- 1Research Coordination and Support Service, Istituto Superiore di Sanità, Rome, Italy
- 2Department of Mental Health, Friuli Centrale Healthcare Agency, Udine, Italy
- 3Central Health Directorate, Friuli-Venezia Giulia Region, Trieste, Italy
- 4Directorate General of Health Prevention, Ministry of Health, Rome, Italy
- 5Emilia-Romagna Region, Bologna, Italy
Personal budgets (PBs) may improve the lives of people with mental health conditions and people with intellectual disability (ID). However, a clear definition of PB, benefits, and challenges is still faded. This work aims to systematically review evidence on PB use in mental health and ID contexts, from both a qualitative and quantitative perspective, and summarize the recent research on interventions, outcomes, and cost-effectiveness of PBs in beneficiaries with mental health conditions and/or ID. The present systematic review is an update of the existing literature analyzed since 2013. We performed a systematic search strategy of articles using the bibliographic databases PubMed and PsycINFO. Six blinded authors screened the works for inclusion/exclusion criteria, and two blinded authors extracted the data. We performed a formal narrative synthesis of the findings from the selected works. A total of 9,800 publications were screened, and 29 were included. Improvement in responsibility and awareness, quality of life, independent living, paid work, clinical, psychological, and social domains, and everyday aspects of the users’ and their carers’ life have been observed in people with mental health conditions and/or ID. However, the PBs need to be less stressful and burdensome in their management for users, carers, and professionals. In addition, more quantitative research is needed to inform PBs’ policymakers.
Systematic Review Registration: [www.crd.york.ac.uk/prospero/], identifier [CRD42020172607].
Introduction
Personalization is a key element of the healthcare policy, as underlined by the World Health Organization (WHO) (1). It is built on a conception of a health system prioritizing human principles and rights, like equality, participation, self-determination, and non-discrimination. This means treating patients from a person-centered perspective, listening to their needs, and recognizing their capacities and freedom to choose their health. A person-centered approach should also tailor integrated services and goods to the needs of the individual with the goal of personal wellbeing (1). In this perspective, the delivery of the innovative intervention to set people at the center of their care and meet their identified health and wellbeing needs is a public health system’s strategic action.
Among organization and management models based on this healthcare approach, personal budget (PB) consists of a sum of money allocated to an individual with the specific aim of fulfilling personal health needs. It derives from an evolution of direct payment, introduced in the United Kingdom in 1997 for disabled people, and subsequently extended and implemented across all adult social care (2, 3). The budget can be directly given to the beneficiary, or it can be managed by an intermediary belonging to the social or the public healthcare, delegated to purchase the services according to the person’s needs (4, 5).
Although the adoption of PB for health and social care is a challenge for the healthcare system, implying a change from the traditional care model, several benefits have been identified. The patient is placed as a subject rather than an object of care and can be actively involved in deciding on how to spend the budget and which services may best suit their personal needs. PBs can promote autonomy and empowerment by giving the patient the chance to participate in care actively, and the beneficiaries may experience more control and flexibility over care providers. Moreover, PBs consider different kinds of essential parts of health, like housing, employment, education, relationships, cultural background, and greater integration between health and social care, finally enabling people to select services they need, may reduce costs, and improve care planning (6). However, concern has also been expressed on PBs. An inner risk of direct payment, for instance, can arise from spending money in ways that do not turn out to be effective or in abuse by PB holders (4). Other consequences may involve the lack of quality and assurance in employment conditions and the risk of creating an unregulated situation (7).
Personal budgets have been tested in different countries, including the United Kingdom, Belgium, Denmark, Italy, Finland, Austria, France, Sweden, Germany, Australia, and the United States, with different types of programs, varying from inclusion criteria related to commissioned services or the person’s degree of choice. Most programs aimed to promote autonomy and independent living, whereas others focused on the caregiver’s system. In Belgium, for instance, the aim was to reduce the use of expensive residential care, while in the United States it was a shortage of long-term staff. The target population also differed between countries. In Canada, PBs were directed to children with learning disabilities, whereas in the United Kingdom the focus was on the elderly and on subjects with long-term disabilities (8).
National and international PB’s experience mainly refers to users in charge of mental health services and their carers (5, 6, 9–11). This population has reported personal satisfaction related to the greater choice and motivation (12), greater participation in community life and supported employment related to self-directed initiatives (13), and overall better quality of life experienced with PBs’ programs (6). For example, the “Florida Self-Directed Care Program” offered to people with persistent mental illness resulted those participants rarely resorted to crisis stabilization units compared to non-participants (8). In a previous review, Webber et al. suggested positive outcomes regarding choice and control, impact on quality of life, service use, and cost-effectiveness for PB users in mental health. However, methodological limitations (i.e., different outcomes measures, limited follow-up periods, small sample size, and qualitative study design) limited the conclusions. Moreover, PB programs were implemented differently among countries, leading to additional difficulties in generalizing practices (14). Additional studies have been conducted in recent years, providing further evidence on the possible benefits of using PB in mental health settings. This is essential to inform current PB policies and practices with people with mental health conditions.
We believe that the inclusion, in the population benefiting of the PBs, of people with intellectual disability (ID) together with people with mental health conditions is important. Higher rate of mental illness in comparison with the general population is consistently observed in adults with ID (15, 16). A wide-ranging prevalence of 14–75% for clinically distinguishable mental illness in people with ID has been identified (17). ID is also considered among the leading psychiatric diagnoses and contributes, along with other mental disorders, to a major burden in terms of disability among young people (18). Mental health services should be prepared to meet the needs of people with ID.
In this study, thus, we aimed (a) to review the literature available from 2013 on PBs’ use in mental health contexts, from both a qualitative and quantitative perspective, and (b) to summarize the recent evidence on interventions, outcomes, and cost-effectiveness of PBs in beneficiaries with mental health conditions and/or with ID.
