- 1Department of Psychiatry, Center for Addiction Medicine (CAM), Massachusetts General Hospital (MGH), Boston, MA, United States
- 2Department of Psychiatry, Harvard Medical School, Boston, MA, United States
- 3Athinoula A. Martinos Center for Biomedical Imaging, Department of Radiology, Massachusetts General Hospital (MGH), Harvard Medical School, Charlestown, MA, United States
Background: Evidence for long-term effectiveness of commercial cannabis products used to treat medical symptoms is inconsistent, despite increasingly widespread use.
Objective: To prospectively evaluate the effects of using cannabis on self-reported symptoms of pain, insomnia, anxiety, depression, and cannabis use disorder (CUD) after 12 months of use.
Methods: This observational cohort study describes outcomes over 9 months following a 12-week randomized, waitlist-controlled trial (RCT: NCT03224468) in which adults (N = 163) who wished to use cannabis to alleviate insomnia, pain, depression, or anxiety symptoms were randomly assigned to obtain a medical marijuana card immediately (immediate card acquisition group) or to delay obtaining a card for 12 weeks delay (delayed card acquisition group). During the 9-month post-randomization period, all participants could use cannabis as they wished and choose their cannabis products, doses, and frequency of use. Insomnia, pain, depression, anxiety, and CUD symptoms were assessed over the 9-month post-randomization period.
Results: After 12 months of using cannabis for medical symptoms, 11.7% of all participants (n = 19), and 17.1% of those using cannabis daily or near-daily (n = 6) developed CUD. Frequency of cannabis use was positively correlated with pain severity and number of CUD symptoms, but not significantly associated with severity of self-reported insomnia, depression, or anxiety symptoms. Depression scores improved throughout the 9 months in all participants, regardless of cannabis use frequency.
Conclusions: Frequency of cannabis use was not associated with improved pain, anxiety, or depression symptoms but was associated with new-onset cannabis use disorder in a significant minority of participants. Daily or near-daily cannabis use appears to have little benefit for these symptoms after 12 months of use.
1. Introduction
With growing state-level legalization of commercial cannabis markets, individuals are increasingly using cannabis products hoping to alleviate symptoms of various chronic medical conditions (1–3). In most US states, people seeking cannabis for medical or psychiatric symptoms must obtain state-specific medical cannabis authorization cards to purchase cannabis products from dispensaries (4, 5). Enrollment in medical cannabis programs increased 4.5-fold from 2016 to 2020 (6). While interest in using commercial cannabis products for medical conditions is high, rigorous data on its safety and effectiveness for symptom relief is sparse (7), and few studies assess longer-term outcomes.
The most common conditions for which individuals obtain medical cannabis cards are pain, insomnia, anxiety and depressed mood (8–10), but evidence for the efficacy of cannabis to treat these symptoms has been mixed (7, 11–18). Studies examining the effects of cannabis on chronic pain have generally had small sample sizes and null results (19), except for some evidence of efficacy for neuropathic pain (19–21). While patients using opioid medications for chronic pain have reported preliminary success in substituting cannabis for these medications (22, 23), electronic health records, including prescription drug monitoring program data from a large multisite medical cannabis program, demonstrated minimal to no change in either opioids or sedative hypnotics over the 6 months of medical cannabis use (24). An ongoing randomized controlled trial is currently assessing the effectiveness of cannabis for pain control and opioid dose reduction (25). A relationship between cannabis use and sleep has been theorized based on connections between the endocannabinoid system and circadian rhythms (26, 27) with research indicating improved sleep in the short term (28–31), but a disruption in sleep quality over long term use (32, 33). The use of cannabis as a therapeutic for anxiety or depression is controversial, as existing trials are limited by small sample sizes, as well as deficits in the overall study designs, which limit the clinical applications of findings (34, 35).
Unlike Food and Drug Association (FDA) approved medications, treatments approved by voter initiatives or legislative action come with little evidence to guide dosing to optimize benefits and minimize adverse effects. Further, recent US national data reports that 3 in 10 adults who use cannabis develop cannabis use disorder (CUD), with 23% developing severe CUD (36) often with tolerance to Δ9-tetrahydrocannabinol (THC) and withdrawal symptoms (37, 38). Data are lacking on whether adults using cannabis for medical purposes develop similar rates of CUD to those who use cannabis for recreational purposes. Rigorous studies of the effects of cannabis use on clinical outcomes will be critical to inform patient and clinician decision-making.
This study describes a prospective, 9-month follow-up of participants enrolled in a randomized clinical trial (RCT; NCT03224468) in which adults seeking cannabis to alleviate pain, insomnia, anxiety, or depression were randomized to immediate card acquisition or 12 weeks delayed card acquisition groups. In the 12-week RCT, immediate cannabis card acquisition was associated with developing CUD, improved self-reported insomnia, and no change in pain, depression, or anxiety symptoms (29). Here, we report cannabis use frequency, CUD, pain, insomnia, anxiety, and depression symptoms over the 9 months following the 12-week randomized phase. Based on results of the RCT, we hypothesized that after 12 months of cannabis use, symptoms of insomnia would improve, but symptoms of CUD would increase. We did not hypothesize any changes in pain, depression, or anxiety symptoms.
2. Methods
This study was approved by the Massachusetts General Brigham Institutional Review Board. All participants provided informed consent. Participants were financially compensated for their time, but the study did not provide or pay for the medical cannabis cards or any cannabis products. Adults without CUD seeking to obtain a medical cannabis card for pain, insomnia, anxiety, or depressive symptoms participated in a 12-week, single-blind randomized pragmatic clinical trial (NCT03224468), described previously (29), in which they were assigned to either obtain a card immediately or to delay card acquisition by 12 weeks. Participants assigned to the immediate card acquisition group were required to obtain a card to participate in the study. All participants were then followed for a 9-month period in which all could obtain medical cannabis cards if they desired, and use the cannabis products of their choice, dose, and frequency following the randomized phase.
