- 1Department of Military Psychology, Faculty of Medical Psychology, Army Medical University (Third Military Medical University), Chongqing, China
- 2Department of Psychiatry, Second Affiliated Hospital, Army Medical University (Third Military Medical University), Chongqing, China
- 3Medical Psychology Department, No. 984 Hospital of PLA, Beijing, China
- 4General Hospital of Xinjiang Military Region, Wulumuqi, China
- 5The 33rd Company of the 11th Battalion, College of Command and Control Engineering, Army Engineering University of PLA, Nanjing, China
- 6Faculty of Medical Psychology, Army Medical University (Third Military Medical University), Chongqing, China
Introduction: This study aimed to explore potential risk factors for mental health concerns, and the prediction model for mental health concerns in Chinese soldiers was constructed through combined eligible risk factors.
Methods: This cross-sectional study was performed on soldiers under direct command from Gansu, Sichuan, and Chongqing in China, and the soldiers were selected by cluster convenient sampling from 16 October 2018 to 10 December 2018. The Symptom Checklist-90 (SCL-90) and three questionnaires (Military Mental Health Status Questionnaire, Military Mental Health Ability Questionnaire, and Mental Quality Questionnaire for Army Men) were administered, including demographics, military careers, and 18 factors.
Results: Of 1,430 Chinese soldiers, 162 soldiers presented mental disorders, with a prevalence of 11.33%. A total of five risk factors were identified, including serving place (Sichuan vs. Gansu: OR, 1.846, 95% CI: 1.028–3.315, P = 0.038; Chongqing vs. Gansu: OR, 3.129, 95% CI, 1.669–5.869, P = 0.003), psychosis (OR, 1.491, 95% CI, 1.152–1.928, P = 0.002), depression (OR, 1.482, 95% CI, 1.349–1.629, P < 0.001), sleep problems (OR, 1.235, 95% CI, 1.162–1.311, P < 0.001), and frustration (OR, 1.050, 95% CI, 1.015–1.087, P = 0.005). The area under the ROC curve by combining these factors was 0.930 (95% CI: 0.907–0.952) for predicting mental disorders in Chinese soldiers.
Conclusion: The findings of this study demonstrate that mental disorders and onset in Chinese soldiers can be predicted on the basis of these three questionnaires, and the predictive value of the combined model was high.
Introduction
Mental health concerns are the most prevalent health problems among the adult population, comprising intellectual, spiritual, and emotional health (1). The World Psychiatric Association addressed four mental health standards, including physical and mental coordination, adaptation to the social environment, wellbeing, and use of one's full range of abilities at work (2). Seven mental disorders contribute to the top 25 causes of disability worldwide, including major depressive disorder ranked #2 and anxiety disorder ranked #9 (3). Studies have reported that the prevalence of mental disorders ranged from 9.6 to 27.8% in the adult population across countries (4, 5), while the prevalence of depressive symptoms in Chinese soldiers was 25.20% (6). The deleterious consequences of these illnesses affect quality of life. Therefore, intervention and prevention strategies should be explored based on the risk factors for the early onset of mental disorders, reducing adverse outcomes related to these illnesses.
Risk factors for the onset of mental disorders have already been identified, including excessive pressure or harsh working environments, and most studies focus on the general population (7–11). Several studies have identified risk factors for mental disorders in military personnel and veterans across countries, and the risk factors in German soldiers included alcohol-use disorders and anxiety disorders (12); the risk factor in American active-duty Navy and Marine Corps soldiers was the gender of woman (13); the risk factors in Chinese military personnel included childhood foster care, the gender of woman, stressful life events, younger age, and being divorced/widowed (14); and the risk factor in American service members deployed to Iraq and Afghanistan was FKBP5 (15). Several studies have illustrated the risk factors for mental disorders among Chinese soldiers, and they point out that age, gender, education, residence, military service, social support, and headache, abdomen ache, diarrhea, or training injury during the training course could affect the progression of mental disorders (6, 16, 17). Soldiers face substantial challenges due to their rapid transition from civilian status to training for combat (18). Moreover, military tasks typically present high intensity. Soldiers must train under extreme and harsh conditions, including cold and heat stress and high altitude (19–21). Furthermore, disturbed routines and latent danger can induce intense pressure on soldiers, damaging sleep patterns and promoting subsequent mental disorders (22). It is essential to construct a prediction model for depression in Chinese soldiers, as it has not been developed for clinical practice. The current study was performed to construct a prediction model to identify soldiers at high risk for mental disorders.
