- 1Department of Psychiatry, University of Pittsburgh School of Medicine, Pittsburgh, PA, United States
- 2The Family Institute at Northwestern University, Evanston, IL, United States
Intervention strategies for those diagnosed with psychotic disorders such as schizophrenia can be effective in reducing symptoms and improving quality of life. While strides have been made in developing prevention and intervention strategies earlier on in the disease progression, among those at clinical high-risk (CHR) for psychosis, challenges with heterogeneity can limit symptom and diagnosis specific treatment. Here, we discuss a newly developed therapy skills group called the Skills Program for Awareness, Connectedness, and Empowerment (SPACE) that integrates different types of behavioral skills – standard and radically open dialectical behavioral therapy as well as cognitive behavioral therapy – for CHR youth between the ages of 13–18 years. With the diathesis-stress framework serving as a foundation, the intervention is divided into three stages. These stages target specific signs and symptoms contributing to the progression of CHR symptoms. Stage 1 targets stress (with the goal of developing awareness and reducing distress), stage 2 targets self-disturbances (with a goal of increasing self-connectedness), and stage 3 targets social connectedness (with a goal of improving social domains of functioning). The focus of this article is to introduce the theoretical framework underlying the pilot skills group and discuss ongoing progress.
Clinical Trial Registration: NCT05398120; https://clinicaltrials.gov/ct2/show/NCT05398120.
1. Introduction
Interventions for those diagnosed with psychotic disorders are well-known, with standard approaches including psychotropic medication, psychosocial treatments, exercise, and family-based interventions (1–6). While these interventions are critical for this group, there are benefits in taking a more developmental approach, intervening before the emergence of psychosis. Individuals at clinical high-risk (CHR) for developing psychosis show signs and symptoms suggestive of possible conversion to psychosis, with approximately 25% of these cases developing psychosis within a 2–3-year period [(7–9)]. This group tends to endorse positive symptoms (e.g., hearing whispers and seeing shadows), negative symptoms (i.e., reductions in motivations and behaviors), cognitive decline, high rates of comorbid diagnoses such as depression and anxiety, and impairments in social and role functioning (8–11). Importantly, no two individuals are alike in their clinical presentations, which can make applying interventions particularly challenging for this group (11). Yet, intervening early on in the course of psychosis progression can perhaps alter an individual’s psychological trajectory.
While psychosocial interventions for those with CHR syndrome have shown efficacy in reducing symptoms [(see 12)], there are still efforts needed to develop and refine interventions given some meta-analytic evidence suggesting an absence of robust effects (13). These findings could be related to several factors including a small number of registered clinical trials, research design and methodological issues, barriers due to mental health stigma, access to clinical care, and/or duration of untreated illness. Clinical heterogeneity, common in this group (11), may also be interfering with treatment progress. Clinical heterogeneity is the notion that individuals can experience unique clinical presentations and perhaps a one size fits all approach to treatment may not be effective (11, 14). For example, in the case of CHR symptoms, one individual may present with unusual thoughts, auditory perceptual aberrations, social anhedonia, and anxiety while another individual may present with visual perceptual aberrations, avolition, and depression.
Here, we discuss the conceptual framework and ongoing progress of a newly developed group intervention called the Skills Program for Awareness, Connectedness, and Empowerment (SPACE) that combines skills from established cognitive behavioral interventions. This integrative skills group may have the potential to address some of the challenges with clinical heterogeneity that can make applying effective treatments for CHR youth particularly difficult. The focus of the group is on common CHR symptoms that may contribute to the emergence of psychosis and/or other psychopathology over time that fall into the categories of (1) difficulty coping with stress (15–17), (2) impairments in self-connectedness (e.g., challenges with self-concept, negative beliefs about self, defeatist beliefs, disrupted identity formation) (18–21), and (3) social impairments (e.g., difficulties developing and maintaining relationships as well as loneliness) (10, 22–24). Furthermore, while this pilot study is a registered clinical trial that has begun recruitment, we hope to introduce this group in this article with the additional goal of incorporating feedback and input from the field in future iterations of the group design.
The three targets of our intervention - stress, self-connectedness, social connectedness - are expanded upon further below. We then introduce our conceptualization for the skills group. Following, group details are provided and then benefits, challenges, and considerations for future work/limitations are discussed.
1.1. Stress
Research investigating risk markers of psychosis conceptualize the etiology of psychosis from a diathesis-stress framework. This hallmark model suggests that interactions between genetics such as familial risk and acquired vulnerability such as prenatal insults can interact and form a constitutional vulnerability, termed the diathesis. Stressors (e.g., psychosocial stress, family environment, neighborhood deprivation, negative life events), and atypical neuro-maturational processes can interact with the diathesis, possibly contributing to the emergence of psychosis-risk symptoms and eventual transition over time (25–27). The updated neural diathesis-stress model suggests that those with a likelihood of developing psychosis may be more sensitive to stressors due to HPA axis abnormalities which can impact dopaminergic and glutamatergic pathways in the brain (25). In fact, elevated cortisol secretion, a correlate of stress reactivity, is suggested to contribute to the emergence of positive symptoms (26, 28). Similarly, higher levels of stress have been found to relate to depressive symptoms as well in this group (29). Individuals with CHR syndrome tend to exhibit less effective coping strategies (30–33) and tend to rate higher levels of stress from situations and events compared to those whose psychosis-risk symptoms remitted (33). This pattern is also present in those experiencing a worsening of symptoms longitudinally (34). Given adolescence is a time of change with increasing responsibilities and demands, and the importance of peer relationships and sensitivity to social related stress become more relevant, the ability to find effective ways to cope with stress is imperative. This need is further bolstered by evidence indicating that effective coping strategies are associated with less severe CHR symptoms (31).
1.2. Self-connectedness
Self-connectedness is a term that refers to the nature in which individuals feel connected to and understand themselves. There are several factors that can contribute to and enhance self-connectedness. This includes understanding one’s experiences, challenging negative self-talk and defeatist performance beliefs, identifying areas that bring meaning and purpose to one’s life through pinpointing values, and improving self-esteem. The way individuals view and understand themselves and their experiences has been of research and clinical interest for decades (35) and is gaining increasing attention in those at risk for psychotic disorders. For example, there is evidence that individuals with CHR syndrome report more negative beliefs about themselves when compared to their typically developing peers (17). Additionally, there is evidence of more defeatist performance beliefs which refer to negative beliefs about one’s abilities to perform in goal-directed activities (36). Drawing from traditional cognitive behavioral models (37), when reinforced and repeated, these beliefs may contribute to the emergence of negative symptoms (i.e., reductions in emotions, behaviors, and motivation) which is a separate and independent dimension from positive symptoms. However, it is important to note that these beliefs are also related to positive symptoms and transition to psychosis. For example, one study of 765 individuals with CHR syndrome and 280 healthy controls found those that transitioned to psychosis tended to have more maladaptive negative self-schemas at the time of transition (38). Furthermore, there is evidence that endorsement of defeatist beliefs is related to neurocognitive impairment in patients with schizophrenia (37). Perhaps targeting neurocognitive impairment may decrease defeatist beliefs by increasing cognitive flexibility (e.g., the ability to flexibly evaluate and challenge thoughts). Altogether, teaching adolescents and young adults tools and techniques to improve their relationships with themselves may be useful and perhaps even a protective factor in the context of the pathogenesis of psychosis.
1.3. Social connectedness
Feeling integrated and having social relationships is critical for overall functioning and quality of life. It has been long established that social related impairments are characteristic of those with CHR syndrome (10, 22, 39, 40). For example, evidence suggests that those with CHR syndrome have fewer social relationships and report experiencing loneliness more often than typically developing peers (23). Furthermore, studies indicate that those with CHR syndrome tend to have lower levels of social support and are overall more isolated (10, 29). Social support predicts clinical course in CHR groups [(e.g., 23, 29)]. Social connectedness could reduce stress and protect an individual from poor clinical outcomes such as worsening of positive symptoms and transition to psychosis. Interestingly and of relevance to the current group skills intervention, it is perhaps possible that challenges with emotional awareness and regulation may be one mechanism underlying these difficulties (41). Social functioning is a predictor of conversion to psychosis (42) which highlights the importance of targeting social domains in this group. It is also possible that comorbid diagnoses such as depression and anxiety disorders interfere with social functioning and further reinforce social isolation and withdrawal (43–47). Additionally, with the accumulating evidence pointing towards increased rates of bullying among this group (48–51), there may be opportunities to refine social related interventions that can target a range of social skills. For example, perhaps training in both verbal and nonverbal social signaling could be useful, as others have shown with social-cognitive interventions such as Cognitive Enhancement Therapy (52). Social development is critical during adolescence and young adulthood period as these skills may influence several domains of functioning throughout one’s life. Social connectedness and support may also serve as a means to reduce stress and as a result, may protect an individual from later psychopathology.
1.4. Psychosocial treatments
Current early intervention strategies for CHR youth include cognitive behavioral therapy (CBT) implemented in both individual and group formats (12). CBT applied to those with CHR syndrome draw heavily from the already developed and established CBT intervention for psychosis (53). CBT models tailored for this population may be especially well-suited to address positive symptoms by providing targeted psychoeducation and directly addressing interpretations of unusual experiences by considering the role of thoughts, feelings, and behavior patterns. To date, there is some evidence for the efficacy of CBT in CHR groups. For example, in one study, Addington et al. (54) implemented CBT in a sample of 51 CHR individuals and observed improvements in positive symptoms, which are central and diagnostic of CHR. However, improvements were not observed in negative symptoms or social functioning. More recently, one group introduced a transdiagnostic cognitive-behavioral treatment for adolescents at high-risk for serious mental illness (schizophrenia and bipolar disorder) which has shown promise (55). Even so, work is needed to improve early intervention and prevention strategies. There may be utility in expanding intervention outcomes beyond transition rates to include additional targets and broadening skills taught in this context.