2.1. Design
Participants completed assessments of clinical symptoms (pain, insomnia, anxiety, depression), cannabis use and CUD at baseline and weeks 2, 4, and 12 of the randomized phase. During the follow-up period, participants completed assessments of clinical symptoms at months 6 and 12 and of cannabis use monthly.
2.2. Participants
Participants were men and women aged 18–65 (inclusive) who expressed an interest in using cannabis to alleviate symptoms of pain, insomnia, anxiety, or depression and were recruited through community advertising; a full description of the sample is reported elsewhere (29). Exclusion criteria included daily or near-daily cannabis use in the prior 3 months, diagnosis of current CUD, other substance use disorder, or serious unstable medical condition at screening or baseline assessments.
2.3. Measurements and outcomes
Cannabis use frequency was collected monthly via REDCap using a 7-point ordinal rating scale. Due to low cell counts, we collapsed the scale down to four ratings: (a) 5–7 days per week, (b) 1–4 days per week, (c) less than once a week, and (d) less than once a month.
We report results for five clinical outcomes. Pain in the past 24 h was assessed by the Pain Severity subscale of the Brief Pain Inventory Short Form (BPI-PS) (39) on a 0–10 point scale (0 = no pain, 10 = worst pain imaginable). Insomnia in the past month was assessed by the Athens Insomnia Scale (AIS) (40) on a 0–24 point scale, with higher scores indicating more severe sleep difficulties. Anxiety and depressive symptoms in the past week were assessed using the corresponding subscales of the Hospital Anxiety and Depression Scale (HADS) (41), each on a 0–21 point scale, with scores of 8–10 indicating borderline abnormal and a score of 11 or greater indicating abnormal levels of anxiety or depression for a given subscale. Cannabis use disorder (CUD) symptoms were assessed in interviews by doctoral-level or registered nurse investigators blinded to group assignment using the CUD Checklist of the Diagnostic and Statistical Manual of Mental Disorders (42), with scores ranging from 0 to 11 (with 2 or more symptoms indicating a CUD diagnosis, and higher scores indicated more severe CUD).
2.4. Analytic plan
All analyses examined how clinical outcomes (cannabis use frequency, symptoms of pain, insomnia, anxiety, depression, and CUD) changed from the end of the RCT to the end of the follow-up period (month 12). Time was assessed via a linear trend, using the number of months since enrollment per participant (accounting for individual variation in the timing of study visits). All analyses included a participant-varying intercept and slope for the time trend. Analyses also included a covariate for a participant's symptom levels at baseline. We used a dummy-coded variable for randomization group (immediate = 1, delayed = 0).
We first assessed change in cannabis use over time, testing for differences by randomization group and for a group by time interaction. We fit the ordinal cannabis use outcome (the 4-point rating scale) using a multi-level cumulative probit regression (43). Analyzing the ordinal ratings using the cumulative probit model avoided systematic errors caused by analyzing ordinal ratings using linear regression (44).
We next assessed change in symptom levels for the five clinical outcomes (symptoms of pain, insomnia, anxiety, depression, and CUD) over time, again testing for differences by randomization group and for a group by time interaction. We fit the clinical inventory scores and CUD symptom counts using a multi-level beta-binomial regression model.
Finally, we reassessed change in symptom levels for the five clinical outcomes over time based on cannabis use frequency, regardless of randomization group. Here, we used an approach based on projective inference (45), fitting as a reference model a cumulative probit regression with subject-varying intercepts and slopes for change over time (expanded to capture linear, quadratic, and cubic trends) applied to participants' full set of 10 monthly cannabis use ratings. We used this reference model to interpolate continuous estimates of cannabis use at months 3, 6, and 12 (when clinical outcomes were collected).
All analyses were conducted in a Bayesian framework, allowing implementation of complex statistical models and intuitive interpretations of uncertainty intervals and p-values as the probability of a test statistic given the data and prior assumptions (46). To address the potential for an inflated risk of false positives (47), we used a model-averaging approach (48), in which results across nested models [i.e., models for (1) a main effect of time, (2) main effects of both time and group/cannabis use, or (3) their interaction] are averaged together based on their predictive utility [e.g., stacking weights based on leave-one-out cross-validation; (49)]. We report estimated standardized effect sizes (ES, mean differences scaled by baseline standard deviations), 95% credible intervals, and posterior p-values. All results are from the model-averaged adjusted estimates. Effects were deemed statistically significant if adjusted posterior p < 0.05.
