- 1Faculty of Health and Life Sciences, School of Applied Social Sciences, De Montfort University, Leicester, United Kingdom
- 2School of Psychology, College of Health and Life Sciences, Aston University, Birmingham, United Kingdom
Background: Alexithymia is an independent predictor of symptoms of eating disorders, but also influences disordered eating in clinical samples indirectly via negative affect (depression and anxiety). The aim of the current work was to establish if alexithymia predicts disordered eating in a non-clinical sample directly and indirectly (via negative affect).
Methods: A sample of healthy females (n = 248) completed measures of depression, anxiety, alexithymia, and disordered eating (drive for thinness, bulimia, and body dissatisfaction). Bias-corrected bootstrapping was used to conduct parallel mediation analyses to determine if negative affect (depression and anxiety) mediated the influence of alexithymia on disordered eating.
Results: The relationship between alexithymia (difficulty identifying feelings) and drive for thinness was mediated by depression but not anxiety. The link between difficulty identifying feelings and bulimia was mediated by anxiety but not depression. The correlation between alexithymia (difficulty describing feelings) and body dissatisfaction was mediated by both depression and anxiety. However, after controlling for negative affect, difficulty identifying feelings remained an independent predictor of drive for thinness, and difficulty describing feelings remained an independent predictor of body dissatisfaction.
Conclusion: Facets of alexithymia (DIF and DDF) directly predict disordered eating in healthy participants as well as indirectly via depression and anxiety. These findings suggest that targeted interventions to improve the ability of individuals to identify and describe their feelings could be beneficial in reducing disordered eating, particularly in those “at risk” of developing eating disorders.
Introduction
Emotion regulation deficits are a core feature of eating disorders: anorexia nervosa (1), bulimia nervosa (2), and binge eating disorder (3). An important factor thought to underlie emotion dysregulation in individuals with eating disorders is alexithymia (4). Alexithymia (ALX) is a multi-faceted construct characterised by problems identifying one’s feelings, distinguishing between feelings and bodily sensations, difficulties in verbally describing one’s feelings to others, a lack of imagination and fantasies, and an externally focussed cognitive style (5). The most widely used measure of alexithymia is the 20-item Toronto Alexithymia Scale [TAS-20 (6, 7)], which consists of three subscales: difficulties identifying feelings (DIF), difficulties describing feelings (DIF), and externally-oriented thinking (EOT).
Studies using the TAS-20 have consistently shown high levels of alexithymia in patients with eating disorders: anorexia nervosa (8, 9), bulimia nervosa (10, 11), and binge eating disorder (12, 13), see also reviews (4, 14). Furthermore, direct links have been reported between scores on the alexithymia subscales DIF and DDF, and symptoms in patients with eating disorders (9, 12, 15, 16), which suggests that these facets might play a role in the development of disordered eating. In line with this proposal, longitudinal evidence revealed that alexithymia (scores on the DIF subscale) is a negative prognostic factor for outcomes in patients with eating disorders (17).
It has been suggested that alexithymia might be an enduring characteristic of individuals who are liable to develop disordered eating. Evidence in support of this proposal comes from studies reporting no change in alexithymia levels in patients in remission from their eating disorder (18, 19). However, other findings have revealed significant reductions in alexithymia as eating disorder symptoms improve (15, 20), which suggests that alexithymia might be a state feature of disordered eating rather than a dispositional influence. Nevertheless, even in studies that show reduced alexithymia scores upon remission, individuals who have experienced eating disorders still tend to report significantly higher alexithymia scores than do healthy controls with no history of disordered eating (10, 15, 16). Taken together, evidence supports the conception of alexithymia as a relatively stable feature of individuals who are at risk of developing disordered eating. This is also consistent with evidence of relative stability of alexithymia in patients with depression (21, 22), anxiety disorders (23), and in the general population (24, 25).
An important issue is that many aspects of disordered eating are dimensional not only across eating disorder diagnoses but also across the general population. For example, taxometric analysis has revealed that that dietary restraint, body dissatisfaction, and drive for thinness are dimensional across clinical and non-clinical samples (26). Furthermore, there is also evidence of a similar dimensional nature to binge eating (27). Given the conception of alexithymia as a trait vulnerability factor for disordered eating, relationships between alexithymia and measures of disordered eating would be expected within non-clinical samples. In line with this expectation, positive associations have been observed between total TAS-20 score and total score on the Eating Disorders Inventory [EDI (28)] in a sample of healthy participants (29). Positive correlations have also been found between the full TAS-20 score and the total score on the Eating Attitudes Test [EAT-26 (30)], and scores on all three subscales of the EAT-26: dieting, bulimia, and oral control (31). In another study the observed relationships between full TAS-20 scores and EAT-26 scores were limited to the total EAT-26 score and score on the bulimia subscale (32). The link between alexithymia (total TAS-20 score) and bulimic behaviours has been confirmed in another non-clinical sample (33). Studies examining the influence of the different facets of alexithymia in healthy participants have revealed that DIF and DDF scores are positively related to scores on the drive for thinness, bulimia, and body dissatisfaction scores on the EDI (34) and to scores on all three subscales of the EAT-26 (35). However, in other work using the EDI scores on the DIF and DDF subscales were only related to scores on the bulimia subscale (36). Taken together there is clear evidence that alexithymia is associated with disordered eating in non-clinical samples, but the nature of this relationship is not stable across studies. Thus, there is a need to examine factors that might influence the relationship between alexithymia and disordered eating.
One potentially important factor is negative affect, particularly depression and anxiety. High levels of alexithymia have been observed in individuals with depression (21, 37–40) and anxiety (23, 38). Furthermore, there is evidence that depression and anxiety are risk factors for the development of eating disorders (41–45). With this in mind, an important theoretical issue concerns whether the link between alexithymia and disordered eating can be explained by comorbid negative affect (depression and/or anxiety). A meta-analysis of the rates of alexithymia in clinically diagnosed eating disorders reported that, in 11 of the 19 studies that had controlled for depression (some also controlled for anxiety), differences in alexithymia between patients with eating disorders and healthy controls disappeared once the influence of negative affect had been controlled (14). When considering the non-clinical data, only three of the seven studies reporting significant relationships between alexithymia and disordered eating had controlled for negative affect. However, two of those that did control for depression reported that relationships between alexithymia and disordered eating remained after controlling for negative affect (29, 33) with only one showing that negative affect fully explained the link between alexithymia and disordered eating (34). One possibility is that negative affect (depression and anxiety) might mediate the effect of alexithymia on disordered eating. That is, alexithymia might influence disordered eating indirectly via negative affect.
One study that examined this proposal used mediation analysis to determine the direct and indirect effects of alexithymia on symptoms of anorexia nervosa, via the mediator depression (46). The direct effect refers to the relationship between alexithymia and anorexia, controlling for the influence of depression. The indirect effect refers to the influence of alexithymia on anorexia that occurs via depression; that is, alexithymia is linked to high levels of depression and high levels of depression are linked to more severe symptoms of anorexia. The results of the mediation analysis revealed evidence of both direct and indirect effects of alexithymia on anorexia (46). Another study examined the direct and indirect effects of alexithymia on disordered eating (measured by the EAT-26) via dual mediators of depression and anxiety within a sample of patients with borderline personality disorder (47). The results of this study showed that both depression and anxiety mediated the influence of alexithymia on disordered eating symptoms (indirect pathway). However, even after controlling for the influence of negative affect, there was still evidence of a direct effect of alexithymia on disordered eating. Taken together these studies suggest that alexithymia in clinical populations is an independent predictor of disordered eating, in addition to an indirect influence via negative affect.
It is important to examine if these relationships hold in a subclinical samples, as rates of subthreshold disordered eating are higher than those of clinically diagnosed eating disorders (48). For example, a recent study conducted in a cohort of Australian adolescents revealed that around 25% of the sample exhibited subclinical levels of disordered eating (49). This is notable as subclinical disordered eating within the general population has been shown to have significant negative effects on quality of life (50). No study has yet directly examined if negative affect mediates the influence of alexithymia on disordered within a non-clinical population. However, one study conducted two separate mediation analyses and demonstrated that depression and anxiety mediated the effect of alexithymia on emotional eating. This suggests there is utility in conducting mediation analyses to understand the complex relationships between alexithymia, mood, and eating behaviour in non-clinical samples.
