
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 27 September 2022
Sec. Anxiety and Stress Disorders
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.977238
This article is part of the Research Topic Obsessive-Compulsive Related Disorders (OCRD) Across the Lifespan View all 10 articles
Introduction: Body dysmorphic disorder (BDD) and depression have been reported to be both prevalent among young people worldwide, resulting in serious implications in their quality of life and social functioning. This is worrying especially in men where mental disorders are often overlooked and under-researched. This study aims to determine the proportion of male university students with symptoms suggestive of body dysmorphic disorder and depression, as well as their perception on their body image.
Methods: In this cross-sectional study, 1,308 male students between the aged of 17–26 years in a private university in Malaysia via self-administered online questionnaire comprising the Patient Health Questionnaire (PHQ)-9, the Body Dysmorphic Disorder Questionnaire (BQQD) and the Body Self-Image Questionnaire (BSIQ), in addition to their sociodemographic parameters. Data analyses were performed with Mann Whitney test, chi square test and Fisher's exact test.
Results: 3.3 and 54.2% of the students had symptoms suggestive of BDD and depression respectively, with up to 9.02% of the students reporting having moderate to severe depression. There was a significant association between BDD symptoms and students staying alone, whilst depression was significantly associated with studying in the rural campus. Furthermore, a significant association was demonstrated between presence of BDD and depression symptoms. Most of the students were dissatisfied with their whole body, especially their height.
Conclusion: The proportion of BDD and depression symptoms among male students in our university is quite high. Universities and the public health sector should develop better support service targeting male university students.
Body dysmorphic disorder (BDD), one of an obsessive-compulsive spectrum disorder, is often described as having distressing or impairing obsessions with perceived physical imperfections that are usually unobservable or appear only slight to others (1–3). Individuals with BDD often have a negative perception on their own body image that leads to significant negative emotions thus affecting their daily functioning (4). BDD in adults usually leads to high rates of social and occupational dysfunction whereas BDD in youth is associated with a poorer academic performance, social withdrawal and higher school dropping out rates (2). Despite the increasing prevalence of BDD among young people worldwide (4–11) and the serious implications toward their quality of life and social functioning, there is still a lack of data on BDD in the general population of Malaysia, especially among young male adults.
Depression is characterized by persistent sadness, anhedonia, trouble sleeping, changes in appetite, loss of energy and difficulty concentrating and is common among university students (12). In Malaysia, it was reported up to 70% of university students admitting that they have symptoms suggesting of depression (13–16). Aside from affecting the academic achievement of students (17), untreated depression may also lead to increased psychological morbidity and other mental disorders (18).
Women are known to be more prone to suffer from internalizing mental disorder, such as major depression and eating disorders (19), while mental illnesses in men are often overlooked and untreated, resulting in higher morbidity and mortality rates (20). Although suicide has been the leading cause for death among young men in several countries, the mental health of this group is generally overlooked (21). This implies that there is an urgent need to study the epidemiology of mental disorders among male adolescence. The current study aims to determine the proportion of symptoms suggesting of BDD and depression among male undergraduate students in a local university as well as their associated factors. Furthermore, this study examines the body self-image perception among these students. We hypothesize that a high number of male Malaysian university students may be a risk of depression and BDD.
This was a single-center cross-sectional study conducted between 11 November 2021 till 20 January 2022. The target population of this study was male foundation students and undergraduates aged from 17 to 26 years from both Universiti Tunku Abdul Rahman (UTAR) Sungai Long Campus and Kampar campus. Ethics approval was obtained before the initiation of the study.
The sample size was calculated based on the formula for estimation for a proportion, where n is the sample size, Z is standard normal deviate 1.960, d is the precision of 0.03, and p is the pre-study estimate of depression among Malaysian medical students as reported by Shamsuddin et al. (13).
