- Department of Early Childhood Education, The Education University of Hong Kong, Hong Kong, Hong Kong SAR, China
Background: The outbreak of COVID-19 in December 2019 has caused unprecedented disruption to the structure of children's daily lives due to school closures, online learning, strict social distancing measures, limited access to outdoor activities and many other restrictions. Since children are more susceptible to stress than adults and there is a growing concern about the potential debilitating consequences of COVID-19 for children's mental health, the present review aims to provide empirical evidence on the groups who are most at risk of mental health problems and uncover the risk and protective factors of children's mental health.
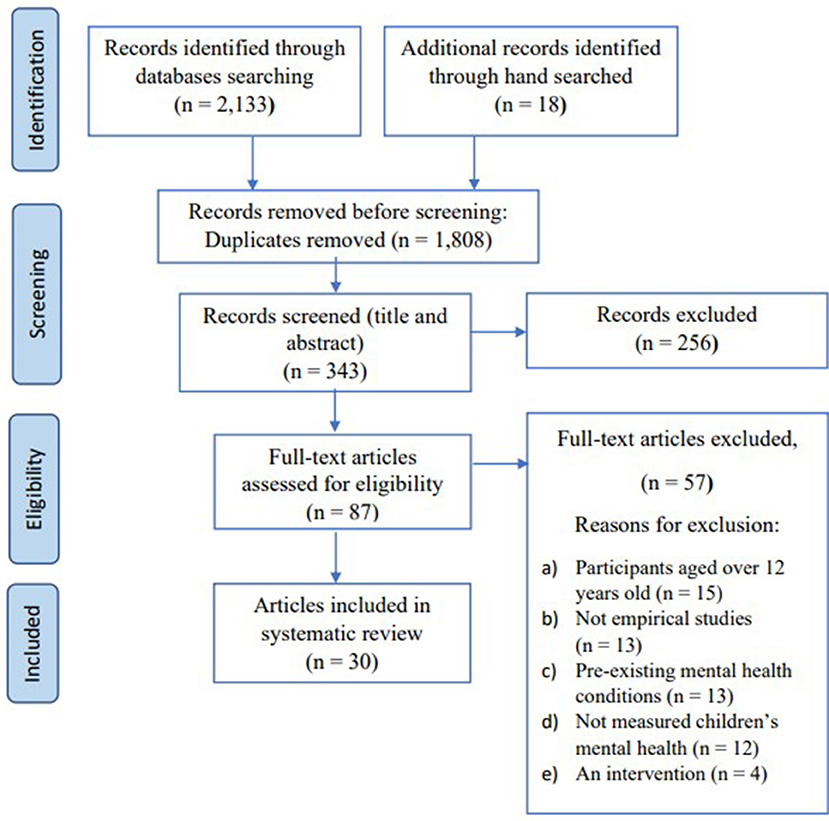
Methods: A systematic search was performed, in accordance with PRISMA guidelines, in the electronic databases Web of Science (including SSCI and A&HI) and EBSCOhost (including ERIC, MEDLINE and APA PsycArticles and APA PsycINFO), for any empirical studies published between January 2020 and February 2022 that focused on children ≤ 12 years old.
Results: An initial search identified 2,133 studies. A total of 30 studies fulfilled the inclusion criteria and were analyzed. The evidence showed that many children were affected by the COVID-19 pandemic and experienced internalizing and externalizing behaviors. Worsened child mental health outcomes reflected socioeconomic inequalities as most at-risk children had parents with low educational attainment, were from families of low socioeconomic status and lived in small homes. Key risk factors were identified, including unhealthy lifestyle behaviors (extended screen time, sleep disturbances and less physical activity), increased pandemic-related stressors among parents and deteriorated mental health of parents, which were directly or indirectly associated with the pandemic safety measures, such as home confinement or social distancing. Protective factors including parents' resilience, positive parent-child relationship and school connectedness in relation to children's mental health were reported.
Conclusion: The overall results highlight the urgent need for the implementation of tailor-made interventions for children with signs of internalizing and externalizing behaviors. Health promotion and prevention strategies by the government to maintain the mental health of children, particularly those from lower SES families who are at higher risk of worsened mental health are essential for post-pandemic policies.
Introduction
The coronavirus disease of 2019 (COVID-19) has been a pandemic with destructive human, social and economic consequences since December 2019. In the absence of effective pharmaceutical interventions for the prevention and control of the novel coronavirus, stringent public health measures such as mask-wearing, strict social distancing, school and workplace closures as well as tough travel restrictions have been extensively implemented to mitigate the spread of COVID-19 (1, 2). Therefore, the pandemic has impacted people's daily lives with differential effects on various age groups (3).
Children are one of the groups who were unprecedently affected by the pandemic [i.e., temporary closure of daycare centers and schools, online homeschooling, limited access to recreational facilities and many other restrictions; (4–8)]. They experienced social isolation from peers, teachers, extended family and community which increases the risk of developing mental health issues such as anxiety and depression (9). In addition, with the disruption of their daily routine due to school closures, some children who are confined at home spend more time on using computers, iPhones or watching television but lack enough physical activities (10, 11). Prior studies found that excessive screen time negatively affected the cognitive and socio-emotional development of children (12, 13) and was associated with sleep disruption (14, 15) which aggravated the physical and psychological health of children (16).
As children have fewer personal resources than adults to cope with the sudden changes brought about by the pandemic (17), parents are the closest ones whom they turn to when unable to have direct contacts with other adults such as teachers and grandparents. However, during the pandemic, most parents have faced many challenges including financial difficulties (wages or salary reductions, job losses) and coping with parenting (working from home while taking care of children's homeschooling, managing their free time and dealing with their demands). Coupled with the parents' own needs but lacking sufficient support from either extended family, friends or other community organizations (18), high levels of parental stress can have a detrimental effect on children's physical and psychological health via parenting (19). Cheng et al. (18) found that parental stress predicted child abuse and neglect.
Since children's mental health is strongly related to their parents' mental health (20), with a recent study reporting that living with a parent with poor mental health increased the odds of poor child mental health (OR = 2.80, 95% CI 2.59–3.03) (21), parents are one of the key factors influencing the development of psychological problems in children (22). Given the increased stress and responsibilities of parents during the pandemic, children may have received insufficient adult support in their daily lives. The exposure to stressors can undermine children's neurobiological and socioemotional development (23). A study by the United Nations International Children's Emergency Fund (UNICEF) on 1,700 children and adolescents from 104 countries found that the brain development of children experiencing high levels of stress can be affected (24). With the escalating fear of contracting the disease and various risk factors, there was an increase in irritability, sleep disorders, anxiety and depression in children (7, 25–27).
Understanding how the pandemic undermines children's mental health is imperative as the effects can be long lasting (28). As argued by Henderson et al. (29), using Bronfenbrenner's ecological systems theory (EST) (30) can help better understand how the impact of the pandemic affects the mesosystem, exosystem, macrosystem and chronosystem which become risk factors for children's microsystem.
Till now, studies on children's mental health remain limited as most studies focus on either adolescents or adults (31, 32). Thus, designing suitable interventions to improve children's mental health becomes difficult without strong empirical evidence (33–35). This systematic review aimed to gather evidence on the current state of knowledge of the types of children who are at greater risk of mental health problems and the associated risk and protective factors for the pediatric population aged 12 years or below. Based on the timely evidence reported, the current review can inform policy makers, school administrators working in kindergartens and primary schools, researchers and healthcare providers and can prompt them to develop tailor-made interventions and devise relevant support programs to strengthen children's resources and help them cope with the risk factors that were identified in this review.
Methods
Search strategy
We searched the electronic databases of Web of Science and EBSCOhost including ERIC, MEDLINE, APA PsycArticles and APA PsycINFO, from January 2020 to February 2022. The Boolean operator was used in the search strategy, with “OR” and/or “AND” used to link search terms. The asterisk “*” was used as a wildcard symbol appended at the end of the terms to search for variations of those terms. We describe the complete search strategy below:
(a) “covid-19” OR “coronavirus” OR “2019-ncov” OR “SARS-CoV-2” OR “cov-19” OR “2019 pandemic” OR “pandemic.”
(b) “mental health” OR “mental illness*” OR “mental disorder*” OR “psychiatric illness*” OR “depress*” OR “anxiety.”