One novel set of intervention skills that has yet to be tested is the efficacy of dialectical behavioral therapy (DBT) group therapy skills for CHR youth. DBT, originally developed by Dr. Marsha Linehan (56), aims to reduce difficulties with several processes including emotion dysregulation and stress. Standard adult DBT skills have been adapted for adolescence as well (57). A related third-wave DBT intervention, Radically Open (RO) DBT, was recently developed for targeting excessive self-control or overcontrol that can contribute to challenges with social connectedness (58). Overcontrolled tendencies are transdiagnostic in nature and these characteristics include cognitive inflexibility, challenges with emotional expression, increased threat sensitivity, reduced reward processing, and loneliness. Since the development of both standard adult and adolescent DBT, and RO DBT, studies find the application of these interventions can lead to improvements in symptoms and outcomes (e.g., stress, interpersonal difficulties, regulating emotions, etc.) across different psychological disorders and processes (58–60). Both adult and adolescent standard and RO DBT target processes relevant to those with CHR syndrome (e.g., anxiety and depression, social impairment, threat sensitivity, emotional expression).
1.5. SPACE group
The SPACE group is a newly developed 21-week skills group that teaches individuals with a CHR syndrome skills to combat challenges with the described domains – stress, self-connectedness, and social connectedness. This group is a clinic-based pilot group expected to recruit a total of 16 individuals with a CHR syndrome (attrition is considered in this final, expected N; please also note N was decided based on current recruitment flow within the clinic). This group is not a randomized control trial (RCT) but is a naturalistic design which may enhance generalizability to other community clinic settings. Please see the “Methods and analysis” section below for more information regarding group details.
2. Methods and analysis
2.1. Aims and hypotheses
It is important to note that all hypotheses are exploratory given the focus on feasibility and the small sample size. Primary aims are to examine whether implementing a skills group as such is feasible by assessing measures such as dropout rates, weekly attendance, and group satisfaction surveys completed by both clinicians and group members. Secondary outcomes include examining changes in central symptom targets (e.g., stress, self-disturbances, and social connectedness). A third aim is to investigate whether there are changes in psychosis-risk conversion scores over the course of the group. A fourth aim is to investigate auxiliary symptoms that may be more indirectly targeted by the skills group (e.g., self-stigma, positive symptoms, negative symptoms, comorbid depression, and emotion dysregulation). With these aims, it is predicted that a skills group integrating components of different types of DBT (e.g., adolescent, RO) as well as CBT will be feasible. Furthermore, it is predicted that reductions in symptoms and increases in functioning will be observed following the intervention.
2.2. Participants
Individuals already receiving services at the Hope Team (website: https://www.hopeteam.pitt.edu) at the University of Pittsburgh Medical Center (Leadership Team: Drs. Leslie Horton, Lauren Bylsma, and Tushita Mayanil) are offered the option to participate in the skills group. Individuals are invited if they are between the ages of 13–18 years. The Hope Team provides individual therapy to those with CHR syndrome drawing on different therapeutic modalities but anchored primarily in CBT. Outcome data for the group are collected pre-post and midway intervention. Individuals can participate in the group if they meet for a CHR syndrome based on criteria outlined in the Structured Interview for Psychosis-Risk Syndromes (SIPS discussed below) (61, 62). This includes meeting criteria for brief intermittent psychotic syndrome (i.e., brief or intermittent frankly psychotic symptoms), attenuated positive symptom syndrome (i.e., recent attenuated positive symptoms), and/or genetic/schizotypal inclusion with deterioration in functioning. Individuals are excluded if they have a history of meeting criteria for a psychotic disorder or develop psychosis over the course of the group. Individuals are able to participate in the study if they have had exposure to CBT or DBT skills given that the skills in this group are adapted for CHR specific symptoms. As mentioned, the reason for this is to adopt a naturalistic design and enhance generalizability to other community settings in this iteration of the group. Furthermore, we collected information on whether individuals were on medications or were receiving additional therapeutic services, but this was not an exclusion criterion of the study. Caregivers are offered the option to participate in separate parent-specific sessions monthly which include discussion of the skills and how parents can help to strengthen and generalize skills. Parents are also asked to complete occasional questionnaires. However, parent participation is not a requirement of the study. Given that this is a pilot study and to facilitate recruitment flow, the group format is rolling admission.
2.3. SPACE group stages
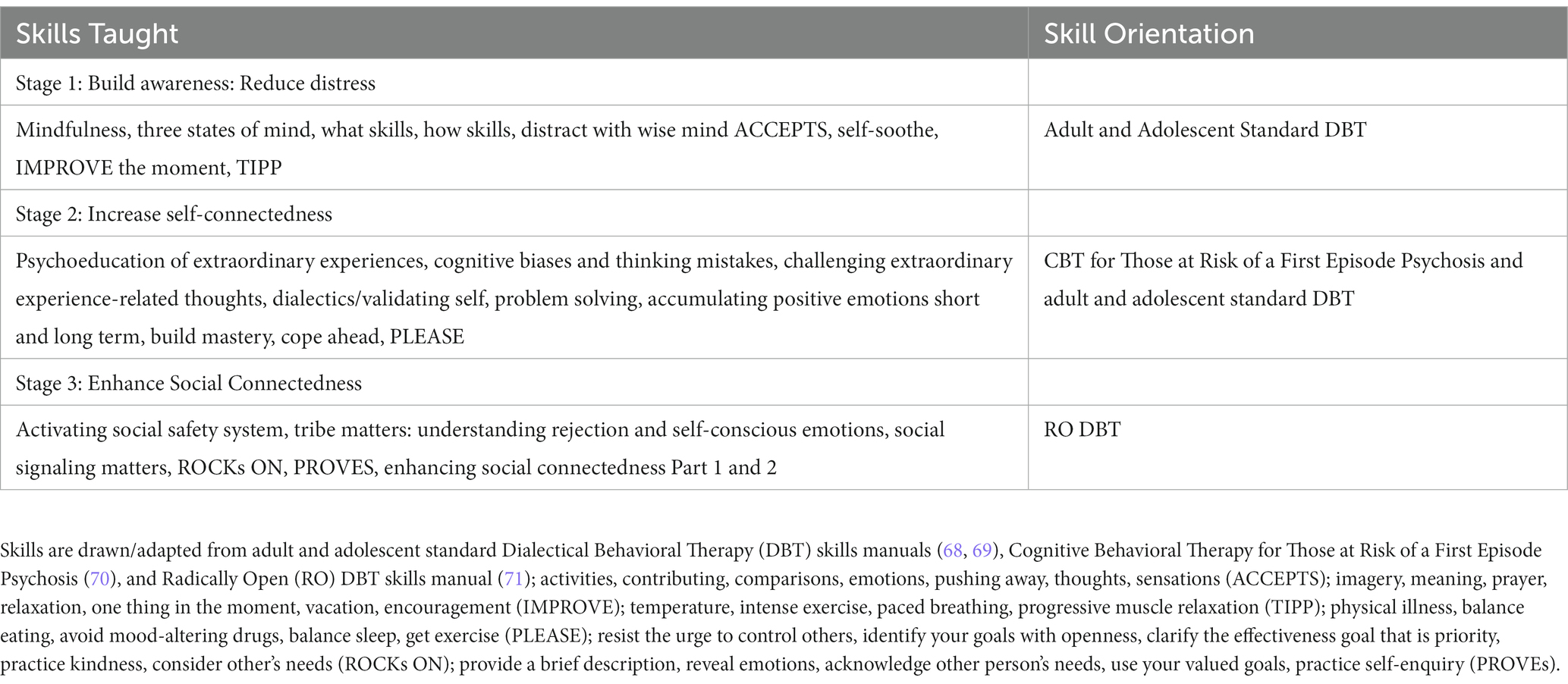
The group was developed drawing from the diathesis stress model (27) including modern conceptualizations of this framework (63) and considering disease driving disease driving mechanisms that contribute to worsening of symptoms. Furthermore, this group was developed in an effort to integrate evidence-based practices that currently exist for a range of targeted symptoms to address heterogeneity. The group is structured keeping traditional DBT skills group formats as a foundation, with mindfulness in the beginning of the group therapy session, followed by home practice review, and ending with new skills teaching and new home practice assignment. The group includes three stages that are approximately 7 weeks each and are intended to target specific disease mechanisms (see Figure 1). In the first stage, which draws from adult and adolescent standard DBT skills (e.g., mindfulness, distress tolerance skills), the goal is for an individual to develop an awareness of their own experiences and reduce challenges managing and coping with stress/anxiety. This includes acquiring skills such as mindfulness to help build awareness of experiences and learn to identify when one is feeling stress and intervene with appropriate distress tolerance skills. Importantly, if an individual is able to develop awareness of problematic experiences and reduce stress, then perhaps this individual may have more cognitive flexibility for stage 2 which is focused on increasing one’s self-connectedness through cognitive intervention. Stage 2 involves helping individuals to build awareness and understanding of experiences, focusing on ways to challenge unhelpful thinking patterns and defeatist beliefs, identify values, and improve problem solving skills to live more in line with one’s values. This stage integrates CBT skills (e.g., CHR psychoeducation, cognitive biases, thought records) (64) and components of adult and adolescent standard DBT’s emotion regulation module (e.g., problem solving, accumulating positive emotions). The third stage is built on the notion that once awareness is increased, stress is more effectively managed, and an individual has a stronger sense of their identity as well as more cognitive flexibility, they can “look outward” and focus on building skills to strengthen social connectedness. Stage 3 skills draw from RO DBT. This involves helping individuals to learn how to manage their social safety system when they feel threat activated in a social situation, understanding rejection, improving social signals, and strengthening interpersonal communication. Skills drawn from CBT/DBT are adapted to include discussions of how these skills can be useful for CHR symptoms specifically.
