
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 03 April 2023
Sec. Psychopathology
Volume 14 - 2023 | https://doi.org/10.3389/fpsyt.2023.1076299
 Erling Inge Kvig1,2*
Erling Inge Kvig1,2* Steinar Nilssen1
Steinar Nilssen1Introduction: Increasingly, diagnostic assessments in clinical practice are made using structured diagnostic interviews or self-rating scales imported into clinical practice from research studies and big-scale surveys. Although structured diagnostic interviews have been shown to be highly reliable in research, the use of such method in clinical contexts are more questionable. In fact the validity and clinical utility of such methods in naturalistic contexts have rarely been evaluated. In this study we report on a replication study of Nordgaard et al (22) Assessing the diagnostic validity of a structured psychiatric interview in a first-admission hospital sample. World Psychiatry, 11 (3): 181–185.
Methods: The study sample comprises 55 first-admitted inpatients to a treatment facility specializing in the assessment and treatment of patients with psychotic disorders.
Results: We found poor agreement between diagnoses generated by Structured Clinical Interview for DSM-IV and Best-estimate consensus diagnoses (κ value 0.21).
Discussion: We identified over-reliance on self-report, vulnerability to response set in dissimulating patients, and a strong diagnosis and comorbidity focus, as possible reasons for misdiagnosis with the SCID. We conclude that structured diagnostic interviews performed by mental health professionals without solid psychopathological knowledge and experience are not recommendable for clinical practice.
Structured diagnostic interviews have rapidly become the gold standard in psychiatric research and diagnostic assessments in clinical practice. Originally developed for use in big-scale surveys and research studies, their recommendations by textbooks in psychiatry (1) and clinical guidelines (2) have made the use of these diagnostic tools widespread also in routine diagnostic assessments.
The historical foundation of the structured interviews was the traditional “mental status” examinations developed in European clinical psychiatry [e.g., Kraepelin (3)], and introduced into American psychiatry by Adolph Meyer in 1917 (4). Although numerous approaches for evaluating mental status have existed since (5), the Mental Status Evaluation Record (MSER) (6) have been influential to later structured diagnostic interviews in general and to the subsequent development of Schedule of Affective Disorders and Schizophrenia [SADS, (7)] and Structured Clinical Interview for DSM [SCID, (8)] (9).
Structured diagnostic interviews were introduced to improve diagnostic reliability (10). The well-known United States-United Kingdom diagnostic project demonstrated very different diagnostic habits among British and American clinicians (11). A solution to such reliability concerns, proposed among others by Robert Spitzer in the polemic paper stating “Are clinicians still necessary?,” was to minimize variance by standardization of psychiatric assessment and diagnostic criteria (12). The purpose of a structured interview is to provide a systematic evaluation by standardizing (1) the specific language of clinical inquiries, (2) the sequencing of these inquiries, and (3) the quantification of responses (9). With the «operational revolution» and the publication of DSM-III, including diagnostic criteria for most mental disorders, structured interviews such as the SCID were developed to standardize DSM-III evaluations of mental disorders. While the previous MSE-based structured interviews were organized around symptoms or topic areas (e.g., observed psychopathology, speech and thought, etc.) to provide comprehensive examination of psychopathology, the SCID is organized by diagnostic categories to provide adequate coverage of DSM inclusion criteria across a broad range of mental disorders.
The specific design of the SCID was developed to reduce variability in diagnostic assessments. Information variance, i.e., variability in the quality and quantity of information elicited across patients, is reduced by defining initial clinical inquiries as obligatory questions, with specification of further branching and probing questions. Inquiries are sequenced in a predefined order to assure adequate coverage of DSM criteria for specific diagnostic categories. Criterion variance, i.e., variability in converting clinical information into diagnostic criteria, is reduced by operational definitions of what is clinically relevant and when criteria are met. Most items are worded in the pathological direction (i.e., affirmative responses signifies impairment), and can be answered with a “yes” or “no.”
The SCID has been found to yield reliable diagnoses for most axis I disorders in research contexts (13–19). However, the validity and clinical utility of structured diagnostic interviews have rarely been explored (20, 21). Validity pertains to the actual correctness and usability of a test, while clinical utility concerns the specificity and sensitivity of tests. In psychiatric research, validity is often explored by examining the psychometric properties inherent to a diagnostic test. In a study by Nordgaard et al. (22), diagnostic validity was examined through measures of agreement and accuracy when compared to a criterion or “gold standard” (i.e., a well validated and generally accepted method). Best estimate consensus diagnoses was used as “gold standard” in the study. In the best estimate consensus procedure, interview data are supplemented with all existing sources of information (e.g., cross-sectional and longitudinal self-report data, observations by clinical staff in inpatient settings, longitudinal data from medical records, judgments from other clinicians, interviews of informants, and other sources) and evaluated by several experienced clinicians, who assign a best-estimate consensus diagnosis. Using the best-estimate consensus procedure as “gold standard,” Nordgaard et al. (22) found overall very low agreement between SCID derived and best-estimate consensus diagnoses (kappa 0.18), indicating major problems with the accuracy of diagnoses based on SCID in clinical settings. Since treatment decisions usually are based on the diagnosis, such diagnostic problems may have profound consequences for the patients. The interpretation of these findings was that, although standardization of psychiatric interviews may minimize information and criterion variability, this does not guarantee the quality (validity) of the information. The authors conclude that structured diagnostic interviews administered by mental health professionals without adequate psychopathological knowledge and experience are not recommendable for clinical work.
