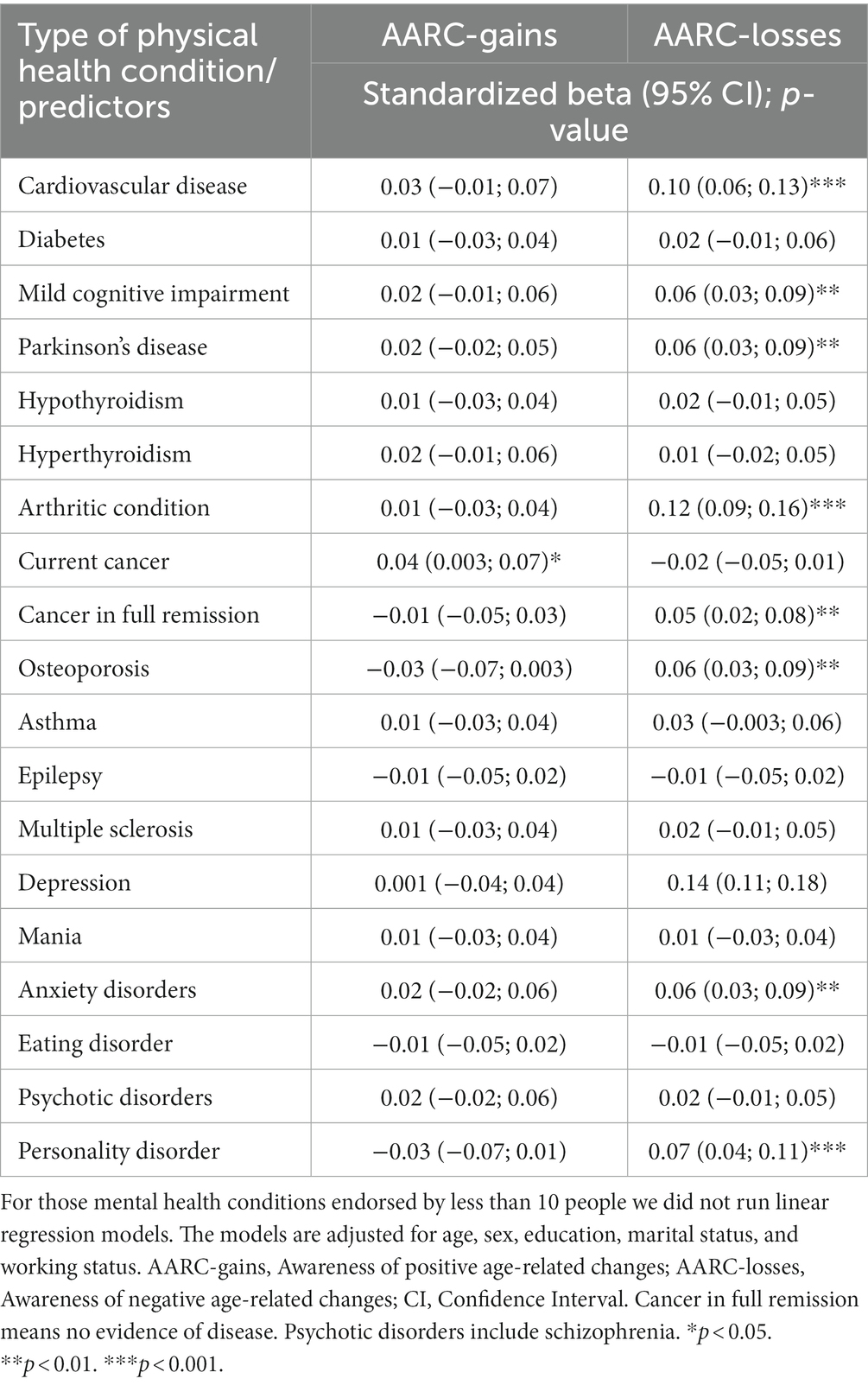
Table 4. All physical and mental health conditions included in the same multiple regression model as predictors of AARC-gains and AARC-losses.