Materials and methods
Subjects
This study design was cross-sectional, and cluster convenience sampling was applied. A sample of 1,430 Chinese soldiers was recruited by direct command from Gansu, Sichuan, and Chongqing. The Medical Ethics Committee of the Third Military Medical University approved this study. All soldiers provided informed consent to participate after being informed of the purpose of the study. Our study was carried out following the Declaration of Helsinki. The recruited individuals met the following criteria: (1) residence in Gansu, Sichuan, and Chongqing; (2) duration of military service ≥ 1.0 years; and (3) educational level of junior high school or above. Individuals who presented severe physical illness, schizophrenia, bipolar disorder, cerebral organic diseases, epilepsy, or substance abuse were excluded. Missing information for demographics and the military careers of soldiers in the questionnaire and individuals who did not complete the study caused by withdrawal, deployment, injuries, or other causes were excluded.
Collection indicators
We collected information on demographics and the military careers of all soldiers, including the location of service, gender, age, professional age, and official rank. In addition, 18 factors were collected using three questionnaires, including the Military Mental Health Status Questionnaire (MMHSQ), Military Mental Health Ability Questionnaire (MMHAQ), and Mental Quality Questionnaire for Army Men (MQQAM) (23–25). There were seven (psychosis, depression, suicidal tendency, post-traumatic stress, sleep problems, social phobia, and antisocial tendency), six (emergency-dealing ability, stress tolerance ability, calm ability, adapting ability, physical control ability, and cooperation ability), and five (intelligence, loyalty, courage, confidence, and frustration) items included in MMHSQ, MMHAQ, and MQQAM, respectively. The content, structure, and criterion validity for MMHSQ, MMHAQ, and MQQAM are relatively good (23–25). The detailed items for MMHSQ, MMHAQ, and MQQAM are shown in the Supplementary material.
Outcome
The mental disorders in the soldiers were assessed using the Symptom Checklist-90 (SCL-90), which includes 90 items. Each item was scored using a 5-point Likert scale. The scores for the SCL-90 range from 90 to 450, reflecting the severity of the symptoms. A total of 10 subscales were included: somatization, obsessive-compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, psychoticism, and additional items (26). Mental disorders were defined using the scores on each subscale ≥ 2.0.
Statistical analysis
All collected data were classified as either categorical or continuous variables. Next, the data for continuous variables were presented as means (standard deviation) or medians (quartile) according to data distribution, while frequencies (proportions) were applied to describe categorical data. The differences in the characteristics of soldiers with and without mental disorders were assessed using t-tests, Kruskal–Wallis tests, chi-square tests, and Cochran–Mantel–Haenszel tests according to the data type and distribution. The distribution of mental disorders was assessed using the SCL-90 according to the serving place, and they were also described as frequencies (proportion). After this, a univariate logistic regression was used to explore potential risk factors (serving place, gender, age, duration of military service, official rank, psychosis, depression, suicidal tendency, post-traumatic stress, sleep problems, social phobia, antisocial tendency, emergency-dealing ability, stress tolerance ability, calm ability, adapting ability, physical control ability, cooperation ability, intelligence, loyalty, courage, confidence, and frustration) and subjected to the multivariate logistic regression model, using α = 0.05 and β = 0.10. Next, the receiver operating characteristic (ROC) curve was constructed based on the identified risk factors, and the area under the curve (AUC) was analyzed. All reported P-values were two-sided. A P < 0.05 was considered statistically significant. All the statistical analyses were conducted using IBM SPSS Statistics for Windows, version 26.0 (SPSS 26.0).
