
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Psychiatry, 15 September 2022
Sec. Psychological Therapy and Psychosomatics
Volume 13 - 2022 | https://doi.org/10.3389/fpsyt.2022.973838
Objective: To systematically evaluate the effectiveness of exposure and response prevention (ERP) combined with medication on obsessive-compulsive disorder (OCD).
Methods: PubMed, Web of Science, EBSCO, Cochrane, Embase, and Science Direct databases were searched to include randomized controlled trials of ERP combined with medication for OCD that met the criteria. The Yale Brown Obsessive Compulsive Scale was used as the primary outcome indicator, and Depression scales were used as secondary outcome indicators. An evaluation of bias risk was conducted to identify possible sources of bias based on methodological and clinical factors. Review Manager 5.3 and Stata 16.0 software was used to perform meta-analysis of the extracted data.
Results: A total of 21 studies with 1113 patients were included. Meta-analysis showed that ERP combined with medication therapy was significantly better than medication therapy alone including selective serotonin reuptake inhibitors, clomipramine and risperidone (MD = –6.60, 95% CI: –8.35 to –4.84, P < 0.00001), but D-cycloserine (DCS) drugs do not enhance the effect of ERP intervention in patients with OCD (MD = 0.15, 95% CI: –0.87 to 1.17, P = 0.77). There is more significant maintenance by combined treatment method of medication plus ERP than medication treatment alone during the follow-up period (MD = –7.14, 95% CI: –9.17 to –5.10, P < 0.00001). DCS drugs did not enhance the effect of ERP intervention on depression in patients with OCD (SMD = –0.08, 95% CI: –0.31 to 0.15, P = 0.50). ERP combined with drug improved patients’ depression levels significantly better than providing drug alone (SMD = –0.40, 95% CI: –0.68 to –0.11, P = 0.006).
Conclusion: Patients with OCD have significant improvement in symptoms of obsessive-compulsive disorder and depression when ERP is combined with medication, however, not enough to prove that DCS can enhance ERP effectiveness.
Obsessive-compulsive disorder (OCD) is a psychological disorder characterized by recurrent intrusive thoughts and repetitive behaviors, which is frequently accompanied by anxiety or depression and has a lifetime prevalence of 2–4% (1). OCD is commonly detected at a late stage, and the longer untreated obsessive-compulsive symptoms persist, the less effective treatment and relapse prevention become (2). Therefore, finding an effective treatment and receiving appropriate treatment in a timely manner is crucial for OCD patients. Selective serotonin reuptake inhibitors (SSRIs) including fluoxetine, paroxetine, sertraline, and fluvoxamine are the first-line pharmacological treatments for OCD (3). However, only 40–60% of patients treated with SSRIs experienced a reduction in their obsessive-compulsive symptoms (4). Although tricyclic drugs (e.g., Chlorpromazine, Clomipramine, etc.) have better efficacy than SSRIs, their side effects are more pronounced and less endurable (5). Exposure and response prevention (ERP) is the first-line psychotherapy for OCD, and research indicates ERP-based therapy has comparable efficacy to SSRIs (4). Notwithstanding, the efficacy of ERP for OCD is highly variable, with approximately 25% of patients dropping out, 60% of patients recovering, and 25% of patients being successfully treated and cured (6).
In the clinical treatment of OCD, choosing medication or psychotherapy based on time and financial costs is a decision that patients need to consider. In order to achieve the best treatment outcome, it is more effective to combine psychotherapy and medication. For patients with mild or moderate symptoms, cognitive behavioral therapy (CBT) including ERP or SSRIs can be used alone, whereas CBT combined with SSRIs is recommended for patients with more severe or resistant conditions (7, 8). CBT combined with medication has shown better interventions in the clinical treatment of OCD, with all combined effect sizes at moderate to high levels (9). However, it has also been found that the efficacy achieved with the combination of sertraline and CBT was not sustained long-term, and that at 52 weeks, sertraline monotherapy was the most effective and cost-effective treatment (10). D-cycloserine (DCS) is a partial N-methyl-D-aspartic acid agonist that was initially utilized to treat tuberculosis (11). Researchers began to wonder whether DCS enhances exposure-based CBT based on the positive effects observed in animal studies investigating the fear-elimination paradigm. However, results were mixed (11). It is unclear whether DCS, as a novel clinical trial drug, will enhance the effectiveness of ERP treatment for patients with OCD.
Current studies have examined CBT combination pharmacotherapy for OCD (4, 12, 13). However, these studies have actually evaluated the effects of mixed forms of CBT, including cognitive therapy, behavioral therapy, and the combination of ERP and cognitive therapy. The study by Ost et al. (13) included 7 cognitive treatments with no components of ERP and 13 combinations of cognitive therapy and ERP. Nevertheless, ERP and cognitive therapy are essentially different theoretical underpinnings (7). Some variants of ERP include informal cognitive techniques (for instance, cognitive restructuring during exposures) and some forms of cognitive therapy include informal exposures (e.g., behavioral experiments that test the validity of the patient’s obsessional beliefs), blurring the distinction between these treatments (14). Cognitive therapy focuses on correcting dysfunctional beliefs about the existence or significance of intrusive thoughts, and its behavioral experiments were used to identify and modify patients’ irrational beliefs, rather than repeatedly confronting anxiety-provoking situations, as in ERP (15). As previous Meta-analyses have primarily focused on any form of CBT combination therapy rather than specifically ERP, their final effect sizes may be attributable to therapy overlaps. Moreover, major depressive disorder is the most common comorbid diagnosis of OCD (16). In this study, a Meta-analysis was therefore conducted on the intervention effects of ERP combined with pharmacological treatment on obsessive-compulsive and depressive symptoms in patients with OCD, providing a foundation for future clinical application.
PubMed, Web of Science, EBSCO, Cochrane, Embase, and Science Direct were searched from build to May 1, 2022. The search term 1 was (exposure response prevention OR exposure and ritual prevention OR ERP OR EXRP) AND (obsessive-compulsive disorder OR obsessive compulsive disorder OR OCD). Search term 2 was (exposure OR ERP OR EXRP) AND (obsessive-compulsive disorder OR obsessive compulsive disorder OR OCD) AND (Randomized OR RCT OR RCTs OR random).