(c) “children*” OR “kids” OR “child*” OR “childhood.”
(d) a AND b AND c;
(e) Remove duplicates from d (if any);
(f) Limit f to “full-text” and “academic journal.”
In addition to electronic databases, the reference section of the included studies was hand-searched for additional relevant studies.
Eligibility criteria
Inclusion and exclusion criteria
The articles included in this review are original studies published in peer-reviewed journals in English. The following inclusion criteria were applied: (i) mental health outcomes quantitatively or qualitatively measured; (ii) children aged 12 years or below; (iii) cross-sectional or longitudinal designs; (iv) original empirical data. The exclusion criteria include: (i) studies published not in English; (ii) children with pre-existing mental health condition (e.g., anxiety disorder or neurodevelopmental disorder) or disability (e.g., cerebral palsy), those who are homeless and those with substance abuse problems) as our objective is to understand the impact of the pandemic on children's mental health, so excluding children with pre-existing mental health/ health issues can provide us with clearer results; (iii) interventions; (iv) case reports, case studies, reviews, meta-analyses, opinions, editorials, commentaries, letters to the editor and conference abstracts.
Selection of sources of evidence
The search of the Web of Science and EBSCOhost including ERIC, MEDLINE and APA PsycArticles and APA PsycINFO yielded a total of 2,133 records. Figure 1 presents the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart describing the search process and the reasons for exclusion in this review (36). Both authors (CSMN and SSLN) first screened all the titles and abstracts independently. We discussed the disagreements and revised the selection. Then SSLN reviewed the full-text articles and 20% of the full-text articles assessed for eligibility were reviewed by CSMN. The inter-rater reliability was 85%. Any disagreements were resolved through discussion and consensus.
Quality assessment, analysis and data synthesis
All the included articles were assessed in accordance with a reported structured questionnaire and its criteria (i.e., good, fair, poor and very poor) with detailed descriptions of the ratings (37). The results were shown in Supplementary Table A1. All the included articles were extracted under a structured frame (38) (i.e., study design, sample size, the selection of participants, measurements, key findings, limitations and implications).
Results
Overview of included studies
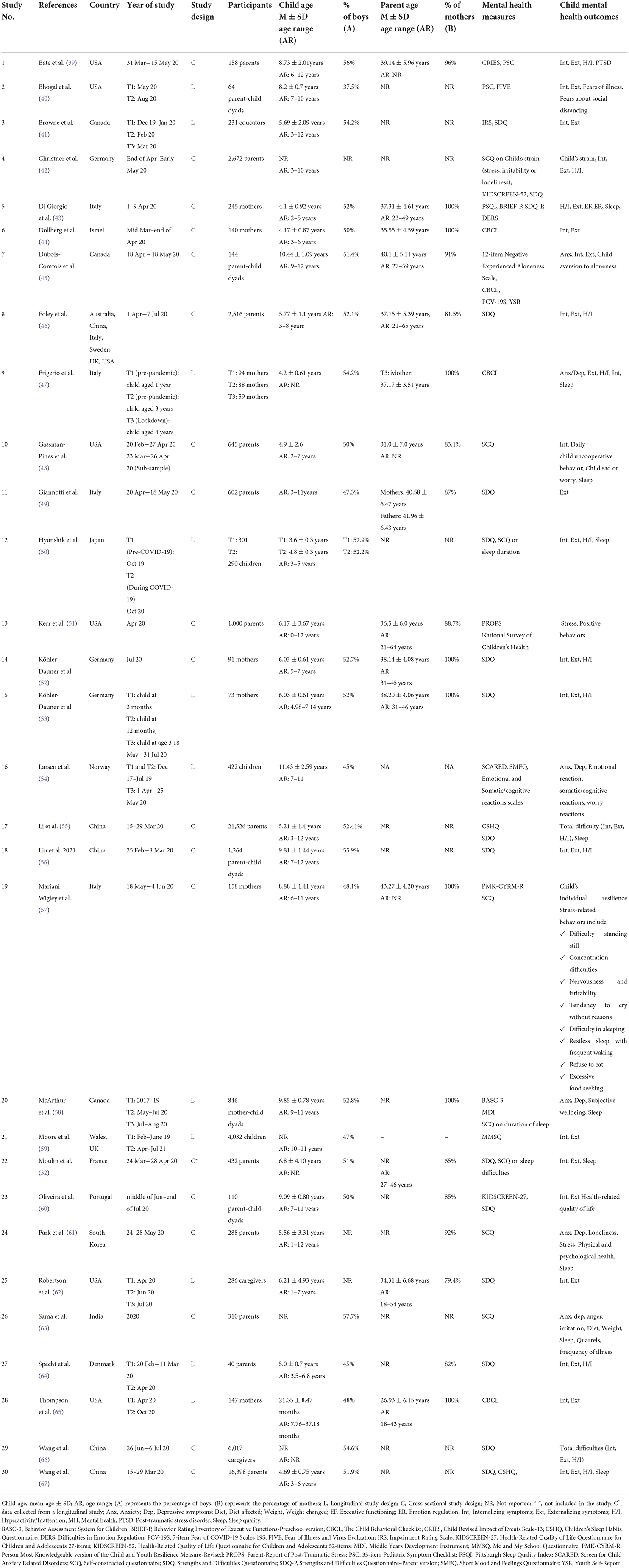
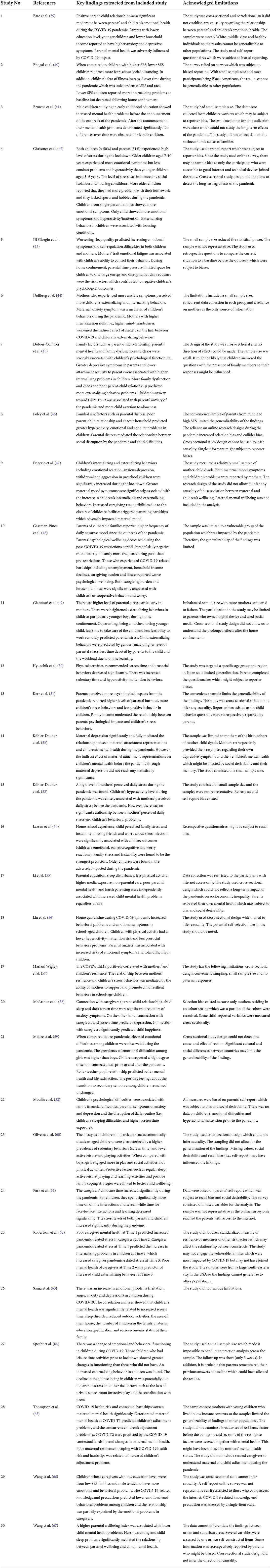
A total of 30 original studies were identified, subsequently analyzed and summarized (see Tables 1, 2 for basic information, findings and limitations of the studies). The included empirical studies were conducted globally, including North America (Canada and U.S.A.), Europe (Denmark, France, Germany, Italy, Norway, Portugal, Sweden, U.K.,), Asia (China, India, Israel, Japan, and South Korea) and Oceania (Australia). Cross-sectional designs were used in 19 studies whereas 11 studies were longitudinal. Data were collected between February 2020 and July 2021 through phone or online surveys. The sample size varied significantly, from 40 to 21,526 participants. Most of the scales [e.g., Strengths and Difficulties Questionnaire (SDQ), Screen for Child Anxiety Related Disorders (SCARED), Child Behavioral Checklist (CBCL) and Children's Sleep Habits Questionnaire (CSHQ)] were validated or widely published in empirical studies on those topics.
Study participants
Although children's mental health is one of the objectives of the current review, children were asked to complete surveys in three included studies only (50, 54, 59). The participants of the 30 included studies were mostly parents except Browne et al.'s study (41) which invited educators to assess children's mental health.
Children's mental health and other associated factors were mainly reported by parents. Among parents, mothers aged between 18 and 65 years were the main participants. Mothers were even the sole participants in seven included studies (43, 44, 47, 52, 53, 57, 65). Compared with mothers, the fathers' participation in research studies was low, so fathers were one of the respondents in ten included studies only [e.g., (32, 39, 45, 46, 48, 49, 51, 60–62, 64)]. Studies using both parent-child dyads as informants were also dearth (40, 45, 56, 58, 60).
