
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 24 July 2023
Sec. Public Mental Health
Volume 14 - 2023 | https://doi.org/10.3389/fpsyt.2023.1049008
 Sajid Hassan1
Sajid Hassan1 Mazhar Iqbal Bhatti2
Mazhar Iqbal Bhatti2 Shazia Habib3
Shazia Habib3 Sidra Fatima4
Sidra Fatima4 Sher Bhader2
Sher Bhader2 Nazeer Hussain Khan1,5*
Nazeer Hussain Khan1,5* Enshe Jiang1*
Enshe Jiang1*Objective: There is a significant need in Pakistan to investigate the psychological effects of infertility on the mental health of infertile men. The current study examined how fear of intimacy affects neuropsychological impairment and evaluated its relationship to other variables including quality of life and mental toughness.
Method: An analytical cross-sectional study was carried out on infertile male patients in various healthcare settings in Punjab, Pakistan. The participants were recruited using a non-probability (purposive) sampling strategy. The sample size was 120 infertile. SPSS 26 was used to analyze the data.
Results: Fear of intimacy was found significant impact on neuropsychological impairment (r = 0.40; ***p < 0.001), as well as fear of intimacy, significantly associated with emotional problems (r = 0.48; **p < 0.01), learning problems (r = 0.33; **p < 0.01), sensory and motor problem (r = 0.55; **p < 0.01), concentration problem (r = 0.21; **p < 0.01), mental & physical in coordination (r = 0.37; **p < 0.01) and depression (r = 0.22; **p < 0.01). Fear of intimacy has negative impact on QoL (r = −0.25; *p > 0.05). Similarly, neuropsychological impairment was found to be negatively associated with QoL (r = −0.52; **p > 0.01). The relationship between fear of intimacy and neuropsychological impairment was found to be significantly mediated by QoL. Furthermore, the findings revealed that mental toughness significantly moderated the relationship between fear of intimacy and neuropsychological impairment.
Conclusion: Overall, infertile men in Pakistan had relatively high levels of fear of intimacy, which largely caused neuropsychological impairment. This study can help neuropsychological researchers, mental health professionals, as well as policymakers in improving clinical mental health practices for infertile patients.
Infertility is defined as the inability to conceive after 1 year of continuous, unprotected sexual activity and affects approximately one out of every five couples globally (1, 2). Around the world, many people between the ages of 15 and 49 are affected by infertility (3). According to a prior study, 15.5% of reproductive-age women in the USA experience infertility (4), 24.5% of women in France (5), and 25.5% of women in China (6). It is recognized that infertility is a global public health issue that affects both genders’ reproductive health (7). There may be between 60 and 80 million infertile couples (8, 9). Infertility is a sad journey for both genders (10, 11).
Male attributes constitute almost 50% of all cases, and nearly 7% of men worldwide are affected by this status (12). Moreover, it has been extensively established that infertility has a substantial influence on both spouses’ mental well-being, with difficulties such as poor self-esteem, sexual misery, miserable, guilt, panic, frustration, and interpersonal troubles between them. Moreover, some studies have found that these negative feelings can be harmful to personal health, marital satisfaction, relationship quality, and even pregnancy, leading to a vicious cycle (13). Potentially negative dose–response associations between stress (14) and unhappiness (15) and sperm quality have been discovered in males (concentration, motility, and total sperm count). Man’s reproductive dysfunction, a significant leading contributor to male infertility, is intimately linked to mental illness (16, 17). Management of infertility is intimately tied to a patient’s mental condition, and coping with infertility has a considerable negative influence on their psychological well-being and general happiness. These might result from two underlying factors: the significance of motherhood in a couple’s lives and the connection between fertility and patients’ cognitive dysfunction as psychological (social, relational, and marital) experiences.
Coping theory was used in this investigation to assess the hypothesized effects. Coping is described as “the neurocognitive and behavioral efforts expended to handle certain external and/or internal pressures which are evaluated as surpassing the human’s capabilities (18).” Coping refers to the adaptive activities taken by an individual in reaction to a damaging illness that impacts his or her lifestyle (19). Inside this contextual model, the adapting hypothesis is the most extensively utilized and accepted in neuropsychology.
Ultimately, how patients cope is determined by the resources accessible to people (quality of life, neurocognitive, psychological, and behavioral) (20). Similarly, in the present study, during infertility illness, infertile patients would question themselves, “What is at risk for me in this scenario?” The main problem is determining the probable consequences of this occurrence (particular internal/external demands) and the personal awareness of the infertility disorder (18). There are two main categories of obstructive illnesses in monitoring: challenges, which are reported cases that are perceived to have positive outcomes (infertile patients will experience low fear of intimacy levels in this study due to infertility), and affects, which are incidents that are interpreted to have negative adverse consequences) (due to high fear of intimacy patient will face the problems of neuropsychological impairment such as). People frequently evaluate their coping choices (mental toughness as an internal resource) in addition to judging the seriousness of disease. Infertile patients make decisions on their amount of control over the circumstance and what they feel should be done about it based on the coping strategies that are accessible to them. As previously stated, coping theory is suited for analyzing the predicted model since it tackles the complete process of how these infertile individuals would adapt to an illness associated with infertility.
In addition to anxiety, sadness, social isolation, and diminished libido, it can cause marital conflict, a sense of helplessness, guilt, humiliation, and worthlessness (21, 22). Studies by Onofre et al. (23) and Bhamani et al. (22) claim that “male factor” infertility accounts for 35% to 50% of cases of infertility in South Asian low and middle-income nations (LMIN). Tragically, societal and cultural factors affect how society views infertile patients. In our patriarchal society, infertile partners who are unable to conceive a child are frequently the target of discrimination and shame (24). As a result, infertile women are left out of social and traditional rituals (25), are physically, emotionally, and verbally mistreated, and frequently get divorced even if the primary problem is with men (25, 26). Thus, infertile individuals who are accused of being childless experience emotional sadness, frustration, poor mental health, and social dysfunction, which may harm their marital relationship (fear of intimacy), as well as their quality of life (27, 28). The phrase “fear of intimacy,” sometimes known as “intimacy avoidance,” refers to a fear of having intimate emotional or physical contact with another person (29). According to some scholars, both intimacy avoidance and marital issues are associated with psychological illnesses (30).
Infertility can have an impact on an individual’s neuropsychological functioning (31), which may lead to neuropsychological impairment. According to the Diagnostic and Statistical Manual of Mental Illnesses, Fifth Edition (DSM-5 American Mental Association 2013), neuropsychological impairment symptoms in psychiatric disorders are characterized by impaired decision-making, attention, memory, and executive function. One of the most prevalent and enduring signs of depressive disorders is neuropsychological impairment. According to Cha et al. (32), neuropsychological impairment is found in more than 90% of patients with mental disorders (MDD). Based on the foregoing data, we can assume that male infertiles’ fear of intimacy (losing marital relationships) may cause their neuropsychological impairment symptoms to worsen over time.
Numerous physiological, psychological, and social effects, such as grief, anxiety, stigma, and social isolation, can have a detrimental influence on the QoL of those who are suffering from infertility (33, 34). QoL is defined similarly by the WHO as “individuals’ judgments of their place in life in respect to their aims, aspirations, standards, and worries, as well as in the context of the culture and value systems in which they live” (35). Fertility QoL thus provides a comprehensive picture of the life circumstances of infertile patients during their infertility period (36, 37). Numerous studies have revealed that the quality of life (QoL) of infertile women was lower than that of their fertile counterparts. Furthermore, it has been shown that low reproductive QoL in infertile women is negatively correlated with medication compliance (38) and may lead to mental dysfunction (39). Various researchers claimed women’s infertility has been connected to a lower quality of life (35, 40). Furthermore, based on Zurlo et al.’s (41) research, we can assume that QoL is an important factor that influences infertile men’s intimacy-related fear as well as their neuropsychological impairment.