Inclusion, screening, and exclusion criteria for the articles were developed in accordance with the PRISMA statement and PICOS principles. Inclusion criteria: (i) Study design (S): randomized controlled trials (RCT) (ii) Study Population (P): studies involving patients with comorbid disorders were considered as long as the primary diagnosis of OCD was present. (iii) Interventions (I): the experimental group received ERP combined with pharmacological intervention. (iv) Comparison (C): the control group received ERP or pharmacological intervention alone. (v) Outcome indicators (O): The Yale Brown Obsessive Compulsive Scale (Y-BOCS) score was used as the primary outcome indicator, and the secondary outcome indicators included Depression scales.
Exclusion criteria: (i) duplicate publications, (ii) not empirical research, (iii) not ERP interventions, (iv) no control groups, (v) not OCD, (vi) review article, (vii) conference abstract, (viii) not RCT, (ix) missing data, (x) not ERP combined with pharmacological intervention, (xi) not Y-BOCS, and (xii) reused data.
The risk of bias evaluation of final included studies was conducted by two psychology master students according to the Cochrane Handbook version 5.0.1. The assessment included following 7 aspects: (i) random sequence generation; (ii) allocation protocol concealment; (iii) blinding of participants and trial personnel; (iv) blinding of outcome assessment; (v) completeness of outcome data; (vi) selective reporting of results; (vii) other biases. The evaluators judged the above 7 aspects as “low bias,” “high bias,” and “unclear,” respectively, and asked a third psychology master student to discuss the evaluation when there was a dispute.
Data were extracted from the final included articles, mainly including (i) the first author, year of publication, and nationality of the articles, (ii) the sample size, gender, and age of the experimental and control groups, (iii) the interventions, intervention duration and follow-up time of the experimental and control groups, and (iv) Mean (M) and Standard Deviations (SD) used for the outcome indicators.
Review Manager 5.3 and Stata 16.0 software was used to conduct Meta-analysis on the extracted data. Firstly, the size of heterogeneity among the studies was judged. In Meta-analysis, the fixed-effects model assumes that the studies are homogeneous, while the random-effects model assumes heterogeneity between studies (17). I2-statistic reflects the proportion of the heterogeneity component in the total variance of the effect size, and I2-statistic > 50% indicates relatively substantial heterogeneity (18). If P ≥ 0.1 and I2-statistic < 50%, the fixed-effect model was used; if P < 0.1 and I2-statistic ≥ 50%, the random-effect model was used; when the heterogeneity was more obvious, Sensitivity analysis, Meta-regression analyses and Subgroup analysis was conducted to explore the source of heterogeneity. Statistical analyses were performed using Mean Different (MD) if the outcome indicators were measured with the same instrument, and Standardized Mean Different (SMD) if the measurement instruments were different. The outcome indicators were statistically analyzed using 95% Confidence Interval (95% CI) and P < 0.05 indicates that the difference is statistically significant.
The search yielded 4,697 relevant articles, and 21 RCT studies were finally included after duplication, reading of titles and abstracts, and further reading of the full text to eliminate articles that did not meet the inclusion criteria. The article inclusion process and results are shown in Figure 1.
The included articles were all RCT studies, and there were no significant differences between experimental groups and control groups at baseline. Nineteen studies reported the reasons and numbers of participants who dropped out, and 15 studies were blinded to outcome assessment. Due to the specificity of psychotherapy, a double-blind design was not possible, and the risk of performance bias was high in all studies. Nine studies described the method of random sequence generation, and 7 of them mentioned allocation concealment. Other risks of bias were unclear. The risk of bias report is summarized in Figure 2, “+” means “low bias,” “-” means “high bias,” and “?” means “unclear.”
The 21 articles included in this study all centered on ERP combined with medication intervention, with 7 studies in children and adolescents and 13 studies in adults. For the control group interventions, nine were pharmacological and twelve were ERP interventions under placebo conditions. Twelve studies reported follow-up data for primary outcome indicators ranging from 1 to 12 months. In addition, 10 studies reported no significant difference between mixed intervention and psychological intervention, 2 studies reported mixed intervention was better than psychological intervention. Six studies reported mixed intervention was better than medication, and 2 studies reported no difference. Basic characteristics of the included studies are shown in Table 1.
A total of 1,113 participants were included in the 21 studies that measured the effectiveness of ERP combined with pharmacotherapy on obsessive-compulsive symptoms as post-treatment data. As shown in Table 2, Meta-analysis showed that the heterogeneity I2-statistic was 86% (P < 0.00001), there were significant difference between the combination treatment group and the control group (MD = –3.18, 95% CI: –4.97 to –1.40, P = 0.0005).
Publication years, intervention measures, and sample ages were examined as potential moderators of effect size. Meta-regression analyses revealed no significant moderation by publication years (t = –1.09, P = 0.29) and sample ages (t = –0.84, P = 0.41). However, intervention measures significantly moderated effect size (t = –3.34, P = 0.004), indicating that the type of intervention measures was the source of variation.
For heterogeneity, the studies were classified into 2 subgroups according to the interventions in the control groups. ERP combined with DCS treatment was not significantly different from ERP treatment in the condition of taking placebo (MD = 0.15, 95% CI: –0.87 to 1.17, P = 0.77), indicating that DCS drugs do not enhance the effect of ERP intervention in patients with OCD. Given the relatively small number of included studies, it was not sufficient to demonstrate that SSRIs do not enhance the efficacy of ERP, although the difference between ERP combined with SSRIs and placebo was not significant (MD = –2.74, 95% CI: –6.37 to 0.89, P = 0.14). ERP combined with drug therapy was significantly better than drug therapy alone, including SSRIs, Clomipramine and Risperidone, with a statistically significant difference (MD = –6.60, 95% CI: –8.35 to –4.84, P < 0.00001), see Figure 3.
