
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 17 August 2022
Sec. Public Mental Health
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.978566
This article is part of the Research TopicBurnout in the Health, Social Care and Beyond: Integrating Individuals and SystemsView all 14 articles
Burnout is often characterized by cognitive deficits and it has been associated with depression and anxiety. However, it is not clear whether cognitive impairment is a burnout consequence or employees with poor cognitive skills are more prone in developing burnout. Moreover, the exact nature of the association between burnout and depression, and burnout and anxiety is still unknown. Depression and anxiety are also related to cognitive impairments but their prospective associations are not fully understood. The aim of the present three-wave longitudinal study was to investigate the causality between cognitive functioning, burnout, depression, and anxiety among non-clinical burnout employees. The cause-effect associations of burnout with depression and anxiety were also explored. Perceived family support as a protective factor against cognitive decline, burnout, depression and anxiety was examined as well. A wide range of cognitive tasks tapping different cognitive domains were administered to employees of the general working population. Burnout, depression, anxiety, and perceived family support were assessed with self-reported questionnaires. Present results suggest that visuospatial functioning deficits are a burnout consequence and they indicate the role of automatic processing skills and executive functions in burnout onset. Additionally, current findings support that burnout is differentiated from depression and anxiety but it is reciprocally associated with the two psychological phenomena. Lastly, current results support the inclusion of perceived family support as an intervention to help individuals who suffer from mental health and cognitive difficulties.
Occupational chronic stress is a growing health risk factor among working populations (1) and burnout is one of its consequences. The concept of burnout is not unitary and its definition depends upon the tool used for its measurement (2). The present paper adopts the approach to burnout as provided by Maslach et al. (3). That is, burnout consists of three dimensions; exhaustion, cynicism, and reduced personal efficacy (3). Exhaustion refers to the depletion of emotional resources; cynicism concerns employees’ distancing from their work, clients etc.; reduced personal efficacy is the negative appraisal of an individual’s work resulting in low work self-esteem (4). Hereafter, the term “burnout” reflects the abovementioned three dimensions. Cognitive performance has become an important aspect in the burnout research during the past decades. Desart et al. (5) proposed a new burnout definition by including two new core symptoms; cognitive and emotional loss of control; a notion that has been supported by other scholars as well (6). Nevertheless, whether cognitive impairment is a burnout consequence or employees with lower cognitive skills are more prone to such stress effects and thus, more vulnerable to burnout is still unclear. An additional limitation concerns the lack of studies investigating non-clinical burnout, as most researchers focus on clinical populations. By taking into consideration the importance of detecting and addressing early the burnout effects, the present study focuses on the examination of non-clinical burnout employees; i.e., employees who have not received a clinical diagnosis (in contrast to the clinical burnout individuals) but report high burnout levels as measured by self-reported questionnaires and they continue working.
Burnout has also been associated with depression and anxiety as burned-out employees often suffer from these two mental health problems (7). Burnout’s comorbidity with depression and anxiety is so common that its empirical distinction from these two mental disorders has been a matter of debate among researchers (8, 9). Additionally, both depression and anxiety have been linked with cognitive impairment (10, 11). Hence, when examining the association between burnout and cognitive functioning researchers also need to consider for possible comorbidity with depression and anxiety as this association might be biased by the presence of these two mental health problems. Another research question that has not received much attention concerns whether individuals with weaker cognitive skills are more susceptible in experiencing psychological distress as a result of the everyday difficulties these individuals might experience.
Several studies (12, 13) and reviews (14, 15) have indicated the negative associations between burnout and cognitive functioning, with executive functioning deficits being the most prominent ones (14). Executive functions are high order cognitive functions and they include cognitive skills such as inhibition, switching (or cognitive flexibility), planning (16), reasoning, and problem solving (17). Employees with poorer executive function skills might be less able to stay focused on tasks, make decisions, and struggle with time management. All these difficulties can potentially lead to burnout onset. At the same time, as burnout levels rise they can further affect executive functions (18); a process that leads to a vicious circle. Although executive deficits are common amongst burned-out employees, they are also the most studied ones (14); overlooking potential associations between burnout and other cognitive functions.
The basic burnout conceptualization regards burnout as a three-dimensional concept. Nevertheless, the consistent associations of burnout with cognitive deficits have led several scholars (5, 6) to enhance our approach to the burnout model by arguing that cognitive deficits should also be included in the burnout definition. Schaufeli et al. (6) identified cognitive deficits as a core burnout component while the authors argued that cognitive impairment is a burnout consequence that emerges due to the lack of energy which is prominent in burnout. However, the causality between burnout and cognitive functioning should first be elucidated before cognitive impairment is included as a core burnout dimension.
Although individuals with poorer executive functioning abilities are more vulnerable to the stress effects (19), the investigation of whether cognitive impairment is a burnout consequence or employees with lower cognitive abilities are more prone in developing burnout is an under-explored research area. Most relevant studies are of a cross-sectional design while longitudinal studies mainly focus to the long-lasting effects of burnout (20, 21). To the authors’ knowledge, so far, only two studies have examined for reversed effects and they provide mixed results. Specifically, in their study, Feuerhahn et al. (22) found that executive functioning deficits were a consequence of the exhaustion burnout dimension while Lemonaki et al. (23) showed that lower cognitive flexibility abilities—but not working memory and inhibition—predicted higher burnout levels. Nevertheless, both studies focused only on the examination of executive functions while they measured this relationship only at two different time points. Hence, it still remains impossible for the form of change of these two variables over time to be determined and the results could possibly reflect measurement error and not a true change over time (24).
Although the cognitive deficits in clinical burnout have been widely recognized (21, 25), the results among non-clinical burnout populations remain inconclusive. Physiological studies suggest the negative effects of burnout as it leads to a decrease of the brain-derived neurotrophic factor (BDNF) (26); a protein which plays in important role on neuroplasticity (27). Decrease BDNF levels have been observed to mediate the negative effects of non-clinical burnout on cognitive functioning (28); a result which indicates that even at its early stages, burnout can disrupt normal brain and cognitive functioning. Studies have observed working memory deficits among non-clinical burnout employees (29) while others have failed to find cognitive impairments (30). Interestingly, some studies observed greater verbal working memory skills (31). A more recent study provides mixed results as the researchers showed that cynicism was negatively related to visuospatial skills but positively related to automatic processing skills (32); possibly indicating the employees’ activation of strategies in order to amplify their efforts during the initial burnout stages.
The sparse evidence regarding the cognitive patterns that characterize non-clinical burnout do not allow for drawing safe conclusions. Two theories that could explain the positive associations between non-clinical burnout and cognitive functioning, and in which the current study draws on, are the cognitive reserve (CR) and the self-regulation theories. The CR theory (33) suggests that when individuals carry out challenging tasks they employ the cognitive reserve process which permits them to use those cognitive strategies and brain networks that are more efficient and thus, enable them to cope with failure. Self-regulation theory (34) concerns one’s ability to inhibit a prepotent response and guide their cognitive, affective and behavioral sources for attaining a goal. That is, an individual’s self-regulation processes enable them to direct their cognitive resources on completing a task (35). Hence, non-clinical burnout employees might be still able to self-regulate and initiate the cognitive reserve in order to achieve optimal performance; a process which could possibly explain the observed greater cognitive performance in certain non-clinical burnout employees. In line with the above theoretical arguments, we hypothesize that:
Hypothesis 1: Non-clinical burnout will be positively related to cognitive functioning.
Depression and anxiety are two mental health problems that often coincide with burnout. This concurrence is so frequent which—along with their conceptual and behavioral similarities—have led to a debate among researchers on whether burnout is distinct—or another form—from these two psychological phenomena (36, 37). So far, the research evidence is inconclusive as some argue that burnout is a specific form of depression (36) while others suggest that burnout is a distinct concept (38); indicating also the importance of developing targeted clinical examinations of the working populations. Recent studies show that although burnout is accompanied by depressed mood and distressed feelings (6, 39), these feelings do not constitute robust and stable burnout characteristics, instead they might result as a reaction to burnout’s onset (39).
Regarding the relationship between burnout and depression, four theoretical models have been proposed: (1) the stability model which proposes that, although burnout and depression are associated with each other, they are independent from one another (40); (2) the burnout-as-antecedent model which suggests that burnout leads to depression and not the opposite (41); (3) the burnout-as-consequence model which assumes that depression leads to burnout and not vice versa (42); (4) the reciprocal effects model which posits that the second and third models are both true (43). Considering the relatively stable significant associations between burnout and depression when examining their predictive relationship, the most comprehensive model to consider is the reciprocal effects model. Although these models concern the burnout-depression relationship, in view of the lack of a similar theoretical framework in this study the same argumentation was assumed for the burnout-anxiety relationship.