In the same way, infernality may affect our cognitive abilities such as control and confidence (42). Similarly, these cognitive abilities close link with mental toughness. Furthermore, mental toughness is a psychological trait that governs how people react to pressure, difficulty, and discomfort independent of their environment (43). The development of psychological resilience can be aided by mental toughness, which can shield against the detrimental psychological impacts of infertility (31). Strong self-esteem, optimism, self-confidence, problem-solving skills, and a happy existence are all traits that are correlated with mental toughness. Thus, it appears that mental toughness is the key to enhancing patients’ quality of life during stressful situations (44, 45). Mentally tough people are more likely to perceive their environment as within their control, to believe they are capable and influential, to stick with their goals even when things go challenging and to see problems as opportunities for growth (46). In line with all of the preceding points, we propose our research model reveals how fear of intimacy effect infertile men’s neuropsychological impairment through mediating influence of QoL as well as how mental tough buffers the effect of fear of intimacy on neuropsychological impairment. In light of the preceding literature, the hypotheses of this investigation were as follows:
H1. Fear of intimacy is positively related to neuropsychological impairment.
H2. Fear of intimacy is negatively related to quality of life.
H3. Neuropsychological impairment is negatively related to Quality of life.
H4. The indirect association between fear of intimacy and neuropsychological impairment is mediated by quality of life.
Mental toughness reduces the negative psychological effects of disease (47). Mental toughness and mental health are positively associated (48). According to current studies, establishing mental toughness is one approach to cope with the psychological health challenges brought on by infertility disease (47). For example, Jones and Parker (49) discovered that higher levels of mental toughness were connected with lower risk factors in terms of the repercussions of the illness that causes infertility. A different study found that persons with higher mental toughness are less likely to become ill (50). Similarly, individuals with poorer mental toughness had more difficulty dealing with the situation’s emotional obstacles. According to the primary component of the coping theory, this study interprets mental toughness, which is a psychological resource for infertile patients that helps them cope with cognitive impairment. According to this study, persons with low mental toughness are more vulnerable to stresses associated with their disease that risk their mental health. These people, who think they lack the ability to satisfy their cognitive demands, are likely to be the most alarmed by the possibility of neuropsychological impairment and QoL. Those with high levels of mental toughness, on the other hand, would suffer less overall neuropsychological impairment and would be less affected by new pressures. This demonstrates that mental fortitude can mitigate the particular relationship between fear of intimacy and neurocognitive impairment. As a result, we proposed the following hypotheses:
H5. The indirect association between fear of intimacy and neuropsychological impairment is moderated by mental toughness.
From December 2021 to May 2022, we conducted a cross-sectional study in Punjab Province, Pakistan. To test hypotheses, the participants were recruited from various healthcare departments. Infertile patients over the age of 18 who had been diagnosed with infertility and could communicate fluently in Urdu were eligible to participate. Infertile patients who were currently infertile with a history of other psychiatric illnesses and cognitive impairments, as well as infertile women, were excluded from the current study. The study encouraged all eligible participants to take part. The researchers confirmed that the participants were well-informed about the study’s goal and procedures. After receiving written informed permission, individuals were asked to complete a structured questionnaire. A closed-ended structured questionnaire with a maximum Likert scale of 1 to 5 (where 1 = strongly disagreed and 5 = strongly agreed) was utilized in the current study, which was first created in English. Respondents were informed that participation was completely voluntary and that they could withdraw from the study at any point during the data collection process. Ethical approval was obtained from the relevant departments, and the responses of the participants were kept secret from any participating firm executive. The survey had 174 participants in total, but the authors only received 133 sets of completed questionnaires, 13 questionnaire sets were eliminated from this study because they were insufficient, leaving 120 questionnaire sets that could be used and had a response rate of 68.96%.
The FIS-HP scale has 18 items. The FIS-HP is being developed to measure an individual’s level of comfort in discussing personal feelings with a professional partner. The items are evaluated on a 5-point scale ranging from 1 (not at all indicative of me) to 5 (extremely characteristic of me), with a total score ranging from 18 to 90. Individuals with high FIS–HP scores indicate fear of sharing, anxiety over close sharing, and fear regarding intimacy. It has a high level of convergent validity. Cronbach’s alpha is 0.88, showing sufficient internal consistency (51).
The MTQ-10 is a short summary of the MTQ-18 that includes the most valuable items in each of the four 4Cs dimensions (i.e., challenge, commitment, control, and confidence). “I generally handle any problems that arise well,” for example. The MTQ-10, like the previous MTQ, assesses a five-point Likert scale, with 1 representing “disagree” and 5 representing “agree.” It assesses the 4Cs as well as provides an overall score of mental toughness (control, commitment, challenge, and confidence). Even though the MTQ-10 has shown promising predictive validity. Cronbach’s alpha is 0.76, and the MTQ-10 has a satisfactory reliability score of 0.77 (52).
The 26-item WHOQOl-BREF self-assessment questionnaire addresses four aspects of QOL (psychological, physical, social, and environmental domains). A high Likert scale score on the WHOQOL five-point BREF indicates a high quality of life while a low score on this scale reveals low QoL. WHOQOL-BREF has a Cronbach value of 0.78, with higher scores indicating better quality of life (53, 54).
The Neuropsychological Impairment Scale (NIS), which has 46 items, will be used in this study. The NIS is a four-point Likert Type Scale that ranges from 1 to 4 such as 1 = “never,” 2 = “sometimes,” 3 = “most of the time” and 4 = “all of the time.” The sum of the scores represents the infertile patient’s overall neuropsychological impairment. The potential range of NIS scores is 46–184. The Neuropsychological Impairment Scale (NIS) assesses emotional, learning, concentration, mental, and physical coordination issues (55). It has satisfactory validity and a 0.83 Cronbach value. NIS has six such subscales as Emotional problems, learning problems, sensory and motor problem, concentration problem, mental & physical in coordination and depression. These all subscales measure an individual’s Neuropsychological Impairment.
A structured survey form was designed to collect initial information from applicants about their demographic variables such as age range, education level, socioeconomic status, family life, mode of treatment, treatment duration, and living style (see Table 1).
The Institutional Ethical Review Committee of the International Islamic University approved the ethical permission (ERC No. IIUI /PSY MSCP 397-21) for conducting research and consent for data collection. Before the start of this study, the study participants signed a written informed consent form. We provided the study participants with complete confidentiality. Only the researchers had access to the data.
In this study, a two-step approach (56) was utilized to test the hypothesized model, as well as SPSS-26 and AMOS-24 were applied for data analysis. The descriptive statistical analysis for the constructs is shown in Table 1. The common method bias (CMB) was also explored. This was done since obtaining data from a single source at the same time might produce problems for CMB in the research (57). To prevent CMB, this study used the Harman single factor assessment technique. If the first element accounted for more than half of the variance in the CMB, the study would have a serious problem. The unrotated analysis found that the first component explained 26.38% of the variance, showing that the CMB was not a significant concern in this research.