Discussion
By analyzing connections between VoA and health conditions, researchers can identify who may be at a greater risk for poorer subjective aging experiences. Given the saliency of VoA to healthy aging processes, and the high prevalence of (multiple) health conditions among middle-aged and older adults, doing so is urgent. We therefore investigated the cross-sectional associations between number and type of physical and mental health conditions and VoA with the multi-dimensional Awareness of Age-Related Change (AARC) gains and losses construct.
Key findings
Health conditions are associated with higher losses, but no different gains
The value of the AARC construct and its associated validated measurement tools is that they allow researchers to simultaneously explore positive vs. negative VoA. Indeed, existing research suggests that positive and negative VoA are two separate constructs rather than two extremes of a single construct (47); for example, just because someone has high negative VoA does not mean that they also have low positive VoA. The AARC construct and measure were designed to simultaneously gage positive and negative VoA across five life domains. Our analysis of how various health conditions are differentially/uniquely associated with AARC-gains vs. AARC-losses provides an initial understanding of the relationship between illness and VoA. This was in line with our hypothesis. However, against our hypothesis a greater number of physical health conditions showed a small association with higher AARC-gains. Moreover, as hypothesized, a greater total number of mental health conditions greatly impacted higher AARC-losses, especially among older people, and this effect hold true the interaction between number of mental health conditions and age. However, a greater number of mental health conditions was not associated with AARC-gains.
Further, having each of the following conditions was associated with higher AARC-losses, but no different AARC-gains: mild cognitive impairment, Parkinson’s disease, arthritis, osteoporosis, cancer in remission, depression, anxiety, a psychotic disorder, and a personality disorder. These results are in line with our hypothesis and extend to additional health conditions existing scholarship which suggests that AARC-losses are more connected to health than AARC-gains (41, 42). More specifically we identified which specific conditions should be further investigated as potentially related to negative VoA in midlife and later life.
It is important to note that the small positive association between physical health conditions and AARC-gains may be a sign of positive coping with illness and resilience. However, further longitudinal investigation is warranted to explore whether AARC-gains match longer term objective gains in these groups, such as reduced functional decline and mortality, as well as whether it is related to greater resilience and positive coping.
Cancer may be unique
Current cancer was the lone health condition that was associated with AARC-gains. Having cancer at the time of the survey was associated with slightly higher AARC-gains, but no different AARC-losses. Though we are unaware of the type of cancer and the life-expectancy prognosis in this sample, cancer can be and is often perceived as a terminal diagnosis. The terminal nature of cancer contrasts with many of the other health conditions in our sample, which are mostly manageable chronic conditions. Cancer’s association with AARC-gains may be a reflection of the way the AARC measure we utilized in this study captured AARC-gains. It is plausible that AARC-gains items such as “I have a better sense of what is important for me” and “I appreciate relationships and people much more” would be endorsed more readily by someone facing a potentially terminal illness because people who sense death is closer are more likely to prioritize close, meaningful relationships than other goals (48). Overall, that cancer was associated with AARC-gains in a way that was unlike every other health condition we analyzed highlights the unique ways in which certain health conditions may differentially be related to positive vs. negative VoA.
Health conditions that more frequently occur in later life are more closely linked to age-related losses than other health conditions
We hypothesized that age would be a significant moderator for the associations between both physical and mental health conditions and AARC-losses. However, age was only a significant moderator of the association between the number of mental health conditions and AARC-losses. That is, the older a person in our sample was, the stronger the connection between more mental health conditions and AARC-losses. Age was not associated with the association between the number of physical health conditions and AARC-losses. However, many type of physical health conditions were associated with AARC-losses, suggesting it may be more about the type of physical health condition rather than the number of total conditions.
As we hypothesized, among all the physical health conditions we investigated, those related to more AARC-losses were an arthritic condition, osteoporosis, mild cognitive impairment, and Parkinson’s disease. These conditions become more frequent with increasing age (49), and may be socially ascribed to older age. Thus, they may be highly salient markers of age-related losses and therefore more connected to AARC-losses than other conditions that are not as closely aligned with older age (i.e., diabetes or asthma).
