- 1The National Clinical Research Center for Mental Disorders and Beijing Key Laboratory of Mental Disorders, Beijing Anding Hospital, Capital Medical University, Beijing, China
- 2Advanced Innovation Center for Human Brain Protection, Capital Medical University, Beijing, China
Objective: Previous studies indicate that more than half of those who died by suicide had a depressive disorder. When discussing the factors associated to suicidal behavior (SB) among patients with major depressive disorder (MDD), sociocultural contexts should also be carefully considered. This case series study explored the factors correlated to SB among MDD patients in Beijing, China.
Methods: The patient information sheets were retrieved from an electronic database that comprised patient medical information. Three forms of binary logistic regression equations were conducted to explore the factors associated to SB among patients with MDD. For the inconsistent variables produced by the three regression models, the propensity score matching (PSM) analysis was done for further verification.
Results: In this retrospective study, 1,091 depressed cases were enrolled. The difference between the SB group and non-SB group in gender, impulsivity, the severity of depression, history of major mental trauma, and family history of suicide were statistically significant in univariate comparisons (P < 0.05); the binary logistic regression analysis and the PSM analysis showed that female gender, history of major mental trauma, impulsivity, family history of suicide and severity of depression were factors correlated to SB among patients with MDD (odds ratios >1).
Conclusions: Female gender, the history of major mental trauma, impulsivity, the severity of depression, and family history of suicide were independently associated with the appearance of SB among MDD patients in Beijing, China. Inevitably, these findings should be viewed with particular caution due to the inherent drawbacks of a retrospective nature. More prospective longitudinal research should be conducted to examine those dynamic alterations in the corresponding confounders.
Introduction
Suicide causes almost 800,000 deaths worldwide, representing 1.5% of the total death toll, with severe consequences for global public health (1). Studies indicate that about 60% of those who died by suicide had a major depressive disorder (MDD), which negatively affects how people think, feel, and act (2, 3). About 50% of people who die of suicide visit their general practitioners within 3 months prior to their deaths, 40% within 1 month, and 20% within 1 week before death (4, 5), indicating the important role of primary care in preventing suicide in this group.
Depression is one of the most frequently seen diseases in public. Most people with MDD have a certain amount of stigma and are reluctant to share their situation with others, which greatly adds to the difficulty in detecting high-risk suicidal individuals (6). In this scenario, it is important to identify the factors associated to suicidal behavior (SB), including suicidal ideation and suicide attempt, among people with MDD, for clinicians to recognize high-risk people and make appropriate interventions, as the suicide rate is reported to be reduced by close monitoring and aggressive treatment (7). Unfortunately, the link between SB-related factors among MDD patients and suicidality is frequently under-reported. For example, more than 2% of traffic accidents are closely related to SB. However, the phenomenon may be underreported, considering that suicides from car accidents may be reported as accidental in national statistics (8). Depression has previously been suggested to be closely related to suicide, but depression severity alone cannot accurately predict SB (9). Consequently, identifying more SB-related factors among depression patients is of great significance.
A previous meta-analysis explored SB-related risk factors among patients with MDD, and the results showed that male gender, prior suicidal attempts, family history of psychiatric disorder, the severity of depression, concurrent diseases, and hopelessness were closely related to SB (4). SB is an outcome of complex impacts of psychotic, mental, physical, cultural, and social factors; thus, determining the correlation factors of SB is difficult. In the present case, 44% of those who commit suicide are 65 or older; this rate is much higher than 18% in the United States (10, 11). Some adverse social and cultural impacts on older adults in rural China were suggested to be a key factor contributing to SB (12). Therefore, when discussing the factors correlated to SB among MDD patients, the sociocultural contexts should also be carefully considered (13).
In terms of society, ~1/4 (24%) of inpatients who commit suicide occur 3 months after discharge from psychiatric hospitals (14). The suicide risk prediction model may be an efficient way to assess the risk of suicide. It uses inpatient medical records and is more accurate than the prediction based on clinical judgment (15). The present preliminary case series study retrospectively explored the factors associated to SB with the help of inpatient medical records through propensity score matching (PSM) and logistic regression analysis. Here, we hypothesized that the factors correlated to SB among MDD patients in Beijing, China, differ from those in other countries due to the difference in sociocultural contexts.
Materials and methods
Study design and data sources
The present case series study retrospectively collected consecutive cases at Beijing Anding Hospital (Beijing, China) between November 1st 2017 and December 31st 2018. The medical records of the patients were obtained using the International Classification of Diseases, Tenth Revision (ICD-10) code in a clinical electronic database comprising the medical data of the patients, such as demographics, outpatient diagnoses, inpatient management, medical procedure, drug prescription and discharge diagnosis (16). The first two authors independently extracted the data information closely related to this study, and inconsistencies were resolved through consultation with the third author. The patients hospitalized repeatedly during the study were excluded to avoid duplicated or over-presented information from individual patients.
Study object and case definition
Depression cases with age 18 or older and < 60 years recorded in the medical records were recruited. Among them, depression was diagnosed following the ICD-10 disease codes in primary/secondary diagnoses, including F32 (depressive episode), F32.2 (the serious depressive episode without any psychotic symptom), F32.3 (the serious depressive episode in the presence of psychotic symptoms), F33 (relapsed depression disease), F33.2 (relapsed depression disease and/or present serious episode without any psychotic symptom), and F33.3 (relapsed depression disease, and present serious episode in the presence of psychotic symptoms). The index data were defined as the date when depression was diagnosed. Furthermore, depressive symptoms may occur in the preclinical stage of dementia (17). Therefore, this study ruled out dementia cases diagnosed (ICD-10 code F00-F03) 2 years after the index date. Finally, the present retrospective work enrolled 1,091 cases of depression.