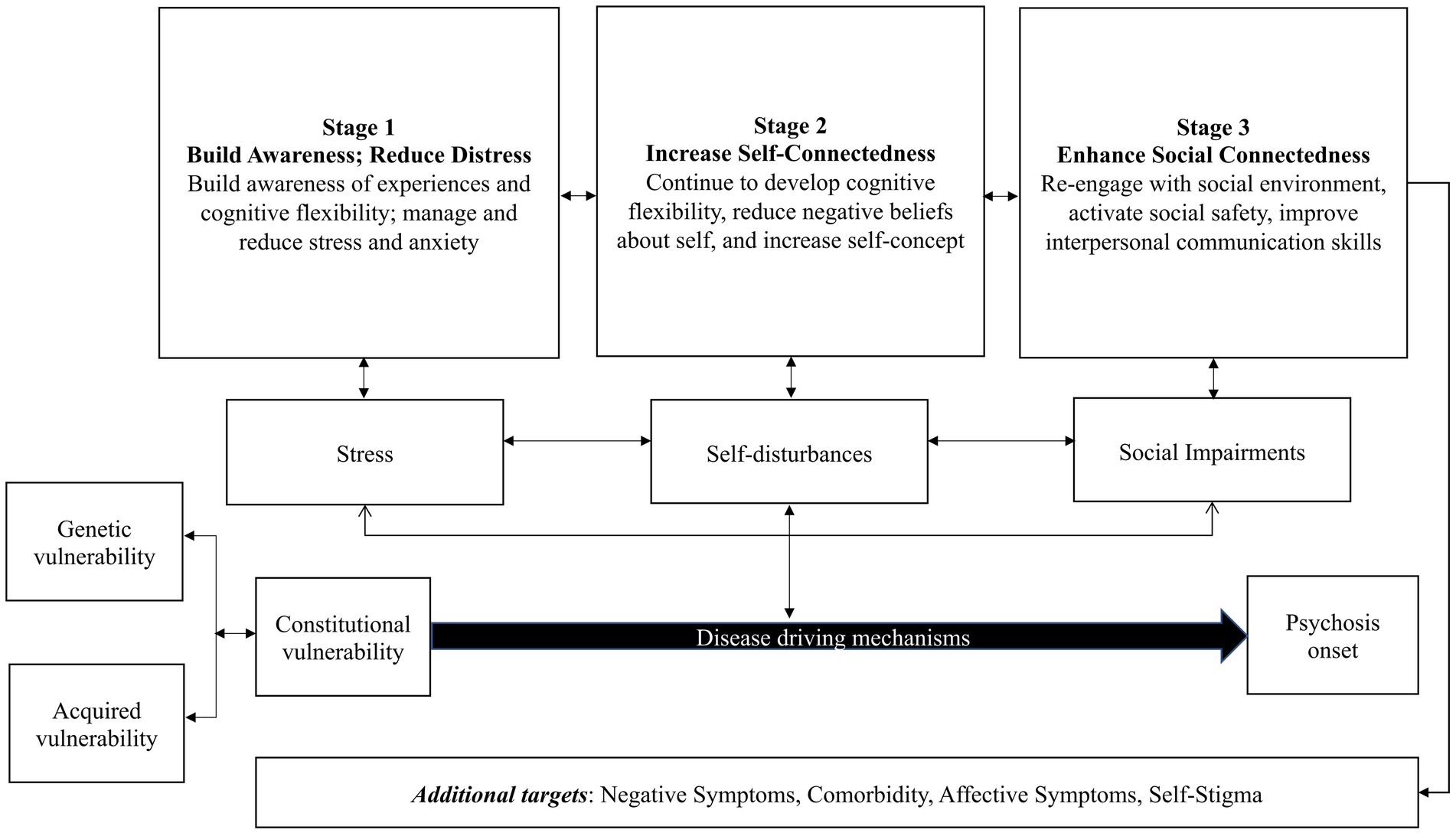
Figure 1. SPACE group conceptual model. The diathesis stress model posits that the onset of psychotic disorders such as schizophrenia can occur through the interaction between genetics and acquired vulnerability. This interaction can lead to a constitutional vulnerability, the diathesis, that can further interact with stress, self-disturbances, and social impairment, possible disease driving mechanisms (amongst others not listed here due to the focus of the framework). The conceptual framework suggests taking an integrative approach to group therapy by targeting stress, self-disturbances, and social impairments could be useful. Furthermore, integrating skills from standard Dialectical Behavioral Therapy [DBT; (68, 69)] such as mindfulness and distress tolerance skills (as in Stage 1 and 2), Cognitive Behavioral Therapy for those at Risk of a First Episode Psychosis [(70); as in Stage 2], and Radically Open DBT skills [(71); as in Stage 3] may address challenges with heterogeneity observed in treatment studies.
2.4. SPACE group details
The 21-week clinic-based skills group meets one time per week. This frequency was chosen in order to have a consistent schedule and also balance the need to ease participant burden because adolescents participating are often attending school and extracurricular activities and parents, who are often providing transportation, technological support, and encouragement are managing their own schedules as well (e.g., work). Furthermore, this weekly frequency is in line with some previous work (65, 66) although this is relatively understudied. Additionally, the use of standalone DBT skills is consistent with previous work in the literature (67). The group occurs on a weekday evening for 90 min. The group is a hybrid format which was developed with the feedback of members preferences to be virtual each week with one-monthly in-person session in place of one of the virtual sessions. While the goal was to be responsive to the group members feedback, it is important to acknowledge that there are limitations of the hybrid approach. For example, with the virtual session approach, there may be less group cohesion and engagement (e.g., turning off the camera, walking away from the screen) and increased distractions (e.g., urges to browse the internet, text). However, some benefits of virtual sessions include the ability for individuals to access care regardless of location. Please also note given the changing circumstances of the COVID-19 pandemic, we are working to incorporate more in-person sessions, with virtual as an option if needed for some members. Additionally, the group has 2–3 co-leader therapists. The group is structured so that it begins with a brief mindfulness practice, homework review, and ends with a new teaching. The new skill teaching involves integrating a balance of didactic (orienting as to why the skill is important and how it can help the target discussed), discussion (with an emphasis on how the skill can be useful for the CHR specific intervention target and symptoms), and skill practice. Throughout the skills group teachings, we refer to CHR experiences as “extraordinary experiences” in line with CBT interventions for this group (64). Furthermore, parent sessions occur monthly and involve reviewing the skills taught that month, discussing how parents can support skills strengthening and generalization, and problem solving any obstacles. Please see Figure 2 for skills group details.
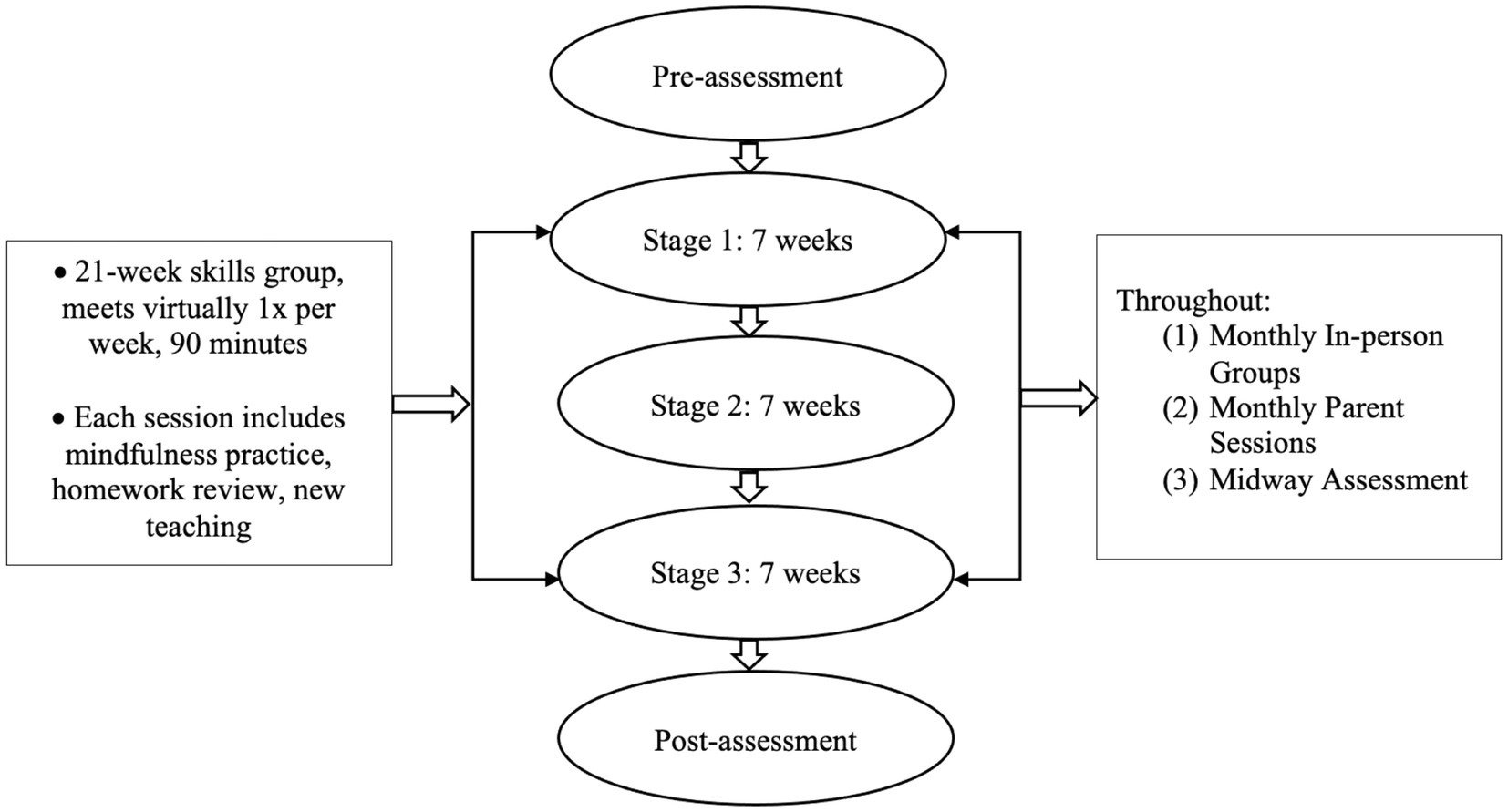
Figure 2. Schematic depicting SPACE group details. Stage 1 goal = Build Awareness; Reduce Distress, Stage 2 goal = Increase Self-Connectedness, Stage 3 goal = Enhance Social Connectedness.