Results
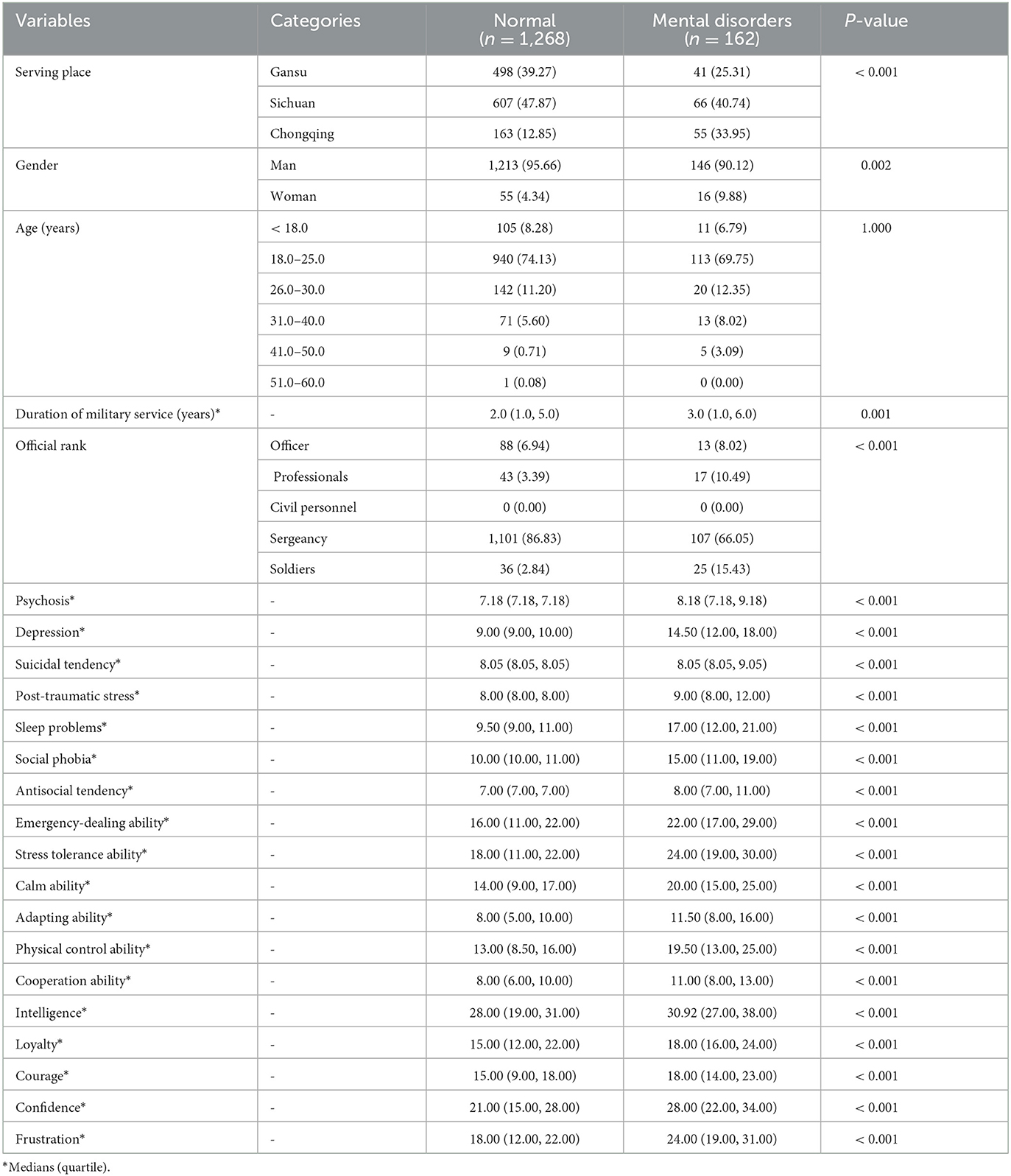
Baseline characteristics
Table 1 shows baseline demographics, military careers, and 18 factors from three questionnaires between normal and mental disorder status. Of 1,430 Chinese soldiers, 162 soldiers (11.33%) presented with mental disorders. We found no significant difference in age between soldiers with and without mental disorders. Significant differences were found between the groups for location, gender, duration of military service, official rank, psychosis, depression, suicidal tendency, post-traumatic stress, sleep problems, social phobia, antisocial tendency, emergency-dealing ability, stress tolerance ability, calm ability, adapting ability, physical control ability, cooperation ability, intelligence, loyalty, courage, confidence, and frustration.
Mental disorder status
The mental disorders in each item from SCL-90 according to service location are summarized in Table 2. The prevalence of mental disorders is listed as follows: as indicated by percentages in items for somatization (4.06%), obsessive-compulsive (7.06%), interpersonal sensitivity (4.55%), depression (3.43%), anxiety (3.50%), hostility (3.78%), phobic anxiety (1.54%), paranoid ideation (2.94%), psychoticism (1.47%), and additional items (4.76%).
