- 1Department of Ageing and Health, Guy’s and St Thomas’ Hospital, London, United Kingdom
- 2Leicester School of Allied Health Sciences, De Montfort University, Leicester, United Kingdom
- 3The Evington Centre, Leicestershire Partnership National Health Service (NHS) Trust, Leicester, United Kingdom
- 4Department of Cardiovascular Sciences, University of Leicester, Leicester, United Kingdom
- 5National Institute for Health Research Leicester Biomedical Research Centre, British Heart Foundation Cardiovascular Research Centre, Glenfield Hospital, Leicester, United Kingdom
Introduction
By 2050, it is projected that the population of over 60 years old will reach 2.1 billion, from 900 million in 2015 (1). A total of 20% of this cohort have a neurological or mental health disorder, which is expected to rise in line with these changing population demographics (2). Anxiety, substance abuse disorders, schizophrenia and bipolar disorder are also seen commonly in older people. Serious mental illness (SMI) is a term used to group several common psychiatric disorders (schizophrenia, bipolar affective disorder and major depressive disorder) which significantly affect functional abilities (3). While the mortality gap remains significant between people living with SMI and the general population, older people with SMI are routinely cared for by old age psychiatrists and have distinct challenges from the younger SMI population (4). These challenges include greater frailty, high levels of physical health morbidity, polypharmacy, and greater levels of cognitive and functional impairments (1). A recent study found that 17.5% of 65–84 year olds have both a physical and mental health condition, rising to ∼30% of over 85 year olds (5). There is a substantial interplay between physical and mental health and people with SMI have a 10–20 year reduction in life expectancy compared to those without (6, 7).
Cardiovascular disease and SMI
Physical ill health is the most significant factor in the widening mortality gap between SMI and the general population (1). Cardiovascular disease (CVD) is the leading cause of mortality worldwide (8), and the major cause of death in SMI (9), and CVD increases with age (10). The relationship is bidirectional, and those with CVD are also at higher risk of adverse mental health (9). Much of this risk is modifiable through better provision and access to physical healthcare (11). A large meta-analysis of observational studies found higher rates of all CVD sub-types amongst those with SMI, but contemporary data in the UK is lacking (12), the last studies being conducted over a decade ago (13, 14). The average age of participants with SMI was ∼50 years in these studies (12–14), and few studies specifically investigate older populations. One of the major challenges to understanding this relationship is the fragmented nature of physical and mental health services, and the lack of integrated data systems through which to achieve this. Furthermore, interventions need to be tailored for older people given the unique challenges associated with managing CVD in SMI with concomitant frailty, cognitive and physical impairments (15). In the UK, CVD was highlighted as a key priority in the National Health Service (NHS) long term plan (16). Inequality of care for patients with SMI was highlighted, and a toolkit has been developed to improve rates of detection, prevention and treatment in SMI (16).
In a large meta-analysis, patients with SMI had a 53% higher risk of CVD and 85% higher CVD-related mortality compared to the general population (12). However, the majority of these studies focused on younger populations. In a large study of over 600,000 of community dwelling over 65-year-olds with SMI or substance use disorders, there was an increased risk of hypertension, ischaemic heart disease, congestive heart failure, and atrial fibrillation compared to community dwelling older people and those in long-term care (17).
Depression is associated with a greater risk of cardiovascular mortality in older adults (18, 19). There is also an increased risk of coronary heart disease in depressive disorders (20–22). Even mild depression has a higher risk of CVD, which is greater amongst those with chronic or recurrent depression (20). Furthermore, there is an increased risk of stroke and cardiovascular related mortality in older people with depression and comorbid hypertension (23, 24).