Overview and predictions
The aims of the current study were to (i) confirm findings that disordered eating is positively related to alexithymia (DIF and DDF) in non-clinical participants, and (ii) to examine if depression and/or anxiety would mediate the influence of alexithymia on disordered eating in a non-clinical sample. Participants completed self-report measures of alexithymia (TAS-20), negative affect (depression and anxiety) and disordered eating (drive for thinness, bulimia, and body dissatisfaction). Mediation analyses were conducted to examine the potential role of negative affect in the relationship between alexithymia and disordered eating. The proposed mediation model is presented in Figure 1. Path (a) is the relationship between the predictor alexithymia subscale and the mediators (depression and anxiety). Path (b) is the relationship between the mediators and the dependent variable (disordered eating). The total effect (c) depicts the combined effects of alexithymia and negative affect on disordered eating. The direct effect (c’) illustrates the relationship between alexithymia and disordered eating, after controlling for the mediators (depression and anxiety), whereas the indirect effect (a + b) refers to the relationship between alexithymia and disordered eating via the mediators. Given that drive for thinness, bulimia, and body dissatisfaction are dimensional factors that cut across clinical and non-clinical populations (26, 27), the findings of direct and indirect effects of alexithymia on disordered eating, observed in clinically diagnosed patients (46, 47), were also expected in our non-clinical sample.
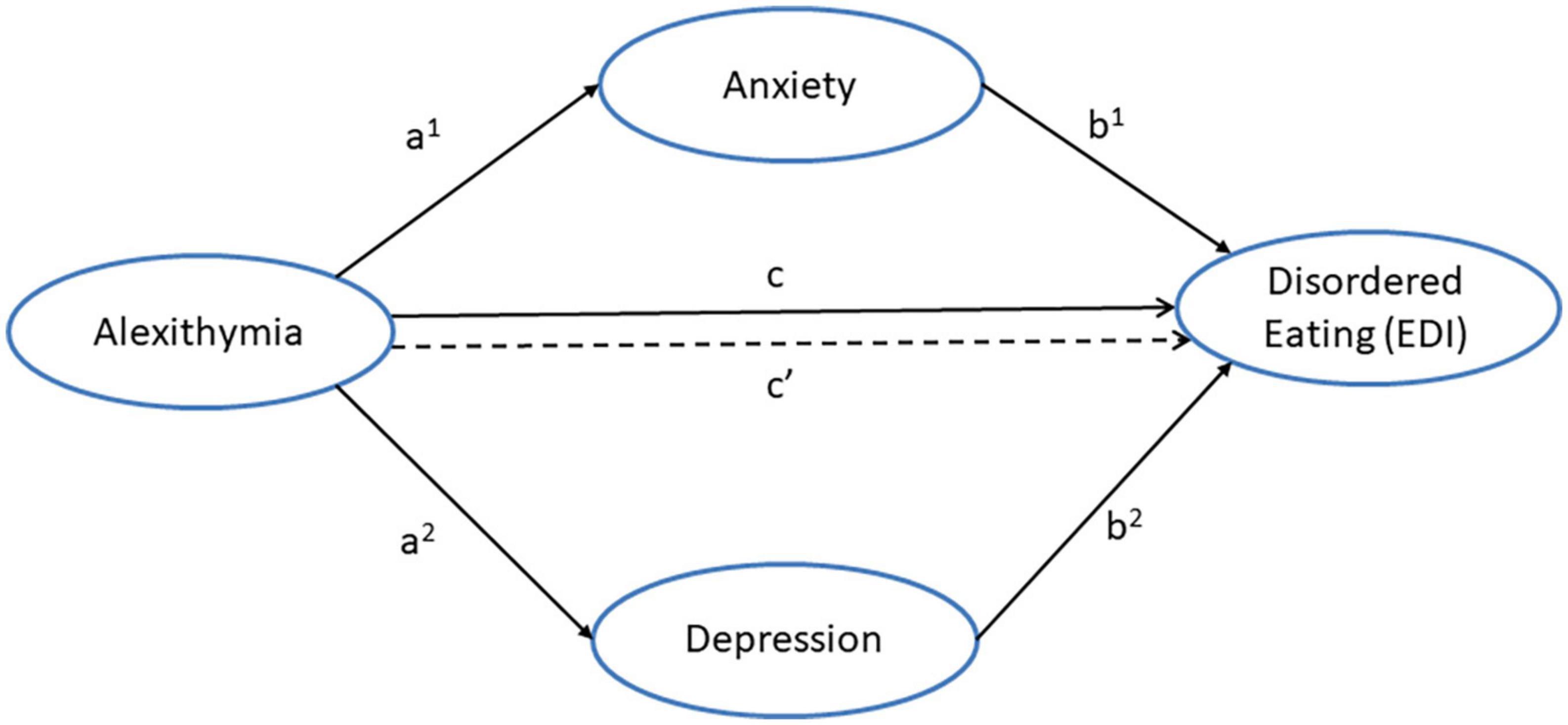
Figure 1. Proposed mediation model illustrating the direct pathway (c’) and indirect pathways between alexithymia and disordered eating via the dual mediators of anxiety (a1 + b1) and depression (a2 + b2).
The predictions for the study are as follows: In line with previous findings (31, 34, 35), it was expected that drive for thinness would be positively related to alexithymia (DIF and DDF). However, given that controlling for negative affect can reduce the strength of the relationship between alexithymia and disordered eating (34), it was expected that depression and anxiety would mediate the relationship between alexithymia (DIF and DDF) and drive for thinness. Nevertheless, evidence that relationships between alexithymia and disordered are evident even after controlling for negative affect (29), suggest that a direct (independent) effect of alexithymia (DIF or DDF) on drive for thinness would still be evident.
In line with prior studies (31–35), it was expected that bulimia would be positively related to alexithymia (DIF and DDF). However, as controlling for negative affect can diminish the relationship between alexithymia and disordered eating (34), it was expected that depression and anxiety would mediate the relationship between DIF (or DDF) and bulimia. Nonetheless, as alexithymia can predict disordered eating independently of negative affect (29, 33), a direct effect of alexithymia (DIF or DDF) on bulimia was expected.
A positive relationship between body dissatisfaction and alexithymia (DIF and DDF) was expected, in line with previous work (29, 34). However, it was predicted that this relationship would be mediated by depression and anxiety, given that controlling for negative affect reduces the strength of relationship between alexithymia and disordered eating (34). Yet, as alexithymia predicts disordered eating, even after controlling for negative mood (29), it was expected that alexithymia (DIF or DDF) would also be an independent predictor of body dissatisfaction.
Materials and methods
Participants
Two-hundred and forty-eight female undergraduate students were recruited from the undergraduate populations of Aston University, Birmingham, UK and De Montfort University, Leicester, UK and took part for course credit. This was an opportunity sample where volunteers responded to electronic adverts on the universities’ research participant schemes. The inclusion criteria were healthy female students aged 18 or above. The exclusion criteria were males, as they differ from females in their expression of disordered eating (51, 52), and a history of depression and/or an eating disorder. The inclusion and exclusion criteria were included in the advert. No screening measure was used to determine clinical history; individuals with a history of depression and/or eating disorders were requested in the advert not to volunteer for the study. Examination of the participant characteristics (see Table 1) would tend to support that the current cohort represents a non-clinical sample. The mean age of the participants was 23.6 (SD = 6.2; range = 18 to 54). The ethnicities of the participants were not recorded, as we had no hypotheses concerning this factor. This sample size was chosen as n≈250 has been shown to result in reliable estimates of relationships between factors (53). It is also notable that the current sample is larger than the cohorts used in the related clinical mediation studies: n = 160 (46) and n = 72 (47). The study was approved by the research ethics committees of both institutions.

Table 1. Participant characteristics: mean values for age, mood, eating behaviour, and alexithymia (standard deviations are presented in parentheses).
Measures
The Toronto Alexithymia Scale [TAS-20; (6) is a 20-item self-report measure assessing three facets of alexithymia: difficulty identifying feelings (DIF; e.g., “I have feelings that I can’t quite identify”), difficulty describing feelings (DDF; e.g., “It is difficult for me to find the right words for my feelings”), and externally oriented thinking (EOT; e.g., “I prefer talking to people about their daily activities rather than their feelings”)]. Participants indicate the extent to which each item describes them using a 5-point Likert scale (1 = strongly disagree, 5 = strongly agree). Scores on the subscales range between 7–35 (DIF), 5–25 (DDF), and 8–40 (EOT) and are summed to give a total TAS-20 score, which ranges between 20 and 100, with higher scores indicating greater alexithymia. The TAS-20 has been shown to be valid (7) and reliable in student samples (54, 55). For example, recent published work by our group reported that scores on all three TAS-20 subscales was good: 0.70 for difficulty identifying feelings, 0.82 for difficulty describing feelings, and 0.71 for externally oriented thinking (56).
The Hospital Anxiety and Depression scale [HADS; (57)] is a 14-item measure of self-reported depression and anxiety. Each item consists of a statement relating to a symptom of depression (e.g., “I feel as if I am slowed down”) or anxiety (e.g., “I feel tense or wound up”) and participants indicate the frequency that they experience that symptom using a 4-point Likert scale. Scores for each item range from 0–3, and for each subscale between 0–21 with higher score equating to greater depression or anxiety. The HADS is a valid and reliable measure of depression and anxiety (58). This measure is also reliable in student samples, for example a recent study demonstrated that that both subscales were reliable: 0.68 for anxiety and 0.77 for depression (59).