Materials and methods
Search strategy
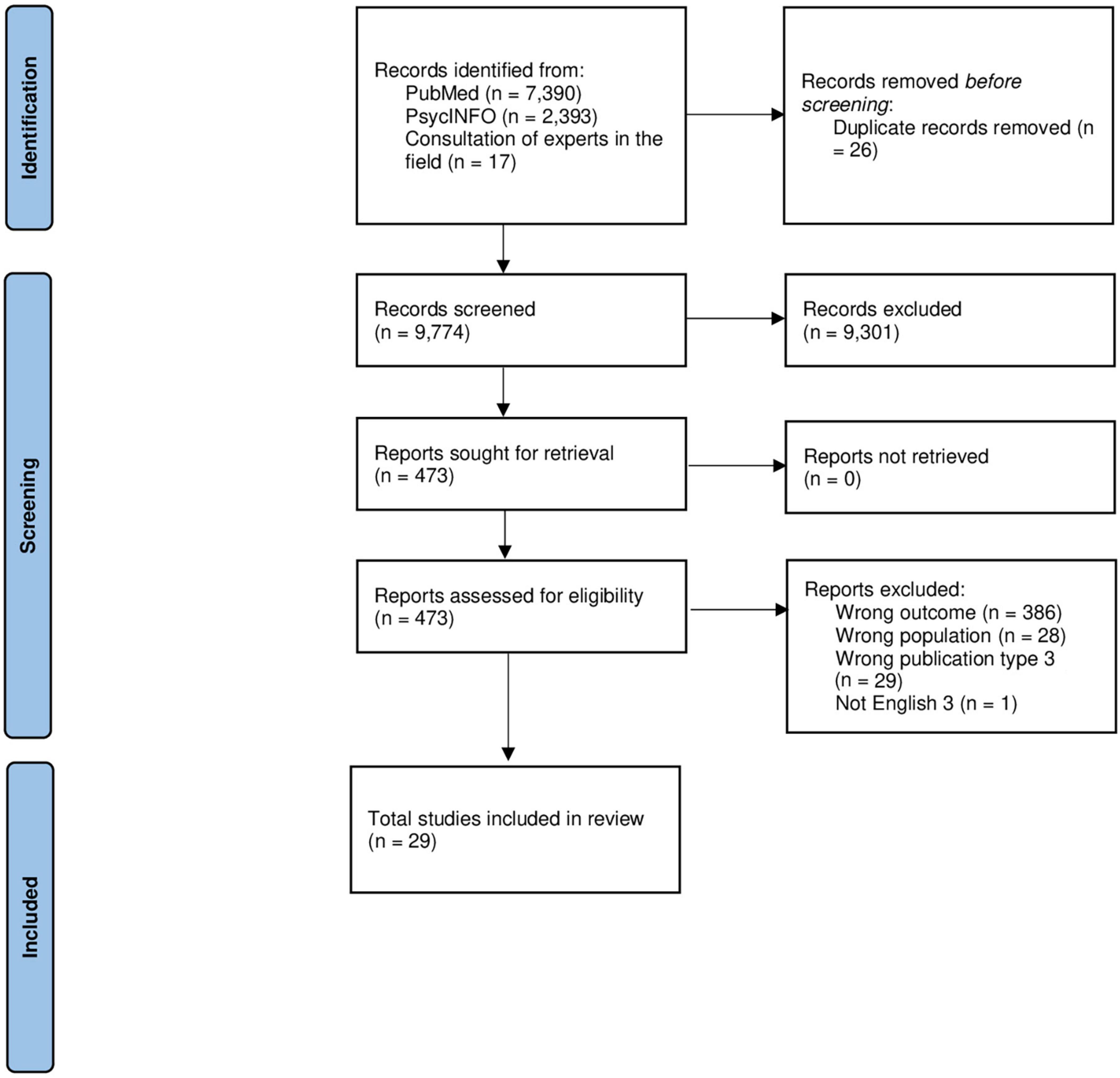
First, we interrogated PROSPERO1 to search for ongoing systematic reviews. Since no systematic reviews were scheduled, our protocol was registered with PROSPERO: CRD42020172607. The present systematic review followed the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [Supplementary Figure 1; (19)]. We performed a systematic search strategy of articles indexed from 01 April 2013 to 15 September 2021 using the bibliographic databases PubMed and PsycINFO. We choose to start our search strategy in April 2013 because the latest systematic review on the field ended its search strategy in that period (14). The search strategy focused on Population, Intervention, Comparison, and Outcomes (PICO) domains. Population: PB for people with mental health conditions and/or people with ID. Intervention: terms related to the PB; Comparison: not applicable; Outcome: desired and undesirable effects of PB. We developed the search strategy using a combination of MeSH (Medical Subject Headings) and terms to capture the available literature on the topic. The present search strategy was used for PubMed database, including planned limits, such that it could be repeated, and was prepared and adapted using appropriate syntax for PsycINFO database. When available, search filters were applied to limit the search to “Humans.” Language restriction to English has been applied. This search strategy was peer-reviewed by experts in the field. Details of the search strategy are presented in Supplementary Table 1. Moreover, the reference lists from identified studies were scanned to identify any other relevant studies. We contacted experts in the field to determine whether there are any ongoing trials or unpublished results in this area.
Selection process
The articles/reviews detected through the search strategy were collected in the Systematic Review Rayyan QCRI application (20), which also supported the authors in excluding duplicates. Six blinded authors screened the works for inclusion and exclusion criteria (LG, MM, AC, FF, EF, and GC), and two blinded authors extracted the data (LG and MM). We included quantitative and qualitative studies that report methods and models of PB for people with mental health conditions. We excluded works not in English and published before April 2013. The works that did not meet the inclusion criteria based on the titles and abstracts were excluded by at least two independent authors. Works were checked in their full text by at least two independent authors. Conflicts were discussed between two authors, and if needed, the consultation of third independent author was requested. Figure 1 illustrates the flow chart of the literature selection process.
Data extraction and synthesis
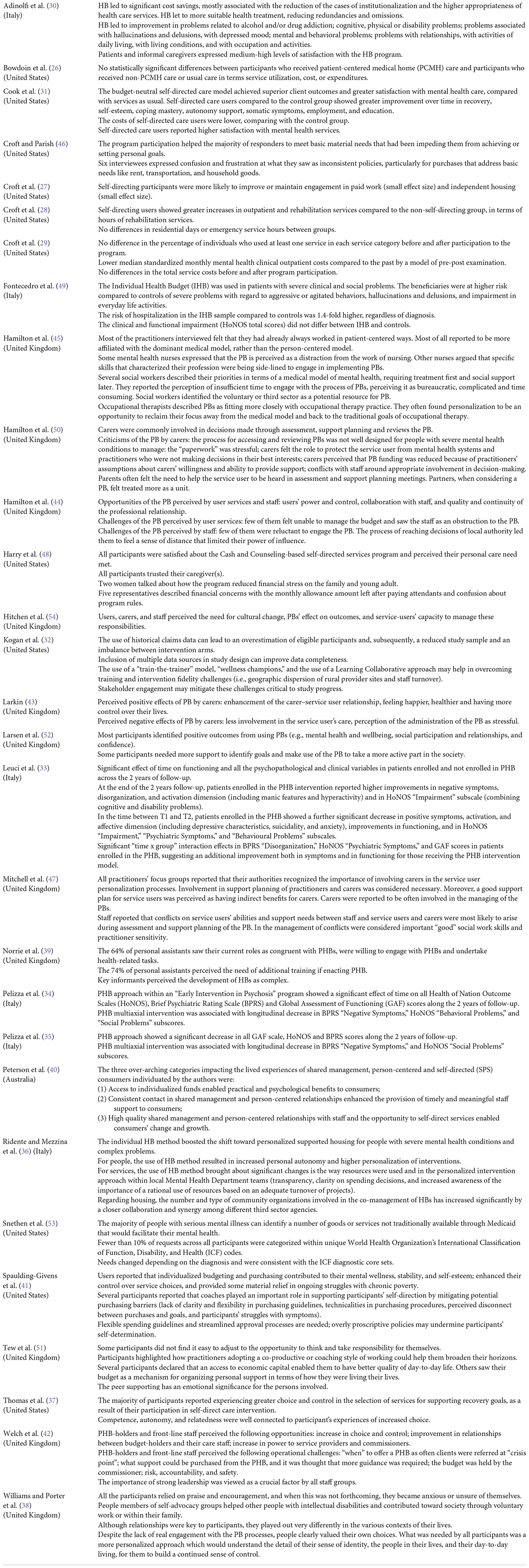
The data of the works that passed the selection process were extracted in a data extraction Excel form (available on request). To ensure consistency across authors, we conducted calibration exercises before starting to extract the data. Two independent authors (LG and MM) collected the general information of the publication: first author, year of publication, country where was conducted the study, funding sources, and potential conflict of interests. We collected the study’s design, description and sample size of the intervention group, description and sample size of the control group(s), age in years of the population (mean, SD, and range), percentage of females, name of the intervention, instrument used to measure the outcomes, length of the follow-up (if present), length of the budget, item purchased (Table 1), and summary of findings (Table 2). The data from the included full texts were extracted and independently cross-checked by two authors (LG and MM). We performed a formal narrative synthesis of the findings from the selected works.