Risk factors for CVD in SMI
There are several reasons that CVD risk is elevated amongst people with SMI relative to the general population (3), and given that age is an independent risk factor for CVD, these risks are only likely to increase further over time. Firstly, there is an increased rate of risk taking behaviors (e.g., smoking, poor diet, sedentary lifestyle) amongst people with SMI (25). A large study of ∼600,000 patients found higher rates of smoking, diabetes and elevated BMI amongst people diagnosed with SMI, although ten year risk in patients aged 40–75 years was similar between those with and without SMI (25). However, those with established CVD were excluded so it is unclear if CVD rates in older people with and without SMI were comparable. Secondly, antipsychotics, mood stabilizers, and some antidepressants have significant adverse metabolic side effects, and poorer CVD outcomes (26, 27). Antipsychotic medications are associated with dyslipidemia, increased insulin resistance, and weight gain (28, 29). In older people, there are specific concerns that both first and second generation antipsychotics may increase the risk of sudden cardiac death in patients with and without dementia (30). Furthermore, antipsychotic use in dementia has been associated with increased risk of both stroke and myocardial infarction (31, 32). One study found comparable CVD risk between first and second generation antipsychotics in older people, although haloperidol and levomepromazine had greater CVD-risk compared to risperidone (30). Coupled with increases in CVD associated with aging, this could significantly worsen CVD prevalence and mortality, although more studies in older people are needed to confirm this. Older people with SMI also experience inequalities in access to physical healthcare (11, 33), and are more likely to be institutionalized earlier (34). Older people experience greater barriers to accessing health services due to financial constraints, physical and mobility impairments, cognitive impairment, and increased dependency (35).
People with SMI also experience significant stigma, are vulnerable, and may have atypical presentations of CVD that are under-recognized by healthcare professionals (36). In older people, presentations can be complicated by the presence of delirium, and recognizing periods of acute illness can be more challenging (37). As a consequence, older people are less likely to be adequately assessed and treated for CVD, which may be compounded by concomitant SMI (36). These factors may also lead to a reduction in access to or engagement with primary and secondary prevention of CVD, such as smoking cessation services, and physical activity programs (3). People with SMI are more likely to have lower socio-economic status (38), with reduced ability to access healthy diets and physical activity services which require subscriptions. Financial barriers are common in older people owing to reduced income, reliance on pensions, and socioeconomic factors (35, 