An important point to discuss is the current group differs from DBT skills groups in many ways. For example, as mentioned, the current group draws from both standard and RO DBT in efforts to compile skills that could be useful for the targets discussed and the broader CHR syndrome. These skills are chosen based off of theoretical models (e.g., diathesis stress model) and the CHR literature. As a result and as shown in Table 1, not all DBT skills are implemented, making this group a DBT informed skills group. This is in efforts to keep the group focused and specific to CHR related symptoms (e.g., targets that are related to positive symptoms, clinical course, and/or transition to psychosis). Furthermore, the skills group does not utilize the interpersonal skills section from adult and adolescent standard DBT skills but instead draws from RO DBT to address the social connectedness target given the emphasis on threat activation with the RO approach. While DBT targets emotion dysregulation, this skills group is intended to target symptoms suggested to contribute to worsening of positive symptoms and/or transition to psychosis. Additionally, each skill taught in the group is anchored around discussions on how the skill can be useful for reducing CHR specific symptoms in the context of the noted domain (e.g., stage 1: reducing stress). For example, distress tolerance skills are discussed in the context of the diathesis stress model and the notion that stress can worsen CHR symptoms is emphasized in the teaching. A common discussion point is how to manage distress from CHR symptoms which is particularly relevant for stage 1. However, the challenges with managing distress from experiences extends beyond stage 1 and into the other two stages of the group (e.g., how to manage distress that interferes with self-connectedness and social connections).
2.5. Primary and secondary outcome measures
As mentioned, all individuals were assessed using the SIPS interview which is the diagnostic interview used to identify CHR syndromes (61, 62). In this interview, questions are asked assessing positive symptom domains (unusual thought content/delusional ideas, suspiciousness/persecutory ideas, grandiose ideas, perceptual abnormalities/hallucinations, disorganized communication). Examples of questions include Have you felt that you are not in control of your own ideas or thoughts? Do you ever feel your eyes are playing tricks on you?
Feasibility is assessed by collecting weekly information on attendance and group satisfaction (Modified Quick Lecomte & Leclerc Scale), group engagement and prosocial behaviors (Participation Scale) (72) and co-leader fidelity measures. Additional feasibility measures collected at baseline, midway, and post group include the Satisfaction with Therapy and Therapist Scale (73). Furthermore, group members and parents complete a brief group survey assessing motivation and goals across timepoints.
Secondary outcomes include direct targets of the group. First, different components of stress are assessed using the Perceived Stress Scale (74), Beck Anxiety Scale (75), Child and Adolescent Mindfulness Measure (76), and Avoidance and Fusion Questionnaire for Youth (77). Second, self-connectedness is assessed using the Defeatist Performance Attitudes measure (78), Cognitive Insight Scale (79), and self-stigma measure [Internalized Stigma of Mental Illness measure (80)]. A test of cognition is collected as well - the Hopkins Verbal Learning Test Revised (81) – in order to assess cognitive changes from learning skills in this section (e.g., cognitive restructuring). Third, social connectedness is measured using the Social and Role Functioning scale (82), and (the Social Connectedness Scale) (83).
Other outcomes include negative symptoms (Negative Symptom Inventory – Psychosis-Risk; (84)), depression [Beck Depression Inventory (85)], NAPLS psychosis risk calculator scores (86), quality of life [Lehman Quality of Life Functional Assessment, (87)], positive symptoms [SIPS, Prodromal Questionnaire (88)], emotion regulation [Emotion Regulation Scale, (89)], trauma [Child Trauma Questionnaire (90)], and coping styles [Youth Over and Undercontrol Measure, (58)]. Please note understanding symptoms such as negative symptoms and depressive changes in response to the intervention can inform our understanding of areas of convergence and divergence between the two constructs, which is an ongoing research question in the field (17, 91–93).
2.6. Statistical considerations and data analysis plan
Given this is a novel, pilot intervention, the current analyses will be exploratory in nature. Linear mixed-effects models, which will account for attrition, will be used to assess changes within each stage and changes over time in behavioral measures; timepoints are baseline, midway, and post-intervention.
2.7. Trial status
Recruitment for baseline assessments began April 26th, 2022. The first group session occurred May 10th, 2022, and at the time of re-submission, the group is in round 2 of stage 1 teachings. Currently, there are 5 active members in the group. Additionally, there have been a total of 6 caregiver sessions. Generally, the current sample of individuals are white, younger adolescents endorsing moderate to moderate–severe levels of positive symptoms, and moderate to average levels of social and role functioning.
3. Discussion
As discussed, this group intervention has the ability to target signs and symptoms (i.e., stress, challenges with self-connectedness, and impairments in social connectedness) contributing to worsening of symptoms or even possible conversion to psychosis. However, there are additional benefits, possible challenges, and considerations for future directions that are useful to discuss which will be the focus of this next section.
3.1. Possible benefits
A possible benefit of the skills intervention is the integration of different behavioral skills that are useful for improving many different psychological processes. DBT skills groups are effective for a wide range of psychiatric illnesses including adults and adolescents with suicidal and self-injurious behaviors, those with eating disorders (94), individuals struggling with addictive behaviors among those with alcohol use disorder (95), and individuals with anxiety and depressive disorders (96–99). The breadth of symptoms DBT may address is particularly relevant for those with a CHR syndrome given that this group, as mentioned, is characterized by unique clinical presentations. Additionally, emotion dysregulation and suicidality are characteristic of some individuals that are identified with the CHR syndrome which DBT is effective for improving (100–105). Furthermore, there is evidence that CBT skills are effective for those with CHR syndrome, with a recent systematic review and meta-analysis (106) suggesting reductions in transition rates and positive symptoms. However, there were no beneficial effects for functioning, depression, quality of life, and distress. While not all behavioral skills are beneficial for each individual with CHR syndrome, the wide range of skills taught in this intervention can allow for one to form a “toolbox,” pulling skills that fit an individual’s needs.
Furthermore, these pilot data have the ability to contribute to the growing literature examining the efficacy of RO DBT for adolescents. As mentioned, RO DBT is intended to target processes related to excessive self-control or overcontrol (58). The emphasis on developing skills to enhance social connectedness could be useful for those with CHR syndrome given this group’s social related impairments. A major component of the theory underlying RO DBT is that heightened threat sensitivity can make it more difficult for an individual to enter a social-safety neurobiological system, and engage in prosocial behaviors (58). This heightened sense of stress and threat sensitivity can emerge due to perceptual abnormalities, unusual thoughts, and/or suspicious beliefs, which could contribute to isolation and social withdrawal (25). Thus, there may be skills specifically targeting the stress and the social safety system (e.g., skills to socially signal openness) that could be useful to draw from RO DBT for this group that can enhance social functions. This could be particularly the case given that social signaling is the main mechanism of change in RO DBT (60). However, while RO DBT skills have shown efficacy for treating disorders such as depression and eating disorders, (58, 98) there is still more research underway in which these data have the potential to contribute to particularly given the transdiagnostic nature of these skills. Furthermore, while there is a growing body of evidence applying RO DBT to adolescents (59, 107), there is more work needed.
It is also possible that this skills group may indirectly target insight and strengthen awareness. The ability to change experiences perhaps begins with having awareness of thoughts, emotions, and behaviors. One critical benefit of mindfulness skills is the ability for one to strengthen awareness of experiences. There is evidence that mindfulness interventions are effective in those diagnosed with psychotic disorders such as schizophrenia for a variety of reasons including helping to facilitate relaxation, reduce stress, and decrease symptoms (108–110). While mindfulness skills and interventions are not well understood in terms of efficacy for individuals with CHR syndrome, there are some pilot studies suggesting integrating mindfulness is feasible in this group (108).
This group could also have beneficial impacts on self-stigma. Adolescence can be an isolating time and individuals may be further isolated by experiences that are different from their peers. There are debates as well as to whether early intervention, in general, may perhaps lead an individual to label themselves in unhelpful ways (111). However, there is also work to suggest that risk communication outweigh these risks (112). Even so, the group format, as opposed to individual therapy alone, can be useful in reducing self-stigma. Self-stigma is a barrier to recovery among those with psychotic disorders but is not well understood before onset (113). Of the work that does exist, there is evidence suggesting that those with CHR syndrome may experience shame related to symptoms (113). Discussing and sharing symptoms with others that may have similar experiences could help to reduce self-stigma, increase feelings of validation, and even foster a sense of resiliency. Furthermore, the use of parent sessions is intended to also provide psychoeducation and support around adolescent group participation; parent participation may also be a path towards breaking down barriers related to self-stigma through increased understanding and communication.
The hybrid approach, in which in-person and telehealth groups are alternated or offered simultaneously, may be useful to combat challenges with access to care. This group intervention has the ability to inform this growing area of research. While the COVID-19 pandemic has caused several challenges, the ability to provide interventions virtually has increased access to treatments and interventions (due to transportation, time constraints, work and school schedules etc.) to those who may otherwise be unable to access in-person treatment. It is important to note that the virtual approach to therapy also has challenges such as assuming individuals have access to a laptop, computer, or phone. This is an area of investigation in which further research is warranted.