The data was analyzed using SPSS 26 and AMOS-24 versions, as well as a structural modeling approach. In the behavioral sciences, structural modeling, a highly general statistical modeling tool, is frequently used (58, 59). The model’s fit was analyzed, and the categories of goodness-of-fit measurements, incremental fit measures, absolute fit measures, and parsimonious fit measures suggested by Khan et al. (60) were measured. x2 = 187.34, df = 141, RMSEA = 0.032, CFI = 0.968, SRMR = 0.039, NFI = 0.926, IFI = 0.943, and GFI = 0.919; all values were within the specified range; the findings indicate that the fit between the measurement model and the data set are satisfactory. To validate the survey questionnaire’s objective and scope, a series of tests, including maximum shared variance (MSV) and average shared variance (ASV), were used. Every loaded item exceeded the acceptable standard value of 0.60 (61). Cronbach’s alpha values range from 0.700 to 0.900 in Table 2, which is higher than the previous researchers’ suggested threshold value of 0.70 (61–63). Additionally, the composite reliability values, which ranged between 0.731 and 0.917, exceeded the predicted threshold of 0.70 established by Nunnally (63). The extracted average variance (AVE) ranged from 0.518 to 0.816, which was somewhat higher than the actual MSV (64, 65) and may be higher than the benchmark value of 0.50 recommended by Bagozzi (64). Furthermore, all ASV values appeared to be lower than MSV. By adding up the results, the convergent validity of the measurement model as an accuracy measuring technique was confirmed. Table 2 provided additional evidence of discriminant validity. As long as all of the AVE square roots were greater than their correlation, the model’s discriminant validity could be said to have been established.
Results from the structural model clearly show that the entire model is technically accurate because the values of x2/df = 1.95, RMSEA = 0.06, CFI = 0.96, GFI = 0.91, IFI = 0.95, and NFI = 0.92 are over the threshold value suggested by Tripp and Hair (66). Results reveal that, as depicted according to Figure 1, the majority of the hypotheses are supported. The results display that fear of intimacy has significant association with neuropsychological impairment (r = 0.40; **p < 0.01). H2: here fear of intimacy is significantly negative associated to QoL (r = − 0.18; *p > 0.05) and H3: that neuropsychological impairment has significant negative effect on the QoL (r = − 0.52; **p < 0.01) (Table 3).
To examine how QoL mediated the relationship between fear of intimacy and neuropsychological impairment, we used the bootstrap approach. We used Milman’s et al. (67) bootstrap approach (bootstrap sample size = 5,000) to generate asymmetric confidence intervals (CIs) for the indirect association because the bootstrapped CIs approach generates asymmetric CIs for the indirect relationship using the respective distributions of the two regression coefficients that comprise the product term, it produces a more accurate estimate of the indirect relationship than conventional methods such as the Sobel test (67). Table 4 displays the findings of the mediating effects that QoL significantly mediated the relationship between fear of intimacy and neuropsychological impairment because CL (−1.31, −0.65) did not contain zero, continuing to support H4.

Table 4. Bootstrap results of the direct effects of fear of intimacy on outcome variables and moderating role of mental toughness.
To examine of the moderating role of mental toughness on the association between fear of intimacy and neuropsychological impairment was presented in Table 4. We used sequentially test four models. Three control variables were entered into model 1; the findings indicated that the control variables are non-significant. The outcomes of model 2, took control variables and intimacy fear into account. With an R2 of 0.18 (F = 26.73, p < 0.01), the outcomes demonstrated that the explained variation was significant. Model 3 has mental toughness as a moderator. The outcomes demonstrated that the explained variance was significant with an R2 of 0.23 (F = 15.98, p < 0.01). Model 4 has an interaction term. With an R2 of 0.26* (F = 12.42, p < 0.05), the results indicated that explained variance is also statistically significant. Overall, the association between fear of intimacy and neuropsychological impairment is significantly moderated by mental toughness. Similar to this, the interaction plot (see Figure 2) using mean centering demonstrated that this association was weaker at the greater level of mental toughness (β = −0.04, p = ns) nonsignificant as opposed to the lower level (β = 0.43, p < 0.001). According to this, patients with a high level of mental toughness experience less intimacy-related fear and sense less neuropsychological impairment. The interaction’s pattern is consistent with H5.
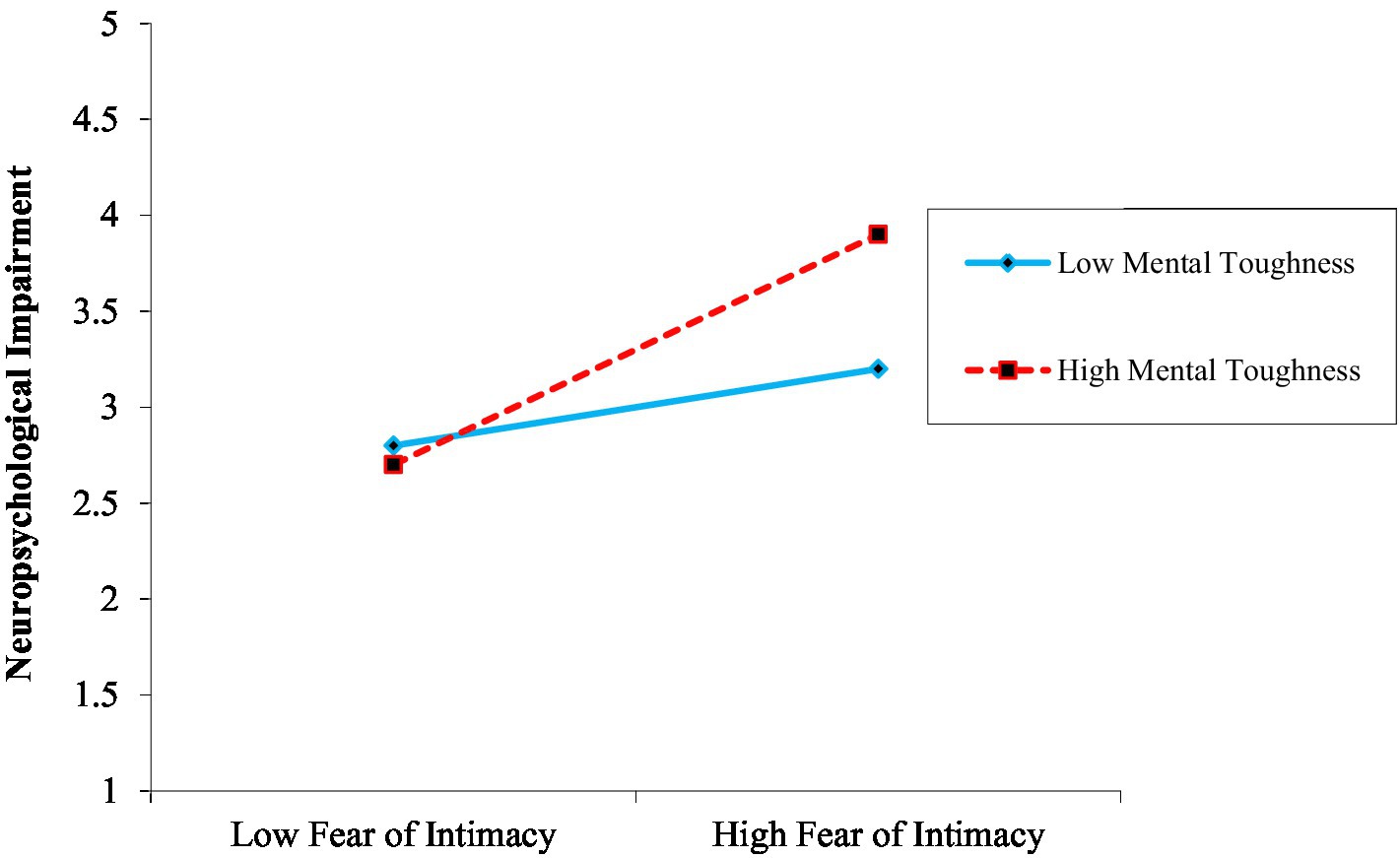
Figure 2. Moderating role of mental toughness on the link between fear of intimacy and neuropsychology impairment.
