
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Psychiatry, 06 March 2023
Sec. Social Psychiatry and Psychiatric Rehabilitation
Volume 14 - 2023 | https://doi.org/10.3389/fpsyt.2023.1055012
Introduction: This systematic review aimed to answer whether we can predict subsequent social functioning in first episode psychosis (FEP) by means of an initial cognitive examination. In order to do this, we gathered longitudinal studies which evaluated neurocognition and/or social cognition regarding their impact on long-term social functioning of FEP patients.
Methods: The MOOSE method was employed and 28 studies covering data from a total of 2572 patients with longitudinal trajectories from 2 months to 5 years were reviewed.
Results: In general, cognitive deficits impacted on the social functioning of the FEP patients across the time. The neurocognitive domains which most closely predicted social functioning were processing speed, sustained attention and working memory. An overall cognitive dysfunction, low IQ and the academic trajectory were also found predictive. Regarding social cognition, the findings were not unanimous.
Discussion: In addition of the impact of each variable, several of the articles found a complex relationship between social cognition, neurocognition, social functioning and negative symptoms, pointing social cognition as a modulator of neurocognition but being modulated as well by negative symptoms. The principal clinical implication of this review is that the initial assessment of FEP patients and their rehabilitation must take cognition into account.
The Handbook of Social Functioning in Schizophrenia (1) defines the impairment in social functioning as the inability of individuals to meet societal defined roles such as homemaker, worker, student, spouse, family member, or friend. In addition, individual’s satisfaction with their ability to meet these roles, their ability to care for themselves and the extent of their leisure and recreational activities are often subsumed under the rubric of social functioning. It is not surprising that having problems to maintain such an active role in society can become incapacitating and undermine one’s quality of life. Despite this, social functioning in psychosis did not begin to attract the interest of researchers until the middle of the 20th century, when the psychiatry field changed its traditional paradigm of the hospitalized psychotic patient to adopted a new global approach to therapy, whose main goal was the integration of the mentally ill in the community (2). This led to broader the attention to the social impairments associated with mental disorders, and finally to the inclusion of deterioration in social and occupational functioning among the diagnostic criteria of DSM-III for schizophrenia.
Nowadays, that interest has been combined with new technological advances, resulting in the development of new antipsychotic treatments in conjunction with innovative models of community care and, more recently, new strategies for early intervention (3). These strategies have been especially useful in First Episode Psychosis (FEP), and even in individuals at Ultra High Risk of Psychosis (UHR), since intervention in the first 2 or 3 years has been shown to reduce the risk of another psychotic episode by 50%, which, in turn, reduces the possibility of making the illness worsen (4). Actually, and due to all these innovations and advances in therapeutic intervention, psychotic symptoms generally decrease in the first year after initiation of treatment in the vast majority of patients, which, hypothetically, should increase the functionality of the individual. This contrasts with the very low rates of recovery found in individuals treated for a FEP when recovery is defined not only in terms of psychotic episodes but, more generally, as social and clinical recovery lasting for at least 2 years (together with mild symptoms): the percentage of patients found to meet these criteria in a meta-analysis of outcome studies reach just to 13.5% (3, 5). Therefore, and with such a definition for recovery in mind, many researchers focused recently in the social functioning and the real-world adjustment of the patient (6) to determine the factors that can afford protection as well as those that represent an improved prognosis in the patient’s social life, with a large number of studies on both aspects (protection and prognosis) having been published since the beginning of this century (2). One of the main factors explored is cognition, since cognitive deficits represent one of schizophrenia’s core features, which affect patients’ functioning and recovery, and seems to be related to high levels of functional disability, even more so than psychopathology (7), what has led recently to a “white paper” of recommendations for good practitioners in therapy and rehabilitation for FEP patients, developed by experts in cognitive remediation (8).
The present review explores and systematizes longitudinal studies published in recent years regarding the above-mentioned relations in patients diagnosed with FEP. We will focus on such cognitive factors and its relation to social functioning by analyzing prospective data. We focus on studies of FEP patients because of their significance for early intervention, and also because of the need to distinguish its course from the one observed in the chronic illness, since both clinical and functional features have been shown to be different (9). Moreover, the advantage of studying this earlier phase of psychosis is that clinical components as long illness duration, aging, effects of long-term medications, chronic hospitalization and other factors related to long-term intervention do not stand as confounding factors. A systematic review found cognitive impairment across domains, up to severe level based on Cohen’s effect size, already in FEP studies (10). However, according this review, differences in levels of impairment are observed between studies, as well as within domains, indicating that further consolidation of cognitive impairment over the course of illness may be present. Thus, our aim is to review how cognitive deficits impact across the time on social functioning in patients diagnosed with FEP. The term cognitive is essentially broad and a complete consensus among authors categorizing cognitive domains is lacking. Therefore, given that we limited our review to FEP patients and longitudinal studies, we decided to broader the cognitive focus to include studies measuring both general aspects of cognition (like the IQ or the academical performance) as well as the domains of cognition as defined by the Neurocognitive Work Group of the DSM-5 (attention, executive function, learning and memory, language, perceptual–motor function, and the newly included social cognition domain) (11). In spite of this, and regarding the different cognitive processes, it must be noted that neurocognition has often been separated from social cognition. Neurocognition refers to the processes of linking and appraising information, and includes cognitive domains that have traditionally been referred to as “cognitive” in the literature, such as speed of processing, working memory, attention, memory, or executive functions. Social cognition refers to the mental operations underlying social interactions such as perception, interpretation, and generation of responses to the intentions, dispositions, and behaviors of others (12) and includes aspects and variables like theory of mind, social perception, social knowledge, attributional biases, and emotion processing, areas that are affected, in an heterogeneity manner, in FEP patients (13). This review will distinguish between neurocognition and social cognition as different constructs that influence each other: the exact form of their relationship is still unclear in the literature, though some studies have underlined social cognition as a mediator between neurocognition and social functioning (14), to outline their role in in FEP patients. On the other hand, only longitudinal studies have been included in the review due to their ability to outline the relation among different variables over a period of time (15). In sum, the final question this review aims to answer is whether we can predict subsequent social functioning in first episode psychosis by means of a cognitive examination. In order to do this, we have gathered information from the literature about general cognition, neurocognition, and social cognition, and we have evaluated their impact on long-term social functioning.