3.2. Current challenges
While there are many benefits to the group, there are challenges we have encountered which we will discuss now and describe some possible solutions that may be useful for other group interventions to consider. First, recruiting individuals with a CHR syndrome can be difficult. Although we are an established clinic which focuses on CHR assessment and intervention and receive regular referrals from the community, there is a greater lack of psychoeducation about the CHR syndrome in the larger social systems including schools, mental health providers, and family, thus, it can be difficult to recruit group members with CHR symptoms. Furthermore, stigma can hinder recruitment as well. One possible solution for this challenge is using rolling admission, which we have implemented, to maximize group recruitment. An additional challenge we have encountered is that there are times in which group members may need higher levels of care and their participation in this study is no longer appropriate. Relatedly, although a participant is identified as having a CHR syndrome, difficulties related to the central targets of the intervention and/or CHR symptoms may not be the primary concern. For example, there may be more imminent diagnoses or concerns that require more comprehensive treatment (e.g., intensive outpatient). As this study is embedded within a larger health care system, we are able to smoothly facilitate this transition. Additionally, some individuals may feel uncomfortable in a group setting due to perhaps social anxiety, trauma, or paranoia related to their CHR status and other intervention may be necessary prior to or instead of participation.
Regarding challenges with running the group itself, group engagement can be difficult to establish with a new group. To address this, we have found weekly reminders, calendar print outs, and group reminder phone calls are some tools that can be useful. Furthermore, parent sessions are important in that we are able to provide psychoeducation to parents who can further support their adolescent’s group participation. Additionally, the maturity level of the group has fluctuated based on ages and cognitive abilities of those enrolled in group. Adapting and approaching the skills to meet the maturity and cognitive levels of participants is one strategy to combat this issue (e.g., using more basic language, asking members to paraphrase, using homework review to assess understanding of skills and provide feedback). There have also been hurdles related to using a hybrid format. First, there are sometimes technology issues (i.e., internet being slow for group members or leaders) which interfere with the flow of a session. Secondly, virtual formats can interfere with cohesion, as discussed, while in-person sessions, anecdotally, tend to have more active engagement, Interestingly, despite high rates of social anxiety in those with a CHR syndrome (44, 45), we have found that group members are more willing to participate in discussions and exercises as group cohesion and engagement is established over time and this is even more the case during in-person sessions.
3.3. Additional considerations for future work and limitations
While this study shows several strengths such as integrating different DBT skills (adult and adolescent standard and RO DBT), the use of a group format, and the targeting of central and auxiliary CHR symptoms in efforts to combat challenges with heterogeneity, there are important limitations to discuss for future work to consider. This includes the use of rolling admission. For the pilot nature of the study, there is rolling admission which means individuals can attend at any point in the group. While there are benefits to this approach such as allowing individuals to receive services immediately rather than having to wait until a certain module, there are drawbacks as well. For example, it may be the case that an individual joins during the self-connectedness module and does not get stage 1 first (e.g., skills for building awareness and reducing distress), thus reducing potential benefits to the ordering of stages suggested by our conceptual model. Furthermore, the hybrid approach may have limitations such as impacts on group cohesion. Additionally, this intervention does not have a comparison group; additional iterations of the group would benefit from a treatment as usual condition. Given that individuals may be receiving other services (e.g., therapy, medication management), and this is not standardized in this study due to pilot/feasibility nature of the approach, it is possible that any improvements may be due to other components of intervention instead of or in addition to group. Furthermore, while skills are being taught pulling from three different modalities, not all skills in each modality are being used which may impact any interpretations regarding the efficacy of DBT skills alone for this group. We also assess verbal memory as a means to understand changes in cognition from skills taught in the self-connectedness section. However, future work should consider applying a more comprehensive battery of cognitive tests.
The current study also includes volunteers from within an existing program which does mimic real-world practice but also limits generalizability (e.g., including individuals who are motivated to participate). Future research and iterations of the group would benefit from including individuals across different programs and perhaps also individuals not already embedded within a CHR clinic. It is also perhaps a limitation of the study that we included individuals on medications and those receiving other therapeutic services. While this is also a strength in that this increases the generalizability of findings, future groups would benefit from assessing medication use and how the intervention is impacted by individuals participating in other therapies. Importantly, our pilot intervention does include a wider age range of 13–18 which may also be a limitation to the study. This age range is in line with the age ranges in CHR studies (114, 115). Furthermore, while the intervention is intended to target clinical heterogeneity and we see this as a strength of this approach, targeting heterogeneity (e.g., taking a broader approach to intervention, teaching skills for several psychological processes) in the sample may also be a limitation that could impact recruitment and results. It is also noteworthy that we did not exclude individuals that have had previous exposure to CBT or DBT given that these skills are adapted to target CHR specific symptoms. However, future iterations of the group will consider the inclusion/exclusion of group members based on previous exposure to CBT and/or DBT modalities. Furthermore, while the intervention is intended to increase our understanding of many symptoms often endorsed by those with a CHR syndrome, it will be particularly important for future iterations of the intervention to examine the relationships between negative symptoms and depression in the context of intervention outcomes. Additional iterations would also benefit from including longer follow up durations of the intervention to examine the impacts of the intervention long-term, transition rates, and retention of skills. One additional important point to consider is that while the intervention focuses on distress, mood, and social functioning, our outcome measures include a battery of measures that assess for CHR symptom changes. While we do have measures assessing for general psychiatric morbidity, future iterations should consider adding more measures that assess psychological processes that are not necessarily unique and specific to CHR symptoms.
4. Conclusion
Few psychosocial interventions exist for those with a CHR syndrome. Given that CHR group are heterogenous in nature, one single intervention may not be effective for reducing central and auxiliary symptoms. Deriving from the diathesis-stress framework, we developed a group intervention, SPACE group, for adolescents and young adults ages 13–18 years, which focuses on building skills to reduce stress, increase self-connectedness, and enhance social connectedness. This group includes psychoeducation and integrates evidence-based skills from CBT and DBT to target specific signs and symptoms which are theorized to contribute to the progression of psychosis.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by University of Pittsburgh Institutional Review Board. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
TG, TM, LB, and LH developed the study concept and design in consultation with MM. TG drafted the article and all authors contributed to writing and revisions. All authors contributed to the article and approved the submitted version.
Funding
This work is supported by the Substance Abuse and Mental Health Services Administration (SAMHSA) CHR-P grant number H79SM081196 to the Pennsylvania Office of Mental Health and Substance Use Services (OMHSAS) and T32MH018269 to TG and T32MH018951 to LA.
Acknowledgments
We would like to acknowledge the therapists helping to lead this intervention. Additionally, we would like to acknowledge the families participating in this pilot study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Firth, J, Cotter, J, Elliott, R, French, P, and Yung, AR. A systematic review and meta-analysis of exercise interventions in schizophrenia patients. Psychol Med. (2015) 45:1343–61. doi: 10.1017/S0033291714003110
2. Hooker, CI, Carol, EE, Eisenstein, TJ, Yin, H, Lincoln, SH, Tully, LM, et al. A pilot study of cognitive training in clinical high risk for psychosis: initial evidence of cognitive benefit. Schizophr Res. (2014) 157:314–6. doi: 10.1016/j.schres.2014.05.034
3. Kane, JM, and Correll, CU. Past and present Progress in the pharmacologic treatment of schizophrenia. J Clin Psychiatry. (2010) 71:1115–24. doi: 10.4088/JCP.10r06264yel
4. Kingdon, DG, and Turkington, D. Cognitive-behavioral therapy of schizophrenia, Cognitive-behavioral therapy of schizophrenia. New York, NY, US: Guilford Press (1994).
5. McFarlane, WR. Family interventions for schizophrenia and the psychoses: a review. Fam Process. (2016) 55:460–82. doi: 10.1111/famp.12235
6. Turner, DT, McGlanaghy, E, Cuijpers, P, van der Gaag, M, Karyotaki, E, and MacBeth, A. A meta-analysis of social skills training and related interventions for psychosis. Schizophr Bull. (2018) 44:475–91. doi: 10.1093/schbul/sbx146
7. Cannon, TD, Cadenhead, K, Cornblatt, B, Woods, SW, Addington, J, Walker, E, et al. Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Arch Gen Psychiatry. (2008) 65:28–37. doi: 10.1001/archgenpsychiatry.2007.3
8. Fusar-Poli, P, Borgwardt, S, Bechdolf, A, Addington, J, Riecher-Rössler, A, Schultze-Lutter, F, et al. The psychosis high-risk state. JAMA Psychiatry. (2013) 70:107–20. doi: 10.1001/jamapsychiatry.2013.269
9. Salazar de Pablo, G, Woods, SW, Drymonitou, G, de Diego, H, and Fusar-Poli, P. Prevalence of individuals at clinical high-risk of psychosis in the general population and clinical samples:systematic review and meta-analysis. Brain Sciences. (2021) 11:1544.