3. Results
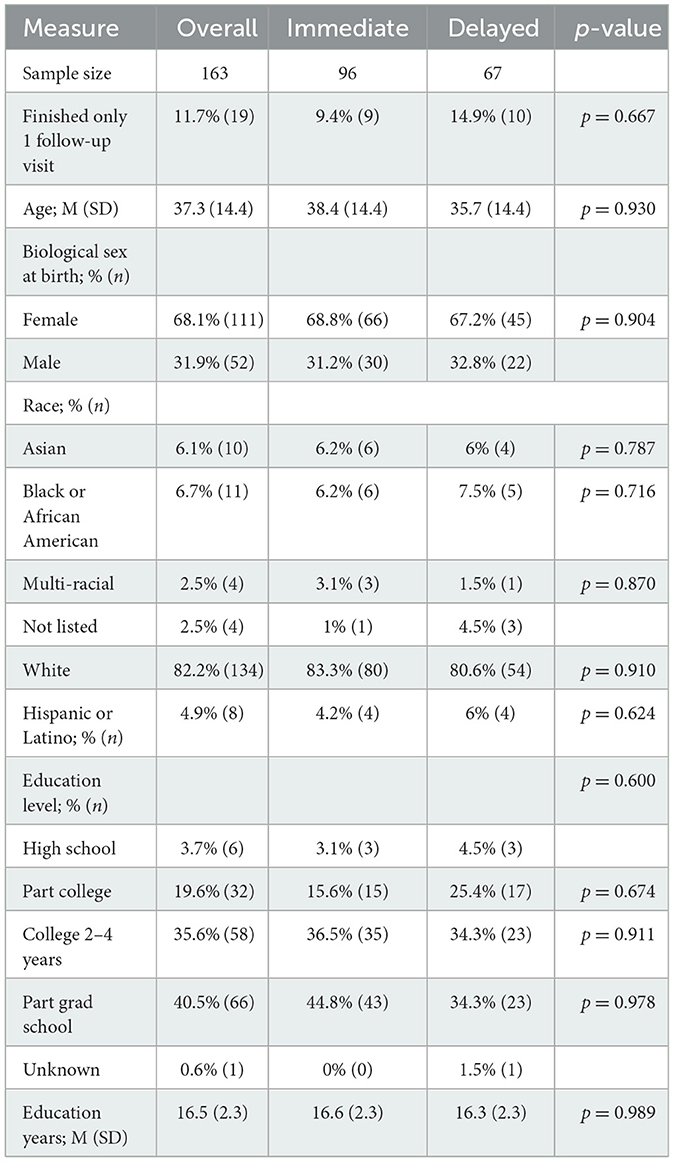
Among the 186 participants enrolled in the original clinical trial, 163 had at least one follow-up assessment (at either 6 or 12 months) with complete data for all five clinical outcomes and for cannabis use. The analytic sample was 68.1% female, 82.2% white, and had an average age of 37.3 (SD = 14.4) years. See Table 1 for additional descriptive characteristics measured at baseline. Participants in the immediate acquisition group were required to obtain a medical cannabis card to be eligible for the clinical trial, thus all (100%) obtained a card. In contrast, only 36.5% of participants assigned to delayed acquisition obtained a card by the 12-month timepoint. Although the majority of participants in the delayed acquisition group did not obtain a card, 74.6% reported using cannabis 1 or more days per week for at least a month during the follow-up period (months 3–12).
As previously reported (29), at the end of the clinical trial (month 3) the immediate acquisition group had higher rates of cannabis use compared to the delayed acquisition group (β = 1.49, CI = 0.99–2.00, post. p < 0.001). However, by month 12 the immediate acquisition group had reduced cannabis use (β = −0.50, CI = −0.88 to −0.08, post. p = 0.020), while the delayed acquisition group had a slight increase in cannabis use frequency (β = 0.38, CI = −0.15–0.86, post. p = 0.132). The immediate acquisition group still had greater use than the delayed group at month 12 (β = 0.61, CI = 0.01–1.31, post. p = 0.046) (Figure 1, Supplementary Table 1).
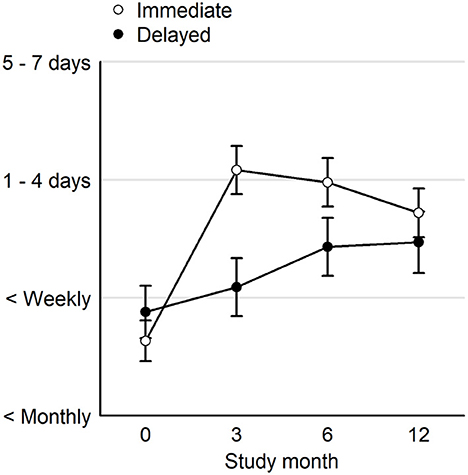
Figure 1. Averages and 95% uncertainty intervals over the 4-point ordinal rating for cannabis use at the start of the clinical trial (Month 0), the end of the clinical trial (Month 3), and the follow up period (Months 6 and 12). Immediate, immediate card acquisition group; Delayed, delayed card acquisition group.
At month 12, 11.7% (n = 19) of participants, and 17.1% of those using cannabis daily or near-daily (n = 6) met DSM-V diagnostic criteria for CUD, defined as 2 or more symptoms of CUD; most had mild (n = 15), defined as 2–3 symptoms, two participants had moderate, defined as 4–5 symptoms, and two participants had severe CUD, defined as 6 or more symptoms. For those with a CUD diagnosis, the most frequently reported CUD symptoms were tolerance (58%), using despite experiencing problems (44%), spending a lot of time using (31%), and craving (31%). The most common combinations of symptoms were tolerance combined with either craving (10%), using more than intended (8%), or wanting to cut back (6%) (Supplementary Figure 1). There was no statistically significant effect of group on number of CUD symptoms by the 12-month timepoint (ES = 0.63, 95% CI = 0.00–1.31, post. p = 0.185).
Averaging over time points, the immediate acquisition group had lower AIS scores (ES = 0.30, −0.53 to −0.08, p = 0.008) and higher BPI scores (ES = 0.15, 0.03–0.27, p = 0.012) compared to the delayed acquisition group. There were, however, no statistically significant time by group interactions on any outcome (Supplementary Table 2, Supplementary Figure 2), indicating that although there was a main effect of group, the groups did not differ in how their clinical symptoms changed over time. Depression scores improved from month 3 to month 12, regardless of randomization group or frequency of cannabis use (ES = −0.13, 95% CI = −0.26 to −0.01, post. p = 0.032). Pain, insomnia, and anxiety symptoms did not change significantly over the follow up period (Table 2).
