
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Psychiatry, 07 February 2023
Sec. Public Mental Health
Volume 14 - 2023 | https://doi.org/10.3389/fpsyt.2023.1063276
This article is part of the Research TopicSystematic Reviews in Ethics and Public Mental HealthView all 4 articles
Objective: Staff’s attitudes to the use of coercion may influence the number of coercive interventions employed and staff willingness to engage in professional development projects aimed at reducing the use of coercion itself. The Staff Attitude to Coercion Scale (SACS) was developed to assess the attitudes of mental healthcare staff to the use of coercion in 2008 and has been employed subsequently. This global study systematically reviews and summarizes the use of the scale in research.
Methods: Seven databases were searched for studies using SACS in articles published in peer reviewed journals and gray literature. In addition, researchers who have asked for permission to use the scale since its development in 2008 were contacted and asked for their possible results. Extracting of data from the papers were performed in pairs of the authors.
Results: Of the 82 identified publications, 26 papers with 5,838 respondents were selected for review. A review of the research questions used in the studies showed that the SACS questionnaire was mostly used in studies of interventions aimed at reducing coercion and further explain variation in the use of coercion.
Conclusion: SACS is, to our best of knowledge, the only questionnaire measuring staff’s attitudes to the use of coercive interventions in mental health services. Its widespread use indicates that the questionnaire is perceived as feasible and useful as well as demonstrating the need for such a tool. However, further research is needed as the relationship between staff attitudes to coercion and the actual use of coercion remains unclear and needs to be further investigated. Staff attitudes to coercion may be a prerequisite for leaders and staff in mental healthcare to engage in service development and quality improvement projects.
The use of coercive practices is contested, with a long history of debate and controversy within mental healthcare (MHC) services (1–3). In line with heightened focus on human and users’ rights in healthcare services in society in general, the health authorities in many countries and international organizations have advocated for a reduction in the use of coercive practices, developing and promoting services based on informed consent instead (4–6).
At the beginning of the 21st century (2003–2005), a multi-center study of the European Evaluation of Coercion in Psychiatry and Harmonization of Best Clinical Practice (EUNOMIA) was carried out to assess the extent of the use of coercion in psychiatry. The results showed differences in the frequency of the use of coercive measures not only between respective countries, but also between institutions or departments, while factors increasing the risk of coercion were divided into three independent groups: characterizing the patient, treatment center, and staff. The quality of work and the atmosphere in the ward, the relationship between patients and staff, and the experience of medical personnel are all important factors affecting the frequency of the use of coercion (7, 8).
As presented, previous research has shown considerable variation in the use of coercive measures in MHC within (9–11) and between countries (12–15). This variation indicates that some MHC institutions deliver care with less use of coercive measures than others (4, 6, 16), but factors influencing variation in the use of coercive practices are not fully understood. However, staff attitudes to the use of coercion are presumed to be one of many factors explaining this variation (17–19).
Attitudes are a central topic of study in social psychology, and a commonly accepted definition of attitudes are “a psychological tendency that is expressed by evaluating a particular entity with some degree of favor or disfavor” (20). Attitudes can vary along the dimensions of strength and valence, where strength indicates how strong the attitude is and valence refers to direction (either positive or negative). Examples of mechanisms forming attitudes are modeling, positive and negative reinforcement, and other learning mechanisms affecting a person’s evaluation of an object or phenomenon (21). Attitudes are often formed and changed in social interactions and through experience with the object of attitude (22). Individuals’ attitudes are assumed to influence their actual behavior. Research has, however, revealed that the connection between people’s attitudes and behavior are complex and less straightforward, as Ajzen (23) describes in “The theory of planned behavior” (23).
The “Staff Attitude to Coercion Scale” (SACS) was developed and published in 2008 as a valid and feasible instrument to measure staff attitudes to coercion (24). Since then, the questionnaire has been used in several countries (25–28). In addition to the original Norwegian and English translation, the SACS questionnaire has been translated into Farsi, German, Polish, and Chinese (25, 26, 28, 29). Japanese, Belgian, and Italian versions have been translated, but are not yet published.
In addition, the questionnaire has been employed in one study in populations with caregivers (30). The SACS questionnaire consists of 15 normative statements about the use of coercion, what one thinks about the use of coercion, and if one believes coercion should be used more or not. Normative statements contain a value judgment. It also contains statements that the use of coercion can cause various types of harm and offense to patients. The use of the questionnaire has shown that the items can be sorted into three dimensions:
SACS I: Coercion is needed for security and care reasons (pragmatic)
SACS II: Coercion may offend and harm patients (critical)
SACS III: Coercion is useful in treatment (positive) Psychometric properties have been assessed in a previous systematic review, which concluded that the included studies provided support for adequate structural validity and internal consistency, while other important measurement properties were not addressed by the studies reviewed. Caution is therefore warranted when interpreting the results of the SACS in terms of aspects such as reliability, criterion validity, and measurement error (31). This is, however, to our knowledge, the first attempt to perform a systematic literature review of the use and results of studies that have used the SACS questionnaire.
The review questions were:
1. How has the SACS questionnaire been used?
2. What research questions have answers been sought for using SACS?
3. What did studies using SACS find regarding staff attitudes to coercion?
- Differences between professions.