Arthritis and osteoporosis are associated with persistent pain that can impact a person’s ability to independently engage in daily tasks (50, 51) and hence be salient in one’s evaluation of age-related losses. Indeed, the associations of pain and functional limitations (29) with AARC-losses have been established (52). Pain is also highly associated with negative emotions (53), which could make someone more prone to feel more negatively about their own aging. It is important to note that in our sample multiple sclerosis, a health condition with pain symptoms, but not strongly associated with age, was not associated with either AARC-gains or AARC-losses. That pain-related conditions that are typically associated with later life (arthritis and osteoarthritis) were associated with AARC-losses but a pain-related condition that is not necessarily associated with later life (multiple sclerosis) was not could underscore the importance of a health condition being social ascribed as one that happens in later life.
In addition to depression and anxiety, personality disorders are associated with AARC
In line with existing studies depression was associated with AARC-losses (1, 9, 29). There are several possible explanations for the relationship between depression and AARC-losses. Each of these possibilities offers an avenue for future research. First, it may be that people with a history of depression are at higher risk of experiencing cognitive difficulties, which can be a direct consequence of depression (54, 55). Relatedly, depression can be a prodrome and accelerating factor for pathological cognitive decline (56). Also, depressive symptomatology can be present among those who face particularly challenging physical health conditions such as cardiovascular and cerebrovascular diseases (56, 57). Finally, people with depression may also be more prone to reflect (i.e., ruminate) over the objective age-related losses they may experience (9). For instance, generally people with negative stable global views about themselves and the word may be both more prone to depressive symptoms and to more promptly recognize the losses they experience and to repetitively think over them without taking action (58–60).
Although there is a plethora of literature linking personality to VoA (61), our study found for the first time that more AARC-losses are related to personality disorders. This may be due to the more restricted social life that individuals with personality disorders typically have (62–66). Poorer social engagement and social support are indeed related to more negative VoA (67–74). The number of participants in our sample with a personality disorder was very small (n = 11), therefore this finding should be taken as suggestive. Nonetheless, it encourages the exploration of other mental health conditions beyond depression and anxiety as correlates of VoA. Extending this existing scholarship to study personality disorders would be valuable.
Limitations
This study has important limitations. First, though establishing cross-sectional associations between AARC and physical and mental health conditions was an important first step, analyzing these associations longitudinally is necessary. Only cross-sectional data were available to us at the time of analysis. However, the ongoing nature of the UK PROTECT study will make it possible to explore this in future studies. Second, participants did not report how long they had each diagnosis, when they were diagnosed, or severity of conditions. Therefore, we were unable to fully compare health conditions that were long-standing (or even life-long) to those that were more recently diagnosed. Further, though most of the health conditions we analyzed are chronic conditions that, once diagnosed, people have to manage their entire lives, some conditions may be cured or reversed (e.g., diabetes). As such, participants may have had some conditions in the past but not at the time of the survey. Because health conditions can contribute to cumulative health disadvantages over a lifetime, it will be important for future research to consider the duration of each diagnosis. Severity of the health conditions should also be considered as a variable that may moderate associations between AARC and health conditions.
Third, for some of the investigated conditions the number of participants reporting the given condition was very low. In some instances, small sample size impeded our ability to estimate an association; in other cases, we computed the estimation but results should be taken as suggestive. Fourth, participants were excluded from study analyses based on self-reported diagnosis of dementia. This is a limitation compared to the use of objective indicators such as doctor-reported diagnosis of dementia. Fifth, though we controlled for gender in our analyses, our sample was mostly comprised of women. A sample with greater gender diversity would allow for more robust gender comparisons given that gender plays a role in VoA (75) and that certain health conditions are more common in older women than men (e.g., osteoporosis) (76). Nonetheless this study included a variety of health conditions and an age-diverse sample. Moreover, it provides initial evidence for the ways in which specific health conditions are connected to AARC, and should encourage future research on specific health conditions.
Conclusion
A higher number of physical and mental health illnesses are associated with higher levels of awareness of age-related losses. Specific health conditions, such as arthritis, depression, and personality disorder may be related to greater vulnerability to negative age-related experiences. These individuals could benefit from some sort of intervention that helps them accept and/or adjust to health-related losses.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by The UK PROTECT study, from which data was used, has ethical approval from the London Bridge NHS Research Ethics Committee and Health Research Authority (Ref: 13/LO/1578). The patients/participants provided their written informed consent to participate in this study.
