- 1Clinical Nursing Teaching and Research Section, The Second Xiangya Hospital, Central South University, Changsha, China
- 2School of Public Health, Kunming Medical University, Kunming, China
- 3School of Psychology, The University of Queensland, St Lucia, QLD, Australia
- 4School of Nursing, Jinan University, Guangzhou, China
- 5Office of the President, Central South University, Changsha, China
Type 1 diabetes and neurodevelopmental disorders are common chronic conditions in childhood and adolescence, and having one may lead to an increased chance of developing the other. Type 1 diabetes mellitus is mainly manifested by elevated blood glucose, while neurodevelopmental diseases are composed of a variety of diseases, which are relatively complex. The purpose of this meta-analysis was to find out the prevalence of type 1 diabetes-related neurodevelopmental disorders in children and adolescents and to explore the potential association between neurodevelopmental disorders and type 1 diabetes. PubMed, Embase and Web of science databases were searched from the inception to May 22, 2022 to identify relevant studies, Finally, 24 original studies were included in the meta-analysis. Prevalence estimates for neurodevelopmental disorders in the type 1 diabetes adolescent and their 95% confidence intervals were pooled using random effects models. The pooled estimates for autism spectrum disorders (ASD) and attention deficit hyperactivity disorder (ADHD) in the type 1 diabetes population were 1.2 and 5.3%, respectively, both of which are higher than the 2019 global prevalence of ASD and ADHD in the general population. The results of the subgroup analysis showed that the prevalence of ASD and ADHD in the T1DM population tended to increase with age. In conclusion, there may be a potential link between the occurrence of type 1 diabetes mellitus and the development of neurodevelopmental disorders in children and adolescents, but more relevant studies are needed to understand the link between the underlying pathogenesis of type 1 diabetes and neurodevelopmental disorders.
Systematic review registration: [https://www.crd.york.ac.uk/PROSPERO/], identifier [CDR42022333443].
Introduction
Neurodevelopmental disorders (NDDs) are a group of complex disorders that are not easily conceptualized. In the DSM-5, NDDs are defined as a group of disorders that occur during development, including autism spectrum disorders (ASD), attention deficit hyperactivity disorder (ADHD), intellectual disability (ID), communication disorders (CD), specific learning disabilities (SLD), and motor disorders (MDs) (1, 2). They are characterized by childhood onset with delays in developmental domains such as cognition, executive functioning, language/communication, social functioning, and adaptive behavior (3), besides, people with ASD also have social and interaction difficulties (4). There are gender differences in the onset of NDDs. The diagnosis rate of males is higher than that of females, and the onset risk of males is 2–4 times higher than that of females (5–8). Regarding to the most common NDDs, previous studies published specific prevalence: 1/6 (17.4%) of American children aged 2–8 suffer from mental, behavioral or developmental disorders (9). In 2018, the global average prevalence of ADHD in school-age children was 5% (range: 2–7%) (10). In addition, according to the Centers for Disease Control, the prevalence of ASD among 8-year-olds in the United States increased from 0.67% in 2000 and 2002 to 2.3% in 2018 (11–13). The additional health, social care and education costs associated with childhood mental illness were estimated at £1.47 billion in 2008 in Britain, which impose a significant social and economic burden (14–16). Furthermore, mental disorders are listed as one of the top 10 causes of the global burden (17) and are seen as a major contributor to the burden of disease (18). Therefore, it is suggested to investigate causal pathways between mental disorders and other severe health issues.
Diabetes is another chronic disease that can be extremely dangerous, which can seriously damage many systems of the body, especially nerves and blood vessels. It is defined as a group of metabolic diseases characterized by hyperglycemia caused by defective insulin secretion, defective insulin action or both. There are two types of diabetes, type 1 diabetes mellitus (T1DM) and type 2 diabetes (19). The prevalence of diabetes is increasing year by year, with 451 million adults worldwide living with diabetes as of 2017, and the number is expected to rise to 693 million by 2045 (20).
Type 1 diabetes is characterized by elevated blood glucose levels due to insulin deficiency caused by loss of pancreatic b-cells, and it is a common chronic disease in children and adolescents, along with mental disorders (2, 21, 22). Studies have shown that T1DM brings great psychological burden to children and adolescents, and greatly increases the risk of mental health problems (23–25). NDDs are more common in children with T1DM compared to the general population (26–28). Vice versa, NDDs may also affect blood glucose control and increase the risk of diabetes complications (29). The International Society for Pediatric and Adolescent Diabetes (ISPAD) notes that mental health problems can lead to serious impacts and long-term consequences in young people with T1DM (30). However, no comprehensive study has examined the relationship between NDDs and T1DM in children and adolescents.
NDDs and T1DM are common in children and adolescents, may have similar pathogenesis, and may occur together. The purpose of this study was to investigate the prevalence of T1DM and NDDs in children and adolescents through meta-analysis and to explore the potential association between these two diseases.
Materials and methods
The Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guideline were followed by this systematic review (31). The protocol has been registered in PROSPERO (CDR42022333443).
Search strategy
We searched Embase, PubMed, and Web of Science databases for relevant articles published as of May 22, 2022. We selected subject terms and keywords related to diabetes, autism, ADHD, ID, CD, SLD, and motor disabilities in different databases, and the detailed retrieval strategy is shown in Supplementary Table 1. Additional studies were identified by manually reviewing of the references of included studies. The study selection process was completed independently by two researchers (X.L. and XN.-X.).
Study inclusion criteria
The inclusion criteria of the studies were as follows: (a) the age of population was 18 years old or below; (b) the population is accompanied by T1DM with NDDs or NDDs with T1DM; (c) The reported study must be published in English; (d) Prevalence estimates or raw data can be used to calculate the prevalence are available in the study; (e) The study to be included must be original studies, and reviews or systematic reviews are excluded. All papers that meet the criteria will be included in the systematic review.
Data extraction and quality assessment
A standardized form was used to extract the following data from the included studies: Author and year of publication, study content (country, study setting, data source, study period, sample size, age, percentage of males), diagnosis and criteria of T1DM and NDDs, outcome (the prevalence of NDDs in T1DM or the prevalence of T1DM in NDDs). If the prevalence estimates were not directly provided in the study, raw data from the article are collected and calculated to obtain prevalence. In addition, we also extracted the types of scales used in the diagnosis of different diseases and the judgment criteria used in the table, which are respectively, expressed as diagnosis and criteria in the table header (Supplementary Table 2). Two researchers (X.L. and XN.-X.) extracted data independently, and disagreements, if any, were resolved through discussion with the third author (YM.-L).