10. Addington, J, Penn, D, Woods, SW, Addington, D, and Perkins, DO. Social functioning in individuals at clinical high risk for psychosis. Schizophr Res. (2008) 99:119–24. doi: 10.1016/j.schres.2007.10.001
11. Fusar-Poli, P, Cappucciati, M, Borgwardt, S, Woods, SW, Addington, J, Nelson, B, et al. Heterogeneity of psychosis risk within individuals at clinical high risk: a meta-analytical stratification. JAMA Psychiatry. (2016) 73:113–20. doi: 10.1001/jamapsychiatry.2015.2324
12. Thompson, E, Millman, ZB, Okuzawa, N, Mittal, V, DeVylder, J, Skadberg, T, et al. Evidence-based early interventions for individuals at clinical high risk for psychosis: a review of treatment components. J Nerv Ment Dis. (2015) 203:342–51. doi: 10.1097/NMD.0000000000000287
13. Davies, C, Radua, J, Cipriani, A, Stahl, D, Provenzani, U, McGuire, P, et al. Efficacy and acceptability of interventions for attenuated positive psychotic symptoms in individuals at clinical high risk of psychosis: a network meta-analysis. Front Psychiatry. (2018) 9:187. doi: 10.3389/fpsyt.2018.00187
14. Gupta, T, and Mittal, VA. Advances in clinical staging, early intervention, and the prevention of psychosis. F1000Res. (2019) 8:2027. doi: 10.12688/f1000research.20346.1
15. Holtzman, CW, Trotman, HD, Goulding, SM, Ryan, AT, MacDonald, AN, Shapiro, DI, et al. Stress and neurodevelopmental processes in the emergence of psychosis. Neuroscience. (2013) 249:172–91. doi: 10.1016/j.neuroscience.2012.12.017
16. Myin-Germeys, I, and van Os, J. Stress-reactivity in psychosis: evidence for an affective pathway to psychosis. Clin Psychol Rev. (2007) 27:409–24. doi: 10.1016/j.cpr.2006.09.005
17. Valli, I, Crossley, NA, Day, F, Stone, J, Tognin, S, Mondelli, V, et al. HPA-axis function and grey matter volume reductions: imaging the diathesis-stress model in individuals at ultra-high risk of psychosis. Transl Psychiatry. (2016) 6:e797–7. doi: 10.1038/tp.2016.68
18. Cowan, HR, McAdams, DP, and Mittal, VA. Core beliefs in healthy youth and youth at ultra high-risk for psychosis: dimensionality and links to depression, anxiety, and attenuated psychotic symptoms. Dev Psychopathol. (2019) 31:379–92. doi: 10.1017/S0954579417001912
19. Koren, D, Reznik, N, Adres, M, Scheyer, R, Apter, A, Steinberg, T, et al. Disturbances of basic self and prodromal symptoms among non-psychotic help-seeking adolescents. Psychol Med. (2013) 43:1365–76. doi: 10.1017/S0033291712002322
20. Nelson, B, Thompson, A, Chanen, AM, Amminger, GP, and Yung, AR. Is basic self-disturbance in ultra-high risk for psychosis (‘prodromal’) patients associated with borderline personality pathology? Early Interv Psychiatry. (2013) 7:306–10. doi: 10.1111/eip.12011
21. Vaernes, TG, Rossberg, JI, and Moller, P. Anomalous self-experiences are strongly associated with negative symptoms in a clinical high-risk for psychosis sample. Compr Psychiatry. (2019) 93:65–72. doi: 10.1016/j.comppsych.2019.07.003
22. Blanchard, JJ, Mueser, KT, and Bellack, AS. Anhedonia, positive and negative affect, and social functioning in schizophrenia. Schizophr Bull. (1998) 24:413–24. doi: 10.1093/oxfordjournals.schbul.a033336
23. Hooker, C, and Park, S. Emotion processing and its relationship to social functioning in schizophrenia patients. Psychiatry Res. (2002) 112:41–50. doi: 10.1016/S0165-1781(02)00177-4
24. Robustelli, BL, Newberry, RE, Whisman, MA, and Mittal, VA. Social relationships in young adults at ultra high risk for psychosis. Psychiatry Res. (2017) 247:345–51. doi: 10.1016/j.psychres.2016.12.008
25. Pruessner, M, Cullen, AE, Aas, M, and Walker, EF. The neural diathesis-stress model of schizophrenia revisited: An update on recent findings considering illness stage and neurobiological and methodological complexities. Neurosci Biobehav Rev. (2017) 73:191–218. doi: 10.1016/j.neubiorev.2016.12.013
26. Walker, E, Mittal, V, and Tessner, K. Stress and the hypothalamic pituitary adrenal axis in the developmental course of schizophrenia. Annu Rev Clin Psychol. (2008) 4:189–216. doi: 10.1146/annurev.clinpsy.4.022007.141248
27. Walker, EF, and Diforio, D. Schizophrenia: a neural diathesis-stress model. Psychol Rev. (1997) 104:667–85. doi: 10.1037/0033-295X.104.4.667
28. Corcoran, C, Malaspina, D, Goetz, R, Gil, R, Gorman, J, and McEwen, B. Elements of the stress cascade and the neurobiology of schizophrenia. Schizophr Res. (2003) 60:13. doi: 10.1016/S0920-9964(03)80037-3
29. Pruessner, M, Iyer, SN, Faridi, K, Joober, R, and Malla, AK. Stress and protective factors in individuals at ultra-high risk for psychosis, first episode psychosis and healthy controls. Schizophr Res. (2011) 129:29–35. doi: 10.1016/j.schres.2011.03.022
30. DeVylder, JE, Ben-David, S, Schobel, SA, Kimhy, D, Malaspina, D, and Corcoran, CM. Temporal association of stress sensitivity and symptoms in individuals at clinical high risk for psychosis. Psychol Med. (2013) 43:259–68. doi: 10.1017/S0033291712001262
31. Jalbrzikowski, M, Sugar, CA, Zinberg, J, Bachman, P, Cannon, TD, and Bearden, CE. Coping styles of individuals at clinical high risk for developing psychosis. Early Interv Psychiatry. (2014) 8:68–76. doi: 10.1111/eip.12005
32. Nordholm, D, Rostrup, E, Mondelli, V, Randers, L, Nielsen, MØ, Wulff, S, et al. Multiple measures of HPA axis function in ultra high risk and first-episode schizophrenia patients. Psychoneuroendocrinology. (2018) 92:72–80. doi: 10.1016/j.psyneuen.2018.03.015
33. Trotman, HD, Holtzman, CW, Walker, EF, Addington, JM, Bearden, CE, Cadenhead, KS, et al. Stress exposure and sensitivity in the clinical high-risk syndrome: initial findings from the North American Prodrome longitudinal study (NAPLS). Schizophr Res. (2014) 160:104–9. doi: 10.1016/j.schres.2014.09.017
34. Ristanovic, I, Vargas, T, Cowan, HR, and Mittal, VA. Consistent exposure to psychosocial stressors and progressive intolerance to stress in individuals at clinical high risk for psychosis. Schizophrenia Bull Open. (2020) 1:sgaa004. doi: 10.1093/schizbullopen/sgaa004
35. Rogers, AH. The self concept in paranoid schizophrenia. J Clin Psychol. (1958) 14:365–6. doi: 10.1002/1097-4679(195810)14:4<365::AID-JCLP2270140406>3.0.CO;2-0
36. Clay, KB, Raugh, IM, Bartolomeo, LA, and Strauss, GP. Defeatist performance beliefs in individuals at clinical high-risk for psychosis and outpatients with chronic schizophrenia. Early Interv Psychiatry. (2021) 15:865–73. doi: 10.1111/eip.13024
37. Grant, PM, and Beck, AT. Defeatist beliefs as a mediator of cognitive impairment, negative symptoms, and functioning in schizophrenia. Schizophr Bull. (2009) 35:798–806. doi: 10.1093/schbul/sbn008
38. Stowkowy, J, Liu, L, Cadenhead, KS, Cannon, TD, Cornblatt, BA, McGlashan, TH, et al. Core schemas in youth at clinical high risk for psychosis. Behav Cogn Psychother. (2016) 44:203–13. doi: 10.1017/S1352465815000144
39. Ahmed, AO, Strauss, GP, Buchanan, RW, Kirkpatrick, B, and Carpenter, WT. Schizophrenia heterogeneity revisited: clinical, cognitive, and psychosocial correlates of statistically-derived negative symptoms subgroups. J Psychiatr Res. (2018) 97:8–15. doi: 10.1016/j.jpsychires.2017.11.004
40. Barbato, M, Liu, L, Cadenhead, KS, Cannon, TD, Cornblatt, BA, McGlashan, TH, et al. Theory of mind, emotion recognition and social perception in individuals at clinical high risk for psychosis: findings from the NAPLS-2 cohort. Schizophrenia Res: Cogn. (2015) 2:133–9. doi: 10.1016/j.scog.2015.04.004
41. Kimhy, D, Ferreira, K, Brucato, G, Vakhrusheva, J, Arendt, L, Gross, J, et al. The impact of emotion awareness and regulation on social functioning in individuals at clinical high-risk for psychosis. Psychol Med. (2016) 46:2907–18. doi: 10.1017/S0033291716000490
42. Fusar-Poli, P, Bonoldi, I, Yung, AR, Borgwardt, S, Kempton, MJ, Valmaggia, L, et al. Predicting psychosis. Arch Gen Psychiatry. (2012) 69:220–9. doi: 10.1001/archgenpsychiatry.2011.1472
43. Addington, J, Farris, M, Stowkowy, J, Santesteban-Echarri, O, Metzak, P, and Kalathil, MS. Predictors of transition to psychosis in individuals at clinical high risk. Curr Psychiatry Rep. (2019) 21:39. doi: 10.1007/s11920-019-1027-y
44. Deng, W., Addington, J., Bearden, C.E., Cadenhead, K.S., Cornblatt, B.A., Mathalon, D.H., et al. (2022). Characterizing sustained social anxiety in individuals at clinical high risk for psychosis: trajectory, risk factors, and functional outcomes. Psychol Med. doi: 10.1017/S0033291722000277, 1–8 [Epub ahead of print].