39). Substance misuse is commonly associated with SMI, remains high in older adults (40), and is associated with CVD (17). Rates of medication non-adherence are higher amongst SMI, which may reduce compliance with preventative therapies (e.g., statins, antihypertensives) (41). In older people with cognitive impairment, non-adherence rates may be further exacerbated, and their ability to engage with physical activity programs are more likely to be impaired (4). Figure 1 summarizes the key risk factors for CVD in older people with SMI.
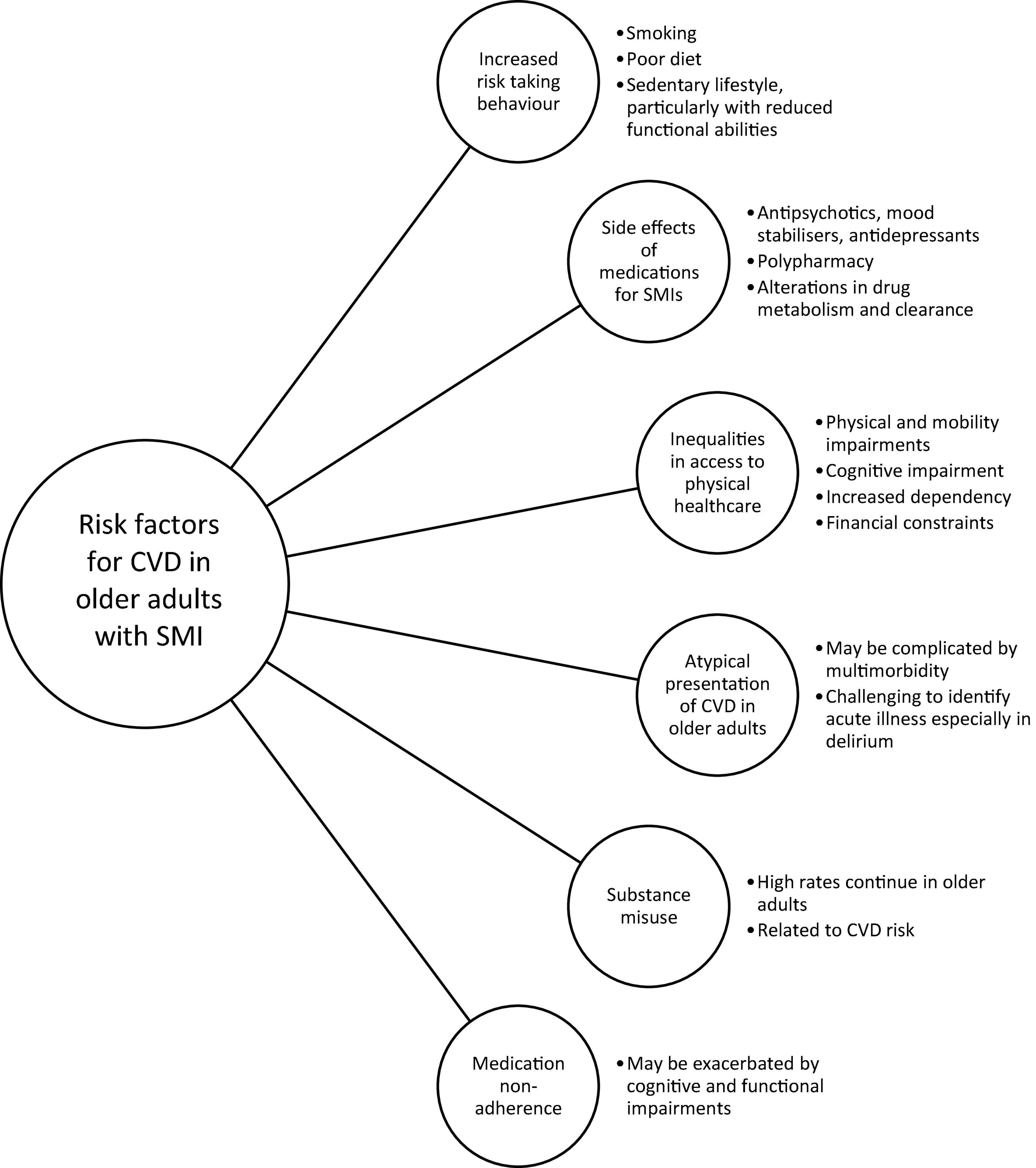
Figure 1. Summary of risk factors for cardiovascular disease (CVD) in older people living with serious mental illness (SMI).
Current management of CVD in SMI
Interventions to address SMI in CVD can be considered under two main categories. Firstly, primary prevention strategies targeting risk factors and comorbidities, and secondly, secondary prevention strategies targeting individuals who have already experienced CVD (3).
A significant proportion of patients with SMI are managed by primary, as well as secondary care, with around one third being managed solely by primary care (42). However, continuity between primary and secondary care services remains inadequate (42), with significant care inequalities (43). Rates of physical comorbidity for people living with SMI in primary care are high, and increasing over time (44). Therefore, primary care is a key area for the implementation of CVD risk assessment and stratification for older people living with SMI. In England, the quality and outcomes framework (QOF), incentivizes practices to undertake CVD risk assessment (45), and the use of tailored risk assessment calculators for SMI will be particularly important in this setting. However, in older people the balance of risk and care priorities is likely to shift with increasing frailty, and a greater focus on quality of life, requiring a more tailored approach to risk management. Furthermore, primary prevention strategies may be less effective later in life (owing to the long duration required for risk reduction), and these calculators may be less applicable to older populations.
Pharmacological management of SMI in older people is challenging. Older people experience significant polypharmacy (more than or equal to five medications), and can affect up to 96.5% of older people (46). Antipsychotic polypharmacy refers to the use of two or more antipsychotics combined with mood stabilizers, antidepressants, anxiolytics or hypnotics (47). Whilst antipsychotic polypharmacy can benefit some patients (47), older people are more vulnerable to adverse effects owing to alterations in drug metabolism and clearance (46). Furthermore, benzodiazepines, antidepressants, and polypharmacy have been linked to increased risk of falls and hip fracture, but the relationship with antipsychotics is less clear (48). However, approaches which simplify treatment regimens, reduce polypharmacy, and minimize side effects are likely to be beneficial.