Summary of the included studies
Children's mental health during COVID-19
The included studies assessed children's mental health by measuring the levels of internalizing (stress, anxiety, depression, anger, irritation, withdrawal, trauma-related symptoms) and externalizing behaviors (aggressive behaviors, hyperactivity/inattention problems, conduct problems) and the level of prosocial behavior. Based on the findings of the included studies, children's mental health was generally on the decline. Children exhibited more stress-related behaviors, anger, irritability, withdrawal symptoms, fear and anxiety (of COVID-19) and higher levels of depressive symptoms. Using repeated cross-sectional surveys before and after the onset of the pandemic, Moore et al. (59) examined the changes in mental health difficulties, life satisfaction, school connectedness and feelings about the transition to secondary school among children aged between 10 and 11 in Wales. The results showed that emotional difficulties increased from 17% in 2019 (prior to the pandemic) to 27% in 2021 among children (OR 1.65; 95% CI 1.23–2.20). Based on 432 parent participants, Moulin El-Aarbaoui et al. (32) reported that 7.2% of French children showed signs of emotional difficulties. In a large population-based study (n = 21,526) by Li et al. (55), 32.3% indicated mental health problems. Sama et al. (63) reported alarmingly high figures - 73.15 and 51.25% of Indian children showed signs of increased irritability and anger, respectively. Christner et al. (42) showed that over 50% of German children reported to be rather or clearly stressed, irritated or lonely during the lockdown.
Apart from internalizing behaviors, children also displayed more externalizing behaviors during the pandemic. Liu et al. (56) reported that the prevalence of behavioral problems among school-aged Chinese children varied from 4.7 to 10.3% while in home quarantine during the pandemic. Moulin El-Aarbaoui et al. (32) found that 24.8% had symptoms of hyperactivity/inattention. Table 3 summarizes the prevalence of mental health problems among children in the included studies. Overall, the results of the included studies consistently point to a decline in child wellbeing globally.
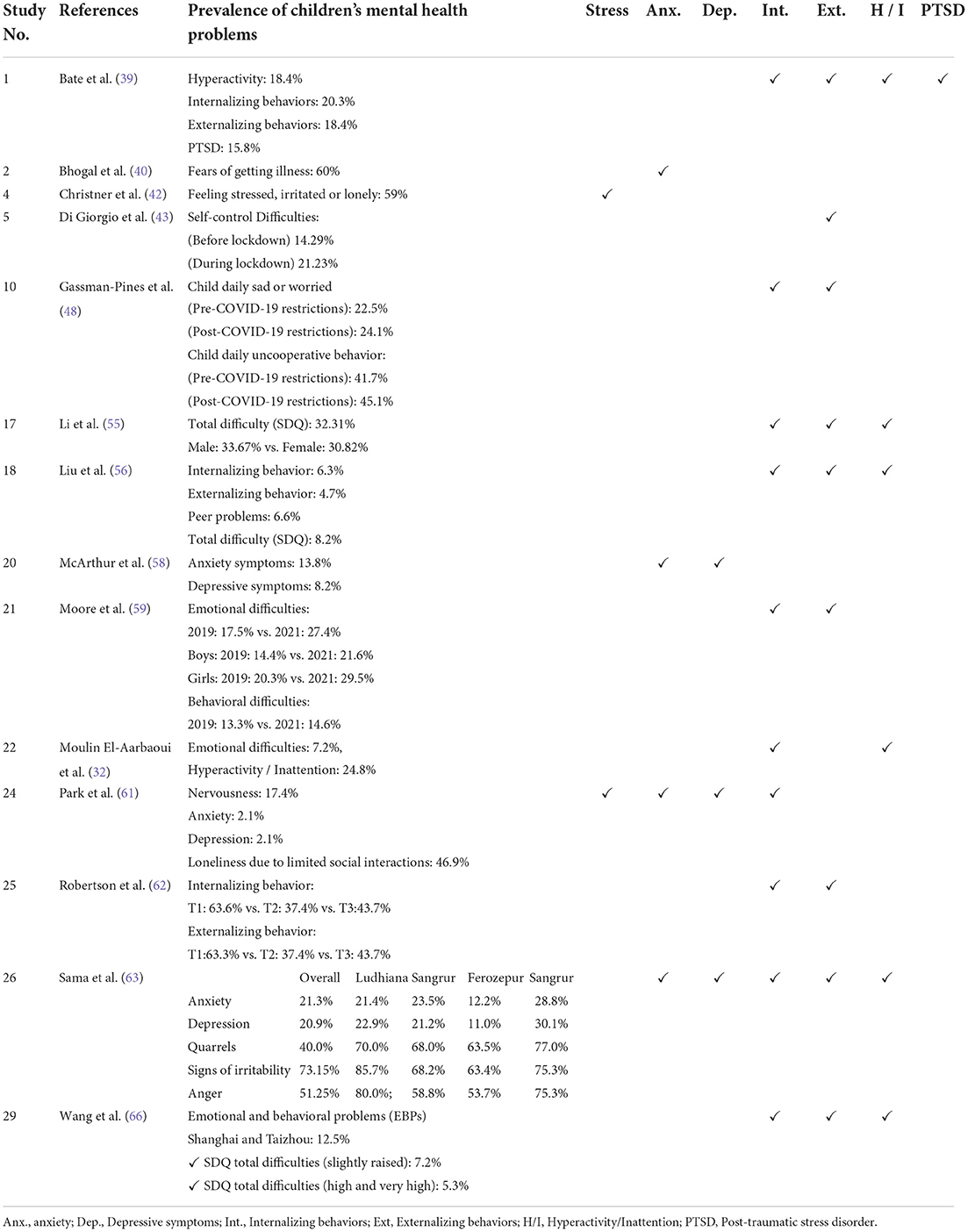
Table 3. Prevalence of children's mental health problems during the COVID-19 pandemic based on the 30 included studies.
Types of children at greater risk of negative mental health outcomes
The results from the included studies demonstrate that there are some children at greater risk of internalizing or externalizing behaviors. Those children are: (1) only child in the family; (2) from parents with low education qualifications; (3) from families of low socioeconomic status (SES); and (4) from a small size home.
Being the only child in the family puts a child at higher risk of mental health problems. Christner et al. (42) revealed that children without siblings experienced more emotional symptoms and hyperactivity/inattention than children with siblings. Sama et al. (63) found that there was a positive correlation between children's mental health (anxiety, depression, anger and irritation) and the number of children in the family (r = 0.04). Since Pearson's correlation was used, which merely provides an indication that there was a relationship between the two variables, and the p- value was not reported, whether the number of children in the family was a predictor of poor mental health for children requires further investigation.
Children of parents with low educational qualifications are also at greater risk of mental health issues. Four of the included studies observed significant links between parental education and children's mental health problems [e.g., (40, 48, 55, 66)]. Bhogal et al. (40) found that children of parents with lower educational qualifications were at higher risk of mental health difficulties by 40%. Li et al. (55) highlighted those children whose parents had low educational qualifications such as middle school or below had a 6% higher risk of mental health difficulties than those whose parents graduated from university. Similar findings were reported by Wang et al. (66) showing a higher prevalence of emotional and behavioral problems in children of caregivers with a lower educational level.
Children of low SES were also burdened by the effects of the pandemic. Bhogal et al. (40) found that children with low SES reported more fears about social distancing than their counterparts with higher SES. Moore et al. (59) found that children from low SES families reported an increase in emotional difficulties from 19.5 to 33.8%, compared to those from more affluent families who reported an increase from 11.7 to 18.5%. Li et al. (55) reported that Chinese children of low SES reported more mental health problems.
Sama et al. (63) found that the size of a child's home was associated with the mental health of children. It is likely that children in cramped living conditions are at greater risk of emotional and behavioral problems in cramped living conditions which may intensify conflicts among siblings or family members resulting in higher levels of psychological stress. Christner et al. (42) found that children living in an apartment reported higher hyperactivity/inattention (M = 4.38, SD = 2.33) than those with a large garden at home (M = 3.93, SD = 2.27).