Covariates
The collected data included gender, age, marital status, hobbies, monthly income, quality of interpersonal relationships, impulsivity, first episode or recurrence, the severity of depression and with/without somatic diseases, history of major mental trauma, drinking, and smoking, as well as family histories of suicide, psychiatric disorder, and SB, including suicidal ideation and suicide attempts. Among them, age groups were classified as groups 18–29, 30–39, 40–49, or 50–59-year old groups; the marital status of patients in married, unmarried, widowed, or divorced; the monthly income into <1,000, 1,000–3,000, 3,001–5,000, and >5,000 RMB (¥); interpersonal relation quality into good, general or poor. Furthermore, the Hamilton Rating Scale (HAMD, with 17 items) was adopted to assess the severity of depression, while suicidal attempts and suicidal ideation were evaluated mainly through in-person interviews by clinicians, according to the 3rd item in HAMD-17. In this study, SB was adopted as the dependent variable, and the others were used as independent variables based on previous findings and practical experience (4, 18, 19).
Data processing and statistical analysis
Statistical analysis was completed with SPSS 26.0 (Chicago, IL, USA) with a significance level of 5%. Prior to the analysis of the inferential data, we determined the normality of the data and the missing data. The categorical descriptive variables (like age, gender) were presented as counts and percentages. In addition, we used the Chi-square test to compare unordered categorical variables and the Wilcoxon test to compare ordered categorical variables between the group of patients with or without SB. Then we carried out a univariate analysis to identify independent variables for SB.
Binary logistic regression analysis helps to determine the independent variables associated with SB in depression cases. To find predicting variables for the regression equation more accurately, this study adopted three common regression models, including univariate, enter, and stepwise filtering (Forward LR) (18, 20, 21). In addition, regression equation validity was validated by the Hosmer-Lemeshow (HL) goodness-of-fit test; the idea of the HL test is to partition the observations into groups and construct a chi-squared statistic that summarizes the discrepancy between the number of observed and expected events within all combinations of group and outcome state. When the accompanying p-value is >0.05, it usually means a good fit effect of the regression equation (22). For unordered multiclass variables, such as marital status, set them as dummy variables in the regression models. The odds ratios (OR) and the relevant 95% confidence intervals (CI) were obtained to test the fitness of the condition within the regression equation, and OR values >1 indicated risk factors; correspondingly, OR values <1 represented protective factors.
Uncertain SB-related independent variables obtained from three logistic regression models were verified by PSM. PSM analysis is an ideal matching approach, which was considered to maximally reduce selection bias within retrospective studies while achieving a similar effect to that of a randomized controlled study (23). The matched analysis 1:1 according to the closest-neighbor matching with the 0–1 tolerance should be done according to the estimated PSM scores (24). For the two groups, those matched variables were further verified by the equilibrium test.
Results
Univariate comparison
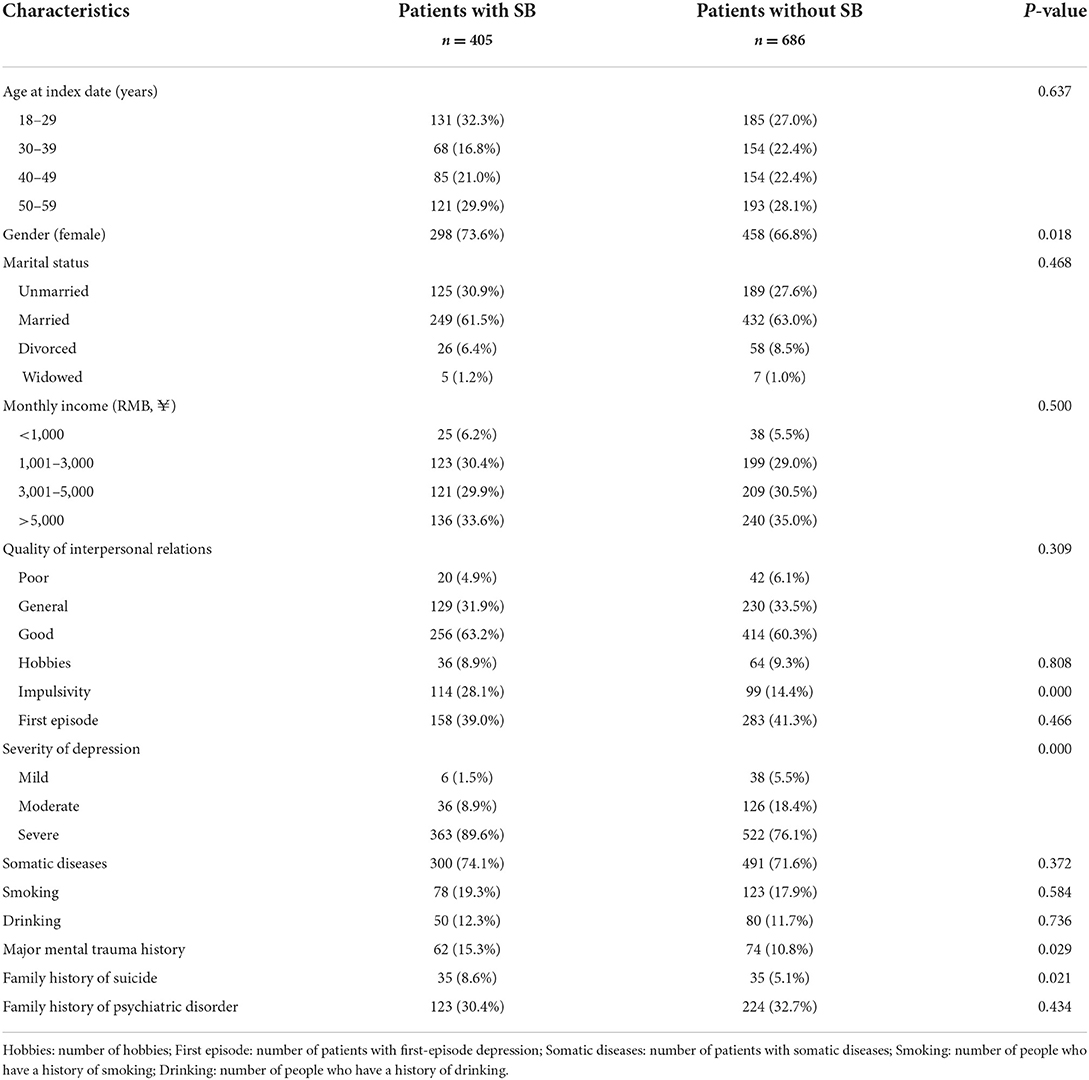
The results of the univariate comparison are listed in Table 1. Differences in genders, the severity of depression, impulsivity, history of major mental trauma, and family history of suicide were statistically significant between the non-SB and SB groups. Specifically, the proportion of women in the patient group with SB increased markedly compared to those without SB, as well as in the aspects of impulsivity, the severity of depression, family history of suicide, and history of major mental trauma. There were no significant differences in age, monthly income, marital status, hobbies, interpersonal relation quality, first episode or recurrence, with/without somatic diseases, histories of drinking and smoking, as well as family history of psychiatric disorder between non-SB and SB groups.