The 14-item rating scale National Institutes of Health Study Quality Assessment Tool for Observational Cohort and Cross-sectional Studies were used to assess the quality of each included study. The quality assessment was performed independently by two researchers (X.L. and XN.-X.) and resolved by negotiation or discussion with the third author (XY.-L).
Statistical analysis
The main outcome of this meta-analysis summarizes the prevalence of NDDs in individuals with type 1 diabetes. Data from people with T1DM with NDDs were analyzed for comparison. Prevalence estimates in each study were weighted by sample size and number of cases and then pooled through meta-analysis. I2 statistics were used to evaluate heterogeneity between studies (32). I2-value less than 30% was considered as low heterogeneity, greater than 60% was interpreted as substantial heterogeneity, and between 30 and 60% was considered as moderate heterogeneity. Publication bias was assessed by visually observing the symmetry of funnel plots and quantitative Egger (33) and Begg (34) tests. If publication bias is found, Duval Tweedie’s “trim and fill” method is used to obtain adjusted estimates (fill estimates) (35). We also looked at the study setting (population-based, clinically based), geographic region (North America, Asia, Europe, Africa), survey period (≤2010, >2010), age range (2–12 years old, ≥ 13 years old) and diagnosis/criteria (single standard, both standard). All statistical analyses were performed using Stata 17.0 software.
Results
Study selection and characteristics
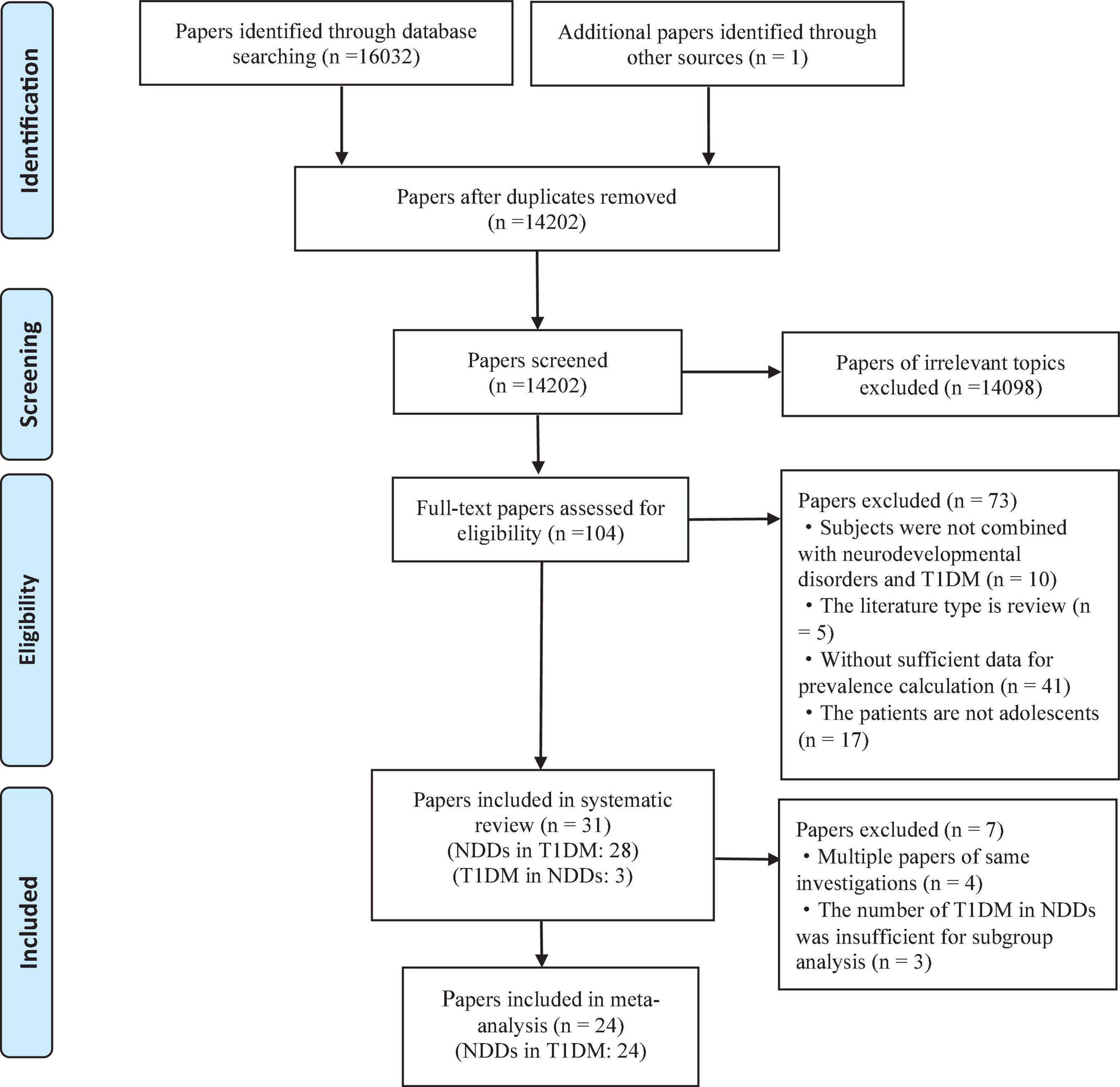
The PRISMA diagram for studying the selection process is shown in Figure 1. Among the retrieved studies, a total of 31 met the inclusion criteria (28 were related to NDDs in T1DM, and 3 were related to T1DM in NDDs) and were included in the systematic review. In the included studies, we excluded studies from the same investigation sources and studies related to T1DM in NDDs that were too small to be meta-analyzed. Finally, 24 studies related to NDDs in T1DM were included in the meta-analysis.
All of the studies were conducted between 1973 and 2019, with 20 population-based studies and 11 clinical-based studies (Supplementary Tables 2, 3). As part of the included papers were conference papers, the total number of papers participating in the quality evaluation was 21. The NIHSQAT (National Institutes of Health Research Quality Assessment Tool) was used to score the quality of all articles included in the analysis with full text, with all articles between 6 and 10 points in quality. A total of four items (20.0%) were rated as excellent (≥10 points) and 16 items (80.0%) were rated as fair (≥6 points). The results of the quality assessment are presented in detail in Supplementary Tables 4, 5.
Autism spectrum disorders/deficit hyperactivity disorder in children and adolescents with type 1 diabetes
Studies on the T1DM and ASD sample were published between 1973 and 2017 and included three clinically based studies and eight population-based studies (22, 23, 26, 36–44). Four studies were conducted in North America, six in Europe. Studies on a sample of patients with T1DM and ADHD, both published between 1973 and 2019, included 14 population-based studies and seven clinically based studies (19, 20, 23, 26, 40, 41, 45–60). One study was conducted in North America, 11 in Europe, one in Africa, and eight in Asia. Of the ASD sample studies, one study (14.3%) was rated as good quality (score ≥ 10), and six studies (85.7%) were rated as general quality (score ≥ 6). Of the ADHD sample studies, two studies (14.3%) were rated as good quality, and 12 studies (85.7%) were rated as general quality.