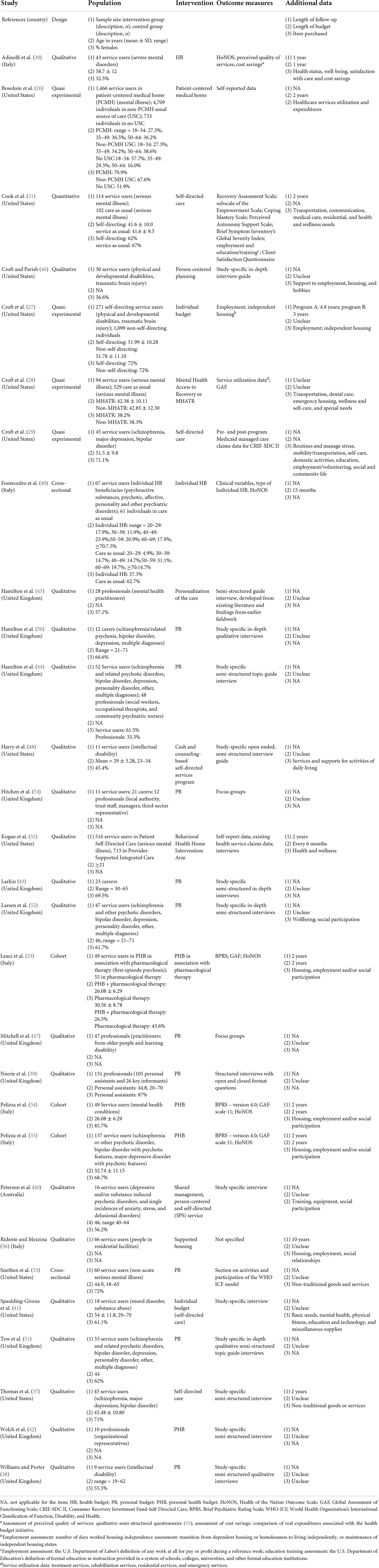
Table 1. Summary of the description of the included works on personal budget for people with mental health conditions.
Quality assessment of the evidence
Two independent authors (MM and LG) assessed risk of bias in the selected studies. Twenty eligible qualitative works were evaluated through 10-questions Critical Appraisal Skills Programme (21) Qualitative Study Checklist; two cross-sectional studies were evaluated using the Joanna Briggs Institute (JBI) Checklist for Analytical Cross-Sectional Studies (22); three cohort studies were evaluated using the Critical Appraisal Skills Programme (23); Critical Appraisal Skills Programme (24) and four quasi-experimental studies were evaluated using the JBI Critical Appraisal Checklist for Quasi-Experimental Studies (non-randomized experimental studies) (25). Any disagreements were solved in conjunction with a third author (AC). Supplementary Tables 2–5 summarize the risk-of-bias assessment results.
Results
The search strategy provided 9,800 works (PubMed, n = 7,390; PsycINFO, n = 2,393, and 17 consulting experts in the field). One author (MM) removed 26 duplicates. A total of 9,774 works were screened for inclusion and exclusion criteria. Based on the titles and abstracts screening, 9,301 not pertinent works were excluded. The remaining 473 works were checked in their full text. Studies not exploring PB (n = 386, wrong outcome) or exploring PB outside the mental health context and/or ID, including dementia, were excluded (n = 28, wrong population). In addition, 29 works were excluded because of reviews, case reports, comments, editorials, and letters (wrong publication type). Finally, one study was excluded because not in English. Conflicts were solved between authors, and for 69 works, the consultation of a third independent author was required. Finally, we evaluated 29 works as eligible for the data extraction process. Figure 1 provides the process of records’ identification and screening, and the eligibility and inclusion actions (19). Supplementary Appendix lists the reference of the 29 works included in the systematic review.
A meta-analysis of the extracted data was not possible since data of the systematic reviews were mostly qualitative and heterogeneous in the description of the PBs.
Risk-of-bias assessment
Regarding the 20 qualitative studies, the case 2A intra-class correlation between reviewers was high (0.94; 95% CI = 0.80–0.98). This value indicates excellent reliability. Risk-of-bias overall rating ranged from 2 to 9 (mean = 5.70; SD = 2.53). The most common weaknesses were observed for the item number 3 (appropriate research design) for 14 studies, number 6 (researcher reflexivity) for 19 studies, number 8 (appropriate data analysis) for 13 studies, and number 9 (clear statement of findings) for 11 studies. Risk-of-bias ratings of the included qualitative studies are reported in Supplementary Table 2.
Regarding the two cross-sectional studies, the case 2A intra-class correlation between reviewers was good (0.81; 95% CI = 0.49–0.93). This value indicates excellent reliability. Risk-of-bias overall rating ranged from 5 to 7 (mean = 6.00; SD = 0.80). In all studies, the weaknesses were observed for the item number 6 (statement of strategies to deal with confounding factors). Risk-of-bias ratings of the included qualitative studies are reported in Supplementary Table 3.
Regarding the three cohort studies, the case 2A intra-class correlation between reviewers was 1 (absolute agreement). The weaknesses observed in all studies were for the domain numbers 5b (consideration of confounding factors in design and/or analysis), 6a (follow-up complete), 6b (follow-up long enough), and 7 (strong exposure and outcome relation). Risk-of-bias ratings of the included qualitative studies are reported in Supplementary Table 4.
Finally, regarding the four quasi-experimental studies, the case 2A intra-class correlation between reviewers was 1 (absolute agreement). Risk-of-bias overall rating ranged from 3 to 8 (mean = 6.00; SD = 2.20). In all studies, we observed weaknesses for the domain number 3 (participants included in any comparisons received similar treatment/care, exposure/intervention). Risk-of-bias ratings of the included qualitative studies are reported in Supplementary Table 5.
Description of the studies
First author, study’s year, country where was conducted the study, study’s design, description and sample size of the intervention group, description and sample size of the control group(s), age in years of the population (mean, SD, and range), percentage of females, name of the intervention, instrument used to measure the outcomes, length of the follow-up (if present), length of the budget, and item purchased are displayed in Table 1. Table 2 shows the findings’ summary of the included studies.