The MOOSE method (Meta-Analyses and Systematic Reviews of Observational Studies) was employed for this review (16). Articles of experimental studies were collected from 5 databases, all accessible within the University of Valencia: Pubmed, WoS (Web of Science), ProQuest, Dialnet and Google Scholar. The search was carried out in February 2022, and covered research carried out over an 11-years period (2010–2021). An initial search for “First Episode Psychosis” (FEP) in WoS rendered 11,465 results, which was narrowed down to 314 results when the search terms “Social Functioning” and “Cognition” were included. Eventually, having excluded reviews and older than 11-years old works, we were left with a final number of 233 articles. Our research from then on focused on title, abstract and keywords of these 233 articles in order to confirm whether or not their variables corresponded with the inclusion criteria of this review, which were the following: longitudinal studies whose variables were related to cognition and social functioning, quality of life and/or patient roles in society; which had been collected systematically and quantitatively and discussed and assessed in the conclusions of the study. The type of psychometric measures used to assess the dependent variables were social scales, such as the Social Functioning Scale (SFS), the Global Assessment of Functioning (GAF) or the Social and Occupational Functioning Assessment Scale (SOFAS), while cognition, whether social cognition or in terms of the classic domains of neurocognition, needed to have been measured using well known psychometric scales such as MATRICS, the Consensus Cognitive Battery (MCCB) or the Brief Assessment of Cognition in Schizophrenia (BACS) (17–21). The flowchart in Figure 1 reflects the decision-making process followed in the selection of the articles reviewed herein.
Eventually, 28 international experimental articles, with varied samples of adult first-episode psychotic patients of both genders were included in this review. The key information collected from these 28 articles can be consulted in Table 1, which highlights samples of participants and duration of the study, main focus, a general observation on quality of the study in statistical terms, and the results of each study regarding the social functioning of their patients. In addition, the Table 2 presents each of the clinical and cognitive scales (both for neurocognitive and social cognition variables) the reviewed studies applied in their measurements (thus, the independent variables) and also the scales they used to measure social functioning as the dependent variable. It should be noted that this table presents all the studies selected according to the aforementioned inclusion criteria, regardless of whether their results were statistically significant or not. In this way, the reader can obtain valuable information about what has been specifically studied regarding cognition and social functioning in each study.
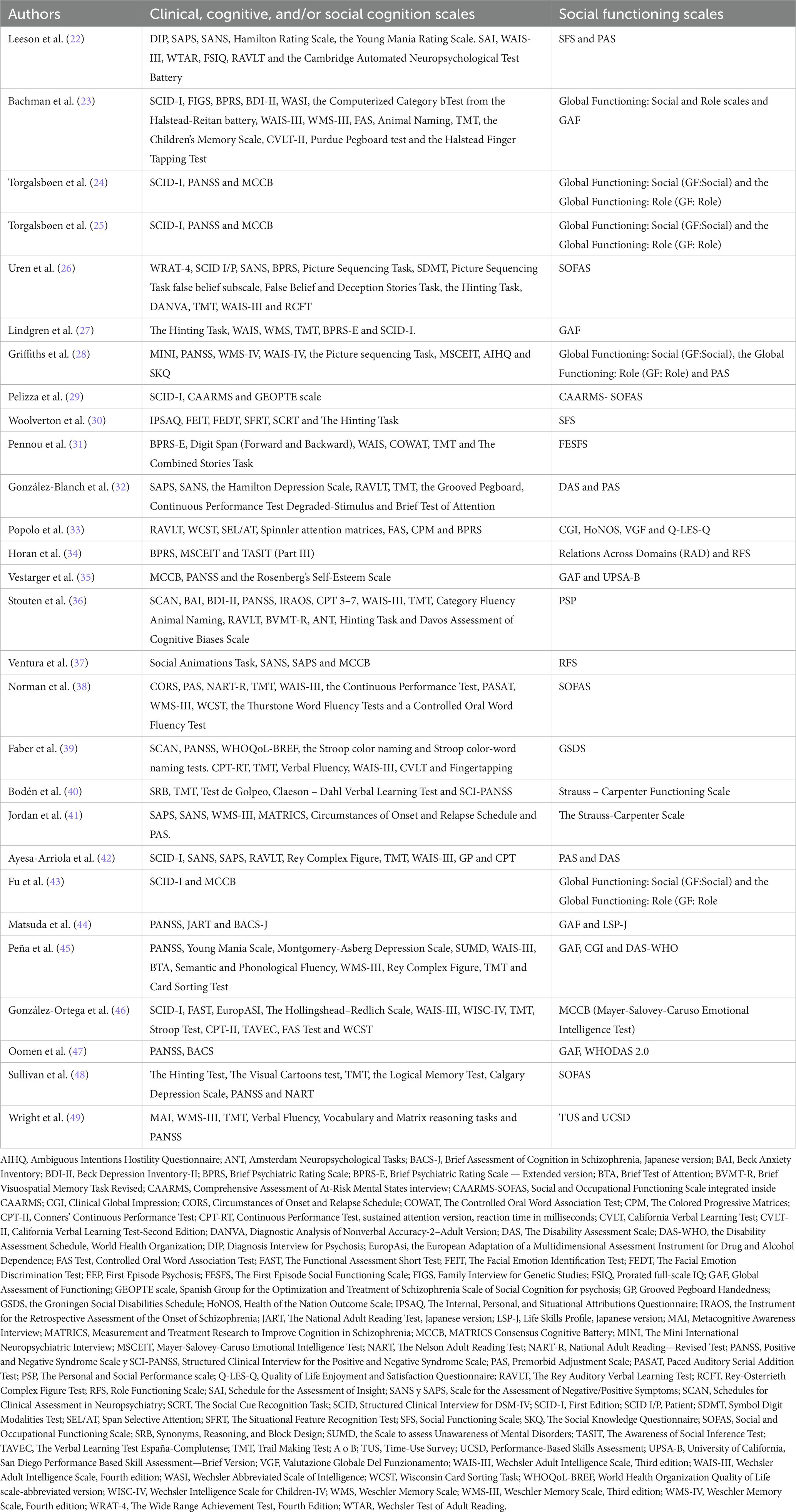
Table 2. Psychometric scales which each reviewed study applied for the measuring of the independent (clinical and cognitive) and dependent (social functioning) variables.