Binary logistic regression analysis
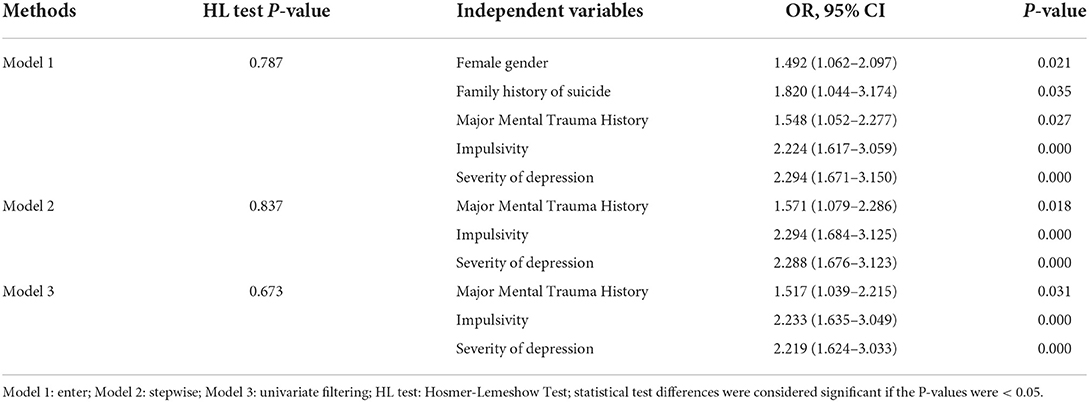
Independent variables associated with SB among depression cases were explored by binary logistic regression after adjusting for confounders (Table 2). As revealed by the HL test, all three regression models showed a favorable fitting effect (All P-values were >0.05). In model 1, the female gender, family history of suicide, major mental trauma history, the severity of depression, and impulsivity were taken into the regression equation, which implied that the female gender, family history of suicide, history of major mental trauma, the severity of depression, and impulsivity were factors correlated to the occurrence of SB. Similarly, in Model 2, we included major mental trauma history, depression severity, and impulsivity into the regression equation. In particular, in model 3, the critical independent variables incorporated into the regression equation were the same as those in model 2.
PSM analysis
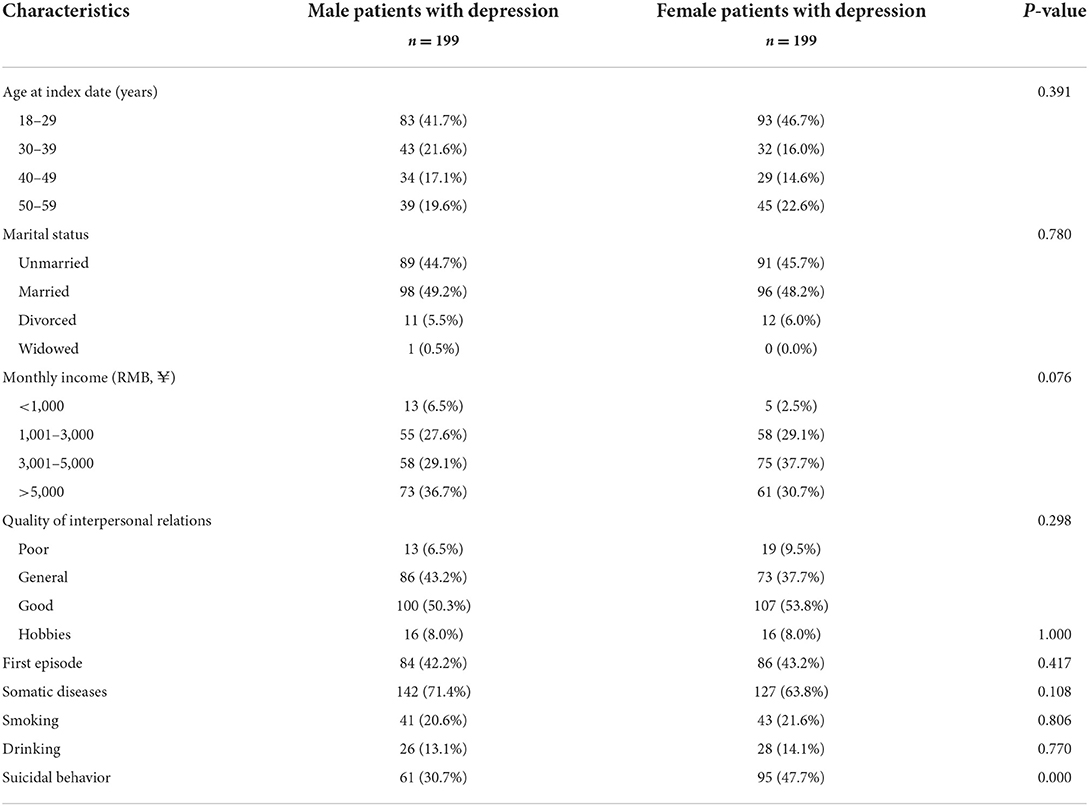
It can be clearly seen from Table 2 that the same independent variables selected from the three regression models were a history of major mental trauma, impulsivity, and severity of depression. Compared to Models 2 and 3, there are two more independent variables, namely female gender and family history of suicide. Suicide is highly familial and has been widely documented around the world. Therefore, it remains unclear whether the female gender was the factor that independently predicted the risk of SB among cases of depression. To better validate the associations of the female gender with SB, the 1,091 cases were classified as two groups according to gender (335 men and 756 women), with age, monthly income, marital status, hobbies, quality of interpersonal relationships, first episode or recurrence, with/without somatic diseases, drinking and smoking being predictive variables in the PSM analysis. A match tolerance of 0.005 was established during the SPSS analysis, without replacement of sampling; meanwhile, the above predictive variables were appropriately balanced according to the PSM analysis between the men's and women's groups. As seen in Table 3, a total of 199 of 335 male patients were matched among 756 female patients, and the female gender remained a factor in independently predicting the risk of SB in cases of depression (P = 0.000).
Discussion
The present case series study retrospectively indicated that female gender, history of major mental trauma, impulsivity, the severity of depression, and family history of suicide were factors associated to SB among adult depression cases based on electronic medical records in Beijing, China. Inevitably, these findings should be viewed with particular caution due to the inherent drawbacks of a retrospective nature.
Many articles investigate the association of gender with suicide-related behaviors, including suicide (which refers to suicide death), suicide attempts, and suicidal ideation. Although in most countries, suicide rates in males are higher than those in females, the prevalence of SB (suicide attempts and suicidal ideation) in females is higher than that in males in almost all countries (4, 14, 25). Thus, depressed inpatients with SB were more likely being females in our study. It is worth noting that the male-female ratios of suicide rates in China were ~1:1, although the gender ratio increased in the last two decades, and these gender ratios were almost 3:1 in most other countries (26, 27). For this, there may be two main reasons. First, there are about five million people in the rural areas of Beijing, and numerous females in the rural areas show a poor sociocultural status. In terms of suicide means, since pesticides are available in almost all families, taking lethal pesticides is often the first choice to commit suicide (28). As a result of being less economically developed compared to urban areas, pesticide poisoning is often not effectively treated, leading to higher suicide rates. Second, rural women are generally less educated and lack effective means of coping with negative events in their lives. Coupled with the fact that there are relatively few mental health services in rural areas, the access for rural women with psychological distress to psychotherapy is relatively poor (29).