Author contributions
SS and ST equally designed the Current study, wrote the manuscript, developed the research questions, and drafted the manuscript. SS conducted study analyses. HB, CB, AC, and AH contributed to collection and acquisition of UK PROTECT data and provided feedback and assistance with editing of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
SS was supported by an ESRC (Economic and Social Research Council) Postdoctoral fellowship (Grant Ref: ES/X007766/1). ST was supported by the United States National Institute on Aging via a T32 postdoctoral fellowship (T32 AG049666).
Acknowledgments
This paper represents independent research coordinated by the University of Exeter and King’s College London and is funded in part by the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London. This research was also supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care South West Peninsula and the National Institute for Health Research (NIHR) Exeter Clinical Research Facility. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Conflict of interest
HB is the funder/head of Ecog Pro Ltd.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1152177/full#supplementary-material
References
1. Dutt, AJ, Gabrian, M, and Wahl, H-W. Awareness of age-related change and depressive symptoms in middle and late adulthood: longitudinal associations and the role of self-regulation and calendar age. J Gerontol B Psychol Sci Soc Sci. (2016) 73:gbw095–53. doi: 10.1093/geronb/gbw095
2. Levy, BR, and Myers, LM. Preventive health behaviors influenced by self-perceptions of aging. Prev Med. (2004) 39:625–9. doi: 10.1016/j.ypmed.2004.02.029
3. Wurm, S, Tomasik, MJ, and Tesch-Römer, C. On the importance of a positive view on ageing for physical exercise among middle-aged and older adults: cross-sectional and longitudinal findings. Psychol Health. (2010) 25:25–42. doi: 10.1080/08870440802311314
4. Beyer, AK, Wolff, JK, Warner, LM, Schuz, B, and Wurm, S. The role of physical activity in the relationship between self-perceptions of ageing and self-rated health in older adults. Psychol Health. (2015) 30:671–85. doi: 10.1080/08870446.2015.1014370
5. Wurm, S, Warner, LM, Ziegelmann, JP, Wolff, JK, and Schuz, B. How do negative self-perceptions of aging become a self-fulfilling prophecy? Psychol Aging. (2013) 28:1088–97. doi: 10.1037/a0032845
6. Beyer, A-K, Wiest, M, and Wurm, S. There is still time to be active: self-perceptions of aging, physical activity, and the role of perceived residual lifetime among older adults. J Aging Phys Act. (2019) 27:807–15. doi: 10.1123/japa.2018-0380
7. Hooker, K, Mejía, ST, Phibbs, S, Tan, EJ, and Stevens, J. Effects of age discrimination on self-perceptions of aging and cancer risk behaviors. The Gerontologist. (2019) 59:S28–37. doi: 10.1093/geront/gny183
8. Brothers, AF, Kornadt, AE, Nehrkorn-Bailey, A, Wahl, H-W, and Diehl, MK. The effects of age stereotypes on physical and mental health are mediated by self-perceptions of aging. J Gerontol B Psychol Sci Soc Sci. (2020) 76:845–57. doi: 10.1093/geronb/gbaa176
9. Dutt, AJ, Wahl, H-W, and Rupprecht, F. Mindful vs. mind full: processing strategies moderate the association between subjective aging experiences and depressive symptoms. Psychol Aging. (2018) 33:630–42. doi: 10.1037/pag0000245
10. Seidler, AL, and Wolff, JK. Bidirectional associations between self-perceptions of aging and processing speed across 3 years. J Gerontopsychol Geriatr Psychiatry. (2017) 30:49–59. doi: 10.1024/1662-9647/a000165
11. Kaspar, R, Wahl, H-W, and Diehl, MK. Awareness of age-related change as a behavioral determinant of survival time in very old age. Front Psychol. (2021) 12:727560. doi: 10.3389/fpsyg.2021.727560