- Differences between genders.
- Age group differences.
- Work experience.
- Relationship with other measures.
- Can Staff Attitudes to Coercion be changed?
- Relationship between staff attitudes to coercion and actual use of coercion.
A systematic literature search was conducted by a librarian using the following databases: MEDLINE via EBSCOhost, PsycINFO via APA PsycNET, Embase via Elsevier, CINAHL via EBSCOhost, the Web of Science via Thomson Reuters, Google Scholar, and OpenGrey. The full search string can be found in Supplementary Appendix A. The search focused on identifying original published studies in the form of articles published in peer reviewed journals. PhDs were also included. In addition, researchers who have asked for permission to use the scale since its development in 2008 were contacted and asked for their possible results. Variants of the following terms were used as search terms:
• SACS
• Staff attitudes to the coercion scale
• Staff attitudes toward the coercion scale
• Staff normative attitudes toward coercion
No restrictions were placed on the language of publication. The first search was performed in February 2021, with an updated search being performed in October 2021. In the update of the search, six new publications were found, but the only one of these that met the inclusion criteria had already been included from other searches. After the initial assessment of the papers, 29 papers were read in full-text versions by two people in pairs, searching for eligibility. In the case of uncertainty, inclusion was discussed and agreed upon by a third reviewer. The systematic review was conducted according to PRISMA guidelines. Figure 1 shows a flow chart of the search process.
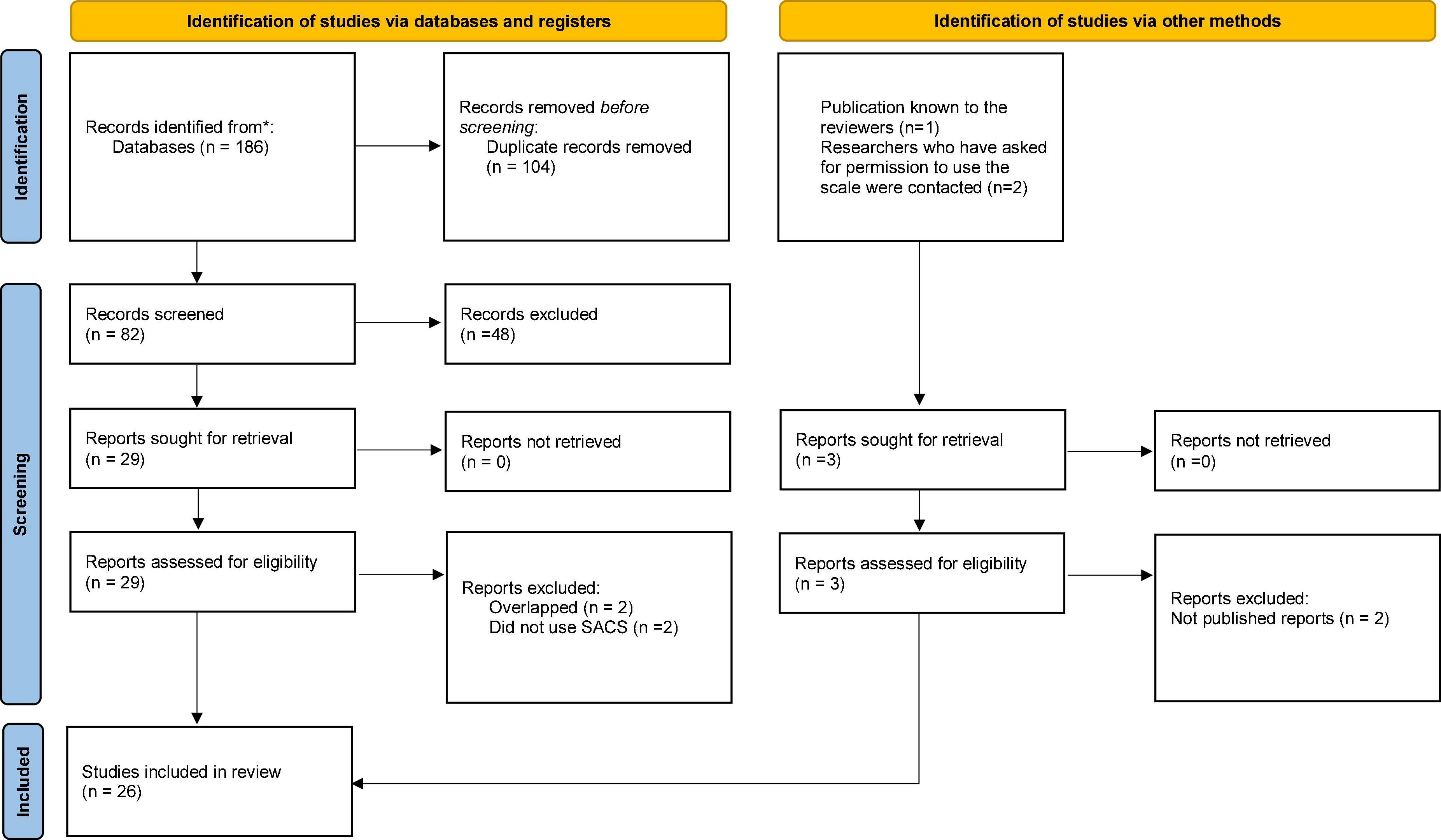
Figure 1. PRISMA 2020 flow diagram for new systematic reviews which included searches of databases, registers, and other sources [adapted from Page et al. (55) and Mahdanian et al. (6)]. *Number of records identified from each database is presented in the Supplementary Appendix A in the description of the database search.