The eating- and weight-related subscales from the Eating Disorders Inventory-II [EDI-II; (28)] were used to measure self-reported disordered eating: drive for thinness (DFT; e.g., “I am terrified of gaining weight”), bulimia (BUL; e.g., “I have gone on eating binges where I have felt that I could not stop”), and body-dissatisfaction (BD; e.g., “I think that my stomach is too big”). Participants rate the extent to which each statement is true of them using a 6-point Likert scale (ranging from always to never). All items are scored from 0–3 (from least to most severe disordered eating). Responses indicating the most severe symptoms are scored three, two, and one, respectively, whilst the remaining three responses are scored zero. Scores on the DFT and Bul subscales range between 0 and 21, and scores on the BD subscale range between 0 and 27. These scales have been shown to have good reliability in student samples (54). For example, recent published work by our group reported that the three eating- and weight-related subscales EDI all showed very good reliability: 0.89 for drive for thinness, 0.78 for bulimia, and 0.91 for body dissatisfaction (60).
Procedure
Volunteers attended individual appointments in a private room within the psychology laboratories at the two universities. Having given full written informed consent, participants completed printed copies of the HADS, TAS-20, and EDI-II in a counterbalanced order.
Data analysis
Data were analysed using Jamovi (version 2; The Jamovi Project, 2021). All data were treated as continuous variables. Spearman correlations were used to determine the significance of the associations between variables (as Shapiro-Wilks tests confirmed that none of the factors were normally distributed). Preliminary analysis revealed that difficulty identifying feelings and difficulty describing feelings subscales, but not the externally oriented thinking subscale, of the TAS-20 were correlated with all measures of disordered eating. Furthermore, DIF and DDF were strongly correlated (0.67) with each other, suggesting they were measuring similar constructs. Partial correlations revealed that, after controlling for DDF, DIF was still significantly associated with DFT and bulimia, but not body dissatisfaction. On the other hand, after controlling for DIF, DDF was only significantly correlated with body dissatisfaction and not DFT or bulimia. Therefore, DIF was included as the predictor in the mediation analyses for DFT and bulimia and DDF was included as the predictor in the mediation analysis for body dissatisfaction. Separate mediation analyses were conducted for each of the three eating subscales with depression and anxiety entered as parallel mediators, in line with previous research (47). The jMM module in Jamovi was used to conduct the mediation analyses. This procedure involved bootstrapping (5,000 iterations) to generate bias-corrected 95% confidence intervals (CI) for each effect. This method has been shown to effectively control for Type 1 errors (61).
Results
Participant characteristics
Comparison of the mean EDI scores from the current study (presented in Table 1) with the norms reported in a large non-clinical student sample (62) revealed that our participants scored significantly higher on all EDI subscales: DFT (mean difference = 1.6), t(248) = 4.12, p < 0.001; BUL (mean difference = 0.41), t(248) = 1.94, p = 0.053; and BD (mean difference = 1.29), t(248) = 2.33, p < 0.05. However, importantly, comparison of the current scores with the norms for a clinical sample (63) revealed that the current scores were significantly lower on all subscales of the EDI: DFT (mean difference = −9.1), t(248) = 22.9, p < 0.001; BUL (mean difference = −5.1), t(248) = 22.4, p < 0.001, and BD (mean difference = −7.38), t(248) = 13.3, p < 0.001, which supports the non-clinical status of the current sample.
Comparison of the mean TAS-20 total score with a recent UK student sample (54) revealed that our sample scored significantly higher, mean difference = 6.14, t(247) = 6.32, p < 0.001. However, importantly, the current TAS-20 score is significantly lower (mean difference = −12.2) than that reported in a sample of clinically diagnosed patients with eating disorders (46); t(205) = 12.5, p < 0.001. Comparison of depression and anxiety scores from the current study with a large UK sample of undergraduate students (64) revealed that the current sample was significantly less anxious (mean difference = −1.63) than the previous sample, t(247) = 5.34, p < 0.001. However, the current participants were slightly more depressed (mean difference = 0.73), t(246) = 3.01, p < 0.01. Importantly, in comparison to a clinical sample (65) the participants in the current were significantly less anxious (mean difference = −6.47, t(246) = 21.2; p < 0.001) and depressed (mean difference = −9.5, t(246) = 39.4, p < 0.001. Taken together the pattern is consistent with our conception of the current sample as non-clinical.
Relationships between age, mood, alexithymia, and disordered eating
Correlational analyses (see Table 2) using Spearman’s tests revealed that disordered eating (drive for thinness, bulimia, and body dissatisfaction) was significantly positively related to alexithymia (DDF and DIF subscale scores, but not EOT) and mood (depression and anxiety). There were also significant associations between alexithymia and mood. It is notable that age was significantly related to alexithymia, disordered eating, and mood1. As observed relationships were based on Spearman correlations the mediational analyses were conducted using the ranked data.
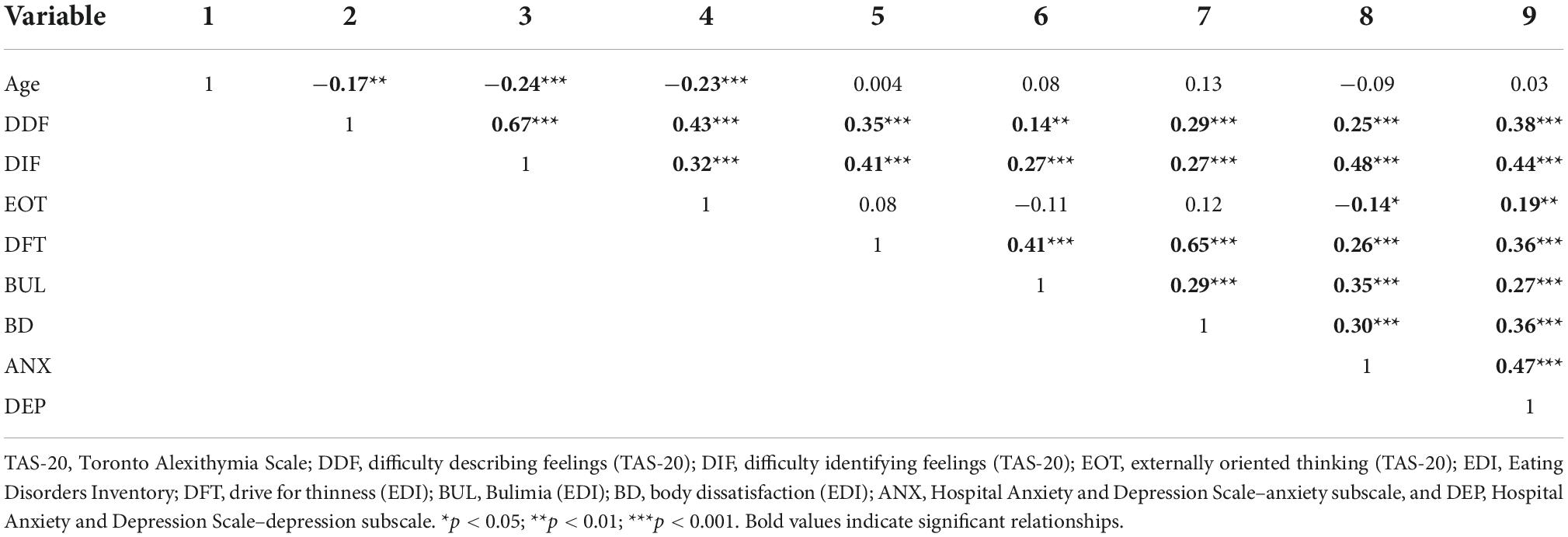
Table 2. Spearman correlation coefficients for the relationships between age, mood, alexithymia, and eating behaviour.
The influence of alexithymia (DIF) and negative affect (depression and anxiety) on drive for thinness
A regression was conducted with difficulty identifying feelings as the predictor variable, drive for thinness as the dependent variable, and anxiety and depression as parallel mediators. The paths of this model are illustrated in Figure 2 and the coefficients and 95% CI from this analysis are presented in Table 3.