Unwanted childlessness may have detrimental effects on the psychological health of infertile people. Infertile patients’ high anxiety, low self-esteem, mood swings, or sadness have all been linked to unfulfilled child wishes (68–73). Even though other scholars have looked into the influence of infertility on individuals’ psychological wellbeing, resilience, family or social support, and mental problem such as depression, anxiety, stress, etc. in the context of gender difference (74–76), whereas this study differed in that it studied the influence of fertility on neuropsychological prospects as well as intimacy-related problem in the context of male infertile patients in a developing country (i.e., Pakistan) by looking at unmentioned variables such as age, education, family structure, mode of treatment, duration of infertility and professional perspectives of just male patients because male infertility has gone almost ignored and unmentioned in the psychoanalytic literature (77).
Past studies were struck by the disparity between the extensive psychological research on infertility in women and the remarkable lack of material on men’s emotional and neuropsychological experiences with infertility (78). Even though reproductive endocrinologists agree that male factor infertility accounts for around 45% of all cases of infertility, this disparity persists (79). Similarly, after looking into the research history, no research work on male infertility has been done in Pakistan while in our patriarchic society male plays a significant role in society and male infertility is a large portion of our population. Similarly, unfortunately in our society women are blamed and the illusion that women are the root cause of infertility without any scientific evidence. The outcomes of this study are largely determined by two aspects one is the cognitive aspect of infertility (neuropsychological and mental toughness) and the second one that women are not only a root cause of infertility.
This article investigated the direct and indirect linkages between fear of intimacy and neuropsychological impairment of infertile patients by interacting and mediating the effect of QoL as well as moderating the effect of mental toughness. The majority of hypotheses were found to be supported in this study’s findings. The finding revealed a significant relationship of fear of intimacy with neuropsychological impairment and a significantly negative relationship with QoL. Furthermore, neuropsychological impairment has a negative relationship with QoL. The overall result of H1 was unique from previous studies (80–82) in the related field. Furthermore, the result showed that QoL significantly mediates the relationship between fear of intimacy and neuropsychological impairment. This finding was challenged by the view of Vo et al. (83) who argued that QoL significantly depends on the cognitive illness. Furthermore, the current research found that mental toughness buffered the influence of fear of intimacy on neuropsychological impairment. This means that fear of intimacy can be reduced by increasing mental toughness, thereby reducing neuropsychological impairment. Results revealed that infertile patients with mental toughness level are likely to neuropsychological impairment because they try to meet cognitive stress higher than optimal level. It is believed that that infertility status reveals a loss of mental toughness (mental control, commitment, and confidences).
Furthermore, in keeping with previous research, infertile men who have nuclear family structure scored significantly higher than infertile patients who have jointed family structure on fear of intimacy, poof QoL and neuropsychological impairment scores as seen in Table 5 which were indirectly associated with Aasen Nilsen et al. (84). Furthermore, results revealed that the infertile patients who were getting treatment from government hospitals had significantly high levels of fear of intimacy, poor mental tough, neuropsychological impairment, and poor QoL in comparison to those who were getting private treatment method (see Table 5) which is also linked with previous researches (85, 86).
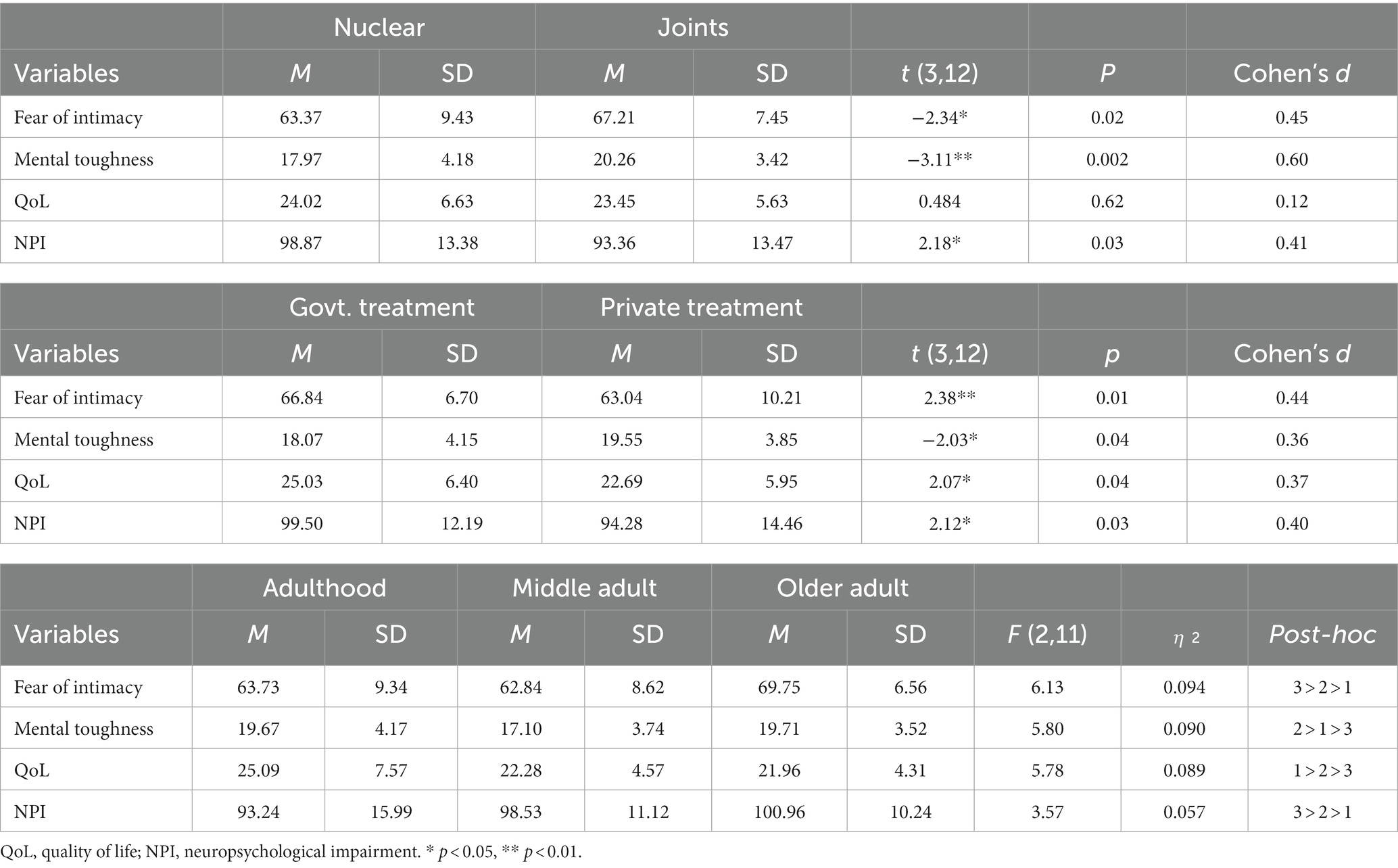
Table 5. Mean, standard deviation, t-test and one-way ANOVA of variance in fear of intimacy, mental toughness, QoL and NPI in the term of across the demographic variables.