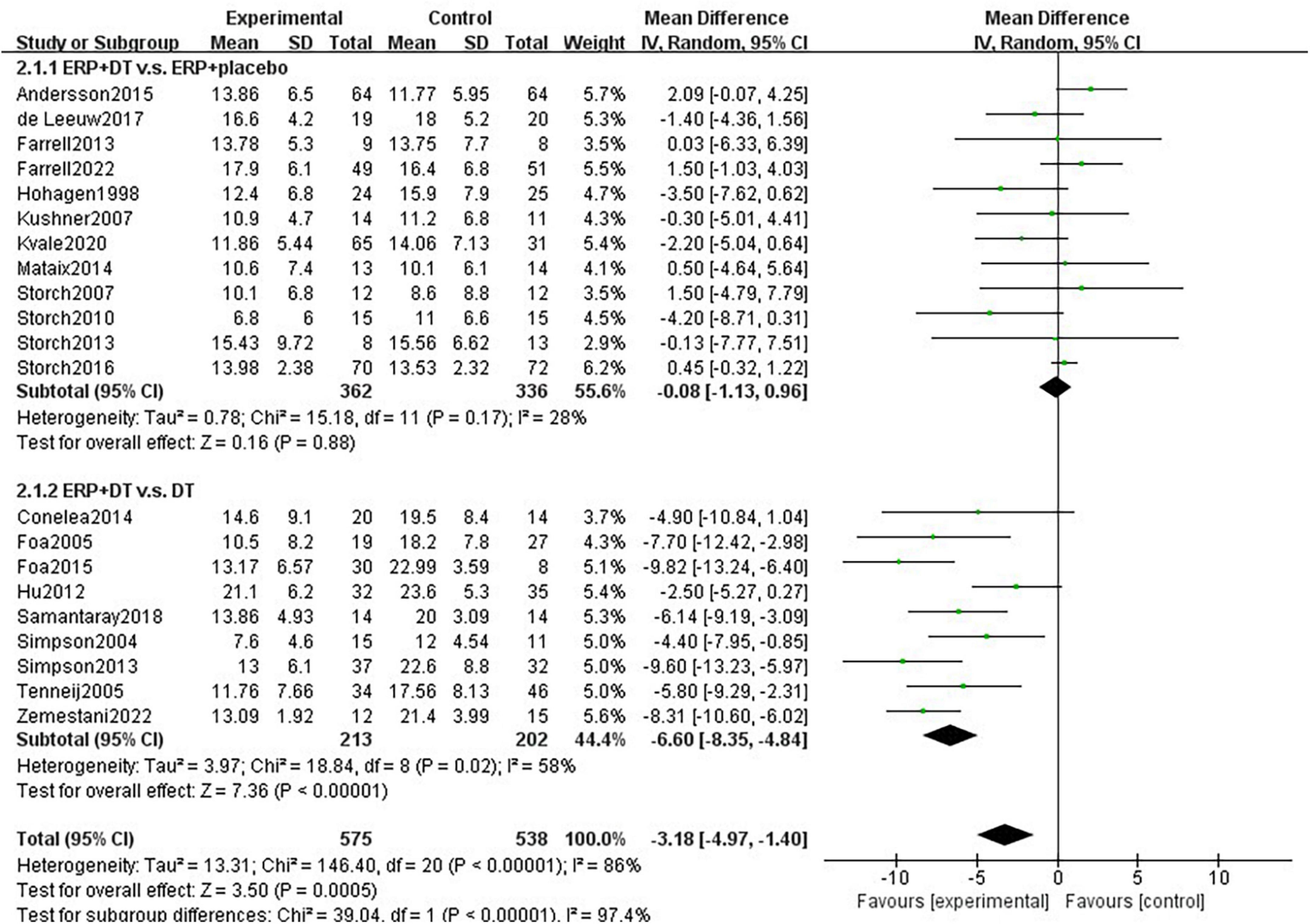
Figure 3. Subgroup analysis of drug type for the effect of combination therapy on the intervention of obsessive-compulsive symptoms in patients with OCD.
A meta-analysis of 12 studies reporting follow-up data on primary outcome indicators found a total of 588 subjects with I2-statistic 80% heterogeneity between studies (P < 0.00001). The combination treatment group had a greater effect than the control group with a statistically significant difference (MD = –3.17, 95% CI: –5.66 to –0.67, P = 0.01).
For heterogeneity, the studies were divided into two subgroups of DCS and drug treatment, according to the control group interventions. Subgroup analysis showed heterogeneity between studies in the DCS group with I2-statistic = 0% (P = 0.69). There was no significant difference in the long-term efficacy of providing ERP treatment alone versus combined DCS treatment in improving obsessive-compulsive symptoms (MD = –0.30, 95% CI: –1.79 to 1.18, P = 0.69). Heterogeneity between studies in the drug treatment group was I2-statistic = 43% (P = 0.14). There is more significant maintenance of treatment effects on the combined treatment than on drug treatment alone during the follow-up period (MD = –7.14, 95% CI: –9.17 to –5.10, P < 0.00001). There was heterogeneity between subgroups (I2-statistic = 96.5%, P < 0.00001), indicating that the type of control group was one of the sources of heterogeneity in this subgroup, see Figure 4.
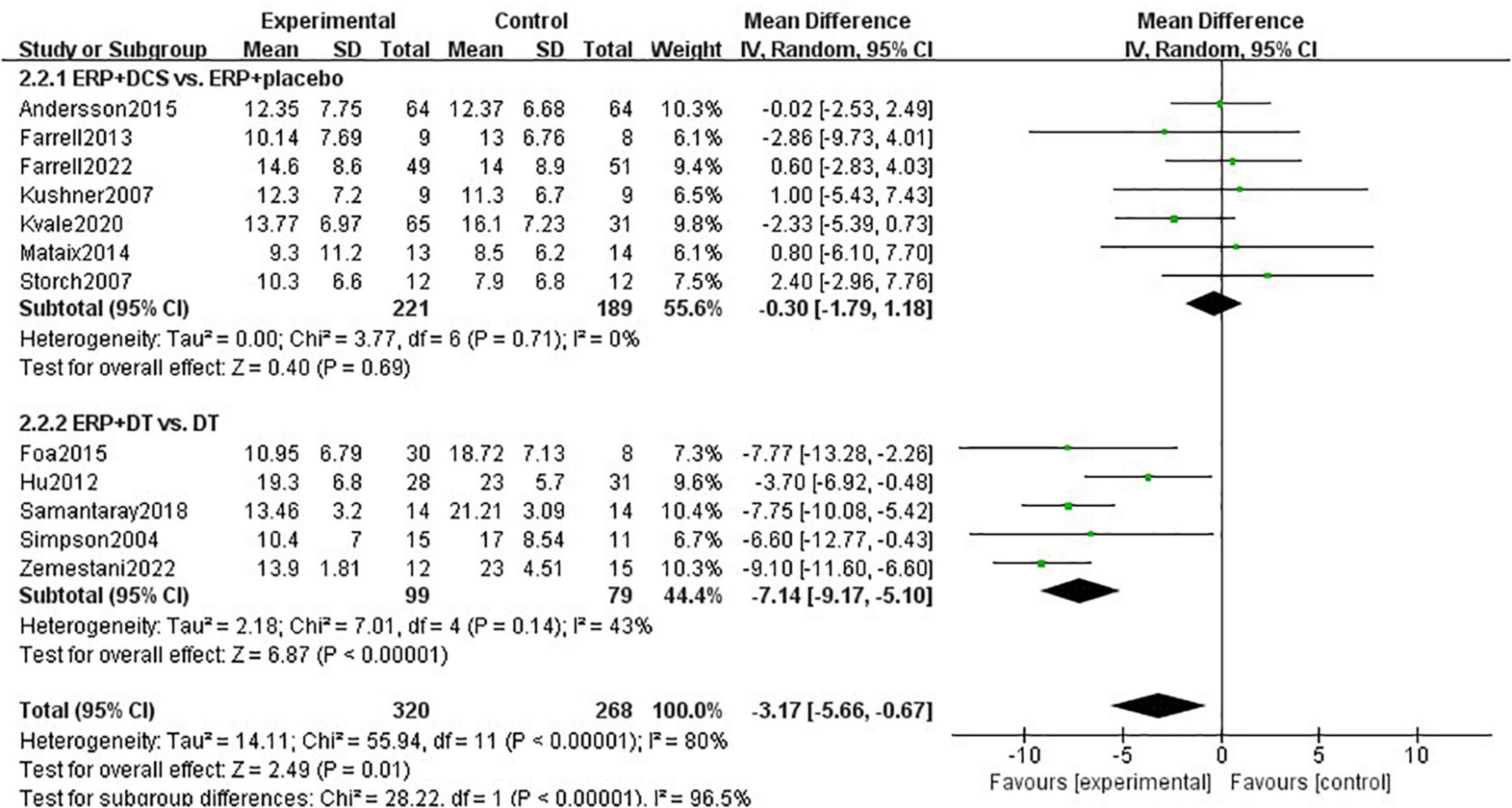
Figure 4. Subgroup analysis of the effect of combination therapy on the intervention of obsessive-compulsive symptoms in patients with OCD during the follow-up period.