Drawing on the above, we suggest that burnout is bidirectionally associated with depression and anxiety but it is a distinct concept. On this basis, the following hypothesis was formulated:
Hypothesis 2: Burnout will be moderately and positively related to depression and anxiety.
Depression and anxiety have been linked with cognitive deficits pertaining to memory (44) and executive functions (45, 46). However, most relevant studies focus on clinical populations. Ganguli et al. (47) showed that depressive symptoms among non-clinical populations were cross-sectionally, but not prospectively, associated with cognitive impairment. To the authors’ knowledge, the examination of everyday anxiety in non-clinical populations so far has received no attention as most studies focus on the effects of specific anxiety disorders on cognitive functions, such as obsessive compulsive (48) and post-traumatic disorder (49). An additional limitation concerns the insufficient evidence examining the role of cognitive functions in the onset of depression and anxiety. Studies have shown that individuals with lower cognitive abilities are more susceptible in developing depression (50) and anxiety (51). This study sought to elucidate the nature of the causality between cognitive functioning and depression, and anxiety.
Based on the above empirical argumentation we propose that:
Hypothesis 3: Non-clinical depression and non-clinical anxiety will be related to lower cognitive performance.
Hypothesis 4: Individuals with poorer cognitive abilities will exhibit higher depression and anxiety levels.
An important area in the burnout research is the investigation of non-work-related factors that can contribute to—or protect against—its onset. Most studies focus on the effects of perceived social support (friend, co-worker support) on mental health (52, 53). Considering the COVID-19 pandemic challenges and the fact that many employees had to work from home, the examination of the effects of family on employees’ mental health is of importance. Although limited, greater levels of perceived family support have been found to protect against burnout onset whereas poor perceived family support appears to enhance it (54, 55). The traditional conceptualization of depression and anxiety mainly focuses on the interpersonal factors affecting the two mental health issues. Nevertheless, although greater levels of family support can reduce mental health problems the reverse could also hold true; i.e., depression and anxiety may lead to a reduction in the quality of one’s family relationships (56). According to Coyne’s interactional theory of depression, depressed individuals provoke negative interaction patterns with others leading to a rejection from them which further increases their depressive feelings, creating a vicious circle (57). Thus, family support could act both as a consequence and contributing factor of burnout, depression and anxiety suggesting mutual reinforcing relationships (58). Although family support has been observed to facilitate cognitive performance (59), the relevant research evidence is sparse.
In line with the above empirical evidence, we hypothesize:
Hypothesis 5: Perceived family support will be negatively related to burnout, depression and anxiety, and positively associated with cognitive performance.
Hypothesis 6: Higher burnout, depression and anxiety levels will predict lower feelings of perceived family support.
As most studies mainly focus on clinical populations, in the present study we sought to examine non-clinical populations via a longitudinal design. Moreover, considering that executive functions are the most studied cognitive functions, we measured a broad range of cognitive functions.
The present study adds to the current literature in four ways. Firstly, by elucidating the association between non-clinical burnout and cognitive functioning and whether cognitive impairment is a burnout consequence, or employees with poorer cognitive abilities are more susceptible in developing burnout. Next, we aim to explore the causality of non-clinical depression and anxiety with cognitive functioning. Third, we endeavor to clarify the nature of the burnout-depression and burnout and anxiety relationships. Lastly, we examine the role of perceived family support in cognitive functioning, burnout, depression, and anxiety.
The ethical procedures according to the declaration of Helsinki when conducting research with human participants were followed. All participants agreed and signed an informed consent form for voluntary participation prior to their participation in the research at all three times of assessment.
Following the methodological procedures of previous longitudinal studies that examined both cross-sectionally (12, 60, 61) and longitudinally (20, 21, 62) the burnout—cognitive functioning relationship, we conducted a baseline study in order to gain an appreciation of the participants’ baseline characteristics (32) and how they developed over time. The present study concerns the longitudinal results after the completion of all three-time measurements.
Details regarding the procedures that were followed have been previously described (32). As both brief and extended time lags can decrease the chances of detecting the effects of the independent to the depended variable (63), participants were examined within an 8 and 17-month period interval after the baseline. That is, after the completion of each wave assessment, the participants who had initially attended the cognitive evaluation were first conducted to participate in the follow-up assessment. The baseline assessment was conducted between September 2018 and January 2019.
The majority of research in the area of burnout suffers from the problem of common method variance among the related survey instruments. The present research avoids this problem by involving participants in an exhaustive in-person cognitive functioning paper-and-pencil test. The structured interview lasted 60 min on average. This assessment procedure is the most reliable and valid way to assess cognitive functioning among individuals, but the interview is time-consuming and demanding for non-clinical burnout participants; and thus, it is more reliable for detecting any cognitive impairments (see Figure 1 for a schematic presentation of the procedure).
The participants were Greek employees of the general working population. Of the 104 participants who were assessed at baseline (T1), 72 of them agreed to participate at the first follow-up (T2) and 55 at the second follow-up (T3). Post hoc G*Power analysis with a medium effect size (f2 = 0.15) revealed a sufficient sample size to identify at least medium effects with a statistical power > 0.80 (β = 0.88) (64). The initial sample was contacted either by phone or in person; and by phone during the two follow-ups. Exclusion criteria included neurological disorders that could affect cognitive functioning (i.e., traumatic brain injury, epilepsy, multiple sclerosis).
Burnout was assessed by administering the Maslach Burnout Inventory—General Survey (MBI-GS) (65); a 16-item Likert-type scale designed to measure the three burnout subscales. All three subscales exhibited good reliabilities at all three time points with Cronbach’s alphas: αt1 = 0.90, αt2 = 0.92 and αt3 = 0.94 for exhaustion; αt1 = 0.71, αt2 = 0.79 and αt3 = 0.83 for cynicism; and αt1 = 0.84, αt2 = 0.85 and αt3 = 0.78 for personal efficacy. The McDonald’s omegas were ωt1 = 0.90, ωt2 = 0.92, ωt3 = 0.94 for exhaustion; ωt1 = 0.73, ωt2 = 0.80, ωt3 = 0.85 for cynicism; and ωt1 = 0.84, ωt2 = 0.82, ωt3 = 0.80 for personal efficacy.
The Hospital Anxiety and Depression Scale (HADS) is comprised of two 7-item subscales for measuring self-reported anxiety and depression (66) and it can be used in both patient and healthy populations (67). Scores ≥ 8 indicate potential case of depression and/or anxiety. Cronbach’s alphas were αt1 = 0.74, αt2 = 0.79 and αt3 = 0.79 for depression, and αt1 = 0.84, αt2 = 0.83 and αt3 = 0.85 for anxiety; the respective McDonald’s omegas were: ωt1 = 0.74, ωt2 = 0.79, ωt3 = 0.74 for depression ωt1 = 0.84, ωt2 = 0.84, ωt3 = 0.85 for anxiety.
The Julkunen Family Support Scale (FSS) (68) consists of 13 items and assesses individual’s subjective feelings of perceived family support; scores > 37 suggest high sense of perceived family support. Cronbach’s alphas were αt1 = 0.81, αt2 = 0.80 and αt3 = 0.82, and McDonald’s omegas were ωt1 = 0.90, ωt2 = 0.81, ωt3 = 0.80.
Seven different cognitive tasks were administered for assessing a wide variety of cognitive functions. Executive functions (i.e., inhibition, interference control, cognitive flexibility, switching, attention/speed of processing) were tested using the Stroop task and the Trail Making test (parts A and B) (69, 70). Auditory working memory was tested with the Digit Span task from Wechsler’s Adult Intelligence Scale Revised (WAIS-R) (71) while visuospatial working memory was assessed using the Corsi Block—Tapping Span task (backwards) (72). Visuospatial skills and visuospatial short-term and long-term memory were measured with the Taylor Complex Figure Test (73). Episodic memory was tested with the Short Story (immediate and delayed recall of a short story) (74). Prospective memory was examined with the use of a self-made test advised by Eskildsen et al. (12).
All tests were administered in a standardized sequence at all three measurements.