Similarly, other scholars had also verified that older adult patients had a higher mental illness (87–89). Similarly, the researcher investigated older adults who have impoverished QoL because they suffer from fear of loneliness and hopelessness as well as cognitive problems (90). This finding is consistent with other studies that were carried out in Ghana, Iraq, and Germany, which also indicated that older adults scored high in intimacy-related problems (91, 92) and cognitive illness (93, 94) as well as poor QoL (95).
However, there are significant gaps in our knowledge of the impact of fear of intimacy on neuropsychological impairment in infertile patients, as well as the consequences of its negative effects on mental toughness and quality of life. In this context, the current study produced novel findings that investigate the impact of infertility patients’ fear of intimacy on neuropsychological impairment as well as QoL. The findings of this study also add to our understanding of the negative link between neuropsychological impairment and QoL. Furthermore, this study has observed sensitive details about how to reduce the negative effects of infernality on patients. Furthermore, the introduction of a moderator and mediator, as well as the use of a time lag approach (96, 97), allowed for a more comprehensive understanding of the impact of fear of intimacy on patient neuropsychological impairment, especially in the infertility dolman.
This study continues the tradition of infertility health behavior and clinical research into mental illness, fear of intimacy, poor mental toughness and QoL, and neuropsychological impairment. It investigates these notions in an understudied environment, namely, how fear of intimacy during infertile working hours might have negative consequences and influence neuropsychological functioning.
This publication, on the other hand, disseminates research by delving deeper into how fear of intimacy and mental toughness generate poor quality of life and how these negative outcomes may induce cognitive impairment. The findings of this study also contribute to the dissemination of previous and existing research by emphasizing the potential buffering of mental toughness on the link between fear of intimacy and neuropsychological impairment. Even though previous substantial clinical investigations on mental toughness neglected potential buffers, several recent studies have also avoided testing the moderators of mental toughness on outcome variables (psychological impairment).
The study’s findings suggest that MT can help reduce the impact of fear of intimacy on cognitive impairment. This study also disseminates the findings of recent studies that suggest that closeness about difficulties itself has a negative impact on QoL in the setting of infertile patients. This study used a multi-level method for purposive as well as experience sampling investigations, which is uncommon in the mental health literature.
There are certain limitations to this study that should be considered. First, the cross-sectional design makes it difficult to draw a causal conclusion between research variables.
Second, our study only included infertile patients from one province’s infertility clinics. As a result, the sample may have an impact on the generalization of the results.
In summary, the current study is an attempt to understand how fear of intimacy, as an important aspect of personality, makes infertile patients more vulnerable to neuropsychological impairments, poor QoL, and poor mental toughness. The primary advantage of investigating the relationship between fear of intimacy and neuropsychological impairment is that it informs providers about the additional assessment needs of infertile patients.
In addition, the researchers propose that qualitative research utilizing narrative analysis or an interpretive phenomenological method may be used to gather real-world data to support the positivist approach used in this study. The research was only conducted in a relational and cross-sectional environment due to the pandemic’s unfavorable effects. Data were obtained physically, using the same logic and a more basic sampling technique. These should be taken into account while interpreting study results.
In this context, research involving infertile men patients who have been infected with the infertility and have recovered is believed to be necessary. Furthermore, adopting multimethod or mixed methods research in terms of data diversity is thought to produce substantial results in terms of external validity. Furthermore, research focused on cross-national comparisons is believed to yield crucial findings in terms of comprehending the nature of the problem.
This study concluded that amongst infertile patients, fear of intimacy was significantly associated with neuropsychological impairment as well as fear of intimacy has positive significant association with emotional problems, learning problems, sensory and motor problem, concentration problem, mental & physical in coordination and depression. Similarly, fear of intimacy was negatively associated with quality of life. Furthermore, QoL was significantly mediated by the association between fear of intimacy and neuropsychological impairment. Moreover, mental toughness moderated the association between fear of intimacy and neuropsychological impairment.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Study was approved by the Islamic International University ethics committee and consent was obtained from the participants. Moreover study has adapted all the guidelines outlined in the declaration of Helsinki ethical principles.
SH, MB, and NK executed the project and wrote the manuscript. SH, SF, and SB had literature reviewed, and data collection. EJ contributed to project administration, funding, and statistical analysis. All authors contributed to the article and approved the submitted version.
The authors acknowledged the financial support from the Postgraduate Education Reform and Quality Improvement Project of Henan Province (No.YJS2022KC30); the Postgraduate Cultivating Innovation and Quality Improvement Action Plan of Henan University (No.YJSJG2022XJ059).
The authors would like to express their gratitude to the referees who helped to improve this paper.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Kopa, Z, Keszthelyi, M, and Sofikitis, N. Administration of antioxidants in the infertile male: when it may have a beneficial effect? Curr Pharm Des. (2021) 27:2665–8. doi: 10.2174/1381612826666200303115552
2. Zegers-Hochschild, F, Adamson, GD, Dyer, S, Racowsky, C, De Mouzon, J, Sokol, R, et al. The international glossary on infertility and fertility care, 2017. Hum Reprod. (2017) 32:1786–801. doi: 10.1093/humrep/dex234
3. Vander Borght, M, and Wyns, C. Fertility and infertility: definition and epidemiology. Clin Biochem. (2018) 62:2–10. doi: 10.1016/j.clinbiochem.2018.03.012
4. Thoma, ME, McLain, AC, Louis, JF, King, RB, Trumble, AC, Sundaram, R, et al. Prevalence of infertility in the United States as estimated by the current duration approach and a traditional constructed approach. Fertil Steril. (2013) 99:1324–1331.e1. doi: 10.1016/j.fertnstert.2012.11.037