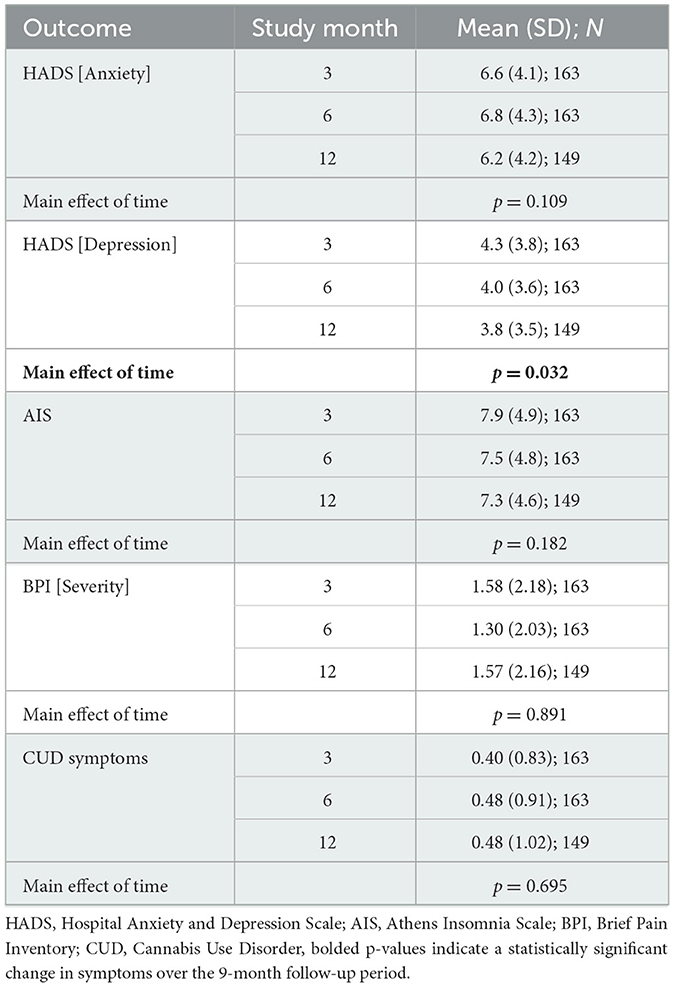
Table 2. Symptoms of insomnia, pain, depression, anxiety, and CUD during the 9-month post-randomization period.
More frequent cannabis use was associated with greater pain (ES = 0.07, 95% CI = 0.02–0.12, post. p = 0.006) and more CUD symptoms (ES = 0.55, 95% CI = 0.31–0.86, post. p < 0.001). More frequent cannabis use was not associated with improvement in insomnia, depression, or anxiety. Those who used cannabis 3 or more days per week were 2.69 times more likely to develop CUD, with disorder rates of 15.4% for those who used 3 or more days compared to disorder rates of 5.6% for those who used <3 days. We found no statistically significant time by cannabis use interactions across any outcome (Table 3).
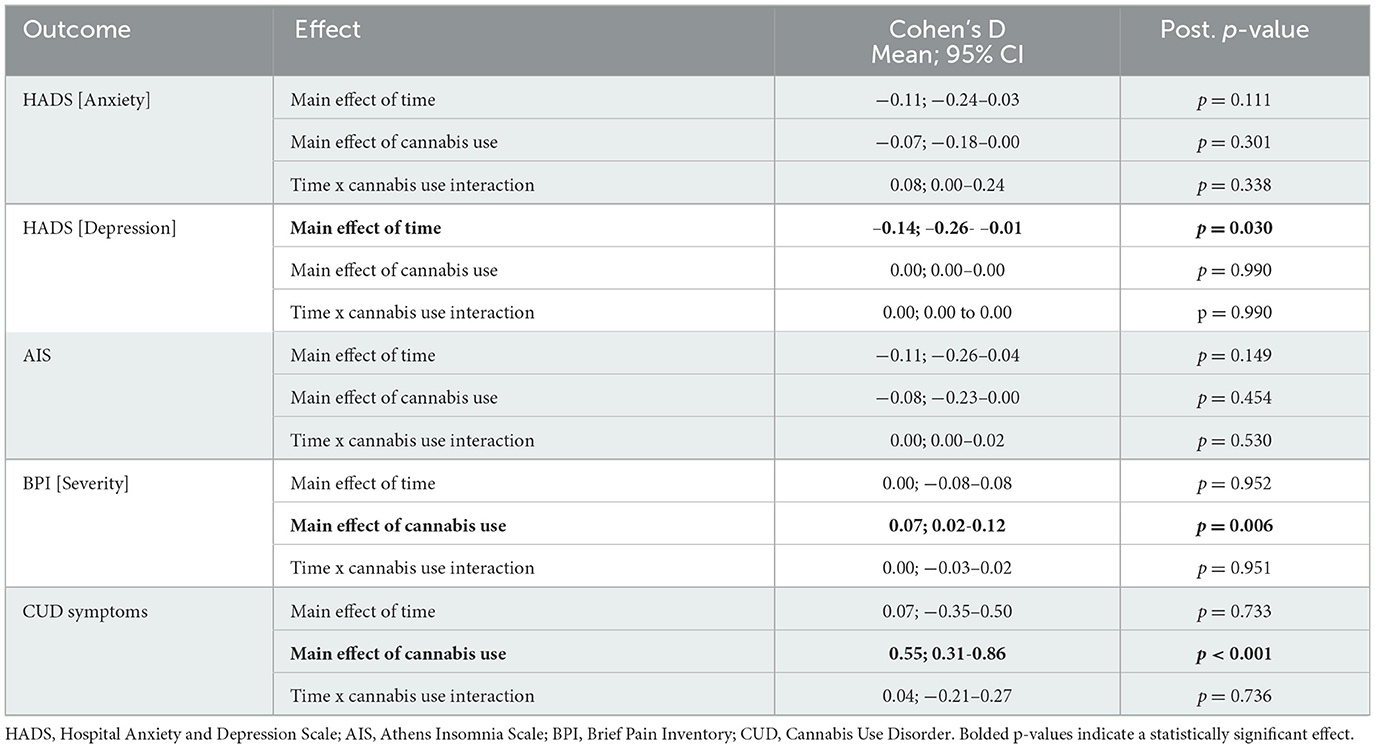
Table 3. Main effects of time and cannabis use frequency and their interaction for each clinical outcome.