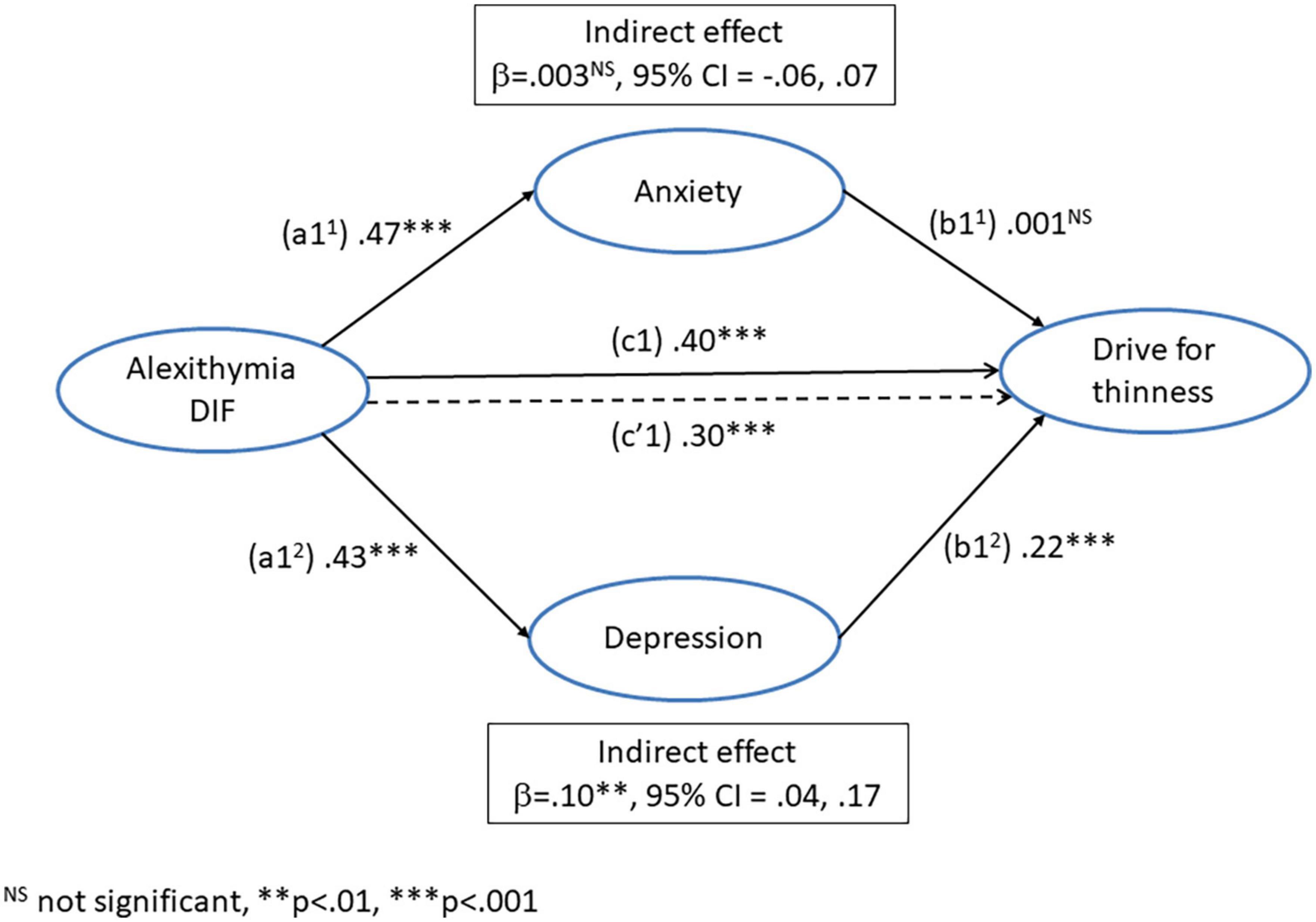
Figure 2. Mediation model for the direct (c1’) and indirect pathways between alexithymia (difficulty identifying feelings) and drive for thinness via the dual mediators of anxiety (a11 + b11) and depression (a12 + b12).

Table 3. Path coefficients and 95% confidence intervals (estimated using bias corrected bootstrapping) for the mediation analyses of difficulty identifying feelings (DIF) on drive for thinness via the parallel mediators of depression and anxiety.
The path (a11) from DIF to anxiety was significant, as was the path (a12) from DIF to depression. The path (b11) from anxiety to drive for thinness was not significant, but the path (b12) from depression to drive for thinness was significant. The total effect of DIF on drive for thinness (c1) was significant, as was the direct effect (c’1), controlling for the influence of depression and anxiety. The indirect effect of DIF on drive for thinness (a11 + b11) via anxiety was not significant. However, the indirect effect via depression (a12 + b12) was significant. This suggests that the influence of DIF on drive for thinness was mediated by depression but not anxiety. However, even after controlling for negative affect, DIF remained an independent predictor of drive for thinness.
The influence of alexithymia (DIF) and negative affect (depression and anxiety) on bulimia
A regression was conducted with difficulty identifying feelings as the predictor variable, bulimia as the dependent variable, and anxiety and depression as parallel mediators. The paths of this model are illustrated in Figure 3 and the coefficients and 95% CI from this analysis are presented in Table 4.
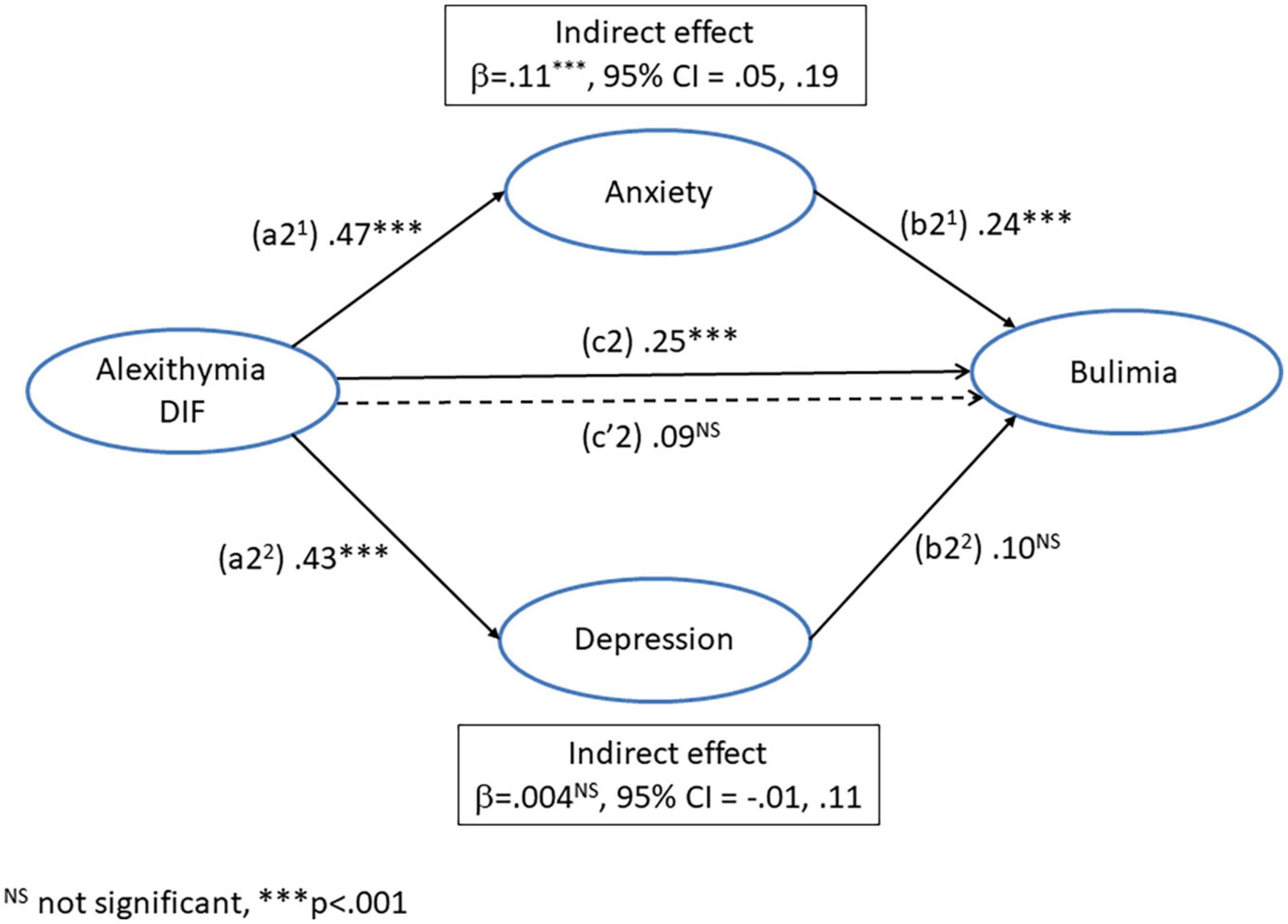
Figure 3. Mediation model for the direct (c2’) and indirect pathways between alexithymia (difficulty identifying feelings) and bulimia via the dual mediators of anxiety (a21 + b21) and depression (a22 + b22).