A random sampling method was used where 2,149 participants were randomly selected from the list of 10,747 male undergraduate students registered in the university, which represented 20% of the total population. All male foundation students and undergraduates from Universiti Tunku Abdul Rahman, between the ages of 17–26 years and students were included in the study and excluded if they refused to participate in this study or were not able to provide informed consent. Students agreeable to participate in the study were given a self-administering online questionnaire. A total of 1,308 students agreed to enroll in the study, showing a calculated response rate of 60.8%, whilst 24 students decline to participate and the remaining 817 students did not respond within the stipulated timeframe.
The questionnaire consists of 7 sections: (i) sociodemographic parameters, (ii) Patient Health Questionnaire-9 (PHQ-9), (iii) Body Dysmorphic Disorder Questionnaire (BDDQ), and (iv) Body Self-Image Questionnaire-Short Form (BISQ-SF). The 6 socio-demographic parameters included age, gender, faculty, household members, history of mental illness, history of recreational drug abuse.
The Patient Health Questionnaire-9 (PHQ-9) is widely used to access the respondents' depression severity levels based on a four-point Likert scale rated from 0 (Not at all) to 3 (nearly every day). This section consisted of 9 questions and the total sum up scores was classified according to the following categories in terms of depression severity level: none or minimal, mild, moderate, moderately severe and severe. This depression subscale has been published in previous studies, showing a Cronbach alpha of 0.86–0.89 respectively (22).
The BDDQ is a self-report screening tool for BDD and consists of 4 questions asking about the concern of the physical appearance and a total score of 4 indicates a possibility of BDD. Phillips et al. reported a sensitivity and specificity of this scale of 100 and 93% respectively (23).
The Body Self-Image Questionnaire-Short Form (BSIQ-SF) is used to access the participant's perceptions toward their body image. This questionnaire has 21 Likert scale questions which each classified into 4 different domains which included negative affect, attractiveness evaluation, physical functionality awareness and height dissatisfaction. Higher dissatisfaction toward body and height is usually indicated by higher scores in negative affect and height dissatisfaction. On the contrary, a higher score in attractiveness evaluation and physical functionality awareness points toward the individual having a higher body satisfaction and more likely to maintain good physical functionality. The results were accessed using 5-point Likert scale included: “Not at all true of myself,” “slightly true,” “about halfway true,” “mostly true,” and “completely true.” The BSIQ-SF has been validated for local use in Malaysia (24).
The data were analyzed with SPSS version 22.0 (IBM, Chicago, USA). Descriptive statistics are presented as frequency and percentage for categorical data and as mean and standard deviation for continuous variable if they are normal distributed or as median and interquartile range (IQR) if they are not normal distributed. In addition to it, all quantitative data was assessed for normal distributions in this study. Chi-square or Fisher's exact test were used to analyse categorical variables. On the other hand, Mann-Whitney test or Kruskal-Wallis test was employed to look for the relationship between categorical data (sociodemographic parameters) and continuous data (BDDQ/ PHQ-9/ BSIQ-SF). For continuous data, Spearman's correlation test was used to analyse the correlation between age and BSIQ scores. For logistic regression, a backward stepwise approach is chosen to determine statistically significant independent variables.
The statistical significance level for all inferential test was set at P < 0.05.
Based on the BDDQ questionnaire, approximately 3.3% out of the 1,308 male undergraduate students reported symptoms suggestive of BDD. Among all the socio-demographic parameters, there is a significant association between BDD symptoms and students staying alone (x2 = 5.726, p = −0.026) (Table 1). There is no significant association between BDD symptoms and students studying medicine and health sciences (x2 = 0.012, p = 0.914) with only 7.5% out of 43 the students with BDD symptoms were from the faculty of medicine and health sciences (Table 1).