12. Robertson, DA, Savva, GM, King-Kallimanis, BL, and Kenny, RA. Negative perceptions of aging and decline in walking speed: a self-fulfilling prophecy. PLoS One. (2015) 10:e0123260. doi: 10.1371/journal.pone.0123260
13. Stephan, Y, Sutin, AR, Luchetti, M, and Terracciano, A. Feeling older and the development of cognitive impairment and dementia. J Gerontol B Psychol Sci Soc Sci. (2017) 72:966–73. doi: 10.1093/geronb/gbw085
14. Stephan, Y, Sutin, AR, and Luchetti, M. Terracciano a. the prospective relationship between subjective aging and inflammation: evidence from the health and retirement study. Psychophysiology. (2022) 60:e14177. doi: 10.1111/psyp.14177
15. Knight, RL, Chalabaev, A, McNarry, MA, Mackintosh, KA, and Hudson, J. Do age stereotype-based interventions affect health-related outcomes in older adults? A systematic review and future directions. Br J Health Psychol. (2021) 27:338–73. doi: 10.1111/bjhp.12548
16. Diehl, MK, and Wahl, H-W. Awareness of age-related change: examination of a (mostly) unexplored concept. J Gerontol B Psychol Sci Soc Sci. (2010) 65B:340–50. doi: 10.1093/geronb/gbp110
17. Miche, M, Wahl, H-W, Diehl, MK, Oswald, F, Kaspar, R, and Kolb, M. Natural occurrence of subjective aging experiences in community-dwelling older adults. J Gerontol B Psychol Sci Soc Sci. (2014) 69:174–87. doi: 10.1093/geronb/gbs164
18. Public Health England. Chapter 1: population change and trends in life expectancy. (2018). Available at: https://www.gov.uk/government/publications/health-profile-for-england-2018/chapter-1-population-change-and-trends-in-life-expectancy.
19. AgeUK. Briefing: Health and Care of Older People in England 2019. (2019). Available at: https://www.ageuk.org.uk/globalassets/age-uk/documents/reports-and-publications/reports-and-briefings/health--wellbeing/age_uk_briefing_state_of_health_and_care_of_older_people_july2019.pdf
20. Sabatini, S, Siebert, JS, Diehl, MK, Brothers, A, and Wahl, H-W. Identifying predictors of self-perceptions of aging based on a range of cognitive, physical, and mental health indicators: twenty-year longitudinal findings from the ILSE study. Psychol Aging. (2022) 37:486–502. doi: 10.1037/pag0000668
21. Stephan, Y, Sutin, AR, and Terracciano, A. Younger subjective age is associated with lower C-reactive protein among older adults. Brain Behav Immun. (2015) 43:33–6. doi: 10.1016/j.bbi.2014.07.019
22. Stephan, Y, Sutin, AR, and Terracciano, A. Subjective age and mortality in three longitudinal samples. Psychosom Med. (2018) 80:659–64. doi: 10.1097/PSY.0000000000000613
23. Mental Health Foundation. Available at: https://www.mentalhealth.org.uk/statistics/mental-health-statistics-older-people (Accessed June 30, 2023).
24. Our world in data. (2023) Available at: https://ourworldindata.org/mental-health (Accessed June 30, 2023).
25. Zisook, S, Lesser, I, Stewart, JW, Wisniewski, SR, Balasubramani, GK, Fava, M, et al. Effect of age at onset on the course of major depressive disorder. Am J Psychiatr. (2007) 164:1539–46. doi: 10.1176/appi.ajp.2007.06101757
26. Sabatini, S, Dritschel, B, Rupprecht, FS, Ukoumunne, OC, Ballard, C, Brooker, H, et al. Rumination moderates the longitudinal associations of awareness of age-related change with depressive and anxiety symptoms. Aging Ment Health. (2023) 1-9:1–9. doi: 10.1080/13607863.2023.2176820
27. Penders, KAP, Peeters, IGP, Metsemakers, JFM, and van Alphen, SPJ. Personality disorders in older adults: a review of epidemiology, assessment, and treatment. Curr Psychiatry Rep. (2020) 22:14. doi: 10.1007/s11920-020-1133-x
28. Schönstein, A, Dallmeier, D, Denkinger, M, Rothenbacher, D, Klenk, J, Bahrmann, A, et al. Health and subjective views on aging: longitudinal findings from the ActiFE Ulm study. J Gerontol Ser B. (2021) 76:1349–59. doi: 10.1093/geronb/gbab023