12 studies with a total of 730 subjects were included, with heterogeneity I2-statistic = 86% (P < 0.00001). With regard to heterogeneity, sensitivity analysis found that I2-statistic decreased to 1% (P = 0.44) after excluding one study (37). The difference between the combination treatment group and the control group was significant (SMD = –0.21, 95% CI: –0.38 to –0.04, P = 0.02). The studies were divided into 2 subgroups of DCS and drug treatment, according to the control group interventions, and two unclassifiable studies were excluded. Subgroup analysis showed that the heterogeneity between studies in the DCS group was I2-statistic = 0% (P = 0.63). DCS drugs did not enhance the effect of ERP intervention on depression in patients with OCD (SMD = –0.08, 95% CI: –0.31 to 0.15, P = 0.50). Heterogeneity between studies in the drug treatment group was I2-statistic = 34% (P = 0.21). ERP combined with drugs improved patients’ depression levels significantly better than providing medication alone (SMD = –0.40, 95% CI: –0.68 to –0.11, P = 0.006), see Figure 5.
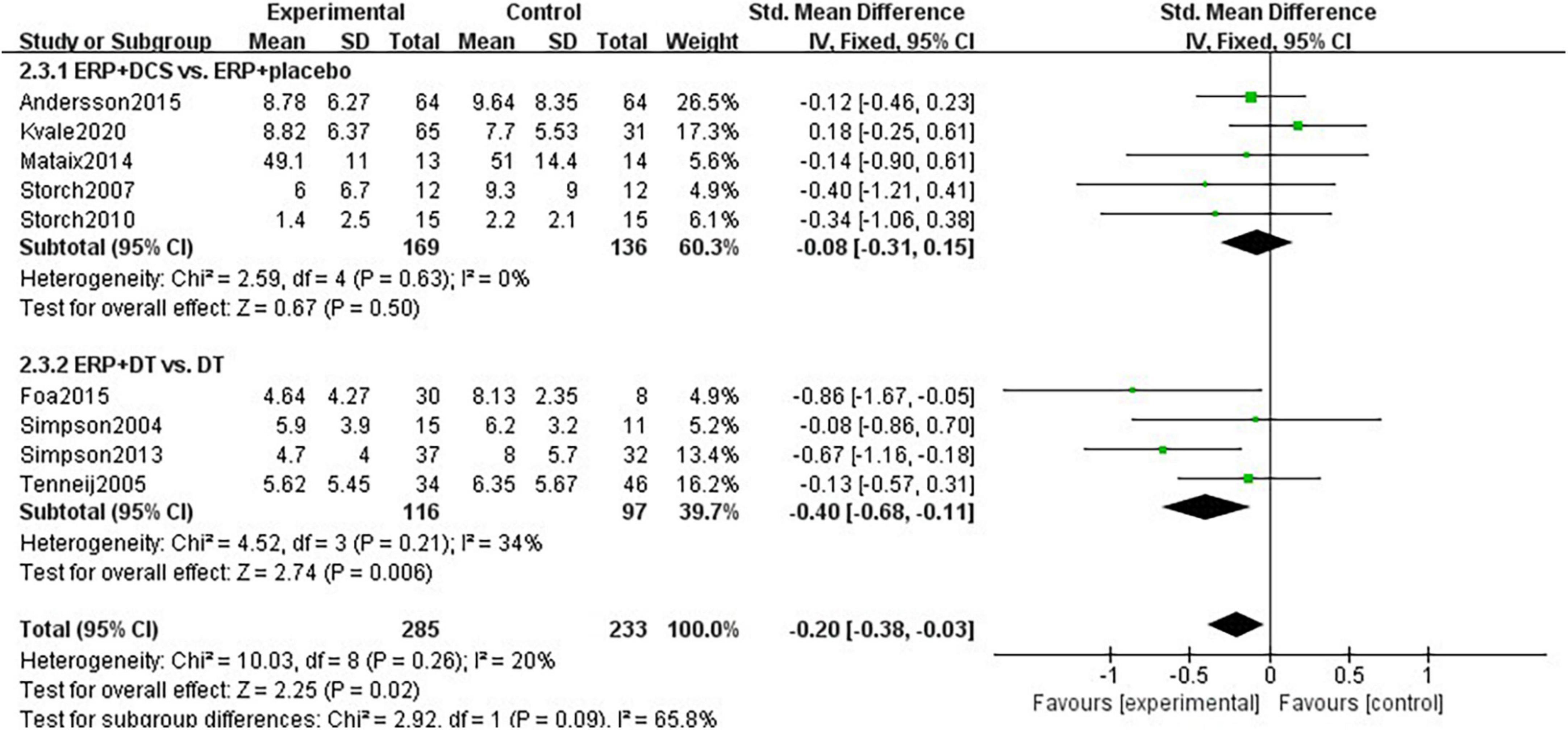
Figure 5. Subgroup analysis of the effect of combination therapy on depression intervention in patients with OCD.