Expectedly, a major history of mental trauma increases the risk of suicide; patients with unfavorable life experiences were associated with a higher risk of SB (30). The types of primary mental trauma are different in various stages of life. The experience of bullying is one of the main trauma associated with SB in children. When you grow up, there are more traumas that trigger SB intention, with emotional trauma being the main cause of adolescent SB. Typically, emotional and physical loss of family is the main factor related to the risk of SB in young adults (31). In fact, hypothalamic-pituitary-adrenal (HPA) axis dysfunction has previously been observed, which stimulates the adrenal cortex to secrete glucocorticoids in times of stress in adult depressed individuals with experience of childhood trauma, but the underlying mechanisms are poorly understood (32). A recent study found that the severity of childhood trauma experience contributes to a lack of response to antidepressant treatment and suggested glucocorticoid resistance as a target for the development of personalized treatment for a subgroup of depressed patients with a history of childhood trauma (33). Although our study did not investigate the types of trauma associated with SB among depressed patients, since negative experiences during childhood have everlasting influences (34), we highlight childhood trauma as an emergency.
Some studies have begun to investigate the effects of psychological and social factors on the pathogenic mechanism of SB (35, 36). More than 1/2 of people with suicidal attempts are impulsive, with many suicidal acts conducted with impulsivity (37). Our study also suggests that more attention should be paid to depressed patients with impulsive traits. This group of population is often accompanied by severe executive dysfunction, such as impaired self-inhibition. Importantly, the relationship between executive impairments and suicide risk has been well-established in previous literature (38), suggesting that we should pay attention to the importance of neuropsychological assessment, such as in terms of executive function or impulsiveness. The analysis of functional connectivity in the resting state (RSFC) has been recognized as a powerful well-established technique for unbiased analysis that reveals correlates of activity in discrete brain regions during rest (39) and could provide important insights into intrinsic FC in depressed cases with SB. Cao et al. (40) found that left prefrontal-parietal connectivity was associated with suicidal ideation and levels of impulsivity, but RSFC of the left prefrontal cortex with the right anterior cingulate cortex was correlated exclusively with impulsivity levels and not suicidal ideation in young depressed patients with suicide attempts. Additionally, they argued that the neural circuits underlying suicide attempts might differ from those that underlie suicidal ideation (40). In particular, impulsivity is often confused with agitation in clinical practice (41), and our study did not investigate the effect of agitation on the regression model. Thus, attention should be paid to the assessment of agitation symptoms in future prospective studies.