We found that 18 studies declared no conflict of interests, while 11 did not provide this information. Eleven studies were conducted in the United Kingdom, 11 in the United States, 6 in Italy, and 1 in Australia. Four quasi-experimental studies were found (26–29). Nine studies reported follow-up data (27, 30–37). A total of 11,541 people participated in the 29 selected studies (range = 9; (38) – 6,908; (26); in studies conducted by the same authors, the participants may overlap). The mean ages of samples ranged from 26.08 (33, 34) to 58.7 (30) years. The proportion of females ranged from 26% (33) to 87% (39). Studies evaluated PB (n = 9), personal health budgets (n = 4), health budget (n = 1), individual budget (n = 1), self-directed care (n = 3), individual health budget (n = 2), patient-centered medical home (PCMH) (n = 1), person-centered planning (n = 1), Mental Health Access to Recovery or MHATR (n = 1), personalization of the care (n = 1), Cash and Counseling-based self-directed services program (n = 1), behavioral health home intervention arm (n = 1), shared management (n = 1), person-centered and self-directed (SPS) service (n = 1), and supported housing (n = 1), as defined by the authors, to define PB, which exist different acronyms (e.g., PB, PHB, and HB). We maintained definitions and acronyms used in each original work.
Eight studies [only two with quantitative data, (30, 31)] contained validated measures (e.g., Health of the Nation Outcome Scales, Brief Psychiatric Rating Scale, Global Assessment of Functioning, and World Health Organization’s International Classification of Functioning, Disability, and Health).
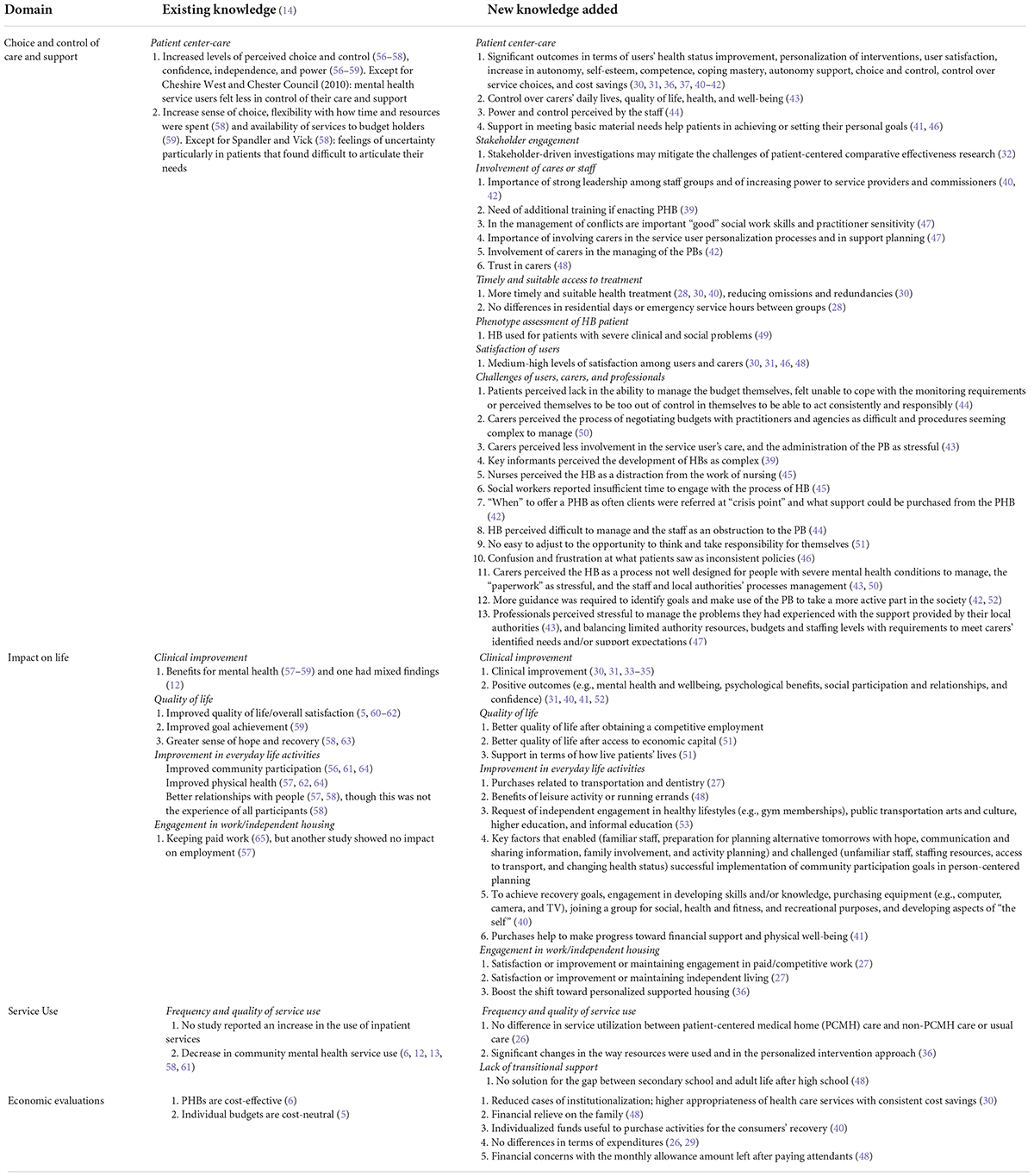
We maintained the domains’ classification given by Webber et al. (14) (i.e., choice and control of care and support; impact on life; service use; economic evaluations) and, for clarity seek, four authors classified the studies based on further subdomains (for choice and control of care and support: patient center-care, stakeholder engagement, involvement of carers or staff, timely and suitable access to treatment, phenotype assessment of HB patient, satisfaction of users, challenges of users, carers, and professionals; for impact on life: clinical improvement, quality of life, improvement in everyday life activities, engagement in work/independent housing, and frequency and quality of service use; for service use: frequency and quality of service use and lack of transitional support).
Choice and control of care and support
Patient center-care
The involvement of patients in the process of managing their care led to significant outcomes in terms of health status improvement, personalization of interventions, user satisfaction, increase in autonomy, self-esteem, competence, coping mastery, autonomy support, choice and control, control over service choices, and cost savings (30, 31, 36, 37, 40–42). Also, personalization can have positive outcomes for carers regarding their control over their daily lives, quality of life, health, and wellbeing (43). Hamilton et al. (44) showed that the staff also perceived users’ power and control. Most of the practitioners interviewed by Hamilton et al. (45) felt that they had already worked in patient-centered ways. However, most of all reported being more affiliated with the dominant medical model than the person-centered model. The Croft and Parish (46) and Spaulding-Givens et al. (41) studies provided insights for helping patients achieve or set their personal goals through the support in meeting their basic material needs.
Stakeholder engagement
Kogan et al. (32) affirmed that stakeholder-driven investigations might mitigate patient-centered comparative effectiveness research challenges.
Involvement of carers or staff
Peterson et al. (40) and Welch et al. (42) highlighted the importance of strong leadership among staff groups and the possibility of increasing power to service providers and commissioners. In the Norrie et al. (39), 64% of personal assistants saw their current roles as congruent with PHBs, were willing to engage with PHBs and undertake health-related tasks. At the same time, 74% of personal assistants perceived the need for additional training if enacting PHB (39). The staff interviewed by Mitchell et al. (47) reported that conflicts on service users’ abilities and support needs between staff and service users and carers were most likely to arise during assessment and support planning of the PB. In the management of conflicts were considered important “good” social work skills and practitioner sensitivity (47).
Mitchell et al. (47) showed that all practitioners’ focus groups reported that their authorities recognized the importance of involving carers in the service user personalization processes and support planning. Moreover, a good support plan for service users was perceived as having indirect benefits for carers. Carers were reported to be often involved in the managing of the PBs (42). Finally, Harry et al. (48) showed that all participants trusted their caregiver(s).