All statistical analyses were performed on SPSS (v.21). One-way ANOVA compare means were conducted to explore for any potential differences between the participants who continued with the follow-ups and the participants who dropped out. Linear mixed model analysis was performed in order to examine for potential predictive relationships. One advantage of this type of analysis is that it uses the full dataset to estimate the examined associations reducing the post hoc volunteer bias (75). The random effects model was chosen. Model selection was based in an unstructured covariance type. The random effects model was chosen for two reasons: (1) we wanted to examine the effects of the predictor variable to the dependent across the three time points and (2) due to the importance of allowing the intercepts for each participant to be different in longitudinal studies (76). Specifically, we specified both participants and time to be correlated with random effects with a scaled identity repeated covariance type. Next, the three MBI-GS subscales were set as covariates and each cognitive task, the total scores on the HADS (depression and anxiety separately) and FSS were considered as dependent variables. Additionally, the total HADS and FSS scores (independently) were set as covariates and each cognitive task and each of the three MBI-GS subscales were set as dependent variables. As not all participants were living with someone else, the linear mixed models, where the FSS total score had been set as the predictive factor, were based on a smaller sample size (N = 80). Statistically significant results were examined for reversed associations. P-values < 0.05 were considered as statistically significant.
All variables were normally distributed as skewness and kurtosis indices were within the normal range. Mahalanobis distance (77) was used in order to identify for multivariate outliers. Two multivariate outliers were detected. However, considering that exclusion of outliers in studies with multiple observations can result in a restriction bias (78), we decided to include the two outliers in the analysis.
Table 1 shows participants’ descriptive characteristics across the three time points. Although there was a statistically significant difference between groups at T1 and T3 as determined by one-way ANOVA [F(2, 228) = 3.482, p = 0.032], a Tukey post-hoc test did not reveal any significant differences between groups across the three time points. Thus, as the participants at all three time points were mainly missing at random, we expected unbiased estimates. Table 2 depicts the significant correlations observed between participants’ descriptive characteristics at T1 and the scores on the MBI-GS (T3) and performance on the cognitive tasks (T3). Concerning participants’ gender, male participants exhibited lower scores (t = -2.54, p < 0.05) on the personal efficacy subscale (M = 4.50, SD = 1.33) comparing to the female participants (M = 5.18, SD = 0.64). With respect to family status, as determined by one-way ANOVA there was a statistical significant difference between participants’ family status at T1 and exhaustion at T3 [F(2, 228) = 4.423, p = 0.008], and performance on the third condition on the Stroop test [F(2, 228) = 3.408, p = 0.024]. Particularly, married participants exhibited significantly lower scores on the exhaustion subscale (M = 2.08, SD = 1.43) compared to the single participants (M = 3.65, SD = 1.56). Married participants performed lower on the third Stroop condition (M = -0.47, SD = 0.78) compared to the single participants (M = 0.37, SD = 0.96). None of the participants’ descriptive characteristics were associated with the scores on the HADS (T3) and FSS (T3) (see Supplementary Material for the correlations coefficients between burnout, depression screening, anxiety, perceived family support and cognitive tasks on each measurement point).
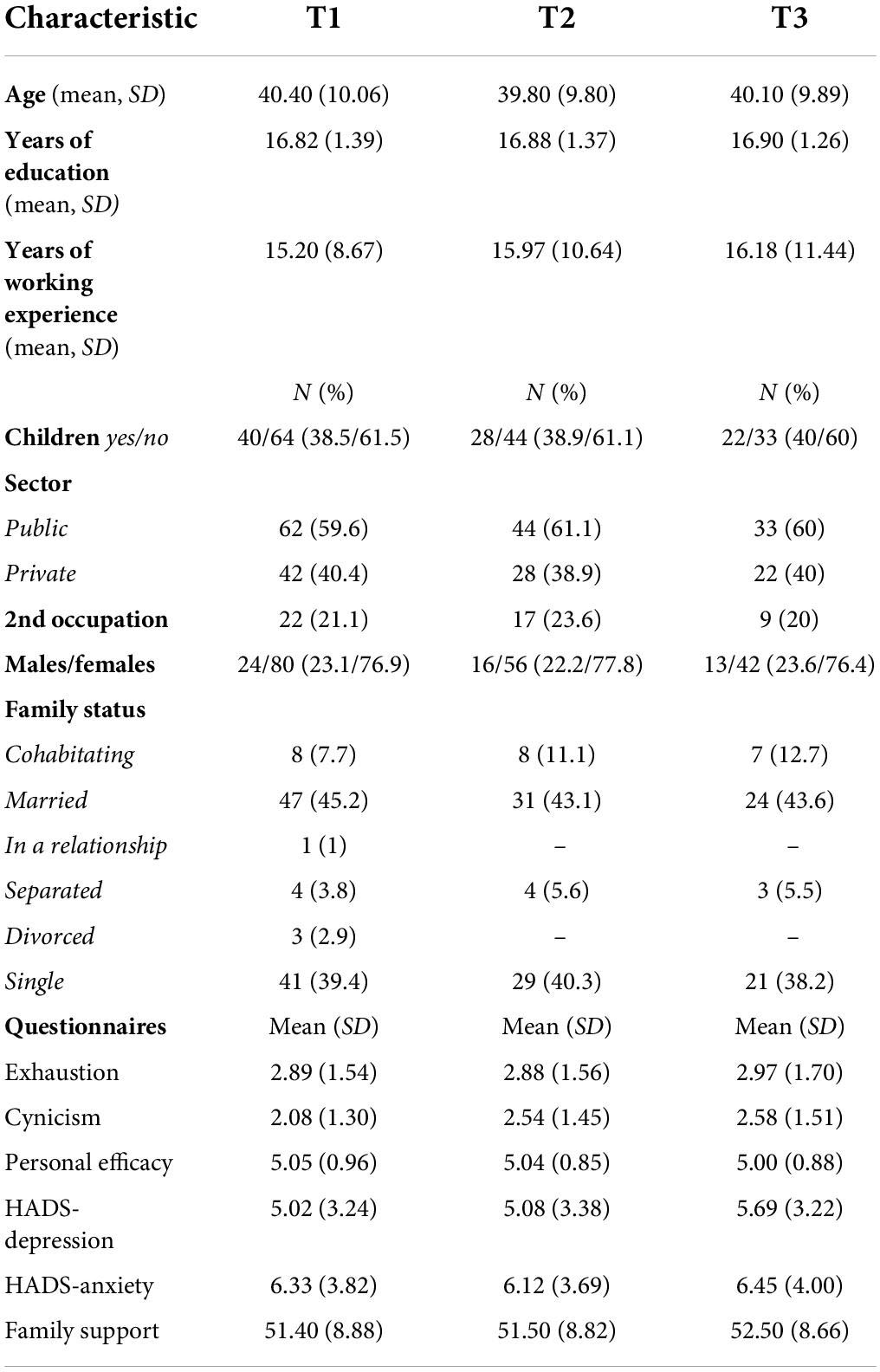
Table 1. Demographic characteristics of the participants at T1 (N = 104), T2 (N = 72), and T3 (N = 55).
As certain demographics were significantly correlated with the performance on certain cognitive tasks (see Table 2), we controlled for these variables. Exhaustion did not predict participants’ cognitive performance in any of the cognitive tasks. Cynicism had significant effects on cognitive performance on the TCFT-copy condition (95% CI = −0.23, −0.01, b = −0.12, p < 0.05) and on the first condition of the Stroop task (95% CI = 0.00, 0.22, b = 0.11, p < 0.05) across the three time points. When we examined for reversed associations, TCFT-copy condition did not have significant effects on cynicism [F(1, 5.179) = 3.60, p = 0.11] while performance on the first Stroop condition had significant effects on cynicism (95% CI = 0.00, 0.38, b = 0.19, p < 0.05). Personal efficacy significantly predicted participants’ performance on the incongruent Stroop condition (95% CI = 0.00, 0.02, b = 0.01, p < 0.01) (see Table 3). When examined for reversed associations, the incongruent Stroop condition also significantly predicted personal efficacy (95% CI = 0.15, 0.53, b = 0.28, p < 0.01) (see Figure 2 for a schematic presentation of the results).
No significant effects of depression screening and anxiety on cognitive performance were observed (all ps > 0.05).