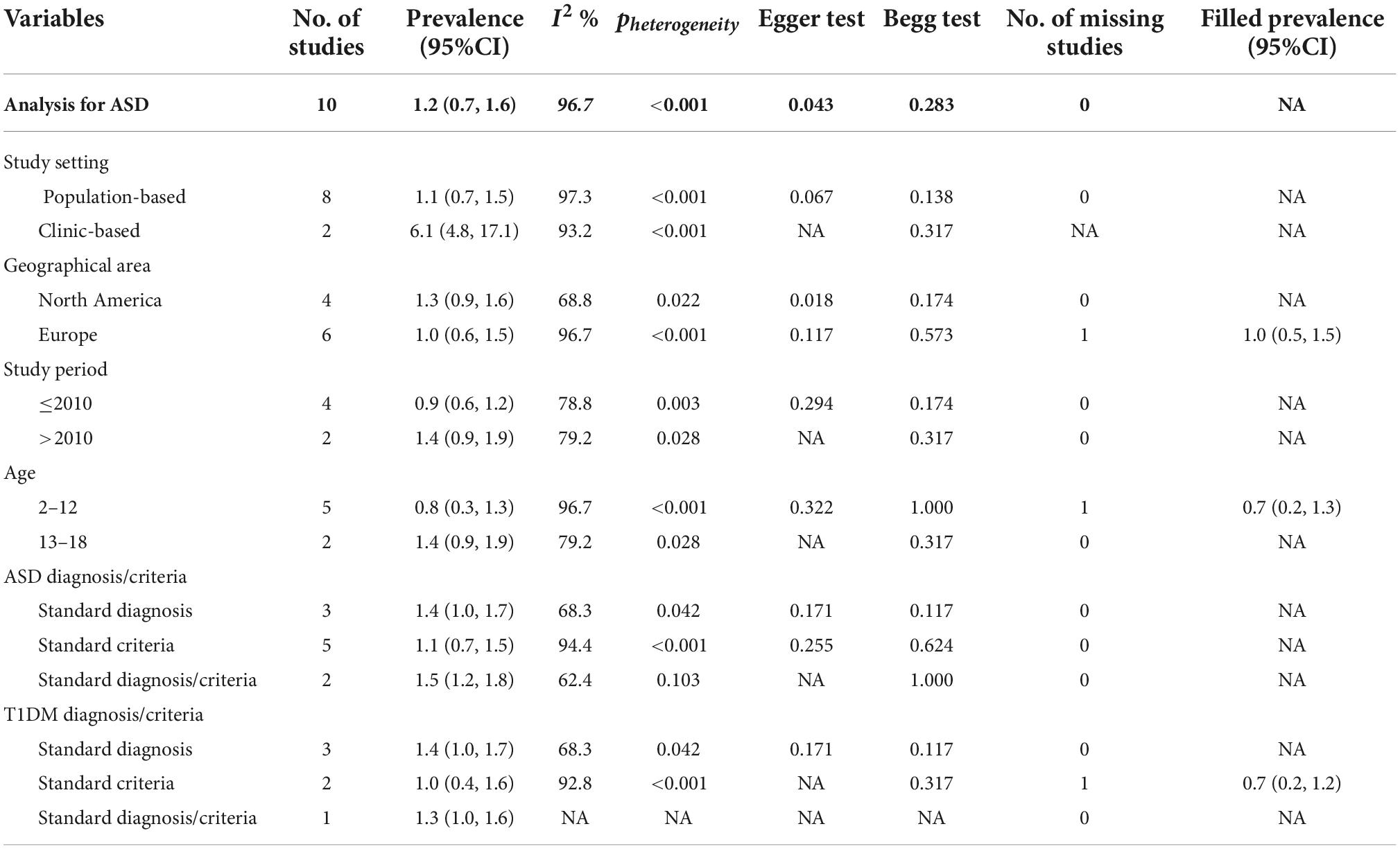
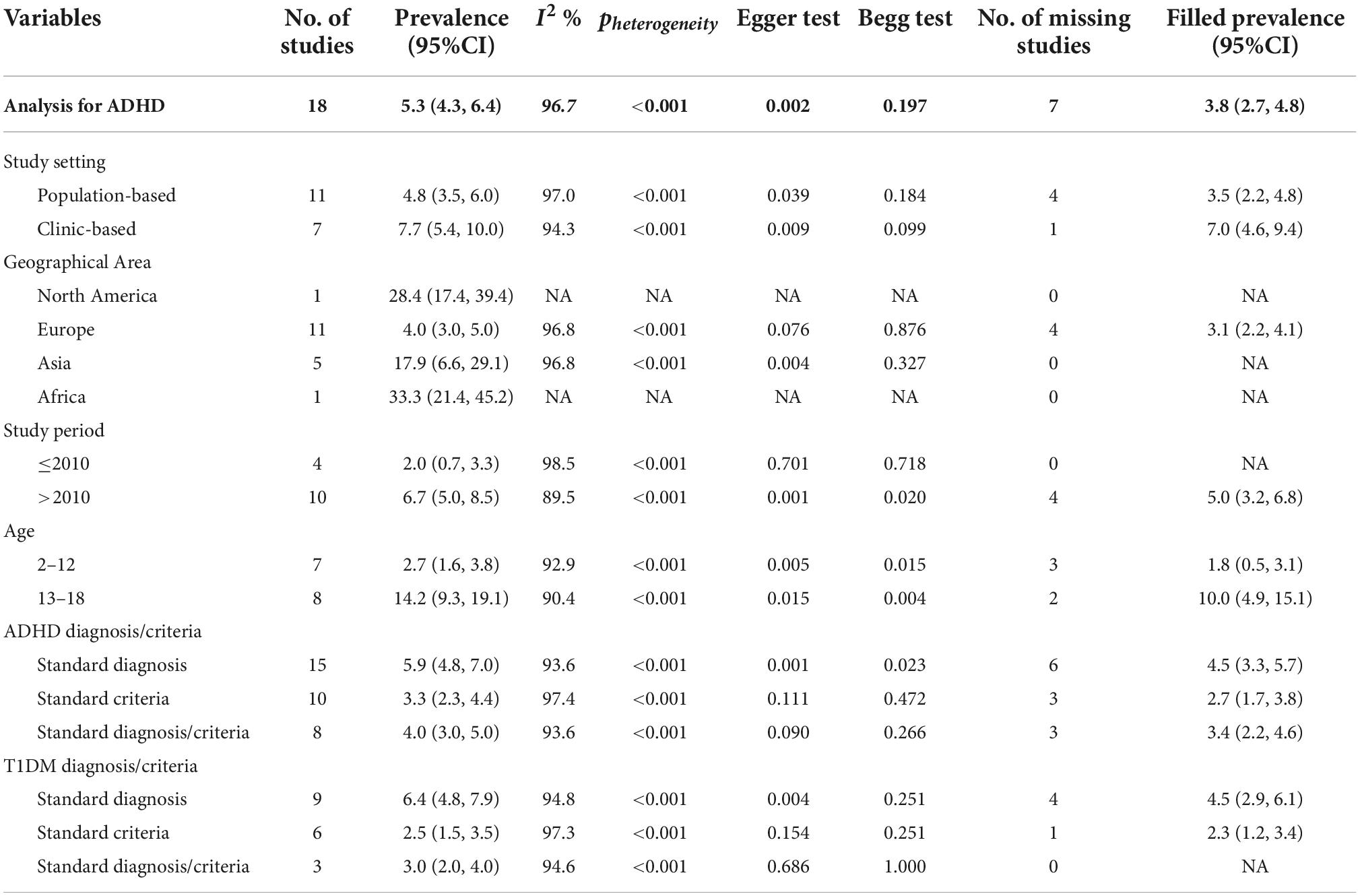
The prevalence of ASD and ADHD in children and adolescents with T1DM was 1.2% (95%CI: 0.9–1.6%) and 5.3% (95%CI: 4.3–6.4%), respectively (Supplementary Figures 1, 2). Subgroup analysis showed that the prevalence of ASD among adolescents/children with T1DM was 1.1% in population-based studies, 6.1% in clinical studies, 1.0 and 1.3% in Europe and North America, 0.9 and 1.4% before and 2010 and after 2010, respectively. The prevalence was 0.8% in 2–12 years and 1.4% in 13–18 years. The prevalence of ADHD was 4.8% in population studies and 7.7% in clinical studies, and 4.0% in Europe, 28.4% in North America, 17.9% in Asia and 33.3% in Africa. The prevalence in 2010 and before and after 2010 was 2.0 and 6.7%, respectively. The prevalence was 2.7% in 2–12 years and 6.7% in 13–18 years, respectively (Tables 1, 2).
Detection of publication bias by funnel plot, Begg test and Egger test (Supplementary Figures 3, 4). The fill prevalence of ADHD in the T1DM children and adolescent population obtained by the “trim and fill” method was 1.3%, whereas ASD had no fill prevalence in the T1DM adolescents.
Except ASD and ADHD, other NDDs retrieved in this study were not included in our meta-analysis.
Type 1 diabetes mellitus in children and adolescents with neurodevelopmental disorders
There were two studies on T1DM among the included children and adolescents with ASD, which were conducted in the United States from 2001 to 2010. One was a clinical study and the other was a population-based study, with a prevalence rate of 0.93 and 0.67%, respectively. The quality evaluation was of general quality. There is only one study related to T1DM in children and adolescent ADHD patients, which is a population-based study conducted in China with a prevalence rate of 0.1%, and it is rated as good quality.
Except ASD and ADHD, there is no study on type 1 diabetes in children and adolescents with other neurodevelopmental disorders that met our inclusion criteria.
Discussion
The results of the study showed that the prevalence of ASD and ADHD in T1DM children and adolescents was 1.1% (95% CI: 0.8–1.5) and 5.3% (95% CI: 4.3, 6.4), respectively, both higher than the global prevalence of ASD and ADHD in the general population in 2019 (0.4 and 1.1%), suggesting that T1DM has an impact on the prevalence of ASD and ADHD. Present study analyzed the prevalence of concurrent NDDs with T1DM in children and adolescents and explored the potential association between T1DM and NDDs.
A growing number of studies have explored the relationship between metabolic disorders and psychiatric disorders, and there has been a gradual increase in research on the relationship between diabetes and psychiatric disorders, as well as a large body of literature exploring the effect of maternal diabetes on the development of neurodevelopmental disorders in offspring (61–65), but the detailed mechanisms remain unclear. Meanwhile, there are fewer original studies on the comorbid psychiatric disorders in patients with T1DM. Our systematic search strategy retrieves all available studies to comprehensively summarize the current evidence. Our subgroup analysis provides evidence for the increased prevalence of ADHD from childhood