Longitudinal articles published between 2010 and 2021 can be found in Table 1. The number of FEP patients in a study ranged from 15 to 282 (with a total sum of 2,572 patients). Nine studies included a control group, and one study compared FEP with a non-FEP group. While all the studies were longitudinal, the time period varied from a minimum of 2 months to a maximum of 5 years after the first evaluation. Specifically, a total of 15 studies were carried out over a time period of less than or equal to 1 year, 9 of them covered a following of between 2 and 3 years, and only four were able to follow the patients for 4–5 years. In general, the studies applied scales among the usual ones well-known in neuropsychology, although not necessarily the same, with which the variability and lack of homogeneity of the measurements was observed as a difficulty when establishing general conclusions of the present review (see Table 2). Almost all the studies used correct statistical measures to assess the predictive value of their data (different regression models, hierarchical clustering, or mediation analyses) and, when a control group was used, the authors were concerned with establishing adequate comparability (using matched controls). The reader interested in the specific measures used by each study can consult it in Table 1.
The cognitive variables evaluated in the different articles have been grouped for a better global organization and understanding. These groups are, firstly, a general listing regarding overall cognitive functioning, including IQ and academic performance; secondly, a listing for specific cognitive domains such as processing speed, attention, working memory, verbal memory, visuospatial processing and reasoning/problem solving; and third and lastly, the general domain of social cognition, with a separated listing for ToM (theory of mind), and metacognition.
Some studies contemplated general cognitive failures through low IQ (mostly applying the WAIS scales) or global cognitive measures through means extracted from cognitive batteries, and their relation with social functioning and disability of FEP patients. For example, a higher IQ at the beginning of the disease was observed to be a predictor of better social functioning with regards to employment and occupation (22) Furthermore, a study identified three predictive clusters of FEP patients that were characterized by distinct cognitive performances. One cluster fell consistently below the sample mean across all cognitive measures, according to the view that there is a subgroup in FEP that has significant globalized cognitive impairments, and premorbid IQ was a significant predictor of group membership. Moreover, the two lower performing clusters both had fewer years of education and were less likely to be employed compared with the subgroup with intact cognition. Poorer general cognitive functioning was associated with poorer participation and functioning in educational, occupational, and social roles at the 6-months follow-up (26). A recent study with the same approaching of clusters observed very similar results, with a trend for significance in the association of social functioning and cognition at the follow-up (47). In addition, another recent study (46) designed cognitive reserve as the sum of IQ plus occupational attainment, and found it significantly related to functionality (though mediated by social cognition as commented further in next sections). In another study, an overall low mean in a battery of neuropsychological tests, indicating worse general cognitive function, predicted higher functional disability after 1 year (but not after 3 years of follow-up) (42). On the other hand, two studies did not find that general cognition was statistically related to social functioning in FEP. One of them (33) reported that quality of life and social functioning were mostly independent of cognitive impairments in a sample of FEP young patients, and the other found no correlation between neurocognition performance and social functioning in a sample of 26 FEP patients followed for 5 years (44).
Education, measured as years of academic achievement, has been suggested to contribute to cognitive reserve, which may act as a protective factor against the deleterious effects of psychotic illness. For instance, although no relationship was detected between cognitive function and a social functioning score (SOFAS) at 5 years in a study, robust correlations appeared between education at onset, premorbid academic adjustment, and overall IQ with full-time occupation and use of disability pension at 5 years (38). The authors suggested that a global measure of intellectual functioning may be a more consistent predictor of functional outcomes than specific indices. As well, they underlined the importance of examining past educational achievement as a possible confound of the relationship between cognitive performance and later functioning. Another study (25) expanded on this idea, directly regarding more years of education at baseline as a predictor for better social and role functioning at 2 years’ follow-up, in a model which, with addition of the attention/vigilance cognitive domain, explained nearly 48% of the variance in social functioning. Indeed, years of education were found to be significant predictors of functional disability at 3-years of disease evolution in another study (42), and were also found to be predictive of role functioning in the follow-up over 4 years in another study (43).
Secondly, all articles which highlighted any of the classic domains of neurocognition and their conclusions were grouped as follows.
Some studies covered the processing speed domain to test its effect on social function in FEP. One study demonstrated that worse processing speed performance at baseline, measured through the WAIS-III Digit Symbol-Coding test, predicted a worse social functioning 1 year later in young FEP patients with adolescent onset psychosis (23), and another study, using the same measure, found that worse processing speed was a significant predictor for real-world functional disability at one-year follow-up (but not at three) in FEP patients, with an OR of 1.57 (42). Finally, a third study, measuring worse processing speed at baseline with the same test, found it to be a significant predictor for most functional outcomes (including social functioning) at 2 years follow-up in FEP patients who developed a schizophrenia syndrome (but not for a group of non-schizophrenia FEP patients) (45). The authors concluded that the performance on processing speed seemed to be a key factor in more severe syndromes, but, however, only a small proportion of the variance was explained by the model, so there must be many other factors that have to be considered. On the other hand, in another study, psychomotor speed was evaluated through a composite score (adding finger tapping and Trail-Making Test) and it was also found highly predictive for poor social functioning (OR = 3.37) after 5 years, even adjusted for antipsychotic drug usage (40). In addition, processing speed, being measured through verbal fluency, predicted recovery (defined as the combination of both symptomatic and social functioning remission) in another study. The authors argued that verbal fluency can be considered to be part of the speed of processing domain, and they concluded that such impairment is a core cognitive deficit in schizophrenia and that from a theoretical perspective, speed of processing and its cognitive components underlie performance in other cognitive domains, being essential for learning and executive functions (39).
Some studies dealt with attentional variables and concluded that the dysfunction in a patient’s attention, especially sustained attention or vigilance, is predictive for worse social functioning (24, 25, 32, 33, 43). As commented before, the sum of the attention/vigilance domain together with more years of education at baseline formed a predictive model which explained a high proportion (48%) of the variance (25). Interestingly, one study pointed that sustained attention was a good predictor for social functioning, but the prediction was accurate (97%) mainly for the disabled FEP patients but not for the recovered group. The authors emphasized the difficulty of predicting functional recovery and the need to address the role of other factors not commonly explored, like psychosocial interventions or personality, in the functional recovery from FEP (32). Finally, a study found selective attention scores significantly correlated with some aspects of social functioning at baseline and a follow-up of 1 year in FEP patients, though this study did not perform an adequate statistical analysis to address attention as a predictive factor (33).