Exhaustion significantly predicted both depression screening (95% CI = 0.57, 1.13, b = 0.85, p < 0.01) and anxiety (95% CI = 0.73, 1.40, b = 1.07, p < 0.01) while it did not have any effects on perceived family support. When examined for reversed associations, both depression screening (95% CI = 0.89, 0.20, b = 0.149, p < 0.01) and anxiety (95% CI = 0.11, 0.21, b = 0.16, p < 0.01) predicted exhaustion. Cynicism was found to have significant effects on depression screening (95% CI = 0.55, 1.11, b = 0.83, p < 0.01) anxiety (95% CI = 0.44, 1.12, b = 0.78, p < 0.01) and perceived family support (95% CI = −2.14, 0.20, b = −1.17, p < 0.05). Personal efficacy had significant effects on anxiety (95% CI = −1.62, −0.48, b = −1.05, p < 0.01) and depression screening (95% CI = −1.42, −0.21, b = −0.81, p < 0.01). No significant effects of personal efficacy in perceived family support were found (see Table 4). When examined for reversed associations, depression screening (95% CI = 0.12, 0.24, b = 0.18, p < 0.01), anxiety (95% CI = 0.10, 0.20, b = 0.15, p < 0.01) and perceived family support (95% CI = −0.06, −0.07, b = −0.03, p < 0.05) had significant effects on cynicism. Moreover, both depression screening (95% CI = −0.18, −0.07, b = −0.12, p < 0.01) and anxiety (95% CI = −0.09, −0.20, b = −0.05, p < 0.01) had significant effects on personal efficacy (see Tables 4, 5).
Perceived family support significantly predicted anxiety (95% CI = −0.20, −0.06, b = −0.13, p < 0.01) and depression screening (95% CI = −0.20, −0.07, b = −0.13, p < 0.01). When examined for reversed associations, depression screening (95% CI = −1.30, −0.46, b = −0.88, p < 0.01) and anxiety (95% CI = −1.07, −0.29, b = −0.68, p < 0.01) also had significant effects on perceived family support. With respect to cognitive functioning, perceived family support had significant effects on participants’ performance on the TCFT-delayed recall condition (95% CI = 0.00, 0.00, b = 0.00, p < 0.01). When examined for reversed associations, performance on the TCFT-delayed recall condition did not predict the levels of perceived family support [F(1, 163.680) = 1.90, p = 0.16] (see Tables 4, 5).
The objectives of the present study were to examine (1) the causality between non-clinical burnout and cognitive functioning, (2) the causality between self-reported depression and anxiety with cognitive performance, (3) the nature of the relationship between burnout and depression screening, and burnout and anxiety, and (4) the role of perceived family support in mental health and cognition.
Our results did not provide robust evidence that non-clinical burnout affects cognitive performance. However, some interesting results were observed. Contrary to our expectations and previous studies (22), baseline exhaustion was not a predictive factor of cognitive functioning. Nonetheless, both cynicism and personal efficacy had significant effects on participants’ performance in certain cognitive tasks (see Figure 2). Particularly, cynicism negatively affected visuospatial abilities while it had positive effects on automatic processes. When we examined for reciprocal associations, visuospatial skills did not predict cynicism, suggesting that decreased visuospatial skills are a consequence of burnout; a cognitive deficit that has been observed in clinical burnout as well (79). By way of contrast, automatic processes had a positive and bidirectional relationship with cynicism. This observation is in line with—and somewhat can be explained by—the findings of Van Dam et al. (80). Specifically, the researchers showed that employees who reported high burnout levels were able to efficiently perform on cognitive tasks and applied high-effort strategies but they also experienced greater distress during task performance. Thus, current results could reflect employees’ struggles to apply high-effort strategies (i.e., by increasing their automatic processing skills) in order to cope with the given task. A positive and reciprocal relationship between personal efficacy and executive functions (inhibition and switching) was also observed. This result is similar to the study of Morgan et al. (81) who observed that greater personal efficacy levels were associated with greater executive functions suggesting that employees’ perception of personal efficacy might be responsible for maintaining optimal cognitive performance.
In line with the CR (33) and self-regulation (34) theories, we argued that successful self-regulation enables employees to activate their cognitive reserve processes in order to optimize their performance. Perhaps, when employees who experience high cynicism levels start to become aware of a depletion of their mental and physical energy, they start to deploy more cognitive resources such as automatic processing skills, which are effortless and implicit and thus, easier to employ. Automatic processing is based on well-learned information (e.g., word reading) and is cue-driven (i.e., is triggered by the context and it is not intentional). Hence, it is an unconscious process which requires few attentional resources and it is more likely to occur among consistent learning environments (82). Greater performance on cognitive tasks that are reliant on automatic processing, such as the Stroop task (83), could indicate that employees who are high on both cynicism and personal efficacy do not yet lack the emotional resources that are needed in order to engage in greater cognitive efforts. Self-efficacy concerns individuals’ judgments on how sufficient they are in accomplishing a task (84) and it has been found to be related with a greater sense of purpose and control (85). Perhaps, employees who are at the initial burnout stages (i.e., high cynicism levels), but also experience a high sense of self-competency, are able to successfully regulate themselves and deploy more cognitive resources in order to compensate for their difficulties.
The reverse association between automatic processes and inhibition at T1 and cynicism, and personal efficacy at T3, respectively, also emphasize the role of executive control in burnout onset. According to the strain vulnerability hypothesis (86), individuals with poor cognitive abilities are more susceptible to stressful stimuli; a hypothesis that has been supported by other researchers as well (19). That is, employees with greater executive functions probably are less intimidated by the stressful working conditions (e.g., high job demands), they are more capable in adjusting their behavior when they face new or challenging work-related tasks and as a result, they experience greater personal efficacy; resulting in a positive spillover effect (87). An observation which could also explain the cognitive resilience among non-clinical burnout populations.
Present results extend our baseline findings (32) by indicating that high scores on certain burnout dimensions can be long-lasting and emphasize the complexity of the nature of relationship between burnout and cognitive functions. Current findings could explain the results of Castaneda et al. (31) who observed positive associations between burnout and cognitive performance, but the cross-sectional design of their study did not allow for the examination of reciprocal associations. Hence, it is possible that participants’ high executive functions led to better cognitive performance. Our findings are in contrast with previous longitudinal studies which suggested that executive functioning deficits are a burnout consequence (22, 23). However, Lemonaki et al. (23) indicated that poorer cognitive flexibility is associated with a later burnout onset. Moreover, our results are also in disagreement with cross-sectional studies that did not observe any significant links between burnout and cognitive functioning (30, 88) as well as with the cross-sectional study of van Dijk et al. (29) who found that non-clinical burnout employees exhibited lower performance comparing to healthy individuals on demanding working memory tasks.
An additional remark concerns the arguments of previous studies regarding the inclusion of cognitive impairments as a core burnout dimension (5, 6). Current findings give partial support to the burnout conceptualization which considers cognitive impairments as a core burnout dimension. Although, visuospatial skills were identified as a burnout consequence, present results show that the relationship between burnout and cognitive functioning is more complex than previously might have been thought. Future studies need not only to investigate the dynamic relationship between burnout and cognitive functions but also need to explore a wide range of cognitive domains in order to gain a more complete picture of this relationship before we consider cognitive impairments as a burnout dimension.
Present results did not show any effects of self-reported depression and anxiety on cognitive functioning; a result that comes in contrast with studies that observed cognitive impairments in individuals suffering from depression (89) and anxiety (90). Most studies identifying cognitive deficits in depression and anxiety examined clinical populations. In the present study the participants reported mostly mild depression and anxiety feelings. Thus, it is possible that cognitive impairment is mainly observed among clinical populations either as a consequence or a cause of depression and/or anxiety. Indeed, it is possible that individuals who experience cognitive deficits might manifest depressive and/or anxiety symptoms due to the realization of those deficits (91). Importantly, as depression and anxiety patients often receive medication treatments, one cannot rule out the possibility that the cognitive deficits could emerge as a result of the medication the patients receive and not from their clinical condition per se.
Concerning perceived family support, it had a positive impact on long-term visuospatial memory. Other studies have also shown the beneficial effects levels of family (59) and social (92) support on cognitive performance. It has been proposed that perceived support and social engagement challenge our cognitive system by stimulating it through the interaction with the members of our social and family networks (93) and thus, enhances individuals’ cognitive reserve (33). Hence, this cognitive stimulation through our social interactions could result to better cognitive performance. The importance of social support becomes evident from research evidence which suggests that psychosocial factors can influence the cognitive functioning of individuals who are at-risk in developing dementia (94).