The severity of depression has been identified as one of the strongest predictors of future suicide attempts (42, 43). In terms of presentation, the severity of depression is often strongly associated with SB in depressed patients, along with other risk factors. For example, Andrewes et al. (44) found that only impulsivity and severity of depression were uniquely predictive of the frequency of suicide attempts. A study conducted in Korea found that 94% of people with suicidal ideation had sleep problems (45). Many studies have found that sleep problems are an independent factor for suicidal ideation, especially short-term sleep (46, 47). However, many studies have found that the relationship between sleep problems and suicidal ideation is mediated by depressive symptoms (45, 48). Hopelessness, worthlessness, helplessness, guilt, and crying are common manifestations of depressive symptoms.
During the last decades, brain imaging techniques provided new approaches to detect structural and functional brain changes in vivo, which may help to understand the relationship between depressive symptoms and SB. A systematic retrospective study found that reductions in the volume of basal ganglia and the hippocampus appeared to be more specific for pediatric unipolar disorder, whereas reduced corpus callosum volume and increased rates of deep white matter hyperintensities were more specific for pediatric bipolar disorder (49). Furthermore, the presence of subcortical alterations within the basal ganglia during childhood could subsequently extend to prefrontal cortical regions that continue to develop into adulthood. The prefrontal cortex has been shown to be strongly associated with executive control as impulsivity (50). In addition, a decrease in axonal plasticity in the hippocampus was also found in brain samples of suicide completers (51). As a retrospective case series study, we did not classify depressive symptoms in a multidimensional way. The very important point is that clinicians should pay more attention to these negative emotions, identify high-risk patients early, and then give them timely psychological intervention.
Studies have revealed that susceptibility to suicide among MDD patients is due to the interaction of multiple environmental and biological factors. Suicide is highly familial, and the results of adoption, twin, and family studies suggest that the aggregation of suicide attempts within families is partly due to genetic factors, with heritability estimates of ~40–55% (52). For example, an earlier study concluded that STin2 gene variants and a family history of suicide were significant predictors of suicide completion in depressed cases (53). Additionally, Wang et al. (54) found that a family history of suicide is the most reliable and robust risk factor for suicidal ideation. Neurocognitive deficits have been proposed as an intermediate phenotype between genes and behavioral outcomes for suicide-related behaviors (55). Furthermore, recently a study found that community youth with a family history of suicide performed worse on executive functioning scores, attention tests, and language reasoning (56), suggesting that enhanced neuropsychological testing could contribute to better screening of patients at risk of suicide.
This study may shed some light on clinical practice. Depression patients with the characteristics of the female, with a history of major mental trauma, a family history of suicide, and an impulsive personality, should receive special attention. Currently, clinicians often wrestle with how best to integrate recent advances in suicide prevention into practice in an efficient and effective manner. Suicide risk assessment screening tools are almost uniformly recommended to screen for depressed individuals with suicidal ideation in many countries; however, clinical practice has realistic time constraints, which often makes the predictive power of risk screening tools very limited. In addition to focusing on the risk factors for SB, which could be presented on the Suicide Risk Assessment Scale, Rudd et al. (57) believe that there are four other identifiable aspects that can be addressed in the interview, including the temporal dynamics and natural variability of suicidal ideation and motivation to die, the importance of assessing constructs other than suicidal ideation that are convincingly related to enduring risk or chronic vulnerability to suicide (58–60), the importance of understanding and assessing the potential for poor individual adherence and cooperation with clinical care, and the elegant utility of the expressed wish of patients to live and wish to die, coupled with reasons for living and reasons for dying (57). Due to cultural differences, the form of the interview may vary between physicians in different countries or regions, but the above recommendations help clinicians screen for depressed patients with suicidal ideation in a simple and straightforward manner.
We acknowledge several limitations to this study. First, compared with prospective cohort studies, such electronic medical records-based case series study is associated with certain inevitable drawbacks, including no details on cognitive impairment and education level, and it is suggested that it plays a key role in mediating SB with depression (61, 62). Second, the sample for this study was drawn from a specialist mental health care provider, so it is likely that depressive syndromes are more severe than those determined in the community samples screened. Third, depression diagnoses were based on ICD-10 codes, and there is no information on the procedure by which diagnoses were made. Fourth, the symptoms identified as covariates were derived from those recorded in the text rather than those that could be determined through a screening instrument. Fifth, due to these heterogeneities in sociocultural contexts and sample sources, this study possibly had a certain restricted application in the corresponding fields. Sixth, currently, factors screened by binary logistic regression analysis are independent of each other, the interdependence between them was not examined. Seventh, as a preliminary clinical retrospective study, we did not subdivide SB into suicidal ideation and suicide attempts; this is also the point that we will focus on in the next step.