Working memory was addressed in various studies in relation to social function in FEP. One study found that baseline working memory significantly predicted social function at 6-months follow-up (24), however, the same cohort of FEP patients did not show such relationship when evaluated at 2-years (25). In addition, working memory also predicted recovery (defined as the combination of both symptomatic and social functioning remission) in a study (39) while another study (43) went a step further, specifying dysfunction of verbal working memory predicted social and role model dysfunction, being the gain in social functioning over time significantly lower for the low working memory group compared to the high working memory group. Finally, a study found that working memory (24%) and visual learning (6%) predicted a 30% of the variance of functional capacity (defining functional capacity as the abilities needed to perform everyday tasks that are considered necessary for independent functioning in the community) when measured at 10-months follow-up from a FEP (35).
Three studies examined verbal declarative memory and learning related to a variety of aspects of social functioning, and the relationship was proven to exist, but in general it was not much strong, or it was mediated by another factor. For instance, a recent study (28) found those with poorer verbal memory seem to struggle to maintain performance in roles such as work or education at one-year follow-up; thus, a better verbal memory was a significant predictor for less likelihood to have a poor role functioning. However, a post-hoc mediating analyses confirmed that negative symptoms significantly mediated the relationship between baseline verbal memory and role functioning at follow-up, and the study concluded that cognition may play a subordinate role in predicting functional outcome in early psychosis, compared to chronic. Another study applied a path analysis and demonstrated that verbal memory was indeed related to functioning, but social cognition acted as a mediator between verbal memory and functioning at follow-up (not at baseline), thus concluding that neurocognition is related to functioning, and that social cognition plays a mediating role (46). Another study found verbal memory was a significant predictor on functionality, but explained only 9% of the variance. Adding consecutive months in symptom remission explained 30%, so, they concluded that sustained remission of symptoms, especially of negative symptoms, made a larger contribution to functional outcome than verbal memory. Interestingly, when the analyses were repeated with global cognition replacing verbal memory, a greater effect of global cognition was not found, suggesting that verbal memory may be a stronger predictor of functioning than overall cognitive performance (41). Finally, a study found that verbal memory worsens at 5-years follow-up, but was unrelated to social functioning (44).
This domain was analyzed in three studies, which measured the ability of the individual with FEP to process visual and spatial stimuli (such as social gestures). Visuospatial processing performance at baseline was seen to be a significant predictor for poorer functional outcome after 2 years for a group of FEP patients who did not develop schizophrenia but other psychotic syndromes (bipolar disorder, delusional disorder and brief psychosis) (45). One study tested the hypothesis that baseline cognitive deficits are a stronger predictor of psychosocial functioning than psychotic symptoms. The hypothesis was partially confirmed through the relation between the areas of vocational/academic performance and social relationships, for both of which visual learning was the strongest predictor for functionality after a year (36). However, another study which tested a similar proposal found visuospatial processing not to be a significant predictor for global functioning outcome (28).
Some studies examined this cognitive domain, as it is included in the MATRICS Consensus Cognitive Battery. One study (43) observed that the style of reasoning and problem-solving seem to have a bearing on the fulfillment of roles in society, cause role functioning was significantly predicted by a combination of attention, working memory, and reasoning/problem solving.
Social Cognition was assessed in a variety of studies. A social cognition impairment sub-score (from a pooled measure which combined a sub-score of classic cognitive domains and a sub-score of social cognition) was a significant predictor of cognitive change and depression at baseline in one study (29) but unfortunately the relationship was not tested for the follow-up. The authors stated that they failed to find relevant associations between functionality (through the SOFAS) and the combined scale they used to measure social cognition, and suggested that patient judgments regarding their socio-cognitive ability have a minimal correlation to their functional outcomes as rated by mental health professionals (29). Another study, using a panel design with cross-lagged correlations, which allow predictive associations between variables over time while controlling for effects at an earlier time point, found that social cognition at baseline and follow-up assessments robustly and broadly predicted functioning at the 12 month of follow-up across the domains of work, independent living, and social networks (34). Moreover, as commented above, a recent study found that social cognition acts as a mediator between cognitive reserve and global functioning, and also between verbal memory and global functioning (46). However, in another study (30) there were no longitudinal associations between social cognition at baseline and any measure of social functioning at 6-month follow-up. These results held both with and without corrections for multiple comparisons.
Theory of mind was analyzed to test whether the inference and attribution of mental states of other individuals relates with social functioning. A study (37) observed compromised ToM abilities present even in remitted FEP patients (in a trait-like manner) and, when analyzing longitudinal data, the mediation analyses indicated that neurocognition was a significant mediator in the relationship between two ToM variables (intentionality and appropriateness) and role functioning at 6 months (interestingly, that was their alternative mediating model, being their original hypothesis that ToM would be the mediator between neurocognition and social functioning, which yielded only a trend for significance). This finding contrasts with another recent study (31), which showed that the addition of the ToM in the STEP3 of a hierarchical regression model of neurocognition on some aspects of social cognition (independent living skills and family) was associated with a significant increase in the variance explained by the model. The authors concluded that theory of mind predicts social functioning better than neurocognition in the case of certain variables. In another study (27) level of social functioning was associated with ToM when age and gender were controlled for, and this association remained significant after controlling for general cognition. This study had a very short time period of following, and they also added that ToM performance was heterogeneous in the whole FEP group, with a large portion of the FEP group showing no deficits. On the other hand, from studies commented previously in the text, one of them demonstrated at the 12-month follow-up that ToM and emotional processing were related to better real-world functioning of FEP patients in a causal manner (34), and another study showed that ToM was also a predictor for problems in social relationships at the 12-month follow-up (36). Nevertheless, we also found contrasting results among the reviewed data: A study found that deficits in ToM were stable over a year but failed to significantly predict social functioning (48), and another study (28) found that some aspects of ToM (attribution and emotion perception) neither were significant predictors for social functioning at 12-months follow-up.
One longitudinal study focused on metacognition in FEP (49), to conclude that a greater metacognitive capacity significantly predicts increased social recovery.