The Egger test indicated that there was a possible publication bias (t = –2.52, 95% CI: –4.12 to –0.38, P = 0.02) for ERP combined with pharmacological interventions. With regard to the funnel plots, the left-right distribution of the plots was slightly asymmetrical, see Figure 6.
ERP emphasizes layered exposure to fear-inducing stimuli or situations based on patient relaxation, while blocking the patient’s ritualized behaviors and cutting off the reinforcing effects that maintain obsessive-compulsive symptoms, ultimately leading to a gradual fading of the conditioned association between symptoms and the triggering stimulus or situation. ERP treatment is more effective in patients with reduced basolateral amygdala-ventromedial prefrontal cortex functional connectivity in the resting state (40). The amygdala and prefrontal cortex are the underlying structures involved in fear conditioning and regression, and could predict outcomes from ERP. SSRIs are currently the most common drugs used internationally to treat OCD (3). The reduction of obsessive-compulsive symptoms in patients treated with SSRIs medications is associated with reduced metabolic levels in the right caudate nucleus, bilateral orbitofrontal cortex, and bilateral anterior cingulate cortex, and with increased activation in the left thalamus and right insula (41). Nevertheless, if SSRIs medication fails, prompt psychological interventions, such as CBT, behavioral therapy, and ERP, are all acceptable measures, and vice versa (42).
It has been suggested that some patients in studies using ERP-based CBT therapies entered the trial under the condition of continuing their antidepressants, whereas in fact they received the combined treatment (43). The result that CBT’s effect was greater than SSRIs and clomipramine may be attributed to the combined effect of the two treatment modalities (8). Subgroup analysis revealed that ERP combination medication was significantly more effective than providing SSRIs or clomipramine medication alone, with statistically significant changes in Y-BOCS scores before and after treatment, which is consistent with the findings of previous studies (24, 32, 39). In OCD patients with limited benefit from SSRI treatment, combined ERP treatment with risperidone was more beneficial, confirming the findings of prior studies focusing on individuals with refractory OCD (25, 33). Although it appears that a combination of pharmacological and psychological treatment is effective, there is no convincing evidence that ERP alone is more effective than combination treatment. A systematic review comparing behavioral and pharmacological therapies similarly stated that combination therapy had little benefit over behavioral therapy in an outpatient setting, but that it was at least superior to pharmacological therapy (12).
Regarding the long-lasting mechanism of treatment effects, one study reported no significant difference between drug and combination therapy groups (25), while others found that combination therapy was significantly better than drug therapy (31, 39). The results of Subgroup analysis revealed that the majority of OCD patients maintained modest efficacy during the follow-up period after ERP combination medication therapy. The follow-up duration included in this study was, however, relatively short, and some of the articles did not offer statistics on long-term treatment or relapse prevention. Since the majority of OCD patients are chronic, more follow-up statistics on long-term treatment are required to determine the duration of symptom improvement without relapse following combination therapy.
Hitherto, the results of clinical studies of DCS enhanced ERP for OCD have been inconsistent. Farrell et al. reported significant improvement in OCD symptoms with DCS enhanced ERP treatment compared to placebo (22). However, Subgroup analysis revealed that DCS does not have a mechanism for enhancing ERP efficacy and did not significantly differ from the placebo group, which is in line with prior findings (19, 21, 29). Nevertheless, it has been suggested that antidepressants may block the effect of DCS in promoting fear extinction, with a higher percentage of symptom improvement in the DCS group among patients not taking antidepressants, and DCS may be utilized as an intensive CBT treatment approach in patients with OCD who are not on antidepressants (19). The analysis revealed no significant difference in the reduction of Y-BOCS scores between the DCS enhanced and placebo enhanced ERP groups during the follow-up period, requiring further confirmation of the mechanism underlying the long-lasting effects of DCS enhanced ERP treatment. However, it has been argued that the augmentation impact of DCS is time-limited, and that the most significant benefits may be an earlier gain in ERP treatment effect, a reduction in the number of treatments required, lower treatment costs and dropout rates (44).
Due to the presence of compulsions and counter-compulsions, patients with OCD commonly suffer anxiety. Furthermore, for ERP treatment to be effective, it is a precondition that patient actively confronts the stimulus or situation (45), which may aggravate the patient’s anxiety during ERP treatment. Compulsion is associated with a large number of psychiatric comorbidities, with anxiety and mood disorders being more common (46). Therefore, patients with comorbidities were not excluded from this study, and several included papers reported co-morbid anxiety or depression in some patients (19, 21, 22, 30, 33–35, 39). The supramarginal gyrus is thought to be related to emotion processing, and its dysfunction may affect patients’ sensitivity to uncomfortable emotions or anxiety, as well as be responsible for exacerbating the co-morbidity of obsessive-compulsive and anxious emotions (47). A Meta-analysis found that neither ERPs nor SSRIs significantly reduced anxiety and depressive symptoms (48). In contrast, Meta-analysis revealed that ERP combined with pharmacotherapy significantly improved depressive symptoms in patients. Alleviating obsessive-compulsive symptoms can ameliorate depressive symptoms to a great extent (49). Approximately one-third of OCD patients currently have comorbid major depressive disorder and roughly two-thirds suffer from a lifetime comorbidity (16). When compulsions are accompanied by a depressive mood, it can interfere with the completion of homework assignments and the development of therapeutic habits during ERP treatment. Combining antidepressants and psychotherapy for OCD patients who have significant depressive symptoms may be more effective than monotherapy (50). In particular, for patients with severe obsessive-compulsive co-morbid depression who do not respond well to therapy alone, a combination of CBT involving ERP and SSRIs is frequently recommended (8).
Recent research evaluated the efficacy and tolerability of three commonly used atypical antipsychotics (risperidone, paliperidone, and aripiprazole) as reinforcing treatments for OCD, which are more likely to be used clinically as augmentation agents to treat patients when SSRIs and ERP have limited treatment effect (51). In addition, ketamine plays an important role in the cortico-striato-thalamo-cortical loop as a potent N-methyl-D-aspartic acid receptor antagonist and glutamatergic modulator. Given the limitations of current OCD treatment and the new evidence that glutamate may improve depression and play a role in OCD pathophysiology, ketamine has emerged as an alternative drug in this field (52).