Extracting data from the papers were also performed in the same pairs of authors. Altogether, 26 papers were included in the review. A list of the 26 included papers is shown in Table 1.
Of the 26 included papers, 17 studies were conducted in Europe (17–19, 24, 26–28, 32–41), two in the USA (42, 43), three in the Middle East (Jordan and Iran) (25, 44, 45), two in India (30, 46), one in Australia (47), and one in Taiwan (29). Of these, eight studies had used an English translation (30, 37, 42–47), six the original Norwegian version (17, 19, 24, 34, 38, 41), eight a German translation (18, 26, 32, 33, 35, 36, 39, 40), two a Polish translation (27, 28), one in Farsi (25), and one in Chinese (29). Altogether, 5,838 informants participated in the studies, but some studies have probably included the same participants, so this number is just an estimate.
Most studies were descriptive and cross-sectional, while five studies were on interventions (38, 40, 41, 43, 45). One study used a pre-post measure design (41), and one study had a randomized controlled trial design (18). One study used a yes/no response instead of the original five-point Likert scale (30), and one study had used a four-point scale (36). Five of the studies had only translation and validation as its purpose (24–28). Two studies analyzed the single items, and not the three subscales (28, 47). Three studies confirmed the original three-factor model (25, 27, 28), and one study found that a one-factor model was better suited (26).
The research questions in all the papers are shown in Table 2. A review of the research questions in the included studies showed that the SACS questionnaire was mostly used in studies aimed at reducing use of coercion or to try to explain variation in the use of coercive interventions. Some studies also aimed at explaining reasons for the use of coercive interventions and geographical variation in use. Five studies were solely validations and translations of the SACS in other cultural settings, and some aimed at describing staffs’ attitudes and investigating the differences between different staff groups. One study investigated why the use of coercion had not declined despite guidance from health authorities.
Most staff considered the use of coercion as necessary for providing “care and security” and supported its use. On the whole, staff seemed to have a pragmatic view on the use of coercive interventions as needed for security reasons (29, 34) and that use of coercion was needed for security reasons: however, staff also commonly reported concerns about coercive measures potentially having offending and harmful effects on the patients (36, 47). Overall, the informants did not seem to view the use of coercive interventions as a treatment intervention (25). Two studies found that attitudes to coercion differed at an individual level between individuals, indicating that attitudes are influenced by individuals’ own personality and values (34, 41). Husum (9) found more difference between individuals than between staff groups (34). Further, two studies found significant differences between wards (34, 41), and one study found stable differences between wards across time (41). The same study found that staff on wards using the most coercive measures also had the most positive attitudes toward the use of coercive measures.
Of the studies with descriptive designs, many reported significant professional differences in attitudes (18, 36). One of the most consistent findings was that nurses were more positive toward coercive interventions and scored higher on the “Coercion as treatment” subscale than psychiatrists and psychologists (18, 27, 28, 36). One study found that most psychiatrists considered coercion as a caring, protective, and safety intervention, but also acknowledged its potential negative impact on patient dignity and therapeutic relationships (48). One study found that staff members with a university education scored lower on the “Coercion as offending” subscale compared to nurses (34); while one study found that staff with more education were significantly less in favor of use of coercion (43). This difference was especially visible concerning the “Coercion as treatment” subscale, where staff with undergraduate degrees were more likely to consider involuntary hospitalization as treatment compared to staff with a post-graduate degree, and to consider the use of coercive measures as treatment (29, 34). One study [Raveesh et al. (30)] compared attitudes to coercion between psychiatrists and caregivers. They found both psychiatrists and caregivers agreed that the use of coercion is related to scarce resources, security concerns, and harm reduction. Both groups agreed that coercion is necessary, but not as treatment. Both psychiatrists and caregivers considered coercion necessary for protection in dangerous situations. Interestingly, they found that reliability was reasonably good for psychiatrists, but not for caregivers (30).
Three studies reported gender differences. Husum et al. (24) found that women had marginally lower scores on the “Coercion as treatment” subscale (24). Krieger et al. (36), however, found no significant gender differences on the subscales (36). Raveesh et al. (30) found that male psychiatrists considered coercion more related to scarce resources and violating patient integrity when compared to other staff (30).
Husum et al. (24) found that staff older than 40 years considered use of coercion to be more an offense against patients than younger staff members (24). Krieger et al. (36), however, did not find any differences in attitudes related to age (36).
Four studies found that more work experience was related to a more critical view of coercion. Two studies found that staff members with the most work experience had a more critical view on “Coercion as offending” in comparison with less experienced staff (28, 36). Two studies found a positive correlation between working experience and the rating of “Coercion as care and security” (33, 44).
Nine studies assessed the relationship between SACS and other concepts and measures. Elmer et al. (32) found that the recognition and application of informal coercion correlated with attitudes toward coercion (32). Hotzy et al. (33) found that a higher score on the “Coercion as treatment” subscale correlated with staff finding it harder to comprehend the legal basis for decisions (33).