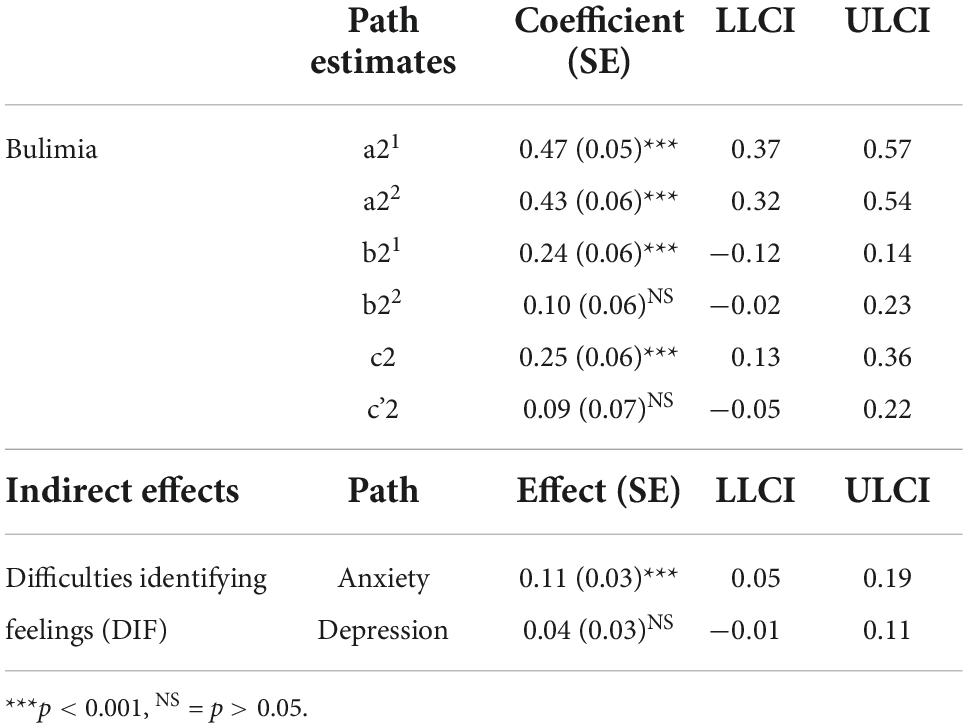
Table 4. Path coefficients and 95% confidence intervals (estimated using bias corrected bootstrapping) for the mediation analyses of difficulty identifying feelings (DIF) on bulimia via the parallel mediators of depression and anxiety.
The path (a21) from DIF to anxiety was significant, as was the path (a22) from DIF to depression. The path (b21) from anxiety to bulimia was significant, but the path (b22) from depression to bulimia was not significant. The total effect of DIF on bulimia (c2) was significant, but the direct effect (c’2) was no longer significant, after controlling for the influence of depression and anxiety. The indirect effect of DIF on bulimia (a21 + b21) via the mediator (anxiety) was significant. However, the indirect effect via depression (a22 + b22) was not significant. This suggests that the influence of DIF on bulimia was mediated by anxiety but not depression. Furthermore, after controlling for negative affect DIF no longer directly predicted bulimia.
The influence of alexithymia (DDF) and negative affect (depression and anxiety) on body dissatisfaction
A regression was conducted with difficulty describing feelings as the predictor variable, body dissatisfaction as the dependent variable, and anxiety and depression as parallel mediators. The paths of this model are illustrated in Figure 4 and the coefficients and 95% CI from this analysis are presented in Table 5.
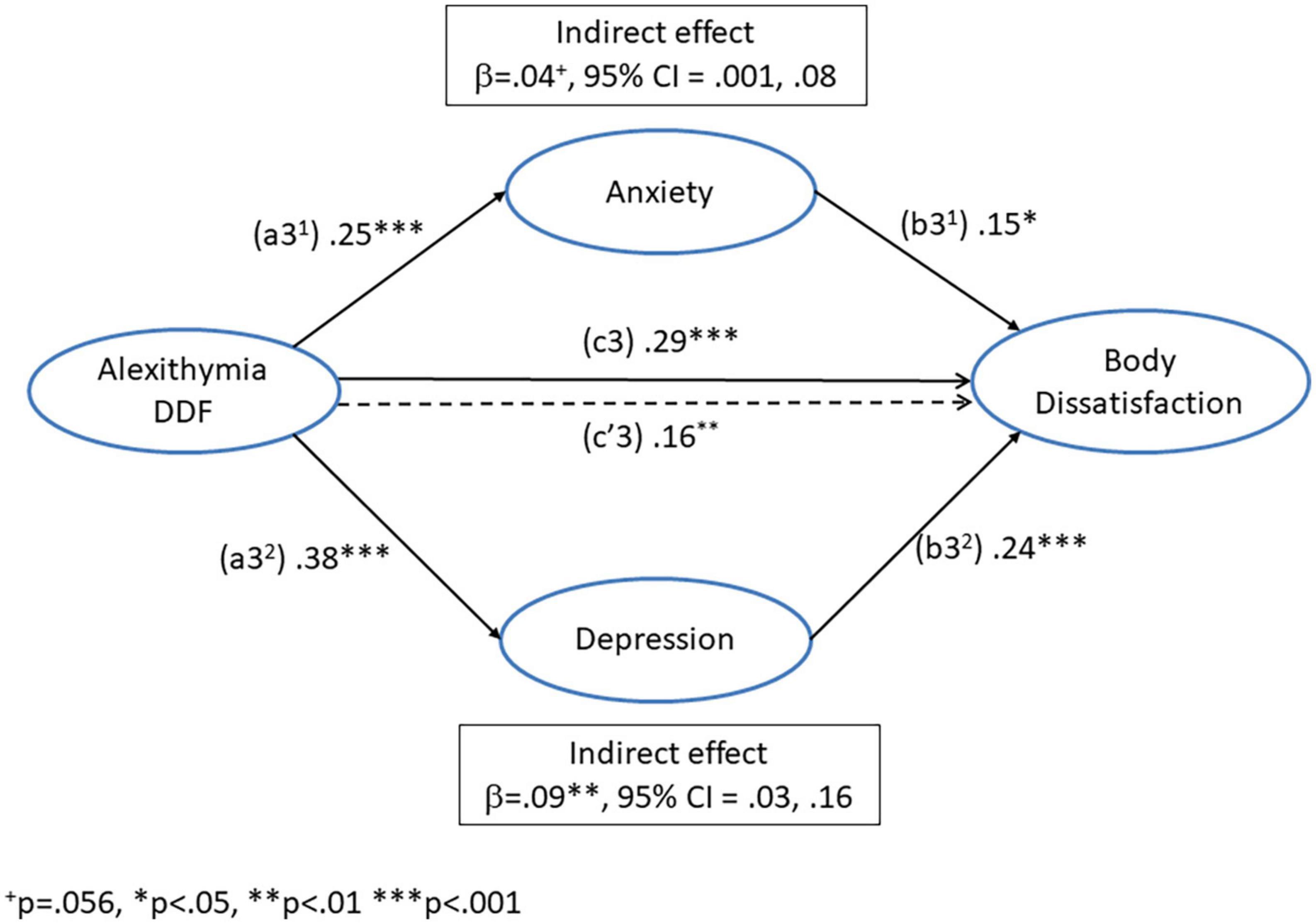
Figure 4. Mediation model for the direct (c3’) and indirect pathways between alexithymia (difficulty describing feelings) and body dissatisfaction via the dual mediators of anxiety (a31 + b31) and depression (a32 + b32).
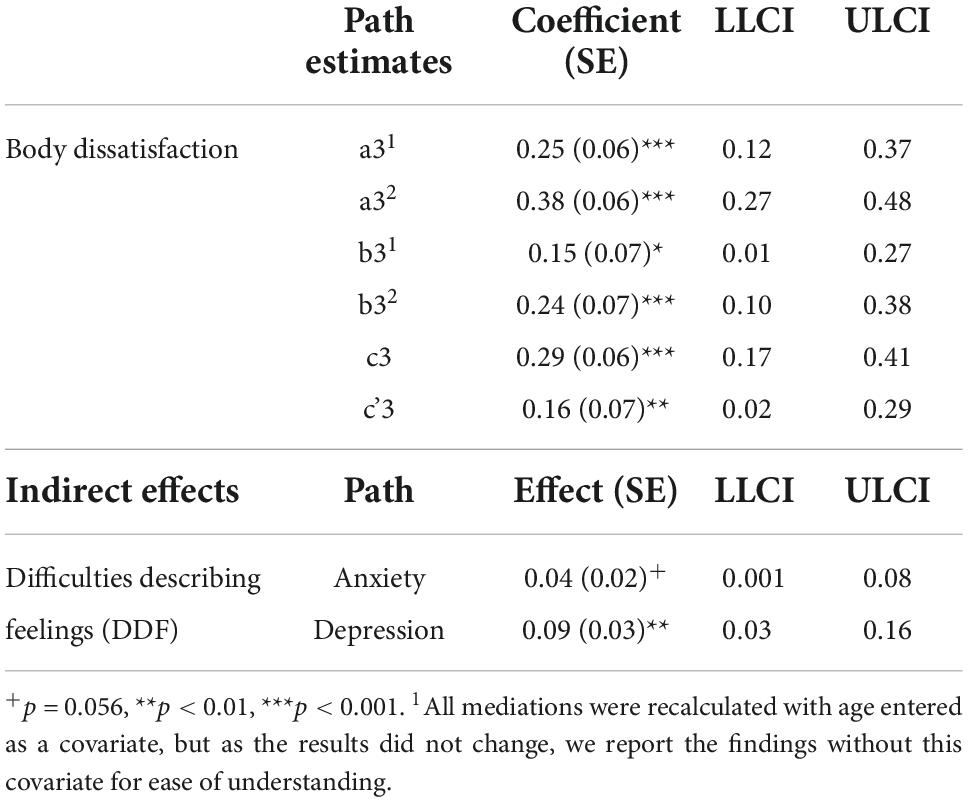
Table 5. Path coefficients and 95% confidence intervals (estimated using bias corrected bootstrapping) for the mediation analyses of difficulty describing feelings (DDF) on body dissatisfaction via the parallel mediators of depression and anxiety.