to age in patients with type 1 diabetes, but the relationship between ASD prevalence and age stratification needs to be further explored. Potential solid studies were identified through the “trim and fill” approach, which means there may be unpublished studies or less obvious results that were not included in our meta-analysis. However, the filled studies and their prevalence were not calculated by retrieval from existing data, and the “trim and fill” method used to adjust the mixed estimates was based on funnel plots (23), so the number of filled studies may not be true, and their estimates of prevalence may not be very accurate. Three mechanisms may be involved in the relationship between type 1 diabetes and neurodevelopmental disorders (Figure 2) (66, 67): Firstly, dysregulated circulating autoantibodies (GAD-Abs). Abnormalities of GAD65 and IA-2 antibodies (Abs) can be detected in the blood of patients with both type 1 diabetes and neurodevelopmental disorders. It was reported that GAD65 and IA-2 antibodies (Abs) are biomarkers for the development of type 1 diabetes mellitus (T1DM) in children and adults and can be detected in the blood months to years before the onset of symptoms (68). In a study with 20 children with ASD and 15 children with ADHD, immunoassays showed that 15% of children with ASD and 17% of children with ADHD had higher serum levels of GAD65 antibodies compared to controls (69). The neurotransmitter gamma amino butyric acid (GABA) is a major neurotropic agent in the central nervous system and plays a key role in the early development of the nervous system, while GAD65 is one of the two enzymes that catalyze the formation of GABA from glutamate (70); therefore, abnormalities in GAD65 may lead to abnormal development of the nervous system. Secondly, Specific single nucleotide polymorphism (SNP) mutations. Studies have shown that SNPs are significantly associated with a range of childhood and adult-onset psychiatric disorders (71), and copy number variants identified in genome-wide studies may contribute to the risk of multiple psychiatric disorders (72). At the same time, an increasing number of SNPs are significantly associated with the pathogenesis of diabetes (73). Thirdly, Abnormal insulin and glucose concentrations. Abnormal insulin and glucose concentrations include insulin deficiency, hyperglycemia, and medically induced hypoglycemia. There is now evidence that insulin plays an important role in neurodevelopment (74), and the effects of insulin overdose and resulting severe hypoglycemia on the central nervous system during T1DM treatment may lead to neurocognitive deficits (75), but there is no clear evidence to confirm the reliability of this theory. Similar to insulin, glucose metabolism is critical for brain development and function (35), and abnormal glucose in children with type 1 diabetes has a greater detrimental effect on central nervous system development (76). Also, a number of studies have shown that glucose abnormalities are associated with impaired neurocognitive function (77), which may lead to psychiatric disorders. In addition, Sillanpaa noted that poor social adjustment and reduced functioning in patients with T1DM may further increase their risk of developing major psychiatric disorders (78).