Timely and suitable access to treatment
Patients with severe and persistent mental disorders that benefit of the person-centered services had timely allocation of funds (40), suitable health treatment (30), and greater increases in outpatient and rehabilitation services compared to the non-self-directing group, in terms of hours of rehabilitation services (28). Indeed, compared with ordinary mental health treatments, the patients’ empowerment aimed at enhancing the individual’s independence and ability to self-manage the process of care contributed to the reduction of redundancies and omissions, producing higher treatment efficiency who, in turn, were likely to express fewer health needs (30).
Phenotype assessment of HB patient
Fontecedro et al. (49) analyzed the use of the individual HB in patients with severe clinical and social problems. They were also at higher risk than controls of aggressive or agitated behaviors, hallucinations and delusions, impairment in everyday life activities, and hospitalization.
Satisfaction of users
Most of the studies found medium–high levels of satisfaction with the HB programs among users and carers (30, 31, 46, 48). For example, Croft and Parish (46) reported that the interviewed perceived value in maintaining therapeutic relationships with providers over time and benefitted from providers’ availability. Welch et al. (42) reported that the PHB holders perceived improved in relationships between budget holders and their care staff as an opportunity given by the HB program. Furthermore, Larkin (43) interviewed carers who perceived enhancement of the carer–service user relationship, felt happier and healthier, and had more control over their lives.
Challenges of users, carers, and professionals
Hamilton et al. (44) showed that some service users felt unsatisfied with HB because they believed that they could not manage the budget themselves, felt unable to cope with the monitoring requirements, or perceived themselves to be too out of control in themselves to act consistently responsibly.
Also, carers found the process of negotiating budgets with practitioners and agencies to be difficult and procedures seeming complex to manage (50), less involvement in the service user’s care, and perceived the administration of the PB as stressful (43). Also, key informants perceived the development of HBs as complex (39).
Some mental health nurses interviewed by Hamilton et al. (45) reported that the PB was perceived as a distraction from nursing work. Other nurses argued that specific skills that characterized their profession were being side-lined to engage in implementing PBs. Several social workers reported the perception of insufficient time to engage with the process of PB, perceiving it as bureaucratic, complicated, and time-consuming. However, social workers identified the voluntary or third sector as a potential resource for PB (45). The frontline staff interviewed by Welch et al. (42) perceived a challenge “when” to offer a PHB as often clients were referred at “crisis point” and what support could be purchased from the PHB.
Several studies found that HB may be stressful for users, carers, and professionals. For example, the PHB was perceived by users as difficult to manage and the staff as an obstruction to the PB (44). Other participants did not find it easy to adjust to the opportunity to think and take responsibility for themselves (51) and expressed confusion and frustration at what they saw as inconsistent policies, particularly for purchases that address basic needs like rent, transportation, and household goods (46).
Carers perceived the HB as a process not well designed for people with severe mental health conditions to manage, the “paperwork” as stressful, and the staff and local authorities’ processes management (43, 50). Larsen et al. (52) and Welch et al. (42) showed that more guidance was required to identify goals and use the PB to take a more active part in society.
Professionals perceived particularly stressful to manage the problems they had experienced with the support provided by their local authorities (43), and balancing limited authority resources, budgets, and staffing levels with requirements to meet carers’ identified needs and/or support expectations (47).
Impact on life
Clinical improvement
Most of the studies reported clinical improvement in patients involved in HB programs. Adinolfi et al. (30) reported improvement in patients with problems related to alcohol and/or drug addiction, cognitive, physical, or disability problems; problems associated with hallucinations and delusions, with depressed mood; mental and behavioral problems; and problems with relationships, with activities of daily living, with living conditions, and with occupation and activities. In addition, the (34, 35) showed improvement in patients using PHB along 2-year follow-up using validated tools (i.e., Health of Nation Outcome Scales—HoNOS), Brief Psychiatric Rating Scale—BPRS, and Global Assessment of Functioning—GAF). Most participants from Larsen et al. (52) and Peterson et al. (40) studies identified positive outcomes (e.g., mental health and wellbeing, psychological benefits, social participation and relationships, and confidence) from using personal-centered services. Leuci et al. (33) showed that patients enrolled in the PHB intervention, at the end of the 2-year follow-up, reported higher improvements in negative symptoms, disorganization, and activation dimension (including manic features and hyperactivity) and in HoNOS “Impairment” subscale. In addition, in the period between T1 and T2, patients enrolled in the PHB showed a further significant decrease in positive symptoms, activation and affective dimension (including depressive characteristics, suicidality, and anxiety), improvements in functioning, and in HoNOS “Impairment,” “Psychiatric Symptoms,” and “Behavioural Problems” subscales. Finally, Cook et al. (31) showed that the intervention users had significantly lower somatic symptom severity over time compared to the control group.
Quality of life
Several participants from the Tew et al. (51) reported that access to economic capital enabled them to have a better quality of day-to-day life. Others saw their budget as a mechanism for organizing personal support in terms of how they were living their lives (51).
Improvement in everyday life activities
Several studies found improvement in the everyday life activities of patients involved in HB. For example, Croft et al. (27) showed that most purchases were related to transportation and dentistry. Nine representatives of the Harry et al. (48) study discussed the benefits of having a care attendant that could take young adults into the community, whether doing a leisure activity or running errands. Snethen et al. (53) participants requested items that facilitated independent engagement in healthy lifestyles (e.g., gym memberships) and public transportation. Fewer participants requested arts and culture, higher education, and informal education. Finally, the majority of Peterson et al. (40) study participants, to achieve recovery goals, engaged in developing skills and/or knowledge, purchasing equipment (e.g., computer, camera, and TV), joining a group for social, health and fitness, and recreational purposes, and developing aspects of “the self.” Participants of the Spaulding-Givens et al. (41) study felt their purchases help them to make progress toward financial support and physical wellbeing.
Engagement in work/independent housing
Two studies showed satisfaction or improvement or maintaining engagement in paid/competitive work (27) and independent living (27) during the HB programs. Ridente and Mezzina (36) showed that the individual HB method boosted the shift toward personalized supported housing for people with severe mental health conditions and complex problems.
Service use
Frequency and quality of service use
On the one hand, Bowdoin et al. (26) showed that service utilization did not differ between participants who received PCMH care and participants who received non-PCMH care or usual care. On the other hand, Ridente and Mezzina (36) showed that the use of HB method brought about significant changes is the way resources were used and in the personalized intervention approach within local Mental Health Department teams (transparency, clarity on spending decisions, and increased awareness of the importance of rational use of resources based on an adequate turnover of projects).
Lack of transitional support
Two interviewed by Harry et al. (48) reported that the Cash and Counseling-based self-directed services program was not used for bridging the gap between secondary school and adult life after high school (i.e., they stayed at home for one or 2 years after high school).
Economic evaluations
On the one hand, Adinolfi et al. (30) observed that HB often led to reducing institutionalization and brings to higher appropriateness of healthcare services with consistent cost savings, two interviewed by Harry et al. (48) reported financial relief on the family, and Peterson et al. (40) showed that individualized funds were useful to purchase activities for the consumers’ recovery.