In a review by Bartels et al. few interventions have been designed specifically for older people with SMI, despite key differences to younger populations (33). However, integrated care models targeting both physical and mental health using psychosocial skills training, illness self-management, collaborative care, and behavioral health homes have shown benefit (33). An emerging area for future research is the use of digital technology, particularly for older people in long-term care and rural communities. Although research has been limited in this area, telehealth has demonstrated feasibility for treatment monitoring in adults with SMI, which could be used in long-term care facilities (49).
Discussion
In summary, people living with SMI are at greater risk for CVD than the general population, but how age modulates this risk is less clear. Despite this, rates of assessment and treatment remain low. Older people face a number of distinct challenges compared to younger people living with SMI, which may benefit from a more comprehensive and holistic approach to care. In particular, principles drawn from comprehensive geriatric assessment may be beneficial, even in younger patients who display early signs of frailty and multi-morbidity. Importantly, approach to risk and balance of priorities are likely to differ considerably between younger and older patients with SMI and a personalized approach to risk management, including principles of advanced care planning, will be particularly important for older people living with SMI and frailty. This could be achieved through more integrated care and liaison between physical and mental health practitioners, and primary and secondary care services. Strategies to address both primary and secondary prevention of CVD have shown mixed results, but the emergence of risk calculators, multi-modal programmes, and measures to improve adherence are promising. Much of these interventions may need to be modified to consider challenges associated with aging, particularly in terms of cognitive and functional impairments. More work is needed to elucidate effective ways to manage CVD risk and encourage adherence in older people living with SMI but also to manage long term complications, and promote and enhance recovery through rehabilitation programmes.
Author contributions
KC, SG, HS, and LB drafted the manuscript. All authors contributed to the article and approved the submitted version.
Funding
LB is an academic clinical lecturer funded by the National Institute for Health Research. The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
2. World Health Organisation [WHO]. Mental Health of Older Adults. Geneva: World Health Organisation (2017).
3. Goldfarb M, De Hert M, Detraux J, Di Palo K, Munir H, Music S, et al. Severe mental illness and cardiovascular disease: JACC state-of-the-art review. J Am Coll Cardiol. (2022) 80:918–33. doi: 10.1016/j.jacc.2022.06.017
4. Royal College of Psychiatrists [RCP]. Caring for the Whole Person. Physical Healthcare of Older Adults with Mental Health Illness: Integration of Care. College Report CR222. London: Royal College of Psychiatrists (2019).
5. Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. (2012) 380:37–43. doi: 10.1016/S0140-6736(12)60240-2
6. Robson D, Gray R. Serious mental illness and physical health problems: a discussion paper. Int J Nurs Stud. (2007) 44:457–66. doi: 10.1016/j.ijnurstu.2006.07.013
7. Hayes JF, Marston L, Walters K, King MB, Osborn DPJ. Mortality gap for people with bipolar disorder and schizophrenia: UK-based cohort study 2000-2014. Br J Psychiatry. (2017) 211:175–81. doi: 10.1192/bjp.bp.117.202606
8. World Health Organisation [WHO]. Cardiovascular Diseases. Geneva: World Health Organisation (2021).
9. De Hert M, Detraux J, Vancampfort D. The intriguing relationship between coronary heart disease and mental disorders. Dialogues Clin Neurosci. (2018) 20:31–40. doi: 10.31887/DCNS.2018.20.1/mdehert
10. Rodgers JL, Jones J, Bolleddu SI, Vanthenapalli S, Rodgers LE, Shah K, et al. Cardiovascular risks associated with gender and aging. J Cardiovasc Dev Dis. (2019) 6:19.