Present results revealed reciprocal associations between burnout and depression screening, and burnout and anxiety displaying significant and positive longitudinal stability. These results are in agreement with previous longitudinal studies where a reciprocal relationship between burnout and depression was observed (43). Importantly, all three burnout components were significantly associated with both depression screening and anxiety suggesting that the two latter psychological phenomena are related equally to overall burnout levels and not to specific burnout components; results that indicate the importance of research studies taking into consideration the multifactorial dimension of burnout and not only its certain components. However, the effect sizes among the variables when the three burnout components were set as the predictors were very strong while the effect sizes when depression screening and anxiety predicted burnout were weaker. This observation advocates toward the hypothesis that burnout could be a precursor of these two psychological phenomena, giving support to the approach of Tavella et al. (39) who argued that depressive symptoms might arise as a consequence of burnout’s effects. Indeed, burned-out employees might be more susceptible in developing depression and anxiety. Hakanen and Schaufeli (41) in their three-wave study showed that burnout predicts depression and not the opposite. However, considering the fact that most longitudinal studies support reciprocal paths, this view cannot be considered strong enough to support the hypothesis that burnout is an antecedent of depression and anxiety. More longitudinal studies examining the reciprocal associations of burnout with depression and anxiety are needed in order to gain a better understanding of how these associations develop over time. Moreover, the investigation of the role of the context (i.e., work-specific and context-general) and how it affects individuals’ mental health could provide further insights on the nature of the two relationships (41).
An additional goal of this study was to examine the bidirectional influences of perceived family support with burnout, depression screening and anxiety. Our results showed robust evidence that perceived family support has reciprocal associations with certain aspects of burnout, depression screening and anxiety in the directions expected. Specifically, high levels of perceived family support were found to decrease cynicism, depression screening and anxiety over time whereas high cynicism, depression screening and anxiety levels negatively affected perceived family support. Nevertheless, the effects of perceived family support on these three factors were higher comparing to the opposite path. These results emphasize the importance of family context in mental health as it can either protect against the development of psychological problems or it can be disrupted by pre-existing psychological difficulties. This observation could be explained on the basis of the conservation of resources model (COR) (95). COR model’s key tenet is that individuals are prompted to protect their resources (i.e., everything they value such as energy, relationships etc.) and when these resources are either threatened or lost, then stress emerges. The COR model indicates the importance of social support which acts as a resource pool when the personal resources have been exhausted (96). Present results recognize the role of perceived family support as a potential protective mechanism against mental health problems. That is, distressed individuals might turn to their family members in order to help them compensate for their lost resources. The COR model could also explain this reversed effect. When negative feelings start to emerge, then individuals start to avoid interactions with their family members as an attempt to preserve their energy resources; as quality family relationships involve active participation among family members, posing demands on the distressed individual’s already limited resources. The reversed associations also give support to Coyne’s interactional theory of depression (1976) and indicate that, not only depression, but other mental health difficulties as well can result in negative interactions with family members and poorer quality of family relations.
Surprisingly, perceived family support was significantly associated only with cynicism, but not with the exhaustion and personal efficacy burnout dimensions. The main conceptual burnout model posits that the three burnout dimensions develop in a subsequent order. That is, high exhaustion feelings lead to high cynicism levels which, consequently, leads to inefficacy (97). However, others have considered cynicism as a coping mechanism against stress and burnout (98, 99). It has been proposed that cynicism can result in negative associations with prosocial behavior and interpersonal conflicts (100, 101). Prosocial behavior is a social behavior that enhances both the wellbeing and integrity of other people or society as a whole via committing in positive behaviors such as helping, cooperating and supporting (102). Hence, a possible interpretation is that high levels of cynicism could result in a more cynical behavior toward family members.
The results indicate that visuospatial functioning deficits are a non-clinical burnout consequence. Visuospatial functions are responsible for the mental representation of objects and spatial relationships, and they allow us to navigate through our environment (103). Thus, these observations posit significant concerns regarding employees’ personal (e.g., driving) and work life, especially for those occupations where integral visuospatial abilities are of importance such as professional drivers, engineers and surgeons as diminished visuospatial skills could put at risk client and patient safety [for a mini review see Koutsimani and Montgomery (104)]. Executive functions are also of importance when encountering stressful situations in the workplace while well-established skills can facilitate performance at the initial burnout stages. As prevention is more desirable than intervention, the building of prevention strategies focusing on the enhancement of executive functions as well as employees’ cognitive strengths could help tackle those conditions resulting in burnout. Although we observed significant links between burnout and cognitive functions, our results are not robust enough to suggest that cognitive impairments could be a core burnout dimension. Moreover, present results support the notion that burnout is distinct from both depression and anxiety. However, these three mental health problems have reciprocal reinforcing associations. Practitioners could build intervention programs focusing on the alleviation of the symptoms of all three psychological phenomena, as all three appear to spill over to individuals’ work and personal life areas. Based on the reinforcing associations, intervention programs could focus on diminishing depression and anxiety feelings by helping employees to gain a more positive perspective toward life which could lead toward a more satisfied outlook of their work, and vice versa. Considering the mutual relationships between perceived family support, cynicism, depression and anxiety, practitioners should consider in adapting techniques focusing on the enhancement of one’s family ties; referring individuals with mental health problems to family therapy could be beneficial for both patients and their families. Finally, practitioners could also consider integrating the strengthening of family ties within cognitive training and neurorehabilitation programs.
Overall, the results of the present study offer important insights on the relationship of burnout with cognitive functioning, depression screening and anxiety and they also underline the important role of family context. Future longitudinal studies are needed in order to disentangle the role of these factors.
The present study is not without limitations. The sample size was relatively small, thus making our results more susceptible in Type I error. Future studies with larger sample sizes will allow a better comprehension of the variables’ predictive associations. Considering that we used the snowball sampling method we cannot rule out the possibility of a potential sampling bias and a higher margin of error. Although no statistically significant differences were observed between the participants who continued with the study and the participants who dropped out, there was a 50% dropout rate at T3 which could result in a bias dropout and thus, to a loss of representativeness of the sample. Indeed, participants at T3 reported higher cynicism levels hence, suggesting that participants’ non-response occurred not at random (NMAR) (105). Moreover, burnout, depression, anxiety and perceived family support were examined through self-reported questionnaires, thus participants’ answers could be affected by potential self-report biases. In addition to this, both depression and anxiety were assessed via a single scale; i.e., the HADS, Although HADS has been found to be appropriate for non-clinical populations (67), the scale covers a limited array of the symptoms characterizing both depression and anxiety. Scales that cover the full range of depression and anxiety symptoms could have provided different results. Even though we measured all studied variables across three different time points, we cannot infer causality. Due to practical reasons, we chose to assess the variables of interest in an 8 and 17-month period interval after the baseline examination. However, the chosen time lags between each wave might not have been sufficient to detect real changes. Indeed, the lack of consensus on the appropriate time lags and thus, the arbitrary time points that are chosen is in itself a methodological limitation in longitudinal studies (106); longer, or shorter, time frames between time intervals in future longitudinal studies could provide further information on the exact associations among these relationships. Lastly, although we examined a broad range of cognitive functions of varying difficulty, more complex cognitive tasks when examining non-clinical burnout employees in future studies should be considered. In fact, although our results show that visuospatial deficits are a cynicism outcome, we cannot overlook the possibility of other cognitive functions underlying this relationship. That is, we assessed visuospatial skills with the administration of a constructional task (i.e., TCFT-copy condition); a task that integrates visual perception with motor response and thus, it includes a spatial component (107). Performance on constructional tasks can be affected by other functions including basic attentional abilities (i.e., sustained and visual attention, alertness and focus). Motor skill performance has been associated with attention (visual and alertness) (108). Although we measured for executive attention (via the Stroop task and TMT—part B) and visual attention (via TMT part—A), it is possible that deficits in these areas might have been missed due to the lack of complexity of the tasks on the general population. The TCFT—copy condition demands competent attention and focus in order to recognize the complex figure and approach the visual information (109). Thus, basic attention deficits that might went undetected could have mediated the relationship between cynicism and visuospatial skills; emphasizing the need for thorough cognitive screening when examining healthy populations.
As non-clinical burnout refers to the early burnout stages where employees are still working, it is of importance to detect its symptoms at this early phase in order to prevent individuals from reaching clinical stages. This study emphasizes the role of executive functions in employees’ mental (emotional and cognitive) resilience while they also reveal the adverse effects of non-clinical burnout in visuospatial abilities; a cognitive domain that has not received much attention in the relevant literature. Although moderate burnout levels (i.e., high cynicism levels) are sufficient to affect optimal cognitive performance, high executive function abilities can protect against both cognitive decline and certain burnout aspects. Our evidence points to the distinction of burnout from depression and anxiety but also support that burnout is not independent from the two psychological syndromes. Additionally, the findings of this study highlight the role of other psychosocial non-work-related factors in both mental health and cognition. Overall, present findings reveal the practical implications of the early detection of burnout and the role of perceived support in both cognitive functioning and mental health. It is of importance to know which factors can affect cognitive performance and mental health, as this will help in the development of more targeted intervention programs.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study.