On the other hand, Bowdoin et al. (26) found no differences in terms of expenditures (sum of direct payments for medical care) between participants who received PCMH care and participants who received non-PCMH care or usual care. Croft et al. (29) showed no differences in the total service costs before and after program participation. Five representatives interviewed by Harry et al. (48) described financial concerns with the monthly allowance amount left after paying attendants.
Discussion
The present systematic review has updated the existing literature since 2013 (14). More than 9,000 publications were screened. The scientific literature on PBs in the last 9 years is significantly increased (Table 3), and many valuable results have been achieved toward the definition of benefits and challenges of PBs for people with mental health conditions.
The studies have been conducted in the United Kingdom (n = 11), United States (n = 11), Italy (n = 6), and one in Australia. The majority of the studies have been conducted using qualitative methodologies (n = 20) based on not validated qualitative study-specific interviews. Only eight studies used validated tools to assess outcomes. One study did not specify the methodology used to assess the outcomes. In addition, the PBs’ outcomes were explored for the most in adult populations (n = 26). Many of the studies (n = 7) did not provide the age of the population interviewed. More than the 50% of females were enrolled in the majority of the studies’ samples (n = 20).
The studies included in the present systematic review show some limitations that make difficult in generalizing the results. First, the distribution of the countries among the included studies is only representative of the state of art in the western world. Also, comparison of PBs among countries is complicated because of the profoundly different characteristics of the healthcare system of reference. Future research should seek to depict the situation of the PB for people with mental health conditions in the rest of the world and describe in detail the characteristics of the healthcare system. Second, many studies included a small sample size, were mostly qualitative design, and did not use validated instruments to measure the outcomes, and the studies’ quality measured by the risk of bias was not always satisfactory. As Webber et al. (14) registered in their review, we also reported that most of the studies lacked justification for the research design and insufficient data analysis rigor. All qualitative studies lacked critical consideration of the researcher’s role, potential bias, and influence. All cross-sectional studies lacked the application of strategies to deal with potential confounding factors. Future cohort studies should seek to consider strategies to deal with confounding factors, strengthen the association between exposure and outcome, complete large time-span follow-ups, and recruit more homogenous experimental and control samples. More evidence-based research practice, longitudinal studies, and good quality studies using validated tools to assess the outcomes need to be conducted to explore in a more systematic manner the outcomes of the PBs. Third, the samples of the included studies were not representative of targeted population and lacked a full description of the phenotype of the participants with mental health conditions. For example, several studies did not describe the severity of the users’ symptoms, if users have intellectual disabilities, communication, or language problems. Finally, the payments used in the PB were often omitted. Those are fundamental aspects to consider when users are called to manage their PBs and should be carefully considered in future research. Also, future studies should seek to explore how and whether the personal PBs may be beneficial for target populations such as women, children, adolescents, elderly, and people with mental health conditions in comorbidity with intellectual disabilities. Fourth, as Webber et al. (14) observed in the studies older than 2013, interpretation is limited by the heterogeneity of the PB protocols: different payment, support, funding mechanisms, outcome measures, and context were described in each study. It urges to conduct large number of studies to be able to combine similar protocols for improving the outcomes’ interpretation.
Keeping into consideration these limitations, we can draw some general lessons. Positive outcomes for patients with mental health conditions utilizing PBs have been confirmed in terms of choice and control. The use of PB for people with mental health conditions showed several benefits in patient empowerment, stakeholder engagement, involvement of carers or staff in the PBs, and timely and suitable access to treatment. In general, several studies showed satisfaction for the PBs (30, 46, 48). Also, PBs improved users’ clinical outcomes, quality of life, and engagement in paid work and independent living. PBs brought to significant changes in the way resources were used and in the personalized intervention approaches (36, 40). PBs brought also to cost savings for the families (48) and the national health systems (30).
Concerns and challenges have been expressed on PBs in several studies. Users and carers perceived difficult and stressful the management and procedures of PBs (39, 43, 44, 46, 50, 51). Carers perceived difficulties in negotiating PBs with professionals (50) and felt less involvement in the care of their beloved ones (43). Professionals perceived the management of PBs as an additional burden in their work (43, 45, 47). Results on change in the frequency of the services’ use, efficacy of the services, and cost savings for the families or healthcare systems are inconsistent. On the one hand, some studies showed no differences in the frequency of service utilization, no solution for the gap in transition services (26, 48), no differences in terms of expenditures (26), and concerns with allowance (48). On the other hand, other studies showed that PBs led to cost savings for the healthcare system (30, 36) and the families (48). Studies that explore potential cost savings led by PBs should be increased in terms of quantity and quality.
The studies included in the present systematic review explored the outcomes of follow-ups longer than 2 years [except for one study Adinolfi et al. (30): 1 year], and two studies had follow-ups even longer [4, 8 years: (27); 10 years: (36)]. A positive aspect is that the recent studies we included in this work extended the time of the follow-ups compared to the studies in Webber et al. conducted before 2013 [follow-ups of 1 year or even less, (14)].
Conclusion
Individuals with mental health conditions and/or with ID have extremely heterogeneous interests and needs that mental health services could address whether users and carers would have the possibility to self-direct their care (53). Being in charge of their own care, being able to express and implement their choice and control in their process of care, and jointly sharing the process management with carers and professionals showed improvement in responsibility and awareness, quality of life, independent living, paid work, clinical, psychological and social domains, and everyday aspects of the users’ and their carers’ life. However, the present systematic review showed that several challenges and concerns arise from the application of PBs and highlight the need to make the management of PBs less stressful and burdensome for users, carers, and professionals.
Data availability statement
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
MS: conception. MS, MM, FF, LG, AC, EF, and GC: design of the work and interpretation of data. MM, FF, LG, AC, EF, and GC: data acquisition. MM, LG, EF, and GC: writing—original draft preparation. MS, MF, and GR: funding acquisition. All authors contributed to the writing—review and editing, and read and agreed to the published version of the manuscript.
Funding
This study has been supported by the Ministry of Health Projects—Directorate General of Health Prevention: Subject, person, citizen: promoting the wellbeing and social inclusion of people with mental disorders through the health budget (Grant Y4F) and “Definizione di criteri e modalità di utilizzo del fondo per la cura di soggetti con disturbo dello spettro autistico” (Grant # 5S13).
Acknowledgments
We thank Tommaso Salvitti for the statistical analysis and Daniele Di Tata for helping in the studies selection.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.974621/full#supplementary-material
Footnotes
References
1. World Health Organization. Regional office for the western pacific. People-centred health care: A policy framework. Manila: World Health Organization, Western Pacific Region (2007).
2. Department of Health. Transforming adult social care. Local authority circular. London: Crown Copyright (2008).
3. Glasby J, Littlechild R, Glasby J. Direct payments and personal budgets: Putting personalisation into practice. 2nd ed. Bristol: Policy Press (2009). p. 217
4. Gadsby EW. Personal budgets and health: A review of the evidence. Policy research unit in commissioning and the healthcare system. Canterbury: Centre for Health Services Studies, Kent (2013). p. 44
5. Glendinning C, Challis D, Fernández JL, Jacobs S, Jones K, Knapp M, et al. Evaluation of the individual budgets pilot programme. Summary report. York: University of York, Social Policy Research Unit (2008). p. 61
6. Forder J, Jones K, Glendinning C, Caiels J, Welch E, Baxter K, et al. Evaluation of the personal health budget pilot programme. Canterbury: University of Kent (2012).