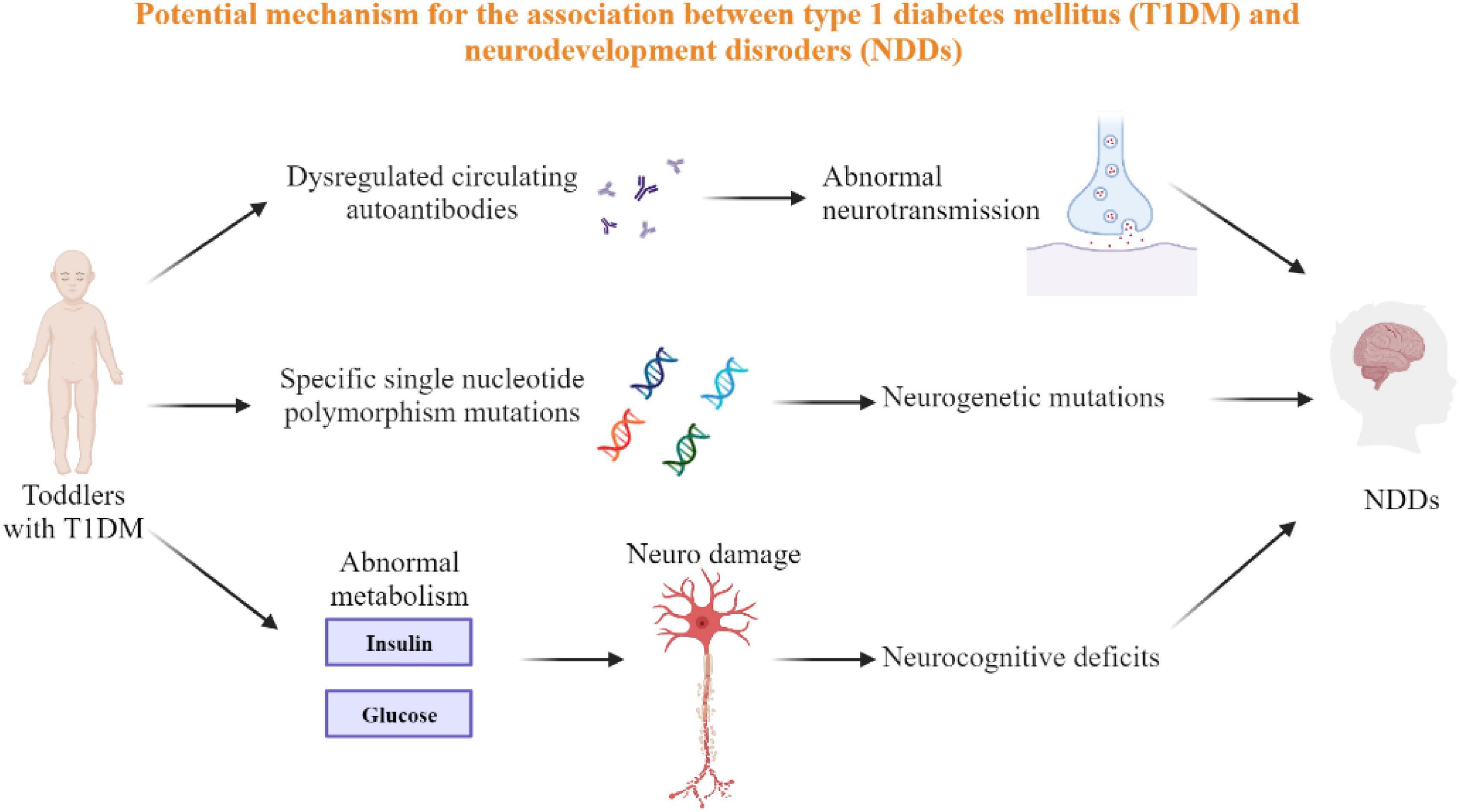
Figure 2. The potential mechanism of T1DM and NDDs. Three possible potential mechanisms for the interaction between type 1 diabetes and neurodevelopmental disorders are circulating autoantibody dysregulation, specific single nucleotide polymorphism mutations, and abnormal insulin and glucose concentrations, all of which involve substances that are associated with both T1DM and NDDs.
There may be some limitations to our analysis. First, the prevalence of mental developmental disorders among people with type 1 diabetes and the incidence of type 1 diabetes among people with mental developmental disorders may be underestimated, as there are still areas where low awareness of mental disorders or inadequate understanding of type 1 diabetes may lead to underdiagnosis and thus affect the accuracy of prevalence. Secondly, the literature is limited, and the results of our regional subgroup analysis for existing literature may not be applicable to all regions of the world. In addition, in the subgroup analysis results of prevalence of ASD in T1DM patients, the low prevalence in some age groups may lead to the unreliable prevalence of ASD in T1DM patients. However, mental disorders include six diseases, but there are few literatures related to some of them and more relevant researches are needed. Finally, recall bias can occur when recording situations through self-reports or parental reports.
In conclusion, this systematic review and meta-analysis suggests that type 1 diabetes is associated with the neurodevelopmental disorders in children and adolescents. There was a significant increase in the prevalence of ASD or ADHD in the adolescent T1DM population compared with that in the general population, and there was a trend for the prevalence of ASD and ADHD to increase with age in the T1DM population, but there is less literature on the association of the prevalence of T1DM in the children and adolescent neurodevelopmental disorders population. The potential link between the two disorders was also explored in this systematic review and meta-analysis, but the mechanisms behind T1DM and psychiatric disorders are not fully understood, and more high-quality studies are needed to elucidate the pathogenesis of T1DM and psychiatric disorders and to explore their intrinsic connections.
Data availability statement
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
Author contributions
Y-ML and X-YL conceived the study design. C-YX and XL conducted data analysis. X-NX conducted study evaluation and wrote the manuscript. All authors have reviewed and approved the submitted version of the manuscript.