Risk factors for children's mental health
Identifying the risk and protective factors is essential to understand why an unprecedented situation such as the COVID-19 pandemic is detrimental to children's mental health (40, 53, 65). Based on the 30 included studies, we identified the following risk factors:
Unhealthy lifestyle factors
Extended screen time
The temporary closure of schools and home confinement to mitigate the spread of COVID-19 translated to a sedentary lifestyle for children, including increased use of screen time and online interactions whereas face-to-face interaction time decreased significantly (68). Based on the cross-sectional data from Portuguese children studying in 3rd and 4th grade and their parents, Oliveira et al. (60) found that there was a higher prevalence of sedentary behaviors including TV and gaming/internet, i.e., activities that required a higher amount of screen time, particularly among socioeconomically vulnerable children. There were gender differences in screen time, with girls spending more time on watching TV and socializing online. Children from families with a negative socioeconomic change spent more time on watching TV and gaming/internet but less time on sleeping. Li et al. (55) assessed Chinese children's mental health problems in relation to factors including socioeconomic inequalities, lifestyle and family environment factors and found that media exposure (≥2 h per day) was independently associated with child mental health problems, regardless of SES.
Based on 846 mother-child dyads, McArthur et al. (58) reported that screen time predicted anxiety and depression in Canadian children. Those who engaged in excessive screen time reported higher levels of anxiety (Beta = 0.11; 95% CI 0.04–0.17) and depression (Beta = 0.09; 95% CI 0.02–0.16) after controlling for pre-pandemic anxiety and depression, respectively. French children with emotional difficulties or symptoms of hyperactivity/inattention reported more screen time (>1 h per day) during COVID-19 (32). It is worth noting that gaming/internet also predicted higher levels of externalizing behavior.
Although most included studies consistently found that there was an association between excessive screen time and children's mental health, Larsen et al. (54) found contradictory results. They did not find any association between the screen time and poor mental health outcomes in children.
Sleep disturbances
Of the 30 included studies, about one-third explored the association between sleep and children's mental health during COVID-19 (32, 43, 47, 48, 50, 55, 58, 61, 63, 67). With the closure of schools, home confinement and social isolation which led to significant changes in children's daily routines and activity patterns, children's sleeping patterns, such as sleep timing (delayed bedtime and rise time) and quality, were altered. Di Giorgio et al. (43) found that children's sleeping time has changed as they go to bed 53 min later and wake up about 66 min later than usual. Another study on 21,526 Chinese parents found that 74.7% parents said their children showed sleep disturbances in terms of bedtime resistance, sleep duration, sleep anxiety, sleep onset delay and night waking (55).
The quality of sleep impacted children's psychological wellbeing. Moulin El-Aarbaoui et al. (32) found that children's emotional difficulties and hyperactivity/inattention symptoms were significantly linked to sleeping difficulties. McArthur et al. (58) found that child sleep (Beta = −0.11; 95% CI −0.19−0.04) predicted anxiety. All the results point to the importance of sleep for children's psychological health.
Less physical activity
The existing literature supports the idea that physical activity is associated with many physical and mental health benefits across all age groups (69). Since children were forced to stay at home due to school closures and home confinement, the limited space at home as well as the restricted outdoor opportunities for children to be physically active were drastically reduced (70). Of the 30 included studies, eight studies (50, 55, 56, 58, 60, 61, 63, 67) examined the relations between physical activity and children's internalizing or externalizing behaviors. In an internet-based survey of 1,264 children, Liu et al. (56) found that when compared with children who did not do any physical activity, children with physical activity had a lower risk of hyperactivity-inattention (OR 0.44 for 1–2 days/week; OR 0.56 for more than 2 days/week) and fewer prosocial behavior problems (OR 0.65 for 1–2 days/week; OR 0.55 for more than 2 days/week). Overall, the results from the included studies consistently showed that there was a decrease in physical activity among children during the pandemic and a decrease in outdoor playtime. This substantial impact on the level of physical activity of children may affect children's physical and mental health (50, 63).
Unfavorable family environment factors
Increased COVID-19-related stressors among parents/primary caregivers
Of the 30 included studies, thirteen studies examined the association between perceived parental stress and children's emotional and behavioral problems during the pandemic (42, 46, 49, 51, 53, 54, 57, 61–66). Parents experienced mounting pandemic-related stress and COVID-19 contextual hardship (65), including an increase in childcare responsibilities, greater home-schooling demands and worries about the balance between increased caring responsibilities and work, family financial instability, fear of the future and many other difficulties, therefore they had higher levels of worries, anxiety and even parental burnout (a syndrome characterized by overwhelming exhaustion and the feeling of lacking achievements as parents) (51), which is detrimental to children's mental health, as children are particularly sensitive to the emotional status of their parents (71). Köhler-Dauner et al. (53) found that there was a positive and significant effect of maternal perceived stress on children's emotional problems and hyperactivity and inattention behaviors. Kerr and colleagues (51) utilized path modeling to analyze cross-sectional data from 1,000 parents and reported that parents who perceived more psychological impacts from the pandemic reported higher levels of parental burnout and less positive behavior in their children. Robertson et al. (62) investigated 286 linguistically, racially and ethnically diverse caregivers and found that caregivers' pandemic-related stress at Time 1 predicted increased child internalizing symptoms at Time 2 which, in turn, predicted increased caregivers' perceived stress at Time 3. The findings based on longitudinal data provided strong evidence for the reciprocal relationship between caregivers' perceived stress and children's mental health. The results further gave prominence to what is highlighted by the family system theorists - families are interconnected and mutually influenced (72).
Noteworthy, parents' negative affect may have spillover effects on their children via parenting (19, 73). The results of a large meta-analysis showed that parents' negative emotions were associated with harsher discipline whereas positive emotions were associated with more supportive parenting (74). Based on a cross-sectional study on 1,264 primary school children, Li and colleagues (55) found that Chinese parents reported exerting harsh parenting (i.e., scolded their child by yelling or shouting to discipline their children and regulate their misbehavior) during the pandemic (aOR 2.06; 95% CI 1.91–2.23). Harsh parenting was independently associated with child mental health problems, regardless of SES.
Deteriorated mental health of parents
Child mental health is closely linked to the wellbeing of the family members (58). This fact is supported by many existing studies, which provide strong empirical evidence that maternal wellbeing predicts child wellbeing (75, 76). About one-fifth of the included studies examined how parents' mental health impacted children's internalizing and externalizing behaviors (32, 39, 44, 45, 55, 56, 66, 67). Wang et al. (67) stressed that better parental wellbeing was associated with a decrease in child mental health problems. Liu et al. (56) found that children with anxious parents were associated with higher levels of emotional symptoms (OR 5.64, 95% CI 2.18–14.58) and total difficulty (i.e., emotional symptoms, conduct problems, hyperactivity/inattention and peer relationship problems) (OR 3.78, 95% CI 1.56–9.15) than children without anxious parents. The findings from the multiple regression analyses showed that more parental depressive symptoms predicted children's internalizing behaviors during the lockdown (45).
The longitudinal data yielded similar results. Frigerio et al. (47) found that children's emotional and behavioral problems significantly increased from the period preceding the lockdown to the period during which the lockdown was taking place and greater maternal mood symptoms were associated with an increase in anxious-depressed, withdrawn and aggressive symptoms of children during the lockdown.
Protective factors for child mental health
Resilience of parents
COVID-19 is a good instance of traumatic stress which creates significant impacts on the parents' resilience to deal with many stressors outlined in the foregoing paragraphs. Of the 30 included studies, only two studies explored the relationship between parents' resilience and children's mental health (57, 65). In Mariani Wigley et al.'s study (57), mothers' resilience was positively correlated with children's resilience. The relationship between mothers' resilience and children's stress-related behaviors was mediated by the mothers' ability to support and promote children's resilient behaviors which influences children's positive adjustment in the face of stressful situations. Therefore, parents' resilience is vital to children's mental health.
Positive parent-child relationships
It is well documented that positive parent-child relationships, which are fostered by positive parenting and supportive parental behavior, can mitigate the child negative outcomes from stressors (77). Some of the included studies examined the association between parent-child relationship and child mental health problems (39, 45, 46, 58). For instance, in Dubois-Comtois et al.'s study (45), closeness in the parent-child relationship was significantly negatively correlated with children's externalizing behaviors. Bate and colleagues (39) revealed that the emotional and behavioral health of children was moderated by positive parent-child relationships during the COVID-19 lockdown. McArthur et al. (58) found that child happiness during the COVID-19 pandemic was predicted by the connectedness to parents/caregivers (Beta = 0.36; 95% CI 0.28–0.39). In addition, lower levels of connectedness to parents/caregivers predicted child anxiety (Beta = −0.16; 95% CI −0.22 to −0.09) and depressive symptoms (Beta = −0.26; 95% CI −0.32 to −0.21) during COVID-19. Therefore, fostering positive parent-child relationships can help improve the mental health outcomes of children.