Exposure to intrusive thoughts poses some risk, and high levels of emotional arousal and discomfort may account for the high ERP dropouts. In contrast to traditional therapies that attempt to eliminate distress directly, acceptance and commitment therapy (ACT) focuses on increasing psychological flexibility, comprehending anxiety, and altering how distress is dealt with. Patients treated with ACT and combination therapy showed more significant improvements in post-treatment obsessive-compulsive symptoms and experiential avoidance compared to those treated with SSRIs alone, according to an RCT (53). The small number of studies, however, does not support a more significant intervention impact of ACT combined with SSRIs. Future research could focus on applying ACT to various subtypes of OCD in order to further validate the effectiveness of ACT in conjunction with medication for OCD patients.
This study confirmed the feasibility of ERP combined with medication in improving obsessive-compulsive symptoms and depressive mood in patients with OCD, but was insufficient to demonstrate that DCS enhances the efficacy of ERP. The inclusion of data from 10 countries worldwide further enhances the generalizability of the results, but there are some limitations. First, the relatively low number of studies and sample sizes inevitably led to lower detection power. Secondly, children and adolescents were included in the analysis along with adult patients. Finally, some studies were excluded for data could not be extracted, which affected the analysis results to some extent. Future studies with larger sample sizes should be designed to validate the findings of this study.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
LM: manuscript writing, study search, data collection, and data analysis. MH: study search, data collection, and data analysis. LL, YW, ZL, and JZ: selected the studies, extracted the data, and assessed the risk of bias. All authors contributed to the article and approved the submitted version.
This study was financially supported by the National Natural Science Foundation of China (81960261).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Huang Y, Wang Y, Wang H. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry. (2019). 6:E11. doi: 10.1016/S2215-0366(19)30074-4
2. Fineberg NA, Dell’osso B, Albert U, Maina G, Geller D, Carmi L, et al. Early intervention for obsessive compulsive disorder: an expert consensus statement. Eur Neuropsychopharmacol. (2019) 29:549–65. doi: 10.1016/j.euroneuro.2019.02.002
3. Issari Y, Jakubovski E, Bartley CA, Pittenger C, Bloch MH. Early onset of response with selective serotonin reuptake inhibitors in obsessive-compulsive disorder: a meta-analysis. J Clin Psychiatry. (2016) 77:E605–11. doi: 10.4088/JCP.14r09758
4. Skapinakis P, Caldwell DM, Hollingworth W, Bryden P, Fineberg NA, Salkovskis P, et al. Pharmacological and psychotherapeutic interventions for management of obsessive-compulsive disorder in adults: a systematic review and network meta-analysis. Lancet Psychiatry. (2016) 3:730–9. doi: 10.1016/S2215-0366(16)30069-4
5. Sanchez-Meca J, Rosa-Alcazar AI, Iniesta-Sepulveda M, Rosa-Alcázar A. Differential efficacy of cognitive-behavioral therapy and pharmacological treatments for pediatric obsessive-compulsive disorder: a meta-analysis. J Anxiety Disord. (2014) 28:31–44. doi: 10.1016/j.janxdis.2013.10.007
6. Van Der Heiden C, Van Rossen K, Dekker A. Metacognitive therapy for obsessive compulsive disorder: a pilot study. J Obsessive Compuls Relat Disord. (2016) 9:24–9. doi: 10.1016/j.jocrd.2016.02.002
7. Reid JE, Laws KR, Drummond L, Vismara M, Grancini B, Mpavaenda D, et al. Cognitive behavioural therapy with exposure and response prevention in the treatment of obsessive-compulsive disorder: a systematic review and meta-analysis of randomised controlled trials. Compr Psychiatry. (2021) 106:152223. doi: 10.1016/j.comppsych.2021.152223
8. Fineberg NA, Hollander E, Pallanti S, Walitza S, Grünblatt E, Dell’Osso BM, et al. Clinical advances in obsessive-compulsive disorder: a position statement by the international college of obsessive-compulsive spectrum disorders. Int Clin Psychopharmacol. (2020) 35:173–93. doi: 10.1097/YIC.0000000000000314
9. Carpenter JK, Andrews LA, Witcraft SM, Powers MB, Smits JAJ, Hofmann SG, et al. Cognitive behavioral therapy for anxiety and related disorders: a meta-analysis of randomized placebo-controlled trials. Depress Anxiety. (2018) 35:502–14. doi: 10.1002/da.22728
10. Fineberg NA, Baldwin DS, Drummond LM, Wyatt S, Hanson J, Gopi S, et al. Optimal treatment for obsessive compulsive disorder: a randomized controlled feasibility study of the clinical-effectiveness and cost-effectiveness of cognitive-behavioural therapy, selective serotonin reuptake inhibitors and their combination in the management of obsessive compulsive disorder. Int Clin Psychopharmacol. (2018) 33:334–48. doi: 10.1097/YIC.0000000000000237
11. Gu W, Storch EA, Zhao Q, Xu T, Wang Z. Effects of D-cycloserine augmentation on cognitive behavioral therapy in patients with obsessive-compulsive disorder: a systematic review and meta-analysis. J Obsessive Compuls Relat Disord. (2017) 13:24–9. doi: 10.1016/j.jocrd.2017.03.001
12. Romanelli RJ, Wu FM, Gamba R, Mojtabai R, Segal JB. Behavioral therapy and serotonin reuptake inhibitor pharmacotherapy in the treatment of obsessive-compulsive disorder: a systematic review and meta-analysis of head-to-head randomized controlled trials. Depress Anxiety. (2014) 31:641–52. doi: 10.1002/da.22232
13. Ost L-G, Havnen A, Hansen B, Hansen B, Kvale G. Cognitive behavioral treatments of obsessive-compulsive disorder. A systematic review and meta-analysis of studies published 1993-2014. Clin Psychol Rev. (2015) 40:156–69. doi: 10.1016/j.cpr.2015.06.003
14. Koran LM, Hanna GL, Hollander E, Nestadt G, Simpson HB. Practice guideline for the treatment of patients with obsessive-compulsive disorder. Am J Psychiatry. (2007) 164(Suppl. 7):5–53.