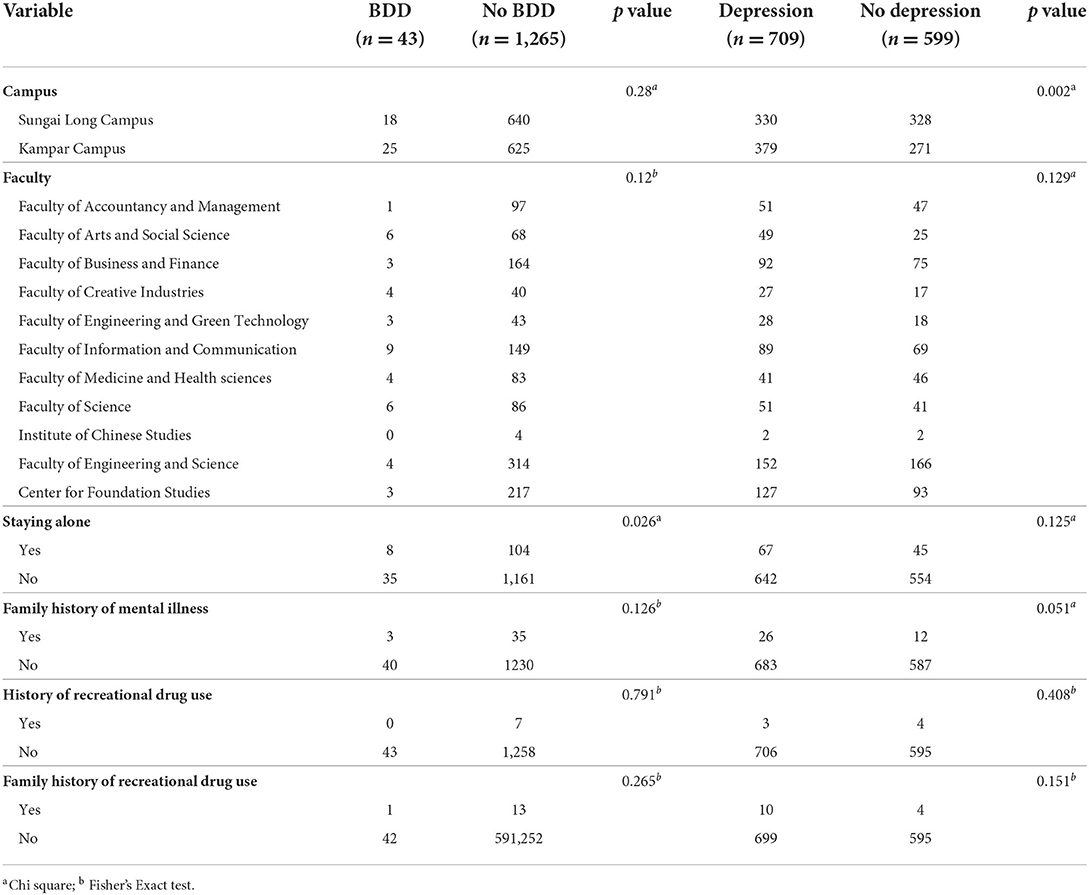
Table 1. Socio-demographic parameters of UTAR male undergraduate students according to BDD and depression status.
Only 793 (60.6%) of all the respondents are worried about their appearance, and among these respondents, 60.4% of them wished they could think about their appearance less. 39.6% of these respondents were dissatisfied with their whole body, while 37.1% were unhappy about their face. In addition, 46.4% of the respondents were concerned that they did not look thin enough or might look too fat, and 30.6% felt that this often upset them a lot.
Due to these dissatisfactions, 127 (16.0%) out of the 793 students admitted that this had gotten in the way of their social activities and 50 (6.3%) claimed that it has caused problems with their school, work, or other activities. Only 2.9% of these 793 students spent more than 3 h thinking about their look, followed by 7.9% spending 1–3 h per day and 89.2% spent less than an hour.
With multivariate logistic regression, after adjusting for family history of mental illness or recreational drug use, personal history of recreational drug use, as well as location of campus, the only significant predictor for BDD symptoms is staying alone (OR = 2.551, 95%CI 1.153–5.649, p = 0.021).
Approximately 54.2% of students reported to have symptoms suggestive of depression in the PHQ-9 questionnaire where 9.02% had symptoms suggestive moderately severe to severe depression while 13.23 and 31.96% had moderate and mild depressive symptoms respectively. No significant association between most of the socio-demographic parameters was seen except for location of the campus (x2 = 8.762, p = −0.003). Almost 50% of male students studying medicine or health sciences had symptoms suggestive of depression, but this only constitutes 6% of all the students claiming to have depression symptoms. There was also no significant association between medical and health sciences students with symptoms of depression (x2 = 2.195, p = 0.138) (Table 1).