7. Pavolini E, Ranci C. Restructuring the welfare state: Reforms in long-term care in Western European countries. J Eur Soc Policy. (2008) 18:246–59. doi: 10.1177/0958928708091058
9. Davey V, Fernández JL, Knapp M, Jolly D, Swift P, Tobin R, et al. Direct payments: A national survey of direct payments policy and practice. London: PSSRU (2007).
10. Riddell S, Pearson C, Jolly D, Barnes C, Priestley M, Mercer G. The development of direct payments in the UK: Implications for social justice. Soc Policy Soc. (2005) 4:75–85. doi: 10.1017/S1474746404002209
11. Alakeson V. The contribution of self-direction to improving the quality of mental health services. Washington, DC: U.S. Department of Health and Human Services (2007).
12. Davidson J, Baxter K, Glendinning C, Jones KC, Forder JE, Caiels J, et al. Personal health budgets: Experiences and outcomes for budget holders at nine months. Fifth interim report. Parassala: Department of Health (2012). p. 77
13. Cook JA, Russell C, Grey DD, Jonikas JA. Economic grand rounds: A self-directed care model for mental health recovery. Psychiatr Serv. (2008) 59:600–2. doi: 10.1176/ps.2008.59.6.600
14. Webber M, Treacy S, Carr S, Clark M, Parker G. The effectiveness of personal budgets for people with mental health problems: A systematic review. J Ment Health. (2014) 23:146–55. doi: 10.3109/09638237.2014.910642
15. Bhaumik S, Tyrer FC, McGrother C, Ganghadaran SK. Psychiatric service use and psychiatric disorders in adults with intellectual disability. J Intellect Disabil Res. (2008) 52:986–95. doi: 10.1111/j.1365-2788.2008.01124.x
16. Sheehan R, Hassiotis A, Walters K, Osborn D, Strydom A, Horsfall L. Mental illness, challenging behaviour, and psychotropic drug prescribing in people with intellectual disability: UK population based cohort study. BMJ. (2015) 351:h4326. doi: 10.1136/bmj.h4326
17. Buckles J. A systematic review of the prevalence of psychiatric disorders in adults with intellectual disability, 2003–2010. J Ment Health Res Intellect Disabil. (2013) 6:181–207. doi: 10.1080/19315864.2011.651682
18. Castelpietra G, Knudsen AKS, Agardh EE, Armocida B, Beghi M, Iburg KM, et al. The burden of mental disorders, substance use disorders and self-harm among young people in Europe, 1990–2019: Findings from the global burden of disease study 2019. Lancet Regional Health Europe. (2022) 16:100341. doi: 10.1016/j.lanepe.2022.100341
19. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
20. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. (2016) 5:1–10. doi: 10.1186/s13643-016-0384-4
21. Critical Appraisal Skills Programme. CASP cohort study checklist. (2018). Available online at: https://casp-uk.net/casp-tools-checklists/ (accessed January 7, 2021).
22. Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, et al. Chapter 7: Systematic reviews of etiology and risk. In: Aromataris E, Munn Z editors. Joanna briggs institute reviewer’s manual. (Adelaide, SU: The Joanna Briggs Institute) (2017).
23. Critical Appraisal Skills Programme. CASP qualitative study checklist. (2019). Available online at: https://casp-uk.net/casp-tools-checklists/ (accessed January 7, 2021).
24. Critical Appraisal Skills Programme. CASP randomised controlled trial standard checklist. (2019). Available online at: https://casp-uk.net/casp-tools-checklists/ (accessed January 7, 2021).
25. Tufanaru C, Munn Z, Aromataris E, Campbell J, Hopp L. Chapter 3: Systematic reviews of effectiveness. In: Aromataris E, Munn Z editors. Joanna briggs institute reviewer’s manual. (Adelaide, SA: The Joanna Briggs Institute) (2017).
26. Bowdoin JJ, Rodriguez-Monguio R, Puleo E, Keller D, Roche J. The patient-centered medical home model: Healthcare services utilization and cost for non-elderly adults with mental illness. J Ment Health. (2018) 27:574–82. doi: 10.1080/09638237.2017.1385744
27. Croft B, İsvan N, Parish SL, Mahoney KJ. Housing and employment outcomes for mental health self-direction participants. Psychiatr Serv. (2018) 69:819–25. doi: 10.1176/appi.ps.201700057
28. Croft B, Battis K, Isvan N, Mahoney KJ. Service utilization before and after self-direction: A quasi-experimental difference-in-differences analysis of Utah’s mental health access to recovery program. Adm Policy Ment Health. (2019) 47:36–46. doi: 10.1007/s10488-019-00969-4
29. Croft B, Battis K, Ostrow L, Salzer MS. Service costs and mental health self-direction: Findings from consumer recovery investment fund self-directed care. Psychiatr Rehabil J. (2019) 42:401–6. doi: 10.1037/prj0000374
30. Adinolfi P, Starace F, Palumbo R. Health outcomes and patient empowerment: The case of health budgets in Italy. J Healthc Manag. (2016) 18:117–33. doi: 10.1177/0972063415625524
31. Cook JA, Shore S, Burke-Miller JK, Jonikas JA, Hamilton M, Ruckdeschel B, et al. Mental health self-directed care financing: Efficacy in improving outcomes and controlling costs for adults with serious mental illness. Psychiatr Serv. (2019) 70:191–201. doi: 10.1176/appi.ps.201800337
32. Kogan JN, Schuster J, Nikolajski C, Schake P, Carney T, Morton SC, et al. Challenges encountered in the conduct of optimal health: A patient-centered comparative effectiveness study of interventions for adults with serious mental illness. Clin Trials. (2017) 14:5–16. doi: 10.1177/1740774516670895
33. Leuci E, Pelizza L, Landi G, Quattrone E, Maestri D, Azzali S, et al. Personal health budget in patients with first episode psychosis: A new rehabilitation model based on a community care system in Italy. Early Interv Psychiatry. (2021) 16:221–30. doi: 10.1111/eip.13145
34. Pelizza L, Leuci E, Landi G, Quattrone E, Azzali S, Pelosi A, et al. The “personal health budget” intervention model in early psychosis: Preliminary findings from the Parma experience. Psychopathology. (2020) 26:209–17. doi: 10.36148/2284-0249-359
35. Pelizza L, Leuci E, Landi G, Maestri D, Paulillo G, Ceroni P, et al. Personal health budget as a new rehabilitation model for severe mental illness within a caring community: An Italian evaluation study of beneficial effects. Aust N Z J Psychiatry. (2020) 55:602–12. doi: 10.1177/0004867420968918
36. Ridente P, Mezzina R. From residential facilities to supported housing: The personal health budget model as a form of coproduction. Int J Ment Health. (2016) 45:59–70. doi: 10.1080/00207411.2016.1146510
37. Thomas EC, Zisman-Ilani Y, Salzer MS. Self-determination and choice in mental health: Qualitative insights from a study of self-directed care. Psychiatr Serv. (2019) 70:801–7. doi: 10.1176/appi.ps.201800544
38. Williams V, Porter S. The meaning of ‘choice and control’for people with intellectual disabilities who are planning their social care and support. J Appl Res Intellect Disabil. (2017) 30:97–108. doi: 10.1111/jar.12222