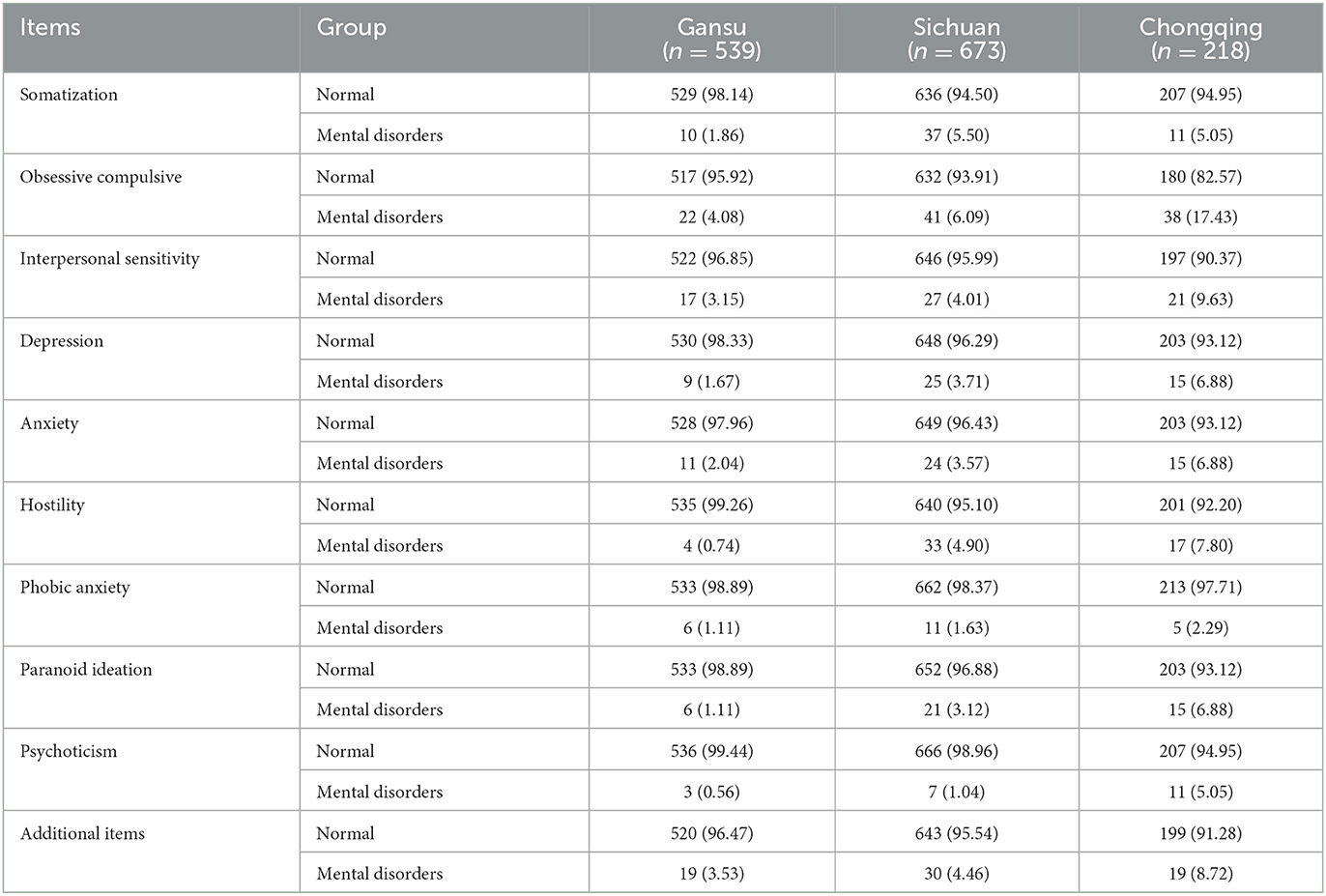
Table 2. Frequencies and proportions of mental disorders in Chinese army soldiers assessed using the Symptom Checklist-90 according to serving place.
Risk factors
Table 3 shows the risk factors for the mental disorders analyzed by univariate logistic regression. We noted that the serving location, gender, age, duration of military service, psychosis, depression, suicidal tendency, post-traumatic stress, sleep problems, social phobia, antisocial tendency, emergency-dealing ability, stress tolerance ability, calm ability, adapting ability, physical control ability, cooperation ability, intelligence, loyalty, courage, confidence, and frustration are significantly associated with the risk of mental disorders. However, the official rank was not associated with the risk of mental disorders. After the multivariate logistic regression was performed, we noted that serving place (Sichuan vs. Gansu: OR, 1.846, 95% CI: 1.028–3.315, P = 0.038; Chongqing vs. Gansu: OR, 3.129, 95% CI, 1.669–5.869, P = 0.003), increased psychosis (OR, 1.491, 95% CI, 1.152–1.928, P = 0.002), depression (OR, 1.482, 95% CI, 1.349–1.629, P < 0.001), sleep problems (OR, 1.235, 95% CI, 1.162–1.311, P < 0.001), and frustration scores (OR, 1.050, 95% CI, 1.015–1.087, P = 0.005) are associated with an increased risk of mental disorders (Table 4).