The median and interquartile range for the PHQ-9 score was 5 (7); the mean and IQR PHQ-9 score for students with symptoms suggestive of depression is significantly higher than those without symptoms (U = 0, p < 0.001). Among all the variables, students from the Kampar campus and with a family history of recreational drug use had significantly higher PHQ-9 median scores respectively compared to students from Sungai Long campus or without family history of recreational drug use (U = 199,188, p = 0.031; U = 5,546.5, p = 0.012). The most frequent symptoms that the respondents had were issues with energy levels (71.5%), followed by little interest or pleasure in doing things (68.4%) and feelings of down and depressed and hopelessness (55.2%) (Table 2).
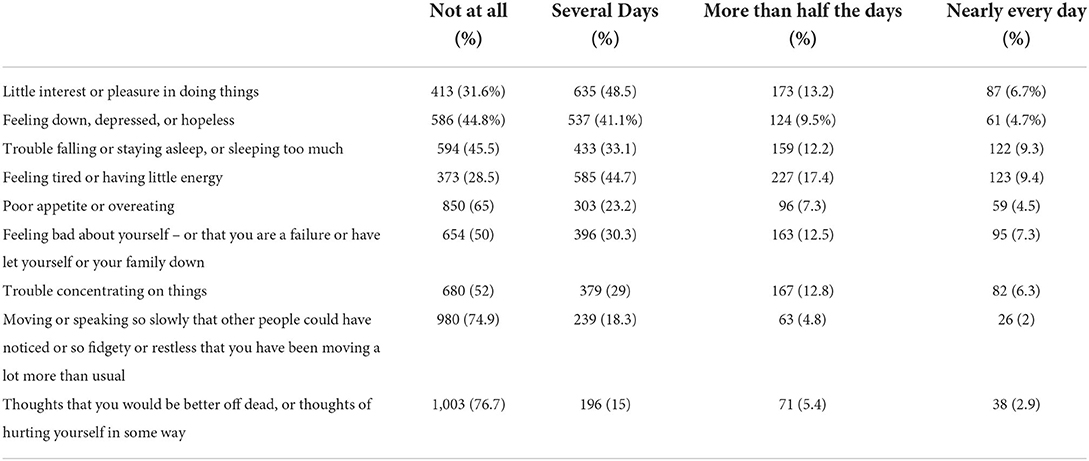
Table 2. Symptoms suggestive of depression and their frequency among UTAR male undergraduate students in the PHQ-9 questionnaire.
With multivariate logistic regression, after adjusting for family history of mental illness or recreational drug use, personal history of recreational drug use, as well as status of living alone, the only significant predictor for symptoms suggestive of depression is location of campus (OR = 1.397, 95%CI 1.122–1.736, p = 0.003).
25.7% of all the 1,308 students did not think they look good in their clothes. Most of the students were unhappy with their height, with 23.8% students often expressed their wish to be taller, 17.9% wished that they could be taller and 13.1% expressed that they would like their body better if they were taller. On the contrary only 6.7% of the students thought that they were overweight and 9.2% wished they were thinner (Table 3).
Respondents with symptoms suggestive of depression based on the PHQ-9 scores, had a significantly higher scores in the negative affect (U = 130,792, p < 0.001) and height dissatisfaction (U = 162,738, p < 0.001) domains, while their scores in the attractive awareness domain was significantly lower (U = 194,876, p = 0.01). Similarly, respondents with symptoms of BDD had significantly higher scores in the negative affect (U = 7,354, p < 0.001) and height dissatisfaction domains (U = 18,526, p < 0.001) but a significantly lower score in the physical functionality domain (U = 20,460, p = 0.005).
There was a significant positive correlation between the PHQ-9 score and the negative affect score (r (1306) = 0.373 p < 0.001), height dissatisfaction score (r (1306) = 0.193 p < 0.001), and the physical functionality score (r (1306) = 0.086 p = 0.002) respectively. However, there was a significant negative correlation between PHQ-9 score and attractive awareness score (r (1306) = −0.089, p = 0.001).