Conclusion
Female gender, the history of major mental trauma, impulsivity, the severity of depression, and family history of suicide were independently associated with the appearance of SB among MDD patients in Beijing, China. Inevitably, these findings should be viewed with particular caution due to the inherent drawbacks of a retrospective nature. More prospective longitudinal research should be conducted to examine those dynamic alterations in the corresponding confounders.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Beijing Anding Hospital Affiliated to Capital Medical University. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
CL, WP, and DZ conceived and designed the research protocol. CL completed the data analyses. FM, TT, and LL assisted with data collection and collation. XL revised the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The present work was supported by the Beijing Municipal Administration of Hospitals Clinical Medicine Development of special funding (ZYLX201815).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
2. Cavanagh JT, Carson AJ, Sharpe M, Lawrie SM. Psychological autopsy studies of suicide: a systematic review. Psychol Med. (2003) 33:395–405. doi: 10.1017/S0033291702006943
3. Wiebenga JX, Eikelenboom M, Heering HD, van Oppen P, Penninx BW. Suicide ideation versus suicide attempt: examining overlapping and differential determinants in a large cohort of patients with depression and/or anxiety. Aust N Z J Psychiatry. (2021) 55:167–79. doi: 10.1177/0004867420951256
4. Hawton K, Casañas ICC, Haw C, Saunders K. Risk factors for suicide in individuals with depression: a systematic review. J Affect Disord. (2013) 147:17–28. doi: 10.1016/j.jad.2013.01.004
5. Pirkis J, Burgess P. Suicide and recency of health care contacts. A systematic review. Br J Psychiatry. (1998) 173:462–74. doi: 10.1192/bjp.173.6.462
6. Lopez V, Sanchez K, Killian MO, Eghaneyan BH. Depression screening and education: an examination of mental health literacy and stigma in a sample of Hispanic women. BMC Public Health. (2018) 18:646. doi: 10.1186/s12889-018-5516-4
7. Büscher R, Torok M, Terhorst Y, Sander L. Internet-based cognitive behavioral therapy to reduce suicidal ideation: a systematic review and meta-analysis. JAMA Netw Open. (2020) 3:e203933. doi: 10.1001/jamanetworkopen.2020.3933
8. Pompili M, Serafini G, Innamorati M, Montebovi F, Palermo M, et al. Car accidents as a method of suicide: a comprehensive overview. Forensic Sci Int. (2012) 223:1–9. doi: 10.1016/j.forsciint.2012.04.012
9. Handley T, Rich J, Davies K, Lewin T, Kelly B. The challenges of predicting suicidal thoughts and behaviours in a sample of rural Australians with depression. Int J Environ Res Public Health. (2018) 15:928. doi: 10.3390/ijerph15050928
10. Wang CW, Chan CL, Yip PS. Suicide rates in China from 2002 to 2011: an update. Soc Psychiatry Psychiatr Epidemiol. (2014) 49:929–41. doi: 10.1007/s00127-013-0789-5
11. Parmet S, Lynm C, Glass RM. JAMA patient page. Suicide in older persons. JAMA. (2004) 291:1158. doi: 10.1001/jama.291.9.1158
12. Li X, Xiao Z, Xiao S. Suicide among the elderly in mainland China. Psychogeriatrics. (2009) 9:62–6. doi: 10.1111/j.1479-8301.2009.00269.x
13. Cho SE, Na KS, Cho SJ, Im S, Kang SG. Geographical and temporal variations in the prevalence of mental disorders in suicide: systematic review and meta-analysis. J Affect Disord. (2016) 190:704–13. doi: 10.1016/j.jad.2015.11.008
14. Olfson M, Marcus SC, Bridge JA. Focusing suicide prevention on periods of high risk. JAMA. (2014) 311:1107–8. doi: 10.1001/jama.2014.501
15. Kessler RC, Warner CH, Ivany C, Petukhova MV, Rose S, Bromet EJ, et al. Predicting suicides after psychiatric hospitalization in US Army soldiers: the Army Study To Assess Risk and rEsilience in Servicemembers (Army STARRS). JAMA Psychiatry. (2015) 72:49–57. doi: 10.1001/jamapsychiatry.2014.1754
16. Cai W, Mueller C, Shetty H, Perera G, Stewart R. Predictors of mortality in people with late-life depression: a retrospective cohort study. J Affect Disord. (2020) 266:695–701. doi: 10.1016/j.jad.2020.01.021
17. Jost BC, Grossberg GT. The evolution of psychiatric symptoms in Alzheimer's disease: a natural history study. J Am Geriatr Soc. (1996) 44:1078–81. doi: 10.1111/j.1532-5415.1996.tb02942.x
18. Liu C, Pan W, Zhu D, Mao P, Ma X. Risk factors for suicidal behavior in late-life depression: a retrospective preliminary clinical study. Geriatr Gerontol Int. (2021) 21:849–54. doi: 10.1111/ggi.14244
19. Omary A. Predictors and confounders of suicidal ideation and suicide attempts among adults with and without depression. Psychiatr Q. (2021) 92:331–45. doi: 10.1007/s11126-020-09800-y
20. Sivakumaran D, Ritz C, Gjøen JE, Vaz M, Selvam S, Ottenhoff THM, et al. Host blood RNA transcript and protein signatures for sputum-independent diagnostics of tuberculosis in adults. Front immunol. (2020) 11:626049. doi: 10.3389/fimmu.2020.626049