Jaeger et al. (35) found that the degree of coercion inherent to interventions comprising persuasion and leverage was underestimated by professionals with a positive attitude and overestimated by those with a negative attitude toward the respective interventions. They conclude that an advanced understanding of the influencing factors of professionals’ attitudes toward coercion could lead to improved training of professionals in utilizing interventions to enhance informed and ethical treatment strategies (35).
Lambert et al. (37) studied the relationship between SACS scores and the interpersonal style of staff. They found that the “Negotiator boundary management” style was associated with the “pragmatic attitude” to coercion, that is, a pragmatic view that coercion (and restrictive practices) is neither positive nor desirable but is sometimes necessary in order to maintain safety and security (37).
Molewijk et al. (19) investigated the relationship between staff being in “moral doubt” and the SACS scores. They found that staff who were more in doubt about the “moral rightness” of coercive interventions were in general more prone to possess a more critical view toward the use of coercion on the “Coercion as offending” subscale. Staff who were more occupied with morality were less prone to view coercion as treatment (19).
Two studies investigated the connection between SACS scores and recovery-oriented interventions. Molewijk et al. (49) studied the relationship between recovery expectations and attitudes to coercion. They found that the more optimistic recovery expectations staff possessed and working on open wards with fewer involuntary admissions and lower bed occupancy were associated with more critical attitudes to coercion (39). Rabenschlag et al. (40) used an RCT design to assess the implementation of a recovery-oriented ward concept and found that staff attitudes to coercion changed significantly in the intervention group compared to the control group (40).
Further, Vandamme et al. (18) studied the connection of staffs’ implicit and explicit attitudes toward use of coercion, and found no association (18). Lastly, Krieger et al. (36) investigated the relationship between staff attitudes to coercion and emotions, such as compassion, helplessness, grief, anxiety, sense of power, anger, guilt, and desperation, which seem to influence staff attitudes and suggest this as a future research topic (36).
Five studies report on change in staff attitudes to coercion. Al-Maraira et al. (45) found that staff attitudes showed change after implementing a training program aimed at altering attitudes based on Ajzen’s Theory of Planned Behavior. After four weeks of training, nurses in the intervention group demonstrated significant change in their attitudes’ mean scores, in the direction of gaining more critical attitudes toward use of coercive practices (45). Molewijk et al. (38) implemented the use of ethical reflection groups in staff groups and also found that attitudes (SACS scores) changed during time in a more negative/critical direction toward coercion after staff engaging in the ethical reflection groups (38).
Further, Orlick (43) found that, after implementing an intervention consisting of training in de-escalation techniques to reduce the use of restrains and seclusion, staff attitudes were found to be more critical to the use of coercion and more concerned about the potentially offending effects of coercive measures. There was, however, also a counterintuitive rise in the “security and care” scale (43). Rabenschlag et al. (40) investigated staff attitudes in relation with implementing a recovery-oriented ward concept and found that staff attitudes toward coercion did not change significantly in the intervention group but did so compared to the control group after intervention (recovery-oriented ward concept) (40). Last, an action-research project aimed at reducing the use of coercive interventions in hospitals found that staffs’ positive attitudes to coercion showed a slight decrease after the study period, as did the means for the actual use of coercion. Fewer staff scored neutral after the study period and showed stronger opinions about the statements in the SACS questionnaire. The findings were not significant, but there was a statistical tendency (41).
Five studies assessed the relationship between attitudes to coercion and the actual use of coercive interventions. Two of these found no substantial association (17, 18); one study found a tendency that staff on wards using the most coercive measures also had more positive attitudes toward coercive measures. The last study found that interventions (de-escalation techniques) did not reduce the use of restraints and seclusion, but staff attitudes did show some change after such interventions (43).
Since its introduction in 2008, several research groups from many countries have used the SACS, which suggests that there is a need for such a tool and that it has been accepted as useful and feasible in the services.
The questionnaire has mainly been used in European countries but has also been used in India and in the Middle East (Jordan and Iran). Most of the studies confirmed the three-dimension model (with a possible exemption for the German translation). The German population was overall more critical to the use of coercion in care than other populations worldwide. One hypothesis could be that this reflects more positive attitudes toward patients in MHC in general in Germany.
On the whole, staff believe that the use of coercion is necessary for security reasons. We found more variation into what extent staff considered coercion could offend or harm patients. Further, we found that few staff considered the use of coercion as a treatment intervention. In general, nurses were found to be more in favor of coercive interventions than psychiatrists and psychologists. Less experienced staff were also found to be more in favor of the use of coercion. Further, we found studies that indicated that staff attitudes may be changed through targeted interventions such as ethical reflection groups and ethical training in general. When it comes to the connection between attitudes and the actual amount of use employed, the results were more divided.
The main reason for using the SACS scale has been in relation to professional development work to reduce the use of coercive interventions. This can be seen in relationship to the stronger emphasis to protect and promote users’ rights, which has been witnessed over the past 20 years (2, 4, 6). Since this review includes studies from the Middle East, India, and Taiwan, this seems to be a worldwide concern (25, 29, 45, 46). The scale has also been used to try to explain geographical variation in the use of coercive measures, which is a consistent finding in previous research (13, 14). Staff attitudes are often presumed to influence the use of coercive measures. What remains, however, is to establish the relationship between staff attitudes and the use of coercive interventions. Only one of the studies included in this review found a statistical tendency toward changes in staff attitudes being associated with a reduction in the use of coercion (41).