The proportions of students at risk of having BDD was almost similar to previous studies which reported 0.6–12.3% of their male cohort having BDD (4–11). Once again, the application of different assessment tools to determine BDD in different studies could have resulted in the large range of prevalence observed. Most of the respondents in our study were dissatisfied with their whole body and face whereas respondent from other studies were more concern with their hair, face, weight and skin (4, 7–9, 25). Separately, there is a significant association between staying alone and BDD, as individuals with BDD often have poor psychosocial functioning and avoids social interaction (26).
Most of our respondents were dissatisfied with their height, as evident by the BSIQ scores. This was in line with other previous literature that reported Asian boys and men are more discontent with their height (27). Men often perceive height as an important component of masculinity. Taller men are thought to be more attractive, more intelligent and more confident (28, 29). A high dissatisfaction in height among our cohort may be due to the fact that a person's height cannot be altered easily without invasive or potentially dangerous intervention (30). However, we did not assess whether height dissatisfaction results in disability or impairment among our respondents and we did not include screening for eating disorders in our study, as this is closely related to BDD. In this, we also believe that height dissatisfaction should be spelled out clearly as a “body area” in the BDDQ owing to its high proportion among young Asian men and possibly improving the sensitivity of the BDDQ questionnaire.
Our study reported up to 54.2% who may be at risk of depression due to the presence of symptoms. This is comparable to other local studies which had reported 33.4–74.4% in their male cohort (13–16). The application of various screening tools for depression in previous studies may explain the large range of prevalence observed whereby most of our male students reported mild depression symptoms, compared to the previous studies where most of their male students had moderate depressive symptoms. However, the global pooled prevalence of depression among both male and female college students were reported to be 33.6% (31).
Interestingly, there were significantly more students at risk of depression in the Kampar campus, which is located in a rural area, contrary to prior studies (15). Our study is the first to report this observation as previous literatures have pointed out a higher prevalence of mental health problems in adolescents residing in urban areas, suggesting a detrimental effect of urbanicity among adolescents (32–34).
Prior studies have reported a higher degree of depression among medical students (31). In our cohort, up to 46.5% of the male undergraduate students enrolled in medical and health sciences had depressive symptoms. The results from our finding was almost similar to previous local studies which reported that 33.3–74.4% Malaysian medical and health science students exhibited symptoms of depression (15, 35–38), suggesting that medical students were more vulnerable to develop depressive symptoms compared to other students (39). This may largely due to the fact that curriculum for medical and health science students are more intense and complex compared to the other students (35, 37, 40, 41). However, no significant association was seen between enrolling in medical and health sciences and depression.
BDD and depression symptoms among our participants were significantly associated with each other (x2 = 9.099, p = 0.003). There is conflicting literature regarding the association of BDD and depression where some literature reported individuals with BDD has a 2.3–4.2 times higher risk for co-existing neuropsychiatric disorders especially depression (11, 42), whilst Pimenta et al. commented that there were no association between BDD and depression in their study (43). However, both studies were conducted in both men and women, while our study only focuses on young men. This association can be partially explained by the higher susceptibility of men with BDD exhibiting negative thought and behavior patterns which increases the vulnerability of developing depression (42).
To our knowledge, this study is the first in the country to determine the proportion of students with symptoms suggestive of body dysmorphic among young adults as well as their perception on their self-image. However, our sample population consists mainly of students of Chinese ethnicity. Hence, our findings may not be generalized to the other universities in the country. Furthermore, both the PHQ-9 and BDIQ only serve as screening tools for depression and BDD and the diagnosis of both mental disorders require a more structured interview by a trained healthcare provider. A mediator or moderator modeling would be more superior to determine the association between the independent variables and the presence of BDD and depression symptoms. In addition to this, the proportion of depressive symptoms could be much higher than expected as the study was conducted during the COVID-19 pandemic where the movement restriction order was being implemented.