15. Wilhelm S, Steketee G, Reilly-Harrington NA, Deckersbach T, Buhlmann U, Baer L, et al. Effectiveness of cognitive therapy for obsessive-compulsive disorder: an open trial. J Cogn Psychother. (2005) 19:173–9. doi: 10.1891/jcop.19.2.173.66792
16. Rickelt J, Viechtbauer W, Lieverse R, Overbeek T, van Balkom AJ, van Oppen P, et al. The relation between depressive and obsessive-compulsive symptoms in obsessive-compulsive disorder: results from a large, naturalistic follow-up study. J Affect Disord. (2016) 203:241–7. doi: 10.1016/j.jad.2016.06.009
17. Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. (2010) 1:97–111. doi: 10.1002/jrsm.12
18. Knoll T, Omar MI, Maclennan S, Hernández V, Canfield S, Yuan Y, et al. Key steps in conducting systematic reviews for underpinning clinical practice guidelines: methodology of the European association of urology. Eur Urol. (2018) 73:290–300. doi: 10.1016/j.eururo.2017.08.016
19. Andersson E, Hedman E, Enander J, Radu Djurfeldt D, Ljótsson B, Cervenka S, et al. D-Cycloserine vs placebo as adjunct to cognitive behavioral therapy for obsessive-compulsive disorder and interaction with antidepressants a randomized clinical trial. JAMA Psychiatry. (2015) 72:659–67. doi: 10.1001/jamapsychiatry.2015.0546
20. Conelea CA, Walther MR, Freeman JB, Garcia AM, Sapyta J, Khanna M, et al. Tic-Related obsessive-compulsive disorder (OCD): phenomenology and treatment outcome in the pediatric OCD treatment study II. J Am Acad Child Adolesc Psychiatry. (2014) 53:1308–16. doi: 10.1016/j.jaac.2014.09.014
21. De Leeuw AS, Van Megen HJGM, Kahn RS, Westenberg HG. D-cycloserine addition to exposure sessions in the treatment of patients with obsessive-compulsive disorder. Eur Psychiatry. (2017) 40:38–44. doi: 10.1016/j.eurpsy.2016.06.011
22. Farrell LJ, Waters AM, Boschen MJ, Hattingh L, McConnell H, Milliner EL, et al. Difficult-To-Treat pediatric obsessive-compulsive disorder: feasibility and preliminary results of a randomized pilot trial of D-Cycloserine-augmented behavior therapy. Depress Anxiety. (2013) 30:723–31. doi: 10.1002/da.22132
23. Farrell LJ, Waters AM, Tiralongo E, Mathieu S, McKenzie M, Garbharran V, et al. Efficacy of D-cycloserine augmented brief intensive cognitive-behavioural therapy for paediatric obsessive-compulsive disorder: a randomised clinical trial. Depress Anxiety. (2022) 39:461–73. doi: 10.1002/da.23242
24. Foa EB, Liebowitz MR, Kozak MJ, Davies S, Campeas R, Franklin ME, et al. Randomized, placebo-controlled trial of exposure and ritual prevention, clomipramine, and their combination in the treatment of obsessive-compulsive disorder. Am J Psychiatry. (2005) 162:151–61. doi: 10.1176/appi.ajp.162.1.151
25. Foa EB, Simpson HB, Rosenfield D, Liebowitz MR, Cahill SP, Huppert JD, et al. Six-Month outcomes from a randomized trial augmenting serotonin reuptake inhibitors with exposure and response prevention or risperidone in adults with obsessive-compulsive disorder. J Clin Psychiatry. (2015) 76:440–6. doi: 10.4088/JCP.14m09044
26. Hohagen F, Winkelmann G, Rasche-Ruchle H, Hand I, König A, Münchau N, et al. Combination of behaviour therapy with fluvoxamine in comparison with behaviour therapy and placebo. Results of a multicentre study. Br J Psychiatry Suppl. (1998) 35:71–8. doi: 10.1192/S0007125000297924
27. Hu X-Z, Wen Y-S, Ma J-D, Han DM, Li YX, Wang SF, et al. A promising randomized trial of a new therapy for obsessive-compulsive disorder. Brain Behav. (2012) 2:443–54. doi: 10.1002/brb3.67
28. Kushner MG, Kim SW, Donahue C, Thuras P, Adson D, Kotlyar M, et al. D-cycloserine augmented exposure therapy for obsessive-compulsive disorder. Biol Psychiatry. (2007) 62:835–8. doi: 10.1016/j.biopsych.2006.12.020
29. Kvale G, Hansen B, Hagen K, Abramowitz JS, Børtveit T, Craske MG, et al. Effect of D-Cycloserine on the effect of concentrated exposure and response prevention in difficult-to-treat obsessive-compulsive disorder a randomized clinical trial. JAMA Netw Open. (2020) 3:e2013249. doi: 10.1001/jamanetworkopen.2020.13249
30. Mataix-Cols D, Turner C, Monzani B, Isomura K, Murphy C, Krebs G, et al. Cognitive behavioural therapy with post-session D-cycloserine augmentation for paediatric obsessive compulsive disorder: pilot randomised controlled trial. Br J Psychiatry. (2014) 204:77–8. doi: 10.1192/bjp.bp.113.126284
31. Samantaray NN, Chaudhury S, Singh P. Efficacy of inhibitory learning theory-based exposure and response prevention and selective serotonin reuptake inhibitor in obsessive-compulsive disorder management: a treatment comparison. Ind Psychiatry J. (2018) 27:53–60. doi: 10.4103/ipj.ipj_35_18
32. Simpson HB, Liebowitz MR, Foa EB, Kozak MJ, Schmidt AB, Rowan V, et al. Post-treatment effects of exposure therapy and clomipramine in obsessive-compulsive disorder. Depress Anxiety. (2004) 19:225–33. doi: 10.1002/da.20003
33. Simpson HB, Foa EB, Liebowitz MR, Huppert JD, Cahill S, Maher MJ, et al. Cognitive-Behavioral therapy vs risperidone for augmenting serotonin reuptake inhibitors in obsessive-compulsive disorder a randomized clinical trial. JAMA Psychiatry. (2013) 70:1190–8. doi: 10.1001/jamapsychiatry.2013.1932
34. Storch EA, Merlo LJ, Bengtson M, Murphy TK, Lewis MH, Yang MC, et al. D-cycloserine does not enhance exposure-response prevention therapy in obsessive-compulsive disorder. Int Clin Psychopharmacol. (2007) 22:230–7. doi: 10.1097/YIC.0b013e32819f8480
35. Storch EA, Murphy TK, Goodman WK, Geffken GR, Lewin AB, Henin A, et al. A preliminary study of d-cycloserine augmentation of cognitive-behavioral therapy in pediatric obsessive-compulsive disorder. Biol Psychiatry. (2010) 68:1073–6. doi: 10.1016/j.biopsych.2010.07.015