School factors
School connectedness
Schools cannot alleviate harms caused by the pandemic (59). However, they can play a crucial role in supporting children through maintaining virtual contacts throughout lockdowns and school closures. Therefore, school connectedness is important to children. School connectedness has been defined in many ways, but it encompasses engaging students academically and in school activities, having a sense of belonging and fairness, developing positive peer relationships as well as feeling supported by teachers and feeling secure at school (78). In Moore et al.'s study (59), surprisingly, there were no changes in school connectedness before and after the pandemic. The participating children reported that they had a good teacher-student relationship which was significantly associated with better mental health and life satisfaction.
Discussion
This systematic review aimed to identify the types of children at risk of developing mental health issues and summarize the risk and protective factors of children's mental health during the pandemic. Overall, the results of the 30 included studies consistently suggested that a negative impact of COVID-19 was observed on children's mental health who exhibited an increase in internalizing and externalizing behaviors. As the included studies were conducted in different countries, it is evident that children's mental health has become an area of concern globally.
Based on the 30 included studies, the worsened child mental health outcomes reflect socioeconomic inequalities. Parents with low education attainment tend to be employed in occupations that do not allow to work from home such as drivers, waiters/waitresses or supermarket workers. Their unstable income has been further affected by the pandemic resulting in either significantly reduced income or loss of employment. Financial insecurity is harmful to individuals' mental health as this can increase stress or anxiety which can worsen parenting practices leading to neglect or physical or verbal punishment or even abuse. Harsh parenting increases the risk of children's mental health problems. In addition, economically disadvantaged children normally live in crowded apartments. However, during the pandemic, housing has been a key determinant of health. Overcrowding and the size of private outdoor space play significant roles in how families adjust to social distancing restrictions and how to minimize the chance of contracting the virus from family members. It is not surprising that children living in cramped homes are more stressed (79). As Patel et al. (80) pointed out, “the pandemic has highlighted the stark inequalities within society, and it will likely exacerbate them” (p. 110). Now is therefore an opportune time for policy makers to introduce legislation to support those disadvantaged families.
Interestingly, being the only child in the family can be a risk factor. It is likely that larger household sizes mitigate some of the negative effects of social isolation, so the number of children in the household is protective of child mental health (81).
Using Bronfenbrenner's ecological systems theory (EST) (82, 83) as a lens enables us to better understand why the pandemic has had considerable impact on children's mental health. According to the EST, a child develops through the interaction of different systems (i.e., the micro-, meso-, exo-, macro- and chronosystems) from the closest to the broadest (84). During the pandemic, the children's microsystem has been compromised (38, 85) by a number of restrictions, such as the prolonged closure of schools, homeschooling and the absence of social support (peer relationships and extended families). All these persistent stressors, including a change in children's structured daily routine, increase the vulnerability of children. In addition, for parents, many pandemic-related stressors, such as juggling on-going work obligations with added childcare responsibilities and trouble in paying bills due to financial problems etc., may amplify any pre-existing mental health problems and result in higher levels of stress, anxiety and distress. If individual resilience is low, the negative psychological effects of stressors cannot be buffered. As a result, stressors may further deteriorate parents' mental health which can adversely affect family functioning resulting in problems such as more family conflicts and poor parent-child relationship. More importantly, due to the bidirectional relationship between parents and children in the microsystem, both parents and children are affected in a reciprocal manner.
During home confinement, the mesosystem has also been affected. With reduced support from collaborations between school and family (86), it is difficult for children to connect with teachers to seek support due to the closure of schools. However, it is vital for students to feel connected with schools as school connectedness has a buffering effect in helping mitigate negative mental health outcomes as shown in the current review (87).
Since both the micro- and mesosystem are embedded within the exosystem which is the layer that a child does not have direct interactions with, the exosystem impacts child development indirectly. For instance, many parents who worked remotely from home during home confinement experienced an increase in negative emotions which may have spillover effects on children indirectly via parenting practices.
The macrosystem can affect other systems as it includes political disturbances, cultural characteristics or economic disruption. During COVID-19, the shutdown measures have caused a substantial decline in the global economy. Some companies were forced to close permanently. Many people had to spend their emergency savings or borrowed loans to support their expenses, so parents have been under a heavy financial burden which is detrimental to their mental health.
The chronosystem, which incorporates the effect of time on individuals' development, includes both normative (e.g., graduation from school) and non-normative life transitions (e.g., parental divorce), environmental events and historical events. In our review, Moore et al. (59) found that there was no evidence that the pandemic had any consequences on children's feelings about the transition from primary to secondary school. The transition from primary to secondary education is a challenge and can be very stressful for children. During the pandemic, children were deprived of a well-planned transition by schools and families which can normally help remove barriers to learning and allow children to reach their full academic potential later on and not feel isolated. Future studies can explore the impact of the pandemic on children's transition in their schooling and psychological wellbeing.
Unhealthy lifestyle factors affect children's mental health. One of the root causes of unhealthy lifestyle is a lack of structured daily routines. Maintaining a structured and pre-planned day is a protective factor of children's mental health (88). Therefore, good and healthy daily habits for children can reduce the risk of mental health problems and improve their psychological wellbeing (89–91). Parents are encouraged to create and maintain healthy structured routines including sleep schedules and family media plans that foster the healthy use of recreational mobile devices (e.g., limits on duration). However, interventions focusing on reducing infants' and toddlers' screen time should be more targeted to parents, particularly parental mental health, screen time, intention to offer mobile devices to children and the needs of using mobile devices (92). Furthermore, since physical activity is associated with psychological health, promoting physical activities that can be performed in a limited space at home should be highly recommended to better support the psychological health of children.
Overall, the included studies have shown the negative impacts of the pandemic on children's mental health through the interaction of different factors. We need to support children's mental health recovery from the pandemic and it is a public health priority which requires effective actions at multiple levels of the society. Since children are particularly vulnerable and need adequate parental support, it is essential to ensure parents' mental health remains good, therefore the provision of more enhanced mental health resources and support programmes to parents to help them reduce stress, anxiety and depressive symptoms is urgently needed. With concerted efforts, children's lives can be improved.
Implications for research
When reviewing all the studies, we observed that first, many empirical studies included both children and adolescents in the same study. The limitation is that the results generated from the studies were imprecise. Designing tailor-made interventions for children becomes more difficult as children and adolescents are at different developmental stages, so future studies on children's mental health are recommended. Second, studies define the age range of children differently, so this makes the comparison of findings difficult. Third, children's data were mostly collected from mothers' reports as they are generally the primary caregivers for children. Although the literature supports this method, it is essential to take into consideration not only mothers but also other caregivers, particularly fathers whose perspectives are limited in the existing literature. Fourth, future research is needed to investigate the longitudinal impact of maternal and paternal mental health on child development due to the COVID-19 pandemic, taking into account multiple time points instead of only two. In addition, since the majority of included studies are quantitative studies, future studies could use mixed methods or longitudinal qualitative studies to capture the experience and impact of the pandemic on children's mental health over time.
Limitations of the review
The present systematic review has several limitations. First, the articles were retrieved from two large electronic databases and hand searched. Only those consisting of the relevant search terms in the title or abstract were reviewed for further analysis. Therefore, the selection of reviewed studies was limited. Second, studies that were not in English, published in conference abstracts, letters, government reports, textbooks and unpublished dissertations were excluded. Third, children with special education needs are excluded in the selection so the mental health of this group of children is less known.