5. Slama, R, Hansen, OKH, Ducot, B, Bohet, A, Sorensen, D, Giorgis Allemand, L, et al. Estimation of the frequency of involuntary infertility on a nation-wide basis. Hum Reprod. (2012) 27:1489–98. doi: 10.1093/humrep/des070
6. Zhou, Z, Zheng, D, Wu, H, Li, R, Xu, S, Kang, Y, et al. Epidemiology of infertility in China: a population-based study. BJOG. (2018) 125:432–41. doi: 10.1111/1471-0528.14966
7. Inhorn, MC, and Patrizio, P. Infertility around the globe: new thinking on gender, reproductive technologies and global movements in the 21st century. Hum Reprod Update. (2015) 21:411–26. doi: 10.1093/humupd/dmv016
8. Poornima, S, Daram, S, Devaki, RK, and Qurratulain, H. Chromosomal abnormalities in couples with primary and secondary infertility: genetic counseling for assisted reproductive techniques (ART). J Reprod Infertil. (2020) 4:269. doi: 10.18502/jri.v21i4.4331
9. Kumar, N, and Singh, AK. Trends of male factor infertility, an important cause of infertility: a review of literature. J Hum Reprod Sci. (2015) 8:191–6. doi: 10.4103/0974-1208.170370
10. Bai, CF, Sun, JW, Li, J, Jing, WH, Zhang, XK, Zhang, X, et al. Gender differences in factors associated with depression in infertility patients. J Adv Nurs. (2019) 75:3515–24. doi: 10.1111/jan.14171
11. Ussher, JM, and Perz, J. Threat of biographical disruption: the gendered construction and experience of infertility following cancer for women and men. BMC Cancer. (2018) 18:1–17. doi: 10.1186/s12885-018-4172-5
12. Alhathal, N, Maddirevula, S, Coskun, S, Alali, H, Assoum, M, Morris, T, et al. A genomics approach to male infertility. Genet Med. (2020) 22:1967–75. doi: 10.1038/s41436-020-0916-0
13. Wang, C, Horby, PW, Hayden, FG, and Gao, GF. A novel coronavirus outbreak of global health concern. Lancet. (2020) 395:470–3. doi: 10.1016/S0140-6736(20)30185-9
14. Liu, C, Li, W, Chen, X, Liu, M, Zuo, L, Chen, L, et al. Dose-response association between transportation noise exposure and type 2 diabetes: a systematic review and meta-analysis of prospective cohort studies. Diabetes Metab Res Rev. (2023) 39:e3595. doi: 10.1002/dmrr.3595
15. Liu, M, Kamper-DeMarco, KE, Zhang, J, Xiao, J, Dong, D, and Xue, P. Time spent on social media and risk of depression in adolescents: a dose–response meta-analysis. Int J Environ Res Public Health. (2022) 19:5164. doi: 10.3390/ijerph19095164
16. Volgsten, H, Skoog Svanberg, A, Ekselius, L, Lundkvist, Ö, and Sundström Poromaa, I. Prevalence of psychiatric disorders in infertile women and men undergoing in vitro fertilization treatment. Hum Reprod. (2008) 23:2056–63. doi: 10.1093/humrep/den154
17. Volgsten, H, Svanberg, AS, Ekselius, L, Lundkvist, Ö, and Poromaa, IS. Risk factors for psychiatric disorders in infertile women and men undergoing in vitro fertilization treatment. Fertil Steril. (2010) 93:1088–96. doi: 10.1016/j.fertnstert.2008.11.008
18. Biggs, A., Brough, P., and Drummond, S.. Lazarus and Folkman’s psychological stress and coping theory in the handbook of stress and health: a guide to research and practice, eds. C. L. Cooper and J. C. Quick (2017) Wiley Blackwell. doi: 10.1002/9781118993811.ch21
19. Lazarus, RS . Toward better research on stress and coping. Am Psychol. (2000) 55:665–73. doi: 10.1037/0003-066X.55.6.665
20. Lazarus, RS, and Folkman, S. Stress, appraisal, and coping. New York, NY. Springer Publishing Company (1984).
21. Aghakhani, N, Ewalds-Kvist, BM, Sheikhan, F, and Khoei, EM. Iranian women’s experiences of infertility: a qualitative study. Int J Reprod Biomed. (2020) 18:65–73. doi: 10.18502/ijrm.v18i1.6203
22. Bhamani, SS, Zahid, N, Zahid, W, Farooq, S, Sachwani, S, Chapman, M, et al. Association of depression and resilience with fertility quality of life among patients presenting to the infertility centre for treatment in Karachi Pakistan. BMC Public Health. (2020) 20:1–11. doi: 10.1186/s12889-020-09706-1
23. Onofre, J, Geenen, L, Cox, A, Van Der Auwera, I, Willendrup, F, Andersen, E, et al. Simplified sperm testing devices: a possible tool to overcome lack of accessibility and inconsistency in male factor infertility diagnosis. An opportunity for low-and middle-income countries. Facts Views Vis Obgyn. (2021) 13:79–93. doi: 10.52054/FVVO.13.1.011
24. McCleary-Sills, J, Namy, S, Nyoni, J, Rweyemamu, D, Salvatory, A, and Teven, E. Stigma, shame and women’s limited agency in help-seeking for intimate partner violence. Glob Public Health. (2016) 11:224–35. doi: 10.1080/17441692.2015.1047391
25. Roberts, L, Renati, S, Solomon, S, and Montgomery, S. Women and infertility in a pronatalist culture: mental health in the slums of Mumbai. Int J Women’s Health. (2020) 12:993–1003. doi: 10.2147/IJWH.S273149
26. Mansour, F, and Mohdy, HA. Intimate partner violence among women with female infertility. Am J Nurs. (2018) 6:309–16.
27. Çambel, B, and Akköz Çevik, S. Prevalence of intimate partner and family violence among women attending infertility clinic and relationship between violence and quality of life. J Obstet Gynaecol. (2022) 42:2082–8. doi: 10.1080/01443615.2021.2024156
28. Willer, EK . Running-in (to) transition: embodied practice under the load of infertility, baby loss, and motherhood. Health Commun. (2021) 36:1176–87. doi: 10.1080/10410236.2020.1748830
29. Grunberg, PH, Da Costa, D, Dennis, CL, O’Connell, S, Lahuec, A, and Zelkowitz, P. How did you cope with such concerns?’: insights from a monitored online infertility peer support forum. Hum Fertil. (2021):1–15. doi: 10.1080/14647273.2021.1959952
30. Gerlock, AA, Grimesey, J, and Sayre, G. Military-related posttraumatic stress disorder and intimate relationship behaviors: a developing dyadic relationship model. J Marital Fam Ther. (2014) 40:344–56. doi: 10.1111/jmft.12017
31. Li, Y, Zhang, X, Shi, M, Guo, S, and Wang, L. Resilience acts as a moderator in the relationship between infertility-related stress and fertility quality of life among women with infertility: a cross-sectional study. Health Qual Life Outcomes. (2019) 17:1–9.
32. Cha, DS, Carmona, NE, Subramaniapillai, M, Mansur, RB, Lee, Y, Lee, JH, et al. Cognitive impairment as measured by the THINC-integrated tool (THINC-it): association with psychosocial function in major depressive disorder. J Affect Disord. (2017) 222:14–20. doi: 10.1016/j.jad.2017.06.036
33. Jahromi, BN, Mansouri, M, Forouhari, S, Poordast, T, and Salehi, A. Quality of life and its influencing factors of couples referred to an infertility center in Shiraz, Iran. Int J Fertil Steril. (2018) 11:293. doi: 10.22074/ijfs.2018.5123
34. Lakatos, E, Szigeti, JF, Ujma, PP, Sexty, R, and Balog, P. Anxiety and depression among infertile women: a cross-sectional survey from Hungary. BMC Womens Health. (2017) 17:1–9. doi: 10.1186/s12905-017-0410-2
35. Evers, K, Maljaars, J, Schepens, H, Vanaken, GJ, and Noens, I. Conceptualization of quality of life in autistic individuals. Dev Med Child Neurol. (2022) 64:950–6. doi: 10.1111/dmcn.15205
36. Masoumi, SZ, Garousian, M, Khani, S, Oliaei, SR, and Shayan, A. Comparison of quality of life, sexual satisfaction and marital satisfaction between fertile and infertile couples. Int J Fertil Steril. (2016) 10:290–6.