The recommendation of the use of structured diagnostic interviews as best standard by the Norwegian health authorities (2) provided an opportunity to investigate the validity and clinical utility of structured interviews as used in routine characterization of mental health patients in a naturalistic setting. In the current study we aimed to replicate the study by Nordgaard et al. (22), and examine the diagnostic validity and clinical utility of a structured diagnostic interview in a naturalistic observational study. We were interested in the following questions:
1. What is the sensitivity, specificity and validity of SCID-generated diagnoses compared with best-estimate consensus diagnoses?
2. What are the reasons for potential discrepancies found between SCID and best estimate consensus diagnoses?
The study was carried out in Northern Norway (population 480,000). Health care is provided by a two-tier public health system, where specialist referrals are made by GPs and emergency clinics in the local municipalities with one or several GPs on duty. Specialist mental health care is provided by psychiatric departments in general hospitals, and in community mental health care centers. A specialist inpatient unit (Regional Unit of Psychosis) for patients needing specialist assessment and treatment for psychotic disorders is located in the general hospital located in Bodø (Nordland hospital), the administrative center for one of the larger counties in Northern Norway.
The study population was consecutive patients admitted to Nordland hospital, Regional Unit of Psychosis. Patients were eligible for inpatient care at the unit if they were between 16 and 65 years and presented with near psychotic or psychotic symptoms as assessed by their referring GP or treating clinician in community mental health or local acute wards. None of the patients were acutely ill. If patients were too unwell at first contact, they were transferred to the acute ward for initiation of treatment, and assessed when transferred back again to the unit. As part of routine assessment patients were given a systematic assessment battery described below as “comprehensive diagnostic assessment.” With the publication of new national guidelines for patients with psychotic disorders in 2013, recommending the use of structured diagnostic interviews, the SCID-I/P (23) was added to routine assessments. This part of the routine assessments is described below as “structured diagnostic assessment.” This assessment was conducted by a specifically trained social worker independent from the clinical team of the patient. The use of a trained social worker and not an experienced psychiatrist or psychologist for the structured diagnostic interviews is similar to how such tools are typically used in research and in clinical practice, and is in line with both the SCID User’s guide (24) and research on structured diagnostic interviews showing no substantial differences in diagnosis made by mental health professionals without background in psychopathology and experienced clinicians (25). All patients were informed that quality control procedures were an integrated part of the treatment program and that all assessments were part of the standard quality control instruments of the health service offered at the Regional unit of Psychosis at Nordland hospital. This paper uses data collected as part of the routine assessment procedure at the unit. The study was approved by the Nordland hospital Data Protection Officer (Personvernombudet), 12 December 2021.
The structured diagnostic interview was conducted by a social worker with clinical experience with severely ill patients, but with no previous training in psychopathology. The interviewer was specifically trained according to the SCID User’s guide (24, 26) and the SCID-101 didactic video course. Before implemented in routine assessment, two training interviews, observed and supervised by an experienced clinical psychologist, were conducted. The structured interview protocol consisted of the SCID-I/P (23) and the Schizotypal Personality Disorder module from SCID-II. The interview was conducted in a fully structured way with the following parts:
1. SCID-I/P Overview: an open-ended overview of the present illness and past episodes. Information on prior treatment, social and occupational functioning, context of the development of symptoms was also collected.
2. SCID-I/P Screening module: containing 12 screening questions where positive answers are followed up in relevant SCID modules later in the interview.
3. SCID-I/P Module A-J: contains separate modules for Mood episodes, Psychotic and associated symptoms, Psychotic disorders, Mood disorders, Substance Use disorders, Anxiety disorders, Somatoform disorders, Eating disorders, Adjustment disorders, Optional module. All relevant modules were completed.
The interviewer asked the mandatory pre-formulated questions in the predefined order, and used additional probes and questions for more information as specified in the SCID-I/P protocol and User’s guide. The average length of the interview was 1.5 h. Allocation of diagnoses, using the SCID-I/P Summary score sheet, was supervised by an experienced clinical psychologist in each individual case.
The comprehensive diagnostic interview was conducted by a treating clinician at the unit and the clinician was either an experienced psychiatrist or clinical psychologist. The clinical data was collected in phenomenologically-oriented, semi-structured interviews, modeled after the original study by Nordgaard et al. (22), with two mutually intertwined parts, and subsequently scored on a composite checklist.