Conclusion
The systematic review summarized important information about children who are at risk of mental health problems in the context of COVID-19 as well as the risk and protective factors of children's mental health. The current review serves as a wake-up call to the government to provide targeted mental health care in the community to support children, especially those severely stressed by the pandemic. Children's mental health should be one of the top priorities of the post-pandemic recovery plan.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
CN contributed to the design of the search strategy, conducted the initial searches, analysis of the findings, and prepared the first draft of the manuscript. SN conducted updated searches, reviewed the articles, and conducted the analysis of the findings. Both authors contributed to the revisions of the manuscript and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.975936/full#supplementary-material
References
1. Ainamani HE, Gumisiriza N, Rukundo GZ. Mental health problems related to COVID-19: a call for psychosocial interventions in Uganda. Psychol Trauma. (2020) 12:809–11. doi: 10.1037/tra0000670
2. Bahadur U, Pokharel S, Munikar S, Wagle CN, Adhikary P, Shahi BB, et al. Anxiety and depression among people living in quarantine centers during COVID-19 pandemic: a mixed method study from western Nepal. PLoS ONE. (2021) 16:e0254126. doi: 10.1371/journal.pone.0254126
3. Babore A, Trumello C, Lombardi L, Candelori C, Chirumbolo A, Cattelino E, et al. Mothers' and children's mental health during the COVID-19 pandemic lockdown: the mediating role of parenting stress. Child Psychiatry Hum Dev. (2021) 1−13. doi: 10.1007/s10578-021-01230-6
4. Cost KT, Crosbie J, Anagnostou E, Birken CS, Charach A, Monga S, et al. Mostly worse, occasionally better: impact of COVID-19 pandemic mental health of Canadian children and adolescents. Eur Child Adolesc Psychiatry. (2021) 31:71–84. doi: 10.1007/s00787-021-01744-3
5. Liu JJ, Bao Y, Huang X, Shi J, Lu L. Mental health considerations for children quarantined because of COVID-19. Lancet Child Adolesc Health. (2020) 4:347–9. doi: 10.1016/S2352-4642(20)30096-1
6. Putri RS, Purwanto A, Pramono R, Asbari M, Wijayanti LM, Hyun CC. Impact of the COVID-19 pandemic on online home learning: an explorative study of primary schools in Indonesia. Int J Adv Sci Technol. (2020) 29:4809–18.
7. Singh S, Roy D, Sinha K, Parveen S, Sharma G, Joshi G. Impact of COVID-19 and lockdown on mental health of children and adolescents: a narrative review with recommendations. Psychiatry Res. (2020) 293:113429. doi: 10.1016/j.psychres.2020.113429
8. Wang C, Xiao S, Sun Y, Wang J, Xu T. Psychosocial impact of respiratory infectious disease pandemics on children: a systematic review. Res Square. (2020) 1–14. doi: 10.21203/rs.3.rs-41460/v1
9. de Laia Almeida IL, Rego JF, Teixerira ACG, Moreira MR. Social isolation and its impact on child and adolescent development: a systematic review. Rev Paul Pediatr. (2022) 40:e2020385. doi: 10.1590/1984-0462/2022/40/2020385
10. Breidokiené R, Jusiene R, Urbonas V, Praninskiene R, Girdzijauskiene S. Sedentary behavior among 6-14-year-old children during the COVID-19 lockdown and its relation to physical and mental health. Healthcare. (2021) 9:756. doi: 10.3390/healthcare9060756
11. Dunton GF, Do B. Wang SD. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the US. BMC Public Health. (2020) 20:1351. doi: 10.1186/s12889-020-09429-3
12. Domingues-Montanari S. Clinical and psychological effects of excessive screen time on children. J Paediatr Child Health. (2016) 53:333–8. doi: 10.1111/jpc.13462
13. Grechyna D. Health Threats Associated with Children Lockdown in Spain During COVID-19. (2020) 1–12. doi: 10.2139/ssrn.3567670
14. Falbe J, Davison KK, Franckle RL, Ganter C, Gortmaker SL, Smith L, et al. Sleep duration, restfulness, and screens in the sleep environment. Pediatr. (2015) 135:e367–75. doi: 10.1542/peds.2014-2306
15. Zhao J, Xu J, He Y, Xiang M. Children and adolescents' sleep patterns and their associations with mental health during the COVID-19 pandemic in Shanghai, China. J Affect Disord. (2022) 301:337–44. doi: 10.1016/j.jad.2021.12.123
16. Arufe-Giráldez V, Sanmiguel-Rodríguez A, Zagalaz-Sánchez ML, Cachón-Zagalaz J., González-Valero G. Sleep, physical activity and screens in 0-4 years Spanish children during the COVID-19 pandemic: were the WHO recommendations met? J Hum Sport Exerc. (2022) 17:484–503. doi: 10.14198/jhse.2022.173.02
17. Liu Y, Lu L, Wang WX, Liu S, Chen HR, Gao X, et al. Job burnout and occupational stressors among Chinese healthcare professionals at county-level health alliances. Int J Environ Res Public Health. (2020) 17:1848. doi: 10.3390/ijerph17061848
18. Cheng TL, Moon M, Artman M. Pediatric Policy Council. Shoring up the safety net for children in the COVID-19 pandemic. Pediatr Res. (2020) 88:349–51. doi: 10.1038/s41390-020-1071-7
19. Ng CSM. Effects of workplace bullying on Chinese children's health, behaviors and school adjustment via parenting: Study protocol for a longitudinal study. BMC Public Health. (2019) 19:129. doi: 10.1186/s12889-019-6458-1
20. Centers for Disease Control Prevention (CDC) Children's mental health. (2022). Available online at: https://www.cdc.gov/childrensmentalhealth/features/mental-health-children-and-parents.html (accessed August 25, 2022).
21. Maguire A, Ross E, O'Reilly D. Parental mental health and risk of poor mental health and death by suicide in offspring: a population-wide data-linkage study. Epidemiol Psychiatr Sci. (2022) 31:1–9. doi: 10.1017/S2045796022000063
22. Stone LL, Mares SW, Otten R, Engels RME, Janssens J. The co-development of parenting stress and childhood internalizing and externalizing problems. J Psychopathol Behav Assess. (2016) 38:76–86. doi: 10.1007/s10862-015-9500-3
23. Fisher PA, Beauchamp KG, Roos LE, Noll LK, Flannery J, Delker BC. The neurobiology of intervention and prevention in early adversity. Annu Rev Clin Psychol. (2016) 12:331–57. doi: 10.1146/annurev-clinpsy-032814-112855
24. World Economic Forum. COVID-19 is Hurting Children's Mental Health. Here's how to help. (2020). Available online at: https://www.weforum.org/agenda/2020/05/covid-19-is-hurting-childrens-mentalhealth/ (accessed August 22, 2022).
25. Golberstein E, Wen H, Miller BF. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatr. (2020) 174:819–20. doi: 10.1001/jamapediatrics.2020.1456
26. Jiao WY, Wang LN, Liu J, Fang SF, Jiao FY, Pettoello-Mantovani M, et al. Behavioral and emotional disorders in children during the COVID-19 epidemic. J Pediatr. (2020) 221:264–6. doi: 10.1016/j.jpeds.2020.03.013
27. Roos LE, Salisbury M, Penner-Goeke L, Cameron EE, Protudjer JLP, Guiliano R et al. Supporting families to protect child health: parenting quality and household needs during the COVID-19 pandemic. PLoS ONE. (2021) 16:e0251720. doi: 10.1371/journal.pone.0251720
28. Clark H, Coll-Seck AM, Banerjee A, Peterson S, Dalglish S, Ameratunga S, et al. A future for the world's children? A WHO-UNICEF-Lancet Commission. Lancet. (2020) 395:605–58. doi: 10.1016/S0140-6736(19)32540-1
29. Henderson MD, Schmus CJ, McDonald CC, Irving SY. The COVID-19 pandemic and the impact on child mental health: a socio-ecological perspective. Pediatr Nurs. (2020) 46:267–72.
30. Bronfenbrenner U. Recent advances in research on the ecology of human development. In: Silbereisen RK, Eyferth K, Rudinger G, editors. Development as Action in Context: Problem Behavior and Normal Youth Development. New York: Springer. (1986). p. 286–309.