The path (a31) from DDF to anxiety was significant, as was the path (a32) from DDF to depression. The path (b31) from anxiety to body dissatisfaction was significant, as was the path (b32) from depression to body dissatisfaction. The total effect of DDF on body dissatisfaction (c3) was significant, as was the direct effect (c’3), after controlling for the influence of depression and anxiety. The indirect effect via depression (a32 + b32) was significant. However, the indirect effect of DDF on body dissatisfaction (a31 + b31) via anxiety was only trend significant (p = 0.056). This suggests that the influence of DDF on body dissatisfaction was mediated by depression and to some extent anxiety. Furthermore, after controlling for negative affect, DDF remained an independent predictor of body dissatisfaction.
Discussion
The aims of the current study were to (i) confirm findings that disordered eating is positively related to alexithymia (DIF and DDF) in healthy participants, and (ii) to examine if depression and/or anxiety would mediate the influence of alexithymia on disordered eating in a non-clinical sample. The expectation that DIF and DDF would be positively related to drive for thinness (DFT) was supported by the current findings. This is consistent with previous studies (31, 33, 35). The prediction that depression and anxiety would mediate the influence of alexithymia on drive for thinness was partially supported, as depression but not anxiety mediated the link between DIF and DFT. As expected, DIF remained as an independent predictor of drive for thinness, after controlling for negative affect. This is consistent with previous work in healthy participants (29). The findings in our non-clinical sample of direct and indirect effects of alexithymia on eating behaviour (drive for thinness) via depression corresponds with evidence from clinical samples (46, 47).
The prediction that DIF and DDF would be positively correlated with bulimia was supported by the current findings. This is consistent with previous studies (31–35). The expectation that depression and anxiety would mediate the influence of alexithymia on bulimia was partially supported, as anxiety but not depression mediated the influence of DIF on bulimia. The prediction that DIF would be an independent predictor of bulimia, after depression and anxiety had been controlled, was also not supported. This is consistent with previous findings that negative affect accounted for the relationship between alexithymia and bulimia (34). However, it does not correspond with evidence that alexithymia is an independent predictor of bulimia (33). The current evidence that anxiety mediated the relationship between DIF and bulimia is consistent with previous work in clinical patients (47), but the finding that depression did not mediate this relationship does not correspond with the results of that study.
The prediction that body dissatisfaction would be positively related to DIF and DDF was supported by the current findings. This is consistent with the evidence from previous studies (29, 34). The expectation that the link between alexithymia and body dissatisfaction would be mediated by depression and anxiety was supported by the current findings, although the mediation by anxiety was only trend significant (p = 0.056). This is consistent with evidence that negative affect accounts for the relationship between alexithymia and disordered eating (34) and with studies in clinical participants (46, 47). Furthermore, the prediction that alexithymia (DDF) would remain as an independent predictor of body dissatisfaction after controlling for the influence of negative affect was supported by the current data. This is consistent with evidence that alexithymia is an independent predictor of disordered eating, after controlling for negative affect (29) and with the findings in clinical samples (46, 47).
Alexithymia is considered a relatively stable trait (24, 25) that is a risk factor for depression (21, 22) and anxiety (23), which in turn are risk factors for disordered eating (41, 43, 44). Thus, one explanation for the current findings is that alexithymia led to increases in negative affect, which then led to disordered eating. Consistent with this line of thought, the proposed explanation for a previous finding that negative affect mediated the influence of interpersonal problems on binge eating, was that interpersonal problems led to higher negative affect, which in turn led to increased tendency to binge eating (66). Longitudinal research is required to confirm the direction of this predictive model.
There are a number of limitations to the current study that need to be considered. Firstly, we did not conduct reliability analyses on the questionnaire data. However, these measures have been shown to be reliable in previous student samples, including in studies published by our group (56, 59, 60). Some of the current findings, i.e., the mediation of drive for thinness by anxiety and the mediation of bulimia by depression were very small effects. Although our sample (n = 248) was larger than the cohorts used in related the clinical mediation studies (46, 47) and similar sample sizes have been shown to lead to stable correlations (53), our study was not powered to detect these very small effects. Nevertheless, a posteriori power analysis based on published sample sizes required for mediation (67) confirm that our study was powered to detect small to medium effect sizes, thus the remaining findings were sufficiently powered. Another issue to consider is the measure of alexithymia that was used in the current study. In line with previous clinical mediation studies (46, 47) we used the TAS-20 to measure alexithymia, thus the findings might not generalise to other measures of alexithymia [e.g., Bermond–Vorst Alexithymia Questionnaire; BVAQ; (68)]. Nevertheless, scores on these measures tend to be significantly correlated. For example, it has been reported (69) that total TAS-20 and BVAQ scores were positively related (r = 0.62), with the subscales measuring difficulty identifying and describing feelings correlating even more strongly (r = 0.7 and r = 0.8, respectively). This suggests that similar findings would have been observed had the BVAQ been used in place of the TAS-20. However, it is notable that self-report measures of emotion processing deficits like the TAS-20 and BVAQ do not always correlate with implicit measures of emotion processing. For example, a recent study showed that participants with obesity reported similar levels of alexithymia to normal weight controls, but demonstrated deficits on an implicit emotion processing task (70). With this in mind, incorporating implicit measures of emotional awareness into future studies as well as self-report questionnaires might improve the predictive power of the model relating alexithymia, negative affect, and disordered eating. Finally, it is notable that the current sample consisted of females only. Future work is needed to examine if alexithymia predicts disordered eating in males and if this relationship is mediated by negative affect.
In sum, the findings of the current study confirmed that depression mediated the influence of alexithymia on drive for thinness and body dissatisfaction but not bulimia. On the other hand, anxiety mediated the influence of alexithymia on bulimia and body dissatisfaction, but not drive for thinness. It is possible that depression might mediate bulimia and anxiety drive for thinness, but the size of these mediation effects was too small to be detected by the current sample. Although negative affect mediated the influence of alexithymia on all measures of disordered eating, alexithymia (DIF and DDF, respectively) was still an independent predictor of drive for thinness and body dissatisfaction. One implication of our work is that future studies examining the potential roles of alexithymia and negative affect in the development of disordered eating should aim for larger sample sizes (n≈400) to ensure that they are also powered to detect very small effects. Another implication is that the influence of alexithymia on disordered eating (at least drive for thinness and body dissatisfaction) cannot be entirely explained by negative affect. The current findings are cross-sectional and correlational and, thus, cannot provide evidence of the direction of causation. However, as alexithymia is considered to be a relatively stable trait that is a risk factor for disordered eating (15, 16), targeted interventions to address deficits in recognising and describing ones feelings could potentially be beneficial for individuals who are “at risk” of developing eating disorders. This is potentially important, as early intervention has been shown to be the key in treating and preventing eating disorders (71).
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: The data is available via Mendeley data DOI: 10.17632/tfbh8vsrkz.3.
Ethics statement
The studies involving human participants were reviewed and approved by the Research Ethics Committees of both Aston University and De Montfort University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
NR and DW designed and supervised the study and wrote the manuscript. Data was collected by undergraduate research assistants. NR analysed the data. Both authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Oldershaw A, Lavender T, Sallis H, Stahl D, Schmidt U. Emotion generation and regulation in anorexia nervosa: a systematic review and meta-analysis of self-report data. Clin Psychol Rev. (2015) 39:83–95. doi: 10.1016/j.cpr.2015.04.005
2. Harrison A, Sullivan S, Tchanturia K, Treasure J. Emotional functioning in eating disorders: attentional bias, emotion recognition and emotion regulation. Psychol Med. (2010) 40:1887–97. doi: 10.1017/S0033291710000036
3. Dingemans A, Danner U, Parks M. Emotion regulation in binge eating disorder: a review. Nutrients. (2017) 9:1274. doi: 10.3390/nu9111274
4. Morie KP, Ridout N. Alexithymia and Maladaptive Regulatory Behaviors in Substance Use Disorders and Eating Disorders. Cambridge: Cambridge University Press (2018).