37. Namdar, A, Naghizadeh, MM, Zamani, M, Yaghmaei, F, and Sameni, MH. Quality of life and general health of infertile women. Health Qual Life Outcomes. (2017) 15:139. doi: 10.1186/s12955-017-0712-y
38. Gameiro, S, Boivin, J, Peronace, L, and Verhaak, CM. Why do patients discontinue fertility treatment? A systematic review of reasons and predictors of discontinuation in fertility treatment. Hum Reprod Update. (2012) 18:652–69. doi: 10.1093/humupd/dms031
39. Li, G, Zhao, D, Wang, Q, Zhou, M, Kong, L, Fang, M, et al. Infertility-related stress and quality of life among infertile women with polycystic ovary syndrome: does body mass index matter? J Psychosom Res. (2022) 158:110908. doi: 10.1016/j.jpsychores.2022.110908
40. Patterson, P, Perz, J, Tindle, R, McDonald, FE, and Ussher, JM. Infertility after cancer: how the need to be a parent, fertility-related social concern, and acceptance of illness influence quality of life. Cancer Nurs. (2021) 44:E244–51. doi: 10.1097/NCC.0000000000000811
41. Zurlo, MC, Della Volta, MFC, and Vallone, F. Predictors of quality of life and psychological health in infertile couples: the moderating role of duration of infertility. Qual Life Res. (2018) 27:945–54. doi: 10.1007/s11136-017-1781-4
42. Budarin, YS, Chirkov, DK, and Magomedov, FB. Digital cooperation in the Russian Federation In: Bogoviz, A.V., Suglobov, A.E., Maloletko, A.N., Kaurova, O.V. (eds). Сooperation and sustainable development. Cham: Springer (2022). 27–38.
43. St Clair-Thompson, H, Bugler, M, Robinson, J, Clough, P, McGeown, SP, and Perry, J. Mental toughness in education: exploring relationships with attainment, attendance, behaviour and peer relationships. Educ Psychol. (2015) 35:886–907. doi: 10.1080/01443410.2014.895294
44. Brand, S, Kalak, N, Gerber, M, Clough, PJ, Lemola, S, Pühse, U, et al. During early and mid-adolescence, greater mental toughness is related to increased sleep quality and quality of life. J Health Psychol. (2016) 21:905–15. doi: 10.1177/1359105314542816
45. Valle, MF, Huebner, ES, and Suldo, SM. An analysis of hope as a psychological strength. J Sch Psychol. (2006) 44:393–406. doi: 10.1016/j.jsp.2006.03.005
46. Clough, P, and Strycharczyk, D. Developing mental toughness: improving performance, wellbeing and positive behaviour in others. London: Kogan Page Publishers (2012).
47. Gerber, M, Feldmeth, AK, Lang, C, Brand, S, Elliot, C, Holsboer-Trachsler, E, et al. The relationship between mental toughness, stress, and burnout among adolescents: a longitudinal study with Swiss vocational students. Psychol Rep. (2015) 117:703–23. doi: 10.2466/14.02.PR0.117c29z6
48. Lin, Y, Mutz, J, Clough, PJ, and Papageorgiou, KA. Mental toughness and individual differences in learning, educational and work performance, psychological well-being, and personality: a systematic review. Front Psychol. (2017) 8:1345. doi: 10.3389/fpsyg.2017.01345
49. Jones, MI, and Parker, JK. Mindfulness mediates the relationship between mental toughness and pain catastrophizing in cyclists. Eur J Sport Sci. (2018) 18:872–81. doi: 10.1080/17461391.2018.1478450
50. Mojtahedi, D, Dagnall, N, Denovan, A, Clough, P, Hull, S, Canning, D, et al. The relationship between mental toughness, job loss, and mental health issues during the COVID-19 pandemic. Front Psych. (2021) 11:607246. doi: 10.3389/fpsyt.2020.607246
51. Lau, Y, and Chan, KS. Psychometric evaluation of the Chinese version of the fear of intimacy with helping professionals scale. PLoS One. (2018) 13:e0196774. doi: 10.1371/journal.pone.0196774
52. Papageorgiou, KA, Malanchini, M, Denovan, A, Clough, PJ, Shakeshaft, N, Schofield, K, et al. Longitudinal associations between narcissism, mental toughness and school achievement. Personal Individ Differ. (2018) 131:105–10. doi: 10.1016/j.paid.2018.04.024
53. Khan, MNS, Akhter, MS, Ayub, M, Alam, S, and Laghari, N. Translation and validation of WHOQOL BREF. J Coll of Physicians Surg Pak. (2003) 13:98–100.
54. World Health Organization . WHOQOL-BREF: introduction, administration, scoring and generic version of the assessment: field trial version, December (No. WHOQOL-BREF) (1996).
55. Naheed, SR . Neuropsychopathology and role of family support in improvement of the stroke patient. Unpublished Ph.D Disertation, National Institute of Psychology, QAU, Islamabad (2000).
56. Anderson, JC, and Gerbing, DW. Structural equation modeling in practice: a review and recommended two-step approach. Psychol Bull. (1988) 103:411–23. doi: 10.1037/0033-2909.103.3.411
57. Podsakoff, PM, MacKenzie, SB, Lee, JY, and Podsakoff, NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol. (2003) 88:879–903. doi: 10.1037/0021-9010.88.5.879
58. Chen, Y, Hou, S, Fu, K, Han, X, and Ye, L. Low-velocity impact response of composite sandwich structures: modelling and experiment. Compos Struct. (2017) 168:322–34. doi: 10.1016/j.compstruct.2017.02.064
59. Sellbom, M, and Tellegen, A. Factor analysis in psychological assessment research: common pitfalls and recommendations. Psychol Assess. (2019) 31:1428–41. doi: 10.1037/pas0000623
60. Khan, NA, Khan, AN, Moin, MF, and Pitafi, AH. A trail of chaos: how psychopathic leadership influence employee satisfaction and turnover intention via self-efficacy in tourism enterprises. J Leis Res. (2021) 52:3:347–369. doi: 10.1080/00222216.2020.1785359
61. Fornell, C, and Larcker, DF. Structural equation models with unobservable variables and measurement error: algebra and statistics. J Mark Res. (1981) 18:382. doi: 10.2307/3150980
64. Bagozzi, RP . Further thoughts on the validity of measures of elation, gladness, and joy. J Pers Soc Psychol. (1991) 61:98–104. doi: 10.1037/0022-3514.61.1.98
65. Khan, NH, Hassan, S, Bahader, S, Fatima, S, Zaidi, SMIH, Virk, R, et al. How daily obstacles affect frontline healthcare professionals’ mental health during omicron: a daily diary study of handwashing behavior. Int J Environ Res Public Health. (2022) 19:8748. doi: 10.3390/ijerph19148748
66. Tripp, CP, and Hair, ML. An infrared study of the reaction of octadecyltrichlorosilane with silica. Langmuir. (1992) 8:1120–6. doi: 10.1021/la00040a018
67. Milman, E, Neimeyer, RA, Fitzpatrick, M, MacKinnon, CJ, Muis, KR, and Cohen, SR. Prolonged grief and the disruption of meaning: establishing a mediation model. J Couns Psychol. (2019) 66:714–25. doi: 10.1037/cou0000370
68. Fisher, JR, and Hammarberg, K. Psychological and social aspects of infertility in men: an overview of the evidence and implications for psychologically informed clinical care and future research. Asian J Androl. (2012) 14:121–9. doi: 10.1038/aja.2011.72