4. Discussion
In this 9-month prospective follow-up analysis of a 12-week RCT of immediate or delayed medical cannabis card acquisition, greater cannabis use frequency was positively associated with more CUD symptoms and greater pain severity and not significantly associated with changes in insomnia, depression, or anxiety symptom severity.
Few studies assess the development of CUD in individuals using cannabis for medical purposes. The current study found that after 1 year of cannabis use, 11.7% of all participants and 17.1% of the daily or near-daily cannabis users had a CUD diagnosis, with 2 participants meeting criteria for severe CUD (6 symptoms). CUD at screening or baseline was exclusionary, so these were all new onset courses of CUD. Epidemiologic surveys of recreational cannabis use have indicated 3 in 10 adults who use cannabis develop CUD (36). Though prevalence in the current study is lower than the 30% 12-month incidence of CUD reported in Hasin et al. (36), it nonetheless indicates that individuals using cannabis for medical reasons may be at risk for CUD. Most current medical cannabis card regulations do not require a follow-up appointment with a certified physician after obtaining a medical cannabis card. This lack of follow-up differs from standard medical practice when prescribing other medications for these conditions such as antidepressants, opioids, and benzodiazepines. Due to the risk for CUD among individuals who use cannabis for medical concerns, a follow-up appointment with the prescribing physician may be warranted to assess balance between symptom improvement and emergence of CUD symptoms.
For those with a CUD diagnosis, the most frequently reported CUD symptoms were tolerance, using despite experiencing problems, spending a lot of time using, and craving. We recognize that there remains controversy in the field about whether a CUD diagnosis is appropriate for patients using cannabis for medical symptoms, rather than recreational purposes alone. For those taking prescription medications in the context of appropriate medical treatment, tolerance and withdrawal do not count as criteria for a substance use disorder. We note, however, that cannabis is not obtained via a prescription, but rather, through a recommendation. Thus, the system created for the regulation and distribution of cannabis for medical purposes is unique; unlike FDA-approved medications, the physician recommending cannabis has no authority over amounts, concentration, doses, or frequency of cannabis use for the patient and often no clinical guidance. Further, for many cannabis users, there is a blurred line between medical and recreational motives (e.g., in those using cannabis for “relaxation” purposes). Therefore, we did not discount tolerance or withdrawal as CUD symptoms in study participants.
The association between more frequent cannabis use and increased pain should be interpreted with caution, as it is unlikely that cannabis use caused or exacerbated pain. Instead, it is possible that individuals experiencing more pain used cannabis more frequently to treat their pain. The association between greater cannabis use and greater pain likely indicates that cannabis is not adequately treating pain symptoms. This viewpoint is supported by a recent position paper from the International Association for the Study of Pain (IASP) that found, after a comprehensive review of research on the use of cannabinoids to treat pain, there was a lack of sufficient evidence to endorse the general use of cannabinoids for the treatment of pain (50). Further, lack of improvement in symptoms of anxiety after 12 months of cannabis use adds to a growing body of literature that does not endorse cannabis as a treatment for these conditions (51). Though there was no significant worsening of symptoms, additional work suggests heavy cannabis use may increase risk for depression (52) and other psychiatric illnesses (53), particularly among adolescents and young adults (54–56). The lack of benefit from cannabis indicates that individuals with these chronic conditions should consider evidence-based treatments. Additionally, because there was no placebo cannabis, and because all participants were seeking cannabis as a potential therapeutic, the trial design created bias toward finding a treatment effect attributable to expectancy. This strengthens our confidence in the null findings for improvement in pain, anxiety, and depression symptoms as a function of frequency of cannabis use. We do note that depression symptoms improved in all participants over time; though there was no significant effect of cannabis frequency, future studies should include non-using control participants in order to tease apart the effects of any cannabis use from the effect of time or study procedures that involve reflecting on and discussing symptoms, which may itself lead to reduction in symptoms (57).
Although we hypothesized improvements in insomnia symptoms, increased frequency of cannabis use did not predict greater improvement in insomnia. There was a main effect of group on insomnia symptoms, driven by improvement in the RCT phase in the immediate card acquisition group (29), but no additional benefit over the 9-month post-randomized period. Interestingly, though participants in the immediate card acquisition group experienced a short-term benefit of cannabis for sleep, their sleep did not continually improve during the 9-month post-randomized period (Supplementary Figure 2). This is in line with prior work on sleep and cannabis use which suggests an initial benefit to insomnia but disruptions in sleep quality if cannabis is used long term (32, 33).
This study should be interpreted in light of its limitations. First, the sample was predominantly female and white which may limit the generalizability of our findings. We used a pragmatic design, meaning that participants chose which cannabis products and how much they used; therefore, this study cannot determine the effect of specific cannabinoids on symptoms of these disorders. It will be important for future studies to quantify which doses and constituents of cannabinoids may be therapeutic. Further, though most participants received a medical cannabis card from a doctor, few received adequate advice on product choice and dosing, largely because the evidence for specific products and doses is lacking. Therefore, it is possible participants were not using cannabis at therapeutic doses. Even so, current regulations state that after receiving a medical cannabis card, individuals may choose their products and dosing, lending ecological validity to this study. We did not assess quality-of-life measures such as stress levels, activity levels, or positive affect. Other studies suggest that even if symptoms themselves do not improve, cannabis may improve these quality-of-life measures (58, 59). Finally, past CUD (>1 year before enrollment) was not exclusionary for this study, though we note that rates of past CUD were low (8.0% of participants) and the time between any CUD diagnosis and trial enrollment was often long (M = 23, SD = 20 years prior to study enrollment).
In conclusion, in this 9-month follow-up study of a 12-week randomized clinical trial of medical cannabis card ownership, we found an association between more frequent cannabis use and increased CUD risk, with no significant improvement in pain, anxiety, insomnia, or depression symptom severity as a function of cannabis use. The current findings call into question the long-term utility of cannabis as an effective tool in relieving clinical symptoms.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Massachusetts General Brigham Institutional Review Board. The patients/participants provided their written informed consent to participate in this study.