45. Kuhney, FS, Damme, KSF, Pelletier-Baldelli, A, Chun, C, Ellman, LM, Schiffman, J, et al. Prevalence and functional consequences of social anxiety in individuals at clinical high-risk for psychosis: perspective from a community sample comparison. Schizophrenia Bull Open. (2021) 2:sgab025. doi: 10.1093/schizbullopen/sgab025
46. McAusland, L, Buchy, L, Cadenhead, KS, Cannon, TD, Cornblatt, BA, Heinssen, R, et al. Anxiety in youth at clinical high risk for psychosis. Early Interv Psychiatry. (2017) 11:480–7. doi: 10.1111/eip.12274
47. Santesteban-Echarri, O, Liu, L, Cadenhead, KS, Tsuang, MT, Cannon, TD, Cornblatt, BA, et al. Anxiety in youth at clinical high-risk for psychosis: a two-year follow-up. Schizophr Res. (2021) 236:87–8. doi: 10.1016/j.schres.2021.08.014
48. Braun, A, Liu, L, Bearden, CE, Cadenhead, KS, Cornblatt, BA, Keshavan, M, et al. Bullying in clinical high risk for psychosis participants from the NAPLS-3 cohort. Soc Psychiatry Psychiatr Epidemiol. (2022) 57:1379–88. doi: 10.1007/s00127-022-02239-5
49. Magaud, E, Nyman, K, and Addington, J. Cyberbullying in those at clinical high risk for psychosis. Early Interv Psychiatry. (2013) 7:427–30. doi: 10.1111/eip.12013
50. Valmaggia, LR, Day, FL, Kroll, J, Laing, J, Byrne, M, Fusar-Poli, P, et al. Bullying victimisation and paranoid ideation in people at ultra high risk for psychosis. Schizophr Res. (2015) 168:68–73. doi: 10.1016/j.schres.2015.08.029
51. Vargas, T, Damme, KS, and Mittal, VA. Bullying victimization in typically developing and clinical high risk (CHR) adolescents: a multimodal imaging study. Schizophr Res. (2019) 213:40–7. doi: 10.1016/j.schres.2018.11.017
52. Friedman-Yakoobian, MS, Parrish, EM, Eack, SM, and Keshavan, MS. Neurocognitive and social cognitive training for youth at clinical high risk (CHR) for psychosis: a randomized controlled feasibility trial. Schizophr Res. (2022) 243:302–6. doi: 10.1016/j.schres.2020.09.005
53. Turner, DT, van der Gaag, M, Karyotaki, E, and Cuijpers, P. Psychological interventions for psychosis: a meta-analysis of comparative outcome studies. AJP. (2014) 171:523–38. doi: 10.1176/appi.ajp.2013.13081159
54. Addington, J, Epstein, I, Liu, L, French, P, Boydell, KM, and Zipursky, RB. A randomized controlled trial of cognitive behavioral therapy for individuals at clinical high risk of psychosis. Schizophr Res. (2011) 125:54–61. doi: 10.1016/j.schres.2010.10.015
55. Weintraub, MJ, Zinberg, J, Bearden, CE, and Miklowitz, DJ. Applying a transdiagnostic cognitive-behavioral treatment to adolescents at high risk for serious mental illness: rationale and preliminary findings. Cogn Behav Pract. (2020) 27:202–14. doi: 10.1016/j.cbpra.2019.07.007
56. Linehan, MM, Schmidt, H III, Dimeff, LA, Craft, JC, Kanter, J, and Comtois, KA. Dialectical behavior therapy for patients with borderline personality disorder and drug-dependence. Am J Addict. (1999) 8:279–92. doi: 10.1080/105504999305686
57. Rathus, JH, and Miller, AL. Dialectical behavior therapy adapted for suicidal adolescents. Suicide Life Threat Behav. (2002) 32:146–57. doi: 10.1521/suli.32.2.146.24399
58. Lynch, TR, Hempel, RJ, and Dunkley, C. Radically open-dialectical behavior therapy for disorders of over-control: signaling matters. APT. (2015) 69:141–62. doi: 10.1176/appi.psychotherapy.2015.69.2.141
59. Baudinet, J, Simic, M, Griffiths, H, Donnelly, C, Stewart, C, and Goddard, E. Targeting maladaptive overcontrol with radically open dialectical behaviour therapy in a day programme for adolescents with restrictive eating disorders: an uncontrolled case series. J Eat Disord. (2020) 8:68. doi: 10.1186/s40337-020-00338-9
60. Gilbert, K, Hall, K, and Codd, RT. Radically open dialectical behavior therapy: social signaling, transdiagnostic utility and current evidence. Psychol Res Behav Manag. (2020) 13:19–28. doi: 10.2147/PRBM.S201848
61. McGlashan, TH, Miller, TJ, Woods, SW, Rosen, JL, Hoffman, RE, and Davidson, L. Structured interview for prodromal syndromes. New Haven, CT: PRIME Research Clinic, Yale School of Medicine (2001).
62. Miller, TJ, McGlashan, TH, Rosen, JL, Cadenhead, K, Ventura, J, McFarlane, W, et al. Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, Interrater reliability, and training to reliability. Schizophr Bull. (2003) 29:703–15. doi: 10.1093/oxfordjournals.schbul.a007040
63. Gupta, T., Damme, K.S., Osborne, K.J., Vargas, T.G., Ristanovic, I., Frosch, I.R., et al. (2022). Comprehensive clinical psychology.
64. van der Gaag, M, Nieman, DH, Rietdijk, J, Dragt, S, Ising, HK, Klaassen, RMC, et al. Cognitive behavioral therapy for subjects at ultrahigh risk for developing psychosis: a randomized controlled clinical trial. Schizophr Bull. (2012) 38:1180–8. doi: 10.1093/schbul/sbs105
65. Lawlor, C, Vitoratou, S, Duffy, J, Cooper, B, De Souza, T, Le Boutillier, C, et al. Managing emotions in psychosis: evaluation of a brief DBT-informed skills group for individuals with psychosis in routine community services. Br J Clin Psychol. (2022) 61:735–56. doi: 10.1111/bjc.12359
66. Ritschel, LA, Guy, L, and Maddox, BB. A pilot study of dialectical behaviour therapy skills training for autistic adults. Behav Cogn Psychother. (2022) 50:187–202. doi: 10.1017/S1352465821000370
67. Valentine, SE, Bankoff, SM, Poulin, RM, Reidler, EB, and Pantalone, DW. The use of dialectical behavior therapy skills training as stand-alone treatment: a systematic review of the treatment outcome literature. J Clin Psychol. (2015) 71:1–20. doi: 10.1002/jclp.22114
70. Van der Gaag, M, Nieman, D, and Van den Berg, D. CBT for Those at Risk of a First Episode Psychosis: Evidence-based psychotherapy for people with an’At Risk Mental State’. Routledge (2013)
71. Lynch, TR. The Skills Training Manual for Radically Open Dialectical Behavior Therapy: A Clinician’s Guide for Treating Disorders of Overcontrol. New Harbinger Publications (2018)
72. Lecomte, T, Leclerc, C, and Wykes, T. Basic cognitive behavioral model used in group CBT for psychosis In: T Lecomte, C Leclerc, and T Wykes, editors. Group CBT for psychosis: A guidebook for clinicians : Oxford University Press (2016)
73. Oei, TP, and Green, A. The satisfaction with therapy and therapist scale-revised (STTS-R) for group psychotherapy: psychometric properties and confirmatory factor analysis. Prof Psychol Res Pract. (2008) 39:435–42. doi: 10.1037/0735-7028.39.4.435
74. Cohen, S, Kamarck, T, and Mermelstein, R. A global measure of perceived stress. J Health Soc Behav. (1983) 24:385. doi: 10.2307/2136404
75. Beck, AT, Brown, G, Kiyosaki, RT, and Lechter, SL. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. (1988) 56:893–7. doi: 10.1037/0022-006X.56.6.893
76. Greco, LA, Baer, RA, and Smith, GT. Assessing Mindfulness in Children and Adolescents: Development and Validation of the Child and Adolescent Mindfulness Measure (CAMM). Psychol Assess. (2011) 23:606–14. doi: 10.1037/a0022819
77. Greco, LA, Lambert, W, and Baer, RA. Psychological inflexibility in childhood and adolescence: development and evaluation of the avoidance and fusion questionnaire for youth. Psychol Assess. (2008) 20:93–102. doi: 10.1037/1040-3590.20.2.93
78. Cane, DB, Olinger, LJ, Gotlib, IH, and Kuiper, NA. Factor structure of the dysfunctional attitude scale in a student population. J Clin Psychol. (1986) 42:307–9. doi: 10.1002/1097-4679(198603)42:2<307::AID-JCLP2270420213>3.0.CO;2-J
79. Beck, AT, Baruch, E, Balter, JM, Steer, RA, and Warman, DM. A new instrument for measuring insight: the Beck cognitive insight scale. Schizophr Res. (2004) 68:319–29. doi: 10.1016/S0920-9964(03)00189-0
80. Boyd Ritsher, J, Otilingam, PG, and Grajales, M. Internalized stigma of mental illness: psychometric properties of a new measure. Psychiatry Res. (2003) 121:31–49. doi: 10.1016/j.psychres.2003.08.008
81. Keefe, RSE, Goldberg, TE, Harvey, PD, Gold, JM, Poe, MP, and Coughenour, L. The brief assessment of cognition in schizophrenia: reliability, sensitivity, and comparison with a standard neurocognitive battery. Schizophr Res. (2004) 68:283–97. doi: 10.1016/j.schres.2003.09.011
82. Cornblatt, BA, Auther, AM, Niendam, T, Smith, CW, Zinberg, J, Bearden, CE, et al. Preliminary findings for two new measures of social and role functioning in the prodromal phase of schizophrenia. Schizophr Bull. (2007) 33:688–702. doi: 10.1093/schbul/sbm029
83. Lee, R, and Robbins, S. Measuring belongingness: the social connectedness and the social assurance scales. J Couns Psychol. (1995) 42:232–41. doi: 10.1037/0022-0167.42.2.232
84. Strauss, GP, Pelletier-Baldelli, A, Visser, KF, Walker, EF, and Mittal, VA. A review of negative symptom assessment strategies in youth at clinical high-risk for psychosis. Schizophr Res. (2020) 222:104–12. doi: 10.1016/j.schres.2020.04.019