Several studies found, however, that staff attitudes could be altered through different kinds of professional development interventions. One of these interventions was the use of ethical reflection groups (49).
In sum, the overall findings about staff attitudes to coercion is that staff believe that the use of coercive measures are important tools in MHC to secure safety and to take care of people that need to be cared for. The findings indicate that staff are concerned with questions of safety. This indicates that, in order to change attitudes and reduce the use of coercive interventions, it is important to take staffs’ feelings, especially fear and perceived safety, seriously. Further, staff seem to not be very concerned about the potential harmful effects of coercive practices. Concerning the question about whether coercive practices are to be considered as treatment interventions, staff vary more in their views.
Descriptive studies of attitudes revealed differences between groups of professionals, mainly between psychiatrists and mental health nurses. Tendencies toward differences between staff with different amounts of experience and between men and women were also found. What remains, however, is to understand how attitude formation occurs. Attitudes may, for example, be developed through a socialization process during professional training itself (50).
Staff Attitude to Coercion Scale are often used in relation to attempts to reduce the use of coercive practices. Research on the relationship between attitudes and actual behavior shows, however, that it is complex (23). During the last 20 years, many attempts have been developed to reduce the use of coercive practices (2, 51). These are often developed as quality improvement projects in services and have showed positive results. In the compendium from WHO “Promoting person-centered and rights-based approaches in hospital-based mental health services,” some of these developments in successful service models promoting voluntariness in service delivery are presented (52). A summary of the attempts to reduce the use of coercive measures in mental health is that they are successful and reach their goals. However, staff attitudes to coercion may be a prerequisite for leaders and staff in MHC to engage in service development and quality improvement projects.
This systematic literature review has some practical implications. SACS can be used as a questionnaire for measuring the effectiveness of professional training. It might also be useful in assessing the risk of burnout. Further, staff members who perceived coercive measures as the best solution for the patient’s problematic behaviors may require support and additional training.
Staff Attitude to Coercion Scale is, to our best of knowledge, the only questionnaire measuring staff attitudes to the use of coercive interventions in MHC services. It is used widely, which demonstrates the need for such a tool. Its widespread use also indicates that the tool is perceived as feasible and useful. Most informants in the samples consider the use of coercion as necessary in potentially dangerous situations, although less agreement is found concerning the use of coercion as treatment and concern as to how the use of coercion may violate patients. The SACS is designated for MHC staff. In the future, it may also be developed to measure attitudes toward coercive intervention in MHC of other groups of informants, like the population in general, the police, or staff in primary healthcare. We found studies that indicated that staff attitudes may be changed through targeted interventions such as ethical reflection groups and ethical training. However, little is known about other types of training that might affect attitudes toward coercion. It would be interesting to see how other programs/models (like Safewards and Six-core strategy) could modify personnel attitudes (53, 54).
While not formally investigated in this review, changes in attitudes toward coercion in society at large may indicate that a revision of the SACS item may be warranted. After almost 15 years, some items seem outdated and some should possibly be altered. Examples of these are those items employing the words “regressive patients” and “insight.” Items may also be interpreted differently in different cultural settings. Topics for future research could therefore be to investigate cultural differences in staff attitudes to coercion more specifically. Another possible future direction in research on staff attitudes is to look more closely at staff emotions. Staffs’ feeling of safety may influence attitudes and the need to feel safe. Also needed is more investigation into the connection between staff attitudes to coercion and decision making in the process of using coercion. Another important topic for research is to investigate further how to motivate leaders in MHC services to engage in professional development work aimed at reducing the use of coercive practices, and especially how to use existing successful experiences and work to implement these in other services.
The SACS measures complex and sensitive issues, like using coercive measures. For this reason, some of the personnel members might modify their answers due to socially desirable response behavior. In future studies, it would be important to compare the SACS results and the social approval needs of the participants. A step in this direction could be to develop leadership and implementation skills in MHC staff, and to investigate the role of attitudes in implementation science. Most studies have used the three-factor model, but one study used a one-dimensional model. While the SACS is developed using three factors in staff attitudes, it could also be useful to explore the possibilities of developing a model that only uses a general attitude toward the use of coercion.
Analysis of the SACS means and standard deviation reveal, in some cases, different methods of counting the results. For this reason, differences found between the studies examined might be attributed not only to the different populations studied or the implementation of the study but also to the different methods of questionnaire validation. In the future, a systematic process of implementation across different countries and languages should include culturally- appropriate translations of the SACS.
The SACS has mainly been used in European countries, India, and in the Middle East (Jordan and Iran).
The main reason for using the SACS scale has been in relation to professional development work to reduce the use of coercive interventions.
Most of the studies confirmed the three-dimension model (with one exemption for the German translation).
In general, staff believe that the use of coercive measures is important to secure safety and to take care of patients.
Further, staff seem to not be very concerned about the potential harmful effects of coercive practices.
Nurses were found to be more in favor of coercive interventions than psychiatrists and psychologists.
Less experienced staff were more in favor of the use of coercion.