1. Mental State Examination: a systematic examination of expressive features (e.g., affect modulation, contact quality, gaze, stereotypes, mannerisms, disorganization, and disorders of language), and objective evaluation of symptoms (e.g., mood, perceptual disturbances, thought content, and cognitive symptoms).
2. Anamnesis, psychosocial history and psychopathology: a detailed history was obtained to provide trajectory and context to further psychopathological examinations, also allowing a conversational interview according to the principles of phenomenological psychopathology. The psychosocial history was complemented with thorough review of medical records and collateral information from relatives.
Data was also collected through routine physical and psychological investigations, including a general physical examination, orienting neurology, blood and lab tests, and psychological investigations of cognition and personality.
Interviews were conducted according to the phenomenological principles proposed by Jaspers and others (27–30). The comprehensive diagnostic interviews began with a detailed and chronological, psychosocial history, providing opportunities for observing expressive features such as thought disorders and negative symptoms, and served as a natural point of departure for specific psychopathological exploration by asking for more details and examples. Psychopathology was explored and evaluated within the context of the patient’s life history and phase of illness. The style was free, dynamic and conversational, where questions or requests for more information were adapted to the patient’s narrative. The structure of the interview relied on the obligation of the interviewer to score all items on a composite checklist, the Operational Criteria Checklist [OPCRIT, (31, 32)], expanded with additional items Schedule for Affective Disorders and Schizophrenia (7), and the Examination of Anomalous Self-Experience (33).
Allocation of diagnoses was done using a best-estimate consensus procedure (34). All data from routine assessments, symptom ratings, referral letters, medical records, collateral information, and para-clinical data was presented in a case conference to a multi-disciplinary team, consisting of several experienced psychiatrists and clinical psychologists. Any differences on symptom criteria were resolved through consensus discussions. A best-estimate diagnosis was allocated to each patient using the OPCRIT system according to the ICD-10 and DSM-IV classification systems. In this study, we compared DSM-IV best-estimate consensus diagnoses to SCID diagnoses.
Unweighted kappa statistics was used to estimate agreement between the two diagnostic procedures for multiple- and dichotomized diagnostic categories. Cohen’s kappa indicates the proportion of agreement beyond that expected by chance. A kappa value that equals 0 indicates that the observed agreement is equal to the chance agreement. As suggested by Landis and Koch (35), the strength of agreement beyond chance for different κ values is Poor (<0), Slight (0–0.20), Fair (0.21–0.40), Moderate (0.41–0.60), Substantial (0.61–0.80), and Almost perfect (0.81–1.00).
Sensitivity and specificity was calculated using 2 × 2 tables that indicate number of false positives and negatives and true positives and negatives. Sensitivity estimates the proportion of persons with the disorder that will be correctly identified, while specificity estimates the proportion of persons without the disorder that will be correctly identified. Sensitivity and specificity values, using best-estimate consensus procedure as gold standard, were calculated for the SCID for multiple- and dichotomized diagnostic categories.