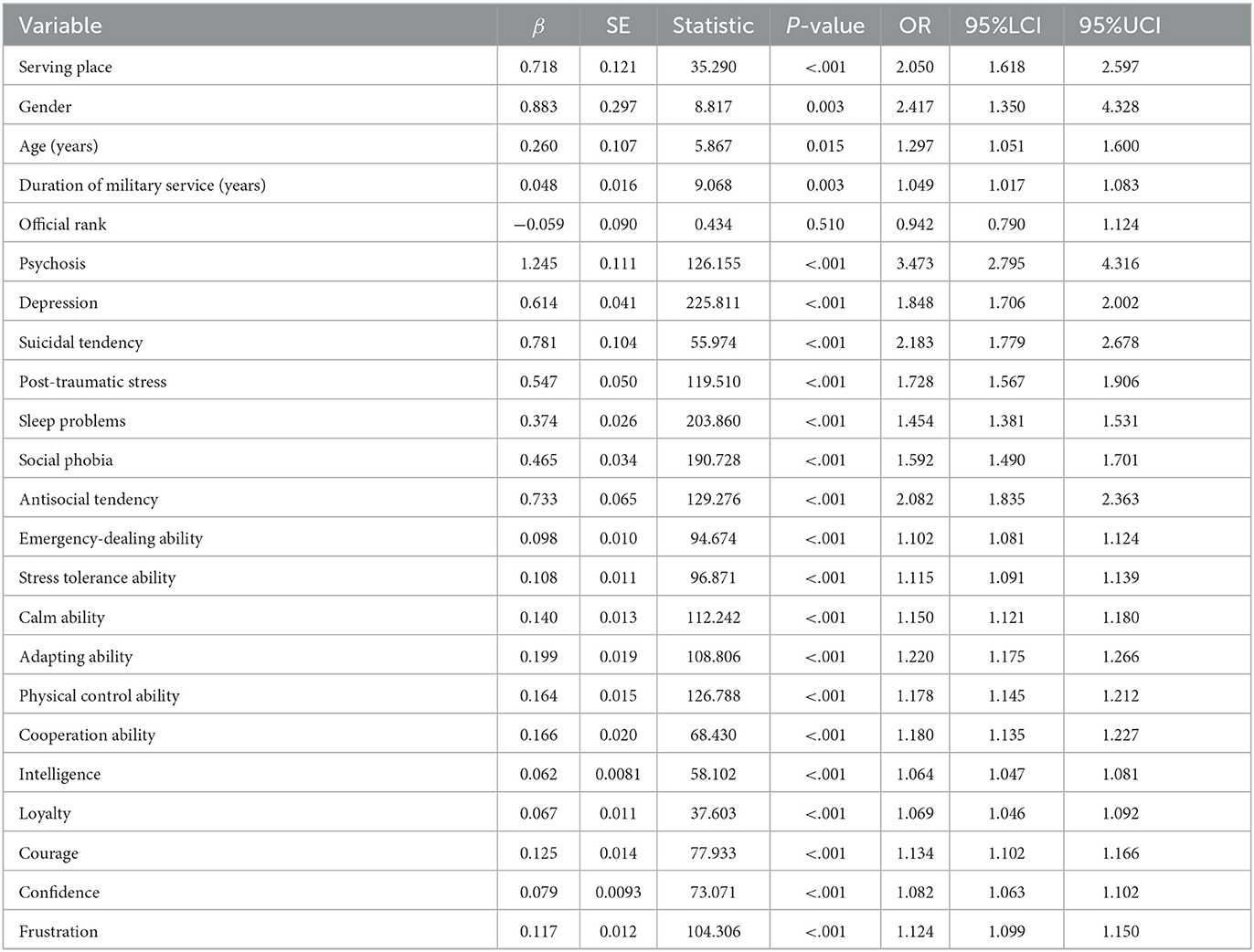
Table 3. Risk factors for mental disorders in Chinese army soldiers assessed using the Symptom Checklist-90 by univariate logistic regression.

Table 4. Risk factors for mental disorders in Chinese army soldiers assessed using the Symptom Checklist-90 by multivariate logistic regression.
Prediction model
We combined service location, psychosis, depression, sleep problems, and frustration to construct the prediction model, and the result is shown in Figure 1. The predictive value of this model was high, and the AUC was 0.930 (95% CI: 0.907–0.952) for predicting mental disorders in Chinese soldiers.
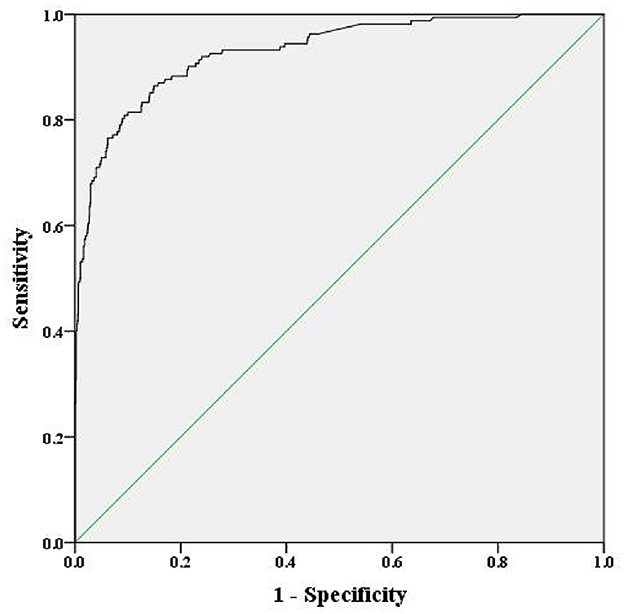
Figure 1. Receiver operating curve of the risk for mental disorders, including the five-component risk factor model (area under the curve = 0.930).