31. Elharake JA, Akbar F, Malik AA, Gilliam W, Omer SB. Mental health impact of COVID-19 among children and college students: a systematic review. Child Psychiatry Hum Dev. (2022) 11:1–13. doi: 10.1007/s10578-021-01297-1
32. *Moulin El-Aarbaoui T, Bustamante JJH, Héron M, Mary-Krause M, Rouquette A, Galéra C, et al. Risk and protective factors related to children's symptoms of emotional difficulties and hyperactivity/inattention during the COVID-19-related lockdown in France: results from a community sample. Eur Child Adolesc Psychiatry. (2021) 9:1–12. doi: 10.1007/s00787-021-01752-3
33. Koller D, Nicholas D, Gearing R, Kalfa O. Pediatric pandemic planning: children's perspectives ad recommendations. Health Soc Care Community. (2010) 18:369–77. doi: 10.1111/j.1365-2524.2009.00907.x
34. Murray CJS. A collaborative approach to meeting the psychosocial needs of children during an influenza pandemic. J Spec Pediatr Nurs. (2010) 15:135–43. doi: 10.1111/j.1744-6155.2009.00229.x
35. Sprang G, Silman M. Using professional organizations to prepare the behavioral health workforce to respond to the needs of pediatric populations impacted by health-related disasters: guiding principles and challenges. Disaster Med Public Health Prep. (2015) 9:642–9. doi: 10.1017/dmp.2015.82
36. Moher D, Liberati A, Tetzlaff J, Altman DG. Reprint—preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Phys Ther. (2009) 89:873–80. doi: 10.1093/ptj/89.9.873
37. Hawker S, Payne S, Kerr C, Hardey M, Powell J. Appraising the evidence: reviewing disparate data systematically. Qual Health Res. (2002) 12:1284–99. doi: 10.1177/1049732302238251
38. Ali A, Hassiotis A, Strydom A, King M. Self stigma in people with intellectual disabilities and courtesy stigma in family carers: a systematic review. Res Dev Disabil. (2012) 33:2122–40. doi: 10.1016/j.ridd.2012.06.013
39. *Bate J, Pham PT, Borelli JL. Be my safe haven: parent–child relationships and emotional health during COVID-19. J Pediatr Psychol. (2021) 46:624–34. doi: 10.1093/jpepsy/jsab046
40. *Bhogal A, Borg B, Jovanovic T, Marusak HA. Are the kids really alright? Impact of COVID-19 on mental health in a majority Black American sample of schoolchildren. Psychiatry Res. (2021) 304:114146. doi: 10.1016/j.psychres.2021.114146
41. *Browne DT, Wade M, May SS, Maguire N, Wise D, Estey K, et al. Children's mental health problems during the initial emergence of COVID-19. Can Psychol. (2021) 62:65–72. doi: 10.1037/cap0000273
42. *Christner N, Essler S, Hazzam A, Paulus M. Children's psychological wellbeing and problem behavior during the COVID-19 pandemic: an online survey during the lockdown period in Germany. PLoS ONE. (2021) 16:e0253473. doi: 10.1371/journal.pone.0253473
43. *Di Giorgio E, Di Riso D, Mioni G, Cellini N. The interplay between mothers' and children behavioral and psychological factors during COVID-19: an Italian study. Eur Child Adolesc Psychiatry. (2020) 30:1401–12. doi: 10.1007/s00787-020-01631-3
44. *Dollberg DG, Hanetz-Gamliel K, Levy S. COVID-19, child's behavior problems, and mother's anxiety and mentalization: a mediated moderation model. Curr Psychol. (2021) 1–12. doi: 10.1007/s12144-021-02476-y
45. *Dubois-Comtois K, Suffren S, St-Laurent D, Milot T, Lemelin JP. Child psychological functioning during the COVID-19 lockdown: an ecological, family-centered approach. J Dev Behav Pediatr. (2021) 42:532–9. doi: 10.1097/DBP.0000000000000935
46. Brocki KC, Frick MA, Ronchi L, Hughes C. Family function and child adjustment difficulties in the COVID-19 pandemic: an international study. Int J Environ Res Public Health. (2021) 18:11136. doi: 10.3390/ijerph182111136
47. *Frigerio A, Nettuno F, Nazzari S. Maternal mood moderates the trajectory of emotional and behavioural problems from pre- to during the COVID-19 lockdown in preschool children. Eur Child Adolesc Psychiatry. (2022) 1–11. doi: 10.1007/s00787-021-01925-0
48. *Gassman-Pines A, Ananat EO, Fitz-Henley J. COVID-19 and parent-child psychological wellbeing. Pediatrics. (2020) 146:e2020007294. doi: 10.1542/peds.2020-007294
49. *Giannotti M, Mazzoni N, Bentenuto A, Venuti P, de Falco S. Family adjustment to COVID-19 lockdown in Italy: parental stress, coparenting, and child externalizing behavior. Fam Process. (2022) 61:745–63. doi: 10.1111/famp.12686
50. *Hyunshik K, Jiameng M, Sunkyoung L, Ying G. Change in Japanese children's 24-hour movement guidelines and mental health during the COVID-19 pandemic. Sci Rep. (2021) 11:22972. doi: 10.1038/s41598-021-01803-4
51. Kerr ML, Fanning KA, Huynh T, Botto I, Kim CN. Parents' self-reported psychological impacts of COVID-19: associations with parental burnout, child behavior, and income. J Pediatr Psychol. (2021) 46:1162–71. doi: 10.1093/jpepsy/jsab089
52. *Köhler-Dauner F, Buchheim A, Hildebrand K, Mayer I, Clemens V, Ziegenhain U, et al. Maternal attachment representation, the risk of increased depressive symptoms and the influence on children's mental health during the SARS-CoV-2-pandemic. J Child Fam Stud. (2021) 31:392–408. doi: 10.1007/s10826-021-02162-4
53. *Köhler-Dauner F, Clemens V, Lange S, Ziegenhain U, Fegert JM. Mothers' daily perceived stress influences their children's mental health during SARS-CoV-2-pandemic—an online survey. Child Adolesc Psychiatry Ment Health. (2021) 15:1–31. doi: 10.1186/s13034-021-00385-3
54. *Larsen L, Helland MS, Holt T. The impact of school closure and social isolation on children in vulnerable families during COVID-19: a focus on children's reactions. Eur Child Adolesc Psychiatry. (2021) 31:1−11. doi: 10.1007/s00787-021-01758-x
55. *Li W, Wang Z, Wang G, Ip P, Sun X, Jiang Y, et al. Socioeconomic inequality in child mental health during the COVID-19 pandemic: first evidence from China. J Affect Disord. (2021) 287:8–14. doi: 10.1016/j.jad.2021.03.009
56. *Liu Q, Zhou Y, Xie X, Xue Q, Zhu K, Wan Z, et al. The prevalence of behavioral problems among school-aged children in home quarantine during the COVID-19 pandemic in China. J Affect Disord. (2021) 279:412–6. doi: 10.1016/j.jad.2020.10.008
57. *Mariani Wigley ILC, Mascheroni E, Bulletti F, Bonichini S. COPEWithME: The role of parental ability to support and promote child resilient behaviors during the COVID-19 emergency. Front Psychol. (2021) 12:732745. doi: 10.3389/fpsyg.2021.732745
58. *McArthur BA, Racine N, McDonald S, Tough S, Madigan S. Child and family factors associated with child mental health and wellbeing during COVID-19. Eur Child Adolesc Psychiatry. (2021) 24:1–11. doi: 10.1007/s00787-021-01849-9
59. *Moore G, Anthony R, Angel L, Hawkins J, Morgan K, Copeland L, et al. Mental health and life satisfaction among 10-11-year-olds in Wales, before and one year after onset of the COVID-19 pandemic. BMC Public Health. (2022) 22:379. doi: 10.1186/s12889-022-12752-6
60. *Oliveira VH, Martins PC, Carvalho GS. Children's daily activities and wellbeing during the COVID-19 lockdown: associations with child and family characteristics. Curr Psychol. (2022) 1–12. doi: 10.1007/s12144-022-02759-y
61. *Park JH, Park JY, Jin KS. What did COVID-19 change? The impact of COVID-19 on Korean parents' and children's daily lives and stress. Child Psychiatry Hum Dev. (2021) 53:172–82. doi: 10.1007/s10578-021-01262-y
62. *Robertson EL, Piscitello J, Schmidt E, Mallar C, Davidson B, Natale, R. Longitudinal transactional relationships between caregiver and child mental health during the COVID-19 global pandemic. Child Adolesc Psychiatry Ment Health. (2021) 15:66. doi: 10.1186/s13034-021-00422-1