PK and AM: conceptualization, methodology, resources, software, and visualization. PK: data curation, formal analysis, funding acquisition, investigation, and writing—original draft. AM: project administration, supervision, validation, and writing—review and editing. Both authors have read and agreed to the published version of the manuscript.
This research was co-financed by Greece and the European Union (European Social Fund- ESF) through the Operational Programme “Human Resources Development, Education and Lifelong Learning” in the context of the project “Strengthening Human Resources Research Potential via Doctorate Research” (MIS-5000432), implemented by the State Scholarships Foundation (IKY).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.978566/full#supplementary-material
1. Leka S, Jain A, World Health Organization. Health Impact of Psychosocial Hazards at Work: An Overview. Geneva: World Health Organization (2010).
2. Kristensen TS, Borritz M, Villadsen E, Christensen KB. The copenhagen burnout inventory: a new tool for the assessment of burnout. Work Stress. (2005) 19:192–207. doi: 10.1080/02678370500297720
3. Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. (2001) 52:397–422. doi: 10.1146/annurev.psych.52.1.397
4. Schaufeli WB, Salanova MS. Burnout, boredom and engagement in the workplace. Introd Contemp Work Psychol. (2014) 12:293–320.
5. Desart S, Schaufeli W, De Witte H. Op zoek naar een nieuwe definitie van burn-out. Tijdsch Steunpunt Werk. (2017) 1:90–1.
6. Schaufeli WB, Desart S, De Witte H. Burnout assessment tool (BAT)—development, validity, and reliability. Int J Environ Res Public Health. (2020) 17:9495. doi: 10.3390/ijerph17249495
7. Ahola K, Hakanen J, Perhoniemi R, Mutanen P. Relationship between burnout and depressive symptoms: a study using the person-centred approach. Burnout Res. (2014) 1:29–37. doi: 10.1016/j.burn.2014.03.003
8. Schonfeld IS, Bianchi R. Burnout and depression: two entities or one? J Clin Psychol. (2016) 72:22–37. doi: 10.1002/jclp.22229
9. van Dam A. Subgroup analysis in burnout: relations between fatigue, anxiety, and depression. Front Psychol. (2016) 7:90. doi: 10.3389/fpsyg.2016.00090
10. Airaksinen E, Larsson M, Forsell Y. Neuropsychological functions in anxiety disorders in population-based samples: evidence of episodic memory dysfunction. J Psychiatr Res. (2005) 39:207–14. doi: 10.1016/j.jpsychires.2004.06.001
11. Byers AL, Covinsky KE, Barnes DE, Yaffe K. Dysthymia and depression increase risk of dementia and mortality among older veterans. Am J Geriatr Psychiatry. (2012) 20:664–72. doi: 10.1097/JGP.0b013e31822001c1
12. Eskildsen A, Andersen LP, Pedersen AD, Vandborg SK, Andersen JH. Work-related stress is associated with impaired neuropsychological test performance: a clinical cross-sectional study. Stress. (2015) 18:198–207. doi: 10.3109/10253890.2015.1004629
13. Österberg K, Karlson B, Malmberg B, Hansen ÅM. A follow-up of cognitive performance and diurnal salivary cortisol changes in former burnout patients. Stress. (2012) 15:589–600. doi: 10.3109/10253890.2011.648972
14. Deligkaris P, Panagopoulou E, Montgomery AJ, Masoura E. Job burnout and cognitive functioning: a systematic review. Work Stress. (2014) 28:107–23.
15. Grossi G, Perski A, Osika W, Savic I. Stress-related exhaustion disorder–clinical manifestation of burnout? A review of assessment methods, sleep impairments, cognitive disturbances, and neuro-biological and physiological changes in clinical burnout. Scand J Psychol. (2015) 56:626–36. doi: 10.1111/sjop.12251
16. Miyake A, Friedman NP, Emerson MJ, Witzki AH, Howerter A, Wager TD. The unity and diversity of executive functions and their contributions to complex “frontal lobe” tasks: a latent variable analysis. Cogn Psychol. (2000) 41:49–100. doi: 10.1006/cogp.1999.0734
17. Diamond A. Executive functions. Annu Rev Psychol. (2013) 64:135–68. doi: 10.1146/annurev-psych-113011-143750
18. Michailidis E, Banks AP. The relationship between burnout and risk-taking in workplace decision-making and decision-making style. Work Stress. (2016) 30:278–92. doi: 10.1080/02678373.2016.1213773
19. Williams PG, Suchy Y, Rau HK. Individual differences in executive functioning: implications for stress regulation. Ann Behav Med. (2009) 37:126–40. doi: 10.1007/s12160-009-9100-0
20. Eskildsen A, Andersen LP, Pedersen AD, Andersen JH. Cognitive impairments in former patients with work-related stress complaints–one year later. Stress. (2016) 19:559–66. doi: 10.1080/10253890.2016.1222370
21. Jonsdottir IH, Nordlund A, Ellbin S, Ljung T, Glise K, Währborg P, et al. Working memory and attention are still impaired after three years in patients with stress-related exhaustion. Scand J Psychol. (2017) 58:504–9. doi: 10.1111/sjop.12394
22. Feuerhahn N, Stamov-Roßnagel C, Wolfram M, Bellingrath S, Kudielka BM. Emotional exhaustion and cognitive performance in apparently healthy teachers: a longitudinal multi-source study. Stress Health. (2013) 29:297–306. doi: 10.1002/smi.2467
23. Lemonaki R, Xanthopoulou D, Bardos AN, Karademas EC, Simos PG. Burnout and job performance: a two-wave study on the mediating role of employee cognitive functioning. Eur J Work Organ Psychol. (2021) 30:692–704. doi: 10.1080/1359432X.2021.1892818
24. Ployhart RE, Vandenberg RJ. Longitudinal research: the theory, design, and analysis of change. J Manage. (2010) 36:94–120. doi: 10.1177/0149206309352110
25. Krabbe D, Ellbin S, Nilsson M, Jonsdottir IH, Samuelsson H. Executive function and attention in patients with stress-related exhaustion: perceived fatigue and effect of distraction. Stress. (2017) 20:333–40. doi: 10.1080/10253890.2017.1336533
26. Chow Y, Masiak J, Mikołajewska E, Mikołajewski D, Wójcik GM, Wallace B, et al. Limbic brain structures and burnout—a systematic review. Adv Med Sci. (2018) 63:192–8. doi: 10.1016/j.advms.2017.11.004
27. Binder DK, Scharfman HE. Brain-derived neurotrophic factor. Growth Fact (Chur Switzerland). (2004) 22:123. doi: 10.1080/08977190410001723308
28. He S, Zhang Y, Zhan J, Wang C, Du X, Yin G, et al. Burnout and cognitive impairment: associated with serum BDNF in a Chinese Han population. Psychoneuroendocrinology. (2017) 77:236–43. doi: 10.1016/j.psyneuen.2017.01.002
29. van Dijk DM, van Rhenen W, Murre JM, Verwijk E. Cognitive functioning, sleep quality, and work performance in non-clinical burnout: the role of working memory. PLoS One. (2020) 15:e0231906. doi: 10.1371/journal.pone.0231906
30. McInerney S, Rowan M, Lawlor B. Burnout and its effect on neurocognitive performance. Irish J Psychol Med. (2012) 29:176–9. doi: 10.1017/S0790966700017213
31. Castaneda AE, Suvisaari J, Marttunen M, Perälä J, Saarni SI, Aalto-Setälä T, et al. Cognitive functioning in relation to burnout symptoms and social and occupational functioning in a population-based sample of young adults. Nordic J Psychiatry. (2011) 65:32–9. doi: 10.3109/08039488.2010.485328
32. Koutsimani P, Montgomery A, Masoura E, Panagopoulou E. Burnout and cognitive performance. Int J Environ Res Public Health. (2021) 18:2145. doi: 10.3390/ijerph18042145
33. Stern Y. What is cognitive reserve? Theory and research application of the reserve concept. J Int Neuropsychol Soc. (2002) 8:448–60. doi: 10.1017/S1355617702813248
34. Baumeister RF, Vohs KD. Self-regulation and the executive function of the self. Hand Self Identity. (2003) 1:197–217. doi: 10.1080/152988602317319302