39. Norrie C, Woolham J, Samsi K, Manthorpe J. Skill mix: The potential for personal assistants to undertake health-related tasks for people with personal health budgets. Health Soc Care Community (2020) 28:922–31. doi: 10.1111/hsc.12923
40. Peterson S, Buchanan A, Falkmer T. The impact of services that offer individualised funds, shared management, person-centred relationships, and self-direction on the lived experiences of consumers with mental illness. IJMHS. (2014) 8:1–14. doi: 10.1186/1752-4458-8-20
41. Spaulding-Givens J, Hughes S, Lacasse JR. Money matters: Participants’ purchasing experiences in a budget authority model of self-directed care. Soc Work Ment Health. (2019) 17:323–43. doi: 10.1080/15332985.2018.1555105
42. Welch E, Jones K, Caiels J, Windle K, Bass R. Implementing personal health budgets in England: A user-led approach to substance misuse. Health Soc Care Community. (2017) 25:1634–43. doi: 10.1111/hsc.12396
43. Larkin M. Developing the knowledge base about carers and personalisation: Contributions made by an exploration of carers’ perspectives on personal budgets and the carer–service user relationship. Health Soc Care Community. (2015) 23:33–41. doi: 10.1111/hsc.12131
44. Hamilton S, Tew J, Szymczynska P, Clewett N, Manthorpe J, Larsen J, et al. Power, choice and control: How do personal budgets affect the experiences of people with mental health problems and their relationships with social workers and other practitioners? Br J Soc Work. (2015) 46:719–36. doi: 10.1093/bjsw/bcv023
45. Hamilton S, Manthorpe J, Szymczynska P, Clewett N, Larsen J, Pinfold V, et al. Implementing personalisation in integrated mental health teams in England. J Interprof Care. (2015) 29:488–93. doi: 10.3109/13561820.2015.1035777
46. Croft B, Parish S. Participants’ assessment of the impact of behavioral health self-direction on recovery. Community Ment. (2016) 52:781–92. doi: 10.1007/s10597-016-9999-0
47. Mitchell W, Brooks J, Glendinning C. Carers’ roles in personal budgets: Tensions and dilemmas in front line practice. Br J Soc Work. (2015) 45:1433–50. doi: 10.1093/bjsw/bcu018
48. Harry ML, MacDonald L, McLuckie A, Battista C, Mahoney EK, Mahoney KJ. Long-term experiences in cash and counseling for young adults with intellectual disabilities: Familial programme representative descriptions. J Appl Res Intellect Disabil. (2017) 30:573–83. doi: 10.1111/jar.12251
49. Fontecedro E, Furlan M, Tossut D, Pascolo-Fabrici E, Balestrieri M, Salvador-Carulla L, et al. Individual health budgets in mental health: Results of its implementation in the Friuli Venezia Giulia region Italy. Int J Environ. (2020) 17:5017. doi: 10.3390/ijerph17145017
50. Hamilton S, Szymczynska P, Clewett N, Manthorpe J, Tew J, Larsen J, et al. The role of family carers in the use of personal budgets by people with mental health problems. Health Soc Care Community. (2015) 25:158–66. doi: 10.1111/hsc.12286
51. Tew J, Larsen J, Hamilton S, Manthorpe J, Clewett N, Pinfold V, et al. ‘And the stuff that I’m able to achieve now is really amazing’: The potential of personal budgets as a mechanism for supporting recovery in mental health. Br J Soc Work. (2015) 45:i79–97. doi: 10.1093/bjsw/bcv097
52. Larsen J, Tew J, Hamilton S, Manthorpe J, Pinfold V, Szymczynska P, et al. Outcomes from personal budgets in mental health: Service users’ experiences in three English local authorities. J Ment Health. (2015) 24:219–24. doi: 10.3109/09638237.2015.1036971
53. Snethen G, Bilger A, Maula EC, Salzer MS. Exploring personal medicine as part of self-directed care: Expanding perspectives on medical necessity. Psychiatr Serv. (2016) 67:883–9. doi: 10.1176/appi.ps.201500311
54. Hitchen S, Williamson GR, Watkins M. Personal budgets for all? Implementing self-directed support in mental health services. Action Res. (2015) 13:372–91. doi: 10.1177/1476750314568207
55. Veltro F, Morosini P, Gigantesco A, Casacchia M, Roncone R, Dell’Acqua G, et al. A new self-report questionnaire called” ABC” to evaluate in a clinical practice the aid perceived from services by relatives, needs and family burden of severe mental illness. Clin Pract Epidemiol Ment Health. (2007) 3:1–6. doi: 10.1186/1745-0179-3-15
56. Eost-Telling C. stockport self directed support pilot in mental health: Final Report of the evaluation of the self directed support pilot. Chester: University of Chester (2010).
57. Hatton C, Waters J. The national personal budget survey. Lancaster, PA: Lancaster University (2011).
58. Spandler H, Vick N. Direct payments, independent living and mental health: An evaluation. London: Health and Social Care Advisory Service (2004).
59. Teague GB, Boaz TL. Evaluation of the adult mental health self-directed care project. Tallahassee, FL: Florida Department of Children and Families (2003).
60. Homer T, Gilder P. A review of self-directed support in Scotland. Edinburgh: Scottish Government Social Research (2008).
61. Rogers L. Self directed support for mental health service users in west Sussex. West Sussex: West Sussex County Council (2009).
62. Shen C, Smyer M, Mahoney KJ, Simon-Rusinowitz L, Shinogle J, Norstrand J, et al. Consumer-directed care for beneficiaries with mental illness: Lessons from New Jersey’s Cash and counseling program. Psychiatr Serv. (2008) 59:1299–306. doi: 10.1176/ps.2008.59.11.1299
63. Coyle D. Recovery budgets in a mental health service: Evaluating recovery budgets for people accessing an early intervention service and the impact of working with self directed services on the team members within a North west of England NHS trust. Chester: University of Chester (2009).
64. Lawson S, Pearmain G, Waters J. Finding our way: The story of self-directed support in Barnsley. West Midlands: In control (2010).
Keywords: personal health budget, individual health budget, personalized care, health and social care policy and practice, mental disorder, intellectual disabilities
Citation: Micai M, Gila L, Caruso A, Fulceri F, Fontecedro E, Castelpietra G, Romano G, Ferri M and Scattoni ML (2022) Benefits and challenges of a personal budget for people with mental health conditions or intellectual disability: A systematic review. Front. Psychiatry 13:974621. doi: 10.3389/fpsyt.2022.974621
Received: 21 June 2022; Accepted: 14 July 2022;
Published: 04 August 2022.
Edited by:
Julian Schwarz, Brandenburg Medical School Theodor Fontane, GermanyCopyright © 2022 Micai, Gila, Caruso, Fulceri, Fontecedro, Castelpietra, Romano, Ferri and Scattoni. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maria Luisa Scattoni, bWFyaWFsdWlzYS5zY2F0dG9uaUBpc3MuaXQ=
†These authors share first authorship
 Martina Micai
Martina Micai Letizia Gila
Letizia Gila Angela Caruso
Angela Caruso Francesca Fulceri
Francesca Fulceri Elisa Fontecedro2
Elisa Fontecedro2 Giulio Castelpietra
Giulio Castelpietra Mila Ferri
Mila Ferri Maria Luisa Scattoni
Maria Luisa Scattoni