69. Holley, SR, Pasch, LA, Bleil, ME, Gregorich, S, Katz, PK, and Adler, NE. Prevalence and predictors of major depressive disorder for fertility treatment patients and their partners. Fertil Steril. (2015) 103:1332–9. doi: 10.1016/j.fertnstert.2015.02.018
70. Li, X, Zhang, X, and Jia, T. Humanization of nature: testing the influences of urban park characteristics and psychological factors on collegers’ perceived restoration. Urban For Urban Green. (2023) 79:127806. doi: 10.1016/j.ufug.2022.127806
71. Lyu, Z, Feng, X, Li, N, Zhao, W, Wei, L, Chen, Y, et al. Human papillomavirus in semen and the risk for male infertility: a systematic review and meta-analysis. BMC Infect Dis. (2017) 17:1–9. doi: 10.1186/s12879-017-2812-z
72. Schick, M, Rösner, S, Toth, B, Strowitzki, T, and Wischmann, T. Exploring involuntary childlessness in men–a qualitative study assessing quality of life, role aspects and control beliefs in men’s perception of the fertility treatment process. Hum Fertil. (2016) 19:32–42. doi: 10.3109/14647273.2016.1154193
73. Wischmann, T, and Thorn, P. (male) infertility: what does it mean to men? New evidence from quantitative and qualitative studies. Reprod Biomed Online. (2013) 27:236–43. doi: 10.1016/j.rbmo.2013.06.002
74. Cao, W, Fang, Z, Hou, G, Han, M, Xu, X, Dong, J, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. (2020) 287:112934. doi: 10.1016/j.psychres.2020.112934
75. Kumar, P, Kumar, N, Aggarwal, P, and Yeap, JA. Working in lockdown: the relationship between COVID-19 induced work stressors, job performance, distress, and life satisfaction. Curr Psychol. (2021) 40:6308–6323. doi: 10.1007/s12144-021-01567-0
76. Zheng, F, Khan, NA, and Hussain, S. The COVID 19 pandemic and digital higher education: exploring the impact of proactive personality on social capital through internet self-efficacy and online interaction quality. Child Youth Serv Rev. (2020) 119:105694–12. doi: 10.1016/j.childyouth.2020.105694
77. Keylor, R, and Apfel, R. Male infertility: integrating an old psychoanalytic story with the research literature. Stud Gend Sex. (2010) 11:60–77. doi: 10.1080/15240651003666326
78. Nagórska, M, Bartosiewicz, A, Obrzut, B, and Darmochwał-Kolarz, D. Gender differences in the experience of infertility concerning polish couples: preliminary research. Int J Environ Res Public Health. (2019) 16:23–37. doi: 10.3390/ijerph16132337
79. Babul-Hirji, R, Hirji, R, and Chitayat, D. Genetic counselling for infertile men of known and unknown etiology. Transl Androl Urol. (2021) 10:1479–85. doi: 10.21037/tau-2019-gcmi-09
80. Halcomb, L . Men and infertility: insights from the sociology of gender. Sociol Compass. (2018) 12:e12624. doi: 10.1111/soc4.12624
81. Hanna, E, and Gough, B. The impact of infertility on men’s work and finances: findings from a qualitative questionnaire study. Gend Work Organ. (2020) 27:581–91. doi: 10.1111/gwao.12414
82. Jamil, S, Shoaib, M, Aziz, W, and Ather, MH. Does male factor infertility impact on self-esteem and sexual relationship? Andrologia. (2020) 52:e13460. doi: 10.1111/and.13460
83. Vo, THM, Nakamura, K, Seino, K, Nguyen, HTL, and Van Vo, T. Fear of falling and cognitive impairment in elderly with different social support levels: findings from a community survey in Central Vietnam. BMC Geriatr. (2020) 20:1–10. doi: 10.1186/s12877-020-01533-8
84. Aasen Nilsen, S, Breivik, K, Wold, B, and Bøe, T. Divorce and family structure in Norway: associations with adolescent mental health. J Divorce Remarriage. (2018) 59:175–94. doi: 10.1080/10502556.2017.1402655
85. Corrigan, PW, and Nieweglowski, K. How does familiarity impact the stigma of mental illness? Clin Psychol Rev. (2019) 70:40–50. doi: 10.1016/j.cpr.2019.02.001
86. St. Vil, NM, St. Vil, C, and Fairfax, CN. Posttraumatic slave syndrome, the patriarchal nuclear family structure, and African American male–female relationships. Soc Work. (2019) 64:139–46. doi: 10.1093/sw/swz002
87. Conejero, I, Olié, E, Courtet, P, and Calati, R. Suicide in older adults: current perspectives. Clin Interv Aging. (2018) 13:691–9. doi: 10.2147/CIA.S130670
88. Mukhtar, S . Psychological impact of COVID-19 on older adults. Curr Med Res Pract. (2020) 10:201–2. doi: 10.1016/j.cmrp.2020.07.016
89. Taylor, HO, Taylor, RJ, Nguyen, AW, and Chatters, L. Social isolation, depression, and psychological distress among older adults. J Aging Health. (2018) 30:229–46. doi: 10.1177/0898264316673511
90. Ghoncheh, KA, Liu, CH, Lin, CY, Saffari, M, Griffiths, MD, and Pakpour, AH. Fear of COVID-19 and religious coping mediate the associations between religiosity and distress among older adults. Health Promot Perspect. (2021) 11:316–22. doi: 10.34172/hpp.2021.40
91. Ganong, K, and Larson, E. Intimacy and belonging: the association between sexual activity and depression among older adults. Soc Ment Health. (2011) 1:153–72. doi: 10.1177/2156869311431612
92. Rheaume, C, and Mitty, E. Sexuality and intimacy in older adults. Geriatr Nurs. (2008) 29:342–9. doi: 10.1016/j.gerinurse.2008.08.004
93. Morris, RG, Worsley, C, and Matthews, D. Neuropsychological assessment in older people: old principles and new directions. Adv Psychiatr Treat. (2000) 6:362–70. doi: 10.1192/apt.6.5.362
94. Rog, LA, Park, LQ, Harvey, DJ, Huang, CJ, Mackin, S, and Farias, ST. The independent contributions of cognitive impairment and neuropsychiatric symptoms to everyday function in older adults. Clin Neuropsychol. (2014) 28:215–36. doi: 10.1080/13854046.2013.876101
95. Huang, R, Ghose, B, and Tang, S. Effect of financial stress on self-rereported health and quality of life among older adults in five developing countries: a cross sectional analysis of WHO-SAGE survey. BMC Geriatr. (2020) 20:1–12. doi: 10.1186/s12877-020-01687-5
96. Detert, JR, and Burris, ER. Leadership behavior and employee voice: is the door really open? Acad Manag J. (2007) 50:869–84. doi: 10.5465/amj.2007.26279183
Keywords: fear of intimacy, quality of life, neuropsychological impairment, mental toughness, infertility
Citation: Hassan S, Bhatti MI, Habib S, Fatima S, Bhader S, Khan NH and Jiang E (2023) How fear of intimacy affects infertile men’s neuropsychological functioning through mental toughness. Front. Psychiatry. 14:1049008. doi: 10.3389/fpsyt.2023.1049008
Received: 20 September 2022; Accepted: 03 May 2023;
Published: 24 July 2023.
Edited by:
Wulf Rössler, Charité University Medicine Berlin, GermanyReviewed by:
Junjun Wang, Soochow University Medical College (SUMC), ChinaCopyright © 2023 Hassan, Bhatti, Habib, Fatima, Bhader, Khan and Jiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nazeer Hussain Khan, a2FrYWtoYW4zNTE0QGdtYWlsLmNvbQ==; Enshe Jiang, ZXNqaWFuZ0BnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.