5. Taylor GJ, Bagby RM. An overview of the alexithymia construct. In: Bar-On R, Parker JDA, editors. The Handbook Of Emotional Intelligence: Theory, Development, Assessment, and Application at Home, School, and in the Workplace. San Francisco, CA: Jossey-Bass (2000). p. 40–67.
6. Bagby RM, Parker JD, Taylor GJ. The twenty-item toronto alexithymia scale—I. Item selection and cross-validation of the factor structure. J Psychosom Res. (1994) 38:23–32. doi: 10.1016/0022-3999(94)90005-1
7. Bagby RM, Taylor GJ, Parker JD. The twenty-item toronto alexithymia scale—II. Convergent, discriminant, and concurrent validity. J Psychosom Res. (1994) 38:33–40. doi: 10.1016/0022-3999(94)90006-X
8. Abbate-Daga G, Quaranta M, Marzola E, Amianto F, Fassino S. The relationship between alexithymia and intolerance of uncertainty in anorexia nervosa. Psychopathology. (2015) 48:202–8. doi: 10.1159/000381587
9. Eizaguirre AE, de Cabezón AOS, de Alda IO, Olariaga LSJ, Juaniz M. Alexithymia and its relationships with anxiety and depression in eating disorders. Pers Individ Differ. (2004) 36:321–31. doi: 10.1016/S0191-8869(03)00099-0
10. Beales DL, Dolton R. Eating disordered patients: personality, alexithymia, and implications for primary care. Br J Gen Pract. (2000) 50:21–6.
11. Speranza M, Corcos M, Loas G, Stéphan P, Guilbaud O, Perez-Diaz F, et al. Depressive personality dimensions and alexithymia in eating disorders. Psychiatry Res. (2005) 135:153–63. doi: 10.1016/j.psychres.2005.04.001
12. Carano A, De Berardis D, Campanella D, Serroni N, Ferri F, Di Iorio G, et al. Alexithymia and suicide ideation in a sample of patients with binge eating disorder. J Psychiatr Pract. (2012) 18:5–11. doi: 10.1097/01.pra.0000410982.08229.99
13. Pinaquy S, Chabrol H, Simon C, Louvet JP, Barbe P. Emotional eating, alexithymia, and binge-eating disorder in obese women. Obesity Res. (2003) 11:195–201. doi: 10.1038/oby.2003.31
14. Westwood H, Kerr-Gaffney J, Stahl D, Tchanturia K. Alexithymia in eating disorders: Systematic review and meta-analyses of studies using the toronto alexithymia scale. J Psychosom Res. (2017) 99:66–81. doi: 10.1016/j.jpsychores.2017.06.007
15. Courty A, Godart N, Lalanne C, Berthoz S. Alexithymia, a compounding factor for eating and social avoidance symptoms in anorexia nervosa. Compr Psychiatry. (2015) 56:217–28. doi: 10.1016/j.comppsych.2014.09.011
16. Tchanturia K, Davies H, Harrison A, Fox JRE, Treasure J, Schmidt U. Altered social hedonic processing in eating disorders. Int J Eat Disord. (2012) 45:962–9. doi: 10.1002/eat.22032
17. Speranza M, Loas G, Wallier J, Corcos M. Predictive value of alexithymia in patients with eating disorders: a 3-year prospective study. J Psycho Res. (2007) 63:365–71. doi: 10.1016/j.jpsychores.2007.03.008
18. Iancu I, Cohen E, Yehuda YB, Kotler M. Treatment of eating disorders improves eating symptoms but not alexithymia and dissociation proneness. Compr Psychiatry. (2006) 47:189–93. doi: 10.1016/j.comppsych.2006.01.001
19. Ohmann S, Popow C, Wurzer M, Karwautz A, Sackl-Pammer P, Schuch B. Emotional aspects of anorexia nervosa: results of prospective naturalistic cognitive behavioral group therapy. Neuropsychiatr. (2013) 27:119–28. doi: 10.1007/s40211-013-0065-7
20. Storch M, Keller F, Weber J, Spindler A, Milos G. Psychoeducation in affect regulation for patients with eating disorders: a randomized controlled feasibility study. Am J Psychother. (2011) 65:81–93. doi: 10.1176/appi.psychotherapy.2011.65.1.81
21. Günther V, Rufer M, Kersting A, Suslow T. Predicting symptoms in major depression after inpatient treatment: the role of alexithymia. Nord J Psychiatry. (2016) 70:392–8. doi: 10.3109/08039488.2016.1146796
22. Luminet O, Bagby RM, Taylor GJ. An evaluation of the absolute and relative stability of alexithymia in patients with major depression. Psychother Psychosom. (2001) 70:254–60. doi: 10.1159/000056263
23. De Berardis DD, Campanella D, Nicola S, Gianna S, Alessandro C, Chiara C, et al. The impact of alexithymia on anxiety disorders: a review of the literature. Curr Psychiatry Rev. (2008) 4:80–6. doi: 10.2174/157340008784529287
24. Salminen J, Saarijärvi S, Toikka T, Kauhanen J, Äärelä E. Alexithymia behaves as a personality trait over a 5-year period in Finnish general population. J Psychosom Res. (2006) 61:275–8. doi: 10.1016/j.jpsychores.2006.01.014
25. Tolmunen T, Heliste M, Lehto SM, Hintikka J, Honkalampi K, Kauhanen J. Stability of alexithymia in the general population: an 11-year follow-up. Comprehens Psychiatry. (2011) 52:536–41. doi: 10.1016/j.comppsych.2010.09.007
26. Holm-Denoma JM, Richey JA, Joiner TE. The latent structure of dietary restraint, body dissatisfaction, and drive for thinness: a series of taxometric analyses. Psychol Assess. (2010) 22:788. doi: 10.1037/a0020132
27. Saules KK, Collings AS, Hoodin F, Angelella NE, Alschuler K, Ivezaj V, et al. The contributions of weight problem perception, BMI, gender, mood, and smoking status to binge eating among college students. Eat Behav. (2009) 10:1–9. doi: 10.1016/j.eatbeh.2008.07.010
28. Garner DM. Eating Disorder Inventory-2; Pro-fessional Manual. Odessa: Psychological Assessment Resources (1991).
29. De Berardis D, Serroni N, Campanella D, Carano A, Gambi F, Valchera A, et al. Alexithymia and its relationships with dissociative experiences, body dissatisfaction and eating disturbances in a non-clinical female sample. Cogn Ther Res. (2009) 33:471–9. doi: 10.1007/s10608-009-9247-9
30. Garner DM, Garfinkel PE. The eating attitudes test: an index of the symptoms of anorexia nervosa. Psychol Med. (1979) 9:273–9. doi: 10.1017/S0033291700030762
31. Zerach GJ. The associations between pathological narcissism, alexithymia and disordered eating attitudes among participants of pro-anorexic online communities. Eat Weight Disord. (2014) 19:337–45. doi: 10.1007/s40519-013-0096-x
32. Sasai K, Tanaka K, Hishimoto A. Alexithymia and its relationships with eating behavior, self esteem, and body esteem in college women. Kobe J Med Sci. (2010) 56:E231–8.
33. Markey MA, Vander Wal JS. The role of emotional intelligence and negative affect in bulimic symptomatology. Compr Psychiatry. (2007) 48:458–64. doi: 10.1016/j.comppsych.2007.05.006
34. Hund AR, Espelage DL. Childhood emotional abuse and disordered eating among undergraduate females: mediating influence of alexithymia and distress. Child Abuse Negl. (2006) 30:393–407. doi: 10.1016/j.chiabu.2005.11.003
35. Kiyotaki Y, Yokoyama K. Relationships of eating disturbances to alexithymia, need for social approval, and gender identity among Japanese female undergraduate students. Pers Individ Differ. (2006) 41:609–18. doi: 10.1016/j.paid.2006.02.013
36. Quinton S, Wagner HL. Alexithymia, ambivalence over emotional expression, and eating attitudes. Pers Individ Differ. (2005) 38:1163–73. doi: 10.1016/j.paid.2004.07.013
37. Conrad R, Wegener I, Imbierowicz K, Liedtke R, Geiser F. Alexithymia, temperament and character as predictors of psychopathology in patients with major depression. Psychiatry Res. (2009) 165:137–44. doi: 10.1016/j.psychres.2007.10.013
38. Honkalampi K, De Berardis D, Vellante F, Viinamäki H. Relations Between Alexithymia and Depressive and Anxiety Disorders and Personality. Cambridge: Cambridge University Press (2018).