There is a high proportion of young male university students who is at risk of developing depression and BDD. Majority of our male university students are dissatisfied with their height, where the level of dissatisfaction significantly correlates with the severity of depressive symptoms. This implicates the dire need for university authorities to take a proactive approach to screen for depression and BDD among university students, as well as to educate them on mental health resilience.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by Science and Research Ethics Committee, University Tunku Abdul Rahman. The patients/participants provided their written informed consent to participate in this study.
WK and WL have made substantial contributions to conception and design of the study, interpretation of the data, and as well as critical revision of the manuscript. ML, XL, YO, TN, and WT have been involved in acquisition of data, analysis and interpretation of data as well as early drafting of the manuscript. All authors have given final approval of the version to be published.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Bjornsson AS, Didie ER, Phillips KA. Body dysmorphic disorder. Dialogues Clin Neurosci. (2010) 12:221–32. doi: 10.31887/DCNS.2010.12.2/abjornsson
2. Krebs G, Fernández de la Cruz L, Mataix-Cols D. Recent advances in understanding and managing body dysmorphic disorder. Evid Based Ment Health. (2017) 20:71–5. doi: 10.1136/eb-2017-102702
3. Hong K, Nezgovorova V, Uzunova G, Schlussel D, Hollander E. Pharmacological treatment of body dysmorphic disorder. Curr Neuropharmacol. (2019) 17:697–702. doi: 10.2174/1570159X16666180426153940
4. Alsaidan MS, Altayar NS, Alshmmari SH, Alshammari MM, Alqahtani FT, Mohajer KA. The prevalence and determinants of body dysmorphic disorder among young social media users: a cross-sectional study. Dermatol Rep. (2020) 12:8774. doi: 10.4081/dr.2020.8774
5. Bohne A, Wilhelm S, Keuthen NJ, Florin I, Baer L, Jenike MA. Prevalence of body dysmorphic disorder in a German college student sample. Psychiatry Res. (2002) 109:101–4. doi: 10.1016/S0165-1781(01)00363-8
6. Bartsch D. Prevalence of body dysmorphic disorder symptoms and associated clinical features among Australian university students. Clin Psychol. (2007) 11:16–23. doi: 10.1080/13284200601178532
7. Taqui AM, Shaikh M, Gowani SA, Shahid F, Khan A, Tayyeb SM, et al. Body Dysmorphic Disorder: Gender differences and prevalence in a Pakistani medical student population. BMC Psychiatry. (2008) 8:20. doi: 10.1186/1471-244X-8-20
8. Liao Y, Knoesen NP, Deng Y, Tang J, Castle DJ, Bookun R, et al. Body dysmorphic disorder, social anxiety and depressive symptoms in Chinese medical students. Soc Psychiatry Psychiatr Epidemiol. (2010) 45:963–71. doi: 10.1007/s00127-009-0139-9
9. Schneider SC, Turner CM, Mond J, Hudson JL. Prevalence and correlates of body dysmorphic disorder in a community sample of adolescents. Aust N Z J Psychiatry. (2017) 51:595–603. doi: 10.1177/0004867416665483
10. Enander J, Ivanov VZ, Mataix-Cols D, Kuja-Halkola R, Ljótsson B, Lundström S, et al. Prevalence and heritability of body dysmorphic symptoms in adolescents and young adults: a population-based nationwide twin study. Psychol Med. (2018) 48:2740–7. doi: 10.1017/S0033291718000375