11. De Hert M, Correll CU, Bobes J, Cetkovich-Bakmas M, Cohen D, Asai I, et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry. (2011) 10:52–77. doi: 10.1002/j.2051-5545.2011.tb00014.x
12. Correll CU, Solmi M, Veronese N, Bortolato B, Rosson S, Santonastaso P, et al. Prevalence, incidence and mortality from cardiovascular disease in patients with pooled and specific severe mental illness: a large-scale meta-analysis of 3,211,768 patients and 113,383,368 controls. World Psychiatry. (2017) 16:163–80. doi: 10.1002/wps.20420
13. Smith DJ, Martin D, McLean G, Langan J, Guthrie B, Mercer SW. Multimorbidity in bipolar disorder and undertreatment of cardiovascular disease: a cross sectional study. BMC Med. (2013) 11:263. doi: 10.1186/1741-7015-11-263
14. Smith DJ, Langan J, McLean G, Guthrie B, Mercer SW. Schizophrenia is associated with excess multiple physical-health comorbidities but low levels of recorded cardiovascular disease in primary care: cross-sectional study. BMJ Open. (2013) 3:e002808. doi: 10.1136/bmjopen-2013-002808
15. Nielsen RE, Banner J, Jensen SE. Cardiovascular disease in patients with severe mental illness. Nat Rev Cardiol. (2021) 18:136–45. doi: 10.1038/s41569-020-00463-7
17. Lin WC, Zhang J, Leung GY, Clark RE. Chronic physical conditions in older adults with mental illness and/or substance use disorders. J Am Geriatr Soc. (2011) 59:1913–21. doi: 10.1111/j.1532-5415.2011.03588.x
18. Sun WJ, Xu L, Chan WM, Lam TH, Schooling CM. Are depressive symptoms associated with cardiovascular mortality among older chinese: a cohort study of 64,000 people in Hong Kong? Am J Geriatr Psychiatry. (2013) 21:1107–15. doi: 10.1016/j.jagp.2013.01.048
19. Wei J, Lu Y, Li K, Goodman M, Xu H. The associations of late-life depression with all-cause and cardiovascular mortality: the NHANES 2005–2014. J Affect Disord. (2022) 300:189–94. doi: 10.1016/j.jad.2021.12.104
20. Haigh EAP, Bogucki OE, Dearborn PJ, Robbins MA, Elias MF. Depressive symptoms prospectively predict cardiovascular disease among older adults: findings from the maine-syracuse longitudinal study. J Health Psychol. (2018) 25:2006–16. doi: 10.1177/1359105318782375
21. Brown JM, Stewart JC, Stump TE, Callahan CM. Risk of coronary heart disease events over 15 years among older adults with depressive symptoms. Am J Geriatr Psychiatry. (2011) 19:721–9. doi: 10.1097/JGP.0b013e3181faee19
22. Péquignot R, Dufouil C, Prugger C, Pérès K, Artero S, Tzourio C, et al. High level of depressive symptoms at repeated study visits and risk of coronary heart disease and stroke over 10 years in older adults: the three-city study. J Am Geriatr Soc. (2016) 64:118–25. doi: 10.1111/jgs.13872
23. Maatouk I, Herzog W, Böhlen F, Quinzler R, Löwe B, Saum K-U, et al. Association of hypertension with depression and generalized anxiety symptoms in a large population-based sample of older adults. J Hypertens. (2016) 34:1711–20. doi: 10.1097/HJH.0000000000001006
24. Simonsick EM, Wallace RB, Blazer DG, Berkman LF. Depressive symptomatology and hypertension-associated morbidity and mortality in older adults. Psychosomatic Med. (1995) 57:427–35. doi: 10.1097/00006842-199509000-00003
25. Rossom RC, Hooker SA, O’Connor PJ, Crain AL, Sperl-Hillen JM. Cardiovascular risk for patients with and without schizophrenia, schizoaffective disorder, or bipolar disorder. J Am Heart Assoc. (2022) 11:e021444. doi: 10.1161/JAHA.121.021444
26. Kilicaslan EE, Karakilic M, Erol A. The relationship between 10 years risk of cardiovascular disease and schizophrenia symptoms: preliminary results. Psychiatry Investig. (2019) 16:933–9. doi: 10.30773/pi.2019.0063
27. Lai FTT, Guthrie B, Mercer SW, Smith DJ, Yip BHK, Chung GKK, et al. Association between antipsychotic use and acute ischemic heart disease in women but not in men: a retrospective cohort study of over one million primary care patients. BMC Med. (2020) 18:289. doi: 10.1186/s12916-020-01765-w