In our review of the recent literature, we have observed that cognition is indeed a key factor in understanding social dysfunction in a first psychotic episode, with significant results reported by 23 of the 28 studies included in our assessment. Anterior reviews, focused in cross-sectional results in patients with schizophrenia, pointed similar conclusions; that is, cognition (neurocognition and social cognition) is significantly related to social functioning in real-world in psychotic patients (50). Our results are in line with this general observation, and extend it to FEP patients who were followed for a variable amount of time and tested with adequate statistical models to find whether cognitive dysfunction at baseline could be predictive for a worse functional outcome at the follow-up. Therefore, the observed initial cognitive deterioration may be, at least in part, the cause of the social functioning deficit. In addition, the anterior reviews observed the variance explained by the statistical model tested in the studies reviewed was generally low. Our results are in line with such observation, which add to the notion of, even being important, cognition function is not enough to explain the level of social disfunction observed in this disease.
A detailed inspection of our review indicated that problems in both overall cognitive ability and IQ at baseline are related to poorer social functioning in the follow-up (22, 26, 38, 42, 43, 46, 47), as we expected based on an initial assessment of the literature. In general, these studies gave support to the notion of cognitive heterogeneity within psychosis patients and confirmed the presence of a part of individuals with psychosis and intact cognitive function, being this classification more based on degree (quantity) of cognitive impairment rather than on specific patterns (quality) of performances in cognitive domains (47). Two of the studies we reviewed did not find any differences (33, 44). In the case of (44) it was concluded that the scale employed to detect social functioning (LSP-J) may not have been sensitive enough for this purpose and their study sample was too small. The (33) study argued that, although they did not detect relationships between greater general cognitive impairment and social functioning, this could be due to the mediating role of social cognition, which was not measured in their study. Moreover, both studies did not address the predictive hypothesis through optimal statistical methodology. With respect to academic performance, all the relevant studies agreed that premorbid academic adjustment improved with a longer academic history, and highlighted a significant positive relationship between the number of years of basic study and social functioning in the longitudinal analyses (25, 38, 42, 43). This indicates that a good academic development during school years can become a protective factor, not so much against the disease itself, but against the loss of social function concomitant to the disease. These results are in line with what we expected based on our assessment of the literature.
On the other hand, when focusing on specific domains of neurocognition, processing speed was found to be a significant predictor of various aspects of social functioning in a bunch of studies (23, 39, 40, 42, 45), and it was even suggested to be essential for the recovery of the patients (39). Attention, specially sustained attention or vigilance (24, 25, 32) was seen significantly predictive of remission (24, 25, 43) and social functioning (24, 25, 32), while selective attention was related to social functioning (33). In the case of working memory, it was seen indeed to be relevant for the prediction of social function: almost all the studies that included this variable (24, 25, 35, 39, 43) agreed that a deteriorated working memory hinders good social function in the follow-up. Interestingly, one cohort of patients show such relation at the 6-moths follow-up (24), but not at the 2 years follow-up (25), thus suggesting that early interventions are useful and capable of rehabilitate both neurocognition and social functioning. Moreover, one study of the above (43) specified that the verbal type of working memory was the most statistically significant. This increased the value to the results observed for the verbal declarative memory domain: various studies (28, 41, 46) observed verbal memory as a significant predictor of poor social functioning. Despite this, one of them found the result mediated by negative symptomatology (28), another one indicated that the variance explained by verbal memory was low (41), and the last one identified social cognition as a mediator between verbal memory and functioning (46). An additional study found that verbal memory worsens at 5 years, but was unrelated to social functioning (44). In sum, it would be of relevance to further investigate this potential relationship between verbal memory failure and social function, since the impaired memory for dynamic social interactions has been suggested as a sign of disease chronification (51), but the results of the longitudinal studies are not as robust as we could expect. On the other hand, the cognitive domain of visuospatial processing did not reach significance as a predictor for social functioning in FEP patients (28) or it was seen as a predictor of functionality mainly for those FEP patients who later developed a non-schizophrenic syndrome (45). Anyway, visual learning (a dominion closer to memory than to visuospatial processing) do was a stronger predictor for functionality after a year (36). In addition to the anterior, role functioning was significantly predicted by a combination of attention, working memory, and the cognitive domain of reasoning/problem solving (43). The general conclusion which emerged from the above-reviewed data is in line with those of previous cross-sectional reviews (52, 53), which showed a significant decline in processing speed, sustained attention, working memory and reasoning/problem related to struggles in social life among individuals with FEP. The present review extends their conclusion to a longitudinal point of view, pointing such cognitive domains are the best predictors for social functioning.
Regarding the studies dealing with social cognition, being this the set of cognitive processes involved in social situations, it makes sense that, if this ability is impaired, it will be an important cause of social functioning deficit in an individual with psychosis. This point has been partially consistent with the results of our review. A study (34) applied an optimal statistical analysis for testing causality, and observed that baseline social cognition impairment led to worse real-world functioning in a 12-month follow-up; however, another two studies (29, 30) did not find such a relationship, one of them find some cross-sectional associations but it did not test for in the follow-up (29), and the other (30) did not find significance for the longitudinal associations. In addition, some authors have suggested that social cognition would play a mediating role in between neurocognition and outcomes of social functionality, which would underline its importance from a clinical point of view, especially when detecting a first episode and undertaking early intervention (50). Specifically, a study (37) identified social cognition acting as a mediator (through the Sobel test) between cognitive reserve and functioning, and between verbal memory and functioning, both of them at follow-up (not at baseline). In another study, centered only in the ToM, the authors tested the hypothesis of social cognition as a mediator between neurocognition and social functioning, yielding a trend for significance (46). Regarding the rest of articles which measured the influence of ToM (as a specific part of social cognition) in functioning, they did not unanimously point to a relationship with social functioning, which we did not expect, since inference of the mental state of the people with whom we interact should be a key factor in social functioning. In fact, while some studies observed ToM significantly predicted social functioning (27, 34, 36) some other did not find such relation (28, 48), or found a poor relation with low variance explained (31), or saw the relationship of ToM on role functioning significantly mediated by neurocognition (37). In the case of the studies with non-significant results (28, 48), both agreed that their measurement of ToM was influenced by negative symptoms. In the first, negative symptoms significantly mediated between baseline memory and role functioning at follow-up (28). Moreover, the severity in social cognition impairment (which was a predictor of cognitive change and depression) appeared to be specifically associated with negative symptoms in another study (29). Therefore, it seems to be that negative symptoms can act as a mediator between neurocognition, social cognition, and social functioning (48). These findings need further investigation since symptoms often improve, whereas social functioning does not. A study (41) proposed that cognitive abilities improve following early remission of symptoms, both positive and negative, and that this remission, in turn, correlates with an improvement in social function; thus, symptomatic remission is undoubtedly important and impacts on the social function of the individual in a parallel way to cognitive function and may even influence it. Finally, in regards to metacognition, one study showed it was a significant predictor of change in functional outcome from baseline to follow-up, with a high proportion of variance explained and independently of negative symptoms (49). Metacognitive capacity has been suggested to mediate the relationship between neurocognition and the individual’s social and occupational function in cross-sectional studies (7). This suggests that the ability to think about own’s thinking, specifically, the mental processes involved in this from a clinical point of view, could be a target for rehabilitation and early intervention in social functioning. Metacognition therapies that focus on maintaining optimal social function may be one of the most appropriate steps towards addressing social rehabilitation in FEP.