Funding
This study was funded by the National Natural Science Foundation of China (81873806).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.982696/full#supplementary-material
References
1. American Psychaitric Association. Diagnostic and statistical manual of mental disorders (DSM-5®). New York, NY: American Psychiatric Pub (2013). doi: 10.1176/appi.books.9780890425596
2. Thapar A, Cooper M, Rutter M. Neurodevelopmental disorders. Lancet Psychiatry. (2017) 4:339–46. doi: 10.1016/S2215-0366(16)30376-5
3. May T, Adesina I, McGillivray J, Rinehart NJ. Sex differences in neurodevelopmental disorders. Curr Opin Neurol. (2019) 32:622–6. doi: 10.1097/WCO.0000000000000714
4. Wang X. Maternal diabetes induces autism-like behavior by hyperglycemia-mediated persistent oxidative stress and suppression of superoxide dismutase 2. Proceedings of the national academy of sciences of the United States of America. (2019). 47 p.
5. Christensen DL, Braun KVN, Baio J. Prevalence and characteristics of autism spectrum disorder among children aged 8 years—autism and developmental disabilities monitoring network, 11 sites, United States, 2012. MMWR Surveill Summ. (2018) 65:1. doi: 10.15585/mmwr.ss6513a1
6. May T, Sciberras E, Brignell A, Williams K. Autism spectrum disorder: updated prevalence and comparison of two birth cohorts in a nationally representative Australian sample. BMJ Open. (2017) 7:e015549. doi: 10.1136/bmjopen-2016-015549
7. Wang T, Liu K, Li Z, Liu K, Li Z, Xu Y, et al. Prevalence of attention deficit/hyperactivity disorder among children and adolescents in China: a systematic review and meta-analysis. BMC Psychiatry. (2017) 17:32. doi: 10.1186/s12888-016-1187-9
8. May T, Williams K. Brief report: gender and age of diagnosis time trends in children with autism using Australian medicare data. J Autism Dev Disord. (2018) 48:4056–62. doi: 10.1007/s10803-018-3609-7
9. Cree RA, Bitsko RH, Robinson LR, Holbrook JR, Danielson ML, Smith DS, et al. Health care, family, and community factors associated with mental, behavioral, and developmental disorders and poverty among children aged 2–8 years — United States, 2016. MMWR. (2018) 67:1377–83. doi: 10.15585/mmwr.mm6750a1
10. Sayal K, Prasad V, Daley D, Ford T, Coghill D. ADHD in children and young people: prevalence, care pathways, and service provision. Lancet Psychiatry. (2018) 5:175–86. doi: 10.1016/S2215-0366(17)30167-0
11. Autism and Developmental Disabilities Monitoring Network Surveillance Year 2000 Principal Investigators. Prevalence of autism spectrum disorders—Autism and developmental disabilities monitoring network, six sites, United States, 2000. MMWR Surveill Summ. (2007) 61:1–19.
12. Autism and Developmental Disabilities Monitoring Network Surveillance Year 2002 Principal Investigators. Prevalence of autism spectrum disorders—Autism and developmental disabilities monitoring network, 14 sites, United States, 2002. MMWR Surveill Summ. (2007) 61:1–19.
13. Maenner MJ, Shaw KA, Bakian AV, Bilder DA, Durkin MS, Esler A, et al. Prevalence and characteristics of autism spectrum disorder among children aged 8 years – autism and developmental disabilities monitoring network, 11 Sites. MMWR Surveill Summ. (2021) 70:1–16.
14. Gilissen C, Hehir-Kwa JY, Thung DT, van de Vorst M, van Bon BW, Willemsen MH, et al. Genome sequencing identifies major causes of severe intellectual disability. Nature. (2014) 511:344–7. doi: 10.1038/nature13394
15. Knapp M, Snell T, Healey A, Guglani S, Evans-Lacko S, Fernandez JL, et al. How do child and adolescent mental health problems influence public sector costs? Interindividual variations in a nationally representative British sample. J Child Psychol Psychiatry. (2015) 56:667–76. doi: 10.1111/jcpp.12327
16. Snell T, Knapp M, Healey A, Guglani S, Evans-Lacko S, Fernandez JL, et al. Economic impact of childhood psychiatric disorder on public sector services in Britain: estimates from national survey data. J Child Psychol Psychiatry. (2013) 54:977–85. doi: 10.1111/jcpp.12055
17. Gbd 2019. Mental disorders collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet Psychiatry. (2022) 9:137–50. doi: 10.1016/S2215-0366(21)00395-3
18. Patel V, Saxena S, Lund C. The lancet commission on global mental health and sustainable development. Lancet. (2018) 392:1553–98. doi: 10.1016/S0140-6736(18)31612-X
19. Mazor-Aronovitch K, Pinhas-Hamiel O, Pivko-Levy D, Modan-Moses D, Levek N, Miller S, et al. Dual diagnosis of type 1 diabetes mellitus and attention deficit hyperactivity disorder. Pediatr Diabetes. (2021) 22:649–55. doi: 10.1111/pedi.13195
20. Sakhr HM, Hassan MH, Desoky T. Possible associations of disturbed neurometals and ammonia with glycaemic control in type 1 diabetic children with attention deficit hyperactivity disorder. Biol Trace Elem Res. (2020) 198:68–76. doi: 10.1007/s12011-020-02063-5
21. Bethin KE, Kanapka LG, Laffel LM, Majidi S, Chaytor NS, MacLeish S, et al. T1D exchange clinic network. autism spectrum disorder in children with type 1 diabetes. Diabet Med. (2019) 36:1282–6. doi: 10.1111/dme.14069
22. Ross C, Ward ZJ, Gomber A, Owais M, Yeh JM, Reddy CL, et al. The prevalence of islet autoantibodies in children and adolescents with type 1 diabetes mellitus: a global scoping review. Front Endocrinol. (2022) 13:815703. doi: 10.3389/fendo.2022.815703
23. Butwicka A, Frisén L, Almqvist C, Zethelius B, Lichtenstein P. Risks of psychiatric disorders and suicide attempts in children and adolescents with type 1 diabetes: a population-based cohort study. Diabetes Care. (2015) 38:453–9. doi: 10.2337/dc14-0262
24. Buchberger B, Huppertz H, Krabbe L, Lux B, Mattivi JT, Siafarikas A. Symptoms of depression and anxiety in youth with type 1 diabetes: a systematic review and meta-analysis. Psychoneuroendocrinology. (2016) 70:70–84. doi: 10.1016/j.psyneuen.2016.04.019
25. Cooper MN, Lin A, Alvares GA, de Klerk NH, Jones TW, Davis EA. Psychiatric disorders during early adulthood in those with childhood onset type 1 diabetes: rates and clinical risk factors from population-based follow-up. Pediatr Diabetes. (2017) 18:599–606. doi: 10.1111/pedi.12469
26. Dybdal D, Tolstrup JS, Sildorf SM. Increasing risk of psychiatric morbidity after childhood onset type 1 diabetes: a population-based cohort study. Diabetologia. (2018) 61:831–8. doi: 10.1007/s00125-017-4517-7
27. Collins MM, Corcoran P, Perry IJ. Anxiety and depression symptoms in patients with diabetes. Diabet Med. (2009) 26:153–61. doi: 10.1111/j.1464-5491.2008.02648.x
28. Petrak F, Hardt J, Wittchen HU. Prevalence of psychiatric disorders in an onset cohort of adults with type 1 diabetes. Diabetes Metab Res Rev. (2003) 19:216–22. doi: 10.1002/dmrr.374
29. Duke DC, Harris MA. Executive function, adherence, and glycemic control in adolescents with type 1 diabetes: a literature review. Curr Diab Rep. (2014) 14:532. doi: 10.1007/s11892-014-0532-y
30. Delamater AM, de Wit M, McDarby V, Malik J, Acerini CL. International society for pediatric and adolescent diabetes. ISPAD clinical practice consensus guidelines 2014. Psychological care of children and adolescents with type 1 diabetes. Pediatr Diabetes. (2014) 20:232–44. doi: 10.1111/pedi.12191
31. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J Clin Epidemiol. (2021) 134:178–89. doi: 10.1016/j.jclinepi.2021.02.003
32. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.1186
33. Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
34. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. (1994) 1994:1088–101. doi: 10.2307/2533446
35. Duval S, Tweedie R. Trim and fill: a simple funnel-plot–based method of testing and adjusting for publication bias in meta-analysis. Biometrics. (2000) 56:455–63. doi: 10.1111/j.0006-341X.2000.00455.x
36. Ferguson L, Franklin V. The prevalence of type 1 diabetes and autistic spectrum disorder in highland region, scotland, and its impact on glycaemic control and care needs. Pediatr Diabetes. (2019) 20:226.