For the purpose of assigning a main diagnosis, we imposed the following hierarchy on the DSM-IV diagnoses (following the hierarchy of ICD-10): (1) schizophrenia, (2) other (non-affective) psychoses, (3) schizotypal disorder, (4) bipolar illness, (5) major depression, (6) other diagnoses (anxiety disorders, adjustment disorder, substance abuse/dependence). If a patient fulfills diagnostic criteria for several diagnoses, then the disorder placed highest in the hierarchy outranks lower placed diagnoses.
Data were analyzed using SPSS (version 24) for Macintosh (Table 1).
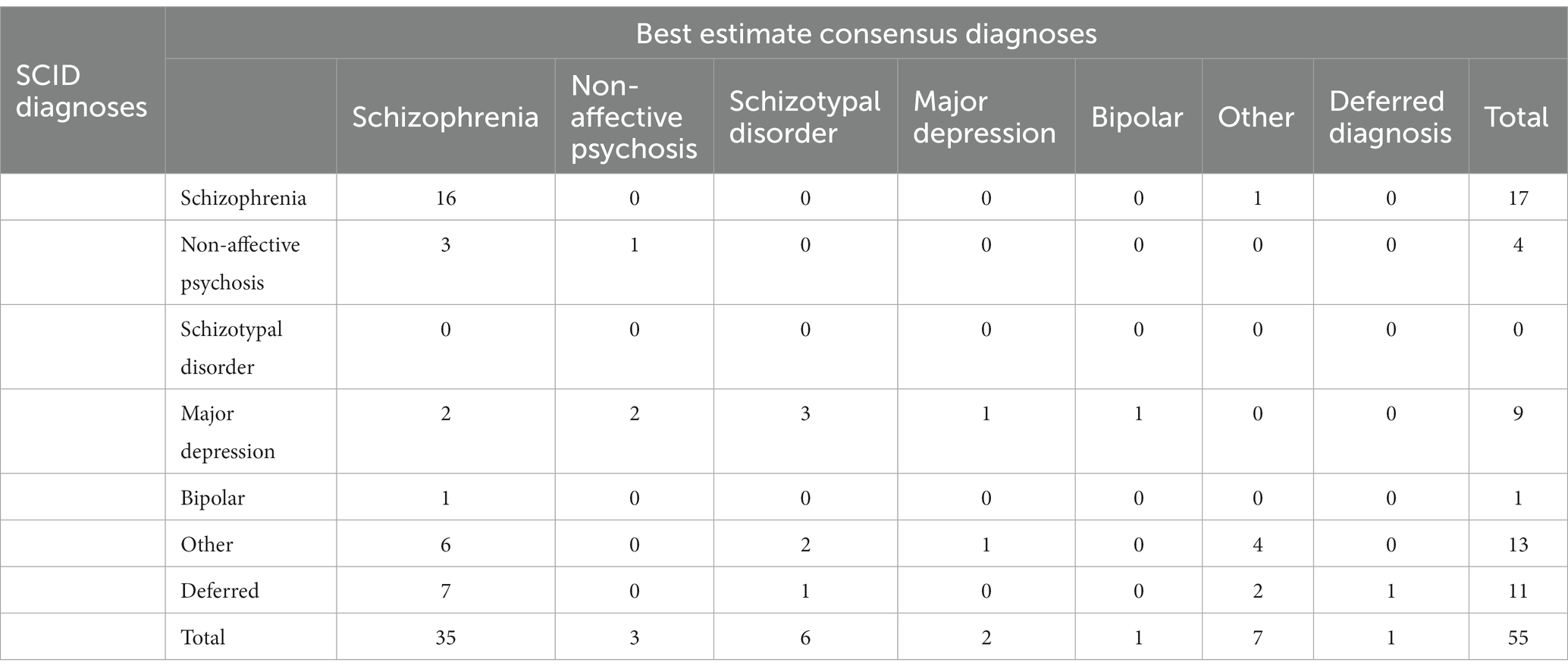
Table 1. DSM-IV diagnoses made by a trained non-clinician using Structured Clinical Interview for DSM-IV (SCID-I/P) vs. those made on the basis of a Best-estimate consensus procedure.
Participants in this study were patients receiving inpatient care between 1 August 2014 and 1 August 2016. The total sample was 74 patients. Of these, 19 patients were excluded from the study sample. Reasons for exclusion were: (1) they were not first-admission patients (n = 11), (2) they were discharged before assessment could be initiated (n = 6), or (3) they could not participate in assessments because of language problems or did not cooperate with assessment (n = 2). The final study sample consisted of 55 patients (n = 55), comprising 43 men (78%) and 12 women (22%). Mean age at entry of the study was 25 years (range 16–40).
All patients were interviewed several times during the first phase of their inpatient stay for the comprehensive diagnostic assessment, and subsequently with the structured diagnostic assessment. Average length of stay was 17 weeks (range 3–67). Mean time from admission to the structured diagnostic interview was 41 days (range 5–230).
Cross tabulation of DSM-IV diagnoses by the two diagnostic procedures appear in Table 2. Kappa of overall concordance between the diagnostic procedures was 0.21. The kappa agreement between SCID and best-estimate diagnoses with the sample dichotomized into the schizophrenia spectrum (schizophrenia, other psychoses, schizotypal disorder) vs. non-spectrum (the remaining diagnostic groups combined) was 0.20.
Using the best estimate consensus diagnoses as gold standard, the sensitivity and specificity of the SCID for schizophrenia alone were 46% and 95%, respectively. The figures for the schizophrenia spectrum (schizophrenia, other non-affective psychoses and schizotypal disorder) were 45.5% and 91%.
In 33 (60%) of the 55 patients, the SCID diagnosis differed from the best-estimate consensus diagnosis. The best-estimate consensus procedure identified more patients with a schizophrenia spectrum diagnosis than the SCID procedure, i.e., 35 vs. 16, respectively. In addition, SCID classified all patients with a best-estimate consensus diagnosis of schizotypal disorder (n = 6) with other or no diagnosis. In explorative analysis, using numerical summaries of the data and visualizations, we identified two possible explanations for these disagreements.
1. Incomplete information: Among the 19 non-identified schizophrenia patients by SCID, seven had a deferred diagnosis, six received other diagnoses such as substance abuse/dependence (n = 4) or anxiety disorder (n = 2), three patients were diagnosed with an affective disorder, while three received a diagnosis of other psychoses (delusional disorder or psychosis NOS).
2. Level of comorbidity: The SCID diagnostic procedure yielded high levels of comorbidity. The number of comorbid diagnoses in addition to the main diagnosis is shown in Table 2. In 27 patients (49%), the SCID generated two or more comorbid conditions. The diagnostic category “Major depression” was the most common diagnosis identified with the SCID, and 19 patients (35%) received this diagnosis either as the main diagnosis or as a comorbid diagnosis.