29. Sabatini, S, Silarova, B, Martyr, A, Collins, R, Ballard, C, Anstey, KJ, et al. Associations of awareness of age-related change with emotional and physical well-being: a systematic review and meta-analysis. The Gerontologist. (2020) 60:e477–90. doi: 10.1093/geront/gnz101
30. Diehl, MK, Wahl, H-W, Barrett, AE, Brothers, AF, Miche, M, Montepare, JM, et al. Awareness of aging: theoretical considerations on an emerging concept. Dev Rev. (2014) 34:93–113. doi: 10.1016/j.dr.2014.01.001
31. Baltes, PB. Theoretical propositions of life-span developmental psychology: on the dynamics between growth and decline. Dev Psychol. (1987) 23:611–26. doi: 10.1037/0012-1649.23.5.611
32. Heckhausen, J, Dixon, RA, and Baltes, PB. Gains and losses in development throughout adulthood as perceived by different adult age groups. Dev Psychol. (1989) 25:109–21. doi: 10.1037/0012-1649.25.1.109
33. Sabatini, S, Ukoumunne, OC, Ballard, C, Brothers, AF, Kaspar, R, Collins, R, et al. International relevance of two measures of awareness of age-related change (AARC). BMC Geriatr. (2020) 20:359. doi: 10.1186/s12877-020-01767-6
34. Neri, AL, Wahl, H-W, Kaspar, R, Diehl, MK, Batistoni, SST, Cachioni, M, et al. Psychometric study of the awareness of age-related change (AARC) short scale translated to Portuguese, applied to Brazilian older adults. Demen Neuropsychol. (2021) 15:230–8. doi: 10.1590/1980-57642021dn15-020011
35. Sabatini, S, Ukoumunne, OC, Brothers, A, Diehl, MK, Wahl, H-W, Ballard, C, et al. Differences in awareness of positive and negative age-related changes accounting for variability in health outcomes. Eur J Ageing. (2022) 19:1087–97. doi: 10.1007/s10433-021-00673-z
36. Wilton-Harding, B, and Windsor, TD. Awareness of age-related change, future time perspective, and implications for goal adjustment in older adulthood. Aging Ment Health. (2021) 26:1189–97. doi: 10.1080/13607863.2021.1893269
37. Sabatini, S, Ukoumunne, OC, Ballard, C, Collins, R, Corbett, A, Brooker, H, et al. Cross-sectional and longitudinal associations between subjective sleep difficulties and self-perceptions of aging. Behav Sleep Med. (2021) 20:732–61. doi: 10.1080/15402002.2021.1994405
38. Zhu, X, and Neupert, SD. Dynamic awareness of age-related losses predict concurrent and subsequent changes in daily inductive reasoning performance. Br J Dev Psychol. (2020) 39:282–98. doi: 10.1111/bjdp.12344
39. Sabatini, S, Ukoumunne, OC, Ballard, C, Collins, R, Anstey, KJ, Diehl, MK, et al. Cross-sectional association between objective cognitive performance and perceived age-related gains and losses in cognition. Int Psychogeriatr. (2021) 33:727–41. doi: 10.1017/S1041610221000375
40. Zhang, S, and Neupert, SD. Awareness of aging mediates the relationship between health and control beliefs: a micro-longitudinal study. Innov Aging. (2020) 4:448. doi: 10.1093/geroni/igaa057.1449
41. Dunsmore, VJ, and Neupert, SD. No pain, no gain? Personality associations with awareness of aging depend on arthritis. Front Psychol. (2022) 13:863152. doi: 10.3389/fpsyg.2022.863152
42. Rupprecht, FS, Sabatini, S, Diehl, MK, Gerstorf, D, Kaspar, R, Schilling, OK, et al. Awareness of age-related change in the context of major life events. Frontiers. Psychiatry. (2022) 13:13. doi: 10.3389/fpsyt.2022.954048
43. Kaspar, R, Gabrian, M, Brothers, AF, Wahl, H-W, and Diehl, MK. Measuring awareness of age-related change: development of a 10-item short form for use in large-scale surveys. The Gerontologist. (2019) 59:e130–40. doi: 10.1093/geront/gnx213
44. Laryionava, K, Schönstein, A, Heußner, P, Hiddemann, W, Winkler, EC, and Wahl, H-W. Experience of time and subjective age when facing a limited lifetime: the case of older adults with advanced cancer. J Aging Health. (2022) 34:736–49. doi: 10.1177/08982643211063162