35. Beal DJ, Weiss HM, Barros E, MacDermid SM. An episodic process model of affective influences on performance. J Appl Psychol. (2005) 90:1054–68. doi: 10.1037/0021-9010.90.6.1054
36. Bianchi R, Schonfeld IS, Laurent E. Burnout–depression overlap: a review. Clin Psychol Rev. (2015) 36:28–41. doi: 10.1016/j.cpr.2015.01.004
37. Sun W, Fu J, Chang Y, Wang L. Epidemiological study on risk factors for anxiety disorder among Chinese doctors. J Occup Health. (2012) 54:1–8. doi: 10.1539/joh.11-0169-OA
38. Koutsimani P, Montgomery A, Georganta K. The relationship between burnout, depression and anxiety: a systematic review and meta-analysis. Front Psychol. (2019) 10:284. doi: 10.3389/fpsyg.2019.00284
39. Tavella G, Hadzi-Pavlovic D, Parker G. Burnout: redefining its key symptoms. Psychiatry Res. (2021) 302:114023. doi: 10.1016/j.psychres.2021.114023
40. Idris MA, Dollard MF, Yulita. Psychosocial safety climate, emotional demands, burnout, and depression: a longitudinal multilevel study in the Malaysian private sector. J Occup Health Psychol. (2014) 19:291–302. doi: 10.1037/a0036599
41. Hakanen JJ, Schaufeli WB. Do burnout and work engagement predict depressive symptoms and life satisfaction? A three-wave seven-year prospective study. J Affect Disord. (2012) 141:415–24. doi: 10.1016/j.jad.2012.02.043
42. Armon G, Shirom A, Melamed S. The big five personality factors as predictors of changes across time in burnout and its facets. J Personal. (2012) 80:403–27. doi: 10.1111/j.1467-6494.2011.00731.x
43. Tóth-Király I, Morin AJ, Salmela-Aro K. Reciprocal associations between burnout and depression: an eight-year longitudinal study. Appl Psychol. (2020) 70:37. doi: 10.1111/apps.12295
44. DeLuca AK, Lenze EJ, Mulsant BH, Butters MA, Karp JF, Dew MA, et al. Comorbid anxiety disorder in late life depression: association with memory decline over four years. Int J Geriatr Psychiatry. (2005) 20:848–54. doi: 10.1002/gps.1366
45. Balderston NL, Vytal KE, O’Connell K, Torrisi S, Letkiewicz A, Ernst M, et al. Anxiety patients show reduced working memory related dlPFC activation during safety and threat. Depress Anxiety. (2017) 34:25–36. doi: 10.1002/da.22518
46. Eysenck MW, Derakshan N, Santos R, Calvo MG. Anxiety and cognitive performance: attentional control theory. Emotion. (2007) 7:336–53. doi: 10.1037/1528-3542.7.2.336
47. Ganguli M, Du Y, Dodge HH, Ratcliff GG, Chang C-CH. Depressive symptoms and cognitive decline in late life: a prospective epidemiological study. Arch Gen Psychiatry. (2006) 63:153–60. doi: 10.1001/archpsyc.63.2.153
48. Kuelz AK, Hohagen F, Voderholzer U. Neuropsychological performance in obsessive-compulsive disorder: a critical review. Biol Psychol. (2004) 65:185–236. doi: 10.1016/j.biopsycho.2003.07.007
49. Brewin CR, Kleiner JS, Vasterling JJ, Field AP. Memory for emotionally neutral information in posttraumatic stress disorder: a meta-analytic investigation. J Abnorm Psychol. (2007) 116:448-63. doi: 10.1037/0021-843X.116.3.448
50. Buthmann J, Cha DS, McIntyre RS. Does cognitive dysfunction predate the onset of incident depression? In: McIntyre RS, Cha DS editors. Cognitive Impairment in Major Depressive Disorder: Clinical Relevance, Biological Substrates, and Treatment Opportunities. Cambridge: Cambridge University Press (2016).
51. Zainal NH, Newman MG. Executive function and other cognitive deficits are distal risk factors of generalized anxiety disorder 9 years later. Psychol Med. (2018) 48:2045. doi: 10.1017/S0033291717003579
52. Prag PW. Stress, burnout, and social support: a review and call for research. Air Med J. (2003) 22:18–22. doi: 10.1016/S1067-991X(03)00021-X
53. Wang X, Shang S, Yang H, Ai H, Wang Y, Chang S, et al. Associations of psychological distress with positive psychological variables and activities of daily living among stroke patients: a cross-sectional study. BMC Psychiatry. (2019) 19:381. doi: 10.1186/s12888-019-2368-0
54. Drummond S, O’Driscoll MP, Brough P, Kalliath T, Siu O-L, Timms C, et al. The relationship of social support with well-being outcomes via work–family conflict: moderating effects of gender, dependants and nationality. Hum Relat. (2017) 70:544–65. doi: 10.1177/0018726716662696
55. Rupert PA, Stevanovic P, Hunley HA. Work-family conflict and burnout among practicing psychologists. Prof Psychol Res Pract. (2009) 40:54. doi: 10.1037/a0012538
56. Park M, Unützer J, Grembowski D. Ethnic and gender variations in the associations between family cohesion, family conflict, and depression in older Asian and Latino adults. J Immigr Minor Health. (2014) 16:1103–10. doi: 10.1007/s10903-013-9926-1
57. Coyne JC. Toward an interactional description of depression. Psychiatry. (1976) 39:28–40. doi: 10.1080/00332747.1976.11023874
58. Wong JJ, Frost ND, Timko C, Heinz AJ, Cronkite R. Depression and family arguments: disentangling reciprocal effects for women and men. Fam Pract. (2020) 37:49–55. doi: 10.1093/fampra/cmz048
59. Zhu S, Hu J, Efird JT. Role of social support in cognitive function among elders. J Clin Nurs. (2012) 21:2118–25. doi: 10.1111/j.1365-2702.2012.04178.x
60. Jonsdottir I, Nordlund A, Ellbin S, Ljung T, Glise K, Währborg P, et al. Cognitive impairment in patients with stress-related exhaustion. Stress. (2013) 16:181–90. doi: 10.3109/10253890.2012.708950
61. Österberg K, Karlson B, Hansen Å. Cognitive performance in patients with burnout, in relation to diurnal salivary cortisol: original research report. Stress. (2009) 12:70–81. doi: 10.1080/10253890802049699
62. Dalgaard VL, Hviid Andersen J, Pedersen AD, Andersen LP, Eskildsen A. Cognitive impairments and recovery in patients with work-related stress complaints–four years later. Stress. (2021) 24:294–302. doi: 10.1080/10253890.2020.1797673
63. Taris TW, Kompier MAJ. Cause and effect: optimizing the designs of longitudinal studies in occupational health psychology. Work Stress (2014) 28:1–8. doi: 10.1080/02678373.2014.878494
64. Faul F, Erdfelder E, Buchner A, Lang A-G. Statistical power analyses using G* Power 3.1: tests for correlation and regression analyses. Behav Res Methods. (2009) 41:1149–60. doi: 10.3758/BRM.41.4.1149
65. Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory. Mountain View, CA: CPP, Inc (2006). doi: 10.1016/B978-012373947-6.00062-3
66. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. (1983) 67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x
67. Crawford J, Henry J, Crombie C, Taylor E. Normative data for the HADS from a large non-clinical sample. Br J Clin Psychol. (2001) 40:429–34. doi: 10.1348/014466501163904
69. Reitan R, Wolfson D. The Halstead-Reitan Neuropsychological Test Battery: Therapy and Clinical Interpretation. Tucson, AZ: Neuropsychological Press (1985).
70. Stroop JR. Studies of interference in serial verbal reactions. J Exp Psychol. (1935) 18:643. doi: 10.1037/h0054651
71. Wechsler D. Wechsler Adult Intelligence Scale–Fourth Edition (WAIS–IV). (Vol. 22). San Antonio, TX: NCS Pearson (2008). 498 p. doi: 10.1037/t15169-000
72. Corsi P. Memory and the Medial Temporal Region of the Brain. Unpublished Doctoral Dissertation. Montreal, QB: McGill University (1972).
73. Hubley A. Scoring System for the Modified Taylor Complex Figure (MTCF). Unpublished Research. Prince George, BC: University of Northern British Columbia (1998).
74. Kosmidis MH, Bozikas V, Vlahou CH, Giaglis G. Neuropsychological Battery (Unpublished Work). Thessaloniki: Aristotele University of Thessaloniki (2011).