39. Honkalampi K, Hintikka J, Tanskanen A, Lehtonen J, Viinamäki H. Depression is strongly associated with alexithymia in the general population. J Psychosom Res. (2000) 48:99–104. doi: 10.1016/S0022-3999(99)00083-5
40. Leweke F, Leichsenring F, Kruse J, Hermes S. Is alexithymia associated with specific mental disorders. Psychopathology. (2012) 45:22–8. doi: 10.1159/000325170
41. Jacobi C, Fittig E, Bryson S, Wilfley D, Kraemer H, Taylor CB. Who is really at risk? Identifying risk factors for subthreshold and full syndrome eating disorders in a high-risk sample. Psychol Med. (2011) 41:1939–49. doi: 10.1017/S0033291710002631
42. Smith KE, Mason TB, Leonard RC, Wetterneck CT, Smith BER, Farrell NR, et al. Affective predictors of the severity and change in eating psychopathology in residential eating disorder treatment: the role of social anxiety. Eat Disord. (2018) 26:66–78. doi: 10.1080/10640266.2018.1418314
43. Stice E, Gau JM, Rohde P, Shaw H. Risk factors that predict future onset of each DSM-5 eating disorder: predictive specificity in high-risk adolescent females. J Abnorm Psychol. (2017) 126:38–51. doi: 10.1037/abn0000219
44. Stice E, Marti CN, Durant S. Risk factors for onset of eating disorders: evidence of multiple risk pathways from an 8-year prospective study. Behav Res Ther. (2011) 49:622–7. doi: 10.1016/j.brat.2011.06.009
45. Strober M. Pathologic fear conditioning and anorexia nervosa: on the search for novel paradigms. Int J Eat Disord. (2004) 35:504–8. doi: 10.1002/eat.20029
46. Torres S, Guerra MP, Lencastre L, Miller K, Vieira FM, Roma-Torres A, et al. Alexithymia in anorexia nervosa: the mediating role of depression. Psychiatry Res. (2015) 225:99–107. doi: 10.1016/j.psychres.2014.10.023
47. Khosravi M. Eating disorders among patients with borderline personality disorder: understanding the prevalence and psychopathology. J Eat Disord. (2020) 8:38. doi: 10.1186/s40337-020-00314-3
48. Stice E, Marti CN, Shaw H, Jaconis M. An 8-year longitudinal study of the natural history of threshold, subthreshold, and partial eating disorders from a community sample of adolescents. J Abnorm Psychol. (2009) 118:587. doi: 10.1037/a0016481
49. Sparti C, Santomauro D, Cruwys T, Burgess P, Harris M. Disordered eating among Australian adolescents: prevalence, functioning, and help received. Int J Eat Disord. (2019) 52:246–54. doi: 10.1002/eat.23032
50. Wade TD, Wilksch SM, Lee C. A longitudinal investigation of the impact of disordered eating on young women’s quality of life. Health Psychol. (2012) 31:352–9. doi: 10.1037/a0025956
51. Culbert KM, Breedlove SM, Sisk CL, Burt SA, Klump KL. The emergence of sex differences in risk for disordered eating attitudes during puberty: a role for prenatal testosterone exposure. J Abnorm Psychol. (2013) 122:420–32. doi: 10.1037/a0031791
52. McCabe MP, Vincent MA. The role of biodevelopmental and psychological factors in disordered eating among adolescent males and females. Eur Eat Disord Rev. (2003) 11:315–28. doi: 10.1002/erv.500
53. Schönbrodt FD, Perugini M. At what sample size do correlations stabilize? J Res Pers. (2013) 47:609–12. doi: 10.1016/j.jrp.2013.05.009
54. Pink AE, Lee M, Price M, Williams C. A serial mediation model of the relationship between alexithymia and BMI: the role of negative affect, negative urgency and emotional eating. Appetite. (2019) 133:270–8. doi: 10.1016/j.appet.2018.11.014
55. Sharpe E, Wallis DJ, Ridout N. The influence of variations in eating disorder-related symptoms on processing of emotional faces in a non-clinical female sample: an eye-tracking study. Psychiatry Res. (2016) 240:321–7. doi: 10.1016/j.psychres.2016.04.065
56. Wallis DJ, Ridout N, Sharpe E. The influence of non-clinical eating-related psychopathology on the recognition of emotion from static faces and realistic social interactions. Eat Behav. (2018) 29:19–24. doi: 10.1016/j.eatbeh.2018.01.004
57. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. (1983) 67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x
58. Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the hospital anxiety and depression scale: an updated literature review. J Psychosom Res. (2002) 52:69–77. doi: 10.1016/S0022-3999(01)00296-3
59. McCloud T, Jones R, Lewis G, Bell V, Tsakanikos E. Effectiveness of a mobile app intervention for anxiety and depression symptoms in university students: randomized controlled trial. JMIR Mhealth Uhealth. (2020) 8:e15418. doi: 10.2196/15418
60. Mang L, Ridout N, Dritschel B. The influence of mood and attitudes towards eating on cognitive and autobiographical memory flexibility in female university students. Psychiatry Res. (2018) 269:444–9. doi: 10.1016/j.psychres.2018.08.055
61. Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. (2008) 40:879–91. doi: 10.3758/BRM.40.3.879
62. Limbert C. The eating disorder inventory: a test of the factor structure and internal consistency in a nonclinical sample. Health Care Women Int. (2004) 25:165–78. doi: 10.1080/07399330490267486
63. Brewin N, Baggott J, Dugard P, Arcelus J. Clinical normative data for eating disorder examination questionnaire and eating disorder inventory for DSM-5 feeding and eating disorder classifications: a retrospective study of patients formerly diagnosed via DSM-IV. Eur Eat Disord Rev. (2014) 22:299–305. doi: 10.1002/erv.2301
64. Andrews B, Wilding JM. The relation of depression and anxiety to life-stress and achievement in students. Br J Psychol. (2004) 95:509–21. doi: 10.1348/0007126042369802
65. Ridout N, Dritschel B, Matthews K, O’Carroll R. Autobiographical memory specificity in response to verbal and pictorial cues in clinical depression. J Behav Ther Exp Psychiatry. (2016) 51:109–15. doi: 10.1016/j.jbtep.2016.01.002
66. Ivanova IV, Tasca GA, Hammond N, Balfour L, Ritchie K, Koszycki D, et al. Negative affect mediates the relationship between interpersonal problems and binge-eating disorder symptoms and psychopathology in a clinical sample: a test of the interpersonal model. Eur Eat Disord Rev. (2015) 23:133–8. doi: 10.1002/erv.2344
67. Fritz MS, MacKinnon DP. Required sample size to detect the mediated effect. Psychol Sci. (2007) 18:233–9. doi: 10.1111/j.1467-9280.2007.01882.x
68. Vorst HCM, Bermond B. Validity and reliability of the bermond–vorst alexithymia questionnaire. Pers Individ Differ. (2001) 30:413–34. doi: 10.1016/S0191-8869(00)00033-7
69. Zech E, Luminet O, Rimé B, Wagner H. Alexithymia and its measurement: confirmatory factor analyses of the 20-item toronto alexithymia scale and the bermond–vorst alexithymia questionnaire. Eur J Pers. (1999) 13:511–32. doi: 10.1002/(SICI)1099-0984(199911/12)13:6<511::AID-PER347>3.0.CO;2-0
70. Scarpina F, Varallo G, Castelnuovo G, Capodaglio P, Molinari E, Mauro A, et al. Implicit facial emotion recognition of fear and anger in obesity. Eat Weight Disord. (2021) 26:1243–51. doi: 10.1007/s40519-020-01010-6
Keywords: emotional awareness, affect, eating disorders, depression, anxiety, mediation
Citation: Wallis DJ and Ridout N (2022) Direct and indirect effects of alexithymia on disordered eating in a non-clinical female sample: Determining the role of negative affect. Front. Psychiatry 13:994024. doi: 10.3389/fpsyt.2022.994024
Received: 14 July 2022; Accepted: 03 November 2022;
Published: 24 November 2022.
Edited by:
Kristen Paula Morie, Yale University, United StatesReviewed by:
Mohsen Khosravi, Zahedan University of Medical Sciences, IranGiorgia Varallo, University of Parma, Italy
Copyright © 2022 Wallis and Ridout. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nathan Ridout, bi5yaWRvdXRAYXN0b24uYWMudWs=
†Present address: Deborah J. Wallis, Department of Psychology, School of Social Sciences, Birmingham City University, Birmingham, United Kingdom
 Deborah J. Wallis
Deborah J. Wallis Nathan Ridout
Nathan Ridout