We found low overall kappa values (κ value 0.21), and slightly lower when comparing spectrum level diagnoses (κ value 0.20). This is in line with the finding of Nordgaard et al. (22), who found comparable low kappa values (κ value 0.18). According to the standard used in the literature on kappa statistics, this corresponds to a category of «questionable agreement» (35, 36). In terms of the clinical utility estimates, we found that the SCID procedure failed to detect 24 out of 44 patients with a schizophrenia spectrum diagnosis (a sensitivity of 45.5%). These findings corroborate those by Nordgaard et al. (22) and point to major problems in applying SCID to clinical settings.
Studies comparing structured diagnostic interviews with other diagnostic procedures have sometimes found better performance than our findings by the structured interviews with kappa values reported between 0.59–0.90 (20, 37, 38). However, in all of these studies, variations in the sources of information used in the compared diagnostic procedures are of great importance. In the study by Basco et al. comparing expert-generated diagnosis with SCID interviews performed by trained psychiatric nurses, (37), an important finding was that SCID generated diagnoses significantly improved with additional data sources such as review of medical records. In studies finding high levels of agreement between SCID generated research diagnosis and routine clinical diagnoses, the SCID diagnoses are reported to be based on interview data and reviews of medical records (39, 40). Indeed, in the study by Fennig et al. (41), SCID elicited data was found to be an incomplete source of data in the detection of psychosis in a first-admission sample. In their sample of first-admission patients with psychosis, 13.7% denied all their psychotic symptoms, while 33.3% revealed only some of their symptoms. The conclusion was that SCID generated diagnoses without incorporating longitudinal and external sources of clinical data, and the generated diagnoses were therefore of questionable validity.
The explorative analysis in the current study highlighted that many patients with a best-estimate consensus diagnosis of schizophrenia spectrum, either received no diagnosis (deferred diagnosis) or other non-psychotic diagnoses such as anxiety, depression or substance abuse. There may be several explanations for this. It is possible that many patients seen in clinical practice tend to dissimulate their psychotic experiences, and the SCID is particularly vulnerable to such response styles. Thus, the use of structured diagnostic interviews, developed in research contexts where participants have consented to take part in a research study, in clinical practice may lead to an over-reliance on the patients willingness to disclose their innermost experiences. This is possibly also compounded with the ways most questions are phrased in structured interviews. In an effort to reduce criterion variance, clinical inquiries in the SCID are designed to be unidirectional where endorsement of a question signifies psychopathology. This transparency, where the patient has a very clear idea of the purpose of questions and is free to modify answers accordingly, may lead to a response set where all psychotic symptoms are denied, leading to either no diagnosis or a non-psychotic diagnosis (9). Another possibility is that the phrasing of many questions in the SCID is very specific, often simply a rephrasing of diagnostic criteria, and some patients may not recognize their own experiences as instances of the symptom. Thus, a patient may deny having thought insertion in response to the question “Do you ever experience certain thoughts that are not your own are being placed in your head?,” could still harbor experiences of alien thoughts, not necessarily “being placed” or “inserted” into his mind, but perhaps rather experienced as simply being there (42).
We also found high levels of comorbidity in the SCID generated diagnoses. This is in part a consequence of the explicit encouragement by the DSM system to make as many diagnoses as necessary to cover the full clinical picture. A similar formulation can be found in ICD-10 but it has a different implication in terms of recorded diagnosis due to its diagnostic hierarchy, which, by contrast, is not present to the same extent in DSM. Thus, rather than focusing on the exploration of symptomatology, the SCID explicitly focuses on diagnoses. This is reflected in the clinical inquiries, where the predetermined questions are presented in a definite order (43), the order being specified by the diagnostic criteria listed in the DSM manual. By contrast, in clinical interviews taking the chronological, psychosocial history as a point of departure for psychopathological exploration, symptoms and signs are more naturally evaluated in the context of the patient’s life history and phase of illness. Rather than evaluating symptoms and signs as related to possible co-occurring disorders, careful exploration of the progression of psychopathology reveal many of these may be psychopathological aspects of the same disorder. In the schizophrenia spectrum, most patients report experiences of depression and anxiety in the course of illness. However, these experiences are not co-occurring independent disorders but are well-known aspects of schizophrenia and should therefore, in ICD-10, typically not be recorded as comorbid diagnoses to the index diagnosis of schizophrenia (44). Psychopathological phenomena are generally interdependent aspects of a whole or a “gestalt” (45). In phenomenological psychopathology, a «psychopathological gestalt» is a «certain unifying structure of experimental, expressive and behavioral phenomena, which transpires through, connects, shapes and colors the symptoms and signs that may occur within a given mental disorder» (46). Multiple nonpsychotic symptoms, perhaps with a pervasive pattern considered atypical of true neurotic disorders conveyed by the classical notion of “pseudoneurotic symptoms” (47), should cause suspicion of a common psychopathological process. But such gestaltic considerations is less likely in criteria-focused structured diagnostic interviews. Preformed questions and the strict sequencing of clinical inquiries, do not allow the “staying with” psychopathological experiences and withholding interpretation in terms of symptoms and signs, until the experience is fully grasped.