Author contributions
JG, RS, and AE contributed to the conceptualization and design of the original study. JG, MC, KP, BT-C, and BH designed the current research question and data analyses. JJ, MP, GP, and MC assisted with data collection. KP and MP organized and cleaned the data. KP performed the statistical analyses. MC, KP, and JJ wrote the first draft of the manuscript. JG and AE provided funding for data collection and salary support. All authors contributed to manuscript revision, read, and approved the submitted version.
Funding
The trial was funded by NIDA R01DA042043, JG. MC was funded by a Louis V. Gerstner III Research Scholar Award from the Gerstner Family Foundation. The contribution by AE was funded in part by K24DA030443. The contribution by JG was funded in part by NIDA K02DA052684.
Conflict of interest
AE reports consulting income in the past 3 years from Charles River Analytics and Karuna Pharmaceuticals and editorial support through Pfizer.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1083334/full#supplementary-material
References
1. Williams AR, Santaella-Tenorio J, Mauro CM, Levin FR, Martins SS. Loose regulation of medical marijuana programs associated with higher rates of adult marijuana use but not cannabis use disorder. Addict Abingdon Engl. (2017) 112:1985–91. doi: 10.1111/add.13904
2. Cerdá M, Wall M, Keyes KM, Galea S, Hasin D. Medical marijuana laws in 50 states: investigating the relationship between state legalization of medical marijuana and marijuana use, abuse and dependence. Drug Alcohol Depend. (2012) 120:22–7. doi: 10.1016/j.drugalcdep.2011.06.011
3. Wen H, Hockenberry JM, Cummings JR. The effect of medical marijuana laws on adolescent and adult use of marijuana, alcohol, and other substances. J Health Econ. (2015) 42:64–80. doi: 10.1016/j.jhealeco.2015.03.007
4. Chapman SA, Spetz J, Lin J, Chan K, Schmidt LA. Capturing heterogeneity in medical marijuana policies: a taxonomy of regulatory regimes across the United States. Subst Use Misuse. (2016) 51:1174–84. doi: 10.3109/10826084.2016.1160932
5. Pacula RL, Smart R. Medical marijuana and marijuana legalization. Annu Rev Clin Psychol. (2017) 13:397–419. doi: 10.1146/annurev-clinpsy-032816-045128
6. Boehnke KF, Dean O, Haffajee RL, Hosanagar A. U.S. trends in registration for medical cannabis and reasons for use from 2016 to 2020: an observational study. Ann Intern Med. (2022) 175:945–51. doi: 10.7326/M22-0217
7. The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. Washington, DC: National Academies of Sciences, Engineering, and Medicine (2017).
8. Boehnke KF, Gangopadhyay S, Clauw DJ, Haffajee RL. Qualifying conditions of medical cannabis license holders in the United States. Health Aff . (2019) 38:295–302. doi: 10.1377/hlthaff.2018.05266
9. Reinarman C, Nunberg H, Lanthier F, Heddleston T. Who are medical marijuana patients? Population characteristics from nine California assessment clinics. J Psychoactive Drugs. (2011) 43:128–35. doi: 10.1080/02791072.2011.587700
10. Kosiba JD, Maisto SA, Ditre JW. Patient-reported use of medical cannabis for pain, anxiety, and depression symptoms: systematic review and meta-analysis. Soc Sci Med. (2019) 233:181–92. doi: 10.1016/j.socscimed.2019.06.005
11. Mücke M, Phillips T, Radbruch L, Petzke F, Häuser W. Cannabis-based medicines for chronic neuropathic pain in adults. Cochrane Database Syst Rev. (2018) 3:Cd012182. doi: 10.1002/14651858.CD012182.pub2
12. Kansagara D, O'Neil M, Nugent S, Freeman M, Low A, Kondo K, et al. Benefits and harms of cannabis in chronic pain or post-traumatic stress disorder: a systematic review. VA ESP Project #05-225 (2017).
13. Goodhines PA, Wedel AV, Dobani F, Zaso MJ, Gellis LA, Park A. Cannabis use for sleep aid among high school students: concurrent and prospective associations with substance use and sleep problems. Addict Behav. (2022) 134:107427. doi: 10.1016/j.addbeh.2022.107427
14. Maddison KJ, Kosky C, Walsh JH. Is there a place for medicinal cannabis in treating patients with sleep disorders? what we know so far. Nat Sci Sleep. (2022) 14:957–68. doi: 10.2147/NSS.S340949
15. Vaillancourt R, Gallagher S, Cameron JD, Dhalla R. Cannabis use in patients with insomnia and sleep disorders: retrospective chart review. Can Pharm J Ott. (2022) 155:175–80. doi: 10.1177/17151635221089617
16. Degenhardt L Hall, W, Lynskey, M. The Association Between Cannabis Use and Depression: A Review of the Evidence. Cambridge: Cambridge University Press (2012).