Staff attitudes could be altered through different kinds of professional development interventions.
The items in SACS are formulated in such a way that there is room for personal interpretations of them. The items, for example, do not address different kinds of coercive interventions like involuntary admission, coercive means, and involuntary medication. It is possible that informants view different kinds of coercive interventions differently; these kinds of differences cannot be distinguished using the questionnaire. A limitation with this systematic review is that not all studies have performed a quality insurance process of the translation. Used in different cultural settings, the items may also have different meanings. The scale has been translated and published into only a few languages (English, German, Polish, Farsi, and Chinese). Because of that, general conclusions regarding attitudes toward coercion are limited. It is difficult to compare and analyze cultural diversity. In the future, the availability of other languages should be promoted. Many of the studies are small professional development projects and should be interpreted with caution. A limitation with this study could be that two of the authors were also involved in the development of the original SACS questionnaire and could possibly be biased. We sought to take this into account by collaborating in pairs with the authors not included in the development of the questionnaire. All authors were also involved in the final interpretation of the findings. It is a challenge and possible limitation in this review that the validation process differs between different studies and countries. The SACS was developed and validated in 2008, but it is still popular and there might be a need to adapt the items to new environments and situations.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
All authors have been involved in the process of assessing the studies for inclusion, analyzing the results, and writing the manuscript.
The University of Oslo has paid for the Open Access Publication.
Many thanks to librarian Åse Marit Hammersbøen at Akershus University Hospital for performing the literature searches.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1063276/full#supplementary-material
1. The Lancet. Institutional and coercive mental health treatment in Europe. Lancet. (2018) 391:282. doi: 10.1016/S0140-6736(18)30108-9
2. Gooding P, McSherry B, Roper C. Preventing and reducing ‘coercion’ in mental health services: an international scoping review of English-language studies. Acta Psychiatrica Scand. (2020) 142:27–39. doi: 10.1111/acps.13152
3. Sunkel C, Saxena S. Rights-based mental health care. Lancet Psychiatry. (2019) 6:9–10. doi: 10.1016/S2215-0366(18)30469-3
4. World Health Organization. Guidance on Community Mental Health Services: Promoting Person-centred and Rights-based Approaches. Geneva: WHO (2021).
5. Puras D, Gooding P. Mental health and human rights in the 21st century. World Psychiatry. (2019) 18:42. doi: 10.1002/wps.20599
6. Artin AM, Laporta M, Bold ND, Funk M, Puras D. Human rights in mental healthcare; a review of current global situation. Am J Geriat Psychiat. (2022). doi: 10.1080/09540261.2022.2027348
7. Kalisova L, Raboch J, Nawka A, Sampogna G, Cihal L, Kallert TW, et al. Do patient and ward-related characteristics influence the use of coercive measures? Results from the EUNOMIA international study. Soc Psychiatry Psychiatr Epidemiol. (2014) 49:1619–29. doi: 10.1007/s00127-014-0872-6
8. Fiorillo A, De Rosa C, Del Vecchio V, Jurjanz L, Schnall K, Onchev G, et al. How to improve clinical practice on involuntary hospital admissions of psychiatric patients: suggestions from the EUNOMIA study. Eur Psychiatry. (2011) 26:201–7. doi: 10.1016/j.eurpsy.2010.01.013
9. Husum T. Staff Attitudes and Use of Coercion in Acute Psychiatric Wards in Norway. Ph.D. thesis. Oslo: University of Oslo (2011).
10. Keown P, McBride O, Twigg L, Crepaz-Keay D, Cyhlarova E, Parsons H, et al. Rates of voluntary and compulsory psychiatric in-patient treatment in England: an ecological study investigating associations with deprivation and demographics. Br J Psychiatry. (2016) 209:157–61. doi: 10.1192/bjp.bp.115.171009
11. Hofstad T, Rugkåsa J, Ose S, Nyttingnes O, Husum T. Measuring the level of compulsory hospitalisation in mental health care: the performance of different measures across areas and over time. Int J Methods Psychiatr Res. (2021) 30:e1881. doi: 10.1002/mpr.1881
12. de Stefano A, Ducci G. Involuntary admission and compulsory treatment in europe: an overview. Int J Mental Health. (2008) 37:10–21. doi: 10.2753/IMH0020-7411370301
13. Jacobsen T. Involuntary treatment in Europe: different countries, different practices. Curr Opin Psychiatry. (2012) 25:307–10. doi: 10.1097/YCO.0b013e32835462e3
14. Sheridan Rains L, Zenina T, Dias M, Jones R, Jeffreys S, Branthonne-Foster S, et al. Variations in patterns of involuntary hospitalisation and in legal frameworks: an international comparative study. Lancet Psychiatry. (2019) 6:403–17. doi: 10.1016/S2215-0366(19)30090-2
15. Bak J, Aggernæs H. Coercion within Danish psychiatry compared with 10 other European countries. Nord J Psychiatry. (2012) 66:297–302. doi: 10.3109/08039488.2011.632645
16. Whitaker L, Smith F, Brasier C, Petrakis M, Brophy L. Engaging with transformative paradigms in mental health. Int J Environ Res Public Health. (2021) 18:9504. doi: 10.3390/ijerph18189504
17. Husum T, Bjørngaard J, Finset A, Ruud T. A cross-sectional prospective study of seclusion, restraint and involuntary medication in acute psychiatric wards: patient, staff and ward characteristics. BMC Health Serv Res. (2010) 10:89. doi: 10.1186/1472-6963-10-89
18. Vandamme A, Wullschleger A, Garbe A, Cole C, Heinz A, Bermpohl F, et al. The role of implicit and explicit staff attitudes in the use of coercive measures in psychiatry. Front Psychiatry. (2021) 12:699446. doi: 10.3389/fpsyt.2021.699446
19. Molewijk B, Kok A, Husum T, Pedersen R, Aasland O. Staff’s normative attitudes towards coercion: the role of moral doubt and professional context-a cross-sectional survey study. BMC Med Ethics. (2017) 18:37. doi: 10.1186/s12910-017-0190-0
20. Chaiken S, Stangor C. Attitudes and attitude change. Ann Rev Psychol. (1987) 38:575–630. doi: 10.1146/annurev.ps.38.020187.003043
21. Maio G, Haddock G, Verplanken B. The Psychology of Attitudes & Attitude Change. Thousand Oaks, CA: SAGE Publications Ltd (2019).