There are some limitations to the generalizability of these findings. The sample size is small, we used only one interviewer for the structured interviews, and the participants were not randomly selected from a general, heterogenous psychiatric population. Participants were all first-time admitted patients and referral was based on evaluation of the presence of psychosis. The study group included a larger proportion of patients with a schizophrenia spectrum diagnosis, making the comparison to other more heterogenous samples uncertain. We do not believe that these limitations seriously question the main findings. One of the strengths is that the study sample is from an ordinary specialist health care responsible for delivering care to patients in a catchment area of 480,000, which makes the ecological relevance high.
The implications of this study for recommendations given in clinical guidelines and the training of clinicians are significant. In clinical practice, accurate diagnosis is of immense value for patients. Clinicians have practical concerns, and diagnoses are crucial for treatment planning and treatment decisions. Patients who are misdiagnosed may receive inadequate or ineffective treatment, and risk readmission with diagnostic reassessments, often with different or even incompatible diagnoses. Using ineffective diagnostic methods in mental health services is costly in terms of the time and resources spent.
Our finding that a structured diagnostic procedure, at least as performed in a fully structured way without solid psychopathological knowledge and without utilizing all available sources of information, is not an adequate way of allocating diagnoses in clinical practice. It is likely that an experienced clinician with training in psychopathology, taking advantage of the possibility to ask further questions and availability of other sources of information, would arrive at more valid diagnoses. Indeed, according to the User’s guide (24), it is allowed to use the SCID as a diagnostic checklist rather than a structured interview, with information obtained from other sources. However, as we argue, some of the problems with structured diagnostic interviews are inherent to the criteria-focused format of the clinical inquiries in the structured methods. This makes it difficult for clinicians using a structured diagnostic interview to make considerations of the gestalt when exploring psychopathology. These considerations are crucial for adequate differential-diagnosis.
Overall, there is a need to revive teaching and training in psychopathology and comprehensive differential-diagnosis. The most important factor for successful interviewing is knowledge of psychopathology. This requires far more than training in a specially selected interview schedule. Training in psychopathology implies academic studies, supervised diagnostic interviews, joint interviews with colleagues, ongoing peer-discussions of psychopathological concepts, and participation in consensus meetings with experts for differential-diagnostic evaluations.
In conclusion, the findings in the current study are largely in agreement with the findings in Nordgaard et al. (22), and it adds further support to their claim that structured diagnostic interviews performed by mental health professionals without solid psychopathological knowledge and experience, is not recommendable for clinical practice.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the participants’ legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
EK was the primary investigator, did the data analysis, wrote the outline and first draft of the manuscript, and is responsible for the overall content as guarantor. EK and SN designed and planned the study and were actively involved in interpretating the results, revising the manuscript and approving the final version. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Malt, UF, Andreassen, OA, Malt, EA, Melle, I, and Årsland, D. Textbook of psychiatry (Lærebok i psykiatri). Oslo: Gyldendal akademisk (2018). 1060 p.
2. Health NDO. National Guideline for the assessment, treatment and follow-up for persons with psychotic disorders (Nasjonal faglig retningslinje for utredning, behandling og oppfølging av personer med psykoselidelser). (2013). Available at: https://www.helsedirektoratet.no/retningslinjer/psykoselidelse
3. Kraepelin, E, and Diefendorf, AR. Clinical psychiatry: A textbook for students and physicians, abstracted and adapted from the 7th German edition of Kraepelin’s Lehrbuch Der Psychiatrie. New York: Macmillan Co (1907). 562 p.
4. Tilley, DH, and Hoffman, JA. Mental status examination: myth or method. Compr Psychiatry. (1981) 22:562–4. doi: 10.1016/0010-440X(81)90004-3
5. Engel, IM. The mental status examination in psychiatry: origin, use, and content. Acad Psychiatry. (1979) 3:99–108. doi: 10.1007/BF03399728
6. Spitzer, RL, Fleiss, JL, Burdock, EI, and Hardesty, AS. The mental status schedule: rationale, reliability and validity. Compr Psychiatry. (1964) 5:384–95. doi: 10.1016/S0010-440X(64)80048-1
7. Endicott, J, and Spitzer, RL. A diagnostic interview: the schedule for affective disorders and schizophrenia. Arch Gen Psychiatry. (1978) 35:837–44. doi: 10.1001/archpsyc.1978.01770310043002
8. Spitzer, RL, Williams, JB, Gibbon, M, and First, MB. The structured clinical interview for DSM-III-R (SCID). I: history, rationale, and description. Arch Gen Psychiatry. (1992) 49:624–9. doi: 10.1001/archpsyc.1992.01820080032005
9. Rogers, R. Handbook of diagnostic and structured interviewing. New York: Guilford Press (2001). 516 p.
10. Nordgaard, J, Sass, LA, and Parnas, J. The psychiatric interview: validity, structure, and subjectivity. Eur Arch Psychiatry Clin Neurosci. (2013) 263:353–64. doi: 10.1007/s00406-012-0366-z
11. Cooper, JE, Kendell, RE, Gurland, BJ, Sharpe, L, Copeland, JRM, and Simon, R. Psychiatric diagnosis in New York and London. London: Oxford University Press (1972).