45. Cohen, J. Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Lawrence Earlbaum Associates (1988).
47. Turner, SG, Hooker, K, and Geldhof, GJ. Self-perceptions of aging: factorial structure and invariance by gender. The Gerontologist. (2020) 61:425–9. doi: 10.1093/geront/gnaa059
48. Carstensen, LL, and Hershfield, HE. Beyond stereotypes: using socioemotional selectivity theory to improve messaging to older adults. Curr Dir Psychol Sci. (2021) 30:327–34. doi: 10.1177/09637214211011468
49. Centers for Disease Control and Prevention https://www.cdc.gov/chronicdisease/data/surveillance.htm (Accessed June 30, 2023).
50. Ahlstrand, I, Björk, M, Thyberg, I, Börsbo, B, and Falkmer, T. Pain and daily activities in rheumatoid arthritis. Disabil Rehabil. (2012) 34:1245–53. doi: 10.3109/09638288.2011.638034
51. Hunter, DJ, and Riordan, EA. The impact of arthritis on pain and quality of life: an a ustralian survey. Int J Rheum Dis. (2014) 17:149–55. doi: 10.1111/1756-185X.12232
52. Sabatini, S, Ukoumunne, OC, Ballard, C, Collins, R, Corbett, A, Brooker, H, et al. The cross-sectional relationship between pain and awareness of age-related changes. Br J Pain. (2020) 15:335–44. doi: 10.1177/2049463720961798
53. Lerman, SF, Rudich, Z, Brill, S, Shalev, H, and Shahar, G. Longitudinal associations between depression, anxiety, pain, and pain-related disability in chronic pain patients. Psychosom Med. (2015) 77:333–41. doi: 10.1097/PSY.0000000000000158
54. Bunce, D, Batterham, PJ, Christensen, H, and Mackinnon, AJ. Causal associations between depression symptoms and cognition in a community-based cohort of older adults. Am J Geriatr Psychiatry. (2014) 22:1583–91. doi: 10.1016/j.jagp.2014.01.004
55. Bhalla, RK, Butters, MA, Becker, JT, Houck, PR, Snitz, BE, Lopez, OL, et al. Patterns of mild cognitive impairment after treatment of depression in the elderly. Am J Geriatr Psychiatry. (2009) 17:308–16. doi: 10.1097/JGP.0b013e318190b8d8
56. Piras, F, Banaj, N, Porcari, DE, and Spalletta, G. Later life depression as risk factor for developing dementia: epidemiological evidence, predictive models, preventive strategies and future trends. Minerva Med. (2021) 112:456–66. doi: 10.23736/S0026-4806.21.07571-6
57. Kales, HC, Maixner, DF, and Mellow, AM. Cerebrovascular disease and late-life depression. Am J Geriatr Psychiatry. (2005) 13:88–98. doi: 10.1097/00019442-200502000-00002
58. Beck, AT. Cognitive models of depression In: RL Leathy and ET Dowd, editors. Clinical advances in cognitive psychotherapy: Theory and application, vol. 14. New York: Springer Publishing Co (2002). 29–61.
59. Williams, M, Watts, FN, MacLeod, C, and Mathews, A. Cognitive psychology and emotional disorders. Chichester: John Wiley & Sons (1988).
60. Abramson, LY, Alloy, LB, Hankin, BL, Haeffel, GJ, MacCoon, DG, and Gibb, BE. Cognitive vulnerability-stress models of depression in a self-regulatory and psychobiological context In: Handbook of depression. New York: Guilford Press (2002). 268–94.
61. Kornadt, AE, Siebert, JS, and Wahl, H-W. The interplay of personality and attitudes toward own aging across two decades of later life. PLoS One. (2019) 14:e0223622. doi: 10.1371/journal.pone.0223622
62. Melle, I, Friis, S, Hauff, E, and Vaglum, P. Social functioning of patients with schizophrenia in high-income welfare societies. Psychiatr Serv. (2000) 51:223–8. doi: 10.1176/appi.ps.51.2.223
63. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®). Washington, DC: American Psychiatric Association (2013).