11. Hakim RF, Alrahmani DA, Ahmed DM, Alharthi NA, Fida AR, Al-Raddadi RM. Association of body dysmorphic disorder with anxiety, depression, and stress among university students. J Taibah Univ Med Sci. (2021) 16:689–94. doi: 10.1016/j.jtumed.2021.05.008
12. Ibrahim AK, Kelly SJ, Adams CE, Glazebrook C. A systematic review of studies of depression prevalence in university students. J Psychiatr Res. (2013) 47:391–400. doi: 10.1016/j.jpsychires.2012.11.015
13. Shamsuddin K, Fadzil F, Wan Ismail WS, Shah SA, Omar K, Muhammad NA, et al. Correlates of depression, anxiety and stress among Malaysian university students. Asian J Psychiatr. (2013) 6:318–23. doi: 10.1016/j.ajp.2013.01.014
14. Islam MA, Kelly SJ, Adams CE, Glazebrook C. Factors associated with depression among university students in malaysia: a cross-sectional study. KnE Life Sci. (2018) 4:415. doi: 10.18502/kls.v4i4.2302
15. Nahas ARF, Elkami RM, Al-Shami AM, Elsayed TM. Prevalence of depression among health sciences students: findings from a public university in Malaysia. J Pharm Bioallied Sci. (2019) 11:170. doi: 10.4103/JPBS.JPBS_263_18
16. Abd Hamid NZ, Ibrahim S, Razali H. Prevalence of depression among university students: a cross-sectional study. Int J Educ Psychol Counsel. (2020) 5:204–10. doi: 10.35631/IJEPC.5360015
17. Moreira de Sousa J, Moreira CA, Telles-Correia D. Anxiety, depression and academic performance: a study amongst portuguese medical students versus non-medical students. Acta Méd Port. (2018) 31:454. doi: 10.20344/amp.9996
18. Lew B, Huen J, Yu P, Yuan L, Wang D, Ping F, et al. Associations between depression, anxiety, stress, hopelessness, subjective well-being, coping styles and suicide in Chinese university students. PLoS ONE. (2019) 14:e0217372. doi: 10.1371/journal.pone.0217372
19. Otten D, Tibubos AN, Schomerus G, Brähler E, Binder H, Kruse J, et al. Similarities and Differences of Mental Health in Women and Men: A Systematic Review of Findings in Three Large German Cohorts. Front Public Health. (2021) 9:553071. doi: 10.3389/fpubh.2021.553071
20. Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results from the 2017 National Survey on Drug Use and Health. (2018). Available online at: https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHFFR2017/NSDUHFFR2017.pdf (accessed May 25, 2022).
21. Rice SM, Purcell R, McGorry PD. Adolescent and young adult male mental health: transforming system failures into proactive models of engagement. J Adolesc Health. (2018) 62:S9–S17. doi: 10.1016/j.jadohealth.2017.07.024
22. Kroenke K, Spitzer RL, Williams JBW. The PHQ-9. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
23. Phillips KA. Understanding Body Dysmorphic Disorder. Oxford: Oxford University Press USA-OSO. [e-book] (2009). Available at: ProQuest Ebook Central https://ebookcentral.proquest.com/lib/utar-ebooks/detail.action?docID=416018&query=The+Broken+Mirror%3A+Understanding+and+treating+Body+Dysmorphic+Disorder (accessed October 29, 2021).
24. Lim CJ, Hamid SA, Yaacob NM, Hairon SM, Cheng KY, Bujang MA. Validation of Malay Version of Body Self-Image Questionnaire-Short Form among Malaysian Young Adults. Malays J Med Sci. (2018) 25:131–141.