12. Spitzer, RL. Psychiatric diagnosis: are clinicians still necessary. Compr Psychiatry. (1983) 24:399–411. doi: 10.1016/0010-440X(83)90032-9
13. Lobbestael, J, Leurgans, M, and Arntz, A. Inter-rater reliability of the structured clinical interview for DSM-IV Axis I disorders (SCID I) and Axis II disorders (SCID II). Clin Psychol Psychother. (2011) 18:75–9. doi: 10.1002/cpp.693
14. Martin, CS, Pollock, NK, Bukstein, OG, and Lynch, KG. Inter-rater reliability of the SCID alcohol and substance use disorders section among adolescents. Drug Alcohol Depend. (2000) 59:173–6. doi: 10.1016/S0376-8716(99)00119-2
15. Segal, DL, Hersen, M, Van Hasselt, VB, Kabacoff, RI, and Roth, L. Reliability of diagnosis in older psychiatric patients using the structured clinical interview for DSM-III-R. J Psychopathol Behav Assess. (1993) 15:347–56. doi: 10.1007/BF00965037
16. Segal, DL, Hersen, M, and Van Hasselt, VB. Reliability of the structured clinical interview for DSM-III-R: an evaluative review. Compr Psychiatry. (1994) 35:316–27. doi: 10.1016/0010-440X(94)90025-6
17. Skre, I, Onstad, S, Torgersen, S, and Kringlen, E. High interrater reliability for the structured clinical interview for DSM-III-R Axis I (SCID-I). Acta Psychiatr Scand. (1991) 84:167–73. doi: 10.1111/j.1600-0447.1991.tb03123.x
18. Zanarini, MC, Skodol, AE, Bender, D, Dolan, R, Sanislow, C, Schaefer, E, et al. The collaborative longitudinal personality disorders study: reliability of axis I and II diagnoses. J Personal Disord. (2000) 14:291–9. doi: 10.1521/pedi.2000.14.4.291
19. Zanarini, MC, and Frankenburg, FR. Attainment and maintenance of reliability of axis I and II disorders over the course of a longitudinal study. Compr Psychiatry. (2001) 42:369–74. doi: 10.1053/comp.2001.24556
20. Fennig, S, Craig, T, Lavelle, J, Kovasznay, B, and Bromet, EJ. Best-estimate versus structured interview-based diagnosis in first-admission psychosis. Compr Psychiatry. (1994) 35:341–8. doi: 10.1016/0010-440X(94)90273-9
21. Kranzler, HR, Kadden, RM, Babor, TF, Tennen, H, and Rounsaville, BJ. Validity of the SCID in substance abuse patients. Addiction. (1996) 91:859–68. doi: 10.1111/j.1360-0443.1996.tb03580.x
22. Nordgaard, J, Revsbech, R, Sæbye, D, and Parnas, J. Assessing the diagnostic validity of a structured psychiatric interview in a first-admission hospital sample. World Psychiatry. (2012) 11:181–5. doi: 10.1002/j.2051-5545.2012.tb00128.x
23. First, MB, Spitzer, RL, Gibbon, M, and Williams, JBW. Structured clinical interview for DSM-IV Axis I disorders (SCID-I), Clinician Version: Administration Booklet. Washington, DC: American Psychiatric Press (1996). 84 p.
24. First, MB, Spitzer, RL, Gibbon, M, and Williams, JBW. User’s guide for the structured clinical interview for DSM-IV Axis I disorders SCID-I: clinician version. Washington, DC: American Psychiatric Press (1997). 132 p.
25. Ventura, J, Liberman, RP, Green, MF, Shaner, A, and Mintz, J. Training and quality assurance with the structured clinical interview for DSM-IV (SCID-I/P). Psychiatry Res. (1998) 79:163–73. doi: 10.1016/S0165-1781(98)00038-9
26. First, MB. User’s guide for the structured clinical interview for DSM-IV Axis II personality disorders: SCID-II. Washington, DC: American Psychiatric Pub (1997). 91 p.
27. Jaspers, K. General psychopathology, vol. XL. Baltimore, MD: Johns Hopkins University Press (1997). 448 p.
28. Chisolm, MS, and Lyketsos, CG. Systematic psychiatric evaluation: A step-by-step guide to applying the perspectives of psychiatry. Baltimore MD: JHU Press (2012). 264 p.
29. Jansson, L, and Nordgaard, J. The psychiatric interview for differential diagnosis. Cham: Springer International Publishing (2016).
30. Henriksen, MG, and Nordgaard, J. A cookbook recipe for the clinical and phenomenologically informed, semi-structured diagnostic interview In: MPA Biondi, M Pallagrosi, and L Fonzi, editors. The clinician in the psychiatric diagnostic process. Cham, Switzerland: Springer (2022). 37–50.