We have repeatedly observed that cognitive deficits impact on the social functioning of the FEP patient from the beginning of the disease and across the time and, therefore, the principal clinical implication of this review is that the rehabilitation interventions must take this factor into account. The neurocognitive domains most closely related to social functioning in FEP seem to be processing speed, sustained attention and working memory, but a general overall cognitive disfunction or a low IQ are also very important for an adaptative social functioning in the future. The initial assessment of the FEP patient should take these aspects into account, as well as consider the patient’s academic trajectory. Regarding social cognition and its effect on social functioning, the findings were not unanimous. A significant predictive relationship was found in some studies, but we found also quite studies with little or no relationship, both in terms of social cognition in general and specifically ToM or metacognition. It is interesting to add that several of the articles found a complex relationship between social cognition, neurocognition, social functioning and negative symptoms, pointing social cognition as a modulator of neurocognition but being modulated as well by negative symptoms. In any case, given the results of the review and in the absence of more studies that clearly establish the kind of mediation relationship which seems to exist among these variables, we conclude that an initial evaluation of social cognition in a FEP patient should be essential. Finally, the present review has a number of strengths and weaknesses. As strengths, longitudinal studies are exhaustively presented, with adequate statistical power and using samples of FEP patients. As weaknesses, we highlight the possible selection bias of the studies, both due to the inclusion criteria and to the articles that are usually reported in the literature, with a greater tendency to show significant results. In addition, the different studies were not observed to be homogeneous when choosing the scales to assess the different constructs, and furthermore, the theoretical constructs themselves are far from being unified in the literature (especially with regard to those that have to do with social cognition) which limits the general conclusions that can be drawn.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
MM-F, MG, and JS contributed to conception and design of the systematic review, and to the definite selection of the included articles. MM-F organized the database and Table 1, and wrote the first draft of the manuscript. MG and JS revised and corrected the manuscript and Tables 1, 2. All authors contributed to final revision and approved the submitted version.
This study was supported by grants from the Generalitat Valenciana (PROMETEO/2020/024; FIS PI20/00473).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1.Mueser, K, and Tarrier, N. The handbook of social functioning in schizophrenia. Boston: Allyn & Bacon (1998).
2.Barbato, A, and D’Avanzo, B. Historical and conceptual developments of psychosocial rehabilitation: beyond illness and disability in a humanistic framework. Int J Ment Health. (2016) 45:97–104. doi: 10.1080/00207411.2015.1132896
3.Zipursky, RB. Why are the outcomes in patients with schizophrenia so poor? J Clin Psychiatry. (2014) 75:20–4. doi: 10.4088/JCP.13065su1.05
4.Fowler, D, Hodgekins, J, French, P, Marshall, M, Freemantle, N, McCrone, P, et al. Social recovery therapy in combination with early intervention services for enhancement of social recovery in patients with first-episode psychosis (SUPEREDEN3): a single-blind, randomized controlled trial. Lancet Psychiatry. (2018) 5:41–50. doi: 10.1016/S2215-0366(17)30476-5
5.Jääskeläinen, E, Juola, P, Hirvonen, N, McGrath, JJ, Saha, S, Isohanni, M, et al. A systematic review and meta-analysis of recovery in schizophrenia. Schizophr Bull. (2013) 39:1296–306. doi: 10.1093/schbul/sbs130
6.Montemagni, C, Del Favero, E, Riccardi, C, Canta, L, Toye, M, Zanalda, E, et al. Effects of cognitive remediation on cognition, metacognition, and social cognition in patients with schizophrenia. Front Psych. (2021) 12:649737. doi: 10.3389/fpsyt.2021.649737
7.Davies, G, Fowler, D, and Greenwood, K. Metacognition as a mediating variable between neurocognition and functional outcome in first episode psychosis. Schizophr Bull. (2017) 43:824–32. doi: 10.1093/schbul/sbw128
8.Bowie, CR, Bell, MD, Fiszdon,, Johannesen, J, Lindenmayer, JP, McGurk, SR, et al. Cognitive remediation for schizophrenia: an expert working group white paper on core techniques. Schiz Res. (2020) 215:49–53. doi: 10.1016/j.schres.2019.10.047
9.Abdin, E, Chong, SA, Vaingankar, JA, Peh, CX, Poon, LY, Rao, S, et al. Trajectories of positive, negative and general psychopathology symptoms in first episode psychosis and their relationship with functioning over a 2-year follow-up period. PLoS One. (2017) 12:e0187141. doi: 10.1371/journal.pone.0187141
10.Aas, M, Dazzan, P, Mondelli, V, Melle, I, Murray, RM, and Pariante, CM. A systematic review of cognitive function in first-episode psychosis, including a discussion on childhood trauma, stress, and inflammation. Front Psych. (2014) 4:182. doi: 10.3389/fpsyt.2013.00182
11.Sachdev, P, Blacker, D, Blazer, D, Ganguli, M, Jeste, DV, Paulsen, JS, et al. Classifying neurocognitive disorders: the DSM-5 approach. Nat Rev Neurol. (2014) 10:634–42. doi: 10.1038/nrneurol.2014.181
12.Torio, I, Bagney, A, Dompablo, M, Campillo, MJ, García-Fernandez, L, Rodriguez-Torresano, J, et al. Neurocognition, social cognition and functional outcome in schizophrenia. Eur J Psych. (2014) 28:201–11. doi: 10.4321/S0213-61632014000400001
13.Bliksted, V, Fagerlund, B, Weed, E, Frith, C, and Videbech, P. Social cognition and neurocognitive deficits in first-episode schizophrenia. Schizophr Res. (2014) 153:9–17. doi: 10.1016/j.schres.2014.01.010
14.Schmidt, SJ, Mueller, DR, and Roder, V. Social cognition as a mediator variable between neurocognition and functional outcome in schizophrenia: empirical review and new results by structural equation modeling. Schizophr Bull. (2011) 37:S41–54. doi: 10.1093/schbul/sbr079
15.Caruana, EJ, Roman, M, Hernández-Sánchez, J, and Solli, P. Longitudinal studies. J Thorac Dis. (2015) 7:537–40. doi: 10.3978/j.issn.2072-1439.2015.10.63
16.Stroup, DF, Berlin, JA, Morton, SC, Olkin, I, Williamson, GD, Rennie, D, et al. Meta-analysis of observational studies. JAMA Psychiat. (2000) 283:2008–12. doi: 10.1001/jama.283.15.2008
17.Birchwood, MAX, Smith, JO, RAY, Cochrane, Wetton, S, and Copestake, S. The social functioning scale the development and validation of a new scale of social adjustment for use in family intervention Programmes with schizophrenic patients. Br J Psychiatry. (1990) 157:853–9. doi: 10.1192/bjp.157.6.853
18.Hall, RC. Global assessment of functioning. Psychosomatics. (1995) 36:267–75. doi: 10.1016/S0033-3182(95)71666-8
19.Nuechterlein, KH, Ph, D, Green, MF, Ph, D, Kern, RS, Ph, D, et al. The MATRICS consensus cognitive battery, part 1: test selection, reliability, and validity. Am J Psychiatry (2008) 165:203–13. doi: 10.1176/appi.ajp.2007.07010042
20.Kern, RS, Nuechterlein, KH, Green, MF, Baade, LE, Fenton, WS, Gold, JM, et al. The MATRICS consensus cognitive battery, part 2: Co-norming and standardization. (2008) 214–220.