Discussion
The prevalence of mental disorders in Chinese soldiers was relatively high. Therefore, researchers should assess potential risk factors and develop a prediction model for their early management to improve the progression and prognosis for mental disorders. We identified 1,430 Chinese soldiers from three service locations. The prevalence of mental disorders was 11.33%. In addition, the prevalence of obsessive-compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, psychoticism, and additional items was highest in Chongqing, while somatization was highest in Sichuan. The risk factors for mental disorders in Chinese soldiers included service location, psychosis, depression, sleep problems, and frustration. Combining these factors, the predictive value of our model was high, and the AUC was 0.930.
The univariate analysis indicated the risk of mental disorders could be affected by serving location, gender, age, duration of military service, psychosis, depression, suicidal tendency, post-traumatic stress, sleep problems, social phobia, antisocial tendency, emergency-dealing ability, stress tolerance ability, calm ability, adapting ability, physical control ability, cooperation ability, intelligence, loyalty, courage, confidence, and frustration, while after adjusting the confounding factors, we noted that service location, psychosis, depression, sleep problems, and frustration are associated with increased mental disorders. Several reasons could explain these results: (1) Military service duration in Chongqing was longer than in Sichuan and Gansu, and more than 50% of the Chongqing portion of the sample included soldiers aged 25 years or more, while this proportion in Sichuan and Gansu was < 30%; thus, the soldiers' age might affect the risk of mental disorders (27). Moreover, the proportion of women in Chongqing (22.94%) was higher than in Sichuan (1.63%) and Gansu (1.86%), meaning the prevalence of mental disorders could be affected by gender (28); (2) the hallucinations and delusions of psychosis could cause an additional risk of mental disorders (29); (3) sleep problems could be induced by an underlying illness or history of mental illness, which might play an important role in promoting panic, anxiety, and depression (30); and (4) frustration is significantly associated with emotional difficulties, which could contribute to the progression of mental disorders (31).
Our study constructed a prediction model for mental disorders in Chinese soldiers. Several similar studies have already been performed on the general population (32, 33). For example, Karasch et al. identified 5,764 cases admitted to inpatient care at the four psychiatric hospitals and found that specific psychiatric diagnoses and suicidal tendencies are major risk factors for involuntary psychiatric hospitalization (32). In addition, Puntis et al. tested an individualized, clinically based trans-diagnostic model for detecting individuals at risk of psychosis and found the prognostic performance was adequate (33). The prediction model in our study showed greater predictive power than the previous models, which indicates the items from three questionnaires could be applied to monitor mental disorders in Chinese soldiers.
The results of this study provide more information for army administrators. The risk factors for mental disorders in Chinese soldiers were identified. Moreover, the combined prediction model was constructed, which could screen soldiers at high risk for mental disorders. Considering the results of this study, early psychological counseling and intervention should be applied for soldiers at high risk to prevent the progression of mental disorders.
We should acknowledge several shortcomings of this study. First, this study was cross-sectional and cannot confirm a causal relationship for predictors. Second, the analysis was not divided into a training and validation set, and an external cohort study should be performed to validate this model. Finally, the SCL-90 has inherent limitations, including cultural adaptation. Finally, all questionnaires hold the risk of “fake good” bias, where the respondent provides answers they think the researcher would like to read or hear, and memory failure.
Conclusion
The study findings reported the prevalence of mental disorders in Chinese soldiers. The identified risk factors included service location, psychosis, depression, sleep problems, and frustration. The prediction model based on these factors provides high predictive value for mental disorders in Chinese soldiers. However, the robustness of the prediction model should be validated in further large-scale prospective studies.
Strengths and limitations of this study
(1) The prevalence of mental disorders in Chinese soldiers was reported.
(2) Identified risk factors included service location, psychosis, depression, sleep problems, and frustration.
(3) The prediction model provides high predictive value for mental disorders in Chinese soldiers.
(4) This study was cross-sectional and cannot confirm a causal relationship between predictors.