28. Pillinger T, McCutcheon RA, Vano L, Mizuno Y, Arumuham A, Hindley G, et al. Comparative effects of 18 antipsychotics on metabolic function in patients with schizophrenia, predictors of metabolic dysregulation, and association with psychopathology: a systematic review and network meta-analysis. Lancet Psychiatry. (2020) 7:64–77. doi: 10.1016/S2215-0366(19)30416-X
29. MacKenzie NE, Kowalchuk C, Agarwal SM, Costa-Dookhan KA, Caravaggio F, Gerretsen P, et al. Antipsychotics, metabolic adverse effects, and cognitive function in schizophrenia. Front Psychiatry. (2018) 9:622. doi: 10.3389/fpsyt.2018.00622
30. Sahlberg M, Holm E, Gislason GH, Køber L, Torp-Pedersen C, Andersson C. Association of selected antipsychotic agents with major adverse cardiovascular events and noncardiovascular mortality in elderly persons. J Am Heart Assoc. (2015) 4:e001666. doi: 10.1161/JAHA.114.001666
31. Wang S, Linkletter C, Dore D, Mor V, Buka S, Maclure M. Age, antipsychotics, and the risk of ischemic stroke in the veterans health administration. Stroke. (2012) 43:28–31. doi: 10.1161/STROKEAHA.111.617191
32. Pariente A, Fourrier-Réglat A, Ducruet T, Farrington P, Béland SG, Dartigues JF, et al. Antipsychotic use and myocardial infarction in older patients with treated dementia. Arch Intern Med. (2012) 172:648–53; discussion 54–5. doi: 10.1001/archinternmed.2012.28
33. Bartels SJ, DiMilia PR, Fortuna KL, Naslund JA. Integrated care for older adults with serious mental illness and medical comorbidity: evidence-based models and future research directions. Clin Geriatr Med. (2020) 36:341–52. doi: 10.1016/j.cger.2019.11.012
34. Andrews AO, Bartels SJ, Xie H, Peacock WJ. Increased risk of nursing home admission among middle aged and older adults with schizophrenia. Am J Geriatr Psychiatry. (2009) 17:697–705. doi: 10.1097/JGP.0b013e3181aad59d
35. Mohd Rosnu NS, Singh DKA, Mat Ludin AF, Ishak WS, Abd Rahman MH, Shahar S. Enablers and barriers of accessing health care services among older adults in south-east Asia: a scoping review. Int J Environ Res Public Health. (2022) 19:7351. doi: 10.3390/ijerph19127351
36. Cunningham R, Poppe K, Peterson D, Every-Palmer S, Soosay I, Jackson R. Prediction of cardiovascular disease risk among people with severe mental illness: a cohort study. PLoS One. (2019) 14:e0221521. doi: 10.1371/journal.pone.0221521
37. Jung YJ, Yoon JL, Kim HS, Lee AY, Kim MY, Cho JJ. Atypical clinical presentation of geriatric syndrome in elderly patients with pneumonia or coronary artery disease. Ann Geriatr Med Res. (2017) 21:158–63. doi: 10.4235/agmr.2017.21.4.158
38. O’Gallagher K, Teo JT, Shah AM, Gaughran F. Interaction between race, ethnicity, severe mental illness, and cardiovascular disease. J Am Heart Assoc. (2022) 11:e025621. doi: 10.1161/JAHA.121.025621
39. Doetsch J, Pilot E, Santana P, Krafft T. Potential barriers in healthcare access of the elderly population influenced by the economic crisis and the troika agreement: a qualitative case study in Lisbon, Portugal. Int J Equity Health. (2017) 16:184. doi: 10.1186/s12939-017-0679-7
40. Wu L-T, Blazer DG. Substance use disorders and psychiatric comorbidity in mid and later life: a review. Int J Epidemiol. (2013) 43:304–17. doi: 10.1093/ije/dyt173
41. Leslie KH, McCowan C, Pell JP. Adherence to cardiovascular medication: a review of systematic reviews. J Public Health (Oxf). (2019) 41:e84–94. doi: 10.1093/pubmed/fdy088
42. Reilly S, Planner C, Hann M, Reeves D, Nazareth I, Lester H. The role of primary care in service provision for people with severe mental illness in the United Kingdom. PLoS One. (2012) 7:e36468. doi: 10.1371/journal.pone.0036468
43. National Mental Health Intelligence Network. Severe Mental Illness (SMI) and Physical Health Inequalities: Briefing. London: National Mental Health Intelligence Network (2018).