21. Stampehl M, Friedman HS, Navaratnam P, Russo P, Park S, Obi EN. Risk assessment of post-discharge mortality among recently hospitalized Medicare heart failure patients with reduced or preserved ejection fraction. Curr Med Res Opin. (2020) 36:179–88. doi: 10.1080/03007995.2019.1662654
22. Nattino G, Pennell ML, Lemeshow S. Assessing the goodness of fit of logistic regression models in large samples: a modification of the Hosmer-Lemeshow test. Biometrics. (2020) 76:549–60. doi: 10.1111/biom.13249
23. Jupiter DC. Propensity score matching: retrospective randomization? J Foot Ankle Surg. (2017) 56:417–20. doi: 10.1053/j.jfas.2017.01.013
24. Han DH, Choi SH, Kang CM, Lee WJ. Propensity score-matching analysis for single-site robotic cholecystectomy versus single-incision laparoscopic cholecystectomy: a retrospective cohort study. Int J Surg. (2020) 78:138–42. doi: 10.1016/j.ijsu.2020.04.042
25. Ribeiro JD, Franklin JC, Fox KR, Bentley KH, Kleiman EM, Chang BP, et al. Self-injurious thoughts and behaviors as risk factors for future suicide ideation, attempts, and death: a meta-analysis of longitudinal studies. Psychol Med. (2016) 46:225–36. doi: 10.1017/S0033291715001804
26. Sun L, Zhang J, Lamis DA, Wang Y. Risk assessment on suicide death and attempt among Chinese rural youths aged 15-34 years. Int J Environ Res Public Health. (2021) 18:13362. doi: 10.3390/ijerph182413362
28. Sun L, Zhang J. Medically serious suicide attempters with or without plan in rural China. J Nerv Ment Dis. (2016) 204:851–54. doi: 10.1097/NMD.0000000000000397
29. Zhang J, Wieczorek W, Conwell Y, Tu XM, Wu BY, Xiao S, et al. Characteristics of young rural Chinese suicides: a psychological autopsy study. Psychol Med. (2010) 40:581–9. doi: 10.1017/S0033291709990808
30. Fjeldsted R, Teasdale TW, Jensen M, Erlangsen A. Suicide in relation to the experience of stressful life events: a population-based study. Arch Suicide Res. (2017) 21:544–55. doi: 10.1080/13811118.2016.1259596
31. Ong MS, Lakoma M, Gees Bhosrekar S, Hickok J, McLean L, Murphy M, et al. Risk factors for suicide attempt in children, adolescents, and young adults hospitalized for mental health disorders. Child Adolesc Ment Health. (2021) 26:134–42. doi: 10.1111/camh.12400
32. Hennings JM, Ising M, Uhr M, Holsboer F, Lucae S. Effects of weariness of life, suicide ideations and suicide attempt on HPA axis regulation in depression. Psychoneuroendocrinology. (2021) 131:105286. doi: 10.1016/j.psyneuen.2021.105286
33. Nikkheslat N, McLaughlin AP, Hastings C, Zajkowska Z, Nettis MA, Mariani N, et al. Childhood trauma, HPA axis activity and antidepressant response in patients with depression. Brain Behav Immun. (2020) 87:229–37. doi: 10.1016/j.bbi.2019.11.024
34. Fjeldsted R, Teasdale TW, Bach B. Childhood trauma, stressful life events, and suicidality in Danish psychiatric outpatients. Nord J Psychiatry. (2020) 74:280–6. doi: 10.1080/08039488.2019.1702096
35. Milner A, Sveticic J, De Leo D. Suicide in the absence of mental disorder? A review of psychological autopsy studies across countries. Int J Soc Psychiatry. (2013) 59:545–54. doi: 10.1177/0020764012444259
36. Pridmore S. Mental disorder and suicide: a faulty connection. Aust N Z J Psychiatry. (2015) 49:18–20. doi: 10.1177/0004867414548904
37. Rimkeviciene J, O'Gorman J, De Leo D. Impulsive suicide attempts: a systematic literature review of definitions, characteristics and risk factors. J Affect Disord. (2015) 171:93–104. doi: 10.1016/j.jad.2014.08.044
38. Bredemeier K, Miller IW. Executive function and suicidality: a systematic qualitative review. Clin Psychol Rev. (2015) 40:170–83. doi: 10.1016/j.cpr.2015.06.005
39. Long Z, Du L, Zhao J, Wu S, Zheng Q, Lei X. Prediction on treatment improvement in depression with resting state connectivity: a coordinate-based meta-analysis. J Affect Disord. (2020) 276:62–8. doi: 10.1016/j.jad.2020.06.072
40. Cao J, Chen X, Chen J, Ai M, Gan Y, He J. The association between resting state functional connectivity and the trait of impulsivity and suicidal ideation in young depressed patients with suicide attempts. Front Psychiatry. (2021) 12:567976. doi: 10.3389/fpsyt.2021.567976
41. Pompili M, Innamorati M, Raja M, Falcone I, Ducci G, Angeletti G, et al. Suicide risk in depression and bipolar disorder: do impulsiveness-aggressiveness and pharmacotherapy predict suicidal intent? Neuropsychiatr Dis Treat. (2018) 4:247–55. doi: 10.2147/NDT.S2192
42. Pallaskorpi S, Suominen K, Ketokivi M, Valtonen H, Arvilommi P, Mantere O, et al. Incidence and predictors of suicide attempts in bipolar I and II disorders: a 5-year follow-up study. Bipolar Disord. (2017) 19:13–22. doi: 10.1111/bdi.12464
43. Kang C, Zheng Y, Yang L, Wang X, Zhao N, Guan TF. Prevalence, risk factors and clinical correlates of suicidal ideation in adolescent patients with depression in a large sample of Chinese. J Affect Disord. (2021) 290:272–8. doi: 10.1016/j.jad.2021.04.073
44. Andrewes HE, Hulbert C, Cotton SM, Betts J, Chanen AM. Relationships between the frequency and severity of non-suicidal self-injury and suicide attempts in youth with borderline personality disorder. Early Interv Psychiatry. (2019) 13:194–201. doi: 10.1111/eip.12461