17. Lev-Ran S, Roerecke M, Le Foll B, George TP, McKenzie K, Rehm J. The association between cannabis use and depression: a systematic review and meta-analysis of longitudinal studies. Psychol Med. (2014) 44:797–810. doi: 10.1017/S0033291713001438
18. Sachedina F, Chan C, Damji RS, de Sanctis OJ. Medical cannabis use in Canada and its impact on anxiety and depression: a retrospective study. Psychiatry Res. (2022) 313:114573. doi: 10.1016/j.psychres.2022.114573
19. Nugent SM, Morasco BJ, O'Neil ME, Freeman M, Low A, Kondo K, et al. The effects of cannabis among adults with chronic pain and an overview of general harms. Ann Intern Med. (2017) 167:319–31. doi: 10.7326/M17-0155
20. Abrams DI, Jay CA, Shade SB, Vizoso H, Reda H, Press S. Cannabis in painful HIV-associated sensory neuropathy: a randomized placebo-controlled trial. Neurology. (2007) 68:515–21. doi: 10.1212/01.wnl.0000253187.66183.9c
21. Serpell M, Ratcliffe S, Hovorka J, Schofield M, Taylor L, Lauder H, et al. A double-blind, randomized, placebo-controlled, parallel group study of THC/CBD spray in peripheral neuropathic pain treatment. Eur J Pain. (2014) 18:999–1012. doi: 10.1002/j.1532-2149.2013.00445.x
22. Haroutounian S, Ratz Y, Ginosar Y, Furmanov K, Saifi F, Meidan R, et al. The effect of medicinal cannabis on pain and quality-of-life outcomes in chronic pain: a prospective open-label study. Clin J Pain. (2016) 32:1036. doi: 10.1097/AJP.0000000000000364
23. Piper BJ, DeKeuster RM, Beals ML, Cobb CM, Burchman CA, Perkinson L, et al. Substitution of medical cannabis for pharmaceutical agents for pain, anxiety, and sleep. J Psychopharmacol. (2017) 31:569–75. doi: 10.1177/0269881117699616
24. Williams AR, Mauro CM, Feng T, Waples J, Martins SS, Haney M. Adult medical cannabinoid use and changes in prescription controlled substance use. Cannabis Cannabinoid Res. (2022). doi: 10.1089/can.2021.0212 [Epub ahead of print].
25. Jashinski J, Grossman E, Quaye A, Cather C, Potter K, Schoenfeld DA, et al. Randomised, pragmatic, waitlist controlled trial of cannabis added to prescription opioid support on opioid dose reduction and pain in adults with chronic non-cancer pain: study protocol. BMJ Open. (2022) 12:e064457. doi: 10.1136/bmjopen-2022-064457
26. Sanford AE, Castillo E, Gannon RL. Cannabinoids and hamster circadian activity rhythms. Brain Res. (2008) 1222:141–8. doi: 10.1016/j.brainres.2008.05.048
27. Vaughn LK, Denning G, Stuhr KL, de Wit H, Hill MN, Hillard CJ. Endocannabinoid signalling: has it got rhythm? Br J Pharmacol. (2010) 160:530–43. doi: 10.1111/j.1476-5381.2010.00790.x
28. Cousens K, DiMascio A. (–)δ9 THC as an hypnotic. Psychopharmacologia. (1973) 33:355–64. doi: 10.1007/BF00437513
29. Gilman JM, Schuster RM, Potter KW, Schmitt W, Wheeler G, Pachas GN, et al. Effect of medical marijuana card ownership on pain, insomnia, and affective disorder symptoms in adults: a randomized clinical trial. JAMA Netw Open. (2022) 5:e222106. doi: 10.1001/jamanetworkopen.2022.2106
30. Nicholson AN, Turner C, Stone BM, Robson PJ. Effect of Delta-9-tetrahydrocannabinol and cannabidiol on nocturnal sleep and early-morning behavior in young adults. J Clin Psychopharmacol. (2004) 24:305–13. doi: 10.1097/01.jcp.0000125688.05091.8f
31. Tervo-Clemmens B, Schmitt W, Wheeler G, Cooke ME, Schuster RM, Hickey S, et al. Cannabis use and sleep quality in daily life: an electronic daily diary study of adults starting cannabis for health concerns. Drug Alcohol Depend. (2023) 243:109760. doi: 10.1016/j.drugalcdep.2022.109760
32. Babson KA, Sottile J, Morabito D. Cannabis, cannabinoids, and sleep: a review of the literature. Curr Psychiatry Rep. (2017) 19:23. doi: 10.1007/s11920-017-0775-9
33. Kuhathasan N, Dufort A, MacKillop J, Gottschalk R, Minuzzi L, Frey BN. The use of cannabinoids for sleep: a critical review on clinical trials. Exp Clin Psychopharmacol. (2019) 27:383–401. doi: 10.1037/pha0000285
34. Turna J, Patterson B, Van Ameringen M. Is cannabis treatment for anxiety, mood, and related disorders ready for prime time? Depress Anxiety. (2017) 34:1006–17. doi: 10.1002/da.22664
35. Van Ameringen M, Zhang J, Patterson B, Turna J. The role of cannabis in treating anxiety: an update. Curr Opin Psychiatry. (2020) 33:1. doi: 10.1097/YCO.0000000000000566
36. Hasin DS, Saha TD, Kerridge BT, Goldstein RB, Chou SP, Zhang H, et al. Prevalence of marijuana use disorders in the United States between 2001-2002 and 2012-2013. JAMA Psychiat. (2015) 72:1235–42. doi: 10.1001/jamapsychiatry.2015.1858
37. Gonzalez S, Cebeira M, Fernandez-Ruiz J. Cannabinoid tolerance and dependence: a review of studies in laboratory animals. Pharmacol Biochem Behav. (2005) 81:300–18. doi: 10.1016/j.pbb.2005.01.028
38. Lichtman AH, Martin BR. Cannabinoid tolerance and dependence. Handb Exp Pharmacol. (2005) 168:691–717. doi: 10.1007/3-540-26573-2_24
39. Cleeland CS, Ryan KM. Pain assessment: global use of the brief pain inventory. Ann Acad Med Singapore. (1994) 23:129–38.
40. Soldatos CR, Dikeos DG, Paparrigopoulos TJ. Athens insomnia scale: validation of an instrument based on ICD-10 criteria. J Psychosom Res. (2000) 48:555–60. doi: 10.1016/S0022-3999(00)00095-7
41. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. (1983) 67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x
42. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. Washington, DC: American Psychiatric Association (2013).