21.Keefe, RSE, Goldberg, TE, Harvey, PD, Gold, JM, Poe, MP, and Coughenour, L. The brief assessment of cognition in schizophrenia: Reliability, sensitivity, and comparison with a standard neurocognitive battery. Schizophr Res (2004) 68:283–97. doi: 10.1016/j.schres.2003.09.011
22.Leeson, VC, Sharma, P, Harrison, M, Ron, MA, Barnes, TR, and Joyce, EM. IQ trajectory, cognitive reserve, and clinical outcome following a first episode of psychosis: a 3-year longitudinal study. Schizophr Bull. (2011) 37:768–77. doi: 10.1093/schbul/sbp143
23.Bachman, P, Niendam, TA, Jalbrzikowski, M, Park, CY, Daley, M, Cannon, TD, et al. Processing speed and neurodevelopment in adolescent-onset psychosis: cognitive slowing predicts social function. J Abnorm Child Psychol. (2012) 40:645–54. doi: 10.1007/s10802-011-9592-5
24.Torgalsbøen, AK, Mohn, C, and Rishovd, RB. Neurocognitive predictors of remission of symptoms and social and role functioning in the early course of first-episode schizophrenia. Psychiatry Res. (2014) 216:1–5. doi: 10.1016/j.psychres.2014.01.031
25.Torgalsbøen, AK, Mohn, C, Czajkowski, N, and Rund, BR. Relationship between neurocognition and functional recovery in first-episode schizophrenia: results from the second year of the Oslo multi-follow-up study. Psychiatry Res. (2015) 227:185–91. doi: 10.1016/j.psychres.2015.03.037
26.Uren, J, Cotton, SM, Killackey, E, Saling, MM, and Allott, K. Cognitive clusters in first-episode psychosis: overlap with healthy controls and relationship to concurrent and prospective symptoms and functioning. Neuropsychology. (2017) 31:787–97. doi: 10.1037/neu0000367
27.Lindgren, M, Torniainen-Holm, M, Heiskanen, I, Voutilainen, G, Pulkkinen, U, Mehtälä, T, et al. Theory of mind in a first-episode psychosis population using the hinting task. Psychiatry Res. (2018) 263:185–92. doi: 10.1016/j.psychres.2018.03.014
28.Griffiths, SL, Birchwood, M, Khan, A, and Wood, SJ. Predictors of social and role outcomes in first episode psychosis: a prospective 12-month study of social cognition, neurocognition and symptoms. Early Interv Psychiatry. (2020) 15:993–1001. doi: 10.1111/eip.13056
29.Pelizza, L, Azzali, S, Garlassi, S, Scazza, I, Paterlini, F, Rocco, LC, et al. A 2-year longitudinal study on subjective experience of social cognition in young people with first episode psychosis. Actas Esp Psiquiatr. (2020) 48:287–301.