(5) The analysis was not divided into a training and validation set, and the model requires further validation.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Third Military Medical University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
MZ: study conception, design, processing data, analysis, drafting, and manuscript revision. ZF, YH, and QT: study conception, design, and manuscript revision. NW: data acquisition, processing data, and psychometric test descriptions. HZ: data acquisition and manuscript revision. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the Foundation for Humanities and Social Science (2018XRW001) and Military Psychology Youth Innovation Fund (KY2018102).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1125411/full#supplementary-material
References
1. Lei X, Liu C, Jiang H. Mental health of college students and associated factors in Hubei of China. PLoS ONE. (20211) 6:e0254183. doi: 10.1371/journal.pone.0254183
2. Wang PS, Aguilar-Gaxiola S, Alonso J. Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. Lancet. (2007) 370:841–50. doi: 10.1016/S0140-6736(07)61414-7
3. Wang PS, Aguilar-Gaxiola S, Alonso J, Angermeyer MC, Borges G, Bromet EJ. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the global burden of disease study 2013. Lancet. (2015) 386:743–800. doi: 10.1016/S0140-6736(15)60692-4
4. Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. (2005) 62:617–27. doi: 10.1001/archpsyc.62.6.617
5. de Graaf R, Ten Have M, van Gool C, van Dorsselaer S. Prevalence of mental disorders and trends from 1996 to 2009. Results from the Netherlands mental health survey and incidence Study-2. Soc Psychiatry Psychiatr Epidemiol. (2012) 47:203–13. doi: 10.1007/s00127-010-0334-8
6. Xiong H, Zhang X, Zhang Y, Ma F, Li Y, Li L. An investigation of the prevalence of depressive symptoms in soldiers during military training. Prev Med. (2005) 41:642–5. doi: 10.1016/j.ypmed.2005.01.010
7. Jiang Y, Tang J, Li R, Zhao J, Song Z, Ge H. Effect of 5-HT2A receptor polymorphisms, work stressors, and social support on job strain among petroleum workers in Xinjiang, China. Int J Environ Res Public Health. (2016) 13:1258. doi: 10.3390/ijerph13121258
8. Wiernik E, Pannier B, Czernichow S, Nabi H, Hanon O, Simon T. Occupational status moderates the association between current perceived stress and high blood pressure: evidence from the IPC cohort study. Hypertension. (2013) 61:571–7. doi: 10.1161/HYPERTENSIONAHA.111.00302
9. Harvey SB, Modini M, Joyce S, Milligan-Saville JS, Tan L, Mykletun A, et al. Can work make you mentally ill? A systematic meta-review of work-related risk factors for common mental health problems. Occup Environ Med. (2017) 74:301–10. doi: 10.1136/oemed-2016-104015
10. Czabała C, Charzyńska K, Mroziak B. Psychosocial interventions in workplace mental health promotion: an overview. Health Promot Int. (2011) 26:i70–84. doi: 10.1093/heapro/dar050
11. Martin A, Sanderson K, Cocker F. Meta-analysis of the effects of health promotion intervention in the workplace on depression and anxiety symptoms. Scand J Work Environ Health. (2009) 35:7–18. doi: 10.5271/sjweh.1295
12. Hummel KV, Trautmann S, Venz J, Thomas S, Schäfer J. Repetitive negative thinking: transdiagnostic correlate and risk factor for mental disorders? A proof-of-concept study in German soldiers before and after deployment to Afghanistan. BMC Psychol. (2021) 9:198. doi: 10.1186/s40359-021-00696-2
13. Hourani LL, Yuan H. The mental health status of women in the navy and marine corps: preliminary findings from the perceptions of wellness and readiness assessment. Mil Med. (1999) 164:174–81. doi: 10.1093/milmed/164.3.174
14. Wang H, Zhang R, Chen Y, Wang H, Zhang Y, Gan J, et al. Social anxiety disorder in the Chinese military: prevalence, comorbidities, impairment, and treatment-seeking. Psychiatry Res. (2014) 220: 903–8. doi: 10.1016/j.psychres.2014.07.063
15. Zhang L, Hu XZ Yu T, Chen Z, Dohl J, Li X, et al. Genetic association of FKBP5 with PTSD in US service members deployed to Iraq and Afghanistan. J Psychiatr Res. (2020) 122:48–53. doi: 10.1016/j.jpsychires.2019.12.014
16. Zhang L, Wang Y, Guo J, Lin H, Chen C, Yao G, et al. correlation study on mental health and social support of peacekeeping soldiers with suicidal ideation in seven countries. Chin J Behav Med Brain Sci. (2013) 12:150–2.