45. Tae H, Jeong BR, Chae JH. Sleep problems as a risk factor for suicide: are certain specific sleep domains associated with increased suicide risk? J Affect Disord. (2019) 252:182–9. doi: 10.1016/j.jad.2019.04.053
46. Goldstein TR, Franzen PL. Sleep difficulties and suicidality in youth: current research and future directions. Curr Opin Psychol. (2020) 34:27–31. doi: 10.1016/j.copsyc.2019.08.021
47. Lee GY, Choi YJ. Association of school, family, and mental health characteristics with suicidal ideation among Korean adolescents. Res Nurs Health. (2015) 38:301–10. doi: 10.1002/nur.21661
48. Bryan CJ, Gonzales J, Rudd MD, Bryan AO, Clemans TA, Ray-Sannerud B, et al. Depression mediates the relation of insomnia severity with suicide risk in three clinical samples of U.S. Military Personnel. Depress Anxiety. (2015) 32:647–55. doi: 10.1002/da.22383
49. Serafini G, Pompili M, Borgwardt S, Houenou J, Geoffroy PA, Jardri R, et al. Brain changes in early-onset bipolar and unipolar depressive disorders: a systematic review in children and adolescents. Eur Child Adolesc Psychiatry. (2019) 23:1023–41. doi: 10.1007/s00787-014-0614-z
50. Friedman NP, Robbins TW. The role of prefrontal cortex in cognitive control and executive function. Neuropsychopharmacology. (2022) 47:72–89. doi: 10.1038/s41386-021-01132-0
51. Glavan D, Gheorman V, Gresita A, Hermann DM, Udristoiu I, Popa-Wagner A. Identification of transcriptome alterations in the prefrontal cortex, hippocampus, amygdala and hippocampus of suicide victims. Sci Rep. (2022) 11:18853. doi: 10.1038/s41598-021-98210-6
52. Brent DA, Melhem N. Familial transmission of suicidal behavior. Psychiatr Clin North Am. (2008) 31:157–77. doi: 10.1016/j.psc.2008.02.001
53. Lopez de Lara C, Dumais A, Rouleau G, Lesage A, Dumont M, Chawky N, et al. STin2 variant and family history of suicide as significant predictors of suicide completion in major depression. Biol Psychiatry. (2006) 59:114–20. doi: 10.1016/j.biopsych.2005.06.021
54. Wang YG, Chen S, Xu ZM, Shen ZH, Wang YQ, Wang YQ, et al. Family history of suicide and high motor impulsivity distinguish suicide attempters from suicide ideators among college students. J Psychiatr Res. (2017) 90:21–5. doi: 10.1016/j.jpsychires.2017.02.006
55. Mann JJ, Arango VA, Avenevoli S, Brent DA, Champagne FA, Clayton, et al. Candidate endophenotypes for genetic studies of suicidal behavior. Biol Psychiatry. (2009) 65:556–63. doi: 10.1016/j.biopsych.2008.11.021
56. Jones JD, Boyd RC, Calkins ME, Moore TM, Ahmed A, Barzilay R, et al. Association between family history of suicide attempt and neurocognitive functioning in community youth. J Child Psychol Psychiatry. (2021) 62:58–65. doi: 10.1111/jcpp.13239
57. Rudd MD, Bryan CJ. Finding effective and efficient ways to integrate research advances into the clinical suicide risk assessment interview. Front Psychiatry. (2022) 13:846244. doi: 10.3389/fpsyt.2022.846244
58. Peak NJ, Overholser JC, Ridley J, Braden A, Fisher L, Bixler J, et al. Too much to bear: psychometric evidence supporting the perceived burdensomeness scale. Crisis. (2016) 37:59–67. doi: 10.1027/0227-5910/a000355
59. Smith PN, Cukrowicz KC. Capable of suicide: a functional model of the acquired capability component of the Interpersonal-Psychological Theory of Suicide. Suicide Life Threat Behav. (2010) 40:266–75. doi: 10.1521/suli.2010.40.3.266
60. Rudd MD, Bryan CJ. The brief suicide cognitions scale: development and clinical application. Front Psychiatry. (2021) 12:737393. doi: 10.3389/fpsyt.2021.737393
61. Roca M, Del Amo AR, Riera-Serra P, Pérez-Ara MA, Castro A, Roman Juan J, et al. Suicidal risk and executive functions in major depressive disorder: a study protocol. BMC Psychiatry. (2019) 19:253. doi: 10.1186/s12888-019-2233-1
62. Lewitzka U, Spirling S, Ritter D, Smolka M, Goodday S, Bauer M, et al. Suicidal ideation vs. suicide attempts: clinical and psychosocial profile differences among depressed patients: a study on personality traits, psychopathological variables, and sociodemographic factors in 228 patients. J Nerv Ment Dis. (2017) 205:361–71. doi: 10.1097/NMD.0000000000000667
Keywords: suicidal behavior, binary logistic regression, major depressive disorder, matching of the propensity score, case series
Citation: Liu C, Pan W, Zhu D, Meng F, Tian T, Li L and Li X (2022) Factors of suicidal behavior among inpatients with major depressive disorder: A retrospective case series. Front. Psychiatry 13:996402. doi: 10.3389/fpsyt.2022.996402
Received: 17 July 2022; Accepted: 07 September 2022;
Published: 23 September 2022.
Edited by:
Kairi Kõlves, Griffith University, AustraliaReviewed by:
Gianluca Serafini, San Martino Hospital (IRCCS), ItalyYongsheng Tong, Peking University, China
Copyright © 2022 Liu, Pan, Zhu, Meng, Tian, Li and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaohong Li, bGl4aWFvaG9uZ19hbmRpbmdAY2NtdS5lZHUuY24=
†These authors have contributed equally to this work
 Chaomeng Liu
Chaomeng Liu Weigang Pan1,2†
Weigang Pan1,2† Dandi Zhu
Dandi Zhu Tengfei Tian
Tengfei Tian