30.Woolverton, CB, Bell, EK, Moe, AM, Harrison-Monroe, P, and Breitborde, NJK. Social cognition and the course of social functioning in first-episode psychosis. Early Interv Psychiatry. (2018) 12:1151–6. doi: 10.1111/eip.12432
31.Pennou, A, Lecomte, T, Khazaal, Y, Potvin, S, Vézina, C, and Bouchard, M. Does theory of mind predict specific domains of social functioning in individuals following a first episode psychosis? Psychiatry Res. (2021) 301:113933. doi: 10.1016/j.psychres.2021.113933
32.González-Blanch, C, Perez-Iglesias, R, Pardo-García, G, Rodríguez-Sánchez, JM, Martínez-García, O, Vázquez-Barquero, JL, et al. Prognostic value of cognitive functioning for global functional recovery in first-episode schizophrenia. Psychol Med. (2010) 40:935–44. doi: 10.1017/S0033291709991267
33.Popolo, R, Vinci, G, and Balbi, A. Cognitive function, social functioning and quality of life in first-episode psychosis: a 1-year longitudinal study. Int J Psychiatry Clin Pract. (2010) 14:33–40. doi: 10.3109/13651500903282881
34.Horan, WP, Green, MF, DeGroot, M, Fiske, A, Hellemann, G, Kee, K, et al. Social cognition in schizophrenia, part 2: 12-month stability and prediction of functional outcome in first-episode patients. Schizophr Bull. (2012) 38:865–72. doi: 10.1093/schbul/sbr001
35.Vesterager, L, Christensen, TØ, Olsen, BB, Krarup, G, Melau, M, Forchhammer, HB, et al. Cognitive and clinical predictors of functional capacity in patients with first episode schizophrenia. Schizophr Res. (2012) 141:251–6. doi: 10.1016/j.schres.2012.08.023
36.Stouten, LH, Veling, W, Laan, W, Van Der, HM, and Van Der, GM. Psychotic symptoms, cognition and affect as predictors of psychosocial problems and functional change in first-episode psychosis. Schizophr Res. (2014) 158:113–9. doi: 10.1016/j.schres.2014.06.023
37.Ventura, J, Ered, A, Gretchen-Doorly, D, Subotnik, KL, Horan, WP, Hellemann, GS, et al. Theory of mind in the early course of schizophrenia: stability, symptom and neurocognitive correlates, and relationship with functioning. Psychol Med. (2015) 45:2031–43. doi: 10.1017/S0033291714003171
38.Norman, RMG, Carr, J, and Manchanda, R. Cognition and the prediction of functioning in patients with a first treated episode of psychosis: a prospective study. Schizophr Res. (2015) 162:138–42. doi: 10.1016/j.schres.2014.12.025
39.Faber, G, Smid, HGOM, Van, GAR, Wunderink, L, Wiersma, D, and Van Den, BRJ. Neurocognition and recovery in first episode psychosis. Psychiatry Res. (2011) 188:1–6. doi: 10.1016/j.psychres.2010.11.010
40.Bodén, R, Abrahamsson, T, Holm, G, and Borg, J. Psychomotor and cognitive deficits as predictors of 5-year outcome in first-episode schizophrenia. Nord J Psychiatry. (2014) 68:282–8. doi: 10.3109/08039488.2013.830771
41.Jordan, G, Lutgens, D, Joober, R, Lepage, M, Iyer, SN, and Malla, A. The relative contribution of cognition and symptomatic remission to functional outcome following treatment of a first episode of psychosis. J Clin Psychiatry. (2014) 75:e566–72. doi: 10.4088/JCP.13m08606
42.Ayesa-Arriola, R, Rodríguez-Sánchez, JM, Pérez-Iglesias, R, González-Blanch, C, Pardo-García, G, Tabares-Seisdedos, R, et al. The relevance of cognitive, clinical and premorbid variables in predicting functional outcome for individuals with first-episode psychosis: a 3 year longitudinal study. Psychiatry Res. (2013) 209:302–8. doi: 10.1016/j.psychres.2013.01.024
43.Fu, S, Czajkowski, N, Rund, BR, and Torgalsbøen, AK. The relationship between level of cognitive impairments and functional outcome trajectories in first-episode schizophrenia. Schizophr Res. (2017) 190:144–9. doi: 10.1016/j.schres.2017.03.002
44.Matsuda, Y, Sato, S, Hatsuse, N, Watanabe, Y, Kishimoto, T, and Ikebuchi, E. Neurocognitive functioning in patients with first-episode schizophrenia 1 year from onset in comparison with patients 5 years from onset. Int J Psychiatry Clin Pract. (2014) 18:63–9. doi: 10.3109/13651501.2013.845220
45.Peña, J, Segarra, R, Ojeda, N, García, J, Eguiluz, JI, and Gutiérrez, M. Do the same factors predict outcome in schizophrenia and non-schizophrenia syndromes after first-episode psychosis? A two-year follow-up study. J Psychiatry Res. (2012) 46:774–81. doi: 10.1016/j.jpsychires.2012.03.014
46.González-Ortega, I, González-Pinto, A, Alberich, S, Echeburúa, E, Bernardo, M, Cabrera, B, et al. Influence of social cognition as a mediator between cognitive reserve and psychosocial functioning in patients with first episode psychosis. Psychol Med. (2020) 50:2702–10. doi: 10.1017/S0033291719002794
47.Oomen, PP, Begemann, MJH, Brand, BA, de Haan, L, Veling, W, Koops, S, et al. Longitudinal clinical and functional outcome in distinct cognitive subgroups of first-episode psychosis: a cluster analysis. Psychol Med. (2021) 19:1–11. doi: 10.1017/S0033291721004153
48.Sullivan, S, Lewis, G, Mohr, C, Herzig, D, Drake, R, Evans, J, et al. The longitudinal association between social functioning and theory of mind in first-episode psychosis. Cogn Neuropsychiatry. (2014) 19:58–80. doi: 10.1080/13546805.2013.799463
49.Wright, AC, Davies, G, Fowler, D, and Greenwood, K. Three-year follow-up study exploring metacognition and function in individuals with first episode psychosis. Front Psych. (2019) 10:182. doi: 10.3389/fpsyt.2019.00182
50.Halverson, TF, Orleans-Pobee, M, Merritt, C, Sheeran, P, Fett, AK, and Penn, DL. Pathways to functional outcomes in schizophrenia spectrum disorders: meta-analysis of social cognitive and neurocognitive predictors. Neurosci Biobehav Rev. (2019) 105:212–9. doi: 10.1016/j.neubiorev.2019.07.020
51.Lee, J, Nuechterlein, KH, Knowlton, BJ, Bearden, CE, Cannon, TD, Fiske, AP, et al. Episodic memory for dynamic social interaction across phase of illness in schizophrenia. Schizophr Bull. (2018) 44:620–30. doi: 10.1093/schbul/sbx081
52.Mesholam-Gately, RI, Giuliano, AJ, Goff, KP, Faraone, SV, and Seidman, LJ. Neurocognition in first-episode schizophrenia: a meta-analytic review. Neuropsychology. (2009) 23:315–36. doi: 10.1037/a0014708
Keywords: first episode psychosis, social functioning, cognition, social cognition, neurocognition, longitudinal studies and systematic review
Citation: Montaner-Ferrer MJ, Gadea M and Sanjuán J (2023) Cognition and social functioning in first episode psychosis: A systematic review of longitudinal studies. Front. Psychiatry. 14:1055012. doi: 10.3389/fpsyt.2023.1055012
Received: 27 September 2022; Accepted: 03 February 2023;
Published: 06 March 2023.
Edited by:
Armida Mucci, University of Campania Luigi Vanvitelli, ItalyReviewed by:
Giulia Agostoni, Vita-Salute San Raffaele University, ItalyCopyright © 2023 Montaner-Ferrer, Gadea and Sanjuán. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marien Gadea, bWFyaWVuLmdhZGVhQHV2LmVz
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.