36. Storch EA, Bussing R, Small BJ, Geffken GR, McNamara JP, Rahman O, et al. Randomized, placebo-controlled trial of cognitive-behavioral therapy alone or combined with sertraline in the treatment of pediatric obsessive-compulsive disorder. Behav Res Ther. (2013) 51:823–9. doi: 10.1016/j.brat.2013.09.007
37. Storch EA, Wilhelm S, Sprich S, Henin A, Micco J, Small BJ, et al. Efficacy of augmentation of cognitive behavior therapy with weight-adjusted d-cycloserine vs placebo in pediatric obsessive-compulsive disorder a randomized clinical trial. JAMA Psychiatry. (2016) 73:779–88. doi: 10.1001/jamapsychiatry.2016.1128
38. Tenneij NH, Van Megen H, Denys D, Westenberg HG. Behavior therapy augments response of patients with obsessive-compulsive disorder responding to drug treatment. J Clin Psychiatry. (2005) 66:1169–75. doi: 10.4088/JCP.v66n0913
39. Zemestani M, Salavati M, Seyedolshohadayi A, Petersen JM, Ong CW, Twohig MP, et al. A preliminary examination of acceptance and commitment therapy versus exposure and response prevention for patients with obsessive-compulsive disorder on an optimal dose of ssris: a randomized controlled trial in Iran. Behav Modif. (2022) 46:553–80. doi: 10.1177/0145445520982977
40. Fullana MA, Zhu X, Alonso P, Real E, López-Solà C, Segalàs C, et al. Basolateral amygdala-ventromedial prefrontal cortex connectivity predicts cognitive behavioural therapy outcome in adults with obsessive-compulsive disorder. J Psychiatry Neurosci. (2017) 42:378–85. doi: 10.1503/jpn.160215
41. Bijanki KR, Pathak YJ, Najera RA, Storch EA, Goodman WK, Simpson HB, et al. Defining functional brain networks underlying obsessive-compulsive disorder (OCD) using treatment-induced neuroimaging changes: a systematic review of the literature. J Neurol Neurosurg Psychiatry. (2021) 92:776–86. doi: 10.1136/jnnp-2020-324478
42. Correll CU, Cortese S, Croatto G, Monaco F, Krinitski D, Arrondo G, et al. Efficacy and acceptability of pharmacological, psychosocial, and brain stimulation interventions in children and adolescents with mental disorders: an umbrella review. World Psychiatry. (2021) 20:244–75. doi: 10.1002/wps.20881
43. Skapinakis P, Caldwell D, Hollingworth W, Bryden P, Fineberg N, Salkovskis P, et al. A systematic review of the clinical effectiveness and cost-effectiveness of pharmacological and psychological interventions for the management of obsessive-compulsive disorder in children/adolescents and adults. Health Technol Assess. (2016) 20:1–392. doi: 10.3310/hta20430
44. Xia J, Du Y, Han J, Liu G, Wang X. D-cycloserine augmentation in behavioral therapy for obsessive-compulsive disorder: a meta-analysis. Drug Des Devel Ther. (2015) 9:2101–17. doi: 10.2147/DDDT.S68994
45. Levy HC, Radomsky AS. Safety behaviour enhances the acceptability of exposure. Cogn Behav Ther. (2014) 43:83–92. doi: 10.1080/16506073.2013.819376
46. Ruscio AM, Stein DJ, Chiu WT, Kessler RC. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry. (2010) 15:53–63. doi: 10.1038/mp.2008.94
47. Brakoulias V, Starcevic V, Belloch A, Brown C, Ferrao YA, Fontenelle LF, et al. Comorbidity, age of onset and suicidality in obsessive-Compulsive disorder (OCD): an international collaboration. Compr Psychiatry. (2017) 76:79–86. doi: 10.1016/j.comppsych.2017.04.002
48. Roshanaei-Moghaddam B, Pauly MC, Atkins DC, Baldwin SA, Stein MB, Roy-Byrne P, et al. Relative effects of CBT and pharmacotherapy in depression versus anxiety: is medication somewhat better for depression, and CBT somewhat better for anxiety? Depress Anxiety. (2011) 28:560–7. doi: 10.1002/da.20829
49. Zandberg LJ, Zang Y, Mclean CP, Yeh R, Simpson HB, Foa EB. Change in obsessive-compulsive symptoms mediates subsequent change in depressive symptoms during exposure and response prevention. Behav Res Ther. (2015) 68:76–81. doi: 10.1016/j.brat.2015.03.005
50. Matsumoto K, Hamatani S, Makino T, Takahashi J, Suzuki F, Ida T, et al. Guided internet-based cognitive behavioral therapy for obsessive-compulsive disorder: a multicenter randomized controlled trial in Japan. Internet Interv. (2022) 28:100515. doi: 10.1016/j.invent.2022.100515
51. Brakoulias V, Stockings E. A systematic review of the use of risperidone, paliperidone and aripiprazole as augmenting agents for obsessive-compulsive disorder. Expert Opin Pharmacother. (2019) 20:47–53. doi: 10.1080/14656566.2018.1540590
52. Bandeira ID, Lins-Silva DH, Cavenaghi VB, Dorea-Bandeira I, Faria-Guimarães D, Barouh JL, et al. Ketamine in the treatment of obsessive-compulsive disorder: a systematic review. Harv Rev Psychiatry. (2022) 30:135–45. doi: 10.1097/HRP.0000000000000330
53. Vakili Y, Gharaee B, Habibi M. Acceptance and commitment therapy, selective serotonin reuptake inhibitors and their combination in the improvement of obsessive-compulsive symptoms and experiential avoidance in patients with obsessive-compulsive disorder. Iran J Psychiatry Behav Sci. (2015) 9:e845. doi: 10.17795/ijpbs845
Keywords: exposure response prevention, obsessive-compulsive disorder, D-cycloserine, selective serotonin reuptake inhibitors, SSRIs, drug treatment, medication, meta-analysis
Citation: Mao L, Hu M, Luo L, Wu Y, Lu Z and Zou J (2022) The effectiveness of exposure and response prevention combined with pharmacotherapy for obsessive-compulsive disorder: A systematic review and meta-analysis. Front. Psychiatry 13:973838. doi: 10.3389/fpsyt.2022.973838
Received: 20 June 2022; Accepted: 22 August 2022;
Published: 15 September 2022.
Edited by:
Angela Fang, University of Washington, United StatesReviewed by:
Michael Grady Wheaton, Columbia University, United StatesCopyright © 2022 Mao, Hu, Luo, Wu, Lu and Zou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maorong Hu, bWFyb24xM0AxMjYuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.