64. Haslam, N, Reichert, T, and Fiske, AP. Aberrant social relations in the personality disorders. Psychol Psychother Theory Res Pract. (2002) 75:19–31. doi: 10.1348/147608302169526
65. Orsmond, GI, Krauss, MW, and Seltzer, MM. Peer relationships and social and recreational activities among adolescents and adults with autism. J Autism Dev Disord. (2004) 34:245–56. doi: 10.1023/B:JADD.0000029547.96610.df
66. Ronchi, L, Banerjee, R, and Lecce, S. Theory of mind and peer relationships: the role of social anxiety. Soc Dev. (2020) 29:478–93. doi: 10.1111/sode.12417
67. O’Brien, EL, and Sharifian, N. Managing expectations: how stress, social support, and aging attitudes affect awareness of age-related changes. J Soc Pers Relat. (2019) 37:986–1007. doi: 10.1177/0265407519883009
68. Robertson, DA, and Kenny, RA. “I'm too old for that”—the association between negative perceptions of aging and disengagement in later life. Personal Individ Differ. (2016) 100:114–9. doi: 10.1016/j.paid.2016.03.096
69. Schwartz, E, Ayalon, L, and Huxhold, O. Exploring the reciprocal associations of perceptions of aging and social involvement. J Gerontol Ser B. (2021) 76:563–73. doi: 10.1093/geronb/gbaa008
70. Montepare, JM. An exploration of subjective age, actual age, age awareness, and engagement in everyday behaviors. Eur J Ageing. (2020) 17:299–307. doi: 10.1007/s10433-019-00534-w
71. Bodner, E. The importance of self-perceptions of aging in predicting late-life loneliness. Int Psychogeriatr. (2022) 34:609–12. doi: 10.1017/S1041610221002830
72. Hu, RX, and Li, LW. Social disconnectedness and loneliness: do self-perceptions of aging play a role? J Gerontol Ser B. (2022) 77:936–45. doi: 10.1093/geronb/gbac008
73. Lin, Y, Zhang, B, and Ma, Y. How do aging self-stereotypes relate to social isolation in older adults? The intervening roles of sense of coherence and cellphone use. Psychol Rep. (2022) 00332941221135483:003329412211354. doi: 10.1177/00332941221135483
74. Moieni, M, Seeman, TE, Robles, TF, Lieberman, MD, Okimoto, S, Lengacher, C, et al. Generativity and social well-being in older women: expectations regarding aging matter. J Gerontol Ser B. (2021) 76:289–94. doi: 10.1093/geronb/gbaa022
75. Sabatini, S, Ukoumunne, OC, Ballard, C, Collins, R, Kim, S, Corbett, A, et al. What does feeling younger or older than one’s chronological age mean to men and women? Qualitative and quantitative findings from the PROTECT study. Psychol Health. (2021) 38:324–47. doi: 10.1080/08870446.2021.1960989
Keywords: views on aging, subjective aging, mental illnesses, diagnosis, chronic health conditions
Citation: Sabatini S, Turner S, Brooker H, Ballard C, Corbett A and Hampshire A (2023) Physical and mental health conditions account for variability in awareness of age-related changes. Front. Psychiatry 14:1152177. doi: 10.3389/fpsyt.2023.1152177
Edited by:
Christina Röcke, University of Zurich, SwitzerlandReviewed by:
Federica Piras, Santa Lucia Foundation (IRCCS), ItalyAnson Kai Chun Chau, The Chinese University of Hong Kong, China
Maria Donata Orfei, IMT School for Advanced Studies Lucca, Italy
Copyright © 2023 Sabatini, Turner, Brooker, Ballard, Corbett and Hampshire. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Serena Sabatini, c2VyZW5hLnNhYmF0aW5pQG5vdHRpbmdoYW0uYWMudWs=
†These authors share first authorship
 Serena Sabatini
Serena Sabatini Shelbie Turner
Shelbie Turner Helen Brooker
Helen Brooker Clive Ballard
Clive Ballard Anne Corbett3
Anne Corbett3 Adam Hampshire
Adam Hampshire