22. Vogel T, Wanke M. Attitudes and Attitude Change. Milton Park: Routledge (2016). doi: 10.4324/9781315754185
23. Ajzen I. The theory of planned behavior. Organ Behav Hum Decision Proc. (1991) 50:179–211. doi: 10.1016/0749-5978(91)90020-T
24. Husum T, Finset A, Ruud T. The staff attitude to coercion scale (SACS): reliability, validity and feasibility. Int J Law Psychiatry. (2008) 31:417–22. doi: 10.1016/j.ijlp.2008.08.002
25. Arab M, Gray S, Hamouzadeh P. Validation of the “staff attitude toward coercion use in treatment of mentally ill patients” questionnaire in selected public psychiatric hospitals of Tehran in 2015. J Hospital. (2017) 16:31–42.
26. Efkemann S, Scholten M, Bottlender R, Juckel G, Gather J. A German version of the staff attitude to coercion scale. development and empirical validation. Front Psychiatr. (2020) 11:573240. doi: 10.3389/fpsyt.2020.573240
27. Lickiewicz J, Husum T, Ruud T, Siqveland J, Musiał Z, Makara-Studzińska M. Measuring staff attitudes to coercion in poland. Front Psychiatry. (2021) 12:745215. doi: 10.3389/fpsyt.2021.745215
28. Kiejna A, Jakubczyk M, Gondek T, Rajba B. Kwestionariusz postaw personelu wobec przymusu (SACS)–polska adaptacja. Psychiatr Pol. (2020) 54:113–24. doi: 10.12740/PP/102438
29. Wu H, Tang I, Lin W, Chang L. Professional values and attitude of psychiatric social workers toward involuntary hospitalization of psychiatric patients. J Soc Work. (2013) 13:419–34.
30. Raveesh B, Pathare S, Noorthoorn E, Gowda G, Lepping P, Bunders-Aelen J. Staff and caregiver attitude to coercion in India. Indian J Psychiatry. (2016) 58(Suppl. 2):S221–9. doi: 10.4103/0019-5545.196847
31. Husum T, Ruud T, Lickiewicz J, Siqveland J. Measurement properties of the staff attitude to coercion scale: a systematic review. Front Psychiatry. (2022) 13:744661. doi: 10.3389/fpsyt.2022.744661
32. Elmer T, Rabenschlag F, Schori D, Zuaboni G, Kozel B, Jaeger S, et al. Informal coercion as a neglected form of communication in psychiatric settings in Germany and Switzerland. Psychiatry Res. (2018) 262:400–6. doi: 10.1016/j.psychres.2017.09.014
33. Hotzy F, Marty S, Moetteli S, Theodoridou A, Hoff P, Jaeger M. Involuntary admission for psychiatric treatment: compliance with the law and legal considerations in referring physicians with different professional backgrounds. Int J Law Psychiatry. (2019) 64:142–9. doi: 10.1016/j.ijlp.2019.03.005
34. Husum T, Bjorngaard J, Finset A, Ruud T. Staff attitudes and thoughts about the use of coercion in acute psychiatric wards. Soc Psychiatry Psychiatr Epidemiol. (2011) 46:893–901.