25. Möllmann A, Dietel FA, Hunger A, Buhlmann U. Prevalence of body dysmorphic disorder and associated features in German adolescents: a self-report survey. Psychiatry Res. (2017) 254:263–7. doi: 10.1016/j.psychres.2017.04.063
26. Kelly MM, Walters C, Phillips KA. Social anxiety and its relationship to functional impairment in body dysmorphic disorder. Behav Ther. (2010) 41:143–53. doi: 10.1016/j.beth.2009.01.005
27. Mellor D, Hucker A, Waterhouse M, Mamat NH, Xu X, Cochrane J, et al. A cross-cultural study investigating body features associated with male adolescents' body dissatisfaction in Australia, China, and Malaysia. Am J Mens Health. (2014) 8:521–31. doi: 10.1177/1557988314528370
28. Helgeson VS. Prototypes and dimensions of masculinity and femininity. Sex Roles. (1994) 31:653–82. doi: 10.1007/BF01544286
29. Ridgeway RT, Tylka TL. College men's perceptions of ideal body composition and shape. Psychol Men Masc. (2005) 6:209–20. doi: 10.1037/1524-9220.6.3.209
30. Talbot D, Mahlberg J. Exploration of height dissatisfaction, muscle dissatisfaction, body ideals, and eating disorder symptoms in men. J Am Coll Health. (2021) 1–6. doi: 10.1080/07448481.2021.1877143
31. Li W, Zhao Z, Chen D, Peng Y, Lu Z. Prevalence and associated factors of depression and anxiety symptoms among college students: a systematic review and meta-analysis. J Child Psychol Psychiatr Allied Discip. (2022). doi: 10.1111/jcpp.13606
32. Sundquist K, Frank G, Sundquist J. Urbanisation and incidence of psychosis and depression. Br J Psychiatry. (2004) 184:293–8. doi: 10.1192/bjp.184.4.293
33. Wang JL. Rural-urban differences in the prevalence of major depression and associated impairment. Soc Psychiatry Psychiatr Epidemiol. (2004) 39:19–25. doi: 10.1007/s00127-004-0698-8
34. Evans BE, Huizink AC, Greaves-Lord K, Tulen JHM, Roelofs K, van der Ende J. Urbanicity, biological stress system functioning and mental health in adolescents. PLoS ONE. (2020) 15:e0228659. doi: 10.1371/journal.pone.0228659
35. Saravanan C, Wilks R. Medical students' experience of and reaction to stress: the role of depression and anxiety. Sci World J. (2014) 2014:1–8. doi: 10.1155/2014/737382
36. Manaf NA, Saravanan C, Zuhrah B. The prevalence and inter-relationship of negative body image perception, depression and susceptibility to eating disorders among female medical undergraduate students. J Clin Diagn Res. (2016) 10:VC01–4. doi: 10.7860/JCDR/2016/16678.7341
37. Gan GG, Yuen Ling H. Anxiety, depression and quality of life of medical students in Malaysia. Med J Malays. (2019) 74:57–61.
38. Fauzi MF, Anuar TS, Teh LK, Lim WF, James RJ, Ahmad R, et al. Stress, Anxiety and depression among a cohort of health sciences undergraduate students: the prevalence and risk factors. Int J Environ Res Public Health. (2021) 18:3269. doi: 10.3390/ijerph18063269
39. Teh CK, Ngom CW, Zulkifli RA, Vellasamy R, Suresh K. Depression, anxiety and stress among undergraduate students: a cross sectional study. Open J Epidemiol. (2015) 05:260–8. doi: 10.4236/ojepi.2015.54030
40. Khan MS, Mahmood S, Badshah A, Ali SU, Jamal Y. Prevalence of depression, anxiety and their associated factors among medical students in Karachi, Pakistan. J Pak Med Assoc. (2006) 56:583–6.
41. Aboalshamat K, Hou XY, Strodl E. Psychological well-being status among medical and dental students in Makkah, Saudi Arabia: a cross-sectional study. Med Teach. (2015) 37:S75–81. doi: 10.3109/0142159X.2015.1006612
42. McFarland MB, Kaminski PL. Men, muscles, and mood: The relationship between self-concept, dysphoria, and body image disturbances. Eat Behav. (2009) 10:68–70. doi: 10.1016/j.eatbeh.2008.10.007
Keywords: body dysmorphia, depression, Malaysian students, height dissatisfaction, obsessive-compulsive disorder
Citation: Kang WH, Loo MY, Leong XM, Ooi YF, Teo WQ, Neoh TJ and Ling WC (2022) Body dysmorphic disorder and depression among male undergraduate students in a Malaysian University. Front. Psychiatry 13:977238. doi: 10.3389/fpsyt.2022.977238
Received: 24 June 2022; Accepted: 25 August 2022;
Published: 27 September 2022.
Edited by:
Katarzyna Prochwicz, Jagiellonian University, PolandReviewed by:
Meenal Pathak, Penn State Milton S. Hershey Medical Center, United StatesCopyright © 2022 Kang, Loo, Leong, Ooi, Teo, Neoh and Ling. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Waye Hann Kang, a2FuZ3doQHV0YXIuZWR1Lm15
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.