85. Beck, AT, Ward, CH, Mendelson, M, Mock, J, and Erbaugh, J. An inventory for measuring depression. Arch Gen Psychiatry. (1961) 4:561–71. doi: 10.1001/archpsyc.1961.01710120031004
86. Cannon, TD, Yu, C, Addington, J, Bearden, CE, Cadenhead, KS, Cornblatt, BA, et al. An individualized risk calculator for research in prodromal psychosis. Am J Psychiatr. (2016) 173:980–8. doi: 10.1176/appi.ajp.2016.15070890
87. Lehman, AF. A quality of life interview for the chronically mentally ill. Eval Program Plann. (1988) 11:51–62. doi: 10.1016/0149-7189(88)90033-X
88. Loewy, RL, Pearson, R, Vinogradov, S, Bearden, CE, and Cannon, TD. Psychosis risk screening with the prodromal questionnaire — brief version (PQ-B). Schizophr Res. (2011) 129:42–6. doi: 10.1016/j.schres.2011.03.029
89. Gross, JJ, and John, OP. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J Pers Soc Psychol. (2003) 85:348–62. doi: 10.1037/0022-3514.85.2.348
90. Bernstein, DP, Stein, JA, Newcomb, MD, Walker, E, Pogge, D, Ahluvalia, T, et al. Development and validation of a brief screening version of the childhood trauma questionnaire. Child Abuse Negl. (2003) 27:169–90. doi: 10.1016/S0145-2134(02)00541-0
91. Addington, J, Piskulic, D, Liu, L, Lockwood, J, Cadenhead, KS, Cannon, TD, et al. Comorbid diagnoses for youth at clinical high risk of psychosis. Schizophr Res. (2017) 190:90–5. doi: 10.1016/j.schres.2017.03.043
92. Gupta, T, Strauss, GP, Cowan, HR, Pelletier-Baldelli, A, Ellman, LM, Schiffman, J, et al. Secondary sources of negative symptoms in those meeting criteria for a clinical high-risk syndrome. Bio Psychiatry Glob Open Sci. (2021b) 1:210–8. doi: 10.1016/j.bpsgos.2021.05.008
93. Piskulic, D, Addington, J, Cadenhead, KS, Cannon, TD, Cornblatt, BA, Heinssen, R, et al. Negative symptoms in individuals at clinical high risk of psychosis. Psychiatry Res. (2012) 196:220–4. doi: 10.1016/j.psychres.2012.02.018
94. Peterson, CM, Van Diest, AMK, Mara, CA, and Matthews, A. Dialectical behavioral therapy skills group as an adjunct to family-based therapy in adolescents with restrictive eating disorders. Eat Disord. (2020) 28:67–79. doi: 10.1080/10640266.2019.1568101
95. Cavicchioli, M, Ramella, P, Vassena, G, Simone, G, Prudenziati, F, Sirtori, F, et al. Dialectical behaviour therapy skills training for the treatment of addictive behaviours among individuals with alcohol use disorder: the effect of emotion regulation and experiential avoidance. Am J Drug Alcohol Abuse. (2020) 46:368–84. doi: 10.1080/00952990.2020.1712411
96. Feldman, G, Harley, R, Kerrigan, M, Jacobo, M, and Fava, M. Change in emotional processing during a dialectical behavior therapy-based skills group for major depressive disorder. Behav Res Ther. (2009) 47:316–21. doi: 10.1016/j.brat.2009.01.005
97. Harley, R, Sprich, S, Safren, S, Jacobo, M, and Fava, M. Adaptation of dialectical behavior therapy skills training Group for Treatment-Resistant Depression. J Nerv Ment Dis. (2008) 196:136–43. doi: 10.1097/NMD.0b013e318162aa3f
98. Lynch, TR, Morse, JQ, Mendelson, T, and Robins, CJ. Dialectical behavior therapy for depressed older adults: a randomized pilot study. Am J Geriatr Psychiatry. (2003) 11:33–45. doi: 10.1097/00019442-200301000-00006
99. Malivoire, BL. Exploring DBT skills training as a treatment avenue for generalized anxiety disorder. Clin Psychol Sci Pract. (2020) 27:e12339. doi: 10.1111/cpsp.12339
100. Gill, KE, Quintero, JM, Poe, SL, Moreira, AD, Brucato, G, Corcoran, CM, et al. Assessing suicidal ideation in individuals at clinical high risk for psychosis. Schizophr Res. (2015) 165:152–6. doi: 10.1016/j.schres.2015.04.022
101. Loewy, RL, Corey, S, Amirfathi, F, Dabit, S, Fulford, D, Pearson, R, et al. Childhood trauma and clinical high risk for psychosis. Schizophrenia Res Childh Trauma Psychosis. (2019) 205:10–4. doi: 10.1016/j.schres.2018.05.003
102. Mayo, D, Corey, S, Kelly, LH, Yohannes, S, Youngquist, AL, Stuart, BK, et al. The role of trauma and stressful life events among individuals at clinical high risk for psychosis: a review. Front Psychiatry. (2017) 8:55. doi: 10.3389/fpsyt.2017.00055
103. Pelizza, L, Poletti, M, Azzali, S, Paterlini, F, Garlassi, S, Scazza, I, et al. Suicidal thinking and behavior in adolescents at ultra-high risk of psychosis: a two-year longitudinal study. Suicide Life Threat Behav. (2019) 49:1637–52. doi: 10.1111/sltb.12549
104. Thompson, JL, Kelly, M, Kimhy, D, Harkavy-Friedman, JM, Khan, S, Messinger, JW, et al. Childhood trauma and prodromal symptoms among individuals at clinical high risk for psychosis. Schizophr Res. (2009) 108:176–81. doi: 10.1016/j.schres.2008.12.005
105. Vines, L, Bridgwater, M, Bachman, P, Hayes, R, Catalano, S, and Jalbrzikowski, M. Elevated emotion reactivity and emotion regulation in individuals at clinical high risk for developing psychosis and those diagnosed with a psychotic disorder. Early Interv Psychiatry. (2022) 16:724–35. doi: 10.1111/eip.13212
106. Zheng, Y, Xu, T, Zhu, Y, Li, C, Wang, J, Livingstone, S, et al. Cognitive behavioral therapy for prodromal stage of psychosis—outcomes for transition, functioning, distress, and quality of life: a systematic review and meta-analysis. Schizophr Bull. (2022) 48:8–19. doi: 10.1093/schbul/sbab044
107. Baudinet, J, Stewart, C, Bennett, E, Konstantellou, A, Parham, R, Smith, K, et al. Radically open dialectical behaviour therapy adapted for adolescents: a case series. BMC Psychiatry. (2021) 21:462. doi: 10.1186/s12888-021-03460-3
108. Alvarez-Jimenez, M, Gleeson, JF, Bendall, S, Penn, DL, Yung, AR, Ryan, RM, et al. Enhancing social functioning in young people at ultra high risk (UHR) for psychosis: a pilot study of a novel strengths and mindfulness-based online social therapy. Schizophr Res. (2018) 202:369–77. doi: 10.1016/j.schres.2018.07.022
109. Johnson, DP, Penn, DL, Fredrickson, BL, Meyer, PS, Kring, AM, and Brantley, M. Loving-kindness meditation to enhance recovery from negative symptoms of schizophrenia. J Clin Psychol. (2009) 65:499–509. doi: 10.1002/jclp.20591
110. Tabak, NT, Horan, WP, and Green, MF. Mindfulness in schizophrenia: associations with self-reported motivation, emotion regulation, dysfunctional attitudes, and negative symptoms. Schizophr Res. (2015) 168:537–42. doi: 10.1016/j.schres.2015.07.030
111. Rüsch, N, Müller, M, Heekeren, K, Theodoridou, A, Metzler, S, Dvorsky, D, et al. Longitudinal course of self-labeling, stigma stress and well-being among young people at risk of psychosis. Schizophr Res. (2014) 158:82–4. doi: 10.1016/j.schres.2014.07.016
112. Schiffman, J, Horton, LE, Landa, Y, and Woods, SW. Considerations for providing feedback to patients and families regarding clinical high-risk for psychosis status. Schizophr Res. (2022) 244:55–7. doi: 10.1016/j.schres.2022.01.059
113. Ho, RWH, Chang, WC, Kwong, VWY, Lau, ESK, Chan, GHK, Jim, OTT, et al. Prediction of self-stigma in early psychosis: 3-year follow-up of the randomized-controlled trial on extended early intervention. Schizophr Res. (2018) 195:463–8. doi: 10.1016/j.schres.2017.09.004
114. Mei, C, van der Gaag, M, Nelson, B, Smit, F, Yuen, HP, Berger, M, et al. Preventive interventions for individuals at ultra high risk for psychosis: An updated and extended meta-analysis. Clin Psychol Rev. (2021) 86:102005. doi: 10.1016/j.cpr.2021.102005
115. Worthington, MA, Miklowitz, DJ, O’Brien, M, Addington, J, Bearden, CE, Cadenhead, KS, et al. Selection for psychosocial treatment for youth at clinical high risk for psychosis based on the north American Prodrome longitudinal study individualized risk calculator. Early Interv Psychiatry. (2021) 15:96–103. doi: 10.1111/eip.12914
Keywords: clinical high-risk, psychosis-risk, group therapy, integrative skills group, heterogeneity, dialectical behavioral therapy
Citation: Gupta T, Antezana L, Porter C, Mayanil T, Bylsma LM, Maslar M and Horton LE (2023) Skills program for awareness, connectedness, and empowerment: A conceptual framework of a skills group for individuals with a psychosis-risk syndrome. Front. Psychiatry. 14:1083368. doi: 10.3389/fpsyt.2023.1083368
Edited by:
Rishab Gupta, Brigham and Women's Hospital, Harvard Medical School, United StatesReviewed by:
Vijay Krishnan, All India Institute of Medical Sciences, Rishikesh, IndiaAditya Kumar Singh Pawar, Johns Hopkins Medicine, Johns Hopkins University, United States
Copyright © 2023 Gupta, Antezana, Porter, Mayanil, Bylsma, Maslar and Horton. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tina Gupta, Z3VwdGF0M0B1cG1jLmVkdQ==
 Tina Gupta
Tina Gupta Ligia Antezana
Ligia Antezana Christian Porter1
Christian Porter1 Lauren M. Bylsma
Lauren M. Bylsma