43. Bürkner PC, Vuorre M. Ordinal regression models in psychology: a tutorial. Adv Methods Pract Psychol Sci. (2019) 2:77–101. doi: 10.1177/2515245918823199
44. Liddell TM, Kruschke JK. Analyzing ordinal data with metric models: what could possibly go wrong? J Exp Soc Psychol. (2018) 79:328–48. doi: 10.1016/j.jesp.2018.08.009
45. Piironen J, Paasiniemi M, Vehtari A. Projective inference in high-dimensional problems: prediction and feature selection. Electron J Stat. (2020) 14:2155–97. doi: 10.1214/20-EJS1711
46. Morey RD, Hoekstra R, Rouder JN, Lee MD, Wagenmakers EJ. The fallacy of placing confidence in confidence intervals. Psychon Bull Rev. (2016) 23:103–23. doi: 10.3758/s13423-015-0947-8
47. Simmons JP, Nelson LD, Simonsohn U. False-Positive Psychology: Undisclosed Flexibility in Data Collection and Analysis Allows Presenting Anything as Significant. Washington, DC, US: American Psychological Association (2016). p. 547.
48. Wasserman L. Bayesian model selection and model averaging. J Math Psychol. (2000) 44:92–107. doi: 10.1006/jmps.1999.1278
49. Yao Y, Vehtari A, Simpson D, Gelman A. Using stacking to average bayesian predictive distributions (with discussion). Bayesian Anal. (2018) 13:917–1007. doi: 10.1214/17-BA1091
50. IASP Presidential Task Force on Cannabis and Cannabinoid Analgesia. International association for the study of pain presidential task force on cannabis and cannabinoid analgesia position statement. Pain. (2021) 162 (Suppl. 1):S1–2. doi: 10.1097/j.pain.0000000000002265
51. Haroutounian S, Arendt-Nielsen L, Belton J, Blyth FM, Degenhardt L, Forti MD, et al. IASP presidential taskforce on cannabis and cannabinoid analgesia: research agenda on the use of cannabinoids, cannabis, and cannabis-based medicines for pain management. Pain. (2021) 162:S117–24. doi: 10.1097/j.pain.0000000000002266
52. Smolkina M, Morley KI, Rijsdijk F, Agrawal A, Bergin JE, Nelson EC, et al. Cannabis and depression: a twin model approach to co-morbidity. Behav Genet. (2017) 47:394–404. doi: 10.1007/s10519-017-9848-0
53. Livne O, Shmulewitz D, Sarvet AL, Wall MM, Hasin DS. Association of cannabis use-related predictor variables and self-reported psychotic disorders: U.S. adults, 2001-2002 and 2012-2013. Am J Psychiatry. (2022) 179:36–45. doi: 10.1176/appi.ajp.2021.21010073
54. Gilman JM, Kuster JK, Lee S, Lee MJ, Kim BW, Makris N, et al. Cannabis use is quantitatively associated with nucleus accumbens and amygdala abnormalities in young adult recreational users. J Neurosci. (2014) 34:5529–38. doi: 10.1523/JNEUROSCI.4745-13.2014
55. Levar N, Francis AN, Smith MJ, Ho WC, Gilman JM. Verbal memory performance and reduced cortical thickness of brain regions along the uncinate fasciculus in young adult cannabis users. Cannabis Cannabinoid Res. (2018) 3:56–65. doi: 10.1089/can.2017.0030
56. Tervo-Clemmens B, Quach A, Calabro FJ, Foran W, Luna B. Meta-analysis and review of functional neuroimaging differences underlying adolescent vulnerability to substance use. Neuroimage. (2020) 209:116476. doi: 10.1016/j.neuroimage.2019.116476
57. Cooke ME, Gilman JM, Lamberth E, Rychik N, Tervo-Clemmens B, Evins AE, et al. Assessing changes in symptoms of depression and anxiety during four weeks of cannabis abstinence among adolescents. Front Psychiatry. (2021) 12. doi: 10.3389/fpsyt.2021.689957
58. Garcia-Romeu A, Elmore J, Mayhugh RE, Schlienz NJ, Martin EL, Strickland JC, et al. Online survey of medicinal cannabis users: qualitative analysis of patient-level data. Front Pharmacol. (2022) 13:965535. doi: 10.3389/fphar.2022.965535
Keywords: cannabis (marijuana), insomnia, pain, anxiety, depression, cannabis use disorder, medical cannabis, medical marijuana
Citation: Cooke ME, Potter KW, Jashinski J, Pascale M, Schuster RM, Tervo-Clemmens B, Hoeppner BB, Pachas GN, Evins AE and Gilman JM (2023) Development of cannabis use disorder in medical cannabis users: A 9-month follow-up of a randomized clinical trial testing effects of medical cannabis card ownership. Front. Psychiatry 14:1083334. doi: 10.3389/fpsyt.2023.1083334
Received: 28 October 2022; Accepted: 13 February 2023;
Published: 07 March 2023.
Edited by:
Yasser Khazaal, Université de Lausanne, SwitzerlandReviewed by:
Emily E. Hartwell, Corporal Michael J. Crescenz VA Medical Center, United StatesYiyang Liu, University of Florida, United States
Emily Atkinson, University of Kentucky, United States
Copyright © 2023 Cooke, Potter, Jashinski, Pascale, Schuster, Tervo-Clemmens, Hoeppner, Pachas, Evins and Gilman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jodi M. Gilman, amdpbG1hbjFAbWdoLmhhcnZhcmQuZWR1
†These authors share first authorship
 Megan E. Cooke
Megan E. Cooke Kevin W. Potter
Kevin W. Potter Julia Jashinski1
Julia Jashinski1 Michael Pascale
Michael Pascale Randi M. Schuster
Randi M. Schuster Brenden Tervo-Clemmens
Brenden Tervo-Clemmens A. Eden Evins
A. Eden Evins Jodi M. Gilman
Jodi M. Gilman