63. Thind PS, Verma MK, Kaur M, Singh D. Implications of COVID-19-induced nationwide lockdown on children's behaviour in Punjab, India. Child Care Health Dev. (2021) 47:128–35. doi: 10.1111/cch.12816
64. Specht IO, Rohde JF. Nielsen AK, Larsen SC, Heitmann BL. Changes in emotional-behavioral functioning among pre-school children following the initial stage Danish COVID-19 lockdown and home confinement. Front Psychol. (2021) 12:643057. doi: 10.3389/fpsyg.2021.643057
65. *Thompson SF, Shimomaeda L, Calhoun R, Moini N, Smith MR, Lengua LJ. Maternal mental health and child adjustment problems in response to the COVID-19 pandemic in families experiencing economic disadvantage. Res Child Adolesc Psychopathol. (2022) 50:695–708. doi: 10.1007/s10802-021-00888-9
66. *Wang J, Chen Y, Guo X, Lin H, Richards M, Wang H, et al. Impact of COVID-19 related knowledge and precautions on emotional and behavioral problems among children during the post-pandemic in China: the explanatory value of emotional problems among caregivers. Front Psychol. (2021) 12:712529. doi: 10.3389/fpsyg.2021.712529
67. *Wang P, Sun X, Li W, Wang Z, He S, Zhai F, et al. Mental health of parents and preschool-aged children during the COVID-19 pandemic: the mediating role of harsh parenting and child sleep disturbances. Front Psychiatry. (2021) 12:746330. doi: 10.3389/fpsyt.2021.746330
68. Moore SA, Faulkner G, Rhodes RE, Brussoni M, Chulak-Bozzer T, Ferguson LJ, et al. Impact of the COVID-19 virus outbreak on movement and play behaviors of Canadian children and youth: a national survey. Int J Behav Nutr Phys Act. (2020) 17:1–11. doi: 10.1186/s12966-020-00987-8
69. Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, et al. The physical activity guidelines for Americans. JAMA. (2018) 320:2020–28. doi: 10.1001/jama.2018.14854
70. Nathan A, George P, Ng M, Wenden E, Bai P, Phiri Z, et al. Impact of COVID-19 restrictions on Western Australian children's physical activity and screen time. Int J Environ Res Public Health. (2021) 18:2583. doi: 10.3390/ijerph18052583
71. Imran N, Zeshan M, Pervaiz Z. Mental health considerations for children & adolescents in COVID-19 Pandemic. Pak J Med Sci. (2020) 36:S67–72. doi: 10.12669/pjms.36.COVID19-S4.2759
72. Kerr ML, Rasmussen HF, Fanning KA, Braaten SM. Parenting during COVID-19: a study of parents' experiences across gender and income levels. Fam Relat. (2021) 1–16. doi: 10.1111/fare.12571
73. Stewart W, Barling J. Fathers' work experiences effect children's behaviors via job-related affect and parenting behaviors. J Organ Behav. (1996)17:221–32.
74. Rueger SY, Katz RL, Risser HJ, Lovejoy MC. Relations between parental affect and parenting behaviors: a meta-analytic review. Parent Sci Pract. (2011) 11:1–33. doi: 10.1080/15295192.2011.539503
75. Masten AS, Narayan AJ. Child development in the context of disaster, war, and terrorism: pathways of risk and resilience. Annu Rev Psychol. (2012) 63:227–57. doi: 10.1146/annurev-psych-120710-100356
76. Prime H, Wade M, Browne DT. Risk and resilience in family wellbeing during the COVID-19 pandemic. Am Psychol. (2020) 75:631–43. doi: 10.1037/amp0000660
77. Eisenberg N, Spinrad TL, Taylor ZE, Liew J. Relations of inhibition and emotion-related parenting to young children's prosocial and vicariously induced distress behavior. Child Dev. (2019) 90:846–58. doi: 10.1111/cdev.12934
78. Libbey HP. Measuring student relationships to schools: attachment, bonding, connectedness, and engagement. J Sch Health. (2004) 74:274–83. doi: 10.1111/j.1746-1561.2004.tb08284.x
79. Amerio A, Brambilla A, Morganti A, Aguglia A, Bianchi D, Santi F, et al. COVID-19 lockdown: housing built environment's efects on mental health. Int J Environ Res Public Health. (2020) 17:16. doi: 10.3390/ijerph17165973
80. Patel JA, Nielsen FBH, Badiani AA, Assi S, Unadkat VA, Patel B, et al. Poverty, inequality and COVID-19: the forgotten vulnerable. Public Health. (2020) 183:110–1. doi: 10.1016/j.puhe.2020.05.006
81. Grinde B, Tambs K. Effect of household size on mental problems in children: results from the Norwegian mother and child cohort study. BMC Psychol. (2016) 4:31. doi: 10.1186/s40359-016-0136-1
82. Bronfenbrenner U. Toward an experimental ecology of human development. Am Psychol. (1977) 32:513–31. doi: 10.1037/0003-066X.32.7.513
83. Bronfenbrenner U. The Ecology of Human Development: Experiments by Nature and Design. Cambridge, MA: Harvard University Press. (1979).
84. Nowicka P, Ek A, Jurca-Simina IE, Bouzas C, Argelich E, Nordin K, et al. Explaining the complex impact of the COVID-19 pandemic on children with overweight and obesity: a comparative ecological analysis of parents' perceptions in three countries. BMC Public Health. (2022) 22:1000. doi: 10.1186/s12889-022-13351-1
85. Chachar AS, Younus S, Ali W. Developmental understanding of death and grief among children during COVID-19 pandemic: application of Bronfenbrenner's bioecological model. Front Psychiatry. (2021) 12:654584. doi: 10.3389/fpsyt.2021.654584
86. Lin PI, Srivastava G, Beckman L, Kim Y, Hallerback M, Barzman D, et al. A framework-based approach to assessing mental health impacts of the COVID-19 pandemic on children and adolescents. Front Psychiatry. (2021) 12:655481. doi: 10.3389/fpsyt.2021.655481
87. Hertz MF, Kilmer G, Verlenden J, Liddon N, Raspberry CN, Barrios LC, et al. Adolescent mental health, connectedness, and mode of school instruction during COVID-19. J Adolesc Health. (2022) 70:57–63. doi: 10.1016/j.jadohealth.2021.10.021
88. Brazendale K, Drenowatz C, Falck RS, Randel AB, Hoffmeyer JD, Hand GA, et al. Depressive symptoms are positively associated with time spent sedentary in healthy young US adults. Prog Prev Med. (2017) 2:1–4. doi: 10.1097/pp9.0000000000000004
89. Coyne SM, Hurst JL, Dyer WJ, Hunt Q, Schvanaveldt E, Brown S et al. Suicide risk in emerging adulthood: associations with screen time over 10 years. J Youth Adolesc. (2021) 50:2324–38. doi: 10.1007/s10964-020-01389-6
90. Khan A, Uddin R, Lee EY. Excessive recreational Internet use was associated with poor mental health in adolescents. Acta Paediatr. (2021) 110:571–3. doi: 10.1111/apa.15528
91. Schonert-Reichl KA. Middle Childhood Inside and Out: The Psychological and Social Worlds of Canadian Children Ages 9–12. Report for the United way of the Lower Mainland. Vancouver, BC: University of British Columbia (2011).
92. Pedrotti BG, Mallmann MY, Almeida CRS, Marques FM, Vescovi G, da Santos Riter H, et al. Infants' and toddlers' digital media use and mothers' mental health: a comparative study before and during the COVID-19 pandemic. Infant Ment Health. (2022) 43:24–35. doi: 10.1002/imhj.21952
*^Studies that were included in this review were marked with an asterisk.
Keywords: COVID-19, mental health, internalizing behaviors, externalizing behaviors, children, systematic review
Citation: Ng CSM and Ng SSL (2022) Impact of the COVID-19 pandemic on children's mental health: A systematic review. Front. Psychiatry 13:975936. doi: 10.3389/fpsyt.2022.975936
Received: 22 June 2022; Accepted: 22 September 2022;
Published: 18 October 2022.
Edited by:
Yanping Bao, Peking University, ChinaReviewed by:
Daniela Marchetti, University of Studies G. d'Annunzio Chieti and Pescara, ItalyAlessandra Gabellone, University of Bari Aldo Moro, Italy
Copyright © 2022 Ng and Ng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Catalina Sau Man Ng, Y3NtbmdAZWR1aGsuaGs=
†ORCID: Catalina Sau Man Ng orcid.org/0000-0002-3096-4877
 Catalina Sau Man Ng
Catalina Sau Man Ng Sally Sui Ling Ng
Sally Sui Ling Ng