44. Reilly S, Olier I, Planner C, Doran T, Reeves D, Ashcroft DM, et al. Inequalities in physical comorbidity: a longitudinal comparative cohort study of people with severe mental illness in the UK. BMJ Open. (2015) 5:e009010. doi: 10.1136/bmjopen-2015-009010
45. British Medical Association [BMA]. Quality and Outcomes Framework Guidance for 2021/22. Report No.: PAR456. London: British Medical Association [BMA] (2021).
46. Pazan F, Wehling M. Polypharmacy in older adults: a narrative review of definitions, epidemiology and consequences. Eur Geriatric Med. (2021) 12:443–52. doi: 10.1007/s41999-021-00479-3
47. Lin SK. Antipsychotic polypharmacy: a dirty little secret or a fashion? Int J Neuropsychopharmacol. (2020) 23:125–31. doi: 10.1093/ijnp/pyz068
48. Izza MAD, Lunt E, Gordon AL, Gladman JRF, Armstrong S, Logan P. Polypharmacy, benzodiazepines, and antidepressants, but not antipsychotics, are associated with increased falls risk in UK care home residents: a prospective multi-centre study. Eur Geriatric Med. (2020) 11:1043–50. doi: 10.1007/s41999-020-00376-1
49. Pratt SI, Bartels SJ, Mueser KT, Naslund JA, Wolfe R, Pixley HS, et al. Feasibility and effectiveness of an automated telehealth intervention to improve illness self-management in people with serious psychiatric and medical disorders. Psychiatr Rehabil J. (2013) 36:297–305. doi: 10.1037/prj0000022
Keywords: ischaemic heart disease, mental health, acute coronary syndrome, chronic heart disease, aged, cardiovascular
Citation: Chin K, Ghosh S, Subramaniam H and Beishon L (2023) Cardiovascular disease in older people with serious mental illness: Current challenges and future directions. Front. Psychiatry 14:1110361. doi: 10.3389/fpsyt.2023.1110361
Received: 28 November 2022; Accepted: 30 January 2023;
Published: 28 February 2023.
Edited by:
Gianfranco Spalletta, Santa Lucia Foundation (IRCCS), ItalyReviewed by:
Massimo Tusconi, University of Cagliari, ItalyFrancesco Monaco, Azienda Sanitaria Locale Salerno, Italy
David Shiers, The University of Manchester, United Kingdom
Copyright © 2023 Chin, Ghosh, Subramaniam and Beishon. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sudip Ghosh, c3VkaXAuZ2hvc2g0QG5ocy5uZXQ=; Lucy Beishon, bGIzMzBAbGUuYWMudWs=
 Katherine Chin
Katherine Chin Sudip Ghosh
Sudip Ghosh Hari Subramaniam
Hari Subramaniam Lucy Beishon
Lucy Beishon