37. Freeman SJ, Roberts W, Daneman D. Type 1 diabetes and autism: is there a link? Diabetes Care. (2005) 28:925–6. doi: 10.2337/diacare.28.4.925
38. Harjutsalo V, Tuomilehto J. Type 1 diabetes and autism: is there a link? Diabetes Care. (2006) 29:484–5; discussion 485. doi: 10.2337/diacare.29.02.06.dc05-1552
39. Kohane IS, McMurry A, Weber G, MacFadden D, Rappaport L, Kunkel L, et al. The co-morbidity burden of children and young adults with autism spectrum disorders. PLoS One. (2012) 7:e33224. doi: 10.1371/journal.pone.0033224
40. Liu S, Kuja-Halkola R, Larsson H, Lichtenstein P, Ludvigsson JF, Svensson AM, et al. Neurodevelopmental disorders, glycemic control, and diabetic complications in type 1 diabetes: a nationwide cohort study. J Clin Endocrinol Metab. (2021) 106:e4459–70. doi: 10.1210/clinem/dgab467
41. Liu S, Kuja-Halkola R, Larsson H, Lichtenstein P, Ludvigsson JF, Svensson AM, et al. Poor glycaemic control is associated with increased risk of neurodevelopmental disorders in childhood-onset type 1 diabetes: a population-based cohort study. Diabetologia. (2021) 64:767–77. doi: 10.1007/s00125-020-05372-5
42. Stanek K, Raymond JK, Majidi S. Prevalence and management of patients with type 1 diabetes and autism spectrum disorder. Diabetes. (2016) 65:A338–9. doi: 10.2337/db16-861-1374
43. Stanek KR, Youngkin EM, Pyle LL, Raymond JK, Driscoll KA, Majidi S. Prevalence and management of patients with type 1 diabetes and autism spectrum disorder. Diabetes. (2019) 20:645–51.
44. Tojjar J. Is there a connection between type 1 diabetes and autism? the prevalence of autism in children with type 1 diabetes and differences in phenotype and biomarkers at diabetes diagnosis. Pediatr Diabetes. (2019) 20:217.
45. Bratina N. Attention deficit hyperactivity disorder and metabolic control in adolescents with type 1 diabetes. Pediatric Diabetes. (2015) 16:137.
46. Castillo K. Prevalence of attention-deficit/hyperactivity disorder in children and adolescents with early onset type 1 diabetes compared to general population peers. Pediatric Diabetes. (2017) 18:52–3.
47. Chen HJ, Lee YJ, Yeh GC, Lin HC. Association of attention-deficit/hyperactivity disorder with diabetes: a population-based study. Pediatr Res. (2013) 73:492–6. doi: 10.1038/pr.2013.5
48. Duke DC. Not paying attention to diabetes: ADHD and diabetes management. Diabetes. (2012) 61:A210.
49. Kapellen TM, Reimann R, Kiess W, Kostev K. Prevalence of medically treated children with ADHD and type 1 diabetes in Germany – analysis of two representative databases. J Pediatr Endocrinol Metab. (2016) 29:1293–7. doi: 10.1515/jpem-2016-0171
51. Lin SY, Lin CL, Hsu WH, Lin CC, Fu YC. Association of attention deficit hyperactivity disorder with recurrent hypoglycemia in type 1 diabetes mellitus. Pediatr Diabetes. (2019) 20:189–96. doi: 10.1111/pedi.12716
52. Lindblad I, Engström AC, Nylander C, Fernell E. Adolescents with type 1 diabetes mellitus and attention-deficit/hyperactivity disorder require specific support from healthcare professionals. Acta Paediatr. (2017) 106:1994–7. doi: 10.1111/apa.13989
53. Macek J, Battelino T, Bizjak M, Zupanc C, Bograf AK, Vesnic S, et al. Impact of attention deficit hyperactivity disorder on metabolic control in adolescents with type1 diabetes. J Psychosom Res. (2019) 126:109816. doi: 10.1016/j.jpsychores.2019.109816
54. Mazor-Aronovitch K, Pinhas-Hamiel O, Pivko-Levy D, Modan-Moses D, Levek N, Miller S, et al. Dual diagnosis of type 1 diabetes and ADHD. Hormone Res Paediatrics. (2019) 91:88–9.