35. Jaeger M, Ketteler D, Rabenschlag F, Theodoridou A. Informal coercion in acute inpatient setting-Knowledge and attitudes held by mental health professionals. Psychiatry Res. (2014) 220:1007–11. doi: 10.1016/j.psychres.2014.08.014
36. Krieger E, Moritz S, Lincoln T, Fischer R, Nagel M. Coercion in psychiatry: a cross-sectional study on staff views and emotions. J Psychiatr Ment Health Nurs. (2020) 29:29. doi: 10.1111/jpm.12643
37. Lambert K, Chu S, Turner P. Professional boundaries of nursing staff in secure mental health services: impact of interpersonal style and attitude toward coercion. J Psychosoc Nurs Ment Health Serv. (2019) 57:16–24. doi: 10.3928/02793695-20180920-05
38. Molewijk B, Pedersen R, Kok A, Førde R, Aasland O. Two years of ethics reflection groups about the use of coercion. Changes over time in employees’ normative attitudes regarding the use of coercion, user involvement, team cooperation and the handling of disagreement. Res Sq. (2020) [Preprint]. doi: 10.21203/rs.3.rs-133457/v1
39. Motteli S, Hotzy F, Lamster F, Horisberger R, Theodoridou A, Vetter S, et al. Optimistic recovery expectations are associated with critical attitudes toward coercion among mental health professionals. Int J Mental Health. (2019) 49:157–69. doi: 10.1080/00207411.2019.1699338
40. Rabenschlag F, Konrad A, Rueegg S, Jaeger M. A recovery-oriented approach for an acute psychiatric ward: is it feasible and how does it affect staff satisfaction? Psychiatric Quar. (2014) 85:225–39. doi: 10.1007/s11126-013-9285-z
41. SINTEF Helse. Det er nå det Begynner!–Hovedrapport fra Prosjektet “Brukerorienterte Alternativer til Tvang i Sykehus” (BAT). SINTEF Rapport A. OSLO: SINTEF Helse (2008). p. 8450.
42. Bartholomew T. The Relationship of Attributions About Inpatient Violence, Attitudes About Coercive Management Strategies and Exposure to Violence. Newark, NJ: Rutgers University-School of Health Professions (2019).
43. Orlick A. Reducing the Use of Physical and Chemical Restraints Through Enhanced De-Escalation Training in Adult Inpatient Psychiatry. Wilkes-Barre, PA: Wilkes University (2020). p. 1–117.
44. Al-Maraira OA, Hayajneh FA. Correlates of psychiatric staff’s attitude toward coercion and their sociodemographic characteristics. Nurs Forum. (2020) 55:603–10. doi: 10.1111/nuf.12476
45. Al-Maraira O, Hayajneh F, Shehadeh J. Psychiatric staff attitudes toward coercive measures: an experimental design. Perspect Psychiatr Care. (2019) 55:734–42. doi: 10.1111/ppc.12422
46. Gowda G, Kumar C, Ray S, Das S, Nanjegowda R, Math S. Caregivers’ attitude and perspective on coercion and restraint practices on psychiatric inpatients from South India. J Neurosci Rural Pract. (2019) 10:261–6. doi: 10.4103/jnrp.jnrp_302_18
47. Gerace A, Muir-Cochrane E. Perceptions of nurses working with psychiatric consumers regarding the elimination of seclusion and restraint in psychiatric inpatient settings and emergency departments: an Australian survey. Int J Mental Health Nursing. (2019) 28:209–25. doi: 10.1111/inm.12522
48. Gowda G, Lepping P, Ray S, Noorthoorn E, Nanjegowda R, Kumar C, et al. Clinician attitude and perspective on the use of coercive measures in clinical practice from tertiary care mental health establishment - a cross-sectional study. Indian J Psychiatry. (2019) 61:151–5. doi: 10.4103/psychiatry.IndianJPsychiatry_336_18
49. Molewijk B, Engerdahl IS, Pedersen R. Two years of moral case deliberations on the use of coercion in mental health care: Which ethical challenges are being discussed by health care professionals? Clin Ethics. (2016) 11:87–96. doi: 10.1177/1477750915622034
50. Aasland O, Husum T, Førde R, Pedersen R. Between authoritarian and dialogical approaches: attitudes and opinions on coercion among professionals in mental health and addiction care in Norway. Int J Law Psychiatry. (2018) 57:106–12. doi: 10.1016/j.ijlp.2018.02.005
51. Gooding P. Mind the gap: researching ‘alternatives to coercion’ in mental health care. In: Sunkel C, Mahomed F, Stein M, Patel V editors. Mental Health, Legal Capacity, and Human Rights. Cambridge: Cambridge University Press (2021). doi: 10.1017/9781108979016.021
52. World Health Organization. Hospital-based Mental Health Services: Promoting Person-centred and Rights-based Approaches. Geneva: World Health Organization (2021).
53. Bowers L, Alexander J, Bilgin H, Botha M, Dack C, James K, et al. Safewards: the empirical basis of the model and a critical appraisal. J Psychiatric Mental Health Nurs. (2014) 21:354–64. doi: 10.1111/jpm.12085
54. Huckshorn K, CAPI, Director N. Six Core Strategies for Reducing Seclusion and Restraint Use. Alexandria: National Association of State Mental health Program Directors (NATC) (2005).
Keywords: mental health, staff, attitudes, assessment, coercion
Citation: Husum TL, Siqveland J, Ruud T and Lickiewicz J (2023) Systematic literature review of the use of Staff Attitudes to Coercion Scale (SACS). Front. Psychiatry 14:1063276. doi: 10.3389/fpsyt.2023.1063276
Received: 06 October 2022; Accepted: 17 January 2023;
Published: 07 February 2023.
Edited by:
Paul Hoff, University of Zurich, SwitzerlandReviewed by:
Lieselotte Mahler, Charité – Universitätsmedizin Berlin, GermanyCopyright © 2023 Husum, Siqveland, Ruud and Lickiewicz. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tonje Lossius Husum,  dG9uamVsb3NAb3Nsb21ldC5ubw==
dG9uamVsb3NAb3Nsb21ldC5ubw==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.