17. Cai WP, Pan Y, Zhang SM, Wei C, Dong W, Deng GH. Relationship between cognitive emotion regulation, social support, resilience and acute stress responses in Chinese soldiers: exploring multiple mediation model. Psychiatry Res. (2017) 256:71–8. doi: 10.1016/j.psychres.2017.06.018
18. Yan J, Wang LJ, Cheng Q, Miao DM, Zhang LY, Yuan SP, et al. Estimated mental health and analysis of relative factors for new Chinese recruits. Mil Med. (2008) 173:1031–4. doi: 10.7205/MILMED.173.10.1031
19. Jones DM, Bailey SP, Roelands B, Buono MJ, Meeusen R. Cold acclimation and cognitive performance: a review. Auton Neurosci. (2017) 208:36–42. doi: 10.1016/j.autneu.2017.11.004
21. Sharma R, Cramer NP, Perry B, Adahman Z, Murphy EK, Xu X, et al. Chronic exposure to high altitude: synaptic, astroglial and memory changes. Sci Rep. (2019) 9: 16406. doi: 10.1038/s41598-019-52563-1
22. Huang Y, Xu J, Zheng S, Xu S, Wang Y, Du J, et al. The risk factors for insomnia and sleep-disordered breathing in military communities: a meta-analysis. PLoS ONE. (2021) 16:e0250779. doi: 10.1371/journal.pone.0250779
23. Wei L. Study on the Assessment of Military Mental Health Status and the Eye Movement Identification. Chongqing: Army Medical University. (2018).
24. Feng H. Development of Military Mental Health Ability Questionnaire and Analysis of Its Demographic Characteristics. Chongqing: Army Medical University. (2018).
25. Feng W, Zhengzhi F, Yaqin L. The compilation of mental quality questionnaire for army men. J Prey Med Chin PEA. (2007) 2:101–4.
26. Prinz U, Nutzinger DO, Schulz H, Petermann F, Braukhaus C, Andreas S. Comparative psychometric analyses of the SCL-90-R and its short versions in patients with affective disorders. BMC Psychiatry. (2013) 13:104. doi: 10.1186/1471-244X-13-104
27. Iranpour S, Sabour S, Koohi F, Saadati HM. The trend and pattern of depression prevalence in the US: data from national health and nutrition examination survey (NHANES) 2005 to 2016. J Affect Disord. (2021) 14:27. doi: 10.1016/j.jad.2021.11.027
28. Teng Z, Su Y, Chen J, Wu R, Tang H, Wu H, et al. Sex Differences in psychological status and fatigue of frontline staff after the COVID-19 outbreak in China: a cross-sectional study. Front Psychol. (2021) 12:676307. doi: 10.3389/fpsyg.2021.676307
29. Buswell G, Haime Z, Lloyd-Evans B, Billings J. A systematic review of PTSD to the experience of psychosis: prevalence and associated factors. BMC Psychiatry. (2021) 21:9. doi: 10.1186/s12888-020-02999-x
30. Jiang YF, Chen JQ, Wang YG, Zhang XD, Hong WK. Sleep quality and mental health status of healthcare professionals during the outbreak of coronavirus disease 2019 (COVID-19). Psychol Health Med. (2021) 15:1–8. doi: 10.1080/13548506.2021.1954669
31. Jibeen T. Frustration intolerance beliefs as predictors of emotional problems in university undergraduates. J Ration Emot Cogn Behav Ther. (2013) 31:16–26. doi: 10.1007/s10942-012-0154-8
32. Karasch O, Schmitz-Buhl M, Mennicken R, Zielasek J, Gouzoulis-Mayfrank E. Identification of risk factors for involuntary psychiatric hospitalization: using environmental socioeconomic data and methods of machine learning to improve prediction. BMC Psychiatry. (2020) 20:401. doi: 10.1186/s12888-020-02803-w
Keywords: mental health, risk factors, prediction model, soldiers, Chinese
Citation: Zhao M, He Y, Tang Q, Wang N, Zheng H and Feng Z (2023) Risk factors and prediction model for mental health in Chinese soldiers. Front. Psychiatry 14:1125411. doi: 10.3389/fpsyt.2023.1125411
Received: 16 December 2022; Accepted: 27 March 2023;
Published: 05 May 2023.
Edited by:
Ashwani Kumar Mishra, All India Institute of Medical Sciences, IndiaReviewed by:
Yee Ming Mok, Institute of Mental Health, SingaporeVivek Verma, Assam University, India
Copyright © 2023 Zhao, He, Tang, Wang, Zheng and Feng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhengzhi Feng, Znp6QHRtbXUuZWR1LmNu
 Mengxue Zhao
Mengxue Zhao Ying He2
Ying He2 Zhengzhi Feng
Zhengzhi Feng