55. Nylander C, Lindström K, Khalifa N, Fernell E. Previously undiagnosed attention-deficit/hyperactivity disorder associated with poor metabolic control in adolescents with type 1 diabetes. Pediatr Diabetes. (2018) 19:816–22. doi: 10.1111/pedi.12651
56. Nylander C, Tindberg Y, Haas J, Swenne I, Torbjörnsdotter T, Åkesson K, et al. Self- and parent-reported executive problems in adolescents with type 1 diabetes are associated with poor metabolic control and low physical activity. Pediatr Diabetes. (2018) 19:98–105. doi: 10.1111/pedi.12520
57. Vinker-Shuster M, Eldor R, Green I, Golan-Cohen A, Manor I, Merzon E. Glycemic control and diabetes related complications in adults with type 1 diabetes mellitus and ADHD. J Atten Disord. (2022) 26:1235–44. doi: 10.1177/10870547211068039
58. Vinker-Shuster M, Golan-Cohen A, Merhasin I, Merzon E. Attention-deficit hyperactivity disorder in pediatric patients with type 1 diabetes mellitus: clinical outcomes and diabetes control. J Dev Behav Pediatr. (2019) 40:330–4. doi: 10.1097/DBP.0000000000000670
59. Yazar A, Akın F, Akça ÖF, Eklioğlu BS, Türe E, Coşkun F, et al. The effect of attention deficit/hyperactivity disorder and other psychiatric disorders on the treatment of pediatric diabetes mellitus. Pediatr Diabetes. (2019) 20:345–52. doi: 10.1111/pedi.12819
60. Zahed G, Shakiba M, Seifi K. The prevalence of psychological disorders among children with diabetes aged 5-12 years old referred to the endocrinology clinic of mofid hospital, tehran, Iran in 2014-2015. Iran J Child Neurol. (2018) 12:101–12.
61. Lu J, Wang Z, Liang Y, Yao P. Rethinking autism: the impact of maternal risk factors on autism development. Am J Transl Res. (2022) 14: 1136–45.
62. Lu J, Xiao M, Guo X, Liang Y, Wang M, Xu J, et al. Maternal diabetes induces immune dysfunction in autistic offspring through oxidative stress in hematopoietic stem cells. Front Psychiatry. (2020) 11:576367. doi: 10.3389/fpsyt.2020.576367
63. Zeng J, Liang Y, Sun R, Huang S, Wang Z, Xiao L, et al. Hematopoietic stem cell transplantation ameliorates maternal diabetes-mediated gastrointestinal symptoms and autism-like behavior in mouse offspring. Ann N Y Acad Sci. (2022) 1512:98–113. doi: 10.1111/nyas.14766
64. Wang X, Lu J, Xie W, Lu X, Liang Y, Li M, et al. Maternal diabetes induces autism-like behavior by hyperglycemia-mediated persistent oxidative stress and suppression of superoxide dismutase 2. Proc Natl Acad Sci USA. (2019) 116:23743–52. doi: 10.1073/pnas.1912625116
65. Liang Y, Yu H, Ke X, Eyles D, Sun R, Wang Z, et al. Vitamin D deficiency worsens maternal diabetes induced neurodevelopmental disorder by potentiating hyperglycemia-mediated epigenetic changes. Ann NY Acad Sci. (2021) 1491:74–88. doi: 10.1111/nyas.14535
66. Cameron FJ, Northam EA, Ryan CM. The effect of type 1 diabetes on the developing brain. Lancet Child Adolesc Health. (2019) 3:427–36. doi: 10.1016/S2352-4642(19)30055-0
67. Cato A, Hershey T. Cognition and type 1 diabetes in children and adolescents. Diabetes Spectr. (2016) 29:197–202. doi: 10.2337/ds16-0036
68. Atkinson MA, Eisenbarth GS, Michels AW. Type 1 diabetes. Lancet. (2014) 383:69–82. doi: 10.1016/S0140-6736(13)60591-7
69. Rout UK, Mungan NK, Dhossche DM. Presence of GAD65 autoantibodies in the serum of children with autism or ADHD. Eur Child Adolesc Psychiatry. (2012) 21:141–7. doi: 10.1007/s00787-012-0245-1
70. Vazifekhah S, Barfi S, Soleimany F, Aliakbar A, Zavvari F, Karimzadeh F. The plasma level of glutamic acid decarboxylase 65 (GAD65) increased in severely autistic Iranian children. Bratisl Lek Listy. (2022) 123:347–51. doi: 10.4149/BLL_2022_054
71. Cross-Disorder Group of the Psychiatric Genomics Consortium. Identification of risk loci with shared effects on five major psychiatric disorders: a genome-wide analysis. Lancet. (2013) 381:1371–9. doi: 10.1016/S0140-6736(12)62129-1
72. Malhotra D, Sebat J. CNVs: harbingers of a rare variant revolution in psychiatric genetics. Cell. (2012) 148:1223–41. doi: 10.1016/j.cell.2012.02.039
73. Howlader M, Sultana MI, Akter F, Hossain MM. Adiponectin gene polymorphisms associated with diabetes mellitus: a descriptive review. Heliyon. (2021) 7:e07851. doi: 10.1016/j.heliyon.2021.e07851
74. Huang CC, Lee CC, Hsu KS. The role of insulin receptor signaling in synaptic plasticity and cognitive function. Chang Gung Med J. (2010) 33:115–25.
75. Korczak DJ, Pereira S, Koulajian K, Matejcek A, Giacca A. Type 1 diabetes mellitus and major depressive disorder: evidence for a biological link. Diabetologia. (2011) 54:2483–93. doi: 10.1007/s00125-011-2240-3
76. Ferensztajn-Rochowiak E, Kaczmarek M, Wojcicka M, Kaufman-Szukalska E, Dziuda S, Remlinger-Molenda A, et al. Glutamate-related antibodies and peripheral insulin-like growth factor in bipolar disorder and lithium prophylaxis. Neuropsychobiology. (2019) 77:49–56. doi: 10.1159/000493740
77. Tylee DS, Sun J, Hess JL, Tahir MA, Sharma E, Malik R, et al. Genetic correlations among psychiatric and immune-related phenotypes based on genome-wide association data. Am J Med Genet B. (2018) 177:641–57. doi: 10.1002/ajmg.b.32652
Keywords: type 1 diabetes mellitus (T1DM), neurodevelopmental disorders (NDDs), prevalence, autism spectrum disorder (ASD), meta-analysis, attention deficit hyperactivity disorder (ADHD)
Citation: Xie X-N, Lei X, Xiao C-Y, Li Y-M and Lei X-Y (2022) Association between type 1 diabetes and neurodevelopmental disorders in children and adolescents: A systematic review and meta-analysis. Front. Psychiatry 13:982696. doi: 10.3389/fpsyt.2022.982696
Received: 30 June 2022; Accepted: 25 October 2022;
Published: 22 November 2022.
Edited by:
Yongjiang Li, Central South University, ChinaReviewed by:
Francesco Monaco, Azienda Sanitaria Locale Salerno, ItalyMarkus Johannes Hofer, The University of Sydney, Australia
Copyright © 2022 Xie, Lei, Xiao, Li and Lei. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ya-Min Li, YW1pbm55QGNzdS5lZHUuY24=; Xian-Yang Lei, c2h5b3VuZ0Bjc3UuZWR1LmNu
 Xue-Ni Xie
Xue-Ni Xie Xue Lei
Xue Lei Chun-Ye Xiao4
Chun-Ye Xiao4 Ya-Min Li
Ya-Min Li