31. McGuffin, P, Farmer, A, and Harvey, I. A polydiagnostic application of operational criteria in studies of psychotic illness. Development and reliability of the OPCRIT system. Arch Gen Psychiatry. (1991) 48:764–70. doi: 10.1001/archpsyc.1991.01810320088015
32. Rucker, J, Newman, S, Gray, J, Gunasinghe, C, Broadbent, M, Brittain, P, et al. OPCRIT+: an electronic system for psychiatric diagnosis and data collection in clinical and research settings. Br J Psychiatry. (2011) 199:151–5. doi: 10.1192/bjp.bp.110.082925
33. Parnas, J, Møller, P, Kircher, T, Thalbitzer, J, Jansson, L, Handest, P, et al. EASE: examination of anomalous self-experience. Psychopathology. (2005) 38:236–58. doi: 10.1159/000088441
34. Leckman, JF, Sholomskas, D, Thompson, WD, Belanger, A, and Weissman, MM. Best estimate of lifetime psychiatric diagnosis: a methodological study. Arch Gen Psychiatry. (1982) 39:879–83. doi: 10.1001/archpsyc.1982.04290080001001
35. Landis, JR, and Koch, GG. The measurement of observer agreement for categorical data. Biometrics. (1977) 33:159–74. doi: 10.2307/2529310
36. Kraemer, HC, Kupfer, DJ, Clarke, DE, Narrow, WE, and Regier, DA. DSM-5: how reliable is reliable enough. Am J Psychiatry. (2012) 169:13–5. doi: 10.1176/appi.ajp.2011.11010050
37. Basco, MR, Bostic, JQ, Davies, D, Rush, AJ, Witte, B, Hendrickse, W, et al. Methods to improve diagnostic accuracy in a community mental health setting. Am J Psychiatr. (2000) 157:1599–605. doi: 10.1176/appi.ajp.157.10.1599
38. Bucholz, KK, Nurnberger, JI, Kramer, JR, Hesselbrock, VM, Schuckit, MA, and Bierut, LJ. Comparison of psychiatric diagnoses from interview reports with those from best-estimate procedures. J Stud Alcohol. (2006) 67:157–68. doi: 10.15288/jsa.2006.67.157
39. Nesvåg, R, Jönsson, EG, Bakken, IJ, Knudsen, GP, Bjella, TD, Reichborn-Kjennerud, T, et al. The quality of severe mental disorder diagnoses in a national health registry as compared to research diagnoses based on structured interview. BMC Psychiatry. (2017) 17:93. doi: 10.1186/s12888-017-1256-8
40. Vares, M, Ekholm, A, Sedvall, GC, Hall, H, and Jönsson, EG. Characterization of patients with schizophrenia and related psychoses: evaluation of different diagnostic procedures. Psychopathology. (2006) 39:286–95. doi: 10.1159/000095733
41. Fennig, S, Bromet, EJ, Jandorf, L, Schwartz, JE, Lavelle, J, and Ram, R. Eliciting psychotic symptoms using a semi-structured diagnostic interview. The importance of collateral sources of information in a first-admission sample. J Nerv Ment Dis. (1994) 182:20–6. doi: 10.1097/00005053-199401000-00005
42. Henriksen, MG, Englander, M, and Nordgaard, J. Methods of data collection in psychopathology: the role of semi-structured, phenomenological interviews. Phenomenol Cogn Sci. (2022) 21:9–30. doi: 10.1007/s11097-021-09730-5
43. Beck, SM, and Perry, JC. The definition and function of interview structure in psychiatric and psychotherapeutic interviews. Psychiatry. (2008) 71:1–12. doi: 10.1521/psyc.2008.71.1.1
44. Mølstrøm, IM, Henriksen, MG, and Nordgaard, J. Differential-diagnostic confusion and non-specificity of affective symptoms and anxiety: an empirical study of first-admission patients. Psychiatry Res. (2020) 291:113302. doi: 10.1016/j.psychres.2020.113302
45. Parnas, J. The core gestalt of schizophrenia. World Psychiatry. (2012) 11:67–9. doi: 10.1016/j.wpsyc.2012.05.002
46. Nordgaard, J. Psychopathology in the schizophrenia spectrum: The subjective dimension. Dissertation. University of Copenhagen; (2021).
Keywords: structured interview, diagnosis, schizophrenia spectrum, psychopathology, phenomenology
Citation: Kvig EI and Nilssen S (2023) Does method matter? Assessing the validity and clinical utility of structured diagnostic interviews among a clinical sample of first-admitted patients with psychosis: A replication study. Front. Psychiatry. 14:1076299. doi: 10.3389/fpsyt.2023.1076299
Received: 26 October 2022; Accepted: 13 March 2023;
Published: 03 April 2023.
Edited by:
Mads Gram Henriksen, University of Copenhagen, DenmarkReviewed by:
Andreas Rosén Rasmussen, University Hospital of Copenhagen, DenmarkCopyright © 2023 Kvig and Nilssen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Erling Inge Kvig, ZWlrQG5sc2gubm8=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.