75. Brownell SE, Kloser MJ, Fukami T, Shavelson RJ. Context matters: volunteer bias, small sample size, and the value of comparison groups in the assessment of research-based undergraduate introductory biology lab courses. J Microbiol Biol Educ. (2013) 14:176–82. doi: 10.1128/jmbe.v14i2.609
76. Twisk JW. Applied Multilevel Analysis: A Practical Guide for Medical Researchers. Cambridge: Cambridge university press (2006). doi: 10.1017/CBO9780511610806
77. Mahalanobis P. On the generalised distance in statistics. Proc Natl Inst Sci India. (1936) 12:49–55.
78. Miller J. Short report: reaction time analysis with outlier exclusion: bias varies with sample size. Q J Exp Psychol Sect A. (1991) 43:907–12. doi: 10.1080/14640749108400962
79. Sandström A, Rhodin IN, Lundberg M, Olsson T, Nyberg L. Impaired cognitive performance in patients with chronic burnout syndrome. Biol Psychol. (2005) 69:271–9. doi: 10.1016/j.biopsycho.2004.08.003
80. Van Dam A, Eling P, Keijsers G, Becker E. Do employees with burnout prefer low-effort performance strategies? IIE Trans Occup Ergono Hum Fact. (2013) 1:190–201. doi: 10.1080/21577323.2013.828666
81. Morgan CA, Russell B, McNeil J, Maxwell J, Snyder PJ, Southwick SM, et al. Baseline burnout symptoms predict visuospatial executive function during survival school training in special operations military personnel. J Int Neuropsychol Soc. (2011) 17:494–501. doi: 10.1017/S1355617711000221
82. Schneider W, Shiffrin RM. Controlled and automatic human information processing: I. Detection, search, and attention. Psychol Rev. (1977) 84:1–66. doi: 10.1037/0033-295X.84.1.1
83. Kahneman D, Henik A. Perceptual organization. In: Kubovy M, Pomerantz J editors. Perceptual Organization and Attention. Hillsdale, NJ: Lawrence Erlbaum Associates (1981). p. 181–211. doi: 10.4324/9781315512372-7
84. Bandura A. Self-efficacy mechanism in human agency. Am Psychol. (1982) 37:122–47. doi: 10.1037/0003-066X.37.2.122
85. Benight CC, Bandura A. Social cognitive theory of posttraumatic recovery: the role of perceived self-efficacy. Behav Res Ther. (2004) 42:1129–48. doi: 10.1016/j.brat.2003.08.008
86. Broadbent DE, Cooper PF, FitzGerald P, Parkes KR. The cognitive failures questionnaire (CFQ) and its correlates. Br J Clin Psychol. (1982) 21:1–16. doi: 10.1111/j.2044-8260.1982.tb01421.x
87. Nilsson A, Bergquist M, Schultz WP. Spillover effects in environmental behaviors, across time and context: a review and research agenda. Environ Educ Res. (2017) 23:573–89. doi: 10.1080/13504622.2016.1250148
88. Wekenborg MK, Hill LK, Miller R, Stalder T, Thayer JF, Sophie Penz M, et al. Reduced self-regulation mirrors the distorting effects of burnout symptomatology on task difficulty perception during an inhibition task. Stress. (2018) 21:511–9. doi: 10.1080/10253890.2018.1479393
89. Yoon S, Shin C, Han C. Depression and cognitive function in mild cognitive impairment: a 1-year follow-up study. J Geriatr Psychiatry Neurol. (2017) 30:280–8. doi: 10.1177/0891988717723741
90. Ribbons K, Lea R, Schofield PW, Lechner-Scott J. Anxiety levels are independently associated with cognitive performance in an Australian multiple sclerosis patient cohort. J Neuropsychiatry Clin Neurosci. (2017) 29:128–34. doi: 10.1176/appi.neuropsych.16050085
91. Ganguli M. Depression, cognitive impairment and dementia: why should clinicians care about the web of causation? Indian J Psychiatry. (2009) 51(Suppl. 1):S29–34.
92. Zamora-Macorra M, de Castro EF, vila-Funes JA, Manrique-Espinoza BS, López-Ridaura R, Sosa-Ortiz AL, et al. The association between social support and cognitive function in Mexican adults aged 50 and older. Arch Gerontol Geriatr. (2017) 68:113–18. doi: 10.1016/j.archger.2016.10.005
93. Fillit HM, Butler RN, O’Connell AW, Albert MS, Birren JE, Cotman CW, et al. Achieving and maintaining cognitive vitality with aging. Mayo Clin Proc. (2002) 77:681–96. doi: 10.4065/77.7.681
94. Zuelsdorff ML, Engelman CD, Friedman EM, Koscik RL, Jonaitis EM, Rue AL, et al. Stressful events, social support, and cognitive function in middle-aged adults with a family history of Alzheimer’s disease. J Aging Health. (2013) 25:944–59. doi: 10.1177/0898264313498416
95. Hobfoll SE. Conservation of resources: a new attempt at conceptualizing stress. Am Psychol. (1989) 44:513–24. doi: 10.1037/0003-066X.44.3.513
96. Hobfoll SE, Freedy J, Lane C, Geller P. Conservation of social resources: social support resource theory. J Soc Personal Relationsh. (1990) 7:465–78. doi: 10.1177/0265407590074004
97. Maslach C, Leiter MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry. (2016) 15:103–11. doi: 10.1002/wps.20311
98. Brandes P, Castro SL, James MS, Martinez AD, Matherly TA, Ferris GR, et al. The interactive effects of job insecurity and organizational cynicism on work effort following a layoff. J Leadersh Organ Stud. (2008) 14:233–47. doi: 10.1177/1071791907311967
99. Brandes P, Das D. Locating behavioral cynicism at work: construct issues and performance implications. In: Perrewé, PL Ganster DC editors. Employee Health, Coping and Methodologies. Amsterdam: Elsevier Science/JAI Press (2006). p. 233–66. doi: 10.1016/S1479-3555(05)05007-9
100. Chiaburu DS, Peng AC, Oh I-S, Banks GC, Lomeli LC. Antecedents and consequences of employee organizational cynicism: a meta-analysis. J Vocat Behav. (2013) 83:181–97. doi: 10.1016/j.jvb.2013.03.007
101. Naus F, Van Iterson A, Roe R. Organizational cynicism: extending the exit, voice, loyalty, and neglect model of employees’ responses to adverse conditions in the workplace. Hum Relat. (2007) 60:683–718. doi: 10.1177/0018726707079198
102. Brief AP, Motowidlo SJ. Prosocial organizational behaviors. Acad Manage Rev. (1986) 11:710–25. doi: 10.5465/amr.1986.4283909
103. Trés ES, Brucki SMD. Visuospatial processing: a review from basic to current concepts. Dement Neuropsychol. (2014) 8:175–81. doi: 10.1590/S1980-57642014DN82000014
104. Koutsimani P, Montgomery A. Burnout and cognitive functioning: are we underestimating the role of visuospatial functions? Front Psychiatry. (2022) 13:775606. doi: 10.3389/fpsyt.2022.775606
105. Little RR, Rubin DB. Statistical Analysis with Missing Data (Second). New York, NY: JohnWiley & Sons (2002). doi: 10.1002/9781119013563
106. Spector PE. Do not cross me: optimizing the use of cross-sectional designs. J Bus Psychol. (2019) 34:125–37. doi: 10.1007/s10869-018-09613-8
107. Lezak MD, Howieson DB, Bigler ED, Tranel D. Neuropsychological Assessment. Oxford: OUP USA (2012).
108. Kasper RW, Elliott JC, Giesbrecht B. Multiple measures of visual attention predict novice motor skill performance when attention is focused externally. Hum Move Sci. (2012) 31:1161–74. doi: 10.1016/j.humov.2011.11.005
Keywords: burnout, cognitive functioning, cognitive impairment, depression, anxiety, perceived family support, longitudinal study
Citation: Koutsimani P and Montgomery A (2022) Cognitive functioning in non-clinical burnout: Using cognitive tasks to disentangle the relationship in a three-wave longitudinal study. Front. Psychiatry 13:978566. doi: 10.3389/fpsyt.2022.978566
Received: 26 June 2022; Accepted: 01 August 2022;
Published: 17 August 2022.
Edited by:
Elisa Harumi Kozasa, Instituto do Cérebro, BrazilReviewed by:
Sergio Luis Schmidt, Rio de Janeiro State Federal University, BrazilCopyright © 2022 Koutsimani and Montgomery. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anthony Montgomery, YW50aG9ueS5tb250Z29tZXJ5QG5vcnRodW1icmlhLmFjLnVr
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.